Rheumatologists should consider the possibility of Chikungunya virus in patients who present with new symmetric polyarthritis, especially if they have just returned from an endemic region such as the Caribbean, according to researchers.
In their paper, first authors Dr. Jonathan J. Miner and Dr. Han-Xian Aw-Yeang and colleagues at Washington University, St. Louis, describe a cohort of 10 Americans who traveled to Haiti within a 20-day period in June 2014 and became infected with Chikungunya virus (CHIKV), an arthritogenic, mosquito-transmitted alphavirus (Arthritis Rheumatol. 2015 Jan. 20 [doi:10.1002/art.39027]).
The virus spread to the Caribbean in 2013 and the United States in 2014. Its acute phase of infection includes symptoms such as fever, headache, rash, arthralgia, arthritis, and myalgia.
The virus is likely to become a unique diagnostic challenge for rheumatologists as the arthritis symptoms mimic seronegative arthritis, the researchers said.
“Eight out of these patients would have met the 2010 ACR/EULAR criteria for RA [rheumatoid arthritis] if the initial fever, rash, and travel to the Caribbean had not been revealed,” they noted.
Most of the patients had joint pain and morning stiffness at least 8 weeks after initial infection, although some reported gradual improvement of their symptoms, the investigators reported.
One of the patients developed fever; diffuse arthritis; an erythematous, maculopapular rash; and severe symmetric polyarthritis that persisted more than 5 months post infection. She was treated with prednisolone but it exacerbated her joint pain and treatment was stopped.
The other patient detailed in the report presented with similar symptoms. His fever and rash resolved within 2 days but his arthritis symptoms persisted. He was treated with NSAIDs that provided only minimal relief.
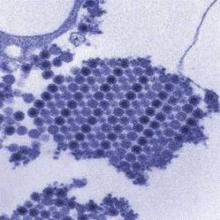
To understand more about the immunologic parameters of the virus, the researchers used cytometry by time of flight to compare the peripheral mononuclear cells from CHIKV-infected patients with those of healthy controls and untreated patients with RA.
They discovered that naive, activated, and effector T killer– and T helper–cell populations occurred in similar percentages in the virus-infected patients and RA patients but not in the healthy controls.
The RA patients, however, had a higher expression of L-selectin expression in CD4+ T cells than did either virus-infected patients or healthy controls.
“These data suggest that lymphocyte phenotypes in patients with Chikungunya infection are similar to each other, with subtle but distinct trends that could potentially distinguish these two groups from healthy controls and from each other,” Dr. Miner and Dr. Aw-Yeang and their associates wrote.
Whether treatment with disease-modifying antirheumatic drugs or biologics used in RA is appropriate or effective is controversial in the absence of randomized controlled trials for CHIKV-related arthritis, they said.
“Immunosuppression in CHIKV-infected patients could be deleterious because viral RNA and antigens can be found in target tissues in the chronic phase in humans and experimental animals,” the authors wrote.
“Rheumatologists, even in non-CHIKV-endemic regions, need to consider CHIKV in their evaluation of symmetric polyarthritis lasting more than 6 weeks by obtaining a history of travel to CHIKV-endemic regions, which are likely to expand in the near future,” the investigators advised.
Patients who may have been exposed to the virus may need serologic testing before initiating immunosuppression, they said.
“Unfortunately, access to CHIKV testing is highly constrained at the current time as it is only available from the [Centers for Disease Control and Prevention] and research laboratories,” they added.
The study was supported by the Barnes-Jewish Hospital Foundation and the Howard Hughes Medical Institute. The authors reported no conflicts of interest.