User login
Is Immunotherapy Best for Unresectable HCC with Moderate Liver Dysfunction?
In the last 10 years, clinical outcomes have improved for patients with unresectable hepatocellular carcinoma (uHCC). The cancer generally comes with chronic liver inflammation, and liver cirrhosis is present in up to 80% of cases.
Clinical trials that have tested systemic immunotherapies have excluded patients who don’t fall into the Child-Pugh class A criteria (CP-A) for liver disease, which is the least severe of the Child-Pugh classes A-C. Therefore, there has been much debate about whether patients who have more liver disease (moderate liver dysfunction) and fit under CP-B criteria, instead of CP-A, should be treated with immune checkpoint inhibitor (ICI) therapy or best supportive care (BSC).
A new study, led by Claudia Angela Maria Fulgenzi, MD, with the Department of Surgery and Cancer at the Imperial College London, England, published in JAMA Oncology on July 18, uses an alternative way to compare outcomes following two different paths of care for uHCC patients with moderate liver dysfunction.
How was the study done and what did the investigators find?
Researchers performed a retrospective, multicenter, international clinical case series of patients treated in routine practice in tertiary care centers across Europe, the United States, and Asia. They compared data from uHCC patients with CP-B who were receiving first-line ICI-based treatment regimens (n = 187) with a cohort of matched patients with CP-B receiving BSC (n = 156). The first-line immunotherapies were the monotherapy nivolumab or the combination (atezolizumab plus bevacizumab).
Immunotherapy was linked with significantly lower risk of death, compared with best supportive care.
ICI exposure was associated with a reduction of about 50% in the risk of death (hazard ratio, 0.55; 95% CI, 0.35-0.86; P < .001).
Is immunotherapy or best supportive care the superior treatment?
The authors wrote that the results point to “improved survival in association with ICI treatment, compared with BSC in patients with uHCC with CP-B liver dysfunction.”
According to the study’s senior author David Pinato, MD, PhD, “this is the first study to suggest that there might be an advantage [of treatment with immunotherapy] in a proportion of people with Child-Pugh B liver dysfunction and particularly so in those patients with more limited disease and portal vein tumor thrombosis.”
Will the findings of this study make treatment allocation for patients with uHCC and moderate liver dysfunction (CP-B) less controversial?
Because it is a retrospective study, Dr. Pinato said in an interview, that the findings are not definitive, but can be used to inform future randomized controlled trials.
Dr. Pinato, who is also with the Imperial College London, added that the findings may also introduce a new question.
Although the study was not powered to look at survival differences across the two immunotherapy options given to the patients, there did not seem to be a striking difference between using one immunotherapy (nivolumab) or a combination (atezolizumab plus bevacizumab), he said.
“This is quite important because we know that combinations are significantly superior to monotherapy in patients with normal liver function but based on our study we might say that this provides preliminary evidence that [superiority of combination therapy] might not be true if the liver function is worse.”
What do these findings add to the literature about how best to treat patients with uHCC and suboptimal liver function?
Without evidence of efficacy and safety for the group in previous studies, the widespread recommendation for those with moderate dysfunction has been BSC.
These findings “pave the way to select potential patient subgroups in clinical practice,” Dr. Pinato said. It also suggests that the safety level of immunotherapy treatments is acceptable in this patient population, so they are not necessarily disadvantaged compared to patients with more preserved liver function.
“This is the best level of evidence currently available to guide treatment decisions in patients with Child-Pugh B who have been universally excluded by prospective clinical trials and for whom there is no randomized comparison,” Dr. Pinato said.
Dr. Pinato reported personal fees from Roche, AstraZeneca, Eisai, Mina Therapeutics, Starpharma, Lift Biosciences, Boston Scientific, and Avammune, and grants from GSK, MSD, and BMS outside the submitted work. Dr. Fulgenzi has no disclosures. Other authors of the new research have multiple ties with pharmaceutical companies. Complete disclosures are available with the full text of the journal article.
In the last 10 years, clinical outcomes have improved for patients with unresectable hepatocellular carcinoma (uHCC). The cancer generally comes with chronic liver inflammation, and liver cirrhosis is present in up to 80% of cases.
Clinical trials that have tested systemic immunotherapies have excluded patients who don’t fall into the Child-Pugh class A criteria (CP-A) for liver disease, which is the least severe of the Child-Pugh classes A-C. Therefore, there has been much debate about whether patients who have more liver disease (moderate liver dysfunction) and fit under CP-B criteria, instead of CP-A, should be treated with immune checkpoint inhibitor (ICI) therapy or best supportive care (BSC).
A new study, led by Claudia Angela Maria Fulgenzi, MD, with the Department of Surgery and Cancer at the Imperial College London, England, published in JAMA Oncology on July 18, uses an alternative way to compare outcomes following two different paths of care for uHCC patients with moderate liver dysfunction.
How was the study done and what did the investigators find?
Researchers performed a retrospective, multicenter, international clinical case series of patients treated in routine practice in tertiary care centers across Europe, the United States, and Asia. They compared data from uHCC patients with CP-B who were receiving first-line ICI-based treatment regimens (n = 187) with a cohort of matched patients with CP-B receiving BSC (n = 156). The first-line immunotherapies were the monotherapy nivolumab or the combination (atezolizumab plus bevacizumab).
Immunotherapy was linked with significantly lower risk of death, compared with best supportive care.
ICI exposure was associated with a reduction of about 50% in the risk of death (hazard ratio, 0.55; 95% CI, 0.35-0.86; P < .001).
Is immunotherapy or best supportive care the superior treatment?
The authors wrote that the results point to “improved survival in association with ICI treatment, compared with BSC in patients with uHCC with CP-B liver dysfunction.”
According to the study’s senior author David Pinato, MD, PhD, “this is the first study to suggest that there might be an advantage [of treatment with immunotherapy] in a proportion of people with Child-Pugh B liver dysfunction and particularly so in those patients with more limited disease and portal vein tumor thrombosis.”
Will the findings of this study make treatment allocation for patients with uHCC and moderate liver dysfunction (CP-B) less controversial?
Because it is a retrospective study, Dr. Pinato said in an interview, that the findings are not definitive, but can be used to inform future randomized controlled trials.
Dr. Pinato, who is also with the Imperial College London, added that the findings may also introduce a new question.
Although the study was not powered to look at survival differences across the two immunotherapy options given to the patients, there did not seem to be a striking difference between using one immunotherapy (nivolumab) or a combination (atezolizumab plus bevacizumab), he said.
“This is quite important because we know that combinations are significantly superior to monotherapy in patients with normal liver function but based on our study we might say that this provides preliminary evidence that [superiority of combination therapy] might not be true if the liver function is worse.”
What do these findings add to the literature about how best to treat patients with uHCC and suboptimal liver function?
Without evidence of efficacy and safety for the group in previous studies, the widespread recommendation for those with moderate dysfunction has been BSC.
These findings “pave the way to select potential patient subgroups in clinical practice,” Dr. Pinato said. It also suggests that the safety level of immunotherapy treatments is acceptable in this patient population, so they are not necessarily disadvantaged compared to patients with more preserved liver function.
“This is the best level of evidence currently available to guide treatment decisions in patients with Child-Pugh B who have been universally excluded by prospective clinical trials and for whom there is no randomized comparison,” Dr. Pinato said.
Dr. Pinato reported personal fees from Roche, AstraZeneca, Eisai, Mina Therapeutics, Starpharma, Lift Biosciences, Boston Scientific, and Avammune, and grants from GSK, MSD, and BMS outside the submitted work. Dr. Fulgenzi has no disclosures. Other authors of the new research have multiple ties with pharmaceutical companies. Complete disclosures are available with the full text of the journal article.
In the last 10 years, clinical outcomes have improved for patients with unresectable hepatocellular carcinoma (uHCC). The cancer generally comes with chronic liver inflammation, and liver cirrhosis is present in up to 80% of cases.
Clinical trials that have tested systemic immunotherapies have excluded patients who don’t fall into the Child-Pugh class A criteria (CP-A) for liver disease, which is the least severe of the Child-Pugh classes A-C. Therefore, there has been much debate about whether patients who have more liver disease (moderate liver dysfunction) and fit under CP-B criteria, instead of CP-A, should be treated with immune checkpoint inhibitor (ICI) therapy or best supportive care (BSC).
A new study, led by Claudia Angela Maria Fulgenzi, MD, with the Department of Surgery and Cancer at the Imperial College London, England, published in JAMA Oncology on July 18, uses an alternative way to compare outcomes following two different paths of care for uHCC patients with moderate liver dysfunction.
How was the study done and what did the investigators find?
Researchers performed a retrospective, multicenter, international clinical case series of patients treated in routine practice in tertiary care centers across Europe, the United States, and Asia. They compared data from uHCC patients with CP-B who were receiving first-line ICI-based treatment regimens (n = 187) with a cohort of matched patients with CP-B receiving BSC (n = 156). The first-line immunotherapies were the monotherapy nivolumab or the combination (atezolizumab plus bevacizumab).
Immunotherapy was linked with significantly lower risk of death, compared with best supportive care.
ICI exposure was associated with a reduction of about 50% in the risk of death (hazard ratio, 0.55; 95% CI, 0.35-0.86; P < .001).
Is immunotherapy or best supportive care the superior treatment?
The authors wrote that the results point to “improved survival in association with ICI treatment, compared with BSC in patients with uHCC with CP-B liver dysfunction.”
According to the study’s senior author David Pinato, MD, PhD, “this is the first study to suggest that there might be an advantage [of treatment with immunotherapy] in a proportion of people with Child-Pugh B liver dysfunction and particularly so in those patients with more limited disease and portal vein tumor thrombosis.”
Will the findings of this study make treatment allocation for patients with uHCC and moderate liver dysfunction (CP-B) less controversial?
Because it is a retrospective study, Dr. Pinato said in an interview, that the findings are not definitive, but can be used to inform future randomized controlled trials.
Dr. Pinato, who is also with the Imperial College London, added that the findings may also introduce a new question.
Although the study was not powered to look at survival differences across the two immunotherapy options given to the patients, there did not seem to be a striking difference between using one immunotherapy (nivolumab) or a combination (atezolizumab plus bevacizumab), he said.
“This is quite important because we know that combinations are significantly superior to monotherapy in patients with normal liver function but based on our study we might say that this provides preliminary evidence that [superiority of combination therapy] might not be true if the liver function is worse.”
What do these findings add to the literature about how best to treat patients with uHCC and suboptimal liver function?
Without evidence of efficacy and safety for the group in previous studies, the widespread recommendation for those with moderate dysfunction has been BSC.
These findings “pave the way to select potential patient subgroups in clinical practice,” Dr. Pinato said. It also suggests that the safety level of immunotherapy treatments is acceptable in this patient population, so they are not necessarily disadvantaged compared to patients with more preserved liver function.
“This is the best level of evidence currently available to guide treatment decisions in patients with Child-Pugh B who have been universally excluded by prospective clinical trials and for whom there is no randomized comparison,” Dr. Pinato said.
Dr. Pinato reported personal fees from Roche, AstraZeneca, Eisai, Mina Therapeutics, Starpharma, Lift Biosciences, Boston Scientific, and Avammune, and grants from GSK, MSD, and BMS outside the submitted work. Dr. Fulgenzi has no disclosures. Other authors of the new research have multiple ties with pharmaceutical companies. Complete disclosures are available with the full text of the journal article.
FROM JAMA ONCOLOGY
Could total mesometrial resection become a new standard treatment for cervical cancer?
These findings suggest that TMMR may be considered a primary treatment option for both early-stage and locally advanced cervical cancer confined to the Müllerian compartment, reported lead author Henrik Falconer, MD, PhD, of Karolinska Institutet, Stockholm, Sweden, and colleagues.
What is the rationale behind TMMR?
“Current international guidelines [for cervical cancer] are primarily based on retrospective case series and a small number of outdated randomized controlled trials,” the investigators wrote in EClinicalMedicine, part of The Lancet publication platform. “The stage-dependent treatment recommendations, with surgery advised for early-stage and radiation therapy for locally advanced disease, may be considered too simplistic, suggesting that early stages of cervical cancer cannot be controlled with surgical resection alone or that locally advanced cervical cancer is inoperable.”
This mindset, they noted, overlooks the complexities of cancer spread. In contrast, TMMR and similar surgical approaches based on the cancer field model are mapped along routes of locoregional dissemination, leading to “excellent local control” in more than 600 cases at the University Hospital of Leipzig, Leipzig, Germany.
To date, however, TMMR’s adoption has been limited, and it has not been compared directly with current guideline treatments, prompting the present study.
What methods were used to compare TMMR with standard treatment?
The study compared TMMR plus therapeutic lymph node dissection (tLND) without adjuvant radiation versus standard treatment (ST) for early-stage (FIGO 2009 IB1, IIA1) and locally advanced (FIGO 2009 IB2, IIA2, IIB) cervical cancer. Standard treatment for patients with early-stage disease involved radical hysterectomy and pelvic lymphadenectomy, with adjuvant chemoradiation dependent upon final pathology. Those with locally advanced disease received definitive chemoradiation.
Data for the standard treatment group were drawn from population-based registries in Sweden, while those for the TMMR group came from the Leipzig Mesometrial Resection Study Database. The final dataset included 1,007 women treated between 2011 and 2020, with 733 undergoing standard treatment and 274 receiving TMMR.
Outcomes included RFS and OS, adjusted for clinical and tumor-related variables.
How did TMMR compare with standard treatment?
TMMR was associated with superior oncologic outcomes compared with standard treatment for early-stage cervical cancer.
Specifically, 5-year RFS was 91.2% for TMMR versus 81.8% for standard therapy (P = .002). In the adjusted analysis, TMMR was associated with a significantly lower hazard of recurrence (hazard ratio [HR], 0.39; 95% CI, 0.22–0.69) and death (HR, 0.42; 95% CI, 0.21-0.86). Also favoring TMMR, absolute difference in the risk of recurrence at 5 years was 9.4% (95% CI 3.2–15.7). In addition, 5-year OS was better in the TMMR group, at 93.3%, compared with 90.3% for standard treatment (P = .034).
Among patients with locally advanced disease, no significant differences in RFS or OS were observed.
Are these data strong enough to make TMMR the new standard treatment?
Dr. Falconer and colleagues concluded that TMMR with tLND “may replace the standard treatment approach in early-stage cervical cancer and furthermore be evaluated as an option in locally advanced cervical cancer confined to the Müllerian compartment.”
While the investigators anticipated demands for randomized controlled trials, they questioned the value of such studies, suggesting that any control arm would be “based on inconsistent or flawed concepts.”
Susan C. Modesitt, MD, director of the gynecologic oncology division of Winship Cancer Institute of Emory University, Atlanta, offered a different perspective.
“They do show encouraging data in the early stage,” Dr. Modesitt said in an interview, “but I would still want to see a randomized controlled trial, because we’ve been burned before.”
She cited the LACC trial, which dispelled strong convictions about the alleged superiority of minimally invasive radical hysterectomy.
“We thought minimally invasive was so good, and we should be doing that to everybody, but we did a trial, and we found worse outcomes,” Dr. Modesitt said. “More of those early-stage women died.”
Dr. Modesitt also pointed out the lack of safety data in the present publication.
“TMMR is a bigger procedure, so I would expect more complications,” she said, noting that rates of urinary injury, nerve injury, and readmission need to be considered alongside efficacy outcomes.
How does TMMR fit into the current treatment landscape for cervical cancer?
“This is a very niche surgery that most places don’t do,” Dr. Modesitt said.
She pointed out that “multiple variations” on the standard radical hysterectomy have been proposed in the past, such as the laterally extended endopelvic resection.
“[TMMR] is not a new concept,” she said. “It’s just a question of how radical it is.”
Instead of developing new types of radical surgery, she said, the trend in the United States is toward de-escalation of surgical treatments altogether, with greater reliance upon medical options, such as immunotherapy.
“[This study] is thought provoking, and I applaud them for doing it,” Dr. Modesitt said. “But I’m not going to go out and do that on my next patient.”
This study was supported by grants from Centre for Clinical Research Sörmland (Sweden) and Region Stockholm (Sweden). Dr. Falconer is a board member of Surgical Science.
These findings suggest that TMMR may be considered a primary treatment option for both early-stage and locally advanced cervical cancer confined to the Müllerian compartment, reported lead author Henrik Falconer, MD, PhD, of Karolinska Institutet, Stockholm, Sweden, and colleagues.
What is the rationale behind TMMR?
“Current international guidelines [for cervical cancer] are primarily based on retrospective case series and a small number of outdated randomized controlled trials,” the investigators wrote in EClinicalMedicine, part of The Lancet publication platform. “The stage-dependent treatment recommendations, with surgery advised for early-stage and radiation therapy for locally advanced disease, may be considered too simplistic, suggesting that early stages of cervical cancer cannot be controlled with surgical resection alone or that locally advanced cervical cancer is inoperable.”
This mindset, they noted, overlooks the complexities of cancer spread. In contrast, TMMR and similar surgical approaches based on the cancer field model are mapped along routes of locoregional dissemination, leading to “excellent local control” in more than 600 cases at the University Hospital of Leipzig, Leipzig, Germany.
To date, however, TMMR’s adoption has been limited, and it has not been compared directly with current guideline treatments, prompting the present study.
What methods were used to compare TMMR with standard treatment?
The study compared TMMR plus therapeutic lymph node dissection (tLND) without adjuvant radiation versus standard treatment (ST) for early-stage (FIGO 2009 IB1, IIA1) and locally advanced (FIGO 2009 IB2, IIA2, IIB) cervical cancer. Standard treatment for patients with early-stage disease involved radical hysterectomy and pelvic lymphadenectomy, with adjuvant chemoradiation dependent upon final pathology. Those with locally advanced disease received definitive chemoradiation.
Data for the standard treatment group were drawn from population-based registries in Sweden, while those for the TMMR group came from the Leipzig Mesometrial Resection Study Database. The final dataset included 1,007 women treated between 2011 and 2020, with 733 undergoing standard treatment and 274 receiving TMMR.
Outcomes included RFS and OS, adjusted for clinical and tumor-related variables.
How did TMMR compare with standard treatment?
TMMR was associated with superior oncologic outcomes compared with standard treatment for early-stage cervical cancer.
Specifically, 5-year RFS was 91.2% for TMMR versus 81.8% for standard therapy (P = .002). In the adjusted analysis, TMMR was associated with a significantly lower hazard of recurrence (hazard ratio [HR], 0.39; 95% CI, 0.22–0.69) and death (HR, 0.42; 95% CI, 0.21-0.86). Also favoring TMMR, absolute difference in the risk of recurrence at 5 years was 9.4% (95% CI 3.2–15.7). In addition, 5-year OS was better in the TMMR group, at 93.3%, compared with 90.3% for standard treatment (P = .034).
Among patients with locally advanced disease, no significant differences in RFS or OS were observed.
Are these data strong enough to make TMMR the new standard treatment?
Dr. Falconer and colleagues concluded that TMMR with tLND “may replace the standard treatment approach in early-stage cervical cancer and furthermore be evaluated as an option in locally advanced cervical cancer confined to the Müllerian compartment.”
While the investigators anticipated demands for randomized controlled trials, they questioned the value of such studies, suggesting that any control arm would be “based on inconsistent or flawed concepts.”
Susan C. Modesitt, MD, director of the gynecologic oncology division of Winship Cancer Institute of Emory University, Atlanta, offered a different perspective.
“They do show encouraging data in the early stage,” Dr. Modesitt said in an interview, “but I would still want to see a randomized controlled trial, because we’ve been burned before.”
She cited the LACC trial, which dispelled strong convictions about the alleged superiority of minimally invasive radical hysterectomy.
“We thought minimally invasive was so good, and we should be doing that to everybody, but we did a trial, and we found worse outcomes,” Dr. Modesitt said. “More of those early-stage women died.”
Dr. Modesitt also pointed out the lack of safety data in the present publication.
“TMMR is a bigger procedure, so I would expect more complications,” she said, noting that rates of urinary injury, nerve injury, and readmission need to be considered alongside efficacy outcomes.
How does TMMR fit into the current treatment landscape for cervical cancer?
“This is a very niche surgery that most places don’t do,” Dr. Modesitt said.
She pointed out that “multiple variations” on the standard radical hysterectomy have been proposed in the past, such as the laterally extended endopelvic resection.
“[TMMR] is not a new concept,” she said. “It’s just a question of how radical it is.”
Instead of developing new types of radical surgery, she said, the trend in the United States is toward de-escalation of surgical treatments altogether, with greater reliance upon medical options, such as immunotherapy.
“[This study] is thought provoking, and I applaud them for doing it,” Dr. Modesitt said. “But I’m not going to go out and do that on my next patient.”
This study was supported by grants from Centre for Clinical Research Sörmland (Sweden) and Region Stockholm (Sweden). Dr. Falconer is a board member of Surgical Science.
These findings suggest that TMMR may be considered a primary treatment option for both early-stage and locally advanced cervical cancer confined to the Müllerian compartment, reported lead author Henrik Falconer, MD, PhD, of Karolinska Institutet, Stockholm, Sweden, and colleagues.
What is the rationale behind TMMR?
“Current international guidelines [for cervical cancer] are primarily based on retrospective case series and a small number of outdated randomized controlled trials,” the investigators wrote in EClinicalMedicine, part of The Lancet publication platform. “The stage-dependent treatment recommendations, with surgery advised for early-stage and radiation therapy for locally advanced disease, may be considered too simplistic, suggesting that early stages of cervical cancer cannot be controlled with surgical resection alone or that locally advanced cervical cancer is inoperable.”
This mindset, they noted, overlooks the complexities of cancer spread. In contrast, TMMR and similar surgical approaches based on the cancer field model are mapped along routes of locoregional dissemination, leading to “excellent local control” in more than 600 cases at the University Hospital of Leipzig, Leipzig, Germany.
To date, however, TMMR’s adoption has been limited, and it has not been compared directly with current guideline treatments, prompting the present study.
What methods were used to compare TMMR with standard treatment?
The study compared TMMR plus therapeutic lymph node dissection (tLND) without adjuvant radiation versus standard treatment (ST) for early-stage (FIGO 2009 IB1, IIA1) and locally advanced (FIGO 2009 IB2, IIA2, IIB) cervical cancer. Standard treatment for patients with early-stage disease involved radical hysterectomy and pelvic lymphadenectomy, with adjuvant chemoradiation dependent upon final pathology. Those with locally advanced disease received definitive chemoradiation.
Data for the standard treatment group were drawn from population-based registries in Sweden, while those for the TMMR group came from the Leipzig Mesometrial Resection Study Database. The final dataset included 1,007 women treated between 2011 and 2020, with 733 undergoing standard treatment and 274 receiving TMMR.
Outcomes included RFS and OS, adjusted for clinical and tumor-related variables.
How did TMMR compare with standard treatment?
TMMR was associated with superior oncologic outcomes compared with standard treatment for early-stage cervical cancer.
Specifically, 5-year RFS was 91.2% for TMMR versus 81.8% for standard therapy (P = .002). In the adjusted analysis, TMMR was associated with a significantly lower hazard of recurrence (hazard ratio [HR], 0.39; 95% CI, 0.22–0.69) and death (HR, 0.42; 95% CI, 0.21-0.86). Also favoring TMMR, absolute difference in the risk of recurrence at 5 years was 9.4% (95% CI 3.2–15.7). In addition, 5-year OS was better in the TMMR group, at 93.3%, compared with 90.3% for standard treatment (P = .034).
Among patients with locally advanced disease, no significant differences in RFS or OS were observed.
Are these data strong enough to make TMMR the new standard treatment?
Dr. Falconer and colleagues concluded that TMMR with tLND “may replace the standard treatment approach in early-stage cervical cancer and furthermore be evaluated as an option in locally advanced cervical cancer confined to the Müllerian compartment.”
While the investigators anticipated demands for randomized controlled trials, they questioned the value of such studies, suggesting that any control arm would be “based on inconsistent or flawed concepts.”
Susan C. Modesitt, MD, director of the gynecologic oncology division of Winship Cancer Institute of Emory University, Atlanta, offered a different perspective.
“They do show encouraging data in the early stage,” Dr. Modesitt said in an interview, “but I would still want to see a randomized controlled trial, because we’ve been burned before.”
She cited the LACC trial, which dispelled strong convictions about the alleged superiority of minimally invasive radical hysterectomy.
“We thought minimally invasive was so good, and we should be doing that to everybody, but we did a trial, and we found worse outcomes,” Dr. Modesitt said. “More of those early-stage women died.”
Dr. Modesitt also pointed out the lack of safety data in the present publication.
“TMMR is a bigger procedure, so I would expect more complications,” she said, noting that rates of urinary injury, nerve injury, and readmission need to be considered alongside efficacy outcomes.
How does TMMR fit into the current treatment landscape for cervical cancer?
“This is a very niche surgery that most places don’t do,” Dr. Modesitt said.
She pointed out that “multiple variations” on the standard radical hysterectomy have been proposed in the past, such as the laterally extended endopelvic resection.
“[TMMR] is not a new concept,” she said. “It’s just a question of how radical it is.”
Instead of developing new types of radical surgery, she said, the trend in the United States is toward de-escalation of surgical treatments altogether, with greater reliance upon medical options, such as immunotherapy.
“[This study] is thought provoking, and I applaud them for doing it,” Dr. Modesitt said. “But I’m not going to go out and do that on my next patient.”
This study was supported by grants from Centre for Clinical Research Sörmland (Sweden) and Region Stockholm (Sweden). Dr. Falconer is a board member of Surgical Science.
FROM THE LANCET
‘Chemoresistance Can Be Reversed’: Toughest Cancers Targeted
In the war against cancer, doctors and patients have long reached for three main weapons to target diseased cells: chemotherapy, radiation, and surgery.
But new research published this month in the journal Nature Materials suggests that manipulating the tissue around those cells — a strategy known as
“Our study shows the importance of the tumor microenvironment and its properties in dictating how cancer progresses and responds to drug treatment,” said first author Bauer LeSavage, PhD, who conducted the study as a postdoctoral researcher in the Bioengineering Department at Stanford University, Stanford, California. “It also demonstrates that chemoresistance can be reversed.”
Each year, about 66,000 people are diagnosed with pancreatic cancer, and 52,000 die from it. It is a particularly lethal type of cancer, with 5-year survival rates hovering around 7% — a rate that has not improved much since 1996 when the first-line chemotherapy drug gemcitabine was approved.
It looks different from many cancers, said Lynn Matrisian, PhD, chief science officer for the nonprofit Pancreatic Cancer Action Network. Instead of a tumorous mass, it is made of islands of cancer cells surrounded by unusually dense fibrous tissue known as the extracellular matrix, which can collapse blood vessels and prevent drugs from reaching the tumor.
For the study, Dr. LeSavage and his team engineered synthetic but lifelike three-dimensional pancreas tissue with varying degrees of stiffness and different biochemical properties. Then they inserted bits of real tumors from patients with pancreatic cancer, watched them grow, and tried to kill them with drugs.
They found that cells growing in a stiff matrix were more resistant to chemotherapy than those growing in a softer matrix. But the story didn’t end there.
They also found that high amounts of the tissue-strengthening protein hyaluronic acid in stiff tissue seemed to signal the cancer cells to develop tiny pumps on their surface which shuttled out the drugs before they could take effect.
When the researchers moved the cancer cells into either a softer matrix or a stiff matrix in which the hyaluronic acid receptor, called CD44, was blocked, the chemotherapy drugs started working again.
“This suggests that if we can disrupt the stiffness signaling that’s happening through the CD44 receptor, we could make patients’ pancreatic cancer treatable again by normal chemotherapy,” said senior study author Sarah Heilshorn, PhD, a professor of materials science and engineering at Stanford. “These results suggest an exciting new direction for new drug development.”
Targeting Nearby Tissue: A Novel Approach to Fighting Chemoresistance
The study is not the first to suggest that chemically targeting the microenvironment surrounding a tumor can influence how patients respond to treatment.
In one recent clinical trial, patients with metastatic pancreatic cancer were given an experimental drug to inhibit a protein called connective tissue growth factor, reduce fibrous tissue, and make pancreatic tumors easier to surgically remove. Results have not been published yet.
Other research suggests that the generic blood pressure drug losartan, when given in combination with chemotherapy and radiation, can boost survival in patients with advanced pancreatic cancer by, in part, improving the health of blood vessels that carry drugs to the tumor.
But other studies of such mechanotherapeutics have yielded inconclusive results, said Dr. Matrisian.
“This paper points to another reason why we should not give up on this approach,” she said.
Ning Wang, PhD, director of the new Institute for Mechanobiology at Northeastern University College of Engineering, Boston, said there is no question that the composition of a tumor’s environment can influence how cancer progresses or responds to drugs. The new paper, he said, adds an important new chapter to the evolving story.
“But it’s very complicated. It’s not as simple as saying make it softer or stiffer and you can change the outcome for the patient,” Dr. Wang said.
In fact, some research has shown that tissue becomes stiffer when cancer arises so it can contain it from spreading.
In one animal study of pancreatic cancer that had spread to the liver, administering drugs to soften the surrounding tissue, or stroma, actually had the opposite effect — accelerating tumor growth and reducing survival rates.
Dr. Wang also noted that any drug designed to influence the extracellular matrix would need to be extremely localized, to prevent damage to other tissues, like bone or heart muscle.
Dr. LeSavage said he sees the paper as a case study in how important the extracellular matrix is and an example of how artificially grown organs or tissues can play a key role in testing how drugs work or don’t work.
He imagines a day when doctors could personalize treatments by taking a bit of a patient’s tumor, growing it in artificial tissue, and seeing how different tissue-altering drugs affect different therapies.
“This isn’t something that is just unique to pancreatic cancer,” he said, noting that the extracellular matrix throughout the body interacts with different cancers. “If we could take someone who has a chemoresistant tumor and convert it into something that is sensitive to existing therapies again, we could give them a second chance.”
A version of this article appeared on Medscape.com.
In the war against cancer, doctors and patients have long reached for three main weapons to target diseased cells: chemotherapy, radiation, and surgery.
But new research published this month in the journal Nature Materials suggests that manipulating the tissue around those cells — a strategy known as
“Our study shows the importance of the tumor microenvironment and its properties in dictating how cancer progresses and responds to drug treatment,” said first author Bauer LeSavage, PhD, who conducted the study as a postdoctoral researcher in the Bioengineering Department at Stanford University, Stanford, California. “It also demonstrates that chemoresistance can be reversed.”
Each year, about 66,000 people are diagnosed with pancreatic cancer, and 52,000 die from it. It is a particularly lethal type of cancer, with 5-year survival rates hovering around 7% — a rate that has not improved much since 1996 when the first-line chemotherapy drug gemcitabine was approved.
It looks different from many cancers, said Lynn Matrisian, PhD, chief science officer for the nonprofit Pancreatic Cancer Action Network. Instead of a tumorous mass, it is made of islands of cancer cells surrounded by unusually dense fibrous tissue known as the extracellular matrix, which can collapse blood vessels and prevent drugs from reaching the tumor.
For the study, Dr. LeSavage and his team engineered synthetic but lifelike three-dimensional pancreas tissue with varying degrees of stiffness and different biochemical properties. Then they inserted bits of real tumors from patients with pancreatic cancer, watched them grow, and tried to kill them with drugs.
They found that cells growing in a stiff matrix were more resistant to chemotherapy than those growing in a softer matrix. But the story didn’t end there.
They also found that high amounts of the tissue-strengthening protein hyaluronic acid in stiff tissue seemed to signal the cancer cells to develop tiny pumps on their surface which shuttled out the drugs before they could take effect.
When the researchers moved the cancer cells into either a softer matrix or a stiff matrix in which the hyaluronic acid receptor, called CD44, was blocked, the chemotherapy drugs started working again.
“This suggests that if we can disrupt the stiffness signaling that’s happening through the CD44 receptor, we could make patients’ pancreatic cancer treatable again by normal chemotherapy,” said senior study author Sarah Heilshorn, PhD, a professor of materials science and engineering at Stanford. “These results suggest an exciting new direction for new drug development.”
Targeting Nearby Tissue: A Novel Approach to Fighting Chemoresistance
The study is not the first to suggest that chemically targeting the microenvironment surrounding a tumor can influence how patients respond to treatment.
In one recent clinical trial, patients with metastatic pancreatic cancer were given an experimental drug to inhibit a protein called connective tissue growth factor, reduce fibrous tissue, and make pancreatic tumors easier to surgically remove. Results have not been published yet.
Other research suggests that the generic blood pressure drug losartan, when given in combination with chemotherapy and radiation, can boost survival in patients with advanced pancreatic cancer by, in part, improving the health of blood vessels that carry drugs to the tumor.
But other studies of such mechanotherapeutics have yielded inconclusive results, said Dr. Matrisian.
“This paper points to another reason why we should not give up on this approach,” she said.
Ning Wang, PhD, director of the new Institute for Mechanobiology at Northeastern University College of Engineering, Boston, said there is no question that the composition of a tumor’s environment can influence how cancer progresses or responds to drugs. The new paper, he said, adds an important new chapter to the evolving story.
“But it’s very complicated. It’s not as simple as saying make it softer or stiffer and you can change the outcome for the patient,” Dr. Wang said.
In fact, some research has shown that tissue becomes stiffer when cancer arises so it can contain it from spreading.
In one animal study of pancreatic cancer that had spread to the liver, administering drugs to soften the surrounding tissue, or stroma, actually had the opposite effect — accelerating tumor growth and reducing survival rates.
Dr. Wang also noted that any drug designed to influence the extracellular matrix would need to be extremely localized, to prevent damage to other tissues, like bone or heart muscle.
Dr. LeSavage said he sees the paper as a case study in how important the extracellular matrix is and an example of how artificially grown organs or tissues can play a key role in testing how drugs work or don’t work.
He imagines a day when doctors could personalize treatments by taking a bit of a patient’s tumor, growing it in artificial tissue, and seeing how different tissue-altering drugs affect different therapies.
“This isn’t something that is just unique to pancreatic cancer,” he said, noting that the extracellular matrix throughout the body interacts with different cancers. “If we could take someone who has a chemoresistant tumor and convert it into something that is sensitive to existing therapies again, we could give them a second chance.”
A version of this article appeared on Medscape.com.
In the war against cancer, doctors and patients have long reached for three main weapons to target diseased cells: chemotherapy, radiation, and surgery.
But new research published this month in the journal Nature Materials suggests that manipulating the tissue around those cells — a strategy known as
“Our study shows the importance of the tumor microenvironment and its properties in dictating how cancer progresses and responds to drug treatment,” said first author Bauer LeSavage, PhD, who conducted the study as a postdoctoral researcher in the Bioengineering Department at Stanford University, Stanford, California. “It also demonstrates that chemoresistance can be reversed.”
Each year, about 66,000 people are diagnosed with pancreatic cancer, and 52,000 die from it. It is a particularly lethal type of cancer, with 5-year survival rates hovering around 7% — a rate that has not improved much since 1996 when the first-line chemotherapy drug gemcitabine was approved.
It looks different from many cancers, said Lynn Matrisian, PhD, chief science officer for the nonprofit Pancreatic Cancer Action Network. Instead of a tumorous mass, it is made of islands of cancer cells surrounded by unusually dense fibrous tissue known as the extracellular matrix, which can collapse blood vessels and prevent drugs from reaching the tumor.
For the study, Dr. LeSavage and his team engineered synthetic but lifelike three-dimensional pancreas tissue with varying degrees of stiffness and different biochemical properties. Then they inserted bits of real tumors from patients with pancreatic cancer, watched them grow, and tried to kill them with drugs.
They found that cells growing in a stiff matrix were more resistant to chemotherapy than those growing in a softer matrix. But the story didn’t end there.
They also found that high amounts of the tissue-strengthening protein hyaluronic acid in stiff tissue seemed to signal the cancer cells to develop tiny pumps on their surface which shuttled out the drugs before they could take effect.
When the researchers moved the cancer cells into either a softer matrix or a stiff matrix in which the hyaluronic acid receptor, called CD44, was blocked, the chemotherapy drugs started working again.
“This suggests that if we can disrupt the stiffness signaling that’s happening through the CD44 receptor, we could make patients’ pancreatic cancer treatable again by normal chemotherapy,” said senior study author Sarah Heilshorn, PhD, a professor of materials science and engineering at Stanford. “These results suggest an exciting new direction for new drug development.”
Targeting Nearby Tissue: A Novel Approach to Fighting Chemoresistance
The study is not the first to suggest that chemically targeting the microenvironment surrounding a tumor can influence how patients respond to treatment.
In one recent clinical trial, patients with metastatic pancreatic cancer were given an experimental drug to inhibit a protein called connective tissue growth factor, reduce fibrous tissue, and make pancreatic tumors easier to surgically remove. Results have not been published yet.
Other research suggests that the generic blood pressure drug losartan, when given in combination with chemotherapy and radiation, can boost survival in patients with advanced pancreatic cancer by, in part, improving the health of blood vessels that carry drugs to the tumor.
But other studies of such mechanotherapeutics have yielded inconclusive results, said Dr. Matrisian.
“This paper points to another reason why we should not give up on this approach,” she said.
Ning Wang, PhD, director of the new Institute for Mechanobiology at Northeastern University College of Engineering, Boston, said there is no question that the composition of a tumor’s environment can influence how cancer progresses or responds to drugs. The new paper, he said, adds an important new chapter to the evolving story.
“But it’s very complicated. It’s not as simple as saying make it softer or stiffer and you can change the outcome for the patient,” Dr. Wang said.
In fact, some research has shown that tissue becomes stiffer when cancer arises so it can contain it from spreading.
In one animal study of pancreatic cancer that had spread to the liver, administering drugs to soften the surrounding tissue, or stroma, actually had the opposite effect — accelerating tumor growth and reducing survival rates.
Dr. Wang also noted that any drug designed to influence the extracellular matrix would need to be extremely localized, to prevent damage to other tissues, like bone or heart muscle.
Dr. LeSavage said he sees the paper as a case study in how important the extracellular matrix is and an example of how artificially grown organs or tissues can play a key role in testing how drugs work or don’t work.
He imagines a day when doctors could personalize treatments by taking a bit of a patient’s tumor, growing it in artificial tissue, and seeing how different tissue-altering drugs affect different therapies.
“This isn’t something that is just unique to pancreatic cancer,” he said, noting that the extracellular matrix throughout the body interacts with different cancers. “If we could take someone who has a chemoresistant tumor and convert it into something that is sensitive to existing therapies again, we could give them a second chance.”
A version of this article appeared on Medscape.com.
Targeted Pancreatic Cancer Screening May Save Lives
TOPLINE:
METHODOLOGY:
- Pancreatic ductal adenocarcinoma has poor 5-year survival rates and is often detected at later stages. General population screening is not recommended, but high-risk individuals, such as those with familial or genetic predispositions, may benefit from regular surveillance.
- The Cancer of the Pancreas Screening (CAPS) program, initiated in 1998, has been evaluating the effectiveness of such targeted surveillance for over two decades, but whether targeted surveillance confers a survival benefit remains unclear.
- The current study evaluated 26 high-risk individuals in the CAPS program who were ultimately diagnosed with pancreatic ductal adenocarcinoma. These high-risk individuals had undergone surveillance with annual endoscopic ultrasonography or MRI prior to diagnosis.
- The researchers compared these 26 individuals with 1504 matched control patients with pancreatic ductal adenocarcinoma from the Surveillance, Epidemiology, and End Results (SEER) database. The high-risk individuals and SEER control patients were matched on age, sex, and year of diagnosis.
- The primary outcomes were tumor stage at diagnosis, overall survival, and pancreatic cancer-specific mortality.
TAKEAWAY:
- High-risk individuals were significantly more likely to be diagnosed with early-stage pancreatic cancer: 38.5% were diagnosed at stage I vs 10.3% in the general US population, and 30.8% were diagnosed at stage II vs 25.1% in the general US population (P < .001).
- The median tumor size at diagnosis was smaller in high-risk individuals than in control patients (2.5 vs 3.6 cm; P < .001), and significantly fewer high-risk individuals had distant metastases at diagnosis (M1 stage) vs control patients (26.9% vs 53.8%; P = .01).
- Overall, high-risk individuals lived about 4.5 years longer — median of 61.7 months vs 8 months for control patients (hazard ratio [HR], 4.19; P < .001). In the 20 high-risk patients with screen-detected cancer, median overall survival was even higher at 144 months.
- The probability of surviving 5 years was significantly better in the high-risk group (50%) than in the control group (9%). And at 5 years, high-risk individuals had a significantly lower probability of dying from pancreatic cancer (HR, 3.58; P < .001).
IN PRACTICE:
Surveillance of high-risk individuals led to detection of “smaller pancreatic cancers, a greater number of patients with stage I disease,” as well as “a much higher likelihood of long-term survival than unscreened patients in the general population,” the authors concluded. “These findings suggest that selective surveillance of individuals at high risk for pancreatic cancer may improve clinical outcomes.”
SOURCE:
This study, with first author Amanda L. Blackford, from Johns Hopkins Medical Institutions, Baltimore, was published online July 3 in JAMA Oncology.
LIMITATIONS:
The findings might have limited generalizability due to enrollment at academic referral centers, limited racial and ethnic diversity, and a small number of high-risk individuals progressing to pancreatic cancer. The study also lacked a control group of unscreened high-risk individuals.
DISCLOSURES:
This study was supported by the National Institutes of Health, Susan Wojcicki and Dennis Troper, and others. Several authors reported financial ties outside this work.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Pancreatic ductal adenocarcinoma has poor 5-year survival rates and is often detected at later stages. General population screening is not recommended, but high-risk individuals, such as those with familial or genetic predispositions, may benefit from regular surveillance.
- The Cancer of the Pancreas Screening (CAPS) program, initiated in 1998, has been evaluating the effectiveness of such targeted surveillance for over two decades, but whether targeted surveillance confers a survival benefit remains unclear.
- The current study evaluated 26 high-risk individuals in the CAPS program who were ultimately diagnosed with pancreatic ductal adenocarcinoma. These high-risk individuals had undergone surveillance with annual endoscopic ultrasonography or MRI prior to diagnosis.
- The researchers compared these 26 individuals with 1504 matched control patients with pancreatic ductal adenocarcinoma from the Surveillance, Epidemiology, and End Results (SEER) database. The high-risk individuals and SEER control patients were matched on age, sex, and year of diagnosis.
- The primary outcomes were tumor stage at diagnosis, overall survival, and pancreatic cancer-specific mortality.
TAKEAWAY:
- High-risk individuals were significantly more likely to be diagnosed with early-stage pancreatic cancer: 38.5% were diagnosed at stage I vs 10.3% in the general US population, and 30.8% were diagnosed at stage II vs 25.1% in the general US population (P < .001).
- The median tumor size at diagnosis was smaller in high-risk individuals than in control patients (2.5 vs 3.6 cm; P < .001), and significantly fewer high-risk individuals had distant metastases at diagnosis (M1 stage) vs control patients (26.9% vs 53.8%; P = .01).
- Overall, high-risk individuals lived about 4.5 years longer — median of 61.7 months vs 8 months for control patients (hazard ratio [HR], 4.19; P < .001). In the 20 high-risk patients with screen-detected cancer, median overall survival was even higher at 144 months.
- The probability of surviving 5 years was significantly better in the high-risk group (50%) than in the control group (9%). And at 5 years, high-risk individuals had a significantly lower probability of dying from pancreatic cancer (HR, 3.58; P < .001).
IN PRACTICE:
Surveillance of high-risk individuals led to detection of “smaller pancreatic cancers, a greater number of patients with stage I disease,” as well as “a much higher likelihood of long-term survival than unscreened patients in the general population,” the authors concluded. “These findings suggest that selective surveillance of individuals at high risk for pancreatic cancer may improve clinical outcomes.”
SOURCE:
This study, with first author Amanda L. Blackford, from Johns Hopkins Medical Institutions, Baltimore, was published online July 3 in JAMA Oncology.
LIMITATIONS:
The findings might have limited generalizability due to enrollment at academic referral centers, limited racial and ethnic diversity, and a small number of high-risk individuals progressing to pancreatic cancer. The study also lacked a control group of unscreened high-risk individuals.
DISCLOSURES:
This study was supported by the National Institutes of Health, Susan Wojcicki and Dennis Troper, and others. Several authors reported financial ties outside this work.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Pancreatic ductal adenocarcinoma has poor 5-year survival rates and is often detected at later stages. General population screening is not recommended, but high-risk individuals, such as those with familial or genetic predispositions, may benefit from regular surveillance.
- The Cancer of the Pancreas Screening (CAPS) program, initiated in 1998, has been evaluating the effectiveness of such targeted surveillance for over two decades, but whether targeted surveillance confers a survival benefit remains unclear.
- The current study evaluated 26 high-risk individuals in the CAPS program who were ultimately diagnosed with pancreatic ductal adenocarcinoma. These high-risk individuals had undergone surveillance with annual endoscopic ultrasonography or MRI prior to diagnosis.
- The researchers compared these 26 individuals with 1504 matched control patients with pancreatic ductal adenocarcinoma from the Surveillance, Epidemiology, and End Results (SEER) database. The high-risk individuals and SEER control patients were matched on age, sex, and year of diagnosis.
- The primary outcomes were tumor stage at diagnosis, overall survival, and pancreatic cancer-specific mortality.
TAKEAWAY:
- High-risk individuals were significantly more likely to be diagnosed with early-stage pancreatic cancer: 38.5% were diagnosed at stage I vs 10.3% in the general US population, and 30.8% were diagnosed at stage II vs 25.1% in the general US population (P < .001).
- The median tumor size at diagnosis was smaller in high-risk individuals than in control patients (2.5 vs 3.6 cm; P < .001), and significantly fewer high-risk individuals had distant metastases at diagnosis (M1 stage) vs control patients (26.9% vs 53.8%; P = .01).
- Overall, high-risk individuals lived about 4.5 years longer — median of 61.7 months vs 8 months for control patients (hazard ratio [HR], 4.19; P < .001). In the 20 high-risk patients with screen-detected cancer, median overall survival was even higher at 144 months.
- The probability of surviving 5 years was significantly better in the high-risk group (50%) than in the control group (9%). And at 5 years, high-risk individuals had a significantly lower probability of dying from pancreatic cancer (HR, 3.58; P < .001).
IN PRACTICE:
Surveillance of high-risk individuals led to detection of “smaller pancreatic cancers, a greater number of patients with stage I disease,” as well as “a much higher likelihood of long-term survival than unscreened patients in the general population,” the authors concluded. “These findings suggest that selective surveillance of individuals at high risk for pancreatic cancer may improve clinical outcomes.”
SOURCE:
This study, with first author Amanda L. Blackford, from Johns Hopkins Medical Institutions, Baltimore, was published online July 3 in JAMA Oncology.
LIMITATIONS:
The findings might have limited generalizability due to enrollment at academic referral centers, limited racial and ethnic diversity, and a small number of high-risk individuals progressing to pancreatic cancer. The study also lacked a control group of unscreened high-risk individuals.
DISCLOSURES:
This study was supported by the National Institutes of Health, Susan Wojcicki and Dennis Troper, and others. Several authors reported financial ties outside this work.
A version of this article appeared on Medscape.com.
Could an EHR Nudge Reduce Unnecessary Biopsies?
Participating surgeons noted that the reminder system added minimal friction to their workflow, as it did not require additional clicks or actions on the day of the patient visit, reported lead author Neil Carleton, PhD, of UPMC Hillman Cancer Center, Pittsburgh, and colleagues in JAMA Surgery (JAMA Surg. 2024 Jul 17. doi: 10.1001/jamasurg.2024.2407).
This effort to reduce the rate of SLNB stems from the Choosing Wisely campaign, which recommends against axillary staging in women 70 years and older with early-stage, clinically node-negative (cN0), hormone receptor–positive (HR+) breast cancer, the investigators said.
“These recommendations were developed because axillary staging did not impact survival, and rates of SLN positivity were low because of the tumor’s biological phenotype,” they wrote. “Even in older patients with tumors that exhibit concerning clinicopathologic features, limited nodal involvement does not often alter receipt of chemotherapy independently from genomic testing. Despite these recommendations, most women still receive axillary surgery.”
How Did the Nudge System Aim to Reduce the Rate of SLNB?
The nudge intervention involved adding a new column to the Epic schedule view, which flagged eligible patients during their first outpatient surgical consultation. The flag appeared as a caution sign or red clipboard icon. When surgeons hovered over the icon, a text box appeared, reminding them to consider omitting SLNB after a detailed review of core biopsy pathology and ultrasonographic imaging.
The intervention was evaluated at eight outpatient clinics within an integrated healthcare system that included seven breast surgical oncologists.
The study began with a 12-month preintervention period to serve as a control, during which time SLNB rate was determined via 194 patients in the target demographic. SLNB rate was again collected during the 12-month intervention period, which involved 193 patients meeting enrollment criteria. Between these periods, the investigators conducted a brief session lasting less than 30 minutes to introduce the surgeons to the rationale and design of the nudge column.
How Effective Was the Nudge System?
The intervention reduced the SLNB rate from 46.9% to 23.8%, representing a 49.3% decrease in use of SLNB. Efficacy was further supported by a significant reduction in SLNB according to an interrupted time series model (adjusted odds ratio, 0.26; 95% confidence interval, 0.07 to 0.90; P = .03). Extended follow-up showed that this effect was durable beyond the intervention period, with a 6-month mean reduction in SLNB of 15.6%.
Omission of SLNB led to higher rates of pathological node positivity during the intervention period (15.2% vs 8.8%), with all positive cases staged as pN1. Adjuvant therapy recommendations were similar between groups and driven by genomic testing, not nodal status. The intervention period also saw a decrease in referrals for lymphedema evaluation (3.6% vs. 6.2%).
How Might the Nudge System Be Implemented in Other Practices?
Although the SLNB nudge system was effective in the present study, likelihood of uptake among practices could vary widely, according to Anne M. Wallace, MD, professor of clinical surgery at UC San Diego Health and director of the Moores Comprehensive Breast Health Program.
On a fundamental level, not all centers use Epic software, which could present issues with compatibility, Dr. Wallace said in an interview. More importantly, she added, many institutions already have EHR-based alerts and reminders in place, so it is not always feasible to add a new nudge for every possible clinical scenario.
“Already there are so many little icons that we have to go through now when we close a note,” she said. “That’s why electronic medical records are becoming one of the leading stressors in medicine.”
This presents a more complex challenge, Dr. Wallace said, particularly as potentially practice-changing data are becoming available, and physicians may not have time to learn about them and integrate them into routine practice. She suggested that the present system may be most appropriate for oncologists in solo practice, or in small group practices where it is more challenging to have routine conversations about changing standards of care.
What Are the Risks of Using the Nudge System?
One of those conversations may surround the validity of the recommendation implemented in the present study.
Although the Society of Surgical Oncology recommends against SLNB in the described demographic, other experts, including Dr. Wallace, take a more nuanced view of the decision.
She noted that some patients with a chronological age of 70 may have a lower biological age, casting doubt on the legitimacy of the age threshold, and those near the threshold may wish to make the decision about staging for themselves.
Beyond these concerns, Dr. Wallace described two potential risks involved in forgoing SLNB.
First, there’s the potential for underestimating the tumor’s severity, she said, as this could mean a trip back to the operating room. A tumor initially thought to be low-grade might later be found to be high-grade, necessitating further surgery. Some patients might refuse additional surgery, leaving the more aggressive tumor untreated.
Second, the nudge system could complicate radiation treatment decisions, Dr. Wallace said. Without full nodal status, some radiation oncologists might push for additional radiation therapy, which incurs a greater treatment burden than SNLB.
What Are Some Alternatives to the Nudge System?
After discussing the strengths and weaknesses of the present EHR-based nudge system, and others like it, Dr. Wallace returned to the importance of ongoing communication among colleagues managing complex cases.
At UC San Diego Health, where oncologists meet weekly for a 2-hour breast cancer conference, “we nudge each other,” she said.
This study was supported by the Shear Family Foundation, UPMC eRecord Ambulatory Decision Support and Analytics, UPMC Hillman Cancer Center Biostatistics Facility, and National Institutes of Health. The investigators disclosed relationships with Pfizer, Amgen, the Lewin Group, and Milestone Pennsylvania, and others.
Participating surgeons noted that the reminder system added minimal friction to their workflow, as it did not require additional clicks or actions on the day of the patient visit, reported lead author Neil Carleton, PhD, of UPMC Hillman Cancer Center, Pittsburgh, and colleagues in JAMA Surgery (JAMA Surg. 2024 Jul 17. doi: 10.1001/jamasurg.2024.2407).
This effort to reduce the rate of SLNB stems from the Choosing Wisely campaign, which recommends against axillary staging in women 70 years and older with early-stage, clinically node-negative (cN0), hormone receptor–positive (HR+) breast cancer, the investigators said.
“These recommendations were developed because axillary staging did not impact survival, and rates of SLN positivity were low because of the tumor’s biological phenotype,” they wrote. “Even in older patients with tumors that exhibit concerning clinicopathologic features, limited nodal involvement does not often alter receipt of chemotherapy independently from genomic testing. Despite these recommendations, most women still receive axillary surgery.”
How Did the Nudge System Aim to Reduce the Rate of SLNB?
The nudge intervention involved adding a new column to the Epic schedule view, which flagged eligible patients during their first outpatient surgical consultation. The flag appeared as a caution sign or red clipboard icon. When surgeons hovered over the icon, a text box appeared, reminding them to consider omitting SLNB after a detailed review of core biopsy pathology and ultrasonographic imaging.
The intervention was evaluated at eight outpatient clinics within an integrated healthcare system that included seven breast surgical oncologists.
The study began with a 12-month preintervention period to serve as a control, during which time SLNB rate was determined via 194 patients in the target demographic. SLNB rate was again collected during the 12-month intervention period, which involved 193 patients meeting enrollment criteria. Between these periods, the investigators conducted a brief session lasting less than 30 minutes to introduce the surgeons to the rationale and design of the nudge column.
How Effective Was the Nudge System?
The intervention reduced the SLNB rate from 46.9% to 23.8%, representing a 49.3% decrease in use of SLNB. Efficacy was further supported by a significant reduction in SLNB according to an interrupted time series model (adjusted odds ratio, 0.26; 95% confidence interval, 0.07 to 0.90; P = .03). Extended follow-up showed that this effect was durable beyond the intervention period, with a 6-month mean reduction in SLNB of 15.6%.
Omission of SLNB led to higher rates of pathological node positivity during the intervention period (15.2% vs 8.8%), with all positive cases staged as pN1. Adjuvant therapy recommendations were similar between groups and driven by genomic testing, not nodal status. The intervention period also saw a decrease in referrals for lymphedema evaluation (3.6% vs. 6.2%).
How Might the Nudge System Be Implemented in Other Practices?
Although the SLNB nudge system was effective in the present study, likelihood of uptake among practices could vary widely, according to Anne M. Wallace, MD, professor of clinical surgery at UC San Diego Health and director of the Moores Comprehensive Breast Health Program.
On a fundamental level, not all centers use Epic software, which could present issues with compatibility, Dr. Wallace said in an interview. More importantly, she added, many institutions already have EHR-based alerts and reminders in place, so it is not always feasible to add a new nudge for every possible clinical scenario.
“Already there are so many little icons that we have to go through now when we close a note,” she said. “That’s why electronic medical records are becoming one of the leading stressors in medicine.”
This presents a more complex challenge, Dr. Wallace said, particularly as potentially practice-changing data are becoming available, and physicians may not have time to learn about them and integrate them into routine practice. She suggested that the present system may be most appropriate for oncologists in solo practice, or in small group practices where it is more challenging to have routine conversations about changing standards of care.
What Are the Risks of Using the Nudge System?
One of those conversations may surround the validity of the recommendation implemented in the present study.
Although the Society of Surgical Oncology recommends against SLNB in the described demographic, other experts, including Dr. Wallace, take a more nuanced view of the decision.
She noted that some patients with a chronological age of 70 may have a lower biological age, casting doubt on the legitimacy of the age threshold, and those near the threshold may wish to make the decision about staging for themselves.
Beyond these concerns, Dr. Wallace described two potential risks involved in forgoing SLNB.
First, there’s the potential for underestimating the tumor’s severity, she said, as this could mean a trip back to the operating room. A tumor initially thought to be low-grade might later be found to be high-grade, necessitating further surgery. Some patients might refuse additional surgery, leaving the more aggressive tumor untreated.
Second, the nudge system could complicate radiation treatment decisions, Dr. Wallace said. Without full nodal status, some radiation oncologists might push for additional radiation therapy, which incurs a greater treatment burden than SNLB.
What Are Some Alternatives to the Nudge System?
After discussing the strengths and weaknesses of the present EHR-based nudge system, and others like it, Dr. Wallace returned to the importance of ongoing communication among colleagues managing complex cases.
At UC San Diego Health, where oncologists meet weekly for a 2-hour breast cancer conference, “we nudge each other,” she said.
This study was supported by the Shear Family Foundation, UPMC eRecord Ambulatory Decision Support and Analytics, UPMC Hillman Cancer Center Biostatistics Facility, and National Institutes of Health. The investigators disclosed relationships with Pfizer, Amgen, the Lewin Group, and Milestone Pennsylvania, and others.
Participating surgeons noted that the reminder system added minimal friction to their workflow, as it did not require additional clicks or actions on the day of the patient visit, reported lead author Neil Carleton, PhD, of UPMC Hillman Cancer Center, Pittsburgh, and colleagues in JAMA Surgery (JAMA Surg. 2024 Jul 17. doi: 10.1001/jamasurg.2024.2407).
This effort to reduce the rate of SLNB stems from the Choosing Wisely campaign, which recommends against axillary staging in women 70 years and older with early-stage, clinically node-negative (cN0), hormone receptor–positive (HR+) breast cancer, the investigators said.
“These recommendations were developed because axillary staging did not impact survival, and rates of SLN positivity were low because of the tumor’s biological phenotype,” they wrote. “Even in older patients with tumors that exhibit concerning clinicopathologic features, limited nodal involvement does not often alter receipt of chemotherapy independently from genomic testing. Despite these recommendations, most women still receive axillary surgery.”
How Did the Nudge System Aim to Reduce the Rate of SLNB?
The nudge intervention involved adding a new column to the Epic schedule view, which flagged eligible patients during their first outpatient surgical consultation. The flag appeared as a caution sign or red clipboard icon. When surgeons hovered over the icon, a text box appeared, reminding them to consider omitting SLNB after a detailed review of core biopsy pathology and ultrasonographic imaging.
The intervention was evaluated at eight outpatient clinics within an integrated healthcare system that included seven breast surgical oncologists.
The study began with a 12-month preintervention period to serve as a control, during which time SLNB rate was determined via 194 patients in the target demographic. SLNB rate was again collected during the 12-month intervention period, which involved 193 patients meeting enrollment criteria. Between these periods, the investigators conducted a brief session lasting less than 30 minutes to introduce the surgeons to the rationale and design of the nudge column.
How Effective Was the Nudge System?
The intervention reduced the SLNB rate from 46.9% to 23.8%, representing a 49.3% decrease in use of SLNB. Efficacy was further supported by a significant reduction in SLNB according to an interrupted time series model (adjusted odds ratio, 0.26; 95% confidence interval, 0.07 to 0.90; P = .03). Extended follow-up showed that this effect was durable beyond the intervention period, with a 6-month mean reduction in SLNB of 15.6%.
Omission of SLNB led to higher rates of pathological node positivity during the intervention period (15.2% vs 8.8%), with all positive cases staged as pN1. Adjuvant therapy recommendations were similar between groups and driven by genomic testing, not nodal status. The intervention period also saw a decrease in referrals for lymphedema evaluation (3.6% vs. 6.2%).
How Might the Nudge System Be Implemented in Other Practices?
Although the SLNB nudge system was effective in the present study, likelihood of uptake among practices could vary widely, according to Anne M. Wallace, MD, professor of clinical surgery at UC San Diego Health and director of the Moores Comprehensive Breast Health Program.
On a fundamental level, not all centers use Epic software, which could present issues with compatibility, Dr. Wallace said in an interview. More importantly, she added, many institutions already have EHR-based alerts and reminders in place, so it is not always feasible to add a new nudge for every possible clinical scenario.
“Already there are so many little icons that we have to go through now when we close a note,” she said. “That’s why electronic medical records are becoming one of the leading stressors in medicine.”
This presents a more complex challenge, Dr. Wallace said, particularly as potentially practice-changing data are becoming available, and physicians may not have time to learn about them and integrate them into routine practice. She suggested that the present system may be most appropriate for oncologists in solo practice, or in small group practices where it is more challenging to have routine conversations about changing standards of care.
What Are the Risks of Using the Nudge System?
One of those conversations may surround the validity of the recommendation implemented in the present study.
Although the Society of Surgical Oncology recommends against SLNB in the described demographic, other experts, including Dr. Wallace, take a more nuanced view of the decision.
She noted that some patients with a chronological age of 70 may have a lower biological age, casting doubt on the legitimacy of the age threshold, and those near the threshold may wish to make the decision about staging for themselves.
Beyond these concerns, Dr. Wallace described two potential risks involved in forgoing SLNB.
First, there’s the potential for underestimating the tumor’s severity, she said, as this could mean a trip back to the operating room. A tumor initially thought to be low-grade might later be found to be high-grade, necessitating further surgery. Some patients might refuse additional surgery, leaving the more aggressive tumor untreated.
Second, the nudge system could complicate radiation treatment decisions, Dr. Wallace said. Without full nodal status, some radiation oncologists might push for additional radiation therapy, which incurs a greater treatment burden than SNLB.
What Are Some Alternatives to the Nudge System?
After discussing the strengths and weaknesses of the present EHR-based nudge system, and others like it, Dr. Wallace returned to the importance of ongoing communication among colleagues managing complex cases.
At UC San Diego Health, where oncologists meet weekly for a 2-hour breast cancer conference, “we nudge each other,” she said.
This study was supported by the Shear Family Foundation, UPMC eRecord Ambulatory Decision Support and Analytics, UPMC Hillman Cancer Center Biostatistics Facility, and National Institutes of Health. The investigators disclosed relationships with Pfizer, Amgen, the Lewin Group, and Milestone Pennsylvania, and others.
FROM JAMA SURGERY
Cognitive Decline Minimal After Endocrine + CDK4/6 Inhibition in BC
“Patients who are diagnosed with advanced breast cancer and start their first-line treatment already show cognitive impairments due to their previous treatments. And luckily, our results show that during first-line treatment for advanced breast cancer with endocrine therapy, with or without a CDK4/6 inhibitor, further cognitive decline is minimal,” lead investigator Maryse Luijendijk, said during her presentation at the annual meeting of the American Society of Clinical Oncology (ASCO).
“It is well known that cancer patients can experience cognitive problems, such as memory loss, problems with concentration or with planning, during or following their treatment,” explained Ms. Luijendijk, a PhD candidate in the department of Psychosocial Research and Epidemiology at the Netherlands Cancer Institute, in Amsterdam. “Much is known about the effects of chemotherapy or irradiation to the brain, but evidence into endocrine therapy is scarce, which is surprising because cognitive effects are biologically plausible.
“We know that estrogen plays an important role in neuronal functioning and that certain types of endocrine therapies are able to cross the blood-brain barrier, where they may interact with estrogen receptors distributed widely throughout the brain … We know that CDK4/6 inhibitors may either negatively affect cognitive function by increased fatigue due to cytokine release or by interrupting the cell cycle of healthy cells, or positively, as they have been associated with reduced inflammation and remyelination.”
Initial results of the SONIA trial, reported at ASCO last year, examined overall and progression-free survival in patients with HR-positive, HER2-negative metastatic breast cancer and no prior treatment for advanced disease. Findings for those who were randomized to treatment with nonsteroidal aromatase inhibition either with or without the addition of CDK4/6 inhibitors showed no between-group differences, explained Ms. Luijendijk.
The new results, described as being from the SONIA-EfFECT (Evaluation of cognitive functioning in patients with metastatic breast cancer treated with endocrine or combined therapy) trial, were based on the authors investigating cognitive functioning in the same cohort used in the SONIA trial plus a control group.
In SONIA-EfFECT, patients who participated in SONIA were asked to identify a female relative or friend without cancer to serve as a cancer-free control. Members of the 130-patient control group were matched for age, education, and computer use.
Participants in the SONIA trial and control group were asked to complete the Amsterdam Cognition Scan, an online neuropsychological test battery at baseline and again after 9 months of treatment. Of those patients from SONIA, 130 had received first-line treatment with aromatase inhibitors with CDK4/6 inhibition (Arm A) and 130 had received aromatase inhibitors without CDK4/6 inhibition (Arm B).
Baseline assessments for SONIA-EfFECT were completed for 260 patients from SONIA and the full 130-person control group. Follow-up assessments were completed for 119 members of the control group and 199 patients from the original SONIA trial (108 from Arm A, and 91 from Arm B). Patients from SONIA who switched to second-line treatment within 9 months were not retested.
Patients in both SONIA arms performed significantly worse than the controls on the domains of verbal memory, working memory, processing speed, executive function, and motor function. In both patient arms and the controls, standardized regression-based change scores showed limited decline in cognitive function over the 9-month interval. Minimal differences in cognitive change were observed between the patients treated with and without CDK4/6 inhibitors, and between patients and the controls, according to the abstract for SONIA-EfFECT, published in the program for the annual meeting of ASCO.
“At baseline, patients show worse cognitive function across all domains compared to the controls. And as expected, there were no differences between the two treatment arms,” Ms. Luijendijk explained. After 9 months of treatment, the testing showed limited further decline among patients, “and even some improvement on some tests,” with minimal differences between treatment arms “implying that cognitive function does not need to be an aspect when deciding on treatment.”
Ms. Luijendijk reported no relevant disclosures.
“Patients who are diagnosed with advanced breast cancer and start their first-line treatment already show cognitive impairments due to their previous treatments. And luckily, our results show that during first-line treatment for advanced breast cancer with endocrine therapy, with or without a CDK4/6 inhibitor, further cognitive decline is minimal,” lead investigator Maryse Luijendijk, said during her presentation at the annual meeting of the American Society of Clinical Oncology (ASCO).
“It is well known that cancer patients can experience cognitive problems, such as memory loss, problems with concentration or with planning, during or following their treatment,” explained Ms. Luijendijk, a PhD candidate in the department of Psychosocial Research and Epidemiology at the Netherlands Cancer Institute, in Amsterdam. “Much is known about the effects of chemotherapy or irradiation to the brain, but evidence into endocrine therapy is scarce, which is surprising because cognitive effects are biologically plausible.
“We know that estrogen plays an important role in neuronal functioning and that certain types of endocrine therapies are able to cross the blood-brain barrier, where they may interact with estrogen receptors distributed widely throughout the brain … We know that CDK4/6 inhibitors may either negatively affect cognitive function by increased fatigue due to cytokine release or by interrupting the cell cycle of healthy cells, or positively, as they have been associated with reduced inflammation and remyelination.”
Initial results of the SONIA trial, reported at ASCO last year, examined overall and progression-free survival in patients with HR-positive, HER2-negative metastatic breast cancer and no prior treatment for advanced disease. Findings for those who were randomized to treatment with nonsteroidal aromatase inhibition either with or without the addition of CDK4/6 inhibitors showed no between-group differences, explained Ms. Luijendijk.
The new results, described as being from the SONIA-EfFECT (Evaluation of cognitive functioning in patients with metastatic breast cancer treated with endocrine or combined therapy) trial, were based on the authors investigating cognitive functioning in the same cohort used in the SONIA trial plus a control group.
In SONIA-EfFECT, patients who participated in SONIA were asked to identify a female relative or friend without cancer to serve as a cancer-free control. Members of the 130-patient control group were matched for age, education, and computer use.
Participants in the SONIA trial and control group were asked to complete the Amsterdam Cognition Scan, an online neuropsychological test battery at baseline and again after 9 months of treatment. Of those patients from SONIA, 130 had received first-line treatment with aromatase inhibitors with CDK4/6 inhibition (Arm A) and 130 had received aromatase inhibitors without CDK4/6 inhibition (Arm B).
Baseline assessments for SONIA-EfFECT were completed for 260 patients from SONIA and the full 130-person control group. Follow-up assessments were completed for 119 members of the control group and 199 patients from the original SONIA trial (108 from Arm A, and 91 from Arm B). Patients from SONIA who switched to second-line treatment within 9 months were not retested.
Patients in both SONIA arms performed significantly worse than the controls on the domains of verbal memory, working memory, processing speed, executive function, and motor function. In both patient arms and the controls, standardized regression-based change scores showed limited decline in cognitive function over the 9-month interval. Minimal differences in cognitive change were observed between the patients treated with and without CDK4/6 inhibitors, and between patients and the controls, according to the abstract for SONIA-EfFECT, published in the program for the annual meeting of ASCO.
“At baseline, patients show worse cognitive function across all domains compared to the controls. And as expected, there were no differences between the two treatment arms,” Ms. Luijendijk explained. After 9 months of treatment, the testing showed limited further decline among patients, “and even some improvement on some tests,” with minimal differences between treatment arms “implying that cognitive function does not need to be an aspect when deciding on treatment.”
Ms. Luijendijk reported no relevant disclosures.
“Patients who are diagnosed with advanced breast cancer and start their first-line treatment already show cognitive impairments due to their previous treatments. And luckily, our results show that during first-line treatment for advanced breast cancer with endocrine therapy, with or without a CDK4/6 inhibitor, further cognitive decline is minimal,” lead investigator Maryse Luijendijk, said during her presentation at the annual meeting of the American Society of Clinical Oncology (ASCO).
“It is well known that cancer patients can experience cognitive problems, such as memory loss, problems with concentration or with planning, during or following their treatment,” explained Ms. Luijendijk, a PhD candidate in the department of Psychosocial Research and Epidemiology at the Netherlands Cancer Institute, in Amsterdam. “Much is known about the effects of chemotherapy or irradiation to the brain, but evidence into endocrine therapy is scarce, which is surprising because cognitive effects are biologically plausible.
“We know that estrogen plays an important role in neuronal functioning and that certain types of endocrine therapies are able to cross the blood-brain barrier, where they may interact with estrogen receptors distributed widely throughout the brain … We know that CDK4/6 inhibitors may either negatively affect cognitive function by increased fatigue due to cytokine release or by interrupting the cell cycle of healthy cells, or positively, as they have been associated with reduced inflammation and remyelination.”
Initial results of the SONIA trial, reported at ASCO last year, examined overall and progression-free survival in patients with HR-positive, HER2-negative metastatic breast cancer and no prior treatment for advanced disease. Findings for those who were randomized to treatment with nonsteroidal aromatase inhibition either with or without the addition of CDK4/6 inhibitors showed no between-group differences, explained Ms. Luijendijk.
The new results, described as being from the SONIA-EfFECT (Evaluation of cognitive functioning in patients with metastatic breast cancer treated with endocrine or combined therapy) trial, were based on the authors investigating cognitive functioning in the same cohort used in the SONIA trial plus a control group.
In SONIA-EfFECT, patients who participated in SONIA were asked to identify a female relative or friend without cancer to serve as a cancer-free control. Members of the 130-patient control group were matched for age, education, and computer use.
Participants in the SONIA trial and control group were asked to complete the Amsterdam Cognition Scan, an online neuropsychological test battery at baseline and again after 9 months of treatment. Of those patients from SONIA, 130 had received first-line treatment with aromatase inhibitors with CDK4/6 inhibition (Arm A) and 130 had received aromatase inhibitors without CDK4/6 inhibition (Arm B).
Baseline assessments for SONIA-EfFECT were completed for 260 patients from SONIA and the full 130-person control group. Follow-up assessments were completed for 119 members of the control group and 199 patients from the original SONIA trial (108 from Arm A, and 91 from Arm B). Patients from SONIA who switched to second-line treatment within 9 months were not retested.
Patients in both SONIA arms performed significantly worse than the controls on the domains of verbal memory, working memory, processing speed, executive function, and motor function. In both patient arms and the controls, standardized regression-based change scores showed limited decline in cognitive function over the 9-month interval. Minimal differences in cognitive change were observed between the patients treated with and without CDK4/6 inhibitors, and between patients and the controls, according to the abstract for SONIA-EfFECT, published in the program for the annual meeting of ASCO.
“At baseline, patients show worse cognitive function across all domains compared to the controls. And as expected, there were no differences between the two treatment arms,” Ms. Luijendijk explained. After 9 months of treatment, the testing showed limited further decline among patients, “and even some improvement on some tests,” with minimal differences between treatment arms “implying that cognitive function does not need to be an aspect when deciding on treatment.”
Ms. Luijendijk reported no relevant disclosures.
FROM ASCO 2024
Does Extended Postop Follow-Up Improve Survival in Gastric Cancer?
TOPLINE:
METHODOLOGY:
- Currently, postgastrectomy cancer surveillance typically lasts 5 years, although some centers now monitor patients beyond this point.
- To investigate the potential benefit of extended surveillance, researchers used Korean National Health Insurance claims data to identify 40,468 patients with gastric cancer who were disease free 5 years after gastrectomy — 14,294 received extended regular follow-up visits and 26,174 did not.
- The extended regular follow-up group was defined as having endoscopy or abdominopelvic CT between 2 months and 2 years before diagnosis of late recurrence or gastric remnant cancer and having two or more examinations between 5.5 and 8.5 years after gastrectomy. Late recurrence was a recurrence diagnosed 5 years after gastrectomy.
- Researchers used Cox proportional hazards regression to evaluate the independent association between follow-up and overall and postrecurrence survival rates.
TAKEAWAY:
- Overall, 5 years postgastrectomy, the incidence of late recurrence or gastric remnant cancer was 7.8% — 4.0% between 5 and 10 years (1610 of 40,468 patients) and 9.4% after 10 years (1528 of 16,287 patients).
- Regular follow-up beyond 5 years was associated with a significant reduction in overall mortality — from 49.4% to 36.9% at 15 years (P < .001). Overall survival after late recurrence or gastric remnant cancer also improved significantly with extended regular follow-up, with the 5-year postrecurrence survival rate increasing from 32.7% to 71.1% (P < .001).
- The combination of endoscopy and abdominopelvic CT provided the highest 5-year postrecurrence survival rate (74.5%), compared with endoscopy alone (54.5%) or CT alone (47.1%).
- A time interval of more than 2 years between a previous endoscopy or abdominopelvic CT and diagnosis of late recurrence or gastric remnant cancer significantly decreased postrecurrence survival (hazard ratio [HR], 1.72 for endoscopy and HR, 1.48 for abdominopelvic CT).
IN PRACTICE:
“These findings suggest that extended regular follow-up after 5 years post gastrectomy should be implemented clinically and that current practice and value of follow-up protocols in postoperative care of patients with gastric cancer be reconsidered,” the authors concluded.
The authors of an accompanying commentary cautioned that, while the study “successfully establishes groundwork for extending surveillance of gastric cancer in high-risk populations, more work is needed to strategically identify those who would benefit most from extended surveillance.”
SOURCE:
The study, with first author Ju-Hee Lee, MD, PhD, Department of Surgery, Hanyang University College of Medicine, Seoul, South Korea, and accompanying commentary were published online on June 18 in JAMA Surgery.
LIMITATIONS:
Recurrent cancer and gastric remnant cancer could not be distinguished from each other because clinical records were not analyzed. The claims database lacked detailed clinical information on individual patients, including cancer stages, and a separate analysis of tumor markers could not be performed.
DISCLOSURES:
The study was funded by a grant from the Korean Gastric Cancer Association. The study authors and commentary authors reported no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Currently, postgastrectomy cancer surveillance typically lasts 5 years, although some centers now monitor patients beyond this point.
- To investigate the potential benefit of extended surveillance, researchers used Korean National Health Insurance claims data to identify 40,468 patients with gastric cancer who were disease free 5 years after gastrectomy — 14,294 received extended regular follow-up visits and 26,174 did not.
- The extended regular follow-up group was defined as having endoscopy or abdominopelvic CT between 2 months and 2 years before diagnosis of late recurrence or gastric remnant cancer and having two or more examinations between 5.5 and 8.5 years after gastrectomy. Late recurrence was a recurrence diagnosed 5 years after gastrectomy.
- Researchers used Cox proportional hazards regression to evaluate the independent association between follow-up and overall and postrecurrence survival rates.
TAKEAWAY:
- Overall, 5 years postgastrectomy, the incidence of late recurrence or gastric remnant cancer was 7.8% — 4.0% between 5 and 10 years (1610 of 40,468 patients) and 9.4% after 10 years (1528 of 16,287 patients).
- Regular follow-up beyond 5 years was associated with a significant reduction in overall mortality — from 49.4% to 36.9% at 15 years (P < .001). Overall survival after late recurrence or gastric remnant cancer also improved significantly with extended regular follow-up, with the 5-year postrecurrence survival rate increasing from 32.7% to 71.1% (P < .001).
- The combination of endoscopy and abdominopelvic CT provided the highest 5-year postrecurrence survival rate (74.5%), compared with endoscopy alone (54.5%) or CT alone (47.1%).
- A time interval of more than 2 years between a previous endoscopy or abdominopelvic CT and diagnosis of late recurrence or gastric remnant cancer significantly decreased postrecurrence survival (hazard ratio [HR], 1.72 for endoscopy and HR, 1.48 for abdominopelvic CT).
IN PRACTICE:
“These findings suggest that extended regular follow-up after 5 years post gastrectomy should be implemented clinically and that current practice and value of follow-up protocols in postoperative care of patients with gastric cancer be reconsidered,” the authors concluded.
The authors of an accompanying commentary cautioned that, while the study “successfully establishes groundwork for extending surveillance of gastric cancer in high-risk populations, more work is needed to strategically identify those who would benefit most from extended surveillance.”
SOURCE:
The study, with first author Ju-Hee Lee, MD, PhD, Department of Surgery, Hanyang University College of Medicine, Seoul, South Korea, and accompanying commentary were published online on June 18 in JAMA Surgery.
LIMITATIONS:
Recurrent cancer and gastric remnant cancer could not be distinguished from each other because clinical records were not analyzed. The claims database lacked detailed clinical information on individual patients, including cancer stages, and a separate analysis of tumor markers could not be performed.
DISCLOSURES:
The study was funded by a grant from the Korean Gastric Cancer Association. The study authors and commentary authors reported no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Currently, postgastrectomy cancer surveillance typically lasts 5 years, although some centers now monitor patients beyond this point.
- To investigate the potential benefit of extended surveillance, researchers used Korean National Health Insurance claims data to identify 40,468 patients with gastric cancer who were disease free 5 years after gastrectomy — 14,294 received extended regular follow-up visits and 26,174 did not.
- The extended regular follow-up group was defined as having endoscopy or abdominopelvic CT between 2 months and 2 years before diagnosis of late recurrence or gastric remnant cancer and having two or more examinations between 5.5 and 8.5 years after gastrectomy. Late recurrence was a recurrence diagnosed 5 years after gastrectomy.
- Researchers used Cox proportional hazards regression to evaluate the independent association between follow-up and overall and postrecurrence survival rates.
TAKEAWAY:
- Overall, 5 years postgastrectomy, the incidence of late recurrence or gastric remnant cancer was 7.8% — 4.0% between 5 and 10 years (1610 of 40,468 patients) and 9.4% after 10 years (1528 of 16,287 patients).
- Regular follow-up beyond 5 years was associated with a significant reduction in overall mortality — from 49.4% to 36.9% at 15 years (P < .001). Overall survival after late recurrence or gastric remnant cancer also improved significantly with extended regular follow-up, with the 5-year postrecurrence survival rate increasing from 32.7% to 71.1% (P < .001).
- The combination of endoscopy and abdominopelvic CT provided the highest 5-year postrecurrence survival rate (74.5%), compared with endoscopy alone (54.5%) or CT alone (47.1%).
- A time interval of more than 2 years between a previous endoscopy or abdominopelvic CT and diagnosis of late recurrence or gastric remnant cancer significantly decreased postrecurrence survival (hazard ratio [HR], 1.72 for endoscopy and HR, 1.48 for abdominopelvic CT).
IN PRACTICE:
“These findings suggest that extended regular follow-up after 5 years post gastrectomy should be implemented clinically and that current practice and value of follow-up protocols in postoperative care of patients with gastric cancer be reconsidered,” the authors concluded.
The authors of an accompanying commentary cautioned that, while the study “successfully establishes groundwork for extending surveillance of gastric cancer in high-risk populations, more work is needed to strategically identify those who would benefit most from extended surveillance.”
SOURCE:
The study, with first author Ju-Hee Lee, MD, PhD, Department of Surgery, Hanyang University College of Medicine, Seoul, South Korea, and accompanying commentary were published online on June 18 in JAMA Surgery.
LIMITATIONS:
Recurrent cancer and gastric remnant cancer could not be distinguished from each other because clinical records were not analyzed. The claims database lacked detailed clinical information on individual patients, including cancer stages, and a separate analysis of tumor markers could not be performed.
DISCLOSURES:
The study was funded by a grant from the Korean Gastric Cancer Association. The study authors and commentary authors reported no conflicts of interest.
A version of this article appeared on Medscape.com.
Factors Linked to Complete Response, Survival in Pancreatic Cancer
TOPLINE:
a multicenter cohort study found. Several factors, including treatment type and tumor features, influenced the outcomes.
METHODOLOGY:
- Preoperative chemo(radio)therapy is increasingly used in patients with localized pancreatic adenocarcinoma and may improve the chance of a pathologic complete response. Achieving a pathologic complete response is associated with improved overall survival.
- However, the evidence on pathologic complete response is based on large national databases or small single-center series. Multicenter studies with in-depth data about complete response are lacking.
- In the current analysis, researchers investigated the incidence and factors associated with pathologic complete response after preoperative chemo(radio)therapy among 1758 patients (mean age, 64 years; 50% men) with localized pancreatic adenocarcinoma who underwent resection after two or more cycles of chemotherapy (with or without radiotherapy).
- Patients were treated at 19 centers in eight countries. The median follow-up was 19 months. Pathologic complete response was defined as the absence of vital tumor cells in the patient’s sampled pancreas specimen after resection.
- Factors associated with overall survival and pathologic complete response were investigated with Cox proportional hazards and logistic regression models, respectively.
TAKEAWAY:
- Researchers found that the rate of pathologic complete response was 4.8% in patients who received chemo(radio)therapy before pancreatic cancer resection.
- Having a pathologic complete response was associated with a 54% lower risk for death (hazard ratio, 0.46). At 5 years, the overall survival rate was 63% in patients with a pathologic complete response vs 30% in patients without one.
- More patients who received preoperative modified FOLFIRINOX achieved a pathologic complete response (58.8% vs 44.7%). Other factors associated with pathologic complete response included tumors located in the pancreatic head (odds ratio [OR], 2.51), tumors > 40 mm at diagnosis (OR, 2.58), partial or complete radiologic response (OR, 13.0), and normal(ized) serum carbohydrate antigen 19-9 after preoperative therapy (OR, 3.76).
- Preoperative radiotherapy (OR, 2.03) and preoperative stereotactic body radiotherapy (OR, 8.91) were also associated with a pathologic complete response; however, preoperative radiotherapy did not improve overall survival, and preoperative stereotactic body radiotherapy was independently associated with worse overall survival. These findings suggest that a pathologic complete response might not always reflect an optimal disease response.
IN PRACTICE:
Although pathologic complete response does not reflect cure, it is associated with better overall survival, the authors wrote. Factors associated with a pathologic complete response may inform treatment decisions.
SOURCE:
The study, with first author Thomas F. Stoop, MD, University of Amsterdam, the Netherlands, was published online on June 18 in JAMA Network Open.
LIMITATIONS:
The study had several limitations. The sample size and the limited number of events precluded comparative subanalyses, as well as a more detailed stratification for preoperative chemotherapy regimens. Information about patients’ race and the presence of BRCA germline mutations, both of which seem to be relevant to the chance of achieving a major pathologic response, was not collected or available.
DISCLOSURES:
No specific funding was noted. Several coauthors have industry relationships outside of the submitted work.
A version of this article first appeared on Medscape.com.
TOPLINE:
a multicenter cohort study found. Several factors, including treatment type and tumor features, influenced the outcomes.
METHODOLOGY:
- Preoperative chemo(radio)therapy is increasingly used in patients with localized pancreatic adenocarcinoma and may improve the chance of a pathologic complete response. Achieving a pathologic complete response is associated with improved overall survival.
- However, the evidence on pathologic complete response is based on large national databases or small single-center series. Multicenter studies with in-depth data about complete response are lacking.
- In the current analysis, researchers investigated the incidence and factors associated with pathologic complete response after preoperative chemo(radio)therapy among 1758 patients (mean age, 64 years; 50% men) with localized pancreatic adenocarcinoma who underwent resection after two or more cycles of chemotherapy (with or without radiotherapy).
- Patients were treated at 19 centers in eight countries. The median follow-up was 19 months. Pathologic complete response was defined as the absence of vital tumor cells in the patient’s sampled pancreas specimen after resection.
- Factors associated with overall survival and pathologic complete response were investigated with Cox proportional hazards and logistic regression models, respectively.
TAKEAWAY:
- Researchers found that the rate of pathologic complete response was 4.8% in patients who received chemo(radio)therapy before pancreatic cancer resection.
- Having a pathologic complete response was associated with a 54% lower risk for death (hazard ratio, 0.46). At 5 years, the overall survival rate was 63% in patients with a pathologic complete response vs 30% in patients without one.
- More patients who received preoperative modified FOLFIRINOX achieved a pathologic complete response (58.8% vs 44.7%). Other factors associated with pathologic complete response included tumors located in the pancreatic head (odds ratio [OR], 2.51), tumors > 40 mm at diagnosis (OR, 2.58), partial or complete radiologic response (OR, 13.0), and normal(ized) serum carbohydrate antigen 19-9 after preoperative therapy (OR, 3.76).
- Preoperative radiotherapy (OR, 2.03) and preoperative stereotactic body radiotherapy (OR, 8.91) were also associated with a pathologic complete response; however, preoperative radiotherapy did not improve overall survival, and preoperative stereotactic body radiotherapy was independently associated with worse overall survival. These findings suggest that a pathologic complete response might not always reflect an optimal disease response.
IN PRACTICE:
Although pathologic complete response does not reflect cure, it is associated with better overall survival, the authors wrote. Factors associated with a pathologic complete response may inform treatment decisions.
SOURCE:
The study, with first author Thomas F. Stoop, MD, University of Amsterdam, the Netherlands, was published online on June 18 in JAMA Network Open.
LIMITATIONS:
The study had several limitations. The sample size and the limited number of events precluded comparative subanalyses, as well as a more detailed stratification for preoperative chemotherapy regimens. Information about patients’ race and the presence of BRCA germline mutations, both of which seem to be relevant to the chance of achieving a major pathologic response, was not collected or available.
DISCLOSURES:
No specific funding was noted. Several coauthors have industry relationships outside of the submitted work.
A version of this article first appeared on Medscape.com.
TOPLINE:
a multicenter cohort study found. Several factors, including treatment type and tumor features, influenced the outcomes.
METHODOLOGY:
- Preoperative chemo(radio)therapy is increasingly used in patients with localized pancreatic adenocarcinoma and may improve the chance of a pathologic complete response. Achieving a pathologic complete response is associated with improved overall survival.
- However, the evidence on pathologic complete response is based on large national databases or small single-center series. Multicenter studies with in-depth data about complete response are lacking.
- In the current analysis, researchers investigated the incidence and factors associated with pathologic complete response after preoperative chemo(radio)therapy among 1758 patients (mean age, 64 years; 50% men) with localized pancreatic adenocarcinoma who underwent resection after two or more cycles of chemotherapy (with or without radiotherapy).
- Patients were treated at 19 centers in eight countries. The median follow-up was 19 months. Pathologic complete response was defined as the absence of vital tumor cells in the patient’s sampled pancreas specimen after resection.
- Factors associated with overall survival and pathologic complete response were investigated with Cox proportional hazards and logistic regression models, respectively.
TAKEAWAY:
- Researchers found that the rate of pathologic complete response was 4.8% in patients who received chemo(radio)therapy before pancreatic cancer resection.
- Having a pathologic complete response was associated with a 54% lower risk for death (hazard ratio, 0.46). At 5 years, the overall survival rate was 63% in patients with a pathologic complete response vs 30% in patients without one.
- More patients who received preoperative modified FOLFIRINOX achieved a pathologic complete response (58.8% vs 44.7%). Other factors associated with pathologic complete response included tumors located in the pancreatic head (odds ratio [OR], 2.51), tumors > 40 mm at diagnosis (OR, 2.58), partial or complete radiologic response (OR, 13.0), and normal(ized) serum carbohydrate antigen 19-9 after preoperative therapy (OR, 3.76).
- Preoperative radiotherapy (OR, 2.03) and preoperative stereotactic body radiotherapy (OR, 8.91) were also associated with a pathologic complete response; however, preoperative radiotherapy did not improve overall survival, and preoperative stereotactic body radiotherapy was independently associated with worse overall survival. These findings suggest that a pathologic complete response might not always reflect an optimal disease response.
IN PRACTICE:
Although pathologic complete response does not reflect cure, it is associated with better overall survival, the authors wrote. Factors associated with a pathologic complete response may inform treatment decisions.
SOURCE:
The study, with first author Thomas F. Stoop, MD, University of Amsterdam, the Netherlands, was published online on June 18 in JAMA Network Open.
LIMITATIONS:
The study had several limitations. The sample size and the limited number of events precluded comparative subanalyses, as well as a more detailed stratification for preoperative chemotherapy regimens. Information about patients’ race and the presence of BRCA germline mutations, both of which seem to be relevant to the chance of achieving a major pathologic response, was not collected or available.
DISCLOSURES:
No specific funding was noted. Several coauthors have industry relationships outside of the submitted work.
A version of this article first appeared on Medscape.com.
Managing Cancer in Pregnancy: Improvements and Considerations
Introduction: Tremendous Progress on Cancer Extends to Cancer in Pregnancy
The biomedical research enterprise that took shape in the United States after World War II has had numerous positive effects, including significant progress made during the past 75-plus years in the diagnosis, prevention, and treatment of cancer.
President Franklin D. Roosevelt’s 1944 request of Dr. Vannevar Bush, director of the then Office of Scientific Research and Development, to organize a program that would advance and apply scientific knowledge for times of peace — just as it been advanced and applied in times of war — culminated in a historic report, Science – The Endless Frontier. Presented in 1945 to President Harry S. Truman, this report helped fuel decades of broad, bold, and coordinated government-sponsored biomedical research aimed at addressing disease and improving the health of the American people (National Science Foundation, 1945).
Discoveries made from research in basic and translational sciences deepened our knowledge of the cellular and molecular underpinnings of cancer, leading to advances in chemotherapy, radiotherapy, and other treatment approaches as well as continual refinements in their application. Similarly, our diagnostic armamentarium has significantly improved.
As a result, we have reduced both the incidence and mortality of cancer. Today, some cancers can be prevented. Others can be reversed or put in remission. Granted, progress has been variable, with some cancers such as ovarian cancer still having relatively low survival rates. Much more needs to be done. Overall, however, the positive effects of the U.S. biomedical research enterprise on cancer are evident. According to the National Cancer Institute’s most recent report on the status of cancer, death rates from cancer fell 1.9% per year on average in females from 2015 to 2019 (Cancer. 2022 Oct 22. doi: 10.1002/cncr.34479).
It is not only patients whose cancer occurs outside of pregnancy who have benefited. When treatment is appropriately selected and timing considerations are made, patients whose cancer is diagnosed during pregnancy — and their children — can have good outcomes.
To explain how the management of cancer in pregnancy has improved, we have invited Gautam G. Rao, MD, gynecologic oncologist and associate professor of obstetrics, gynecology, and reproductive sciences at the University of Maryland School of Medicine, to write this installment of the Master Class in Obstetrics. As Dr. Rao explains, radiation is not as dangerous to the fetus as once thought, and the safety of many chemotherapeutic regimens in pregnancy has been documented. Obstetricians can and should counsel patients, he explains, about the likelihood of good maternal and fetal outcomes.
E. Albert Reece, MD, PhD, MBA, a maternal-fetal medicine specialist, is dean emeritus of the University of Maryland School of Medicine, former university executive vice president; currently the endowed professor and director of the Center for Advanced Research Training and Innovation (CARTI), and senior scientist in the Center for Birth Defects Research. Dr. Reece reported no relevant disclosures. He is the medical editor of this column. Contact him at obnews@mdedge.com.
Managing Cancer in Pregnancy
Cancer can cause fear and distress for any patient, but when cancer is diagnosed during pregnancy, an expectant mother fears not only for her own health but for the health of her unborn child. Fortunately, ob.gyn.s and multidisciplinary teams have good reason to reassure patients about the likelihood of good outcomes.
Cancer treatment in pregnancy has improved with advancements in imaging and chemotherapy, and while maternal and fetal outcomes of prenatal cancer treatment are not well reported, evidence acquired in recent years from case series and retrospective studies shows that most imaging studies and procedural diagnostic tests – and many treatments – can be performed safely in pregnancy.
Decades ago, we avoided CT scans during pregnancy because of concerns about radiation exposure to the fetus, leaving some patients without an accurate staging of their cancer. Today, we have evidence that a CT scan is generally safe in pregnancy. Similarly, the safety of many chemotherapeutic regimens in pregnancy has been documented in recent decades,and the use of chemotherapy during pregnancy has increased progressively. Radiation is also commonly utilized in the management of cancers that may occur during pregnancy, such as breast cancer.1
Considerations of timing are often central to decision-making; chemotherapy and radiotherapy are generally avoided in the first trimester to prevent structural fetal anomalies, for instance, and delaying cancer treatment is often warranted when the patient is a few weeks away from delivery. On occasion, iatrogenic preterm birth is considered when the risks to the mother of delaying a necessary cancer treatment outweigh the risks to the fetus of prematurity.1
Pregnancy termination is rarely indicated, however, and information gathered over the past 2 decades suggests that fetal and placental metastases are rare.1 There is broad agreement that prenatal treatment of cancer in pregnancy should adhere as much as possible to protocols and guidelines for nonpregnant patients and that treatment delays driven by fear of fetal anomalies and miscarriage are unnecessary.
Cancer Incidence, Use of Diagnostic Imaging
Data on the incidence of cancer in pregnancy comes from population-based cancer registries, and unfortunately, these data are not standardized and are often incomplete. Many studies include cancer diagnosed up to 1 year after pregnancy, and some include preinvasive disease. Estimates therefore vary considerably (see Table 1 for a sampling of estimates incidences.)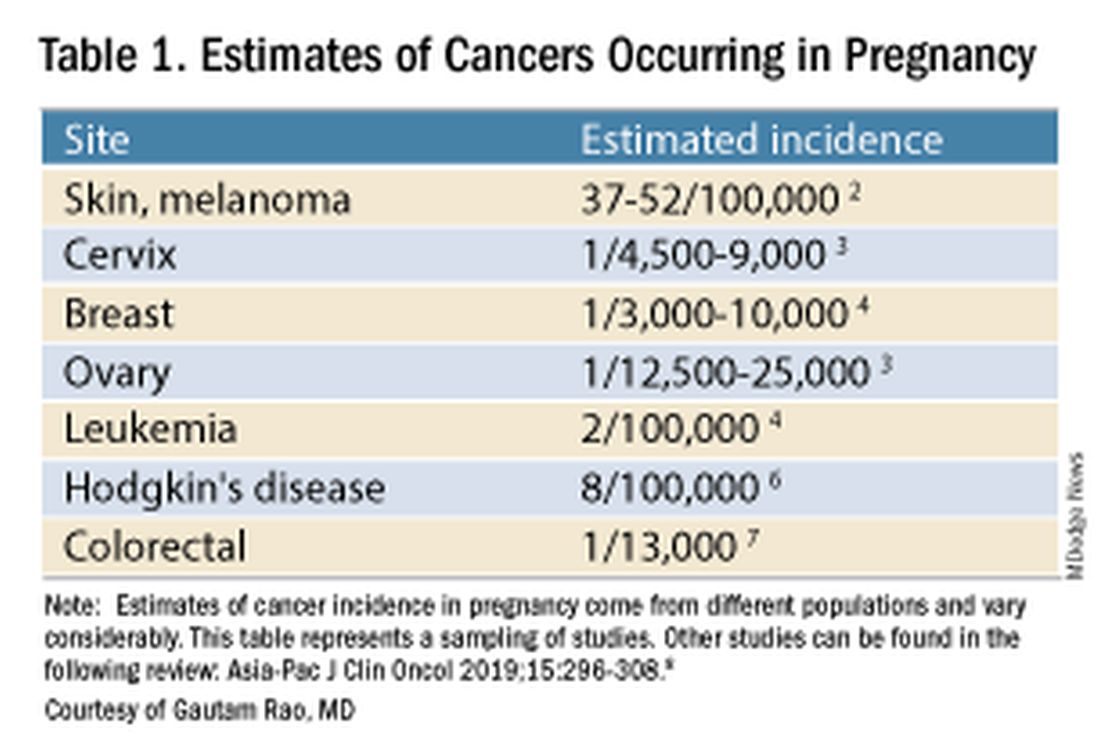
It has been reported, and often cited in the literature, that invasive malignancy complicates one in 1,000 pregnancies and that the incidence of cancer in pregnancy (invasive and noninvasive malignancies) has been rising over time.8 Increasing maternal age is believed to be playing a role in this rise; as women delay childbearing, they enter the age range in which some cancers become more common. Additionally, improvements in screening and diagnostics have led to earlier cancer detection. The incidence of ovarian neoplasms found during pregnancy has increased, for instance, with the routine use of diagnostic ultrasound in pregnancy.1
Among the studies showing an increased incidence of pregnancy-associated cancer is a population-based study in Australia, which found that from 1994 to 2007 the crude incidence of pregnancy-associated cancer increased from 112.3 to 191.5 per 100,000 pregnancies (P < .001).9 A cohort study in the United States documented an increase in incidence from 75.0 per 100,000 pregnancies in 2002 to 138.5 per 100,000 pregnancies in 2012.10
Overall, the literature shows us that the skin, cervix, and breast are also common sites for malignancy during pregnancy.1 According to a 2022 review, breast cancer during pregnancy is less often hormone receptor–positive and more frequently triple negative compared with age-matched controls.11 The frequencies of other pregnancy-associated cancers appear overall to be similar to that of cancer occurring in all women across their reproductive years.1
Too often, diagnosis is delayed because cancer symptoms can be masked by or can mimic normal physiological changes in pregnancy. For instance, breast cancer can be difficult to diagnose during pregnancy and lactation due to anatomic changes in the breast parenchyma. Several studies published in the 1990s showed that breast cancer presents at a more advanced stage in pregnant patients than in nonpregnant patients because of this delay.1 Skin changes suggestive of melanoma can be attributed to hyperpigmentation of pregnancy, for instance. Several observational studies have suggested that thicker melanomas found in pregnancy may be because of delayed diagnosis.8
It is important that we thoroughly investigate signs and symptoms suggestive of a malignancy and not automatically attribute these symptoms to the pregnancy itself. Cervical biopsy of a mass or lesion suspicious for cervical cancer can be done safely during pregnancy and should not be delayed or deferred.
Fetal radiation exposure from radiologic examinations has long been a concern, but we know today that while the imaging modality should be chosen to minimize fetal radiation exposure, CT scans and even PET scans should be performed if these exams are deemed best for evaluation. Embryonic exposure to a dose of less than 50 mGy is rarely if at all associated with fetal malformations or miscarriage and a radiation dose of 100 mGy may be considered a floor for consideration of therapeutic termination of pregnancy.1,8
CT exams are associated with a fetal dose far less than 50 mGy (see Table 2 for radiation doses).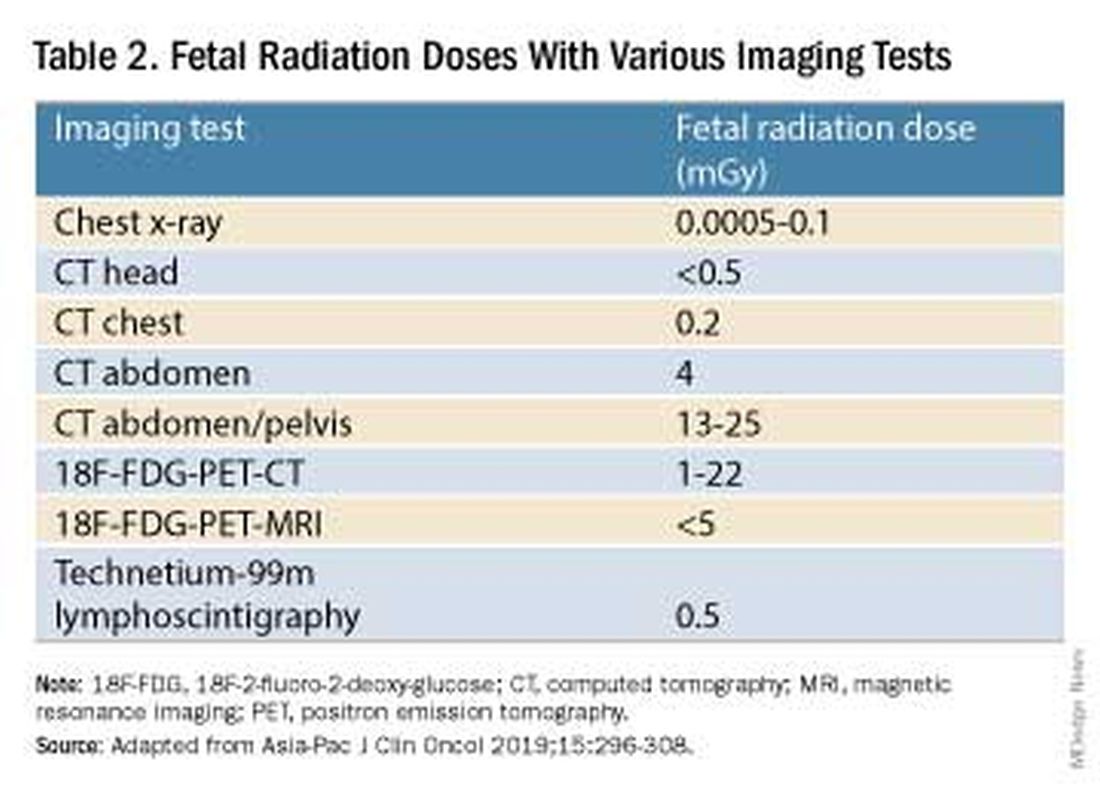
Magnetic resonance imaging with a magnet strength of 3 Tesla or less in any trimester is not associated with an increased risk of harm to the fetus or in early childhood, but the contrast agent gadolinium should be avoided in pregnancy as it has been associated with an increased risk of stillbirth, neonatal death, and childhood inflammatory, rheumatologic, and infiltrative skin lesions.1,8,12
Chemotherapy, Surgery, and Radiation in Pregnancy
The management of cancer during pregnancy requires a multidisciplinary team including medical, gynecologic, or radiation oncologists, and maternal-fetal medicine specialists (Figure 1). Prematurity and low birth weight are frequent complications for fetuses exposed to chemotherapy, although there is some uncertainty as to whether the treatment is causative. However, congenital anomalies no longer are a major concern, provided that drugs are appropriately selected and that fetal exposure occurs during the second or third trimester.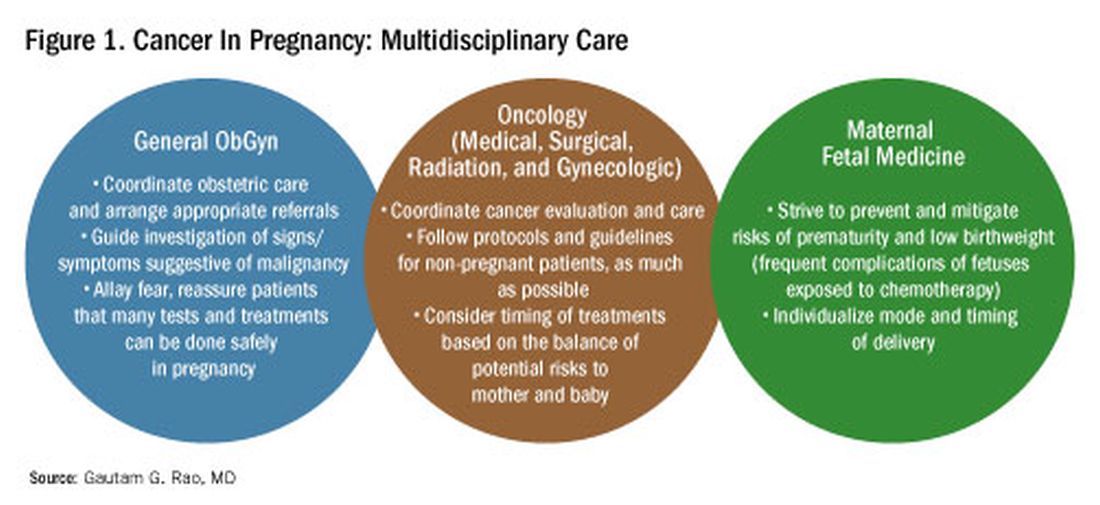
For instance, alkylating agents including cisplatin (an important drug in the management of gynecologic malignancies) have been associated with congenital anomalies in the first trimester but not in the second and third trimesters, and a variety of antimetabolites — excluding methotrexate and aminopterin — similarly have been shown to be relatively safe when used after the first trimester.1
Small studies have shown no long-term effects of chemotherapy exposure on postnatal growth and long-term neurologic/neurocognitive function,1 but this is an area that needs more research.
Also in need of investigation is the safety of newer agents in pregnancy. Data are limited on the use of new targeted treatments, monoclonal antibodies, and immunotherapies in pregnancy and their effects on the fetus, with current knowledge coming mainly from single case reports.13
Until more is learned — a challenge given that pregnant women are generally excluded from clinical trials — management teams are generally postponing use of these therapies until after delivery. Considering the pace of new developments revolutionizing cancer treatment, this topic will likely get more complex and confusing before we begin acquiring sufficient knowledge.
The timing of surgery for malignancy in pregnancy is similarly based on the balance of maternal and fetal risks, including the risk of maternal disease progression, the risk of preterm delivery, and the prevention of fetal metastases. In general, the safest time is the second trimester.
Maternal surgery in the third trimester may be associated with a risk of premature labor and altered uteroplacental perfusion. A 2005 systematic review of 12,452 women who underwent nonobstetric surgery during pregnancy provides some reassurance, however; compared with the general obstetric population, there was no increase in the rate of miscarriage or major birth defects.14
Radiotherapy used to be contraindicated in pregnancy but many experts today believe it can be safely utilized provided the uterus is out of field and is protected from scattered radiation. The head, neck, and breast, for instance, can be treated with newer radiotherapies, including stereotactic ablative radiation therapy.8 Patients with advanced cervical cancer often receive chemotherapy during pregnancy to slow metastatic growth followed by definitive treatment with postpartum radiation or surgery.
More research is needed, but available data on maternal outcomes are encouraging. For instance, there appear to be no significant differences in short- and long-term complications or survival between women who are pregnant and nonpregnant when treated for invasive cervical cancer.8 Similarly, while earlier studies of breast cancer diagnosed during pregnancy suggested a poor prognosis, data now show similar prognoses for pregnant and nonpregnant patients when controlled for stage.1
Dr. Rao is a gynecologic oncologist and associate professor of obstetrics, gynecology, and reproductive sciences at the University of Maryland School of Medicine, Baltimore. He reported no relevant disclosures.
References
1. Rao GG. Chapter 42. Clinical Obstetrics: The Fetus & Mother, 4th ed. Reece EA et al. (eds): 2021.
2. Bannister-Tyrrell M et al. Aust N Z J Obstet Gynaecol. 2014;55:116-122.
3. Oehler MK et al. Aust N Z J Obstet Gynaecol. 2003;43(6):414-420.
4. Ruiz R et al. Breast. 2017;35:136-141. doi: 10.1016/j.breast.2017.07.008.
5. Nolan S et al. Am J Obstet Gynecol. 2019;220(1):S480. doi: 10.1016/j.ajog.2018.11.752.
6. El-Messidi A et al. J Perinat Med. 2015;43(6):683-688. doi: 10.1515/jpm-2014-0133.
7. Pellino G et al. Eur J Gastroenterol Hepatol. 2017;29(7):743-753. doi: 10.1097/MEG.0000000000000863.
8. Eastwood-Wilshere N et al. Asia-Pac J Clin Oncol. 2019;15:296-308.
9. Lee YY et al. BJOG. 2012;119(13):1572-1582.
10. Cottreau CM et al. J Womens Health (Larchmt). 2019 Feb;28(2):250-257.
11. Boere I et al. Best Pract Res Clin Obstet Gynaecol. 2022;82:46-59.
12. Ray JG et al. JAMA 2016;316(9):952-961.
13. Schwab R et al. Cancers. (Basel) 2021;13(12):3048.
14. Cohen-Kerem et al. Am J Surg. 2005;190(3):467-473.
Introduction: Tremendous Progress on Cancer Extends to Cancer in Pregnancy
The biomedical research enterprise that took shape in the United States after World War II has had numerous positive effects, including significant progress made during the past 75-plus years in the diagnosis, prevention, and treatment of cancer.
President Franklin D. Roosevelt’s 1944 request of Dr. Vannevar Bush, director of the then Office of Scientific Research and Development, to organize a program that would advance and apply scientific knowledge for times of peace — just as it been advanced and applied in times of war — culminated in a historic report, Science – The Endless Frontier. Presented in 1945 to President Harry S. Truman, this report helped fuel decades of broad, bold, and coordinated government-sponsored biomedical research aimed at addressing disease and improving the health of the American people (National Science Foundation, 1945).
Discoveries made from research in basic and translational sciences deepened our knowledge of the cellular and molecular underpinnings of cancer, leading to advances in chemotherapy, radiotherapy, and other treatment approaches as well as continual refinements in their application. Similarly, our diagnostic armamentarium has significantly improved.
As a result, we have reduced both the incidence and mortality of cancer. Today, some cancers can be prevented. Others can be reversed or put in remission. Granted, progress has been variable, with some cancers such as ovarian cancer still having relatively low survival rates. Much more needs to be done. Overall, however, the positive effects of the U.S. biomedical research enterprise on cancer are evident. According to the National Cancer Institute’s most recent report on the status of cancer, death rates from cancer fell 1.9% per year on average in females from 2015 to 2019 (Cancer. 2022 Oct 22. doi: 10.1002/cncr.34479).
It is not only patients whose cancer occurs outside of pregnancy who have benefited. When treatment is appropriately selected and timing considerations are made, patients whose cancer is diagnosed during pregnancy — and their children — can have good outcomes.
To explain how the management of cancer in pregnancy has improved, we have invited Gautam G. Rao, MD, gynecologic oncologist and associate professor of obstetrics, gynecology, and reproductive sciences at the University of Maryland School of Medicine, to write this installment of the Master Class in Obstetrics. As Dr. Rao explains, radiation is not as dangerous to the fetus as once thought, and the safety of many chemotherapeutic regimens in pregnancy has been documented. Obstetricians can and should counsel patients, he explains, about the likelihood of good maternal and fetal outcomes.
E. Albert Reece, MD, PhD, MBA, a maternal-fetal medicine specialist, is dean emeritus of the University of Maryland School of Medicine, former university executive vice president; currently the endowed professor and director of the Center for Advanced Research Training and Innovation (CARTI), and senior scientist in the Center for Birth Defects Research. Dr. Reece reported no relevant disclosures. He is the medical editor of this column. Contact him at obnews@mdedge.com.
Managing Cancer in Pregnancy
Cancer can cause fear and distress for any patient, but when cancer is diagnosed during pregnancy, an expectant mother fears not only for her own health but for the health of her unborn child. Fortunately, ob.gyn.s and multidisciplinary teams have good reason to reassure patients about the likelihood of good outcomes.
Cancer treatment in pregnancy has improved with advancements in imaging and chemotherapy, and while maternal and fetal outcomes of prenatal cancer treatment are not well reported, evidence acquired in recent years from case series and retrospective studies shows that most imaging studies and procedural diagnostic tests – and many treatments – can be performed safely in pregnancy.
Decades ago, we avoided CT scans during pregnancy because of concerns about radiation exposure to the fetus, leaving some patients without an accurate staging of their cancer. Today, we have evidence that a CT scan is generally safe in pregnancy. Similarly, the safety of many chemotherapeutic regimens in pregnancy has been documented in recent decades,and the use of chemotherapy during pregnancy has increased progressively. Radiation is also commonly utilized in the management of cancers that may occur during pregnancy, such as breast cancer.1
Considerations of timing are often central to decision-making; chemotherapy and radiotherapy are generally avoided in the first trimester to prevent structural fetal anomalies, for instance, and delaying cancer treatment is often warranted when the patient is a few weeks away from delivery. On occasion, iatrogenic preterm birth is considered when the risks to the mother of delaying a necessary cancer treatment outweigh the risks to the fetus of prematurity.1
Pregnancy termination is rarely indicated, however, and information gathered over the past 2 decades suggests that fetal and placental metastases are rare.1 There is broad agreement that prenatal treatment of cancer in pregnancy should adhere as much as possible to protocols and guidelines for nonpregnant patients and that treatment delays driven by fear of fetal anomalies and miscarriage are unnecessary.
Cancer Incidence, Use of Diagnostic Imaging
Data on the incidence of cancer in pregnancy comes from population-based cancer registries, and unfortunately, these data are not standardized and are often incomplete. Many studies include cancer diagnosed up to 1 year after pregnancy, and some include preinvasive disease. Estimates therefore vary considerably (see Table 1 for a sampling of estimates incidences.)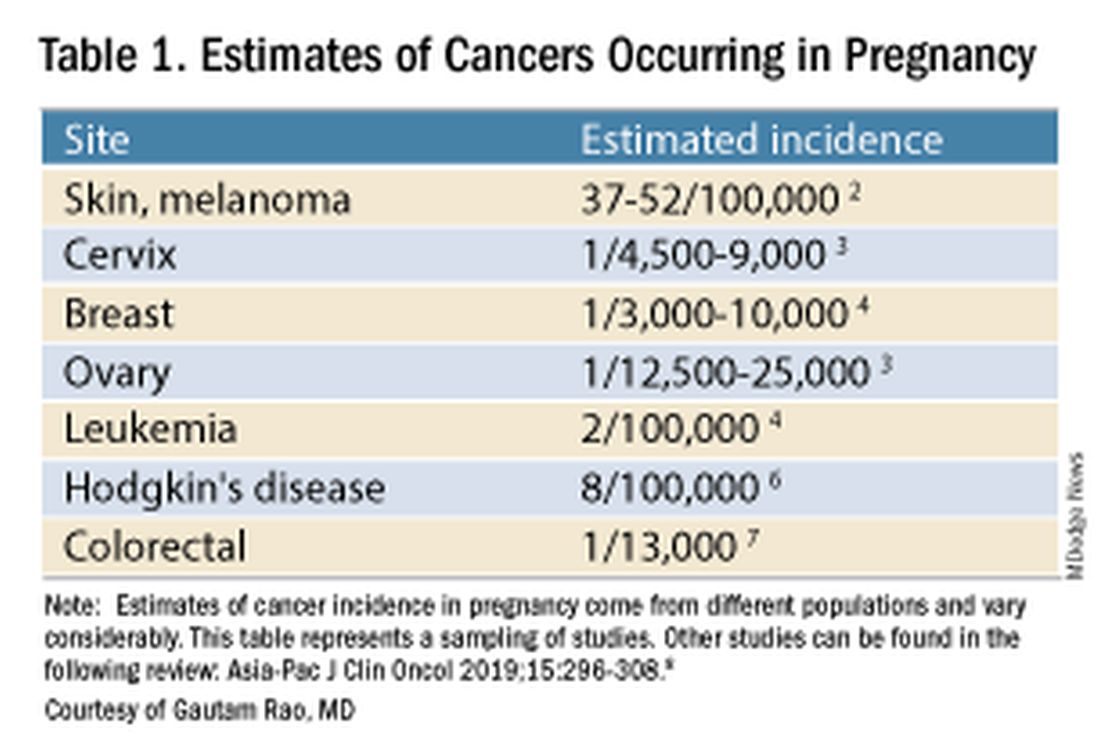
It has been reported, and often cited in the literature, that invasive malignancy complicates one in 1,000 pregnancies and that the incidence of cancer in pregnancy (invasive and noninvasive malignancies) has been rising over time.8 Increasing maternal age is believed to be playing a role in this rise; as women delay childbearing, they enter the age range in which some cancers become more common. Additionally, improvements in screening and diagnostics have led to earlier cancer detection. The incidence of ovarian neoplasms found during pregnancy has increased, for instance, with the routine use of diagnostic ultrasound in pregnancy.1
Among the studies showing an increased incidence of pregnancy-associated cancer is a population-based study in Australia, which found that from 1994 to 2007 the crude incidence of pregnancy-associated cancer increased from 112.3 to 191.5 per 100,000 pregnancies (P < .001).9 A cohort study in the United States documented an increase in incidence from 75.0 per 100,000 pregnancies in 2002 to 138.5 per 100,000 pregnancies in 2012.10
Overall, the literature shows us that the skin, cervix, and breast are also common sites for malignancy during pregnancy.1 According to a 2022 review, breast cancer during pregnancy is less often hormone receptor–positive and more frequently triple negative compared with age-matched controls.11 The frequencies of other pregnancy-associated cancers appear overall to be similar to that of cancer occurring in all women across their reproductive years.1
Too often, diagnosis is delayed because cancer symptoms can be masked by or can mimic normal physiological changes in pregnancy. For instance, breast cancer can be difficult to diagnose during pregnancy and lactation due to anatomic changes in the breast parenchyma. Several studies published in the 1990s showed that breast cancer presents at a more advanced stage in pregnant patients than in nonpregnant patients because of this delay.1 Skin changes suggestive of melanoma can be attributed to hyperpigmentation of pregnancy, for instance. Several observational studies have suggested that thicker melanomas found in pregnancy may be because of delayed diagnosis.8
It is important that we thoroughly investigate signs and symptoms suggestive of a malignancy and not automatically attribute these symptoms to the pregnancy itself. Cervical biopsy of a mass or lesion suspicious for cervical cancer can be done safely during pregnancy and should not be delayed or deferred.
Fetal radiation exposure from radiologic examinations has long been a concern, but we know today that while the imaging modality should be chosen to minimize fetal radiation exposure, CT scans and even PET scans should be performed if these exams are deemed best for evaluation. Embryonic exposure to a dose of less than 50 mGy is rarely if at all associated with fetal malformations or miscarriage and a radiation dose of 100 mGy may be considered a floor for consideration of therapeutic termination of pregnancy.1,8
CT exams are associated with a fetal dose far less than 50 mGy (see Table 2 for radiation doses).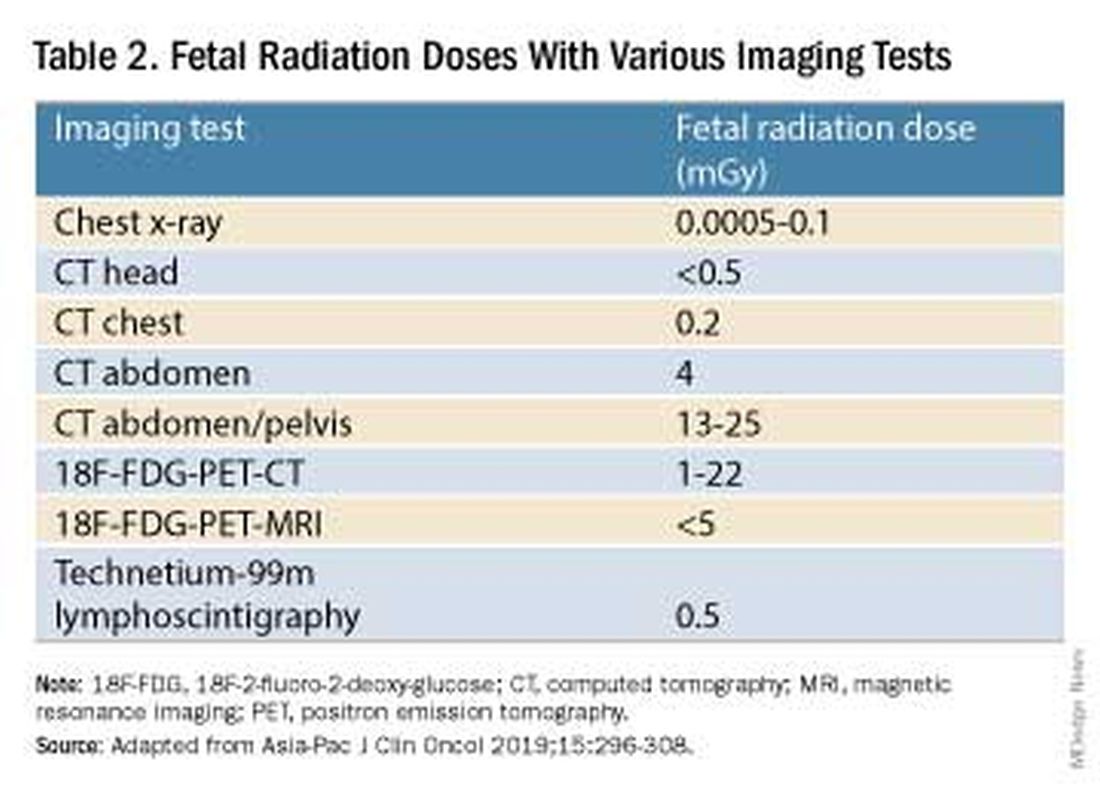
Magnetic resonance imaging with a magnet strength of 3 Tesla or less in any trimester is not associated with an increased risk of harm to the fetus or in early childhood, but the contrast agent gadolinium should be avoided in pregnancy as it has been associated with an increased risk of stillbirth, neonatal death, and childhood inflammatory, rheumatologic, and infiltrative skin lesions.1,8,12
Chemotherapy, Surgery, and Radiation in Pregnancy
The management of cancer during pregnancy requires a multidisciplinary team including medical, gynecologic, or radiation oncologists, and maternal-fetal medicine specialists (Figure 1). Prematurity and low birth weight are frequent complications for fetuses exposed to chemotherapy, although there is some uncertainty as to whether the treatment is causative. However, congenital anomalies no longer are a major concern, provided that drugs are appropriately selected and that fetal exposure occurs during the second or third trimester.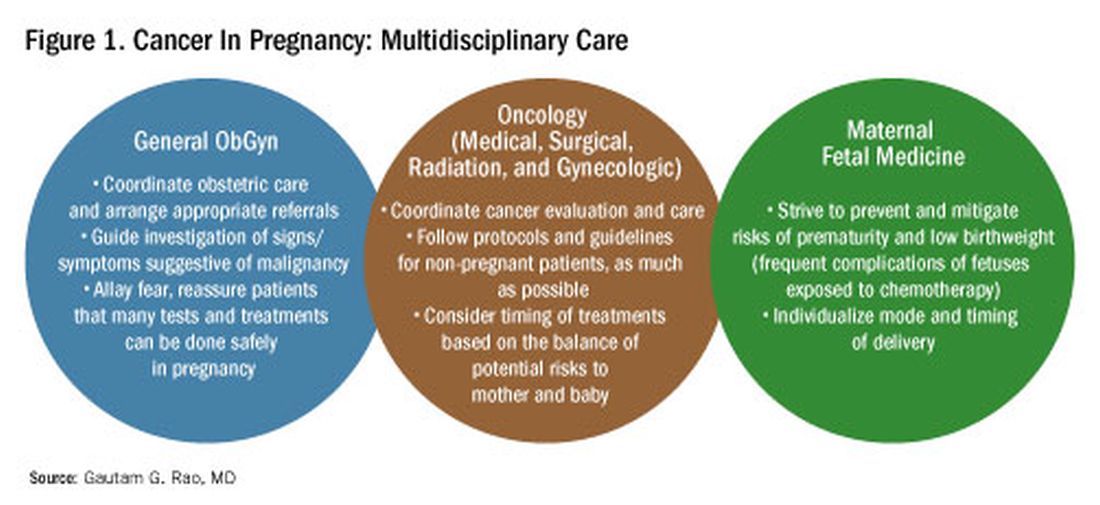
For instance, alkylating agents including cisplatin (an important drug in the management of gynecologic malignancies) have been associated with congenital anomalies in the first trimester but not in the second and third trimesters, and a variety of antimetabolites — excluding methotrexate and aminopterin — similarly have been shown to be relatively safe when used after the first trimester.1
Small studies have shown no long-term effects of chemotherapy exposure on postnatal growth and long-term neurologic/neurocognitive function,1 but this is an area that needs more research.
Also in need of investigation is the safety of newer agents in pregnancy. Data are limited on the use of new targeted treatments, monoclonal antibodies, and immunotherapies in pregnancy and their effects on the fetus, with current knowledge coming mainly from single case reports.13
Until more is learned — a challenge given that pregnant women are generally excluded from clinical trials — management teams are generally postponing use of these therapies until after delivery. Considering the pace of new developments revolutionizing cancer treatment, this topic will likely get more complex and confusing before we begin acquiring sufficient knowledge.
The timing of surgery for malignancy in pregnancy is similarly based on the balance of maternal and fetal risks, including the risk of maternal disease progression, the risk of preterm delivery, and the prevention of fetal metastases. In general, the safest time is the second trimester.
Maternal surgery in the third trimester may be associated with a risk of premature labor and altered uteroplacental perfusion. A 2005 systematic review of 12,452 women who underwent nonobstetric surgery during pregnancy provides some reassurance, however; compared with the general obstetric population, there was no increase in the rate of miscarriage or major birth defects.14
Radiotherapy used to be contraindicated in pregnancy but many experts today believe it can be safely utilized provided the uterus is out of field and is protected from scattered radiation. The head, neck, and breast, for instance, can be treated with newer radiotherapies, including stereotactic ablative radiation therapy.8 Patients with advanced cervical cancer often receive chemotherapy during pregnancy to slow metastatic growth followed by definitive treatment with postpartum radiation or surgery.
More research is needed, but available data on maternal outcomes are encouraging. For instance, there appear to be no significant differences in short- and long-term complications or survival between women who are pregnant and nonpregnant when treated for invasive cervical cancer.8 Similarly, while earlier studies of breast cancer diagnosed during pregnancy suggested a poor prognosis, data now show similar prognoses for pregnant and nonpregnant patients when controlled for stage.1
Dr. Rao is a gynecologic oncologist and associate professor of obstetrics, gynecology, and reproductive sciences at the University of Maryland School of Medicine, Baltimore. He reported no relevant disclosures.
References
1. Rao GG. Chapter 42. Clinical Obstetrics: The Fetus & Mother, 4th ed. Reece EA et al. (eds): 2021.
2. Bannister-Tyrrell M et al. Aust N Z J Obstet Gynaecol. 2014;55:116-122.
3. Oehler MK et al. Aust N Z J Obstet Gynaecol. 2003;43(6):414-420.
4. Ruiz R et al. Breast. 2017;35:136-141. doi: 10.1016/j.breast.2017.07.008.
5. Nolan S et al. Am J Obstet Gynecol. 2019;220(1):S480. doi: 10.1016/j.ajog.2018.11.752.
6. El-Messidi A et al. J Perinat Med. 2015;43(6):683-688. doi: 10.1515/jpm-2014-0133.
7. Pellino G et al. Eur J Gastroenterol Hepatol. 2017;29(7):743-753. doi: 10.1097/MEG.0000000000000863.
8. Eastwood-Wilshere N et al. Asia-Pac J Clin Oncol. 2019;15:296-308.
9. Lee YY et al. BJOG. 2012;119(13):1572-1582.
10. Cottreau CM et al. J Womens Health (Larchmt). 2019 Feb;28(2):250-257.
11. Boere I et al. Best Pract Res Clin Obstet Gynaecol. 2022;82:46-59.
12. Ray JG et al. JAMA 2016;316(9):952-961.
13. Schwab R et al. Cancers. (Basel) 2021;13(12):3048.
14. Cohen-Kerem et al. Am J Surg. 2005;190(3):467-473.
Introduction: Tremendous Progress on Cancer Extends to Cancer in Pregnancy
The biomedical research enterprise that took shape in the United States after World War II has had numerous positive effects, including significant progress made during the past 75-plus years in the diagnosis, prevention, and treatment of cancer.
President Franklin D. Roosevelt’s 1944 request of Dr. Vannevar Bush, director of the then Office of Scientific Research and Development, to organize a program that would advance and apply scientific knowledge for times of peace — just as it been advanced and applied in times of war — culminated in a historic report, Science – The Endless Frontier. Presented in 1945 to President Harry S. Truman, this report helped fuel decades of broad, bold, and coordinated government-sponsored biomedical research aimed at addressing disease and improving the health of the American people (National Science Foundation, 1945).
Discoveries made from research in basic and translational sciences deepened our knowledge of the cellular and molecular underpinnings of cancer, leading to advances in chemotherapy, radiotherapy, and other treatment approaches as well as continual refinements in their application. Similarly, our diagnostic armamentarium has significantly improved.
As a result, we have reduced both the incidence and mortality of cancer. Today, some cancers can be prevented. Others can be reversed or put in remission. Granted, progress has been variable, with some cancers such as ovarian cancer still having relatively low survival rates. Much more needs to be done. Overall, however, the positive effects of the U.S. biomedical research enterprise on cancer are evident. According to the National Cancer Institute’s most recent report on the status of cancer, death rates from cancer fell 1.9% per year on average in females from 2015 to 2019 (Cancer. 2022 Oct 22. doi: 10.1002/cncr.34479).
It is not only patients whose cancer occurs outside of pregnancy who have benefited. When treatment is appropriately selected and timing considerations are made, patients whose cancer is diagnosed during pregnancy — and their children — can have good outcomes.
To explain how the management of cancer in pregnancy has improved, we have invited Gautam G. Rao, MD, gynecologic oncologist and associate professor of obstetrics, gynecology, and reproductive sciences at the University of Maryland School of Medicine, to write this installment of the Master Class in Obstetrics. As Dr. Rao explains, radiation is not as dangerous to the fetus as once thought, and the safety of many chemotherapeutic regimens in pregnancy has been documented. Obstetricians can and should counsel patients, he explains, about the likelihood of good maternal and fetal outcomes.
E. Albert Reece, MD, PhD, MBA, a maternal-fetal medicine specialist, is dean emeritus of the University of Maryland School of Medicine, former university executive vice president; currently the endowed professor and director of the Center for Advanced Research Training and Innovation (CARTI), and senior scientist in the Center for Birth Defects Research. Dr. Reece reported no relevant disclosures. He is the medical editor of this column. Contact him at obnews@mdedge.com.
Managing Cancer in Pregnancy
Cancer can cause fear and distress for any patient, but when cancer is diagnosed during pregnancy, an expectant mother fears not only for her own health but for the health of her unborn child. Fortunately, ob.gyn.s and multidisciplinary teams have good reason to reassure patients about the likelihood of good outcomes.
Cancer treatment in pregnancy has improved with advancements in imaging and chemotherapy, and while maternal and fetal outcomes of prenatal cancer treatment are not well reported, evidence acquired in recent years from case series and retrospective studies shows that most imaging studies and procedural diagnostic tests – and many treatments – can be performed safely in pregnancy.
Decades ago, we avoided CT scans during pregnancy because of concerns about radiation exposure to the fetus, leaving some patients without an accurate staging of their cancer. Today, we have evidence that a CT scan is generally safe in pregnancy. Similarly, the safety of many chemotherapeutic regimens in pregnancy has been documented in recent decades,and the use of chemotherapy during pregnancy has increased progressively. Radiation is also commonly utilized in the management of cancers that may occur during pregnancy, such as breast cancer.1
Considerations of timing are often central to decision-making; chemotherapy and radiotherapy are generally avoided in the first trimester to prevent structural fetal anomalies, for instance, and delaying cancer treatment is often warranted when the patient is a few weeks away from delivery. On occasion, iatrogenic preterm birth is considered when the risks to the mother of delaying a necessary cancer treatment outweigh the risks to the fetus of prematurity.1
Pregnancy termination is rarely indicated, however, and information gathered over the past 2 decades suggests that fetal and placental metastases are rare.1 There is broad agreement that prenatal treatment of cancer in pregnancy should adhere as much as possible to protocols and guidelines for nonpregnant patients and that treatment delays driven by fear of fetal anomalies and miscarriage are unnecessary.
Cancer Incidence, Use of Diagnostic Imaging
Data on the incidence of cancer in pregnancy comes from population-based cancer registries, and unfortunately, these data are not standardized and are often incomplete. Many studies include cancer diagnosed up to 1 year after pregnancy, and some include preinvasive disease. Estimates therefore vary considerably (see Table 1 for a sampling of estimates incidences.)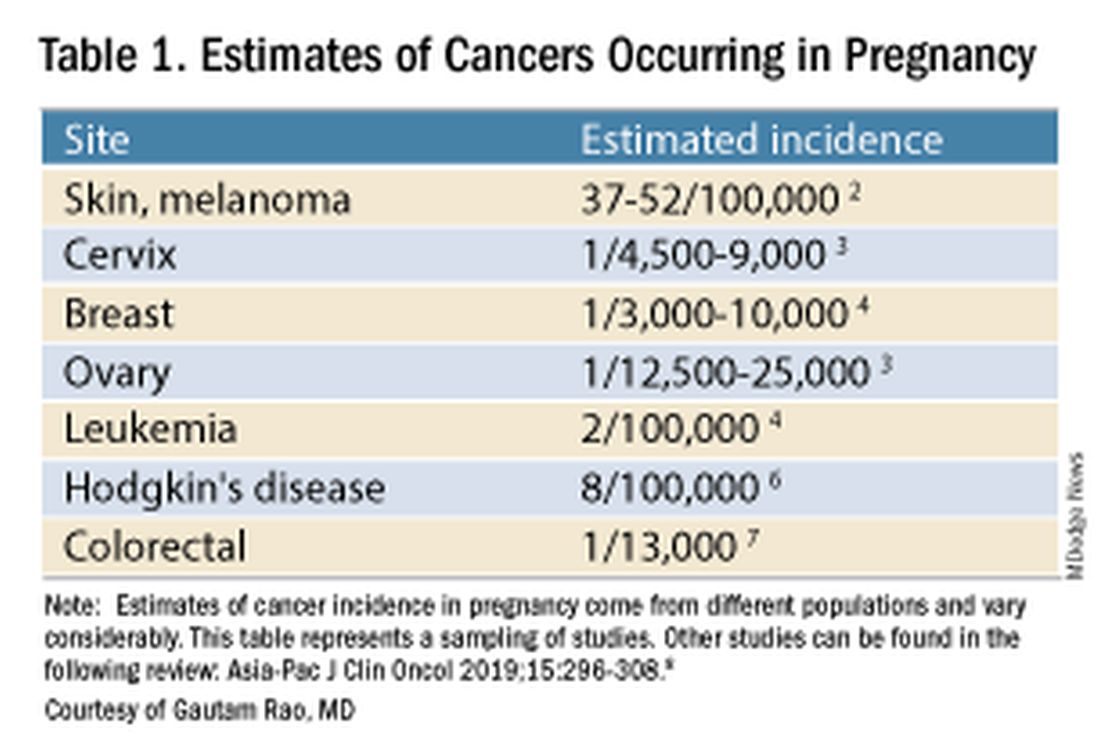
It has been reported, and often cited in the literature, that invasive malignancy complicates one in 1,000 pregnancies and that the incidence of cancer in pregnancy (invasive and noninvasive malignancies) has been rising over time.8 Increasing maternal age is believed to be playing a role in this rise; as women delay childbearing, they enter the age range in which some cancers become more common. Additionally, improvements in screening and diagnostics have led to earlier cancer detection. The incidence of ovarian neoplasms found during pregnancy has increased, for instance, with the routine use of diagnostic ultrasound in pregnancy.1
Among the studies showing an increased incidence of pregnancy-associated cancer is a population-based study in Australia, which found that from 1994 to 2007 the crude incidence of pregnancy-associated cancer increased from 112.3 to 191.5 per 100,000 pregnancies (P < .001).9 A cohort study in the United States documented an increase in incidence from 75.0 per 100,000 pregnancies in 2002 to 138.5 per 100,000 pregnancies in 2012.10
Overall, the literature shows us that the skin, cervix, and breast are also common sites for malignancy during pregnancy.1 According to a 2022 review, breast cancer during pregnancy is less often hormone receptor–positive and more frequently triple negative compared with age-matched controls.11 The frequencies of other pregnancy-associated cancers appear overall to be similar to that of cancer occurring in all women across their reproductive years.1
Too often, diagnosis is delayed because cancer symptoms can be masked by or can mimic normal physiological changes in pregnancy. For instance, breast cancer can be difficult to diagnose during pregnancy and lactation due to anatomic changes in the breast parenchyma. Several studies published in the 1990s showed that breast cancer presents at a more advanced stage in pregnant patients than in nonpregnant patients because of this delay.1 Skin changes suggestive of melanoma can be attributed to hyperpigmentation of pregnancy, for instance. Several observational studies have suggested that thicker melanomas found in pregnancy may be because of delayed diagnosis.8
It is important that we thoroughly investigate signs and symptoms suggestive of a malignancy and not automatically attribute these symptoms to the pregnancy itself. Cervical biopsy of a mass or lesion suspicious for cervical cancer can be done safely during pregnancy and should not be delayed or deferred.
Fetal radiation exposure from radiologic examinations has long been a concern, but we know today that while the imaging modality should be chosen to minimize fetal radiation exposure, CT scans and even PET scans should be performed if these exams are deemed best for evaluation. Embryonic exposure to a dose of less than 50 mGy is rarely if at all associated with fetal malformations or miscarriage and a radiation dose of 100 mGy may be considered a floor for consideration of therapeutic termination of pregnancy.1,8
CT exams are associated with a fetal dose far less than 50 mGy (see Table 2 for radiation doses).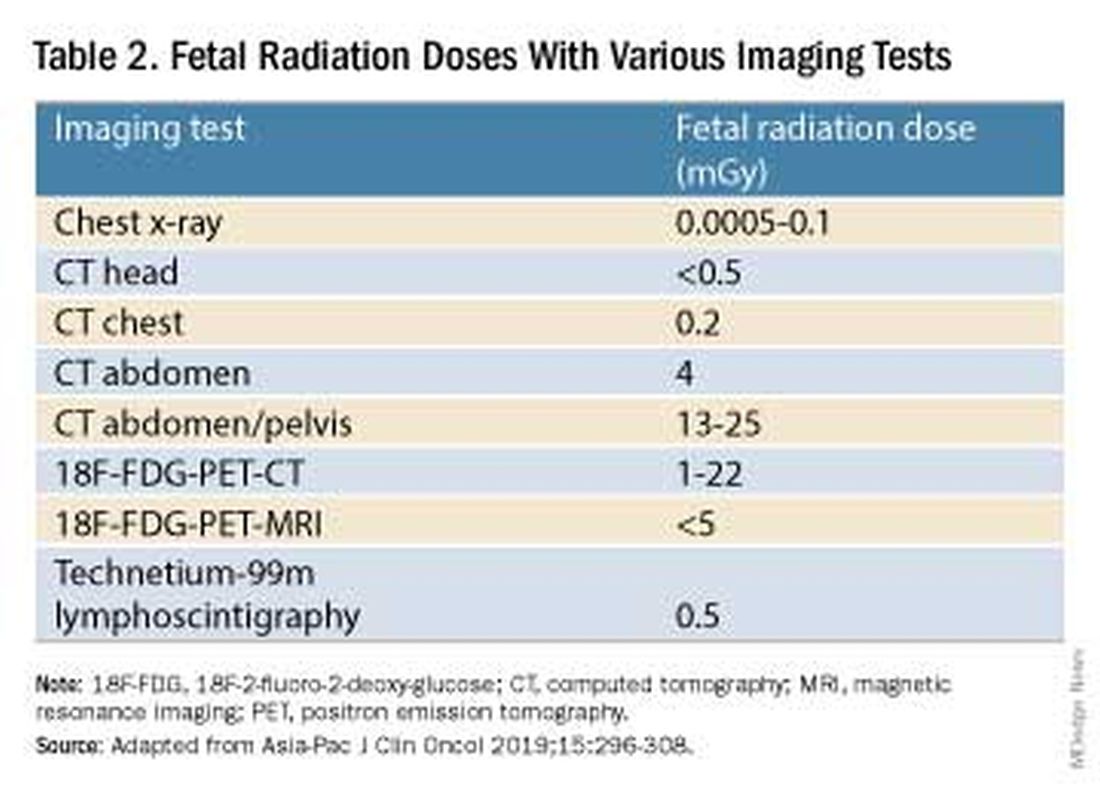
Magnetic resonance imaging with a magnet strength of 3 Tesla or less in any trimester is not associated with an increased risk of harm to the fetus or in early childhood, but the contrast agent gadolinium should be avoided in pregnancy as it has been associated with an increased risk of stillbirth, neonatal death, and childhood inflammatory, rheumatologic, and infiltrative skin lesions.1,8,12
Chemotherapy, Surgery, and Radiation in Pregnancy
The management of cancer during pregnancy requires a multidisciplinary team including medical, gynecologic, or radiation oncologists, and maternal-fetal medicine specialists (Figure 1). Prematurity and low birth weight are frequent complications for fetuses exposed to chemotherapy, although there is some uncertainty as to whether the treatment is causative. However, congenital anomalies no longer are a major concern, provided that drugs are appropriately selected and that fetal exposure occurs during the second or third trimester.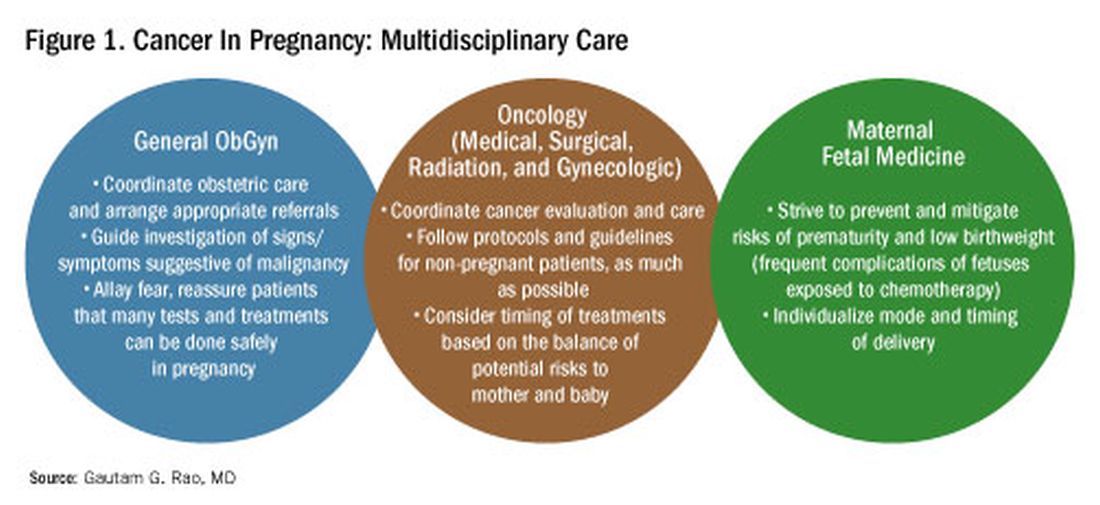
For instance, alkylating agents including cisplatin (an important drug in the management of gynecologic malignancies) have been associated with congenital anomalies in the first trimester but not in the second and third trimesters, and a variety of antimetabolites — excluding methotrexate and aminopterin — similarly have been shown to be relatively safe when used after the first trimester.1
Small studies have shown no long-term effects of chemotherapy exposure on postnatal growth and long-term neurologic/neurocognitive function,1 but this is an area that needs more research.
Also in need of investigation is the safety of newer agents in pregnancy. Data are limited on the use of new targeted treatments, monoclonal antibodies, and immunotherapies in pregnancy and their effects on the fetus, with current knowledge coming mainly from single case reports.13
Until more is learned — a challenge given that pregnant women are generally excluded from clinical trials — management teams are generally postponing use of these therapies until after delivery. Considering the pace of new developments revolutionizing cancer treatment, this topic will likely get more complex and confusing before we begin acquiring sufficient knowledge.
The timing of surgery for malignancy in pregnancy is similarly based on the balance of maternal and fetal risks, including the risk of maternal disease progression, the risk of preterm delivery, and the prevention of fetal metastases. In general, the safest time is the second trimester.
Maternal surgery in the third trimester may be associated with a risk of premature labor and altered uteroplacental perfusion. A 2005 systematic review of 12,452 women who underwent nonobstetric surgery during pregnancy provides some reassurance, however; compared with the general obstetric population, there was no increase in the rate of miscarriage or major birth defects.14
Radiotherapy used to be contraindicated in pregnancy but many experts today believe it can be safely utilized provided the uterus is out of field and is protected from scattered radiation. The head, neck, and breast, for instance, can be treated with newer radiotherapies, including stereotactic ablative radiation therapy.8 Patients with advanced cervical cancer often receive chemotherapy during pregnancy to slow metastatic growth followed by definitive treatment with postpartum radiation or surgery.
More research is needed, but available data on maternal outcomes are encouraging. For instance, there appear to be no significant differences in short- and long-term complications or survival between women who are pregnant and nonpregnant when treated for invasive cervical cancer.8 Similarly, while earlier studies of breast cancer diagnosed during pregnancy suggested a poor prognosis, data now show similar prognoses for pregnant and nonpregnant patients when controlled for stage.1
Dr. Rao is a gynecologic oncologist and associate professor of obstetrics, gynecology, and reproductive sciences at the University of Maryland School of Medicine, Baltimore. He reported no relevant disclosures.
References
1. Rao GG. Chapter 42. Clinical Obstetrics: The Fetus & Mother, 4th ed. Reece EA et al. (eds): 2021.
2. Bannister-Tyrrell M et al. Aust N Z J Obstet Gynaecol. 2014;55:116-122.
3. Oehler MK et al. Aust N Z J Obstet Gynaecol. 2003;43(6):414-420.
4. Ruiz R et al. Breast. 2017;35:136-141. doi: 10.1016/j.breast.2017.07.008.
5. Nolan S et al. Am J Obstet Gynecol. 2019;220(1):S480. doi: 10.1016/j.ajog.2018.11.752.
6. El-Messidi A et al. J Perinat Med. 2015;43(6):683-688. doi: 10.1515/jpm-2014-0133.
7. Pellino G et al. Eur J Gastroenterol Hepatol. 2017;29(7):743-753. doi: 10.1097/MEG.0000000000000863.
8. Eastwood-Wilshere N et al. Asia-Pac J Clin Oncol. 2019;15:296-308.
9. Lee YY et al. BJOG. 2012;119(13):1572-1582.
10. Cottreau CM et al. J Womens Health (Larchmt). 2019 Feb;28(2):250-257.
11. Boere I et al. Best Pract Res Clin Obstet Gynaecol. 2022;82:46-59.
12. Ray JG et al. JAMA 2016;316(9):952-961.
13. Schwab R et al. Cancers. (Basel) 2021;13(12):3048.
14. Cohen-Kerem et al. Am J Surg. 2005;190(3):467-473.
Genetics and Lifestyle Choices Can Affect Early Prostate Cancer Deaths
TOPLINE:
METHODOLOGY:
- About one third of men die from prostate cancer before age 75, highlighting the need for prevention strategies that target high-risk populations.
- In the current study, researchers analyzed data from two prospective cohort studies — the Malmö Diet and Cancer Study (MDCS) and the Health Professionals Follow-Up Study (HPFS) — which included 19,607 men with a median age at inclusion of 59 years (MDCS) and 65.1 years (HPFS) followed from 1991 to 2019.
- Participants were categorized by genetic risk and lifestyle score. Genetic risk was defined using a multiancestry polygenic risk score (PRS) for overall prostate cancer that included 400 genetic risk variants.
- A healthy lifestyle score was defined as 3-6, while an unhealthy lifestyle score was 0-2. Lifestyle factors included smoking, weight, physical activity, and diet.
- The researchers calculated hazard ratios (HRs) for the association between genetic and lifestyle factors and prostate cancer death.
TAKEAWAY:
- Combining the PRS and family history of cancer, 67% of men overall (13,186 of 19,607) were considered to have higher genetic risk, and about 30% overall had an unhealthy lifestyle score of 0-2.
- Men at higher genetic risk accounted for 88% (94 of 107) of early prostate cancer deaths.
- Compared with men at lower genetic risk, those at higher genetic risk had more than a threefold higher rate of early prostate cancer death (HR, 3.26) and more than a twofold increased rate of late prostate cancer death (HR, 2.26) as well as a higher lifetime risk for prostate cancer death.
- Among men at higher genetic risk, an unhealthy lifestyle was associated with a higher risk of early prostate cancer death, with smoking and a BMI of ≥ 30 being significant factors. Depending on the definition of a healthy lifestyle, the researchers estimated that 22%-36% of early prostate cancer deaths among men at higher genetic risk might be preventable.
IN PRACTICE:
“Based on data from two prospective cohort studies, this analysis provides evidence for targeting men at increased genetic risk with prevention strategies aimed at reducing premature deaths from prostate cancer,” the researchers concluded.
SOURCE:
The study, with first author Anna Plym, PhD, Department of Medical Epidemiology and Biostatistics, Karolinska Institutet in Stockholm, Sweden, was published online on July 3 in JAMA Network Open.
LIMITATIONS:
Differences in prostate cancer testing and treatment may account for some of the observed association between a healthy lifestyle and prostate cancer death. This analysis provides an estimate of what is achievable in terms of prevention had everyone adopted a healthy lifestyle. The authors only considered factors at study entry, which would not include changes that happen later.
DISCLOSURES:
The study authors reported several disclosures. Fredrik Wiklund, PhD, received grants from GE Healthcare, personal fees from Janssen, Varian Medical Systems, and WebMD, and stock options and personal fees from Cortechs Labs outside the submitted work. Adam S. Kibel, MD, received personal fees from Janssen, Pfizer, Bristol Myers Squibb, Cellvax, Merck, and Roche and served as a consultant for Bristol Myers Squibb and Candel outside the submitted work. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- About one third of men die from prostate cancer before age 75, highlighting the need for prevention strategies that target high-risk populations.
- In the current study, researchers analyzed data from two prospective cohort studies — the Malmö Diet and Cancer Study (MDCS) and the Health Professionals Follow-Up Study (HPFS) — which included 19,607 men with a median age at inclusion of 59 years (MDCS) and 65.1 years (HPFS) followed from 1991 to 2019.
- Participants were categorized by genetic risk and lifestyle score. Genetic risk was defined using a multiancestry polygenic risk score (PRS) for overall prostate cancer that included 400 genetic risk variants.
- A healthy lifestyle score was defined as 3-6, while an unhealthy lifestyle score was 0-2. Lifestyle factors included smoking, weight, physical activity, and diet.
- The researchers calculated hazard ratios (HRs) for the association between genetic and lifestyle factors and prostate cancer death.
TAKEAWAY:
- Combining the PRS and family history of cancer, 67% of men overall (13,186 of 19,607) were considered to have higher genetic risk, and about 30% overall had an unhealthy lifestyle score of 0-2.
- Men at higher genetic risk accounted for 88% (94 of 107) of early prostate cancer deaths.
- Compared with men at lower genetic risk, those at higher genetic risk had more than a threefold higher rate of early prostate cancer death (HR, 3.26) and more than a twofold increased rate of late prostate cancer death (HR, 2.26) as well as a higher lifetime risk for prostate cancer death.
- Among men at higher genetic risk, an unhealthy lifestyle was associated with a higher risk of early prostate cancer death, with smoking and a BMI of ≥ 30 being significant factors. Depending on the definition of a healthy lifestyle, the researchers estimated that 22%-36% of early prostate cancer deaths among men at higher genetic risk might be preventable.
IN PRACTICE:
“Based on data from two prospective cohort studies, this analysis provides evidence for targeting men at increased genetic risk with prevention strategies aimed at reducing premature deaths from prostate cancer,” the researchers concluded.
SOURCE:
The study, with first author Anna Plym, PhD, Department of Medical Epidemiology and Biostatistics, Karolinska Institutet in Stockholm, Sweden, was published online on July 3 in JAMA Network Open.
LIMITATIONS:
Differences in prostate cancer testing and treatment may account for some of the observed association between a healthy lifestyle and prostate cancer death. This analysis provides an estimate of what is achievable in terms of prevention had everyone adopted a healthy lifestyle. The authors only considered factors at study entry, which would not include changes that happen later.
DISCLOSURES:
The study authors reported several disclosures. Fredrik Wiklund, PhD, received grants from GE Healthcare, personal fees from Janssen, Varian Medical Systems, and WebMD, and stock options and personal fees from Cortechs Labs outside the submitted work. Adam S. Kibel, MD, received personal fees from Janssen, Pfizer, Bristol Myers Squibb, Cellvax, Merck, and Roche and served as a consultant for Bristol Myers Squibb and Candel outside the submitted work. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- About one third of men die from prostate cancer before age 75, highlighting the need for prevention strategies that target high-risk populations.
- In the current study, researchers analyzed data from two prospective cohort studies — the Malmö Diet and Cancer Study (MDCS) and the Health Professionals Follow-Up Study (HPFS) — which included 19,607 men with a median age at inclusion of 59 years (MDCS) and 65.1 years (HPFS) followed from 1991 to 2019.
- Participants were categorized by genetic risk and lifestyle score. Genetic risk was defined using a multiancestry polygenic risk score (PRS) for overall prostate cancer that included 400 genetic risk variants.
- A healthy lifestyle score was defined as 3-6, while an unhealthy lifestyle score was 0-2. Lifestyle factors included smoking, weight, physical activity, and diet.
- The researchers calculated hazard ratios (HRs) for the association between genetic and lifestyle factors and prostate cancer death.
TAKEAWAY:
- Combining the PRS and family history of cancer, 67% of men overall (13,186 of 19,607) were considered to have higher genetic risk, and about 30% overall had an unhealthy lifestyle score of 0-2.
- Men at higher genetic risk accounted for 88% (94 of 107) of early prostate cancer deaths.
- Compared with men at lower genetic risk, those at higher genetic risk had more than a threefold higher rate of early prostate cancer death (HR, 3.26) and more than a twofold increased rate of late prostate cancer death (HR, 2.26) as well as a higher lifetime risk for prostate cancer death.
- Among men at higher genetic risk, an unhealthy lifestyle was associated with a higher risk of early prostate cancer death, with smoking and a BMI of ≥ 30 being significant factors. Depending on the definition of a healthy lifestyle, the researchers estimated that 22%-36% of early prostate cancer deaths among men at higher genetic risk might be preventable.
IN PRACTICE:
“Based on data from two prospective cohort studies, this analysis provides evidence for targeting men at increased genetic risk with prevention strategies aimed at reducing premature deaths from prostate cancer,” the researchers concluded.
SOURCE:
The study, with first author Anna Plym, PhD, Department of Medical Epidemiology and Biostatistics, Karolinska Institutet in Stockholm, Sweden, was published online on July 3 in JAMA Network Open.
LIMITATIONS:
Differences in prostate cancer testing and treatment may account for some of the observed association between a healthy lifestyle and prostate cancer death. This analysis provides an estimate of what is achievable in terms of prevention had everyone adopted a healthy lifestyle. The authors only considered factors at study entry, which would not include changes that happen later.
DISCLOSURES:
The study authors reported several disclosures. Fredrik Wiklund, PhD, received grants from GE Healthcare, personal fees from Janssen, Varian Medical Systems, and WebMD, and stock options and personal fees from Cortechs Labs outside the submitted work. Adam S. Kibel, MD, received personal fees from Janssen, Pfizer, Bristol Myers Squibb, Cellvax, Merck, and Roche and served as a consultant for Bristol Myers Squibb and Candel outside the submitted work. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.




