ISTANBUL – Systemic sclerosis overlap syndromes follow a path of disease progression distinctly different from that of limited or diffuse cutaneous systemic sclerosis, according to a new analysis from the German Network for Systemic Scleroderma.
"This study shows for the first time that patients suffering from systemic sclerosis overlap syndromes should be viewed as a distinct systemic sclerosis subset," Dr. Pia Moinzadeh noted at the annual congress of the European Academy of Dermatology and Venereology.
Those with systemic sclerosis overlap syndromes (SSc-OS) are a heterogeneous subgroup of patients who have the clinical features of SSc according to American College of Rheumatology criteria simultaneously with the characteristic findings of at least one other connective tissue disease, such as dermatomyositis, Sjögren’s syndrome, rheumatoid arthritis, or lupus erythematosus.
The registry of the German Network for Systemic Scleroderma is a uniquely large and inclusive ongoing prospective data base directed by a joint committee of dermatologists and rheumatologists. More than 6 years ago, when the investigators realized that a sizable fraction of patients enrolled in the national registry didn’t fit within the classic bimodal SSc categorization scheme composed of two subtypes – limited cutaneous and diffuse cutaneous SSc – they proposed three additional SSc subtypes. These are SSc-OS, undifferentiated scleroderma, and sclerosis sine scleroderma.
The focus of Dr. Moinzadeh’s EADV presentation was on SSc-OS. Of 3,240 SSc patients in the German registry, patients with OS comprise 11%, while those with limited cutaneous SSc make up 43%, those with diffuse cutaneous disease account for 31%, and the remainder of patients have undifferentiated scleroderma or sclerosis sine scleroderma.
The validity of the SSc-OS diagnostic construct has been controversial. Some experts have contended that patients with SSc-OS ought to be lumped under the headings of limited cutaneous SSc or diffuse cutaneous SSc, depending on the extent of skin involvement. However, the unparalleled size, inclusiveness, and long-term prospective follow-up provided by the German registry have resulted in evidence that argues to the contrary, according to Dr. Moinzadeh, a rheumatologist at the University of Cologne (Germany).
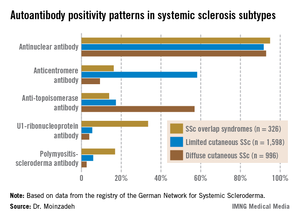
She reported on 326 patients with SSc-OS, 1,598 with limited cutaneous SSc, and 996 with diffuse cutaneous SSc prospectively followed through the German registry for a mean of 10.1 years. The follow-up data indicate SSc-OS evolves differently from either limited cutaneous SSc or diffuse cutaneous SSc. It also displays a distinctive pattern of organ involvement and autoantibody positivity, she noted.
The group with SSc-OS had a mean modified Rodnan skin score of 6.7, similar to the 7.2 score in the limited cutaneous SSc group and markedly less than the 15.8 in the diffuse cutaneous SSc patients. While this might suggest that patients with SSc-OS have a milder course of disease comparable to limited cutaneous SSc, in fact they progressed more rapidly, with earlier and more widespread significant organ involvement and a higher disease burden than the limited cutaneous SSc group, according to Dr. Moinzadeh.
Patients with SSc-OS developed musculoskeletal involvement far more frequently than others. Sixty-seven percent were affected, compared with 38% of patients with limited cutaneous SSc and 48% with diffuse cutaneous SSc. The patients in the SSc-OS group also developed musculoskeletal involvement earlier.
Lung fibrosis occurred in 38% of patients with SSc-OS, 27% of patients with limited cutaneous SSc, and 63% with diffuse cutaneous SSc. Cardiac involvement occurred in 15% with SSc-OS, 10% with limited cutaneous SSc, and 19% with diffuse cutaneous SSc. The onset of these manifestations of SSc in the SSc-OS subgroup was significantly earlier than in the limited cutaneous SSc patients but later than with diffuse cutaneous SSc.
Progression to esophageal and renal involvement, as well as pulmonary arterial hypertension, in the SSc-OS group occurred significantly earlier than in the limited cutaneous SSC patients, but again was later than with diffuse cutaneous SSC.
The autoantibody status of the three subgroups showed distinct differences (see graphic).
The German Network for Systemic Scleroderma is funded by the German Federal Ministry of Education and Research. Dr. Moinzadeh reported having no financial conflicts.