User login
A new use for dating apps: Chasing STDs
Heather Meador and Anna Herber-Downey use dating apps on the job – and their boss knows it.
Both are public health nurses employed by Linn County Public Health in eastern Iowa. They’ve learned that dating apps are the most efficient way to inform users that people they previously met on the sites may have exposed them to sexually transmitted infections.
A nationwide surge in STIs, also known as STDs – with reported cases of gonorrhea and syphilis increasing 10% and 7%, respectively, from 2019 to 2020, according to the Centers for Disease Control and Prevention – isn’t sparing Iowa. The duo has found that the telephone call, a traditional method of contact tracing, no longer works well.
“When I started 12 years ago, we called everyone,” said Ms. Meador, the county health department’s clinical branch supervisor. “It’s getting harder and harder to just call someone on the phone.”
Even texting is ineffective, they said. And people aren’t necessarily answering messages on Facebook. The dating apps are where they’re at.
Because many people are meeting sex partners online – via sites like Grindr or Snapchat, which are headquartered in West Hollywood and Santa Monica, Calif., respectively – contact tracers often don’t have much information to go on, just a screen name or a picture.
So, about a year ago, Ms. Meador and her colleagues got approval from their bosses at the local level to build profiles on the app, through which they can contact the sex partners of infected people.
Traditionally, contact tracers interview people infected with an STI about their recent encounters and then reach out to those partners to tell them about the potential exposure.
Linn County contact tracers use the apps throughout their workday. Grindr, in particular, relies on geolocation, showing users matches who are close by. So the tracers use the apps when they’re out and about, hoping to wander into the same neighborhoods as the person diagnosed with an STI. Sometimes users “tap” the contract tracers to see whether they’re interested – in dating, that is.
When the public health officials spot someone they’re looking for, they send a message asking for a call. It’s a successful method: Ms. Herber-Downey estimated they make an initial contact 75% of the time.
Linn County’s decision to move online comes as STI rates rise nationally, funding to fight them falls, and people adopt new technologies to meet people and seek fun. “STIs are increasing way faster than the funding we have,” said Leo Parker, director of prevention programs for the National Coalition of STD Directors, all while public health departments – many underfunded – are grappling with new behaviors.
“Social media companies have billions; we have tens of thousands,” said Jeffrey Klausner, MD, MPH, a University of Southern California, Los Angeles, public health professor, who previously served as San Francisco’s director of STD prevention and control services. That funding disparity means few public health departments have staff members who can go online. “It’s only really in major cities that they have anyone who’s tasked for that,” Dr. Klausner said.
Even when departments have enough employees to take on the challenge, institutional support can be lacking. Some public health officials question employees who log into the apps. Dr. Klausner once testified on behalf of a Ventura County, Calif., contact tracer who was fired for using sex sites for work.
But with people migrating online to meet partners, following them there makes sense. “We’re now in a digital age,” Mr. Parker said. Individuals might not be out, or might be questioning their identity, making online venues comfortable, anonymous spaces for romance – which, in turn, means people are harder to reach face-to-face, at least at first.
What’s more, online spaces like Grindr are effective public health tools beyond contact tracing. They can be useful ways to get the word out about public health concerns.
Mr. Parker and the Linn County officials said public service announcements on dating apps – advocating for condom use or sharing the business hours for sexual health clinics – do seem to lead people to services. “We do have individuals coming in, saying, ‘I saw you had free testing. I saw it on Grindr,’ ” Mr. Parker said.
Grindr, which touts itself as the biggest dating app focused on LGBTQ+ people, pushes out messages and information to its members, said Jack Harrison-Quintana, director of Grindr for Equality. That engagement intensified during a 2015 meningitis outbreak among LGBTQ+ communities in Chicago, for example.
During that outbreak, the app sent citywide messages about vaccination. Then Mr. Harrison-Quintana took advantage of the service’s design: Using the site’s geolocating capabilities, Grindr workers targeted messages to specific neighborhoods. “We could go in and really go block to block and say, ‘Is this where the cases are showing up?’ ” he said. If so, they sent more messages to that area.
That campaign encouraged further efforts from the app, which regularly sends public health messages about everything from COVID-19 to monkeypox to the platform’s base of roughly 11 million monthly users. Grindr also allows users to display their HIV status and indicate whether they’re vaccinated against COVID, monkeypox, and meningitis.
There are a couple of things Grindr won’t do, however. The company won’t allow public health departments to create institutional accounts. And it won’t allow automated notifications about STI exposures to be sent to users.
That’s due to privacy concerns, the company said, despite calls from public health advocates to deploy better messaging features. Grindr believes that a government presence on the app would be too intrusive and that even anonymous notifications would allow users to trace infections back to their source. (When asked about public health officials who join the site on their own, company spokesperson Patrick Lenihan said: “Individuals are free to say something like ‘I’m a public health professional – ask me about my work!’ in their profile and are free to discuss sexual and public health matters however they see fit.”)
Grindr’s position – however disappointing to some in the public health world – reflects a longtime balancing act attempted by the private sector, which aims to square government concerns with users’ privacy interests.
Dr. Klausner pointed to a 1999 syphilis outbreak in San Francisco as one of the first times he saw how those interests could be at odds. The outbreak was traced to an AOL chatroom. Based on his research, Dr. Klausner said it seemed as though people could go online and “get a sex partner faster than you can get a pizza delivered.”
But persuading New York–based Time Warner, eventually AOL’s corporate parent, to cooperate was time-intensive and tricky – gaining entrée into the chatroom required help from the New York attorney general’s office.
The online industry has advanced since then, Dr. Klausner said. He helped one service develop a system to send digital postcards to potentially exposed people. “Congratulations, you got syphilis,” the postcards read. “They were edgy postcards,” he said, although some options were less “snarky.”
Overall, however, the dating app world is still “bifurcated,” he said. For public health efforts, apps that appeal to LGBTQ+ users are generally more helpful than those that predominantly cater to heterosexual clients.
That’s due to the community’s history with sexual health, explained Jen Hecht, a leader of Building Healthy Online Communities, a public health group partnering with dating apps. “Folks in the queer community have – what – 30, 40 years of thinking about HIV?” she said.
Even though STIs affect everyone, “the norm and the expectation is not there” for straight-focused dating apps, she said. Indeed, neither Match Group nor Bumble – the corporations with the biggest apps focused on heterosexual dating, both based in Texas – responded to multiple requests for comment from KHN.
But users, at least so far, seem to appreciate the app-based interventions. Mr. Harrison-Quintana said Grindr has landed on a just-the-facts approach to conveying health information. He has never received any backlash, “which has been very nice.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Heather Meador and Anna Herber-Downey use dating apps on the job – and their boss knows it.
Both are public health nurses employed by Linn County Public Health in eastern Iowa. They’ve learned that dating apps are the most efficient way to inform users that people they previously met on the sites may have exposed them to sexually transmitted infections.
A nationwide surge in STIs, also known as STDs – with reported cases of gonorrhea and syphilis increasing 10% and 7%, respectively, from 2019 to 2020, according to the Centers for Disease Control and Prevention – isn’t sparing Iowa. The duo has found that the telephone call, a traditional method of contact tracing, no longer works well.
“When I started 12 years ago, we called everyone,” said Ms. Meador, the county health department’s clinical branch supervisor. “It’s getting harder and harder to just call someone on the phone.”
Even texting is ineffective, they said. And people aren’t necessarily answering messages on Facebook. The dating apps are where they’re at.
Because many people are meeting sex partners online – via sites like Grindr or Snapchat, which are headquartered in West Hollywood and Santa Monica, Calif., respectively – contact tracers often don’t have much information to go on, just a screen name or a picture.
So, about a year ago, Ms. Meador and her colleagues got approval from their bosses at the local level to build profiles on the app, through which they can contact the sex partners of infected people.
Traditionally, contact tracers interview people infected with an STI about their recent encounters and then reach out to those partners to tell them about the potential exposure.
Linn County contact tracers use the apps throughout their workday. Grindr, in particular, relies on geolocation, showing users matches who are close by. So the tracers use the apps when they’re out and about, hoping to wander into the same neighborhoods as the person diagnosed with an STI. Sometimes users “tap” the contract tracers to see whether they’re interested – in dating, that is.
When the public health officials spot someone they’re looking for, they send a message asking for a call. It’s a successful method: Ms. Herber-Downey estimated they make an initial contact 75% of the time.
Linn County’s decision to move online comes as STI rates rise nationally, funding to fight them falls, and people adopt new technologies to meet people and seek fun. “STIs are increasing way faster than the funding we have,” said Leo Parker, director of prevention programs for the National Coalition of STD Directors, all while public health departments – many underfunded – are grappling with new behaviors.
“Social media companies have billions; we have tens of thousands,” said Jeffrey Klausner, MD, MPH, a University of Southern California, Los Angeles, public health professor, who previously served as San Francisco’s director of STD prevention and control services. That funding disparity means few public health departments have staff members who can go online. “It’s only really in major cities that they have anyone who’s tasked for that,” Dr. Klausner said.
Even when departments have enough employees to take on the challenge, institutional support can be lacking. Some public health officials question employees who log into the apps. Dr. Klausner once testified on behalf of a Ventura County, Calif., contact tracer who was fired for using sex sites for work.
But with people migrating online to meet partners, following them there makes sense. “We’re now in a digital age,” Mr. Parker said. Individuals might not be out, or might be questioning their identity, making online venues comfortable, anonymous spaces for romance – which, in turn, means people are harder to reach face-to-face, at least at first.
What’s more, online spaces like Grindr are effective public health tools beyond contact tracing. They can be useful ways to get the word out about public health concerns.
Mr. Parker and the Linn County officials said public service announcements on dating apps – advocating for condom use or sharing the business hours for sexual health clinics – do seem to lead people to services. “We do have individuals coming in, saying, ‘I saw you had free testing. I saw it on Grindr,’ ” Mr. Parker said.
Grindr, which touts itself as the biggest dating app focused on LGBTQ+ people, pushes out messages and information to its members, said Jack Harrison-Quintana, director of Grindr for Equality. That engagement intensified during a 2015 meningitis outbreak among LGBTQ+ communities in Chicago, for example.
During that outbreak, the app sent citywide messages about vaccination. Then Mr. Harrison-Quintana took advantage of the service’s design: Using the site’s geolocating capabilities, Grindr workers targeted messages to specific neighborhoods. “We could go in and really go block to block and say, ‘Is this where the cases are showing up?’ ” he said. If so, they sent more messages to that area.
That campaign encouraged further efforts from the app, which regularly sends public health messages about everything from COVID-19 to monkeypox to the platform’s base of roughly 11 million monthly users. Grindr also allows users to display their HIV status and indicate whether they’re vaccinated against COVID, monkeypox, and meningitis.
There are a couple of things Grindr won’t do, however. The company won’t allow public health departments to create institutional accounts. And it won’t allow automated notifications about STI exposures to be sent to users.
That’s due to privacy concerns, the company said, despite calls from public health advocates to deploy better messaging features. Grindr believes that a government presence on the app would be too intrusive and that even anonymous notifications would allow users to trace infections back to their source. (When asked about public health officials who join the site on their own, company spokesperson Patrick Lenihan said: “Individuals are free to say something like ‘I’m a public health professional – ask me about my work!’ in their profile and are free to discuss sexual and public health matters however they see fit.”)
Grindr’s position – however disappointing to some in the public health world – reflects a longtime balancing act attempted by the private sector, which aims to square government concerns with users’ privacy interests.
Dr. Klausner pointed to a 1999 syphilis outbreak in San Francisco as one of the first times he saw how those interests could be at odds. The outbreak was traced to an AOL chatroom. Based on his research, Dr. Klausner said it seemed as though people could go online and “get a sex partner faster than you can get a pizza delivered.”
But persuading New York–based Time Warner, eventually AOL’s corporate parent, to cooperate was time-intensive and tricky – gaining entrée into the chatroom required help from the New York attorney general’s office.
The online industry has advanced since then, Dr. Klausner said. He helped one service develop a system to send digital postcards to potentially exposed people. “Congratulations, you got syphilis,” the postcards read. “They were edgy postcards,” he said, although some options were less “snarky.”
Overall, however, the dating app world is still “bifurcated,” he said. For public health efforts, apps that appeal to LGBTQ+ users are generally more helpful than those that predominantly cater to heterosexual clients.
That’s due to the community’s history with sexual health, explained Jen Hecht, a leader of Building Healthy Online Communities, a public health group partnering with dating apps. “Folks in the queer community have – what – 30, 40 years of thinking about HIV?” she said.
Even though STIs affect everyone, “the norm and the expectation is not there” for straight-focused dating apps, she said. Indeed, neither Match Group nor Bumble – the corporations with the biggest apps focused on heterosexual dating, both based in Texas – responded to multiple requests for comment from KHN.
But users, at least so far, seem to appreciate the app-based interventions. Mr. Harrison-Quintana said Grindr has landed on a just-the-facts approach to conveying health information. He has never received any backlash, “which has been very nice.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Heather Meador and Anna Herber-Downey use dating apps on the job – and their boss knows it.
Both are public health nurses employed by Linn County Public Health in eastern Iowa. They’ve learned that dating apps are the most efficient way to inform users that people they previously met on the sites may have exposed them to sexually transmitted infections.
A nationwide surge in STIs, also known as STDs – with reported cases of gonorrhea and syphilis increasing 10% and 7%, respectively, from 2019 to 2020, according to the Centers for Disease Control and Prevention – isn’t sparing Iowa. The duo has found that the telephone call, a traditional method of contact tracing, no longer works well.
“When I started 12 years ago, we called everyone,” said Ms. Meador, the county health department’s clinical branch supervisor. “It’s getting harder and harder to just call someone on the phone.”
Even texting is ineffective, they said. And people aren’t necessarily answering messages on Facebook. The dating apps are where they’re at.
Because many people are meeting sex partners online – via sites like Grindr or Snapchat, which are headquartered in West Hollywood and Santa Monica, Calif., respectively – contact tracers often don’t have much information to go on, just a screen name or a picture.
So, about a year ago, Ms. Meador and her colleagues got approval from their bosses at the local level to build profiles on the app, through which they can contact the sex partners of infected people.
Traditionally, contact tracers interview people infected with an STI about their recent encounters and then reach out to those partners to tell them about the potential exposure.
Linn County contact tracers use the apps throughout their workday. Grindr, in particular, relies on geolocation, showing users matches who are close by. So the tracers use the apps when they’re out and about, hoping to wander into the same neighborhoods as the person diagnosed with an STI. Sometimes users “tap” the contract tracers to see whether they’re interested – in dating, that is.
When the public health officials spot someone they’re looking for, they send a message asking for a call. It’s a successful method: Ms. Herber-Downey estimated they make an initial contact 75% of the time.
Linn County’s decision to move online comes as STI rates rise nationally, funding to fight them falls, and people adopt new technologies to meet people and seek fun. “STIs are increasing way faster than the funding we have,” said Leo Parker, director of prevention programs for the National Coalition of STD Directors, all while public health departments – many underfunded – are grappling with new behaviors.
“Social media companies have billions; we have tens of thousands,” said Jeffrey Klausner, MD, MPH, a University of Southern California, Los Angeles, public health professor, who previously served as San Francisco’s director of STD prevention and control services. That funding disparity means few public health departments have staff members who can go online. “It’s only really in major cities that they have anyone who’s tasked for that,” Dr. Klausner said.
Even when departments have enough employees to take on the challenge, institutional support can be lacking. Some public health officials question employees who log into the apps. Dr. Klausner once testified on behalf of a Ventura County, Calif., contact tracer who was fired for using sex sites for work.
But with people migrating online to meet partners, following them there makes sense. “We’re now in a digital age,” Mr. Parker said. Individuals might not be out, or might be questioning their identity, making online venues comfortable, anonymous spaces for romance – which, in turn, means people are harder to reach face-to-face, at least at first.
What’s more, online spaces like Grindr are effective public health tools beyond contact tracing. They can be useful ways to get the word out about public health concerns.
Mr. Parker and the Linn County officials said public service announcements on dating apps – advocating for condom use or sharing the business hours for sexual health clinics – do seem to lead people to services. “We do have individuals coming in, saying, ‘I saw you had free testing. I saw it on Grindr,’ ” Mr. Parker said.
Grindr, which touts itself as the biggest dating app focused on LGBTQ+ people, pushes out messages and information to its members, said Jack Harrison-Quintana, director of Grindr for Equality. That engagement intensified during a 2015 meningitis outbreak among LGBTQ+ communities in Chicago, for example.
During that outbreak, the app sent citywide messages about vaccination. Then Mr. Harrison-Quintana took advantage of the service’s design: Using the site’s geolocating capabilities, Grindr workers targeted messages to specific neighborhoods. “We could go in and really go block to block and say, ‘Is this where the cases are showing up?’ ” he said. If so, they sent more messages to that area.
That campaign encouraged further efforts from the app, which regularly sends public health messages about everything from COVID-19 to monkeypox to the platform’s base of roughly 11 million monthly users. Grindr also allows users to display their HIV status and indicate whether they’re vaccinated against COVID, monkeypox, and meningitis.
There are a couple of things Grindr won’t do, however. The company won’t allow public health departments to create institutional accounts. And it won’t allow automated notifications about STI exposures to be sent to users.
That’s due to privacy concerns, the company said, despite calls from public health advocates to deploy better messaging features. Grindr believes that a government presence on the app would be too intrusive and that even anonymous notifications would allow users to trace infections back to their source. (When asked about public health officials who join the site on their own, company spokesperson Patrick Lenihan said: “Individuals are free to say something like ‘I’m a public health professional – ask me about my work!’ in their profile and are free to discuss sexual and public health matters however they see fit.”)
Grindr’s position – however disappointing to some in the public health world – reflects a longtime balancing act attempted by the private sector, which aims to square government concerns with users’ privacy interests.
Dr. Klausner pointed to a 1999 syphilis outbreak in San Francisco as one of the first times he saw how those interests could be at odds. The outbreak was traced to an AOL chatroom. Based on his research, Dr. Klausner said it seemed as though people could go online and “get a sex partner faster than you can get a pizza delivered.”
But persuading New York–based Time Warner, eventually AOL’s corporate parent, to cooperate was time-intensive and tricky – gaining entrée into the chatroom required help from the New York attorney general’s office.
The online industry has advanced since then, Dr. Klausner said. He helped one service develop a system to send digital postcards to potentially exposed people. “Congratulations, you got syphilis,” the postcards read. “They were edgy postcards,” he said, although some options were less “snarky.”
Overall, however, the dating app world is still “bifurcated,” he said. For public health efforts, apps that appeal to LGBTQ+ users are generally more helpful than those that predominantly cater to heterosexual clients.
That’s due to the community’s history with sexual health, explained Jen Hecht, a leader of Building Healthy Online Communities, a public health group partnering with dating apps. “Folks in the queer community have – what – 30, 40 years of thinking about HIV?” she said.
Even though STIs affect everyone, “the norm and the expectation is not there” for straight-focused dating apps, she said. Indeed, neither Match Group nor Bumble – the corporations with the biggest apps focused on heterosexual dating, both based in Texas – responded to multiple requests for comment from KHN.
But users, at least so far, seem to appreciate the app-based interventions. Mr. Harrison-Quintana said Grindr has landed on a just-the-facts approach to conveying health information. He has never received any backlash, “which has been very nice.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
The clitoris steps into the spotlight with major scientific discovery
The patients of Jill Krapf, MD, are often too embarrassed to tell her about discomfort in their clitoris.
“I ask all of my patients about clitoral pain, and it is often the first time they have ever been asked about this,” says Dr. Krapf, the associate director of the Center for Vulvovaginal Disorders, a private clinic in Washington and New York.
Dr. Krapf is an ob.gyn. who specializes in female sexual pain that involves the pelvis, vagina, and vulva.
Many of the conditions Dr. Krapf treats don’t have outward symptoms that appear abnormal, but internally, there are damaged or irritated nerves that can result in hypersensitivity, unwanted arousal, or pain.
“Most recent research indicates that even a herniated disk or tear in the spine can lead to clitoral or vulvar symptoms, just like sciatica pain that shoots down the leg is related to issues in the spine,” Dr. Krapf says.
Dr. Krapf was excited to read of a new discovery: Dr. Krapf and other doctors are hopeful that the attention to the clitoris will spark more interest and comprehensive education among people in their field. They also hope it will empower patients to seek medical help if they are having issues with their clitoris.
“Female sexual health has historically been underfunded, especially compared with male sexual health, like erectile dysfunction,” Dr. Krapf says. “Optimizing vulvar and vaginal health is not only necessary for sexual well-being.”
Blair Peters, MD, a plastic surgeon who specializes in gender-affirming care, led the study, which was presented at the Sexual Medicine Society of North America conference in October. Dr. Peters says he hopes that the new information decreases stigma that the clitoris is not worthy of the same medical attention that other organs of the body receive.
When the clitoris doesn’t properly function, there can be harm to a person’s physical and mental health. Paying attention to discomfort in the clitoris, and seeking medical attention, can help catch and prevent some urinary and vaginal infections.
“The fact that it took until 2022 for someone to do this work speaks to how little attention the clitoris has received,” says Dr. Peters, an assistant professor of surgery at the Oregon Health and Science University School of Medicine, Portland.
What’s inside?
Dr. Peters and his colleagues completed the study by taking clitoral nerve tissue from seven adult transgender men who had received gender-affirming genital surgery. The tissues were dyed and magnified 1,000 times under a microscope so the researchers could count nerve fibers.
Dr. Peters says the finding is important because many surgeries take place in the groin region – like hip replacements, episiotomies during childbirth, and pelvic mesh procedures – and the revived attention to the clitoris may help health care providers know where nerves are so that injuries from medical mistakes are prevented.
“Nerves are at risk of damage if it’s not understood where they are at all times,” he says.
Dr. Peters hopes the new finding will help create new surgical techniques for nerve repair and offer insight for gender-affirming phalloplasty, which is the surgical construction of a penis often for transmasculine people.
Ownership of the body part
When it comes to the clitoris, no one type of doctor has specialized in the sex organ.
Urologists, gynecologists, plastic surgeons, and sex therapists all address potential problems that can arise with the clitoris and its surrounding body parts. But specialists like Dr. Krapf are few and far between.
It wasn’t until 2005 that Australian urologist Helen O’Connell found that the clitoris is filled with erectile and non-erectile tissues that are often hidden in anatomy drawings by fat and bone. And it wasn’t until the early 2000s that researchers began delving in earnest into the anatomy of the clitoris and how it functions.
And a 2018 study showed that if more doctors examined the clitoris, they could identify issues like adhesions or infections in the area, most of which can be treated without surgery.
A body part built for pleasure
Randi Levinson, a sex, marriage, and family therapist in Los Angeles, sees patients who have less sensation in the clitoris or pain while having sex, many of whom have recently given birth or are going through menopause.
Women often become embarrassed when they can’t orgasm, or have less sensation in the clitoris, but tend to avoid seeking medical advice, she says. Normalizing discussions about women’s pleasure and the vast anatomy that supports it may help some of her patients.
“The more normal it is to talk about and explore women’s pleasure, the less shame women will have when getting help when they aren’t experiencing pleasure,” Ms. Levinson says. “I have many ... clients who experience pain and discomfort with sex [after pregnancy] and no longer feel pleasure and are concerned that something is wrong with them.”
A version of this article first appeared on WebMD.com.
The patients of Jill Krapf, MD, are often too embarrassed to tell her about discomfort in their clitoris.
“I ask all of my patients about clitoral pain, and it is often the first time they have ever been asked about this,” says Dr. Krapf, the associate director of the Center for Vulvovaginal Disorders, a private clinic in Washington and New York.
Dr. Krapf is an ob.gyn. who specializes in female sexual pain that involves the pelvis, vagina, and vulva.
Many of the conditions Dr. Krapf treats don’t have outward symptoms that appear abnormal, but internally, there are damaged or irritated nerves that can result in hypersensitivity, unwanted arousal, or pain.
“Most recent research indicates that even a herniated disk or tear in the spine can lead to clitoral or vulvar symptoms, just like sciatica pain that shoots down the leg is related to issues in the spine,” Dr. Krapf says.
Dr. Krapf was excited to read of a new discovery: Dr. Krapf and other doctors are hopeful that the attention to the clitoris will spark more interest and comprehensive education among people in their field. They also hope it will empower patients to seek medical help if they are having issues with their clitoris.
“Female sexual health has historically been underfunded, especially compared with male sexual health, like erectile dysfunction,” Dr. Krapf says. “Optimizing vulvar and vaginal health is not only necessary for sexual well-being.”
Blair Peters, MD, a plastic surgeon who specializes in gender-affirming care, led the study, which was presented at the Sexual Medicine Society of North America conference in October. Dr. Peters says he hopes that the new information decreases stigma that the clitoris is not worthy of the same medical attention that other organs of the body receive.
When the clitoris doesn’t properly function, there can be harm to a person’s physical and mental health. Paying attention to discomfort in the clitoris, and seeking medical attention, can help catch and prevent some urinary and vaginal infections.
“The fact that it took until 2022 for someone to do this work speaks to how little attention the clitoris has received,” says Dr. Peters, an assistant professor of surgery at the Oregon Health and Science University School of Medicine, Portland.
What’s inside?
Dr. Peters and his colleagues completed the study by taking clitoral nerve tissue from seven adult transgender men who had received gender-affirming genital surgery. The tissues were dyed and magnified 1,000 times under a microscope so the researchers could count nerve fibers.
Dr. Peters says the finding is important because many surgeries take place in the groin region – like hip replacements, episiotomies during childbirth, and pelvic mesh procedures – and the revived attention to the clitoris may help health care providers know where nerves are so that injuries from medical mistakes are prevented.
“Nerves are at risk of damage if it’s not understood where they are at all times,” he says.
Dr. Peters hopes the new finding will help create new surgical techniques for nerve repair and offer insight for gender-affirming phalloplasty, which is the surgical construction of a penis often for transmasculine people.
Ownership of the body part
When it comes to the clitoris, no one type of doctor has specialized in the sex organ.
Urologists, gynecologists, plastic surgeons, and sex therapists all address potential problems that can arise with the clitoris and its surrounding body parts. But specialists like Dr. Krapf are few and far between.
It wasn’t until 2005 that Australian urologist Helen O’Connell found that the clitoris is filled with erectile and non-erectile tissues that are often hidden in anatomy drawings by fat and bone. And it wasn’t until the early 2000s that researchers began delving in earnest into the anatomy of the clitoris and how it functions.
And a 2018 study showed that if more doctors examined the clitoris, they could identify issues like adhesions or infections in the area, most of which can be treated without surgery.
A body part built for pleasure
Randi Levinson, a sex, marriage, and family therapist in Los Angeles, sees patients who have less sensation in the clitoris or pain while having sex, many of whom have recently given birth or are going through menopause.
Women often become embarrassed when they can’t orgasm, or have less sensation in the clitoris, but tend to avoid seeking medical advice, she says. Normalizing discussions about women’s pleasure and the vast anatomy that supports it may help some of her patients.
“The more normal it is to talk about and explore women’s pleasure, the less shame women will have when getting help when they aren’t experiencing pleasure,” Ms. Levinson says. “I have many ... clients who experience pain and discomfort with sex [after pregnancy] and no longer feel pleasure and are concerned that something is wrong with them.”
A version of this article first appeared on WebMD.com.
The patients of Jill Krapf, MD, are often too embarrassed to tell her about discomfort in their clitoris.
“I ask all of my patients about clitoral pain, and it is often the first time they have ever been asked about this,” says Dr. Krapf, the associate director of the Center for Vulvovaginal Disorders, a private clinic in Washington and New York.
Dr. Krapf is an ob.gyn. who specializes in female sexual pain that involves the pelvis, vagina, and vulva.
Many of the conditions Dr. Krapf treats don’t have outward symptoms that appear abnormal, but internally, there are damaged or irritated nerves that can result in hypersensitivity, unwanted arousal, or pain.
“Most recent research indicates that even a herniated disk or tear in the spine can lead to clitoral or vulvar symptoms, just like sciatica pain that shoots down the leg is related to issues in the spine,” Dr. Krapf says.
Dr. Krapf was excited to read of a new discovery: Dr. Krapf and other doctors are hopeful that the attention to the clitoris will spark more interest and comprehensive education among people in their field. They also hope it will empower patients to seek medical help if they are having issues with their clitoris.
“Female sexual health has historically been underfunded, especially compared with male sexual health, like erectile dysfunction,” Dr. Krapf says. “Optimizing vulvar and vaginal health is not only necessary for sexual well-being.”
Blair Peters, MD, a plastic surgeon who specializes in gender-affirming care, led the study, which was presented at the Sexual Medicine Society of North America conference in October. Dr. Peters says he hopes that the new information decreases stigma that the clitoris is not worthy of the same medical attention that other organs of the body receive.
When the clitoris doesn’t properly function, there can be harm to a person’s physical and mental health. Paying attention to discomfort in the clitoris, and seeking medical attention, can help catch and prevent some urinary and vaginal infections.
“The fact that it took until 2022 for someone to do this work speaks to how little attention the clitoris has received,” says Dr. Peters, an assistant professor of surgery at the Oregon Health and Science University School of Medicine, Portland.
What’s inside?
Dr. Peters and his colleagues completed the study by taking clitoral nerve tissue from seven adult transgender men who had received gender-affirming genital surgery. The tissues were dyed and magnified 1,000 times under a microscope so the researchers could count nerve fibers.
Dr. Peters says the finding is important because many surgeries take place in the groin region – like hip replacements, episiotomies during childbirth, and pelvic mesh procedures – and the revived attention to the clitoris may help health care providers know where nerves are so that injuries from medical mistakes are prevented.
“Nerves are at risk of damage if it’s not understood where they are at all times,” he says.
Dr. Peters hopes the new finding will help create new surgical techniques for nerve repair and offer insight for gender-affirming phalloplasty, which is the surgical construction of a penis often for transmasculine people.
Ownership of the body part
When it comes to the clitoris, no one type of doctor has specialized in the sex organ.
Urologists, gynecologists, plastic surgeons, and sex therapists all address potential problems that can arise with the clitoris and its surrounding body parts. But specialists like Dr. Krapf are few and far between.
It wasn’t until 2005 that Australian urologist Helen O’Connell found that the clitoris is filled with erectile and non-erectile tissues that are often hidden in anatomy drawings by fat and bone. And it wasn’t until the early 2000s that researchers began delving in earnest into the anatomy of the clitoris and how it functions.
And a 2018 study showed that if more doctors examined the clitoris, they could identify issues like adhesions or infections in the area, most of which can be treated without surgery.
A body part built for pleasure
Randi Levinson, a sex, marriage, and family therapist in Los Angeles, sees patients who have less sensation in the clitoris or pain while having sex, many of whom have recently given birth or are going through menopause.
Women often become embarrassed when they can’t orgasm, or have less sensation in the clitoris, but tend to avoid seeking medical advice, she says. Normalizing discussions about women’s pleasure and the vast anatomy that supports it may help some of her patients.
“The more normal it is to talk about and explore women’s pleasure, the less shame women will have when getting help when they aren’t experiencing pleasure,” Ms. Levinson says. “I have many ... clients who experience pain and discomfort with sex [after pregnancy] and no longer feel pleasure and are concerned that something is wrong with them.”
A version of this article first appeared on WebMD.com.
Test strips ID fetal tissue in vaginal blood
A rapid test strip can accurately identify embryonic or fetal tissue in vaginal blood at the bedside, say authors of a paper published in Obstetrics and Gynecology.
The strip, called the ROM Plus test, can detect alpha-fetoprotein (AFP) and insulin-like growth factor–binding protein 1 (IGFBP-1) to identify the presence of the tissue, researchers say.
A positive test could help diagnose miscarriage and rule out ectopic pregnancy.
The ROM Plus test was originally created for diagnosing rupture of amniotic membranes and has been approved by the Food and Drug Administration. This study describes an off-label use of the test.
Lead author Michelle Volovsky, MD, of the department of obstetrics and gynecology at Maimonides Medical Center in Brooklyn, N.Y., said that in the current legal climate for abortion care, the test could have an additional use for women having vaginal bleeding.
“This test could be used as evidence to confirm that a miscarriage has occurred, and hence, a D&C (dilation and curettage) procedure in that case is not an induced abortion of a viable pregnancy,” Dr. Volovsky said.
Women in study
Three groups of reproductive-age women (totaling 90) were included in the study.
One was a negative control group consisting of nonpregnant women undergoing D&C or experiencing vaginal bleeding (n = 23). The positive control group of women had confirmed intrauterine pregnancy undergoing D&C (n = 31), and the third group was a study group of pregnant women with first-trimester bleeding (n = 36). Twelve women in the study group had confirmed ectopic pregnancies.
High sensitivity and specificity
Overall, 47 women had confirmed embryonic or fetal tissue in vaginal or uterine blood samples. The test strip was accurately positive in 45 of those 47 cases for a test sensitivity of 95.7%. The other 43 had confirmed absence of embryonic or fetal tissue in their vaginal or uterine blood samples.
The test had high specificity as well. “In the absence of embryonic or fetal tissue, such as vaginal blood sampled in cases of ectopic pregnancy, threatened or complete miscarriage, or nonpregnant individuals, the test strip had a specificity of 97.7% for obtaining a negative result,” the authors wrote.
The researchers noted that the high sensitivity and specificity were seen as all tests were performed in real-time, common clinical scenarios encountered in a high-volume, urban ob.gyn. unit.
First-trimester bleeding can be common
First-trimester bleeding occurs in 20%-40% of pregnancies and results in almost 500,000 emergency department visits in the United States every year, the authors wrote.
The most common causes include threatened miscarriage, but more serious etiologies include ectopic pregnancy.
Because criteria often are not met for ectopic pregnancy, many women are told they have a pregnancy of unknown location, which can lead to extensive and expensive follow-up.
“The current study was designed to offer a simple diagnostic alternative that does not require the use of an automated laboratory analyzer,” the authors wrote.
The test could be used by patients with confirmed intrauterine pregnancies at home – a highly desirable feature for people hesitant to come into medical offices or who live in remote areas, they noted.
Questions about test’s use
Lauren Thaxton, MD, assistant professor in the department of women’s health at the University of Texas at Austin, told this publication she sees the ease of use by patients at home as the biggest benefit of the test strips.
She said she’s not sure they would add much benefit otherwise because “we already have a pretty great way of identifying pregnancy tissue by floating the products of conception.”
She said the traditional “floating products” method is very inexpensive, involving a pan and strainer, and may be more comprehensive in that it can determine whether a miscarriage is finished.
She also wonders whether in the current legal climate of abortion laws, the test could be used not only to prove that an abortion didn’t happen but used as evidence the opposite way to criminalize abortion.
It’s unfortunate that we are evaluating new technology as ‘could this cause more harm than good?’ But I think it would be wrong not to recognize the long history of criminalization of abortion as well as the current reproductive health and policy climate,” Dr. Thaxton said.
Coauthors Amir Mor, MD, PhD, and Hugh Taylor, MD, hold U.S. patent rights related to the methods described in this article. Coauthor David Seifer, MD, received payment from the Women’s Integrated Network and Rutgers Medical School. In this article the authors describe off-label use of the ROM Plus test kit, produced by Laborie USA. This device was used to test vaginal blood for the presence of embryonic or fetal products. The other authors did not report any potential conflicts of interest. Dr. Thaxton reports no relevant financial relationships.
A rapid test strip can accurately identify embryonic or fetal tissue in vaginal blood at the bedside, say authors of a paper published in Obstetrics and Gynecology.
The strip, called the ROM Plus test, can detect alpha-fetoprotein (AFP) and insulin-like growth factor–binding protein 1 (IGFBP-1) to identify the presence of the tissue, researchers say.
A positive test could help diagnose miscarriage and rule out ectopic pregnancy.
The ROM Plus test was originally created for diagnosing rupture of amniotic membranes and has been approved by the Food and Drug Administration. This study describes an off-label use of the test.
Lead author Michelle Volovsky, MD, of the department of obstetrics and gynecology at Maimonides Medical Center in Brooklyn, N.Y., said that in the current legal climate for abortion care, the test could have an additional use for women having vaginal bleeding.
“This test could be used as evidence to confirm that a miscarriage has occurred, and hence, a D&C (dilation and curettage) procedure in that case is not an induced abortion of a viable pregnancy,” Dr. Volovsky said.
Women in study
Three groups of reproductive-age women (totaling 90) were included in the study.
One was a negative control group consisting of nonpregnant women undergoing D&C or experiencing vaginal bleeding (n = 23). The positive control group of women had confirmed intrauterine pregnancy undergoing D&C (n = 31), and the third group was a study group of pregnant women with first-trimester bleeding (n = 36). Twelve women in the study group had confirmed ectopic pregnancies.
High sensitivity and specificity
Overall, 47 women had confirmed embryonic or fetal tissue in vaginal or uterine blood samples. The test strip was accurately positive in 45 of those 47 cases for a test sensitivity of 95.7%. The other 43 had confirmed absence of embryonic or fetal tissue in their vaginal or uterine blood samples.
The test had high specificity as well. “In the absence of embryonic or fetal tissue, such as vaginal blood sampled in cases of ectopic pregnancy, threatened or complete miscarriage, or nonpregnant individuals, the test strip had a specificity of 97.7% for obtaining a negative result,” the authors wrote.
The researchers noted that the high sensitivity and specificity were seen as all tests were performed in real-time, common clinical scenarios encountered in a high-volume, urban ob.gyn. unit.
First-trimester bleeding can be common
First-trimester bleeding occurs in 20%-40% of pregnancies and results in almost 500,000 emergency department visits in the United States every year, the authors wrote.
The most common causes include threatened miscarriage, but more serious etiologies include ectopic pregnancy.
Because criteria often are not met for ectopic pregnancy, many women are told they have a pregnancy of unknown location, which can lead to extensive and expensive follow-up.
“The current study was designed to offer a simple diagnostic alternative that does not require the use of an automated laboratory analyzer,” the authors wrote.
The test could be used by patients with confirmed intrauterine pregnancies at home – a highly desirable feature for people hesitant to come into medical offices or who live in remote areas, they noted.
Questions about test’s use
Lauren Thaxton, MD, assistant professor in the department of women’s health at the University of Texas at Austin, told this publication she sees the ease of use by patients at home as the biggest benefit of the test strips.
She said she’s not sure they would add much benefit otherwise because “we already have a pretty great way of identifying pregnancy tissue by floating the products of conception.”
She said the traditional “floating products” method is very inexpensive, involving a pan and strainer, and may be more comprehensive in that it can determine whether a miscarriage is finished.
She also wonders whether in the current legal climate of abortion laws, the test could be used not only to prove that an abortion didn’t happen but used as evidence the opposite way to criminalize abortion.
It’s unfortunate that we are evaluating new technology as ‘could this cause more harm than good?’ But I think it would be wrong not to recognize the long history of criminalization of abortion as well as the current reproductive health and policy climate,” Dr. Thaxton said.
Coauthors Amir Mor, MD, PhD, and Hugh Taylor, MD, hold U.S. patent rights related to the methods described in this article. Coauthor David Seifer, MD, received payment from the Women’s Integrated Network and Rutgers Medical School. In this article the authors describe off-label use of the ROM Plus test kit, produced by Laborie USA. This device was used to test vaginal blood for the presence of embryonic or fetal products. The other authors did not report any potential conflicts of interest. Dr. Thaxton reports no relevant financial relationships.
A rapid test strip can accurately identify embryonic or fetal tissue in vaginal blood at the bedside, say authors of a paper published in Obstetrics and Gynecology.
The strip, called the ROM Plus test, can detect alpha-fetoprotein (AFP) and insulin-like growth factor–binding protein 1 (IGFBP-1) to identify the presence of the tissue, researchers say.
A positive test could help diagnose miscarriage and rule out ectopic pregnancy.
The ROM Plus test was originally created for diagnosing rupture of amniotic membranes and has been approved by the Food and Drug Administration. This study describes an off-label use of the test.
Lead author Michelle Volovsky, MD, of the department of obstetrics and gynecology at Maimonides Medical Center in Brooklyn, N.Y., said that in the current legal climate for abortion care, the test could have an additional use for women having vaginal bleeding.
“This test could be used as evidence to confirm that a miscarriage has occurred, and hence, a D&C (dilation and curettage) procedure in that case is not an induced abortion of a viable pregnancy,” Dr. Volovsky said.
Women in study
Three groups of reproductive-age women (totaling 90) were included in the study.
One was a negative control group consisting of nonpregnant women undergoing D&C or experiencing vaginal bleeding (n = 23). The positive control group of women had confirmed intrauterine pregnancy undergoing D&C (n = 31), and the third group was a study group of pregnant women with first-trimester bleeding (n = 36). Twelve women in the study group had confirmed ectopic pregnancies.
High sensitivity and specificity
Overall, 47 women had confirmed embryonic or fetal tissue in vaginal or uterine blood samples. The test strip was accurately positive in 45 of those 47 cases for a test sensitivity of 95.7%. The other 43 had confirmed absence of embryonic or fetal tissue in their vaginal or uterine blood samples.
The test had high specificity as well. “In the absence of embryonic or fetal tissue, such as vaginal blood sampled in cases of ectopic pregnancy, threatened or complete miscarriage, or nonpregnant individuals, the test strip had a specificity of 97.7% for obtaining a negative result,” the authors wrote.
The researchers noted that the high sensitivity and specificity were seen as all tests were performed in real-time, common clinical scenarios encountered in a high-volume, urban ob.gyn. unit.
First-trimester bleeding can be common
First-trimester bleeding occurs in 20%-40% of pregnancies and results in almost 500,000 emergency department visits in the United States every year, the authors wrote.
The most common causes include threatened miscarriage, but more serious etiologies include ectopic pregnancy.
Because criteria often are not met for ectopic pregnancy, many women are told they have a pregnancy of unknown location, which can lead to extensive and expensive follow-up.
“The current study was designed to offer a simple diagnostic alternative that does not require the use of an automated laboratory analyzer,” the authors wrote.
The test could be used by patients with confirmed intrauterine pregnancies at home – a highly desirable feature for people hesitant to come into medical offices or who live in remote areas, they noted.
Questions about test’s use
Lauren Thaxton, MD, assistant professor in the department of women’s health at the University of Texas at Austin, told this publication she sees the ease of use by patients at home as the biggest benefit of the test strips.
She said she’s not sure they would add much benefit otherwise because “we already have a pretty great way of identifying pregnancy tissue by floating the products of conception.”
She said the traditional “floating products” method is very inexpensive, involving a pan and strainer, and may be more comprehensive in that it can determine whether a miscarriage is finished.
She also wonders whether in the current legal climate of abortion laws, the test could be used not only to prove that an abortion didn’t happen but used as evidence the opposite way to criminalize abortion.
It’s unfortunate that we are evaluating new technology as ‘could this cause more harm than good?’ But I think it would be wrong not to recognize the long history of criminalization of abortion as well as the current reproductive health and policy climate,” Dr. Thaxton said.
Coauthors Amir Mor, MD, PhD, and Hugh Taylor, MD, hold U.S. patent rights related to the methods described in this article. Coauthor David Seifer, MD, received payment from the Women’s Integrated Network and Rutgers Medical School. In this article the authors describe off-label use of the ROM Plus test kit, produced by Laborie USA. This device was used to test vaginal blood for the presence of embryonic or fetal products. The other authors did not report any potential conflicts of interest. Dr. Thaxton reports no relevant financial relationships.
FROM OBSTETRICS AND GYNECOLOGY
Treating recurrent vulvovaginal candidiasis

Recurrent vulvovaginal candidiasis (RVVC) is a common cause of vaginitis and gynecologic morbidity in the United States and globally.1 RVVC is defined as at least 3 laboratory-confirmed (for example, culture, nucleic acid amplification test [NAAT]) symptomatic episodes in the previous 12 months.2 Common symptoms include vulvar pruritus, erythema, local skin and mucosal irritation, and abnormal discharge that may be thick and white or thin and watery.
The true incidence of RVVC is difficult to determine due to clinical diagnostic inaccuracy that results in over- and underdiagnosis of VVC and the general availability of over-the-counter topical antifungal medications that individuals who self-diagnose use to treat VVC.3
Causative organisms
Vulvovaginal yeast infections are caused by Candida species, a family of ubiquitous fungi that are a part of normal genitourinary and gastrointestinal flora.4 As such, these infections are commonly termed VVC. The presence of Candida species in the vagina without evidence of inflammation is not considered an infection but rather is more consistent with vaginal colonization. Inflammation in the setting of Candida species is what characterizes a true VVC infection.4
Candida albicans is responsible for the vast majority of VVC cases in the United States, with Candida glabrata accounting for most of the remaining infections.5 The majority of RVVC infections that are caused by C albicans are due to azole-sensitive strains (85%–95% of infections).2C glabrata, by contrast, is intrinsically resistant to azoles, which is thought primarily to be due to overexpression of drug efflux pumps that remove active drug from the cell.6,7
Why does VVC reoccur?
The pathogenesis of RVVC is not well understood. Predisposing factors may include frequent or recent antibiotic use, poorly controlled diabetes, immunodeficiency, and other host factors. However, many cases of RVVC are idiopathic and no predisposing or underlying conditions are identified.7
The role of genetic factors in predisposing to or triggering RVVC is unclear and is an area of ongoing investigation.2 Longitudinal DNA-typing studies suggest that recurrent disease is usually due to relapse from a persistent vaginal reservoir of organisms (that is, vaginal colonization) or endogenous reinfection with identical strains of susceptible C albicans.8,9 Symptomatic VVC likely results when the symbiotic balance between yeast and the normal vaginal microbiota is disrupted (by either Candida species overgrowth or changes in host immune factors).2 Less commonly, “recurrent” infections may in fact be due to azole-resistant Candida and non-Candida species.2
Clinical aspects and diagnosis of VVC
Signs and symptoms suggestive of VVC include vulvovaginal erythema, edema, vaginal discharge, vulvovaginal pruritus, and irritation. Given the lack of specificity of individual clinical findings in diagnosing VVC, or for distinguishing between other common causes of vaginitis (such as bacterial vaginosis and trichomoniasis), laboratory testing (that is, microscopy) should be performed in combination with a clinical exam in order to make a confident diagnosis of VVC.10 Self-diagnosis of VVC is inaccurate and is not recommended, as misdiagnosis and inappropriate treatment is cost ineffective, delays accurate diagnoses, and may contribute to growing azole resistance.
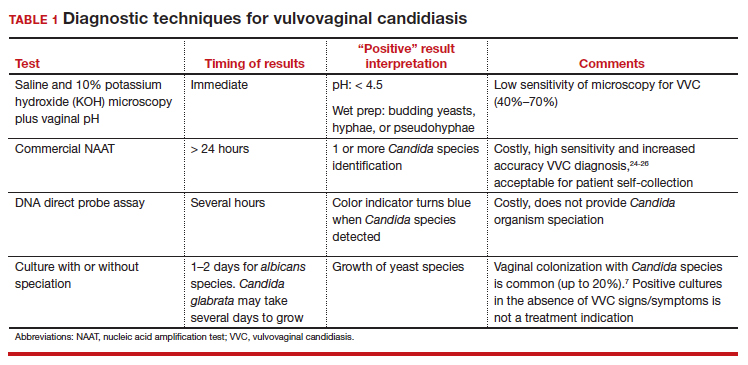
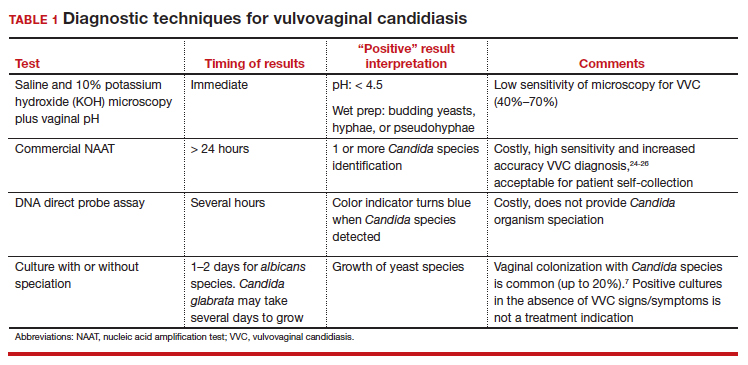
In patients with signs and symptoms of VVC, saline and potassium hydroxide microscopy should be performed.7 TABLE 1 summarizes other major diagnostic techniques for VVC.
Diagnostic considerations
Non-albicans Candida species, such as C glabrata, may be associated with minimally symptomatic or completely asymptomatic infections and may not be identified easily on wet mount as it does not form pseudohyphae or hyphae.11 Therefore, culture and susceptibility or NAAT testing is highly recommended for patients who remain symptomatic and/or have a nondiagnostic microscopy and a normal vaginal pH.7
Treatment options
Prior to May 2022, there had been no drugs approved by the US Food and Drug Administration (FDA) to treat RVVC. The mainstay of treatment is long-term maintenance therapy to achieve mycologic remission (TABLE 2).

In general, recurrent episodes of VVC should be treated with a longer duration of therapy (for example, oral fluconazole 150 mg every 72 hours for a total of 3 doses or topical azole for 7–14 days).7 If recurrent maintenance/suppressive therapy is started, the induction phase should be longer as well, at least 10 to 14 days with a topical or oral azole followed by a 6-month or longer course of weekly oral or topical azole therapy (such as 6–12 months).12,13
Patients with underlying immunodeficiency (such as poorly controlled diabetes, chronic corticosteroid treatment) may need prolonged courses of therapy. Correction of modifiable conditions and optimization of comorbidities should be prioritized—for example, optimized glucose control, weight loss, durable viral suppression, and so on. Of note, symptomatic VVC is more frequent among individuals with HIV and correlates with severity of immunodeficiency. Pharmacologic options for RVVC for individuals with HIV do not differ from standard recommendations.14
Fluconazole
Fluconazole is a safe, affordable, and convenient prescription oral medication that can be used for initial and maintenance/suppressive therapy.2 Fluconazole levels in vaginal secretions remain at therapeutic concentrations for at least 72 hours after a 150-mg dose.15 Induction therapy consists of oral fluconazole 150 mg every 72 hours for a total of 3 doses, followed by a maintenance regimen of a once-weekly dose of oral fluconazole 150 mg for a total of 6 months. Unfortunately, up to 55% of patients will experience a relapse in symptoms.12
Routine liver function test monitoring is not indicated for fluconazole maintenance therapy, but it should be performed if patients are treated with daily or long-term alternative oral azole medications, such as ketoconazole and itraconazole.
During pregnancy, only topical azole therapy is recommended for use, given the potential risk for adverse fetal outcomes, such as spontaneous abortion and congenital malformations, with fetal exposure to oral fluconazole ingested by the pregnant person.16 Fluconazole is present in breast milk, but it is safe to use during lactation when used at recommended doses.17
Continue to: Options for fluconazole-resistant C albicans infection...
Options for fluconazole-resistant C albicans infection
Patients who have RVVC with frequent and/or prolonged use of fluconazole are at risk for developing azole-resistant isolates of C albicans.12 For patients found to have azole-resistant infections, treatment options include increasing the azole dose based on isolate minimal inhibitory concentrations (MIC) to various antifungals, therapy with a non-fluconazole azole regimen, or switching to a different therapeutic drug class altogether.7
Options for non- albicans Candida species infection
Given the intrinsic resistance to azole therapy in some non-albicans Candida species (specifically C glabrata and Candida krusei), boric acid or nystatin regimens can be used. An induction course of vaginal boric acid is given as 600 mg per vagina daily for up to 14 days and is associated with a 70% rate of mycologic control.7 Boric acid is known to cause local irritation and dermatitis for both the patient and any sexual partners. If ingested orally, boric acid is associated with significant toxicity and even death.7
Vaginal nystatin also may be considered, with an induction course of 100,000 U for 14 days, with a similar regimen recommended for maintenance therapy. However, data are limited on maintenance regimens for RVVC due to non-albicans Candida species.2
Gentian violet
Gentian violet is a topical antiseptic agent that is available over the counter. Use of this agent is uncommon given the availability of highly effective azole-based therapy. Although useful due to its antipruritic properties, gentian violet can be messy to use and tends to stain clothing permanently.
Gentian violet use may be considered in cases of refractory RVVC with or without azole-resistant infections; it is applied as a 1% or 2% solution directly to affected areas for 10 to 14 days.18
Lactobacilli probiotics and dietary changes
Data that support the oral and/or vaginal use of probiotics that contain live lactobacilli are conflicting. In the absence of conclusive evidence to support probiotic use to treat and prevent RVVC, as well as variable quality of available products, use of these agents is not recommended.19
No controlled studies have evaluated the role of various diets in preventing RVVC; thus, no specific dietary changes are recommended.
Behavioral therapy
Available evidence does not support the treatment of sexual partners of patients with RVVC.7
Continue to: What’s new in treatment?...
What’s new in treatment?
Until recently, the main standard of care for RVVC has been oral fluconazole-based therapy. For patients whose symptoms do not respond to oral fluconazole therapy, oteseconazole is now available as a noninferior treatment option to fluconazole for both induction and maintenance therapy. Like other azoles, oteseconazole works by inhibiting a fungal enzyme (CYP51) that is essential in fungal cell membrane integrity and fungal growth.20 Oteseconazole is a more selective inhibitor of the fungal CYP51 enzyme and has demonstrated excellent potency against Candida species in in vitro pharmacologic studies.21
In a phase 3 study that evaluated the safety and efficacy of oteseconazole in the treatment and prevention of RVVC, oteseconazole was found to be both safe and efficacious in both the induction and maintenance phases of treatment for RVVC.20 In this trial, induction and maintenance with oteseconazole was compared with induction with fluconazole and placebo maintenance. Among the 185 participants with culture-verified RVVC, the oteseconazole regimen (n = 123) was associated with fewer recurrences of culture-verified VVC infections than was the fluconazole induction/placebo maintenance regimen (n = 62) during the 48-week maintenance phase of therapy (5% vs 42%).20
Single- and dual-drug dosing regimens of oteseconazole are recommended based on previous trial data that compared safety and efficacy of oteseconazole versus fluconazole induction therapy and oteseconazole versus placebo maintenance therapy.22 However, widespread use of oteseconazole regimens are limited due to its higher costs and limited access to the drug outside of a research setting.20
Single-drug induction therapy with oteseconazole consists of a single 600-mg oral dose on day 1 followed by a second dose of 450 mg orally on day 2. Starting on day 14, maintenance therapy starts with a single oral dose of 150 mg and is continued weekly for 11 weeks.22
Dual-drug induction therapy consists of oral fluconazole 150 mg on days 1, 4, and 7 followed by daily dosing of oral oteseconazole 150 mg on days 14 through 20. Then, starting on day 28, weekly dosing of oral oteseconazole 150 mg is continued for 11 weeks.22
Effects on pregnancy and lactation. Concerns of oteseconazole’s fetal teratogenicity are based on animal reproduction studies that reported ocular abnormalities from in utero exposure. Human data are insufficient to determine if oteseconazole is excreted in breast milk or what its effects are on milk production. Among breastfed infants whose mothers were exposed to oteseconazole during lactation, no adverse outcomes were reported, but follow up of oteseconazole-exposed infants was limited. 22 Therefore, use of oteseconazole among pregnant and/or lactating persons with RVVC is contraindicated at this time. The long-half life (approximately 138 days) of oteseconazole may preclude use among persons attempting pregnancy. 22
Other therapies. The other common classes of antifungal therapy used in the treatment of RVVC include the polyenes (for example, amphotericin B) and echinocandins (such as caspofungin) drug classes. Emerging azole-resistance among Candida species has been recognized as a significant concern from the Centers for Disease Control and Prevention. 7 Echinocandins, which are generally better tolerated and have a lower adverse side effect profile than polyenes, are a promising therapeutic class, but currently they are limited to intravenous options. SCY-078, a novel oral echinocandin in development, has shown in vitro fungicidal activity against multiple albicans and non-albicans Candida species in pharmacokinetic/pharmacodynamic studies.23
Continued development of alternative, non-azole-based therapies for Candida species is needed.●
- Sobel JD. Epidemiology and pathogenesis of recurrent vulvovaginal candidiasis. Am J Obstet Gynecol. 1985;152(7 pt 2):924-935. doi:10.1016/S0002-9378(85)80003-x
- Sobel JD. Recurrent vulvovaginal candidiasis. Am J Obstet Gynecol. 2016;214:15-21. doi:10.1016/j.ajog.2015.06.067
- Rathod SD, Buffler PA. Highly-cited estimates of the cumulative incidence and recurrence of vulvovaginal candidiasis are inadequately documented. BMC Womens Health. 2014;14:43. doi:10.1186/1472-6874-14-43
- Eckert LO, Lentz GM. Genital tract infections: vulva, vagina, cervix, toxic shock syndrome, endometritis, and salpingitis. In: Gershenson DM, Lentz GM, Valea FA, et al, eds. Comprehensive Gynecology. 8th ed. Elsevier; 2022:515-542.
- Gonçalves B, Ferreira C, Alves CT, et al. Vulvovaginal candidiasis: epidemiology, microbiology and risk factors. Crit Rev Microbiol. 2016;42:905-927. doi:10.3109/1040841X.2015.1091805
- Sobel JD, Sobel R. Current treatment options for vulvovaginal candidiasis caused by azole-resistant Candida species. Expert Opin Pharmacother. 2018;19:971-977. doi:10.1080/14656566.2018.1476490
- Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep. 2021;70:1-187. doi:10.15585/mmwr.rr7004a1
- Vazquez JA, Sobel JD, Demitriou R, et al. Karyotyping of Candida albicans isolates obtained longitudinally in women with recurrent vulvovaginal candidiasis. J Infect Dis. 1994;170:1566-1569. doi:10.1093/infdis/170.6.1566
- Lockhart SR, Reed BD, Pierson CL, et al. Most frequent scenario for recurrent Candida vaginitis is strain maintenance with “substrain shuffling”: demonstration by sequential DNA fingerprinting with probes Ca3, C1, and CARE2. J Clin Microbiol. 1996;34:767-777. doi:10.1128/jcm.34.4.767-777.1996
- Anderson MR, Klink K, Cohrssen A. Evaluation of vaginal complaints. JAMA. 2004;291:1368-1379. doi:10.1001/jama.291.11.1368
- Sobel JD. Vulvovaginal candidosis. Lancet. 2007;369:1961-1971. doi:10.1016/S0140-6736(07)60917-9
- Collins LM, Moore R, Sobel JD. Prognosis and long-term outcome of women with idiopathic recurrent vulvovaginal candidiasis caused by Candida albicans. J Low Genit Tract Dis. 2020;24:48-52. doi:10.1097/LGT.0000000000000496
- Pappas PG, Kauffman CA, Andes DR, et al. Clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis. 2016;62:e1-50. doi:10.1093/cid/civ933
- Duerr A, Heilig CM, Meikle SF, et al; HER Study Group. Incident and persistent vulvovaginal candidiasis among human immunodeficiency virus–infected women: risk factors and severity. Obstet Gynecol. 2003;101:548-556. doi:10.1016/s0029-7844(02)02729-1
- Houang ET, Chappatte O, Byrne D, et al. Fluconazole levels in plasma and vaginal secretions of patients after a 150-milligram single oral dose and rate of eradication of infection in vaginal candidiasis. Antimicrob Agents Chemother. 1990;34:909-910. doi:10.1128/AAC.34.5.909
- Bérard A, Sheehy O, Zhao JP, et al. Associations between low- and high-dose oral fluconazole and pregnancy outcomes: 3 nested case-control studies. CMAJ. 2019;191:E179-E187. doi:10.1503/cmaj.180963
- Fluconazole. In: Drugs and Lactation Database (LactMed). National Library of Medicine (US); 2006. Revised October 31, 2018. Accessed September 23, 2022. http://www.ncbi.nlm.nih.gov/books/NBK501223/
- White DJ, Johnson EM, Warnock DW. Management of persistent vulvo vaginal candidosis due to azole-resistant Candida glabrata. Genitourin Med. 1993;69:112-114. doi:10.1136/sti.69.2.112
- Falagas ME, Betsi GI, Athanasiou S. Probiotics for prevention of recurrent vulvovaginal candidiasis: a review. J Antimicrob Chemother. 2006;58:266-272. doi:10.1093/jac/dkl246
- Martens MG, Maximos B, Degenhardt T, et al. Phase 3 study evaluating the safety and efficacy of oteseconazole in the treatment of recurrent vulvovaginal candidiasis and acute vulvovaginal candidiasis infections. Am J Obstet Gynecol. 2022:S0002-9378(22)005774. doi:10.1016/j.ajog.2022.07.023
- Sobel JD, Nyirjesy P. Oteseconazole: an advance in treatment of recurrent vulvovaginal candidiasis. Future Microbiol. 2021;16:1453-1461. doi:10.2217/fmb-2021-0173
- Vivjoa (oteseconazole). Prescribing information. Mycovia Pharmaceuticals, Inc. April 2022. https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/215888s000lbl.pdf
- Scorneaux B, Angulo D, Borroto-Esoda K, et al. SCY-078 is fungicidal against Candida species in time-kill studies. Antimicrob Agents Chemother. 2017;61:e01961-16. doi:10.1128/AAC.01961-16
- Schwebke JR, Taylor SN, Ackerman R, et al. Clinical validation of the Aptima bacterial vaginosis and Aptima Candida/Trichomonas vaginitis assays: results from a prospective multicenter clinical study. J Clin Microbiol. 2020;58:e01643-19. doi:10.1128/JCM.01643-19
- Schwebke JR, Gaydos CA, Nyirjesy P, et al. Diagnostic performance of a molecular test versus clinician assessment of vaginitis. J Clin Microbiol. 2018;56:e00252-18. doi:10.1128/JCM.00252-18
- Broache M, Cammarata CL, Stonebraker E, et al. Performance of a vaginal panel assay compared with the clinical diagnosis of vaginitis. Obstet Gynecol. 2021;138:853-859. doi:10.1097/AOG.0000000000004592

Recurrent vulvovaginal candidiasis (RVVC) is a common cause of vaginitis and gynecologic morbidity in the United States and globally.1 RVVC is defined as at least 3 laboratory-confirmed (for example, culture, nucleic acid amplification test [NAAT]) symptomatic episodes in the previous 12 months.2 Common symptoms include vulvar pruritus, erythema, local skin and mucosal irritation, and abnormal discharge that may be thick and white or thin and watery.
The true incidence of RVVC is difficult to determine due to clinical diagnostic inaccuracy that results in over- and underdiagnosis of VVC and the general availability of over-the-counter topical antifungal medications that individuals who self-diagnose use to treat VVC.3
Causative organisms
Vulvovaginal yeast infections are caused by Candida species, a family of ubiquitous fungi that are a part of normal genitourinary and gastrointestinal flora.4 As such, these infections are commonly termed VVC. The presence of Candida species in the vagina without evidence of inflammation is not considered an infection but rather is more consistent with vaginal colonization. Inflammation in the setting of Candida species is what characterizes a true VVC infection.4
Candida albicans is responsible for the vast majority of VVC cases in the United States, with Candida glabrata accounting for most of the remaining infections.5 The majority of RVVC infections that are caused by C albicans are due to azole-sensitive strains (85%–95% of infections).2C glabrata, by contrast, is intrinsically resistant to azoles, which is thought primarily to be due to overexpression of drug efflux pumps that remove active drug from the cell.6,7
Why does VVC reoccur?
The pathogenesis of RVVC is not well understood. Predisposing factors may include frequent or recent antibiotic use, poorly controlled diabetes, immunodeficiency, and other host factors. However, many cases of RVVC are idiopathic and no predisposing or underlying conditions are identified.7
The role of genetic factors in predisposing to or triggering RVVC is unclear and is an area of ongoing investigation.2 Longitudinal DNA-typing studies suggest that recurrent disease is usually due to relapse from a persistent vaginal reservoir of organisms (that is, vaginal colonization) or endogenous reinfection with identical strains of susceptible C albicans.8,9 Symptomatic VVC likely results when the symbiotic balance between yeast and the normal vaginal microbiota is disrupted (by either Candida species overgrowth or changes in host immune factors).2 Less commonly, “recurrent” infections may in fact be due to azole-resistant Candida and non-Candida species.2
Clinical aspects and diagnosis of VVC
Signs and symptoms suggestive of VVC include vulvovaginal erythema, edema, vaginal discharge, vulvovaginal pruritus, and irritation. Given the lack of specificity of individual clinical findings in diagnosing VVC, or for distinguishing between other common causes of vaginitis (such as bacterial vaginosis and trichomoniasis), laboratory testing (that is, microscopy) should be performed in combination with a clinical exam in order to make a confident diagnosis of VVC.10 Self-diagnosis of VVC is inaccurate and is not recommended, as misdiagnosis and inappropriate treatment is cost ineffective, delays accurate diagnoses, and may contribute to growing azole resistance.
In patients with signs and symptoms of VVC, saline and potassium hydroxide microscopy should be performed.7 TABLE 1 summarizes other major diagnostic techniques for VVC.
Diagnostic considerations
Non-albicans Candida species, such as C glabrata, may be associated with minimally symptomatic or completely asymptomatic infections and may not be identified easily on wet mount as it does not form pseudohyphae or hyphae.11 Therefore, culture and susceptibility or NAAT testing is highly recommended for patients who remain symptomatic and/or have a nondiagnostic microscopy and a normal vaginal pH.7
Treatment options
Prior to May 2022, there had been no drugs approved by the US Food and Drug Administration (FDA) to treat RVVC. The mainstay of treatment is long-term maintenance therapy to achieve mycologic remission (TABLE 2).

In general, recurrent episodes of VVC should be treated with a longer duration of therapy (for example, oral fluconazole 150 mg every 72 hours for a total of 3 doses or topical azole for 7–14 days).7 If recurrent maintenance/suppressive therapy is started, the induction phase should be longer as well, at least 10 to 14 days with a topical or oral azole followed by a 6-month or longer course of weekly oral or topical azole therapy (such as 6–12 months).12,13
Patients with underlying immunodeficiency (such as poorly controlled diabetes, chronic corticosteroid treatment) may need prolonged courses of therapy. Correction of modifiable conditions and optimization of comorbidities should be prioritized—for example, optimized glucose control, weight loss, durable viral suppression, and so on. Of note, symptomatic VVC is more frequent among individuals with HIV and correlates with severity of immunodeficiency. Pharmacologic options for RVVC for individuals with HIV do not differ from standard recommendations.14
Fluconazole
Fluconazole is a safe, affordable, and convenient prescription oral medication that can be used for initial and maintenance/suppressive therapy.2 Fluconazole levels in vaginal secretions remain at therapeutic concentrations for at least 72 hours after a 150-mg dose.15 Induction therapy consists of oral fluconazole 150 mg every 72 hours for a total of 3 doses, followed by a maintenance regimen of a once-weekly dose of oral fluconazole 150 mg for a total of 6 months. Unfortunately, up to 55% of patients will experience a relapse in symptoms.12
Routine liver function test monitoring is not indicated for fluconazole maintenance therapy, but it should be performed if patients are treated with daily or long-term alternative oral azole medications, such as ketoconazole and itraconazole.
During pregnancy, only topical azole therapy is recommended for use, given the potential risk for adverse fetal outcomes, such as spontaneous abortion and congenital malformations, with fetal exposure to oral fluconazole ingested by the pregnant person.16 Fluconazole is present in breast milk, but it is safe to use during lactation when used at recommended doses.17
Continue to: Options for fluconazole-resistant C albicans infection...
Options for fluconazole-resistant C albicans infection
Patients who have RVVC with frequent and/or prolonged use of fluconazole are at risk for developing azole-resistant isolates of C albicans.12 For patients found to have azole-resistant infections, treatment options include increasing the azole dose based on isolate minimal inhibitory concentrations (MIC) to various antifungals, therapy with a non-fluconazole azole regimen, or switching to a different therapeutic drug class altogether.7
Options for non- albicans Candida species infection
Given the intrinsic resistance to azole therapy in some non-albicans Candida species (specifically C glabrata and Candida krusei), boric acid or nystatin regimens can be used. An induction course of vaginal boric acid is given as 600 mg per vagina daily for up to 14 days and is associated with a 70% rate of mycologic control.7 Boric acid is known to cause local irritation and dermatitis for both the patient and any sexual partners. If ingested orally, boric acid is associated with significant toxicity and even death.7
Vaginal nystatin also may be considered, with an induction course of 100,000 U for 14 days, with a similar regimen recommended for maintenance therapy. However, data are limited on maintenance regimens for RVVC due to non-albicans Candida species.2
Gentian violet
Gentian violet is a topical antiseptic agent that is available over the counter. Use of this agent is uncommon given the availability of highly effective azole-based therapy. Although useful due to its antipruritic properties, gentian violet can be messy to use and tends to stain clothing permanently.
Gentian violet use may be considered in cases of refractory RVVC with or without azole-resistant infections; it is applied as a 1% or 2% solution directly to affected areas for 10 to 14 days.18
Lactobacilli probiotics and dietary changes
Data that support the oral and/or vaginal use of probiotics that contain live lactobacilli are conflicting. In the absence of conclusive evidence to support probiotic use to treat and prevent RVVC, as well as variable quality of available products, use of these agents is not recommended.19
No controlled studies have evaluated the role of various diets in preventing RVVC; thus, no specific dietary changes are recommended.
Behavioral therapy
Available evidence does not support the treatment of sexual partners of patients with RVVC.7
Continue to: What’s new in treatment?...
What’s new in treatment?
Until recently, the main standard of care for RVVC has been oral fluconazole-based therapy. For patients whose symptoms do not respond to oral fluconazole therapy, oteseconazole is now available as a noninferior treatment option to fluconazole for both induction and maintenance therapy. Like other azoles, oteseconazole works by inhibiting a fungal enzyme (CYP51) that is essential in fungal cell membrane integrity and fungal growth.20 Oteseconazole is a more selective inhibitor of the fungal CYP51 enzyme and has demonstrated excellent potency against Candida species in in vitro pharmacologic studies.21
In a phase 3 study that evaluated the safety and efficacy of oteseconazole in the treatment and prevention of RVVC, oteseconazole was found to be both safe and efficacious in both the induction and maintenance phases of treatment for RVVC.20 In this trial, induction and maintenance with oteseconazole was compared with induction with fluconazole and placebo maintenance. Among the 185 participants with culture-verified RVVC, the oteseconazole regimen (n = 123) was associated with fewer recurrences of culture-verified VVC infections than was the fluconazole induction/placebo maintenance regimen (n = 62) during the 48-week maintenance phase of therapy (5% vs 42%).20
Single- and dual-drug dosing regimens of oteseconazole are recommended based on previous trial data that compared safety and efficacy of oteseconazole versus fluconazole induction therapy and oteseconazole versus placebo maintenance therapy.22 However, widespread use of oteseconazole regimens are limited due to its higher costs and limited access to the drug outside of a research setting.20
Single-drug induction therapy with oteseconazole consists of a single 600-mg oral dose on day 1 followed by a second dose of 450 mg orally on day 2. Starting on day 14, maintenance therapy starts with a single oral dose of 150 mg and is continued weekly for 11 weeks.22
Dual-drug induction therapy consists of oral fluconazole 150 mg on days 1, 4, and 7 followed by daily dosing of oral oteseconazole 150 mg on days 14 through 20. Then, starting on day 28, weekly dosing of oral oteseconazole 150 mg is continued for 11 weeks.22
Effects on pregnancy and lactation. Concerns of oteseconazole’s fetal teratogenicity are based on animal reproduction studies that reported ocular abnormalities from in utero exposure. Human data are insufficient to determine if oteseconazole is excreted in breast milk or what its effects are on milk production. Among breastfed infants whose mothers were exposed to oteseconazole during lactation, no adverse outcomes were reported, but follow up of oteseconazole-exposed infants was limited. 22 Therefore, use of oteseconazole among pregnant and/or lactating persons with RVVC is contraindicated at this time. The long-half life (approximately 138 days) of oteseconazole may preclude use among persons attempting pregnancy. 22
Other therapies. The other common classes of antifungal therapy used in the treatment of RVVC include the polyenes (for example, amphotericin B) and echinocandins (such as caspofungin) drug classes. Emerging azole-resistance among Candida species has been recognized as a significant concern from the Centers for Disease Control and Prevention. 7 Echinocandins, which are generally better tolerated and have a lower adverse side effect profile than polyenes, are a promising therapeutic class, but currently they are limited to intravenous options. SCY-078, a novel oral echinocandin in development, has shown in vitro fungicidal activity against multiple albicans and non-albicans Candida species in pharmacokinetic/pharmacodynamic studies.23
Continued development of alternative, non-azole-based therapies for Candida species is needed.●

Recurrent vulvovaginal candidiasis (RVVC) is a common cause of vaginitis and gynecologic morbidity in the United States and globally.1 RVVC is defined as at least 3 laboratory-confirmed (for example, culture, nucleic acid amplification test [NAAT]) symptomatic episodes in the previous 12 months.2 Common symptoms include vulvar pruritus, erythema, local skin and mucosal irritation, and abnormal discharge that may be thick and white or thin and watery.
The true incidence of RVVC is difficult to determine due to clinical diagnostic inaccuracy that results in over- and underdiagnosis of VVC and the general availability of over-the-counter topical antifungal medications that individuals who self-diagnose use to treat VVC.3
Causative organisms
Vulvovaginal yeast infections are caused by Candida species, a family of ubiquitous fungi that are a part of normal genitourinary and gastrointestinal flora.4 As such, these infections are commonly termed VVC. The presence of Candida species in the vagina without evidence of inflammation is not considered an infection but rather is more consistent with vaginal colonization. Inflammation in the setting of Candida species is what characterizes a true VVC infection.4
Candida albicans is responsible for the vast majority of VVC cases in the United States, with Candida glabrata accounting for most of the remaining infections.5 The majority of RVVC infections that are caused by C albicans are due to azole-sensitive strains (85%–95% of infections).2C glabrata, by contrast, is intrinsically resistant to azoles, which is thought primarily to be due to overexpression of drug efflux pumps that remove active drug from the cell.6,7
Why does VVC reoccur?
The pathogenesis of RVVC is not well understood. Predisposing factors may include frequent or recent antibiotic use, poorly controlled diabetes, immunodeficiency, and other host factors. However, many cases of RVVC are idiopathic and no predisposing or underlying conditions are identified.7
The role of genetic factors in predisposing to or triggering RVVC is unclear and is an area of ongoing investigation.2 Longitudinal DNA-typing studies suggest that recurrent disease is usually due to relapse from a persistent vaginal reservoir of organisms (that is, vaginal colonization) or endogenous reinfection with identical strains of susceptible C albicans.8,9 Symptomatic VVC likely results when the symbiotic balance between yeast and the normal vaginal microbiota is disrupted (by either Candida species overgrowth or changes in host immune factors).2 Less commonly, “recurrent” infections may in fact be due to azole-resistant Candida and non-Candida species.2
Clinical aspects and diagnosis of VVC
Signs and symptoms suggestive of VVC include vulvovaginal erythema, edema, vaginal discharge, vulvovaginal pruritus, and irritation. Given the lack of specificity of individual clinical findings in diagnosing VVC, or for distinguishing between other common causes of vaginitis (such as bacterial vaginosis and trichomoniasis), laboratory testing (that is, microscopy) should be performed in combination with a clinical exam in order to make a confident diagnosis of VVC.10 Self-diagnosis of VVC is inaccurate and is not recommended, as misdiagnosis and inappropriate treatment is cost ineffective, delays accurate diagnoses, and may contribute to growing azole resistance.
In patients with signs and symptoms of VVC, saline and potassium hydroxide microscopy should be performed.7 TABLE 1 summarizes other major diagnostic techniques for VVC.
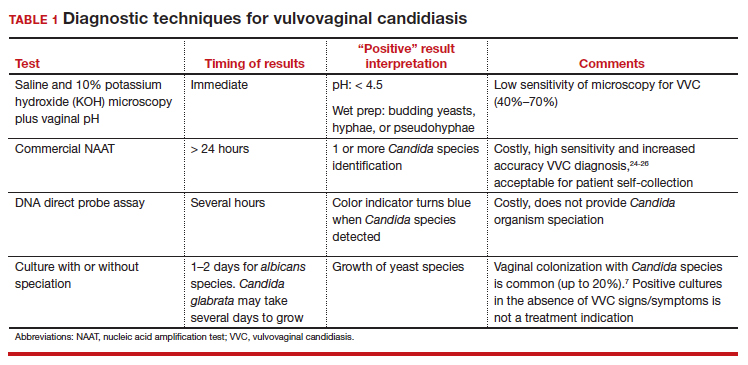
Diagnostic considerations
Non-albicans Candida species, such as C glabrata, may be associated with minimally symptomatic or completely asymptomatic infections and may not be identified easily on wet mount as it does not form pseudohyphae or hyphae.11 Therefore, culture and susceptibility or NAAT testing is highly recommended for patients who remain symptomatic and/or have a nondiagnostic microscopy and a normal vaginal pH.7
Treatment options
Prior to May 2022, there had been no drugs approved by the US Food and Drug Administration (FDA) to treat RVVC. The mainstay of treatment is long-term maintenance therapy to achieve mycologic remission (TABLE 2).

In general, recurrent episodes of VVC should be treated with a longer duration of therapy (for example, oral fluconazole 150 mg every 72 hours for a total of 3 doses or topical azole for 7–14 days).7 If recurrent maintenance/suppressive therapy is started, the induction phase should be longer as well, at least 10 to 14 days with a topical or oral azole followed by a 6-month or longer course of weekly oral or topical azole therapy (such as 6–12 months).12,13
Patients with underlying immunodeficiency (such as poorly controlled diabetes, chronic corticosteroid treatment) may need prolonged courses of therapy. Correction of modifiable conditions and optimization of comorbidities should be prioritized—for example, optimized glucose control, weight loss, durable viral suppression, and so on. Of note, symptomatic VVC is more frequent among individuals with HIV and correlates with severity of immunodeficiency. Pharmacologic options for RVVC for individuals with HIV do not differ from standard recommendations.14
Fluconazole
Fluconazole is a safe, affordable, and convenient prescription oral medication that can be used for initial and maintenance/suppressive therapy.2 Fluconazole levels in vaginal secretions remain at therapeutic concentrations for at least 72 hours after a 150-mg dose.15 Induction therapy consists of oral fluconazole 150 mg every 72 hours for a total of 3 doses, followed by a maintenance regimen of a once-weekly dose of oral fluconazole 150 mg for a total of 6 months. Unfortunately, up to 55% of patients will experience a relapse in symptoms.12
Routine liver function test monitoring is not indicated for fluconazole maintenance therapy, but it should be performed if patients are treated with daily or long-term alternative oral azole medications, such as ketoconazole and itraconazole.
During pregnancy, only topical azole therapy is recommended for use, given the potential risk for adverse fetal outcomes, such as spontaneous abortion and congenital malformations, with fetal exposure to oral fluconazole ingested by the pregnant person.16 Fluconazole is present in breast milk, but it is safe to use during lactation when used at recommended doses.17
Continue to: Options for fluconazole-resistant C albicans infection...
Options for fluconazole-resistant C albicans infection
Patients who have RVVC with frequent and/or prolonged use of fluconazole are at risk for developing azole-resistant isolates of C albicans.12 For patients found to have azole-resistant infections, treatment options include increasing the azole dose based on isolate minimal inhibitory concentrations (MIC) to various antifungals, therapy with a non-fluconazole azole regimen, or switching to a different therapeutic drug class altogether.7
Options for non- albicans Candida species infection
Given the intrinsic resistance to azole therapy in some non-albicans Candida species (specifically C glabrata and Candida krusei), boric acid or nystatin regimens can be used. An induction course of vaginal boric acid is given as 600 mg per vagina daily for up to 14 days and is associated with a 70% rate of mycologic control.7 Boric acid is known to cause local irritation and dermatitis for both the patient and any sexual partners. If ingested orally, boric acid is associated with significant toxicity and even death.7
Vaginal nystatin also may be considered, with an induction course of 100,000 U for 14 days, with a similar regimen recommended for maintenance therapy. However, data are limited on maintenance regimens for RVVC due to non-albicans Candida species.2
Gentian violet
Gentian violet is a topical antiseptic agent that is available over the counter. Use of this agent is uncommon given the availability of highly effective azole-based therapy. Although useful due to its antipruritic properties, gentian violet can be messy to use and tends to stain clothing permanently.
Gentian violet use may be considered in cases of refractory RVVC with or without azole-resistant infections; it is applied as a 1% or 2% solution directly to affected areas for 10 to 14 days.18
Lactobacilli probiotics and dietary changes
Data that support the oral and/or vaginal use of probiotics that contain live lactobacilli are conflicting. In the absence of conclusive evidence to support probiotic use to treat and prevent RVVC, as well as variable quality of available products, use of these agents is not recommended.19
No controlled studies have evaluated the role of various diets in preventing RVVC; thus, no specific dietary changes are recommended.
Behavioral therapy
Available evidence does not support the treatment of sexual partners of patients with RVVC.7
Continue to: What’s new in treatment?...
What’s new in treatment?
Until recently, the main standard of care for RVVC has been oral fluconazole-based therapy. For patients whose symptoms do not respond to oral fluconazole therapy, oteseconazole is now available as a noninferior treatment option to fluconazole for both induction and maintenance therapy. Like other azoles, oteseconazole works by inhibiting a fungal enzyme (CYP51) that is essential in fungal cell membrane integrity and fungal growth.20 Oteseconazole is a more selective inhibitor of the fungal CYP51 enzyme and has demonstrated excellent potency against Candida species in in vitro pharmacologic studies.21
In a phase 3 study that evaluated the safety and efficacy of oteseconazole in the treatment and prevention of RVVC, oteseconazole was found to be both safe and efficacious in both the induction and maintenance phases of treatment for RVVC.20 In this trial, induction and maintenance with oteseconazole was compared with induction with fluconazole and placebo maintenance. Among the 185 participants with culture-verified RVVC, the oteseconazole regimen (n = 123) was associated with fewer recurrences of culture-verified VVC infections than was the fluconazole induction/placebo maintenance regimen (n = 62) during the 48-week maintenance phase of therapy (5% vs 42%).20
Single- and dual-drug dosing regimens of oteseconazole are recommended based on previous trial data that compared safety and efficacy of oteseconazole versus fluconazole induction therapy and oteseconazole versus placebo maintenance therapy.22 However, widespread use of oteseconazole regimens are limited due to its higher costs and limited access to the drug outside of a research setting.20
Single-drug induction therapy with oteseconazole consists of a single 600-mg oral dose on day 1 followed by a second dose of 450 mg orally on day 2. Starting on day 14, maintenance therapy starts with a single oral dose of 150 mg and is continued weekly for 11 weeks.22
Dual-drug induction therapy consists of oral fluconazole 150 mg on days 1, 4, and 7 followed by daily dosing of oral oteseconazole 150 mg on days 14 through 20. Then, starting on day 28, weekly dosing of oral oteseconazole 150 mg is continued for 11 weeks.22
Effects on pregnancy and lactation. Concerns of oteseconazole’s fetal teratogenicity are based on animal reproduction studies that reported ocular abnormalities from in utero exposure. Human data are insufficient to determine if oteseconazole is excreted in breast milk or what its effects are on milk production. Among breastfed infants whose mothers were exposed to oteseconazole during lactation, no adverse outcomes were reported, but follow up of oteseconazole-exposed infants was limited. 22 Therefore, use of oteseconazole among pregnant and/or lactating persons with RVVC is contraindicated at this time. The long-half life (approximately 138 days) of oteseconazole may preclude use among persons attempting pregnancy. 22
Other therapies. The other common classes of antifungal therapy used in the treatment of RVVC include the polyenes (for example, amphotericin B) and echinocandins (such as caspofungin) drug classes. Emerging azole-resistance among Candida species has been recognized as a significant concern from the Centers for Disease Control and Prevention. 7 Echinocandins, which are generally better tolerated and have a lower adverse side effect profile than polyenes, are a promising therapeutic class, but currently they are limited to intravenous options. SCY-078, a novel oral echinocandin in development, has shown in vitro fungicidal activity against multiple albicans and non-albicans Candida species in pharmacokinetic/pharmacodynamic studies.23
Continued development of alternative, non-azole-based therapies for Candida species is needed.●
- Sobel JD. Epidemiology and pathogenesis of recurrent vulvovaginal candidiasis. Am J Obstet Gynecol. 1985;152(7 pt 2):924-935. doi:10.1016/S0002-9378(85)80003-x
- Sobel JD. Recurrent vulvovaginal candidiasis. Am J Obstet Gynecol. 2016;214:15-21. doi:10.1016/j.ajog.2015.06.067
- Rathod SD, Buffler PA. Highly-cited estimates of the cumulative incidence and recurrence of vulvovaginal candidiasis are inadequately documented. BMC Womens Health. 2014;14:43. doi:10.1186/1472-6874-14-43
- Eckert LO, Lentz GM. Genital tract infections: vulva, vagina, cervix, toxic shock syndrome, endometritis, and salpingitis. In: Gershenson DM, Lentz GM, Valea FA, et al, eds. Comprehensive Gynecology. 8th ed. Elsevier; 2022:515-542.
- Gonçalves B, Ferreira C, Alves CT, et al. Vulvovaginal candidiasis: epidemiology, microbiology and risk factors. Crit Rev Microbiol. 2016;42:905-927. doi:10.3109/1040841X.2015.1091805
- Sobel JD, Sobel R. Current treatment options for vulvovaginal candidiasis caused by azole-resistant Candida species. Expert Opin Pharmacother. 2018;19:971-977. doi:10.1080/14656566.2018.1476490
- Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep. 2021;70:1-187. doi:10.15585/mmwr.rr7004a1
- Vazquez JA, Sobel JD, Demitriou R, et al. Karyotyping of Candida albicans isolates obtained longitudinally in women with recurrent vulvovaginal candidiasis. J Infect Dis. 1994;170:1566-1569. doi:10.1093/infdis/170.6.1566
- Lockhart SR, Reed BD, Pierson CL, et al. Most frequent scenario for recurrent Candida vaginitis is strain maintenance with “substrain shuffling”: demonstration by sequential DNA fingerprinting with probes Ca3, C1, and CARE2. J Clin Microbiol. 1996;34:767-777. doi:10.1128/jcm.34.4.767-777.1996
- Anderson MR, Klink K, Cohrssen A. Evaluation of vaginal complaints. JAMA. 2004;291:1368-1379. doi:10.1001/jama.291.11.1368
- Sobel JD. Vulvovaginal candidosis. Lancet. 2007;369:1961-1971. doi:10.1016/S0140-6736(07)60917-9
- Collins LM, Moore R, Sobel JD. Prognosis and long-term outcome of women with idiopathic recurrent vulvovaginal candidiasis caused by Candida albicans. J Low Genit Tract Dis. 2020;24:48-52. doi:10.1097/LGT.0000000000000496
- Pappas PG, Kauffman CA, Andes DR, et al. Clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis. 2016;62:e1-50. doi:10.1093/cid/civ933
- Duerr A, Heilig CM, Meikle SF, et al; HER Study Group. Incident and persistent vulvovaginal candidiasis among human immunodeficiency virus–infected women: risk factors and severity. Obstet Gynecol. 2003;101:548-556. doi:10.1016/s0029-7844(02)02729-1
- Houang ET, Chappatte O, Byrne D, et al. Fluconazole levels in plasma and vaginal secretions of patients after a 150-milligram single oral dose and rate of eradication of infection in vaginal candidiasis. Antimicrob Agents Chemother. 1990;34:909-910. doi:10.1128/AAC.34.5.909
- Bérard A, Sheehy O, Zhao JP, et al. Associations between low- and high-dose oral fluconazole and pregnancy outcomes: 3 nested case-control studies. CMAJ. 2019;191:E179-E187. doi:10.1503/cmaj.180963
- Fluconazole. In: Drugs and Lactation Database (LactMed). National Library of Medicine (US); 2006. Revised October 31, 2018. Accessed September 23, 2022. http://www.ncbi.nlm.nih.gov/books/NBK501223/
- White DJ, Johnson EM, Warnock DW. Management of persistent vulvo vaginal candidosis due to azole-resistant Candida glabrata. Genitourin Med. 1993;69:112-114. doi:10.1136/sti.69.2.112
- Falagas ME, Betsi GI, Athanasiou S. Probiotics for prevention of recurrent vulvovaginal candidiasis: a review. J Antimicrob Chemother. 2006;58:266-272. doi:10.1093/jac/dkl246
- Martens MG, Maximos B, Degenhardt T, et al. Phase 3 study evaluating the safety and efficacy of oteseconazole in the treatment of recurrent vulvovaginal candidiasis and acute vulvovaginal candidiasis infections. Am J Obstet Gynecol. 2022:S0002-9378(22)005774. doi:10.1016/j.ajog.2022.07.023
- Sobel JD, Nyirjesy P. Oteseconazole: an advance in treatment of recurrent vulvovaginal candidiasis. Future Microbiol. 2021;16:1453-1461. doi:10.2217/fmb-2021-0173
- Vivjoa (oteseconazole). Prescribing information. Mycovia Pharmaceuticals, Inc. April 2022. https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/215888s000lbl.pdf
- Scorneaux B, Angulo D, Borroto-Esoda K, et al. SCY-078 is fungicidal against Candida species in time-kill studies. Antimicrob Agents Chemother. 2017;61:e01961-16. doi:10.1128/AAC.01961-16
- Schwebke JR, Taylor SN, Ackerman R, et al. Clinical validation of the Aptima bacterial vaginosis and Aptima Candida/Trichomonas vaginitis assays: results from a prospective multicenter clinical study. J Clin Microbiol. 2020;58:e01643-19. doi:10.1128/JCM.01643-19
- Schwebke JR, Gaydos CA, Nyirjesy P, et al. Diagnostic performance of a molecular test versus clinician assessment of vaginitis. J Clin Microbiol. 2018;56:e00252-18. doi:10.1128/JCM.00252-18
- Broache M, Cammarata CL, Stonebraker E, et al. Performance of a vaginal panel assay compared with the clinical diagnosis of vaginitis. Obstet Gynecol. 2021;138:853-859. doi:10.1097/AOG.0000000000004592
- Sobel JD. Epidemiology and pathogenesis of recurrent vulvovaginal candidiasis. Am J Obstet Gynecol. 1985;152(7 pt 2):924-935. doi:10.1016/S0002-9378(85)80003-x
- Sobel JD. Recurrent vulvovaginal candidiasis. Am J Obstet Gynecol. 2016;214:15-21. doi:10.1016/j.ajog.2015.06.067
- Rathod SD, Buffler PA. Highly-cited estimates of the cumulative incidence and recurrence of vulvovaginal candidiasis are inadequately documented. BMC Womens Health. 2014;14:43. doi:10.1186/1472-6874-14-43
- Eckert LO, Lentz GM. Genital tract infections: vulva, vagina, cervix, toxic shock syndrome, endometritis, and salpingitis. In: Gershenson DM, Lentz GM, Valea FA, et al, eds. Comprehensive Gynecology. 8th ed. Elsevier; 2022:515-542.
- Gonçalves B, Ferreira C, Alves CT, et al. Vulvovaginal candidiasis: epidemiology, microbiology and risk factors. Crit Rev Microbiol. 2016;42:905-927. doi:10.3109/1040841X.2015.1091805
- Sobel JD, Sobel R. Current treatment options for vulvovaginal candidiasis caused by azole-resistant Candida species. Expert Opin Pharmacother. 2018;19:971-977. doi:10.1080/14656566.2018.1476490
- Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep. 2021;70:1-187. doi:10.15585/mmwr.rr7004a1
- Vazquez JA, Sobel JD, Demitriou R, et al. Karyotyping of Candida albicans isolates obtained longitudinally in women with recurrent vulvovaginal candidiasis. J Infect Dis. 1994;170:1566-1569. doi:10.1093/infdis/170.6.1566
- Lockhart SR, Reed BD, Pierson CL, et al. Most frequent scenario for recurrent Candida vaginitis is strain maintenance with “substrain shuffling”: demonstration by sequential DNA fingerprinting with probes Ca3, C1, and CARE2. J Clin Microbiol. 1996;34:767-777. doi:10.1128/jcm.34.4.767-777.1996
- Anderson MR, Klink K, Cohrssen A. Evaluation of vaginal complaints. JAMA. 2004;291:1368-1379. doi:10.1001/jama.291.11.1368
- Sobel JD. Vulvovaginal candidosis. Lancet. 2007;369:1961-1971. doi:10.1016/S0140-6736(07)60917-9
- Collins LM, Moore R, Sobel JD. Prognosis and long-term outcome of women with idiopathic recurrent vulvovaginal candidiasis caused by Candida albicans. J Low Genit Tract Dis. 2020;24:48-52. doi:10.1097/LGT.0000000000000496
- Pappas PG, Kauffman CA, Andes DR, et al. Clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis. 2016;62:e1-50. doi:10.1093/cid/civ933
- Duerr A, Heilig CM, Meikle SF, et al; HER Study Group. Incident and persistent vulvovaginal candidiasis among human immunodeficiency virus–infected women: risk factors and severity. Obstet Gynecol. 2003;101:548-556. doi:10.1016/s0029-7844(02)02729-1
- Houang ET, Chappatte O, Byrne D, et al. Fluconazole levels in plasma and vaginal secretions of patients after a 150-milligram single oral dose and rate of eradication of infection in vaginal candidiasis. Antimicrob Agents Chemother. 1990;34:909-910. doi:10.1128/AAC.34.5.909
- Bérard A, Sheehy O, Zhao JP, et al. Associations between low- and high-dose oral fluconazole and pregnancy outcomes: 3 nested case-control studies. CMAJ. 2019;191:E179-E187. doi:10.1503/cmaj.180963
- Fluconazole. In: Drugs and Lactation Database (LactMed). National Library of Medicine (US); 2006. Revised October 31, 2018. Accessed September 23, 2022. http://www.ncbi.nlm.nih.gov/books/NBK501223/
- White DJ, Johnson EM, Warnock DW. Management of persistent vulvo vaginal candidosis due to azole-resistant Candida glabrata. Genitourin Med. 1993;69:112-114. doi:10.1136/sti.69.2.112
- Falagas ME, Betsi GI, Athanasiou S. Probiotics for prevention of recurrent vulvovaginal candidiasis: a review. J Antimicrob Chemother. 2006;58:266-272. doi:10.1093/jac/dkl246
- Martens MG, Maximos B, Degenhardt T, et al. Phase 3 study evaluating the safety and efficacy of oteseconazole in the treatment of recurrent vulvovaginal candidiasis and acute vulvovaginal candidiasis infections. Am J Obstet Gynecol. 2022:S0002-9378(22)005774. doi:10.1016/j.ajog.2022.07.023
- Sobel JD, Nyirjesy P. Oteseconazole: an advance in treatment of recurrent vulvovaginal candidiasis. Future Microbiol. 2021;16:1453-1461. doi:10.2217/fmb-2021-0173
- Vivjoa (oteseconazole). Prescribing information. Mycovia Pharmaceuticals, Inc. April 2022. https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/215888s000lbl.pdf
- Scorneaux B, Angulo D, Borroto-Esoda K, et al. SCY-078 is fungicidal against Candida species in time-kill studies. Antimicrob Agents Chemother. 2017;61:e01961-16. doi:10.1128/AAC.01961-16
- Schwebke JR, Taylor SN, Ackerman R, et al. Clinical validation of the Aptima bacterial vaginosis and Aptima Candida/Trichomonas vaginitis assays: results from a prospective multicenter clinical study. J Clin Microbiol. 2020;58:e01643-19. doi:10.1128/JCM.01643-19
- Schwebke JR, Gaydos CA, Nyirjesy P, et al. Diagnostic performance of a molecular test versus clinician assessment of vaginitis. J Clin Microbiol. 2018;56:e00252-18. doi:10.1128/JCM.00252-18
- Broache M, Cammarata CL, Stonebraker E, et al. Performance of a vaginal panel assay compared with the clinical diagnosis of vaginitis. Obstet Gynecol. 2021;138:853-859. doi:10.1097/AOG.0000000000004592
“Blind” endometrial sampling: A call to end the practice

Linda Bradley, MD: The standard in ObGyn for many years has been our reliance on the blind dilation and curettage (D&C)—it has been the mainstay for evaluation of the endometrial cavity. We know that it has risks, but most importantly, the procedure has low sensitivity for detecting focal pathology. This basic lack of confirmation of lesions makes a diagnosis impossible and patients are challenged in getting adequate treatment, and will not, since they may not know what options they have for the treatment of intrauterine pathology.
Because it is a “blind procedure,” done without looking, we don’t know the endpoints, such as when is the procedure completed, how do we know we removed all of the lesions? Let’s look at our colleagues, like GI and colorectal physicians. If a patient presents with rectal bleeding, we would perform an exam, followed by either a colonoscopy or sigmoidoscopy. If a patient were vomiting up blood, a gastroenterologist would perform an upper endoscopy, look with a tube to see if there is an ulcer or something else as a source of the bleeding. If a patient were bleeding from the bladder, a urologist would use a cystoscope for direct inspection.
Unfortunately for gynecologists, only about 15% to 25% of us will use hysteroscopy as a diagnostic method2—a method that has excellent sensitivity in detecting endocervical disease, intrauterine disease, and proximal tubal pathology. Compared with blind curettage, we can visualize the cavity; we can sample the cavity directly; we can determine what the patient has and determine the proper surgical procedure, medical therapy, or reassurance that a patient may be offered. We often are looking at focal lesions, lesions in the uterine cavity that could be cancer, so we can make a diagnosis. Or we may be looking at small things, like endometrial hyperplasia, endocervical or endometrial polyps, retained products of conception, or fibroids. We can look at uterine pathology as well as anatomic issues and malformations—such as bicornuate or septate uterus.
I actually say, “My hysteroscope is my stethoscope” because it allows us to evaluate for many things. The beauty of the new office hysteroscopes is that they are miniaturized. Doctors now have the ability to use reusable devices that are as small as 3 millimeters. There are disposable ones that are up to 3.5 to 4 millimeters in size. Gynecologists have the options to choose from reusuable rigid or flexible hysteroscopes or completely disposable devices. So, truly, we now should not have an excuse for evaluating a woman’s anatomy, especially for bleeding. We should no longer rely, as we have for the last century or more, just on blind sampling, because we miss focal lesions.
OBG Management: When was the hysteroscope first introduced into the field?
Dr. Bradley: The technology employed in hysteroscopy has been around really since the last 150+ years, introduced by Dr. Pantaleoni. We just have not embraced its usefulness in our clinical practice for many years. Today, about 15% to 25% of gynecologists practicing in the United States are performing hysteroscopy in the office.1
OBG Management: How does using hysteroscopy contribute to better patient outcomes?
Dr. Bradley: We can get a more accurate diagnosis—fewer false-negatives and a high degree of sensitivity in detecting focal lesions. With D&C, much focal pathology can be left behind. In a 2001 study, 105 symptomatic postmenopausal women with bleeding and thickened lining of the uterus greater than 5 mm on ultrasound underwent blind D&C. They found that 80% of the women had intracavitary lesions and 90% had focal lesions. In fact, 87% of the patients with focal lesions still had residual pathology after the blind D&C.3 The D&C procedure missed 58% of polyps, 50% of endometrial hyperplasia, 60% of cases of complex atypical hyperplasia, and even 11% of endometrial cancers. So these numbers are just not very good. Direct inspection of the uterus, with uninterrupted visualization through hysteroscopy, with removal of lesions under direct visualization, should be our goal.
Blind sampling also poses greater risk for things like perforation. In addition, you not only can miss lesions by just scraping the endometrium, D&C also can leave lesions just floating around in the uterine cavity, with those lesions never retrieved. With office hysteroscopy, the physician can be more successful in treating a condition because once you see what is going on in the uterine cavity, you can say, “Okay, I can fix this with a surgical procedure. What instruments do I need? How much time is it going to take? Is this a straightforward case? Is it more complicated? Do I let an intern do the case? Is this for a more senior resident or fellow?” So I think it helps to direct the next steps for surgical management and even medical management, which also could be what we call “one-stop shopping.” For instance, for directed biopsies for removal of small polyps, for patients that can tolerate the procedure a little longer, the diagnostic hysteroscopy then becomes a management, an operative procedure, that really, for myself, can be done in the office. Removal of larger fibroids, because of fluid management and other concerns, would not be done in the office. Most patients tolerate office procedures, but it also depends on a patient’s weight, and her ability to relax during the procedure.
The ultimate goal for hysteroscopy is a minimum of diagnosis, meaning in less than 2, 3 minutes, you can look inside the uterus. Our devices are 3 millimeters in size; I tell my patients, it’s the size of “a piece of spaghetti or pasta,” and we will just take a look. If we see a polyp, okay, if your office is not equipped, because then you need a different type of equipment for removal, then take her to the operating room. The patient would be under brief anesthesia and go home an hour or 2 later. So really, for physicians, we just need to embrace the technology to make a diagnosis, just look, and then from there decide what is next.
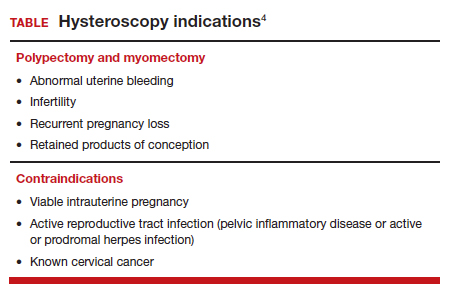
OBG Management: What techniques do you use to minimize or eliminate patient discomfort during hysteroscopy?...
OBG Management: What techniques do you use to minimize or eliminate patient discomfort during hysteroscopy?
Dr. Bradley: I think first is always be patient-centric. Let patients be prepared for the procedure. We have reading materials; our nurses explain the procedure. In the office, I try to prepare the patient for success. I let her know what is going on. A friend, family member can be with her. We have a nurse that understands the procedure; she explains it well. We have a type of bed that allows the patients’ legs to rest more comfortably in the stirrups—a leg rest kind of stirrup. We use a heating pad. Some patients like to hear music. Some patients like to have aromatherapy. We are quick and efficient, and typically just talk to the patient throughout the procedure. Although some patients don’t like this explanatory, “talkative” approach—they say, “Dr. Bradley, just do the procedure. I don’t want to know you are touching the cervix. I don’t want to know that you’re prepping. Just do it.”
But I like what we called it when I was growing up: vocal-local (talk to your patient and explain as you proceed). It’s like local anesthesia. For these procedures in the office you usually do not have to use numbing medicine or a paracervical block. Look at the patient’s age, number of years in menopause, whether or not she has delivered vaginally, and what her cervix looks like. Does she have a sexually transmitted infection or pelvic inflammatory disease? Sometimes we will use misoprostol, my personal preference is oral, but there are data to suggest that vaginal can be of help.4 We suggest Motrin, Tylenol an hour or 2 before, and we always want patients to not come in on an empty stomach. There is also the option of primrose oil, a supplement, that patients buy at the drug store in the vitamin section. It’s used for cervical softening. It is taken orally.5-7
If they want, patients can watch a video—similar to watching childbirth videos when I used to deliver babies. At some point we started putting mirrors where women could see their efforts of pushing a baby out, as it might give them more willpower to push harder. Some people don’t want to look. But the majority of women will do well in this setting. I do have a small number of women that just say, “I can’t do this in the office,” and so in those cases, they can go to the operating room. But the main idea is, even in an operating room, you are not just doing a D&C. You are still going to look inside with a hysteroscope and have a great panoramic view of what is going on, and remove a lesion with an instrument while you watch. Not a process of looking with the hysteroscope, scraping with a curettage, and thinking that you are complete. Targeted removal of focal lesions under continuous visualization is the goal.
OBG Management: Can you describe the goals of the consensus document on ending blind sampling co-created by the European Society of Gynecologic Endoscopy, AAGL, and the Global Community on Hysteroscopy?
Dr. Bradley: Our goal for this year is to get a systematic review and guidelines paper written that speaks to what we have just talked about. We want to have as many articles about why blind sampling is not beneficial, with too many misses, and now we have new technology available. We want to speak to physicians to solve the conundrum of bleeding, with equivocal ultrasounds, equivocal saline infusion, sonograms, equivocal MRIs—be able to take a look. Let’s come up to speed like our other colleagues in other specialties that “look.” A systematic review guideline document will provide the evidence that blind D&C is fraught with problems and how often we miss disease and its inherent risk.
We need to, by itself, for most of our patients, abandon D&C because we have too many missed diagnoses. As doctors we have to be lifelong learners. There was no robot back in the day. We were not able to do laparoscopic hysterectomies, there were no MRIs. I remember in our city, there was one CT scan. We just did not have a lot of technology. The half-life of medical knowledge used to be decades—you graduated in the ‘60s, you could be a great gynecologist for the next 30 years because there was not that much going on. When I finished in the mid to late ‘80s, there was no hysteroscopy training. But I have come to see its value, the science behind it.
So what I say to doctors is, “We learn so many new things, we shouldn’t get stuck in just saying, ‘I didn’t do this when I was in training.’” And if your thought is, “Oh, in my practice, I don’t have that many cases,” you still need to be able to know who in your community can be a resource to your patients. As Maya Angelou says, “When you know better, you should do better.” And that’s where I am now—to be a lifelong learner, and just do it.
Lastly, patient influence is very important. If patients ask, “How are you going to do the procedure?” it’s a driver for change. By utilizing hysteroscopy in the evaluation of the intrauterine cavity, we have the opportunity to change the face of evaluation and treatment for abnormal uterine bleeding.●
To maximize visualization and procedure ease, schedule office hysteroscopy shortly after menstruation for reproductive-age women with regular menstrual cycles, which corresponds to timing of the thinnest endometrial lining.1 By contrast, the luteal phase of the menstrual cycle may be associated with the presence of secretory endometrium, which may mimic endometrial polyps or obscure intrauterine pathology, including FIGO type 1 and 2 submucous leiomyomas.
The following patients can have their procedures scheduled at any time, as they do not regularly cycle:
- those receiving continuous hormonal contraception
- women taking menopausal hormonal therapy
- women on progestin therapy (including those using intrauterine devices).
For patients with irregular cycles, timing is crucial as the topography of the endometrium can be variable. To increase successful visualization and diagnostic accuracy, a short course of combined hormonal contraceptives2 or progestin therapy3,4 can be considered for 10-14 days, followed by a withdrawal menses, and immediate procedure scheduling after bleeding subsides, as this will produce a thin endometrium. This approach may be especially beneficial for operative procedures such as polypectomy in order to promote complete specimen extraction.
Pharmacologic endometrial preparation also is an option and has been associated with decreased procedure time and improved patient and clinician satisfaction during operative hysteroscopy.2,3 We discourage the use of hormonal pre-treatment for diagnostic hysteroscopy alone, as this may alter endometrial histology and provide misleading results. Overall, data related to pharmacologic endometrial preparation are limited to small studies with varying treatment protocols, and an optimal regimen has yet to be determined.
References
1. The use of hysteroscopy for the diagnosis and treatment of intrauterine pathology: ACOG Committee Opinion, number 800. Obstet Gynecol. 2020;135:e138-e148. doi:10.1097/AOG.0000000000003712.
2. Cicinelli E, Pinto V, Quattromini P, et al. Endometrial preparation with estradiol plus dienogest (Qlaira) for office hysteroscopic polypectomy: randomized pilot study. J Minim Invasive Gynecol. 2012;19:356-359. doi:10.1016/j.jmig.2011.12.020.
3. Laganà AS, Vitale SG, Muscia V, et al. Endometrial preparation with dienogest before hysteroscopic surgery: a systematic review. Arch Gynecol Obstet. 2017;295:661-667. doi:10.1007/s00404-016-4244-1.
4. Ciebiera M, Zgliczyńska M, Zgliczyński S, et al. Oral desogestrel as endometrial preparation before operative hysteroscopy: a systematic review. Gynecol Obstet Invest. 2021;86:209-217. doi:10.1159/000514584.
- Orlando MS, Bradley LD. Implementation of office hysteroscopy for the evaluation and treatment of intrauterine pathology. Obstet Gynecol. August 3, 2022. doi: 10.1097/ AOG.0000000000004898.
- Salazar CA, Isaacson KB. Office operative hysteroscopy: an update. J Minim Invasive Gynecol. 2018;25:199-208.
- Epstein E, Ramirez A, Skoog L, et al. Dilatation and curettage fails to detect most focal lesions in the uterine cavity in women with postmenopausal bleeding. Acta Obstet Gynecol Scand. 2001;80:1131-1136. doi:10.1034/j.1600-0412.2001.801210.x.
- The use of hysteroscopy for the diagnosis and treatment of intrauterine pathology: ACOG Committee Opinion, number 800. Obstet Gynecol. 2020;135:e138-e148. doi:10.1097/ AOG.0000000000003712.
- Vahdat M, Tahermanesh K, Mehdizadeh Kashi A, et al. Evening Primrose Oil effect on the ease of cervical ripening and dilatation before operative hysteroscopy. Thrita. 2015;4:7-10. doi:10.5812/thrita.29876
- Nouri B, Baghestani A, Pooransari P. Evening primrose versus misoprostol for cervical dilatation before gynecologic surgeries: a double-blind randomized clinical trial. J Obstet Gynecol Cancer Res. 2021;6:87-94. doi:10.30699/jogcr.6.2.87
- Verano RMA, Veloso-borromeo MG. The efficacy of evening primrose oil as a cervical ripening agent for gynecologic procedures: a single-blinded, randomized controlled trial. PJOG. 2015;39:24-28.

Linda Bradley, MD: The standard in ObGyn for many years has been our reliance on the blind dilation and curettage (D&C)—it has been the mainstay for evaluation of the endometrial cavity. We know that it has risks, but most importantly, the procedure has low sensitivity for detecting focal pathology. This basic lack of confirmation of lesions makes a diagnosis impossible and patients are challenged in getting adequate treatment, and will not, since they may not know what options they have for the treatment of intrauterine pathology.
Because it is a “blind procedure,” done without looking, we don’t know the endpoints, such as when is the procedure completed, how do we know we removed all of the lesions? Let’s look at our colleagues, like GI and colorectal physicians. If a patient presents with rectal bleeding, we would perform an exam, followed by either a colonoscopy or sigmoidoscopy. If a patient were vomiting up blood, a gastroenterologist would perform an upper endoscopy, look with a tube to see if there is an ulcer or something else as a source of the bleeding. If a patient were bleeding from the bladder, a urologist would use a cystoscope for direct inspection.
Unfortunately for gynecologists, only about 15% to 25% of us will use hysteroscopy as a diagnostic method2—a method that has excellent sensitivity in detecting endocervical disease, intrauterine disease, and proximal tubal pathology. Compared with blind curettage, we can visualize the cavity; we can sample the cavity directly; we can determine what the patient has and determine the proper surgical procedure, medical therapy, or reassurance that a patient may be offered. We often are looking at focal lesions, lesions in the uterine cavity that could be cancer, so we can make a diagnosis. Or we may be looking at small things, like endometrial hyperplasia, endocervical or endometrial polyps, retained products of conception, or fibroids. We can look at uterine pathology as well as anatomic issues and malformations—such as bicornuate or septate uterus.
I actually say, “My hysteroscope is my stethoscope” because it allows us to evaluate for many things. The beauty of the new office hysteroscopes is that they are miniaturized. Doctors now have the ability to use reusable devices that are as small as 3 millimeters. There are disposable ones that are up to 3.5 to 4 millimeters in size. Gynecologists have the options to choose from reusuable rigid or flexible hysteroscopes or completely disposable devices. So, truly, we now should not have an excuse for evaluating a woman’s anatomy, especially for bleeding. We should no longer rely, as we have for the last century or more, just on blind sampling, because we miss focal lesions.
OBG Management: When was the hysteroscope first introduced into the field?
Dr. Bradley: The technology employed in hysteroscopy has been around really since the last 150+ years, introduced by Dr. Pantaleoni. We just have not embraced its usefulness in our clinical practice for many years. Today, about 15% to 25% of gynecologists practicing in the United States are performing hysteroscopy in the office.1
OBG Management: How does using hysteroscopy contribute to better patient outcomes?
Dr. Bradley: We can get a more accurate diagnosis—fewer false-negatives and a high degree of sensitivity in detecting focal lesions. With D&C, much focal pathology can be left behind. In a 2001 study, 105 symptomatic postmenopausal women with bleeding and thickened lining of the uterus greater than 5 mm on ultrasound underwent blind D&C. They found that 80% of the women had intracavitary lesions and 90% had focal lesions. In fact, 87% of the patients with focal lesions still had residual pathology after the blind D&C.3 The D&C procedure missed 58% of polyps, 50% of endometrial hyperplasia, 60% of cases of complex atypical hyperplasia, and even 11% of endometrial cancers. So these numbers are just not very good. Direct inspection of the uterus, with uninterrupted visualization through hysteroscopy, with removal of lesions under direct visualization, should be our goal.
Blind sampling also poses greater risk for things like perforation. In addition, you not only can miss lesions by just scraping the endometrium, D&C also can leave lesions just floating around in the uterine cavity, with those lesions never retrieved. With office hysteroscopy, the physician can be more successful in treating a condition because once you see what is going on in the uterine cavity, you can say, “Okay, I can fix this with a surgical procedure. What instruments do I need? How much time is it going to take? Is this a straightforward case? Is it more complicated? Do I let an intern do the case? Is this for a more senior resident or fellow?” So I think it helps to direct the next steps for surgical management and even medical management, which also could be what we call “one-stop shopping.” For instance, for directed biopsies for removal of small polyps, for patients that can tolerate the procedure a little longer, the diagnostic hysteroscopy then becomes a management, an operative procedure, that really, for myself, can be done in the office. Removal of larger fibroids, because of fluid management and other concerns, would not be done in the office. Most patients tolerate office procedures, but it also depends on a patient’s weight, and her ability to relax during the procedure.
The ultimate goal for hysteroscopy is a minimum of diagnosis, meaning in less than 2, 3 minutes, you can look inside the uterus. Our devices are 3 millimeters in size; I tell my patients, it’s the size of “a piece of spaghetti or pasta,” and we will just take a look. If we see a polyp, okay, if your office is not equipped, because then you need a different type of equipment for removal, then take her to the operating room. The patient would be under brief anesthesia and go home an hour or 2 later. So really, for physicians, we just need to embrace the technology to make a diagnosis, just look, and then from there decide what is next.
OBG Management: What techniques do you use to minimize or eliminate patient discomfort during hysteroscopy?...
OBG Management: What techniques do you use to minimize or eliminate patient discomfort during hysteroscopy?
Dr. Bradley: I think first is always be patient-centric. Let patients be prepared for the procedure. We have reading materials; our nurses explain the procedure. In the office, I try to prepare the patient for success. I let her know what is going on. A friend, family member can be with her. We have a nurse that understands the procedure; she explains it well. We have a type of bed that allows the patients’ legs to rest more comfortably in the stirrups—a leg rest kind of stirrup. We use a heating pad. Some patients like to hear music. Some patients like to have aromatherapy. We are quick and efficient, and typically just talk to the patient throughout the procedure. Although some patients don’t like this explanatory, “talkative” approach—they say, “Dr. Bradley, just do the procedure. I don’t want to know you are touching the cervix. I don’t want to know that you’re prepping. Just do it.”
But I like what we called it when I was growing up: vocal-local (talk to your patient and explain as you proceed). It’s like local anesthesia. For these procedures in the office you usually do not have to use numbing medicine or a paracervical block. Look at the patient’s age, number of years in menopause, whether or not she has delivered vaginally, and what her cervix looks like. Does she have a sexually transmitted infection or pelvic inflammatory disease? Sometimes we will use misoprostol, my personal preference is oral, but there are data to suggest that vaginal can be of help.4 We suggest Motrin, Tylenol an hour or 2 before, and we always want patients to not come in on an empty stomach. There is also the option of primrose oil, a supplement, that patients buy at the drug store in the vitamin section. It’s used for cervical softening. It is taken orally.5-7
If they want, patients can watch a video—similar to watching childbirth videos when I used to deliver babies. At some point we started putting mirrors where women could see their efforts of pushing a baby out, as it might give them more willpower to push harder. Some people don’t want to look. But the majority of women will do well in this setting. I do have a small number of women that just say, “I can’t do this in the office,” and so in those cases, they can go to the operating room. But the main idea is, even in an operating room, you are not just doing a D&C. You are still going to look inside with a hysteroscope and have a great panoramic view of what is going on, and remove a lesion with an instrument while you watch. Not a process of looking with the hysteroscope, scraping with a curettage, and thinking that you are complete. Targeted removal of focal lesions under continuous visualization is the goal.
OBG Management: Can you describe the goals of the consensus document on ending blind sampling co-created by the European Society of Gynecologic Endoscopy, AAGL, and the Global Community on Hysteroscopy?
Dr. Bradley: Our goal for this year is to get a systematic review and guidelines paper written that speaks to what we have just talked about. We want to have as many articles about why blind sampling is not beneficial, with too many misses, and now we have new technology available. We want to speak to physicians to solve the conundrum of bleeding, with equivocal ultrasounds, equivocal saline infusion, sonograms, equivocal MRIs—be able to take a look. Let’s come up to speed like our other colleagues in other specialties that “look.” A systematic review guideline document will provide the evidence that blind D&C is fraught with problems and how often we miss disease and its inherent risk.
We need to, by itself, for most of our patients, abandon D&C because we have too many missed diagnoses. As doctors we have to be lifelong learners. There was no robot back in the day. We were not able to do laparoscopic hysterectomies, there were no MRIs. I remember in our city, there was one CT scan. We just did not have a lot of technology. The half-life of medical knowledge used to be decades—you graduated in the ‘60s, you could be a great gynecologist for the next 30 years because there was not that much going on. When I finished in the mid to late ‘80s, there was no hysteroscopy training. But I have come to see its value, the science behind it.
So what I say to doctors is, “We learn so many new things, we shouldn’t get stuck in just saying, ‘I didn’t do this when I was in training.’” And if your thought is, “Oh, in my practice, I don’t have that many cases,” you still need to be able to know who in your community can be a resource to your patients. As Maya Angelou says, “When you know better, you should do better.” And that’s where I am now—to be a lifelong learner, and just do it.
Lastly, patient influence is very important. If patients ask, “How are you going to do the procedure?” it’s a driver for change. By utilizing hysteroscopy in the evaluation of the intrauterine cavity, we have the opportunity to change the face of evaluation and treatment for abnormal uterine bleeding.●
To maximize visualization and procedure ease, schedule office hysteroscopy shortly after menstruation for reproductive-age women with regular menstrual cycles, which corresponds to timing of the thinnest endometrial lining.1 By contrast, the luteal phase of the menstrual cycle may be associated with the presence of secretory endometrium, which may mimic endometrial polyps or obscure intrauterine pathology, including FIGO type 1 and 2 submucous leiomyomas.
The following patients can have their procedures scheduled at any time, as they do not regularly cycle:
- those receiving continuous hormonal contraception
- women taking menopausal hormonal therapy
- women on progestin therapy (including those using intrauterine devices).
For patients with irregular cycles, timing is crucial as the topography of the endometrium can be variable. To increase successful visualization and diagnostic accuracy, a short course of combined hormonal contraceptives2 or progestin therapy3,4 can be considered for 10-14 days, followed by a withdrawal menses, and immediate procedure scheduling after bleeding subsides, as this will produce a thin endometrium. This approach may be especially beneficial for operative procedures such as polypectomy in order to promote complete specimen extraction.
Pharmacologic endometrial preparation also is an option and has been associated with decreased procedure time and improved patient and clinician satisfaction during operative hysteroscopy.2,3 We discourage the use of hormonal pre-treatment for diagnostic hysteroscopy alone, as this may alter endometrial histology and provide misleading results. Overall, data related to pharmacologic endometrial preparation are limited to small studies with varying treatment protocols, and an optimal regimen has yet to be determined.
References
1. The use of hysteroscopy for the diagnosis and treatment of intrauterine pathology: ACOG Committee Opinion, number 800. Obstet Gynecol. 2020;135:e138-e148. doi:10.1097/AOG.0000000000003712.
2. Cicinelli E, Pinto V, Quattromini P, et al. Endometrial preparation with estradiol plus dienogest (Qlaira) for office hysteroscopic polypectomy: randomized pilot study. J Minim Invasive Gynecol. 2012;19:356-359. doi:10.1016/j.jmig.2011.12.020.
3. Laganà AS, Vitale SG, Muscia V, et al. Endometrial preparation with dienogest before hysteroscopic surgery: a systematic review. Arch Gynecol Obstet. 2017;295:661-667. doi:10.1007/s00404-016-4244-1.
4. Ciebiera M, Zgliczyńska M, Zgliczyński S, et al. Oral desogestrel as endometrial preparation before operative hysteroscopy: a systematic review. Gynecol Obstet Invest. 2021;86:209-217. doi:10.1159/000514584.

Linda Bradley, MD: The standard in ObGyn for many years has been our reliance on the blind dilation and curettage (D&C)—it has been the mainstay for evaluation of the endometrial cavity. We know that it has risks, but most importantly, the procedure has low sensitivity for detecting focal pathology. This basic lack of confirmation of lesions makes a diagnosis impossible and patients are challenged in getting adequate treatment, and will not, since they may not know what options they have for the treatment of intrauterine pathology.
Because it is a “blind procedure,” done without looking, we don’t know the endpoints, such as when is the procedure completed, how do we know we removed all of the lesions? Let’s look at our colleagues, like GI and colorectal physicians. If a patient presents with rectal bleeding, we would perform an exam, followed by either a colonoscopy or sigmoidoscopy. If a patient were vomiting up blood, a gastroenterologist would perform an upper endoscopy, look with a tube to see if there is an ulcer or something else as a source of the bleeding. If a patient were bleeding from the bladder, a urologist would use a cystoscope for direct inspection.
Unfortunately for gynecologists, only about 15% to 25% of us will use hysteroscopy as a diagnostic method2—a method that has excellent sensitivity in detecting endocervical disease, intrauterine disease, and proximal tubal pathology. Compared with blind curettage, we can visualize the cavity; we can sample the cavity directly; we can determine what the patient has and determine the proper surgical procedure, medical therapy, or reassurance that a patient may be offered. We often are looking at focal lesions, lesions in the uterine cavity that could be cancer, so we can make a diagnosis. Or we may be looking at small things, like endometrial hyperplasia, endocervical or endometrial polyps, retained products of conception, or fibroids. We can look at uterine pathology as well as anatomic issues and malformations—such as bicornuate or septate uterus.
I actually say, “My hysteroscope is my stethoscope” because it allows us to evaluate for many things. The beauty of the new office hysteroscopes is that they are miniaturized. Doctors now have the ability to use reusable devices that are as small as 3 millimeters. There are disposable ones that are up to 3.5 to 4 millimeters in size. Gynecologists have the options to choose from reusuable rigid or flexible hysteroscopes or completely disposable devices. So, truly, we now should not have an excuse for evaluating a woman’s anatomy, especially for bleeding. We should no longer rely, as we have for the last century or more, just on blind sampling, because we miss focal lesions.
OBG Management: When was the hysteroscope first introduced into the field?
Dr. Bradley: The technology employed in hysteroscopy has been around really since the last 150+ years, introduced by Dr. Pantaleoni. We just have not embraced its usefulness in our clinical practice for many years. Today, about 15% to 25% of gynecologists practicing in the United States are performing hysteroscopy in the office.1
OBG Management: How does using hysteroscopy contribute to better patient outcomes?
Dr. Bradley: We can get a more accurate diagnosis—fewer false-negatives and a high degree of sensitivity in detecting focal lesions. With D&C, much focal pathology can be left behind. In a 2001 study, 105 symptomatic postmenopausal women with bleeding and thickened lining of the uterus greater than 5 mm on ultrasound underwent blind D&C. They found that 80% of the women had intracavitary lesions and 90% had focal lesions. In fact, 87% of the patients with focal lesions still had residual pathology after the blind D&C.3 The D&C procedure missed 58% of polyps, 50% of endometrial hyperplasia, 60% of cases of complex atypical hyperplasia, and even 11% of endometrial cancers. So these numbers are just not very good. Direct inspection of the uterus, with uninterrupted visualization through hysteroscopy, with removal of lesions under direct visualization, should be our goal.
Blind sampling also poses greater risk for things like perforation. In addition, you not only can miss lesions by just scraping the endometrium, D&C also can leave lesions just floating around in the uterine cavity, with those lesions never retrieved. With office hysteroscopy, the physician can be more successful in treating a condition because once you see what is going on in the uterine cavity, you can say, “Okay, I can fix this with a surgical procedure. What instruments do I need? How much time is it going to take? Is this a straightforward case? Is it more complicated? Do I let an intern do the case? Is this for a more senior resident or fellow?” So I think it helps to direct the next steps for surgical management and even medical management, which also could be what we call “one-stop shopping.” For instance, for directed biopsies for removal of small polyps, for patients that can tolerate the procedure a little longer, the diagnostic hysteroscopy then becomes a management, an operative procedure, that really, for myself, can be done in the office. Removal of larger fibroids, because of fluid management and other concerns, would not be done in the office. Most patients tolerate office procedures, but it also depends on a patient’s weight, and her ability to relax during the procedure.
The ultimate goal for hysteroscopy is a minimum of diagnosis, meaning in less than 2, 3 minutes, you can look inside the uterus. Our devices are 3 millimeters in size; I tell my patients, it’s the size of “a piece of spaghetti or pasta,” and we will just take a look. If we see a polyp, okay, if your office is not equipped, because then you need a different type of equipment for removal, then take her to the operating room. The patient would be under brief anesthesia and go home an hour or 2 later. So really, for physicians, we just need to embrace the technology to make a diagnosis, just look, and then from there decide what is next.
OBG Management: What techniques do you use to minimize or eliminate patient discomfort during hysteroscopy?...
OBG Management: What techniques do you use to minimize or eliminate patient discomfort during hysteroscopy?
Dr. Bradley: I think first is always be patient-centric. Let patients be prepared for the procedure. We have reading materials; our nurses explain the procedure. In the office, I try to prepare the patient for success. I let her know what is going on. A friend, family member can be with her. We have a nurse that understands the procedure; she explains it well. We have a type of bed that allows the patients’ legs to rest more comfortably in the stirrups—a leg rest kind of stirrup. We use a heating pad. Some patients like to hear music. Some patients like to have aromatherapy. We are quick and efficient, and typically just talk to the patient throughout the procedure. Although some patients don’t like this explanatory, “talkative” approach—they say, “Dr. Bradley, just do the procedure. I don’t want to know you are touching the cervix. I don’t want to know that you’re prepping. Just do it.”
But I like what we called it when I was growing up: vocal-local (talk to your patient and explain as you proceed). It’s like local anesthesia. For these procedures in the office you usually do not have to use numbing medicine or a paracervical block. Look at the patient’s age, number of years in menopause, whether or not she has delivered vaginally, and what her cervix looks like. Does she have a sexually transmitted infection or pelvic inflammatory disease? Sometimes we will use misoprostol, my personal preference is oral, but there are data to suggest that vaginal can be of help.4 We suggest Motrin, Tylenol an hour or 2 before, and we always want patients to not come in on an empty stomach. There is also the option of primrose oil, a supplement, that patients buy at the drug store in the vitamin section. It’s used for cervical softening. It is taken orally.5-7
If they want, patients can watch a video—similar to watching childbirth videos when I used to deliver babies. At some point we started putting mirrors where women could see their efforts of pushing a baby out, as it might give them more willpower to push harder. Some people don’t want to look. But the majority of women will do well in this setting. I do have a small number of women that just say, “I can’t do this in the office,” and so in those cases, they can go to the operating room. But the main idea is, even in an operating room, you are not just doing a D&C. You are still going to look inside with a hysteroscope and have a great panoramic view of what is going on, and remove a lesion with an instrument while you watch. Not a process of looking with the hysteroscope, scraping with a curettage, and thinking that you are complete. Targeted removal of focal lesions under continuous visualization is the goal.
OBG Management: Can you describe the goals of the consensus document on ending blind sampling co-created by the European Society of Gynecologic Endoscopy, AAGL, and the Global Community on Hysteroscopy?
Dr. Bradley: Our goal for this year is to get a systematic review and guidelines paper written that speaks to what we have just talked about. We want to have as many articles about why blind sampling is not beneficial, with too many misses, and now we have new technology available. We want to speak to physicians to solve the conundrum of bleeding, with equivocal ultrasounds, equivocal saline infusion, sonograms, equivocal MRIs—be able to take a look. Let’s come up to speed like our other colleagues in other specialties that “look.” A systematic review guideline document will provide the evidence that blind D&C is fraught with problems and how often we miss disease and its inherent risk.
We need to, by itself, for most of our patients, abandon D&C because we have too many missed diagnoses. As doctors we have to be lifelong learners. There was no robot back in the day. We were not able to do laparoscopic hysterectomies, there were no MRIs. I remember in our city, there was one CT scan. We just did not have a lot of technology. The half-life of medical knowledge used to be decades—you graduated in the ‘60s, you could be a great gynecologist for the next 30 years because there was not that much going on. When I finished in the mid to late ‘80s, there was no hysteroscopy training. But I have come to see its value, the science behind it.
So what I say to doctors is, “We learn so many new things, we shouldn’t get stuck in just saying, ‘I didn’t do this when I was in training.’” And if your thought is, “Oh, in my practice, I don’t have that many cases,” you still need to be able to know who in your community can be a resource to your patients. As Maya Angelou says, “When you know better, you should do better.” And that’s where I am now—to be a lifelong learner, and just do it.
Lastly, patient influence is very important. If patients ask, “How are you going to do the procedure?” it’s a driver for change. By utilizing hysteroscopy in the evaluation of the intrauterine cavity, we have the opportunity to change the face of evaluation and treatment for abnormal uterine bleeding.●
To maximize visualization and procedure ease, schedule office hysteroscopy shortly after menstruation for reproductive-age women with regular menstrual cycles, which corresponds to timing of the thinnest endometrial lining.1 By contrast, the luteal phase of the menstrual cycle may be associated with the presence of secretory endometrium, which may mimic endometrial polyps or obscure intrauterine pathology, including FIGO type 1 and 2 submucous leiomyomas.
The following patients can have their procedures scheduled at any time, as they do not regularly cycle:
- those receiving continuous hormonal contraception
- women taking menopausal hormonal therapy
- women on progestin therapy (including those using intrauterine devices).
For patients with irregular cycles, timing is crucial as the topography of the endometrium can be variable. To increase successful visualization and diagnostic accuracy, a short course of combined hormonal contraceptives2 or progestin therapy3,4 can be considered for 10-14 days, followed by a withdrawal menses, and immediate procedure scheduling after bleeding subsides, as this will produce a thin endometrium. This approach may be especially beneficial for operative procedures such as polypectomy in order to promote complete specimen extraction.
Pharmacologic endometrial preparation also is an option and has been associated with decreased procedure time and improved patient and clinician satisfaction during operative hysteroscopy.2,3 We discourage the use of hormonal pre-treatment for diagnostic hysteroscopy alone, as this may alter endometrial histology and provide misleading results. Overall, data related to pharmacologic endometrial preparation are limited to small studies with varying treatment protocols, and an optimal regimen has yet to be determined.
References
1. The use of hysteroscopy for the diagnosis and treatment of intrauterine pathology: ACOG Committee Opinion, number 800. Obstet Gynecol. 2020;135:e138-e148. doi:10.1097/AOG.0000000000003712.
2. Cicinelli E, Pinto V, Quattromini P, et al. Endometrial preparation with estradiol plus dienogest (Qlaira) for office hysteroscopic polypectomy: randomized pilot study. J Minim Invasive Gynecol. 2012;19:356-359. doi:10.1016/j.jmig.2011.12.020.
3. Laganà AS, Vitale SG, Muscia V, et al. Endometrial preparation with dienogest before hysteroscopic surgery: a systematic review. Arch Gynecol Obstet. 2017;295:661-667. doi:10.1007/s00404-016-4244-1.
4. Ciebiera M, Zgliczyńska M, Zgliczyński S, et al. Oral desogestrel as endometrial preparation before operative hysteroscopy: a systematic review. Gynecol Obstet Invest. 2021;86:209-217. doi:10.1159/000514584.
- Orlando MS, Bradley LD. Implementation of office hysteroscopy for the evaluation and treatment of intrauterine pathology. Obstet Gynecol. August 3, 2022. doi: 10.1097/ AOG.0000000000004898.
- Salazar CA, Isaacson KB. Office operative hysteroscopy: an update. J Minim Invasive Gynecol. 2018;25:199-208.
- Epstein E, Ramirez A, Skoog L, et al. Dilatation and curettage fails to detect most focal lesions in the uterine cavity in women with postmenopausal bleeding. Acta Obstet Gynecol Scand. 2001;80:1131-1136. doi:10.1034/j.1600-0412.2001.801210.x.
- The use of hysteroscopy for the diagnosis and treatment of intrauterine pathology: ACOG Committee Opinion, number 800. Obstet Gynecol. 2020;135:e138-e148. doi:10.1097/ AOG.0000000000003712.
- Vahdat M, Tahermanesh K, Mehdizadeh Kashi A, et al. Evening Primrose Oil effect on the ease of cervical ripening and dilatation before operative hysteroscopy. Thrita. 2015;4:7-10. doi:10.5812/thrita.29876
- Nouri B, Baghestani A, Pooransari P. Evening primrose versus misoprostol for cervical dilatation before gynecologic surgeries: a double-blind randomized clinical trial. J Obstet Gynecol Cancer Res. 2021;6:87-94. doi:10.30699/jogcr.6.2.87
- Verano RMA, Veloso-borromeo MG. The efficacy of evening primrose oil as a cervical ripening agent for gynecologic procedures: a single-blinded, randomized controlled trial. PJOG. 2015;39:24-28.
- Orlando MS, Bradley LD. Implementation of office hysteroscopy for the evaluation and treatment of intrauterine pathology. Obstet Gynecol. August 3, 2022. doi: 10.1097/ AOG.0000000000004898.
- Salazar CA, Isaacson KB. Office operative hysteroscopy: an update. J Minim Invasive Gynecol. 2018;25:199-208.
- Epstein E, Ramirez A, Skoog L, et al. Dilatation and curettage fails to detect most focal lesions in the uterine cavity in women with postmenopausal bleeding. Acta Obstet Gynecol Scand. 2001;80:1131-1136. doi:10.1034/j.1600-0412.2001.801210.x.
- The use of hysteroscopy for the diagnosis and treatment of intrauterine pathology: ACOG Committee Opinion, number 800. Obstet Gynecol. 2020;135:e138-e148. doi:10.1097/ AOG.0000000000003712.
- Vahdat M, Tahermanesh K, Mehdizadeh Kashi A, et al. Evening Primrose Oil effect on the ease of cervical ripening and dilatation before operative hysteroscopy. Thrita. 2015;4:7-10. doi:10.5812/thrita.29876
- Nouri B, Baghestani A, Pooransari P. Evening primrose versus misoprostol for cervical dilatation before gynecologic surgeries: a double-blind randomized clinical trial. J Obstet Gynecol Cancer Res. 2021;6:87-94. doi:10.30699/jogcr.6.2.87
- Verano RMA, Veloso-borromeo MG. The efficacy of evening primrose oil as a cervical ripening agent for gynecologic procedures: a single-blinded, randomized controlled trial. PJOG. 2015;39:24-28.
Resection of infected sacrohysteropexy mesh
Early estrogen loss increases cardiovascular risk in women
The relationship between estrogen levels and heart health makes it particularly important for clinicians to be aware of those patients who might be at risk for cardiovascular disease despite not having other traditional risk factors, according to a presentation Oct. 12 at the North American Menopause Society annual meeting in Atlanta.
”Endogenous estrogens are protective for cardiovascular disease in premenopausal women,” Chrisandra L. Shufelt, MD, chair of the division of general internal medicine and associate director of the Women’s Health Research Center at Mayo Clinic in Jacksonville, Fla., told attendees. Yet, “a substantial population of young women are dying prematurely from cardiovascular disease,” with rates of cardiovascular death increasing in women aged 35-44 even as rates have decreased in postmenopausal women and in men. One potential reason may be premature estrogen loss.
Dr. Shufelt reminded attendees of four major causes of premature estrogen loss: Natural premature menopause, surgical menopause, chemotherapy-induced menopause, and premature ovarian insufficiency. But she would go on to discuss a less widely recognized condition, functional hypothalamic amenorrhea, that also may be contributing to increased cardiovascular risk.
First, Dr. Shufelt reviewed the evidence supporting the relationship between estrogen and cardiovascular health, starting with the Framingham study’s findings that cardiovascular disease is approximately two to four times more common in postmenopausal women than in premenopausal women, depending on the age range.
“Menopause at an early age, particularly under the age of 40, matters,” Dr. Shufelt said. “So we should be discussing this with our patients.”
Surgical menopause makes a difference to cardiovascular health as well, she said. In women under age 35, for example, the risk of a nonfatal heart attack in those with a bilateral oophorectomy was 7.7 times greater than in women who retained both ovaries and their uterus, and 1.5 times greater in women who had a hysterectomy without bilateral oophorectomy.
In a 2019 study, surgical premature menopause was associated with an 87% increased risk of heart disease even after researchers accounted for age, cardiovascular risk factors, and some forms of hormone therapy. The increased risk from natural premature menopause, on the other hand, was lower – a 36% increased risk of heart disease – compared with those producing endogenous hormones. Although randomized controlled trials are unavailable and unlikely to be done, the Nurses’ Health Study and the Danish Nurses Cohort Study, both observational studies, found that heart disease risk was diminished in those taking hormone therapy after surgical premature menopause.
Recommendations for premature or early menopause, from a wide range of different medical societies including NAMS, are that women without contraindications be given estrogen-based hormone therapy until the average age of natural menopause. Though not included in the same guidance, research has also shown that estrogen after oophorectomy does not increase the risk of breast cancer in women with a BRCA1 mutation, Dr. Shufelt said. Hormone therapy for premature or early menopause should adequately replace the levels women have lost and that means younger menopausal women often need higher doses than what older women receive, such as 2 mg/day of oral estradiol rather than the standard doses of 0.5 or 1 mg/day.
Functional hypothalamic amenorrhea and cardiovascular risk
Dr. Shufelt then discussed functional hypothalamic amenorrhea (hypogonadotropic hypogonadism), a common type of secondary amenorrhea that affects at least 1.4 million U.S. women. Diagnosis includes lack of a period for at least 3 months in someone who previously menstruated plus lab values below 50 pg/mL for estradiol, below 10 mIU/L for follicle stimulating hormone, and below 10 mIU/L for luteinizing hormone. Causes of this reversible form of infertility can include stress, overexercising, undereating, or some combination of these, plus an underlying genetic predisposition.
“After ruling out polycystic ovary syndrome, prolactinoma, and thyroid dysfunction, clinicians need to consider the diagnosis of hypothalamic amenorrhea,” Dr. Shufelt said. This condition goes beyond low estrogen levels: Women have elevated cortisol, low thyroid levels, low leptin levels, and increased ghrelin.
”This is not going away,” Dr. Shufelt said, sharing data on stress levels among U.S. adults, particularly Gen Z and millennial adults, noting that the ongoing “national mental health crisis” may be contributing to functional hypothalamic amenorrhea.
A 2020 substudy from the Nurses’ Health Study II found an increased risk of premature death in those who didn’t have a period or always had irregular periods starting as early as 14-17 years old. The increased risk of premature death rose with age in those with irregular or absent cycles – a 37% higher risk in 18- to 22-year-olds and a 39% increased risk in 29- to 46-year-olds.
But clinicians aren’t adequately identifying the “phenotype of the hypothalamic women,” Dr. Shufelt said, despite research showing overlap between hypothalamic amenorrhea and a higher risk of cardiovascular disease. Hypothalamic amenorrhea is so understudied that the last original research on the topic was in 2008, Dr. Shufelt said in an interview. ”No research except mine has been done to evaluate heart health in these young women,” she said.
Dr. Shufelt described a study she led involving 30 women with functional hypothalamic amenorrhea, 29 women with normal menstrual cycles, and 30 women who were recently menopausal and not on hormone therapy. The women with hypothalamic amenorrhea had average stress levels but their depression scores were higher than those of the other two groups.
The results showed that women with hypothalamic amenorrhea had lower estradiol and leptin levels and higher testosterone levels compared with the control group, and they had higher cortisol levels than those of both groups. Despite having similar body mass indexes as the control and menopausal groups, women with hypothalamic amenorrhea had lower blood pressure than that of the other two groups, yet they had higher cholesterol levels than those of the control group. EndoPAT© (Itamar Medical) testing showed that they had poor vascular function.
“In fact, one-third of the women [with hypothalamic amenorrhea] entered the trial with a diagnosis of what would be considered endothelial dysfunction,” Dr. Shufelt said. “Our results demonstrated significantly higher circulating levels of serum proinflammatory cytokines in the women with hypothalamic amenorrhea compared to eumenorrheic controls.”
Dr. Shufelt’s team then tested whether giving estradiol to the women with hypothalamic amenorrhea for 12 weeks would improve their vascular health, but they saw no significant differences between the women who received estrogen and those who received placebo.
“Endothelial function is partly mediated by estrogen, and it was expected that giving back estrogen would ‘fix’ the endothelium, but that is not what happened,” Nanette Santoro, MD, professor and chair of obstetrics and gynecology at the University of Colorado at Denver, Aurora, said in interview. “The mechanisms that maintain vascular function in women are not limited to hormones,” said Dr. Santoro, who was not involved in Dr. Shufelt’s study but attended her lecture. “We need to think beyond the simple model of estrogen-good, no-estrogen-bad.”
Dr. Santoro noted how easy it is to overlook the women who may have cardiovascular risk because of hypothalamic amenorrhea.
“Because many women with functional hypothalamic amenorrhea are super athletic and do not have the typical features of people with cardiometabolic disease – such as glucose intolerance, obesity, abnormal cholesterol or triglycerides, or high blood pressure – clinicians tend to think of them as healthy and to think that simply giving back hormones will fix the problems with bone density and vascular function, but that is not enough,” Dr. Santoro said. “The cognitive-behavioral therapy model for treatment of women with functional hypothalamic amenorrhea addresses the stress-related factors that drive the disorder, and this needs to be considered the standard of care for treatment.”
Stephanie S. Faubion, MD, professor of medicine and director of Mayo Clinic’s Center for Women’s Health in Jacksonville, Fla., who was not involved in Dr. Shufelt’s presentation, also emphasized the importance of recognizing functional hypothalamic amenorrhea.
“This is an underrecognized entity to begin with, and the fact that these women appear to be at increased risk for vascular dysfunction and potentially increased risk for cardiovascular disease down the road makes it even more important for clinicians to identify them and provide interventions early on,” Dr. Faubion said in an interview. “These women need to be identified and the etiology of the amenorrhea addressed, whether it relates to overexercising, being underweight, or experiencing significant stressors that have led to the loss of menstrual cycles.”
Dr. Shufelt’s research was funded by the National Institutes of Health. She had no disclosures. Dr. Santoro is a member of the scientific advisory board for Astellas, Menogenix, Amazon Ember, and Que Oncology, and she consults for Ansh Labs. Dr. Faubion had no disclosures.
The relationship between estrogen levels and heart health makes it particularly important for clinicians to be aware of those patients who might be at risk for cardiovascular disease despite not having other traditional risk factors, according to a presentation Oct. 12 at the North American Menopause Society annual meeting in Atlanta.
”Endogenous estrogens are protective for cardiovascular disease in premenopausal women,” Chrisandra L. Shufelt, MD, chair of the division of general internal medicine and associate director of the Women’s Health Research Center at Mayo Clinic in Jacksonville, Fla., told attendees. Yet, “a substantial population of young women are dying prematurely from cardiovascular disease,” with rates of cardiovascular death increasing in women aged 35-44 even as rates have decreased in postmenopausal women and in men. One potential reason may be premature estrogen loss.
Dr. Shufelt reminded attendees of four major causes of premature estrogen loss: Natural premature menopause, surgical menopause, chemotherapy-induced menopause, and premature ovarian insufficiency. But she would go on to discuss a less widely recognized condition, functional hypothalamic amenorrhea, that also may be contributing to increased cardiovascular risk.
First, Dr. Shufelt reviewed the evidence supporting the relationship between estrogen and cardiovascular health, starting with the Framingham study’s findings that cardiovascular disease is approximately two to four times more common in postmenopausal women than in premenopausal women, depending on the age range.
“Menopause at an early age, particularly under the age of 40, matters,” Dr. Shufelt said. “So we should be discussing this with our patients.”
Surgical menopause makes a difference to cardiovascular health as well, she said. In women under age 35, for example, the risk of a nonfatal heart attack in those with a bilateral oophorectomy was 7.7 times greater than in women who retained both ovaries and their uterus, and 1.5 times greater in women who had a hysterectomy without bilateral oophorectomy.
In a 2019 study, surgical premature menopause was associated with an 87% increased risk of heart disease even after researchers accounted for age, cardiovascular risk factors, and some forms of hormone therapy. The increased risk from natural premature menopause, on the other hand, was lower – a 36% increased risk of heart disease – compared with those producing endogenous hormones. Although randomized controlled trials are unavailable and unlikely to be done, the Nurses’ Health Study and the Danish Nurses Cohort Study, both observational studies, found that heart disease risk was diminished in those taking hormone therapy after surgical premature menopause.
Recommendations for premature or early menopause, from a wide range of different medical societies including NAMS, are that women without contraindications be given estrogen-based hormone therapy until the average age of natural menopause. Though not included in the same guidance, research has also shown that estrogen after oophorectomy does not increase the risk of breast cancer in women with a BRCA1 mutation, Dr. Shufelt said. Hormone therapy for premature or early menopause should adequately replace the levels women have lost and that means younger menopausal women often need higher doses than what older women receive, such as 2 mg/day of oral estradiol rather than the standard doses of 0.5 or 1 mg/day.
Functional hypothalamic amenorrhea and cardiovascular risk
Dr. Shufelt then discussed functional hypothalamic amenorrhea (hypogonadotropic hypogonadism), a common type of secondary amenorrhea that affects at least 1.4 million U.S. women. Diagnosis includes lack of a period for at least 3 months in someone who previously menstruated plus lab values below 50 pg/mL for estradiol, below 10 mIU/L for follicle stimulating hormone, and below 10 mIU/L for luteinizing hormone. Causes of this reversible form of infertility can include stress, overexercising, undereating, or some combination of these, plus an underlying genetic predisposition.
“After ruling out polycystic ovary syndrome, prolactinoma, and thyroid dysfunction, clinicians need to consider the diagnosis of hypothalamic amenorrhea,” Dr. Shufelt said. This condition goes beyond low estrogen levels: Women have elevated cortisol, low thyroid levels, low leptin levels, and increased ghrelin.
”This is not going away,” Dr. Shufelt said, sharing data on stress levels among U.S. adults, particularly Gen Z and millennial adults, noting that the ongoing “national mental health crisis” may be contributing to functional hypothalamic amenorrhea.
A 2020 substudy from the Nurses’ Health Study II found an increased risk of premature death in those who didn’t have a period or always had irregular periods starting as early as 14-17 years old. The increased risk of premature death rose with age in those with irregular or absent cycles – a 37% higher risk in 18- to 22-year-olds and a 39% increased risk in 29- to 46-year-olds.
But clinicians aren’t adequately identifying the “phenotype of the hypothalamic women,” Dr. Shufelt said, despite research showing overlap between hypothalamic amenorrhea and a higher risk of cardiovascular disease. Hypothalamic amenorrhea is so understudied that the last original research on the topic was in 2008, Dr. Shufelt said in an interview. ”No research except mine has been done to evaluate heart health in these young women,” she said.
Dr. Shufelt described a study she led involving 30 women with functional hypothalamic amenorrhea, 29 women with normal menstrual cycles, and 30 women who were recently menopausal and not on hormone therapy. The women with hypothalamic amenorrhea had average stress levels but their depression scores were higher than those of the other two groups.
The results showed that women with hypothalamic amenorrhea had lower estradiol and leptin levels and higher testosterone levels compared with the control group, and they had higher cortisol levels than those of both groups. Despite having similar body mass indexes as the control and menopausal groups, women with hypothalamic amenorrhea had lower blood pressure than that of the other two groups, yet they had higher cholesterol levels than those of the control group. EndoPAT© (Itamar Medical) testing showed that they had poor vascular function.
“In fact, one-third of the women [with hypothalamic amenorrhea] entered the trial with a diagnosis of what would be considered endothelial dysfunction,” Dr. Shufelt said. “Our results demonstrated significantly higher circulating levels of serum proinflammatory cytokines in the women with hypothalamic amenorrhea compared to eumenorrheic controls.”
Dr. Shufelt’s team then tested whether giving estradiol to the women with hypothalamic amenorrhea for 12 weeks would improve their vascular health, but they saw no significant differences between the women who received estrogen and those who received placebo.
“Endothelial function is partly mediated by estrogen, and it was expected that giving back estrogen would ‘fix’ the endothelium, but that is not what happened,” Nanette Santoro, MD, professor and chair of obstetrics and gynecology at the University of Colorado at Denver, Aurora, said in interview. “The mechanisms that maintain vascular function in women are not limited to hormones,” said Dr. Santoro, who was not involved in Dr. Shufelt’s study but attended her lecture. “We need to think beyond the simple model of estrogen-good, no-estrogen-bad.”
Dr. Santoro noted how easy it is to overlook the women who may have cardiovascular risk because of hypothalamic amenorrhea.
“Because many women with functional hypothalamic amenorrhea are super athletic and do not have the typical features of people with cardiometabolic disease – such as glucose intolerance, obesity, abnormal cholesterol or triglycerides, or high blood pressure – clinicians tend to think of them as healthy and to think that simply giving back hormones will fix the problems with bone density and vascular function, but that is not enough,” Dr. Santoro said. “The cognitive-behavioral therapy model for treatment of women with functional hypothalamic amenorrhea addresses the stress-related factors that drive the disorder, and this needs to be considered the standard of care for treatment.”
Stephanie S. Faubion, MD, professor of medicine and director of Mayo Clinic’s Center for Women’s Health in Jacksonville, Fla., who was not involved in Dr. Shufelt’s presentation, also emphasized the importance of recognizing functional hypothalamic amenorrhea.
“This is an underrecognized entity to begin with, and the fact that these women appear to be at increased risk for vascular dysfunction and potentially increased risk for cardiovascular disease down the road makes it even more important for clinicians to identify them and provide interventions early on,” Dr. Faubion said in an interview. “These women need to be identified and the etiology of the amenorrhea addressed, whether it relates to overexercising, being underweight, or experiencing significant stressors that have led to the loss of menstrual cycles.”
Dr. Shufelt’s research was funded by the National Institutes of Health. She had no disclosures. Dr. Santoro is a member of the scientific advisory board for Astellas, Menogenix, Amazon Ember, and Que Oncology, and she consults for Ansh Labs. Dr. Faubion had no disclosures.
The relationship between estrogen levels and heart health makes it particularly important for clinicians to be aware of those patients who might be at risk for cardiovascular disease despite not having other traditional risk factors, according to a presentation Oct. 12 at the North American Menopause Society annual meeting in Atlanta.
”Endogenous estrogens are protective for cardiovascular disease in premenopausal women,” Chrisandra L. Shufelt, MD, chair of the division of general internal medicine and associate director of the Women’s Health Research Center at Mayo Clinic in Jacksonville, Fla., told attendees. Yet, “a substantial population of young women are dying prematurely from cardiovascular disease,” with rates of cardiovascular death increasing in women aged 35-44 even as rates have decreased in postmenopausal women and in men. One potential reason may be premature estrogen loss.
Dr. Shufelt reminded attendees of four major causes of premature estrogen loss: Natural premature menopause, surgical menopause, chemotherapy-induced menopause, and premature ovarian insufficiency. But she would go on to discuss a less widely recognized condition, functional hypothalamic amenorrhea, that also may be contributing to increased cardiovascular risk.
First, Dr. Shufelt reviewed the evidence supporting the relationship between estrogen and cardiovascular health, starting with the Framingham study’s findings that cardiovascular disease is approximately two to four times more common in postmenopausal women than in premenopausal women, depending on the age range.
“Menopause at an early age, particularly under the age of 40, matters,” Dr. Shufelt said. “So we should be discussing this with our patients.”
Surgical menopause makes a difference to cardiovascular health as well, she said. In women under age 35, for example, the risk of a nonfatal heart attack in those with a bilateral oophorectomy was 7.7 times greater than in women who retained both ovaries and their uterus, and 1.5 times greater in women who had a hysterectomy without bilateral oophorectomy.
In a 2019 study, surgical premature menopause was associated with an 87% increased risk of heart disease even after researchers accounted for age, cardiovascular risk factors, and some forms of hormone therapy. The increased risk from natural premature menopause, on the other hand, was lower – a 36% increased risk of heart disease – compared with those producing endogenous hormones. Although randomized controlled trials are unavailable and unlikely to be done, the Nurses’ Health Study and the Danish Nurses Cohort Study, both observational studies, found that heart disease risk was diminished in those taking hormone therapy after surgical premature menopause.
Recommendations for premature or early menopause, from a wide range of different medical societies including NAMS, are that women without contraindications be given estrogen-based hormone therapy until the average age of natural menopause. Though not included in the same guidance, research has also shown that estrogen after oophorectomy does not increase the risk of breast cancer in women with a BRCA1 mutation, Dr. Shufelt said. Hormone therapy for premature or early menopause should adequately replace the levels women have lost and that means younger menopausal women often need higher doses than what older women receive, such as 2 mg/day of oral estradiol rather than the standard doses of 0.5 or 1 mg/day.
Functional hypothalamic amenorrhea and cardiovascular risk
Dr. Shufelt then discussed functional hypothalamic amenorrhea (hypogonadotropic hypogonadism), a common type of secondary amenorrhea that affects at least 1.4 million U.S. women. Diagnosis includes lack of a period for at least 3 months in someone who previously menstruated plus lab values below 50 pg/mL for estradiol, below 10 mIU/L for follicle stimulating hormone, and below 10 mIU/L for luteinizing hormone. Causes of this reversible form of infertility can include stress, overexercising, undereating, or some combination of these, plus an underlying genetic predisposition.
“After ruling out polycystic ovary syndrome, prolactinoma, and thyroid dysfunction, clinicians need to consider the diagnosis of hypothalamic amenorrhea,” Dr. Shufelt said. This condition goes beyond low estrogen levels: Women have elevated cortisol, low thyroid levels, low leptin levels, and increased ghrelin.
”This is not going away,” Dr. Shufelt said, sharing data on stress levels among U.S. adults, particularly Gen Z and millennial adults, noting that the ongoing “national mental health crisis” may be contributing to functional hypothalamic amenorrhea.
A 2020 substudy from the Nurses’ Health Study II found an increased risk of premature death in those who didn’t have a period or always had irregular periods starting as early as 14-17 years old. The increased risk of premature death rose with age in those with irregular or absent cycles – a 37% higher risk in 18- to 22-year-olds and a 39% increased risk in 29- to 46-year-olds.
But clinicians aren’t adequately identifying the “phenotype of the hypothalamic women,” Dr. Shufelt said, despite research showing overlap between hypothalamic amenorrhea and a higher risk of cardiovascular disease. Hypothalamic amenorrhea is so understudied that the last original research on the topic was in 2008, Dr. Shufelt said in an interview. ”No research except mine has been done to evaluate heart health in these young women,” she said.
Dr. Shufelt described a study she led involving 30 women with functional hypothalamic amenorrhea, 29 women with normal menstrual cycles, and 30 women who were recently menopausal and not on hormone therapy. The women with hypothalamic amenorrhea had average stress levels but their depression scores were higher than those of the other two groups.
The results showed that women with hypothalamic amenorrhea had lower estradiol and leptin levels and higher testosterone levels compared with the control group, and they had higher cortisol levels than those of both groups. Despite having similar body mass indexes as the control and menopausal groups, women with hypothalamic amenorrhea had lower blood pressure than that of the other two groups, yet they had higher cholesterol levels than those of the control group. EndoPAT© (Itamar Medical) testing showed that they had poor vascular function.
“In fact, one-third of the women [with hypothalamic amenorrhea] entered the trial with a diagnosis of what would be considered endothelial dysfunction,” Dr. Shufelt said. “Our results demonstrated significantly higher circulating levels of serum proinflammatory cytokines in the women with hypothalamic amenorrhea compared to eumenorrheic controls.”
Dr. Shufelt’s team then tested whether giving estradiol to the women with hypothalamic amenorrhea for 12 weeks would improve their vascular health, but they saw no significant differences between the women who received estrogen and those who received placebo.
“Endothelial function is partly mediated by estrogen, and it was expected that giving back estrogen would ‘fix’ the endothelium, but that is not what happened,” Nanette Santoro, MD, professor and chair of obstetrics and gynecology at the University of Colorado at Denver, Aurora, said in interview. “The mechanisms that maintain vascular function in women are not limited to hormones,” said Dr. Santoro, who was not involved in Dr. Shufelt’s study but attended her lecture. “We need to think beyond the simple model of estrogen-good, no-estrogen-bad.”
Dr. Santoro noted how easy it is to overlook the women who may have cardiovascular risk because of hypothalamic amenorrhea.
“Because many women with functional hypothalamic amenorrhea are super athletic and do not have the typical features of people with cardiometabolic disease – such as glucose intolerance, obesity, abnormal cholesterol or triglycerides, or high blood pressure – clinicians tend to think of them as healthy and to think that simply giving back hormones will fix the problems with bone density and vascular function, but that is not enough,” Dr. Santoro said. “The cognitive-behavioral therapy model for treatment of women with functional hypothalamic amenorrhea addresses the stress-related factors that drive the disorder, and this needs to be considered the standard of care for treatment.”
Stephanie S. Faubion, MD, professor of medicine and director of Mayo Clinic’s Center for Women’s Health in Jacksonville, Fla., who was not involved in Dr. Shufelt’s presentation, also emphasized the importance of recognizing functional hypothalamic amenorrhea.
“This is an underrecognized entity to begin with, and the fact that these women appear to be at increased risk for vascular dysfunction and potentially increased risk for cardiovascular disease down the road makes it even more important for clinicians to identify them and provide interventions early on,” Dr. Faubion said in an interview. “These women need to be identified and the etiology of the amenorrhea addressed, whether it relates to overexercising, being underweight, or experiencing significant stressors that have led to the loss of menstrual cycles.”
Dr. Shufelt’s research was funded by the National Institutes of Health. She had no disclosures. Dr. Santoro is a member of the scientific advisory board for Astellas, Menogenix, Amazon Ember, and Que Oncology, and she consults for Ansh Labs. Dr. Faubion had no disclosures.
FROM NAMS 2022
Few transgender teens discontinue hormones in young adulthood
Most adolescents with gender dysphoria who took puberty-blocking drugs for at least 3 months and then progressed to cross-sex hormone treatment were still taking hormones as they entered adulthood, new research of patients at a pioneering Dutch clinic shows.
The study negates past findings that large numbers of youth regret transitioning, say Maria Anna Theodora Catharina van der Loos, MD, and colleagues from the Centre of Expertise on Gender Dysphoria, Amsterdam, in their article published online in The Lancet Child & Adolescent Health. They believe the difference between their findings and those of other studies lies in proper diagnostic evaluation.
“The study aims to demonstrate, with a methodology that is more than adequate, that transgender people who begin their transition in childhood-adolescence do not give up,” Adrián Carrasco Munera, MD, a specialist in family and community medicine and member of the LGTBIQ+ Health Group of the Madrid Society of Family and Community Medicine told the UK Science Media Centre.
The cohort included 720 youth: 220 (31%) were assigned male at birth (AMAB) and 500 (69%) were assigned female at birth (AFAB). At the start of puberty-blocking treatment with a gonadotrophin-releasing hormone agonist, the median age of patients was 14.1 years for AMAB and 16.0 years for AFAB.
Of that cohort, 704 (98%) continued hormone therapy to the end of data collection (Dec. 31, 2018), at which point the median age of patients was 20 years for AMAB and 19 years for AFAB.
Careful consideration of patient needs
All the patients received care at the “Dutch Clinic,” which more than 20 years ago pioneered the approach of giving puberty-blocking drugs to children looking to transition, followed by cross-sex hormones. The study includes the “complete adolescent population” at the facility who met the inclusion criteria.
A similar U.S. study published earlier this year found that 74.4% of individuals who had started gender-affirming hormones before age 18 were still on them 4 years after starting medical treatment.
“However, it is unclear how many of these adolescents [in the U.S. study] used puberty-suppressing treatment before gender-affirming hormone treatment and to what extent they underwent diagnostic evaluation before initiation of medical treatment,” say Dr. van der Loos and colleagues.
She told this news organization that her clinic provides “a thorough diagnostic and mental health assessment” and discussion of fertility preservation prior to any youth being prescribed puberty blockers or cross-sex hormones.
About 40% of adolescents assessed by the gender clinic in Amsterdam go on to receive hormonal treatment.
“The gender identity unit of the Amsterdam UMC is a world leader in all aspects of transgender medicine and is governed by protocolized actions. This is reflected in the quality of the data and methodology of the study, and therefore of its conclusions,” endocrinologist Gilberto Pérez López, MD, Gregorio Marañón General University Hospital, Madrid, told the UK Science Media Centre.
“These findings can and should help and guide the current public and legal debate on the initiation of medical treatment in transgender minors.”
However, he cautioned the study is limited by the fact that the data come from a registry and they looked at only prescriptions issued and not compliance.
Another interesting thing to note in the research is that almost 70% of patients were born girls and they presented at the gender clinics later in adolescence than the natal boys.
“We don’t have a sound reason for this,” Dr. van der Loos noted.
Study limitations
She also acknowledges that the short follow-up data in some individuals make it difficult to draw conclusions about regret, to some extent.
The average use of cross-sex hormones in their study was 3.5 years for males transitioning to females and 2.3 years for females transitioning to males, so on average, this wouldn’t be long enough to see regret, she acknowledged.
Prior research shows that if youth decide to detransition to their natal sex, this can take, on average, 5 years from the start of medical therapy among born females and 7 years among born males.
However, some born males in the study had been taking hormones for 20 years and some natal females for 15 years, said Dr. van der Loos.
Another limitation is that the research only followed individuals until the end of 2018 while some government data estimate that the number of teens identifying as transgender has nearly doubled over the past 5 years.
The authors, Dr. Munera, and Dr. Lopez have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Most adolescents with gender dysphoria who took puberty-blocking drugs for at least 3 months and then progressed to cross-sex hormone treatment were still taking hormones as they entered adulthood, new research of patients at a pioneering Dutch clinic shows.
The study negates past findings that large numbers of youth regret transitioning, say Maria Anna Theodora Catharina van der Loos, MD, and colleagues from the Centre of Expertise on Gender Dysphoria, Amsterdam, in their article published online in The Lancet Child & Adolescent Health. They believe the difference between their findings and those of other studies lies in proper diagnostic evaluation.
“The study aims to demonstrate, with a methodology that is more than adequate, that transgender people who begin their transition in childhood-adolescence do not give up,” Adrián Carrasco Munera, MD, a specialist in family and community medicine and member of the LGTBIQ+ Health Group of the Madrid Society of Family and Community Medicine told the UK Science Media Centre.
The cohort included 720 youth: 220 (31%) were assigned male at birth (AMAB) and 500 (69%) were assigned female at birth (AFAB). At the start of puberty-blocking treatment with a gonadotrophin-releasing hormone agonist, the median age of patients was 14.1 years for AMAB and 16.0 years for AFAB.
Of that cohort, 704 (98%) continued hormone therapy to the end of data collection (Dec. 31, 2018), at which point the median age of patients was 20 years for AMAB and 19 years for AFAB.
Careful consideration of patient needs
All the patients received care at the “Dutch Clinic,” which more than 20 years ago pioneered the approach of giving puberty-blocking drugs to children looking to transition, followed by cross-sex hormones. The study includes the “complete adolescent population” at the facility who met the inclusion criteria.
A similar U.S. study published earlier this year found that 74.4% of individuals who had started gender-affirming hormones before age 18 were still on them 4 years after starting medical treatment.
“However, it is unclear how many of these adolescents [in the U.S. study] used puberty-suppressing treatment before gender-affirming hormone treatment and to what extent they underwent diagnostic evaluation before initiation of medical treatment,” say Dr. van der Loos and colleagues.
She told this news organization that her clinic provides “a thorough diagnostic and mental health assessment” and discussion of fertility preservation prior to any youth being prescribed puberty blockers or cross-sex hormones.
About 40% of adolescents assessed by the gender clinic in Amsterdam go on to receive hormonal treatment.
“The gender identity unit of the Amsterdam UMC is a world leader in all aspects of transgender medicine and is governed by protocolized actions. This is reflected in the quality of the data and methodology of the study, and therefore of its conclusions,” endocrinologist Gilberto Pérez López, MD, Gregorio Marañón General University Hospital, Madrid, told the UK Science Media Centre.
“These findings can and should help and guide the current public and legal debate on the initiation of medical treatment in transgender minors.”
However, he cautioned the study is limited by the fact that the data come from a registry and they looked at only prescriptions issued and not compliance.
Another interesting thing to note in the research is that almost 70% of patients were born girls and they presented at the gender clinics later in adolescence than the natal boys.
“We don’t have a sound reason for this,” Dr. van der Loos noted.
Study limitations
She also acknowledges that the short follow-up data in some individuals make it difficult to draw conclusions about regret, to some extent.
The average use of cross-sex hormones in their study was 3.5 years for males transitioning to females and 2.3 years for females transitioning to males, so on average, this wouldn’t be long enough to see regret, she acknowledged.
Prior research shows that if youth decide to detransition to their natal sex, this can take, on average, 5 years from the start of medical therapy among born females and 7 years among born males.
However, some born males in the study had been taking hormones for 20 years and some natal females for 15 years, said Dr. van der Loos.
Another limitation is that the research only followed individuals until the end of 2018 while some government data estimate that the number of teens identifying as transgender has nearly doubled over the past 5 years.
The authors, Dr. Munera, and Dr. Lopez have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Most adolescents with gender dysphoria who took puberty-blocking drugs for at least 3 months and then progressed to cross-sex hormone treatment were still taking hormones as they entered adulthood, new research of patients at a pioneering Dutch clinic shows.
The study negates past findings that large numbers of youth regret transitioning, say Maria Anna Theodora Catharina van der Loos, MD, and colleagues from the Centre of Expertise on Gender Dysphoria, Amsterdam, in their article published online in The Lancet Child & Adolescent Health. They believe the difference between their findings and those of other studies lies in proper diagnostic evaluation.
“The study aims to demonstrate, with a methodology that is more than adequate, that transgender people who begin their transition in childhood-adolescence do not give up,” Adrián Carrasco Munera, MD, a specialist in family and community medicine and member of the LGTBIQ+ Health Group of the Madrid Society of Family and Community Medicine told the UK Science Media Centre.
The cohort included 720 youth: 220 (31%) were assigned male at birth (AMAB) and 500 (69%) were assigned female at birth (AFAB). At the start of puberty-blocking treatment with a gonadotrophin-releasing hormone agonist, the median age of patients was 14.1 years for AMAB and 16.0 years for AFAB.
Of that cohort, 704 (98%) continued hormone therapy to the end of data collection (Dec. 31, 2018), at which point the median age of patients was 20 years for AMAB and 19 years for AFAB.
Careful consideration of patient needs
All the patients received care at the “Dutch Clinic,” which more than 20 years ago pioneered the approach of giving puberty-blocking drugs to children looking to transition, followed by cross-sex hormones. The study includes the “complete adolescent population” at the facility who met the inclusion criteria.
A similar U.S. study published earlier this year found that 74.4% of individuals who had started gender-affirming hormones before age 18 were still on them 4 years after starting medical treatment.
“However, it is unclear how many of these adolescents [in the U.S. study] used puberty-suppressing treatment before gender-affirming hormone treatment and to what extent they underwent diagnostic evaluation before initiation of medical treatment,” say Dr. van der Loos and colleagues.
She told this news organization that her clinic provides “a thorough diagnostic and mental health assessment” and discussion of fertility preservation prior to any youth being prescribed puberty blockers or cross-sex hormones.
About 40% of adolescents assessed by the gender clinic in Amsterdam go on to receive hormonal treatment.
“The gender identity unit of the Amsterdam UMC is a world leader in all aspects of transgender medicine and is governed by protocolized actions. This is reflected in the quality of the data and methodology of the study, and therefore of its conclusions,” endocrinologist Gilberto Pérez López, MD, Gregorio Marañón General University Hospital, Madrid, told the UK Science Media Centre.
“These findings can and should help and guide the current public and legal debate on the initiation of medical treatment in transgender minors.”
However, he cautioned the study is limited by the fact that the data come from a registry and they looked at only prescriptions issued and not compliance.
Another interesting thing to note in the research is that almost 70% of patients were born girls and they presented at the gender clinics later in adolescence than the natal boys.
“We don’t have a sound reason for this,” Dr. van der Loos noted.
Study limitations
She also acknowledges that the short follow-up data in some individuals make it difficult to draw conclusions about regret, to some extent.
The average use of cross-sex hormones in their study was 3.5 years for males transitioning to females and 2.3 years for females transitioning to males, so on average, this wouldn’t be long enough to see regret, she acknowledged.
Prior research shows that if youth decide to detransition to their natal sex, this can take, on average, 5 years from the start of medical therapy among born females and 7 years among born males.
However, some born males in the study had been taking hormones for 20 years and some natal females for 15 years, said Dr. van der Loos.
Another limitation is that the research only followed individuals until the end of 2018 while some government data estimate that the number of teens identifying as transgender has nearly doubled over the past 5 years.
The authors, Dr. Munera, and Dr. Lopez have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
It’s about location: PCOS symptoms differ depending where you live
Geographic location within the United States appears to have an impact on the specific symptoms of polycystic ovary syndrome (PCOS) that any one particular woman will develop, according to a new prospective cohort study.
Women in California were more likely to exhibit high levels of testosterone (hyperandrogenism), while women in Alabama with PCOS had more metabolic dysfunction and hirsutism.
And although the women in Alabama were younger and had a higher body mass index (BMI), even after adjusting for these factors, the clinical differences were still present between the geographic locations, the authors said.
“This study suggests there are regional differences in hormonal and metabolic parameters in women with PCOS in California and Alabama, highlighting the impact of differing genetic and environmental modulators on PCOS development,” Katherine VanHise, MD, of Cedars-Sinai Medical Center, Los Angeles, and colleagues wrote in their article, published online in the Journal of Clinical Endocrinology and Metabolism.
Genetic and environmental factors play a role
Prior research has looked at variations in symptoms of PCOS across countries and identified differences in hirsutism and its prevalence, which is greater in Middle Eastern, Mediterranean, and Indian women, noted senior author Margareta D. Pisarska, MD.
And women of some other backgrounds “are at increased risk of developing metabolic syndrome and insulin resistance, including South Asian, African, and Hispanic women, so they are at a greater risk trajectory of developing manifestations later on in life that can ultimately lead to adverse outcomes in overall health,” Dr. Pisarska, director of the division of reproductive endocrinology and infertility in obstetrics and gynecology at Cedars-Sinai, told this news organization.
“We do see regional differences in the diagnosis of PCOS [in the United States] as well as the manifestations of PCOS including high andrenoemia, hirsutism, and metabolic parameters ... and we need to better understand it because, at least in the entire population, weight was not the entire factor contributing to these differences,” she explained.
“So there are definitely environmental factors and possibly genetic factors that we need to take into consideration as we try to study these women and try to help them decrease their risk of metabolic syndrome later in life,” she noted.
Differences not attributable to race either
PCOS is a common endocrine disorder affecting women and female adolescents worldwide. Diagnosis usually requires at least two of the following to be present: ovulatory dysfunction, hyperandrogenism, and/or polycystic ovarian morphology.
Because of the prior work that had identified differences in symptoms among women with PCOS in different countries, the investigators set out to determine if women of the same race would have distinct hormonal and metabolic traits of PCOS in two geographical locations in the United States, suggesting geo-epidemiologic contributors of the disease
They evaluated 889 women at the University of Alabama at Birmingham and 721 at Cedars-Sinai Medical Center. Participants in Birmingham were a mean age of 28 years, had a mean BMI of 33.1 kg/m2, a mean waist-to-hip ratio of 0.8, and a mean hirsute rate of 84.6%. Participants in California were a mean age of 29.5 years, had an average BMI of 30.1 kg/m2, a mean waist-to-hip ratio of 0.9, and a mean hirsute rate of 72.8%.
The study team gathered data on menstrual cycle history, metabolic and hormonal parameters, and demographic data for each participant. They assessed hirsutism based on modified Ferriman-Gallwey scores of four or more. Patients were classified as having hyperandrogenemia if they had elevated androgen values greater than the 95th percentile of all values or androgen values that exceeded laboratory reference ranges.
The findings showed that Alabama women with PCOS had elevated homeostatic model assessment for insulin resistance scores (adjusted beta coefficient, 3.6; P < .001) and were more likely to be hirsute (adjusted odds ratio, 1.8; P < .001) after adjustment for BMI and age than those in California.
In contrast, women with PCOS in California were more likely to have elevated free testosterone and total testosterone values than women in Alabama (both P < .001). These findings persisted after adjusting for age and BMI.
When stratified by White race, these findings were similar. Notably, BMI and waist-to-hip ratio did not vary between regions in Black women with PCOS, although variations in metabolic dysfunction and androgen profiles persisted.
“This study supports regional differences in hormonal and metabolic parameters in women with PCOS in the United States, highlighting the impact of the environment on PCOS phenotype. Individuals of the same race in different geographical locations of the United States may have differing genetic predispositions for developing diseases such as PCOS,” the researchers said.
“Ongoing research is needed to identify modifiable environmental risk factors for PCOS that may be race and ethnic specific to bring precision medicine to the management of PCOS,” they conclude.
This work was supported in part by grants from the National Institutes of Health and an endowment of the Helping Hand of Los Angeles. Dr. VanHise reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Geographic location within the United States appears to have an impact on the specific symptoms of polycystic ovary syndrome (PCOS) that any one particular woman will develop, according to a new prospective cohort study.
Women in California were more likely to exhibit high levels of testosterone (hyperandrogenism), while women in Alabama with PCOS had more metabolic dysfunction and hirsutism.
And although the women in Alabama were younger and had a higher body mass index (BMI), even after adjusting for these factors, the clinical differences were still present between the geographic locations, the authors said.
“This study suggests there are regional differences in hormonal and metabolic parameters in women with PCOS in California and Alabama, highlighting the impact of differing genetic and environmental modulators on PCOS development,” Katherine VanHise, MD, of Cedars-Sinai Medical Center, Los Angeles, and colleagues wrote in their article, published online in the Journal of Clinical Endocrinology and Metabolism.
Genetic and environmental factors play a role
Prior research has looked at variations in symptoms of PCOS across countries and identified differences in hirsutism and its prevalence, which is greater in Middle Eastern, Mediterranean, and Indian women, noted senior author Margareta D. Pisarska, MD.
And women of some other backgrounds “are at increased risk of developing metabolic syndrome and insulin resistance, including South Asian, African, and Hispanic women, so they are at a greater risk trajectory of developing manifestations later on in life that can ultimately lead to adverse outcomes in overall health,” Dr. Pisarska, director of the division of reproductive endocrinology and infertility in obstetrics and gynecology at Cedars-Sinai, told this news organization.
“We do see regional differences in the diagnosis of PCOS [in the United States] as well as the manifestations of PCOS including high andrenoemia, hirsutism, and metabolic parameters ... and we need to better understand it because, at least in the entire population, weight was not the entire factor contributing to these differences,” she explained.
“So there are definitely environmental factors and possibly genetic factors that we need to take into consideration as we try to study these women and try to help them decrease their risk of metabolic syndrome later in life,” she noted.
Differences not attributable to race either
PCOS is a common endocrine disorder affecting women and female adolescents worldwide. Diagnosis usually requires at least two of the following to be present: ovulatory dysfunction, hyperandrogenism, and/or polycystic ovarian morphology.
Because of the prior work that had identified differences in symptoms among women with PCOS in different countries, the investigators set out to determine if women of the same race would have distinct hormonal and metabolic traits of PCOS in two geographical locations in the United States, suggesting geo-epidemiologic contributors of the disease
They evaluated 889 women at the University of Alabama at Birmingham and 721 at Cedars-Sinai Medical Center. Participants in Birmingham were a mean age of 28 years, had a mean BMI of 33.1 kg/m2, a mean waist-to-hip ratio of 0.8, and a mean hirsute rate of 84.6%. Participants in California were a mean age of 29.5 years, had an average BMI of 30.1 kg/m2, a mean waist-to-hip ratio of 0.9, and a mean hirsute rate of 72.8%.
The study team gathered data on menstrual cycle history, metabolic and hormonal parameters, and demographic data for each participant. They assessed hirsutism based on modified Ferriman-Gallwey scores of four or more. Patients were classified as having hyperandrogenemia if they had elevated androgen values greater than the 95th percentile of all values or androgen values that exceeded laboratory reference ranges.
The findings showed that Alabama women with PCOS had elevated homeostatic model assessment for insulin resistance scores (adjusted beta coefficient, 3.6; P < .001) and were more likely to be hirsute (adjusted odds ratio, 1.8; P < .001) after adjustment for BMI and age than those in California.
In contrast, women with PCOS in California were more likely to have elevated free testosterone and total testosterone values than women in Alabama (both P < .001). These findings persisted after adjusting for age and BMI.
When stratified by White race, these findings were similar. Notably, BMI and waist-to-hip ratio did not vary between regions in Black women with PCOS, although variations in metabolic dysfunction and androgen profiles persisted.
“This study supports regional differences in hormonal and metabolic parameters in women with PCOS in the United States, highlighting the impact of the environment on PCOS phenotype. Individuals of the same race in different geographical locations of the United States may have differing genetic predispositions for developing diseases such as PCOS,” the researchers said.
“Ongoing research is needed to identify modifiable environmental risk factors for PCOS that may be race and ethnic specific to bring precision medicine to the management of PCOS,” they conclude.
This work was supported in part by grants from the National Institutes of Health and an endowment of the Helping Hand of Los Angeles. Dr. VanHise reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Geographic location within the United States appears to have an impact on the specific symptoms of polycystic ovary syndrome (PCOS) that any one particular woman will develop, according to a new prospective cohort study.
Women in California were more likely to exhibit high levels of testosterone (hyperandrogenism), while women in Alabama with PCOS had more metabolic dysfunction and hirsutism.
And although the women in Alabama were younger and had a higher body mass index (BMI), even after adjusting for these factors, the clinical differences were still present between the geographic locations, the authors said.
“This study suggests there are regional differences in hormonal and metabolic parameters in women with PCOS in California and Alabama, highlighting the impact of differing genetic and environmental modulators on PCOS development,” Katherine VanHise, MD, of Cedars-Sinai Medical Center, Los Angeles, and colleagues wrote in their article, published online in the Journal of Clinical Endocrinology and Metabolism.
Genetic and environmental factors play a role
Prior research has looked at variations in symptoms of PCOS across countries and identified differences in hirsutism and its prevalence, which is greater in Middle Eastern, Mediterranean, and Indian women, noted senior author Margareta D. Pisarska, MD.
And women of some other backgrounds “are at increased risk of developing metabolic syndrome and insulin resistance, including South Asian, African, and Hispanic women, so they are at a greater risk trajectory of developing manifestations later on in life that can ultimately lead to adverse outcomes in overall health,” Dr. Pisarska, director of the division of reproductive endocrinology and infertility in obstetrics and gynecology at Cedars-Sinai, told this news organization.
“We do see regional differences in the diagnosis of PCOS [in the United States] as well as the manifestations of PCOS including high andrenoemia, hirsutism, and metabolic parameters ... and we need to better understand it because, at least in the entire population, weight was not the entire factor contributing to these differences,” she explained.
“So there are definitely environmental factors and possibly genetic factors that we need to take into consideration as we try to study these women and try to help them decrease their risk of metabolic syndrome later in life,” she noted.
Differences not attributable to race either
PCOS is a common endocrine disorder affecting women and female adolescents worldwide. Diagnosis usually requires at least two of the following to be present: ovulatory dysfunction, hyperandrogenism, and/or polycystic ovarian morphology.
Because of the prior work that had identified differences in symptoms among women with PCOS in different countries, the investigators set out to determine if women of the same race would have distinct hormonal and metabolic traits of PCOS in two geographical locations in the United States, suggesting geo-epidemiologic contributors of the disease
They evaluated 889 women at the University of Alabama at Birmingham and 721 at Cedars-Sinai Medical Center. Participants in Birmingham were a mean age of 28 years, had a mean BMI of 33.1 kg/m2, a mean waist-to-hip ratio of 0.8, and a mean hirsute rate of 84.6%. Participants in California were a mean age of 29.5 years, had an average BMI of 30.1 kg/m2, a mean waist-to-hip ratio of 0.9, and a mean hirsute rate of 72.8%.
The study team gathered data on menstrual cycle history, metabolic and hormonal parameters, and demographic data for each participant. They assessed hirsutism based on modified Ferriman-Gallwey scores of four or more. Patients were classified as having hyperandrogenemia if they had elevated androgen values greater than the 95th percentile of all values or androgen values that exceeded laboratory reference ranges.
The findings showed that Alabama women with PCOS had elevated homeostatic model assessment for insulin resistance scores (adjusted beta coefficient, 3.6; P < .001) and were more likely to be hirsute (adjusted odds ratio, 1.8; P < .001) after adjustment for BMI and age than those in California.
In contrast, women with PCOS in California were more likely to have elevated free testosterone and total testosterone values than women in Alabama (both P < .001). These findings persisted after adjusting for age and BMI.
When stratified by White race, these findings were similar. Notably, BMI and waist-to-hip ratio did not vary between regions in Black women with PCOS, although variations in metabolic dysfunction and androgen profiles persisted.
“This study supports regional differences in hormonal and metabolic parameters in women with PCOS in the United States, highlighting the impact of the environment on PCOS phenotype. Individuals of the same race in different geographical locations of the United States may have differing genetic predispositions for developing diseases such as PCOS,” the researchers said.
“Ongoing research is needed to identify modifiable environmental risk factors for PCOS that may be race and ethnic specific to bring precision medicine to the management of PCOS,” they conclude.
This work was supported in part by grants from the National Institutes of Health and an endowment of the Helping Hand of Los Angeles. Dr. VanHise reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY AND METABOLISM
CVS cuts prices of menstrual products, covers sales tax in some states
CVS is cutting the cost of its store-branded menstrual products and paying state sales taxes on them in a dozen states.
The drug store chain said that starting Thursday it was reducing prices on CVS Health and Live Better tampons, menstrual pads, liners, and cups by 25%.
“Women deserve quality when it comes to the products they may need each month,” CVS said in a statement. “We’re paying the tax on period products on behalf of our customers where and when possible, and are working to help eliminate the tax nationwide.”
The store is also trying to equalize costs between men’s and women’s hygiene products, like razors.
The chain is paying sales taxes on period products in these 12 states: Arkansas, Georgia, Hawaii, Louisiana, Missouri, South Carolina, Tennessee, Texas, Utah, Virginia, Wisconsin, and West Virginia.
It can’t pay the taxes in other states that have them because of laws that prevent third parties from paying taxes for a customer.
“This move will highlight their commitment to addressing women’s health and pave the way for reducing menstrual inequity,” Padmini Murthy, MD, the global health lead for the American Medical Women’s Association, said in an email to CNN, “and not just to promote the use of CVS products.”
Twenty-three states don’t tax feminine hygiene products, says the Alliance for Period Supplies, an advocacy group seeking to expand access to menstrual supplies.
“Too often period products are taxed as luxury items and not recognized as basic necessities,” the organization said. “Period products are taxed at a similar rate to items like decor, electronics, makeup, and toys.”
Tampon prices rose 12.2% for the year ending Oct. 2, according to market research firm IRI.
And 25% of women struggle to buy the products because of the expense, says the group.
A version of this article first appeared on WebMD.com.
CVS is cutting the cost of its store-branded menstrual products and paying state sales taxes on them in a dozen states.
The drug store chain said that starting Thursday it was reducing prices on CVS Health and Live Better tampons, menstrual pads, liners, and cups by 25%.
“Women deserve quality when it comes to the products they may need each month,” CVS said in a statement. “We’re paying the tax on period products on behalf of our customers where and when possible, and are working to help eliminate the tax nationwide.”
The store is also trying to equalize costs between men’s and women’s hygiene products, like razors.
The chain is paying sales taxes on period products in these 12 states: Arkansas, Georgia, Hawaii, Louisiana, Missouri, South Carolina, Tennessee, Texas, Utah, Virginia, Wisconsin, and West Virginia.
It can’t pay the taxes in other states that have them because of laws that prevent third parties from paying taxes for a customer.
“This move will highlight their commitment to addressing women’s health and pave the way for reducing menstrual inequity,” Padmini Murthy, MD, the global health lead for the American Medical Women’s Association, said in an email to CNN, “and not just to promote the use of CVS products.”
Twenty-three states don’t tax feminine hygiene products, says the Alliance for Period Supplies, an advocacy group seeking to expand access to menstrual supplies.
“Too often period products are taxed as luxury items and not recognized as basic necessities,” the organization said. “Period products are taxed at a similar rate to items like decor, electronics, makeup, and toys.”
Tampon prices rose 12.2% for the year ending Oct. 2, according to market research firm IRI.
And 25% of women struggle to buy the products because of the expense, says the group.
A version of this article first appeared on WebMD.com.
CVS is cutting the cost of its store-branded menstrual products and paying state sales taxes on them in a dozen states.
The drug store chain said that starting Thursday it was reducing prices on CVS Health and Live Better tampons, menstrual pads, liners, and cups by 25%.
“Women deserve quality when it comes to the products they may need each month,” CVS said in a statement. “We’re paying the tax on period products on behalf of our customers where and when possible, and are working to help eliminate the tax nationwide.”
The store is also trying to equalize costs between men’s and women’s hygiene products, like razors.
The chain is paying sales taxes on period products in these 12 states: Arkansas, Georgia, Hawaii, Louisiana, Missouri, South Carolina, Tennessee, Texas, Utah, Virginia, Wisconsin, and West Virginia.
It can’t pay the taxes in other states that have them because of laws that prevent third parties from paying taxes for a customer.
“This move will highlight their commitment to addressing women’s health and pave the way for reducing menstrual inequity,” Padmini Murthy, MD, the global health lead for the American Medical Women’s Association, said in an email to CNN, “and not just to promote the use of CVS products.”
Twenty-three states don’t tax feminine hygiene products, says the Alliance for Period Supplies, an advocacy group seeking to expand access to menstrual supplies.
“Too often period products are taxed as luxury items and not recognized as basic necessities,” the organization said. “Period products are taxed at a similar rate to items like decor, electronics, makeup, and toys.”
Tampon prices rose 12.2% for the year ending Oct. 2, according to market research firm IRI.
And 25% of women struggle to buy the products because of the expense, says the group.
A version of this article first appeared on WebMD.com.