When used to treat anxiety or depressive disorders, antidepressants can cause a variety of adverse effects, including emotional blunting. Emotional blunting has been described as emotional numbness, indifference, decreased responsiveness, or numbing. In a study of 669 patients who had been receiving antidepressants (selective serotonin reuptake inhibitors [SSRIs], serotonin-norepinephrine reuptake inhibitors [SNRIs], or other antidepressants), 46% said they had experienced emotional blunting.1 A 2019 study found that approximately one-third of patients with unipolar depression or bipolar depression stopped taking their antidepressant due to emotional blunting.2
Historically, there has been difficulty parsing out emotional blunting (a general decrease of all range of emotions) from anhedonia (a restriction of positive emotions). Additionally, some researchers have questioned if the blunting of emotions is part of depressive symptomatology. In a study of 38 adults, most felt able to differentiate emotional blunting due to antidepressants by considering the resolution of other depressive symptoms and timeline of onset.3
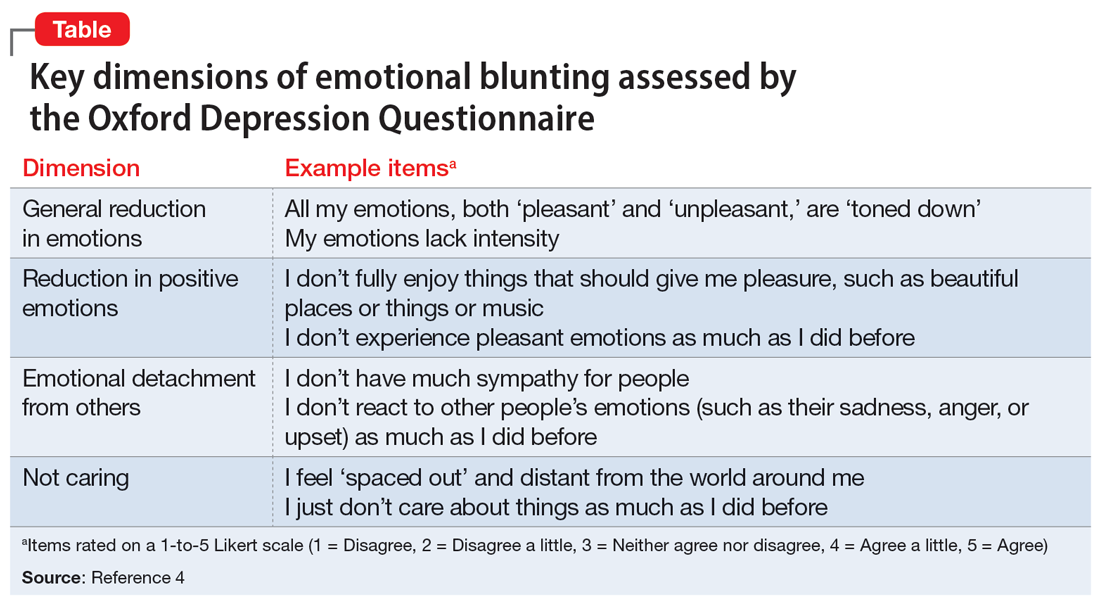
A significant limitation has been how clinicians measure or assess emotional blunting. The Oxford Depression Questionnaire (ODQ), previously known as the Oxford Questionnaire on the Emotional Side-effects of Antidepressants, was created based on a qualitative survey of patients who endorsed emotional blunting.4 A validated scale, the ODQ divides emotional blunting into 4 dimensions:
- general reduction in emotions
- reduction in positive emotions
- emotional detachment from others
- not caring.4
The sections of ODQ focus on exploring specific aspects of patients’ emotional experiences, comparing experiences in the past week to before the development of illness/emotional blunting, and patients’ opinions about antidepressants. Example statements from the ODQ (Table4) may help clinicians better understand and explore emotional blunting with their patients.
There are 2 leading theories behind the mechanism of emotional blunting on antidepressants, both focused on serotonin. The first theory offers that SSRIs alter frontal lobe activity through serotonergic effects. The second theory is focused on the downward effects of serotonin on dopamine in reward pathways.5
Treatment options: Limited evidence
Data on how to address antidepressant-induced emotional blunting are limited and based largely on case reports. One open-label study (N = 143) found that patients experiencing emotional blunting while taking SSRIs and SNRIs who were switched to vortioxetine had a statistically significant decrease in ODQ total score; 50% reported no emotional blunting.6 Options to address emotional blunting include decreasing the antidepressant dose, augmenting with or switching to another agent, or considering other treatments such as neuromodulation.5 Further research is necessary to clarify which intervention is best.
Clinicians will encounter emotional blunting in patients who are taking antidepressants. It is important to recognize and address these symptoms to help improve patients’ adherence and overall quality of life.