User login
For MD-IQ on Family Practice News, but a regular topic for Rheumatology News
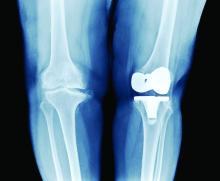
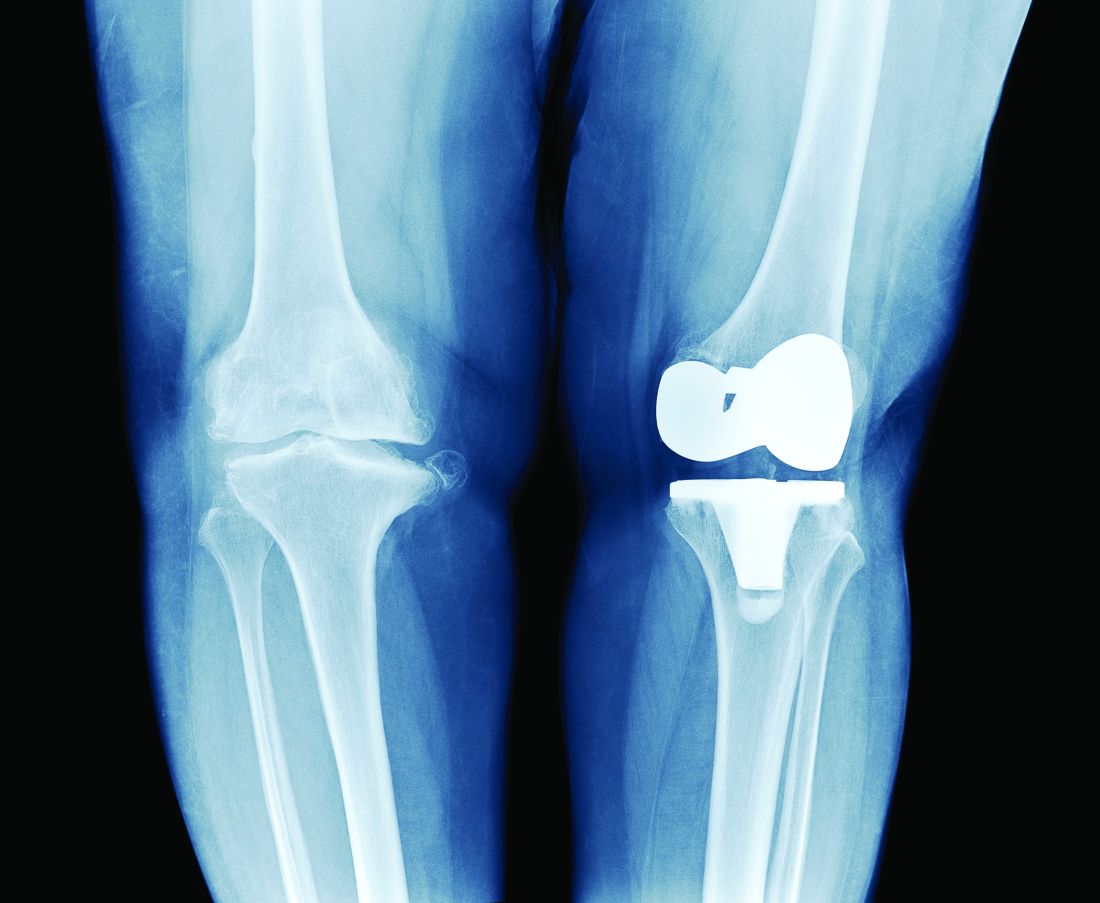
PT may lower risk of long-term opioid use after knee replacement
A new study has found that physical therapy may lead to a reduced risk of long-term opioid use in patients who have undergone total knee replacement (TKR).
“Greater number of PT intervention sessions and earlier initiation of outpatient PT care after TKR were associated with lower odds of long-term opioid use,” authors from Boston University wrote in their report on the study, which was published online Oct. 27 in JAMA Network Open.
“In previous large studies, we’ve seen that physical therapy can reduce pain in people with knee osteoarthritis, which is usually the primary indication for TKR,” study coauthor Deepak Kumar, PT, PhD, said in an interview. “But the association of physical therapy with opioid use in people with knee replacement has not yet been explored.
“The reason we focused on opioid use in these patients is because the number of knee replacement surgeries is going up exponentially,” Dr. Kumar said. “And, depending on which data you look at, from one-third to up to half of people who undergo knee replacement and have used opioids before end up becoming long-term users. Even in people who have not used them before, 5%-8% become long-term users after the surgery.
“Given how many surgeries are happening – and that number is expected to keep going up – the number of people who are becoming long-term opioid users is not trivial,” he said.
Study details
To assess the value of PT in reducing opioid use in this subset of patients, the authors reviewed records from the OptumLabs Data Warehouse insurance claims database to identify 67,322 eligible participants aged 40 or older who underwent TKR from Jan. 1, 2001, to Dec. 31, 2016. Of those patients, 38,408 were opioid naive and 28,914 had taken opioids before. The authors evaluated long-term opioid use – defined as 90 days or more of filled prescriptions – during a 12-month outcome assessment period that varied depending on differences in post-TKR PT start date and duration.
The researchers found a significantly lower likelihood of long-term opioid use associated with receipt of any PT before TKR among patients who had not taken opioids before (adjusted odds ratio [aOR], 0.75; 95% confidence interval, 0.60-0.95) and those who had taken opioids in the past (aOR, 0.75; 95% CI, 0.70-0.80).
Investigators found that 2.2% of participants in the opioid-naive group and 32.5% of those in the opioid-experienced group used opioids long-term after TKR. Approximately 76% of participants overall received outpatient PT within the 90 days after surgery, and the receipt of post-TKR PT at any point was associated with lower odds of long-term opioid use in the opioid-experienced group (aOR, 0.75; 95% CI, 0.70-0.79).
Among the opioid-experienced group, receiving between 6 and 12 PT sessions (aOR, 0.82; 95% CI, 0.75-0.90) or ≥ 13 sessions (aOR, 0.71; 95% CI, 0.65-0.77) were both associated with lower odds of long-term opioid use, compared with those who received 1-5 sessions. Beginning PT 31-60 days or 61-90 days after surgery was associated with greater odds of long-term opioid use across both cohorts, compared with those who initiated therapy within 30 days of TKR.
Physical therapy: Underexplored option for pain in knee replacement
One finding caught the researchers slightly off guard: There was no association between active physical therapy and reduced odds of long-term opioid use. “From prior studies, at least in people with knee osteoarthritis, we know that active interventions were more useful than passive interventions,” Dr. Kumar said.
That said, he added that there is still some professional uncertainty regarding “the right type or the right components of physical therapy for managing pain in this population.” Regardless, he believes their study emphasizes the benefits of PT as a pain alleviator in these patients, especially those who have previously used opioids.
“Pharmaceuticals have side effects. Injections are not super effective,” he said. “The idea behind focusing on physical therapy interventions is that it’s widely available, it does you no harm, and it could potentially be lower cost to both the payers and the providers.”
The authors acknowledged their study’s limitations, including not adjusting for opioid use within the 90 days after surgery as well as the different outcome assessment periods for pre-TKR and post-TKR PT exposures. In addition, they admitted that some of the patients who received PT could have been among those less likely to be treated with opioids, and vice versa. “A randomized clinical trial,” they wrote, “would be required to disentangle these issues.”
The study was supported by grants from the National Institutes of Health and the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Kumar reported receiving grants from the National Institutes of Health during the conduct of the study and grants from Pfizer for unrelated projects outside the submitted work. The full list of author disclosures can be found with the original article.
A version of this article first appeared on Medscape.com.
A new study has found that physical therapy may lead to a reduced risk of long-term opioid use in patients who have undergone total knee replacement (TKR).
“Greater number of PT intervention sessions and earlier initiation of outpatient PT care after TKR were associated with lower odds of long-term opioid use,” authors from Boston University wrote in their report on the study, which was published online Oct. 27 in JAMA Network Open.
“In previous large studies, we’ve seen that physical therapy can reduce pain in people with knee osteoarthritis, which is usually the primary indication for TKR,” study coauthor Deepak Kumar, PT, PhD, said in an interview. “But the association of physical therapy with opioid use in people with knee replacement has not yet been explored.
“The reason we focused on opioid use in these patients is because the number of knee replacement surgeries is going up exponentially,” Dr. Kumar said. “And, depending on which data you look at, from one-third to up to half of people who undergo knee replacement and have used opioids before end up becoming long-term users. Even in people who have not used them before, 5%-8% become long-term users after the surgery.
“Given how many surgeries are happening – and that number is expected to keep going up – the number of people who are becoming long-term opioid users is not trivial,” he said.
Study details
To assess the value of PT in reducing opioid use in this subset of patients, the authors reviewed records from the OptumLabs Data Warehouse insurance claims database to identify 67,322 eligible participants aged 40 or older who underwent TKR from Jan. 1, 2001, to Dec. 31, 2016. Of those patients, 38,408 were opioid naive and 28,914 had taken opioids before. The authors evaluated long-term opioid use – defined as 90 days or more of filled prescriptions – during a 12-month outcome assessment period that varied depending on differences in post-TKR PT start date and duration.
The researchers found a significantly lower likelihood of long-term opioid use associated with receipt of any PT before TKR among patients who had not taken opioids before (adjusted odds ratio [aOR], 0.75; 95% confidence interval, 0.60-0.95) and those who had taken opioids in the past (aOR, 0.75; 95% CI, 0.70-0.80).
Investigators found that 2.2% of participants in the opioid-naive group and 32.5% of those in the opioid-experienced group used opioids long-term after TKR. Approximately 76% of participants overall received outpatient PT within the 90 days after surgery, and the receipt of post-TKR PT at any point was associated with lower odds of long-term opioid use in the opioid-experienced group (aOR, 0.75; 95% CI, 0.70-0.79).
Among the opioid-experienced group, receiving between 6 and 12 PT sessions (aOR, 0.82; 95% CI, 0.75-0.90) or ≥ 13 sessions (aOR, 0.71; 95% CI, 0.65-0.77) were both associated with lower odds of long-term opioid use, compared with those who received 1-5 sessions. Beginning PT 31-60 days or 61-90 days after surgery was associated with greater odds of long-term opioid use across both cohorts, compared with those who initiated therapy within 30 days of TKR.
Physical therapy: Underexplored option for pain in knee replacement
One finding caught the researchers slightly off guard: There was no association between active physical therapy and reduced odds of long-term opioid use. “From prior studies, at least in people with knee osteoarthritis, we know that active interventions were more useful than passive interventions,” Dr. Kumar said.
That said, he added that there is still some professional uncertainty regarding “the right type or the right components of physical therapy for managing pain in this population.” Regardless, he believes their study emphasizes the benefits of PT as a pain alleviator in these patients, especially those who have previously used opioids.
“Pharmaceuticals have side effects. Injections are not super effective,” he said. “The idea behind focusing on physical therapy interventions is that it’s widely available, it does you no harm, and it could potentially be lower cost to both the payers and the providers.”
The authors acknowledged their study’s limitations, including not adjusting for opioid use within the 90 days after surgery as well as the different outcome assessment periods for pre-TKR and post-TKR PT exposures. In addition, they admitted that some of the patients who received PT could have been among those less likely to be treated with opioids, and vice versa. “A randomized clinical trial,” they wrote, “would be required to disentangle these issues.”
The study was supported by grants from the National Institutes of Health and the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Kumar reported receiving grants from the National Institutes of Health during the conduct of the study and grants from Pfizer for unrelated projects outside the submitted work. The full list of author disclosures can be found with the original article.
A version of this article first appeared on Medscape.com.
A new study has found that physical therapy may lead to a reduced risk of long-term opioid use in patients who have undergone total knee replacement (TKR).
“Greater number of PT intervention sessions and earlier initiation of outpatient PT care after TKR were associated with lower odds of long-term opioid use,” authors from Boston University wrote in their report on the study, which was published online Oct. 27 in JAMA Network Open.
“In previous large studies, we’ve seen that physical therapy can reduce pain in people with knee osteoarthritis, which is usually the primary indication for TKR,” study coauthor Deepak Kumar, PT, PhD, said in an interview. “But the association of physical therapy with opioid use in people with knee replacement has not yet been explored.
“The reason we focused on opioid use in these patients is because the number of knee replacement surgeries is going up exponentially,” Dr. Kumar said. “And, depending on which data you look at, from one-third to up to half of people who undergo knee replacement and have used opioids before end up becoming long-term users. Even in people who have not used them before, 5%-8% become long-term users after the surgery.
“Given how many surgeries are happening – and that number is expected to keep going up – the number of people who are becoming long-term opioid users is not trivial,” he said.
Study details
To assess the value of PT in reducing opioid use in this subset of patients, the authors reviewed records from the OptumLabs Data Warehouse insurance claims database to identify 67,322 eligible participants aged 40 or older who underwent TKR from Jan. 1, 2001, to Dec. 31, 2016. Of those patients, 38,408 were opioid naive and 28,914 had taken opioids before. The authors evaluated long-term opioid use – defined as 90 days or more of filled prescriptions – during a 12-month outcome assessment period that varied depending on differences in post-TKR PT start date and duration.
The researchers found a significantly lower likelihood of long-term opioid use associated with receipt of any PT before TKR among patients who had not taken opioids before (adjusted odds ratio [aOR], 0.75; 95% confidence interval, 0.60-0.95) and those who had taken opioids in the past (aOR, 0.75; 95% CI, 0.70-0.80).
Investigators found that 2.2% of participants in the opioid-naive group and 32.5% of those in the opioid-experienced group used opioids long-term after TKR. Approximately 76% of participants overall received outpatient PT within the 90 days after surgery, and the receipt of post-TKR PT at any point was associated with lower odds of long-term opioid use in the opioid-experienced group (aOR, 0.75; 95% CI, 0.70-0.79).
Among the opioid-experienced group, receiving between 6 and 12 PT sessions (aOR, 0.82; 95% CI, 0.75-0.90) or ≥ 13 sessions (aOR, 0.71; 95% CI, 0.65-0.77) were both associated with lower odds of long-term opioid use, compared with those who received 1-5 sessions. Beginning PT 31-60 days or 61-90 days after surgery was associated with greater odds of long-term opioid use across both cohorts, compared with those who initiated therapy within 30 days of TKR.
Physical therapy: Underexplored option for pain in knee replacement
One finding caught the researchers slightly off guard: There was no association between active physical therapy and reduced odds of long-term opioid use. “From prior studies, at least in people with knee osteoarthritis, we know that active interventions were more useful than passive interventions,” Dr. Kumar said.
That said, he added that there is still some professional uncertainty regarding “the right type or the right components of physical therapy for managing pain in this population.” Regardless, he believes their study emphasizes the benefits of PT as a pain alleviator in these patients, especially those who have previously used opioids.
“Pharmaceuticals have side effects. Injections are not super effective,” he said. “The idea behind focusing on physical therapy interventions is that it’s widely available, it does you no harm, and it could potentially be lower cost to both the payers and the providers.”
The authors acknowledged their study’s limitations, including not adjusting for opioid use within the 90 days after surgery as well as the different outcome assessment periods for pre-TKR and post-TKR PT exposures. In addition, they admitted that some of the patients who received PT could have been among those less likely to be treated with opioids, and vice versa. “A randomized clinical trial,” they wrote, “would be required to disentangle these issues.”
The study was supported by grants from the National Institutes of Health and the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Kumar reported receiving grants from the National Institutes of Health during the conduct of the study and grants from Pfizer for unrelated projects outside the submitted work. The full list of author disclosures can be found with the original article.
A version of this article first appeared on Medscape.com.
PRP injections don’t top placebo for ankle osteoarthritis
Platelet-rich plasma (PRP) injections did not significantly improve pain or function when compared with placebo injections in patients with ankle osteoarthritis (OA), a new study has found.
“Previous evidence for PRP injections in ankle osteoarthritis was limited to 4 small case series with methodological flaws,” wrote Liam D. A. Paget, MD, of the University of Amsterdam, and coauthors. The study was published online Oct. 26 in JAMA.
To assess the value of PRP injections as a treatment for ankle OA, the researchers launched a double-blind, randomized clinical trial of Dutch patients with notable ankle pain and tibiotalar joint space narrowing. From six sites in the Netherlands, 100 patients (45% women, mean age 56 years) were split into two groups: one that received two intra-articular injections of PRP 6 weeks apart (n = 48) and one that received two injections of saline placebo (n = 52).
At baseline, mean American Orthopaedic Foot and Ankle Society (AOFAS) scores were 63 in the PRP group and 64 in the placebo group (range 0-100, with higher scores indicating less pain and more function). At 26-week follow-up, the mean AOFAS score improved by 10 points in the PRP group (95% confidence interval, 6-14; P < .001) and by 11 points in the placebo group (95% CI, 7-15; P < .001). The adjusted between-group difference for AOFAS improvement over 26 weeks was –1 point (95% CI, –6 to 3; P = .56).
There was one serious adverse event in the placebo group – a transient ischemic attack 3 weeks after the first injection – but it was deemed unrelated.
Searching for answers regarding PRP and osteoarthritis
“From my standpoint, this study is a great step forward to where the field needs to be, which is honing in on longer-term studies that are standardizing PRP and teasing out its effects,” Prathap Jayaram, MD, director of regenerative sports medicine at the Baylor College of Medicine in Houston, said in an interview.
He highlighted the authors’ acknowledgment of previous studies in which PRP injections appeared effective in treating knee OA, including their statement that the “results reported here for ankle osteoarthritis were not consistent with these potentially beneficial effects in knee osteoarthritis.”
“They’re acknowledging that this does have some benefit in knees,” he said. “Could that translate toward the ankle?”
“PRP did lead to an improvement,” he added. “There just wasn’t a big enough difference to say one was superior to the other.”
Citing his team’s recent preclinical study that was published in Osteoarthritis and Cartilage, Dr. Jayaram emphasized the possibility that PRP could have much-needed disease-modifying effects in osteoarthritis. More work is needed to pin down the details.
“We need more mechanistic studies to be done so we can actually identify the therapeutic properties in PRP and leverage them to track reproducible outcomes,” he said, adding that “simply put, your blood and my blood might be different. There is going to be heterogeneity there. The analogy I give my patients is, when they take an antibiotic, we have a specific dose, a specific drug, and a specific duration. It’s very standardized. We’re just not there yet with PRP.”
The authors acknowledged their study’s limitations, including a likely inability to generalize their results to other platelet-rich blood products as well as a lack of composition analysis of the PRP they used. That said, they added that this particular PRP has been “analyzed previously” for another trial and noted that such analysis is not typically performed in a clinical setting.
The study was supported by a grant from the Dutch Arthritis Society. Its authors reported several potential conflicts of interest, including receiving their own grants from the Dutch Arthritis Society and other organizations, as well as accepting loaned Hettich centrifuges from a medical device company for the study.
A version of this article first appeared on Medscape.com.
Platelet-rich plasma (PRP) injections did not significantly improve pain or function when compared with placebo injections in patients with ankle osteoarthritis (OA), a new study has found.
“Previous evidence for PRP injections in ankle osteoarthritis was limited to 4 small case series with methodological flaws,” wrote Liam D. A. Paget, MD, of the University of Amsterdam, and coauthors. The study was published online Oct. 26 in JAMA.
To assess the value of PRP injections as a treatment for ankle OA, the researchers launched a double-blind, randomized clinical trial of Dutch patients with notable ankle pain and tibiotalar joint space narrowing. From six sites in the Netherlands, 100 patients (45% women, mean age 56 years) were split into two groups: one that received two intra-articular injections of PRP 6 weeks apart (n = 48) and one that received two injections of saline placebo (n = 52).
At baseline, mean American Orthopaedic Foot and Ankle Society (AOFAS) scores were 63 in the PRP group and 64 in the placebo group (range 0-100, with higher scores indicating less pain and more function). At 26-week follow-up, the mean AOFAS score improved by 10 points in the PRP group (95% confidence interval, 6-14; P < .001) and by 11 points in the placebo group (95% CI, 7-15; P < .001). The adjusted between-group difference for AOFAS improvement over 26 weeks was –1 point (95% CI, –6 to 3; P = .56).
There was one serious adverse event in the placebo group – a transient ischemic attack 3 weeks after the first injection – but it was deemed unrelated.
Searching for answers regarding PRP and osteoarthritis
“From my standpoint, this study is a great step forward to where the field needs to be, which is honing in on longer-term studies that are standardizing PRP and teasing out its effects,” Prathap Jayaram, MD, director of regenerative sports medicine at the Baylor College of Medicine in Houston, said in an interview.
He highlighted the authors’ acknowledgment of previous studies in which PRP injections appeared effective in treating knee OA, including their statement that the “results reported here for ankle osteoarthritis were not consistent with these potentially beneficial effects in knee osteoarthritis.”
“They’re acknowledging that this does have some benefit in knees,” he said. “Could that translate toward the ankle?”
“PRP did lead to an improvement,” he added. “There just wasn’t a big enough difference to say one was superior to the other.”
Citing his team’s recent preclinical study that was published in Osteoarthritis and Cartilage, Dr. Jayaram emphasized the possibility that PRP could have much-needed disease-modifying effects in osteoarthritis. More work is needed to pin down the details.
“We need more mechanistic studies to be done so we can actually identify the therapeutic properties in PRP and leverage them to track reproducible outcomes,” he said, adding that “simply put, your blood and my blood might be different. There is going to be heterogeneity there. The analogy I give my patients is, when they take an antibiotic, we have a specific dose, a specific drug, and a specific duration. It’s very standardized. We’re just not there yet with PRP.”
The authors acknowledged their study’s limitations, including a likely inability to generalize their results to other platelet-rich blood products as well as a lack of composition analysis of the PRP they used. That said, they added that this particular PRP has been “analyzed previously” for another trial and noted that such analysis is not typically performed in a clinical setting.
The study was supported by a grant from the Dutch Arthritis Society. Its authors reported several potential conflicts of interest, including receiving their own grants from the Dutch Arthritis Society and other organizations, as well as accepting loaned Hettich centrifuges from a medical device company for the study.
A version of this article first appeared on Medscape.com.
Platelet-rich plasma (PRP) injections did not significantly improve pain or function when compared with placebo injections in patients with ankle osteoarthritis (OA), a new study has found.
“Previous evidence for PRP injections in ankle osteoarthritis was limited to 4 small case series with methodological flaws,” wrote Liam D. A. Paget, MD, of the University of Amsterdam, and coauthors. The study was published online Oct. 26 in JAMA.
To assess the value of PRP injections as a treatment for ankle OA, the researchers launched a double-blind, randomized clinical trial of Dutch patients with notable ankle pain and tibiotalar joint space narrowing. From six sites in the Netherlands, 100 patients (45% women, mean age 56 years) were split into two groups: one that received two intra-articular injections of PRP 6 weeks apart (n = 48) and one that received two injections of saline placebo (n = 52).
At baseline, mean American Orthopaedic Foot and Ankle Society (AOFAS) scores were 63 in the PRP group and 64 in the placebo group (range 0-100, with higher scores indicating less pain and more function). At 26-week follow-up, the mean AOFAS score improved by 10 points in the PRP group (95% confidence interval, 6-14; P < .001) and by 11 points in the placebo group (95% CI, 7-15; P < .001). The adjusted between-group difference for AOFAS improvement over 26 weeks was –1 point (95% CI, –6 to 3; P = .56).
There was one serious adverse event in the placebo group – a transient ischemic attack 3 weeks after the first injection – but it was deemed unrelated.
Searching for answers regarding PRP and osteoarthritis
“From my standpoint, this study is a great step forward to where the field needs to be, which is honing in on longer-term studies that are standardizing PRP and teasing out its effects,” Prathap Jayaram, MD, director of regenerative sports medicine at the Baylor College of Medicine in Houston, said in an interview.
He highlighted the authors’ acknowledgment of previous studies in which PRP injections appeared effective in treating knee OA, including their statement that the “results reported here for ankle osteoarthritis were not consistent with these potentially beneficial effects in knee osteoarthritis.”
“They’re acknowledging that this does have some benefit in knees,” he said. “Could that translate toward the ankle?”
“PRP did lead to an improvement,” he added. “There just wasn’t a big enough difference to say one was superior to the other.”
Citing his team’s recent preclinical study that was published in Osteoarthritis and Cartilage, Dr. Jayaram emphasized the possibility that PRP could have much-needed disease-modifying effects in osteoarthritis. More work is needed to pin down the details.
“We need more mechanistic studies to be done so we can actually identify the therapeutic properties in PRP and leverage them to track reproducible outcomes,” he said, adding that “simply put, your blood and my blood might be different. There is going to be heterogeneity there. The analogy I give my patients is, when they take an antibiotic, we have a specific dose, a specific drug, and a specific duration. It’s very standardized. We’re just not there yet with PRP.”
The authors acknowledged their study’s limitations, including a likely inability to generalize their results to other platelet-rich blood products as well as a lack of composition analysis of the PRP they used. That said, they added that this particular PRP has been “analyzed previously” for another trial and noted that such analysis is not typically performed in a clinical setting.
The study was supported by a grant from the Dutch Arthritis Society. Its authors reported several potential conflicts of interest, including receiving their own grants from the Dutch Arthritis Society and other organizations, as well as accepting loaned Hettich centrifuges from a medical device company for the study.
A version of this article first appeared on Medscape.com.
Tramadol linked to higher risk of mortality, compared with codeine
Tramadol is increasingly used to manage chronic noncancer pain, but as compared with opioids, it appears to be linked to a higher risk for adverse outcomes, according to new data.
Among a cohort of patients who received a prescription for either tramadol or codeine for orthopedic-related pain, tramadol was significantly associated with a higher risk of mortality, cardiovascular events, and fractures.
However, there was no significant difference in the risk of falls, delirium, constipation, opioid abuse/dependence, or sleep disorders between the two drugs.
“However, this is a retrospective cohort study, and despite it providing information that would otherwise be impossible to gather – such as from randomized controlled trials – clinicians should not solely base their decision on this study,” cautioned lead author Carlen Reyes, MD, PhD, of the Institut Universitari d’Investigació en Atenció Primària (IDIAP Jordi Gol), Barcelona.
Dr. Reyes noted that the intake of tramadol and codeine was analyzed using the number of “packages” that were dispensed, as an approximation of the real intake. “Logically we could think that the more packages dispensed of one drug, the more dose the patient is taking, but this is not always true given the availability of different doses commercialized of tramadol and different doses prescribed,” she said. “Given that we did not account for the real dose prescribed, we can only suspect an increased risk of these outcomes and reinforce the need for further prospective studies with more specific dose-response analysis comparing tramadol and codeine.”
The paper was published Oct. 19 in JAMA.
Tramadol has been considered to be a relatively safe opioid and was even strongly recommended by the American Academy of Orthopaedic Surgeons for patients experiencing symptomatic knee osteoarthritis. The authors point out that studies looking at opioid use from 2019 to 2020 show that tramadol was the most prescribed opioid in England, the Netherlands, and Spain.
In the United States, the age-adjusted rate of drug overdose deaths from synthetic opioids rose from 1.0 per 100 000 in 2013 to 11.4 in 2019. Most of these deaths were attributable to fentanyl but some were also related to tramadol.
But despite its wide use in managing chronic noncancer pain, results of recent studies suggest adverse outcomes as compared with other agents. Last year, one study found that older patients who received tramadol had a significant increase in the risk of hip fracture vs. those using NSAIDs or codeine. Another study, also published in 2020, showed that patients with osteoarthritis who were treated with tramadol had a 20%-50% higher risk of dying during the first year of treatment than did patients who were treated with NSAIDs.
In the current paper, Dr. Reyes and colleagues evaluated the association of tramadol with mortality and other adverse clinical outcomes in outpatient settings, compared with codeine.
They conducted a retrospective, population-based, propensity score–matched cohort study using a primary care database that routinely collects medical records and pharmacy dispensations for more than 80% of the population of Catalonia, Spain. The cohort included people 18 years or older who had been prescribed tramadol or codeine from 2007 to 2017 and were followed up to Dec. 31, 2017.
After propensity score matching, the final analysis included 368,960 participants: 184,480 in the tramadol arm and 184,480 in the codeine arm.
The mean age of patients was 52.7 years in the tramadol arm and 53.5 years in the codeine arm, and the prevalence of cancer was 3.2% and 3.3%, respectively. The most common diagnoses in this cohort were back pain (47.5% vs. 48.5%), neck/shoulder pain (28.6% vs. 29.5%), and osteoarthritis (15.3% vs. 15.5%). The most commonly used drugs were ibuprofen (34.4% vs. 34.3%) and paracetamol/acetaminophen (37.1% vs. 36.8%)
Higher risk of adverse outcomes
As compared with codeine, tramadol use was significantly associated with a higher risk of mortality (13.00 vs. 5.61 per 1,000 person-years; hazard ratio, 2.31; 95% confidence interval, 2.08-2.56); absolute rate differences (7.37 per 1,000 person-years; 95% CI, 6.09-8.78), cardiovascular events (10.03 vs. 8.67 per 1,000 person-years; HR, 1.15; 95% CI, 1.05-1.27; ARD, 1.36 per 1,000 person-years; 95% CI, 0.45-2.36), and fractures (12.26 vs. 8.13 per 1,000 person-years; HR, 1.50; 95% CI, 1.37-1.65; ARD, 4.10 per 1,000 person-years; 95% CI, 3.02-5.29).
A subgroup and sensitivity analysis showed that the increased mortality risk associated with tramadol was significantly higher in younger persons vs. older ones (HR, 3.14; 95% CI, 1.82-5.41 vs. 2.39; 95% CI, 2.20-2.60]; P < .001 for interaction). In addition, women had a significantly greater risk of cardiovascular events versus men (HR, 1.32; 95% CI, 1.19-1.46] vs. 1.03; 95% CI, 0.9-1.13]; P < .001 for interaction).
Potential for confounding
Weighing in on the data, Daniel Solomon, MD, MPH, chief of clinical sciences, division of rheumatology, Brigham and Women’s Hospital, and professor of medicine, Harvard Medical School, Boston, noted that because it is extremely unlikely that anyone will ever conduct a large, head-to-head safety trial comparing different opioids, the results of this paper are important to consider.
“However, as the authors appropriately caution, this type of analysis is limited by the strong potential for residual confounding,” he said. “In other words, even though the authors used state-of-the-art methods to limit imbalances between the patients initiating tramadol versus codeine, there is strong reason to believe that imbalances that may account for the differences in adverse events exist.”
For example, he noted that if one looks at the distribution of comorbid conditions in the before-matching group, tramadol initiators demonstrate a higher frequency of chronic kidney disease, diabetes, and overall chronic comorbid diseases. “This suggests to me that prescribers apply selection criteria when choosing who to prescribe which opioid,” Dr. Solomon explained.
“While the authors’ use of propensity score matching limits confounding, it only can improve balance for measured confounders,” he said. “Other factors not measured in this type of data set – blood pressure, pain, physical activity, tobacco use, body mass index – may still demonstrate imbalances even after matching.”
But after these limitations are taken into consideration, the results remain concerning, Dr. Solomon emphasized, particularly the all-cause mortality excess of tramadol versus codeine users. “This study did not include cause of death, which would help the reader understand why users of tramadol were dying more frequently,” he added. “It also might help in understanding whether this is a true biologic effect or residual confounding.”
Perceived safety
In an accompanying editorial, Howard S. Kim, MD, MS, and colleagues from Northwestern University, Chicago, write that the greatest risk of tramadol may involve the perception that it is “inherently safer than other opioids.”
“In actuality, the mechanisms of action and variable metabolism of tramadol in a given population create considerable therapeutic uncertainty and introduce additional risk exposure,” they say, as demonstrated in the current study.
Therefore, when clinicians determine that an opioid is needed for pain relief, it may be a better option to select a pure opioid agonist that has a more predictable therapeutic effect and known adverse effect profile, such as morphine or hydrocodone. “This would allow clinicians and patients to more properly weigh the risks and benefits of initiating opioid therapy through shared decision-making and prompt the level of counseling on safe use, storage, and disposal practices that all opioids deserve,” write the editorialists.
The study was funded by the Fundació Institut Universitari per a la recerca a l’Atenció Primària de Salut Jordi Gol i Gurina. The research was supported by the National Institute for Health Research Oxford Biomedical Research Centre. Dr. Reyes has disclosed no relevant financial relationships. Dr. Solomon disclosed salary support from research contracts to his hospital from Amgen, AbbVie, Moderna, the Rheumatology Research Foundation, and National Institutes of Health; and royalties from UpToDate. Dr. Kim reported unrelated grant support from the Agency for Healthcare Research and Quality.
A version of this article first appeared on Medscape.com.
Tramadol is increasingly used to manage chronic noncancer pain, but as compared with opioids, it appears to be linked to a higher risk for adverse outcomes, according to new data.
Among a cohort of patients who received a prescription for either tramadol or codeine for orthopedic-related pain, tramadol was significantly associated with a higher risk of mortality, cardiovascular events, and fractures.
However, there was no significant difference in the risk of falls, delirium, constipation, opioid abuse/dependence, or sleep disorders between the two drugs.
“However, this is a retrospective cohort study, and despite it providing information that would otherwise be impossible to gather – such as from randomized controlled trials – clinicians should not solely base their decision on this study,” cautioned lead author Carlen Reyes, MD, PhD, of the Institut Universitari d’Investigació en Atenció Primària (IDIAP Jordi Gol), Barcelona.
Dr. Reyes noted that the intake of tramadol and codeine was analyzed using the number of “packages” that were dispensed, as an approximation of the real intake. “Logically we could think that the more packages dispensed of one drug, the more dose the patient is taking, but this is not always true given the availability of different doses commercialized of tramadol and different doses prescribed,” she said. “Given that we did not account for the real dose prescribed, we can only suspect an increased risk of these outcomes and reinforce the need for further prospective studies with more specific dose-response analysis comparing tramadol and codeine.”
The paper was published Oct. 19 in JAMA.
Tramadol has been considered to be a relatively safe opioid and was even strongly recommended by the American Academy of Orthopaedic Surgeons for patients experiencing symptomatic knee osteoarthritis. The authors point out that studies looking at opioid use from 2019 to 2020 show that tramadol was the most prescribed opioid in England, the Netherlands, and Spain.
In the United States, the age-adjusted rate of drug overdose deaths from synthetic opioids rose from 1.0 per 100 000 in 2013 to 11.4 in 2019. Most of these deaths were attributable to fentanyl but some were also related to tramadol.
But despite its wide use in managing chronic noncancer pain, results of recent studies suggest adverse outcomes as compared with other agents. Last year, one study found that older patients who received tramadol had a significant increase in the risk of hip fracture vs. those using NSAIDs or codeine. Another study, also published in 2020, showed that patients with osteoarthritis who were treated with tramadol had a 20%-50% higher risk of dying during the first year of treatment than did patients who were treated with NSAIDs.
In the current paper, Dr. Reyes and colleagues evaluated the association of tramadol with mortality and other adverse clinical outcomes in outpatient settings, compared with codeine.
They conducted a retrospective, population-based, propensity score–matched cohort study using a primary care database that routinely collects medical records and pharmacy dispensations for more than 80% of the population of Catalonia, Spain. The cohort included people 18 years or older who had been prescribed tramadol or codeine from 2007 to 2017 and were followed up to Dec. 31, 2017.
After propensity score matching, the final analysis included 368,960 participants: 184,480 in the tramadol arm and 184,480 in the codeine arm.
The mean age of patients was 52.7 years in the tramadol arm and 53.5 years in the codeine arm, and the prevalence of cancer was 3.2% and 3.3%, respectively. The most common diagnoses in this cohort were back pain (47.5% vs. 48.5%), neck/shoulder pain (28.6% vs. 29.5%), and osteoarthritis (15.3% vs. 15.5%). The most commonly used drugs were ibuprofen (34.4% vs. 34.3%) and paracetamol/acetaminophen (37.1% vs. 36.8%)
Higher risk of adverse outcomes
As compared with codeine, tramadol use was significantly associated with a higher risk of mortality (13.00 vs. 5.61 per 1,000 person-years; hazard ratio, 2.31; 95% confidence interval, 2.08-2.56); absolute rate differences (7.37 per 1,000 person-years; 95% CI, 6.09-8.78), cardiovascular events (10.03 vs. 8.67 per 1,000 person-years; HR, 1.15; 95% CI, 1.05-1.27; ARD, 1.36 per 1,000 person-years; 95% CI, 0.45-2.36), and fractures (12.26 vs. 8.13 per 1,000 person-years; HR, 1.50; 95% CI, 1.37-1.65; ARD, 4.10 per 1,000 person-years; 95% CI, 3.02-5.29).
A subgroup and sensitivity analysis showed that the increased mortality risk associated with tramadol was significantly higher in younger persons vs. older ones (HR, 3.14; 95% CI, 1.82-5.41 vs. 2.39; 95% CI, 2.20-2.60]; P < .001 for interaction). In addition, women had a significantly greater risk of cardiovascular events versus men (HR, 1.32; 95% CI, 1.19-1.46] vs. 1.03; 95% CI, 0.9-1.13]; P < .001 for interaction).
Potential for confounding
Weighing in on the data, Daniel Solomon, MD, MPH, chief of clinical sciences, division of rheumatology, Brigham and Women’s Hospital, and professor of medicine, Harvard Medical School, Boston, noted that because it is extremely unlikely that anyone will ever conduct a large, head-to-head safety trial comparing different opioids, the results of this paper are important to consider.
“However, as the authors appropriately caution, this type of analysis is limited by the strong potential for residual confounding,” he said. “In other words, even though the authors used state-of-the-art methods to limit imbalances between the patients initiating tramadol versus codeine, there is strong reason to believe that imbalances that may account for the differences in adverse events exist.”
For example, he noted that if one looks at the distribution of comorbid conditions in the before-matching group, tramadol initiators demonstrate a higher frequency of chronic kidney disease, diabetes, and overall chronic comorbid diseases. “This suggests to me that prescribers apply selection criteria when choosing who to prescribe which opioid,” Dr. Solomon explained.
“While the authors’ use of propensity score matching limits confounding, it only can improve balance for measured confounders,” he said. “Other factors not measured in this type of data set – blood pressure, pain, physical activity, tobacco use, body mass index – may still demonstrate imbalances even after matching.”
But after these limitations are taken into consideration, the results remain concerning, Dr. Solomon emphasized, particularly the all-cause mortality excess of tramadol versus codeine users. “This study did not include cause of death, which would help the reader understand why users of tramadol were dying more frequently,” he added. “It also might help in understanding whether this is a true biologic effect or residual confounding.”
Perceived safety
In an accompanying editorial, Howard S. Kim, MD, MS, and colleagues from Northwestern University, Chicago, write that the greatest risk of tramadol may involve the perception that it is “inherently safer than other opioids.”
“In actuality, the mechanisms of action and variable metabolism of tramadol in a given population create considerable therapeutic uncertainty and introduce additional risk exposure,” they say, as demonstrated in the current study.
Therefore, when clinicians determine that an opioid is needed for pain relief, it may be a better option to select a pure opioid agonist that has a more predictable therapeutic effect and known adverse effect profile, such as morphine or hydrocodone. “This would allow clinicians and patients to more properly weigh the risks and benefits of initiating opioid therapy through shared decision-making and prompt the level of counseling on safe use, storage, and disposal practices that all opioids deserve,” write the editorialists.
The study was funded by the Fundació Institut Universitari per a la recerca a l’Atenció Primària de Salut Jordi Gol i Gurina. The research was supported by the National Institute for Health Research Oxford Biomedical Research Centre. Dr. Reyes has disclosed no relevant financial relationships. Dr. Solomon disclosed salary support from research contracts to his hospital from Amgen, AbbVie, Moderna, the Rheumatology Research Foundation, and National Institutes of Health; and royalties from UpToDate. Dr. Kim reported unrelated grant support from the Agency for Healthcare Research and Quality.
A version of this article first appeared on Medscape.com.
Tramadol is increasingly used to manage chronic noncancer pain, but as compared with opioids, it appears to be linked to a higher risk for adverse outcomes, according to new data.
Among a cohort of patients who received a prescription for either tramadol or codeine for orthopedic-related pain, tramadol was significantly associated with a higher risk of mortality, cardiovascular events, and fractures.
However, there was no significant difference in the risk of falls, delirium, constipation, opioid abuse/dependence, or sleep disorders between the two drugs.
“However, this is a retrospective cohort study, and despite it providing information that would otherwise be impossible to gather – such as from randomized controlled trials – clinicians should not solely base their decision on this study,” cautioned lead author Carlen Reyes, MD, PhD, of the Institut Universitari d’Investigació en Atenció Primària (IDIAP Jordi Gol), Barcelona.
Dr. Reyes noted that the intake of tramadol and codeine was analyzed using the number of “packages” that were dispensed, as an approximation of the real intake. “Logically we could think that the more packages dispensed of one drug, the more dose the patient is taking, but this is not always true given the availability of different doses commercialized of tramadol and different doses prescribed,” she said. “Given that we did not account for the real dose prescribed, we can only suspect an increased risk of these outcomes and reinforce the need for further prospective studies with more specific dose-response analysis comparing tramadol and codeine.”
The paper was published Oct. 19 in JAMA.
Tramadol has been considered to be a relatively safe opioid and was even strongly recommended by the American Academy of Orthopaedic Surgeons for patients experiencing symptomatic knee osteoarthritis. The authors point out that studies looking at opioid use from 2019 to 2020 show that tramadol was the most prescribed opioid in England, the Netherlands, and Spain.
In the United States, the age-adjusted rate of drug overdose deaths from synthetic opioids rose from 1.0 per 100 000 in 2013 to 11.4 in 2019. Most of these deaths were attributable to fentanyl but some were also related to tramadol.
But despite its wide use in managing chronic noncancer pain, results of recent studies suggest adverse outcomes as compared with other agents. Last year, one study found that older patients who received tramadol had a significant increase in the risk of hip fracture vs. those using NSAIDs or codeine. Another study, also published in 2020, showed that patients with osteoarthritis who were treated with tramadol had a 20%-50% higher risk of dying during the first year of treatment than did patients who were treated with NSAIDs.
In the current paper, Dr. Reyes and colleagues evaluated the association of tramadol with mortality and other adverse clinical outcomes in outpatient settings, compared with codeine.
They conducted a retrospective, population-based, propensity score–matched cohort study using a primary care database that routinely collects medical records and pharmacy dispensations for more than 80% of the population of Catalonia, Spain. The cohort included people 18 years or older who had been prescribed tramadol or codeine from 2007 to 2017 and were followed up to Dec. 31, 2017.
After propensity score matching, the final analysis included 368,960 participants: 184,480 in the tramadol arm and 184,480 in the codeine arm.
The mean age of patients was 52.7 years in the tramadol arm and 53.5 years in the codeine arm, and the prevalence of cancer was 3.2% and 3.3%, respectively. The most common diagnoses in this cohort were back pain (47.5% vs. 48.5%), neck/shoulder pain (28.6% vs. 29.5%), and osteoarthritis (15.3% vs. 15.5%). The most commonly used drugs were ibuprofen (34.4% vs. 34.3%) and paracetamol/acetaminophen (37.1% vs. 36.8%)
Higher risk of adverse outcomes
As compared with codeine, tramadol use was significantly associated with a higher risk of mortality (13.00 vs. 5.61 per 1,000 person-years; hazard ratio, 2.31; 95% confidence interval, 2.08-2.56); absolute rate differences (7.37 per 1,000 person-years; 95% CI, 6.09-8.78), cardiovascular events (10.03 vs. 8.67 per 1,000 person-years; HR, 1.15; 95% CI, 1.05-1.27; ARD, 1.36 per 1,000 person-years; 95% CI, 0.45-2.36), and fractures (12.26 vs. 8.13 per 1,000 person-years; HR, 1.50; 95% CI, 1.37-1.65; ARD, 4.10 per 1,000 person-years; 95% CI, 3.02-5.29).
A subgroup and sensitivity analysis showed that the increased mortality risk associated with tramadol was significantly higher in younger persons vs. older ones (HR, 3.14; 95% CI, 1.82-5.41 vs. 2.39; 95% CI, 2.20-2.60]; P < .001 for interaction). In addition, women had a significantly greater risk of cardiovascular events versus men (HR, 1.32; 95% CI, 1.19-1.46] vs. 1.03; 95% CI, 0.9-1.13]; P < .001 for interaction).
Potential for confounding
Weighing in on the data, Daniel Solomon, MD, MPH, chief of clinical sciences, division of rheumatology, Brigham and Women’s Hospital, and professor of medicine, Harvard Medical School, Boston, noted that because it is extremely unlikely that anyone will ever conduct a large, head-to-head safety trial comparing different opioids, the results of this paper are important to consider.
“However, as the authors appropriately caution, this type of analysis is limited by the strong potential for residual confounding,” he said. “In other words, even though the authors used state-of-the-art methods to limit imbalances between the patients initiating tramadol versus codeine, there is strong reason to believe that imbalances that may account for the differences in adverse events exist.”
For example, he noted that if one looks at the distribution of comorbid conditions in the before-matching group, tramadol initiators demonstrate a higher frequency of chronic kidney disease, diabetes, and overall chronic comorbid diseases. “This suggests to me that prescribers apply selection criteria when choosing who to prescribe which opioid,” Dr. Solomon explained.
“While the authors’ use of propensity score matching limits confounding, it only can improve balance for measured confounders,” he said. “Other factors not measured in this type of data set – blood pressure, pain, physical activity, tobacco use, body mass index – may still demonstrate imbalances even after matching.”
But after these limitations are taken into consideration, the results remain concerning, Dr. Solomon emphasized, particularly the all-cause mortality excess of tramadol versus codeine users. “This study did not include cause of death, which would help the reader understand why users of tramadol were dying more frequently,” he added. “It also might help in understanding whether this is a true biologic effect or residual confounding.”
Perceived safety
In an accompanying editorial, Howard S. Kim, MD, MS, and colleagues from Northwestern University, Chicago, write that the greatest risk of tramadol may involve the perception that it is “inherently safer than other opioids.”
“In actuality, the mechanisms of action and variable metabolism of tramadol in a given population create considerable therapeutic uncertainty and introduce additional risk exposure,” they say, as demonstrated in the current study.
Therefore, when clinicians determine that an opioid is needed for pain relief, it may be a better option to select a pure opioid agonist that has a more predictable therapeutic effect and known adverse effect profile, such as morphine or hydrocodone. “This would allow clinicians and patients to more properly weigh the risks and benefits of initiating opioid therapy through shared decision-making and prompt the level of counseling on safe use, storage, and disposal practices that all opioids deserve,” write the editorialists.
The study was funded by the Fundació Institut Universitari per a la recerca a l’Atenció Primària de Salut Jordi Gol i Gurina. The research was supported by the National Institute for Health Research Oxford Biomedical Research Centre. Dr. Reyes has disclosed no relevant financial relationships. Dr. Solomon disclosed salary support from research contracts to his hospital from Amgen, AbbVie, Moderna, the Rheumatology Research Foundation, and National Institutes of Health; and royalties from UpToDate. Dr. Kim reported unrelated grant support from the Agency for Healthcare Research and Quality.
A version of this article first appeared on Medscape.com.
U.S. arthritis prevalence continues steady rise; activity limitations grow more rapidly
Nearly a quarter of adults in the United States have been diagnosed with various forms of arthritis, new federal estimates report. The disorders limit the activities of 43.9% of them. Researchers also report that adults with poorer mental or physical health and those who are more disadvantaged socially are most vulnerable to arthritis.
“There is a substantial unmet need for existing, evidence-based, arthritis-appropriate interventions for people with arthritis to minimize activity limitations,” study coauthor and Centers for Disease Control and Prevention epidemiologist Kristina Theis, PhD, MPH, told this news organization. “Our findings show that interventions addressing self-management, education, physical activity, workplace accommodations, and mental health, among other areas, are all indicated for people with arthritis.”
The CDC report was published Oct. 8 in Morbidity and Mortality Weekly Report. Researchers estimated the number of arthritis cases on the basis of in-person interviews conducted with tens of thousands of U.S. adults as part of the National Health Interview Survey during 2016-2018. In the report, the researchers considered arthritis to include general arthritis, rheumatoid arthritis, gout, lupus, and fibromyalgia.
Activity limitations rose faster than predicted
According to the report, an estimated 58.5 million U.S. adults (23.7%; 21.5% age-standardized) told interviewers that they had been diagnosed with arthritis conditions. Of those, 25.7 million (43.9%; 40.8% age-standardized) had arthritis-attributable activity limitations (AAALs), which represents 10.4% of all adults.
The number of adults who reported having arthritis rose by 4.1 million from previous estimates for the years 2013-2015, a number that’s on pace with predictions. The number in the AAAL category rose by 2 million, a jump that’s higher than what had been predicted.
“The aging of the population is one factor in the increasing number of people with arthritis, even though arthritis is not an inevitable part of aging,” Dr. Theis said. “Individual factors, such as body mass index or other health conditions, and societal factors, such as educational and economic opportunities, likely play a role.”
Arthritis was especially common among those aged ≥ 65 years (50.4%), those who were unable to work or were disabled (52.3%), and those who self-reported fair/poor health (51.2%) or joint symptoms in the past 30 days (52.2%). The rate of arthritis was also high among those whose activities of daily living (ADL) were limited (54.8%) and those whose instrumental activities of daily living (IADL) were limited (55.9%).
The researchers report that the percentage of AAAL was also high among the following groups: “adults with joint symptoms in the past 30 days (51.6%), adults who were unable to work or disabled (54.7%), adults of other/multiple races (54.5%) or non-Hispanic American Indian or Alaska Natives (60.7%), adults with low income (53.3%) or poor/near poor income-to-poverty ratios (63.3%), or with moderate psychological distress (59.5%). AAAL was reported by a high proportion of adults with arthritis who had an ADL disability (82.6%), IADL disability (80.4%), serious psychological distress (76.3%), or fair/poor self-rated health (72.6%).”
The researchers found that among all adults with arthritis, the percentage of adults with arthritis was high among women (59.3%), those with obesity or overweight (74.2%), and those who weren’t sufficiently active (58%).
Comments on latest findings
Michael LaValley, PhD, biostatistician at the Boston University School of Public Health, who has studied arthritis statistics, told this news organization that the findings “fall right in line with the trends that have been observed in arthritis over the past 20 years. The prevalence is increasing, which certainly seems to be influenced by the aging population in the U.S.”
As for specific conditions, he said the rate of osteoarthritis may be influenced by older Americans and by those with obesity and sedentary behavior. “There is also some thinking that there may be environmental factors increasing the risk for some types of arthritis, but nothing conclusive. There also may be more clinical attention paid to arthritic conditions, leading to more people being diagnosed or even just suspecting that they have arthritis.”
It’s difficult to disentangle connections between arthritis and risk factors such as poverty, he said. “There almost certainly are occupational exposures that put people at risk of osteoarthritis – having to kneel, stoop, and lift heavy things – or other musculoskeletal conditions like lower back pain. These exposures are most likely in jobs that would predominantly go to people with few other options because of lower levels of income and education. People in these jobs would also be more likely to have financial stresses that lead to increased psychological distress and less time to take care of their health.”
Also, he said, “There is probably some reverse causation with the occupational results, self-related health, and psychological distress. These could all be affected by a person’s arthritis. Having arthritis may interfere with getting a better-paying job, and arthritis could certainly reduce someone’s self-reported health and induce psychological distress.”
The authors and LaValley have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Nearly a quarter of adults in the United States have been diagnosed with various forms of arthritis, new federal estimates report. The disorders limit the activities of 43.9% of them. Researchers also report that adults with poorer mental or physical health and those who are more disadvantaged socially are most vulnerable to arthritis.
“There is a substantial unmet need for existing, evidence-based, arthritis-appropriate interventions for people with arthritis to minimize activity limitations,” study coauthor and Centers for Disease Control and Prevention epidemiologist Kristina Theis, PhD, MPH, told this news organization. “Our findings show that interventions addressing self-management, education, physical activity, workplace accommodations, and mental health, among other areas, are all indicated for people with arthritis.”
The CDC report was published Oct. 8 in Morbidity and Mortality Weekly Report. Researchers estimated the number of arthritis cases on the basis of in-person interviews conducted with tens of thousands of U.S. adults as part of the National Health Interview Survey during 2016-2018. In the report, the researchers considered arthritis to include general arthritis, rheumatoid arthritis, gout, lupus, and fibromyalgia.
Activity limitations rose faster than predicted
According to the report, an estimated 58.5 million U.S. adults (23.7%; 21.5% age-standardized) told interviewers that they had been diagnosed with arthritis conditions. Of those, 25.7 million (43.9%; 40.8% age-standardized) had arthritis-attributable activity limitations (AAALs), which represents 10.4% of all adults.
The number of adults who reported having arthritis rose by 4.1 million from previous estimates for the years 2013-2015, a number that’s on pace with predictions. The number in the AAAL category rose by 2 million, a jump that’s higher than what had been predicted.
“The aging of the population is one factor in the increasing number of people with arthritis, even though arthritis is not an inevitable part of aging,” Dr. Theis said. “Individual factors, such as body mass index or other health conditions, and societal factors, such as educational and economic opportunities, likely play a role.”
Arthritis was especially common among those aged ≥ 65 years (50.4%), those who were unable to work or were disabled (52.3%), and those who self-reported fair/poor health (51.2%) or joint symptoms in the past 30 days (52.2%). The rate of arthritis was also high among those whose activities of daily living (ADL) were limited (54.8%) and those whose instrumental activities of daily living (IADL) were limited (55.9%).
The researchers report that the percentage of AAAL was also high among the following groups: “adults with joint symptoms in the past 30 days (51.6%), adults who were unable to work or disabled (54.7%), adults of other/multiple races (54.5%) or non-Hispanic American Indian or Alaska Natives (60.7%), adults with low income (53.3%) or poor/near poor income-to-poverty ratios (63.3%), or with moderate psychological distress (59.5%). AAAL was reported by a high proportion of adults with arthritis who had an ADL disability (82.6%), IADL disability (80.4%), serious psychological distress (76.3%), or fair/poor self-rated health (72.6%).”
The researchers found that among all adults with arthritis, the percentage of adults with arthritis was high among women (59.3%), those with obesity or overweight (74.2%), and those who weren’t sufficiently active (58%).
Comments on latest findings
Michael LaValley, PhD, biostatistician at the Boston University School of Public Health, who has studied arthritis statistics, told this news organization that the findings “fall right in line with the trends that have been observed in arthritis over the past 20 years. The prevalence is increasing, which certainly seems to be influenced by the aging population in the U.S.”
As for specific conditions, he said the rate of osteoarthritis may be influenced by older Americans and by those with obesity and sedentary behavior. “There is also some thinking that there may be environmental factors increasing the risk for some types of arthritis, but nothing conclusive. There also may be more clinical attention paid to arthritic conditions, leading to more people being diagnosed or even just suspecting that they have arthritis.”
It’s difficult to disentangle connections between arthritis and risk factors such as poverty, he said. “There almost certainly are occupational exposures that put people at risk of osteoarthritis – having to kneel, stoop, and lift heavy things – or other musculoskeletal conditions like lower back pain. These exposures are most likely in jobs that would predominantly go to people with few other options because of lower levels of income and education. People in these jobs would also be more likely to have financial stresses that lead to increased psychological distress and less time to take care of their health.”
Also, he said, “There is probably some reverse causation with the occupational results, self-related health, and psychological distress. These could all be affected by a person’s arthritis. Having arthritis may interfere with getting a better-paying job, and arthritis could certainly reduce someone’s self-reported health and induce psychological distress.”
The authors and LaValley have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Nearly a quarter of adults in the United States have been diagnosed with various forms of arthritis, new federal estimates report. The disorders limit the activities of 43.9% of them. Researchers also report that adults with poorer mental or physical health and those who are more disadvantaged socially are most vulnerable to arthritis.
“There is a substantial unmet need for existing, evidence-based, arthritis-appropriate interventions for people with arthritis to minimize activity limitations,” study coauthor and Centers for Disease Control and Prevention epidemiologist Kristina Theis, PhD, MPH, told this news organization. “Our findings show that interventions addressing self-management, education, physical activity, workplace accommodations, and mental health, among other areas, are all indicated for people with arthritis.”
The CDC report was published Oct. 8 in Morbidity and Mortality Weekly Report. Researchers estimated the number of arthritis cases on the basis of in-person interviews conducted with tens of thousands of U.S. adults as part of the National Health Interview Survey during 2016-2018. In the report, the researchers considered arthritis to include general arthritis, rheumatoid arthritis, gout, lupus, and fibromyalgia.
Activity limitations rose faster than predicted
According to the report, an estimated 58.5 million U.S. adults (23.7%; 21.5% age-standardized) told interviewers that they had been diagnosed with arthritis conditions. Of those, 25.7 million (43.9%; 40.8% age-standardized) had arthritis-attributable activity limitations (AAALs), which represents 10.4% of all adults.
The number of adults who reported having arthritis rose by 4.1 million from previous estimates for the years 2013-2015, a number that’s on pace with predictions. The number in the AAAL category rose by 2 million, a jump that’s higher than what had been predicted.
“The aging of the population is one factor in the increasing number of people with arthritis, even though arthritis is not an inevitable part of aging,” Dr. Theis said. “Individual factors, such as body mass index or other health conditions, and societal factors, such as educational and economic opportunities, likely play a role.”
Arthritis was especially common among those aged ≥ 65 years (50.4%), those who were unable to work or were disabled (52.3%), and those who self-reported fair/poor health (51.2%) or joint symptoms in the past 30 days (52.2%). The rate of arthritis was also high among those whose activities of daily living (ADL) were limited (54.8%) and those whose instrumental activities of daily living (IADL) were limited (55.9%).
The researchers report that the percentage of AAAL was also high among the following groups: “adults with joint symptoms in the past 30 days (51.6%), adults who were unable to work or disabled (54.7%), adults of other/multiple races (54.5%) or non-Hispanic American Indian or Alaska Natives (60.7%), adults with low income (53.3%) or poor/near poor income-to-poverty ratios (63.3%), or with moderate psychological distress (59.5%). AAAL was reported by a high proportion of adults with arthritis who had an ADL disability (82.6%), IADL disability (80.4%), serious psychological distress (76.3%), or fair/poor self-rated health (72.6%).”
The researchers found that among all adults with arthritis, the percentage of adults with arthritis was high among women (59.3%), those with obesity or overweight (74.2%), and those who weren’t sufficiently active (58%).
Comments on latest findings
Michael LaValley, PhD, biostatistician at the Boston University School of Public Health, who has studied arthritis statistics, told this news organization that the findings “fall right in line with the trends that have been observed in arthritis over the past 20 years. The prevalence is increasing, which certainly seems to be influenced by the aging population in the U.S.”
As for specific conditions, he said the rate of osteoarthritis may be influenced by older Americans and by those with obesity and sedentary behavior. “There is also some thinking that there may be environmental factors increasing the risk for some types of arthritis, but nothing conclusive. There also may be more clinical attention paid to arthritic conditions, leading to more people being diagnosed or even just suspecting that they have arthritis.”
It’s difficult to disentangle connections between arthritis and risk factors such as poverty, he said. “There almost certainly are occupational exposures that put people at risk of osteoarthritis – having to kneel, stoop, and lift heavy things – or other musculoskeletal conditions like lower back pain. These exposures are most likely in jobs that would predominantly go to people with few other options because of lower levels of income and education. People in these jobs would also be more likely to have financial stresses that lead to increased psychological distress and less time to take care of their health.”
Also, he said, “There is probably some reverse causation with the occupational results, self-related health, and psychological distress. These could all be affected by a person’s arthritis. Having arthritis may interfere with getting a better-paying job, and arthritis could certainly reduce someone’s self-reported health and induce psychological distress.”
The authors and LaValley have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AAOS updates guidelines for nonoperative knee OA treatment
After nearly a decade, the American Academy of Orthopaedic Surgeons has updated its guidance on nonoperative treatment for knee osteoarthritis.
The clinical practice guidelines, released Sept. 13, 2021, is the third edition of the orthopedic society’s clinical practice recommendations.
According to Robert Brophy, MD, FAAOS, an orthopedic surgeon at Washington University, St. Louis, and cochair of the AAOS clinical practice guideline work group, the AAOS guidelines are a “living document” that needs periodic updating as new research comes to light.
“The methodology for maintaining the AAOS guidelines aims to update guideline documents at least every 10 years,” Dr. Brophy said in an interview. “Since the last edition was from 2013, it was time to provide an updated guideline on this very important topic that affects such a high percentage of our patients and providers.”
The guidelines work group, composed of 12 medical doctors and 1 physical therapist, evaluated the evidence for 29 areas of treatment.
A rating scale based on available evidence and the strength of related medical studies labeled each treatment area as demonstrating strong, moderate, or limited evidence.
Eight treatment modalities weighed in with strong evidence for or against their use: lateral wedge insoles, topical or oral NSAIDs, exercise (supervised or unsupervised), self-management programs, patient education programs, oral acetaminophen, and oral opioids.
According to Dr. Brophy, many of the recommendations assigned a strong evidence base were similar to the prior edition of the guidelines.
Oral medications
NSAIDs and acetaminophen still remain steadfast options for the treatment of knee pain secondary to OA.
The most notable change was that opioids, which have a long history of being used to treat pain, are strongly recommended not to be used for arthritis.
“Reflecting the growing awareness of and emphasis on the opioid epidemic, one of the strongest changes between the current and prior guidelines centers on the use of opioid medications,” Dr. Brophy said. “In the prior guideline, a strong recommendation was made in favor of tramadol with an inconclusive recommendation made regarding other opioid medications. The updated guideline demonstrates clearly the evidence does not support the use of opioid medications – including tramadol – to treat knee osteoarthritis.”
This may require some education for both patients and doctors to buy in that knee pain can be treated adequately with NSAIDs and acetaminophen.
Patients may not understand that anti-inflammatory drugs treat the pain they are experiencing. They may equate an opioid with a “pain pill” and may need education from their doctor that NSAIDs and acetaminophen not only can relieve their pain, but also avoid potential adverse events prior to or after surgery should they progress to knee replacement surgery.
Furthermore, primary care physicians may not be looking at the long-term picture. Solving a short-term pain problem with opioids may limit the medication’s ability to provide pain relief after surgery should a patient develop a tolerance to the medication’s effects.
Recommendations on hip and foot alignment interventions
When it comes to alignment and joint stresses, the knee is sometimes considered the innocent bystander of hip and foot alignment.
Insoles. How the hip and foot align with each can determine the amount of weight that passes through the medial (inner) or lateral (outer) compartment of the knee. To that end, lateral foot insoles have been used in the past for unloading parts of the knee.
Nevertheless, recent evidence has failed to demonstrate a significant benefit for insoles in the setting of OA knee pain, earning the practice a strong recommendation against its use.
High-tibial osteotomy (HTO). The weight-bearing axis of the lower-extremity axis can also be realigned with HTO. The procedure shifts the body’s weight slightly to the opposite side of the knee.
Newer research has led the practice to be downgraded one level in the new guideline, from moderate to limited, despite its widespread use.
It will, however, likely continue to be used as an alternative to total knee replacement in younger patients and to shift weight away from an area of the knee where cartilage is being restored with a concomitant surgical procedure, according to the work group. They noted that additional research studies on the long-term efficacy of the procedure are still needed.
Topical treatments. The guideline authors gave these a strong recommendation. Gels with anti-inflammatory medication have long been available but were prescription only or of considerable cost. Now several affordable over-the-counter options with the same prescription strength can be found in pharmacies and supermarkets.
What makes these medications unique is that they have an NSAID medication in the formulation, which the vast majority of topical treatments found on shelves do not. They also benefit patients who are unable to tolerate oral NSAIDs because of gastrointestinal side effects.
Comparison with 2019 OARSI recommendations
In 2019, the Osteoarthritis Research Society International also published guidelines for the management of OA of the hand, hip, and knee.
Thomas Trojian, MD, a family medicine physician with expertise in sports medicine in York, Pa., and member of both the AAOS and OARSI recommendation committees, noted that the OARSI guidelines are meant to be practical guidelines of stepwise nonoperative treatment.
He said in an interview that “the OARSI guidelines recommend dietary weight management, education, and land-based [exercise] therapy, next topical NSAIDs, then injection therapy.”
Intra-articular steroids and viscosupplementation injection therapy in the form of hyaluronic acid derivatives continue to be a mainstay of treatment for both groups.
The AAOS group notably gave a moderate strength recommendation for intra-articular steroid injections with the caveat that the effects typically only last for 3 months. They also included newer extended-release steroid injections in the recommendation, stating that the evidence moderately suggests they provide more benefit than traditional short-acting steroid injections.
Methodology differs between guidelines
In the areas where the guidelines don’t fully line up, it is important to remember the methodology of each group often drives the guidelines and recommendations.
According to Yale Fillingham, MD, an orthopedic surgeon in group private practice in the greater Philadelphia area and the other cochair of the AAOS guidelines committee, the biggest difference between the AAOS and OARSI guidelines is that, although the OARSI guidelines are also grounded in the literature, the recommendation level was based on voting among panel members.
“The AAOS methodology requires the recommendation and strength of the recommendation to be dictated primarily by the best available evidence in the literature and much less on the expertise and opinion of the voting panel,” Dr. Fillingham said in an interview.
He pointed out that the AAOS voting panel can alter the guideline by adjusting the strength of the recommendation but noted it was only in very clearly defined situations. Therefore, the differences in methodology between the groups make it difficult to directly compare the two guidelines.
Multiple guidelines do, however, point to the importance of the issue. Dr. Fillingham commented: “The numerous organizations that have produced guidelines on the treatment of knee osteoarthritis are a testament to the widespread and profound impact of knee osteoarthritis on our health care system and society.”
As a member of both recommendation groups, Dr. Trojian finds both guidelines reveal the importance of understanding that knee OA is a chronic illness. “There are ways we can manage knee OA and reduce the morbidity. ... The core skills of motivational interviewing are important. Open-ended questions, affirmation, reflection, and summarizing are needed to help patients find and remove roadblocks to promote lifestyle changes.”
Dr. Brophy, Dr. Trojian, and Dr. Fillingham have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
After nearly a decade, the American Academy of Orthopaedic Surgeons has updated its guidance on nonoperative treatment for knee osteoarthritis.
The clinical practice guidelines, released Sept. 13, 2021, is the third edition of the orthopedic society’s clinical practice recommendations.
According to Robert Brophy, MD, FAAOS, an orthopedic surgeon at Washington University, St. Louis, and cochair of the AAOS clinical practice guideline work group, the AAOS guidelines are a “living document” that needs periodic updating as new research comes to light.
“The methodology for maintaining the AAOS guidelines aims to update guideline documents at least every 10 years,” Dr. Brophy said in an interview. “Since the last edition was from 2013, it was time to provide an updated guideline on this very important topic that affects such a high percentage of our patients and providers.”
The guidelines work group, composed of 12 medical doctors and 1 physical therapist, evaluated the evidence for 29 areas of treatment.
A rating scale based on available evidence and the strength of related medical studies labeled each treatment area as demonstrating strong, moderate, or limited evidence.
Eight treatment modalities weighed in with strong evidence for or against their use: lateral wedge insoles, topical or oral NSAIDs, exercise (supervised or unsupervised), self-management programs, patient education programs, oral acetaminophen, and oral opioids.
According to Dr. Brophy, many of the recommendations assigned a strong evidence base were similar to the prior edition of the guidelines.
Oral medications
NSAIDs and acetaminophen still remain steadfast options for the treatment of knee pain secondary to OA.
The most notable change was that opioids, which have a long history of being used to treat pain, are strongly recommended not to be used for arthritis.
“Reflecting the growing awareness of and emphasis on the opioid epidemic, one of the strongest changes between the current and prior guidelines centers on the use of opioid medications,” Dr. Brophy said. “In the prior guideline, a strong recommendation was made in favor of tramadol with an inconclusive recommendation made regarding other opioid medications. The updated guideline demonstrates clearly the evidence does not support the use of opioid medications – including tramadol – to treat knee osteoarthritis.”
This may require some education for both patients and doctors to buy in that knee pain can be treated adequately with NSAIDs and acetaminophen.
Patients may not understand that anti-inflammatory drugs treat the pain they are experiencing. They may equate an opioid with a “pain pill” and may need education from their doctor that NSAIDs and acetaminophen not only can relieve their pain, but also avoid potential adverse events prior to or after surgery should they progress to knee replacement surgery.
Furthermore, primary care physicians may not be looking at the long-term picture. Solving a short-term pain problem with opioids may limit the medication’s ability to provide pain relief after surgery should a patient develop a tolerance to the medication’s effects.
Recommendations on hip and foot alignment interventions
When it comes to alignment and joint stresses, the knee is sometimes considered the innocent bystander of hip and foot alignment.
Insoles. How the hip and foot align with each can determine the amount of weight that passes through the medial (inner) or lateral (outer) compartment of the knee. To that end, lateral foot insoles have been used in the past for unloading parts of the knee.
Nevertheless, recent evidence has failed to demonstrate a significant benefit for insoles in the setting of OA knee pain, earning the practice a strong recommendation against its use.
High-tibial osteotomy (HTO). The weight-bearing axis of the lower-extremity axis can also be realigned with HTO. The procedure shifts the body’s weight slightly to the opposite side of the knee.
Newer research has led the practice to be downgraded one level in the new guideline, from moderate to limited, despite its widespread use.
It will, however, likely continue to be used as an alternative to total knee replacement in younger patients and to shift weight away from an area of the knee where cartilage is being restored with a concomitant surgical procedure, according to the work group. They noted that additional research studies on the long-term efficacy of the procedure are still needed.
Topical treatments. The guideline authors gave these a strong recommendation. Gels with anti-inflammatory medication have long been available but were prescription only or of considerable cost. Now several affordable over-the-counter options with the same prescription strength can be found in pharmacies and supermarkets.
What makes these medications unique is that they have an NSAID medication in the formulation, which the vast majority of topical treatments found on shelves do not. They also benefit patients who are unable to tolerate oral NSAIDs because of gastrointestinal side effects.
Comparison with 2019 OARSI recommendations
In 2019, the Osteoarthritis Research Society International also published guidelines for the management of OA of the hand, hip, and knee.
Thomas Trojian, MD, a family medicine physician with expertise in sports medicine in York, Pa., and member of both the AAOS and OARSI recommendation committees, noted that the OARSI guidelines are meant to be practical guidelines of stepwise nonoperative treatment.
He said in an interview that “the OARSI guidelines recommend dietary weight management, education, and land-based [exercise] therapy, next topical NSAIDs, then injection therapy.”
Intra-articular steroids and viscosupplementation injection therapy in the form of hyaluronic acid derivatives continue to be a mainstay of treatment for both groups.
The AAOS group notably gave a moderate strength recommendation for intra-articular steroid injections with the caveat that the effects typically only last for 3 months. They also included newer extended-release steroid injections in the recommendation, stating that the evidence moderately suggests they provide more benefit than traditional short-acting steroid injections.
Methodology differs between guidelines
In the areas where the guidelines don’t fully line up, it is important to remember the methodology of each group often drives the guidelines and recommendations.
According to Yale Fillingham, MD, an orthopedic surgeon in group private practice in the greater Philadelphia area and the other cochair of the AAOS guidelines committee, the biggest difference between the AAOS and OARSI guidelines is that, although the OARSI guidelines are also grounded in the literature, the recommendation level was based on voting among panel members.
“The AAOS methodology requires the recommendation and strength of the recommendation to be dictated primarily by the best available evidence in the literature and much less on the expertise and opinion of the voting panel,” Dr. Fillingham said in an interview.
He pointed out that the AAOS voting panel can alter the guideline by adjusting the strength of the recommendation but noted it was only in very clearly defined situations. Therefore, the differences in methodology between the groups make it difficult to directly compare the two guidelines.
Multiple guidelines do, however, point to the importance of the issue. Dr. Fillingham commented: “The numerous organizations that have produced guidelines on the treatment of knee osteoarthritis are a testament to the widespread and profound impact of knee osteoarthritis on our health care system and society.”
As a member of both recommendation groups, Dr. Trojian finds both guidelines reveal the importance of understanding that knee OA is a chronic illness. “There are ways we can manage knee OA and reduce the morbidity. ... The core skills of motivational interviewing are important. Open-ended questions, affirmation, reflection, and summarizing are needed to help patients find and remove roadblocks to promote lifestyle changes.”
Dr. Brophy, Dr. Trojian, and Dr. Fillingham have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
After nearly a decade, the American Academy of Orthopaedic Surgeons has updated its guidance on nonoperative treatment for knee osteoarthritis.
The clinical practice guidelines, released Sept. 13, 2021, is the third edition of the orthopedic society’s clinical practice recommendations.
According to Robert Brophy, MD, FAAOS, an orthopedic surgeon at Washington University, St. Louis, and cochair of the AAOS clinical practice guideline work group, the AAOS guidelines are a “living document” that needs periodic updating as new research comes to light.
“The methodology for maintaining the AAOS guidelines aims to update guideline documents at least every 10 years,” Dr. Brophy said in an interview. “Since the last edition was from 2013, it was time to provide an updated guideline on this very important topic that affects such a high percentage of our patients and providers.”
The guidelines work group, composed of 12 medical doctors and 1 physical therapist, evaluated the evidence for 29 areas of treatment.
A rating scale based on available evidence and the strength of related medical studies labeled each treatment area as demonstrating strong, moderate, or limited evidence.
Eight treatment modalities weighed in with strong evidence for or against their use: lateral wedge insoles, topical or oral NSAIDs, exercise (supervised or unsupervised), self-management programs, patient education programs, oral acetaminophen, and oral opioids.
According to Dr. Brophy, many of the recommendations assigned a strong evidence base were similar to the prior edition of the guidelines.
Oral medications
NSAIDs and acetaminophen still remain steadfast options for the treatment of knee pain secondary to OA.
The most notable change was that opioids, which have a long history of being used to treat pain, are strongly recommended not to be used for arthritis.
“Reflecting the growing awareness of and emphasis on the opioid epidemic, one of the strongest changes between the current and prior guidelines centers on the use of opioid medications,” Dr. Brophy said. “In the prior guideline, a strong recommendation was made in favor of tramadol with an inconclusive recommendation made regarding other opioid medications. The updated guideline demonstrates clearly the evidence does not support the use of opioid medications – including tramadol – to treat knee osteoarthritis.”
This may require some education for both patients and doctors to buy in that knee pain can be treated adequately with NSAIDs and acetaminophen.
Patients may not understand that anti-inflammatory drugs treat the pain they are experiencing. They may equate an opioid with a “pain pill” and may need education from their doctor that NSAIDs and acetaminophen not only can relieve their pain, but also avoid potential adverse events prior to or after surgery should they progress to knee replacement surgery.
Furthermore, primary care physicians may not be looking at the long-term picture. Solving a short-term pain problem with opioids may limit the medication’s ability to provide pain relief after surgery should a patient develop a tolerance to the medication’s effects.
Recommendations on hip and foot alignment interventions
When it comes to alignment and joint stresses, the knee is sometimes considered the innocent bystander of hip and foot alignment.
Insoles. How the hip and foot align with each can determine the amount of weight that passes through the medial (inner) or lateral (outer) compartment of the knee. To that end, lateral foot insoles have been used in the past for unloading parts of the knee.
Nevertheless, recent evidence has failed to demonstrate a significant benefit for insoles in the setting of OA knee pain, earning the practice a strong recommendation against its use.
High-tibial osteotomy (HTO). The weight-bearing axis of the lower-extremity axis can also be realigned with HTO. The procedure shifts the body’s weight slightly to the opposite side of the knee.
Newer research has led the practice to be downgraded one level in the new guideline, from moderate to limited, despite its widespread use.
It will, however, likely continue to be used as an alternative to total knee replacement in younger patients and to shift weight away from an area of the knee where cartilage is being restored with a concomitant surgical procedure, according to the work group. They noted that additional research studies on the long-term efficacy of the procedure are still needed.
Topical treatments. The guideline authors gave these a strong recommendation. Gels with anti-inflammatory medication have long been available but were prescription only or of considerable cost. Now several affordable over-the-counter options with the same prescription strength can be found in pharmacies and supermarkets.
What makes these medications unique is that they have an NSAID medication in the formulation, which the vast majority of topical treatments found on shelves do not. They also benefit patients who are unable to tolerate oral NSAIDs because of gastrointestinal side effects.
Comparison with 2019 OARSI recommendations
In 2019, the Osteoarthritis Research Society International also published guidelines for the management of OA of the hand, hip, and knee.
Thomas Trojian, MD, a family medicine physician with expertise in sports medicine in York, Pa., and member of both the AAOS and OARSI recommendation committees, noted that the OARSI guidelines are meant to be practical guidelines of stepwise nonoperative treatment.
He said in an interview that “the OARSI guidelines recommend dietary weight management, education, and land-based [exercise] therapy, next topical NSAIDs, then injection therapy.”
Intra-articular steroids and viscosupplementation injection therapy in the form of hyaluronic acid derivatives continue to be a mainstay of treatment for both groups.
The AAOS group notably gave a moderate strength recommendation for intra-articular steroid injections with the caveat that the effects typically only last for 3 months. They also included newer extended-release steroid injections in the recommendation, stating that the evidence moderately suggests they provide more benefit than traditional short-acting steroid injections.
Methodology differs between guidelines
In the areas where the guidelines don’t fully line up, it is important to remember the methodology of each group often drives the guidelines and recommendations.
According to Yale Fillingham, MD, an orthopedic surgeon in group private practice in the greater Philadelphia area and the other cochair of the AAOS guidelines committee, the biggest difference between the AAOS and OARSI guidelines is that, although the OARSI guidelines are also grounded in the literature, the recommendation level was based on voting among panel members.
“The AAOS methodology requires the recommendation and strength of the recommendation to be dictated primarily by the best available evidence in the literature and much less on the expertise and opinion of the voting panel,” Dr. Fillingham said in an interview.
He pointed out that the AAOS voting panel can alter the guideline by adjusting the strength of the recommendation but noted it was only in very clearly defined situations. Therefore, the differences in methodology between the groups make it difficult to directly compare the two guidelines.
Multiple guidelines do, however, point to the importance of the issue. Dr. Fillingham commented: “The numerous organizations that have produced guidelines on the treatment of knee osteoarthritis are a testament to the widespread and profound impact of knee osteoarthritis on our health care system and society.”
As a member of both recommendation groups, Dr. Trojian finds both guidelines reveal the importance of understanding that knee OA is a chronic illness. “There are ways we can manage knee OA and reduce the morbidity. ... The core skills of motivational interviewing are important. Open-ended questions, affirmation, reflection, and summarizing are needed to help patients find and remove roadblocks to promote lifestyle changes.”
Dr. Brophy, Dr. Trojian, and Dr. Fillingham have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Cannabidiol found no better than placebo for hand arthritis pain
Use of cannabidiol (CBD) as an add-on pain management technique in patients with either hand osteoarthritis (OA) or psoriatic arthritis (PsA) did not significantly decrease pain intensity when compared with a placebo in a randomized, double-blind trial described as the first of its kind to investigate the effect of pure CBD as an add-on analgesic therapy in patients with joint disease.
Although data on the use of medical cannabis as a modulator of joint pain are limited, some studies suggest an effect from CBD without the addition of delta-9-tetrahydrocannabinol (THC), wrote Jonathan Vela, MD, of Aalborg (Denmark) University Hospital, and colleagues.
CBD is being used for pain conditions despite a lack of data on safety and effectiveness, the researchers emphasized. Notably, in a 2018 online survey, 62% of respondents reported using CBD for medical conditions, primarily for chronic pain and arthritis or joint pain, they wrote.
In a study published in the journal Pain, the researchers randomized 59 adults with PsA and 77 adults with hand OA to 20-30 mg of synthetic CBD or a placebo daily for 12 weeks in addition to conventional pain management. Patients initially received either oral CBD 10 mg or a placebo tablet once daily, increasing to 10 mg twice daily after 2 weeks, and once again up to 10 mg three times daily at 4 weeks if the patient did not experience more than 20-mm improvement on the visual analog scale (VAS).
The primary outcome in the trial was patient-reported pain intensity during the last 24 hours as assessed on a paper-based 100-mm VAS with the text, “How much pain have you experienced in the most symptomatic joint during the last 24 hours?” with 0 representing no pain and 100 representing the worst pain imaginable.
Overall, both CBD and placebo groups achieved significant reductions in pain intensity of 11-12 mm at 12 weeks. The mean between-group difference on the VAS was 0.23 mm (P = .96). Twenty-two percent of patients who received CBD and 21% who received placebo demonstrated a pain intensity reduction greater than 30 mm on the VAS. Pain reduction greater than 50% was reported by 17 patients (25%) in the CBD group and 16 (27%) in the placebo group. CBD had a similar effect in patients with either PsA or hand OA.
Four serious adverse events occurred during the 12-week study period, but none of these were deemed adverse drug reactions. Serious adverse events in the CBD patients included one case of ductal carcinoma and one case of lipotymia; serious adverse events in the placebo group included one case of acute shoulder fracture and one case of malignant hypertension. Fifty-nine patients reported adverse events during the study. The CBD group reported more ear-nose-throat adverse events, compared with the placebo group (8 vs. 0).
The researchers assessed the impact of CBD vs. placebo on sleep quality, depression, anxiety, or pain catastrophizing scores using the Pittsburgh Sleep Quality Index, Hospital Anxiety and Depression Scale, Pain Catastrophizing Scale, and Health Assessment Questionnaire but found no differences in patients taking CBD vs. placebo.
The study findings were limited by several factors, including the potentially insufficient dose level to evoke a pain relief response, and a lack of data on additional daily use of analgesics or of the study drug beyond the prescribed dosage, the researchers noted.
The results were strengthened by the randomized, double-blind trial design and its relatively large sample size, they wrote. However, the researchers also cautioned that their study focused on CBD as a single ingredient, and the results might not generalize to other CBD formulations. They also noted that more research is needed to examine both higher doses of CBD and different types of pain disorders.
The study was supported by the Danish Psoriasis Foundation Grant and the Danish Rheumatism Foundation. The researchers had no financial conflicts to disclose.
Use of cannabidiol (CBD) as an add-on pain management technique in patients with either hand osteoarthritis (OA) or psoriatic arthritis (PsA) did not significantly decrease pain intensity when compared with a placebo in a randomized, double-blind trial described as the first of its kind to investigate the effect of pure CBD as an add-on analgesic therapy in patients with joint disease.
Although data on the use of medical cannabis as a modulator of joint pain are limited, some studies suggest an effect from CBD without the addition of delta-9-tetrahydrocannabinol (THC), wrote Jonathan Vela, MD, of Aalborg (Denmark) University Hospital, and colleagues.
CBD is being used for pain conditions despite a lack of data on safety and effectiveness, the researchers emphasized. Notably, in a 2018 online survey, 62% of respondents reported using CBD for medical conditions, primarily for chronic pain and arthritis or joint pain, they wrote.
In a study published in the journal Pain, the researchers randomized 59 adults with PsA and 77 adults with hand OA to 20-30 mg of synthetic CBD or a placebo daily for 12 weeks in addition to conventional pain management. Patients initially received either oral CBD 10 mg or a placebo tablet once daily, increasing to 10 mg twice daily after 2 weeks, and once again up to 10 mg three times daily at 4 weeks if the patient did not experience more than 20-mm improvement on the visual analog scale (VAS).
The primary outcome in the trial was patient-reported pain intensity during the last 24 hours as assessed on a paper-based 100-mm VAS with the text, “How much pain have you experienced in the most symptomatic joint during the last 24 hours?” with 0 representing no pain and 100 representing the worst pain imaginable.
Overall, both CBD and placebo groups achieved significant reductions in pain intensity of 11-12 mm at 12 weeks. The mean between-group difference on the VAS was 0.23 mm (P = .96). Twenty-two percent of patients who received CBD and 21% who received placebo demonstrated a pain intensity reduction greater than 30 mm on the VAS. Pain reduction greater than 50% was reported by 17 patients (25%) in the CBD group and 16 (27%) in the placebo group. CBD had a similar effect in patients with either PsA or hand OA.
Four serious adverse events occurred during the 12-week study period, but none of these were deemed adverse drug reactions. Serious adverse events in the CBD patients included one case of ductal carcinoma and one case of lipotymia; serious adverse events in the placebo group included one case of acute shoulder fracture and one case of malignant hypertension. Fifty-nine patients reported adverse events during the study. The CBD group reported more ear-nose-throat adverse events, compared with the placebo group (8 vs. 0).
The researchers assessed the impact of CBD vs. placebo on sleep quality, depression, anxiety, or pain catastrophizing scores using the Pittsburgh Sleep Quality Index, Hospital Anxiety and Depression Scale, Pain Catastrophizing Scale, and Health Assessment Questionnaire but found no differences in patients taking CBD vs. placebo.
The study findings were limited by several factors, including the potentially insufficient dose level to evoke a pain relief response, and a lack of data on additional daily use of analgesics or of the study drug beyond the prescribed dosage, the researchers noted.
The results were strengthened by the randomized, double-blind trial design and its relatively large sample size, they wrote. However, the researchers also cautioned that their study focused on CBD as a single ingredient, and the results might not generalize to other CBD formulations. They also noted that more research is needed to examine both higher doses of CBD and different types of pain disorders.
The study was supported by the Danish Psoriasis Foundation Grant and the Danish Rheumatism Foundation. The researchers had no financial conflicts to disclose.
Use of cannabidiol (CBD) as an add-on pain management technique in patients with either hand osteoarthritis (OA) or psoriatic arthritis (PsA) did not significantly decrease pain intensity when compared with a placebo in a randomized, double-blind trial described as the first of its kind to investigate the effect of pure CBD as an add-on analgesic therapy in patients with joint disease.
Although data on the use of medical cannabis as a modulator of joint pain are limited, some studies suggest an effect from CBD without the addition of delta-9-tetrahydrocannabinol (THC), wrote Jonathan Vela, MD, of Aalborg (Denmark) University Hospital, and colleagues.
CBD is being used for pain conditions despite a lack of data on safety and effectiveness, the researchers emphasized. Notably, in a 2018 online survey, 62% of respondents reported using CBD for medical conditions, primarily for chronic pain and arthritis or joint pain, they wrote.
In a study published in the journal Pain, the researchers randomized 59 adults with PsA and 77 adults with hand OA to 20-30 mg of synthetic CBD or a placebo daily for 12 weeks in addition to conventional pain management. Patients initially received either oral CBD 10 mg or a placebo tablet once daily, increasing to 10 mg twice daily after 2 weeks, and once again up to 10 mg three times daily at 4 weeks if the patient did not experience more than 20-mm improvement on the visual analog scale (VAS).
The primary outcome in the trial was patient-reported pain intensity during the last 24 hours as assessed on a paper-based 100-mm VAS with the text, “How much pain have you experienced in the most symptomatic joint during the last 24 hours?” with 0 representing no pain and 100 representing the worst pain imaginable.
Overall, both CBD and placebo groups achieved significant reductions in pain intensity of 11-12 mm at 12 weeks. The mean between-group difference on the VAS was 0.23 mm (P = .96). Twenty-two percent of patients who received CBD and 21% who received placebo demonstrated a pain intensity reduction greater than 30 mm on the VAS. Pain reduction greater than 50% was reported by 17 patients (25%) in the CBD group and 16 (27%) in the placebo group. CBD had a similar effect in patients with either PsA or hand OA.
Four serious adverse events occurred during the 12-week study period, but none of these were deemed adverse drug reactions. Serious adverse events in the CBD patients included one case of ductal carcinoma and one case of lipotymia; serious adverse events in the placebo group included one case of acute shoulder fracture and one case of malignant hypertension. Fifty-nine patients reported adverse events during the study. The CBD group reported more ear-nose-throat adverse events, compared with the placebo group (8 vs. 0).
The researchers assessed the impact of CBD vs. placebo on sleep quality, depression, anxiety, or pain catastrophizing scores using the Pittsburgh Sleep Quality Index, Hospital Anxiety and Depression Scale, Pain Catastrophizing Scale, and Health Assessment Questionnaire but found no differences in patients taking CBD vs. placebo.
The study findings were limited by several factors, including the potentially insufficient dose level to evoke a pain relief response, and a lack of data on additional daily use of analgesics or of the study drug beyond the prescribed dosage, the researchers noted.
The results were strengthened by the randomized, double-blind trial design and its relatively large sample size, they wrote. However, the researchers also cautioned that their study focused on CBD as a single ingredient, and the results might not generalize to other CBD formulations. They also noted that more research is needed to examine both higher doses of CBD and different types of pain disorders.
The study was supported by the Danish Psoriasis Foundation Grant and the Danish Rheumatism Foundation. The researchers had no financial conflicts to disclose.
FROM PAIN
Diet, exercise in older adults with knee OA have long-term payoff
Older patients with knee osteoarthritis (OA) who underwent lengthy diet and exercise interventions reported less pain and maintained some weight loss years after the program ended, according to a new study published in Arthritis Care & Research.
“These data imply that clinicians who treat people with knee osteoarthritis have a variety of nonpharmacologic options that preserve clinically important effects 3.5 years after the treatments end,” wrote lead author Stephen P. Messier, PhD, professor and director of the J.B. Snow Biomechanics Laboratory at Wake Forest University, Winston-Salem, N.C.
The study involved patients with overweight or obesity aged 55 years or older who were previously enrolled in the 1.5-year Intensive Diet and Exercise for Arthritis (IDEA) trial.
“You have to remember, this is 3.5 years after the IDEA trial ended,” Dr. Messier said in an interview. “There was no contact with them for that entire time; you’d expect, based on the literature, that they’d revert back to where they were before they entered the trial. And certainly, there was some regression, there was some weight regain, but the important part of the study is that, even after 3.5 years, and even with some weight regain, there were some clinically important effects that lasted.”
“What we feel now is that if we can somehow prepare people better for that time after they finish a weight loss intervention, from a psychological standpoint, it will make a real difference,” he added. “We are very good at helping people have the confidence to lose weight. But having the confidence to lose weight is totally different than having confidence to maintain weight loss. If we can give folks an intervention that has a psychological component, hopefully we can increase their confidence to maintain the weight loss that they attained.”
Study details
Of the 184 participants who were contacted for a follow-up visit, 94 consented to participate, 67% of whom were females and 88% of whom were White. A total of 27 participants had completed the diet and exercise intervention, and another 35 completed the diet-only and 32 exercise-only interventions.
In the 3.5-year period between the IDEA trial’s end and follow-up, body weight increased by 5.9 kg in the diet and exercise group (P < .0001) and by 3.1 kg in the diet-only group (P = .0006) but decreased in the exercise-only group by 1.0 kg (P = .25). However, from baseline to 5-year follow-up, all groups saw a reduction in body weight. Mean weight loss was –3.7 kg for the diet and exercise group (P = .0007), –5.8 kg for the diet group (P < .0001), and –2.9 kg for the exercise group (P = .003). Body mass index also decreased in all groups: by –1.2 kg/m2 in the diet and exercise group (P = .001), by –2.0 kg/m2 in the diet group (P < .0001), and by –1.0 kg/m2 in the exercise group (P = .004).
Pain – as measured by the Western Ontario and McMaster Universities Arthritis Index (WOMAC) score – was reduced in all groups across 5-year follow-up: –1.2 (P = .03) for the diet and exercise group, –1.5 (P = .001) for the diet-only group, and –1.6 (P = .0008) for the exercise-only group. WOMAC function also significantly improved relative to baseline by 6.2 (P = .0001) in the diet and exercise group, by 6.1 (P < .0001) in the diet group, and by 3.7 (P = .01) in the exercise-only group.
Finding time to advise on weight loss, exercise
“If exercise and weight loss were easy, this country wouldn’t be in the state we’re in,” Tuhina Neogi, MD, PhD, of Boston University said in an interview. “Shared decision-making and personalized medicine are important; unfortunately, for the majority of physicians – particularly primary care physicians, where a good deal of OA management is undertaken – they don’t have a lot of time in their 20 minutes with a patient who has OA to counsel individuals toward a healthy weight and physical activity program when they’re also addressing common comorbidities seen in OA such as diabetes and heart disease.
“But as we know,” she added, “when you do address weight loss and physical activity, it has wide-ranging health benefits. This study provides support for utilizing formal diet and exercise programs to achieve important and durable benefits for people with OA.”
Dr. Neogi did note one of the study’s acknowledged limitations: Only slightly more than half of the contacted participants returned for follow-up. Though the authors stated that the individuals who returned were representative of both the pool of potential participants and the IDEA cohort as a whole, “we don’t want to make too many inferences when you don’t have the whole study population available,” she said. “The people who have agreed to come back 3.5 years later for follow-up testing, maybe they are a little more health conscious, more resilient. Those people might be systematically different than the people who [did not return], even though most of the factors were not statistically different between the groups.
“Whatever positive attributes they may have, though, we need to understand more about them,” she added. “We need to know how they maintained the benefits they had 3.5 years prior. That kind of understanding is important to inform long-term strategies in OA management.”
Dr. Messier highlighted a related, ongoing study he’s leading in which more than 800 overweight patients in North Carolina who suffer from knee pain are being led through diet and exercise interventions in a community setting. The goal is to replicate the IDEA results outside of a clinical trial setting and show skeptical physicians that diet and exercise can be enacted and maintained in this subset of patients.
“I think we know how effective weight loss is, especially when combined with exercise, in reducing pain, improving function, improving quality of life in these patients,” he said. “The next step is to allow them to maintain those benefits for a long period of time after the intervention ends.”
The study was supported by grants from the National Institutes of Health and by General Nutrition Centers. Its authors reported no potential conflicts of interest.
Older patients with knee osteoarthritis (OA) who underwent lengthy diet and exercise interventions reported less pain and maintained some weight loss years after the program ended, according to a new study published in Arthritis Care & Research.
“These data imply that clinicians who treat people with knee osteoarthritis have a variety of nonpharmacologic options that preserve clinically important effects 3.5 years after the treatments end,” wrote lead author Stephen P. Messier, PhD, professor and director of the J.B. Snow Biomechanics Laboratory at Wake Forest University, Winston-Salem, N.C.
The study involved patients with overweight or obesity aged 55 years or older who were previously enrolled in the 1.5-year Intensive Diet and Exercise for Arthritis (IDEA) trial.
“You have to remember, this is 3.5 years after the IDEA trial ended,” Dr. Messier said in an interview. “There was no contact with them for that entire time; you’d expect, based on the literature, that they’d revert back to where they were before they entered the trial. And certainly, there was some regression, there was some weight regain, but the important part of the study is that, even after 3.5 years, and even with some weight regain, there were some clinically important effects that lasted.”
“What we feel now is that if we can somehow prepare people better for that time after they finish a weight loss intervention, from a psychological standpoint, it will make a real difference,” he added. “We are very good at helping people have the confidence to lose weight. But having the confidence to lose weight is totally different than having confidence to maintain weight loss. If we can give folks an intervention that has a psychological component, hopefully we can increase their confidence to maintain the weight loss that they attained.”
Study details
Of the 184 participants who were contacted for a follow-up visit, 94 consented to participate, 67% of whom were females and 88% of whom were White. A total of 27 participants had completed the diet and exercise intervention, and another 35 completed the diet-only and 32 exercise-only interventions.
In the 3.5-year period between the IDEA trial’s end and follow-up, body weight increased by 5.9 kg in the diet and exercise group (P < .0001) and by 3.1 kg in the diet-only group (P = .0006) but decreased in the exercise-only group by 1.0 kg (P = .25). However, from baseline to 5-year follow-up, all groups saw a reduction in body weight. Mean weight loss was –3.7 kg for the diet and exercise group (P = .0007), –5.8 kg for the diet group (P < .0001), and –2.9 kg for the exercise group (P = .003). Body mass index also decreased in all groups: by –1.2 kg/m2 in the diet and exercise group (P = .001), by –2.0 kg/m2 in the diet group (P < .0001), and by –1.0 kg/m2 in the exercise group (P = .004).
Pain – as measured by the Western Ontario and McMaster Universities Arthritis Index (WOMAC) score – was reduced in all groups across 5-year follow-up: –1.2 (P = .03) for the diet and exercise group, –1.5 (P = .001) for the diet-only group, and –1.6 (P = .0008) for the exercise-only group. WOMAC function also significantly improved relative to baseline by 6.2 (P = .0001) in the diet and exercise group, by 6.1 (P < .0001) in the diet group, and by 3.7 (P = .01) in the exercise-only group.
Finding time to advise on weight loss, exercise
“If exercise and weight loss were easy, this country wouldn’t be in the state we’re in,” Tuhina Neogi, MD, PhD, of Boston University said in an interview. “Shared decision-making and personalized medicine are important; unfortunately, for the majority of physicians – particularly primary care physicians, where a good deal of OA management is undertaken – they don’t have a lot of time in their 20 minutes with a patient who has OA to counsel individuals toward a healthy weight and physical activity program when they’re also addressing common comorbidities seen in OA such as diabetes and heart disease.
“But as we know,” she added, “when you do address weight loss and physical activity, it has wide-ranging health benefits. This study provides support for utilizing formal diet and exercise programs to achieve important and durable benefits for people with OA.”
Dr. Neogi did note one of the study’s acknowledged limitations: Only slightly more than half of the contacted participants returned for follow-up. Though the authors stated that the individuals who returned were representative of both the pool of potential participants and the IDEA cohort as a whole, “we don’t want to make too many inferences when you don’t have the whole study population available,” she said. “The people who have agreed to come back 3.5 years later for follow-up testing, maybe they are a little more health conscious, more resilient. Those people might be systematically different than the people who [did not return], even though most of the factors were not statistically different between the groups.
“Whatever positive attributes they may have, though, we need to understand more about them,” she added. “We need to know how they maintained the benefits they had 3.5 years prior. That kind of understanding is important to inform long-term strategies in OA management.”
Dr. Messier highlighted a related, ongoing study he’s leading in which more than 800 overweight patients in North Carolina who suffer from knee pain are being led through diet and exercise interventions in a community setting. The goal is to replicate the IDEA results outside of a clinical trial setting and show skeptical physicians that diet and exercise can be enacted and maintained in this subset of patients.
“I think we know how effective weight loss is, especially when combined with exercise, in reducing pain, improving function, improving quality of life in these patients,” he said. “The next step is to allow them to maintain those benefits for a long period of time after the intervention ends.”
The study was supported by grants from the National Institutes of Health and by General Nutrition Centers. Its authors reported no potential conflicts of interest.
Older patients with knee osteoarthritis (OA) who underwent lengthy diet and exercise interventions reported less pain and maintained some weight loss years after the program ended, according to a new study published in Arthritis Care & Research.
“These data imply that clinicians who treat people with knee osteoarthritis have a variety of nonpharmacologic options that preserve clinically important effects 3.5 years after the treatments end,” wrote lead author Stephen P. Messier, PhD, professor and director of the J.B. Snow Biomechanics Laboratory at Wake Forest University, Winston-Salem, N.C.
The study involved patients with overweight or obesity aged 55 years or older who were previously enrolled in the 1.5-year Intensive Diet and Exercise for Arthritis (IDEA) trial.
“You have to remember, this is 3.5 years after the IDEA trial ended,” Dr. Messier said in an interview. “There was no contact with them for that entire time; you’d expect, based on the literature, that they’d revert back to where they were before they entered the trial. And certainly, there was some regression, there was some weight regain, but the important part of the study is that, even after 3.5 years, and even with some weight regain, there were some clinically important effects that lasted.”
“What we feel now is that if we can somehow prepare people better for that time after they finish a weight loss intervention, from a psychological standpoint, it will make a real difference,” he added. “We are very good at helping people have the confidence to lose weight. But having the confidence to lose weight is totally different than having confidence to maintain weight loss. If we can give folks an intervention that has a psychological component, hopefully we can increase their confidence to maintain the weight loss that they attained.”
Study details
Of the 184 participants who were contacted for a follow-up visit, 94 consented to participate, 67% of whom were females and 88% of whom were White. A total of 27 participants had completed the diet and exercise intervention, and another 35 completed the diet-only and 32 exercise-only interventions.
In the 3.5-year period between the IDEA trial’s end and follow-up, body weight increased by 5.9 kg in the diet and exercise group (P < .0001) and by 3.1 kg in the diet-only group (P = .0006) but decreased in the exercise-only group by 1.0 kg (P = .25). However, from baseline to 5-year follow-up, all groups saw a reduction in body weight. Mean weight loss was –3.7 kg for the diet and exercise group (P = .0007), –5.8 kg for the diet group (P < .0001), and –2.9 kg for the exercise group (P = .003). Body mass index also decreased in all groups: by –1.2 kg/m2 in the diet and exercise group (P = .001), by –2.0 kg/m2 in the diet group (P < .0001), and by –1.0 kg/m2 in the exercise group (P = .004).
Pain – as measured by the Western Ontario and McMaster Universities Arthritis Index (WOMAC) score – was reduced in all groups across 5-year follow-up: –1.2 (P = .03) for the diet and exercise group, –1.5 (P = .001) for the diet-only group, and –1.6 (P = .0008) for the exercise-only group. WOMAC function also significantly improved relative to baseline by 6.2 (P = .0001) in the diet and exercise group, by 6.1 (P < .0001) in the diet group, and by 3.7 (P = .01) in the exercise-only group.
Finding time to advise on weight loss, exercise
“If exercise and weight loss were easy, this country wouldn’t be in the state we’re in,” Tuhina Neogi, MD, PhD, of Boston University said in an interview. “Shared decision-making and personalized medicine are important; unfortunately, for the majority of physicians – particularly primary care physicians, where a good deal of OA management is undertaken – they don’t have a lot of time in their 20 minutes with a patient who has OA to counsel individuals toward a healthy weight and physical activity program when they’re also addressing common comorbidities seen in OA such as diabetes and heart disease.
“But as we know,” she added, “when you do address weight loss and physical activity, it has wide-ranging health benefits. This study provides support for utilizing formal diet and exercise programs to achieve important and durable benefits for people with OA.”
Dr. Neogi did note one of the study’s acknowledged limitations: Only slightly more than half of the contacted participants returned for follow-up. Though the authors stated that the individuals who returned were representative of both the pool of potential participants and the IDEA cohort as a whole, “we don’t want to make too many inferences when you don’t have the whole study population available,” she said. “The people who have agreed to come back 3.5 years later for follow-up testing, maybe they are a little more health conscious, more resilient. Those people might be systematically different than the people who [did not return], even though most of the factors were not statistically different between the groups.
“Whatever positive attributes they may have, though, we need to understand more about them,” she added. “We need to know how they maintained the benefits they had 3.5 years prior. That kind of understanding is important to inform long-term strategies in OA management.”
Dr. Messier highlighted a related, ongoing study he’s leading in which more than 800 overweight patients in North Carolina who suffer from knee pain are being led through diet and exercise interventions in a community setting. The goal is to replicate the IDEA results outside of a clinical trial setting and show skeptical physicians that diet and exercise can be enacted and maintained in this subset of patients.
“I think we know how effective weight loss is, especially when combined with exercise, in reducing pain, improving function, improving quality of life in these patients,” he said. “The next step is to allow them to maintain those benefits for a long period of time after the intervention ends.”
The study was supported by grants from the National Institutes of Health and by General Nutrition Centers. Its authors reported no potential conflicts of interest.
FROM ARTHRITIS CARE & RESEARCH
High tibial osteotomy achieves sustained improvements in knee OA
A study of long-term outcomes after medial opening wedge high tibial osteotomy for knee osteoarthritis suggests the procedure is associated with significant and sustained improvements in pain, function, quality of life, and gait biomechanics.
At the OARSI 2021 World Congress, PhD candidate Codie Primeau, MSc, of the Fowler Kennedy Sport Medicine Clinic at the University of Western Ontario, London, presented the findings from a 10-year prospective cohort study of 102 patients with symptomatic medial compartment knee osteoarthritis who underwent medial opening wedge high tibial osteotomy but did not get a total knee replacement during the study.
The surgical procedure aims to correct malalignment by redistributing knee joint loads away from the affected compartment of the knee, with the ultimate goal of slowing disease progression and improving pain and function, Mr. Primeau told the conference, which was sponsored by the Osteoarthritis Research Society International.
At 10 years, the procedure was associated with a mean 14.3-point improvement in the 0-100 Knee Injury and Osteoarthritis Outcome Score (KOOS) for pain, a mean 12-point improvement in the score for function in daily living, a 15.5-point improvement in the score for function in sport and recreation, and a 24.5-point improvement in knee-related quality of life score. Researchers also saw a 35%-45% reduction in the magnitude of the external knee adduction moment from baseline, and a gradual reduction in the knee flexion moment over the course of the study.
While the improvements did decline somewhat over the 10 years, 53% of patients still met the criteria for responder at the end of the follow-up period, meaning that they had a relative change of at least 20% in both KOOS pain and function scores, and an absolute change of at least 10 points.
Mr. Primeau noted that the patient population represented those who were the best candidates for high tibial osteotomy, in that they were keen to avoid total knee replacement.
“While these types of patients may have the best outcomes, our studies suggest patients traditionally not considered ideal candidates for HTO [high tibial osteotomy] – such as females, and patients with limited disease in other knee compartments – also have large improvements in pain and function after HTO, and around 70% of those patients do not get a total knee replacement within 10 years,” he said in an interview.
Mr. Primeau suggested that the improvements achieved with high tibial osteotomy might extend the time before a knee replacement is required, or even help some patients avoid it altogether.
“Importantly, recent studies show HTO does not complicate future joint replacement surgery,” he said. “One can get a knee replacement after HTO; the reverse is not possible.”
The ideal patient for a high tibial osteotomy would be one whose osteoarthritis was confined to the medial compartment of the knee, was younger – in their 40s or 50s – and with relatively high activity levels, he said. Some studies also suggest better outcomes in men than women.
In response to an audience question about the rehabilitation requirements after high tibial osteotomy, Mr. Primeau commented that the design of the plates used in the procedure have changed over time, and this has influenced rehabilitation needs. When the study began, patients needed anywhere from 8 to 12 weeks of no weight bearing, using crutches, to allow for bone consolidation to occur.
“Since then, plate designs have changed a lot, and patients are able to start ambulating as early as 2 weeks after the surgery now,” he said. The rehabilitation is similar to what is required for knee osteoarthritis in general, focusing on range of motion, strengthening, proprioception, and muscle training.
No conflicts of interest were declared.
A study of long-term outcomes after medial opening wedge high tibial osteotomy for knee osteoarthritis suggests the procedure is associated with significant and sustained improvements in pain, function, quality of life, and gait biomechanics.
At the OARSI 2021 World Congress, PhD candidate Codie Primeau, MSc, of the Fowler Kennedy Sport Medicine Clinic at the University of Western Ontario, London, presented the findings from a 10-year prospective cohort study of 102 patients with symptomatic medial compartment knee osteoarthritis who underwent medial opening wedge high tibial osteotomy but did not get a total knee replacement during the study.
The surgical procedure aims to correct malalignment by redistributing knee joint loads away from the affected compartment of the knee, with the ultimate goal of slowing disease progression and improving pain and function, Mr. Primeau told the conference, which was sponsored by the Osteoarthritis Research Society International.
At 10 years, the procedure was associated with a mean 14.3-point improvement in the 0-100 Knee Injury and Osteoarthritis Outcome Score (KOOS) for pain, a mean 12-point improvement in the score for function in daily living, a 15.5-point improvement in the score for function in sport and recreation, and a 24.5-point improvement in knee-related quality of life score. Researchers also saw a 35%-45% reduction in the magnitude of the external knee adduction moment from baseline, and a gradual reduction in the knee flexion moment over the course of the study.
While the improvements did decline somewhat over the 10 years, 53% of patients still met the criteria for responder at the end of the follow-up period, meaning that they had a relative change of at least 20% in both KOOS pain and function scores, and an absolute change of at least 10 points.
Mr. Primeau noted that the patient population represented those who were the best candidates for high tibial osteotomy, in that they were keen to avoid total knee replacement.
“While these types of patients may have the best outcomes, our studies suggest patients traditionally not considered ideal candidates for HTO [high tibial osteotomy] – such as females, and patients with limited disease in other knee compartments – also have large improvements in pain and function after HTO, and around 70% of those patients do not get a total knee replacement within 10 years,” he said in an interview.
Mr. Primeau suggested that the improvements achieved with high tibial osteotomy might extend the time before a knee replacement is required, or even help some patients avoid it altogether.
“Importantly, recent studies show HTO does not complicate future joint replacement surgery,” he said. “One can get a knee replacement after HTO; the reverse is not possible.”
The ideal patient for a high tibial osteotomy would be one whose osteoarthritis was confined to the medial compartment of the knee, was younger – in their 40s or 50s – and with relatively high activity levels, he said. Some studies also suggest better outcomes in men than women.
In response to an audience question about the rehabilitation requirements after high tibial osteotomy, Mr. Primeau commented that the design of the plates used in the procedure have changed over time, and this has influenced rehabilitation needs. When the study began, patients needed anywhere from 8 to 12 weeks of no weight bearing, using crutches, to allow for bone consolidation to occur.
“Since then, plate designs have changed a lot, and patients are able to start ambulating as early as 2 weeks after the surgery now,” he said. The rehabilitation is similar to what is required for knee osteoarthritis in general, focusing on range of motion, strengthening, proprioception, and muscle training.
No conflicts of interest were declared.
A study of long-term outcomes after medial opening wedge high tibial osteotomy for knee osteoarthritis suggests the procedure is associated with significant and sustained improvements in pain, function, quality of life, and gait biomechanics.
At the OARSI 2021 World Congress, PhD candidate Codie Primeau, MSc, of the Fowler Kennedy Sport Medicine Clinic at the University of Western Ontario, London, presented the findings from a 10-year prospective cohort study of 102 patients with symptomatic medial compartment knee osteoarthritis who underwent medial opening wedge high tibial osteotomy but did not get a total knee replacement during the study.
The surgical procedure aims to correct malalignment by redistributing knee joint loads away from the affected compartment of the knee, with the ultimate goal of slowing disease progression and improving pain and function, Mr. Primeau told the conference, which was sponsored by the Osteoarthritis Research Society International.
At 10 years, the procedure was associated with a mean 14.3-point improvement in the 0-100 Knee Injury and Osteoarthritis Outcome Score (KOOS) for pain, a mean 12-point improvement in the score for function in daily living, a 15.5-point improvement in the score for function in sport and recreation, and a 24.5-point improvement in knee-related quality of life score. Researchers also saw a 35%-45% reduction in the magnitude of the external knee adduction moment from baseline, and a gradual reduction in the knee flexion moment over the course of the study.
While the improvements did decline somewhat over the 10 years, 53% of patients still met the criteria for responder at the end of the follow-up period, meaning that they had a relative change of at least 20% in both KOOS pain and function scores, and an absolute change of at least 10 points.
Mr. Primeau noted that the patient population represented those who were the best candidates for high tibial osteotomy, in that they were keen to avoid total knee replacement.
“While these types of patients may have the best outcomes, our studies suggest patients traditionally not considered ideal candidates for HTO [high tibial osteotomy] – such as females, and patients with limited disease in other knee compartments – also have large improvements in pain and function after HTO, and around 70% of those patients do not get a total knee replacement within 10 years,” he said in an interview.
Mr. Primeau suggested that the improvements achieved with high tibial osteotomy might extend the time before a knee replacement is required, or even help some patients avoid it altogether.
“Importantly, recent studies show HTO does not complicate future joint replacement surgery,” he said. “One can get a knee replacement after HTO; the reverse is not possible.”
The ideal patient for a high tibial osteotomy would be one whose osteoarthritis was confined to the medial compartment of the knee, was younger – in their 40s or 50s – and with relatively high activity levels, he said. Some studies also suggest better outcomes in men than women.
In response to an audience question about the rehabilitation requirements after high tibial osteotomy, Mr. Primeau commented that the design of the plates used in the procedure have changed over time, and this has influenced rehabilitation needs. When the study began, patients needed anywhere from 8 to 12 weeks of no weight bearing, using crutches, to allow for bone consolidation to occur.
“Since then, plate designs have changed a lot, and patients are able to start ambulating as early as 2 weeks after the surgery now,” he said. The rehabilitation is similar to what is required for knee osteoarthritis in general, focusing on range of motion, strengthening, proprioception, and muscle training.
No conflicts of interest were declared.
FROM OARSI 2021
Which comes first in osteoarthritis: The damage or the pain?
Is innervation of cartilage the driving force behind development of osteoarthritis and subsequent pain, or is the degeneration of joints in osteoarthritis affecting nerves and creating pain?
This was the question underpinning a fascinating debate at the OARSI 2021 World Congress, featuring two giants of the OA research community: Anne-Marie Malfait, MD, PhD, professor of medicine in the division of rheumatology at Rush Medical College, Chicago, and Stefan Lohmander, MD, PhD, professor emeritus of orthopedics at Lund (Sweden) University in Sweden.
At stake in the discussion is a greater understanding of the physiological processes that underpin both the development of OA in joints and the experience of pain in patients with OA.
Dr. Lohmander started by pointing out that, while pain is the primary symptoms of OA, it does not always overlap with the physiological processes of the disease, as measured by techniques such as MRI, x-ray, biomarkers, and gait analysis.
“This lack of complete overlap is often a problem when doing our clinical trials,” Dr. Lohmander told the conference, sponsored by Osteoarthritis Research Society International. “When talking about osteoarthritis, we also need to remind ourselves every so often that we are speaking of either the symptoms or the disease and maybe not always the both of them.”
While a healthy joint has pain receptors everywhere but the cartilage, studies have found that the osteoarthritic joint brings blood vessels, sensory nerves, and cells expressing nerve growth factor from the subchondral bone into even noncalcified articular cartilage, he said.
These nociceptor neurons are mechanosensitive, so mechanical injury to the joint triggers inflammation, and the inflammatory proteins themselves act on the nociceptors to generate pain signals in the brain, “so clearly, it is the joint that signals the brain,” Dr. Lohmander said.
However, Dr. Malfait pointed out that there is a body of evidence from animal studies showing that the absence of sensory nerves in joints – either from disease or removal – is associated with the onset or worsening of OA.
“Healthy nerves are really important to ensure healthy joints,” Dr. Malfait said. She said age-related loss of sensory nerves always preceded age-related OA, and was also associated with age-related loss of proprioception and vibratory perception.
Interestingly, animal studies suggest that removing intra-articular nociceptors can actually have a protective effect on the osteoarthritic joint, Dr. Malfait said. Studies in humans who have experienced neurologic lesions also suggests improvement in conditions such as rheumatoid arthritis.
She raised the idea of neurogenic inflammation: that peripheral neurons are releasing vasoactive mediators that contribute to inflammation in tissues. “These nerves and nerve products are talking to all the different cells in the joints,” she said.
Defending his argument that joint pathology is the cause of pain, not the pain causing the joint pathology, Dr. Lohmander gave the example of studies that looked at radiographic abnormalities between two knees of the same patient who also had discordant pain measures for each knee. This research “showed strong association between radiographic osteoarthritis and knee pain, supporting the argument that structural abnormalities cause knee pain,” he said.
Martin van der Esch, PhD, of the Amsterdam University of Applied Sciences, said the debate was one of the highlights of the conference because it addressed such an important and longstanding question in OA.
“Is osteoarthritis leading to a generalized pain, so involvement of the nervous system, but the source – the causality – is in the joint?” he said in an interview. “Or is it the other way around, so that means is there first a problem inside the nervous system – including also the vascular system – and which is presented in the joint?”
It is more than an academic discussion because the conclusions of that could mean different treatment approaches are needed for different groups of patients, and raises the different ways of thinking about OA, he said.
None of the sources for this story declared having any relevant conflicts of interest.
Is innervation of cartilage the driving force behind development of osteoarthritis and subsequent pain, or is the degeneration of joints in osteoarthritis affecting nerves and creating pain?
This was the question underpinning a fascinating debate at the OARSI 2021 World Congress, featuring two giants of the OA research community: Anne-Marie Malfait, MD, PhD, professor of medicine in the division of rheumatology at Rush Medical College, Chicago, and Stefan Lohmander, MD, PhD, professor emeritus of orthopedics at Lund (Sweden) University in Sweden.
At stake in the discussion is a greater understanding of the physiological processes that underpin both the development of OA in joints and the experience of pain in patients with OA.
Dr. Lohmander started by pointing out that, while pain is the primary symptoms of OA, it does not always overlap with the physiological processes of the disease, as measured by techniques such as MRI, x-ray, biomarkers, and gait analysis.
“This lack of complete overlap is often a problem when doing our clinical trials,” Dr. Lohmander told the conference, sponsored by Osteoarthritis Research Society International. “When talking about osteoarthritis, we also need to remind ourselves every so often that we are speaking of either the symptoms or the disease and maybe not always the both of them.”
While a healthy joint has pain receptors everywhere but the cartilage, studies have found that the osteoarthritic joint brings blood vessels, sensory nerves, and cells expressing nerve growth factor from the subchondral bone into even noncalcified articular cartilage, he said.
These nociceptor neurons are mechanosensitive, so mechanical injury to the joint triggers inflammation, and the inflammatory proteins themselves act on the nociceptors to generate pain signals in the brain, “so clearly, it is the joint that signals the brain,” Dr. Lohmander said.
However, Dr. Malfait pointed out that there is a body of evidence from animal studies showing that the absence of sensory nerves in joints – either from disease or removal – is associated with the onset or worsening of OA.
“Healthy nerves are really important to ensure healthy joints,” Dr. Malfait said. She said age-related loss of sensory nerves always preceded age-related OA, and was also associated with age-related loss of proprioception and vibratory perception.
Interestingly, animal studies suggest that removing intra-articular nociceptors can actually have a protective effect on the osteoarthritic joint, Dr. Malfait said. Studies in humans who have experienced neurologic lesions also suggests improvement in conditions such as rheumatoid arthritis.
She raised the idea of neurogenic inflammation: that peripheral neurons are releasing vasoactive mediators that contribute to inflammation in tissues. “These nerves and nerve products are talking to all the different cells in the joints,” she said.
Defending his argument that joint pathology is the cause of pain, not the pain causing the joint pathology, Dr. Lohmander gave the example of studies that looked at radiographic abnormalities between two knees of the same patient who also had discordant pain measures for each knee. This research “showed strong association between radiographic osteoarthritis and knee pain, supporting the argument that structural abnormalities cause knee pain,” he said.
Martin van der Esch, PhD, of the Amsterdam University of Applied Sciences, said the debate was one of the highlights of the conference because it addressed such an important and longstanding question in OA.
“Is osteoarthritis leading to a generalized pain, so involvement of the nervous system, but the source – the causality – is in the joint?” he said in an interview. “Or is it the other way around, so that means is there first a problem inside the nervous system – including also the vascular system – and which is presented in the joint?”
It is more than an academic discussion because the conclusions of that could mean different treatment approaches are needed for different groups of patients, and raises the different ways of thinking about OA, he said.
None of the sources for this story declared having any relevant conflicts of interest.
Is innervation of cartilage the driving force behind development of osteoarthritis and subsequent pain, or is the degeneration of joints in osteoarthritis affecting nerves and creating pain?
This was the question underpinning a fascinating debate at the OARSI 2021 World Congress, featuring two giants of the OA research community: Anne-Marie Malfait, MD, PhD, professor of medicine in the division of rheumatology at Rush Medical College, Chicago, and Stefan Lohmander, MD, PhD, professor emeritus of orthopedics at Lund (Sweden) University in Sweden.
At stake in the discussion is a greater understanding of the physiological processes that underpin both the development of OA in joints and the experience of pain in patients with OA.
Dr. Lohmander started by pointing out that, while pain is the primary symptoms of OA, it does not always overlap with the physiological processes of the disease, as measured by techniques such as MRI, x-ray, biomarkers, and gait analysis.
“This lack of complete overlap is often a problem when doing our clinical trials,” Dr. Lohmander told the conference, sponsored by Osteoarthritis Research Society International. “When talking about osteoarthritis, we also need to remind ourselves every so often that we are speaking of either the symptoms or the disease and maybe not always the both of them.”
While a healthy joint has pain receptors everywhere but the cartilage, studies have found that the osteoarthritic joint brings blood vessels, sensory nerves, and cells expressing nerve growth factor from the subchondral bone into even noncalcified articular cartilage, he said.
These nociceptor neurons are mechanosensitive, so mechanical injury to the joint triggers inflammation, and the inflammatory proteins themselves act on the nociceptors to generate pain signals in the brain, “so clearly, it is the joint that signals the brain,” Dr. Lohmander said.
However, Dr. Malfait pointed out that there is a body of evidence from animal studies showing that the absence of sensory nerves in joints – either from disease or removal – is associated with the onset or worsening of OA.
“Healthy nerves are really important to ensure healthy joints,” Dr. Malfait said. She said age-related loss of sensory nerves always preceded age-related OA, and was also associated with age-related loss of proprioception and vibratory perception.
Interestingly, animal studies suggest that removing intra-articular nociceptors can actually have a protective effect on the osteoarthritic joint, Dr. Malfait said. Studies in humans who have experienced neurologic lesions also suggests improvement in conditions such as rheumatoid arthritis.
She raised the idea of neurogenic inflammation: that peripheral neurons are releasing vasoactive mediators that contribute to inflammation in tissues. “These nerves and nerve products are talking to all the different cells in the joints,” she said.
Defending his argument that joint pathology is the cause of pain, not the pain causing the joint pathology, Dr. Lohmander gave the example of studies that looked at radiographic abnormalities between two knees of the same patient who also had discordant pain measures for each knee. This research “showed strong association between radiographic osteoarthritis and knee pain, supporting the argument that structural abnormalities cause knee pain,” he said.
Martin van der Esch, PhD, of the Amsterdam University of Applied Sciences, said the debate was one of the highlights of the conference because it addressed such an important and longstanding question in OA.
“Is osteoarthritis leading to a generalized pain, so involvement of the nervous system, but the source – the causality – is in the joint?” he said in an interview. “Or is it the other way around, so that means is there first a problem inside the nervous system – including also the vascular system – and which is presented in the joint?”
It is more than an academic discussion because the conclusions of that could mean different treatment approaches are needed for different groups of patients, and raises the different ways of thinking about OA, he said.
None of the sources for this story declared having any relevant conflicts of interest.
FROM OARSI 2021
Stable, supportive shoes reduce walking pain in severe knee OA
Wearing stable, supportive footwear reduces knee pain to a significantly greater extent than what’s felt with flat, flexible shoes in patients with severe knee osteoarthritis, according to results of a randomized, controlled trial presented at the OARSI 2021 World Congress.
Clinical guidelines for knee OA emphasize the importance of patients self-managing their condition with exercise, weight control, and appropriate footwear. However, there is limited evidence on which footwear is best, and some guidelines advocate stable supportive shoes based solely on expert opinion, Kade Paterson, PhD, of the University of Melbourne told the conference, sponsored by Osteoarthritis Research Society International.
“Recent research suggests that another type of shoe style – termed flat, flexible shoes – may be more beneficial,” Dr. Paterson said, citing a randomized, controlled trial that found greater improvement in pain and function with flat flexible shoes, compared with neutral tennis shoes. “Flat, flexible shoes are generally lighter, and have thinner, more flexible soles.”
In this study, which was published earlier this year in Annals of Internal Medicine, 164 individuals with knee OA who had experienced knee pain on most days of the past month were randomized to wear either stable, supportive shoes or flat, flexible shoes for at least 6 hours a day for 6 months. Six of each shoe type – three male styles and three female styles – were offered, having been chosen based on a survey in which participants were asked about a selection of commercially available shoes they were most likely to wear.
Researchers found participants who wore the stable, supportive shoes had significantly greater reductions in knee pain on walking during the previous week, representing a mean difference of 1.1 units on an 11-point numerical rating scale. More patients in the stable, supportive shoe arm of the study achieved minimal clinically important difference in pain than did those in the flat, flexible shoe group.
Stable, supportive shoes were also associated with greater improvements in knee-related quality of life scores and greater improvements in overall pain. However, there was no significant difference between the two groups in function. Patients wearing flat, flexible shoes reported significantly more adverse events – mainly onset of or increases in knee pain.
Dr. Paterson said the results were surprising, given previous research suggesting a benefit from lighter flat, flexible shoes. “Some previous research showed that those shoes reduced knee joint forces that were associated with pain and reduced it more than stable, supportive shoes, and based on the biomechanical research, we thought would be flat, flexible shoes,” he said in an interview.
Another observation to come from the study was the poor quality of most patients’ everyday shoes. Dr. Paterson said that most of the participants’ usual shoes were very old, and many were also wearing inappropriate footwear for knee OA, including shoes with heels or slippers.
“We would strongly recommend that clinicians ask patients to even bring in their most commonly worn shoes and then recommend new shoes, and based on our data, certainly stable supportive shoes,” he said.
Commenting on the findings, Jos Runhaar, PhD, of Erasmus University Medical Center in Rotterdam, the Netherlands, said this study provided high-quality evidence for this specific intervention in this specific group of patients, namely those with more severe, end-stage OA who had long-lasting changes in their foot posture and gait.
“Based on this, I would say that restoring the original posture of the foot – because that’s how the stable, supportive shoes are probably designed – is more beneficial than actually supporting the natural gait that people are already adapted to at that stage,” Dr. Runhaar said in an interview.
Dr. Paterson noted that the findings of the study were not generalizable to people with mild knee OA, and also that the study did not compare either shoe type with participants’ usual shoes.
The study and three authors were supported by the Australian National Health and Medical Research Council. No conflicts of interest were declared.
Wearing stable, supportive footwear reduces knee pain to a significantly greater extent than what’s felt with flat, flexible shoes in patients with severe knee osteoarthritis, according to results of a randomized, controlled trial presented at the OARSI 2021 World Congress.
Clinical guidelines for knee OA emphasize the importance of patients self-managing their condition with exercise, weight control, and appropriate footwear. However, there is limited evidence on which footwear is best, and some guidelines advocate stable supportive shoes based solely on expert opinion, Kade Paterson, PhD, of the University of Melbourne told the conference, sponsored by Osteoarthritis Research Society International.
“Recent research suggests that another type of shoe style – termed flat, flexible shoes – may be more beneficial,” Dr. Paterson said, citing a randomized, controlled trial that found greater improvement in pain and function with flat flexible shoes, compared with neutral tennis shoes. “Flat, flexible shoes are generally lighter, and have thinner, more flexible soles.”
In this study, which was published earlier this year in Annals of Internal Medicine, 164 individuals with knee OA who had experienced knee pain on most days of the past month were randomized to wear either stable, supportive shoes or flat, flexible shoes for at least 6 hours a day for 6 months. Six of each shoe type – three male styles and three female styles – were offered, having been chosen based on a survey in which participants were asked about a selection of commercially available shoes they were most likely to wear.
Researchers found participants who wore the stable, supportive shoes had significantly greater reductions in knee pain on walking during the previous week, representing a mean difference of 1.1 units on an 11-point numerical rating scale. More patients in the stable, supportive shoe arm of the study achieved minimal clinically important difference in pain than did those in the flat, flexible shoe group.
Stable, supportive shoes were also associated with greater improvements in knee-related quality of life scores and greater improvements in overall pain. However, there was no significant difference between the two groups in function. Patients wearing flat, flexible shoes reported significantly more adverse events – mainly onset of or increases in knee pain.
Dr. Paterson said the results were surprising, given previous research suggesting a benefit from lighter flat, flexible shoes. “Some previous research showed that those shoes reduced knee joint forces that were associated with pain and reduced it more than stable, supportive shoes, and based on the biomechanical research, we thought would be flat, flexible shoes,” he said in an interview.
Another observation to come from the study was the poor quality of most patients’ everyday shoes. Dr. Paterson said that most of the participants’ usual shoes were very old, and many were also wearing inappropriate footwear for knee OA, including shoes with heels or slippers.
“We would strongly recommend that clinicians ask patients to even bring in their most commonly worn shoes and then recommend new shoes, and based on our data, certainly stable supportive shoes,” he said.
Commenting on the findings, Jos Runhaar, PhD, of Erasmus University Medical Center in Rotterdam, the Netherlands, said this study provided high-quality evidence for this specific intervention in this specific group of patients, namely those with more severe, end-stage OA who had long-lasting changes in their foot posture and gait.
“Based on this, I would say that restoring the original posture of the foot – because that’s how the stable, supportive shoes are probably designed – is more beneficial than actually supporting the natural gait that people are already adapted to at that stage,” Dr. Runhaar said in an interview.
Dr. Paterson noted that the findings of the study were not generalizable to people with mild knee OA, and also that the study did not compare either shoe type with participants’ usual shoes.
The study and three authors were supported by the Australian National Health and Medical Research Council. No conflicts of interest were declared.
Wearing stable, supportive footwear reduces knee pain to a significantly greater extent than what’s felt with flat, flexible shoes in patients with severe knee osteoarthritis, according to results of a randomized, controlled trial presented at the OARSI 2021 World Congress.
Clinical guidelines for knee OA emphasize the importance of patients self-managing their condition with exercise, weight control, and appropriate footwear. However, there is limited evidence on which footwear is best, and some guidelines advocate stable supportive shoes based solely on expert opinion, Kade Paterson, PhD, of the University of Melbourne told the conference, sponsored by Osteoarthritis Research Society International.
“Recent research suggests that another type of shoe style – termed flat, flexible shoes – may be more beneficial,” Dr. Paterson said, citing a randomized, controlled trial that found greater improvement in pain and function with flat flexible shoes, compared with neutral tennis shoes. “Flat, flexible shoes are generally lighter, and have thinner, more flexible soles.”
In this study, which was published earlier this year in Annals of Internal Medicine, 164 individuals with knee OA who had experienced knee pain on most days of the past month were randomized to wear either stable, supportive shoes or flat, flexible shoes for at least 6 hours a day for 6 months. Six of each shoe type – three male styles and three female styles – were offered, having been chosen based on a survey in which participants were asked about a selection of commercially available shoes they were most likely to wear.
Researchers found participants who wore the stable, supportive shoes had significantly greater reductions in knee pain on walking during the previous week, representing a mean difference of 1.1 units on an 11-point numerical rating scale. More patients in the stable, supportive shoe arm of the study achieved minimal clinically important difference in pain than did those in the flat, flexible shoe group.
Stable, supportive shoes were also associated with greater improvements in knee-related quality of life scores and greater improvements in overall pain. However, there was no significant difference between the two groups in function. Patients wearing flat, flexible shoes reported significantly more adverse events – mainly onset of or increases in knee pain.
Dr. Paterson said the results were surprising, given previous research suggesting a benefit from lighter flat, flexible shoes. “Some previous research showed that those shoes reduced knee joint forces that were associated with pain and reduced it more than stable, supportive shoes, and based on the biomechanical research, we thought would be flat, flexible shoes,” he said in an interview.
Another observation to come from the study was the poor quality of most patients’ everyday shoes. Dr. Paterson said that most of the participants’ usual shoes were very old, and many were also wearing inappropriate footwear for knee OA, including shoes with heels or slippers.
“We would strongly recommend that clinicians ask patients to even bring in their most commonly worn shoes and then recommend new shoes, and based on our data, certainly stable supportive shoes,” he said.
Commenting on the findings, Jos Runhaar, PhD, of Erasmus University Medical Center in Rotterdam, the Netherlands, said this study provided high-quality evidence for this specific intervention in this specific group of patients, namely those with more severe, end-stage OA who had long-lasting changes in their foot posture and gait.
“Based on this, I would say that restoring the original posture of the foot – because that’s how the stable, supportive shoes are probably designed – is more beneficial than actually supporting the natural gait that people are already adapted to at that stage,” Dr. Runhaar said in an interview.
Dr. Paterson noted that the findings of the study were not generalizable to people with mild knee OA, and also that the study did not compare either shoe type with participants’ usual shoes.
The study and three authors were supported by the Australian National Health and Medical Research Council. No conflicts of interest were declared.
FROM OARSI 2021