“Canst thou not minister to a mind diseased, pluck from the memory a rooted sorrow, raze out the written troubles of the brain, and with some sweet oblivious antidote cleanse the stuffed bosom of that perilous stuff which weighs upon the heart?”
– William Shakespeare, Macbeth
For many years, the United States has been experiencing a shortage of psychiatrists. Currently, there are only 28,000 to 33,000 psychiatrists in active patient care practice in the United States.1,2 The lack of psychiatrists is pronounced in many areas of the country, including rural regions, some urban neighborhoods, and community health centers. In approximately half of US counties, there are no psychiatrists at all.3
While patients with mental illnesses often are treated in primary care settings, the need for qualified mental health clinicians remains acute. Two-thirds of primary care physicians report difficulty in referring patients for mental health care, due to the shortage of clinicians and long wait times for patients to be seen.4 In the Department of Veterans Affairs (VA), the shortage of qualified psychiatrists is even more acute, due to ongoing combat operations and an increased number of missions and manpower requirements to complete them, which also has increased veterans’ mental health needs during life after their service.5
The outlook for providing adequate numbers of psychiatrists in the future is even more concerning. Based on a population analysis, Satiani et al6 predicts an extreme shortage of psychiatrists for the next 30 years, with the availability of psychiatrists per population expected to reach an all-time low by 2024. Based on ratios from the Department of Health and Human Services, this would mean a shortage of 14,000 to 31,000 psychiatrists over the next 5 to 6 years alone. This is due primarily to the expected retirement of more than 25,000 psychiatrists age >55 during the next 5 years. With mental illness becoming the costliest medical condition in the United States, at $201 billion annually, the potential impact of this shortage is alarming.6
Addressing the shortage
Efforts aimed at increasing the number of psychiatrists, improving access to care, and improving efficiency of care have focused on expanding recruitment and training capacity in psychiatry residency programs, utilizing new models such as telepsychiatry and Assertive Community Treatment (ACT) teams, increasing the number of Certified Community Behavioral Health Clinics, and embedding psychiatrists in large primary care practices.7 Another avenue for addressing the psychiatrist shortage has been the training and hiring of more advanced practice clinicians, including physician assistants (PAs) and nurse practitioners (NPs). Approximately 11,000 PAs and NPs specialize in psychiatry in the United States; this number represents more than one-third of the current psychiatrist workforce. This substantially adds to the available mental health professionals who can assess, monitor, and treat mental health conditions, and creates an opportunity for further growth to help make up for the expected shortfall of psychiatrists. In an analysis of a data set that included information on 90% of physician practices in the United States, Martsolf et al8 found that in 2016, 28% of specialty practices employed advanced practice clinicians.
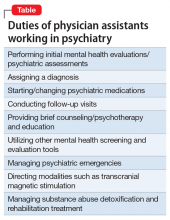
Physician assistants and NPs make up the largest group of non-physician mental health professionals who can prescribe medications. Physician assistant training is most closely aligned with the allopathic training model of physicians.9 Some typical duties of PAs working in a psychiatric setting are outlined in the Table.
How many PAs elect to specialize in psychiatry, compared with the percentage of physicians who choose psychiatry as a career? Data from the National Commission on Certification of Physician Assistants (NCCPA) revealed that in 2018 there were 1,470 PAs working in psychiatry, or approximately 1.5% of all PAs in practice.10 In comparison, approximately 5% of physicians complete residency training in psychiatry.2
Continue to: Although the need for more...