User login
Are ObGyns knowledgeable about the risk factors for hepatitis C virus in pregnancy?
The American College of Obstetricians and Gynecologists (ACOG) recommends risk-based screening for hepatitis C virus (HCV) infection during pregnancy.1 However, the prevalence of HCV among pregnant women in the United States is on the rise. From 2009 to 2014, HCV infection present at delivery increased 89%.2 In addition, the risk of an HCV-infected mother transmitting the infection to her baby is about 4% to 7% per pregnancy.3 Currently, the Infectious Diseases Society of America and the American Association for the Study of Liver Diseases recommend universal HCV screening in pregnancy.4
Researchers at Tufts Medical Center in Boston, Massachusetts, a tertiary care center, presented survey findings on HCV screening among ObGyns at ACOG’s 2019 Annual Clinical and Scientific Meeting in Nashville, Tennessee.5 Katherine G. Koniares, MD, and colleagues sought to assess the opinions and clinical practices of ObGyns by emailing a 10-question electronic survey to providers. A total of 38 of 41 providers (93%) responded to the survey.
Survey results show lack of knowledge on risk factors
In response to the question, “Which pregnant patients do you believe should be screened for HCV,” 43.2% of providers stated “all pregnant women,” while 54.1% said “only pregnant women with risk factors for HCV.” A small percentage (2.7%) responded that they were not sure.
Providers also were asked which patients in their practice they screen for HCV. In response, 77.8% stated that they screen pregnant women for HCV based on risk factors, while 13.9% screen all pregnant patients for HCV; 8.3% do not screen for HCV.
When asked which risk factors providers use to screen patients for HCV, 42% to 85% said they screen for each indicated risk factor. Only 36% of providers, however, correctly identified all risk factors (for example, receiving blood products from donors who later tested positive for HCV; unexplained liver disease; and percutaneous/parenteral exposures in an unregulated setting, such as receiving tattoos outside a licensed parlor).
Further study needed on universal screening
The researchers assert that risk-based screening for HCV is not effective and that further research on universal HCV screening in pregnant patients is needed.
- American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 86: Viral hepatitis in pregnancy. Obstet Gynecol. 2007;110:941-956.
- Patrick SW, Bauer AM, Warren MD, et al. Hepatitis C virus infection among women giving birth—Tennessee and the United States, 2009-2014. MMWR Morbid Mortal Weekly Rep. 2017;66:470-473.
- Koneru A, Nelson N, Hariri S, et al. Increased hepatitis C virus (HCV) detection in women of childbearing age and potential risk for vertical transmission—United States and Kentucky, 2011-2014. MMWR Morbid Mortal Weekly Rep. 2016;65:705-710.
- American Association for the Study of Liver Diseases (AASLD) and the Infectious Diseases Society of America (IDSA). Recommendations for testing, management, and treating, hepatitis C. HCV testing and linkage to care. https://www.hcvguidelines.org/.
- Koniares KG, Fadlallah H, Kolettis DS, et al. A survey of hepatitis C virus (HCV) screening in pregnancy among ObGyns at a tertiary care center. Poster presented at: American College of Obstetricians and Gynecologists Annual Clinical and Scientific Meeting; May 3-6, 2019; Nashville, TN.
The American College of Obstetricians and Gynecologists (ACOG) recommends risk-based screening for hepatitis C virus (HCV) infection during pregnancy.1 However, the prevalence of HCV among pregnant women in the United States is on the rise. From 2009 to 2014, HCV infection present at delivery increased 89%.2 In addition, the risk of an HCV-infected mother transmitting the infection to her baby is about 4% to 7% per pregnancy.3 Currently, the Infectious Diseases Society of America and the American Association for the Study of Liver Diseases recommend universal HCV screening in pregnancy.4
Researchers at Tufts Medical Center in Boston, Massachusetts, a tertiary care center, presented survey findings on HCV screening among ObGyns at ACOG’s 2019 Annual Clinical and Scientific Meeting in Nashville, Tennessee.5 Katherine G. Koniares, MD, and colleagues sought to assess the opinions and clinical practices of ObGyns by emailing a 10-question electronic survey to providers. A total of 38 of 41 providers (93%) responded to the survey.
Survey results show lack of knowledge on risk factors
In response to the question, “Which pregnant patients do you believe should be screened for HCV,” 43.2% of providers stated “all pregnant women,” while 54.1% said “only pregnant women with risk factors for HCV.” A small percentage (2.7%) responded that they were not sure.
Providers also were asked which patients in their practice they screen for HCV. In response, 77.8% stated that they screen pregnant women for HCV based on risk factors, while 13.9% screen all pregnant patients for HCV; 8.3% do not screen for HCV.
When asked which risk factors providers use to screen patients for HCV, 42% to 85% said they screen for each indicated risk factor. Only 36% of providers, however, correctly identified all risk factors (for example, receiving blood products from donors who later tested positive for HCV; unexplained liver disease; and percutaneous/parenteral exposures in an unregulated setting, such as receiving tattoos outside a licensed parlor).
Further study needed on universal screening
The researchers assert that risk-based screening for HCV is not effective and that further research on universal HCV screening in pregnant patients is needed.
The American College of Obstetricians and Gynecologists (ACOG) recommends risk-based screening for hepatitis C virus (HCV) infection during pregnancy.1 However, the prevalence of HCV among pregnant women in the United States is on the rise. From 2009 to 2014, HCV infection present at delivery increased 89%.2 In addition, the risk of an HCV-infected mother transmitting the infection to her baby is about 4% to 7% per pregnancy.3 Currently, the Infectious Diseases Society of America and the American Association for the Study of Liver Diseases recommend universal HCV screening in pregnancy.4
Researchers at Tufts Medical Center in Boston, Massachusetts, a tertiary care center, presented survey findings on HCV screening among ObGyns at ACOG’s 2019 Annual Clinical and Scientific Meeting in Nashville, Tennessee.5 Katherine G. Koniares, MD, and colleagues sought to assess the opinions and clinical practices of ObGyns by emailing a 10-question electronic survey to providers. A total of 38 of 41 providers (93%) responded to the survey.
Survey results show lack of knowledge on risk factors
In response to the question, “Which pregnant patients do you believe should be screened for HCV,” 43.2% of providers stated “all pregnant women,” while 54.1% said “only pregnant women with risk factors for HCV.” A small percentage (2.7%) responded that they were not sure.
Providers also were asked which patients in their practice they screen for HCV. In response, 77.8% stated that they screen pregnant women for HCV based on risk factors, while 13.9% screen all pregnant patients for HCV; 8.3% do not screen for HCV.
When asked which risk factors providers use to screen patients for HCV, 42% to 85% said they screen for each indicated risk factor. Only 36% of providers, however, correctly identified all risk factors (for example, receiving blood products from donors who later tested positive for HCV; unexplained liver disease; and percutaneous/parenteral exposures in an unregulated setting, such as receiving tattoos outside a licensed parlor).
Further study needed on universal screening
The researchers assert that risk-based screening for HCV is not effective and that further research on universal HCV screening in pregnant patients is needed.
- American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 86: Viral hepatitis in pregnancy. Obstet Gynecol. 2007;110:941-956.
- Patrick SW, Bauer AM, Warren MD, et al. Hepatitis C virus infection among women giving birth—Tennessee and the United States, 2009-2014. MMWR Morbid Mortal Weekly Rep. 2017;66:470-473.
- Koneru A, Nelson N, Hariri S, et al. Increased hepatitis C virus (HCV) detection in women of childbearing age and potential risk for vertical transmission—United States and Kentucky, 2011-2014. MMWR Morbid Mortal Weekly Rep. 2016;65:705-710.
- American Association for the Study of Liver Diseases (AASLD) and the Infectious Diseases Society of America (IDSA). Recommendations for testing, management, and treating, hepatitis C. HCV testing and linkage to care. https://www.hcvguidelines.org/.
- Koniares KG, Fadlallah H, Kolettis DS, et al. A survey of hepatitis C virus (HCV) screening in pregnancy among ObGyns at a tertiary care center. Poster presented at: American College of Obstetricians and Gynecologists Annual Clinical and Scientific Meeting; May 3-6, 2019; Nashville, TN.
- American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 86: Viral hepatitis in pregnancy. Obstet Gynecol. 2007;110:941-956.
- Patrick SW, Bauer AM, Warren MD, et al. Hepatitis C virus infection among women giving birth—Tennessee and the United States, 2009-2014. MMWR Morbid Mortal Weekly Rep. 2017;66:470-473.
- Koneru A, Nelson N, Hariri S, et al. Increased hepatitis C virus (HCV) detection in women of childbearing age and potential risk for vertical transmission—United States and Kentucky, 2011-2014. MMWR Morbid Mortal Weekly Rep. 2016;65:705-710.
- American Association for the Study of Liver Diseases (AASLD) and the Infectious Diseases Society of America (IDSA). Recommendations for testing, management, and treating, hepatitis C. HCV testing and linkage to care. https://www.hcvguidelines.org/.
- Koniares KG, Fadlallah H, Kolettis DS, et al. A survey of hepatitis C virus (HCV) screening in pregnancy among ObGyns at a tertiary care center. Poster presented at: American College of Obstetricians and Gynecologists Annual Clinical and Scientific Meeting; May 3-6, 2019; Nashville, TN.
Is elagolix safely effective at reducing heavy uterine bleeding in premenopausal women with uterine fibroids?
Uterine fibroids affect up to two-thirds of all women.1 The current medical treatment options for uterine fibroids include on- and off-label use of oral contraceptives, hormonal intrauterine devices, gonadotropin-releasing hormone (GnRH) receptor agonists, and progestins. Data on the oral GnRH antagonist elagolix, US Food and Drug Administration–approved to treat endometriosis, were presented at the 2019 Annual Clinical and Scientific Meeting of the American College of Obstetricians and Gynecologists.
Study details
In the Eularis I trial, a total of 412 women with heavy menstrual bleeding (>80 mL/cycle of menstrual blood loss) were included in the double-blind, randomized, placebo-controlled, 6-month, phase 3 study. Women were premenopausal, ranged in age from 18 to 51 years, and were assigned in a 1:1:2 ratio to placebo, elagolix 300 mg twice daily, or elagolix 300 mg twice daily in combination with 1 mg estradiol/0.5 mg norethindrone acetate once-daily add-back therapy. A total of 328 women completed treatment.
At 6 months, 84.1%, 68.5%, and 8.7% of women taking elagolix alone, elagolix plus estradiol/norethindrone acetate, and placebo experienced a bleeding reduction that was 50% or greater from baseline.
Half of women who were treated with elagolix plus hormonal add-back therapy experienced adverse events, compared with 80% of women who took elagolix alone and 38% of women taking placebo. At study conclusion, the change from baseline for lumbar spine bone mass density was not significantly different from placebo for elagolix plus hormonal add-back therapy, but it was significantly different for elagolix alone compared with placebo.2
EULARIS II
A second study of safety and efficacy, which also was a double-blind, randomized, placebo-controlled, 6-month, phase 3 study, found that 76% of women randomly assigned to elagolix plus estradiol/norethindrone acetate experienced a bleeding reduction that was 50% or greater from baseline.3
Both EULARIS studies were funded by AbbVie, Inc.
- Al-Hendy A, Myers ER, Stewart E. Uterine fibroids: burden and unmet medical need. Semin Reprod Med . 2017;35:473-480.
- Elagolix reduced heavy menstrual bleeding with uterine fibroids: primary, 6-month, phase 3 results [press release]. New York, NY: W2O group; May 1, 2019.
- AbbVie announces positive topline results from phase 3 extension study evaluating investigational elagolix in women with uterine fibroids [press release]. New York, NY: PRNewswire; August 22, 2018.
Uterine fibroids affect up to two-thirds of all women.1 The current medical treatment options for uterine fibroids include on- and off-label use of oral contraceptives, hormonal intrauterine devices, gonadotropin-releasing hormone (GnRH) receptor agonists, and progestins. Data on the oral GnRH antagonist elagolix, US Food and Drug Administration–approved to treat endometriosis, were presented at the 2019 Annual Clinical and Scientific Meeting of the American College of Obstetricians and Gynecologists.
Study details
In the Eularis I trial, a total of 412 women with heavy menstrual bleeding (>80 mL/cycle of menstrual blood loss) were included in the double-blind, randomized, placebo-controlled, 6-month, phase 3 study. Women were premenopausal, ranged in age from 18 to 51 years, and were assigned in a 1:1:2 ratio to placebo, elagolix 300 mg twice daily, or elagolix 300 mg twice daily in combination with 1 mg estradiol/0.5 mg norethindrone acetate once-daily add-back therapy. A total of 328 women completed treatment.
At 6 months, 84.1%, 68.5%, and 8.7% of women taking elagolix alone, elagolix plus estradiol/norethindrone acetate, and placebo experienced a bleeding reduction that was 50% or greater from baseline.
Half of women who were treated with elagolix plus hormonal add-back therapy experienced adverse events, compared with 80% of women who took elagolix alone and 38% of women taking placebo. At study conclusion, the change from baseline for lumbar spine bone mass density was not significantly different from placebo for elagolix plus hormonal add-back therapy, but it was significantly different for elagolix alone compared with placebo.2
EULARIS II
A second study of safety and efficacy, which also was a double-blind, randomized, placebo-controlled, 6-month, phase 3 study, found that 76% of women randomly assigned to elagolix plus estradiol/norethindrone acetate experienced a bleeding reduction that was 50% or greater from baseline.3
Both EULARIS studies were funded by AbbVie, Inc.
Uterine fibroids affect up to two-thirds of all women.1 The current medical treatment options for uterine fibroids include on- and off-label use of oral contraceptives, hormonal intrauterine devices, gonadotropin-releasing hormone (GnRH) receptor agonists, and progestins. Data on the oral GnRH antagonist elagolix, US Food and Drug Administration–approved to treat endometriosis, were presented at the 2019 Annual Clinical and Scientific Meeting of the American College of Obstetricians and Gynecologists.
Study details
In the Eularis I trial, a total of 412 women with heavy menstrual bleeding (>80 mL/cycle of menstrual blood loss) were included in the double-blind, randomized, placebo-controlled, 6-month, phase 3 study. Women were premenopausal, ranged in age from 18 to 51 years, and were assigned in a 1:1:2 ratio to placebo, elagolix 300 mg twice daily, or elagolix 300 mg twice daily in combination with 1 mg estradiol/0.5 mg norethindrone acetate once-daily add-back therapy. A total of 328 women completed treatment.
At 6 months, 84.1%, 68.5%, and 8.7% of women taking elagolix alone, elagolix plus estradiol/norethindrone acetate, and placebo experienced a bleeding reduction that was 50% or greater from baseline.
Half of women who were treated with elagolix plus hormonal add-back therapy experienced adverse events, compared with 80% of women who took elagolix alone and 38% of women taking placebo. At study conclusion, the change from baseline for lumbar spine bone mass density was not significantly different from placebo for elagolix plus hormonal add-back therapy, but it was significantly different for elagolix alone compared with placebo.2
EULARIS II
A second study of safety and efficacy, which also was a double-blind, randomized, placebo-controlled, 6-month, phase 3 study, found that 76% of women randomly assigned to elagolix plus estradiol/norethindrone acetate experienced a bleeding reduction that was 50% or greater from baseline.3
Both EULARIS studies were funded by AbbVie, Inc.
- Al-Hendy A, Myers ER, Stewart E. Uterine fibroids: burden and unmet medical need. Semin Reprod Med . 2017;35:473-480.
- Elagolix reduced heavy menstrual bleeding with uterine fibroids: primary, 6-month, phase 3 results [press release]. New York, NY: W2O group; May 1, 2019.
- AbbVie announces positive topline results from phase 3 extension study evaluating investigational elagolix in women with uterine fibroids [press release]. New York, NY: PRNewswire; August 22, 2018.
- Al-Hendy A, Myers ER, Stewart E. Uterine fibroids: burden and unmet medical need. Semin Reprod Med . 2017;35:473-480.
- Elagolix reduced heavy menstrual bleeding with uterine fibroids: primary, 6-month, phase 3 results [press release]. New York, NY: W2O group; May 1, 2019.
- AbbVie announces positive topline results from phase 3 extension study evaluating investigational elagolix in women with uterine fibroids [press release]. New York, NY: PRNewswire; August 22, 2018.
Society of Gynecologic Surgeons 2019 meeting: Daily reporting from Fellow Scholar
WEDNESDAY, 4/3/2019. DAY 4 OF SGS.
Sadly, the annual Society of Gynecologic Surgeons meeting is wrapping up, and we will soon be leaving sunny Tucson! The last morning of conference proceedings was jam-packed with more outstanding oral and video presentations. We heard about topics such as the burden of postoperative catheterization, dietary patterns associated with postoperative defecatory symptoms, and more surgical tips and tricks to take back to our own institutions. At the end of the morning, the Distinguished Surgeon award was presented to the talented and deserving J. Marion Sims Endowed Chair of Obstetrics and Gynecology at UAB Medicine in Birmingham Dr. Holly E. Richter. The SGS Presidential Gavel was then passed from current SGS President Dr. Rajiv Gala to the incoming 46th President Dr. Peter Rosenblatt, Director of the Urogynecology and Pelvic Reconstructive Surgery Division at Mount Auburn Hospital in Cambridge, Massachusetts.
#SGS2019 was an amazingly successful conference! Beautiful surroundings, emerging science and education, and respectful inquiry was plentiful. I enjoyed all of the networking, reconnecting, and relaxing, and could not ask for a better community of GYN surgeons to have shared this with. I can’t wait to return to Pittsburgh to implement all the new things that I have learned. Thanks to the Society of Gynecologic Surgeons, OBG MANAGEMENT, and all the sponsors of the Fellows Scholar Program for supporting each of the scholars and this blog!
If you were at all intrigued by the happenings reported here, please consider attending the SGS meeting in 2020! The conference will be located in Jacksonville, Florida! See you there!
Thanks for following along! #SGS2019 out.
Continue to: TUESDAY, 4/2/19. DAY 3...
TUESDAY, 4/2/19. DAY 3.
The third day of the annual meeting of the Society of Gynecologic Surgeons started off with several academic roundtables hosted by experts in the field. The general session got underway with more fantastic oral and video presentations and, as usual, plenty of lively discussion and education ensued! The 45th SGS President Dr. Rajiv Gala (@rgala_nola) gave his presidential address, where he spoke so genuinely about how SGS is looking forward in our field. After all, the best way to predict your future is to create it! Be on the lookout on Twitter for Dr. Gala’s selfie with his “SGS Family” that he took during his address!
This year’s Telinde Lecture was given by Dr. Marcela G. del Carmen, titled “Health Care Disparities in Gynecologic Oncology Surgery.” She gave an informative and eye-opening lecture on the disparities that still exist in our field, specifically in patients with cancer. The morning session was rounded out with a mentoring panel, featuring Drs. B. Star Hampton, Bobby Shull, Peggy Norton, Tom Nolan, and Deborah Myers. Plenty of sage advice was offered. Thanks to Dr. Shull for reminding us to “be gracious; kindness never goes out of style,” and to be “a citizen of the world.”
Conference goers took the afternoon to enjoy leisure activities in the beautiful Arizona surroundings, including mountain biking, yoga, golf, and poolside lounging. The evening was filled with the excitement of the annual “SGS Got Talent” show! Fabulous performances and delicious food and drinks were just half of the fun, though. The life-size play on hungry, hungry hippos—“Hungry, Hungry Surgeons”—competition was the hit of the night!
Tomorrow is the last day of #SGS2019. Be sure to follow along for the final day of coverage!
Continue to: MONDAY, 4/1/19. DAY 2...
MONDAY, 4/1/19. DAY 2.
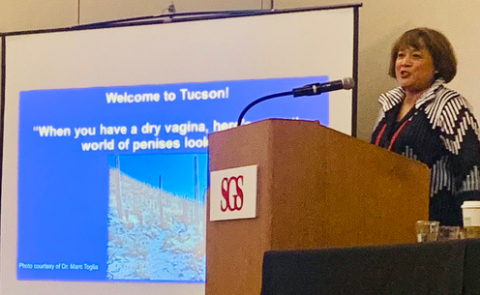
The first day of the general sessions started off with a cleverly titled breakfast symposium, “Postmenopausal sexuality: A bit dry but a must-have conversation,” by the brilliant and entertaining duo of Cheryl Iglesia (@cheryliglesia) and Sheryl Kingsberg (@SherylKingsburg) #CherylandSheryl.
Cheryl Iglesia, MD
The new members of the Society of Gynecologic Surgeons were recognized, and there were several outstanding oral and video presentations throughout the morning. A range of topics were discussed, including vaginal surgery education, patient perspectives on adverse events, and postoperative pain management. In addition, Dr. Gary Dunnington (@GLDunnington), Chair of Surgery at Indiana University School of Medicine in Indianapolis, gave the keynote lecture on “Measuring and improving performance in surgical training,” reminding us to continually strive for change.
After a brief lunch and stroll around the exhibit hall, the afternoon session kicked off with a special guest lecture on vaginal rejuvenation and energy-based therapies for female genital cosmetic surgery by Cheryl Iglesia (@cheryliglesia). Next, a distinguished panel of experts from all gynecologic subspecialties gave their opinions on “Working together to shape the future of gynecologic surgery.” What a treat to see such important topics discussed by all the giants of our field sitting in one room: Society of Gynecologic Surgeons President Rajiv Gala, MD; ACOG President Elect Ted Anderson, MD; American Urogynecologic Society President Geoffrey W. Cundiff, MD; Society of Gynecologic Oncology President Elect Warner Huh, MD; Society of Reproductive Surgeons Immediate Past President Samantha Pfeifer, MD; and AAGL President Marie Fidela R. Paraiso, MD.
Supplemented by popcorn, the Videofest featured a series of informative and impressive videos—from management of removal of the Essure hysteroscopic contraceptive device to tips and tricks to navigate a pelvic kidney. The Fellows’ Pelvic Research Network (FPRN), a network of fellows from both minimally invasive gynecologic surgery and urogynecology programs that facilitates multicenter research, met and discussed ongoing and upcoming studies. Exciting work is coming your way thanks to the collaboration of the FPRN!
We concluded an excellent first day of general sessions with an awards ceremony and President’s reception. It was an evening filled with networking, catching up with old colleagues, and meeting new friends. I look forward to another day of scholarship and education tomorrow! Follow @lauraknewcomb, @GynSurgery, and @MDedgeObGyn on Twitter for updates.
Continue to: SUNDAY, 3/31/19. DAY 1 AT SGS...
SUNDAY, 3/31/19. DAY 1 AT SGS.
Hello from Tucson! I woke up to a beautiful Arizona sunrise, with cacti as far as the eye can see; a great start to what is surely going to be an educational scientific conference of the Society of Gynecologic Surgeons! Be sure to follow me on Twitter to stay in the loop real-time: @lauraknewcomb. And don’t forget to check out our conference hashtag #SGS2019.
Postgrad courses kick off
Quality improvement bootcamp
Dr. Bob Flora (@RFFlora) gave a great “Teach the Teacher” session, reviewing different methods for performing quality improvement projects in your own workspace, including the Institute for Healthcare Improvement (IHI) Model for Improvement (www.IHI.org). We also had the opportunity to learn and play with QI Macros (KnowWare International Inc) and Lucid Chart (Lucid Software Inc) programs—which are excellent tools to assist in quality improvement data analysis and presentation. Try them out if you have never used them before!
Sex and surgery
The sex and surgery postgraduate course was a lively discussion centering on:
- the links between gynecologic surgery and sexual function
- how to measure sexual function and incorporate discussion into our pre- and post-operative counseling
- how to approach the patient with postoperative sexual concerns.
As surgeons, we admitted that an anatomic approach with surgery will not always be successful in treating sexual complaints, as sexuality encompasses psychological, social/cultural, interpersonal, and biological aspects. We agreed that further studies are needed to examine the issue, using sexual function as a primary endpoint, because the concern is of critical importance to our patients.
Social media workshop
The talented SGS Social Media Committee, including influencers Dr. Mireille Truong (@MIS_MDT) and Dr. Elisa Jorgensen (@ejiorgensenmd) gave us the run-down on how to host a successful Twitter journal club and how to be a responsible and influential influencer on various social media avenues. They encouraged us to take advantage of the virtual space that connects so many more people than we could interact with without it!
Hands-on laparoscopic suturing simulation
This course was an excellent comprehensive laparoscopic suturing course. It began with a detailed outline of basic principles and slowly built on these concepts until we were performing laparoscopic myomectomies on a high-fidelity model. We can’t wait to implement these principles in the operating room next week! Thanks to the talented faculty who taught all the tips and tricks of the experts!
Conservative and definitive surgical strategies for fibroid management
Drs. Megan Wasson (@WassonMegan), Arnold Advincula (@arnieadvincula), and others taught all the nuances of managing fibroids and difficult surgical cases. Participants learned several tips, tricks, and techniques to use to manage fibroids—for example the “bow and arrow” and “push and tuck” techniques when performing a hysteroscopic myomectomy with a resectoscope.
Women’s leadership forum
During the evening women’s leadership forum, Drs. Catherine Matthews and Kimberly Kenton (@KimKenton1) highlighted the differences between mentorship and sponsorship. While most female physicians identify meaningful mentorship relationships, women lack sponsorship to advance their careers. Furthermore, more women-to-women sponsorship relationships are needed to improve and achieve gender equality.
Lastly, we all enjoyed the Arizona sunset with a welcome reception on the lawn. It was a great first day and we are all looking forward to an exciting general session on Monday! Stay tuned for more!

#SGS2019 attendees enjoying the welcome reception
WEDNESDAY, 4/3/2019. DAY 4 OF SGS.
Sadly, the annual Society of Gynecologic Surgeons meeting is wrapping up, and we will soon be leaving sunny Tucson! The last morning of conference proceedings was jam-packed with more outstanding oral and video presentations. We heard about topics such as the burden of postoperative catheterization, dietary patterns associated with postoperative defecatory symptoms, and more surgical tips and tricks to take back to our own institutions. At the end of the morning, the Distinguished Surgeon award was presented to the talented and deserving J. Marion Sims Endowed Chair of Obstetrics and Gynecology at UAB Medicine in Birmingham Dr. Holly E. Richter. The SGS Presidential Gavel was then passed from current SGS President Dr. Rajiv Gala to the incoming 46th President Dr. Peter Rosenblatt, Director of the Urogynecology and Pelvic Reconstructive Surgery Division at Mount Auburn Hospital in Cambridge, Massachusetts.
#SGS2019 was an amazingly successful conference! Beautiful surroundings, emerging science and education, and respectful inquiry was plentiful. I enjoyed all of the networking, reconnecting, and relaxing, and could not ask for a better community of GYN surgeons to have shared this with. I can’t wait to return to Pittsburgh to implement all the new things that I have learned. Thanks to the Society of Gynecologic Surgeons, OBG MANAGEMENT, and all the sponsors of the Fellows Scholar Program for supporting each of the scholars and this blog!
If you were at all intrigued by the happenings reported here, please consider attending the SGS meeting in 2020! The conference will be located in Jacksonville, Florida! See you there!
Thanks for following along! #SGS2019 out.
Continue to: TUESDAY, 4/2/19. DAY 3...
TUESDAY, 4/2/19. DAY 3.
The third day of the annual meeting of the Society of Gynecologic Surgeons started off with several academic roundtables hosted by experts in the field. The general session got underway with more fantastic oral and video presentations and, as usual, plenty of lively discussion and education ensued! The 45th SGS President Dr. Rajiv Gala (@rgala_nola) gave his presidential address, where he spoke so genuinely about how SGS is looking forward in our field. After all, the best way to predict your future is to create it! Be on the lookout on Twitter for Dr. Gala’s selfie with his “SGS Family” that he took during his address!
This year’s Telinde Lecture was given by Dr. Marcela G. del Carmen, titled “Health Care Disparities in Gynecologic Oncology Surgery.” She gave an informative and eye-opening lecture on the disparities that still exist in our field, specifically in patients with cancer. The morning session was rounded out with a mentoring panel, featuring Drs. B. Star Hampton, Bobby Shull, Peggy Norton, Tom Nolan, and Deborah Myers. Plenty of sage advice was offered. Thanks to Dr. Shull for reminding us to “be gracious; kindness never goes out of style,” and to be “a citizen of the world.”
Conference goers took the afternoon to enjoy leisure activities in the beautiful Arizona surroundings, including mountain biking, yoga, golf, and poolside lounging. The evening was filled with the excitement of the annual “SGS Got Talent” show! Fabulous performances and delicious food and drinks were just half of the fun, though. The life-size play on hungry, hungry hippos—“Hungry, Hungry Surgeons”—competition was the hit of the night!
Tomorrow is the last day of #SGS2019. Be sure to follow along for the final day of coverage!
Continue to: MONDAY, 4/1/19. DAY 2...
MONDAY, 4/1/19. DAY 2.
The first day of the general sessions started off with a cleverly titled breakfast symposium, “Postmenopausal sexuality: A bit dry but a must-have conversation,” by the brilliant and entertaining duo of Cheryl Iglesia (@cheryliglesia) and Sheryl Kingsberg (@SherylKingsburg) #CherylandSheryl.
Cheryl Iglesia, MD
The new members of the Society of Gynecologic Surgeons were recognized, and there were several outstanding oral and video presentations throughout the morning. A range of topics were discussed, including vaginal surgery education, patient perspectives on adverse events, and postoperative pain management. In addition, Dr. Gary Dunnington (@GLDunnington), Chair of Surgery at Indiana University School of Medicine in Indianapolis, gave the keynote lecture on “Measuring and improving performance in surgical training,” reminding us to continually strive for change.
After a brief lunch and stroll around the exhibit hall, the afternoon session kicked off with a special guest lecture on vaginal rejuvenation and energy-based therapies for female genital cosmetic surgery by Cheryl Iglesia (@cheryliglesia). Next, a distinguished panel of experts from all gynecologic subspecialties gave their opinions on “Working together to shape the future of gynecologic surgery.” What a treat to see such important topics discussed by all the giants of our field sitting in one room: Society of Gynecologic Surgeons President Rajiv Gala, MD; ACOG President Elect Ted Anderson, MD; American Urogynecologic Society President Geoffrey W. Cundiff, MD; Society of Gynecologic Oncology President Elect Warner Huh, MD; Society of Reproductive Surgeons Immediate Past President Samantha Pfeifer, MD; and AAGL President Marie Fidela R. Paraiso, MD.
Supplemented by popcorn, the Videofest featured a series of informative and impressive videos—from management of removal of the Essure hysteroscopic contraceptive device to tips and tricks to navigate a pelvic kidney. The Fellows’ Pelvic Research Network (FPRN), a network of fellows from both minimally invasive gynecologic surgery and urogynecology programs that facilitates multicenter research, met and discussed ongoing and upcoming studies. Exciting work is coming your way thanks to the collaboration of the FPRN!
We concluded an excellent first day of general sessions with an awards ceremony and President’s reception. It was an evening filled with networking, catching up with old colleagues, and meeting new friends. I look forward to another day of scholarship and education tomorrow! Follow @lauraknewcomb, @GynSurgery, and @MDedgeObGyn on Twitter for updates.
Continue to: SUNDAY, 3/31/19. DAY 1 AT SGS...
SUNDAY, 3/31/19. DAY 1 AT SGS.
Hello from Tucson! I woke up to a beautiful Arizona sunrise, with cacti as far as the eye can see; a great start to what is surely going to be an educational scientific conference of the Society of Gynecologic Surgeons! Be sure to follow me on Twitter to stay in the loop real-time: @lauraknewcomb. And don’t forget to check out our conference hashtag #SGS2019.
Postgrad courses kick off
Quality improvement bootcamp
Dr. Bob Flora (@RFFlora) gave a great “Teach the Teacher” session, reviewing different methods for performing quality improvement projects in your own workspace, including the Institute for Healthcare Improvement (IHI) Model for Improvement (www.IHI.org). We also had the opportunity to learn and play with QI Macros (KnowWare International Inc) and Lucid Chart (Lucid Software Inc) programs—which are excellent tools to assist in quality improvement data analysis and presentation. Try them out if you have never used them before!
Sex and surgery
The sex and surgery postgraduate course was a lively discussion centering on:
- the links between gynecologic surgery and sexual function
- how to measure sexual function and incorporate discussion into our pre- and post-operative counseling
- how to approach the patient with postoperative sexual concerns.
As surgeons, we admitted that an anatomic approach with surgery will not always be successful in treating sexual complaints, as sexuality encompasses psychological, social/cultural, interpersonal, and biological aspects. We agreed that further studies are needed to examine the issue, using sexual function as a primary endpoint, because the concern is of critical importance to our patients.
Social media workshop
The talented SGS Social Media Committee, including influencers Dr. Mireille Truong (@MIS_MDT) and Dr. Elisa Jorgensen (@ejiorgensenmd) gave us the run-down on how to host a successful Twitter journal club and how to be a responsible and influential influencer on various social media avenues. They encouraged us to take advantage of the virtual space that connects so many more people than we could interact with without it!
Hands-on laparoscopic suturing simulation
This course was an excellent comprehensive laparoscopic suturing course. It began with a detailed outline of basic principles and slowly built on these concepts until we were performing laparoscopic myomectomies on a high-fidelity model. We can’t wait to implement these principles in the operating room next week! Thanks to the talented faculty who taught all the tips and tricks of the experts!
Conservative and definitive surgical strategies for fibroid management
Drs. Megan Wasson (@WassonMegan), Arnold Advincula (@arnieadvincula), and others taught all the nuances of managing fibroids and difficult surgical cases. Participants learned several tips, tricks, and techniques to use to manage fibroids—for example the “bow and arrow” and “push and tuck” techniques when performing a hysteroscopic myomectomy with a resectoscope.
Women’s leadership forum
During the evening women’s leadership forum, Drs. Catherine Matthews and Kimberly Kenton (@KimKenton1) highlighted the differences between mentorship and sponsorship. While most female physicians identify meaningful mentorship relationships, women lack sponsorship to advance their careers. Furthermore, more women-to-women sponsorship relationships are needed to improve and achieve gender equality.
Lastly, we all enjoyed the Arizona sunset with a welcome reception on the lawn. It was a great first day and we are all looking forward to an exciting general session on Monday! Stay tuned for more!

#SGS2019 attendees enjoying the welcome reception
WEDNESDAY, 4/3/2019. DAY 4 OF SGS.
Sadly, the annual Society of Gynecologic Surgeons meeting is wrapping up, and we will soon be leaving sunny Tucson! The last morning of conference proceedings was jam-packed with more outstanding oral and video presentations. We heard about topics such as the burden of postoperative catheterization, dietary patterns associated with postoperative defecatory symptoms, and more surgical tips and tricks to take back to our own institutions. At the end of the morning, the Distinguished Surgeon award was presented to the talented and deserving J. Marion Sims Endowed Chair of Obstetrics and Gynecology at UAB Medicine in Birmingham Dr. Holly E. Richter. The SGS Presidential Gavel was then passed from current SGS President Dr. Rajiv Gala to the incoming 46th President Dr. Peter Rosenblatt, Director of the Urogynecology and Pelvic Reconstructive Surgery Division at Mount Auburn Hospital in Cambridge, Massachusetts.
#SGS2019 was an amazingly successful conference! Beautiful surroundings, emerging science and education, and respectful inquiry was plentiful. I enjoyed all of the networking, reconnecting, and relaxing, and could not ask for a better community of GYN surgeons to have shared this with. I can’t wait to return to Pittsburgh to implement all the new things that I have learned. Thanks to the Society of Gynecologic Surgeons, OBG MANAGEMENT, and all the sponsors of the Fellows Scholar Program for supporting each of the scholars and this blog!
If you were at all intrigued by the happenings reported here, please consider attending the SGS meeting in 2020! The conference will be located in Jacksonville, Florida! See you there!
Thanks for following along! #SGS2019 out.
Continue to: TUESDAY, 4/2/19. DAY 3...
TUESDAY, 4/2/19. DAY 3.
The third day of the annual meeting of the Society of Gynecologic Surgeons started off with several academic roundtables hosted by experts in the field. The general session got underway with more fantastic oral and video presentations and, as usual, plenty of lively discussion and education ensued! The 45th SGS President Dr. Rajiv Gala (@rgala_nola) gave his presidential address, where he spoke so genuinely about how SGS is looking forward in our field. After all, the best way to predict your future is to create it! Be on the lookout on Twitter for Dr. Gala’s selfie with his “SGS Family” that he took during his address!
This year’s Telinde Lecture was given by Dr. Marcela G. del Carmen, titled “Health Care Disparities in Gynecologic Oncology Surgery.” She gave an informative and eye-opening lecture on the disparities that still exist in our field, specifically in patients with cancer. The morning session was rounded out with a mentoring panel, featuring Drs. B. Star Hampton, Bobby Shull, Peggy Norton, Tom Nolan, and Deborah Myers. Plenty of sage advice was offered. Thanks to Dr. Shull for reminding us to “be gracious; kindness never goes out of style,” and to be “a citizen of the world.”
Conference goers took the afternoon to enjoy leisure activities in the beautiful Arizona surroundings, including mountain biking, yoga, golf, and poolside lounging. The evening was filled with the excitement of the annual “SGS Got Talent” show! Fabulous performances and delicious food and drinks were just half of the fun, though. The life-size play on hungry, hungry hippos—“Hungry, Hungry Surgeons”—competition was the hit of the night!
Tomorrow is the last day of #SGS2019. Be sure to follow along for the final day of coverage!
Continue to: MONDAY, 4/1/19. DAY 2...
MONDAY, 4/1/19. DAY 2.
The first day of the general sessions started off with a cleverly titled breakfast symposium, “Postmenopausal sexuality: A bit dry but a must-have conversation,” by the brilliant and entertaining duo of Cheryl Iglesia (@cheryliglesia) and Sheryl Kingsberg (@SherylKingsburg) #CherylandSheryl.
Cheryl Iglesia, MD
The new members of the Society of Gynecologic Surgeons were recognized, and there were several outstanding oral and video presentations throughout the morning. A range of topics were discussed, including vaginal surgery education, patient perspectives on adverse events, and postoperative pain management. In addition, Dr. Gary Dunnington (@GLDunnington), Chair of Surgery at Indiana University School of Medicine in Indianapolis, gave the keynote lecture on “Measuring and improving performance in surgical training,” reminding us to continually strive for change.
After a brief lunch and stroll around the exhibit hall, the afternoon session kicked off with a special guest lecture on vaginal rejuvenation and energy-based therapies for female genital cosmetic surgery by Cheryl Iglesia (@cheryliglesia). Next, a distinguished panel of experts from all gynecologic subspecialties gave their opinions on “Working together to shape the future of gynecologic surgery.” What a treat to see such important topics discussed by all the giants of our field sitting in one room: Society of Gynecologic Surgeons President Rajiv Gala, MD; ACOG President Elect Ted Anderson, MD; American Urogynecologic Society President Geoffrey W. Cundiff, MD; Society of Gynecologic Oncology President Elect Warner Huh, MD; Society of Reproductive Surgeons Immediate Past President Samantha Pfeifer, MD; and AAGL President Marie Fidela R. Paraiso, MD.
Supplemented by popcorn, the Videofest featured a series of informative and impressive videos—from management of removal of the Essure hysteroscopic contraceptive device to tips and tricks to navigate a pelvic kidney. The Fellows’ Pelvic Research Network (FPRN), a network of fellows from both minimally invasive gynecologic surgery and urogynecology programs that facilitates multicenter research, met and discussed ongoing and upcoming studies. Exciting work is coming your way thanks to the collaboration of the FPRN!
We concluded an excellent first day of general sessions with an awards ceremony and President’s reception. It was an evening filled with networking, catching up with old colleagues, and meeting new friends. I look forward to another day of scholarship and education tomorrow! Follow @lauraknewcomb, @GynSurgery, and @MDedgeObGyn on Twitter for updates.
Continue to: SUNDAY, 3/31/19. DAY 1 AT SGS...
SUNDAY, 3/31/19. DAY 1 AT SGS.
Hello from Tucson! I woke up to a beautiful Arizona sunrise, with cacti as far as the eye can see; a great start to what is surely going to be an educational scientific conference of the Society of Gynecologic Surgeons! Be sure to follow me on Twitter to stay in the loop real-time: @lauraknewcomb. And don’t forget to check out our conference hashtag #SGS2019.
Postgrad courses kick off
Quality improvement bootcamp
Dr. Bob Flora (@RFFlora) gave a great “Teach the Teacher” session, reviewing different methods for performing quality improvement projects in your own workspace, including the Institute for Healthcare Improvement (IHI) Model for Improvement (www.IHI.org). We also had the opportunity to learn and play with QI Macros (KnowWare International Inc) and Lucid Chart (Lucid Software Inc) programs—which are excellent tools to assist in quality improvement data analysis and presentation. Try them out if you have never used them before!
Sex and surgery
The sex and surgery postgraduate course was a lively discussion centering on:
- the links between gynecologic surgery and sexual function
- how to measure sexual function and incorporate discussion into our pre- and post-operative counseling
- how to approach the patient with postoperative sexual concerns.
As surgeons, we admitted that an anatomic approach with surgery will not always be successful in treating sexual complaints, as sexuality encompasses psychological, social/cultural, interpersonal, and biological aspects. We agreed that further studies are needed to examine the issue, using sexual function as a primary endpoint, because the concern is of critical importance to our patients.
Social media workshop
The talented SGS Social Media Committee, including influencers Dr. Mireille Truong (@MIS_MDT) and Dr. Elisa Jorgensen (@ejiorgensenmd) gave us the run-down on how to host a successful Twitter journal club and how to be a responsible and influential influencer on various social media avenues. They encouraged us to take advantage of the virtual space that connects so many more people than we could interact with without it!
Hands-on laparoscopic suturing simulation
This course was an excellent comprehensive laparoscopic suturing course. It began with a detailed outline of basic principles and slowly built on these concepts until we were performing laparoscopic myomectomies on a high-fidelity model. We can’t wait to implement these principles in the operating room next week! Thanks to the talented faculty who taught all the tips and tricks of the experts!
Conservative and definitive surgical strategies for fibroid management
Drs. Megan Wasson (@WassonMegan), Arnold Advincula (@arnieadvincula), and others taught all the nuances of managing fibroids and difficult surgical cases. Participants learned several tips, tricks, and techniques to use to manage fibroids—for example the “bow and arrow” and “push and tuck” techniques when performing a hysteroscopic myomectomy with a resectoscope.
Women’s leadership forum
During the evening women’s leadership forum, Drs. Catherine Matthews and Kimberly Kenton (@KimKenton1) highlighted the differences between mentorship and sponsorship. While most female physicians identify meaningful mentorship relationships, women lack sponsorship to advance their careers. Furthermore, more women-to-women sponsorship relationships are needed to improve and achieve gender equality.
Lastly, we all enjoyed the Arizona sunset with a welcome reception on the lawn. It was a great first day and we are all looking forward to an exciting general session on Monday! Stay tuned for more!

#SGS2019 attendees enjoying the welcome reception
Nationwide implementation of MIS reduced complications and increased survival in early-stage endometrial cancer
To determine if a nationwide implementation of robotic minimally invasive surgery (MIS) influenced the risk of severe complications and survival among women with early-stage endometrial cancer, a group of researchers from the University of Southern Denmark studied the Danish Gynecological Cancer Database, a nationwide, mandatory prospective registration of new cases of women with endometrial cancer who received their surgical treatment in a public hospital.1 Siv Joergensen, MD, reported results at the 47th AAGL Global Congress on Minimally Invasive Gynecology annual meeting on November 13, 2018, in Las Vegas, Nevada.
The transition to robotic MIS was undertaken in Denmark from 2008 to 2013, with the centralization of endometrial cancer treatment in 2012. Over the span of 10 years, the surgical approach to treatment changed from 97% open access surgery to 95% MIS.
For the prospective cohort study, more than 7,000 women with endometrial cancer who received a hysterectomy from January 2005 to June 2015 were grouped by those receiving surgical care before (group 1) and after (group 2) robotic MIS implementation in Denmark. A total of 5,654 women with FIGO Stage I–II endometrial cancer were included in the final study.
Severe complications were 7.3% in group 1 and 6.2% in group 2 (odds ratio, 1.38; 95% confidence interval [CI], 1.10–1.73). Five-year survival rates were significantly lower before robotic MIS was implemented (hazard ratio, 1.22; 95% CI, 1.05–1.41), and no difference was found between laparoscopic and robotic MIS.
The authors concluded that nationwide implementation of robotic MIS enabled a shift toward all types of MIS (with a 73% reduction in hysterectomies performed by laparotomy) and translated into reduced risk of severe complications and increased survival.
How do these results compare with those in the United States?
According to Erica Dun, MD, MPH, who provided commentary for Dr. Joergensen’s study, the United States adopted robotic MIS in the early 2000s. Around 2008, 14% of hysterectomies performed for early-stage endometrial cancer were done through a MIS approach.2 In 2014, after a study in which Walker and colleagues found that laparoscopy was safe and feasible compared with laparotomy,3 the American College of Obstetricians and Gynecologists, jointly with the Society of Gynecologic Oncologists, stated that “MIS should be embraced as the standard surgical approach for comprehensive surgical staging in women with endometrial cancer.”4
Dr. Dun pointed out that Casarin and colleagues found in 2018 that 71.4% of surgeries performed in the United States for endometrial cancer were performed through MIS.5 That number rose to 86.5% MIS (72.5% robot-assisted) for centers of the National Comprehensive Cancer Network.6
Dr. Dun concluded that nationwide implementation of robotic MIS is feasible for gynecologic oncologists, and it is beneficial for patients.
1. Joergensen SL. Nationwide implementation of robotic minimally invasive surgery for endometrial cancer increases survival and reduces complications. Poster presented at: 47th AAGL Global Congress on Minimally Invasive Gynecology; November 11-15, 2018; Las Vegas, NV.
2. Jacoby VL, Autry A, Jacobson G, et al. Nationwide use of laparoscopic hysterectomy compared with abdominal and vaginal approaches. Obstet Gynecol. 2009;114:1041-1048.
3. Walker JL, Piedmonte MR, Spirtos NM, et al. Laparoscopy compared with laparotomy for comprehensive surgical staging of uterine cancer: Gynecologic Oncology Group Study LAP2. J Clin Oncol. 2009;27:5331-5336.
4. American College of Obstetricians and Gynecologists, Society of Gynecologic Oncologists. Practice bulletin no. 149: endometrial cancer. Obstet Gynecol. 2015;125:1006-1026.
5. Casarin J, et al. Adaptation of minimally invasive surgery and decrease in surgical morbidity for endometrial cancer treatment in the United States. Obstet Gynecol. 2018;131:304-311.
6. Bergstrom, Aloisi A, Armbruster S, et al. Minimally invasive hysterectomy surgery rates for endometrial cancer performed at National Comprehensive Cancer Network (NCCN) Centers. Gynecol Oncol. 2018;148:480-484.
To determine if a nationwide implementation of robotic minimally invasive surgery (MIS) influenced the risk of severe complications and survival among women with early-stage endometrial cancer, a group of researchers from the University of Southern Denmark studied the Danish Gynecological Cancer Database, a nationwide, mandatory prospective registration of new cases of women with endometrial cancer who received their surgical treatment in a public hospital.1 Siv Joergensen, MD, reported results at the 47th AAGL Global Congress on Minimally Invasive Gynecology annual meeting on November 13, 2018, in Las Vegas, Nevada.
The transition to robotic MIS was undertaken in Denmark from 2008 to 2013, with the centralization of endometrial cancer treatment in 2012. Over the span of 10 years, the surgical approach to treatment changed from 97% open access surgery to 95% MIS.
For the prospective cohort study, more than 7,000 women with endometrial cancer who received a hysterectomy from January 2005 to June 2015 were grouped by those receiving surgical care before (group 1) and after (group 2) robotic MIS implementation in Denmark. A total of 5,654 women with FIGO Stage I–II endometrial cancer were included in the final study.
Severe complications were 7.3% in group 1 and 6.2% in group 2 (odds ratio, 1.38; 95% confidence interval [CI], 1.10–1.73). Five-year survival rates were significantly lower before robotic MIS was implemented (hazard ratio, 1.22; 95% CI, 1.05–1.41), and no difference was found between laparoscopic and robotic MIS.
The authors concluded that nationwide implementation of robotic MIS enabled a shift toward all types of MIS (with a 73% reduction in hysterectomies performed by laparotomy) and translated into reduced risk of severe complications and increased survival.
How do these results compare with those in the United States?
According to Erica Dun, MD, MPH, who provided commentary for Dr. Joergensen’s study, the United States adopted robotic MIS in the early 2000s. Around 2008, 14% of hysterectomies performed for early-stage endometrial cancer were done through a MIS approach.2 In 2014, after a study in which Walker and colleagues found that laparoscopy was safe and feasible compared with laparotomy,3 the American College of Obstetricians and Gynecologists, jointly with the Society of Gynecologic Oncologists, stated that “MIS should be embraced as the standard surgical approach for comprehensive surgical staging in women with endometrial cancer.”4
Dr. Dun pointed out that Casarin and colleagues found in 2018 that 71.4% of surgeries performed in the United States for endometrial cancer were performed through MIS.5 That number rose to 86.5% MIS (72.5% robot-assisted) for centers of the National Comprehensive Cancer Network.6
Dr. Dun concluded that nationwide implementation of robotic MIS is feasible for gynecologic oncologists, and it is beneficial for patients.
To determine if a nationwide implementation of robotic minimally invasive surgery (MIS) influenced the risk of severe complications and survival among women with early-stage endometrial cancer, a group of researchers from the University of Southern Denmark studied the Danish Gynecological Cancer Database, a nationwide, mandatory prospective registration of new cases of women with endometrial cancer who received their surgical treatment in a public hospital.1 Siv Joergensen, MD, reported results at the 47th AAGL Global Congress on Minimally Invasive Gynecology annual meeting on November 13, 2018, in Las Vegas, Nevada.
The transition to robotic MIS was undertaken in Denmark from 2008 to 2013, with the centralization of endometrial cancer treatment in 2012. Over the span of 10 years, the surgical approach to treatment changed from 97% open access surgery to 95% MIS.
For the prospective cohort study, more than 7,000 women with endometrial cancer who received a hysterectomy from January 2005 to June 2015 were grouped by those receiving surgical care before (group 1) and after (group 2) robotic MIS implementation in Denmark. A total of 5,654 women with FIGO Stage I–II endometrial cancer were included in the final study.
Severe complications were 7.3% in group 1 and 6.2% in group 2 (odds ratio, 1.38; 95% confidence interval [CI], 1.10–1.73). Five-year survival rates were significantly lower before robotic MIS was implemented (hazard ratio, 1.22; 95% CI, 1.05–1.41), and no difference was found between laparoscopic and robotic MIS.
The authors concluded that nationwide implementation of robotic MIS enabled a shift toward all types of MIS (with a 73% reduction in hysterectomies performed by laparotomy) and translated into reduced risk of severe complications and increased survival.
How do these results compare with those in the United States?
According to Erica Dun, MD, MPH, who provided commentary for Dr. Joergensen’s study, the United States adopted robotic MIS in the early 2000s. Around 2008, 14% of hysterectomies performed for early-stage endometrial cancer were done through a MIS approach.2 In 2014, after a study in which Walker and colleagues found that laparoscopy was safe and feasible compared with laparotomy,3 the American College of Obstetricians and Gynecologists, jointly with the Society of Gynecologic Oncologists, stated that “MIS should be embraced as the standard surgical approach for comprehensive surgical staging in women with endometrial cancer.”4
Dr. Dun pointed out that Casarin and colleagues found in 2018 that 71.4% of surgeries performed in the United States for endometrial cancer were performed through MIS.5 That number rose to 86.5% MIS (72.5% robot-assisted) for centers of the National Comprehensive Cancer Network.6
Dr. Dun concluded that nationwide implementation of robotic MIS is feasible for gynecologic oncologists, and it is beneficial for patients.
1. Joergensen SL. Nationwide implementation of robotic minimally invasive surgery for endometrial cancer increases survival and reduces complications. Poster presented at: 47th AAGL Global Congress on Minimally Invasive Gynecology; November 11-15, 2018; Las Vegas, NV.
2. Jacoby VL, Autry A, Jacobson G, et al. Nationwide use of laparoscopic hysterectomy compared with abdominal and vaginal approaches. Obstet Gynecol. 2009;114:1041-1048.
3. Walker JL, Piedmonte MR, Spirtos NM, et al. Laparoscopy compared with laparotomy for comprehensive surgical staging of uterine cancer: Gynecologic Oncology Group Study LAP2. J Clin Oncol. 2009;27:5331-5336.
4. American College of Obstetricians and Gynecologists, Society of Gynecologic Oncologists. Practice bulletin no. 149: endometrial cancer. Obstet Gynecol. 2015;125:1006-1026.
5. Casarin J, et al. Adaptation of minimally invasive surgery and decrease in surgical morbidity for endometrial cancer treatment in the United States. Obstet Gynecol. 2018;131:304-311.
6. Bergstrom, Aloisi A, Armbruster S, et al. Minimally invasive hysterectomy surgery rates for endometrial cancer performed at National Comprehensive Cancer Network (NCCN) Centers. Gynecol Oncol. 2018;148:480-484.
1. Joergensen SL. Nationwide implementation of robotic minimally invasive surgery for endometrial cancer increases survival and reduces complications. Poster presented at: 47th AAGL Global Congress on Minimally Invasive Gynecology; November 11-15, 2018; Las Vegas, NV.
2. Jacoby VL, Autry A, Jacobson G, et al. Nationwide use of laparoscopic hysterectomy compared with abdominal and vaginal approaches. Obstet Gynecol. 2009;114:1041-1048.
3. Walker JL, Piedmonte MR, Spirtos NM, et al. Laparoscopy compared with laparotomy for comprehensive surgical staging of uterine cancer: Gynecologic Oncology Group Study LAP2. J Clin Oncol. 2009;27:5331-5336.
4. American College of Obstetricians and Gynecologists, Society of Gynecologic Oncologists. Practice bulletin no. 149: endometrial cancer. Obstet Gynecol. 2015;125:1006-1026.
5. Casarin J, et al. Adaptation of minimally invasive surgery and decrease in surgical morbidity for endometrial cancer treatment in the United States. Obstet Gynecol. 2018;131:304-311.
6. Bergstrom, Aloisi A, Armbruster S, et al. Minimally invasive hysterectomy surgery rates for endometrial cancer performed at National Comprehensive Cancer Network (NCCN) Centers. Gynecol Oncol. 2018;148:480-484.
Patient-centric pain management decision aid reduces opioid use posthysterectomy
Investigators at the University of Michigan, Ann Arbor, found that a simple patient decision aid can be a useful tool in providing adequate postsurgical pain control to patients while reducing the number of opioid tablets in the community. The shared decision-making aid focuses on educating the patient about opioid use and engages her in an appropriate postoperative pain management plan. Results from this prospective quality improvement study were presented in a poster at the 47th AAGL Global Congress on Minimally Invasive Gynecology (Las Vegas, Nevada, November 11–15, 2018).1
Annmarie Vilkins, DO, and colleagues’ aim was to evaluate the impact of shared decision-making through the use of a patient decision aid targeting posthysterectomy pain management and opioid use. Can such a targeted strategy help decrease posthysterectomy opioid distribution in the community without compromising patient pain control or satisfaction?
The authors noted that more than 46 people die each day from an overdose involving prescription opioids.2 Studies have shown that patients actually use significantly fewer opioid tablets than the amount clinicians generally prescribe following ObGyn surgeries.3,4 Unused prescription opioid availability has the potential for accidental use or intentional misuse of the unneeded drugs by others.
Study methods
The investigators included all English-speaking patients undergoing hysterectomy for benign disease at their institution from March 1 through July 31, 2018. Data were analyzed from women undergoing laparoscopic, vaginal, or abdominal hysterectomy before (n = 195) and after (n = 177) the decision aid was implemented.
Preoperative education. In the preoperative area, patients were uniformly educated regarding postoperative pain expectations (for example, it is normal to have some pain; the goal is to manage your pain so you can function; some women do not require opioid medications after surgery), risks of opioid medications (such as dependence or addiction; misuse of leftover pills by others), adverse effects (drowsiness; confusion), and the recommended postoperative pain management schedule.
Postoperatively, pain medications included ibuprofen around the clock, acetaminophen as needed (used with caution when hydrocodone with acetaminophen was also prescribed), and opioids only if needed.
Discharge medication planning. Using a visual scale, the investigators then educated patients regarding the maximum number of opioid tablets permitted to be prescribed according to department guidelines and the average number of opioid tablets that a typical patient uses. The number of opioid tablets prescribed varied based on route of hysterectomy (laparoscopic, abdominal, or vaginal). For example, for a laparoscopic hysterectomy, the maximum allowed prescription for oxycodone was 20 tablets, while patients used an average number of 10 tablets.
The patient was then asked to choose her desired number of tablets with which she would like to be discharged.
Structured telephone calls were made to patients 2 weeks postoperatively.
Impact of the decision aid on opioid prescribing
Before implementation of the decision aid, the average number of opioid pills prescribed at discharge was 25 (median, 20–35), while that number dropped to 10 (median, 10–15) after the aid’s implementation. Similarly, the average oral morphine equivalents (OMEs) at time of discharge was 150 (interquartile range [IQR], 120–200) before decision aid implementation and 75 (IQR, 25–150) after decision aid implementation. Similar reductions in average OMEs were observed before and after the aid’s implementation across the 3 hysterectomy routes.
Continue to: According to the type of opioid...
According to the type of opioid prescribed at discharge, hydrocodone 5 mg was prescribed in 99 cases (50.8%) before decision aid implementation and in 14 cases (7.9%) after implementation. By contrast, oxycodone 5 mg was prescribed in 85 cases (43.6%) before implementation and in 149 cases (84.2%) after implementation.
The number of refill requests was similar before (n = 11 [5.6%]) and after (n = 12 [6.8%]) the aid’s implementation.
Tool reduced opioid availability in the community
The use of a simple patient decision aid—which focuses on opioid education and engages patients in an appropriate postoperative pain management plan—can result in fewer opioid tablets in the community while still providing adequate pain control, the authors concluded.
Online resource. For more on targeted strategies to optimize opioid prescribing after surgery, visit the University of Michigan’s Opioid Prescribing Engagement Network (OPEN) at http://michigan-open.org.
- Vilkins A, Till S, Lim R, et al. The impact of shared decision making on post-hysterectomy opioid prescribing. Poster presented at: 47th AAGL Global Congress on Minimally Invasive Gynecology; November 11-15, 2018; Las Vegas, NV.
- Seth P, Scholl L, Rudd RA, et al. Overdose deaths involving opioids, cocaine, and psychostimulants—United States, 2015–2016. MMWR Morb Mortal Wkly Rep. 2018;67:349-358.
- Bateman BT, Cole NM, Maeda A, et al. Patterns of opioid prescription and use after cesarean delivery. Obstet Gynecol. 2017;130:29-35.
- As-Sanie S, Till S, Mowers EL, et al. Opioid prescribing patterns, patient use, and postoperative pain after hysterectomy for benign indications. Obstet Gynecol. 2017;130:1261-1268.
Investigators at the University of Michigan, Ann Arbor, found that a simple patient decision aid can be a useful tool in providing adequate postsurgical pain control to patients while reducing the number of opioid tablets in the community. The shared decision-making aid focuses on educating the patient about opioid use and engages her in an appropriate postoperative pain management plan. Results from this prospective quality improvement study were presented in a poster at the 47th AAGL Global Congress on Minimally Invasive Gynecology (Las Vegas, Nevada, November 11–15, 2018).1
Annmarie Vilkins, DO, and colleagues’ aim was to evaluate the impact of shared decision-making through the use of a patient decision aid targeting posthysterectomy pain management and opioid use. Can such a targeted strategy help decrease posthysterectomy opioid distribution in the community without compromising patient pain control or satisfaction?
The authors noted that more than 46 people die each day from an overdose involving prescription opioids.2 Studies have shown that patients actually use significantly fewer opioid tablets than the amount clinicians generally prescribe following ObGyn surgeries.3,4 Unused prescription opioid availability has the potential for accidental use or intentional misuse of the unneeded drugs by others.
Study methods
The investigators included all English-speaking patients undergoing hysterectomy for benign disease at their institution from March 1 through July 31, 2018. Data were analyzed from women undergoing laparoscopic, vaginal, or abdominal hysterectomy before (n = 195) and after (n = 177) the decision aid was implemented.
Preoperative education. In the preoperative area, patients were uniformly educated regarding postoperative pain expectations (for example, it is normal to have some pain; the goal is to manage your pain so you can function; some women do not require opioid medications after surgery), risks of opioid medications (such as dependence or addiction; misuse of leftover pills by others), adverse effects (drowsiness; confusion), and the recommended postoperative pain management schedule.
Postoperatively, pain medications included ibuprofen around the clock, acetaminophen as needed (used with caution when hydrocodone with acetaminophen was also prescribed), and opioids only if needed.
Discharge medication planning. Using a visual scale, the investigators then educated patients regarding the maximum number of opioid tablets permitted to be prescribed according to department guidelines and the average number of opioid tablets that a typical patient uses. The number of opioid tablets prescribed varied based on route of hysterectomy (laparoscopic, abdominal, or vaginal). For example, for a laparoscopic hysterectomy, the maximum allowed prescription for oxycodone was 20 tablets, while patients used an average number of 10 tablets.
The patient was then asked to choose her desired number of tablets with which she would like to be discharged.
Structured telephone calls were made to patients 2 weeks postoperatively.
Impact of the decision aid on opioid prescribing
Before implementation of the decision aid, the average number of opioid pills prescribed at discharge was 25 (median, 20–35), while that number dropped to 10 (median, 10–15) after the aid’s implementation. Similarly, the average oral morphine equivalents (OMEs) at time of discharge was 150 (interquartile range [IQR], 120–200) before decision aid implementation and 75 (IQR, 25–150) after decision aid implementation. Similar reductions in average OMEs were observed before and after the aid’s implementation across the 3 hysterectomy routes.
Continue to: According to the type of opioid...
According to the type of opioid prescribed at discharge, hydrocodone 5 mg was prescribed in 99 cases (50.8%) before decision aid implementation and in 14 cases (7.9%) after implementation. By contrast, oxycodone 5 mg was prescribed in 85 cases (43.6%) before implementation and in 149 cases (84.2%) after implementation.
The number of refill requests was similar before (n = 11 [5.6%]) and after (n = 12 [6.8%]) the aid’s implementation.
Tool reduced opioid availability in the community
The use of a simple patient decision aid—which focuses on opioid education and engages patients in an appropriate postoperative pain management plan—can result in fewer opioid tablets in the community while still providing adequate pain control, the authors concluded.
Online resource. For more on targeted strategies to optimize opioid prescribing after surgery, visit the University of Michigan’s Opioid Prescribing Engagement Network (OPEN) at http://michigan-open.org.
Investigators at the University of Michigan, Ann Arbor, found that a simple patient decision aid can be a useful tool in providing adequate postsurgical pain control to patients while reducing the number of opioid tablets in the community. The shared decision-making aid focuses on educating the patient about opioid use and engages her in an appropriate postoperative pain management plan. Results from this prospective quality improvement study were presented in a poster at the 47th AAGL Global Congress on Minimally Invasive Gynecology (Las Vegas, Nevada, November 11–15, 2018).1
Annmarie Vilkins, DO, and colleagues’ aim was to evaluate the impact of shared decision-making through the use of a patient decision aid targeting posthysterectomy pain management and opioid use. Can such a targeted strategy help decrease posthysterectomy opioid distribution in the community without compromising patient pain control or satisfaction?
The authors noted that more than 46 people die each day from an overdose involving prescription opioids.2 Studies have shown that patients actually use significantly fewer opioid tablets than the amount clinicians generally prescribe following ObGyn surgeries.3,4 Unused prescription opioid availability has the potential for accidental use or intentional misuse of the unneeded drugs by others.
Study methods
The investigators included all English-speaking patients undergoing hysterectomy for benign disease at their institution from March 1 through July 31, 2018. Data were analyzed from women undergoing laparoscopic, vaginal, or abdominal hysterectomy before (n = 195) and after (n = 177) the decision aid was implemented.
Preoperative education. In the preoperative area, patients were uniformly educated regarding postoperative pain expectations (for example, it is normal to have some pain; the goal is to manage your pain so you can function; some women do not require opioid medications after surgery), risks of opioid medications (such as dependence or addiction; misuse of leftover pills by others), adverse effects (drowsiness; confusion), and the recommended postoperative pain management schedule.
Postoperatively, pain medications included ibuprofen around the clock, acetaminophen as needed (used with caution when hydrocodone with acetaminophen was also prescribed), and opioids only if needed.
Discharge medication planning. Using a visual scale, the investigators then educated patients regarding the maximum number of opioid tablets permitted to be prescribed according to department guidelines and the average number of opioid tablets that a typical patient uses. The number of opioid tablets prescribed varied based on route of hysterectomy (laparoscopic, abdominal, or vaginal). For example, for a laparoscopic hysterectomy, the maximum allowed prescription for oxycodone was 20 tablets, while patients used an average number of 10 tablets.
The patient was then asked to choose her desired number of tablets with which she would like to be discharged.
Structured telephone calls were made to patients 2 weeks postoperatively.
Impact of the decision aid on opioid prescribing
Before implementation of the decision aid, the average number of opioid pills prescribed at discharge was 25 (median, 20–35), while that number dropped to 10 (median, 10–15) after the aid’s implementation. Similarly, the average oral morphine equivalents (OMEs) at time of discharge was 150 (interquartile range [IQR], 120–200) before decision aid implementation and 75 (IQR, 25–150) after decision aid implementation. Similar reductions in average OMEs were observed before and after the aid’s implementation across the 3 hysterectomy routes.
Continue to: According to the type of opioid...
According to the type of opioid prescribed at discharge, hydrocodone 5 mg was prescribed in 99 cases (50.8%) before decision aid implementation and in 14 cases (7.9%) after implementation. By contrast, oxycodone 5 mg was prescribed in 85 cases (43.6%) before implementation and in 149 cases (84.2%) after implementation.
The number of refill requests was similar before (n = 11 [5.6%]) and after (n = 12 [6.8%]) the aid’s implementation.
Tool reduced opioid availability in the community
The use of a simple patient decision aid—which focuses on opioid education and engages patients in an appropriate postoperative pain management plan—can result in fewer opioid tablets in the community while still providing adequate pain control, the authors concluded.
Online resource. For more on targeted strategies to optimize opioid prescribing after surgery, visit the University of Michigan’s Opioid Prescribing Engagement Network (OPEN) at http://michigan-open.org.
- Vilkins A, Till S, Lim R, et al. The impact of shared decision making on post-hysterectomy opioid prescribing. Poster presented at: 47th AAGL Global Congress on Minimally Invasive Gynecology; November 11-15, 2018; Las Vegas, NV.
- Seth P, Scholl L, Rudd RA, et al. Overdose deaths involving opioids, cocaine, and psychostimulants—United States, 2015–2016. MMWR Morb Mortal Wkly Rep. 2018;67:349-358.
- Bateman BT, Cole NM, Maeda A, et al. Patterns of opioid prescription and use after cesarean delivery. Obstet Gynecol. 2017;130:29-35.
- As-Sanie S, Till S, Mowers EL, et al. Opioid prescribing patterns, patient use, and postoperative pain after hysterectomy for benign indications. Obstet Gynecol. 2017;130:1261-1268.
- Vilkins A, Till S, Lim R, et al. The impact of shared decision making on post-hysterectomy opioid prescribing. Poster presented at: 47th AAGL Global Congress on Minimally Invasive Gynecology; November 11-15, 2018; Las Vegas, NV.
- Seth P, Scholl L, Rudd RA, et al. Overdose deaths involving opioids, cocaine, and psychostimulants—United States, 2015–2016. MMWR Morb Mortal Wkly Rep. 2018;67:349-358.
- Bateman BT, Cole NM, Maeda A, et al. Patterns of opioid prescription and use after cesarean delivery. Obstet Gynecol. 2017;130:29-35.
- As-Sanie S, Till S, Mowers EL, et al. Opioid prescribing patterns, patient use, and postoperative pain after hysterectomy for benign indications. Obstet Gynecol. 2017;130:1261-1268.