Take-Home Points
- Proper patient selection is critical as extensive postoperative rehabilitation is required to obtain an excellent outcome.
- Open and arthroscopic approaches are effective treatment options for elbow contractures.
- Elbow stability must be restored to obtain a successful outcome.
- Knowledge of neurovascular anatomy is essential to prevent neurologic complications.
- Prophylactic ulnar nerve release should be considered, especially in patients with limited flexion.
Elbow stiffness has several etiologies, posttraumatic being the most common. Elbow stiffness can have debilitating functional effects necessitating treatment. In a biomechanical study of normal elbow function, Morrey and colleagues 1 determined that a flexion extension arc of 100° (30 °-130°) and a forearm rotation arc of 100° (50 ° pronation-50 ° supination) are required in 90% of activities of daily living. Similarly, elbow flexion of <105° was poorly tolerated, whereas patients could easier adapt to flexion contractures up to 40°. 2
The goal of initial evaluation should be to establish the cause of the contracture and the patient’s functional demands and ability to cooperate in the extensive postoperative rehabilitation that is essential in achieving an excellent functional outcome. In a thorough clinical examination, the clinician must note skin, range of motion (ROM), ligamentous stability, and neurovascular structures and give special attention to ulnar nerve function and symptoms. Mid-arc pain suggests additional intra-articular pathology, as stiffness typically causes pain only at the limits of motion as osteophytes impinge and soft tissue is under maximal tension. Routine elbow radiographs are required in all cases, and computed tomography (CT) can be useful in evaluating osseous sources of contracture. Suspected ligamentous instability and cartilaginous defects particularly in the setting of mid-arc pain are best evaluated with magnetic resonance imaging. 3
In this 5-point review, we evaluate treatment options as well as rehabilitation protocols in the management of elbow stiffness.
1 Anatomy of Contracture: The Usual Suspects
The cause of elbow stiffness is incompletely understood. Several posited contributing factors include biology, complex intra-articular anatomy, capsular distention favoring a flexed position, and tenuous postoperative fixation necessitating prolonged immobilization. Identifying intrinsic and extrinsic anatomical sources of stiffness can help guide treatment. 4 Intrinsic pathology includes intra-articular malunion, osteophytes, loose bodies, and adhesions; extrinsic pathology includes soft-tissue contracture, heterotopic ossification, and extra-articular malunion.
Compared with the normal elbow, the capsule becomes thickened and fibrotic and thereby prevents motion. Severe contractures, and extension contractures in particular, may require release of the posterior medial capsule and the posterior medial collateral ligament (MCL) to regain motion. In a series of 42 patients with flexion <100°, Park and colleagues 5 noted that all patients required release of the posterior band of the MCL to regain flexion. Other muscular impediments to motion include contracture of the brachialis and scarring of the triceps to the posterior humerus. Scarring of the triceps to the humerus can limit flexion.
In the posttrauma setting, intra-articular and extra-articular malunion must be considered. Extension malunion of the distal humerus can reduce flexion, 6 and shortening with compromise of the olecranon and coronoid fossae can limit both flexion and extension.
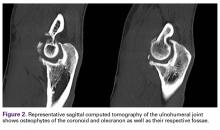
Last, heterotopic ossification and osteophytes should be assessed as potential causes of limited ROM. Both the coronoid process and the olecranon can develop osteophytes, and their respective fossae should be assessed with CT. Posterior impingement is rare at the tip of the olecranon; it occurs because of "widening" of the olecranon by "Mickey Mouse ear" osteophytes and bony encroachment along the medial and lateral columns. Thus, the olecranon must be narrowed and the fossa widened and deepened.
In case of concomitant ligament instability, we prefer to reconstruct the ligament first, and then perform contracture release as a staged procedure. We favor a staged approach because the rehabilitation regimens for instability and contracture release are diametrically opposed: Instability requires immobilization, and contracture release requires immediate motion. Last, incision placement and ulnar nerve management are crucial in minimizing the potential complications of the second procedure.
2 Nonoperative Treatment
In the absence of significant bony impediments to motion—such as heterotopic ossification or malunion—initial treatment should commence with nonoperative therapy. Therapy should be initiated as soon as concern for stiffness arises in order to prevent contracture. Initial nonoperative treatment can also serve as an important litmus test of postoperative adherence. Adequate patient relaxation is crucial in avoiding co-contracture resisting stretching forces. Passive ROM exercises use sustained force to allow time-dependent stress relaxation to increase tissue length as well as fatigue antagonist muscles. In addition, hold-and-relax techniques apply isometric resistance to induce relaxation of antagonist muscles. 7 Active ROM should emphasize triceps isolation and elbow extension to prevent scarring of the triceps to the posterior humerus.
Corrective splinting can be an effective adjuvant to physiotherapy. Static progressive turnbuckle splints was described as an effective treatment for both elbow flexion and extension contractures, effecting an average 43° increase in elbow motion in a series of 15 patients. 8 Similarly, Gelinas and colleagues 9 noted improvement among 22 patients treated with turnbuckle splinting for an average of 4.5 months. In addition, serial extension splints may be used in the treatment of elbow flexion contractures.
3 Open Contacture Release and Surgical Approach
When nonoperative therapies fail to restore the functional arc of motion, patients with flexion contractures or extension contractures of >30° may be indicated for contracture release. Surgical approach should be determined by meticulous preoperative planning that notes prior incisions and CT findings. It can be helpful to organize common offending structures and their effects on flexion and extension ( Table).
Careful attention to bony architecture and joint space can provide valuable information about motion impingement and arthrosis. In most cases, both the anterior compartment and the posterior compartment must be addressed, but this can often be achieved with a medial or lateral approach alone. Figure 1 shows a lateral radiograph of an active weightlifter with –10° of extension and 90° of flexion. CT showed osteophytes primarily over the anterior and posterior compartments of the ulnohumeral joint ( Figure 2 ). Ulnar nerve paresthesia dictated our approach from the medial side.A medial over-the-top approach uses the medial supracondylar ridge as a landmark, subperiosteally reflecting the brachialis anteriorly. 10 The ulnar nerve is neurolyzed and protected posteriorly. The flexor-pronator mass is split distally and elevated along with the brachialis as a single sleeve of muscle. The coronal plane of dissection should be the anterior half of the lateral epicondyle to avoid injury to the MCL. Large Bennett or Hohmann retractors can hinge on the lateral border of the humerus and provide clear visualization of the anterior capsule and the ulnohumeral joint. Exposure of the radiocapitellar joint is possible, but this joint is very deep in the operative field, and caution should be taken excising the anterolateral capsule because of the risk of radial nerve injury. The ulnar nerve can be temporarily transposed anteriorly to dissect posteriorly along the supracondylar ridge of the humerus. The triceps is reflected off the distal humerus. Occasionally, the posterior band of the MCL must be resected in severe extension contractures. If possible, the anterior bundle should be preserved. With this approach, the anterior capsule, distal humerus, coronoid process, posterior MCL, posterior capsule, and triceps can be addressed. The zone anterior to the radial head and the anterolateral and posterolateral capsule cannot be safely exposed with a medial approach. As described by Wada and colleagues, 11 a primarily medial approach resulted in an average 64° increase in arc of motion.
The lateral approach, commonly referred to as the column approach , uses the lateral supracondylar ridge to release distal fibers of the brachioradialis and the extensor carpi radialis longus (ECRL) ( Figure 3 ). This exposure is limited by the radial nerve proximally and the posterior interosseous the ECRL and the extensor carpi radialis brevis. After the ECRL and the distal brachioradialis are released from the humerus, the superolateral capsule is visualized. After the brachialis and the radial nerve are elevated off the capsule, the capsule can be safely excised extending medially. Limited forearm rotation can also be addressed, as the proximal radioulnar joint (PRUJ) and the radiocapitellar joint can be exposed through this approach. Given the limits of lateral exposure, in some cases we release the lateral ulnar collateral ligament to better "hinge" open the elbow and obtain better visualization of the PRUJ and the medial joint. In isolation, the ligament can be repaired with suture anchors without causing instability or delaying rehabilitation. Husband and Hastings 12 described a lateral approach with a mean 46° increased arc of motion—similar to the lateral column procedure with a mean 45° increased arc of motion, described by Mansat and Morrey. 13 Last, a single posterior approach with wide medial and lateral flaps can also be used, but this has the distinct disadvantage of a risk of seroma or hematoma owing to the large dead space created. We typically prefer to initially approach contractures medially, as this allows ulnar nerve symptoms to be addressed. A lateral approach can be added to address forearm rotation and facilitate protection of the radial nerve/PIN during anterolateral capsular release in significant flexion contractures. Presence of heterotopic ossification or extra-articular malunion must also be considered, as it may dictate the surgical approach. If circumferential release of the elbow soft tissue and complete stripping of the distal humerus are performed for contracture release, simple collateral ligament repairs will be inadequate in providing stability immediately after surgery. In these extreme circumstances, we prefer to protect the ligament repair withan internal joint stabilizer (Skeletal Dynamics) ( Figure 4 ) and to initiate motion therapy immediately. External fixation (hinged or unhinged is rarely used in our practice.
4 Arthroscopic Contracture Release and Technique
Recently, arthroscopic elbow contracture release, a technically demanding but effective treatment option, has gained popularity. Knowledge of neurovascular anatomy is a prerequisite to the prevention of devastating neurologic complications (ulnar, median, and radial nerve transections have been described 14,15). Relative contraindications include extensive heterotopic ossification, ulnar nerve transposition, and limited arthroscopic experience. Functional improvements as well as average 26 ° to 42° increases in arc of motion have been described with arthroscopic release. 16-18 In thin-framed patients with dense elbow capsular scarring (severe loss of elbow motion with hard block) and small joint space, arthroscopic release and particularly arthroscope insertion are notoriously difficult.
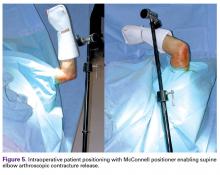
The patient may be placed in the prone, lateral decubitus, or supine position, depending on surgeon preference ( Figure 5 ). Before surgery, portals and the ulnar nerve should be carefully outlined. 19
The median, ulnar, and medial antebrachial cutaneous nerves are at risk during placement of the proximal anteromedial portal, and the radial and lateral antebrachial cutaneous nerves are at risk during proximal anterolateral portal placement. Ulnar nerve decompression may also be performed through a limited incision before arthroscopic contracture release, and the nerve is protected during use of the shaver along the posteromedial joint capsule. Fluid management is required to ensure proper visualization and avoid excessive swelling.We prefer to start by entering the posterior compartment and using the shaver to create a working space. All bone work and resectioning should be performed before capsular resection. After the joint and the olecranon fossa are identified, soft-tissue and bony débridement of the olecranon and the fossa can be performed. Care should be taken to protect the ulnar nerve when the posteromedial corner or medial gutter is approached.
The anterior compartment is then visualized through the proximal anteromedial portal, and a working anterolateral portal is established ( Figures 6A-6D ). Often, bone forms in the coronoid fossa and the supracapitellar area, and this bone is resected. After completion of the bone work, the capsule is released or resected. In osteoarthritis cases, the capsule is usually relatively normal, and simple release proximally or distally is sufficient. In posttraumatic stiffness, however, marked capsular thickening and arthrofibrosis may occur, and in these cases more thorough capsular resection is advised. The capsulectomy is begun anteromedially, where the brachialis protects the median nerve and the brachial vessels. As the lateral border of the brachialis is approached, extreme caution must be taken to prevent radial or PIN injury. After the brachioradialis is visualized, more aggressive resection can be performed. Last, given the high risk of superficial infection classically associated with elbow arthroscopy, portal sites must be tightly closed and drains retained until scant drainage is noted. 155 Additional Considerations
After surgery, the elbow is immobilized in maximal extension and supination with an anterior splint, and therapy is initiated either immediately or after temporary immobilization. 16,19,20 Regional anesthesia is crucial in obtaining adequate pain control and establishing an immediate postoperative therapy program. The utility of continuous passive motion (CPM) in postoperative protocols is controversial. A retrospective case-control study of 32 patients matched on age, diagnosis, and contraction severity found no benefit of CPM use, and increased costs and hospital length of stay, leading the authors to recommend against CPM use. 20
Neurovascular risks are associated with both open and arthroscopic elbow contracture release. Particularly concerning is the risk of traction ulnar neuropathy, described in upward of 20% of patients. 21 Anatomical studies have found decreases in cubital tunnel and ulnar nerve area as elbow flexion increases with corresponding increased intraneural pressure, 22 leading some authors to recommend prophylactic ulnar nerve release with limited preoperative flexion. 15 Nevertheless, despite transposition, ulnar nerve symptoms were noted in 8 of 40 patients who underwent open contracture release for posttraumatic loss of elbow flexion. 5 In a retrospective review of 164 open and arthroscopic elbow contracture releases, Williams and colleagues 21 noted an 8.1% rate of postoperative new-onset ulnar nerve symptoms. The rate of ulnar neuropathy was nonsignificantly elevated among patients with preoperative flexion of <100° (15.2% vs 3.7%; P = .057). Recently, a retrospective review of 564 consecutive arthroscopic contracture releases found a significantly higher rate of delayed-onset ulnar neuritis among patients without prophylactic ulnar nerve decompression or transposition (11% vs 3%; P < .001). 23 Further analysis revealed that, compared with decompression, ulnar nerve transposition did not offer additional benefit but was associated with a significantly higher rate of wound complications (19% vs 4%; P = .03). We favor prophylactic release, particularly in the setting of preoperative extension contracture. For open contracture release from the lateral approach, however, we do not routinely release the ulnar nerve unless there were preoperative symptoms.
Although open and arthroscopic contracture releases can provide durable outcomes in the setting of painless elbow stiffness, options are more limited in the treatment of the painful stiff elbow. Total elbow arthroplasty remains an option in low-demand elderly patients but is not without significant risk of complications. 24 In addition, durability concerns and postoperative restrictions make total elbow arthroplasty less attractive to younger patients. Interposition arthroplasty may be indicated as a salvage procedure in the treatment of a young or high-demand patient with a stiff painful elbow. 25 Elbow stability is crucial in obtaining a successful outcome, and data on optimal graft choices are limited.
Conclusion
Elbow stiffness, a common complication of trauma, significantly impairs activities of daily living. Early after trauma, therapy should be initiated to prevent contracture. In the absence of symptomatic arthritis, both open and arthroscopic contracture releases are effective surgical treatments in properly selected and motivated patients. Although more research is needed to establish the optimal surgical approach, severity and anatomical cause of contracture should guide decisions as to which approach to use. Having a thorough understanding of neurovascular anatomy and of prophylactic ulnar nerve decompression in the setting of limited preoperative flexion can mitigate complications.