BOSTON – Medical marijuana is now legal in 23 states, but there remains essentially no systematic approach for evaluating whether available products have the capacity to provide medical benefits, according to a status report presented at the International Conference on Opioids.
Often, medical marijuana is marketed on the basis of its psychoactive component, tetrahydrocannabinol (THC), but a substantial body of data suggests that it is the cannabidiol (CBD) content that is most responsible for appetite stimulation, antiemetic effects, and many other medicinal properties, according to Michael E. Schatman, Ph.D., executive director of the Foundation for Ethics in Pain Care, Bellevue, Wash.
“Contrary to popular belief, THC is not the most relevant cannabinoid for medical application,” Dr. Schatman said. On the premise that more is better, higher THC content generally correlates with higher cost for medical marijuana as it does for marijuana marketed for recreational use, according to Dr. Schatman. But he disagreed with that notion.
More than 100 cannabinoids are in marijuana, Dr. Schatman said. Although he maintained that CBD might be the most important constituent for many of the medicinal indications for marijuana, he acknowledged that the data are mostly suggestive. Few studies have differentiated marijuana for its therapeutic effects based on representative concentrations of different constituents even if Dr. Schatman cited clinical and experimental work correlating CBD with benefit on a variety of therapeutic targets, including inflammation.
“There is no medical marijuana but medical marijuanas,” said Dr. Schatman, suggesting that specific therapeutic benefits would be expected to differ markedly according to the constituents even if little information exists about the optimal levels of any of these constituents.
For recreational use, THC content is a reasonable quality metric, Dr. Schatman said. THC content predicts the “high” of marijuana. While inducing a state of euphoria might indeed be the goal for some medicinal marijuana applications, high THC content also poses the greatest risk of psychosis, disordered thoughts, and impaired functionality, he said. To this extent, greater THC content might not predict greater benefit.
In the absence of regulatory oversight, the marketing of marijuana rather than the science of its effect dominates all discussion, Dr. Schatman said. He cited data showing a steep increase in THC content subsequent to the growing rate of state legalizations.
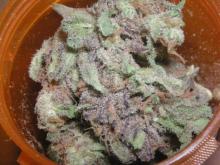
“Dispensaries are selling medical marijuana with THC contents as high as 33% with names like Super Brain Damage OG,” Dr. Schatman said. Given the potential for unwanted side effects at THC dose levels likely to impair cognitive function, Dr. Schatman said it might be reasonable to question the therapeutic intent when products feature THC content at levels this high.
So far, only New Jersey has restricted THC content of medical marijuana, placing the ceiling at 10%, Dr. Schatman said. Compared to the 1970s, when street marijuana typically had THC content of about 1% to 2%, Dr. Schatman suggested that even 10% is likely to be excessive if the goal is not be get “stoned.” However, he expressed even greater concern about the declining content of CBD, which he suggested has been inversely related to THC.
“We’ve essentially bred the CBD out of marijuana,” Dr. Schatman reported. One advertisement from a medical marijuana dispensary that he reproduced prominently advertised THC levels at 20% but CBD levels at 0.38%. Whether greater medicinal benefits would be realized if those percentages were reversed is not known, but Dr. Schatman said rational clinical decisions are impossible without data.
“Until the patient knows what he or she is getting, cannabis will not necessarily be medicine in most cases,” Dr. Schatman said. He believes the marijuana should be held to the same standards of efficacy and safety as other drugs. The ideal for moving this field forward might be regulation by the Food and Drug Administration, Dr. Schatman said. But he also called for more rigorous trials of the marijuana constituents to determine which are most important for achieving the specific benefits for which marijuana is being prescribed.
Dr. Schatman is on the speaker’s bureau for Mallinckrodt.