Supracondylar humerus fractures, which are the most common elbow fractures in the pediatric population, account for approximately 3% of all pediatric fractures.1 Complications of the injury or surgery include pin migration (2%), pin-site infection (1%), malunion, loss of reduction, compartment syndrome, nerve injury, and cubitus varus.1 A less frequently reported complication is avascular necrosis (AVN) of the trochlea.
First reported in 1948, posttraumatic deformity of the trochlea has appeared sparingly throughout the literature.2 This complication has been reported in varying fracture patterns and degrees of injury. The exact incidence is unknown because AVN of the humerus can occur without known trauma. The etiology of the deformity is thought to be interruption of the blood supply of the trochlea. Patterns include type A (AVN of the lateral ossification center) and type B (AVN of the entire medial crista along with a metaphyseal portion). Type A necrosis leads to early degenerative joint disease and loss of range of motion (ROM); angular deformities are uncommon. Type B AVN results in a progressive varus deformity of the trochlea.3 The deformities typically worsen as the child ages. Late-onset ulnar neuropathy can be seen, as medial condyle hypoplasia allows the ulnar nerve to move anterior with the medial head of the triceps. Treatment options address the sequelae and include observation, muscle strengthening, supracondylar osteotomy, and ulnar nerve transposition. Arthroscopic joint débridement has been shown, in short-term follow-up, to relieve pain and restore motion.4
We present 5 cases of AVN of the trochlea after supracondylar humerus fractures to highlight this unusual complication. Unlike more common complications of supracondylar humerus fractures, AVN of the trochlea can be a late clinical finding. We speculate that, in cases resulting from nondisplaced fractures, tamponade from fracture hematoma may play a role. It is important to keep this complication in the differential diagnosis of patients with a history of a supracondylar humerus fracture and unexplained elbow motion loss or pain.
Case Reports
Retrospective data were collected for all patients after approval by the institutional review board at our institution. Patients were identified by a computerized search using the Current Procedural Terminology code for closed reduction percutaneous pinning of supracondylar humerus fracture. The search was limited to patients treated at our institution from 2000 to 2012; 1159 patients were initially identified. Three patients were found to have postoperative AVN of the trochlea; 2 other patients were treated at an outside hospital and were identified by surgeon recall. These 5 cases are presented here.
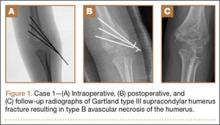
Case 1
A girl aged 5 years, 3 months sustained a Gartland type III supracondylar humerus fracture. She was originally seen at an outside facility and transferred to our tertiary care facility for definitive management. She underwent closed reduction and fixation with 3 lateral-based pins 1 day after her injury. Her pins and cast were removed 22 days postoperatively. She returned to full elbow function after her fracture care; 6 months later, she returned to the clinic with painless, decreased flexion of her elbow to 95º. Radiographs showed a lucency of the trochlea extending into the metaphysis (Figure 1). Thirteen months postoperatively, her examination was unchanged with motion at 0º to 95º; her radiographs showed a persistent lateral and medial lucency of the trochlea consistent with type B AVN involving the medial crista.
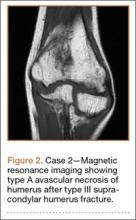
Case 2
An 8-year-old girl sustained a Gartland type III supracondylar humerus fracture that was treated at an outside facility with closed reduction and fixation with lateral pins. She had an uneventful postoperative course with painless return of motion. She presented 6 months after her surgery with progressive decreased ROM. She underwent conservative treatment with therapy and stretching without much improvement. She presented to our institution 4 years postoperatively with painless decreased motion from 40º to 110º. Radiographs showed dissolution of the lateral ossification center of the trochlea with a fishtail deformity consistent with type A AVN. Magnetic resonance imaging (MRI) confirmed AVN of the trochlea (Figure 2).
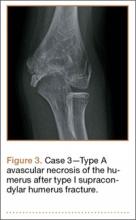
Case 3
A girl aged 5 years, 6 months sustained a Gartland type I supracondylar humerus fracture that was treated uneventfully by casting. She did not have a reduction or manipulation and healed without complications. She returned to the clinic 3 years after the injury complaining of intermittent elbow pain, neglect, and loss of motion. Her ROM was 0º to 110º. Radiographs showed dissolution of the lateral trochlea with sclerosis of the metaphysis consistent with a type A deformity (Figure 3). Contralateral radiographs were not obtained. MRI confirmed AVN of the trochlea.