Estrogen therapy is highly effective in the treatment of hot flashes among postmenopausal women. For postmenopausal women with a uterus, estrogen treatment for hot flashes is almost always combined with a progestin to reduce the risk of endometrial polyps, hyperplasia, and cancer. For instance, in the Postmenopausal Estrogen/Progestin Interventions Trial, 62% of the women with a uterus treated with conjugated equine estrogen (CEE) 0.625 mg daily without a progestin developed endometrial hyperplasia.1
In the United States, the most commonly prescribed progestin for hormone therapy has been medroxyprogesterone acetate (MPA; Provera). However, data from the Women’s Health Initiative (WHI) trials indicate that MPA, when combined with CEE, may have adverse health effects among postmenopausal women.
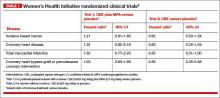
Among women 50 to 59 years of age with a uterus, the combination of CEE plus MPA was associated with a trend toward an increased risk of breast cancer, coronary heart disease, and myocardial infarction.2 In contrast, among women 50 to 59 years of age without a uterus, CEE monotherapy was associated with a trend toward a decreased risk of invasive breast cancer, coronary heart disease, and myocardial infarction (TABLE 1).
Among women 50 to 79 years of age with a uterus, the combination of CEE plus MPA was associated with a significantly increased risk of breast cancer (hazard ratio [HR], 1.24; 95% confidence interval [CI], 1.01–1.53; P = .04).2 In contrast, among women 50 to 79 years of age without a uterus, CEE monotherapy was associated with a trend toward a decreased risk of breast cancer (HR, 0.79; 95% CI, 0.61–1.02, P = .07).2
Related article: In the latest report from the WHI, the data contradict the conclusions. Holly Thacker, MD (Commentary; March 2014)
When the analysis was limited to women consistently adherent to their CEE monotherapy, the estrogen treatment significantly decreased the risk of invasive breast cancer (HR, 0.67; 95% CI, 0.47–0.97; P = .03).3
The addition of MPA to CEE appears to reverse some of the health benefits of CEE monotherapy, although the biological mechanisms are unclear. This observation should prompt us to explore alternative and novel treatments of vasomotor symptoms that do not utilize MPA. Some options for MPA-free hormone therapy include:
- transdermal estradiol plus micronized progesterone
- CEE plus a levonorgestrel-releasing intrauterine system
- bazedoxifene plus CEE.
In addition, nonhormonal treatment of hot flashes is an option, with selective serotonin reuptake inhibitors (SSRIs).
Related article: Is one oral estrogen formulation safer than another for menopausal women? Andrew M. Kaunitz, MD (Examining the Evidence; January 2014)
When using an estrogen plus progestin regimen to treat hot flashes, many experts favor a combination of low-dose transdermal estradiol and oral micronized progesterone (Prometrium). This combination is believed by some experts to result in a lower risk of venous thromboembolism, stroke, cardiovascular disease, and breast cancer than an estrogen-MPA combination.4–7
When prescribing transdermal estradiol plus oral micronized progesterone for a woman within 1 to 2 years of her last menses, a cyclic regimen can help reduce episodes of irregular, unscheduled uterine bleeding. I often use this cyclic regimen: transdermal estradiol 0.0375 mg plus cyclic oral micronized progesterone 200 mg prior to bedtime for calendar days 1 to 12.
When using transdermal estradiol plus oral micronized progesterone in a woman more than 2 years from her last menses, a continuous regimen is often prescribed. I often use this continuous regimen: transdermal estradiol 0.0375 mg plus continuous oral micronized progesterone 100 mg daily prior to bedtime.
Related article: When should a menopausal woman discontinue hormone therapy? Andrew M. Kaunitz, MD (Cases in Menopause; February 2014)
Estrogen plus a levonorgestrel-releasing intrauterine systemThe levonorgestrel intrauterine system (LNG-IUS; 20 µg daily; Mirena) is frequently used in Europe to protect the endometrium against the adverse effects of estrogen therapy in postmenopausal women. In a meta-analysis of five clinical trials involving postmenopausal women, the LNG-IUS provided excellent protection against endometrial hyperplasia, compared with MPA.8
One caution about using the LNG-IUS system with estrogen in postmenopausal women is that an observational study of all women with breast cancer in Finland from 1995 through 2007 reported a significantly increased risk of breast cancer among postmenopausal women using an LNG-IUS compared with women who did not use hormones or used only estrogen because they had a hysterectomy (TABLE 2).9 This study was not a randomized clinical trial and patients at higher baseline risk for breast cancer, including women with a high body mass index, may have been preferentially treated with an LNG-IUS. More information is needed to better understand the relationship between the LNG-IUS and breast cancer in postmenopausal women.
Related article: What we’ve learned from 2 decades’ experience with the LNG-IUS. Q&A with Oskari Heikinheimo, MD, PhD (February 2011)
Progestin-free hormone treatment, bazedoxifene plus CEE
The main reason for adding a progestin to estrogen therapy for vasomotor symptoms in postmenopausal women with a uterus is to prevent estrogen-induced development of endometrial polyps, hyperplasia, and cancer. A major innovation in hormone therapy is the discovery that third-generation selective estrogen receptor modulators (SERMs), such as bazedoxifene (BZA), can prevent estrogen-induced development of endometrial polyps, hyperplasia, and cancer but do not interfere with the efficacy of estrogen in the treatment of vasomotor symptoms.
BZA is an estrogen agonist in bone and an estrogen antagonist in the endometrium.10–12 The combination of BZA (20 mg daily) plus CEE (0.45 mg daily) (Duavee) is approved for the treatment of moderate to severe vasomotor symptoms and prevention of osteoporosis.13–15 Over 24 months of therapy, various doses of BZA plus CEE reduced reported daily hot flashes by 52% to 86%.16 In the same study, placebo treatment was associated with a 17% reduction in hot flashes.16
The main adverse effect of BZA/CEE is an increased risk of deep venous thrombosis. Therefore, BZA/CEE is contraindicated in women with a known thrombophilia or a personal history of hormone-induced deep venous thrombosis. The effect of BZA/CEE on the risk of developing invasive breast cancer is not known; over 52 weeks of therapy it did not increase breast density on mammogram.17,18
BZA/CEE is a remarkable advance in hormone therapy. It is progestin-free, uses estrogen to treat vasomotor symptoms, and uses BZA to protect the endometrium against estrogen-induced hyperplasia.
Related article: New option for treating menopausal vasomotor symptoms receives FDA approval. (News for your Practice; October 2013)
Nonhormone treatment of vasomotor symptoms Paroxetine mesylateFor postmenopausal women with vasomotor symptoms who cannot take estrogen, SSRIs are modestly effective in reducing moderate to severe hot flashes. The US Food and Drug Administration recently approved paroxetine mesylate (Brisdelle) for the treatment of postmenopausal vasomotor symptoms. The approved dose is 7.5 mg daily taken at bedtime.
Data supporting the efficacy of paroxetine mesylate are available from two studies involving 1,184 menopausal women with vasomotor symptoms randomly assigned to receive paroxetine 7.5 mg daily or placebo for 12 weeks of treatment.19-22 In one of the two clinical trials, women treated with paroxetine mesylate 7.5 mg daily had 5.6 fewer moderate to severe hot flashes daily after 12 weeks of treatment compared with 3.9 fewer hot flashes with placebo (median treatment difference, 1.7; P<.001).21