User login
Simplifying or Switching Antiretroviral Therapy in Treatment-Experienced Adults Living With HIV
A 57-year-old man living with HIV has been followed at a local infectious disease clinic for more than 15 years. He acquired HIV disease through heterosexual contact. He lives alone and works at a convenience store; he has not been sexually active for the past 5 years. He smokes 10 cigarettes a day, but does not drink alcohol or use illicit drugs. He had been on coformulated emtricitabine/tenofovir disoproxil fumarate (TDF) and coformulated lopinavir/ritonavir, which he had taken conscientiously, since May 2008, without noticing any adverse reactions from this regimen. His HIV viral load had been undetectable, and his CD4 count had hovered between 600 and 700 cells/µL. Although he was on atorvastatin for dyslipidemia, his fasting lipid profile, performed in 2018, revealed a total cholesterol level of 200 mg/dL;triglyceride, 247 mg/dL; high-density lipoprotein (HDL), 43 mg/dL; and low-density lipoprotein (LDL), 132 mg/dL. In April 2019, his HIV regimen was switched to bictegravir/emtricitabine/tenofovir alafenamide (TAF). Blood tests performed in December 2019 revealed undetectable HIV viral load; an increased CD4 count to 849 cell/µL; total cholesterol, 140 mg/dL; triglyceride, 115 mg/dL; HDL, 60 mg/dL; and LDL, 90 mg/dL.
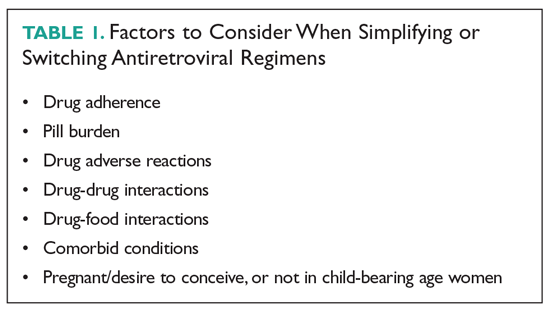
SIMPLIFYING ART
Virologically Suppressed Patients Without Drug-Resistant Virus
Treatment adherence is of paramount importance to ensure treatment success. Patients with a viral load that is undetectable or nearly undetectable without drug resistance could be taking ART regimens consisting of more than 1 pill and/or that require more than once-daily dosing. Decreasing pill burden or dosing frequency can help to improve adherence to treatment. In addition, older-generation ART agents are usually more toxic and less potent than newer-generation agents, so another important objective of switching older drugs to newer drugs is to decrease adverse reactions and improve virologic suppression. Selection of an ART regimen should be guided by the results of resistance testing (genotyping and phenotyping tests) and previous treatment history. After switching a patient’s ART regimen, plasma HIV viral load and CD4 count should be closely monitored.2 The following 3-drug, single-tablet, once-daily ART regimens can be used in patients who are virologically stable (ordered chronologically by FDA approval dates).
Efavirenz/Emtricitabine/TDF (Atripla)
Coformulated efavirenz/emtricitabine/TDF was the first single-tablet, once-daily, fixed-dose combination approved by the FDA (July 2006). Approval was based on a 48- week clinical trial involving 244 adults with HIV infection that showed that 80% of participants achieved a marked reduction in HIV viral load and a significant increase in CD4 cell count.3 Of the 3 components, efavirenz has unique central nervous system (CNS) adverse effects that could reduce adherence. Patients who were started on this fixed-dose combination commonly reported dizziness, headache, nightmare, insomnia, and impaired concentration.4 However, the CNS side effects resolved within the first 4 weeks of therapy, and less than 5% of patients quit taking the drug. Primate studies showed efavirenz is teratogenic, but studies in pregnant women did not find efavirenz to be more teratogenic than other ART agents.5
Emtricitabine/Rilpivirine/TDF (Complera)
Coformulated emtricitabine/rilpivirine/TDF was approved based on data from two 48-week, phase 3, double-blind, randomized controlled trials (ECHO and THRIVE) that evaluated the safety and efficacy of rilpivirine compared to efavirenz among treatment-naive adults with HIV infection.7,8 Rilpivirine is well tolerated and causes fewer CNS symptoms compared to efavirenz. The main caveat for rilpivirine is drug-drug interactions. It should not be coadministered with CYP inducers, such as rifampin, phenytoin, or St. John’s wort, as coadministration can cause subtherapeutic blood levels of rilpivirine. Because increased levels of rilpivirine can prolong QTc on electrocardiogram (ECG), an ECG should be obtained before starting an ART regimen that contains rilpivirine, especially in the presence of CYP 3A4 inhibitors.9
Elvitegravir/Cobicistat/Emtricitabine/TDF (Stribild)
This coformulation was approved based on data from 2 randomized, double-blind, controlled trials, Study 102 and Study 103, in treatment-naive patients with HIV (n = 1408). In Study 102, participants were randomized to receive either elvitegravir/cobicistat/emtricitabine/TDF or efavirenz/emtricitabine/TDF (Atripla).10 In Study 103, participants were randomized to receive either elvitegravir/cobicistat/emtricitabine/TDF or atazanavir + ritonavir + emtricitabine/TDF. In both studies, the primary endpoint was virologic success (HIV-1 RNA < 50 copies/mL) at 48 weeks, and elvitegravir/cobicistat/emtricitabine/TDF was noninferior compared to the other regimens.11
Abacavir/Dolutegravir/Lamivudine (Triumeq)
Approval of abacavir/dolutegravir/lamivudine (Triumeq) in August 2014 was based on SINGLE, a noninferiority trial involving 833 treatment-naive adults that compared dolutegravir and abacavir/lamivudine (the separate components of Triumeq) to efavirenz/emtricitabine/TDF. At 96 weeks, more patients in the dolutegravir and abacavir/lamivudine arm achieved an undetectable HIV viral load (80% versus 72%).13
Elvitegravir/Cobicistat/Emtricitabine/TAF (Genvoya)
Approval of coformulated elvitegravir/cobicistat/emtricitabine/TAF was supported by data from two 48-week phase 3, double-blind studies (Studies 104 and 111) involving 1733 treatment-naive patients that compared the regimen to elvitegravir/cobicistat/emtricitabine/TDF (Stribild). Both studies demonstrated that elvitegravir/cobicistat/emtricitabine/TAF was statistically noninferior, and it was favored in regard to certain renal and bone laboratory parameters.15 Studies comparing TAF and TDF have demonstrated that TAF is less likely to cause loss of bone mineral density and nephrotoxicity compared to TDF.16,17
Emtricitabine/Rilpivirine/TAF (Odefsey)
Coformulated emtricitabine/rilpivirine/TAF was approved based, in part, on positive bioequivalence studies demonstrating that it achieved similar drug levels of emtricitabine and TAF as coformulated elvitegravir/cobicistat/emtricitabine/TAF and similar drug levels of rilpivirine as individually dosed rilpivirine.18 The safety, efficacy, and tolerability of this coformulation is supported by clinical studies of rilpivirine-based therapy and emtricitabine/TAF-based therapy in a range of patients with HIV.18
Bictegravir/Emtricitabine/TAF (Biktarvy)
The coformulation bictegravir/emtricitabine/TAF was approved based on 4 phase 3 studies: Studies 1489 and 1490 in treatment-naive adults, and Studies 1844 and 1878 in virologically suppressed adults. In Study 1489, 629 treatment-naive adults were randomized 1:1 to receive coformulated bictegravir/emtricitabine/TAF or coformulated abacavir/dolutegravir/lamivudine. At week 48, similar percentages of patients in each arm achieved the primary endpoint of HIV-1 RNA < 50 copies/mL. In Study 1490, 645 treatment-naive adults were randomized 1:1 to receive coformulated bictegravir/emtricitabine/TAF or dolutegravir + emtricitabine/TAF. At week 48, similar percentages of patients in each arm achieved the primary endpoint of virologic success (HIV-1 RNA < 50 copies/mL).19,20
Darunavir/Cobicistat/Emtricitabine/TAF (Symtuza)
Approval of coformulated darunavir/cobicistat/emtricitabine/TAF was based on data from two 48-week, noninferiority, phase 3 studies that assessed the safety and efficacy of the coformulation versus a control regimen (darunavir/cobicistat plus emtricitabine/TDF) in adults with no prior ART history (AMBER) and in virologically suppressed adults (EMERALD). In the randomized, double-blind, multicenter controlled AMBER trial, at week 48, 91.4% of patients in the study group and 88.4% in the control group achieved viral suppression (HIV-1 RNA < 50 copies/mL), and virologic failure rates were low in both groups (HIV-1 RNA ≥ 50 copies/mL; 4.4% versus 3.3%, respectively).21
Doravirine/Lamivudine/TDF (Delstrigo)
Coformulated doravirine/lamivudine/TDF was approved based on data from 2 randomized, double-blind, controlled phase 3 trials, DRIVE-AHEAD and DRIVE-FORWARD. The former trial compared coformulated doravirine/lamivudine/TDF with efavirenz/emtricitabine/TDF in 728 treatment-naive patients. At 48 weeks, 84.3% in the doravirine/lamivudine/TDF arm and 80.8% in the efavirenz/emtricitabine/TDF arm met the primary endpoint of HIV-1 RNA < 50 copies/mL. Thus, doravirine/lamivudine/TDF showed sustained viral suppression and noninferiority compared to efavirenz/emtricitabine/TDF.23 The DRIVE-FORWARD trial investigated doravirine compared with ritonavir-boosted darunavir, each in combination with 2 NRTIs (TDF with emtricitabine or abacavir with lamivudine). At week 48, 84% of patients in the doravirine arm and 80% in the ritonavir-boosted darunavir arm achieved the primary endpoint of HIV-1 RNA < 50 copies/mL.24
Two-Drug, Single-Tablet, Once-Daily Regimens
Experts have long recommended that optimal treatment of HIV must consist of 3 active drugs, with trials both in the United States and Europe demonstrating decreased morbidity and mortality with 3-drug therapy.25,26 However, newer, more potent 2-drug therapy is giving more choices to people living with HIV. The single-tablet, 2-drug regimens currently available are dolutegravir/rilpivirine and dolutegravir/lamivudine. There are theoretical benefits of 2-drug therapy, such as minimizing long-term toxicities, avoidance of some drug-drug interactions, and preservation of drugs for future treatment options. At this time, a 2-drug simplification regimen can be a viable option for selected virologically stable populations.
Dolutegravir/Rilpivirine (Juluca)
Dolutegravir/rilpivirine has been shown to be noninferior to standard therapy at 48-weeks, although it is associated with a higher discontinuation rate because of side effects.27 This option can be particularly useful in patients who have contraindications to NRTIs or renal dysfunction, but it has been studied only in patients without resistance who are already virologically suppressed. Ongoing studies are looking at 2-versus 3-drug therapies for HIV treatment-experienced patients. Most of these use PIs as a backbone because of their potency and high barrier to resistance. The advent of second-generation integrase inhibitors offers additional options.
Dolutegravir/Lamivudine (Dovato)
The GEMINI-1 and GEMINI-2 trials demonstrated that dolutegravir/lamivudine was noninferior to dolutegravir/TDF/emtricitabine.28 Based on these 2 studies, new guidelines have added dolutegravir/lamivudine as a recommended first-line therapy. For now, the recommendation is to use dolutegravir/lamivudine in individuals where NRTIs are contraindicated, and it should not be used in patients with chronic hepatitis B. Additionally, 3 studies have demonstrated the safety and efficacy of switching to dolutegravir/lamivudine.29-31 In the TANGO trial, neither virologic failures nor resistant virus were identified at 48 weeks following the switch.32 Although there are benefits of simplification with this regimen, including lower toxicity, lower costs, and saving other NRTIs in case of resistance, there should be no rush to switch patients to a 2-drug regimen. This is a viable strategy in patients without baseline resistance who have preserved T-cells and do not have hepatitis B.
SWITCHING ART AGENTS IN SELECTED CLINICAL SCENARIOS
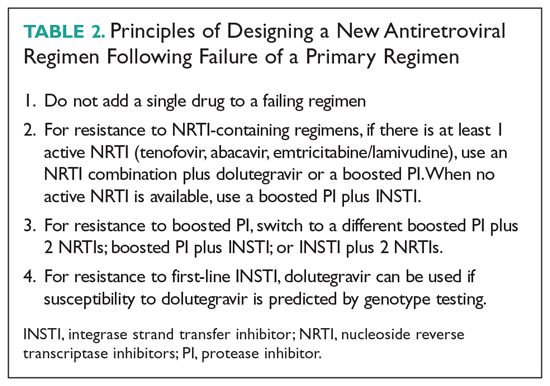
Virologic Failure
One of the main goals of ART is maximal and durable suppression of HIV viral load to prevent the development of drug-resistant mutations.2 When patients are unable to achieve durable virologic suppression or have virologic rebound, the cause of virologic failure needs to be investigated. Virologic failure is defined as the inability to achieve or maintain viral suppression to a level below 200 copies/mL, whereas rebound is defined as an HIV RNA level exceeding 200 copies/mL after virologic suppression.33 A common cause of virologic failure is patient nonadherence, which can be related to a range of factors, including psychosocial issues and affordability of medications. Innate viral resistance can be the result of transmitted drug resistance at the time of infection or be acquired during unsuppressed viral replication secondary to inherent error-prone reverse transcriptase.33 Pharmacokinetic factors that affect blood levels of ART, such as drug-drug interactions, also can be a key factor in HIV drug resistance.
Patients With Limited Treatment Options
Despite advances in ART, some patients exhaust the existing regimens, leading to development of multidrug resistance and limited treatment options. In light of the treatment challenges in this group of patients, the FDA has recently approved 2 antiretroviral agents to target multidrug-resistant HIV: ibalizumab and fostemsavir.
Pregnancy
ART is used during pregnancy to maintain the pregnant woman’s health and to prevent perinatal transmission. Pregnancy can present unique challenges to effective ART, and therapy decisions should be made based on short-term and long-term safety data, pharmacokinetics, and tolerability. With few exceptions, women who are on a stable ART regimen and present for care should continue the same regimen.38 Key exceptions, due to increased toxicity, include didanosine, indinavir, nelfinavir, stavudine, and treatment-dose ritonavir. Cobicistat-based regimens (atazanavir, darunavir, elvitegravir) have altered pharmacokinetics during the second and third trimesters of pregnancy, leading to reduced mean steady-state minimum concentrations.39 Because increasing plasma HIV RNA level is associated with transmission to infants, women continuing cobicistat-based ART treatments should undergo more frequent viral load measurements.40 If viral rebound occurs late in pregnancy, especially shortly before delivery, achieving viral suppression can be more difficult. Therefore, women on a suppressed ART regimen containing cobicistat should consider switching to a different recommended regimen.38
Geriatric Populations
Although HIV is seen predominantly in younger patients, 48% of persons living with HIV are older than 50 years and 8% are 65 years of age or older.46 With effective antiretroviral treatment, we will continue to see an aging population of people living with HIV. There are no specific guidelines regarding the treatment of older adults, but HIV treatment can have its own challenges. Physiologic declines in renal function occur with aging, which can be compounded by an increasing prevalence of diabetes and decreased muscle mass, making estimations of renal function unreliable.47 Physiologic changes with age, such as decline in renal and hepatic function, decreasing metabolism via cytochrome P450, and body composition, influence drug pharmacokinetics and can in turn potentiate drug toxicities.48 Comorbid states and polypharmacy can complicate care. The prevalence of polypharmacy in the elderly is high, 93%, and is increasing.49,50 A study found that in those aged 65 years or older with HIV, 65% had at least 1 potential drug-drug interaction, and 6.6% had a potential severe drug-drug interaction.50 These patients are thus at risk of poor drug adherence, which in HIV therapy can lead to rebound viremia and resistance.
Renal Insufficiency
Several commonly used ART agents have nephrotoxic potential. The most common manifestations of nephrotoxicity are tubular toxicity, crystal nephropathy, and interstitial nephritis. Of these, acute tubular toxicity caused by TDF is the most widely reported. About 2% of those taking TDF developed treatment-limiting renal insufficiency, manifested as Fanconi syndrome.53 Higher plasma levels of TDF are associated with increased nephrotoxicity.55 Guidelines recommend switching from TDF if the estimated glomerular filtration rate (eGFR) declines by > 25% or the eGFr is < 60/mL/min/1.73 m2. Wever et al reports that in TDF-associated nephrotoxicity, only 42% of patients reached their pre-TDF eGFR.54TAF, a prodrug of TDF, is associated with reduced levels of TDF and is hypothesized to have fewer adverse effects.55 A pooled analysis comparing renal adverse effects of TDF and TAF reported no cases of renal dysfunction in the TAF group, supporting its safety; however, acute kidney injury has also been reported with TAF.56,57 Switching from TDF to TAF in patients with renal dysfunction has been shown to lead to improvement in proteinuria, but the impact remains unclear.53
Dyslipidemia and Cardiovascular Risk
Aside from the traditional cardiovascular risks, PIs, TAF, and efavirenz can negatively affect the lipid profile, with changes in LDL and triglycerides appearing as early as 2 weeks after initiating therapy. An observational study from Spain showed that treatment with TAF worsens the lipid profile in comparison to patients treated with TDF for elvitegravir/cobicistat-based therapies; patients on TAF were twice as likely to need lipid-lower drugs in comparison to those in the TDF arm.61 Similarly, patients who changed from a TDF-based regimen to TAF for improved renal and bone safety profiles had significant changes in both total cholesterol and LDL.65Other NRTIs do not negatively affect lipid profile. Although NNRTIs can increase LDL, this is usually offset by an increase in HDL.62 Of the NNRTIs, the incidence of increased LDL is higher with efavirenz, but it also can cause an increase in HDL; in contrast, patients switched from efavirenz to rilpivirine have a better lipid profile.63,64 PIs, especially older ones such as lopinavir/ritonavir, are associated with lipid abnormalities. For patients who develop dyslipidemia as a result of using older PIs, switching to a darunavir or atazanavir regimen or even integrase inhibitors, which are considered lipid neutral, is recommended.63 When making adjustments in ART, care should be taken in prescribing abacavir to individuals with risk factors for coronary artery disease. Although there is no consensus, some randomized controlled trials suggested an association between myocardial infarction and abacavir, whereas others have not.66,67
HIV and Hepatis B Co-infection
In patients with HIV and hepatitis B co-infection, ART regimens should contain 1 drug that is active against hepatitis B (lamivudine, emtricitabine, TDF, or TAF). Clinicians should monitor liver function for hepatitis B reactivation and liver function when a regimen that contains anti-hepatitis B drugs is stopped because discontinuation of these regimens can result in acute, and sometimes fatal, liver damage.2
Financial Considerations
With out-of-pocket expenses and co-pays, some patients may have to switch ART regimens for financial reasons. Additionally, switching to generic versions of ART has been proposed as a means of saving resources for government programs already facing budgetary constraints. A study published in 2013 using generic-based ART versus branded ART showed a potential savings of almost $1 billion per year.68 A key barrier to the use of generic-based ART is patient skepticism regarding the performance of these medications. Branded ART regimens are also co-formulated, creating the perception that taking more pills will lead to noncompliance and therefore place the patient at risk of viral rebound. In a study from France, only 17% of patients were willing to switch to generic medications if doing so increased pill burden.69 In the same study, 75% physicians were generally willing to prescribe generics; however, that number dropped to 26% if the patient’s pill burden would increase.69 Paradoxically, because of the patchwork of insurance, government assistance, Medicaid, and Medicare, changing to generic-based ART may increase patients’ co-pays.
1. Benson CA, Gandhi RT, et al. Antiretroviral drugs for treatment and prevention of HIV infection in adults. 2018 recommendations of the International Antiviral Society-USA Panel. JAMA. 2018; 320:379-396.
2. Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents living with HIV. http://www.aidsinfo.nih.gov/ContentFiles/ AdultandAdolescentGL.pdf. Accessed July 14, 2020.
3. FDA approves the first once-a-day three-drug combination tablet for treatment of HIV-1. https://aidsinfo.nih.gov/news/769/fda-approves-the-first-once-a-day-three-drug-combination-tablet-for-treatment-of-hiv-1. Accessed July 14, 2020.
4. Apostolova N, Funes HA, Blas-Garcia A, et al. Efavirenz and the CNS: what we already know and questions that need to be answered. J Antimicrob Chemother. 2015;70:2693-2708.
5. de Béthune MP. Non-nucleoside reverse transcriptase inhibitors (NNRTIs), their discovery, development, and use in the treatment of HIV-1 infection: a review of the last 20 years (1989-2009). Antiviral Res. 2010;85:75-90.
6. Carey D, Puls R, Amin J, et al. Efficacy and safety of efanvirenz 400mg daily versus 600 mg daily: 96-week data from the randomized, double-blind, placebo-controlled, non-inferiority ENCORE1 study. Lancet Infect Dis. 2015;15:793-802.
7. Molina JM, Cahn P, Grinsztejn B, et al; ECHO study group. Rilpivirine versus efavirenz with tenofovir and emtricitabine in treatment-naive adults infected with HIV-1 (ECHO): a phase 3 randomised double-blind active-controlled trial. Lancet. 2011;378:238-246.
8. Cohen CJ, Andrade-Villanueva J, Clotet B, et al. THRIVE study group Rilpivirine versus efavirenz with two background nucleoside or nucleotide reverse transcriptase inhibitors in treatment-naive adults infected with HIV-1 (THRIVE): a phase 3, randomised, non-inferiority trial. Lancet. 2011;378:229-237.
9. James C, Preninger L, Sweet M. Rilpivirine: A second-generation nonnucleoside reverse transcriptase inhibitor. Am J Health Syst Pharm. 2012;69:857-861.
10. Zolopa A, Sax PE, DeJesus E, et al. GS-US-236-0102 Study Team A randomized double-blind comparison of coformulated elvitegravir/cobicistat/emtricitabine/tenofovir disoproxil fumarate versus efavirenz/emtricitabine/tenofovir disoproxil fumarate for initial treatment of HIV-1 infection: analysis of week 96 results. J Acquir Immune Defic Syndr. 2013;63:96-100.
11. DeJesus E, Rockstroh JK, Henry K, et al. GS-236-0103 Study Team Co-formulated elvitegravir, cobicistat, emtricitabine, and tenofovir disoproxil fumarate versus ritonavir-boosted atazanavir plus co-formulated emtricitabine and tenofovir disoproxil fumarate for initial treatment of HIV-1 infection: a randomised, double-blind, phase 3, non-inferiority trial. Lancet. 2012;379:2429-2438.
12. Sherman EM, et al. Cobicistat: review of a pharmacokinetic enhancer for HIV infection. Clin Ther. 2015;37:1876-1893.
13. Walmsley S, Baumgarten A, Berenguer J, et al. Dolutegravir plus abacavir/lamivudine for the treatment of HIV-1 infection in antiretroviral therapy-naive patients: week 96 and week 144 results from the SINGLE randomized clinical trial. J Acquir Immune Defic Syndr. 2015;70:515-519.
14. Barbarino JM, Kroetz DL, Altman RB, Klein TE. PharmGKB summary: abacavir pathway. Pharmacogenet Genomics. 2014;24:276-282.
15. Sax PE, Wohl DA, Yin MT, et al. Tenofovir alafenamide versus tenofovir disoproxil fumarate, coformulated with elvitegravir, cobicistat, and emtricitabine, for initial treatment of HIV-1 infection: two randomized, double-blind, phase 3, non-inferiority trials. Lancet. 2015;385:2606–2615.
16. DeJesus E, Haas B, Segal-Maurer S, et al. Superior efficacy and improved renal and bone safety after switching from a tenofovir disoproxil fumarate regimen to a tenofovir alafenamide-based regimen through 96 weeks of treatment. AIDS Res Hum Retroviruses. 2016;34:337-342.
17. Maggiolo F, Rizzardini G, Raff F, et al. Bone mineral density in virologically suppressed people aged 60 years or older with HIV-1 switching from a regimen containing tenofovir disoproxil fumarate to an elvitegravir, cobicistat, emtricitabine, and tenofovir alafenamide single-tablet regimen: a multicentre, open-label, phase 3b, randomised trial. Lancet HIV. 2019;6: e655-e666.
18. Ogbuagu O. Rilpivirine, emtricitabine and tenofovir alafenamide: single-tablet combination for the treatment of HIV-1 infection in selected patients. Expert Rev Anti Infect Ther. 2016;;14:1113-1126.
19. Gallant J, Lazzarin A, Mills A, et al. Bictegravir, emtricitabine, and tenofovir alafenamide versus dolutegravir, abacavir, and lamivudine for initial treatment of HIV-1 infection (GS-US-380-1489): a double-blind, multicentre, phase 3, randomised controlled non-inferiority trial. Lancet. 2017;390:2063-2072.
20. Sax PE, Pozniak A, Montes ML, et al. Coformulated bictegravir, emtricitabine, and tenofovir alafenamide versus dolutegravir with emtricitabine and tenofovir alafenamide, for the initial treatment of HIV-1 infection (GS-US-1490): a randomised, double-blind, multicenter, phase 3, non-inferiority trial. Lancet. 2017;390:2073-2082.
21. Eron JJ, Orkin C, Gallant J, et al. A week-48 randomized phase-3 trial of darunavir/cobicistat/emtricitabine/tenofovir alafenamide in treatment-naive HIV-1 patients. AIDS. 2018;32:1431-1442.
22. Orkin C, Molina JM, Negredo E, et al;. EMERALD study group. Efficacy and safety of switching from boosted protease inhibitors plus emtricitabine/tenofovir disoproxil fumarate regimens to the once-daily complete HIV-1 regimen of darunavir/cobicistat/emtricitabine/tenofovir alafenamide (D/C/F/TAF) in virologically suppressed, HIV-1-infected adults through 48 weeks (EMERALD): a phase 3, randomized, non-inferiority trial. Lancet HIV. 2018;5:e23-e34.
23. Orkin C, Squires KE, Molina JM, et al. Doravirine/lamivudine/tenofovir disoproxil fumarate is non-inferior to efavirenz/emtricitabine/tenofovir disoproxil fumarate in treatment-naive adults with human immunodeficiency virus-1 infection: week 48 results of the DRIVE-AHEAD Trial. Clin Infect Dis. 2019;68:535-544.
24. Molina JM, Squires K, Sax PE, et al. Doravirine versus ritonavir-boosted darunavir in antiretroviral-naive adults with HIV-1 (DRIVE-FORWARD): 48-week results of a randomised, double-blind, phase 3, non-inferiority trial. Lancet HIV. 2018;5:e211-e220.
25. Palella FJ, Delaney KM, Moorman ACE, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med. 1998;338:853-860.
26. Mocroft A, Vella S, Benfiedl TL. Changing patterns of mortality across Europe in patients infected with HIV-1. Lancet. 1998;3552:1725-1730.
27. Libre JM, Hugh CC, Castelli F, et al. Efficacy, safety, and tolerability of dolutegravir-rilpivirine for the maintenance of virological suppression in adults with HIV-1: phase 3, randomized, noninferiority SWORD-1 and SWORD-2 studies. Lancet. 2018;391:839-849.
28. Cahn P, Madero JS, Arribas JR, et al. Durable efficacy of dolutegravir plus lamivudine in antiretroviral treatment-naive adults with HIV-1 infection: 96-week results from the GEMINI-1 and GEMINI-2 randomized clinical trials. J Acquir Immune Defic Syndr. 2020;83:310-318.
29. Joly V, Burdet C, Landman R, et al. Dolutegravir and lamivudine maintenance therapy in HIV-1 virologically suppressed patients: results of the ANRS 167 trial (LAMIDOL). J Antimicrob Chemother. 2019;74:739-745.
30. Li JZ, Sax PE, Marconi VC, et al. No significant changes to residual viremia after switch to dolutegravir and lamivudine in a randomized trial. Open Forum Infect Dis. 2019;6:ofz056.
31. Taiwo BO, Marconi VC, Verzins B, et al. Dolutegravir plus lamivudine maintains human immunodeficiency virus-1 suppression through week 48 in a pilot randomized trial. Clin Infect Dis. 2018;66:1794-1979.
32. Van Wyk J, Ajana F, Bisshop F, et al. Efficacy and safety of switching to dolutegravir/lamivudine fixed-dose 2-drug regimen vs continuing a tenofovir alafenamide–based 3- or 4-drug regimen for maintenance of virologic suppression in adults living with human immunodeficiency virus type 1: phase 3, randomized, noninferiority TANGO Study. Clin Infect Dis. Jan 6;ciz1243. doi: 10.1093/cid/ciz1243.
33. Cutrell J, Jodlowski T, Bedimo R. The management of treatment-experienced HIV patients (including virologic failure and switches). Ther Adv Infectious Dis. 2020;7:1-15.
34. Devereux, HL, Youle, M, Johnson, MA, et al. Rapid decline in detectability of HIV-1 drug resistance mutations after stopping therapy. AIDS. 1999;13:F123-F127.
35. Gatanaga H, Tsukada K, Honda H, et al. Detection of HIV type 1 load by the Roche Cobas TaqMan assay in patients with viral loads previously undetectable by the Roche Cobas Amplicor Monitor. Clin Infect Dis. 2009;48:260-262.
36. Emu B, Fessel J, Schrader S, et al. Phase 3 study of ibalizumab for multidrug-resistant HIV-1. N Engl J Med. 2018;379:645-654.
37. Kozal M, Aberg J, Pialoux G, et al. Fostemsavir in adults with multidrug-resistant HIV-1 infection. N Engl J Med. 2020; 382:1232-1243.
38. Department of Health and Human Services (HHS) Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission. recommendations for use of antiretroviral drugs in pregnant HIV-1-infected women for maternal health and interventions to reduce perinatal HIV transmission in the United States. http://aidsinfo.nih.gov/guidelines/html/3/perinatal-guidelines/0/ Accessed on July 13, 2020.
39. Boyd SD, Sampson MR, Viswanathan P, et al. Cobicistat-containing antiretroviral regimens are not recommended during pregnancy: viewpoint. AIDS. 2019;33:1089-1093.
40. Garcia PM, Kalish LA, Pitt J, et al. Maternal levels of plasma human immunodeficiency virus type 1 RNA and the risk of perinatal transmission. N Engl J Med. 1999;341:394-402.
41. Stek A, Best BM, Wang J, et al. Pharmacokinetics of once versus twice daily darunavir In pregnant HIV-infected women. J Acquir Immune Defic Syndr. 2015;70:33-41.
42. Stek A, Best B, Capparelli E, et al. Pharmacokinetics of increased dose darunavir during late pregnancy and postpartum. Presented at: 23rd Conference on Retroviruses and Opportunistic Infections. 2016. Boston, MA.
43. Mirochnick M, Best BM, Stek AM, et al. Atazanavir pharmacokinetics with and without tenofovir during pregnancy. J Acquir Immune Defic Syndr. 2011;56:412-419.
44. Schalkwijk S, Colbers A, Konopnicki D, et al. Lowered rilpivirine exposure during third trimester of pregnancy in HIV-1-positive women. Clin Infect Dis. 2017;65:1335-1341.
45. Zash R, Holmes L, Diseko M, et al. Neural-tube defects and antiretroviral treatment regimens in Botswana. N Engl J Med. 2019;381:827-840.
46. Centers for Disease Control and Prevention. HIV Surveillance Report, 2017; vol. 29. www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published November 2018.
47. Rhee MS, Greenblatt DJ. Pharmacologic consideration for the use of antiretroviral agents in the elderly. J Clin Pharmacol. 2008;481212-1225.
48. Nguyen, N, Holodniy M. HIV infection in the elderly. Clin Interv Aging. 2008;3:453-472.
49. Gleason LJ, Luque AE, Shah K. Polypharmacy in the HIV-infected older adult population. Clin Interv Aging. 2013;8749-763.
50. Bastida C, Grau A, Marquez M, et al. Polypharmacy and potential drug-drug interactions in an HIV-infected elderly population. Farm Hosp. 2017;41:618-624.
51. Brown TT, Hoy J, Borderi M, et al. Recommendations for evaluation and management of bone disease in HIV. Clin Infect Dis. 2015;60:1242-1251.
52. Mocroft A, Lundgren JD, Ross M, et al. Cumulative and current exposure to potentially nephrotoxic antiretrovirals and development of chronic kidney disease in HIV-positive individuals with a normal baseline estimated glomerular filtration rate: a prospective international cohort study. Lancet HIV. 2016;3:e23-32.
53. Ryom L, Mocroft A, Kirk O, et al. D:A:D Study Group. Association between antiretroviral exposure and renal impairment among HIV-positive persons with normal baseline renal function: the D:A:D study. J Infect Dis. 2013;207:1359.
54. Wever K, van Agtmael MA, Carr A. Incomplete reversibility of tenofovir related renal toxicity in HIV-infected men. J Acquir Immune Defic Syndr. 2010;55:78-81.
55. Hall AM, Hendry BM, Nitsch D, Connolly JO. Tenofovir-associated kidney toxicity in HIV-infected patients: a review of the evidence. Am J Kidney Dis. 2011; 57:773-780.
56. Gupta SK, Post FA, Arribas JR, et al. Renal safety of tenofovir alafenamide vs. tenofovir disoproxil fumarate: a pooled analysis of 26 clinical trials. AIDS. 2019;33:1455-1465.
57. Novick TK, Choi MJ, Rosenberg AZ, et al, Tenofovir alafenamide nephrotoxicity in an HIV-positive patient: A case report. Medicine (Baltimore). 2017;96:e8046.
58. Surial B, Ledergerber B, Calmy A, et al. Swiss HIV Cohort Study, changes in renal function after switching from TDF to TAF in HIV-infected individuals: a prospective cohort study. J Infect Dis. jiaa125, https://doi.org/10.1093/infdis/jiaa125.
59. McLaughlin MM, Guerrero AJ, Merker A. Renal effects of non-tenofovir antiretroviral therapy in patients living with HIV. Drugs Context. 2018;7:212519.
60. German P, Liu H, Szwarcberg J, et al. Effect of cobicistat on glomerular filtration rate in subjects with normal and impaired renal function. J Acquir Immune Defic Syndr. 2012;61:32-40.
61. Cid-Silva P, Fernandez-Bargiela N, Margusino-Framinan L, et al. Treatment with tenofovir alafenamide fumarate worsens the lipid profile of HIV-infected patients versus treatment with tenofovir disoproxil fumarate, each coformulated with elvitegravir, cobicistat, and emtricitabine. Basic Clin Pharmacol Toxicol. 2019;124:479-490.
62. Fontas E, van Leth F, Sabin CA, et al. Lipid profiles in HIV-infected patients receiving combination antiretroviral therapy: are different antiretroviral drugs associated with different lipid profiles?. J Infect Dis. 2004;189:1056-1074.
63. Tebas P, Sension M, Arribas J, et al. Lipid levels and changes in body fat distribution in treatment-naive, HIV-1-Infected adults treated with rilpivirine or Efavirenz for 96 weeks in the ECHO and THRIVE trials. Clin Infect Dis. 2014;59:425-434.
64. Taramasso L, Tatarelli P, Ricci E, et al. Improvement of lipid profile after switching from efavirenz or ritonavir-boosted protease inhibitors to rilpivirine or once-daily integrase inhibitors: results from a large observational cohort study (SCOLTA). BMC Infect Dis. 2018;18:357.
65. Lacey A, Savinelli, S, Barco, EA, et al. The UCD ID Cohort Study; Investigating the effect of antiretroviral switch to tenofovir alafenamide on lipid profiles in people living with HIV. AIDS. 2020;341161-1170.
66. Marcus JL, Neugebauer RS, Leyden WA, et al. Use of abacavir and risk of cardiovascular disease among HIV-infected individuals. J Acquir Immune Defic Syndr. 2016;71:413-419.
67. Ribaudo HJ, Benson CA, Zheng Y, et al. No risk of myocardial infarction associated with initial antiretroviral treatment containing abacavir: short and long-term results from ACTG A5001/ALLRT. Clin Infect Dis. 2011;52:929-940.
68. Walensky RP, Sax PE, Nakamura YM, et al. Economic savings versus health losses: the cost-effectiveness of generic antiretroviral therapy in the United States. Ann Intern Med. 2013;158:84-92.
69. Jacomet C, Allavena C, Peyrol F, et al. Perception of antiretroviral generic medicines: one-day survey of HIV-infected patients and their physicians in France. PLoS One. 2015;10:e0117214-e0117214.
A 57-year-old man living with HIV has been followed at a local infectious disease clinic for more than 15 years. He acquired HIV disease through heterosexual contact. He lives alone and works at a convenience store; he has not been sexually active for the past 5 years. He smokes 10 cigarettes a day, but does not drink alcohol or use illicit drugs. He had been on coformulated emtricitabine/tenofovir disoproxil fumarate (TDF) and coformulated lopinavir/ritonavir, which he had taken conscientiously, since May 2008, without noticing any adverse reactions from this regimen. His HIV viral load had been undetectable, and his CD4 count had hovered between 600 and 700 cells/µL. Although he was on atorvastatin for dyslipidemia, his fasting lipid profile, performed in 2018, revealed a total cholesterol level of 200 mg/dL;triglyceride, 247 mg/dL; high-density lipoprotein (HDL), 43 mg/dL; and low-density lipoprotein (LDL), 132 mg/dL. In April 2019, his HIV regimen was switched to bictegravir/emtricitabine/tenofovir alafenamide (TAF). Blood tests performed in December 2019 revealed undetectable HIV viral load; an increased CD4 count to 849 cell/µL; total cholesterol, 140 mg/dL; triglyceride, 115 mg/dL; HDL, 60 mg/dL; and LDL, 90 mg/dL.
SIMPLIFYING ART
Virologically Suppressed Patients Without Drug-Resistant Virus
Treatment adherence is of paramount importance to ensure treatment success. Patients with a viral load that is undetectable or nearly undetectable without drug resistance could be taking ART regimens consisting of more than 1 pill and/or that require more than once-daily dosing. Decreasing pill burden or dosing frequency can help to improve adherence to treatment. In addition, older-generation ART agents are usually more toxic and less potent than newer-generation agents, so another important objective of switching older drugs to newer drugs is to decrease adverse reactions and improve virologic suppression. Selection of an ART regimen should be guided by the results of resistance testing (genotyping and phenotyping tests) and previous treatment history. After switching a patient’s ART regimen, plasma HIV viral load and CD4 count should be closely monitored.2 The following 3-drug, single-tablet, once-daily ART regimens can be used in patients who are virologically stable (ordered chronologically by FDA approval dates).
Efavirenz/Emtricitabine/TDF (Atripla)
Coformulated efavirenz/emtricitabine/TDF was the first single-tablet, once-daily, fixed-dose combination approved by the FDA (July 2006). Approval was based on a 48- week clinical trial involving 244 adults with HIV infection that showed that 80% of participants achieved a marked reduction in HIV viral load and a significant increase in CD4 cell count.3 Of the 3 components, efavirenz has unique central nervous system (CNS) adverse effects that could reduce adherence. Patients who were started on this fixed-dose combination commonly reported dizziness, headache, nightmare, insomnia, and impaired concentration.4 However, the CNS side effects resolved within the first 4 weeks of therapy, and less than 5% of patients quit taking the drug. Primate studies showed efavirenz is teratogenic, but studies in pregnant women did not find efavirenz to be more teratogenic than other ART agents.5
Emtricitabine/Rilpivirine/TDF (Complera)
Coformulated emtricitabine/rilpivirine/TDF was approved based on data from two 48-week, phase 3, double-blind, randomized controlled trials (ECHO and THRIVE) that evaluated the safety and efficacy of rilpivirine compared to efavirenz among treatment-naive adults with HIV infection.7,8 Rilpivirine is well tolerated and causes fewer CNS symptoms compared to efavirenz. The main caveat for rilpivirine is drug-drug interactions. It should not be coadministered with CYP inducers, such as rifampin, phenytoin, or St. John’s wort, as coadministration can cause subtherapeutic blood levels of rilpivirine. Because increased levels of rilpivirine can prolong QTc on electrocardiogram (ECG), an ECG should be obtained before starting an ART regimen that contains rilpivirine, especially in the presence of CYP 3A4 inhibitors.9
Elvitegravir/Cobicistat/Emtricitabine/TDF (Stribild)
This coformulation was approved based on data from 2 randomized, double-blind, controlled trials, Study 102 and Study 103, in treatment-naive patients with HIV (n = 1408). In Study 102, participants were randomized to receive either elvitegravir/cobicistat/emtricitabine/TDF or efavirenz/emtricitabine/TDF (Atripla).10 In Study 103, participants were randomized to receive either elvitegravir/cobicistat/emtricitabine/TDF or atazanavir + ritonavir + emtricitabine/TDF. In both studies, the primary endpoint was virologic success (HIV-1 RNA < 50 copies/mL) at 48 weeks, and elvitegravir/cobicistat/emtricitabine/TDF was noninferior compared to the other regimens.11
Abacavir/Dolutegravir/Lamivudine (Triumeq)
Approval of abacavir/dolutegravir/lamivudine (Triumeq) in August 2014 was based on SINGLE, a noninferiority trial involving 833 treatment-naive adults that compared dolutegravir and abacavir/lamivudine (the separate components of Triumeq) to efavirenz/emtricitabine/TDF. At 96 weeks, more patients in the dolutegravir and abacavir/lamivudine arm achieved an undetectable HIV viral load (80% versus 72%).13
Elvitegravir/Cobicistat/Emtricitabine/TAF (Genvoya)
Approval of coformulated elvitegravir/cobicistat/emtricitabine/TAF was supported by data from two 48-week phase 3, double-blind studies (Studies 104 and 111) involving 1733 treatment-naive patients that compared the regimen to elvitegravir/cobicistat/emtricitabine/TDF (Stribild). Both studies demonstrated that elvitegravir/cobicistat/emtricitabine/TAF was statistically noninferior, and it was favored in regard to certain renal and bone laboratory parameters.15 Studies comparing TAF and TDF have demonstrated that TAF is less likely to cause loss of bone mineral density and nephrotoxicity compared to TDF.16,17
Emtricitabine/Rilpivirine/TAF (Odefsey)
Coformulated emtricitabine/rilpivirine/TAF was approved based, in part, on positive bioequivalence studies demonstrating that it achieved similar drug levels of emtricitabine and TAF as coformulated elvitegravir/cobicistat/emtricitabine/TAF and similar drug levels of rilpivirine as individually dosed rilpivirine.18 The safety, efficacy, and tolerability of this coformulation is supported by clinical studies of rilpivirine-based therapy and emtricitabine/TAF-based therapy in a range of patients with HIV.18
Bictegravir/Emtricitabine/TAF (Biktarvy)
The coformulation bictegravir/emtricitabine/TAF was approved based on 4 phase 3 studies: Studies 1489 and 1490 in treatment-naive adults, and Studies 1844 and 1878 in virologically suppressed adults. In Study 1489, 629 treatment-naive adults were randomized 1:1 to receive coformulated bictegravir/emtricitabine/TAF or coformulated abacavir/dolutegravir/lamivudine. At week 48, similar percentages of patients in each arm achieved the primary endpoint of HIV-1 RNA < 50 copies/mL. In Study 1490, 645 treatment-naive adults were randomized 1:1 to receive coformulated bictegravir/emtricitabine/TAF or dolutegravir + emtricitabine/TAF. At week 48, similar percentages of patients in each arm achieved the primary endpoint of virologic success (HIV-1 RNA < 50 copies/mL).19,20
Darunavir/Cobicistat/Emtricitabine/TAF (Symtuza)
Approval of coformulated darunavir/cobicistat/emtricitabine/TAF was based on data from two 48-week, noninferiority, phase 3 studies that assessed the safety and efficacy of the coformulation versus a control regimen (darunavir/cobicistat plus emtricitabine/TDF) in adults with no prior ART history (AMBER) and in virologically suppressed adults (EMERALD). In the randomized, double-blind, multicenter controlled AMBER trial, at week 48, 91.4% of patients in the study group and 88.4% in the control group achieved viral suppression (HIV-1 RNA < 50 copies/mL), and virologic failure rates were low in both groups (HIV-1 RNA ≥ 50 copies/mL; 4.4% versus 3.3%, respectively).21
Doravirine/Lamivudine/TDF (Delstrigo)
Coformulated doravirine/lamivudine/TDF was approved based on data from 2 randomized, double-blind, controlled phase 3 trials, DRIVE-AHEAD and DRIVE-FORWARD. The former trial compared coformulated doravirine/lamivudine/TDF with efavirenz/emtricitabine/TDF in 728 treatment-naive patients. At 48 weeks, 84.3% in the doravirine/lamivudine/TDF arm and 80.8% in the efavirenz/emtricitabine/TDF arm met the primary endpoint of HIV-1 RNA < 50 copies/mL. Thus, doravirine/lamivudine/TDF showed sustained viral suppression and noninferiority compared to efavirenz/emtricitabine/TDF.23 The DRIVE-FORWARD trial investigated doravirine compared with ritonavir-boosted darunavir, each in combination with 2 NRTIs (TDF with emtricitabine or abacavir with lamivudine). At week 48, 84% of patients in the doravirine arm and 80% in the ritonavir-boosted darunavir arm achieved the primary endpoint of HIV-1 RNA < 50 copies/mL.24
Two-Drug, Single-Tablet, Once-Daily Regimens
Experts have long recommended that optimal treatment of HIV must consist of 3 active drugs, with trials both in the United States and Europe demonstrating decreased morbidity and mortality with 3-drug therapy.25,26 However, newer, more potent 2-drug therapy is giving more choices to people living with HIV. The single-tablet, 2-drug regimens currently available are dolutegravir/rilpivirine and dolutegravir/lamivudine. There are theoretical benefits of 2-drug therapy, such as minimizing long-term toxicities, avoidance of some drug-drug interactions, and preservation of drugs for future treatment options. At this time, a 2-drug simplification regimen can be a viable option for selected virologically stable populations.
Dolutegravir/Rilpivirine (Juluca)
Dolutegravir/rilpivirine has been shown to be noninferior to standard therapy at 48-weeks, although it is associated with a higher discontinuation rate because of side effects.27 This option can be particularly useful in patients who have contraindications to NRTIs or renal dysfunction, but it has been studied only in patients without resistance who are already virologically suppressed. Ongoing studies are looking at 2-versus 3-drug therapies for HIV treatment-experienced patients. Most of these use PIs as a backbone because of their potency and high barrier to resistance. The advent of second-generation integrase inhibitors offers additional options.
Dolutegravir/Lamivudine (Dovato)
The GEMINI-1 and GEMINI-2 trials demonstrated that dolutegravir/lamivudine was noninferior to dolutegravir/TDF/emtricitabine.28 Based on these 2 studies, new guidelines have added dolutegravir/lamivudine as a recommended first-line therapy. For now, the recommendation is to use dolutegravir/lamivudine in individuals where NRTIs are contraindicated, and it should not be used in patients with chronic hepatitis B. Additionally, 3 studies have demonstrated the safety and efficacy of switching to dolutegravir/lamivudine.29-31 In the TANGO trial, neither virologic failures nor resistant virus were identified at 48 weeks following the switch.32 Although there are benefits of simplification with this regimen, including lower toxicity, lower costs, and saving other NRTIs in case of resistance, there should be no rush to switch patients to a 2-drug regimen. This is a viable strategy in patients without baseline resistance who have preserved T-cells and do not have hepatitis B.
SWITCHING ART AGENTS IN SELECTED CLINICAL SCENARIOS
Virologic Failure
One of the main goals of ART is maximal and durable suppression of HIV viral load to prevent the development of drug-resistant mutations.2 When patients are unable to achieve durable virologic suppression or have virologic rebound, the cause of virologic failure needs to be investigated. Virologic failure is defined as the inability to achieve or maintain viral suppression to a level below 200 copies/mL, whereas rebound is defined as an HIV RNA level exceeding 200 copies/mL after virologic suppression.33 A common cause of virologic failure is patient nonadherence, which can be related to a range of factors, including psychosocial issues and affordability of medications. Innate viral resistance can be the result of transmitted drug resistance at the time of infection or be acquired during unsuppressed viral replication secondary to inherent error-prone reverse transcriptase.33 Pharmacokinetic factors that affect blood levels of ART, such as drug-drug interactions, also can be a key factor in HIV drug resistance.
Patients With Limited Treatment Options
Despite advances in ART, some patients exhaust the existing regimens, leading to development of multidrug resistance and limited treatment options. In light of the treatment challenges in this group of patients, the FDA has recently approved 2 antiretroviral agents to target multidrug-resistant HIV: ibalizumab and fostemsavir.
Pregnancy
ART is used during pregnancy to maintain the pregnant woman’s health and to prevent perinatal transmission. Pregnancy can present unique challenges to effective ART, and therapy decisions should be made based on short-term and long-term safety data, pharmacokinetics, and tolerability. With few exceptions, women who are on a stable ART regimen and present for care should continue the same regimen.38 Key exceptions, due to increased toxicity, include didanosine, indinavir, nelfinavir, stavudine, and treatment-dose ritonavir. Cobicistat-based regimens (atazanavir, darunavir, elvitegravir) have altered pharmacokinetics during the second and third trimesters of pregnancy, leading to reduced mean steady-state minimum concentrations.39 Because increasing plasma HIV RNA level is associated with transmission to infants, women continuing cobicistat-based ART treatments should undergo more frequent viral load measurements.40 If viral rebound occurs late in pregnancy, especially shortly before delivery, achieving viral suppression can be more difficult. Therefore, women on a suppressed ART regimen containing cobicistat should consider switching to a different recommended regimen.38
Geriatric Populations
Although HIV is seen predominantly in younger patients, 48% of persons living with HIV are older than 50 years and 8% are 65 years of age or older.46 With effective antiretroviral treatment, we will continue to see an aging population of people living with HIV. There are no specific guidelines regarding the treatment of older adults, but HIV treatment can have its own challenges. Physiologic declines in renal function occur with aging, which can be compounded by an increasing prevalence of diabetes and decreased muscle mass, making estimations of renal function unreliable.47 Physiologic changes with age, such as decline in renal and hepatic function, decreasing metabolism via cytochrome P450, and body composition, influence drug pharmacokinetics and can in turn potentiate drug toxicities.48 Comorbid states and polypharmacy can complicate care. The prevalence of polypharmacy in the elderly is high, 93%, and is increasing.49,50 A study found that in those aged 65 years or older with HIV, 65% had at least 1 potential drug-drug interaction, and 6.6% had a potential severe drug-drug interaction.50 These patients are thus at risk of poor drug adherence, which in HIV therapy can lead to rebound viremia and resistance.
Renal Insufficiency
Several commonly used ART agents have nephrotoxic potential. The most common manifestations of nephrotoxicity are tubular toxicity, crystal nephropathy, and interstitial nephritis. Of these, acute tubular toxicity caused by TDF is the most widely reported. About 2% of those taking TDF developed treatment-limiting renal insufficiency, manifested as Fanconi syndrome.53 Higher plasma levels of TDF are associated with increased nephrotoxicity.55 Guidelines recommend switching from TDF if the estimated glomerular filtration rate (eGFR) declines by > 25% or the eGFr is < 60/mL/min/1.73 m2. Wever et al reports that in TDF-associated nephrotoxicity, only 42% of patients reached their pre-TDF eGFR.54TAF, a prodrug of TDF, is associated with reduced levels of TDF and is hypothesized to have fewer adverse effects.55 A pooled analysis comparing renal adverse effects of TDF and TAF reported no cases of renal dysfunction in the TAF group, supporting its safety; however, acute kidney injury has also been reported with TAF.56,57 Switching from TDF to TAF in patients with renal dysfunction has been shown to lead to improvement in proteinuria, but the impact remains unclear.53
Dyslipidemia and Cardiovascular Risk
Aside from the traditional cardiovascular risks, PIs, TAF, and efavirenz can negatively affect the lipid profile, with changes in LDL and triglycerides appearing as early as 2 weeks after initiating therapy. An observational study from Spain showed that treatment with TAF worsens the lipid profile in comparison to patients treated with TDF for elvitegravir/cobicistat-based therapies; patients on TAF were twice as likely to need lipid-lower drugs in comparison to those in the TDF arm.61 Similarly, patients who changed from a TDF-based regimen to TAF for improved renal and bone safety profiles had significant changes in both total cholesterol and LDL.65Other NRTIs do not negatively affect lipid profile. Although NNRTIs can increase LDL, this is usually offset by an increase in HDL.62 Of the NNRTIs, the incidence of increased LDL is higher with efavirenz, but it also can cause an increase in HDL; in contrast, patients switched from efavirenz to rilpivirine have a better lipid profile.63,64 PIs, especially older ones such as lopinavir/ritonavir, are associated with lipid abnormalities. For patients who develop dyslipidemia as a result of using older PIs, switching to a darunavir or atazanavir regimen or even integrase inhibitors, which are considered lipid neutral, is recommended.63 When making adjustments in ART, care should be taken in prescribing abacavir to individuals with risk factors for coronary artery disease. Although there is no consensus, some randomized controlled trials suggested an association between myocardial infarction and abacavir, whereas others have not.66,67
HIV and Hepatis B Co-infection
In patients with HIV and hepatitis B co-infection, ART regimens should contain 1 drug that is active against hepatitis B (lamivudine, emtricitabine, TDF, or TAF). Clinicians should monitor liver function for hepatitis B reactivation and liver function when a regimen that contains anti-hepatitis B drugs is stopped because discontinuation of these regimens can result in acute, and sometimes fatal, liver damage.2
Financial Considerations
With out-of-pocket expenses and co-pays, some patients may have to switch ART regimens for financial reasons. Additionally, switching to generic versions of ART has been proposed as a means of saving resources for government programs already facing budgetary constraints. A study published in 2013 using generic-based ART versus branded ART showed a potential savings of almost $1 billion per year.68 A key barrier to the use of generic-based ART is patient skepticism regarding the performance of these medications. Branded ART regimens are also co-formulated, creating the perception that taking more pills will lead to noncompliance and therefore place the patient at risk of viral rebound. In a study from France, only 17% of patients were willing to switch to generic medications if doing so increased pill burden.69 In the same study, 75% physicians were generally willing to prescribe generics; however, that number dropped to 26% if the patient’s pill burden would increase.69 Paradoxically, because of the patchwork of insurance, government assistance, Medicaid, and Medicare, changing to generic-based ART may increase patients’ co-pays.
A 57-year-old man living with HIV has been followed at a local infectious disease clinic for more than 15 years. He acquired HIV disease through heterosexual contact. He lives alone and works at a convenience store; he has not been sexually active for the past 5 years. He smokes 10 cigarettes a day, but does not drink alcohol or use illicit drugs. He had been on coformulated emtricitabine/tenofovir disoproxil fumarate (TDF) and coformulated lopinavir/ritonavir, which he had taken conscientiously, since May 2008, without noticing any adverse reactions from this regimen. His HIV viral load had been undetectable, and his CD4 count had hovered between 600 and 700 cells/µL. Although he was on atorvastatin for dyslipidemia, his fasting lipid profile, performed in 2018, revealed a total cholesterol level of 200 mg/dL;triglyceride, 247 mg/dL; high-density lipoprotein (HDL), 43 mg/dL; and low-density lipoprotein (LDL), 132 mg/dL. In April 2019, his HIV regimen was switched to bictegravir/emtricitabine/tenofovir alafenamide (TAF). Blood tests performed in December 2019 revealed undetectable HIV viral load; an increased CD4 count to 849 cell/µL; total cholesterol, 140 mg/dL; triglyceride, 115 mg/dL; HDL, 60 mg/dL; and LDL, 90 mg/dL.
SIMPLIFYING ART
Virologically Suppressed Patients Without Drug-Resistant Virus
Treatment adherence is of paramount importance to ensure treatment success. Patients with a viral load that is undetectable or nearly undetectable without drug resistance could be taking ART regimens consisting of more than 1 pill and/or that require more than once-daily dosing. Decreasing pill burden or dosing frequency can help to improve adherence to treatment. In addition, older-generation ART agents are usually more toxic and less potent than newer-generation agents, so another important objective of switching older drugs to newer drugs is to decrease adverse reactions and improve virologic suppression. Selection of an ART regimen should be guided by the results of resistance testing (genotyping and phenotyping tests) and previous treatment history. After switching a patient’s ART regimen, plasma HIV viral load and CD4 count should be closely monitored.2 The following 3-drug, single-tablet, once-daily ART regimens can be used in patients who are virologically stable (ordered chronologically by FDA approval dates).
Efavirenz/Emtricitabine/TDF (Atripla)
Coformulated efavirenz/emtricitabine/TDF was the first single-tablet, once-daily, fixed-dose combination approved by the FDA (July 2006). Approval was based on a 48- week clinical trial involving 244 adults with HIV infection that showed that 80% of participants achieved a marked reduction in HIV viral load and a significant increase in CD4 cell count.3 Of the 3 components, efavirenz has unique central nervous system (CNS) adverse effects that could reduce adherence. Patients who were started on this fixed-dose combination commonly reported dizziness, headache, nightmare, insomnia, and impaired concentration.4 However, the CNS side effects resolved within the first 4 weeks of therapy, and less than 5% of patients quit taking the drug. Primate studies showed efavirenz is teratogenic, but studies in pregnant women did not find efavirenz to be more teratogenic than other ART agents.5
Emtricitabine/Rilpivirine/TDF (Complera)
Coformulated emtricitabine/rilpivirine/TDF was approved based on data from two 48-week, phase 3, double-blind, randomized controlled trials (ECHO and THRIVE) that evaluated the safety and efficacy of rilpivirine compared to efavirenz among treatment-naive adults with HIV infection.7,8 Rilpivirine is well tolerated and causes fewer CNS symptoms compared to efavirenz. The main caveat for rilpivirine is drug-drug interactions. It should not be coadministered with CYP inducers, such as rifampin, phenytoin, or St. John’s wort, as coadministration can cause subtherapeutic blood levels of rilpivirine. Because increased levels of rilpivirine can prolong QTc on electrocardiogram (ECG), an ECG should be obtained before starting an ART regimen that contains rilpivirine, especially in the presence of CYP 3A4 inhibitors.9
Elvitegravir/Cobicistat/Emtricitabine/TDF (Stribild)
This coformulation was approved based on data from 2 randomized, double-blind, controlled trials, Study 102 and Study 103, in treatment-naive patients with HIV (n = 1408). In Study 102, participants were randomized to receive either elvitegravir/cobicistat/emtricitabine/TDF or efavirenz/emtricitabine/TDF (Atripla).10 In Study 103, participants were randomized to receive either elvitegravir/cobicistat/emtricitabine/TDF or atazanavir + ritonavir + emtricitabine/TDF. In both studies, the primary endpoint was virologic success (HIV-1 RNA < 50 copies/mL) at 48 weeks, and elvitegravir/cobicistat/emtricitabine/TDF was noninferior compared to the other regimens.11
Abacavir/Dolutegravir/Lamivudine (Triumeq)
Approval of abacavir/dolutegravir/lamivudine (Triumeq) in August 2014 was based on SINGLE, a noninferiority trial involving 833 treatment-naive adults that compared dolutegravir and abacavir/lamivudine (the separate components of Triumeq) to efavirenz/emtricitabine/TDF. At 96 weeks, more patients in the dolutegravir and abacavir/lamivudine arm achieved an undetectable HIV viral load (80% versus 72%).13
Elvitegravir/Cobicistat/Emtricitabine/TAF (Genvoya)
Approval of coformulated elvitegravir/cobicistat/emtricitabine/TAF was supported by data from two 48-week phase 3, double-blind studies (Studies 104 and 111) involving 1733 treatment-naive patients that compared the regimen to elvitegravir/cobicistat/emtricitabine/TDF (Stribild). Both studies demonstrated that elvitegravir/cobicistat/emtricitabine/TAF was statistically noninferior, and it was favored in regard to certain renal and bone laboratory parameters.15 Studies comparing TAF and TDF have demonstrated that TAF is less likely to cause loss of bone mineral density and nephrotoxicity compared to TDF.16,17
Emtricitabine/Rilpivirine/TAF (Odefsey)
Coformulated emtricitabine/rilpivirine/TAF was approved based, in part, on positive bioequivalence studies demonstrating that it achieved similar drug levels of emtricitabine and TAF as coformulated elvitegravir/cobicistat/emtricitabine/TAF and similar drug levels of rilpivirine as individually dosed rilpivirine.18 The safety, efficacy, and tolerability of this coformulation is supported by clinical studies of rilpivirine-based therapy and emtricitabine/TAF-based therapy in a range of patients with HIV.18
Bictegravir/Emtricitabine/TAF (Biktarvy)
The coformulation bictegravir/emtricitabine/TAF was approved based on 4 phase 3 studies: Studies 1489 and 1490 in treatment-naive adults, and Studies 1844 and 1878 in virologically suppressed adults. In Study 1489, 629 treatment-naive adults were randomized 1:1 to receive coformulated bictegravir/emtricitabine/TAF or coformulated abacavir/dolutegravir/lamivudine. At week 48, similar percentages of patients in each arm achieved the primary endpoint of HIV-1 RNA < 50 copies/mL. In Study 1490, 645 treatment-naive adults were randomized 1:1 to receive coformulated bictegravir/emtricitabine/TAF or dolutegravir + emtricitabine/TAF. At week 48, similar percentages of patients in each arm achieved the primary endpoint of virologic success (HIV-1 RNA < 50 copies/mL).19,20
Darunavir/Cobicistat/Emtricitabine/TAF (Symtuza)
Approval of coformulated darunavir/cobicistat/emtricitabine/TAF was based on data from two 48-week, noninferiority, phase 3 studies that assessed the safety and efficacy of the coformulation versus a control regimen (darunavir/cobicistat plus emtricitabine/TDF) in adults with no prior ART history (AMBER) and in virologically suppressed adults (EMERALD). In the randomized, double-blind, multicenter controlled AMBER trial, at week 48, 91.4% of patients in the study group and 88.4% in the control group achieved viral suppression (HIV-1 RNA < 50 copies/mL), and virologic failure rates were low in both groups (HIV-1 RNA ≥ 50 copies/mL; 4.4% versus 3.3%, respectively).21
Doravirine/Lamivudine/TDF (Delstrigo)
Coformulated doravirine/lamivudine/TDF was approved based on data from 2 randomized, double-blind, controlled phase 3 trials, DRIVE-AHEAD and DRIVE-FORWARD. The former trial compared coformulated doravirine/lamivudine/TDF with efavirenz/emtricitabine/TDF in 728 treatment-naive patients. At 48 weeks, 84.3% in the doravirine/lamivudine/TDF arm and 80.8% in the efavirenz/emtricitabine/TDF arm met the primary endpoint of HIV-1 RNA < 50 copies/mL. Thus, doravirine/lamivudine/TDF showed sustained viral suppression and noninferiority compared to efavirenz/emtricitabine/TDF.23 The DRIVE-FORWARD trial investigated doravirine compared with ritonavir-boosted darunavir, each in combination with 2 NRTIs (TDF with emtricitabine or abacavir with lamivudine). At week 48, 84% of patients in the doravirine arm and 80% in the ritonavir-boosted darunavir arm achieved the primary endpoint of HIV-1 RNA < 50 copies/mL.24
Two-Drug, Single-Tablet, Once-Daily Regimens
Experts have long recommended that optimal treatment of HIV must consist of 3 active drugs, with trials both in the United States and Europe demonstrating decreased morbidity and mortality with 3-drug therapy.25,26 However, newer, more potent 2-drug therapy is giving more choices to people living with HIV. The single-tablet, 2-drug regimens currently available are dolutegravir/rilpivirine and dolutegravir/lamivudine. There are theoretical benefits of 2-drug therapy, such as minimizing long-term toxicities, avoidance of some drug-drug interactions, and preservation of drugs for future treatment options. At this time, a 2-drug simplification regimen can be a viable option for selected virologically stable populations.
Dolutegravir/Rilpivirine (Juluca)
Dolutegravir/rilpivirine has been shown to be noninferior to standard therapy at 48-weeks, although it is associated with a higher discontinuation rate because of side effects.27 This option can be particularly useful in patients who have contraindications to NRTIs or renal dysfunction, but it has been studied only in patients without resistance who are already virologically suppressed. Ongoing studies are looking at 2-versus 3-drug therapies for HIV treatment-experienced patients. Most of these use PIs as a backbone because of their potency and high barrier to resistance. The advent of second-generation integrase inhibitors offers additional options.
Dolutegravir/Lamivudine (Dovato)
The GEMINI-1 and GEMINI-2 trials demonstrated that dolutegravir/lamivudine was noninferior to dolutegravir/TDF/emtricitabine.28 Based on these 2 studies, new guidelines have added dolutegravir/lamivudine as a recommended first-line therapy. For now, the recommendation is to use dolutegravir/lamivudine in individuals where NRTIs are contraindicated, and it should not be used in patients with chronic hepatitis B. Additionally, 3 studies have demonstrated the safety and efficacy of switching to dolutegravir/lamivudine.29-31 In the TANGO trial, neither virologic failures nor resistant virus were identified at 48 weeks following the switch.32 Although there are benefits of simplification with this regimen, including lower toxicity, lower costs, and saving other NRTIs in case of resistance, there should be no rush to switch patients to a 2-drug regimen. This is a viable strategy in patients without baseline resistance who have preserved T-cells and do not have hepatitis B.
SWITCHING ART AGENTS IN SELECTED CLINICAL SCENARIOS
Virologic Failure
One of the main goals of ART is maximal and durable suppression of HIV viral load to prevent the development of drug-resistant mutations.2 When patients are unable to achieve durable virologic suppression or have virologic rebound, the cause of virologic failure needs to be investigated. Virologic failure is defined as the inability to achieve or maintain viral suppression to a level below 200 copies/mL, whereas rebound is defined as an HIV RNA level exceeding 200 copies/mL after virologic suppression.33 A common cause of virologic failure is patient nonadherence, which can be related to a range of factors, including psychosocial issues and affordability of medications. Innate viral resistance can be the result of transmitted drug resistance at the time of infection or be acquired during unsuppressed viral replication secondary to inherent error-prone reverse transcriptase.33 Pharmacokinetic factors that affect blood levels of ART, such as drug-drug interactions, also can be a key factor in HIV drug resistance.
Patients With Limited Treatment Options
Despite advances in ART, some patients exhaust the existing regimens, leading to development of multidrug resistance and limited treatment options. In light of the treatment challenges in this group of patients, the FDA has recently approved 2 antiretroviral agents to target multidrug-resistant HIV: ibalizumab and fostemsavir.
Pregnancy
ART is used during pregnancy to maintain the pregnant woman’s health and to prevent perinatal transmission. Pregnancy can present unique challenges to effective ART, and therapy decisions should be made based on short-term and long-term safety data, pharmacokinetics, and tolerability. With few exceptions, women who are on a stable ART regimen and present for care should continue the same regimen.38 Key exceptions, due to increased toxicity, include didanosine, indinavir, nelfinavir, stavudine, and treatment-dose ritonavir. Cobicistat-based regimens (atazanavir, darunavir, elvitegravir) have altered pharmacokinetics during the second and third trimesters of pregnancy, leading to reduced mean steady-state minimum concentrations.39 Because increasing plasma HIV RNA level is associated with transmission to infants, women continuing cobicistat-based ART treatments should undergo more frequent viral load measurements.40 If viral rebound occurs late in pregnancy, especially shortly before delivery, achieving viral suppression can be more difficult. Therefore, women on a suppressed ART regimen containing cobicistat should consider switching to a different recommended regimen.38
Geriatric Populations
Although HIV is seen predominantly in younger patients, 48% of persons living with HIV are older than 50 years and 8% are 65 years of age or older.46 With effective antiretroviral treatment, we will continue to see an aging population of people living with HIV. There are no specific guidelines regarding the treatment of older adults, but HIV treatment can have its own challenges. Physiologic declines in renal function occur with aging, which can be compounded by an increasing prevalence of diabetes and decreased muscle mass, making estimations of renal function unreliable.47 Physiologic changes with age, such as decline in renal and hepatic function, decreasing metabolism via cytochrome P450, and body composition, influence drug pharmacokinetics and can in turn potentiate drug toxicities.48 Comorbid states and polypharmacy can complicate care. The prevalence of polypharmacy in the elderly is high, 93%, and is increasing.49,50 A study found that in those aged 65 years or older with HIV, 65% had at least 1 potential drug-drug interaction, and 6.6% had a potential severe drug-drug interaction.50 These patients are thus at risk of poor drug adherence, which in HIV therapy can lead to rebound viremia and resistance.
Renal Insufficiency
Several commonly used ART agents have nephrotoxic potential. The most common manifestations of nephrotoxicity are tubular toxicity, crystal nephropathy, and interstitial nephritis. Of these, acute tubular toxicity caused by TDF is the most widely reported. About 2% of those taking TDF developed treatment-limiting renal insufficiency, manifested as Fanconi syndrome.53 Higher plasma levels of TDF are associated with increased nephrotoxicity.55 Guidelines recommend switching from TDF if the estimated glomerular filtration rate (eGFR) declines by > 25% or the eGFr is < 60/mL/min/1.73 m2. Wever et al reports that in TDF-associated nephrotoxicity, only 42% of patients reached their pre-TDF eGFR.54TAF, a prodrug of TDF, is associated with reduced levels of TDF and is hypothesized to have fewer adverse effects.55 A pooled analysis comparing renal adverse effects of TDF and TAF reported no cases of renal dysfunction in the TAF group, supporting its safety; however, acute kidney injury has also been reported with TAF.56,57 Switching from TDF to TAF in patients with renal dysfunction has been shown to lead to improvement in proteinuria, but the impact remains unclear.53
Dyslipidemia and Cardiovascular Risk
Aside from the traditional cardiovascular risks, PIs, TAF, and efavirenz can negatively affect the lipid profile, with changes in LDL and triglycerides appearing as early as 2 weeks after initiating therapy. An observational study from Spain showed that treatment with TAF worsens the lipid profile in comparison to patients treated with TDF for elvitegravir/cobicistat-based therapies; patients on TAF were twice as likely to need lipid-lower drugs in comparison to those in the TDF arm.61 Similarly, patients who changed from a TDF-based regimen to TAF for improved renal and bone safety profiles had significant changes in both total cholesterol and LDL.65Other NRTIs do not negatively affect lipid profile. Although NNRTIs can increase LDL, this is usually offset by an increase in HDL.62 Of the NNRTIs, the incidence of increased LDL is higher with efavirenz, but it also can cause an increase in HDL; in contrast, patients switched from efavirenz to rilpivirine have a better lipid profile.63,64 PIs, especially older ones such as lopinavir/ritonavir, are associated with lipid abnormalities. For patients who develop dyslipidemia as a result of using older PIs, switching to a darunavir or atazanavir regimen or even integrase inhibitors, which are considered lipid neutral, is recommended.63 When making adjustments in ART, care should be taken in prescribing abacavir to individuals with risk factors for coronary artery disease. Although there is no consensus, some randomized controlled trials suggested an association between myocardial infarction and abacavir, whereas others have not.66,67
HIV and Hepatis B Co-infection
In patients with HIV and hepatitis B co-infection, ART regimens should contain 1 drug that is active against hepatitis B (lamivudine, emtricitabine, TDF, or TAF). Clinicians should monitor liver function for hepatitis B reactivation and liver function when a regimen that contains anti-hepatitis B drugs is stopped because discontinuation of these regimens can result in acute, and sometimes fatal, liver damage.2
Financial Considerations
With out-of-pocket expenses and co-pays, some patients may have to switch ART regimens for financial reasons. Additionally, switching to generic versions of ART has been proposed as a means of saving resources for government programs already facing budgetary constraints. A study published in 2013 using generic-based ART versus branded ART showed a potential savings of almost $1 billion per year.68 A key barrier to the use of generic-based ART is patient skepticism regarding the performance of these medications. Branded ART regimens are also co-formulated, creating the perception that taking more pills will lead to noncompliance and therefore place the patient at risk of viral rebound. In a study from France, only 17% of patients were willing to switch to generic medications if doing so increased pill burden.69 In the same study, 75% physicians were generally willing to prescribe generics; however, that number dropped to 26% if the patient’s pill burden would increase.69 Paradoxically, because of the patchwork of insurance, government assistance, Medicaid, and Medicare, changing to generic-based ART may increase patients’ co-pays.
1. Benson CA, Gandhi RT, et al. Antiretroviral drugs for treatment and prevention of HIV infection in adults. 2018 recommendations of the International Antiviral Society-USA Panel. JAMA. 2018; 320:379-396.
2. Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents living with HIV. http://www.aidsinfo.nih.gov/ContentFiles/ AdultandAdolescentGL.pdf. Accessed July 14, 2020.
3. FDA approves the first once-a-day three-drug combination tablet for treatment of HIV-1. https://aidsinfo.nih.gov/news/769/fda-approves-the-first-once-a-day-three-drug-combination-tablet-for-treatment-of-hiv-1. Accessed July 14, 2020.
4. Apostolova N, Funes HA, Blas-Garcia A, et al. Efavirenz and the CNS: what we already know and questions that need to be answered. J Antimicrob Chemother. 2015;70:2693-2708.
5. de Béthune MP. Non-nucleoside reverse transcriptase inhibitors (NNRTIs), their discovery, development, and use in the treatment of HIV-1 infection: a review of the last 20 years (1989-2009). Antiviral Res. 2010;85:75-90.
6. Carey D, Puls R, Amin J, et al. Efficacy and safety of efanvirenz 400mg daily versus 600 mg daily: 96-week data from the randomized, double-blind, placebo-controlled, non-inferiority ENCORE1 study. Lancet Infect Dis. 2015;15:793-802.
7. Molina JM, Cahn P, Grinsztejn B, et al; ECHO study group. Rilpivirine versus efavirenz with tenofovir and emtricitabine in treatment-naive adults infected with HIV-1 (ECHO): a phase 3 randomised double-blind active-controlled trial. Lancet. 2011;378:238-246.
8. Cohen CJ, Andrade-Villanueva J, Clotet B, et al. THRIVE study group Rilpivirine versus efavirenz with two background nucleoside or nucleotide reverse transcriptase inhibitors in treatment-naive adults infected with HIV-1 (THRIVE): a phase 3, randomised, non-inferiority trial. Lancet. 2011;378:229-237.
9. James C, Preninger L, Sweet M. Rilpivirine: A second-generation nonnucleoside reverse transcriptase inhibitor. Am J Health Syst Pharm. 2012;69:857-861.
10. Zolopa A, Sax PE, DeJesus E, et al. GS-US-236-0102 Study Team A randomized double-blind comparison of coformulated elvitegravir/cobicistat/emtricitabine/tenofovir disoproxil fumarate versus efavirenz/emtricitabine/tenofovir disoproxil fumarate for initial treatment of HIV-1 infection: analysis of week 96 results. J Acquir Immune Defic Syndr. 2013;63:96-100.
11. DeJesus E, Rockstroh JK, Henry K, et al. GS-236-0103 Study Team Co-formulated elvitegravir, cobicistat, emtricitabine, and tenofovir disoproxil fumarate versus ritonavir-boosted atazanavir plus co-formulated emtricitabine and tenofovir disoproxil fumarate for initial treatment of HIV-1 infection: a randomised, double-blind, phase 3, non-inferiority trial. Lancet. 2012;379:2429-2438.
12. Sherman EM, et al. Cobicistat: review of a pharmacokinetic enhancer for HIV infection. Clin Ther. 2015;37:1876-1893.
13. Walmsley S, Baumgarten A, Berenguer J, et al. Dolutegravir plus abacavir/lamivudine for the treatment of HIV-1 infection in antiretroviral therapy-naive patients: week 96 and week 144 results from the SINGLE randomized clinical trial. J Acquir Immune Defic Syndr. 2015;70:515-519.
14. Barbarino JM, Kroetz DL, Altman RB, Klein TE. PharmGKB summary: abacavir pathway. Pharmacogenet Genomics. 2014;24:276-282.
15. Sax PE, Wohl DA, Yin MT, et al. Tenofovir alafenamide versus tenofovir disoproxil fumarate, coformulated with elvitegravir, cobicistat, and emtricitabine, for initial treatment of HIV-1 infection: two randomized, double-blind, phase 3, non-inferiority trials. Lancet. 2015;385:2606–2615.
16. DeJesus E, Haas B, Segal-Maurer S, et al. Superior efficacy and improved renal and bone safety after switching from a tenofovir disoproxil fumarate regimen to a tenofovir alafenamide-based regimen through 96 weeks of treatment. AIDS Res Hum Retroviruses. 2016;34:337-342.
17. Maggiolo F, Rizzardini G, Raff F, et al. Bone mineral density in virologically suppressed people aged 60 years or older with HIV-1 switching from a regimen containing tenofovir disoproxil fumarate to an elvitegravir, cobicistat, emtricitabine, and tenofovir alafenamide single-tablet regimen: a multicentre, open-label, phase 3b, randomised trial. Lancet HIV. 2019;6: e655-e666.
18. Ogbuagu O. Rilpivirine, emtricitabine and tenofovir alafenamide: single-tablet combination for the treatment of HIV-1 infection in selected patients. Expert Rev Anti Infect Ther. 2016;;14:1113-1126.
19. Gallant J, Lazzarin A, Mills A, et al. Bictegravir, emtricitabine, and tenofovir alafenamide versus dolutegravir, abacavir, and lamivudine for initial treatment of HIV-1 infection (GS-US-380-1489): a double-blind, multicentre, phase 3, randomised controlled non-inferiority trial. Lancet. 2017;390:2063-2072.
20. Sax PE, Pozniak A, Montes ML, et al. Coformulated bictegravir, emtricitabine, and tenofovir alafenamide versus dolutegravir with emtricitabine and tenofovir alafenamide, for the initial treatment of HIV-1 infection (GS-US-1490): a randomised, double-blind, multicenter, phase 3, non-inferiority trial. Lancet. 2017;390:2073-2082.
21. Eron JJ, Orkin C, Gallant J, et al. A week-48 randomized phase-3 trial of darunavir/cobicistat/emtricitabine/tenofovir alafenamide in treatment-naive HIV-1 patients. AIDS. 2018;32:1431-1442.
22. Orkin C, Molina JM, Negredo E, et al;. EMERALD study group. Efficacy and safety of switching from boosted protease inhibitors plus emtricitabine/tenofovir disoproxil fumarate regimens to the once-daily complete HIV-1 regimen of darunavir/cobicistat/emtricitabine/tenofovir alafenamide (D/C/F/TAF) in virologically suppressed, HIV-1-infected adults through 48 weeks (EMERALD): a phase 3, randomized, non-inferiority trial. Lancet HIV. 2018;5:e23-e34.
23. Orkin C, Squires KE, Molina JM, et al. Doravirine/lamivudine/tenofovir disoproxil fumarate is non-inferior to efavirenz/emtricitabine/tenofovir disoproxil fumarate in treatment-naive adults with human immunodeficiency virus-1 infection: week 48 results of the DRIVE-AHEAD Trial. Clin Infect Dis. 2019;68:535-544.
24. Molina JM, Squires K, Sax PE, et al. Doravirine versus ritonavir-boosted darunavir in antiretroviral-naive adults with HIV-1 (DRIVE-FORWARD): 48-week results of a randomised, double-blind, phase 3, non-inferiority trial. Lancet HIV. 2018;5:e211-e220.
25. Palella FJ, Delaney KM, Moorman ACE, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med. 1998;338:853-860.
26. Mocroft A, Vella S, Benfiedl TL. Changing patterns of mortality across Europe in patients infected with HIV-1. Lancet. 1998;3552:1725-1730.
27. Libre JM, Hugh CC, Castelli F, et al. Efficacy, safety, and tolerability of dolutegravir-rilpivirine for the maintenance of virological suppression in adults with HIV-1: phase 3, randomized, noninferiority SWORD-1 and SWORD-2 studies. Lancet. 2018;391:839-849.
28. Cahn P, Madero JS, Arribas JR, et al. Durable efficacy of dolutegravir plus lamivudine in antiretroviral treatment-naive adults with HIV-1 infection: 96-week results from the GEMINI-1 and GEMINI-2 randomized clinical trials. J Acquir Immune Defic Syndr. 2020;83:310-318.
29. Joly V, Burdet C, Landman R, et al. Dolutegravir and lamivudine maintenance therapy in HIV-1 virologically suppressed patients: results of the ANRS 167 trial (LAMIDOL). J Antimicrob Chemother. 2019;74:739-745.
30. Li JZ, Sax PE, Marconi VC, et al. No significant changes to residual viremia after switch to dolutegravir and lamivudine in a randomized trial. Open Forum Infect Dis. 2019;6:ofz056.
31. Taiwo BO, Marconi VC, Verzins B, et al. Dolutegravir plus lamivudine maintains human immunodeficiency virus-1 suppression through week 48 in a pilot randomized trial. Clin Infect Dis. 2018;66:1794-1979.
32. Van Wyk J, Ajana F, Bisshop F, et al. Efficacy and safety of switching to dolutegravir/lamivudine fixed-dose 2-drug regimen vs continuing a tenofovir alafenamide–based 3- or 4-drug regimen for maintenance of virologic suppression in adults living with human immunodeficiency virus type 1: phase 3, randomized, noninferiority TANGO Study. Clin Infect Dis. Jan 6;ciz1243. doi: 10.1093/cid/ciz1243.
33. Cutrell J, Jodlowski T, Bedimo R. The management of treatment-experienced HIV patients (including virologic failure and switches). Ther Adv Infectious Dis. 2020;7:1-15.
34. Devereux, HL, Youle, M, Johnson, MA, et al. Rapid decline in detectability of HIV-1 drug resistance mutations after stopping therapy. AIDS. 1999;13:F123-F127.
35. Gatanaga H, Tsukada K, Honda H, et al. Detection of HIV type 1 load by the Roche Cobas TaqMan assay in patients with viral loads previously undetectable by the Roche Cobas Amplicor Monitor. Clin Infect Dis. 2009;48:260-262.
36. Emu B, Fessel J, Schrader S, et al. Phase 3 study of ibalizumab for multidrug-resistant HIV-1. N Engl J Med. 2018;379:645-654.
37. Kozal M, Aberg J, Pialoux G, et al. Fostemsavir in adults with multidrug-resistant HIV-1 infection. N Engl J Med. 2020; 382:1232-1243.
38. Department of Health and Human Services (HHS) Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission. recommendations for use of antiretroviral drugs in pregnant HIV-1-infected women for maternal health and interventions to reduce perinatal HIV transmission in the United States. http://aidsinfo.nih.gov/guidelines/html/3/perinatal-guidelines/0/ Accessed on July 13, 2020.
39. Boyd SD, Sampson MR, Viswanathan P, et al. Cobicistat-containing antiretroviral regimens are not recommended during pregnancy: viewpoint. AIDS. 2019;33:1089-1093.
40. Garcia PM, Kalish LA, Pitt J, et al. Maternal levels of plasma human immunodeficiency virus type 1 RNA and the risk of perinatal transmission. N Engl J Med. 1999;341:394-402.
41. Stek A, Best BM, Wang J, et al. Pharmacokinetics of once versus twice daily darunavir In pregnant HIV-infected women. J Acquir Immune Defic Syndr. 2015;70:33-41.
42. Stek A, Best B, Capparelli E, et al. Pharmacokinetics of increased dose darunavir during late pregnancy and postpartum. Presented at: 23rd Conference on Retroviruses and Opportunistic Infections. 2016. Boston, MA.
43. Mirochnick M, Best BM, Stek AM, et al. Atazanavir pharmacokinetics with and without tenofovir during pregnancy. J Acquir Immune Defic Syndr. 2011;56:412-419.
44. Schalkwijk S, Colbers A, Konopnicki D, et al. Lowered rilpivirine exposure during third trimester of pregnancy in HIV-1-positive women. Clin Infect Dis. 2017;65:1335-1341.
45. Zash R, Holmes L, Diseko M, et al. Neural-tube defects and antiretroviral treatment regimens in Botswana. N Engl J Med. 2019;381:827-840.
46. Centers for Disease Control and Prevention. HIV Surveillance Report, 2017; vol. 29. www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published November 2018.
47. Rhee MS, Greenblatt DJ. Pharmacologic consideration for the use of antiretroviral agents in the elderly. J Clin Pharmacol. 2008;481212-1225.
48. Nguyen, N, Holodniy M. HIV infection in the elderly. Clin Interv Aging. 2008;3:453-472.
49. Gleason LJ, Luque AE, Shah K. Polypharmacy in the HIV-infected older adult population. Clin Interv Aging. 2013;8749-763.
50. Bastida C, Grau A, Marquez M, et al. Polypharmacy and potential drug-drug interactions in an HIV-infected elderly population. Farm Hosp. 2017;41:618-624.
51. Brown TT, Hoy J, Borderi M, et al. Recommendations for evaluation and management of bone disease in HIV. Clin Infect Dis. 2015;60:1242-1251.
52. Mocroft A, Lundgren JD, Ross M, et al. Cumulative and current exposure to potentially nephrotoxic antiretrovirals and development of chronic kidney disease in HIV-positive individuals with a normal baseline estimated glomerular filtration rate: a prospective international cohort study. Lancet HIV. 2016;3:e23-32.
53. Ryom L, Mocroft A, Kirk O, et al. D:A:D Study Group. Association between antiretroviral exposure and renal impairment among HIV-positive persons with normal baseline renal function: the D:A:D study. J Infect Dis. 2013;207:1359.
54. Wever K, van Agtmael MA, Carr A. Incomplete reversibility of tenofovir related renal toxicity in HIV-infected men. J Acquir Immune Defic Syndr. 2010;55:78-81.
55. Hall AM, Hendry BM, Nitsch D, Connolly JO. Tenofovir-associated kidney toxicity in HIV-infected patients: a review of the evidence. Am J Kidney Dis. 2011; 57:773-780.
56. Gupta SK, Post FA, Arribas JR, et al. Renal safety of tenofovir alafenamide vs. tenofovir disoproxil fumarate: a pooled analysis of 26 clinical trials. AIDS. 2019;33:1455-1465.
57. Novick TK, Choi MJ, Rosenberg AZ, et al, Tenofovir alafenamide nephrotoxicity in an HIV-positive patient: A case report. Medicine (Baltimore). 2017;96:e8046.
58. Surial B, Ledergerber B, Calmy A, et al. Swiss HIV Cohort Study, changes in renal function after switching from TDF to TAF in HIV-infected individuals: a prospective cohort study. J Infect Dis. jiaa125, https://doi.org/10.1093/infdis/jiaa125.
59. McLaughlin MM, Guerrero AJ, Merker A. Renal effects of non-tenofovir antiretroviral therapy in patients living with HIV. Drugs Context. 2018;7:212519.
60. German P, Liu H, Szwarcberg J, et al. Effect of cobicistat on glomerular filtration rate in subjects with normal and impaired renal function. J Acquir Immune Defic Syndr. 2012;61:32-40.
61. Cid-Silva P, Fernandez-Bargiela N, Margusino-Framinan L, et al. Treatment with tenofovir alafenamide fumarate worsens the lipid profile of HIV-infected patients versus treatment with tenofovir disoproxil fumarate, each coformulated with elvitegravir, cobicistat, and emtricitabine. Basic Clin Pharmacol Toxicol. 2019;124:479-490.
62. Fontas E, van Leth F, Sabin CA, et al. Lipid profiles in HIV-infected patients receiving combination antiretroviral therapy: are different antiretroviral drugs associated with different lipid profiles?. J Infect Dis. 2004;189:1056-1074.
63. Tebas P, Sension M, Arribas J, et al. Lipid levels and changes in body fat distribution in treatment-naive, HIV-1-Infected adults treated with rilpivirine or Efavirenz for 96 weeks in the ECHO and THRIVE trials. Clin Infect Dis. 2014;59:425-434.
64. Taramasso L, Tatarelli P, Ricci E, et al. Improvement of lipid profile after switching from efavirenz or ritonavir-boosted protease inhibitors to rilpivirine or once-daily integrase inhibitors: results from a large observational cohort study (SCOLTA). BMC Infect Dis. 2018;18:357.
65. Lacey A, Savinelli, S, Barco, EA, et al. The UCD ID Cohort Study; Investigating the effect of antiretroviral switch to tenofovir alafenamide on lipid profiles in people living with HIV. AIDS. 2020;341161-1170.
66. Marcus JL, Neugebauer RS, Leyden WA, et al. Use of abacavir and risk of cardiovascular disease among HIV-infected individuals. J Acquir Immune Defic Syndr. 2016;71:413-419.
67. Ribaudo HJ, Benson CA, Zheng Y, et al. No risk of myocardial infarction associated with initial antiretroviral treatment containing abacavir: short and long-term results from ACTG A5001/ALLRT. Clin Infect Dis. 2011;52:929-940.
68. Walensky RP, Sax PE, Nakamura YM, et al. Economic savings versus health losses: the cost-effectiveness of generic antiretroviral therapy in the United States. Ann Intern Med. 2013;158:84-92.
69. Jacomet C, Allavena C, Peyrol F, et al. Perception of antiretroviral generic medicines: one-day survey of HIV-infected patients and their physicians in France. PLoS One. 2015;10:e0117214-e0117214.
1. Benson CA, Gandhi RT, et al. Antiretroviral drugs for treatment and prevention of HIV infection in adults. 2018 recommendations of the International Antiviral Society-USA Panel. JAMA. 2018; 320:379-396.
2. Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents living with HIV. http://www.aidsinfo.nih.gov/ContentFiles/ AdultandAdolescentGL.pdf. Accessed July 14, 2020.
3. FDA approves the first once-a-day three-drug combination tablet for treatment of HIV-1. https://aidsinfo.nih.gov/news/769/fda-approves-the-first-once-a-day-three-drug-combination-tablet-for-treatment-of-hiv-1. Accessed July 14, 2020.
4. Apostolova N, Funes HA, Blas-Garcia A, et al. Efavirenz and the CNS: what we already know and questions that need to be answered. J Antimicrob Chemother. 2015;70:2693-2708.
5. de Béthune MP. Non-nucleoside reverse transcriptase inhibitors (NNRTIs), their discovery, development, and use in the treatment of HIV-1 infection: a review of the last 20 years (1989-2009). Antiviral Res. 2010;85:75-90.
6. Carey D, Puls R, Amin J, et al. Efficacy and safety of efanvirenz 400mg daily versus 600 mg daily: 96-week data from the randomized, double-blind, placebo-controlled, non-inferiority ENCORE1 study. Lancet Infect Dis. 2015;15:793-802.
7. Molina JM, Cahn P, Grinsztejn B, et al; ECHO study group. Rilpivirine versus efavirenz with tenofovir and emtricitabine in treatment-naive adults infected with HIV-1 (ECHO): a phase 3 randomised double-blind active-controlled trial. Lancet. 2011;378:238-246.
8. Cohen CJ, Andrade-Villanueva J, Clotet B, et al. THRIVE study group Rilpivirine versus efavirenz with two background nucleoside or nucleotide reverse transcriptase inhibitors in treatment-naive adults infected with HIV-1 (THRIVE): a phase 3, randomised, non-inferiority trial. Lancet. 2011;378:229-237.
9. James C, Preninger L, Sweet M. Rilpivirine: A second-generation nonnucleoside reverse transcriptase inhibitor. Am J Health Syst Pharm. 2012;69:857-861.
10. Zolopa A, Sax PE, DeJesus E, et al. GS-US-236-0102 Study Team A randomized double-blind comparison of coformulated elvitegravir/cobicistat/emtricitabine/tenofovir disoproxil fumarate versus efavirenz/emtricitabine/tenofovir disoproxil fumarate for initial treatment of HIV-1 infection: analysis of week 96 results. J Acquir Immune Defic Syndr. 2013;63:96-100.
11. DeJesus E, Rockstroh JK, Henry K, et al. GS-236-0103 Study Team Co-formulated elvitegravir, cobicistat, emtricitabine, and tenofovir disoproxil fumarate versus ritonavir-boosted atazanavir plus co-formulated emtricitabine and tenofovir disoproxil fumarate for initial treatment of HIV-1 infection: a randomised, double-blind, phase 3, non-inferiority trial. Lancet. 2012;379:2429-2438.
12. Sherman EM, et al. Cobicistat: review of a pharmacokinetic enhancer for HIV infection. Clin Ther. 2015;37:1876-1893.
13. Walmsley S, Baumgarten A, Berenguer J, et al. Dolutegravir plus abacavir/lamivudine for the treatment of HIV-1 infection in antiretroviral therapy-naive patients: week 96 and week 144 results from the SINGLE randomized clinical trial. J Acquir Immune Defic Syndr. 2015;70:515-519.
14. Barbarino JM, Kroetz DL, Altman RB, Klein TE. PharmGKB summary: abacavir pathway. Pharmacogenet Genomics. 2014;24:276-282.
15. Sax PE, Wohl DA, Yin MT, et al. Tenofovir alafenamide versus tenofovir disoproxil fumarate, coformulated with elvitegravir, cobicistat, and emtricitabine, for initial treatment of HIV-1 infection: two randomized, double-blind, phase 3, non-inferiority trials. Lancet. 2015;385:2606–2615.
16. DeJesus E, Haas B, Segal-Maurer S, et al. Superior efficacy and improved renal and bone safety after switching from a tenofovir disoproxil fumarate regimen to a tenofovir alafenamide-based regimen through 96 weeks of treatment. AIDS Res Hum Retroviruses. 2016;34:337-342.
17. Maggiolo F, Rizzardini G, Raff F, et al. Bone mineral density in virologically suppressed people aged 60 years or older with HIV-1 switching from a regimen containing tenofovir disoproxil fumarate to an elvitegravir, cobicistat, emtricitabine, and tenofovir alafenamide single-tablet regimen: a multicentre, open-label, phase 3b, randomised trial. Lancet HIV. 2019;6: e655-e666.
18. Ogbuagu O. Rilpivirine, emtricitabine and tenofovir alafenamide: single-tablet combination for the treatment of HIV-1 infection in selected patients. Expert Rev Anti Infect Ther. 2016;;14:1113-1126.
19. Gallant J, Lazzarin A, Mills A, et al. Bictegravir, emtricitabine, and tenofovir alafenamide versus dolutegravir, abacavir, and lamivudine for initial treatment of HIV-1 infection (GS-US-380-1489): a double-blind, multicentre, phase 3, randomised controlled non-inferiority trial. Lancet. 2017;390:2063-2072.
20. Sax PE, Pozniak A, Montes ML, et al. Coformulated bictegravir, emtricitabine, and tenofovir alafenamide versus dolutegravir with emtricitabine and tenofovir alafenamide, for the initial treatment of HIV-1 infection (GS-US-1490): a randomised, double-blind, multicenter, phase 3, non-inferiority trial. Lancet. 2017;390:2073-2082.
21. Eron JJ, Orkin C, Gallant J, et al. A week-48 randomized phase-3 trial of darunavir/cobicistat/emtricitabine/tenofovir alafenamide in treatment-naive HIV-1 patients. AIDS. 2018;32:1431-1442.
22. Orkin C, Molina JM, Negredo E, et al;. EMERALD study group. Efficacy and safety of switching from boosted protease inhibitors plus emtricitabine/tenofovir disoproxil fumarate regimens to the once-daily complete HIV-1 regimen of darunavir/cobicistat/emtricitabine/tenofovir alafenamide (D/C/F/TAF) in virologically suppressed, HIV-1-infected adults through 48 weeks (EMERALD): a phase 3, randomized, non-inferiority trial. Lancet HIV. 2018;5:e23-e34.
23. Orkin C, Squires KE, Molina JM, et al. Doravirine/lamivudine/tenofovir disoproxil fumarate is non-inferior to efavirenz/emtricitabine/tenofovir disoproxil fumarate in treatment-naive adults with human immunodeficiency virus-1 infection: week 48 results of the DRIVE-AHEAD Trial. Clin Infect Dis. 2019;68:535-544.
24. Molina JM, Squires K, Sax PE, et al. Doravirine versus ritonavir-boosted darunavir in antiretroviral-naive adults with HIV-1 (DRIVE-FORWARD): 48-week results of a randomised, double-blind, phase 3, non-inferiority trial. Lancet HIV. 2018;5:e211-e220.
25. Palella FJ, Delaney KM, Moorman ACE, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med. 1998;338:853-860.
26. Mocroft A, Vella S, Benfiedl TL. Changing patterns of mortality across Europe in patients infected with HIV-1. Lancet. 1998;3552:1725-1730.
27. Libre JM, Hugh CC, Castelli F, et al. Efficacy, safety, and tolerability of dolutegravir-rilpivirine for the maintenance of virological suppression in adults with HIV-1: phase 3, randomized, noninferiority SWORD-1 and SWORD-2 studies. Lancet. 2018;391:839-849.
28. Cahn P, Madero JS, Arribas JR, et al. Durable efficacy of dolutegravir plus lamivudine in antiretroviral treatment-naive adults with HIV-1 infection: 96-week results from the GEMINI-1 and GEMINI-2 randomized clinical trials. J Acquir Immune Defic Syndr. 2020;83:310-318.
29. Joly V, Burdet C, Landman R, et al. Dolutegravir and lamivudine maintenance therapy in HIV-1 virologically suppressed patients: results of the ANRS 167 trial (LAMIDOL). J Antimicrob Chemother. 2019;74:739-745.
30. Li JZ, Sax PE, Marconi VC, et al. No significant changes to residual viremia after switch to dolutegravir and lamivudine in a randomized trial. Open Forum Infect Dis. 2019;6:ofz056.
31. Taiwo BO, Marconi VC, Verzins B, et al. Dolutegravir plus lamivudine maintains human immunodeficiency virus-1 suppression through week 48 in a pilot randomized trial. Clin Infect Dis. 2018;66:1794-1979.
32. Van Wyk J, Ajana F, Bisshop F, et al. Efficacy and safety of switching to dolutegravir/lamivudine fixed-dose 2-drug regimen vs continuing a tenofovir alafenamide–based 3- or 4-drug regimen for maintenance of virologic suppression in adults living with human immunodeficiency virus type 1: phase 3, randomized, noninferiority TANGO Study. Clin Infect Dis. Jan 6;ciz1243. doi: 10.1093/cid/ciz1243.
33. Cutrell J, Jodlowski T, Bedimo R. The management of treatment-experienced HIV patients (including virologic failure and switches). Ther Adv Infectious Dis. 2020;7:1-15.
34. Devereux, HL, Youle, M, Johnson, MA, et al. Rapid decline in detectability of HIV-1 drug resistance mutations after stopping therapy. AIDS. 1999;13:F123-F127.
35. Gatanaga H, Tsukada K, Honda H, et al. Detection of HIV type 1 load by the Roche Cobas TaqMan assay in patients with viral loads previously undetectable by the Roche Cobas Amplicor Monitor. Clin Infect Dis. 2009;48:260-262.
36. Emu B, Fessel J, Schrader S, et al. Phase 3 study of ibalizumab for multidrug-resistant HIV-1. N Engl J Med. 2018;379:645-654.
37. Kozal M, Aberg J, Pialoux G, et al. Fostemsavir in adults with multidrug-resistant HIV-1 infection. N Engl J Med. 2020; 382:1232-1243.
38. Department of Health and Human Services (HHS) Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission. recommendations for use of antiretroviral drugs in pregnant HIV-1-infected women for maternal health and interventions to reduce perinatal HIV transmission in the United States. http://aidsinfo.nih.gov/guidelines/html/3/perinatal-guidelines/0/ Accessed on July 13, 2020.
39. Boyd SD, Sampson MR, Viswanathan P, et al. Cobicistat-containing antiretroviral regimens are not recommended during pregnancy: viewpoint. AIDS. 2019;33:1089-1093.
40. Garcia PM, Kalish LA, Pitt J, et al. Maternal levels of plasma human immunodeficiency virus type 1 RNA and the risk of perinatal transmission. N Engl J Med. 1999;341:394-402.
41. Stek A, Best BM, Wang J, et al. Pharmacokinetics of once versus twice daily darunavir In pregnant HIV-infected women. J Acquir Immune Defic Syndr. 2015;70:33-41.
42. Stek A, Best B, Capparelli E, et al. Pharmacokinetics of increased dose darunavir during late pregnancy and postpartum. Presented at: 23rd Conference on Retroviruses and Opportunistic Infections. 2016. Boston, MA.
43. Mirochnick M, Best BM, Stek AM, et al. Atazanavir pharmacokinetics with and without tenofovir during pregnancy. J Acquir Immune Defic Syndr. 2011;56:412-419.
44. Schalkwijk S, Colbers A, Konopnicki D, et al. Lowered rilpivirine exposure during third trimester of pregnancy in HIV-1-positive women. Clin Infect Dis. 2017;65:1335-1341.
45. Zash R, Holmes L, Diseko M, et al. Neural-tube defects and antiretroviral treatment regimens in Botswana. N Engl J Med. 2019;381:827-840.
46. Centers for Disease Control and Prevention. HIV Surveillance Report, 2017; vol. 29. www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published November 2018.
47. Rhee MS, Greenblatt DJ. Pharmacologic consideration for the use of antiretroviral agents in the elderly. J Clin Pharmacol. 2008;481212-1225.
48. Nguyen, N, Holodniy M. HIV infection in the elderly. Clin Interv Aging. 2008;3:453-472.
49. Gleason LJ, Luque AE, Shah K. Polypharmacy in the HIV-infected older adult population. Clin Interv Aging. 2013;8749-763.
50. Bastida C, Grau A, Marquez M, et al. Polypharmacy and potential drug-drug interactions in an HIV-infected elderly population. Farm Hosp. 2017;41:618-624.
51. Brown TT, Hoy J, Borderi M, et al. Recommendations for evaluation and management of bone disease in HIV. Clin Infect Dis. 2015;60:1242-1251.
52. Mocroft A, Lundgren JD, Ross M, et al. Cumulative and current exposure to potentially nephrotoxic antiretrovirals and development of chronic kidney disease in HIV-positive individuals with a normal baseline estimated glomerular filtration rate: a prospective international cohort study. Lancet HIV. 2016;3:e23-32.
53. Ryom L, Mocroft A, Kirk O, et al. D:A:D Study Group. Association between antiretroviral exposure and renal impairment among HIV-positive persons with normal baseline renal function: the D:A:D study. J Infect Dis. 2013;207:1359.
54. Wever K, van Agtmael MA, Carr A. Incomplete reversibility of tenofovir related renal toxicity in HIV-infected men. J Acquir Immune Defic Syndr. 2010;55:78-81.
55. Hall AM, Hendry BM, Nitsch D, Connolly JO. Tenofovir-associated kidney toxicity in HIV-infected patients: a review of the evidence. Am J Kidney Dis. 2011; 57:773-780.
56. Gupta SK, Post FA, Arribas JR, et al. Renal safety of tenofovir alafenamide vs. tenofovir disoproxil fumarate: a pooled analysis of 26 clinical trials. AIDS. 2019;33:1455-1465.
57. Novick TK, Choi MJ, Rosenberg AZ, et al, Tenofovir alafenamide nephrotoxicity in an HIV-positive patient: A case report. Medicine (Baltimore). 2017;96:e8046.
58. Surial B, Ledergerber B, Calmy A, et al. Swiss HIV Cohort Study, changes in renal function after switching from TDF to TAF in HIV-infected individuals: a prospective cohort study. J Infect Dis. jiaa125, https://doi.org/10.1093/infdis/jiaa125.
59. McLaughlin MM, Guerrero AJ, Merker A. Renal effects of non-tenofovir antiretroviral therapy in patients living with HIV. Drugs Context. 2018;7:212519.
60. German P, Liu H, Szwarcberg J, et al. Effect of cobicistat on glomerular filtration rate in subjects with normal and impaired renal function. J Acquir Immune Defic Syndr. 2012;61:32-40.
61. Cid-Silva P, Fernandez-Bargiela N, Margusino-Framinan L, et al. Treatment with tenofovir alafenamide fumarate worsens the lipid profile of HIV-infected patients versus treatment with tenofovir disoproxil fumarate, each coformulated with elvitegravir, cobicistat, and emtricitabine. Basic Clin Pharmacol Toxicol. 2019;124:479-490.
62. Fontas E, van Leth F, Sabin CA, et al. Lipid profiles in HIV-infected patients receiving combination antiretroviral therapy: are different antiretroviral drugs associated with different lipid profiles?. J Infect Dis. 2004;189:1056-1074.
63. Tebas P, Sension M, Arribas J, et al. Lipid levels and changes in body fat distribution in treatment-naive, HIV-1-Infected adults treated with rilpivirine or Efavirenz for 96 weeks in the ECHO and THRIVE trials. Clin Infect Dis. 2014;59:425-434.
64. Taramasso L, Tatarelli P, Ricci E, et al. Improvement of lipid profile after switching from efavirenz or ritonavir-boosted protease inhibitors to rilpivirine or once-daily integrase inhibitors: results from a large observational cohort study (SCOLTA). BMC Infect Dis. 2018;18:357.
65. Lacey A, Savinelli, S, Barco, EA, et al. The UCD ID Cohort Study; Investigating the effect of antiretroviral switch to tenofovir alafenamide on lipid profiles in people living with HIV. AIDS. 2020;341161-1170.
66. Marcus JL, Neugebauer RS, Leyden WA, et al. Use of abacavir and risk of cardiovascular disease among HIV-infected individuals. J Acquir Immune Defic Syndr. 2016;71:413-419.
67. Ribaudo HJ, Benson CA, Zheng Y, et al. No risk of myocardial infarction associated with initial antiretroviral treatment containing abacavir: short and long-term results from ACTG A5001/ALLRT. Clin Infect Dis. 2011;52:929-940.
68. Walensky RP, Sax PE, Nakamura YM, et al. Economic savings versus health losses: the cost-effectiveness of generic antiretroviral therapy in the United States. Ann Intern Med. 2013;158:84-92.
69. Jacomet C, Allavena C, Peyrol F, et al. Perception of antiretroviral generic medicines: one-day survey of HIV-infected patients and their physicians in France. PLoS One. 2015;10:e0117214-e0117214.
Weight gain persists as HIV-treatment issue
People living with HIV who put on extra pounds and develop metabolic syndrome or related disorders linked in part to certain antiretroviral agents remain a concern today, even as the drugs used to suppress HIV infection have evolved over the decades.
Linkage of HIV treatment with lipodystrophy and insulin resistance or diabetes began in the 1990s with protease inhibitors (Clin Infect Dis. 2000 Jun;30[suppl 2]:s135-42). Several reports over the years also tied any form of effective antiretroviral therapy to weight gain in HIV patients (Antivir Ther. 2012;17[7]:1281-9). More recently, reports have rattled the HIV-treatment community by associating alarmingly high levels of weight gain with a useful and relatively new drug, tenofovir alafenamide fumarate (TAF) – a nucleoside reverse transcriptase inhibitor (NRTI) approved for use in the United States in late 2016, as well as certain agents from an entirely different antiretroviral therapy (ART) class, the integrase strand transfer inhibitors (INSTIs). Both TAF and the INSTIs have come to play major roles in the HIV-treatment landscape, despite relevant and concerning recent weight gain observations with these drugs, such as in a 2019 meta-analysis of eight trials with 5,680 treatment-naive patients who started ART during 2003-2015 (Clin Infect Dis. 2019 Oct 14;doi: 10.1093/cid/ciz999).
“Weight gain is clearly seen in studies of dolutegravir [DTG] or bictegravir [BTG] with TAF,” wrote W.D. Francois Venter, PhD and Andrew Hill, PhD in a recent published commentary on the topic (Lancet HIV. 2020 Jun 1;7[6]:e389-400). Both DTG and BTG are INSTI class members.
“Excessive weight gain, defined as more than 10% over baseline, has recently been observed among people with HIV initiating or switching to regimens incorporating TAF, an INSTI, or both, particularly DTG,” wrote Jordan E. Lake, MD, an HIV specialist at the University of Texas Health Science Center at Houston, in a recent commentary posted online. Women and Black patients “are at even greater risk for excessive weight gain,” Dr. Lake added.
“In recent times, it has emerged that weight gain is more pronounced with the integrase inhibitor class of agents, especially dolutegravir and bictegravir, the so-called second-generation” INSTIs, said Anna Maria Geretti, MD, a professor of clinical infection, microbiology, and immunology at the University of Liverpool, England. ”The effect is more pronounced in women and people of non-White ethnicity, and is of concern because of the associated potential risk of metabolic syndrome, cardiovascular disease, etc.,” Dr. Geretti said in an interview.
The unprecedented susceptibility to weight gain seen recently in non-White women may in part have resulted from the tendency of many earlier treatment trials to have cohorts comprised predominantly of White men, Dr. Venter noted in an interview.
Alarming weight gains reported
Perhaps the most eye-popping example of the potential for weight gain with the combination of TAF with an INSTI came in a recent report from the ADVANCE trial, a randomized, head-to-head comparison of three regimens in 1,053 HIV patients in South Africa. After 144 weeks on a regimen of TAF (Vemlidy), DTG (Tivicay), and FTC (emtricitabine, Emtriva), another NRTI, women gained an averaged of more than 12 kg, compared with their baseline weight, significantly more than in two comparator groups, Simiso Sokhela, MB, reported at the virtual meeting of the International AIDS conference. The women in ADVANCE on the TAF-DTG-FTC regimen also had an 11% rate of incident metabolic syndrome during their first 96 weeks on treatment, compared with rates of 8% among patients on a different form of tenofovir, tenofovir disoproxil fumarate (TDF), along with DTG-FTC, and 5% among those on TDF–EFV (efavirenz, Sustiva)–FTC said Dr. Sokhela, an HIV researcher at Ezintsha, a division of the University of the Witwatersrand in Johannesburg, South Africa.
“We believe that these results support the World Health Organization guidelines that reserve TAF for only patients with osteoporosis or impaired renal function,” Dr. Sokhela said during a press briefing at the conference. The WHO guidelines list the first-line regimen as TDF-DTG-3TC (lamivudine; Epivir) or FTC. “The risk for becoming obese continued to increase after 96 weeks” of chronic use of these drugs, she added.
“All regimens are now brilliant at viral control. Finding the ones that don’t make patients obese or have other long-term side effects is now the priority,” noted Dr. Venter, a professor and HIV researcher at University of the Witwatersrand, head of Ezintsha, and lead investigator of ADVANCE. Clinicians and researchers have recently thought that combining TAF and an INSTI plus FTC or a similar NRTI “would be the ultimate regimen to replace the nonnucleoside reverse transcriptase inhibitors (NNRTIs)” such as EFV, “but now we have a major headache” with unexpectedly high weight gains in some patients, Dr. Venter said.
Weight gains “over 10 kg are unlikely to be acceptable in any circumstances, especially when starting body mass index is already borderline overweight,” wrote Dr. Venter along with Dr. Hill in their commentary. Until recently, many clinicians chalked up weight gain on newly begun ART as a manifestation of the patient’s “return-to-health,” but this interpretation “gives a positive spin to a potentially serious and common side effect,” they added.
More from ADVANCE
The primary efficacy endpoint of ADVANCE was suppression of viral load to less than 50 RNA copies/mL after 48 weeks on treatment, and the result showed that the TAF-DTG-FTC regimen and the TDF-DTG-FTC regimen were each noninferior to the control regimen of TDF-EFV-FTC (New Engl J Med. 2019 Aug 29;381[9]:803-15). Virtually all of the enrolled patients were Black, and 59% were women. Planned follow-up of all patients ran for 96 weeks. After 48 weeks, weight gain among the women averaged 6.4 kg, 3.2 kg, and 1.7 kg in the TAF-DTG, TDF-DTG, and TDF-EFV arms respectively. After 96 weeks, the average weight gains among women were 8.2 kg, 4.6 kg, and 3.2 kg, respectively, in new results reported by Dr. Sokhela at the IAC. Follow-up to 144 weeks was partial and included about a quarter of the enrolled women, with gains averaging 12.3 kg, 7.4 kg, and 5.5 kg respectively. The pattern of weight gain among men tracked the pattern in women, but the magnitude of gain was less. Among men followed for 144 weeks, average gain among those on TAF-DTG-FTC was 7.2 kg, the largest gain seen among men on any regimen and at any follow-up time in the study.
Dr. Sokhela also reported data on body composition analyses, which showed that the weight gains were largely in fat rather than lean tissue, fat accumulation was significantly greater in women than men, and that in both sexes fat accumulated roughly equally in the trunk and on limbs.
An additional analysis looked at the incidence of new-onset obesity among the women who had a normal body mass index at baseline. After 96 weeks, incident obesity occurred in 14% of women on the TAG-DTG-FTC regimen, 8% on TDF-DTG-FTC, and in 2% of women maintained on TDF-EFV-FTC, said Dr. Hill in a separate report at the conference.
Weight starts to weigh in
“I am very mindful of weight gain potential, and I talk to patients about it. It doesn’t determine what regimen I choose for a patient” right now, “but it’s only a matter of time before it starts influencing what we do, particularly if we can achieve efficacy with fewer drugs,” commented Babafemi O. Taiwo, MD, professor of medicine and chief of infectious diseases at Northwestern University in Chicago. “I’ve had some patients show up with a weight gain of 20 kg, and that shouldn’t happen,” he said during a recent online educational session. Dr. Taiwo said his recent practice has been to warn patients about possible weight gain and to urge them to get back in touch with him quickly if it happens.
“Virologic suppression is the most important goal with ART, and the U.S. Department of Health and Human Services currently recommends INSTI-based ART for most PWH [people with HIV],” wrote Dr. Lake in April 2020. “I counsel all PWH initiating ART about the potential for weight gain, and I discuss their current diet and healthy lifestyle habits. I explain to patients that we will monitor their weight, and if weight gain seems more than either of us are comfortable with then we will reassess. Only a small percentage of patients experience excessive weight gain after starting ART.” Dr. Lake also stressed that she had not yet begun to change the regimen a patient is on solely because of weight gain. “We do not know whether this weight gain is reversible,” she noted.
“I do not anticipate that a risk of weight gain at present will dictate a change in guidelines,” said Dr. Geretti. “Drugs such as dolutegravir and bictegravir are very effective, and they are unlikely to cause drug resistance. Further data on the mechanism of weight gain and the reversibility after a change of treatment will help refine drug selection in the near future,” she predicted.
“I consider weight gain when prescribing because my patients hear about this. It’s a side effect that my patients really care about, and I don’t blame them,” said Lisa Hightow-Weidman, MD, a professor and HIV specialist at the University of North Carolina at Chapel Hill, during an on-line educational session. “If you don’t discuss it with a patient and then weight gain happens and the patient finds out [the known risk from their treatment] they may have an issue,” she noted. But weight gain is not a reason to avoid these drugs. “They are great medications in many ways, with once-daily regimens and few side effects.”
Weight gain during pregnancy a special concern
An additional analysis of data from ADVANCE presented at the conference highlighted what the observed weight gain on ART could mean for women who become pregnant while on treatment. Based on a systematic literature review, the ADVANCE investigators calculated the relative risk for six obesity-related pregnancy complications, compared with nonobese women: preterm delivery, gestational diabetes, gestational hypertension, preeclampsia, postpartum hemorrhage, and caesarean delivery. Based on the obesity changes among women on their assigned ART in ADVANCE, the researchers calculated the predicted incidence of these six complications. The analysis showed that for every 1,000 women, those on TAG-DTG-FTC would have an excess of 53 obesity-related pregnancy complications, those on TDF-DTG-FTC would develop 28 excess pregnancy complications, and those on TDG-EFV-FTC would have four excess complications, reported Dr. Hill at the International AIDS conference.
The researchers also ran a similar simulation for the incidence of neonatal complications that could result when mothers are obese because of their ART. The six neonatal complications included in this analysis were small for gestational age, large for gestational age, macrosomia, neonatal death, stillbirth, and neural tube defects. Based on the excess rate of incident obesity, they calculated that for every 1,000 pregnancies women on TAD-DTG-FTC would have 24 additional infants born with one of these complications, women on TDF-DTG-FTC would have an excess of 13 of these events, and women on TDG-EFV-FTC would have an excess of three such obesity-related neonatal complications, Dr. Hill said.
Sorting out the drugs
Results from several additional studies reported at the conference have started trying to discern exactly which ART drugs and regimens pose the greatest weight gain risk and which have the least risk while retaining high efficacy and resistance barriers.
Further evidence implicating any type of ART as a driver of increased weight came from a review of 8,256 adults infected with HIV and members of the Kaiser Permanente health system in three U.S. regions during 2000-2016. Researchers matched these cases using several demographic factors with just under 130,000 members without HIV. Those infected by HIV had half the prevalence of obesity as the matched controls at baseline. During 12 years of follow-up, those infected with HIV had a threefold higher rate of weight gain than those who were uninfected. Annual weight gain averaged 0.06 kg/year among the uninfected people and 0.22 kg/year among those infected with HIV, a statistically significant difference that was consistent regardless of whether people started the study at a normal body mass index, overweight, or obese, reported Michael J. Silverberg, PhD, an epidemiologist with Kaiser Permanente in Oakland, Calif.
Another study tried to focus on the weight gain impact when patients on three-drug ART regimens changed from taking TDF to TAF. This analysis used data collected in the OPERA (Observational Pharmaco-Epidemiology Research & Analysis) longitudinal cohort of about 115,000 U.S. PWH. The observational cohort included nearly 7,000 patients who made a TDF-to-TAF switch, including 3,288 patients who maintained treatment during this switch with an INSTI, 1,454 who maintained a background regimen based on a NNRTI, 1,430 patients who also switched from an INSTI to a different drug, and 747 patients maintained on a boosted dose of a protease inhibitor. All patients were well controlled on their baseline regimen, with at least two consecutive measures showing undetectable viral load.
Patients who maintained their background regimens while changing from TDF to TAF had a 2.0-2.6 kg increase in weight during the 9 months immediately following their switch to TAF, reported Patrick Mallon, MB, a professor of microbial diseases at University College Dublin. Among the patients who both switched to TAF and also switched to treatment with an INSTI, weight gain during the 9 months after the switch averaged 2.6-4.5 kg, depending on which INSTI was started. Patients who switched to treatment with elvitegravir/cobicistat (an INSTI plus a boosting agent) averaged a gain of 2.6 kg during 9 months, those who switched to DTG averaged a 3.1-kg gain, and those who switched to BTG averaged a 4.6-kg increase, Dr. Mallon reported at the conference.
These findings “give us a good sense that the weight gain is real. This is not just overeating or not exercising, but weight changes coincidental with a change in HIV treatment,” commented David Wohl, MD, professor of medicine and site leader of the HIV Prevention and Treatment Clinical Trials Unit at the University of North Carolina at Chapel Hill, during an online educational session.
Contrary to this evidence suggesting a consistent uptick in weight when patients start TAF treatment was a recent report on 629 HIV patients randomized to treatment with TAF-BTG-FTC or abacavir (an NRTI, Ziagen)–DTG-3TC, which found similar weight gains between these two regimens after 144 weeks on treatment (Lancet HIV. 2020 Jun;7[6]:e389-400). This finding had the effect of “strengthening the argument that TAF is simply an innocent bystander” and does not play a central role in weight gain, and supporting the notion that the alternative tenofovir formulation, TDF, differs from TAF by promoting weight loss, Dr. Venter and Dr. Hill suggested in their commentary that accompanied this report.
The new findings from Dr. Mallon raise “serious questions about the way we have moved to TAF as a replacement for TDF, especially because the benefits [from TAF] are for a small subgroup – patients with renal disease or osteoporosis,” Dr. Venter said in an interview. “The question is, will we see weight gain like this” if TAF was combined with a non-INSTI drug? he wondered.
While some study results have suggested a mitigating effect from TDF on weight gain, that wasn’t the case in the AFRICOS (African Cohort Study) study of 1,954 PWH who started treatment with TDF-DTG-FTC (742 patients) or a different three-drug regimen. After a median of 225 days on treatment, those who started on TDF-DTG-FTC had an adjusted, 85% higher rate of developing a high body mass index, compared with patients on a different ART regimen, Julie Ake, MD, reported in a talk at the conference. Her conclusion focused on the possible involvement of DTG: “Consistent with previous reports, dolutegravir was significantly associated with an increased risk of developing high body mass index,” said Dr. Ake, director of the U.S. Military HIV Research Program in Bethesda, Md. and leader of AFRICOS.
A potential workaround to some drugs that cause excessive the weight gain is to just not use them. That was part of the rationale for the TANGO study, which took 741 HIV-infected patients with successful viral suppression on a regimen of TAF-FTC plus one or two additional agents and switched half of them to a TAF-less, two-drug regimen of DTG-FTC. This open-label study’s primary endpoint was noninferiority for viral suppression of the DTG-FTC regimen, compared with patients who stayed on their starting regimen, and the results proved that DTG-FTC was just as effective over 48 weeks for this outcome (Clin Infect Dis. 2020 Jan 6. doi: 10.1093/cid/ciz1243).
At the conference, TANGO’s lead investigator, Jean van Wyk, MD, reported the weight and metabolic effects of the switch. The results showed a similar and small weight gain (on average less than 1 kg) during 48 week follow-up regardless of whether patients remained on their baseline, TAF-containing regimen or switched to DTG-FTC, said Dr. van Wyk, global medical lead for HIV treatment at Viiv Healthcare, the company that markets DTG. About three-quarters of patients in both arms received “boosted” dosages of their drugs, and in this subgroup, patients on DTG-FTC showed statistically significant benefits in several lipid levels, fasting glucose level, and in their degree of insulin resistance. Dr. van Wyk said. These between-group differences were not statistically significant among the “unboosted” patients, and the results failed to show a significant between-group difference in the incidence of metabolic syndrome.
Dr. Venter called these results “exciting,” and noted that he already uses the DTG-FTC two-drug combination “a lot” to treat PWH and renal disease.
A second alternative regimen showcased in a talk at the conference used the three-drug regimen of TDF-FTC plus the NNRTI, DOR (doravirine, Pifeltro). The DRIVE-SHIFT trial enrolled 670 HIV patients with successfully suppressed viral load on conventional regimens who were either switched to TDF-DOR-FTC or maintained on their baseline treatment. After 48 weeks, results confirmed the primary efficacy endpoint of noninferiority for maintenance of suppression with the investigational regimen (J Acquir Immune Defic Syndr. 2019 Aug;81[4]:463-72).
A post-hoc analysis looked at weight changes among these patients after as much as 144 weeks of follow-up. The results showed that patients switched to TDF-DOR-FTC had an average weight increase of 1.2-1.4 kg after more than 2 years on the new regimen, with fewer than 10% of patients having a 10% or greater weight gain with DOR, a “next-generation” NNRTI, reported Princy N. Kumar, MD, professor at Georgetown University and chief of infectious diseases at MedStar Georgetown University Hospital in Washington. “Weight gain was minimal, even over the long term,” she noted.
The tested DOR-based regimen also looks “very exciting,” but the populations it’s been tested have also been largely limited to White men, and limited data exist about the regimen’s performance in pregnant women, commented Dr. Venter. The DRIVE-SHIRT patient cohort was about 85% men, and about three-quarters White.
More weight data needed
HIV-treatment researchers and clinicians seem agreed that weight gain and other metabolic effects from HIV treatment need more assessment and evidence because current data, while suggestive, is also inconclusive.
“Clinical trials are desperately needed to understand the mechanisms of and potential therapeutic options for excessive weight gain on ART,” wrote Dr. Lake in her commentary in April. “While more research is needed,” the new data reported at the virtual International AIDS conference “get us closer to understanding the effects of integrase inhibitors and TAF on weight and the potential metabolic consequences,” she commented as chair of the conference session where these reports occurred.
“Further data on the mechanism of weight gain and its reversibility after a change of treatment will help refine drug selection in the near future,” predicted Dr. Geretti.
“It’s hard to understand physiologically how drugs from such different classes all seem to have weight effects; it’s maddening,” said Dr. Venter. “We need decent studies in all patient populations. That will now be the priority,” he declared. “Patients shouldn’t have to choose” between drugs that most effectively control their HIV infection and drugs that don’t pose a risk for weight gain or metabolic derangements. PWH “should not have to face obesity as their new epidemic,” he wrote with Dr. Hill.
ADVANCE was funded in part by Viiv, the company that markets dolutegravir (Tivicay), and received drugs supplied by Gilead and Viiv. TANGO was sponsored by Viiv. DRIVE-SHIFT was funded by Merck, the company that markets doravirine (Pifeltro). Dr. Lake, Dr. Sokhela, Dr. Ake, and Dr. Kumar had no disclosures, Dr. Venter has received personal fees from Adcock Ingraham, Aspen Healthcare, Johnson and Johnson, Merck, Mylan, Roche, and Viiv. Dr. Hill has received payments from Merck. Dr. Geretti has received honoraria and research funding from Gilead, Jansse, Roche, and Viiv. Dr. Taiwo has had financial relationships with Gilead, Janssen, and Viiv. Dr. Hightow-Weidman has received honoraria from Gilead and Jansse. Dr. Wohl has been a consultant to Gilead, Johnson and Johnson, and Merck. Dr. Silverberg received research funding from Gilead. Dr. Mallon has been an advisor to and speaker on behalf of Bristol-Myers Squibb, Cilag, Gilead, Jansse, Merck Sharp & Dohme, and Viiv. Dr. van Wyk is a Viiv employee.
People living with HIV who put on extra pounds and develop metabolic syndrome or related disorders linked in part to certain antiretroviral agents remain a concern today, even as the drugs used to suppress HIV infection have evolved over the decades.
Linkage of HIV treatment with lipodystrophy and insulin resistance or diabetes began in the 1990s with protease inhibitors (Clin Infect Dis. 2000 Jun;30[suppl 2]:s135-42). Several reports over the years also tied any form of effective antiretroviral therapy to weight gain in HIV patients (Antivir Ther. 2012;17[7]:1281-9). More recently, reports have rattled the HIV-treatment community by associating alarmingly high levels of weight gain with a useful and relatively new drug, tenofovir alafenamide fumarate (TAF) – a nucleoside reverse transcriptase inhibitor (NRTI) approved for use in the United States in late 2016, as well as certain agents from an entirely different antiretroviral therapy (ART) class, the integrase strand transfer inhibitors (INSTIs). Both TAF and the INSTIs have come to play major roles in the HIV-treatment landscape, despite relevant and concerning recent weight gain observations with these drugs, such as in a 2019 meta-analysis of eight trials with 5,680 treatment-naive patients who started ART during 2003-2015 (Clin Infect Dis. 2019 Oct 14;doi: 10.1093/cid/ciz999).
“Weight gain is clearly seen in studies of dolutegravir [DTG] or bictegravir [BTG] with TAF,” wrote W.D. Francois Venter, PhD and Andrew Hill, PhD in a recent published commentary on the topic (Lancet HIV. 2020 Jun 1;7[6]:e389-400). Both DTG and BTG are INSTI class members.
“Excessive weight gain, defined as more than 10% over baseline, has recently been observed among people with HIV initiating or switching to regimens incorporating TAF, an INSTI, or both, particularly DTG,” wrote Jordan E. Lake, MD, an HIV specialist at the University of Texas Health Science Center at Houston, in a recent commentary posted online. Women and Black patients “are at even greater risk for excessive weight gain,” Dr. Lake added.
“In recent times, it has emerged that weight gain is more pronounced with the integrase inhibitor class of agents, especially dolutegravir and bictegravir, the so-called second-generation” INSTIs, said Anna Maria Geretti, MD, a professor of clinical infection, microbiology, and immunology at the University of Liverpool, England. ”The effect is more pronounced in women and people of non-White ethnicity, and is of concern because of the associated potential risk of metabolic syndrome, cardiovascular disease, etc.,” Dr. Geretti said in an interview.
The unprecedented susceptibility to weight gain seen recently in non-White women may in part have resulted from the tendency of many earlier treatment trials to have cohorts comprised predominantly of White men, Dr. Venter noted in an interview.
Alarming weight gains reported
Perhaps the most eye-popping example of the potential for weight gain with the combination of TAF with an INSTI came in a recent report from the ADVANCE trial, a randomized, head-to-head comparison of three regimens in 1,053 HIV patients in South Africa. After 144 weeks on a regimen of TAF (Vemlidy), DTG (Tivicay), and FTC (emtricitabine, Emtriva), another NRTI, women gained an averaged of more than 12 kg, compared with their baseline weight, significantly more than in two comparator groups, Simiso Sokhela, MB, reported at the virtual meeting of the International AIDS conference. The women in ADVANCE on the TAF-DTG-FTC regimen also had an 11% rate of incident metabolic syndrome during their first 96 weeks on treatment, compared with rates of 8% among patients on a different form of tenofovir, tenofovir disoproxil fumarate (TDF), along with DTG-FTC, and 5% among those on TDF–EFV (efavirenz, Sustiva)–FTC said Dr. Sokhela, an HIV researcher at Ezintsha, a division of the University of the Witwatersrand in Johannesburg, South Africa.
“We believe that these results support the World Health Organization guidelines that reserve TAF for only patients with osteoporosis or impaired renal function,” Dr. Sokhela said during a press briefing at the conference. The WHO guidelines list the first-line regimen as TDF-DTG-3TC (lamivudine; Epivir) or FTC. “The risk for becoming obese continued to increase after 96 weeks” of chronic use of these drugs, she added.
“All regimens are now brilliant at viral control. Finding the ones that don’t make patients obese or have other long-term side effects is now the priority,” noted Dr. Venter, a professor and HIV researcher at University of the Witwatersrand, head of Ezintsha, and lead investigator of ADVANCE. Clinicians and researchers have recently thought that combining TAF and an INSTI plus FTC or a similar NRTI “would be the ultimate regimen to replace the nonnucleoside reverse transcriptase inhibitors (NNRTIs)” such as EFV, “but now we have a major headache” with unexpectedly high weight gains in some patients, Dr. Venter said.
Weight gains “over 10 kg are unlikely to be acceptable in any circumstances, especially when starting body mass index is already borderline overweight,” wrote Dr. Venter along with Dr. Hill in their commentary. Until recently, many clinicians chalked up weight gain on newly begun ART as a manifestation of the patient’s “return-to-health,” but this interpretation “gives a positive spin to a potentially serious and common side effect,” they added.
More from ADVANCE
The primary efficacy endpoint of ADVANCE was suppression of viral load to less than 50 RNA copies/mL after 48 weeks on treatment, and the result showed that the TAF-DTG-FTC regimen and the TDF-DTG-FTC regimen were each noninferior to the control regimen of TDF-EFV-FTC (New Engl J Med. 2019 Aug 29;381[9]:803-15). Virtually all of the enrolled patients were Black, and 59% were women. Planned follow-up of all patients ran for 96 weeks. After 48 weeks, weight gain among the women averaged 6.4 kg, 3.2 kg, and 1.7 kg in the TAF-DTG, TDF-DTG, and TDF-EFV arms respectively. After 96 weeks, the average weight gains among women were 8.2 kg, 4.6 kg, and 3.2 kg, respectively, in new results reported by Dr. Sokhela at the IAC. Follow-up to 144 weeks was partial and included about a quarter of the enrolled women, with gains averaging 12.3 kg, 7.4 kg, and 5.5 kg respectively. The pattern of weight gain among men tracked the pattern in women, but the magnitude of gain was less. Among men followed for 144 weeks, average gain among those on TAF-DTG-FTC was 7.2 kg, the largest gain seen among men on any regimen and at any follow-up time in the study.
Dr. Sokhela also reported data on body composition analyses, which showed that the weight gains were largely in fat rather than lean tissue, fat accumulation was significantly greater in women than men, and that in both sexes fat accumulated roughly equally in the trunk and on limbs.
An additional analysis looked at the incidence of new-onset obesity among the women who had a normal body mass index at baseline. After 96 weeks, incident obesity occurred in 14% of women on the TAG-DTG-FTC regimen, 8% on TDF-DTG-FTC, and in 2% of women maintained on TDF-EFV-FTC, said Dr. Hill in a separate report at the conference.
Weight starts to weigh in
“I am very mindful of weight gain potential, and I talk to patients about it. It doesn’t determine what regimen I choose for a patient” right now, “but it’s only a matter of time before it starts influencing what we do, particularly if we can achieve efficacy with fewer drugs,” commented Babafemi O. Taiwo, MD, professor of medicine and chief of infectious diseases at Northwestern University in Chicago. “I’ve had some patients show up with a weight gain of 20 kg, and that shouldn’t happen,” he said during a recent online educational session. Dr. Taiwo said his recent practice has been to warn patients about possible weight gain and to urge them to get back in touch with him quickly if it happens.
“Virologic suppression is the most important goal with ART, and the U.S. Department of Health and Human Services currently recommends INSTI-based ART for most PWH [people with HIV],” wrote Dr. Lake in April 2020. “I counsel all PWH initiating ART about the potential for weight gain, and I discuss their current diet and healthy lifestyle habits. I explain to patients that we will monitor their weight, and if weight gain seems more than either of us are comfortable with then we will reassess. Only a small percentage of patients experience excessive weight gain after starting ART.” Dr. Lake also stressed that she had not yet begun to change the regimen a patient is on solely because of weight gain. “We do not know whether this weight gain is reversible,” she noted.
“I do not anticipate that a risk of weight gain at present will dictate a change in guidelines,” said Dr. Geretti. “Drugs such as dolutegravir and bictegravir are very effective, and they are unlikely to cause drug resistance. Further data on the mechanism of weight gain and the reversibility after a change of treatment will help refine drug selection in the near future,” she predicted.
“I consider weight gain when prescribing because my patients hear about this. It’s a side effect that my patients really care about, and I don’t blame them,” said Lisa Hightow-Weidman, MD, a professor and HIV specialist at the University of North Carolina at Chapel Hill, during an on-line educational session. “If you don’t discuss it with a patient and then weight gain happens and the patient finds out [the known risk from their treatment] they may have an issue,” she noted. But weight gain is not a reason to avoid these drugs. “They are great medications in many ways, with once-daily regimens and few side effects.”
Weight gain during pregnancy a special concern
An additional analysis of data from ADVANCE presented at the conference highlighted what the observed weight gain on ART could mean for women who become pregnant while on treatment. Based on a systematic literature review, the ADVANCE investigators calculated the relative risk for six obesity-related pregnancy complications, compared with nonobese women: preterm delivery, gestational diabetes, gestational hypertension, preeclampsia, postpartum hemorrhage, and caesarean delivery. Based on the obesity changes among women on their assigned ART in ADVANCE, the researchers calculated the predicted incidence of these six complications. The analysis showed that for every 1,000 women, those on TAG-DTG-FTC would have an excess of 53 obesity-related pregnancy complications, those on TDF-DTG-FTC would develop 28 excess pregnancy complications, and those on TDG-EFV-FTC would have four excess complications, reported Dr. Hill at the International AIDS conference.
The researchers also ran a similar simulation for the incidence of neonatal complications that could result when mothers are obese because of their ART. The six neonatal complications included in this analysis were small for gestational age, large for gestational age, macrosomia, neonatal death, stillbirth, and neural tube defects. Based on the excess rate of incident obesity, they calculated that for every 1,000 pregnancies women on TAD-DTG-FTC would have 24 additional infants born with one of these complications, women on TDF-DTG-FTC would have an excess of 13 of these events, and women on TDG-EFV-FTC would have an excess of three such obesity-related neonatal complications, Dr. Hill said.
Sorting out the drugs
Results from several additional studies reported at the conference have started trying to discern exactly which ART drugs and regimens pose the greatest weight gain risk and which have the least risk while retaining high efficacy and resistance barriers.
Further evidence implicating any type of ART as a driver of increased weight came from a review of 8,256 adults infected with HIV and members of the Kaiser Permanente health system in three U.S. regions during 2000-2016. Researchers matched these cases using several demographic factors with just under 130,000 members without HIV. Those infected by HIV had half the prevalence of obesity as the matched controls at baseline. During 12 years of follow-up, those infected with HIV had a threefold higher rate of weight gain than those who were uninfected. Annual weight gain averaged 0.06 kg/year among the uninfected people and 0.22 kg/year among those infected with HIV, a statistically significant difference that was consistent regardless of whether people started the study at a normal body mass index, overweight, or obese, reported Michael J. Silverberg, PhD, an epidemiologist with Kaiser Permanente in Oakland, Calif.
Another study tried to focus on the weight gain impact when patients on three-drug ART regimens changed from taking TDF to TAF. This analysis used data collected in the OPERA (Observational Pharmaco-Epidemiology Research & Analysis) longitudinal cohort of about 115,000 U.S. PWH. The observational cohort included nearly 7,000 patients who made a TDF-to-TAF switch, including 3,288 patients who maintained treatment during this switch with an INSTI, 1,454 who maintained a background regimen based on a NNRTI, 1,430 patients who also switched from an INSTI to a different drug, and 747 patients maintained on a boosted dose of a protease inhibitor. All patients were well controlled on their baseline regimen, with at least two consecutive measures showing undetectable viral load.
Patients who maintained their background regimens while changing from TDF to TAF had a 2.0-2.6 kg increase in weight during the 9 months immediately following their switch to TAF, reported Patrick Mallon, MB, a professor of microbial diseases at University College Dublin. Among the patients who both switched to TAF and also switched to treatment with an INSTI, weight gain during the 9 months after the switch averaged 2.6-4.5 kg, depending on which INSTI was started. Patients who switched to treatment with elvitegravir/cobicistat (an INSTI plus a boosting agent) averaged a gain of 2.6 kg during 9 months, those who switched to DTG averaged a 3.1-kg gain, and those who switched to BTG averaged a 4.6-kg increase, Dr. Mallon reported at the conference.
These findings “give us a good sense that the weight gain is real. This is not just overeating or not exercising, but weight changes coincidental with a change in HIV treatment,” commented David Wohl, MD, professor of medicine and site leader of the HIV Prevention and Treatment Clinical Trials Unit at the University of North Carolina at Chapel Hill, during an online educational session.
Contrary to this evidence suggesting a consistent uptick in weight when patients start TAF treatment was a recent report on 629 HIV patients randomized to treatment with TAF-BTG-FTC or abacavir (an NRTI, Ziagen)–DTG-3TC, which found similar weight gains between these two regimens after 144 weeks on treatment (Lancet HIV. 2020 Jun;7[6]:e389-400). This finding had the effect of “strengthening the argument that TAF is simply an innocent bystander” and does not play a central role in weight gain, and supporting the notion that the alternative tenofovir formulation, TDF, differs from TAF by promoting weight loss, Dr. Venter and Dr. Hill suggested in their commentary that accompanied this report.
The new findings from Dr. Mallon raise “serious questions about the way we have moved to TAF as a replacement for TDF, especially because the benefits [from TAF] are for a small subgroup – patients with renal disease or osteoporosis,” Dr. Venter said in an interview. “The question is, will we see weight gain like this” if TAF was combined with a non-INSTI drug? he wondered.
While some study results have suggested a mitigating effect from TDF on weight gain, that wasn’t the case in the AFRICOS (African Cohort Study) study of 1,954 PWH who started treatment with TDF-DTG-FTC (742 patients) or a different three-drug regimen. After a median of 225 days on treatment, those who started on TDF-DTG-FTC had an adjusted, 85% higher rate of developing a high body mass index, compared with patients on a different ART regimen, Julie Ake, MD, reported in a talk at the conference. Her conclusion focused on the possible involvement of DTG: “Consistent with previous reports, dolutegravir was significantly associated with an increased risk of developing high body mass index,” said Dr. Ake, director of the U.S. Military HIV Research Program in Bethesda, Md. and leader of AFRICOS.
A potential workaround to some drugs that cause excessive the weight gain is to just not use them. That was part of the rationale for the TANGO study, which took 741 HIV-infected patients with successful viral suppression on a regimen of TAF-FTC plus one or two additional agents and switched half of them to a TAF-less, two-drug regimen of DTG-FTC. This open-label study’s primary endpoint was noninferiority for viral suppression of the DTG-FTC regimen, compared with patients who stayed on their starting regimen, and the results proved that DTG-FTC was just as effective over 48 weeks for this outcome (Clin Infect Dis. 2020 Jan 6. doi: 10.1093/cid/ciz1243).
At the conference, TANGO’s lead investigator, Jean van Wyk, MD, reported the weight and metabolic effects of the switch. The results showed a similar and small weight gain (on average less than 1 kg) during 48 week follow-up regardless of whether patients remained on their baseline, TAF-containing regimen or switched to DTG-FTC, said Dr. van Wyk, global medical lead for HIV treatment at Viiv Healthcare, the company that markets DTG. About three-quarters of patients in both arms received “boosted” dosages of their drugs, and in this subgroup, patients on DTG-FTC showed statistically significant benefits in several lipid levels, fasting glucose level, and in their degree of insulin resistance. Dr. van Wyk said. These between-group differences were not statistically significant among the “unboosted” patients, and the results failed to show a significant between-group difference in the incidence of metabolic syndrome.
Dr. Venter called these results “exciting,” and noted that he already uses the DTG-FTC two-drug combination “a lot” to treat PWH and renal disease.
A second alternative regimen showcased in a talk at the conference used the three-drug regimen of TDF-FTC plus the NNRTI, DOR (doravirine, Pifeltro). The DRIVE-SHIFT trial enrolled 670 HIV patients with successfully suppressed viral load on conventional regimens who were either switched to TDF-DOR-FTC or maintained on their baseline treatment. After 48 weeks, results confirmed the primary efficacy endpoint of noninferiority for maintenance of suppression with the investigational regimen (J Acquir Immune Defic Syndr. 2019 Aug;81[4]:463-72).
A post-hoc analysis looked at weight changes among these patients after as much as 144 weeks of follow-up. The results showed that patients switched to TDF-DOR-FTC had an average weight increase of 1.2-1.4 kg after more than 2 years on the new regimen, with fewer than 10% of patients having a 10% or greater weight gain with DOR, a “next-generation” NNRTI, reported Princy N. Kumar, MD, professor at Georgetown University and chief of infectious diseases at MedStar Georgetown University Hospital in Washington. “Weight gain was minimal, even over the long term,” she noted.
The tested DOR-based regimen also looks “very exciting,” but the populations it’s been tested have also been largely limited to White men, and limited data exist about the regimen’s performance in pregnant women, commented Dr. Venter. The DRIVE-SHIRT patient cohort was about 85% men, and about three-quarters White.
More weight data needed
HIV-treatment researchers and clinicians seem agreed that weight gain and other metabolic effects from HIV treatment need more assessment and evidence because current data, while suggestive, is also inconclusive.
“Clinical trials are desperately needed to understand the mechanisms of and potential therapeutic options for excessive weight gain on ART,” wrote Dr. Lake in her commentary in April. “While more research is needed,” the new data reported at the virtual International AIDS conference “get us closer to understanding the effects of integrase inhibitors and TAF on weight and the potential metabolic consequences,” she commented as chair of the conference session where these reports occurred.
“Further data on the mechanism of weight gain and its reversibility after a change of treatment will help refine drug selection in the near future,” predicted Dr. Geretti.
“It’s hard to understand physiologically how drugs from such different classes all seem to have weight effects; it’s maddening,” said Dr. Venter. “We need decent studies in all patient populations. That will now be the priority,” he declared. “Patients shouldn’t have to choose” between drugs that most effectively control their HIV infection and drugs that don’t pose a risk for weight gain or metabolic derangements. PWH “should not have to face obesity as their new epidemic,” he wrote with Dr. Hill.
ADVANCE was funded in part by Viiv, the company that markets dolutegravir (Tivicay), and received drugs supplied by Gilead and Viiv. TANGO was sponsored by Viiv. DRIVE-SHIFT was funded by Merck, the company that markets doravirine (Pifeltro). Dr. Lake, Dr. Sokhela, Dr. Ake, and Dr. Kumar had no disclosures, Dr. Venter has received personal fees from Adcock Ingraham, Aspen Healthcare, Johnson and Johnson, Merck, Mylan, Roche, and Viiv. Dr. Hill has received payments from Merck. Dr. Geretti has received honoraria and research funding from Gilead, Jansse, Roche, and Viiv. Dr. Taiwo has had financial relationships with Gilead, Janssen, and Viiv. Dr. Hightow-Weidman has received honoraria from Gilead and Jansse. Dr. Wohl has been a consultant to Gilead, Johnson and Johnson, and Merck. Dr. Silverberg received research funding from Gilead. Dr. Mallon has been an advisor to and speaker on behalf of Bristol-Myers Squibb, Cilag, Gilead, Jansse, Merck Sharp & Dohme, and Viiv. Dr. van Wyk is a Viiv employee.
People living with HIV who put on extra pounds and develop metabolic syndrome or related disorders linked in part to certain antiretroviral agents remain a concern today, even as the drugs used to suppress HIV infection have evolved over the decades.
Linkage of HIV treatment with lipodystrophy and insulin resistance or diabetes began in the 1990s with protease inhibitors (Clin Infect Dis. 2000 Jun;30[suppl 2]:s135-42). Several reports over the years also tied any form of effective antiretroviral therapy to weight gain in HIV patients (Antivir Ther. 2012;17[7]:1281-9). More recently, reports have rattled the HIV-treatment community by associating alarmingly high levels of weight gain with a useful and relatively new drug, tenofovir alafenamide fumarate (TAF) – a nucleoside reverse transcriptase inhibitor (NRTI) approved for use in the United States in late 2016, as well as certain agents from an entirely different antiretroviral therapy (ART) class, the integrase strand transfer inhibitors (INSTIs). Both TAF and the INSTIs have come to play major roles in the HIV-treatment landscape, despite relevant and concerning recent weight gain observations with these drugs, such as in a 2019 meta-analysis of eight trials with 5,680 treatment-naive patients who started ART during 2003-2015 (Clin Infect Dis. 2019 Oct 14;doi: 10.1093/cid/ciz999).
“Weight gain is clearly seen in studies of dolutegravir [DTG] or bictegravir [BTG] with TAF,” wrote W.D. Francois Venter, PhD and Andrew Hill, PhD in a recent published commentary on the topic (Lancet HIV. 2020 Jun 1;7[6]:e389-400). Both DTG and BTG are INSTI class members.
“Excessive weight gain, defined as more than 10% over baseline, has recently been observed among people with HIV initiating or switching to regimens incorporating TAF, an INSTI, or both, particularly DTG,” wrote Jordan E. Lake, MD, an HIV specialist at the University of Texas Health Science Center at Houston, in a recent commentary posted online. Women and Black patients “are at even greater risk for excessive weight gain,” Dr. Lake added.
“In recent times, it has emerged that weight gain is more pronounced with the integrase inhibitor class of agents, especially dolutegravir and bictegravir, the so-called second-generation” INSTIs, said Anna Maria Geretti, MD, a professor of clinical infection, microbiology, and immunology at the University of Liverpool, England. ”The effect is more pronounced in women and people of non-White ethnicity, and is of concern because of the associated potential risk of metabolic syndrome, cardiovascular disease, etc.,” Dr. Geretti said in an interview.
The unprecedented susceptibility to weight gain seen recently in non-White women may in part have resulted from the tendency of many earlier treatment trials to have cohorts comprised predominantly of White men, Dr. Venter noted in an interview.
Alarming weight gains reported
Perhaps the most eye-popping example of the potential for weight gain with the combination of TAF with an INSTI came in a recent report from the ADVANCE trial, a randomized, head-to-head comparison of three regimens in 1,053 HIV patients in South Africa. After 144 weeks on a regimen of TAF (Vemlidy), DTG (Tivicay), and FTC (emtricitabine, Emtriva), another NRTI, women gained an averaged of more than 12 kg, compared with their baseline weight, significantly more than in two comparator groups, Simiso Sokhela, MB, reported at the virtual meeting of the International AIDS conference. The women in ADVANCE on the TAF-DTG-FTC regimen also had an 11% rate of incident metabolic syndrome during their first 96 weeks on treatment, compared with rates of 8% among patients on a different form of tenofovir, tenofovir disoproxil fumarate (TDF), along with DTG-FTC, and 5% among those on TDF–EFV (efavirenz, Sustiva)–FTC said Dr. Sokhela, an HIV researcher at Ezintsha, a division of the University of the Witwatersrand in Johannesburg, South Africa.
“We believe that these results support the World Health Organization guidelines that reserve TAF for only patients with osteoporosis or impaired renal function,” Dr. Sokhela said during a press briefing at the conference. The WHO guidelines list the first-line regimen as TDF-DTG-3TC (lamivudine; Epivir) or FTC. “The risk for becoming obese continued to increase after 96 weeks” of chronic use of these drugs, she added.
“All regimens are now brilliant at viral control. Finding the ones that don’t make patients obese or have other long-term side effects is now the priority,” noted Dr. Venter, a professor and HIV researcher at University of the Witwatersrand, head of Ezintsha, and lead investigator of ADVANCE. Clinicians and researchers have recently thought that combining TAF and an INSTI plus FTC or a similar NRTI “would be the ultimate regimen to replace the nonnucleoside reverse transcriptase inhibitors (NNRTIs)” such as EFV, “but now we have a major headache” with unexpectedly high weight gains in some patients, Dr. Venter said.
Weight gains “over 10 kg are unlikely to be acceptable in any circumstances, especially when starting body mass index is already borderline overweight,” wrote Dr. Venter along with Dr. Hill in their commentary. Until recently, many clinicians chalked up weight gain on newly begun ART as a manifestation of the patient’s “return-to-health,” but this interpretation “gives a positive spin to a potentially serious and common side effect,” they added.
More from ADVANCE
The primary efficacy endpoint of ADVANCE was suppression of viral load to less than 50 RNA copies/mL after 48 weeks on treatment, and the result showed that the TAF-DTG-FTC regimen and the TDF-DTG-FTC regimen were each noninferior to the control regimen of TDF-EFV-FTC (New Engl J Med. 2019 Aug 29;381[9]:803-15). Virtually all of the enrolled patients were Black, and 59% were women. Planned follow-up of all patients ran for 96 weeks. After 48 weeks, weight gain among the women averaged 6.4 kg, 3.2 kg, and 1.7 kg in the TAF-DTG, TDF-DTG, and TDF-EFV arms respectively. After 96 weeks, the average weight gains among women were 8.2 kg, 4.6 kg, and 3.2 kg, respectively, in new results reported by Dr. Sokhela at the IAC. Follow-up to 144 weeks was partial and included about a quarter of the enrolled women, with gains averaging 12.3 kg, 7.4 kg, and 5.5 kg respectively. The pattern of weight gain among men tracked the pattern in women, but the magnitude of gain was less. Among men followed for 144 weeks, average gain among those on TAF-DTG-FTC was 7.2 kg, the largest gain seen among men on any regimen and at any follow-up time in the study.
Dr. Sokhela also reported data on body composition analyses, which showed that the weight gains were largely in fat rather than lean tissue, fat accumulation was significantly greater in women than men, and that in both sexes fat accumulated roughly equally in the trunk and on limbs.
An additional analysis looked at the incidence of new-onset obesity among the women who had a normal body mass index at baseline. After 96 weeks, incident obesity occurred in 14% of women on the TAG-DTG-FTC regimen, 8% on TDF-DTG-FTC, and in 2% of women maintained on TDF-EFV-FTC, said Dr. Hill in a separate report at the conference.
Weight starts to weigh in
“I am very mindful of weight gain potential, and I talk to patients about it. It doesn’t determine what regimen I choose for a patient” right now, “but it’s only a matter of time before it starts influencing what we do, particularly if we can achieve efficacy with fewer drugs,” commented Babafemi O. Taiwo, MD, professor of medicine and chief of infectious diseases at Northwestern University in Chicago. “I’ve had some patients show up with a weight gain of 20 kg, and that shouldn’t happen,” he said during a recent online educational session. Dr. Taiwo said his recent practice has been to warn patients about possible weight gain and to urge them to get back in touch with him quickly if it happens.
“Virologic suppression is the most important goal with ART, and the U.S. Department of Health and Human Services currently recommends INSTI-based ART for most PWH [people with HIV],” wrote Dr. Lake in April 2020. “I counsel all PWH initiating ART about the potential for weight gain, and I discuss their current diet and healthy lifestyle habits. I explain to patients that we will monitor their weight, and if weight gain seems more than either of us are comfortable with then we will reassess. Only a small percentage of patients experience excessive weight gain after starting ART.” Dr. Lake also stressed that she had not yet begun to change the regimen a patient is on solely because of weight gain. “We do not know whether this weight gain is reversible,” she noted.
“I do not anticipate that a risk of weight gain at present will dictate a change in guidelines,” said Dr. Geretti. “Drugs such as dolutegravir and bictegravir are very effective, and they are unlikely to cause drug resistance. Further data on the mechanism of weight gain and the reversibility after a change of treatment will help refine drug selection in the near future,” she predicted.
“I consider weight gain when prescribing because my patients hear about this. It’s a side effect that my patients really care about, and I don’t blame them,” said Lisa Hightow-Weidman, MD, a professor and HIV specialist at the University of North Carolina at Chapel Hill, during an on-line educational session. “If you don’t discuss it with a patient and then weight gain happens and the patient finds out [the known risk from their treatment] they may have an issue,” she noted. But weight gain is not a reason to avoid these drugs. “They are great medications in many ways, with once-daily regimens and few side effects.”
Weight gain during pregnancy a special concern
An additional analysis of data from ADVANCE presented at the conference highlighted what the observed weight gain on ART could mean for women who become pregnant while on treatment. Based on a systematic literature review, the ADVANCE investigators calculated the relative risk for six obesity-related pregnancy complications, compared with nonobese women: preterm delivery, gestational diabetes, gestational hypertension, preeclampsia, postpartum hemorrhage, and caesarean delivery. Based on the obesity changes among women on their assigned ART in ADVANCE, the researchers calculated the predicted incidence of these six complications. The analysis showed that for every 1,000 women, those on TAG-DTG-FTC would have an excess of 53 obesity-related pregnancy complications, those on TDF-DTG-FTC would develop 28 excess pregnancy complications, and those on TDG-EFV-FTC would have four excess complications, reported Dr. Hill at the International AIDS conference.
The researchers also ran a similar simulation for the incidence of neonatal complications that could result when mothers are obese because of their ART. The six neonatal complications included in this analysis were small for gestational age, large for gestational age, macrosomia, neonatal death, stillbirth, and neural tube defects. Based on the excess rate of incident obesity, they calculated that for every 1,000 pregnancies women on TAD-DTG-FTC would have 24 additional infants born with one of these complications, women on TDF-DTG-FTC would have an excess of 13 of these events, and women on TDG-EFV-FTC would have an excess of three such obesity-related neonatal complications, Dr. Hill said.
Sorting out the drugs
Results from several additional studies reported at the conference have started trying to discern exactly which ART drugs and regimens pose the greatest weight gain risk and which have the least risk while retaining high efficacy and resistance barriers.
Further evidence implicating any type of ART as a driver of increased weight came from a review of 8,256 adults infected with HIV and members of the Kaiser Permanente health system in three U.S. regions during 2000-2016. Researchers matched these cases using several demographic factors with just under 130,000 members without HIV. Those infected by HIV had half the prevalence of obesity as the matched controls at baseline. During 12 years of follow-up, those infected with HIV had a threefold higher rate of weight gain than those who were uninfected. Annual weight gain averaged 0.06 kg/year among the uninfected people and 0.22 kg/year among those infected with HIV, a statistically significant difference that was consistent regardless of whether people started the study at a normal body mass index, overweight, or obese, reported Michael J. Silverberg, PhD, an epidemiologist with Kaiser Permanente in Oakland, Calif.
Another study tried to focus on the weight gain impact when patients on three-drug ART regimens changed from taking TDF to TAF. This analysis used data collected in the OPERA (Observational Pharmaco-Epidemiology Research & Analysis) longitudinal cohort of about 115,000 U.S. PWH. The observational cohort included nearly 7,000 patients who made a TDF-to-TAF switch, including 3,288 patients who maintained treatment during this switch with an INSTI, 1,454 who maintained a background regimen based on a NNRTI, 1,430 patients who also switched from an INSTI to a different drug, and 747 patients maintained on a boosted dose of a protease inhibitor. All patients were well controlled on their baseline regimen, with at least two consecutive measures showing undetectable viral load.
Patients who maintained their background regimens while changing from TDF to TAF had a 2.0-2.6 kg increase in weight during the 9 months immediately following their switch to TAF, reported Patrick Mallon, MB, a professor of microbial diseases at University College Dublin. Among the patients who both switched to TAF and also switched to treatment with an INSTI, weight gain during the 9 months after the switch averaged 2.6-4.5 kg, depending on which INSTI was started. Patients who switched to treatment with elvitegravir/cobicistat (an INSTI plus a boosting agent) averaged a gain of 2.6 kg during 9 months, those who switched to DTG averaged a 3.1-kg gain, and those who switched to BTG averaged a 4.6-kg increase, Dr. Mallon reported at the conference.
These findings “give us a good sense that the weight gain is real. This is not just overeating or not exercising, but weight changes coincidental with a change in HIV treatment,” commented David Wohl, MD, professor of medicine and site leader of the HIV Prevention and Treatment Clinical Trials Unit at the University of North Carolina at Chapel Hill, during an online educational session.
Contrary to this evidence suggesting a consistent uptick in weight when patients start TAF treatment was a recent report on 629 HIV patients randomized to treatment with TAF-BTG-FTC or abacavir (an NRTI, Ziagen)–DTG-3TC, which found similar weight gains between these two regimens after 144 weeks on treatment (Lancet HIV. 2020 Jun;7[6]:e389-400). This finding had the effect of “strengthening the argument that TAF is simply an innocent bystander” and does not play a central role in weight gain, and supporting the notion that the alternative tenofovir formulation, TDF, differs from TAF by promoting weight loss, Dr. Venter and Dr. Hill suggested in their commentary that accompanied this report.
The new findings from Dr. Mallon raise “serious questions about the way we have moved to TAF as a replacement for TDF, especially because the benefits [from TAF] are for a small subgroup – patients with renal disease or osteoporosis,” Dr. Venter said in an interview. “The question is, will we see weight gain like this” if TAF was combined with a non-INSTI drug? he wondered.
While some study results have suggested a mitigating effect from TDF on weight gain, that wasn’t the case in the AFRICOS (African Cohort Study) study of 1,954 PWH who started treatment with TDF-DTG-FTC (742 patients) or a different three-drug regimen. After a median of 225 days on treatment, those who started on TDF-DTG-FTC had an adjusted, 85% higher rate of developing a high body mass index, compared with patients on a different ART regimen, Julie Ake, MD, reported in a talk at the conference. Her conclusion focused on the possible involvement of DTG: “Consistent with previous reports, dolutegravir was significantly associated with an increased risk of developing high body mass index,” said Dr. Ake, director of the U.S. Military HIV Research Program in Bethesda, Md. and leader of AFRICOS.
A potential workaround to some drugs that cause excessive the weight gain is to just not use them. That was part of the rationale for the TANGO study, which took 741 HIV-infected patients with successful viral suppression on a regimen of TAF-FTC plus one or two additional agents and switched half of them to a TAF-less, two-drug regimen of DTG-FTC. This open-label study’s primary endpoint was noninferiority for viral suppression of the DTG-FTC regimen, compared with patients who stayed on their starting regimen, and the results proved that DTG-FTC was just as effective over 48 weeks for this outcome (Clin Infect Dis. 2020 Jan 6. doi: 10.1093/cid/ciz1243).
At the conference, TANGO’s lead investigator, Jean van Wyk, MD, reported the weight and metabolic effects of the switch. The results showed a similar and small weight gain (on average less than 1 kg) during 48 week follow-up regardless of whether patients remained on their baseline, TAF-containing regimen or switched to DTG-FTC, said Dr. van Wyk, global medical lead for HIV treatment at Viiv Healthcare, the company that markets DTG. About three-quarters of patients in both arms received “boosted” dosages of their drugs, and in this subgroup, patients on DTG-FTC showed statistically significant benefits in several lipid levels, fasting glucose level, and in their degree of insulin resistance. Dr. van Wyk said. These between-group differences were not statistically significant among the “unboosted” patients, and the results failed to show a significant between-group difference in the incidence of metabolic syndrome.
Dr. Venter called these results “exciting,” and noted that he already uses the DTG-FTC two-drug combination “a lot” to treat PWH and renal disease.
A second alternative regimen showcased in a talk at the conference used the three-drug regimen of TDF-FTC plus the NNRTI, DOR (doravirine, Pifeltro). The DRIVE-SHIFT trial enrolled 670 HIV patients with successfully suppressed viral load on conventional regimens who were either switched to TDF-DOR-FTC or maintained on their baseline treatment. After 48 weeks, results confirmed the primary efficacy endpoint of noninferiority for maintenance of suppression with the investigational regimen (J Acquir Immune Defic Syndr. 2019 Aug;81[4]:463-72).
A post-hoc analysis looked at weight changes among these patients after as much as 144 weeks of follow-up. The results showed that patients switched to TDF-DOR-FTC had an average weight increase of 1.2-1.4 kg after more than 2 years on the new regimen, with fewer than 10% of patients having a 10% or greater weight gain with DOR, a “next-generation” NNRTI, reported Princy N. Kumar, MD, professor at Georgetown University and chief of infectious diseases at MedStar Georgetown University Hospital in Washington. “Weight gain was minimal, even over the long term,” she noted.
The tested DOR-based regimen also looks “very exciting,” but the populations it’s been tested have also been largely limited to White men, and limited data exist about the regimen’s performance in pregnant women, commented Dr. Venter. The DRIVE-SHIRT patient cohort was about 85% men, and about three-quarters White.
More weight data needed
HIV-treatment researchers and clinicians seem agreed that weight gain and other metabolic effects from HIV treatment need more assessment and evidence because current data, while suggestive, is also inconclusive.
“Clinical trials are desperately needed to understand the mechanisms of and potential therapeutic options for excessive weight gain on ART,” wrote Dr. Lake in her commentary in April. “While more research is needed,” the new data reported at the virtual International AIDS conference “get us closer to understanding the effects of integrase inhibitors and TAF on weight and the potential metabolic consequences,” she commented as chair of the conference session where these reports occurred.
“Further data on the mechanism of weight gain and its reversibility after a change of treatment will help refine drug selection in the near future,” predicted Dr. Geretti.
“It’s hard to understand physiologically how drugs from such different classes all seem to have weight effects; it’s maddening,” said Dr. Venter. “We need decent studies in all patient populations. That will now be the priority,” he declared. “Patients shouldn’t have to choose” between drugs that most effectively control their HIV infection and drugs that don’t pose a risk for weight gain or metabolic derangements. PWH “should not have to face obesity as their new epidemic,” he wrote with Dr. Hill.
ADVANCE was funded in part by Viiv, the company that markets dolutegravir (Tivicay), and received drugs supplied by Gilead and Viiv. TANGO was sponsored by Viiv. DRIVE-SHIFT was funded by Merck, the company that markets doravirine (Pifeltro). Dr. Lake, Dr. Sokhela, Dr. Ake, and Dr. Kumar had no disclosures, Dr. Venter has received personal fees from Adcock Ingraham, Aspen Healthcare, Johnson and Johnson, Merck, Mylan, Roche, and Viiv. Dr. Hill has received payments from Merck. Dr. Geretti has received honoraria and research funding from Gilead, Jansse, Roche, and Viiv. Dr. Taiwo has had financial relationships with Gilead, Janssen, and Viiv. Dr. Hightow-Weidman has received honoraria from Gilead and Jansse. Dr. Wohl has been a consultant to Gilead, Johnson and Johnson, and Merck. Dr. Silverberg received research funding from Gilead. Dr. Mallon has been an advisor to and speaker on behalf of Bristol-Myers Squibb, Cilag, Gilead, Jansse, Merck Sharp & Dohme, and Viiv. Dr. van Wyk is a Viiv employee.
FROM AIDS 2020
Easy access to PrEP reduces rates of HIV acquisition
When people were offered preexposure prophylaxis (PrEP) outside of traditional clinics, regardless of specific risk factors, as part of the Sustainable East Africa Research in Community Health (SEARCH) study, new HIV acquisitions dropped by 74%.
It’s a valuable lesson to providers around the world, said Catherine Koss, MD, assistant professor of medicine in HIV, infectious disease, and global medicine at the University of California, San Francisco.
“We haven’t really seen PrEP being scaled up and offered at such a broad level in communities,” Koss said during the International AIDS Conference 2020.
The first part of SEARCH, which looked at the impact of universal testing and access to HIV treatment immediately after diagnosis, showed that the strategy resulted in a population-wide 30% reduction in new HIV acquisitions. In other words, treatment alone wasn’t enough to end the HIV epidemic.
But the researchers always knew “there were likely going to be new HIV infections,” even with universal HIV testing and treatment, Koss said.
So the second part of the study was designed to see whether PrEP — with the combination of tenofovir disoproxil fumarate plus emtricitabine (Truvada, Gilead Sciences) — could further reduce rates of HIV acquisition.
PrEP out in the community
During the PrEP part of the SEARCH study, researchers discussed HIV risk with adults in 16 communities in rural Kenya and Uganda during population-level testing that took place at health fairs, beaches, trading centers, other community sites, and even in participants’ homes. PrEP was offered to anyone in a relationship with someone living with HIV, to anyone determined to be at elevated risk for infection by a previously validated algorithm, and to anyone who did not fit those criteria but who wanted a prescription.
Of the 15,632 adults eligible for PrEP, 5,447 (35%) chose to start the HIV prevention pill.
A rapid-enrollment protocol meant that people received their prescription at the time of screening or soon after that. Participants underwent testing for HIV antibodies — also out in the community — at weeks 4 and 12, and every 12 weeks thereafter; this will continue out to week 144.
HIV-negative adults who were part of the larger SEARCH cohort in the year before PrEP was made available — and from the same communities — served as the control group.
Interim 60-week data show that the rate of acquisition was 74% lower in the PrEP group than in the control group (incidence rate ratio, 0.26; P = .01). In women, the acquisition rate was 76% lower (incidence rate ratio, 0.24; P = .04), and in men, it was 40% lower (incidence rate ratio, 0.60; P = .54).
The reduction was not significant for men, probably because so few men acquired HIV, Koss reported. The powerful drop in new HIV cases overall was related to PrEP use by women; cases in women fell from 1.52 to 0.40 per 100 person-years.
Blood tests showed that 72% of the people who acquired HIV during the study period had not taken a PrEP pill for at least 30 days before their diagnosis.
“Making PrEP more easily accessible and more community-based could be very powerful in the United States,” said Koss.
“Allowing people to test for HIV and start PrEP outside of health clinics or standard health facilities could help reach more people,” she told Medscape Medical News. “Many of the people who benefit from PrEP may not otherwise need to seek medical care regularly if they’re otherwise healthy and often young.”
When PrEP is made available — easily available — people will pick it up, they will take it away, they will put it in their mouths, and they will not get HIV.
The findings were hailed by others in the field of HIV prevention.
“They’re fantastic,” said Jared Baeten, MD, vice dean of the School of Public Health and professor of global health, medicine, and epidemiology at the University of Washington in Seattle. He was involved in Partners PrEP, a study of PrEP use in mixed-HIV-status couples, the Partners Demonstration Project, and HOPE, a study of the dapivirine ring for HIV prevention.
“These data provide real evidence that when PrEP is made available — easily available — people will pick it up, they will take it away, they will put it in their mouths, and they will not get HIV,” he said in an interview.
Even more, they clarify something that has stymied American regulators and clinicians.
Early studies of PrEP use by single women were stopped because participants weren’t taking the pills; adherence was so low that researchers couldn’t show efficacy. Since then, various trials — including Partners PrEP — have shown that PrEP works in women, but doubts have lingered, leading women to “get the short end of the stick in discussions about PrEP,” Baeten explained.
“There really shouldn’t be questions anymore,” he said. “These findings should put to rest any question about women in Africa being able to benefit from PrEP.”
This article first appeared on Medscape.com.
When people were offered preexposure prophylaxis (PrEP) outside of traditional clinics, regardless of specific risk factors, as part of the Sustainable East Africa Research in Community Health (SEARCH) study, new HIV acquisitions dropped by 74%.
It’s a valuable lesson to providers around the world, said Catherine Koss, MD, assistant professor of medicine in HIV, infectious disease, and global medicine at the University of California, San Francisco.
“We haven’t really seen PrEP being scaled up and offered at such a broad level in communities,” Koss said during the International AIDS Conference 2020.
The first part of SEARCH, which looked at the impact of universal testing and access to HIV treatment immediately after diagnosis, showed that the strategy resulted in a population-wide 30% reduction in new HIV acquisitions. In other words, treatment alone wasn’t enough to end the HIV epidemic.
But the researchers always knew “there were likely going to be new HIV infections,” even with universal HIV testing and treatment, Koss said.
So the second part of the study was designed to see whether PrEP — with the combination of tenofovir disoproxil fumarate plus emtricitabine (Truvada, Gilead Sciences) — could further reduce rates of HIV acquisition.
PrEP out in the community
During the PrEP part of the SEARCH study, researchers discussed HIV risk with adults in 16 communities in rural Kenya and Uganda during population-level testing that took place at health fairs, beaches, trading centers, other community sites, and even in participants’ homes. PrEP was offered to anyone in a relationship with someone living with HIV, to anyone determined to be at elevated risk for infection by a previously validated algorithm, and to anyone who did not fit those criteria but who wanted a prescription.
Of the 15,632 adults eligible for PrEP, 5,447 (35%) chose to start the HIV prevention pill.
A rapid-enrollment protocol meant that people received their prescription at the time of screening or soon after that. Participants underwent testing for HIV antibodies — also out in the community — at weeks 4 and 12, and every 12 weeks thereafter; this will continue out to week 144.
HIV-negative adults who were part of the larger SEARCH cohort in the year before PrEP was made available — and from the same communities — served as the control group.
Interim 60-week data show that the rate of acquisition was 74% lower in the PrEP group than in the control group (incidence rate ratio, 0.26; P = .01). In women, the acquisition rate was 76% lower (incidence rate ratio, 0.24; P = .04), and in men, it was 40% lower (incidence rate ratio, 0.60; P = .54).
The reduction was not significant for men, probably because so few men acquired HIV, Koss reported. The powerful drop in new HIV cases overall was related to PrEP use by women; cases in women fell from 1.52 to 0.40 per 100 person-years.
Blood tests showed that 72% of the people who acquired HIV during the study period had not taken a PrEP pill for at least 30 days before their diagnosis.
“Making PrEP more easily accessible and more community-based could be very powerful in the United States,” said Koss.
“Allowing people to test for HIV and start PrEP outside of health clinics or standard health facilities could help reach more people,” she told Medscape Medical News. “Many of the people who benefit from PrEP may not otherwise need to seek medical care regularly if they’re otherwise healthy and often young.”
When PrEP is made available — easily available — people will pick it up, they will take it away, they will put it in their mouths, and they will not get HIV.
The findings were hailed by others in the field of HIV prevention.
“They’re fantastic,” said Jared Baeten, MD, vice dean of the School of Public Health and professor of global health, medicine, and epidemiology at the University of Washington in Seattle. He was involved in Partners PrEP, a study of PrEP use in mixed-HIV-status couples, the Partners Demonstration Project, and HOPE, a study of the dapivirine ring for HIV prevention.
“These data provide real evidence that when PrEP is made available — easily available — people will pick it up, they will take it away, they will put it in their mouths, and they will not get HIV,” he said in an interview.
Even more, they clarify something that has stymied American regulators and clinicians.
Early studies of PrEP use by single women were stopped because participants weren’t taking the pills; adherence was so low that researchers couldn’t show efficacy. Since then, various trials — including Partners PrEP — have shown that PrEP works in women, but doubts have lingered, leading women to “get the short end of the stick in discussions about PrEP,” Baeten explained.
“There really shouldn’t be questions anymore,” he said. “These findings should put to rest any question about women in Africa being able to benefit from PrEP.”
This article first appeared on Medscape.com.
When people were offered preexposure prophylaxis (PrEP) outside of traditional clinics, regardless of specific risk factors, as part of the Sustainable East Africa Research in Community Health (SEARCH) study, new HIV acquisitions dropped by 74%.
It’s a valuable lesson to providers around the world, said Catherine Koss, MD, assistant professor of medicine in HIV, infectious disease, and global medicine at the University of California, San Francisco.
“We haven’t really seen PrEP being scaled up and offered at such a broad level in communities,” Koss said during the International AIDS Conference 2020.
The first part of SEARCH, which looked at the impact of universal testing and access to HIV treatment immediately after diagnosis, showed that the strategy resulted in a population-wide 30% reduction in new HIV acquisitions. In other words, treatment alone wasn’t enough to end the HIV epidemic.
But the researchers always knew “there were likely going to be new HIV infections,” even with universal HIV testing and treatment, Koss said.
So the second part of the study was designed to see whether PrEP — with the combination of tenofovir disoproxil fumarate plus emtricitabine (Truvada, Gilead Sciences) — could further reduce rates of HIV acquisition.
PrEP out in the community
During the PrEP part of the SEARCH study, researchers discussed HIV risk with adults in 16 communities in rural Kenya and Uganda during population-level testing that took place at health fairs, beaches, trading centers, other community sites, and even in participants’ homes. PrEP was offered to anyone in a relationship with someone living with HIV, to anyone determined to be at elevated risk for infection by a previously validated algorithm, and to anyone who did not fit those criteria but who wanted a prescription.
Of the 15,632 adults eligible for PrEP, 5,447 (35%) chose to start the HIV prevention pill.
A rapid-enrollment protocol meant that people received their prescription at the time of screening or soon after that. Participants underwent testing for HIV antibodies — also out in the community — at weeks 4 and 12, and every 12 weeks thereafter; this will continue out to week 144.
HIV-negative adults who were part of the larger SEARCH cohort in the year before PrEP was made available — and from the same communities — served as the control group.
Interim 60-week data show that the rate of acquisition was 74% lower in the PrEP group than in the control group (incidence rate ratio, 0.26; P = .01). In women, the acquisition rate was 76% lower (incidence rate ratio, 0.24; P = .04), and in men, it was 40% lower (incidence rate ratio, 0.60; P = .54).
The reduction was not significant for men, probably because so few men acquired HIV, Koss reported. The powerful drop in new HIV cases overall was related to PrEP use by women; cases in women fell from 1.52 to 0.40 per 100 person-years.
Blood tests showed that 72% of the people who acquired HIV during the study period had not taken a PrEP pill for at least 30 days before their diagnosis.
“Making PrEP more easily accessible and more community-based could be very powerful in the United States,” said Koss.
“Allowing people to test for HIV and start PrEP outside of health clinics or standard health facilities could help reach more people,” she told Medscape Medical News. “Many of the people who benefit from PrEP may not otherwise need to seek medical care regularly if they’re otherwise healthy and often young.”
When PrEP is made available — easily available — people will pick it up, they will take it away, they will put it in their mouths, and they will not get HIV.
The findings were hailed by others in the field of HIV prevention.
“They’re fantastic,” said Jared Baeten, MD, vice dean of the School of Public Health and professor of global health, medicine, and epidemiology at the University of Washington in Seattle. He was involved in Partners PrEP, a study of PrEP use in mixed-HIV-status couples, the Partners Demonstration Project, and HOPE, a study of the dapivirine ring for HIV prevention.
“These data provide real evidence that when PrEP is made available — easily available — people will pick it up, they will take it away, they will put it in their mouths, and they will not get HIV,” he said in an interview.
Even more, they clarify something that has stymied American regulators and clinicians.
Early studies of PrEP use by single women were stopped because participants weren’t taking the pills; adherence was so low that researchers couldn’t show efficacy. Since then, various trials — including Partners PrEP — have shown that PrEP works in women, but doubts have lingered, leading women to “get the short end of the stick in discussions about PrEP,” Baeten explained.
“There really shouldn’t be questions anymore,” he said. “These findings should put to rest any question about women in Africa being able to benefit from PrEP.”
This article first appeared on Medscape.com.
HSCT or systemic treatment should be offered to HIV+ patients with lymphoma
Systemic or hematopoietic stem cell transplantation (HSCT) treatment of HIV-positive lymphoma patients resulted in improved outcomes, compared with nonsystemic treatment, according to the results of a large database study.
Researchers Thejus T. Jayakrishnan, MD, and colleagues examined patients with lymphoma diagnosed between 2004 and 2015 from the National Cancer Database. Patients were categorized as HIV positive and HIV negative. First-line lymphoma treatment was categorized as no systemic therapy reported, systemic therapy, or HSCT. Multivariate analysis was used to predict treatment and survival, according to Dr. Jayakrishnan, a resident at the department of internal medicine, Allegheny Health Network, Pittsburgh.
A total of 11,160 HIV-positive vs. 349,607 HIV-negative patients were analyzed, including mostly men, with a comorbidity index of 0. The most common lymphoma among HIV-positive patients was diffuse large B-cell lymphoma, according to the report in Clinical Lymphoma, Myeloma & Leukemia.
Among HIV-positive patients, 792 had no systemic treatment, 10,328 underwent systemic treatment, and 40 received HSCT treatment. The results showed that treatment of HIV-positive lymphoma patients resulted in improved outcomes: 3-year overall survival was 43.6% for nonsystemic treatment versus 58.1% for systemic (hazard ratio, 0.56; 95% confidence interval, 0.52-0.61; P < .005) versus 62.2% for HSCT therapy (HR, 0.42; 95% CI, 0.14-1.3; P = .08), the lack of significance in the latter could be caused in part by the small number of patients treated. Outcomes for both treatment regimens were lower, however, compared with non-HIV patients.
“The present study demonstrates improvement in survival outcomes for HIV-positive patients with lymphoma with treatments when feasible, but these outcomes are poor when compared to HIV-negative patients,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Jayakrishnan TT et al. Clin Lymph Myeloma Leuk. 2020 Feb 20. doi: 10.1016/j.clml.2020.06.003.
Systemic or hematopoietic stem cell transplantation (HSCT) treatment of HIV-positive lymphoma patients resulted in improved outcomes, compared with nonsystemic treatment, according to the results of a large database study.
Researchers Thejus T. Jayakrishnan, MD, and colleagues examined patients with lymphoma diagnosed between 2004 and 2015 from the National Cancer Database. Patients were categorized as HIV positive and HIV negative. First-line lymphoma treatment was categorized as no systemic therapy reported, systemic therapy, or HSCT. Multivariate analysis was used to predict treatment and survival, according to Dr. Jayakrishnan, a resident at the department of internal medicine, Allegheny Health Network, Pittsburgh.
A total of 11,160 HIV-positive vs. 349,607 HIV-negative patients were analyzed, including mostly men, with a comorbidity index of 0. The most common lymphoma among HIV-positive patients was diffuse large B-cell lymphoma, according to the report in Clinical Lymphoma, Myeloma & Leukemia.
Among HIV-positive patients, 792 had no systemic treatment, 10,328 underwent systemic treatment, and 40 received HSCT treatment. The results showed that treatment of HIV-positive lymphoma patients resulted in improved outcomes: 3-year overall survival was 43.6% for nonsystemic treatment versus 58.1% for systemic (hazard ratio, 0.56; 95% confidence interval, 0.52-0.61; P < .005) versus 62.2% for HSCT therapy (HR, 0.42; 95% CI, 0.14-1.3; P = .08), the lack of significance in the latter could be caused in part by the small number of patients treated. Outcomes for both treatment regimens were lower, however, compared with non-HIV patients.
“The present study demonstrates improvement in survival outcomes for HIV-positive patients with lymphoma with treatments when feasible, but these outcomes are poor when compared to HIV-negative patients,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Jayakrishnan TT et al. Clin Lymph Myeloma Leuk. 2020 Feb 20. doi: 10.1016/j.clml.2020.06.003.
Systemic or hematopoietic stem cell transplantation (HSCT) treatment of HIV-positive lymphoma patients resulted in improved outcomes, compared with nonsystemic treatment, according to the results of a large database study.
Researchers Thejus T. Jayakrishnan, MD, and colleagues examined patients with lymphoma diagnosed between 2004 and 2015 from the National Cancer Database. Patients were categorized as HIV positive and HIV negative. First-line lymphoma treatment was categorized as no systemic therapy reported, systemic therapy, or HSCT. Multivariate analysis was used to predict treatment and survival, according to Dr. Jayakrishnan, a resident at the department of internal medicine, Allegheny Health Network, Pittsburgh.
A total of 11,160 HIV-positive vs. 349,607 HIV-negative patients were analyzed, including mostly men, with a comorbidity index of 0. The most common lymphoma among HIV-positive patients was diffuse large B-cell lymphoma, according to the report in Clinical Lymphoma, Myeloma & Leukemia.
Among HIV-positive patients, 792 had no systemic treatment, 10,328 underwent systemic treatment, and 40 received HSCT treatment. The results showed that treatment of HIV-positive lymphoma patients resulted in improved outcomes: 3-year overall survival was 43.6% for nonsystemic treatment versus 58.1% for systemic (hazard ratio, 0.56; 95% confidence interval, 0.52-0.61; P < .005) versus 62.2% for HSCT therapy (HR, 0.42; 95% CI, 0.14-1.3; P = .08), the lack of significance in the latter could be caused in part by the small number of patients treated. Outcomes for both treatment regimens were lower, however, compared with non-HIV patients.
“The present study demonstrates improvement in survival outcomes for HIV-positive patients with lymphoma with treatments when feasible, but these outcomes are poor when compared to HIV-negative patients,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Jayakrishnan TT et al. Clin Lymph Myeloma Leuk. 2020 Feb 20. doi: 10.1016/j.clml.2020.06.003.
FROM CLINICAL LYMPHOMA, MYELOMA & LEUKEMIA
Injection beats pill for long-lasting HIV prevention
Injections of cabotegravir (ViiV Healthcare) given every other month are more effective in blocking HIV transmission than is the once-a-day combination of tenofovir disoproxil fumarate and emtricitabine (Truvada, Gilead Science), new data from the HPTN 083 trial show.
The findings “could transform the HIV prevention landscape for so many people,” said Megan Coleman, DNP, from Whitman-Walker Health in Washington, DC, who regularly prescribes Truvada as pre-exposure prophylaxis (PrEP).
At Whitman-Walker alone, about 3000 people were taking the pill in early 2020, but “for some people, taking a pill every day just isn’t a viable option,” said Coleman. “To have something that can support a patient’s choice and a patient’s ability to reduce their own risk of HIV is amazing.”
Final results from the trial — which looked at the drug in cisgender men and transgender women who have sex with men — were presented at the International AIDS Conference 2020.
Early Study Termination
Half of the 4566 study participants — from 43 sites in Africa, Asia, Latin America, and the United States — were younger than 30 years, 12.4% were transgender women, 29.7% were black, and 46.1% were Hispanic.
By design, ViiV Healthcare, the study sponsor, required that 50% of American participants be black to reflect the population at risk for HIV in the United States, said Raphael Landovitz, MD, from the UCLA David Geffen School of Medicine in Los Angeles, who is protocol chair for HPTN 083. In fact, 49.7% of the American cohort was black and 17.8% was Hispanic.
Patients randomized to the cabotegravir group received daily oral cabotegravir plus daily oral placebo for 5 weeks, to assess safety, followed by a cabotegravir injection at weeks 5 and 9 and every 2 months thereafter out to week 153 plus daily oral placebo. Patients randomized to the Truvada group received daily oral Truvada plus daily oral placebo for 5 weeks, followed by daily oral Truvada plus placebo injection, on the same schedule, out to week 153.
After the final injection, all participants continued on daily oral Truvada for 48 weeks.
The researchers expected to wait until 172 participants acquired HIV; they decided at the outset that this number would be sufficient to power a decision on whether or not cabotegravir injections are better than daily oral Truvada. But by May 2020, when 52 of the study participants had acquired HIV, the results were so lopsided in favor of cabotegravir that the trial was stopped. At that point, all participants were offered cabotegravir injections every 2 months.
Thirty-nine of the 52 (75%) new HIV infections occurred in the Truvada group. In fact, (hazard ratio, 0.34).
“This definitively establishes the superiority of cabotegravir,” said Landovitz.
He and his colleagues had been legitimately concerned that HIV acquisition would be so low in the trial that they wouldn’t be able to show how effective the injectable was. The success of Truvada PrEP has made it difficult to design prevention trials.
“We know that Truvada works extremely well, so the fact that we were able to show that cabotegravir in this population works better” is a powerful observation, said Landovitz. This is especially true because the rates of sexually transmitted infections — which are thought to increase risk for HIV transmission — were so high. Overall, 16.5% of the participants tested positive for syphilis during the trial, 13.3% tested positive for gonorrhea, and 21.1% tested positive for Chlamydia.
Five Surprising Seroconversions
Eleven of the 15 HIV infections in the cabotegravir group occurred in people who had received at least one injection. Three of these infections actually occurred during the first 5 weeks of the study when participants were taking oral cabotegravir, two occurred when participants chose to discontinue the injection and return to daily oral Truvada, and one occurred after a participant missed the injection for a prolonged period of time.
But five of the transmissions occurred in participants who appeared to be perfectly adherent.
Landovitz offered a number of possible reasons for this surprising finding.
“Number one could be that there’s something about these five particular individuals such that they grind up and eliminate the cabotegravir faster than other people, so an 8-week interval is too long for them,” he explained. “Another possibility, although pretty rare, is that there is a rare circulating virus that is intrinsically resistant to cabotegravir.”
Breakthrough HIV transmissions have been rare in people taking oral PrEP.
Disruptions caused by the COVID-19 pandemic have meant that the researchers don’t yet have the data on drug-resistant mutations or drug levels for these five participants, but they will.
“I suspect the truth is that there will never be a 100% failsafe HIV prevention mechanism,” said Landovitz.
“Impressive” Findings
The findings were greeted with excitement, although questions remain.
They are “impressive,” especially the data on black and Hispanic participants, said Paul Sax, MD, medical director of the Division of Infectious Diseases at Brigham and Women’s Hospital in Boston.
However, he said he is interested in the data showing that although participants in both groups gained weight during the study, there was early weight loss in the Truvada group, meaning that those in the cabotegravir group weighed more at the end of the study than those in the Truvada group.
“I’ve been watching the data on weight with integrase inhibitors,” he explained, including weight data specific to Truvada and to the combination of emtricitabine and tenofovir alafenamide (Descovy, Gilead). It looks like Truvada “has some sort of weight-suppressive effects. That’s going to be a thing we’re going to have to watch.”
Coleman said she is already thinking about patients at Whitman-Walker who might do well on cabotegravir and those who can start PrEP for the first time with this option.
“Not only would people probably switch to this option, but maybe people would be interested in starting a biomedical prevention approach that isn’t a pill every day,” she said. “It’s just exciting to have another option. Hopefully, in a few years, we’ll have implantable devices and rings; I can’t even imagine what all those brilliant minds are coming up with.”
But that’s still a ways off. First, cabotegravir has yet to be approved for HIV prevention, and ideally, eventually, there will be a way to determine if cabotegravir is safe for each patient that doesn’t involve a month of daily pills.
“We need to solve that problem because it’s so complicated to do an oral lead-in for a month or so,” said Carl Dieffenbach, PhD, director of the Division of AIDS at the National Institute of Allergy and Infectious Diseases, National Institutes of Health. “Otherwise it’s not going to be feasible.”
We need to make sure this gets licensed for men and women and transgender individuals.
Even with these positive data, Dieffenbach and other officials are not keen to have ViiV apply for licensing right away. Last October, Descovy was the second oral PrEP pill approved for HIV prevention, but only for use by gay men and transgender women — it hadn’t been well studied in cisgender women — causing an outcry. Now, officials are suggesting that ViiV not make the same mistake.
They are urging the company to hold off until data from the sister study of the medication in women — HPTN 084 — is completed in 2022.
“We need to make sure this gets licensed for men and women and transgender individuals,” Dieffenbach told Medscape Medical News. “We just need to give this a little more time and then build a plan with contingencies, so that if something happens, we still have collected all the safety data in women so we can say it’s safe.”
ViiV seems to be making such a plan.
“Our goal is to seek approval across all genders and we will work with the FDA and other regulatory agencies to map out a plan to achieve this goal,” said Kimberly Smith, MD, head of research and development at ViiV Healthcare.
The World Health Organization (WHO), meanwhile, doesn’t expect to change its guidelines on HIV prevention medications until data from HPTN 084 are reported.
“What’s important when we look at guidelines is that we also look across populations,” said Meg Doherty, coordinator of treatment and care in the Department of HIV/AIDS at WHO. “We’re waiting to know more about how cabotegravir works in women, because we certainly want to have prevention drugs that can be used in men and women at different age ranges and, ideally, during pregnancy.”
International AIDS Conference 2020: Abstracts OAXLB01. Presented July 8, 2020.
This article first appeared on Medscape.com.
Injections of cabotegravir (ViiV Healthcare) given every other month are more effective in blocking HIV transmission than is the once-a-day combination of tenofovir disoproxil fumarate and emtricitabine (Truvada, Gilead Science), new data from the HPTN 083 trial show.
The findings “could transform the HIV prevention landscape for so many people,” said Megan Coleman, DNP, from Whitman-Walker Health in Washington, DC, who regularly prescribes Truvada as pre-exposure prophylaxis (PrEP).
At Whitman-Walker alone, about 3000 people were taking the pill in early 2020, but “for some people, taking a pill every day just isn’t a viable option,” said Coleman. “To have something that can support a patient’s choice and a patient’s ability to reduce their own risk of HIV is amazing.”
Final results from the trial — which looked at the drug in cisgender men and transgender women who have sex with men — were presented at the International AIDS Conference 2020.
Early Study Termination
Half of the 4566 study participants — from 43 sites in Africa, Asia, Latin America, and the United States — were younger than 30 years, 12.4% were transgender women, 29.7% were black, and 46.1% were Hispanic.
By design, ViiV Healthcare, the study sponsor, required that 50% of American participants be black to reflect the population at risk for HIV in the United States, said Raphael Landovitz, MD, from the UCLA David Geffen School of Medicine in Los Angeles, who is protocol chair for HPTN 083. In fact, 49.7% of the American cohort was black and 17.8% was Hispanic.
Patients randomized to the cabotegravir group received daily oral cabotegravir plus daily oral placebo for 5 weeks, to assess safety, followed by a cabotegravir injection at weeks 5 and 9 and every 2 months thereafter out to week 153 plus daily oral placebo. Patients randomized to the Truvada group received daily oral Truvada plus daily oral placebo for 5 weeks, followed by daily oral Truvada plus placebo injection, on the same schedule, out to week 153.
After the final injection, all participants continued on daily oral Truvada for 48 weeks.
The researchers expected to wait until 172 participants acquired HIV; they decided at the outset that this number would be sufficient to power a decision on whether or not cabotegravir injections are better than daily oral Truvada. But by May 2020, when 52 of the study participants had acquired HIV, the results were so lopsided in favor of cabotegravir that the trial was stopped. At that point, all participants were offered cabotegravir injections every 2 months.
Thirty-nine of the 52 (75%) new HIV infections occurred in the Truvada group. In fact, (hazard ratio, 0.34).
“This definitively establishes the superiority of cabotegravir,” said Landovitz.
He and his colleagues had been legitimately concerned that HIV acquisition would be so low in the trial that they wouldn’t be able to show how effective the injectable was. The success of Truvada PrEP has made it difficult to design prevention trials.
“We know that Truvada works extremely well, so the fact that we were able to show that cabotegravir in this population works better” is a powerful observation, said Landovitz. This is especially true because the rates of sexually transmitted infections — which are thought to increase risk for HIV transmission — were so high. Overall, 16.5% of the participants tested positive for syphilis during the trial, 13.3% tested positive for gonorrhea, and 21.1% tested positive for Chlamydia.
Five Surprising Seroconversions
Eleven of the 15 HIV infections in the cabotegravir group occurred in people who had received at least one injection. Three of these infections actually occurred during the first 5 weeks of the study when participants were taking oral cabotegravir, two occurred when participants chose to discontinue the injection and return to daily oral Truvada, and one occurred after a participant missed the injection for a prolonged period of time.
But five of the transmissions occurred in participants who appeared to be perfectly adherent.
Landovitz offered a number of possible reasons for this surprising finding.
“Number one could be that there’s something about these five particular individuals such that they grind up and eliminate the cabotegravir faster than other people, so an 8-week interval is too long for them,” he explained. “Another possibility, although pretty rare, is that there is a rare circulating virus that is intrinsically resistant to cabotegravir.”
Breakthrough HIV transmissions have been rare in people taking oral PrEP.
Disruptions caused by the COVID-19 pandemic have meant that the researchers don’t yet have the data on drug-resistant mutations or drug levels for these five participants, but they will.
“I suspect the truth is that there will never be a 100% failsafe HIV prevention mechanism,” said Landovitz.
“Impressive” Findings
The findings were greeted with excitement, although questions remain.
They are “impressive,” especially the data on black and Hispanic participants, said Paul Sax, MD, medical director of the Division of Infectious Diseases at Brigham and Women’s Hospital in Boston.
However, he said he is interested in the data showing that although participants in both groups gained weight during the study, there was early weight loss in the Truvada group, meaning that those in the cabotegravir group weighed more at the end of the study than those in the Truvada group.
“I’ve been watching the data on weight with integrase inhibitors,” he explained, including weight data specific to Truvada and to the combination of emtricitabine and tenofovir alafenamide (Descovy, Gilead). It looks like Truvada “has some sort of weight-suppressive effects. That’s going to be a thing we’re going to have to watch.”
Coleman said she is already thinking about patients at Whitman-Walker who might do well on cabotegravir and those who can start PrEP for the first time with this option.
“Not only would people probably switch to this option, but maybe people would be interested in starting a biomedical prevention approach that isn’t a pill every day,” she said. “It’s just exciting to have another option. Hopefully, in a few years, we’ll have implantable devices and rings; I can’t even imagine what all those brilliant minds are coming up with.”
But that’s still a ways off. First, cabotegravir has yet to be approved for HIV prevention, and ideally, eventually, there will be a way to determine if cabotegravir is safe for each patient that doesn’t involve a month of daily pills.
“We need to solve that problem because it’s so complicated to do an oral lead-in for a month or so,” said Carl Dieffenbach, PhD, director of the Division of AIDS at the National Institute of Allergy and Infectious Diseases, National Institutes of Health. “Otherwise it’s not going to be feasible.”
We need to make sure this gets licensed for men and women and transgender individuals.
Even with these positive data, Dieffenbach and other officials are not keen to have ViiV apply for licensing right away. Last October, Descovy was the second oral PrEP pill approved for HIV prevention, but only for use by gay men and transgender women — it hadn’t been well studied in cisgender women — causing an outcry. Now, officials are suggesting that ViiV not make the same mistake.
They are urging the company to hold off until data from the sister study of the medication in women — HPTN 084 — is completed in 2022.
“We need to make sure this gets licensed for men and women and transgender individuals,” Dieffenbach told Medscape Medical News. “We just need to give this a little more time and then build a plan with contingencies, so that if something happens, we still have collected all the safety data in women so we can say it’s safe.”
ViiV seems to be making such a plan.
“Our goal is to seek approval across all genders and we will work with the FDA and other regulatory agencies to map out a plan to achieve this goal,” said Kimberly Smith, MD, head of research and development at ViiV Healthcare.
The World Health Organization (WHO), meanwhile, doesn’t expect to change its guidelines on HIV prevention medications until data from HPTN 084 are reported.
“What’s important when we look at guidelines is that we also look across populations,” said Meg Doherty, coordinator of treatment and care in the Department of HIV/AIDS at WHO. “We’re waiting to know more about how cabotegravir works in women, because we certainly want to have prevention drugs that can be used in men and women at different age ranges and, ideally, during pregnancy.”
International AIDS Conference 2020: Abstracts OAXLB01. Presented July 8, 2020.
This article first appeared on Medscape.com.
Injections of cabotegravir (ViiV Healthcare) given every other month are more effective in blocking HIV transmission than is the once-a-day combination of tenofovir disoproxil fumarate and emtricitabine (Truvada, Gilead Science), new data from the HPTN 083 trial show.
The findings “could transform the HIV prevention landscape for so many people,” said Megan Coleman, DNP, from Whitman-Walker Health in Washington, DC, who regularly prescribes Truvada as pre-exposure prophylaxis (PrEP).
At Whitman-Walker alone, about 3000 people were taking the pill in early 2020, but “for some people, taking a pill every day just isn’t a viable option,” said Coleman. “To have something that can support a patient’s choice and a patient’s ability to reduce their own risk of HIV is amazing.”
Final results from the trial — which looked at the drug in cisgender men and transgender women who have sex with men — were presented at the International AIDS Conference 2020.
Early Study Termination
Half of the 4566 study participants — from 43 sites in Africa, Asia, Latin America, and the United States — were younger than 30 years, 12.4% were transgender women, 29.7% were black, and 46.1% were Hispanic.
By design, ViiV Healthcare, the study sponsor, required that 50% of American participants be black to reflect the population at risk for HIV in the United States, said Raphael Landovitz, MD, from the UCLA David Geffen School of Medicine in Los Angeles, who is protocol chair for HPTN 083. In fact, 49.7% of the American cohort was black and 17.8% was Hispanic.
Patients randomized to the cabotegravir group received daily oral cabotegravir plus daily oral placebo for 5 weeks, to assess safety, followed by a cabotegravir injection at weeks 5 and 9 and every 2 months thereafter out to week 153 plus daily oral placebo. Patients randomized to the Truvada group received daily oral Truvada plus daily oral placebo for 5 weeks, followed by daily oral Truvada plus placebo injection, on the same schedule, out to week 153.
After the final injection, all participants continued on daily oral Truvada for 48 weeks.
The researchers expected to wait until 172 participants acquired HIV; they decided at the outset that this number would be sufficient to power a decision on whether or not cabotegravir injections are better than daily oral Truvada. But by May 2020, when 52 of the study participants had acquired HIV, the results were so lopsided in favor of cabotegravir that the trial was stopped. At that point, all participants were offered cabotegravir injections every 2 months.
Thirty-nine of the 52 (75%) new HIV infections occurred in the Truvada group. In fact, (hazard ratio, 0.34).
“This definitively establishes the superiority of cabotegravir,” said Landovitz.
He and his colleagues had been legitimately concerned that HIV acquisition would be so low in the trial that they wouldn’t be able to show how effective the injectable was. The success of Truvada PrEP has made it difficult to design prevention trials.
“We know that Truvada works extremely well, so the fact that we were able to show that cabotegravir in this population works better” is a powerful observation, said Landovitz. This is especially true because the rates of sexually transmitted infections — which are thought to increase risk for HIV transmission — were so high. Overall, 16.5% of the participants tested positive for syphilis during the trial, 13.3% tested positive for gonorrhea, and 21.1% tested positive for Chlamydia.
Five Surprising Seroconversions
Eleven of the 15 HIV infections in the cabotegravir group occurred in people who had received at least one injection. Three of these infections actually occurred during the first 5 weeks of the study when participants were taking oral cabotegravir, two occurred when participants chose to discontinue the injection and return to daily oral Truvada, and one occurred after a participant missed the injection for a prolonged period of time.
But five of the transmissions occurred in participants who appeared to be perfectly adherent.
Landovitz offered a number of possible reasons for this surprising finding.
“Number one could be that there’s something about these five particular individuals such that they grind up and eliminate the cabotegravir faster than other people, so an 8-week interval is too long for them,” he explained. “Another possibility, although pretty rare, is that there is a rare circulating virus that is intrinsically resistant to cabotegravir.”
Breakthrough HIV transmissions have been rare in people taking oral PrEP.
Disruptions caused by the COVID-19 pandemic have meant that the researchers don’t yet have the data on drug-resistant mutations or drug levels for these five participants, but they will.
“I suspect the truth is that there will never be a 100% failsafe HIV prevention mechanism,” said Landovitz.
“Impressive” Findings
The findings were greeted with excitement, although questions remain.
They are “impressive,” especially the data on black and Hispanic participants, said Paul Sax, MD, medical director of the Division of Infectious Diseases at Brigham and Women’s Hospital in Boston.
However, he said he is interested in the data showing that although participants in both groups gained weight during the study, there was early weight loss in the Truvada group, meaning that those in the cabotegravir group weighed more at the end of the study than those in the Truvada group.
“I’ve been watching the data on weight with integrase inhibitors,” he explained, including weight data specific to Truvada and to the combination of emtricitabine and tenofovir alafenamide (Descovy, Gilead). It looks like Truvada “has some sort of weight-suppressive effects. That’s going to be a thing we’re going to have to watch.”
Coleman said she is already thinking about patients at Whitman-Walker who might do well on cabotegravir and those who can start PrEP for the first time with this option.
“Not only would people probably switch to this option, but maybe people would be interested in starting a biomedical prevention approach that isn’t a pill every day,” she said. “It’s just exciting to have another option. Hopefully, in a few years, we’ll have implantable devices and rings; I can’t even imagine what all those brilliant minds are coming up with.”
But that’s still a ways off. First, cabotegravir has yet to be approved for HIV prevention, and ideally, eventually, there will be a way to determine if cabotegravir is safe for each patient that doesn’t involve a month of daily pills.
“We need to solve that problem because it’s so complicated to do an oral lead-in for a month or so,” said Carl Dieffenbach, PhD, director of the Division of AIDS at the National Institute of Allergy and Infectious Diseases, National Institutes of Health. “Otherwise it’s not going to be feasible.”
We need to make sure this gets licensed for men and women and transgender individuals.
Even with these positive data, Dieffenbach and other officials are not keen to have ViiV apply for licensing right away. Last October, Descovy was the second oral PrEP pill approved for HIV prevention, but only for use by gay men and transgender women — it hadn’t been well studied in cisgender women — causing an outcry. Now, officials are suggesting that ViiV not make the same mistake.
They are urging the company to hold off until data from the sister study of the medication in women — HPTN 084 — is completed in 2022.
“We need to make sure this gets licensed for men and women and transgender individuals,” Dieffenbach told Medscape Medical News. “We just need to give this a little more time and then build a plan with contingencies, so that if something happens, we still have collected all the safety data in women so we can say it’s safe.”
ViiV seems to be making such a plan.
“Our goal is to seek approval across all genders and we will work with the FDA and other regulatory agencies to map out a plan to achieve this goal,” said Kimberly Smith, MD, head of research and development at ViiV Healthcare.
The World Health Organization (WHO), meanwhile, doesn’t expect to change its guidelines on HIV prevention medications until data from HPTN 084 are reported.
“What’s important when we look at guidelines is that we also look across populations,” said Meg Doherty, coordinator of treatment and care in the Department of HIV/AIDS at WHO. “We’re waiting to know more about how cabotegravir works in women, because we certainly want to have prevention drugs that can be used in men and women at different age ranges and, ideally, during pregnancy.”
International AIDS Conference 2020: Abstracts OAXLB01. Presented July 8, 2020.
This article first appeared on Medscape.com.
Neural tube defect risk from dolutegravir drops as clinical experience grows
The newest data, based on 3,591 deliveries among women in Botswana infected by HIV and treated with dolutegravir at the time of conception during a little more than 5.5 years through April 2020, showed that dolutegravir use at conception linked with 7 cases of neonatal neural tube defects (NTDs), a 0.19% rate that exceeded comparator rates by about 1 in every 1,000 deliveries, far below the 0.94% rate initially found and that raised a red flag 2 years ago (New Engl J Med. 2018 Sep 6;379[10]:979-81). “The prevalence of NTDs among infants born to women on dolutegravir at conception may be stabilizing at approximately 2 per 1,000,” said Rebecca Zash, MD, during the virtual meeting of the International AIDS conference.
“This small absolute risk for neural tube defects is far outweighed by the potential benefits from dolutegravir” for better tolerability than alternative drugs and fewer drug-drug interactions. “This should allow for broader use of dolutegravir in women,” added Dr. Zash, an HIV specialist at Beth Israel Deaconess Medical Center and codirector of the Placental Scientific Working Group of the Harvard University Center for AIDS Research, both in Boston.
“What this has taught us is that women are not a niche population” of people infected with HIV, but rather constitute about half of HIV patients worldwide. “Maintaining gender equity in HIV treatment requires safety data for treatments during pregnancy,” she said during a press briefing.
The new findings mean that it’s “time to lay to rest” concerns about neural tube defects (NTDs) in infants born to women treated with dolutegravir, “given the incredible benefits of dolutegravir,” commented Monica Gandhi, MD, professor of medicine and associate chief of the division of HIV, infectious disease, and global medicine at the University of California, San Francisco. Another benefit from removing any caveats about use of dolutegravir in women who could become pregnant is that it would simplify treatment recommendations and make dolutegravir the unqualified first-line agent for treating HIV infection, Dr. Gandhi said during the briefing. “It’s super reassuring to have these data, as the incidence of NTDs goes down and down,” she added.
Following the alarm raised by initial findings from the Tsepamo study in 2018, Dr. Zash and associates first updated their data through March 2019, when they reported a revised cumulative NTD incidence rate of 0.3% (New Engl J Med. 2019 Aug 29;381[9]:827-40). The Tsepamo study began by following the pregnancy outcomes of women at eight Botswana sites during August 2014–July 2018, representing 45% of the country’s deliveries. This expanded to 18 sites and 72% of deliveries during July-September 2018, and then starting in September 2019 the scope slightly reduced to 16 Botswana sites with 70% of the nation’s deliveries.
Folate supplementation to women who might conceive is vital, but remains spotty in Botswana. “Folate supplementation is a no-brainer, but has had really slow adoption in many countries,” Dr. Zash said. “Folate supplementation, especially in food so that everyone gets it, will reduce NTDs by half.” The two most recent cases of infants born with a NTD to mothers who had been on dolutegravir at conception occurred in mothers who had received no folate supplementation, Dr. Zash reported.
The most recent HIV treatment guidelines for adults from the Department of Health & Human Services, which date from late 2019, designated dolutegravir plus lamivudine as a first-line regimen for most, but flagged it as an “alternative” antiretroviral drug when treating women who have childbearing potential and are either trying to conceive or are sexually active but not using contraception.
The study had no commercial funding. Dr. Zash has been a researcher in studies funded by CytoDyn, Fulcrum, and Gilead. Dr. Gandhi had no commercial disclosures.
The newest data, based on 3,591 deliveries among women in Botswana infected by HIV and treated with dolutegravir at the time of conception during a little more than 5.5 years through April 2020, showed that dolutegravir use at conception linked with 7 cases of neonatal neural tube defects (NTDs), a 0.19% rate that exceeded comparator rates by about 1 in every 1,000 deliveries, far below the 0.94% rate initially found and that raised a red flag 2 years ago (New Engl J Med. 2018 Sep 6;379[10]:979-81). “The prevalence of NTDs among infants born to women on dolutegravir at conception may be stabilizing at approximately 2 per 1,000,” said Rebecca Zash, MD, during the virtual meeting of the International AIDS conference.
“This small absolute risk for neural tube defects is far outweighed by the potential benefits from dolutegravir” for better tolerability than alternative drugs and fewer drug-drug interactions. “This should allow for broader use of dolutegravir in women,” added Dr. Zash, an HIV specialist at Beth Israel Deaconess Medical Center and codirector of the Placental Scientific Working Group of the Harvard University Center for AIDS Research, both in Boston.
“What this has taught us is that women are not a niche population” of people infected with HIV, but rather constitute about half of HIV patients worldwide. “Maintaining gender equity in HIV treatment requires safety data for treatments during pregnancy,” she said during a press briefing.
The new findings mean that it’s “time to lay to rest” concerns about neural tube defects (NTDs) in infants born to women treated with dolutegravir, “given the incredible benefits of dolutegravir,” commented Monica Gandhi, MD, professor of medicine and associate chief of the division of HIV, infectious disease, and global medicine at the University of California, San Francisco. Another benefit from removing any caveats about use of dolutegravir in women who could become pregnant is that it would simplify treatment recommendations and make dolutegravir the unqualified first-line agent for treating HIV infection, Dr. Gandhi said during the briefing. “It’s super reassuring to have these data, as the incidence of NTDs goes down and down,” she added.
Following the alarm raised by initial findings from the Tsepamo study in 2018, Dr. Zash and associates first updated their data through March 2019, when they reported a revised cumulative NTD incidence rate of 0.3% (New Engl J Med. 2019 Aug 29;381[9]:827-40). The Tsepamo study began by following the pregnancy outcomes of women at eight Botswana sites during August 2014–July 2018, representing 45% of the country’s deliveries. This expanded to 18 sites and 72% of deliveries during July-September 2018, and then starting in September 2019 the scope slightly reduced to 16 Botswana sites with 70% of the nation’s deliveries.
Folate supplementation to women who might conceive is vital, but remains spotty in Botswana. “Folate supplementation is a no-brainer, but has had really slow adoption in many countries,” Dr. Zash said. “Folate supplementation, especially in food so that everyone gets it, will reduce NTDs by half.” The two most recent cases of infants born with a NTD to mothers who had been on dolutegravir at conception occurred in mothers who had received no folate supplementation, Dr. Zash reported.
The most recent HIV treatment guidelines for adults from the Department of Health & Human Services, which date from late 2019, designated dolutegravir plus lamivudine as a first-line regimen for most, but flagged it as an “alternative” antiretroviral drug when treating women who have childbearing potential and are either trying to conceive or are sexually active but not using contraception.
The study had no commercial funding. Dr. Zash has been a researcher in studies funded by CytoDyn, Fulcrum, and Gilead. Dr. Gandhi had no commercial disclosures.
The newest data, based on 3,591 deliveries among women in Botswana infected by HIV and treated with dolutegravir at the time of conception during a little more than 5.5 years through April 2020, showed that dolutegravir use at conception linked with 7 cases of neonatal neural tube defects (NTDs), a 0.19% rate that exceeded comparator rates by about 1 in every 1,000 deliveries, far below the 0.94% rate initially found and that raised a red flag 2 years ago (New Engl J Med. 2018 Sep 6;379[10]:979-81). “The prevalence of NTDs among infants born to women on dolutegravir at conception may be stabilizing at approximately 2 per 1,000,” said Rebecca Zash, MD, during the virtual meeting of the International AIDS conference.
“This small absolute risk for neural tube defects is far outweighed by the potential benefits from dolutegravir” for better tolerability than alternative drugs and fewer drug-drug interactions. “This should allow for broader use of dolutegravir in women,” added Dr. Zash, an HIV specialist at Beth Israel Deaconess Medical Center and codirector of the Placental Scientific Working Group of the Harvard University Center for AIDS Research, both in Boston.
“What this has taught us is that women are not a niche population” of people infected with HIV, but rather constitute about half of HIV patients worldwide. “Maintaining gender equity in HIV treatment requires safety data for treatments during pregnancy,” she said during a press briefing.
The new findings mean that it’s “time to lay to rest” concerns about neural tube defects (NTDs) in infants born to women treated with dolutegravir, “given the incredible benefits of dolutegravir,” commented Monica Gandhi, MD, professor of medicine and associate chief of the division of HIV, infectious disease, and global medicine at the University of California, San Francisco. Another benefit from removing any caveats about use of dolutegravir in women who could become pregnant is that it would simplify treatment recommendations and make dolutegravir the unqualified first-line agent for treating HIV infection, Dr. Gandhi said during the briefing. “It’s super reassuring to have these data, as the incidence of NTDs goes down and down,” she added.
Following the alarm raised by initial findings from the Tsepamo study in 2018, Dr. Zash and associates first updated their data through March 2019, when they reported a revised cumulative NTD incidence rate of 0.3% (New Engl J Med. 2019 Aug 29;381[9]:827-40). The Tsepamo study began by following the pregnancy outcomes of women at eight Botswana sites during August 2014–July 2018, representing 45% of the country’s deliveries. This expanded to 18 sites and 72% of deliveries during July-September 2018, and then starting in September 2019 the scope slightly reduced to 16 Botswana sites with 70% of the nation’s deliveries.
Folate supplementation to women who might conceive is vital, but remains spotty in Botswana. “Folate supplementation is a no-brainer, but has had really slow adoption in many countries,” Dr. Zash said. “Folate supplementation, especially in food so that everyone gets it, will reduce NTDs by half.” The two most recent cases of infants born with a NTD to mothers who had been on dolutegravir at conception occurred in mothers who had received no folate supplementation, Dr. Zash reported.
The most recent HIV treatment guidelines for adults from the Department of Health & Human Services, which date from late 2019, designated dolutegravir plus lamivudine as a first-line regimen for most, but flagged it as an “alternative” antiretroviral drug when treating women who have childbearing potential and are either trying to conceive or are sexually active but not using contraception.
The study had no commercial funding. Dr. Zash has been a researcher in studies funded by CytoDyn, Fulcrum, and Gilead. Dr. Gandhi had no commercial disclosures.
FROM AIDS 2020
Brazilian patient in HIV remission, negative antibody test
A 35-year-old Brazilian man who participated in a trial in which he received an intensified antiretroviral regimen plus supplemental vitamin B3 for 48 weeks has joined the short list of patients who have experienced a period of remission from HIV in the absence of effective treatment.
Along with the Mississippi baby, a San Francisco man, a 24-year-old Thai man, a 9-year-old South African child, and the London and Berlin patients, the Brazilian man has an undetectable viral load and, more than a year after stopping treatment, his HIV antibody test is negative.
But as with the Berlin and London patients, it seems unlikely that – even if the man remains HIV free into the future – the circumstances of his remission will be broadly applicable to other people with HIV, said Carl Dieffenbach, PhD, director of the Division of AIDS at the National Institute of Allergy and Infectious Diseases, National Institutes of Health.
“I don’t think it’s replicable,” Dieffenbach told Medscape Medical News. Researchers should still try to confirm the finding, but they will probably learn more by studying the man’s unique genetic characteristics and immune system “than to go out and treat another 200 people with the same protocol.”
‘Shock-and-kill strategy’
The man had been on treatment since his HIV diagnosis in 2012, and was one of 30 people to enroll in a Brazilian study – the Multi Interventional Study Exploring HIV-1 Residual Replication: A Step Toward HIV Eradication and Sterilizing Cure – in 2016. At that point, his regimen consisted of the combination of efavirenz, lamivudine, and tenofovir disoproxil fumarate (Symfi, Mylan Pharmaceuticals) and his viral load was undetectable.
He was one of five people in the study to be randomized to receive the integrase inhibitor dolutegravir (Tivicay, ViiV Healthcare), the CCR5 receptor inhibitor maraviroc (Selzentry, ViiV Healthcare), and twice-daily nicotinamide 500 mg, a form of vitamin B3, in addition to his regular regimen for 48 weeks.
Nicotinamide has been used for decades because of its anti-infective properties, particularly in tuberculosis. In vitro, it also works to reverse HIV latency, said study investigator Ricardo Diaz, MD, from the Federal University of São Paulo, who presented the data at a press conference for the International AIDS Conference (AIDS) 2020.
“This is a shock-and-kill strategy,” said Leila Giron, PhD, from the Wistar Institute in Philadelphia, who was one of the study investigators. “We did in vitro studies to make sure nicotinamide took HIV out of the cells.”
“The cell machinery changed a lot,” she told Medscape Medical News. “And because it’s a B vitamin, all five participants didn’t have any side effects.”
But the patient was the only person in his treatment group to experience viral load “blips” during treatment – at weeks 16 and 24. And viral DNA was present at low levels in his peripheral blood spots and rectal tissue at baseline and at 48 weeks, and his HIV antibodies dropped from 91.8 RLU at baseline to 58.0 RLU at week 48.
“He had a decline in cell activation, inflammation, and a very deep decline in antibody titers,” Diaz reported.
After 48 weeks of the intensified treatment, the patient returned to his usual regimen for 3 years. Then, in March 2019, he agreed to try an analytical treatment interruption and discontinued all HIV treatment.
“What’s interesting is right before the analytical treatment interruption, the HIV DNA sequences were completely negative,” said Diaz.
Every 3 weeks for the next 64.7 weeks, his viral load came back undetectable, and so did HIV DNA in blood spots. One thing did change, though: in February 2020, the man’s HIV antibody test came back negative.
The team checked that he wasn’t still taking his antiretroviral medication, which might have explained the undetectable viral load, and he wasn’t.
Surprise, skepticism, and hope
The results have prompted surprise, skepticism, and questions from clinicians and researchers.
said Anton Pozniak, MD, from Chelsea and Westminster Hospital in London, who is cochair of AIDS 2020.
“They need a bigger study to see whether or not [the participant] is one of these guys who stopped treatment and might take a year or two, or four, to rebound,” he said. But if other studies replicate the results, the control of HIV in “one in five people would still be huge.”
The rationale behind treatment intensification for HIV remission is that “the three-drug ART regimen was perhaps insufficient to completely block HIV replication” in the reservoirs, even though that replication could be happening below levels detectable with current tests, said Laura Persaud, MD, from the Johns Hopkins University School of Medicine in Baltimore, who is chair of the International Maternal Pediatric Adolescent AIDS Clinical Trial Network (IMPAACT) HIV Cure Committee and was not involved in the study.
“The idea was to see if you could accelerate the decay of the reservoir” if you added medications that targeted different parts of the HIV lifecycle. Symfi, for instance, targets just one step in the viral replication process: the point where HIV RNA reverse transcribes itself into DNA so it can integrate into immune cells. But CCR5 inhibitors block entry of HIV into the cell in the first place, and integrase inhibitors, like raltegravir (Isentress, Merck) and dolutegravir, prevent HIV DNA from integrating into the host chromosome after it has reverse transcribed itself.
Still, recent data suggest that treatment intensification might not be as effective as hypothesized, she said. And the nicotinamide study was in vitro. To what extent this is a direct result of this treatment strategy is unclear.
“It’s hard to believe, in this small study, that this agent [nicotinamide] would have such a striking effect on DNA proviral levels,” she said. “We learn from each of these cases. But this is a single case, with multiple mechanisms that may have contributed to the outcome here. To what extent this is a direct result of this treatment strategy is unclear.”
Only time will tell, and Persaud knows this first hand. Back in 2014, she presented data at another HIV conference on the Mississippi baby who, after 21 months of no treatment, still didn›t have an HIV viral load.
At the time, the baby was hailed as “functionally cured,” but just 6 months later, the virus returned.
Dieffenbach agrees. “There are 10,000 genetic variations that need to be considered, and it all adds up to a unique individual,” he said of the Brazilian patient. “This one is one person, and it’s still early days.”
Counseling patients on niacin supplementation
Some clinicians are already bracing for the flood of people with HIV now wanting to take, or who are already taking, a niacin supplement because of this case, said Laura Waters, MD, from Mortimer Market Centre in London, who is chair of the British HIV Association.
But nicotinamide is different than nicotinic acid, which is what many people mean when they talk about niacin supplementation, according to data from the Office of Dietary Supplements (ODS) at the National Institutes of Health. Nicotinic acid has been used as a supplement for people with high cholesterol for years. Most Americans get more than the recommended daily intake of both types of niacin – 16 mg for adult men and 14 mg for adult women – in their regular diet, according to the 2015/16 National Health and Nutrition Examination Survey.
The Brazilian patient received a total daily dose of nicotinamide of 1000 mg, which is not associated with any adverse effects. Doses above 3000 mg daily can lead to diarrhea and a decrease in platelet count, according to the ODS.
Although Diaz said he doesn’t think people with HIV should run out and start taking a supplement right away, Waters said she sees it as inevitable.
The good news is that if people really are taking nicotinamide – not nicotinic acid – it seems “fairly well tolerated without many side effects,” she said, but added: “I expect shortages of nicotinamide from tomorrow.”
This story first appeared on Medscape.com.
A 35-year-old Brazilian man who participated in a trial in which he received an intensified antiretroviral regimen plus supplemental vitamin B3 for 48 weeks has joined the short list of patients who have experienced a period of remission from HIV in the absence of effective treatment.
Along with the Mississippi baby, a San Francisco man, a 24-year-old Thai man, a 9-year-old South African child, and the London and Berlin patients, the Brazilian man has an undetectable viral load and, more than a year after stopping treatment, his HIV antibody test is negative.
But as with the Berlin and London patients, it seems unlikely that – even if the man remains HIV free into the future – the circumstances of his remission will be broadly applicable to other people with HIV, said Carl Dieffenbach, PhD, director of the Division of AIDS at the National Institute of Allergy and Infectious Diseases, National Institutes of Health.
“I don’t think it’s replicable,” Dieffenbach told Medscape Medical News. Researchers should still try to confirm the finding, but they will probably learn more by studying the man’s unique genetic characteristics and immune system “than to go out and treat another 200 people with the same protocol.”
‘Shock-and-kill strategy’
The man had been on treatment since his HIV diagnosis in 2012, and was one of 30 people to enroll in a Brazilian study – the Multi Interventional Study Exploring HIV-1 Residual Replication: A Step Toward HIV Eradication and Sterilizing Cure – in 2016. At that point, his regimen consisted of the combination of efavirenz, lamivudine, and tenofovir disoproxil fumarate (Symfi, Mylan Pharmaceuticals) and his viral load was undetectable.
He was one of five people in the study to be randomized to receive the integrase inhibitor dolutegravir (Tivicay, ViiV Healthcare), the CCR5 receptor inhibitor maraviroc (Selzentry, ViiV Healthcare), and twice-daily nicotinamide 500 mg, a form of vitamin B3, in addition to his regular regimen for 48 weeks.
Nicotinamide has been used for decades because of its anti-infective properties, particularly in tuberculosis. In vitro, it also works to reverse HIV latency, said study investigator Ricardo Diaz, MD, from the Federal University of São Paulo, who presented the data at a press conference for the International AIDS Conference (AIDS) 2020.
“This is a shock-and-kill strategy,” said Leila Giron, PhD, from the Wistar Institute in Philadelphia, who was one of the study investigators. “We did in vitro studies to make sure nicotinamide took HIV out of the cells.”
“The cell machinery changed a lot,” she told Medscape Medical News. “And because it’s a B vitamin, all five participants didn’t have any side effects.”
But the patient was the only person in his treatment group to experience viral load “blips” during treatment – at weeks 16 and 24. And viral DNA was present at low levels in his peripheral blood spots and rectal tissue at baseline and at 48 weeks, and his HIV antibodies dropped from 91.8 RLU at baseline to 58.0 RLU at week 48.
“He had a decline in cell activation, inflammation, and a very deep decline in antibody titers,” Diaz reported.
After 48 weeks of the intensified treatment, the patient returned to his usual regimen for 3 years. Then, in March 2019, he agreed to try an analytical treatment interruption and discontinued all HIV treatment.
“What’s interesting is right before the analytical treatment interruption, the HIV DNA sequences were completely negative,” said Diaz.
Every 3 weeks for the next 64.7 weeks, his viral load came back undetectable, and so did HIV DNA in blood spots. One thing did change, though: in February 2020, the man’s HIV antibody test came back negative.
The team checked that he wasn’t still taking his antiretroviral medication, which might have explained the undetectable viral load, and he wasn’t.
Surprise, skepticism, and hope
The results have prompted surprise, skepticism, and questions from clinicians and researchers.
said Anton Pozniak, MD, from Chelsea and Westminster Hospital in London, who is cochair of AIDS 2020.
“They need a bigger study to see whether or not [the participant] is one of these guys who stopped treatment and might take a year or two, or four, to rebound,” he said. But if other studies replicate the results, the control of HIV in “one in five people would still be huge.”
The rationale behind treatment intensification for HIV remission is that “the three-drug ART regimen was perhaps insufficient to completely block HIV replication” in the reservoirs, even though that replication could be happening below levels detectable with current tests, said Laura Persaud, MD, from the Johns Hopkins University School of Medicine in Baltimore, who is chair of the International Maternal Pediatric Adolescent AIDS Clinical Trial Network (IMPAACT) HIV Cure Committee and was not involved in the study.
“The idea was to see if you could accelerate the decay of the reservoir” if you added medications that targeted different parts of the HIV lifecycle. Symfi, for instance, targets just one step in the viral replication process: the point where HIV RNA reverse transcribes itself into DNA so it can integrate into immune cells. But CCR5 inhibitors block entry of HIV into the cell in the first place, and integrase inhibitors, like raltegravir (Isentress, Merck) and dolutegravir, prevent HIV DNA from integrating into the host chromosome after it has reverse transcribed itself.
Still, recent data suggest that treatment intensification might not be as effective as hypothesized, she said. And the nicotinamide study was in vitro. To what extent this is a direct result of this treatment strategy is unclear.
“It’s hard to believe, in this small study, that this agent [nicotinamide] would have such a striking effect on DNA proviral levels,” she said. “We learn from each of these cases. But this is a single case, with multiple mechanisms that may have contributed to the outcome here. To what extent this is a direct result of this treatment strategy is unclear.”
Only time will tell, and Persaud knows this first hand. Back in 2014, she presented data at another HIV conference on the Mississippi baby who, after 21 months of no treatment, still didn›t have an HIV viral load.
At the time, the baby was hailed as “functionally cured,” but just 6 months later, the virus returned.
Dieffenbach agrees. “There are 10,000 genetic variations that need to be considered, and it all adds up to a unique individual,” he said of the Brazilian patient. “This one is one person, and it’s still early days.”
Counseling patients on niacin supplementation
Some clinicians are already bracing for the flood of people with HIV now wanting to take, or who are already taking, a niacin supplement because of this case, said Laura Waters, MD, from Mortimer Market Centre in London, who is chair of the British HIV Association.
But nicotinamide is different than nicotinic acid, which is what many people mean when they talk about niacin supplementation, according to data from the Office of Dietary Supplements (ODS) at the National Institutes of Health. Nicotinic acid has been used as a supplement for people with high cholesterol for years. Most Americans get more than the recommended daily intake of both types of niacin – 16 mg for adult men and 14 mg for adult women – in their regular diet, according to the 2015/16 National Health and Nutrition Examination Survey.
The Brazilian patient received a total daily dose of nicotinamide of 1000 mg, which is not associated with any adverse effects. Doses above 3000 mg daily can lead to diarrhea and a decrease in platelet count, according to the ODS.
Although Diaz said he doesn’t think people with HIV should run out and start taking a supplement right away, Waters said she sees it as inevitable.
The good news is that if people really are taking nicotinamide – not nicotinic acid – it seems “fairly well tolerated without many side effects,” she said, but added: “I expect shortages of nicotinamide from tomorrow.”
This story first appeared on Medscape.com.
A 35-year-old Brazilian man who participated in a trial in which he received an intensified antiretroviral regimen plus supplemental vitamin B3 for 48 weeks has joined the short list of patients who have experienced a period of remission from HIV in the absence of effective treatment.
Along with the Mississippi baby, a San Francisco man, a 24-year-old Thai man, a 9-year-old South African child, and the London and Berlin patients, the Brazilian man has an undetectable viral load and, more than a year after stopping treatment, his HIV antibody test is negative.
But as with the Berlin and London patients, it seems unlikely that – even if the man remains HIV free into the future – the circumstances of his remission will be broadly applicable to other people with HIV, said Carl Dieffenbach, PhD, director of the Division of AIDS at the National Institute of Allergy and Infectious Diseases, National Institutes of Health.
“I don’t think it’s replicable,” Dieffenbach told Medscape Medical News. Researchers should still try to confirm the finding, but they will probably learn more by studying the man’s unique genetic characteristics and immune system “than to go out and treat another 200 people with the same protocol.”
‘Shock-and-kill strategy’
The man had been on treatment since his HIV diagnosis in 2012, and was one of 30 people to enroll in a Brazilian study – the Multi Interventional Study Exploring HIV-1 Residual Replication: A Step Toward HIV Eradication and Sterilizing Cure – in 2016. At that point, his regimen consisted of the combination of efavirenz, lamivudine, and tenofovir disoproxil fumarate (Symfi, Mylan Pharmaceuticals) and his viral load was undetectable.
He was one of five people in the study to be randomized to receive the integrase inhibitor dolutegravir (Tivicay, ViiV Healthcare), the CCR5 receptor inhibitor maraviroc (Selzentry, ViiV Healthcare), and twice-daily nicotinamide 500 mg, a form of vitamin B3, in addition to his regular regimen for 48 weeks.
Nicotinamide has been used for decades because of its anti-infective properties, particularly in tuberculosis. In vitro, it also works to reverse HIV latency, said study investigator Ricardo Diaz, MD, from the Federal University of São Paulo, who presented the data at a press conference for the International AIDS Conference (AIDS) 2020.
“This is a shock-and-kill strategy,” said Leila Giron, PhD, from the Wistar Institute in Philadelphia, who was one of the study investigators. “We did in vitro studies to make sure nicotinamide took HIV out of the cells.”
“The cell machinery changed a lot,” she told Medscape Medical News. “And because it’s a B vitamin, all five participants didn’t have any side effects.”
But the patient was the only person in his treatment group to experience viral load “blips” during treatment – at weeks 16 and 24. And viral DNA was present at low levels in his peripheral blood spots and rectal tissue at baseline and at 48 weeks, and his HIV antibodies dropped from 91.8 RLU at baseline to 58.0 RLU at week 48.
“He had a decline in cell activation, inflammation, and a very deep decline in antibody titers,” Diaz reported.
After 48 weeks of the intensified treatment, the patient returned to his usual regimen for 3 years. Then, in March 2019, he agreed to try an analytical treatment interruption and discontinued all HIV treatment.
“What’s interesting is right before the analytical treatment interruption, the HIV DNA sequences were completely negative,” said Diaz.
Every 3 weeks for the next 64.7 weeks, his viral load came back undetectable, and so did HIV DNA in blood spots. One thing did change, though: in February 2020, the man’s HIV antibody test came back negative.
The team checked that he wasn’t still taking his antiretroviral medication, which might have explained the undetectable viral load, and he wasn’t.
Surprise, skepticism, and hope
The results have prompted surprise, skepticism, and questions from clinicians and researchers.
said Anton Pozniak, MD, from Chelsea and Westminster Hospital in London, who is cochair of AIDS 2020.
“They need a bigger study to see whether or not [the participant] is one of these guys who stopped treatment and might take a year or two, or four, to rebound,” he said. But if other studies replicate the results, the control of HIV in “one in five people would still be huge.”
The rationale behind treatment intensification for HIV remission is that “the three-drug ART regimen was perhaps insufficient to completely block HIV replication” in the reservoirs, even though that replication could be happening below levels detectable with current tests, said Laura Persaud, MD, from the Johns Hopkins University School of Medicine in Baltimore, who is chair of the International Maternal Pediatric Adolescent AIDS Clinical Trial Network (IMPAACT) HIV Cure Committee and was not involved in the study.
“The idea was to see if you could accelerate the decay of the reservoir” if you added medications that targeted different parts of the HIV lifecycle. Symfi, for instance, targets just one step in the viral replication process: the point where HIV RNA reverse transcribes itself into DNA so it can integrate into immune cells. But CCR5 inhibitors block entry of HIV into the cell in the first place, and integrase inhibitors, like raltegravir (Isentress, Merck) and dolutegravir, prevent HIV DNA from integrating into the host chromosome after it has reverse transcribed itself.
Still, recent data suggest that treatment intensification might not be as effective as hypothesized, she said. And the nicotinamide study was in vitro. To what extent this is a direct result of this treatment strategy is unclear.
“It’s hard to believe, in this small study, that this agent [nicotinamide] would have such a striking effect on DNA proviral levels,” she said. “We learn from each of these cases. But this is a single case, with multiple mechanisms that may have contributed to the outcome here. To what extent this is a direct result of this treatment strategy is unclear.”
Only time will tell, and Persaud knows this first hand. Back in 2014, she presented data at another HIV conference on the Mississippi baby who, after 21 months of no treatment, still didn›t have an HIV viral load.
At the time, the baby was hailed as “functionally cured,” but just 6 months later, the virus returned.
Dieffenbach agrees. “There are 10,000 genetic variations that need to be considered, and it all adds up to a unique individual,” he said of the Brazilian patient. “This one is one person, and it’s still early days.”
Counseling patients on niacin supplementation
Some clinicians are already bracing for the flood of people with HIV now wanting to take, or who are already taking, a niacin supplement because of this case, said Laura Waters, MD, from Mortimer Market Centre in London, who is chair of the British HIV Association.
But nicotinamide is different than nicotinic acid, which is what many people mean when they talk about niacin supplementation, according to data from the Office of Dietary Supplements (ODS) at the National Institutes of Health. Nicotinic acid has been used as a supplement for people with high cholesterol for years. Most Americans get more than the recommended daily intake of both types of niacin – 16 mg for adult men and 14 mg for adult women – in their regular diet, according to the 2015/16 National Health and Nutrition Examination Survey.
The Brazilian patient received a total daily dose of nicotinamide of 1000 mg, which is not associated with any adverse effects. Doses above 3000 mg daily can lead to diarrhea and a decrease in platelet count, according to the ODS.
Although Diaz said he doesn’t think people with HIV should run out and start taking a supplement right away, Waters said she sees it as inevitable.
The good news is that if people really are taking nicotinamide – not nicotinic acid – it seems “fairly well tolerated without many side effects,” she said, but added: “I expect shortages of nicotinamide from tomorrow.”
This story first appeared on Medscape.com.
FDA OKs first-in-class HIV therapy for patients with few options
Fostemsavir is indicated for use in combination with other antiretroviral (ARV) agents in heavily treatment-experienced adults with multidrug-resistant HIV-1 infection who fail to achieve viral suppression on other regimens due to resistance, intolerance, or safety considerations.
“This approval marks a new class of antiretroviral medications that may benefit patients who have run out of HIV treatment options,” Jeff Murray, MD, deputy director of the Division of Antivirals in the FDA’s Center for Drug Evaluation and Research, said in a statement.
“The availability of new classes of antiretroviral drugs is critical for heavily treatment-experienced patients living with multidrug resistant HIV infection — helping people living with hard-to-treat HIV who are at greater risk for HIV-related complications to potentially live longer, healthier lives,” he said.
Fostemsavir 600 mg extended-release tablets are taken twice daily.
In the phase 3 BRIGHTE study, 60% of adults who added fostemsavir to optimized background ARV therapy achieved and maintained viral suppression through 96 weeks and saw clinically meaningful improvements in CD4+ T cells.
Most of the 371 participants in the study had been on anti-HIV therapy for more than 15 years (71%), had been exposed to five or more different HIV treatment regimens (85%), and/or had a history of AIDS (86%).
The most common adverse reactions with fostemsavir are nausea, fatigue, and diarrhea. Serious drug reactions included liver enzyme elevations in patients co-infected with hepatitis B or C virus and three cases of severe immune reconstitution inflammatory syndrome.
“Exciting” Advance
“There is a small group of heavily treatment-experienced adults living with HIV who are not able to maintain viral suppression with currently available medication and, without effective new options, are at great risk of progressing to AIDS,” Deborah Waterhouse, CEO of ViiV Healthcare, said in a news release.
“The approval of Rukobia is a culmination of incredibly complex research, development, and manufacturing efforts to ensure we leave no person living with HIV behind,” she said.
“As a novel HIV attachment inhibitor, fostemsavir targets the first step of the viral lifecycle offering a new mechanism of action to treat people living with HIV,” Jacob P. Lalezari, MD, chief executive officer and director of Quest Clinical Research, commented in the release.
Fostemsavir is an “exciting” advance for the heavily treatment-experienced population and “an advancement the HIV community has long been waiting for. As an activist as well as researcher, I am very grateful to ViiV Healthcare for their commitment to heavily-treatment experienced people living with HIV,” he added.
Fostemsavir was reviewed and approved under the FDA’s fast track and breakthrough therapy designations, which are intended to facilitate and expedite the development and review of new drugs to address unmet medical need in the treatment of a serious or life-threatening condition.
Full prescribing information is available online.
This article first appeared on Medscape.com.
Fostemsavir is indicated for use in combination with other antiretroviral (ARV) agents in heavily treatment-experienced adults with multidrug-resistant HIV-1 infection who fail to achieve viral suppression on other regimens due to resistance, intolerance, or safety considerations.
“This approval marks a new class of antiretroviral medications that may benefit patients who have run out of HIV treatment options,” Jeff Murray, MD, deputy director of the Division of Antivirals in the FDA’s Center for Drug Evaluation and Research, said in a statement.
“The availability of new classes of antiretroviral drugs is critical for heavily treatment-experienced patients living with multidrug resistant HIV infection — helping people living with hard-to-treat HIV who are at greater risk for HIV-related complications to potentially live longer, healthier lives,” he said.
Fostemsavir 600 mg extended-release tablets are taken twice daily.
In the phase 3 BRIGHTE study, 60% of adults who added fostemsavir to optimized background ARV therapy achieved and maintained viral suppression through 96 weeks and saw clinically meaningful improvements in CD4+ T cells.
Most of the 371 participants in the study had been on anti-HIV therapy for more than 15 years (71%), had been exposed to five or more different HIV treatment regimens (85%), and/or had a history of AIDS (86%).
The most common adverse reactions with fostemsavir are nausea, fatigue, and diarrhea. Serious drug reactions included liver enzyme elevations in patients co-infected with hepatitis B or C virus and three cases of severe immune reconstitution inflammatory syndrome.
“Exciting” Advance
“There is a small group of heavily treatment-experienced adults living with HIV who are not able to maintain viral suppression with currently available medication and, without effective new options, are at great risk of progressing to AIDS,” Deborah Waterhouse, CEO of ViiV Healthcare, said in a news release.
“The approval of Rukobia is a culmination of incredibly complex research, development, and manufacturing efforts to ensure we leave no person living with HIV behind,” she said.
“As a novel HIV attachment inhibitor, fostemsavir targets the first step of the viral lifecycle offering a new mechanism of action to treat people living with HIV,” Jacob P. Lalezari, MD, chief executive officer and director of Quest Clinical Research, commented in the release.
Fostemsavir is an “exciting” advance for the heavily treatment-experienced population and “an advancement the HIV community has long been waiting for. As an activist as well as researcher, I am very grateful to ViiV Healthcare for their commitment to heavily-treatment experienced people living with HIV,” he added.
Fostemsavir was reviewed and approved under the FDA’s fast track and breakthrough therapy designations, which are intended to facilitate and expedite the development and review of new drugs to address unmet medical need in the treatment of a serious or life-threatening condition.
Full prescribing information is available online.
This article first appeared on Medscape.com.
Fostemsavir is indicated for use in combination with other antiretroviral (ARV) agents in heavily treatment-experienced adults with multidrug-resistant HIV-1 infection who fail to achieve viral suppression on other regimens due to resistance, intolerance, or safety considerations.
“This approval marks a new class of antiretroviral medications that may benefit patients who have run out of HIV treatment options,” Jeff Murray, MD, deputy director of the Division of Antivirals in the FDA’s Center for Drug Evaluation and Research, said in a statement.
“The availability of new classes of antiretroviral drugs is critical for heavily treatment-experienced patients living with multidrug resistant HIV infection — helping people living with hard-to-treat HIV who are at greater risk for HIV-related complications to potentially live longer, healthier lives,” he said.
Fostemsavir 600 mg extended-release tablets are taken twice daily.
In the phase 3 BRIGHTE study, 60% of adults who added fostemsavir to optimized background ARV therapy achieved and maintained viral suppression through 96 weeks and saw clinically meaningful improvements in CD4+ T cells.
Most of the 371 participants in the study had been on anti-HIV therapy for more than 15 years (71%), had been exposed to five or more different HIV treatment regimens (85%), and/or had a history of AIDS (86%).
The most common adverse reactions with fostemsavir are nausea, fatigue, and diarrhea. Serious drug reactions included liver enzyme elevations in patients co-infected with hepatitis B or C virus and three cases of severe immune reconstitution inflammatory syndrome.
“Exciting” Advance
“There is a small group of heavily treatment-experienced adults living with HIV who are not able to maintain viral suppression with currently available medication and, without effective new options, are at great risk of progressing to AIDS,” Deborah Waterhouse, CEO of ViiV Healthcare, said in a news release.
“The approval of Rukobia is a culmination of incredibly complex research, development, and manufacturing efforts to ensure we leave no person living with HIV behind,” she said.
“As a novel HIV attachment inhibitor, fostemsavir targets the first step of the viral lifecycle offering a new mechanism of action to treat people living with HIV,” Jacob P. Lalezari, MD, chief executive officer and director of Quest Clinical Research, commented in the release.
Fostemsavir is an “exciting” advance for the heavily treatment-experienced population and “an advancement the HIV community has long been waiting for. As an activist as well as researcher, I am very grateful to ViiV Healthcare for their commitment to heavily-treatment experienced people living with HIV,” he added.
Fostemsavir was reviewed and approved under the FDA’s fast track and breakthrough therapy designations, which are intended to facilitate and expedite the development and review of new drugs to address unmet medical need in the treatment of a serious or life-threatening condition.
Full prescribing information is available online.
This article first appeared on Medscape.com.
Holistic HIV care broadens scope to noncommunicable diseases
Several HIV management efforts in African groups have developed differentiated service delivery models for people living with HIV who also have noncommunicable diseases, offering diagnostic and management strategies that can treat HIV patients holistically and address their range of health issues.
These efforts allow “countries with effective HIV programs to leverage lessons learned and best practices to enhance chronic noncommunicable disease” management, Miriam Rabkin, MD, said at the virtual meeting of the International AIDS conference. This approach aims to address the “growing prevalence of chronic noncommunicable diseases in low- and middle-income countries,” and the recognition that ”people living with HIV have the same or higher prevalence” of chronic noncommunicable diseases as that of others in the region where they live, said Dr. Rabkin, an epidemiologist at Columbia University in New York and director for health systems strengthening at ICAP, an international AIDS care program run at Columbia. The differentiated service delivery model derived from the premise that “one size does not fit all,” and that effective interventions must be “tailored” to the social and clinical circumstances of specific regions, she explained.
One program has focused on introducing more contemporary methods for diagnosing leukemias, lymphomas, and melanomas using flow cytometry at the Uganda National Health Laboratory Service in Kampala. This change in testing, which became available to patients starting in February 2019, has allowed diagnostics with fresh specimens that require minimal processing and results returned to referring physicians within 48 hours, a significant upgrade from the 1- to 4-week delay that was typical in the past, said Steven J. Kussick, MD, a hematopathologist and associate medical director of PhenoPath, a commercial pathology laboratory in Seattle.
The idea was to “leverage existing HIV laboratory capabilities to transform cancer diagnosis in sub-Saharan Africa,” he said during his talk at the conference. The flow cytometry approach allows an experienced pathologist like Dr. Kussick to diagnose clearcut cases in “5 seconds,” he said. The lab has already run specimens from more than 200 patients, and estimates an ability to handle specimens from about 250 patients per year at a total annual cost of roughly $60,000, an apparently sustainable operating model, said Dr. Kussick, who serves as a full-time consultant to the operation and was also instrumental in the 5-year process that created the diagnostic program. Future improvements planned for this program include bringing on-line a higher complexity diagnostic assay that’s closer to what is currently standard U.S. testing, digital imaging to facilitate consultation with remote experts, adding immunochemistry assays to allow diagnosis of solid tumors, and opening of a second laboratory in Kenya.
Another noncommunicable disease intervention in Africa that’s building on existing infrastructure for dealing with HIV infection is targeting hypertension, the most lethal risk factor globally for preventable deaths, said Jennifer Cohn, MD, senior vice president for cardiovascular health at the New York–based Resolve to Save Lives initiative. “We need to learn from what’s been done for HIV to rapidly incorporate and scale differentiated service models,” she said.
HIV and hypertension, along with diabetes, “are beginning to be recognized as ‘syndemics,’ ”synergistic pandemics, that need a holistic approach. A recent review of the topic reported that in the seven sub-Saharan countries with the highest HIV infection prevalence the percentage of adults with hypertension ranged from 20% to 24% (Curr Opin HIV AIDS. 2020 Jul;15[4]:356-60). Projections call for a “dramatic” increase in the prevalence of hypertension in both the general population and among people living with HIV, Dr. Cohn said.
As an example of the potential for combining HIV and antihypertensive care into a one-stop protocol, she cited a model program launched at Makarere University in Kampala, Uganda, that integrates HIV and antihypertensive treatment. Recent data from the program showed that among HIV-infected individuals 24% also had hypertension, and while the program lagged in putting only 28% of these hypertensive patients on a blood pressure-lowering regimen, more than three quarters of these patients on treatment successfully reached their goal blood pressure, proving the feasibility of the combined approach, Dr. Cohn said.
“Starting and scaling with differentiated service delivery models for noncommunicable diseases can help overcome barriers to uptake of care,” concluded Dr. Cohn. “As HIV cohorts age, we have to adapt and ensure we are providing quality, holistic care, including care for high impact noncommunicable diseases such as hypertension.”
Dr. Rabkin and Dr. Cohn had no disclosures.
Several HIV management efforts in African groups have developed differentiated service delivery models for people living with HIV who also have noncommunicable diseases, offering diagnostic and management strategies that can treat HIV patients holistically and address their range of health issues.
These efforts allow “countries with effective HIV programs to leverage lessons learned and best practices to enhance chronic noncommunicable disease” management, Miriam Rabkin, MD, said at the virtual meeting of the International AIDS conference. This approach aims to address the “growing prevalence of chronic noncommunicable diseases in low- and middle-income countries,” and the recognition that ”people living with HIV have the same or higher prevalence” of chronic noncommunicable diseases as that of others in the region where they live, said Dr. Rabkin, an epidemiologist at Columbia University in New York and director for health systems strengthening at ICAP, an international AIDS care program run at Columbia. The differentiated service delivery model derived from the premise that “one size does not fit all,” and that effective interventions must be “tailored” to the social and clinical circumstances of specific regions, she explained.
One program has focused on introducing more contemporary methods for diagnosing leukemias, lymphomas, and melanomas using flow cytometry at the Uganda National Health Laboratory Service in Kampala. This change in testing, which became available to patients starting in February 2019, has allowed diagnostics with fresh specimens that require minimal processing and results returned to referring physicians within 48 hours, a significant upgrade from the 1- to 4-week delay that was typical in the past, said Steven J. Kussick, MD, a hematopathologist and associate medical director of PhenoPath, a commercial pathology laboratory in Seattle.
The idea was to “leverage existing HIV laboratory capabilities to transform cancer diagnosis in sub-Saharan Africa,” he said during his talk at the conference. The flow cytometry approach allows an experienced pathologist like Dr. Kussick to diagnose clearcut cases in “5 seconds,” he said. The lab has already run specimens from more than 200 patients, and estimates an ability to handle specimens from about 250 patients per year at a total annual cost of roughly $60,000, an apparently sustainable operating model, said Dr. Kussick, who serves as a full-time consultant to the operation and was also instrumental in the 5-year process that created the diagnostic program. Future improvements planned for this program include bringing on-line a higher complexity diagnostic assay that’s closer to what is currently standard U.S. testing, digital imaging to facilitate consultation with remote experts, adding immunochemistry assays to allow diagnosis of solid tumors, and opening of a second laboratory in Kenya.
Another noncommunicable disease intervention in Africa that’s building on existing infrastructure for dealing with HIV infection is targeting hypertension, the most lethal risk factor globally for preventable deaths, said Jennifer Cohn, MD, senior vice president for cardiovascular health at the New York–based Resolve to Save Lives initiative. “We need to learn from what’s been done for HIV to rapidly incorporate and scale differentiated service models,” she said.
HIV and hypertension, along with diabetes, “are beginning to be recognized as ‘syndemics,’ ”synergistic pandemics, that need a holistic approach. A recent review of the topic reported that in the seven sub-Saharan countries with the highest HIV infection prevalence the percentage of adults with hypertension ranged from 20% to 24% (Curr Opin HIV AIDS. 2020 Jul;15[4]:356-60). Projections call for a “dramatic” increase in the prevalence of hypertension in both the general population and among people living with HIV, Dr. Cohn said.
As an example of the potential for combining HIV and antihypertensive care into a one-stop protocol, she cited a model program launched at Makarere University in Kampala, Uganda, that integrates HIV and antihypertensive treatment. Recent data from the program showed that among HIV-infected individuals 24% also had hypertension, and while the program lagged in putting only 28% of these hypertensive patients on a blood pressure-lowering regimen, more than three quarters of these patients on treatment successfully reached their goal blood pressure, proving the feasibility of the combined approach, Dr. Cohn said.
“Starting and scaling with differentiated service delivery models for noncommunicable diseases can help overcome barriers to uptake of care,” concluded Dr. Cohn. “As HIV cohorts age, we have to adapt and ensure we are providing quality, holistic care, including care for high impact noncommunicable diseases such as hypertension.”
Dr. Rabkin and Dr. Cohn had no disclosures.
Several HIV management efforts in African groups have developed differentiated service delivery models for people living with HIV who also have noncommunicable diseases, offering diagnostic and management strategies that can treat HIV patients holistically and address their range of health issues.
These efforts allow “countries with effective HIV programs to leverage lessons learned and best practices to enhance chronic noncommunicable disease” management, Miriam Rabkin, MD, said at the virtual meeting of the International AIDS conference. This approach aims to address the “growing prevalence of chronic noncommunicable diseases in low- and middle-income countries,” and the recognition that ”people living with HIV have the same or higher prevalence” of chronic noncommunicable diseases as that of others in the region where they live, said Dr. Rabkin, an epidemiologist at Columbia University in New York and director for health systems strengthening at ICAP, an international AIDS care program run at Columbia. The differentiated service delivery model derived from the premise that “one size does not fit all,” and that effective interventions must be “tailored” to the social and clinical circumstances of specific regions, she explained.
One program has focused on introducing more contemporary methods for diagnosing leukemias, lymphomas, and melanomas using flow cytometry at the Uganda National Health Laboratory Service in Kampala. This change in testing, which became available to patients starting in February 2019, has allowed diagnostics with fresh specimens that require minimal processing and results returned to referring physicians within 48 hours, a significant upgrade from the 1- to 4-week delay that was typical in the past, said Steven J. Kussick, MD, a hematopathologist and associate medical director of PhenoPath, a commercial pathology laboratory in Seattle.
The idea was to “leverage existing HIV laboratory capabilities to transform cancer diagnosis in sub-Saharan Africa,” he said during his talk at the conference. The flow cytometry approach allows an experienced pathologist like Dr. Kussick to diagnose clearcut cases in “5 seconds,” he said. The lab has already run specimens from more than 200 patients, and estimates an ability to handle specimens from about 250 patients per year at a total annual cost of roughly $60,000, an apparently sustainable operating model, said Dr. Kussick, who serves as a full-time consultant to the operation and was also instrumental in the 5-year process that created the diagnostic program. Future improvements planned for this program include bringing on-line a higher complexity diagnostic assay that’s closer to what is currently standard U.S. testing, digital imaging to facilitate consultation with remote experts, adding immunochemistry assays to allow diagnosis of solid tumors, and opening of a second laboratory in Kenya.
Another noncommunicable disease intervention in Africa that’s building on existing infrastructure for dealing with HIV infection is targeting hypertension, the most lethal risk factor globally for preventable deaths, said Jennifer Cohn, MD, senior vice president for cardiovascular health at the New York–based Resolve to Save Lives initiative. “We need to learn from what’s been done for HIV to rapidly incorporate and scale differentiated service models,” she said.
HIV and hypertension, along with diabetes, “are beginning to be recognized as ‘syndemics,’ ”synergistic pandemics, that need a holistic approach. A recent review of the topic reported that in the seven sub-Saharan countries with the highest HIV infection prevalence the percentage of adults with hypertension ranged from 20% to 24% (Curr Opin HIV AIDS. 2020 Jul;15[4]:356-60). Projections call for a “dramatic” increase in the prevalence of hypertension in both the general population and among people living with HIV, Dr. Cohn said.
As an example of the potential for combining HIV and antihypertensive care into a one-stop protocol, she cited a model program launched at Makarere University in Kampala, Uganda, that integrates HIV and antihypertensive treatment. Recent data from the program showed that among HIV-infected individuals 24% also had hypertension, and while the program lagged in putting only 28% of these hypertensive patients on a blood pressure-lowering regimen, more than three quarters of these patients on treatment successfully reached their goal blood pressure, proving the feasibility of the combined approach, Dr. Cohn said.
“Starting and scaling with differentiated service delivery models for noncommunicable diseases can help overcome barriers to uptake of care,” concluded Dr. Cohn. “As HIV cohorts age, we have to adapt and ensure we are providing quality, holistic care, including care for high impact noncommunicable diseases such as hypertension.”
Dr. Rabkin and Dr. Cohn had no disclosures.
FROM AIDS 2020
COVID-19 disruptions ‘life threatening’ for people with HIV
When the COVID-19 pandemic led to a blanket shelter-in-place order in California in March, it did more than shut down in-person visits at Ward 86, the HIV clinic for publicly insured patients at San Francisco General Hospital. It also led to a decrease in viral suppression among the clinic›s clients. By the end of June, the percentage of patients with an undetectable viral load had dropped by nearly one-third.
This is exactly what Monica Gandhi, MD, associate division chief of HIV, infectious diseases, and global medicine at the University of California, San Francisco, and medical director of the clinic, was afraid of.
“We’re profoundly worried about the impact of COVID-19 on actual treatment outcomes,” said Dr. Gandhi, cochair of the virtual International AIDS Conference (AIDS) 2020.
And it’s not just the clinic’s clients at risk. Of the 106 countries served by the Global Fund to Fight HIV, Tuberculosis, and Malaria, 85% saw disruptions in HIV programs, according to a report released last month.
These service disruptions are considerable and “life threatening,” affecting some of the people at greatest risk for HIV acquisition and poor outcomes – such as people engaged in transactional sex (40%), men who have sex with men (37%), and transgender people (31%) – the 2020 Global AIDS Update, released today by UNAIDS, reports.
“In sub-Saharan Africa alone, if there is a 6-month interruption in HIV treatment services, it will account for an additional 500,000 deaths. That doubles the number of deaths in sub-Saharan Africa alone and brings us back to 2008 mortality levels,” said Shannon Hader, MD, deputy executive director of UNAIDS. “We just can’t allow that to happen.”
In addition, 73 countries are at risk of running out of HIV medications, according to a World Health Organization report, also released today.
Quantifying the impact
The impact is not the same for all patients, said Anton Pozniak, MD, consulting physician in HIV medicine at the Chelsea and Westminster Hospital in London, and international cochair of AIDS 2020.
For some, COVID-19 has not changed much. Their viral loads remain undetectable and all they need is multimonth supplies of their antiretroviral therapy (ART) medications, he told Medscape Medical News. Still, he said he worries about the well-documented effects that social isolation is having on the mental health of these patients, and the increase in substance use associated with the pandemic.
Then there is a small group of patients with HIV who had put off starting ART before the pandemic, but now want to start, he reported.
And finally, there are the people for whom the fear of COVID-19 has crippled their ability to get care.
There are people who have decided they don’t want to come to the hospital or come to the clinic because they’re scared of getting COVID-19.
“It’s really very striking,” said Dr. Pozniak. “There are people who have decided they don’t want to come to the hospital or come to the clinic because they’re scared of getting COVID-19. We’ve offered to deliver treatment, but they don’t want the stigma of parcels of drugs arriving.”
In a study presented at the conference, four of 12 care and substance-use treatment facilities in Europe and North America – including Seattle and Philadelphia – reported patients taking longer to fill ART prescriptions. And four of the 12 also reported that clients who injected drugs and were at risk for or living with HIV were having trouble adhering to prescribed therapies. In addition, at 11 of the sites, HIV testing has either nearly or completely shut down.
Structural barriers to telemedicine
And then there are structural barriers to care – poverty, lack of transportation, lack of or slow internet access, and lack of insurance – which affect 10% to 20% of the people with HIV that Jodie Dionne-Odom, MD, sees at the 1917 Ryan White HIV clinic at the University of Alabama at Birmingham.
These are the patients she said she worries about most, the ones who, even before COVID-19, were barely managing to pay their rent, car payments, and cell phone bills.
“With COVID-19 and being at home or being laid off, those things could no longer be paid. They’ve lost their phone, they’ve lost their car,” said Dionne-Odom, chief of women’s health services for the clinic. “That’s a really significant impact, because that’s exactly the group you can’t reach by telemedicine.”
In March, when the 1917 Clinic began providing the majority of services online, these people fell off the radar, said Aadia Rana, MD, associate professor of infectious diseases at the University of Alabama at Birmingham, who also works at the clinic.
This is not for lack of trying, she explained. Staff called patients weekly to check in and reschedule appointments, but there were some they just couldn’t reach.
Although the data for the second quarter have not yet been analyzed, “I would expect that our typically close to 90% viral suppression rate is going to decrease,” she said.
This decrease is likely widespread, said Rana, who is principle investigator of the Long-Acting Therapy to Improve Treatment Success in Daily Life (LATITUDE) study.
Many of the 33 sites involved in LATITUDE shut down in the early months of the pandemic, but some are now coming back online. In fact, “we are getting all these pleas from sites around the country saying, ‘Hey, once LATITUDE is open for enrollment, we have so many people who would now be eligible’,” she told Medscape Medical News.
“Why are they now eligible and they weren’t eligible before? I’m assuming it’s because they now have a detectable viral load,” which is one of the requirements for enrollment in LATITUDE, she explained.
Impact on the LGBTI community
At the onset of the COVID-19 pandemic, Erik Lamontagne, senior economist at UNAIDS, wondered how the quarantine was affecting LGBTI people.
To find out, he and his colleagues launched a survey asking just that. He is also coprinciple investigator of the LGBT Happiness Survey, a multicountry survey of LGBTI people launched last year.
The 13,562 LGBTI respondents came from 138 countries or territories. Of the 1,140 respondents living with HIV, 26% had seen their HIV care disrupted or restricted in some way during the pandemic, and 55% of those had no more than a month’s worth of HIV medications on hand.
But the pandemic hasn’t just affected people already living with HIV, Mr. Lamontagne reported. Nine of 10 respondents were living under some form of stay-at-home order, 73% were not meeting their basic needs, 37% had missed meals as a result of economic hardship, and half of those who were still working expected to lose their jobs.
Many could not afford to quarantine, Mr. Lamontagne told Medscape Medical News. And financial resources were stretched so thin that about 1% of respondents reported engaging in transactional sex for the first time. Some reported that their economic circumstances were so dire that they couldn’t require clients to wear condoms, increasing their risk for both COVID-19 and HIV.
“What they can eat in the evening is what they can earn during the day,” Mr. Lamontagne explained.
Unfortunately, it is the people already in a situation of economic vulnerability – often those from the LGBTI community – who are most affected by COVID-19, he added.
PrEP use changing
The pandemic has also affected the use of pre-exposure prophylaxis (PrEP).
South African women taking PrEP to protect themselves from HIV during pregnancy were 2.36 times more likely to miss a clinic visit to refill their prescription after COVID-19 lockdowns began than before, data presented at the conference showed. The women cited fear of acquiring COVID-19 at the medical facility, fear of police, transportation barriers, and long clinic wait times to explain the missed visits.
A study on the use of PrEP at Fenway Health, a sexual health clinic in Boston, showed a 278% increase in unfilled PrEP prescriptions after stay-at-home orders and a 72.1% drop in new PrEP prescriptions.
It’s unclear what these data, which will be presented at the conference later this week, mean, said Douglas Krakower, MD, assistant professor of medicine and population medicine at Harvard Medical School in Boston.
“We don’t know whether this represents people having trouble accessing PrEP” out of concern about getting COVID “or concerns about financial implications,” he explained.
“They may have had hardships from unemployment or other financial constraints” and have lost insurance or are still having to pay copays, he told Medscape Medical News. Or it could just be that they’re not going out or having sex, so they’ve discontinued the medication.
“Anecdotally we’ve heard that some patients are sheltering in place and not having sex and so have chosen not to use PrEP,” he added.
It’s also possible that people are rationing pills or have moved themselves to the PrEP 2-1-1 protocol, which is used only when someone is having sex, said Dr. Krakower, citing a study showing that sexual behavior is continuing as usual during quarantine for about half the gay men in the United States.
Resilience and fragility
It’s not just people living with HIV whose routines have changed during the pandemic. A survey of HIV clinicians around the world conducted by the International Association of Providers of AIDS Care showed that 88% of HIV clinicians have been pulled away from their regular work to manage COVID-19 in their communities.
But the COVID-19 pandemic shows no signs of stopping, and clinicians are now having to re-engage with their HIV patients.
“What COVID-19 has represented for us is a looking glass to see the resilience, but also the fragility, in HIV responses, not just in the global south, but also in the global north,” José Zuniga, PhD, IAPAC president and chief executive officer, said during a preconference session on controlling the HIV epidemic.
For Dr. Dionne-Odom, reopening the 1917 Clinic in Alabama meant tracking down patients who could not participate in telemedicine. Fortunately (or unfortunately, depending on how you look at it), the clinic, which serves a population with a high level of economic insecurity, has worked to get as many phone numbers as possible for each patient. So when the clinic opened back up, staff was able to call family members, friends, and trusted contacts to bring their patients back into the clinic.
“No one wanted to reopen too quickly,” said Dr. Dionne-Odom. “But having people come in allowed us to do all the other things that are the key part of HIV care: getting them connected with a social worker and making sure they have enough food, helping them with their electricity bills and their housing issues, all the wrap-around services that are so crucial for these patients.”
This article first appeared on Medscape.com.
When the COVID-19 pandemic led to a blanket shelter-in-place order in California in March, it did more than shut down in-person visits at Ward 86, the HIV clinic for publicly insured patients at San Francisco General Hospital. It also led to a decrease in viral suppression among the clinic›s clients. By the end of June, the percentage of patients with an undetectable viral load had dropped by nearly one-third.
This is exactly what Monica Gandhi, MD, associate division chief of HIV, infectious diseases, and global medicine at the University of California, San Francisco, and medical director of the clinic, was afraid of.
“We’re profoundly worried about the impact of COVID-19 on actual treatment outcomes,” said Dr. Gandhi, cochair of the virtual International AIDS Conference (AIDS) 2020.
And it’s not just the clinic’s clients at risk. Of the 106 countries served by the Global Fund to Fight HIV, Tuberculosis, and Malaria, 85% saw disruptions in HIV programs, according to a report released last month.
These service disruptions are considerable and “life threatening,” affecting some of the people at greatest risk for HIV acquisition and poor outcomes – such as people engaged in transactional sex (40%), men who have sex with men (37%), and transgender people (31%) – the 2020 Global AIDS Update, released today by UNAIDS, reports.
“In sub-Saharan Africa alone, if there is a 6-month interruption in HIV treatment services, it will account for an additional 500,000 deaths. That doubles the number of deaths in sub-Saharan Africa alone and brings us back to 2008 mortality levels,” said Shannon Hader, MD, deputy executive director of UNAIDS. “We just can’t allow that to happen.”
In addition, 73 countries are at risk of running out of HIV medications, according to a World Health Organization report, also released today.
Quantifying the impact
The impact is not the same for all patients, said Anton Pozniak, MD, consulting physician in HIV medicine at the Chelsea and Westminster Hospital in London, and international cochair of AIDS 2020.
For some, COVID-19 has not changed much. Their viral loads remain undetectable and all they need is multimonth supplies of their antiretroviral therapy (ART) medications, he told Medscape Medical News. Still, he said he worries about the well-documented effects that social isolation is having on the mental health of these patients, and the increase in substance use associated with the pandemic.
Then there is a small group of patients with HIV who had put off starting ART before the pandemic, but now want to start, he reported.
And finally, there are the people for whom the fear of COVID-19 has crippled their ability to get care.
There are people who have decided they don’t want to come to the hospital or come to the clinic because they’re scared of getting COVID-19.
“It’s really very striking,” said Dr. Pozniak. “There are people who have decided they don’t want to come to the hospital or come to the clinic because they’re scared of getting COVID-19. We’ve offered to deliver treatment, but they don’t want the stigma of parcels of drugs arriving.”
In a study presented at the conference, four of 12 care and substance-use treatment facilities in Europe and North America – including Seattle and Philadelphia – reported patients taking longer to fill ART prescriptions. And four of the 12 also reported that clients who injected drugs and were at risk for or living with HIV were having trouble adhering to prescribed therapies. In addition, at 11 of the sites, HIV testing has either nearly or completely shut down.
Structural barriers to telemedicine
And then there are structural barriers to care – poverty, lack of transportation, lack of or slow internet access, and lack of insurance – which affect 10% to 20% of the people with HIV that Jodie Dionne-Odom, MD, sees at the 1917 Ryan White HIV clinic at the University of Alabama at Birmingham.
These are the patients she said she worries about most, the ones who, even before COVID-19, were barely managing to pay their rent, car payments, and cell phone bills.
“With COVID-19 and being at home or being laid off, those things could no longer be paid. They’ve lost their phone, they’ve lost their car,” said Dionne-Odom, chief of women’s health services for the clinic. “That’s a really significant impact, because that’s exactly the group you can’t reach by telemedicine.”
In March, when the 1917 Clinic began providing the majority of services online, these people fell off the radar, said Aadia Rana, MD, associate professor of infectious diseases at the University of Alabama at Birmingham, who also works at the clinic.
This is not for lack of trying, she explained. Staff called patients weekly to check in and reschedule appointments, but there were some they just couldn’t reach.
Although the data for the second quarter have not yet been analyzed, “I would expect that our typically close to 90% viral suppression rate is going to decrease,” she said.
This decrease is likely widespread, said Rana, who is principle investigator of the Long-Acting Therapy to Improve Treatment Success in Daily Life (LATITUDE) study.
Many of the 33 sites involved in LATITUDE shut down in the early months of the pandemic, but some are now coming back online. In fact, “we are getting all these pleas from sites around the country saying, ‘Hey, once LATITUDE is open for enrollment, we have so many people who would now be eligible’,” she told Medscape Medical News.
“Why are they now eligible and they weren’t eligible before? I’m assuming it’s because they now have a detectable viral load,” which is one of the requirements for enrollment in LATITUDE, she explained.
Impact on the LGBTI community
At the onset of the COVID-19 pandemic, Erik Lamontagne, senior economist at UNAIDS, wondered how the quarantine was affecting LGBTI people.
To find out, he and his colleagues launched a survey asking just that. He is also coprinciple investigator of the LGBT Happiness Survey, a multicountry survey of LGBTI people launched last year.
The 13,562 LGBTI respondents came from 138 countries or territories. Of the 1,140 respondents living with HIV, 26% had seen their HIV care disrupted or restricted in some way during the pandemic, and 55% of those had no more than a month’s worth of HIV medications on hand.
But the pandemic hasn’t just affected people already living with HIV, Mr. Lamontagne reported. Nine of 10 respondents were living under some form of stay-at-home order, 73% were not meeting their basic needs, 37% had missed meals as a result of economic hardship, and half of those who were still working expected to lose their jobs.
Many could not afford to quarantine, Mr. Lamontagne told Medscape Medical News. And financial resources were stretched so thin that about 1% of respondents reported engaging in transactional sex for the first time. Some reported that their economic circumstances were so dire that they couldn’t require clients to wear condoms, increasing their risk for both COVID-19 and HIV.
“What they can eat in the evening is what they can earn during the day,” Mr. Lamontagne explained.
Unfortunately, it is the people already in a situation of economic vulnerability – often those from the LGBTI community – who are most affected by COVID-19, he added.
PrEP use changing
The pandemic has also affected the use of pre-exposure prophylaxis (PrEP).
South African women taking PrEP to protect themselves from HIV during pregnancy were 2.36 times more likely to miss a clinic visit to refill their prescription after COVID-19 lockdowns began than before, data presented at the conference showed. The women cited fear of acquiring COVID-19 at the medical facility, fear of police, transportation barriers, and long clinic wait times to explain the missed visits.
A study on the use of PrEP at Fenway Health, a sexual health clinic in Boston, showed a 278% increase in unfilled PrEP prescriptions after stay-at-home orders and a 72.1% drop in new PrEP prescriptions.
It’s unclear what these data, which will be presented at the conference later this week, mean, said Douglas Krakower, MD, assistant professor of medicine and population medicine at Harvard Medical School in Boston.
“We don’t know whether this represents people having trouble accessing PrEP” out of concern about getting COVID “or concerns about financial implications,” he explained.
“They may have had hardships from unemployment or other financial constraints” and have lost insurance or are still having to pay copays, he told Medscape Medical News. Or it could just be that they’re not going out or having sex, so they’ve discontinued the medication.
“Anecdotally we’ve heard that some patients are sheltering in place and not having sex and so have chosen not to use PrEP,” he added.
It’s also possible that people are rationing pills or have moved themselves to the PrEP 2-1-1 protocol, which is used only when someone is having sex, said Dr. Krakower, citing a study showing that sexual behavior is continuing as usual during quarantine for about half the gay men in the United States.
Resilience and fragility
It’s not just people living with HIV whose routines have changed during the pandemic. A survey of HIV clinicians around the world conducted by the International Association of Providers of AIDS Care showed that 88% of HIV clinicians have been pulled away from their regular work to manage COVID-19 in their communities.
But the COVID-19 pandemic shows no signs of stopping, and clinicians are now having to re-engage with their HIV patients.
“What COVID-19 has represented for us is a looking glass to see the resilience, but also the fragility, in HIV responses, not just in the global south, but also in the global north,” José Zuniga, PhD, IAPAC president and chief executive officer, said during a preconference session on controlling the HIV epidemic.
For Dr. Dionne-Odom, reopening the 1917 Clinic in Alabama meant tracking down patients who could not participate in telemedicine. Fortunately (or unfortunately, depending on how you look at it), the clinic, which serves a population with a high level of economic insecurity, has worked to get as many phone numbers as possible for each patient. So when the clinic opened back up, staff was able to call family members, friends, and trusted contacts to bring their patients back into the clinic.
“No one wanted to reopen too quickly,” said Dr. Dionne-Odom. “But having people come in allowed us to do all the other things that are the key part of HIV care: getting them connected with a social worker and making sure they have enough food, helping them with their electricity bills and their housing issues, all the wrap-around services that are so crucial for these patients.”
This article first appeared on Medscape.com.
When the COVID-19 pandemic led to a blanket shelter-in-place order in California in March, it did more than shut down in-person visits at Ward 86, the HIV clinic for publicly insured patients at San Francisco General Hospital. It also led to a decrease in viral suppression among the clinic›s clients. By the end of June, the percentage of patients with an undetectable viral load had dropped by nearly one-third.
This is exactly what Monica Gandhi, MD, associate division chief of HIV, infectious diseases, and global medicine at the University of California, San Francisco, and medical director of the clinic, was afraid of.
“We’re profoundly worried about the impact of COVID-19 on actual treatment outcomes,” said Dr. Gandhi, cochair of the virtual International AIDS Conference (AIDS) 2020.
And it’s not just the clinic’s clients at risk. Of the 106 countries served by the Global Fund to Fight HIV, Tuberculosis, and Malaria, 85% saw disruptions in HIV programs, according to a report released last month.
These service disruptions are considerable and “life threatening,” affecting some of the people at greatest risk for HIV acquisition and poor outcomes – such as people engaged in transactional sex (40%), men who have sex with men (37%), and transgender people (31%) – the 2020 Global AIDS Update, released today by UNAIDS, reports.
“In sub-Saharan Africa alone, if there is a 6-month interruption in HIV treatment services, it will account for an additional 500,000 deaths. That doubles the number of deaths in sub-Saharan Africa alone and brings us back to 2008 mortality levels,” said Shannon Hader, MD, deputy executive director of UNAIDS. “We just can’t allow that to happen.”
In addition, 73 countries are at risk of running out of HIV medications, according to a World Health Organization report, also released today.
Quantifying the impact
The impact is not the same for all patients, said Anton Pozniak, MD, consulting physician in HIV medicine at the Chelsea and Westminster Hospital in London, and international cochair of AIDS 2020.
For some, COVID-19 has not changed much. Their viral loads remain undetectable and all they need is multimonth supplies of their antiretroviral therapy (ART) medications, he told Medscape Medical News. Still, he said he worries about the well-documented effects that social isolation is having on the mental health of these patients, and the increase in substance use associated with the pandemic.
Then there is a small group of patients with HIV who had put off starting ART before the pandemic, but now want to start, he reported.
And finally, there are the people for whom the fear of COVID-19 has crippled their ability to get care.
There are people who have decided they don’t want to come to the hospital or come to the clinic because they’re scared of getting COVID-19.
“It’s really very striking,” said Dr. Pozniak. “There are people who have decided they don’t want to come to the hospital or come to the clinic because they’re scared of getting COVID-19. We’ve offered to deliver treatment, but they don’t want the stigma of parcels of drugs arriving.”
In a study presented at the conference, four of 12 care and substance-use treatment facilities in Europe and North America – including Seattle and Philadelphia – reported patients taking longer to fill ART prescriptions. And four of the 12 also reported that clients who injected drugs and were at risk for or living with HIV were having trouble adhering to prescribed therapies. In addition, at 11 of the sites, HIV testing has either nearly or completely shut down.
Structural barriers to telemedicine
And then there are structural barriers to care – poverty, lack of transportation, lack of or slow internet access, and lack of insurance – which affect 10% to 20% of the people with HIV that Jodie Dionne-Odom, MD, sees at the 1917 Ryan White HIV clinic at the University of Alabama at Birmingham.
These are the patients she said she worries about most, the ones who, even before COVID-19, were barely managing to pay their rent, car payments, and cell phone bills.
“With COVID-19 and being at home or being laid off, those things could no longer be paid. They’ve lost their phone, they’ve lost their car,” said Dionne-Odom, chief of women’s health services for the clinic. “That’s a really significant impact, because that’s exactly the group you can’t reach by telemedicine.”
In March, when the 1917 Clinic began providing the majority of services online, these people fell off the radar, said Aadia Rana, MD, associate professor of infectious diseases at the University of Alabama at Birmingham, who also works at the clinic.
This is not for lack of trying, she explained. Staff called patients weekly to check in and reschedule appointments, but there were some they just couldn’t reach.
Although the data for the second quarter have not yet been analyzed, “I would expect that our typically close to 90% viral suppression rate is going to decrease,” she said.
This decrease is likely widespread, said Rana, who is principle investigator of the Long-Acting Therapy to Improve Treatment Success in Daily Life (LATITUDE) study.
Many of the 33 sites involved in LATITUDE shut down in the early months of the pandemic, but some are now coming back online. In fact, “we are getting all these pleas from sites around the country saying, ‘Hey, once LATITUDE is open for enrollment, we have so many people who would now be eligible’,” she told Medscape Medical News.
“Why are they now eligible and they weren’t eligible before? I’m assuming it’s because they now have a detectable viral load,” which is one of the requirements for enrollment in LATITUDE, she explained.
Impact on the LGBTI community
At the onset of the COVID-19 pandemic, Erik Lamontagne, senior economist at UNAIDS, wondered how the quarantine was affecting LGBTI people.
To find out, he and his colleagues launched a survey asking just that. He is also coprinciple investigator of the LGBT Happiness Survey, a multicountry survey of LGBTI people launched last year.
The 13,562 LGBTI respondents came from 138 countries or territories. Of the 1,140 respondents living with HIV, 26% had seen their HIV care disrupted or restricted in some way during the pandemic, and 55% of those had no more than a month’s worth of HIV medications on hand.
But the pandemic hasn’t just affected people already living with HIV, Mr. Lamontagne reported. Nine of 10 respondents were living under some form of stay-at-home order, 73% were not meeting their basic needs, 37% had missed meals as a result of economic hardship, and half of those who were still working expected to lose their jobs.
Many could not afford to quarantine, Mr. Lamontagne told Medscape Medical News. And financial resources were stretched so thin that about 1% of respondents reported engaging in transactional sex for the first time. Some reported that their economic circumstances were so dire that they couldn’t require clients to wear condoms, increasing their risk for both COVID-19 and HIV.
“What they can eat in the evening is what they can earn during the day,” Mr. Lamontagne explained.
Unfortunately, it is the people already in a situation of economic vulnerability – often those from the LGBTI community – who are most affected by COVID-19, he added.
PrEP use changing
The pandemic has also affected the use of pre-exposure prophylaxis (PrEP).
South African women taking PrEP to protect themselves from HIV during pregnancy were 2.36 times more likely to miss a clinic visit to refill their prescription after COVID-19 lockdowns began than before, data presented at the conference showed. The women cited fear of acquiring COVID-19 at the medical facility, fear of police, transportation barriers, and long clinic wait times to explain the missed visits.
A study on the use of PrEP at Fenway Health, a sexual health clinic in Boston, showed a 278% increase in unfilled PrEP prescriptions after stay-at-home orders and a 72.1% drop in new PrEP prescriptions.
It’s unclear what these data, which will be presented at the conference later this week, mean, said Douglas Krakower, MD, assistant professor of medicine and population medicine at Harvard Medical School in Boston.
“We don’t know whether this represents people having trouble accessing PrEP” out of concern about getting COVID “or concerns about financial implications,” he explained.
“They may have had hardships from unemployment or other financial constraints” and have lost insurance or are still having to pay copays, he told Medscape Medical News. Or it could just be that they’re not going out or having sex, so they’ve discontinued the medication.
“Anecdotally we’ve heard that some patients are sheltering in place and not having sex and so have chosen not to use PrEP,” he added.
It’s also possible that people are rationing pills or have moved themselves to the PrEP 2-1-1 protocol, which is used only when someone is having sex, said Dr. Krakower, citing a study showing that sexual behavior is continuing as usual during quarantine for about half the gay men in the United States.
Resilience and fragility
It’s not just people living with HIV whose routines have changed during the pandemic. A survey of HIV clinicians around the world conducted by the International Association of Providers of AIDS Care showed that 88% of HIV clinicians have been pulled away from their regular work to manage COVID-19 in their communities.
But the COVID-19 pandemic shows no signs of stopping, and clinicians are now having to re-engage with their HIV patients.
“What COVID-19 has represented for us is a looking glass to see the resilience, but also the fragility, in HIV responses, not just in the global south, but also in the global north,” José Zuniga, PhD, IAPAC president and chief executive officer, said during a preconference session on controlling the HIV epidemic.
For Dr. Dionne-Odom, reopening the 1917 Clinic in Alabama meant tracking down patients who could not participate in telemedicine. Fortunately (or unfortunately, depending on how you look at it), the clinic, which serves a population with a high level of economic insecurity, has worked to get as many phone numbers as possible for each patient. So when the clinic opened back up, staff was able to call family members, friends, and trusted contacts to bring their patients back into the clinic.
“No one wanted to reopen too quickly,” said Dr. Dionne-Odom. “But having people come in allowed us to do all the other things that are the key part of HIV care: getting them connected with a social worker and making sure they have enough food, helping them with their electricity bills and their housing issues, all the wrap-around services that are so crucial for these patients.”
This article first appeared on Medscape.com.