User login
Stalked by a ‘patient’
CASE: Delusions and threats
For over 20 months, Ms. I, age 48, sends a psychiatric resident letters and postcards that total approximately 3,000 pages and come from dozens of return addresses. Ms. I expresses romantic feelings toward the resident and believes that he was her physician and prescribed medications, including “mood stabilizers.” The resident never treated Ms. I; to his knowledge, he has never interacted with her.
Ms. I describes the resident’s refusal to continue treating her as “abandonment” and states that she is contemplating self-harm because of this rejection. In her letters, Ms. I admits that she was a long-term patient in a state psychiatric hospital in her home state and suffers from persistent auditory hallucinations. She also wants a romantic relationship with the resident and repeatedly threatens the resident’s female acquaintances and former romantic partners whose relationships she had surmised from news articles available on the Internet. Ms. I also threatens to strangle the resident. The resident sends her multiple written requests that she cease contact, but they are not acknowledged.
The authors’ observations
Stalking—repeated, unwanted attention or communication that would cause a reasonable person fear—is a serious threat for many psychiatric clinicians.1 Prevalence rates among mental health care providers range from 3% to 21%.2,3 Most stalkers have engaged in previous stalking behavior.3
Being stalked is highly distressing,4 and mental health professionals often do not reveal such experiences to colleagues.5 Irrational feelings of guilt or embarrassment, such as being thought to have poorly managed interactions with the stalker, often motivate a self-imposed silence (Table 1).6 This isolation may foster anxiety, interfere with receiving problem-solving advice, and increase physical vulnerability. In the case involving Ms. I, the psychiatric resident’s primary responsibility is safeguarding his own physical and psychological welfare.
Clinicians who work in a hospital or other institutional setting who are being stalked should inform their supervisors and the facility’s security personnel. Security personnel may be able to gather data about the stalker, decrease the stalker’s ability to communicate with the victim, and reduce unwanted physical access to the victim by distributing a photo of the stalker or installing a camera or receptionist-controlled door lock in patient entryways. Security personnel also may collaborate with local law enforcement. Having a third party respond to a stalker’s aggressive behavior—rather than the victim responding directly—avoids rewarding the stalker, which may generate further unwanted contact.7 Any intervention by the victim may increase the risk of violence, creating an “intervention dilemma.” Resnick8 argues that before deciding how best to address the stalker’s behavior, a stalking victim must “first separate the risk of continued stalking from the risk that the stalker will commit a violent act.”
Mental health professionals in private practice who are being stalked should consider retaining an attorney. An attorney often can maintain privacy of communications regarding the stalker via the attorney-client and attorney-work product privileges, which may help during legal proceedings.
Table 1
Factors that can impede psychiatrists from reporting stalking
| Fear of being perceived as a failure |
| Embarrassment |
| High professional tolerance for antisocial and threatening behavior |
| Misplaced sense of duty |
| Source: Reference 6 |
RESPONSE: Involving police
Over 2 months, Ms. I phones the resident’s home 105 times (the resident screens the calls). During 1 call, she states that she is hidden in a closet in her home and will hurt herself unless the resident “resumes” her psychiatric care. The resident contacts police in his city and Ms. I’s community, but authorities are reluctant to act when he acknowledges that he is not Ms. I’s psychiatrist and does not know her. Police officers in Ms. I’s hometown tell the resident no one answered the door when they visited her home. They state that they would enter the residence forcibly only if Ms. I’s physician or a family member asked them to do so, and because the resident admits that he is not her psychiatrist, they cannot take further action. Ms. I leaves the resident a phone message several hours later to inform him she is safe.
The authors’ observations
Stalking-induced countertransference responses may lead a psychiatrist to unwittingly place himself in harm’s way. For example, intense rage at a stalker’s request for treatment may generate guilt that motivates the psychiatrist to agree to treat the stalker. Feelings of helplessness may produce a frantic desire to do something even when such activity is ill-advised. Psychiatrists may develop a tolerance for antisocial or threatening behavior—which is common in mental health settings—and could accept unnecessary risks.
A psychiatrist who is being stalked may be able to assist a mentally ill stalker in a way that does not create a duty to treat and does not expose the psychiatrist to harm, such as contacting a mobile crisis intervention team, a mental health professional who recently treated the stalker, a family member of the stalker, or law enforcement personnel. A psychiatrist who is thrust from the role of helper to victim and must protect his or her own well-being instead of attending to a patient’s welfare is prone to suffer substantial countertransference distress.
The situation with Ms. I was particularly challenging because the resident did not know her complete history and therefore had little information to gauge how likely she was to act on her aggressive threats. Factors that predict future violence include:
- a history of violence
- significant prior criminality
- young age at first arrest
- concomitant substance abuse
- male sex.9
Unfortunately, other than sex, this data regarding Ms. I could not be readily obtained.
A psychiatrist’s duty
Although sympathetic to his stalker’s distress, the resident did not want to treat this woman, nor was he ethically or legally obligated to do so. An individual’s wish to be treated by a particular psychiatrist does not create a duty for the psychiatrist to satisfy this wish.10 State-based “Good Samaritan” laws encourage physicians to assist those in acute need by shielding them from liability, as long as they reasonably act within the scope of their expertise.11 However, they do not require a physician to care for an individual in acute need. A delusional wish for treatment or a false belief of already being in treatment does not create a duty to care for a person.
OUTCOME: Seeking help
Ms. I’s phone calls and letters continue. The resident discusses the situation with his associate residency director, who refers him to the hospital’s legal and investigative staffs. Based on advice from the hospital’s private investigator, the resident sends Ms. I a formal “cease and desist” letter that threatens her with legal action and possible jail time. The staff at the front desk of the clinic where the resident works and the hospital’s security department are instructed to watch for a visitor with Ms. I’s name and description, although the hospital’s investigator is unable to obtain a photograph of her. Shortly after the resident sends the letter, Ms. I ceases communication.
The authors’ observations
This case is unusual because most stalking victims know their stalkers. Identifying a stalker’s motivation can be helpful in formulating a risk assessment. One classification system recognizes 5 categories of stalkers: rejected, intimacy seeking, incompetent, resentful, and predatory (Table 2).1 Rejected stalkers appear to pose the greatest risk of violence and homicide.8 However, all stalkers may pose a risk of violence and therefore all stalking behavior should be treated seriously.
Table 2
Classification of stalkers
| Category | Common features |
|---|---|
| Rejected | Most have a personality disorder; often seeking reconciliation and revenge; most frequent victims are ex-romantic partners, but also target estranged relatives, former friends |
| Intimacy seeking | Erotomania; “morbid infatuation” |
| Incompetent | Lacking social skills; often have stalked others |
| Resentful | Pursuing a vendetta; generally feeling aggrieved |
| Predatory | Often comorbid with paraphilias; may have past convictions for sex offenses |
| Source: Adapted from reference 1 | |
Responding to a stalker
The approach should be tailored to the stalker’s characteristics.12 Silence—ie, lack of acknowledgement of a stalker’s intrusions—is one tactic.13 Consistent and persistent lack of engagement may bore the stalker, but also may provoke frustration or narcissistic or paranoia-fueled rage, and increased efforts to interact with the mental health professional. Other responses include:
- obtaining a protection or restraining order
- promoting the stalker’s participation in adversarial civil litigation, such as a lawsuit
- issuing verbal counterthreats.
Restraining orders are controversial and assessments of their effectiveness vary.14 How well a restraining order works may depend on the stalker’s:
- ability to appreciate reality, and how likely he or she is to experience anxiety when confronted with adverse consequences of his or her actions
- how consistently, rapidly, and harshly the criminal justice system responds to violations of restraining orders.
Restraining orders also may provide the victim a false sense of security.15 One of her letters revealed that Ms. I violated a criminal plea arrangement years earlier, which suggests she was capable of violating a restraining order.
Litigation. A stalker may initiate civil litigation against the victim to feel that he or she has an impact on the victim, which may reduce the stalker’s risk of violence if he or she is emotionally engaged in the litigation. Based on the authors’ experience, as long as the stalker is talking, he or she generally is less likely to act out violently and terminate a satisfying process. Adversarial civil litigation could give a stalker the opportunity to be “close” to the victim and a means of expressing aggressive wishes. The benefit of litigation lasts only as long as the case persists and the stalker believes he or she may prevail. In one of her letters, Ms. I bragged that she had represented herself as a pro se litigant in a complex civil matter, suggesting that she might be constructively channeled into litigation.
Promoting litigation carries significant risk.16 Being a defendant in pro se litigation may be emotionally and financially stressful. This approach may be desirable if the psychiatrist’s institution is willing to offer substantial support. For example, an institution may provide legal assistance—including helping to defray the cost of litigation—and litigation-related scheduling flexibility. An attorney may serve as a boundary between the victim and the pro se litigant’s sometimes ceaseless, time-devouring, anxiety-inducing legal maneuvers.
Counterthreats. Warning a stalker that he or she will face severe civil and criminal consequences if his or her behavior continues can make clear that his or her conduct is unacceptable.17 Such warnings may be delivered verbally or in writing by a legal representative, law enforcement personnel, a private security agent, or the victim.
Issuing a counterthreat can be risky. Stalkers with antisocial or narcissistic personality features may perceive a counterthreat as narcissistically diminishing, and to save face will escalate their stalking in retaliation. Avoid counterthreats if you believe the stalker might be psychotic because destabilizing such an individual—such as by precipitating a short psychotic episode—may increase unpredictability and diminish their responsive to interventions.
Ms. I’s contact with the resident lasted approximately 20 months, slightly less than the average 26 months reported in a survey of mental health professionals.3 Because stalkers are unpredictable, the psychiatric resident remains cautious.
Related Resources
- National Center for Victims of Crime. Stalking resource center. www.victimsofcrime.org/our-programs/stalking-resource-center.
- Mullen PE, Pathé M, Purcell R. Stalkers and their victims. New York, NY: Cambridge University Press; 2009.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Mullen PE, Pathé M, Purcell R, et al. Study of stalkers. Am J Psychiatry. 1999;156(8):1244-1249.
2. Sandberg DA, McNiel DE, Binder RL. Stalking threatening, and harassing behavior by psychiatric patients toward clinicians. J Am Acad Psychiatry Law. 2002;30(2):221-229.
3. McIvor R, Potter L, Davies L. Stalking behavior by patients towards psychiatrists in a large mental health organization. Int J Soc Psychiatry. 2008;54(4):350-357.
4. Mullen PE, Pathé M. Stalking. Crime and Justice. 2002;29:273-318.
5. Bird S. Strategies for managing and minimizing the impact of harassment and stalking by patients. ANZ J Surg. 2009;79(7-8):537-538.
6. Sinwelski SA, Vinton L. Stalking: the constant threat of violence. Affilia. 2001;16(1):46-65.
7. Meloy JR. Commentary: stalking threatening, and harassing behavior by patients—the risk-management response. J Am Acad Psychiatry Law. 2002;30(2):230-231.
8. Resnick PJ. Stalking risk assessment. In: Pinals DA, ed. Stalking: psychiatric perspectives and practical approaches. New York, NY: Oxford University Press; 2007:61–84.
9. Dietz PE. Defenses against dangerous people when arrest and commitment fail. In: Simon RI, ed. American Psychiatric Press review of clinical psychiatry and the law. 1st ed. Washington, DC: American Psychiatric Press; 1989:205–219.
10. Hilliard J. Termination of treatment with troublesome patients. In: Lifson LE, Simon RI, eds. The mental health practitioner and the law: a comprehensive handbook. Cambridge, MA: Harvard University Press; 1998:216–224.
11. Paterick TJ, Paterick BB, Paterick TE. Implications of Good Samaritan laws for physicians. J Med Pract Manage. 2008;23(6):372-375.
12. MacKenzie RD, James DV. Management and treatment of stalkers: problems options, and solutions. Behav Sci Law. 2011;29(2):220-239.
13. Fremouw WJ, Westrup D, Pennypacker J. Stalking on campus: the prevalence and strategies for coping with stalking. J Forensic Sci. 1997;42(4):666-669.
14. Nicastro AM, Cousins AV, Spitzberg BH. The tactical face of stalking. Journal of Criminal Justice. 2000;28(1):69-82.
15. Spitzberg BH. The tactical topography of stalking victimization and management. Trauma Violence Abuse. 2002;3(4):261-288.
16. Pathé M, MacKenzie R, Mullen PE. Stalking by law: damaging victims and rewarding offenders. J Law Med. 2004;12(1):103-111.
17. Lion JR, Herschler JA. The stalking of physicians by their patients. In: Meloy JR. The psychology of stalking: clinical and forensic perspectives. San Diego, CA: Academic Press; 1998:163–173.
CASE: Delusions and threats
For over 20 months, Ms. I, age 48, sends a psychiatric resident letters and postcards that total approximately 3,000 pages and come from dozens of return addresses. Ms. I expresses romantic feelings toward the resident and believes that he was her physician and prescribed medications, including “mood stabilizers.” The resident never treated Ms. I; to his knowledge, he has never interacted with her.
Ms. I describes the resident’s refusal to continue treating her as “abandonment” and states that she is contemplating self-harm because of this rejection. In her letters, Ms. I admits that she was a long-term patient in a state psychiatric hospital in her home state and suffers from persistent auditory hallucinations. She also wants a romantic relationship with the resident and repeatedly threatens the resident’s female acquaintances and former romantic partners whose relationships she had surmised from news articles available on the Internet. Ms. I also threatens to strangle the resident. The resident sends her multiple written requests that she cease contact, but they are not acknowledged.
The authors’ observations
Stalking—repeated, unwanted attention or communication that would cause a reasonable person fear—is a serious threat for many psychiatric clinicians.1 Prevalence rates among mental health care providers range from 3% to 21%.2,3 Most stalkers have engaged in previous stalking behavior.3
Being stalked is highly distressing,4 and mental health professionals often do not reveal such experiences to colleagues.5 Irrational feelings of guilt or embarrassment, such as being thought to have poorly managed interactions with the stalker, often motivate a self-imposed silence (Table 1).6 This isolation may foster anxiety, interfere with receiving problem-solving advice, and increase physical vulnerability. In the case involving Ms. I, the psychiatric resident’s primary responsibility is safeguarding his own physical and psychological welfare.
Clinicians who work in a hospital or other institutional setting who are being stalked should inform their supervisors and the facility’s security personnel. Security personnel may be able to gather data about the stalker, decrease the stalker’s ability to communicate with the victim, and reduce unwanted physical access to the victim by distributing a photo of the stalker or installing a camera or receptionist-controlled door lock in patient entryways. Security personnel also may collaborate with local law enforcement. Having a third party respond to a stalker’s aggressive behavior—rather than the victim responding directly—avoids rewarding the stalker, which may generate further unwanted contact.7 Any intervention by the victim may increase the risk of violence, creating an “intervention dilemma.” Resnick8 argues that before deciding how best to address the stalker’s behavior, a stalking victim must “first separate the risk of continued stalking from the risk that the stalker will commit a violent act.”
Mental health professionals in private practice who are being stalked should consider retaining an attorney. An attorney often can maintain privacy of communications regarding the stalker via the attorney-client and attorney-work product privileges, which may help during legal proceedings.
Table 1
Factors that can impede psychiatrists from reporting stalking
| Fear of being perceived as a failure |
| Embarrassment |
| High professional tolerance for antisocial and threatening behavior |
| Misplaced sense of duty |
| Source: Reference 6 |
RESPONSE: Involving police
Over 2 months, Ms. I phones the resident’s home 105 times (the resident screens the calls). During 1 call, she states that she is hidden in a closet in her home and will hurt herself unless the resident “resumes” her psychiatric care. The resident contacts police in his city and Ms. I’s community, but authorities are reluctant to act when he acknowledges that he is not Ms. I’s psychiatrist and does not know her. Police officers in Ms. I’s hometown tell the resident no one answered the door when they visited her home. They state that they would enter the residence forcibly only if Ms. I’s physician or a family member asked them to do so, and because the resident admits that he is not her psychiatrist, they cannot take further action. Ms. I leaves the resident a phone message several hours later to inform him she is safe.
The authors’ observations
Stalking-induced countertransference responses may lead a psychiatrist to unwittingly place himself in harm’s way. For example, intense rage at a stalker’s request for treatment may generate guilt that motivates the psychiatrist to agree to treat the stalker. Feelings of helplessness may produce a frantic desire to do something even when such activity is ill-advised. Psychiatrists may develop a tolerance for antisocial or threatening behavior—which is common in mental health settings—and could accept unnecessary risks.
A psychiatrist who is being stalked may be able to assist a mentally ill stalker in a way that does not create a duty to treat and does not expose the psychiatrist to harm, such as contacting a mobile crisis intervention team, a mental health professional who recently treated the stalker, a family member of the stalker, or law enforcement personnel. A psychiatrist who is thrust from the role of helper to victim and must protect his or her own well-being instead of attending to a patient’s welfare is prone to suffer substantial countertransference distress.
The situation with Ms. I was particularly challenging because the resident did not know her complete history and therefore had little information to gauge how likely she was to act on her aggressive threats. Factors that predict future violence include:
- a history of violence
- significant prior criminality
- young age at first arrest
- concomitant substance abuse
- male sex.9
Unfortunately, other than sex, this data regarding Ms. I could not be readily obtained.
A psychiatrist’s duty
Although sympathetic to his stalker’s distress, the resident did not want to treat this woman, nor was he ethically or legally obligated to do so. An individual’s wish to be treated by a particular psychiatrist does not create a duty for the psychiatrist to satisfy this wish.10 State-based “Good Samaritan” laws encourage physicians to assist those in acute need by shielding them from liability, as long as they reasonably act within the scope of their expertise.11 However, they do not require a physician to care for an individual in acute need. A delusional wish for treatment or a false belief of already being in treatment does not create a duty to care for a person.
OUTCOME: Seeking help
Ms. I’s phone calls and letters continue. The resident discusses the situation with his associate residency director, who refers him to the hospital’s legal and investigative staffs. Based on advice from the hospital’s private investigator, the resident sends Ms. I a formal “cease and desist” letter that threatens her with legal action and possible jail time. The staff at the front desk of the clinic where the resident works and the hospital’s security department are instructed to watch for a visitor with Ms. I’s name and description, although the hospital’s investigator is unable to obtain a photograph of her. Shortly after the resident sends the letter, Ms. I ceases communication.
The authors’ observations
This case is unusual because most stalking victims know their stalkers. Identifying a stalker’s motivation can be helpful in formulating a risk assessment. One classification system recognizes 5 categories of stalkers: rejected, intimacy seeking, incompetent, resentful, and predatory (Table 2).1 Rejected stalkers appear to pose the greatest risk of violence and homicide.8 However, all stalkers may pose a risk of violence and therefore all stalking behavior should be treated seriously.
Table 2
Classification of stalkers
| Category | Common features |
|---|---|
| Rejected | Most have a personality disorder; often seeking reconciliation and revenge; most frequent victims are ex-romantic partners, but also target estranged relatives, former friends |
| Intimacy seeking | Erotomania; “morbid infatuation” |
| Incompetent | Lacking social skills; often have stalked others |
| Resentful | Pursuing a vendetta; generally feeling aggrieved |
| Predatory | Often comorbid with paraphilias; may have past convictions for sex offenses |
| Source: Adapted from reference 1 | |
Responding to a stalker
The approach should be tailored to the stalker’s characteristics.12 Silence—ie, lack of acknowledgement of a stalker’s intrusions—is one tactic.13 Consistent and persistent lack of engagement may bore the stalker, but also may provoke frustration or narcissistic or paranoia-fueled rage, and increased efforts to interact with the mental health professional. Other responses include:
- obtaining a protection or restraining order
- promoting the stalker’s participation in adversarial civil litigation, such as a lawsuit
- issuing verbal counterthreats.
Restraining orders are controversial and assessments of their effectiveness vary.14 How well a restraining order works may depend on the stalker’s:
- ability to appreciate reality, and how likely he or she is to experience anxiety when confronted with adverse consequences of his or her actions
- how consistently, rapidly, and harshly the criminal justice system responds to violations of restraining orders.
Restraining orders also may provide the victim a false sense of security.15 One of her letters revealed that Ms. I violated a criminal plea arrangement years earlier, which suggests she was capable of violating a restraining order.
Litigation. A stalker may initiate civil litigation against the victim to feel that he or she has an impact on the victim, which may reduce the stalker’s risk of violence if he or she is emotionally engaged in the litigation. Based on the authors’ experience, as long as the stalker is talking, he or she generally is less likely to act out violently and terminate a satisfying process. Adversarial civil litigation could give a stalker the opportunity to be “close” to the victim and a means of expressing aggressive wishes. The benefit of litigation lasts only as long as the case persists and the stalker believes he or she may prevail. In one of her letters, Ms. I bragged that she had represented herself as a pro se litigant in a complex civil matter, suggesting that she might be constructively channeled into litigation.
Promoting litigation carries significant risk.16 Being a defendant in pro se litigation may be emotionally and financially stressful. This approach may be desirable if the psychiatrist’s institution is willing to offer substantial support. For example, an institution may provide legal assistance—including helping to defray the cost of litigation—and litigation-related scheduling flexibility. An attorney may serve as a boundary between the victim and the pro se litigant’s sometimes ceaseless, time-devouring, anxiety-inducing legal maneuvers.
Counterthreats. Warning a stalker that he or she will face severe civil and criminal consequences if his or her behavior continues can make clear that his or her conduct is unacceptable.17 Such warnings may be delivered verbally or in writing by a legal representative, law enforcement personnel, a private security agent, or the victim.
Issuing a counterthreat can be risky. Stalkers with antisocial or narcissistic personality features may perceive a counterthreat as narcissistically diminishing, and to save face will escalate their stalking in retaliation. Avoid counterthreats if you believe the stalker might be psychotic because destabilizing such an individual—such as by precipitating a short psychotic episode—may increase unpredictability and diminish their responsive to interventions.
Ms. I’s contact with the resident lasted approximately 20 months, slightly less than the average 26 months reported in a survey of mental health professionals.3 Because stalkers are unpredictable, the psychiatric resident remains cautious.
Related Resources
- National Center for Victims of Crime. Stalking resource center. www.victimsofcrime.org/our-programs/stalking-resource-center.
- Mullen PE, Pathé M, Purcell R. Stalkers and their victims. New York, NY: Cambridge University Press; 2009.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE: Delusions and threats
For over 20 months, Ms. I, age 48, sends a psychiatric resident letters and postcards that total approximately 3,000 pages and come from dozens of return addresses. Ms. I expresses romantic feelings toward the resident and believes that he was her physician and prescribed medications, including “mood stabilizers.” The resident never treated Ms. I; to his knowledge, he has never interacted with her.
Ms. I describes the resident’s refusal to continue treating her as “abandonment” and states that she is contemplating self-harm because of this rejection. In her letters, Ms. I admits that she was a long-term patient in a state psychiatric hospital in her home state and suffers from persistent auditory hallucinations. She also wants a romantic relationship with the resident and repeatedly threatens the resident’s female acquaintances and former romantic partners whose relationships she had surmised from news articles available on the Internet. Ms. I also threatens to strangle the resident. The resident sends her multiple written requests that she cease contact, but they are not acknowledged.
The authors’ observations
Stalking—repeated, unwanted attention or communication that would cause a reasonable person fear—is a serious threat for many psychiatric clinicians.1 Prevalence rates among mental health care providers range from 3% to 21%.2,3 Most stalkers have engaged in previous stalking behavior.3
Being stalked is highly distressing,4 and mental health professionals often do not reveal such experiences to colleagues.5 Irrational feelings of guilt or embarrassment, such as being thought to have poorly managed interactions with the stalker, often motivate a self-imposed silence (Table 1).6 This isolation may foster anxiety, interfere with receiving problem-solving advice, and increase physical vulnerability. In the case involving Ms. I, the psychiatric resident’s primary responsibility is safeguarding his own physical and psychological welfare.
Clinicians who work in a hospital or other institutional setting who are being stalked should inform their supervisors and the facility’s security personnel. Security personnel may be able to gather data about the stalker, decrease the stalker’s ability to communicate with the victim, and reduce unwanted physical access to the victim by distributing a photo of the stalker or installing a camera or receptionist-controlled door lock in patient entryways. Security personnel also may collaborate with local law enforcement. Having a third party respond to a stalker’s aggressive behavior—rather than the victim responding directly—avoids rewarding the stalker, which may generate further unwanted contact.7 Any intervention by the victim may increase the risk of violence, creating an “intervention dilemma.” Resnick8 argues that before deciding how best to address the stalker’s behavior, a stalking victim must “first separate the risk of continued stalking from the risk that the stalker will commit a violent act.”
Mental health professionals in private practice who are being stalked should consider retaining an attorney. An attorney often can maintain privacy of communications regarding the stalker via the attorney-client and attorney-work product privileges, which may help during legal proceedings.
Table 1
Factors that can impede psychiatrists from reporting stalking
| Fear of being perceived as a failure |
| Embarrassment |
| High professional tolerance for antisocial and threatening behavior |
| Misplaced sense of duty |
| Source: Reference 6 |
RESPONSE: Involving police
Over 2 months, Ms. I phones the resident’s home 105 times (the resident screens the calls). During 1 call, she states that she is hidden in a closet in her home and will hurt herself unless the resident “resumes” her psychiatric care. The resident contacts police in his city and Ms. I’s community, but authorities are reluctant to act when he acknowledges that he is not Ms. I’s psychiatrist and does not know her. Police officers in Ms. I’s hometown tell the resident no one answered the door when they visited her home. They state that they would enter the residence forcibly only if Ms. I’s physician or a family member asked them to do so, and because the resident admits that he is not her psychiatrist, they cannot take further action. Ms. I leaves the resident a phone message several hours later to inform him she is safe.
The authors’ observations
Stalking-induced countertransference responses may lead a psychiatrist to unwittingly place himself in harm’s way. For example, intense rage at a stalker’s request for treatment may generate guilt that motivates the psychiatrist to agree to treat the stalker. Feelings of helplessness may produce a frantic desire to do something even when such activity is ill-advised. Psychiatrists may develop a tolerance for antisocial or threatening behavior—which is common in mental health settings—and could accept unnecessary risks.
A psychiatrist who is being stalked may be able to assist a mentally ill stalker in a way that does not create a duty to treat and does not expose the psychiatrist to harm, such as contacting a mobile crisis intervention team, a mental health professional who recently treated the stalker, a family member of the stalker, or law enforcement personnel. A psychiatrist who is thrust from the role of helper to victim and must protect his or her own well-being instead of attending to a patient’s welfare is prone to suffer substantial countertransference distress.
The situation with Ms. I was particularly challenging because the resident did not know her complete history and therefore had little information to gauge how likely she was to act on her aggressive threats. Factors that predict future violence include:
- a history of violence
- significant prior criminality
- young age at first arrest
- concomitant substance abuse
- male sex.9
Unfortunately, other than sex, this data regarding Ms. I could not be readily obtained.
A psychiatrist’s duty
Although sympathetic to his stalker’s distress, the resident did not want to treat this woman, nor was he ethically or legally obligated to do so. An individual’s wish to be treated by a particular psychiatrist does not create a duty for the psychiatrist to satisfy this wish.10 State-based “Good Samaritan” laws encourage physicians to assist those in acute need by shielding them from liability, as long as they reasonably act within the scope of their expertise.11 However, they do not require a physician to care for an individual in acute need. A delusional wish for treatment or a false belief of already being in treatment does not create a duty to care for a person.
OUTCOME: Seeking help
Ms. I’s phone calls and letters continue. The resident discusses the situation with his associate residency director, who refers him to the hospital’s legal and investigative staffs. Based on advice from the hospital’s private investigator, the resident sends Ms. I a formal “cease and desist” letter that threatens her with legal action and possible jail time. The staff at the front desk of the clinic where the resident works and the hospital’s security department are instructed to watch for a visitor with Ms. I’s name and description, although the hospital’s investigator is unable to obtain a photograph of her. Shortly after the resident sends the letter, Ms. I ceases communication.
The authors’ observations
This case is unusual because most stalking victims know their stalkers. Identifying a stalker’s motivation can be helpful in formulating a risk assessment. One classification system recognizes 5 categories of stalkers: rejected, intimacy seeking, incompetent, resentful, and predatory (Table 2).1 Rejected stalkers appear to pose the greatest risk of violence and homicide.8 However, all stalkers may pose a risk of violence and therefore all stalking behavior should be treated seriously.
Table 2
Classification of stalkers
| Category | Common features |
|---|---|
| Rejected | Most have a personality disorder; often seeking reconciliation and revenge; most frequent victims are ex-romantic partners, but also target estranged relatives, former friends |
| Intimacy seeking | Erotomania; “morbid infatuation” |
| Incompetent | Lacking social skills; often have stalked others |
| Resentful | Pursuing a vendetta; generally feeling aggrieved |
| Predatory | Often comorbid with paraphilias; may have past convictions for sex offenses |
| Source: Adapted from reference 1 | |
Responding to a stalker
The approach should be tailored to the stalker’s characteristics.12 Silence—ie, lack of acknowledgement of a stalker’s intrusions—is one tactic.13 Consistent and persistent lack of engagement may bore the stalker, but also may provoke frustration or narcissistic or paranoia-fueled rage, and increased efforts to interact with the mental health professional. Other responses include:
- obtaining a protection or restraining order
- promoting the stalker’s participation in adversarial civil litigation, such as a lawsuit
- issuing verbal counterthreats.
Restraining orders are controversial and assessments of their effectiveness vary.14 How well a restraining order works may depend on the stalker’s:
- ability to appreciate reality, and how likely he or she is to experience anxiety when confronted with adverse consequences of his or her actions
- how consistently, rapidly, and harshly the criminal justice system responds to violations of restraining orders.
Restraining orders also may provide the victim a false sense of security.15 One of her letters revealed that Ms. I violated a criminal plea arrangement years earlier, which suggests she was capable of violating a restraining order.
Litigation. A stalker may initiate civil litigation against the victim to feel that he or she has an impact on the victim, which may reduce the stalker’s risk of violence if he or she is emotionally engaged in the litigation. Based on the authors’ experience, as long as the stalker is talking, he or she generally is less likely to act out violently and terminate a satisfying process. Adversarial civil litigation could give a stalker the opportunity to be “close” to the victim and a means of expressing aggressive wishes. The benefit of litigation lasts only as long as the case persists and the stalker believes he or she may prevail. In one of her letters, Ms. I bragged that she had represented herself as a pro se litigant in a complex civil matter, suggesting that she might be constructively channeled into litigation.
Promoting litigation carries significant risk.16 Being a defendant in pro se litigation may be emotionally and financially stressful. This approach may be desirable if the psychiatrist’s institution is willing to offer substantial support. For example, an institution may provide legal assistance—including helping to defray the cost of litigation—and litigation-related scheduling flexibility. An attorney may serve as a boundary between the victim and the pro se litigant’s sometimes ceaseless, time-devouring, anxiety-inducing legal maneuvers.
Counterthreats. Warning a stalker that he or she will face severe civil and criminal consequences if his or her behavior continues can make clear that his or her conduct is unacceptable.17 Such warnings may be delivered verbally or in writing by a legal representative, law enforcement personnel, a private security agent, or the victim.
Issuing a counterthreat can be risky. Stalkers with antisocial or narcissistic personality features may perceive a counterthreat as narcissistically diminishing, and to save face will escalate their stalking in retaliation. Avoid counterthreats if you believe the stalker might be psychotic because destabilizing such an individual—such as by precipitating a short psychotic episode—may increase unpredictability and diminish their responsive to interventions.
Ms. I’s contact with the resident lasted approximately 20 months, slightly less than the average 26 months reported in a survey of mental health professionals.3 Because stalkers are unpredictable, the psychiatric resident remains cautious.
Related Resources
- National Center for Victims of Crime. Stalking resource center. www.victimsofcrime.org/our-programs/stalking-resource-center.
- Mullen PE, Pathé M, Purcell R. Stalkers and their victims. New York, NY: Cambridge University Press; 2009.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Mullen PE, Pathé M, Purcell R, et al. Study of stalkers. Am J Psychiatry. 1999;156(8):1244-1249.
2. Sandberg DA, McNiel DE, Binder RL. Stalking threatening, and harassing behavior by psychiatric patients toward clinicians. J Am Acad Psychiatry Law. 2002;30(2):221-229.
3. McIvor R, Potter L, Davies L. Stalking behavior by patients towards psychiatrists in a large mental health organization. Int J Soc Psychiatry. 2008;54(4):350-357.
4. Mullen PE, Pathé M. Stalking. Crime and Justice. 2002;29:273-318.
5. Bird S. Strategies for managing and minimizing the impact of harassment and stalking by patients. ANZ J Surg. 2009;79(7-8):537-538.
6. Sinwelski SA, Vinton L. Stalking: the constant threat of violence. Affilia. 2001;16(1):46-65.
7. Meloy JR. Commentary: stalking threatening, and harassing behavior by patients—the risk-management response. J Am Acad Psychiatry Law. 2002;30(2):230-231.
8. Resnick PJ. Stalking risk assessment. In: Pinals DA, ed. Stalking: psychiatric perspectives and practical approaches. New York, NY: Oxford University Press; 2007:61–84.
9. Dietz PE. Defenses against dangerous people when arrest and commitment fail. In: Simon RI, ed. American Psychiatric Press review of clinical psychiatry and the law. 1st ed. Washington, DC: American Psychiatric Press; 1989:205–219.
10. Hilliard J. Termination of treatment with troublesome patients. In: Lifson LE, Simon RI, eds. The mental health practitioner and the law: a comprehensive handbook. Cambridge, MA: Harvard University Press; 1998:216–224.
11. Paterick TJ, Paterick BB, Paterick TE. Implications of Good Samaritan laws for physicians. J Med Pract Manage. 2008;23(6):372-375.
12. MacKenzie RD, James DV. Management and treatment of stalkers: problems options, and solutions. Behav Sci Law. 2011;29(2):220-239.
13. Fremouw WJ, Westrup D, Pennypacker J. Stalking on campus: the prevalence and strategies for coping with stalking. J Forensic Sci. 1997;42(4):666-669.
14. Nicastro AM, Cousins AV, Spitzberg BH. The tactical face of stalking. Journal of Criminal Justice. 2000;28(1):69-82.
15. Spitzberg BH. The tactical topography of stalking victimization and management. Trauma Violence Abuse. 2002;3(4):261-288.
16. Pathé M, MacKenzie R, Mullen PE. Stalking by law: damaging victims and rewarding offenders. J Law Med. 2004;12(1):103-111.
17. Lion JR, Herschler JA. The stalking of physicians by their patients. In: Meloy JR. The psychology of stalking: clinical and forensic perspectives. San Diego, CA: Academic Press; 1998:163–173.
1. Mullen PE, Pathé M, Purcell R, et al. Study of stalkers. Am J Psychiatry. 1999;156(8):1244-1249.
2. Sandberg DA, McNiel DE, Binder RL. Stalking threatening, and harassing behavior by psychiatric patients toward clinicians. J Am Acad Psychiatry Law. 2002;30(2):221-229.
3. McIvor R, Potter L, Davies L. Stalking behavior by patients towards psychiatrists in a large mental health organization. Int J Soc Psychiatry. 2008;54(4):350-357.
4. Mullen PE, Pathé M. Stalking. Crime and Justice. 2002;29:273-318.
5. Bird S. Strategies for managing and minimizing the impact of harassment and stalking by patients. ANZ J Surg. 2009;79(7-8):537-538.
6. Sinwelski SA, Vinton L. Stalking: the constant threat of violence. Affilia. 2001;16(1):46-65.
7. Meloy JR. Commentary: stalking threatening, and harassing behavior by patients—the risk-management response. J Am Acad Psychiatry Law. 2002;30(2):230-231.
8. Resnick PJ. Stalking risk assessment. In: Pinals DA, ed. Stalking: psychiatric perspectives and practical approaches. New York, NY: Oxford University Press; 2007:61–84.
9. Dietz PE. Defenses against dangerous people when arrest and commitment fail. In: Simon RI, ed. American Psychiatric Press review of clinical psychiatry and the law. 1st ed. Washington, DC: American Psychiatric Press; 1989:205–219.
10. Hilliard J. Termination of treatment with troublesome patients. In: Lifson LE, Simon RI, eds. The mental health practitioner and the law: a comprehensive handbook. Cambridge, MA: Harvard University Press; 1998:216–224.
11. Paterick TJ, Paterick BB, Paterick TE. Implications of Good Samaritan laws for physicians. J Med Pract Manage. 2008;23(6):372-375.
12. MacKenzie RD, James DV. Management and treatment of stalkers: problems options, and solutions. Behav Sci Law. 2011;29(2):220-239.
13. Fremouw WJ, Westrup D, Pennypacker J. Stalking on campus: the prevalence and strategies for coping with stalking. J Forensic Sci. 1997;42(4):666-669.
14. Nicastro AM, Cousins AV, Spitzberg BH. The tactical face of stalking. Journal of Criminal Justice. 2000;28(1):69-82.
15. Spitzberg BH. The tactical topography of stalking victimization and management. Trauma Violence Abuse. 2002;3(4):261-288.
16. Pathé M, MacKenzie R, Mullen PE. Stalking by law: damaging victims and rewarding offenders. J Law Med. 2004;12(1):103-111.
17. Lion JR, Herschler JA. The stalking of physicians by their patients. In: Meloy JR. The psychology of stalking: clinical and forensic perspectives. San Diego, CA: Academic Press; 1998:163–173.
Psychotropic-induced dry mouth: Don’t overlook this potentially serious side effect
Discuss this article at www.facebook.com/CurrentPsychiatry
Xerostomia, commonly known as “dry mouth,” is a reported side effect of >1,800 drugs from >80 classes.1 This condition often goes unrecognized and untreated, but it can significantly affect patients’ quality of life and cause oral and medical health problems.2,3 Although psychotropic medications are not the only offenders, they comprise a large portion of the agents that can cause dry mouth. Antidepressants, anticonvulsants, anxiolytics, antipsychotics, anticholinergics, and alpha agonists can cause xerostomia.4 The risk of salivary hypofunction increases with polypharmacy and may be especially likely when ≥3 drugs are taken per day.5
Among all reported side effects of antidepressants and antipsychotics, dry mouth often is the most prevalent complaint. For example, in a study of 5 antidepressants 35% to 46% of patients reported dry mouth.6 Rates are similar in users of various antipsychotics. Patients with severe, persistent mental illness often cite side effects as the primary reason for psychotropic noncompliance.7-9
Few psychiatrists routinely screen patients for xerostomia, and if a patient reports this side effect, they may be unlikely to address it or understand its implications because of more pressing concerns such as psychosis or risk of suicide. Historically, education in general medical training about the effects of oral health on a patient’s overall health has been limited. It is crucial for psychiatrists to be aware of potential problems related to dry mouth and the impact it can have on their patients. In this article, we:
- describe how dry mouth can impact a patient’s oral, medical, and psychiatric health
- provide psychiatrists with an understanding of pathology related to xerostomia
- explain how psychiatrists can screen for xerostomia
- discuss the benefits patients may receive when psychiatrists collaborate with dental clinicians to manage this condition.
Implications of xerostomia
Saliva provides a protective function. It is an antimicrobial, buffering, and lubricating agent that aids cleansing and removal of food debris within the mouth. It also helps maintain oral mucosa and remineralizing of tooth structure.10
Psychotropics can affect the amount of saliva secreted and may alter the composition of saliva via their receptor affects on the dual sympathetic and parasympathetic innervations of the salivary glands.11 When the protective environment produced by saliva is altered, patients may start to develop oral problems before experiencing dryness. A 50% reduction in saliva flow may occur before they become aware of the problem.12,13
Patients may not taste food properly, experience cracked lips, or have trouble eating, oral pain, or dentures that no longer fit well.14 Additionally, oral diseases such as dental decay and periodontal disease (Photos 1 and 2), inflamed soft tissue, and candidiasis (Photo 3) also may occur.10,15 Patients may begin to notice dry mouth when they wake at night, which could disrupt sleep. Patients with xerostomia can accumulate excessive amounts of plaque on their teeth and the dorsum of the tongue. The increased bacterial count and release of volatile sulfide gases that occur with dry mouth may explain some cases of halitosis.16,17 Patients also may have difficulty swallowing or speaking and be unaware of the oral health destruction occurring as a result of reduced saliva. Some experts report oral bacteria levels can skyrocket as much as 10-fold in people who take medications that cause dry mouth.18
Infections of the mouth can create havoc elsewhere in the body. The evidence base that establishes an association between periodontal disease and other chronic inflammatory conditions such as diabetes, cardiovascular disease, cancer, and rheumatoid arthritis is steadily growing.19-22 Periodontal disease also is a risk factor for preeclampsia and other illnesses that can negatively affect neonatal health.23,24
Failure to recognize xerostomia caused by psychotropic medications may lead to an increase in cavities, periodontal disease, and chronic systemic inflammatory conditions that can shorten a patient’s life span. Recognizing and treating causes of xerostomia is vital because doing so may halt this chain of events.
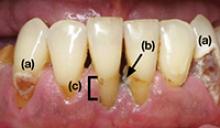
Photo 1
This patient complained of dry mouth and exhibits decay (a) and evidence of periodontal disease. Plaque and calculus is present (b), along with gingival recession from the loss of attachment and bone (c). This patient was taking venlafaxine, zolpidem, and alprazolam
Photo 2
Dental cavities were restored with tooth-colored restorations (arrows) on this patient, who has xerostomia. Every effort must be made to manage this patient’s dry mouth or the restorations may fail due to recurrent decay
Photo 3
This partial denture wearer, who complained of dry mouth, has evidence of palatal irritation and sores as a result of xerostomia and use of a partial denture. This patient was taking bupropion, esomeprazole, and tolterodine
Psychiatric patients’ oral health
Psychiatric patients’ oral health status often is poor. Several studies found that compared with the general population, patients who have severe, persistent mental illness are at higher risk to be missing teeth, schedule fewer visits to the dentist, and neglect oral hygiene.25-28 Periodontal disease also could be a problem in these patients.29 Although some evidence suggests mental illness may make patients less likely to go to the dentist, psychotropic medications also may contribute to their dental difficulties.
Screening for xerostomia
Simply advising patients of the problems related to xerostomia and asking several questions may help prevent pain and deterioration in function within the oral cavity (Table 1).14,30
You can perform a simple in-office assessment of the oral cavity by visual inspection and by placing a dry tongue blade against the inside of the cheek mucosa. If the blade sticks to the mucosa and a gentle tug is needed to lift it away, xerostomia may be present.30 Conversely, a healthy mouth will have a collection of saliva on the floor of the oral cavity, and pulling a tongue blade away from the inside of the cheek will not require any effort (Photos 4 and 5).
Table 1
Screening questions for xerostomia
| Does the amount of saliva in your mouth seem to have decreased? |
| Do you have any trouble swallowing, speaking, or eating dry foods? |
| Do you sip liquids more often to help you swallow? |
| Do you notice any dryness or cracking of your lips? |
| Do you have mouth sores or a burning feeling in the mouth? |
| When was the last time you saw your dentist? (Patients with xerostomia may need to see their dentist more frequently) |
| Are you aware of any halitosis (ie, mouth odor)? |
| Source: Reference 14 |
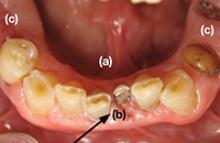
Photo 4
The arrow shows the normal appearance of saliva collecting on the floor of the mouth
Photo 5
This patient complained of dry mouth. Note the floor of the mouth is free of saliva (a). Decay is present (b), and the patient is missing posterior teeth (c). This patient was taking clonidine, metoprolol, hydrochlorothiazide, amlodipine, and irbesartan
Treatment options
Patients who have reduced salivary flow as a result of a medication may become so affected by dryness that their drug regimen may need to be changed. However, the greatest concern is for deteriorating oral health among patients who may be unaware xerostomia is occurring.31
Counsel patients who take medications that can affect their salivary function about the importance of seeing a dentist regularly, and provide referrals when appropriate. Depending upon the patient’s oral health, dentists recommend patients with xerostomia have their teeth cleaned/examined 3 or 4 times per year, rather than the 2 times per year allowed by third-party payers (ie, insurance companies). Also advise patients to be diligent in their oral hygiene practices, including flossing and brushing the teeth and tongue, and to avoid foods that are sticky and/or have high sucrose content (Table 2). Recommend using a toothpaste containing fluoride—preferably one free of sodium lauryl sulfate, which could contribute to mouth sores14—and drinking fluoridated water. Explain to patients that their dentist may recommend in-office high-fluoride applications, high-fluoride prescription toothpaste, and/or “mouth trays” that contain high fluoride gel. Tell patients to avoid cigarettes and caffeinated beverages, which can increase dryness. Alcohol use should be minimized and mouth rinses containing alcohol should not be used.
Many over-the-counter products are available to address xerostomia, including toothpastes, mouth rinses, and gels. Salivary substitutes—which are available as sprays, liquids, tablets, and swab sticks—imitate saliva and may provide a temporary reprieve from dryness. Although none of these products will cure dry mouth, they may help manage the condition. Advise patients to eat foods that stimulate saliva production, such as carrots, apples, and celery, and to chew sugarless gum and candies, which also will stimulate salivary flow.
The FDA has approved 2 prescription drugs for treating xerostomia: cevimeline and pilocarpine. Cevimeline is approved for treating dry mouth associated with Sjögren’s syndrome and pilocarpine is approved for treating dry mouth caused by head and neck radiation therapy; however, these medications’ role in treating dry mouth in psychiatric patients has not been investigated. Both agents are contraindicated in patients with narrow-angle glaucoma, uncontrolled asthma, or liver disease, and should be prescribed with caution for patients with cardiovascular disease, chronic respiratory conditions, or kidney disease.32
Acupuncture and electrostimulation are being studied as a treatment for xerostomia. Trials have found acupuncture improves symptoms of xerostomia,33,34 and 1 study found electrostimulation improved xerostomia in patients with Sjögren’s syndrome.35 Both approaches require more study to confirm their effectiveness.33-35
Table 2
Managing dry mouth: What to tell patients
| Oral hygiene. Tell patients to be diligent in their oral hygiene practices, including brushing and flossing. They should use a toothpaste containing fluoride—preferably one free of sodium lauryl sulfate—and schedule regular dental visits, where they can receive high-fluoride applications or be prescribed high-fluoride prescription toothpastes |
| Diet. Advise patients to avoid foods high in sucrose content, rinse their mouth with water soon after eating, and drink fluoridated water regularly. Tell them that they may be able to stimulate saliva flow with sugarless gum, candies, and foods such as celery and carrots |
| Drying agents. Instruct patients to avoid cigarettes, caffeinated beverages, and mouth rinses that contain alcohol. Explain that some patients may benefit from sleeping in a room with a cool air humidifier |
| Over-the-counter products. Suggest patients try salivary substitutes, which are dispensed in spray bottles, rinses, swish bottles, or oral swab sticks. In addition, products such as dry-mouth toothpaste and moisturizing gels also may help relieve their symptoms |
- Persson K, Axtelius B, Söderfeldt B, et al. Monitoring oral health and dental attendance in an outpatient psychiatric population. J Psychiatr Ment Health Nurs. 2009;16(3):263-271.
- Keene JJ Jr, Galasko GT, Land MF. Antidepressant use in psychiatry and medicine: importance for dental practice. J Am Dent Assoc. 2003;134(1):71-79.
Drug Brand Names
- Alprazolam • Xanax
- Amlodipine • Norvasc
- Bupropion • Wellbutrin, Zyban
- Cevimeline • Evoxac
- Clonidine • Catapres, Kapvay, others
- Esomeprazole • Nexium
- Irbesartan • Avapro
- Metoprolol • Lopressor, Toprol
- Pilocarpine • Salagen
- Tolterodine • Detrol
- Venlafaxine • Effexor
- Zolpidem • Ambien
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Drymouth.info. Overview of drugs and dry mouth. http://drymouth.info/practitioner/overview.asp. Accessed September 2, 2011.
2. Stewart CM, Berg KM, Cha S, et al. Salivary dysfunction and quality of life in Sjögren syndrome: a critical oral-systemic connection. J Am Dent Assoc. 2008;139(3):291-299.
3. Friedman PK. Xerostomia: The invisible oral health condition. http://www.dentistryiq.com/index/display/article-display/295922/articles/woman-dentist-journal/health/xerostomia-the-invisible-oral-health-condition.html. Accessed September 6, 2011.
4. Physician Desk Reference. Montvale NJ: PDR Network LLC.; 2011.
5. Bardow A, Lagerlof F, Nauntofte B, et al. The role of saliva. In: Fejerskov O, Kidd E, eds. Dental caries: the disease and its clinical management. Oxford, United Kingdom: Blackwell Munksgaard; 2008:195.
6. Vanderkooy JD, Kennedy SH, Bagby RM. Antidepressant side effects in depression patients treated in a naturalistic setting: a study of bupropion moclobemide, paroxetine, sertraline, and venlafaxine. Can J Psychiatry. 2002;47(2):174-180.
7. Löffler W, Kilian R, Toumi M, et al. Schizophrenic patients’ subjective reasons for compliance and noncompliance with neuroleptic treatment. Pharmacopsychiatry. 2003;36(3):105-112.
8. Lambert M, Conus P, Eide P, et al. Impact of present and past antipsychotic side effects on attitude toward typical antipsychotic treatment and adherence. Eur Psychiatry. 2004;19(7):415-422.
9. Rettenbacher MA, Hofer A, Eder U, et al. Compliance in schizophrenia: psychopathology, side effects, and patients’ attitudes toward the illness and medication. J Clin Psychiatry. 2004;65(9):1211-1218.
10. Bulkacz J, Carranza FA. Defense mechanisms of the gingiva. In: Newman MG, Takei HH, Klokkevold PR, et al, eds. Carranza’s clinical periodontology. St. Louis, MO: Elsevier Saunders; 2011:69–70.
11. Szabadi E, Tavernor S. Hypo-and hyper-salivation induced by psychoactive drugs. CNS Drugs. 1999;11(6):449-466.
12. Guggenheimer J, Moore PA. Xerostomia: etiology recognition and treatment. J Am Dent Assoc. 2003;134(1):61-69.
13. Dawes C. Physiological factors affecting salivary flow rate oral sugar clearance, and the sensation of dry mouth in man. J Dent Res. 1987;66:648-653.
14. Bartels CL. Xerostomia information for dentists. http://www.homesteadschools.com/dental/courses/Xerostomia/Course.htm. Accessed August 15, 2011.
15. Sitheeque MA, Samaranayake LP. Chronic hyperplastic candidosis/candidiasis (candidal leukoplakia). Crit Rev Oral Biol Med. 2003;14(4):253-267.
16. Porter SR, Scully C. Oral malodour (halitosis). BMJ. 2006;333(7569):632-635.
17. Quirynen M, Van den Veide S, Vanderkerckhove B, et al. Oral malodor. In: Newman MG, Takei HH, Klokkevold PR, et al, eds. Carranza’s clinical periodontology. St. Louis, MO: Elsevier Saunders; 2011:333.
18. Papas A. Dry mouth from drugs: more than just an annoying side effect. Tufts University Heath and Nutrition Letter. 2000;3.-
19. American Academy of Periodontology. Gum disease information from the American Academy of Periodontology http://perio.org. Accessed August 12, 2011.
20. Geismar K, Stoltze K, Sigurd B, et al. Periodontal disease and coronary heart disease. J Periodontol. 2006;77(9):1547-1554.
21. Lee HJ, Garcia RI, Janket SJ, et al. The association between cumulative periodontal disease and stroke history in older adults. J Periodontol. 2006;77(10):1744-1754.
22. Friedewald VE, Kornman KS, Beck JD, et al. The American Journal of Cardiology and Journal of Periodontology editors’ consensus: periodontitis and atherosclerotic cardiovascular disease. J Periodontol. 2009;80(7):1021-1032.
23. Contreras A, Herrera JA, Soto JE, et al. Periodontitis is associated with preeclampsia in pregnant women. J Periodontol. 2006;77(2):182-188.
24. Dasanayake AP, Li Y, Wiener H, et al. Salivary Actinomyces naeslundii genospecies 2 and Lactobacillus casei levels predict pregnancy outcomes. J Periodontol. 2005;76(2):171-177.
25. McCreadie RG, Stevens H, Henderson J, et al. The dental health of people with schizophrenia. Acta Psychiatr Scand. 2004;110(4):306-310.
26. Anttila S, Knuuttila M, Ylöstalo P, et al. Symptoms of depression and anxiety in relation to dental health behavior and self-perceived dental treatment need. Eur J Oral Sci. 2006;114(2):109-114.
27. Sjögren R, Nordström G. Oral health status of psychiatric patients. J Clin Nurs. 2000;9(4):632-638.
28. Ramon T, Grinshpoon A, Zusman SP, et al. Oral health and treatment needs of institutionalized chronic psychiatric patients in Israel. Eur Psychiatry. 2003;18(3):101-105.
29. Portilla MI, Mafla AC, Arteaga JJ. Periodontal status in female psychiatric patients. Colomb Med. 2009;40(2):167-176.
30. Navazesh M. ADA Council on Scientific Affairs and Division of Science. How can oral health care providers determine if patients have dry mouth? J Am Dent Assoc. 2003;134(5):613-620.
31. Mignogna MD, Fedele S, Lo Russo L, et al. Sjögren’s syndrome: the diagnostic potential of early oral manifestations preceding hyposalivation/xerostomia. J Oral Pathol Med. 2005;34(1):1-6.
32. Spolarich AE. Managing the side effects of medications. J Dent Hyg. 2000;74(1):57-69.
33. Johnstone PA, Niemtzow RC, Riffenburgh RH. Acupuncture for xerostomia: clinical update. Cancer. 2002;94(4):1151-1156.
34. Garcia MK, Chiang JS, Cohen L, et al. Acupuncture for radiation-induced xerostomia in patients with cancer: a pilot study. Head Neck. 2009;31(10):1360-1368.
35. Strietzel FP, Lafaurie GI, Mendoza GR, et al. Efficacy and safety of an intraoral electrostimulation device for xerostomia relief: a multicenter, randomized trial. Arthritis Rheum. 2011;63(1):180-190.
Discuss this article at www.facebook.com/CurrentPsychiatry
Xerostomia, commonly known as “dry mouth,” is a reported side effect of >1,800 drugs from >80 classes.1 This condition often goes unrecognized and untreated, but it can significantly affect patients’ quality of life and cause oral and medical health problems.2,3 Although psychotropic medications are not the only offenders, they comprise a large portion of the agents that can cause dry mouth. Antidepressants, anticonvulsants, anxiolytics, antipsychotics, anticholinergics, and alpha agonists can cause xerostomia.4 The risk of salivary hypofunction increases with polypharmacy and may be especially likely when ≥3 drugs are taken per day.5
Among all reported side effects of antidepressants and antipsychotics, dry mouth often is the most prevalent complaint. For example, in a study of 5 antidepressants 35% to 46% of patients reported dry mouth.6 Rates are similar in users of various antipsychotics. Patients with severe, persistent mental illness often cite side effects as the primary reason for psychotropic noncompliance.7-9
Few psychiatrists routinely screen patients for xerostomia, and if a patient reports this side effect, they may be unlikely to address it or understand its implications because of more pressing concerns such as psychosis or risk of suicide. Historically, education in general medical training about the effects of oral health on a patient’s overall health has been limited. It is crucial for psychiatrists to be aware of potential problems related to dry mouth and the impact it can have on their patients. In this article, we:
- describe how dry mouth can impact a patient’s oral, medical, and psychiatric health
- provide psychiatrists with an understanding of pathology related to xerostomia
- explain how psychiatrists can screen for xerostomia
- discuss the benefits patients may receive when psychiatrists collaborate with dental clinicians to manage this condition.
Implications of xerostomia
Saliva provides a protective function. It is an antimicrobial, buffering, and lubricating agent that aids cleansing and removal of food debris within the mouth. It also helps maintain oral mucosa and remineralizing of tooth structure.10
Psychotropics can affect the amount of saliva secreted and may alter the composition of saliva via their receptor affects on the dual sympathetic and parasympathetic innervations of the salivary glands.11 When the protective environment produced by saliva is altered, patients may start to develop oral problems before experiencing dryness. A 50% reduction in saliva flow may occur before they become aware of the problem.12,13
Patients may not taste food properly, experience cracked lips, or have trouble eating, oral pain, or dentures that no longer fit well.14 Additionally, oral diseases such as dental decay and periodontal disease (Photos 1 and 2), inflamed soft tissue, and candidiasis (Photo 3) also may occur.10,15 Patients may begin to notice dry mouth when they wake at night, which could disrupt sleep. Patients with xerostomia can accumulate excessive amounts of plaque on their teeth and the dorsum of the tongue. The increased bacterial count and release of volatile sulfide gases that occur with dry mouth may explain some cases of halitosis.16,17 Patients also may have difficulty swallowing or speaking and be unaware of the oral health destruction occurring as a result of reduced saliva. Some experts report oral bacteria levels can skyrocket as much as 10-fold in people who take medications that cause dry mouth.18
Infections of the mouth can create havoc elsewhere in the body. The evidence base that establishes an association between periodontal disease and other chronic inflammatory conditions such as diabetes, cardiovascular disease, cancer, and rheumatoid arthritis is steadily growing.19-22 Periodontal disease also is a risk factor for preeclampsia and other illnesses that can negatively affect neonatal health.23,24
Failure to recognize xerostomia caused by psychotropic medications may lead to an increase in cavities, periodontal disease, and chronic systemic inflammatory conditions that can shorten a patient’s life span. Recognizing and treating causes of xerostomia is vital because doing so may halt this chain of events.
Photo 1
This patient complained of dry mouth and exhibits decay (a) and evidence of periodontal disease. Plaque and calculus is present (b), along with gingival recession from the loss of attachment and bone (c). This patient was taking venlafaxine, zolpidem, and alprazolam
Photo 2
Dental cavities were restored with tooth-colored restorations (arrows) on this patient, who has xerostomia. Every effort must be made to manage this patient’s dry mouth or the restorations may fail due to recurrent decay
Photo 3
This partial denture wearer, who complained of dry mouth, has evidence of palatal irritation and sores as a result of xerostomia and use of a partial denture. This patient was taking bupropion, esomeprazole, and tolterodine
Psychiatric patients’ oral health
Psychiatric patients’ oral health status often is poor. Several studies found that compared with the general population, patients who have severe, persistent mental illness are at higher risk to be missing teeth, schedule fewer visits to the dentist, and neglect oral hygiene.25-28 Periodontal disease also could be a problem in these patients.29 Although some evidence suggests mental illness may make patients less likely to go to the dentist, psychotropic medications also may contribute to their dental difficulties.
Screening for xerostomia
Simply advising patients of the problems related to xerostomia and asking several questions may help prevent pain and deterioration in function within the oral cavity (Table 1).14,30
You can perform a simple in-office assessment of the oral cavity by visual inspection and by placing a dry tongue blade against the inside of the cheek mucosa. If the blade sticks to the mucosa and a gentle tug is needed to lift it away, xerostomia may be present.30 Conversely, a healthy mouth will have a collection of saliva on the floor of the oral cavity, and pulling a tongue blade away from the inside of the cheek will not require any effort (Photos 4 and 5).
Table 1
Screening questions for xerostomia
| Does the amount of saliva in your mouth seem to have decreased? |
| Do you have any trouble swallowing, speaking, or eating dry foods? |
| Do you sip liquids more often to help you swallow? |
| Do you notice any dryness or cracking of your lips? |
| Do you have mouth sores or a burning feeling in the mouth? |
| When was the last time you saw your dentist? (Patients with xerostomia may need to see their dentist more frequently) |
| Are you aware of any halitosis (ie, mouth odor)? |
| Source: Reference 14 |
Photo 4
The arrow shows the normal appearance of saliva collecting on the floor of the mouth
Photo 5
This patient complained of dry mouth. Note the floor of the mouth is free of saliva (a). Decay is present (b), and the patient is missing posterior teeth (c). This patient was taking clonidine, metoprolol, hydrochlorothiazide, amlodipine, and irbesartan
Treatment options
Patients who have reduced salivary flow as a result of a medication may become so affected by dryness that their drug regimen may need to be changed. However, the greatest concern is for deteriorating oral health among patients who may be unaware xerostomia is occurring.31
Counsel patients who take medications that can affect their salivary function about the importance of seeing a dentist regularly, and provide referrals when appropriate. Depending upon the patient’s oral health, dentists recommend patients with xerostomia have their teeth cleaned/examined 3 or 4 times per year, rather than the 2 times per year allowed by third-party payers (ie, insurance companies). Also advise patients to be diligent in their oral hygiene practices, including flossing and brushing the teeth and tongue, and to avoid foods that are sticky and/or have high sucrose content (Table 2). Recommend using a toothpaste containing fluoride—preferably one free of sodium lauryl sulfate, which could contribute to mouth sores14—and drinking fluoridated water. Explain to patients that their dentist may recommend in-office high-fluoride applications, high-fluoride prescription toothpaste, and/or “mouth trays” that contain high fluoride gel. Tell patients to avoid cigarettes and caffeinated beverages, which can increase dryness. Alcohol use should be minimized and mouth rinses containing alcohol should not be used.
Many over-the-counter products are available to address xerostomia, including toothpastes, mouth rinses, and gels. Salivary substitutes—which are available as sprays, liquids, tablets, and swab sticks—imitate saliva and may provide a temporary reprieve from dryness. Although none of these products will cure dry mouth, they may help manage the condition. Advise patients to eat foods that stimulate saliva production, such as carrots, apples, and celery, and to chew sugarless gum and candies, which also will stimulate salivary flow.
The FDA has approved 2 prescription drugs for treating xerostomia: cevimeline and pilocarpine. Cevimeline is approved for treating dry mouth associated with Sjögren’s syndrome and pilocarpine is approved for treating dry mouth caused by head and neck radiation therapy; however, these medications’ role in treating dry mouth in psychiatric patients has not been investigated. Both agents are contraindicated in patients with narrow-angle glaucoma, uncontrolled asthma, or liver disease, and should be prescribed with caution for patients with cardiovascular disease, chronic respiratory conditions, or kidney disease.32
Acupuncture and electrostimulation are being studied as a treatment for xerostomia. Trials have found acupuncture improves symptoms of xerostomia,33,34 and 1 study found electrostimulation improved xerostomia in patients with Sjögren’s syndrome.35 Both approaches require more study to confirm their effectiveness.33-35
Table 2
Managing dry mouth: What to tell patients
| Oral hygiene. Tell patients to be diligent in their oral hygiene practices, including brushing and flossing. They should use a toothpaste containing fluoride—preferably one free of sodium lauryl sulfate—and schedule regular dental visits, where they can receive high-fluoride applications or be prescribed high-fluoride prescription toothpastes |
| Diet. Advise patients to avoid foods high in sucrose content, rinse their mouth with water soon after eating, and drink fluoridated water regularly. Tell them that they may be able to stimulate saliva flow with sugarless gum, candies, and foods such as celery and carrots |
| Drying agents. Instruct patients to avoid cigarettes, caffeinated beverages, and mouth rinses that contain alcohol. Explain that some patients may benefit from sleeping in a room with a cool air humidifier |
| Over-the-counter products. Suggest patients try salivary substitutes, which are dispensed in spray bottles, rinses, swish bottles, or oral swab sticks. In addition, products such as dry-mouth toothpaste and moisturizing gels also may help relieve their symptoms |
- Persson K, Axtelius B, Söderfeldt B, et al. Monitoring oral health and dental attendance in an outpatient psychiatric population. J Psychiatr Ment Health Nurs. 2009;16(3):263-271.
- Keene JJ Jr, Galasko GT, Land MF. Antidepressant use in psychiatry and medicine: importance for dental practice. J Am Dent Assoc. 2003;134(1):71-79.
Drug Brand Names
- Alprazolam • Xanax
- Amlodipine • Norvasc
- Bupropion • Wellbutrin, Zyban
- Cevimeline • Evoxac
- Clonidine • Catapres, Kapvay, others
- Esomeprazole • Nexium
- Irbesartan • Avapro
- Metoprolol • Lopressor, Toprol
- Pilocarpine • Salagen
- Tolterodine • Detrol
- Venlafaxine • Effexor
- Zolpidem • Ambien
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Discuss this article at www.facebook.com/CurrentPsychiatry
Xerostomia, commonly known as “dry mouth,” is a reported side effect of >1,800 drugs from >80 classes.1 This condition often goes unrecognized and untreated, but it can significantly affect patients’ quality of life and cause oral and medical health problems.2,3 Although psychotropic medications are not the only offenders, they comprise a large portion of the agents that can cause dry mouth. Antidepressants, anticonvulsants, anxiolytics, antipsychotics, anticholinergics, and alpha agonists can cause xerostomia.4 The risk of salivary hypofunction increases with polypharmacy and may be especially likely when ≥3 drugs are taken per day.5
Among all reported side effects of antidepressants and antipsychotics, dry mouth often is the most prevalent complaint. For example, in a study of 5 antidepressants 35% to 46% of patients reported dry mouth.6 Rates are similar in users of various antipsychotics. Patients with severe, persistent mental illness often cite side effects as the primary reason for psychotropic noncompliance.7-9
Few psychiatrists routinely screen patients for xerostomia, and if a patient reports this side effect, they may be unlikely to address it or understand its implications because of more pressing concerns such as psychosis or risk of suicide. Historically, education in general medical training about the effects of oral health on a patient’s overall health has been limited. It is crucial for psychiatrists to be aware of potential problems related to dry mouth and the impact it can have on their patients. In this article, we:
- describe how dry mouth can impact a patient’s oral, medical, and psychiatric health
- provide psychiatrists with an understanding of pathology related to xerostomia
- explain how psychiatrists can screen for xerostomia
- discuss the benefits patients may receive when psychiatrists collaborate with dental clinicians to manage this condition.
Implications of xerostomia
Saliva provides a protective function. It is an antimicrobial, buffering, and lubricating agent that aids cleansing and removal of food debris within the mouth. It also helps maintain oral mucosa and remineralizing of tooth structure.10
Psychotropics can affect the amount of saliva secreted and may alter the composition of saliva via their receptor affects on the dual sympathetic and parasympathetic innervations of the salivary glands.11 When the protective environment produced by saliva is altered, patients may start to develop oral problems before experiencing dryness. A 50% reduction in saliva flow may occur before they become aware of the problem.12,13
Patients may not taste food properly, experience cracked lips, or have trouble eating, oral pain, or dentures that no longer fit well.14 Additionally, oral diseases such as dental decay and periodontal disease (Photos 1 and 2), inflamed soft tissue, and candidiasis (Photo 3) also may occur.10,15 Patients may begin to notice dry mouth when they wake at night, which could disrupt sleep. Patients with xerostomia can accumulate excessive amounts of plaque on their teeth and the dorsum of the tongue. The increased bacterial count and release of volatile sulfide gases that occur with dry mouth may explain some cases of halitosis.16,17 Patients also may have difficulty swallowing or speaking and be unaware of the oral health destruction occurring as a result of reduced saliva. Some experts report oral bacteria levels can skyrocket as much as 10-fold in people who take medications that cause dry mouth.18
Infections of the mouth can create havoc elsewhere in the body. The evidence base that establishes an association between periodontal disease and other chronic inflammatory conditions such as diabetes, cardiovascular disease, cancer, and rheumatoid arthritis is steadily growing.19-22 Periodontal disease also is a risk factor for preeclampsia and other illnesses that can negatively affect neonatal health.23,24
Failure to recognize xerostomia caused by psychotropic medications may lead to an increase in cavities, periodontal disease, and chronic systemic inflammatory conditions that can shorten a patient’s life span. Recognizing and treating causes of xerostomia is vital because doing so may halt this chain of events.
Photo 1
This patient complained of dry mouth and exhibits decay (a) and evidence of periodontal disease. Plaque and calculus is present (b), along with gingival recession from the loss of attachment and bone (c). This patient was taking venlafaxine, zolpidem, and alprazolam
Photo 2
Dental cavities were restored with tooth-colored restorations (arrows) on this patient, who has xerostomia. Every effort must be made to manage this patient’s dry mouth or the restorations may fail due to recurrent decay
Photo 3
This partial denture wearer, who complained of dry mouth, has evidence of palatal irritation and sores as a result of xerostomia and use of a partial denture. This patient was taking bupropion, esomeprazole, and tolterodine
Psychiatric patients’ oral health
Psychiatric patients’ oral health status often is poor. Several studies found that compared with the general population, patients who have severe, persistent mental illness are at higher risk to be missing teeth, schedule fewer visits to the dentist, and neglect oral hygiene.25-28 Periodontal disease also could be a problem in these patients.29 Although some evidence suggests mental illness may make patients less likely to go to the dentist, psychotropic medications also may contribute to their dental difficulties.
Screening for xerostomia
Simply advising patients of the problems related to xerostomia and asking several questions may help prevent pain and deterioration in function within the oral cavity (Table 1).14,30
You can perform a simple in-office assessment of the oral cavity by visual inspection and by placing a dry tongue blade against the inside of the cheek mucosa. If the blade sticks to the mucosa and a gentle tug is needed to lift it away, xerostomia may be present.30 Conversely, a healthy mouth will have a collection of saliva on the floor of the oral cavity, and pulling a tongue blade away from the inside of the cheek will not require any effort (Photos 4 and 5).
Table 1
Screening questions for xerostomia
| Does the amount of saliva in your mouth seem to have decreased? |
| Do you have any trouble swallowing, speaking, or eating dry foods? |
| Do you sip liquids more often to help you swallow? |
| Do you notice any dryness or cracking of your lips? |
| Do you have mouth sores or a burning feeling in the mouth? |
| When was the last time you saw your dentist? (Patients with xerostomia may need to see their dentist more frequently) |
| Are you aware of any halitosis (ie, mouth odor)? |
| Source: Reference 14 |
Photo 4
The arrow shows the normal appearance of saliva collecting on the floor of the mouth
Photo 5
This patient complained of dry mouth. Note the floor of the mouth is free of saliva (a). Decay is present (b), and the patient is missing posterior teeth (c). This patient was taking clonidine, metoprolol, hydrochlorothiazide, amlodipine, and irbesartan
Treatment options
Patients who have reduced salivary flow as a result of a medication may become so affected by dryness that their drug regimen may need to be changed. However, the greatest concern is for deteriorating oral health among patients who may be unaware xerostomia is occurring.31
Counsel patients who take medications that can affect their salivary function about the importance of seeing a dentist regularly, and provide referrals when appropriate. Depending upon the patient’s oral health, dentists recommend patients with xerostomia have their teeth cleaned/examined 3 or 4 times per year, rather than the 2 times per year allowed by third-party payers (ie, insurance companies). Also advise patients to be diligent in their oral hygiene practices, including flossing and brushing the teeth and tongue, and to avoid foods that are sticky and/or have high sucrose content (Table 2). Recommend using a toothpaste containing fluoride—preferably one free of sodium lauryl sulfate, which could contribute to mouth sores14—and drinking fluoridated water. Explain to patients that their dentist may recommend in-office high-fluoride applications, high-fluoride prescription toothpaste, and/or “mouth trays” that contain high fluoride gel. Tell patients to avoid cigarettes and caffeinated beverages, which can increase dryness. Alcohol use should be minimized and mouth rinses containing alcohol should not be used.
Many over-the-counter products are available to address xerostomia, including toothpastes, mouth rinses, and gels. Salivary substitutes—which are available as sprays, liquids, tablets, and swab sticks—imitate saliva and may provide a temporary reprieve from dryness. Although none of these products will cure dry mouth, they may help manage the condition. Advise patients to eat foods that stimulate saliva production, such as carrots, apples, and celery, and to chew sugarless gum and candies, which also will stimulate salivary flow.
The FDA has approved 2 prescription drugs for treating xerostomia: cevimeline and pilocarpine. Cevimeline is approved for treating dry mouth associated with Sjögren’s syndrome and pilocarpine is approved for treating dry mouth caused by head and neck radiation therapy; however, these medications’ role in treating dry mouth in psychiatric patients has not been investigated. Both agents are contraindicated in patients with narrow-angle glaucoma, uncontrolled asthma, or liver disease, and should be prescribed with caution for patients with cardiovascular disease, chronic respiratory conditions, or kidney disease.32
Acupuncture and electrostimulation are being studied as a treatment for xerostomia. Trials have found acupuncture improves symptoms of xerostomia,33,34 and 1 study found electrostimulation improved xerostomia in patients with Sjögren’s syndrome.35 Both approaches require more study to confirm their effectiveness.33-35
Table 2
Managing dry mouth: What to tell patients
| Oral hygiene. Tell patients to be diligent in their oral hygiene practices, including brushing and flossing. They should use a toothpaste containing fluoride—preferably one free of sodium lauryl sulfate—and schedule regular dental visits, where they can receive high-fluoride applications or be prescribed high-fluoride prescription toothpastes |
| Diet. Advise patients to avoid foods high in sucrose content, rinse their mouth with water soon after eating, and drink fluoridated water regularly. Tell them that they may be able to stimulate saliva flow with sugarless gum, candies, and foods such as celery and carrots |
| Drying agents. Instruct patients to avoid cigarettes, caffeinated beverages, and mouth rinses that contain alcohol. Explain that some patients may benefit from sleeping in a room with a cool air humidifier |
| Over-the-counter products. Suggest patients try salivary substitutes, which are dispensed in spray bottles, rinses, swish bottles, or oral swab sticks. In addition, products such as dry-mouth toothpaste and moisturizing gels also may help relieve their symptoms |
- Persson K, Axtelius B, Söderfeldt B, et al. Monitoring oral health and dental attendance in an outpatient psychiatric population. J Psychiatr Ment Health Nurs. 2009;16(3):263-271.
- Keene JJ Jr, Galasko GT, Land MF. Antidepressant use in psychiatry and medicine: importance for dental practice. J Am Dent Assoc. 2003;134(1):71-79.
Drug Brand Names
- Alprazolam • Xanax
- Amlodipine • Norvasc
- Bupropion • Wellbutrin, Zyban
- Cevimeline • Evoxac
- Clonidine • Catapres, Kapvay, others
- Esomeprazole • Nexium
- Irbesartan • Avapro
- Metoprolol • Lopressor, Toprol
- Pilocarpine • Salagen
- Tolterodine • Detrol
- Venlafaxine • Effexor
- Zolpidem • Ambien
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Drymouth.info. Overview of drugs and dry mouth. http://drymouth.info/practitioner/overview.asp. Accessed September 2, 2011.
2. Stewart CM, Berg KM, Cha S, et al. Salivary dysfunction and quality of life in Sjögren syndrome: a critical oral-systemic connection. J Am Dent Assoc. 2008;139(3):291-299.
3. Friedman PK. Xerostomia: The invisible oral health condition. http://www.dentistryiq.com/index/display/article-display/295922/articles/woman-dentist-journal/health/xerostomia-the-invisible-oral-health-condition.html. Accessed September 6, 2011.
4. Physician Desk Reference. Montvale NJ: PDR Network LLC.; 2011.
5. Bardow A, Lagerlof F, Nauntofte B, et al. The role of saliva. In: Fejerskov O, Kidd E, eds. Dental caries: the disease and its clinical management. Oxford, United Kingdom: Blackwell Munksgaard; 2008:195.
6. Vanderkooy JD, Kennedy SH, Bagby RM. Antidepressant side effects in depression patients treated in a naturalistic setting: a study of bupropion moclobemide, paroxetine, sertraline, and venlafaxine. Can J Psychiatry. 2002;47(2):174-180.
7. Löffler W, Kilian R, Toumi M, et al. Schizophrenic patients’ subjective reasons for compliance and noncompliance with neuroleptic treatment. Pharmacopsychiatry. 2003;36(3):105-112.
8. Lambert M, Conus P, Eide P, et al. Impact of present and past antipsychotic side effects on attitude toward typical antipsychotic treatment and adherence. Eur Psychiatry. 2004;19(7):415-422.
9. Rettenbacher MA, Hofer A, Eder U, et al. Compliance in schizophrenia: psychopathology, side effects, and patients’ attitudes toward the illness and medication. J Clin Psychiatry. 2004;65(9):1211-1218.
10. Bulkacz J, Carranza FA. Defense mechanisms of the gingiva. In: Newman MG, Takei HH, Klokkevold PR, et al, eds. Carranza’s clinical periodontology. St. Louis, MO: Elsevier Saunders; 2011:69–70.
11. Szabadi E, Tavernor S. Hypo-and hyper-salivation induced by psychoactive drugs. CNS Drugs. 1999;11(6):449-466.
12. Guggenheimer J, Moore PA. Xerostomia: etiology recognition and treatment. J Am Dent Assoc. 2003;134(1):61-69.
13. Dawes C. Physiological factors affecting salivary flow rate oral sugar clearance, and the sensation of dry mouth in man. J Dent Res. 1987;66:648-653.
14. Bartels CL. Xerostomia information for dentists. http://www.homesteadschools.com/dental/courses/Xerostomia/Course.htm. Accessed August 15, 2011.
15. Sitheeque MA, Samaranayake LP. Chronic hyperplastic candidosis/candidiasis (candidal leukoplakia). Crit Rev Oral Biol Med. 2003;14(4):253-267.
16. Porter SR, Scully C. Oral malodour (halitosis). BMJ. 2006;333(7569):632-635.
17. Quirynen M, Van den Veide S, Vanderkerckhove B, et al. Oral malodor. In: Newman MG, Takei HH, Klokkevold PR, et al, eds. Carranza’s clinical periodontology. St. Louis, MO: Elsevier Saunders; 2011:333.
18. Papas A. Dry mouth from drugs: more than just an annoying side effect. Tufts University Heath and Nutrition Letter. 2000;3.-
19. American Academy of Periodontology. Gum disease information from the American Academy of Periodontology http://perio.org. Accessed August 12, 2011.
20. Geismar K, Stoltze K, Sigurd B, et al. Periodontal disease and coronary heart disease. J Periodontol. 2006;77(9):1547-1554.
21. Lee HJ, Garcia RI, Janket SJ, et al. The association between cumulative periodontal disease and stroke history in older adults. J Periodontol. 2006;77(10):1744-1754.
22. Friedewald VE, Kornman KS, Beck JD, et al. The American Journal of Cardiology and Journal of Periodontology editors’ consensus: periodontitis and atherosclerotic cardiovascular disease. J Periodontol. 2009;80(7):1021-1032.
23. Contreras A, Herrera JA, Soto JE, et al. Periodontitis is associated with preeclampsia in pregnant women. J Periodontol. 2006;77(2):182-188.
24. Dasanayake AP, Li Y, Wiener H, et al. Salivary Actinomyces naeslundii genospecies 2 and Lactobacillus casei levels predict pregnancy outcomes. J Periodontol. 2005;76(2):171-177.
25. McCreadie RG, Stevens H, Henderson J, et al. The dental health of people with schizophrenia. Acta Psychiatr Scand. 2004;110(4):306-310.
26. Anttila S, Knuuttila M, Ylöstalo P, et al. Symptoms of depression and anxiety in relation to dental health behavior and self-perceived dental treatment need. Eur J Oral Sci. 2006;114(2):109-114.
27. Sjögren R, Nordström G. Oral health status of psychiatric patients. J Clin Nurs. 2000;9(4):632-638.
28. Ramon T, Grinshpoon A, Zusman SP, et al. Oral health and treatment needs of institutionalized chronic psychiatric patients in Israel. Eur Psychiatry. 2003;18(3):101-105.
29. Portilla MI, Mafla AC, Arteaga JJ. Periodontal status in female psychiatric patients. Colomb Med. 2009;40(2):167-176.
30. Navazesh M. ADA Council on Scientific Affairs and Division of Science. How can oral health care providers determine if patients have dry mouth? J Am Dent Assoc. 2003;134(5):613-620.
31. Mignogna MD, Fedele S, Lo Russo L, et al. Sjögren’s syndrome: the diagnostic potential of early oral manifestations preceding hyposalivation/xerostomia. J Oral Pathol Med. 2005;34(1):1-6.
32. Spolarich AE. Managing the side effects of medications. J Dent Hyg. 2000;74(1):57-69.
33. Johnstone PA, Niemtzow RC, Riffenburgh RH. Acupuncture for xerostomia: clinical update. Cancer. 2002;94(4):1151-1156.
34. Garcia MK, Chiang JS, Cohen L, et al. Acupuncture for radiation-induced xerostomia in patients with cancer: a pilot study. Head Neck. 2009;31(10):1360-1368.
35. Strietzel FP, Lafaurie GI, Mendoza GR, et al. Efficacy and safety of an intraoral electrostimulation device for xerostomia relief: a multicenter, randomized trial. Arthritis Rheum. 2011;63(1):180-190.
1. Drymouth.info. Overview of drugs and dry mouth. http://drymouth.info/practitioner/overview.asp. Accessed September 2, 2011.
2. Stewart CM, Berg KM, Cha S, et al. Salivary dysfunction and quality of life in Sjögren syndrome: a critical oral-systemic connection. J Am Dent Assoc. 2008;139(3):291-299.
3. Friedman PK. Xerostomia: The invisible oral health condition. http://www.dentistryiq.com/index/display/article-display/295922/articles/woman-dentist-journal/health/xerostomia-the-invisible-oral-health-condition.html. Accessed September 6, 2011.
4. Physician Desk Reference. Montvale NJ: PDR Network LLC.; 2011.
5. Bardow A, Lagerlof F, Nauntofte B, et al. The role of saliva. In: Fejerskov O, Kidd E, eds. Dental caries: the disease and its clinical management. Oxford, United Kingdom: Blackwell Munksgaard; 2008:195.
6. Vanderkooy JD, Kennedy SH, Bagby RM. Antidepressant side effects in depression patients treated in a naturalistic setting: a study of bupropion moclobemide, paroxetine, sertraline, and venlafaxine. Can J Psychiatry. 2002;47(2):174-180.
7. Löffler W, Kilian R, Toumi M, et al. Schizophrenic patients’ subjective reasons for compliance and noncompliance with neuroleptic treatment. Pharmacopsychiatry. 2003;36(3):105-112.
8. Lambert M, Conus P, Eide P, et al. Impact of present and past antipsychotic side effects on attitude toward typical antipsychotic treatment and adherence. Eur Psychiatry. 2004;19(7):415-422.
9. Rettenbacher MA, Hofer A, Eder U, et al. Compliance in schizophrenia: psychopathology, side effects, and patients’ attitudes toward the illness and medication. J Clin Psychiatry. 2004;65(9):1211-1218.
10. Bulkacz J, Carranza FA. Defense mechanisms of the gingiva. In: Newman MG, Takei HH, Klokkevold PR, et al, eds. Carranza’s clinical periodontology. St. Louis, MO: Elsevier Saunders; 2011:69–70.
11. Szabadi E, Tavernor S. Hypo-and hyper-salivation induced by psychoactive drugs. CNS Drugs. 1999;11(6):449-466.
12. Guggenheimer J, Moore PA. Xerostomia: etiology recognition and treatment. J Am Dent Assoc. 2003;134(1):61-69.
13. Dawes C. Physiological factors affecting salivary flow rate oral sugar clearance, and the sensation of dry mouth in man. J Dent Res. 1987;66:648-653.
14. Bartels CL. Xerostomia information for dentists. http://www.homesteadschools.com/dental/courses/Xerostomia/Course.htm. Accessed August 15, 2011.
15. Sitheeque MA, Samaranayake LP. Chronic hyperplastic candidosis/candidiasis (candidal leukoplakia). Crit Rev Oral Biol Med. 2003;14(4):253-267.
16. Porter SR, Scully C. Oral malodour (halitosis). BMJ. 2006;333(7569):632-635.
17. Quirynen M, Van den Veide S, Vanderkerckhove B, et al. Oral malodor. In: Newman MG, Takei HH, Klokkevold PR, et al, eds. Carranza’s clinical periodontology. St. Louis, MO: Elsevier Saunders; 2011:333.
18. Papas A. Dry mouth from drugs: more than just an annoying side effect. Tufts University Heath and Nutrition Letter. 2000;3.-
19. American Academy of Periodontology. Gum disease information from the American Academy of Periodontology http://perio.org. Accessed August 12, 2011.
20. Geismar K, Stoltze K, Sigurd B, et al. Periodontal disease and coronary heart disease. J Periodontol. 2006;77(9):1547-1554.
21. Lee HJ, Garcia RI, Janket SJ, et al. The association between cumulative periodontal disease and stroke history in older adults. J Periodontol. 2006;77(10):1744-1754.
22. Friedewald VE, Kornman KS, Beck JD, et al. The American Journal of Cardiology and Journal of Periodontology editors’ consensus: periodontitis and atherosclerotic cardiovascular disease. J Periodontol. 2009;80(7):1021-1032.
23. Contreras A, Herrera JA, Soto JE, et al. Periodontitis is associated with preeclampsia in pregnant women. J Periodontol. 2006;77(2):182-188.
24. Dasanayake AP, Li Y, Wiener H, et al. Salivary Actinomyces naeslundii genospecies 2 and Lactobacillus casei levels predict pregnancy outcomes. J Periodontol. 2005;76(2):171-177.
25. McCreadie RG, Stevens H, Henderson J, et al. The dental health of people with schizophrenia. Acta Psychiatr Scand. 2004;110(4):306-310.
26. Anttila S, Knuuttila M, Ylöstalo P, et al. Symptoms of depression and anxiety in relation to dental health behavior and self-perceived dental treatment need. Eur J Oral Sci. 2006;114(2):109-114.
27. Sjögren R, Nordström G. Oral health status of psychiatric patients. J Clin Nurs. 2000;9(4):632-638.
28. Ramon T, Grinshpoon A, Zusman SP, et al. Oral health and treatment needs of institutionalized chronic psychiatric patients in Israel. Eur Psychiatry. 2003;18(3):101-105.
29. Portilla MI, Mafla AC, Arteaga JJ. Periodontal status in female psychiatric patients. Colomb Med. 2009;40(2):167-176.
30. Navazesh M. ADA Council on Scientific Affairs and Division of Science. How can oral health care providers determine if patients have dry mouth? J Am Dent Assoc. 2003;134(5):613-620.
31. Mignogna MD, Fedele S, Lo Russo L, et al. Sjögren’s syndrome: the diagnostic potential of early oral manifestations preceding hyposalivation/xerostomia. J Oral Pathol Med. 2005;34(1):1-6.
32. Spolarich AE. Managing the side effects of medications. J Dent Hyg. 2000;74(1):57-69.
33. Johnstone PA, Niemtzow RC, Riffenburgh RH. Acupuncture for xerostomia: clinical update. Cancer. 2002;94(4):1151-1156.
34. Garcia MK, Chiang JS, Cohen L, et al. Acupuncture for radiation-induced xerostomia in patients with cancer: a pilot study. Head Neck. 2009;31(10):1360-1368.
35. Strietzel FP, Lafaurie GI, Mendoza GR, et al. Efficacy and safety of an intraoral electrostimulation device for xerostomia relief: a multicenter, randomized trial. Arthritis Rheum. 2011;63(1):180-190.
How proposed changes to personality disorders in DSM-5 will affect researchers
A complex subject
Thank you for your excellent article “Pharmacologic treatment of borderline personality disorder” (Current Psychiatry, August 2011, p. 30-40). This subject is very complex and poorly understood, both in primary diagnosis and the implications it has on other axis I conditions. Your attempts to educate and suggest possible treatment options are appreciated.
Bruce Miller, PA-C
Department of Corrections
VA Medical Center
Sartell, MN
Thank you for your excellent article “Pharmacologic treatment of borderline personality disorder” (Current Psychiatry, August 2011, p. 30-40). This subject is very complex and poorly understood, both in primary diagnosis and the implications it has on other axis I conditions. Your attempts to educate and suggest possible treatment options are appreciated.
Bruce Miller, PA-C
Department of Corrections
VA Medical Center
Sartell, MN
Thank you for your excellent article “Pharmacologic treatment of borderline personality disorder” (Current Psychiatry, August 2011, p. 30-40). This subject is very complex and poorly understood, both in primary diagnosis and the implications it has on other axis I conditions. Your attempts to educate and suggest possible treatment options are appreciated.
Bruce Miller, PA-C
Department of Corrections
VA Medical Center
Sartell, MN
Redefining personality disorders: Proposed revisions for DSM-5
A major update to the diagnostic manual used by mental health clinicians around the world is expected to inspire lively debate. Proposed revisions to the personality disorders (PD) section of the next edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), which is scheduled to be published in 2013, have generated great controversy because they would introduce a dimensional model to the categorical system and 4 PDs would be eliminated.
“The importance of personality functioning and personality traits is the major innovation here,” said Andrew Skodol, MD, the DSM-5 Personality and Personality Disorders Work Group’s chair and a Research Professor of Psychiatry at the University of Arizona College of Medicine. “In the past, we viewed personality disorders as binary. You either had one or you didn’t. But we now understand that personality pathology is a matter of degree.”1
Mark Zimmerman, MD, has written several papers—some of which are in press—about how these revisions might impact clinicians and whether the revisions are necessary. He is Director of the Rhode Island Methods to Improve Diagnostic Assessment and Services (MIDAS) project, an ongoing clinical research study involving the integration of research assessment methods into clinical practice.
Proposed revisions, rationale, and literature reviews for DSM-5 are available at www.DSM5.org and anyone, including the general public, was invited to provide feedback through the Web site. Current Psychiatry Associate Editor Donald W. Black, MD, interviewed Dr. Zimmerman on June 29, 2011, just a few days after the latest proposed revision was posted on June 21, 2011.
DR. BLACK: What is your understanding of the DSM-5 Personality Disorders Work Group proposal to revamp the PD category?
DR. ZIMMERMAN: The initial proposal, released in February 2010, was complex and generated a fair amount of critical commentary related to the marked changes in the approach toward diagnosis of PDs. That proposal replaced diagnostic criteria with a prototype description of personality types that patients would need to match. It also eliminated 5 PDs—paranoid, schizoid, histrionic, dependent, and narcissistic—retained antisocial, avoidant, borderline, obsessive-compulsive, and schizotypal, and introduced trait level ratings. The June 21 revision proposes eliminating only 4 disorders—narcissistic was retained—and the Work Group is no longer suggesting using prototypes but instead have diagnostic criteria (Table).2,3 We do not know if this is the final proposal because similar to the first proposal, it is not presented with much supporting empirical evidence that demonstrates its superiority toward diagnosing PDs compared with the DSM-IV approach.
Table
Personality disorder criteria: DSM-IV vs DSM-5
| DSM-IV | DSM-5 proposal (posted June 21, 2011) |
|---|---|
| General diagnostic criteria | |
|
|
| Personality disorders included | |
| Antisocial, avoidant, borderline, dependent, histrionic, narcissistic, obsessive-compulsive, paranoid, schizoid, schizotypal, personality disorder not otherwise specified | Antisocial, avoidant, borderline, narcissistic, obsessive-compulsive, schizotypal, personality disorder trait specified (requires a rating of significant impairment in personality functioning, combined with the presence of pathological trait domains or facets) |
| Source: References 2,3 | |
I’m not suggesting that the DSM-IV approach is without problems. My attitude is that before going forward with a change to the official diagnostic nomenclature, you need to clearly establish that the new way of doing things is better than the previous way by whatever metric you use.
DR. BLACK: Do you believe there is a need to revamp or revise the DSM-IV PD criteria?
DR. ZIMMERMAN: I think a number of the arguments put forth by the DSM-5 Work Group as justifications for revising the criteria do not hold up to empirical study.
One of the issues is the argument that there’s too much comorbidity among PDs. The theory is that disorders are not unique diagnostic entities if they are so frequently comorbid with other disorders. But how much comorbidity is too much? The DSM-5 Work Group doesn’t say. Oldham et al4 found comorbidity rates of 70% to 90%, depending on which semi-structured diagnostic interview was used; however, this was among individuals presenting for psychodynamic treatment of PDs.
I wanted to look at the comorbidity rates in nontreatment-seeking samples to find out if treatment seeking is associated with comorbidity. I reviewed the literature and identified 7 general population epidemiological studies that presented data on the number of individuals with ≥2 PD diagnoses. In these studies, the comorbidity rate is approximately 25%, which is one-half or less than the rates found in patient populations.5 This finding suggested to me that this may not be a nosology problem unless you think 25% comorbidity is too high. The DSM-5 people don’t speak to that, although quite frankly with 10 PDs I don’t think the 25% comorbidity rate is excessive. However, a comorbidity rate of 25% was much lower than that found in patient samples and suggests to me that one of the primary stated reasons of deleting 4 PDs may not be valid.
DR. BLACK: Assuming there is a need to revise the PD section, how would you have gone about that process?
DR. ZIMMERMAN: Whatever deficiencies you perceive in the criteria, the process should be that you come up with an alternative, examine the alternative empirically, and this is followed by independent replication that the new approach is superior to the prior one. My view is that it is not sufficient justification to make a change because there is a problem with the prior approach.
We can argue as to whether there really are problems with, for example, the categorical nature of classification. My research group and I wrote a paper arguing that DSM-IV can be interpreted as having a dimensional component (Box).6 DSM-IV suggests that clinicians record on axis II that a patient has some traits of a disorder even when the full criteria are not met. With that in mind, we conceptualized DSM-IV as having a 3-point dimension, where 0 means no traits of the disorder, 1 indicates subthreshold traits, and 2 indicates that the disorder is present. In a study of >2,000 patients, we found that DSM-IV’s 3-point dimensional approach was as highly associated with measures of psychosocial morbidity as more finely graded dimensional systems.6 We therefore concluded that DSM-IV already includes a dimensional system and questioned why we need to change that approach.
Zimmerman et al suggested that DSM-IV personality disorder (PD) criteria can be thought of as a dimensional system.6 They evaluated 2,150 psychiatric outpatients using semi-structured diagnostic interviews and computed dimensional PD scores in 3 ways:
- 3-point dimension, where 0 means no traits of the disorder, 1 indicates subthreshold traits, and 2 indicates that the disorder is present
- number of DSM-IV criteria met
- 5-point dimension analogous to what was being proposed for DSM-5.
Patients also were evaluated for the presence of a PD based on DSM-IV diagnostic threshold. They then correlated these assessment methods with 7 indices of psychosocial morbidity—the number of current axis I disorders, Global Assessment of Functioning scores, unemployment in the past 5 years, number of psychiatric hospitalizations, level of psychosocial functioning, suicidal ideation at the time of the evaluation, and number of lifetime suicide attempts. All methods of dimensional assessment were more highly correlated with psychosocial morbidity than categorical classification and there was no difference among the 3 dimensional methods.
One of my concerns with the dimensional system as currently proposed is the uncertain significance and possible implications of someone being given a low, non-zero rating. How might this play out in a custody evaluation of someone who is said to be “a little borderline”? What might the implications of non-zero ratings be in obtaining life insurance? The potential practical consequences of low ratings have not, to my knowledge, been discussed. Because of this concern we decided to do a study to determine if there was any clinical significance to low dimensional scores. I had hypothesized that if we compared individuals who had no criteria and only 1 BPD criterion, there would be no difference.
To be frank, I was seeking to show that there was no validity to low levels of pathology and therefore the DSM-5 group probably is getting into dangerous territory. In fact, we found that there were rather significant and robust differences between individuals with 0 criteria and 1 criterion.7 Even though this finding didn’t support my hypothesis, I thought it was significant because it supported the DSM-5 Work Group and I felt compelled to publish that data.
We now had 2 interesting pieces of information. A few years ago we published a study on borderline personality disorder (BPD) that found once you hit the diagnostic threshold it made no difference how many criteria you met.8 On the other hand, when you were below the diagnostic threshold, having 1 criterion vs 0 made a big difference. In addition, a fair number of studies show that dimensional models capture more of the variance in personality pathology than categorical variables.9-12
This lead to our next study in which we hypothesized that dimensionality was only important when the person didn’t meet criteria, not when they did meet criteria.13 So we divided patients in the MIDAS study into those with 0 to 4 BPD criteria and those with ≥5 and counted the number of criteria that were met. Then we correlated each of those 2 dimensional scores with various indicators of illness severity, such as number of suicide attempts, number of psychiatric hospitalizations, and amount of time missed from work in the past 5 years. We found that for individuals who already achieved the diagnostic threshold there were very low correlations with these psychosocial morbidity variables. But for patients with subthreshold symptomatology, there were significant correlations and those correlations were significantly higher than the correlations for the other group. We therefore suggested that dimensionality is important but only when you don’t meet the diagnostic threshold. Thus, we came to the conclusion that DSM-IV already provides for capturing the important dimensional nature of PDs.
DR. BLACK: I’ve discussed this issue with a number of people who basically say doctors tend to think categorically, they don’t think along dimensions. Would it be difficult for psychiatrists to accept this type of system because it’s so different from how physicians are trained to think?
DR. ZIMMERMAN: I think doctors do think categorically and about traits, not necessarily disorders. For example, we’ll see a patient and a clinician will say he’s overly perfectionistic, but there’s no perfectionistic disorder in DSM-IV. This patient may or may not have obsessive-compulsive personality disorder.
I think assessment and diagnosis in routine clinical practice are not nearly as comprehensive as in research. I think psychiatrists often are picking up on traits that they think are clinically significant, but even within that context, they’re thinking categorically, that the patient is perfectionistic rather than rating him a 7 on a scale from 0 to 10 in terms of perfectionism.
Eliminated disorders
DR. BLACK: The proposal will cut the number of PDs to 6 plus personality disorder trait specified and those remaining are to be called types. How did the DSM-5 Work Group select the 5 (now 4) disorders to get rid of? Did they just pick ones that were infrequently used?
DR. ZIMMERMAN: They retained the disorders that were studied in the Collaborative Longitudinal Personality Disorders Study study14 plus others with well established validity.
DR. BLACK: What do you think about that plan to reduce the number of PDs?
DR. ZIMMERMAN: The biggest problem I have is that the DSM-5 Work Group didn’t present any data on the implications of their plan. The conceptual justification was to reduce comorbidity rates. Well, you can hypothesize that comorbidity would actually increase if you retained only those disorders that are more frequently comorbid with other disorders. Would there be any individuals who only have 1 of the excluded diagnoses? Would there be false negatives? They didn’t indicate whether comorbidity would drop and by how much. And they didn’t indicate if there would be a potential impact on missing cases.
We did such an analysis because we had the data set available from the MIDAS project.15 We wanted to know if you excluded the 5 diagnoses that (at the time) were proposed for exclusion—narcissistic, paranoid, schizoid, dependent, and histrionic—what percentage of individuals would no longer be diagnosed with a PD? Second, how much would comorbidity rates change? And third, how did individuals who would no longer be diagnosed with a PD compare with individuals who never had a PD?
We found that the comorbidity rates did, in fact, drop from 30% to 21%. We found that the rate of PDs dropped only a little, but approximately 10% of individuals who previously would have been diagnosed with a PD would no longer be diagnosed. We compared individuals in the excluded group—those who had only 1 of the PDs that would no longer be considered a PD—with a group of patients who had a retained PD and also compared them to individuals with no PD. We found that the retained PD group and the excluded group did not differ on measures of psychosocial morbidity, such as Global Assessment of Functioning scores, hospitalizations, suicidality, number of current axis I disorders, etc. Also, the excluded group clearly was different than the no PD group. We questioned whether or not those in the excluded group might end up being false negative diagnoses in DSM-5. Certainly DSM-5 provides a provision to use trait ratings to still diagnose a PD, called personality disorder trait specified, which would be somewhat analogous to PD not otherwise specified (NOS).
It’s ironic insofar as another of the issues considered by the DSM-5 Work Group to be a problem with axis II is lack of coverage and that too many individuals are diagnosed with PD NOS. Their proposal to exclude PDs could result in more individuals being diagnosed with PD NOS. I know the group would disagree with that perspective, but they provided no evidence to support its view.
As I said at the beginning of this interview, I think we should be talking about this from a scientific perspective and nothing more than that.
Related Resource
- Widiger TA, Simonsen E, Sirovatka PJ, et al. Dimensional models of personality disorders: Refining the research agenda for DSM-V. Arlington, VA: American Psychiatric Publishing, Inc; 2007.
Disclosures
- Dr. Zimmerman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
- Dr. Black receives research support from AstraZeneca and Psyadon.
1. DSM-5 revisions for personality disorders reflect major change. Public comment period for proposed diagnostic criteria extended through July 15 [news release]. Arlington, VA: American Psychiatric Association; July 7, 2011. http://www.psych.org/MainMenu/Newsroom/NewsReleases/2011-News-Releases_1/DSM-5-Revisions-for-Personality-Disorders-Reflect-Major-Change-.aspx?FT=.pdf. Accessed July 26, 2011.
2. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
3. Personality disorders. American Psychiatric Association DSM-5 development. http://www.dsm5.org/proposedrevision/Pages/PersonalityDisorders.aspx. Updated June 21, 2011. Accessed July 26, 2011.
4. Oldham JM, Skodol AE, Kellman HD, et al. Diagnosis of DSM-III-R personality disorders by two structured interviews: patterns of comorbidity. Am J Psychiatry. 1992;149(2):213-220.
5. Zimmerman M. Is there adequate empirical justification for radically revising the personality disorders section for DSM-5? Personality Disorders: Theory, Research and Treatment. In press.
6. Zimmerman M, Chelminski I, Young D, et al. Does DSM-IV already capture the dimensional nature of personality disorders? J Clin Psychiatry. In press.
7. Zimmerman M, Chelminski I, Young D, et al. Does the presence of one feature of borderline personality disorder have clinical significance?: Implications for dimensional ratings of personality disorders. J Clin Psychiatry. In press.
8. Asnaani A, Chelminski I, Young D, et al. Heterogeneity of borderline personality disorder: do the number of criteria met make a difference? J Pers Disord. 2007;21(6):615-625.
9. Skodol AE, Oldham JM, Bender DS, et al. Dimensional representations of DSM-IV personality disorders: relationships to functional impairment. Am J Psychiatry. 2005;162:1919-1925.
10. Durbin CE, Klein DN. Ten-year stability of personality disorders among outpatients with mood disorders. J Abnorm Psychol. 2006;115:75-84.
11. Grilo CM, Sanislow CA, Gunderson JG, et al. Two-year stability and change of schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders. J Consult Clin Psychol. 2004;72:767-775.
12. Morey LC, Hopwood CJ, Gunderson JG, et al. Comparison of alternative models for personality disorders. Psychol Med. 2007;37:983-994.
13. Zimmerman M, Chelminski I, Young D, et al. Is dimensional scoring of borderline personality disorder only important for subthreshold levels of severity? J Pers Disord. In press.
14. Gunderson JG, Shea MT, Skodol AE, et al. The Collaborative Longitudinal Personality Disorders Study: development, aims, design, and sample characteristics. J Pers Disord. 2000;14(4):300-315.
15. Zimmerman M, Chelminski I, Young D, et al. Impact of deleting 5 DSM-IV personality disorders on prevalence, comorbidity, and the association between personality disorder pathology and psychosocial morbidity. J Clin Psychiatry. In press.
A major update to the diagnostic manual used by mental health clinicians around the world is expected to inspire lively debate. Proposed revisions to the personality disorders (PD) section of the next edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), which is scheduled to be published in 2013, have generated great controversy because they would introduce a dimensional model to the categorical system and 4 PDs would be eliminated.
“The importance of personality functioning and personality traits is the major innovation here,” said Andrew Skodol, MD, the DSM-5 Personality and Personality Disorders Work Group’s chair and a Research Professor of Psychiatry at the University of Arizona College of Medicine. “In the past, we viewed personality disorders as binary. You either had one or you didn’t. But we now understand that personality pathology is a matter of degree.”1
Mark Zimmerman, MD, has written several papers—some of which are in press—about how these revisions might impact clinicians and whether the revisions are necessary. He is Director of the Rhode Island Methods to Improve Diagnostic Assessment and Services (MIDAS) project, an ongoing clinical research study involving the integration of research assessment methods into clinical practice.
Proposed revisions, rationale, and literature reviews for DSM-5 are available at www.DSM5.org and anyone, including the general public, was invited to provide feedback through the Web site. Current Psychiatry Associate Editor Donald W. Black, MD, interviewed Dr. Zimmerman on June 29, 2011, just a few days after the latest proposed revision was posted on June 21, 2011.
DR. BLACK: What is your understanding of the DSM-5 Personality Disorders Work Group proposal to revamp the PD category?
DR. ZIMMERMAN: The initial proposal, released in February 2010, was complex and generated a fair amount of critical commentary related to the marked changes in the approach toward diagnosis of PDs. That proposal replaced diagnostic criteria with a prototype description of personality types that patients would need to match. It also eliminated 5 PDs—paranoid, schizoid, histrionic, dependent, and narcissistic—retained antisocial, avoidant, borderline, obsessive-compulsive, and schizotypal, and introduced trait level ratings. The June 21 revision proposes eliminating only 4 disorders—narcissistic was retained—and the Work Group is no longer suggesting using prototypes but instead have diagnostic criteria (Table).2,3 We do not know if this is the final proposal because similar to the first proposal, it is not presented with much supporting empirical evidence that demonstrates its superiority toward diagnosing PDs compared with the DSM-IV approach.
Table
Personality disorder criteria: DSM-IV vs DSM-5
| DSM-IV | DSM-5 proposal (posted June 21, 2011) |
|---|---|
| General diagnostic criteria | |
|
|
| Personality disorders included | |
| Antisocial, avoidant, borderline, dependent, histrionic, narcissistic, obsessive-compulsive, paranoid, schizoid, schizotypal, personality disorder not otherwise specified | Antisocial, avoidant, borderline, narcissistic, obsessive-compulsive, schizotypal, personality disorder trait specified (requires a rating of significant impairment in personality functioning, combined with the presence of pathological trait domains or facets) |
| Source: References 2,3 | |
I’m not suggesting that the DSM-IV approach is without problems. My attitude is that before going forward with a change to the official diagnostic nomenclature, you need to clearly establish that the new way of doing things is better than the previous way by whatever metric you use.
DR. BLACK: Do you believe there is a need to revamp or revise the DSM-IV PD criteria?
DR. ZIMMERMAN: I think a number of the arguments put forth by the DSM-5 Work Group as justifications for revising the criteria do not hold up to empirical study.
One of the issues is the argument that there’s too much comorbidity among PDs. The theory is that disorders are not unique diagnostic entities if they are so frequently comorbid with other disorders. But how much comorbidity is too much? The DSM-5 Work Group doesn’t say. Oldham et al4 found comorbidity rates of 70% to 90%, depending on which semi-structured diagnostic interview was used; however, this was among individuals presenting for psychodynamic treatment of PDs.
I wanted to look at the comorbidity rates in nontreatment-seeking samples to find out if treatment seeking is associated with comorbidity. I reviewed the literature and identified 7 general population epidemiological studies that presented data on the number of individuals with ≥2 PD diagnoses. In these studies, the comorbidity rate is approximately 25%, which is one-half or less than the rates found in patient populations.5 This finding suggested to me that this may not be a nosology problem unless you think 25% comorbidity is too high. The DSM-5 people don’t speak to that, although quite frankly with 10 PDs I don’t think the 25% comorbidity rate is excessive. However, a comorbidity rate of 25% was much lower than that found in patient samples and suggests to me that one of the primary stated reasons of deleting 4 PDs may not be valid.
DR. BLACK: Assuming there is a need to revise the PD section, how would you have gone about that process?
DR. ZIMMERMAN: Whatever deficiencies you perceive in the criteria, the process should be that you come up with an alternative, examine the alternative empirically, and this is followed by independent replication that the new approach is superior to the prior one. My view is that it is not sufficient justification to make a change because there is a problem with the prior approach.
We can argue as to whether there really are problems with, for example, the categorical nature of classification. My research group and I wrote a paper arguing that DSM-IV can be interpreted as having a dimensional component (Box).6 DSM-IV suggests that clinicians record on axis II that a patient has some traits of a disorder even when the full criteria are not met. With that in mind, we conceptualized DSM-IV as having a 3-point dimension, where 0 means no traits of the disorder, 1 indicates subthreshold traits, and 2 indicates that the disorder is present. In a study of >2,000 patients, we found that DSM-IV’s 3-point dimensional approach was as highly associated with measures of psychosocial morbidity as more finely graded dimensional systems.6 We therefore concluded that DSM-IV already includes a dimensional system and questioned why we need to change that approach.
Zimmerman et al suggested that DSM-IV personality disorder (PD) criteria can be thought of as a dimensional system.6 They evaluated 2,150 psychiatric outpatients using semi-structured diagnostic interviews and computed dimensional PD scores in 3 ways:
- 3-point dimension, where 0 means no traits of the disorder, 1 indicates subthreshold traits, and 2 indicates that the disorder is present
- number of DSM-IV criteria met
- 5-point dimension analogous to what was being proposed for DSM-5.
Patients also were evaluated for the presence of a PD based on DSM-IV diagnostic threshold. They then correlated these assessment methods with 7 indices of psychosocial morbidity—the number of current axis I disorders, Global Assessment of Functioning scores, unemployment in the past 5 years, number of psychiatric hospitalizations, level of psychosocial functioning, suicidal ideation at the time of the evaluation, and number of lifetime suicide attempts. All methods of dimensional assessment were more highly correlated with psychosocial morbidity than categorical classification and there was no difference among the 3 dimensional methods.
One of my concerns with the dimensional system as currently proposed is the uncertain significance and possible implications of someone being given a low, non-zero rating. How might this play out in a custody evaluation of someone who is said to be “a little borderline”? What might the implications of non-zero ratings be in obtaining life insurance? The potential practical consequences of low ratings have not, to my knowledge, been discussed. Because of this concern we decided to do a study to determine if there was any clinical significance to low dimensional scores. I had hypothesized that if we compared individuals who had no criteria and only 1 BPD criterion, there would be no difference.
To be frank, I was seeking to show that there was no validity to low levels of pathology and therefore the DSM-5 group probably is getting into dangerous territory. In fact, we found that there were rather significant and robust differences between individuals with 0 criteria and 1 criterion.7 Even though this finding didn’t support my hypothesis, I thought it was significant because it supported the DSM-5 Work Group and I felt compelled to publish that data.
We now had 2 interesting pieces of information. A few years ago we published a study on borderline personality disorder (BPD) that found once you hit the diagnostic threshold it made no difference how many criteria you met.8 On the other hand, when you were below the diagnostic threshold, having 1 criterion vs 0 made a big difference. In addition, a fair number of studies show that dimensional models capture more of the variance in personality pathology than categorical variables.9-12
This lead to our next study in which we hypothesized that dimensionality was only important when the person didn’t meet criteria, not when they did meet criteria.13 So we divided patients in the MIDAS study into those with 0 to 4 BPD criteria and those with ≥5 and counted the number of criteria that were met. Then we correlated each of those 2 dimensional scores with various indicators of illness severity, such as number of suicide attempts, number of psychiatric hospitalizations, and amount of time missed from work in the past 5 years. We found that for individuals who already achieved the diagnostic threshold there were very low correlations with these psychosocial morbidity variables. But for patients with subthreshold symptomatology, there were significant correlations and those correlations were significantly higher than the correlations for the other group. We therefore suggested that dimensionality is important but only when you don’t meet the diagnostic threshold. Thus, we came to the conclusion that DSM-IV already provides for capturing the important dimensional nature of PDs.
DR. BLACK: I’ve discussed this issue with a number of people who basically say doctors tend to think categorically, they don’t think along dimensions. Would it be difficult for psychiatrists to accept this type of system because it’s so different from how physicians are trained to think?
DR. ZIMMERMAN: I think doctors do think categorically and about traits, not necessarily disorders. For example, we’ll see a patient and a clinician will say he’s overly perfectionistic, but there’s no perfectionistic disorder in DSM-IV. This patient may or may not have obsessive-compulsive personality disorder.
I think assessment and diagnosis in routine clinical practice are not nearly as comprehensive as in research. I think psychiatrists often are picking up on traits that they think are clinically significant, but even within that context, they’re thinking categorically, that the patient is perfectionistic rather than rating him a 7 on a scale from 0 to 10 in terms of perfectionism.
Eliminated disorders
DR. BLACK: The proposal will cut the number of PDs to 6 plus personality disorder trait specified and those remaining are to be called types. How did the DSM-5 Work Group select the 5 (now 4) disorders to get rid of? Did they just pick ones that were infrequently used?
DR. ZIMMERMAN: They retained the disorders that were studied in the Collaborative Longitudinal Personality Disorders Study study14 plus others with well established validity.
DR. BLACK: What do you think about that plan to reduce the number of PDs?
DR. ZIMMERMAN: The biggest problem I have is that the DSM-5 Work Group didn’t present any data on the implications of their plan. The conceptual justification was to reduce comorbidity rates. Well, you can hypothesize that comorbidity would actually increase if you retained only those disorders that are more frequently comorbid with other disorders. Would there be any individuals who only have 1 of the excluded diagnoses? Would there be false negatives? They didn’t indicate whether comorbidity would drop and by how much. And they didn’t indicate if there would be a potential impact on missing cases.
We did such an analysis because we had the data set available from the MIDAS project.15 We wanted to know if you excluded the 5 diagnoses that (at the time) were proposed for exclusion—narcissistic, paranoid, schizoid, dependent, and histrionic—what percentage of individuals would no longer be diagnosed with a PD? Second, how much would comorbidity rates change? And third, how did individuals who would no longer be diagnosed with a PD compare with individuals who never had a PD?
We found that the comorbidity rates did, in fact, drop from 30% to 21%. We found that the rate of PDs dropped only a little, but approximately 10% of individuals who previously would have been diagnosed with a PD would no longer be diagnosed. We compared individuals in the excluded group—those who had only 1 of the PDs that would no longer be considered a PD—with a group of patients who had a retained PD and also compared them to individuals with no PD. We found that the retained PD group and the excluded group did not differ on measures of psychosocial morbidity, such as Global Assessment of Functioning scores, hospitalizations, suicidality, number of current axis I disorders, etc. Also, the excluded group clearly was different than the no PD group. We questioned whether or not those in the excluded group might end up being false negative diagnoses in DSM-5. Certainly DSM-5 provides a provision to use trait ratings to still diagnose a PD, called personality disorder trait specified, which would be somewhat analogous to PD not otherwise specified (NOS).
It’s ironic insofar as another of the issues considered by the DSM-5 Work Group to be a problem with axis II is lack of coverage and that too many individuals are diagnosed with PD NOS. Their proposal to exclude PDs could result in more individuals being diagnosed with PD NOS. I know the group would disagree with that perspective, but they provided no evidence to support its view.
As I said at the beginning of this interview, I think we should be talking about this from a scientific perspective and nothing more than that.
Related Resource
- Widiger TA, Simonsen E, Sirovatka PJ, et al. Dimensional models of personality disorders: Refining the research agenda for DSM-V. Arlington, VA: American Psychiatric Publishing, Inc; 2007.
Disclosures
- Dr. Zimmerman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
- Dr. Black receives research support from AstraZeneca and Psyadon.
A major update to the diagnostic manual used by mental health clinicians around the world is expected to inspire lively debate. Proposed revisions to the personality disorders (PD) section of the next edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), which is scheduled to be published in 2013, have generated great controversy because they would introduce a dimensional model to the categorical system and 4 PDs would be eliminated.
“The importance of personality functioning and personality traits is the major innovation here,” said Andrew Skodol, MD, the DSM-5 Personality and Personality Disorders Work Group’s chair and a Research Professor of Psychiatry at the University of Arizona College of Medicine. “In the past, we viewed personality disorders as binary. You either had one or you didn’t. But we now understand that personality pathology is a matter of degree.”1
Mark Zimmerman, MD, has written several papers—some of which are in press—about how these revisions might impact clinicians and whether the revisions are necessary. He is Director of the Rhode Island Methods to Improve Diagnostic Assessment and Services (MIDAS) project, an ongoing clinical research study involving the integration of research assessment methods into clinical practice.
Proposed revisions, rationale, and literature reviews for DSM-5 are available at www.DSM5.org and anyone, including the general public, was invited to provide feedback through the Web site. Current Psychiatry Associate Editor Donald W. Black, MD, interviewed Dr. Zimmerman on June 29, 2011, just a few days after the latest proposed revision was posted on June 21, 2011.
DR. BLACK: What is your understanding of the DSM-5 Personality Disorders Work Group proposal to revamp the PD category?
DR. ZIMMERMAN: The initial proposal, released in February 2010, was complex and generated a fair amount of critical commentary related to the marked changes in the approach toward diagnosis of PDs. That proposal replaced diagnostic criteria with a prototype description of personality types that patients would need to match. It also eliminated 5 PDs—paranoid, schizoid, histrionic, dependent, and narcissistic—retained antisocial, avoidant, borderline, obsessive-compulsive, and schizotypal, and introduced trait level ratings. The June 21 revision proposes eliminating only 4 disorders—narcissistic was retained—and the Work Group is no longer suggesting using prototypes but instead have diagnostic criteria (Table).2,3 We do not know if this is the final proposal because similar to the first proposal, it is not presented with much supporting empirical evidence that demonstrates its superiority toward diagnosing PDs compared with the DSM-IV approach.
Table
Personality disorder criteria: DSM-IV vs DSM-5
| DSM-IV | DSM-5 proposal (posted June 21, 2011) |
|---|---|
| General diagnostic criteria | |
|
|
| Personality disorders included | |
| Antisocial, avoidant, borderline, dependent, histrionic, narcissistic, obsessive-compulsive, paranoid, schizoid, schizotypal, personality disorder not otherwise specified | Antisocial, avoidant, borderline, narcissistic, obsessive-compulsive, schizotypal, personality disorder trait specified (requires a rating of significant impairment in personality functioning, combined with the presence of pathological trait domains or facets) |
| Source: References 2,3 | |
I’m not suggesting that the DSM-IV approach is without problems. My attitude is that before going forward with a change to the official diagnostic nomenclature, you need to clearly establish that the new way of doing things is better than the previous way by whatever metric you use.
DR. BLACK: Do you believe there is a need to revamp or revise the DSM-IV PD criteria?
DR. ZIMMERMAN: I think a number of the arguments put forth by the DSM-5 Work Group as justifications for revising the criteria do not hold up to empirical study.
One of the issues is the argument that there’s too much comorbidity among PDs. The theory is that disorders are not unique diagnostic entities if they are so frequently comorbid with other disorders. But how much comorbidity is too much? The DSM-5 Work Group doesn’t say. Oldham et al4 found comorbidity rates of 70% to 90%, depending on which semi-structured diagnostic interview was used; however, this was among individuals presenting for psychodynamic treatment of PDs.
I wanted to look at the comorbidity rates in nontreatment-seeking samples to find out if treatment seeking is associated with comorbidity. I reviewed the literature and identified 7 general population epidemiological studies that presented data on the number of individuals with ≥2 PD diagnoses. In these studies, the comorbidity rate is approximately 25%, which is one-half or less than the rates found in patient populations.5 This finding suggested to me that this may not be a nosology problem unless you think 25% comorbidity is too high. The DSM-5 people don’t speak to that, although quite frankly with 10 PDs I don’t think the 25% comorbidity rate is excessive. However, a comorbidity rate of 25% was much lower than that found in patient samples and suggests to me that one of the primary stated reasons of deleting 4 PDs may not be valid.
DR. BLACK: Assuming there is a need to revise the PD section, how would you have gone about that process?
DR. ZIMMERMAN: Whatever deficiencies you perceive in the criteria, the process should be that you come up with an alternative, examine the alternative empirically, and this is followed by independent replication that the new approach is superior to the prior one. My view is that it is not sufficient justification to make a change because there is a problem with the prior approach.
We can argue as to whether there really are problems with, for example, the categorical nature of classification. My research group and I wrote a paper arguing that DSM-IV can be interpreted as having a dimensional component (Box).6 DSM-IV suggests that clinicians record on axis II that a patient has some traits of a disorder even when the full criteria are not met. With that in mind, we conceptualized DSM-IV as having a 3-point dimension, where 0 means no traits of the disorder, 1 indicates subthreshold traits, and 2 indicates that the disorder is present. In a study of >2,000 patients, we found that DSM-IV’s 3-point dimensional approach was as highly associated with measures of psychosocial morbidity as more finely graded dimensional systems.6 We therefore concluded that DSM-IV already includes a dimensional system and questioned why we need to change that approach.
Zimmerman et al suggested that DSM-IV personality disorder (PD) criteria can be thought of as a dimensional system.6 They evaluated 2,150 psychiatric outpatients using semi-structured diagnostic interviews and computed dimensional PD scores in 3 ways:
- 3-point dimension, where 0 means no traits of the disorder, 1 indicates subthreshold traits, and 2 indicates that the disorder is present
- number of DSM-IV criteria met
- 5-point dimension analogous to what was being proposed for DSM-5.
Patients also were evaluated for the presence of a PD based on DSM-IV diagnostic threshold. They then correlated these assessment methods with 7 indices of psychosocial morbidity—the number of current axis I disorders, Global Assessment of Functioning scores, unemployment in the past 5 years, number of psychiatric hospitalizations, level of psychosocial functioning, suicidal ideation at the time of the evaluation, and number of lifetime suicide attempts. All methods of dimensional assessment were more highly correlated with psychosocial morbidity than categorical classification and there was no difference among the 3 dimensional methods.
One of my concerns with the dimensional system as currently proposed is the uncertain significance and possible implications of someone being given a low, non-zero rating. How might this play out in a custody evaluation of someone who is said to be “a little borderline”? What might the implications of non-zero ratings be in obtaining life insurance? The potential practical consequences of low ratings have not, to my knowledge, been discussed. Because of this concern we decided to do a study to determine if there was any clinical significance to low dimensional scores. I had hypothesized that if we compared individuals who had no criteria and only 1 BPD criterion, there would be no difference.
To be frank, I was seeking to show that there was no validity to low levels of pathology and therefore the DSM-5 group probably is getting into dangerous territory. In fact, we found that there were rather significant and robust differences between individuals with 0 criteria and 1 criterion.7 Even though this finding didn’t support my hypothesis, I thought it was significant because it supported the DSM-5 Work Group and I felt compelled to publish that data.
We now had 2 interesting pieces of information. A few years ago we published a study on borderline personality disorder (BPD) that found once you hit the diagnostic threshold it made no difference how many criteria you met.8 On the other hand, when you were below the diagnostic threshold, having 1 criterion vs 0 made a big difference. In addition, a fair number of studies show that dimensional models capture more of the variance in personality pathology than categorical variables.9-12
This lead to our next study in which we hypothesized that dimensionality was only important when the person didn’t meet criteria, not when they did meet criteria.13 So we divided patients in the MIDAS study into those with 0 to 4 BPD criteria and those with ≥5 and counted the number of criteria that were met. Then we correlated each of those 2 dimensional scores with various indicators of illness severity, such as number of suicide attempts, number of psychiatric hospitalizations, and amount of time missed from work in the past 5 years. We found that for individuals who already achieved the diagnostic threshold there were very low correlations with these psychosocial morbidity variables. But for patients with subthreshold symptomatology, there were significant correlations and those correlations were significantly higher than the correlations for the other group. We therefore suggested that dimensionality is important but only when you don’t meet the diagnostic threshold. Thus, we came to the conclusion that DSM-IV already provides for capturing the important dimensional nature of PDs.
DR. BLACK: I’ve discussed this issue with a number of people who basically say doctors tend to think categorically, they don’t think along dimensions. Would it be difficult for psychiatrists to accept this type of system because it’s so different from how physicians are trained to think?
DR. ZIMMERMAN: I think doctors do think categorically and about traits, not necessarily disorders. For example, we’ll see a patient and a clinician will say he’s overly perfectionistic, but there’s no perfectionistic disorder in DSM-IV. This patient may or may not have obsessive-compulsive personality disorder.
I think assessment and diagnosis in routine clinical practice are not nearly as comprehensive as in research. I think psychiatrists often are picking up on traits that they think are clinically significant, but even within that context, they’re thinking categorically, that the patient is perfectionistic rather than rating him a 7 on a scale from 0 to 10 in terms of perfectionism.
Eliminated disorders
DR. BLACK: The proposal will cut the number of PDs to 6 plus personality disorder trait specified and those remaining are to be called types. How did the DSM-5 Work Group select the 5 (now 4) disorders to get rid of? Did they just pick ones that were infrequently used?
DR. ZIMMERMAN: They retained the disorders that were studied in the Collaborative Longitudinal Personality Disorders Study study14 plus others with well established validity.
DR. BLACK: What do you think about that plan to reduce the number of PDs?
DR. ZIMMERMAN: The biggest problem I have is that the DSM-5 Work Group didn’t present any data on the implications of their plan. The conceptual justification was to reduce comorbidity rates. Well, you can hypothesize that comorbidity would actually increase if you retained only those disorders that are more frequently comorbid with other disorders. Would there be any individuals who only have 1 of the excluded diagnoses? Would there be false negatives? They didn’t indicate whether comorbidity would drop and by how much. And they didn’t indicate if there would be a potential impact on missing cases.
We did such an analysis because we had the data set available from the MIDAS project.15 We wanted to know if you excluded the 5 diagnoses that (at the time) were proposed for exclusion—narcissistic, paranoid, schizoid, dependent, and histrionic—what percentage of individuals would no longer be diagnosed with a PD? Second, how much would comorbidity rates change? And third, how did individuals who would no longer be diagnosed with a PD compare with individuals who never had a PD?
We found that the comorbidity rates did, in fact, drop from 30% to 21%. We found that the rate of PDs dropped only a little, but approximately 10% of individuals who previously would have been diagnosed with a PD would no longer be diagnosed. We compared individuals in the excluded group—those who had only 1 of the PDs that would no longer be considered a PD—with a group of patients who had a retained PD and also compared them to individuals with no PD. We found that the retained PD group and the excluded group did not differ on measures of psychosocial morbidity, such as Global Assessment of Functioning scores, hospitalizations, suicidality, number of current axis I disorders, etc. Also, the excluded group clearly was different than the no PD group. We questioned whether or not those in the excluded group might end up being false negative diagnoses in DSM-5. Certainly DSM-5 provides a provision to use trait ratings to still diagnose a PD, called personality disorder trait specified, which would be somewhat analogous to PD not otherwise specified (NOS).
It’s ironic insofar as another of the issues considered by the DSM-5 Work Group to be a problem with axis II is lack of coverage and that too many individuals are diagnosed with PD NOS. Their proposal to exclude PDs could result in more individuals being diagnosed with PD NOS. I know the group would disagree with that perspective, but they provided no evidence to support its view.
As I said at the beginning of this interview, I think we should be talking about this from a scientific perspective and nothing more than that.
Related Resource
- Widiger TA, Simonsen E, Sirovatka PJ, et al. Dimensional models of personality disorders: Refining the research agenda for DSM-V. Arlington, VA: American Psychiatric Publishing, Inc; 2007.
Disclosures
- Dr. Zimmerman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
- Dr. Black receives research support from AstraZeneca and Psyadon.
1. DSM-5 revisions for personality disorders reflect major change. Public comment period for proposed diagnostic criteria extended through July 15 [news release]. Arlington, VA: American Psychiatric Association; July 7, 2011. http://www.psych.org/MainMenu/Newsroom/NewsReleases/2011-News-Releases_1/DSM-5-Revisions-for-Personality-Disorders-Reflect-Major-Change-.aspx?FT=.pdf. Accessed July 26, 2011.
2. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
3. Personality disorders. American Psychiatric Association DSM-5 development. http://www.dsm5.org/proposedrevision/Pages/PersonalityDisorders.aspx. Updated June 21, 2011. Accessed July 26, 2011.
4. Oldham JM, Skodol AE, Kellman HD, et al. Diagnosis of DSM-III-R personality disorders by two structured interviews: patterns of comorbidity. Am J Psychiatry. 1992;149(2):213-220.
5. Zimmerman M. Is there adequate empirical justification for radically revising the personality disorders section for DSM-5? Personality Disorders: Theory, Research and Treatment. In press.
6. Zimmerman M, Chelminski I, Young D, et al. Does DSM-IV already capture the dimensional nature of personality disorders? J Clin Psychiatry. In press.
7. Zimmerman M, Chelminski I, Young D, et al. Does the presence of one feature of borderline personality disorder have clinical significance?: Implications for dimensional ratings of personality disorders. J Clin Psychiatry. In press.
8. Asnaani A, Chelminski I, Young D, et al. Heterogeneity of borderline personality disorder: do the number of criteria met make a difference? J Pers Disord. 2007;21(6):615-625.
9. Skodol AE, Oldham JM, Bender DS, et al. Dimensional representations of DSM-IV personality disorders: relationships to functional impairment. Am J Psychiatry. 2005;162:1919-1925.
10. Durbin CE, Klein DN. Ten-year stability of personality disorders among outpatients with mood disorders. J Abnorm Psychol. 2006;115:75-84.
11. Grilo CM, Sanislow CA, Gunderson JG, et al. Two-year stability and change of schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders. J Consult Clin Psychol. 2004;72:767-775.
12. Morey LC, Hopwood CJ, Gunderson JG, et al. Comparison of alternative models for personality disorders. Psychol Med. 2007;37:983-994.
13. Zimmerman M, Chelminski I, Young D, et al. Is dimensional scoring of borderline personality disorder only important for subthreshold levels of severity? J Pers Disord. In press.
14. Gunderson JG, Shea MT, Skodol AE, et al. The Collaborative Longitudinal Personality Disorders Study: development, aims, design, and sample characteristics. J Pers Disord. 2000;14(4):300-315.
15. Zimmerman M, Chelminski I, Young D, et al. Impact of deleting 5 DSM-IV personality disorders on prevalence, comorbidity, and the association between personality disorder pathology and psychosocial morbidity. J Clin Psychiatry. In press.
1. DSM-5 revisions for personality disorders reflect major change. Public comment period for proposed diagnostic criteria extended through July 15 [news release]. Arlington, VA: American Psychiatric Association; July 7, 2011. http://www.psych.org/MainMenu/Newsroom/NewsReleases/2011-News-Releases_1/DSM-5-Revisions-for-Personality-Disorders-Reflect-Major-Change-.aspx?FT=.pdf. Accessed July 26, 2011.
2. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
3. Personality disorders. American Psychiatric Association DSM-5 development. http://www.dsm5.org/proposedrevision/Pages/PersonalityDisorders.aspx. Updated June 21, 2011. Accessed July 26, 2011.
4. Oldham JM, Skodol AE, Kellman HD, et al. Diagnosis of DSM-III-R personality disorders by two structured interviews: patterns of comorbidity. Am J Psychiatry. 1992;149(2):213-220.
5. Zimmerman M. Is there adequate empirical justification for radically revising the personality disorders section for DSM-5? Personality Disorders: Theory, Research and Treatment. In press.
6. Zimmerman M, Chelminski I, Young D, et al. Does DSM-IV already capture the dimensional nature of personality disorders? J Clin Psychiatry. In press.
7. Zimmerman M, Chelminski I, Young D, et al. Does the presence of one feature of borderline personality disorder have clinical significance?: Implications for dimensional ratings of personality disorders. J Clin Psychiatry. In press.
8. Asnaani A, Chelminski I, Young D, et al. Heterogeneity of borderline personality disorder: do the number of criteria met make a difference? J Pers Disord. 2007;21(6):615-625.
9. Skodol AE, Oldham JM, Bender DS, et al. Dimensional representations of DSM-IV personality disorders: relationships to functional impairment. Am J Psychiatry. 2005;162:1919-1925.
10. Durbin CE, Klein DN. Ten-year stability of personality disorders among outpatients with mood disorders. J Abnorm Psychol. 2006;115:75-84.
11. Grilo CM, Sanislow CA, Gunderson JG, et al. Two-year stability and change of schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders. J Consult Clin Psychol. 2004;72:767-775.
12. Morey LC, Hopwood CJ, Gunderson JG, et al. Comparison of alternative models for personality disorders. Psychol Med. 2007;37:983-994.
13. Zimmerman M, Chelminski I, Young D, et al. Is dimensional scoring of borderline personality disorder only important for subthreshold levels of severity? J Pers Disord. In press.
14. Gunderson JG, Shea MT, Skodol AE, et al. The Collaborative Longitudinal Personality Disorders Study: development, aims, design, and sample characteristics. J Pers Disord. 2000;14(4):300-315.
15. Zimmerman M, Chelminski I, Young D, et al. Impact of deleting 5 DSM-IV personality disorders on prevalence, comorbidity, and the association between personality disorder pathology and psychosocial morbidity. J Clin Psychiatry. In press.
Strategies for improving pharmacotherapy for patients with BPD
Pharmacologic treatment of borderline personality disorder
As psychiatry’s understanding of borderline personality disorder (BPD) grows, the literature clearly describes the seriousness of BPD, as well as these patients’ high utilization of treatment. Pharmacotherapy for BPD remains controversial. The most recent American Psychiatric Association practice guidelines focus on using symptom domains of this heterogeneous illness to guide medication selection, yet when these guidelines were published, there was a lack of data to support this recommendation.1
This article evaluates medications for BPD and emerging data supporting matching medications to BPD symptom domains, with an emphasis on making choices that advance clinical practice. We conclude by reviewing studies of combined pharmacotherapy and dialectical behavior therapy (DBT) and describing how a multidisciplinary team approach can enhance BPD treatment.
Early research
Early studies of pharmacotherapy for BPD began after the development of the Diagnostic Interview for Borderlines2,3 and DSM-III criteria for BPD.4 Researchers recruited patients who fulfilled the diagnostic criteria; however, these participants’ symptom profiles were highly heterogeneous. Although such studies can be useful when starting to test new treatments—especially if they are able to show efficacy over placebo or explore safety—they are less helpful in guiding clinical practice.
During the 1980s, low doses of first-generation antipsychotics were evaluated based on hypotheses that BPD was related to schizophrenia. Case series5 and placebo-controlled trials6,7 pointed to symptom reduction over time and greater than placebo for BPD patients. Interestingly, in a small study of BPD inpatients, Soloff et al8 compared the first-generation antipsychotic haloperidol to amitriptyline and found amitriptyline led to symptom worsening in some patients. Cowdry and Gardner9 compared alprazolam, carbamazepine, trifluoperazine, and tranylcypromine in a double-blind, placebo-controlled crossover trial of 16 female BPD outpatients. They found antipsychotics were not useful. Further, the study found behavioral disinhibition when a benzodiazepine (alprazolam) was used alone in impulsive patients.
These studies provided a basis for the idea that medications could help reduce BPD symptoms. However, some early investigators noted that antipsychotics’ side effects led some patients to discontinue treatment.6
Next-generation studies
Antidepressants. Interest in exploring pharmacologic treatments for BPD diminished after the early efficacy trials. Several events led to a reemergence of this interest, including the FDA’s approval of the selective serotonin reuptake inhibitor fluoxetine for depression in 1987. Some investigators hypothesized fluoxetine’s antidepressant properties could help treat BPD symptoms and perhaps the serotonin reuptake action could diminish impulsivity.10 Case series and a double-blind, placebo-controlled trial11 demonstrated fluoxetine’s efficacy in BPD. In 1 study, Salzman et al12 found fluoxetine’s greatest impact was on “anger,” a major affective dimension of BPD.
Mood stabilizers. When valproic acid emerged as a successful treatment for bipolar disorder, researchers turned their attention to mood-stabilizing anticonvulsants for BPD. Numerous case series and controlled trials provided evidence of its efficacy.13,14 This was the first time subtypes of BPD patients were tested prospectively—with the hypothesis that the mood-stabilizing anticonvulsants would diminish impulsivity and aggression. The positive results of Hollander et al13 and Frankenburg and Zanarini14 in assessing divalproex in BPD patients with bipolar II disorder has implications for targeted treatment (discussed below).
Newer antipsychotics. The introduction of second-generation antipsychotics (SGA) led some researchers to explore whether these agents could decrease BPD symptoms. Case series15 and some (but not all) placebo-controlled trials have demonstrated benefit from SGAs such as olanzapine,16-18 aripiprazole,19 and quetiapine.20,21 Initial research on risperidone22 and ziprasidone also suggested efficacy for BPD. Two placebo-controlled studies of olanzapine examined which symptom groups were most helped; each reported a broad effect.16,17 However, not all studies of SGAs for BPD patients have been positive.18 Further, metabolic side effects have been noted for several SGAs, including olanzapine.18
Omega-3 fatty acids. Some studies examining omega-3 fatty acids have sparked an ongoing interest in this compound. In an 8-week, double-blind, pilot study of 30 women with BPD, Zanarini23 found omega-3 fatty acids demonstrated efficacy over placebo.
Most studies of BPD pharmacotherapy have used a classic clinical trial design, which does not easily translate into recommendations regarding medication selection for individual patients, especially those with BPD and comorbid illnesses. Also, existing trials have not fully explored starting doses, and no maintenance studies have been published. Therefore, many clinical application questions remain unresolved. However, some early treatment recommendations are supported by recent meta-analyses that demonstrate effects of medication classes for specific symptom domains.
Careful identification of comorbid psychiatric disorders is a rational first step. Diagnosing comorbid disorders, such as bipolar disorder, will determine medication choice and impact length of treatment. In a double-blind study of 30 women with BPD and comorbid bipolar II disorder, Frankenburg and Zanarini14 found divalproex had a statistically significant effect compared with placebo and could be considered for this specific population.
When treating a BPD patient who has a comorbid illness, it is important not to ignore BPD symptoms. The chronic emotional dysregulation and ongoing safety issues require psychiatrists to educate patients about these symptoms and to address them in a multidisciplinary manner.
Clarifying prominent symptom domains can help steer pharmacologic management. Many trials have attempted to focus on specific symptom domains, including cognitive-perceptual disturbances, impulsivity, and affective dysregulation. Table 124 lists BPD symptom domains and associated characteristics.
Table 1
Symptom domains of BPD
| Cognitive-perceptual symptoms |
| Suspiciousness |
| Referential thinking |
| Paranoid ideation |
| Illusions |
| Derealization |
| Depersonalization |
| Hallucination-like symptoms |
| Impulsive-behavioral dyscontrol |
| Impulsive aggression |
| Deliberate self-harm |
| Impulsive sexual behavior |
| Substance abuse |
| Impulsive spending |
| Affective dysregulation |
| Mood lability |
| Rejection sensitivity |
| Intense anger out of proportion to the stimuli |
| Sudden depressive mood episodes |
| BPD: borderline personality disorder Source: Reference 24 |
Dosing strategy
Developing a medication management strategy for BPD patients requires a thoughtful approach. When faced with a patient who has overwhelming distress, it is tempting to start with high medication doses; however, clinical experience suggests starting cautiously with lower doses will yield better tolerability and adherence. Based on our clinical experience, patients with BPD tend to be highly perceptive to physiologic stimuli and medication side effects.
Further research is needed to answer clinical questions regarding optimal dosing strategy and treatment, but some studies suggest when using SGAs, doses equivalent to one-third or one-half the dose used for treating schizophrenia may be appropriate.1,2,17,18 However, for fluoxetine, investigators have espoused using a dosage higher than generally used for depression.10 For mood-stabilizing anticonvulsants, almost all studies employed the same doses used for bipolar disorder.25 Some studies of valproic acid have verified appropriate blood levels—generally 50 to 100 μg/mL.
Controlled trials have not determined whether medications for patients with BPD should be used briefly during times of stress or for longer periods. Many studies of medication for BPD have been relatively brief trials that explored whether the drug has any potential efficacy. In our opinion, this issue currently is being addressed in clinical practice in a trial-and-error manner.
Clues to targeted treatment
Although pharmacotherapy for BPD subtypes remains controversial, recent meta-analyses by Ingenhoven24 and Nose26 and a Cochrane Review27 (with subsequent online update28) have identified evidence that supports the use of specific medications for treating BPD symptoms. These studies’ authors acknowledge replication studies are required because of the limited nature of the available data. In contrast, a meta-analysis conducted by the National Collaborating Centre for Mental Health29 did not identify sufficient evidence for medication use in BPD on which to base official guidelines to advise health care providers in the United Kingdom. The only medication recommendation in this meta-analysis is to consider prescribing short-term sedative antihistamines during crises; this recommendation is not supported by any clinical trial.
In a meta-analysis of 21 placebo-controlled trials of patients with BPD and/or schizotypal personality disorder, Inghoven et al24 used multiple domains and subdomains, including cognitive-perceptual symptoms, impulsive-behavioral dyscontrol, affective dysregulation, anger, and mood lability, to assess the efficacy of medication use (Table 2).24 They found:
- Antipsychotics seemed to have a moderate effect on cognitive-perceptual symptoms and a moderate-to-large effect on anger.
- Antidepressants had a small effect on anxiety, but no other domains.
- Mood stabilizers had a very large effect on impulsive-behavioral dyscontrol and anger, a large effect on anxiety, and a moderate effect on depressed mood.
- Regarding global functioning, mood stabilizers had a greater effect than antipsychotics. Both led to greater change than antidepressants.
A 2010 Cochrane Review meta-analysis initially conducted by Leib27 with subsequent online update by Stoffers28 included 28 studies with a total of 1,742 patients and also identified symptom-targeted BPD domains. This study analyzed pooled data and found support for the use of specific medications, including certain antipsychotics, mood stabilizers, and antidepressants, for specific BPD symptoms (Table 3).28 The authors recommended data be interpreted cautiously, however, because many of the clinical trials included in their meta-analysis have not been replicated and generalizability from research populations to clinical populations is not well understood.
Table 2
Which medications improve which BPD symptoms?
| Medication | Symptom domain | Effect |
|---|---|---|
| Antipsychotics | Cognitive-perceptual | Moderate |
| Anger | Moderate/large | |
| Antidepressants | Anxiety | Small |
| Anger | Small | |
| Mood stabilizers | Impulsive-behavioral dyscontrol | Very large |
| Anger | Very large | |
| Anxiety | Large | |
| Depressed mood | Moderate | |
| BPD: borderline personality disorder Source: Reference 24 | ||
Table 3
Pharmacotherapy for BPD: Results of a Cochrane review
| Class | Medication(s) |
|---|---|
| Cognitive-perceptual symptoms | |
| Antipsychotics | Olanzapine, aripiprazole |
| Impulsive-behavioral dyscontrol | |
| Mood stabilizers | Topiramate, lamotrigine |
| Antipsychotics | Aripiprazole |
| Affective dysregulation | |
| Antidepressants | Amitriptylinea (depressed mood) |
| Mood stabilizers | Topiramate, lamotrigine (anger), valproate (depressed mood) |
| Antipsychotics | Haloperidol (anger), olanzapine, aripiprazole |
| Omega-3 fatty acids | Fish oil (depression) |
| Suicidal behavior/suicidality | |
| Antipsychotics | Flupenthixol decanoate |
| Omega-3 fatty acids | Fish oil |
| Interpersonal problems | |
| Antipsychotics | Aripiprazole |
| Mood stabilizers | Valproate, topiramate |
| No improvement on any outcome: ziprasidone, thiothixene, phenelzine, fluoxetine, fluvoxamine, carbamazepine | |
| aDo not prescribe to suicidal patients BPD: borderline personality disorder Source: Reference 28 | |
DBT and pharmacotherapy
As is the case with many studies of psychiatric medications, early efficacy studies of pharmacotherapy for BPD did not include structured psychosocial treatment. In 2 double-blind, placebo-controlled trials with a total of 84 patients receiving DBT, those assigned to olanzapine had better outcomes on objective rating scales than those on placebo.30,31 Similar trials testing fluoxetine showed no advantage for the drug over placebo.32 In a pilot study by Moen et al,25 17 patients were assigned to “condensed DBT” before being randomized to divalproex extended release or placebo. Two patients remitted in the first 4 weeks and continued to improve without medication. If replicated, this finding may point to a targeted approach to the timing of medication initiation.
Clinical recommendations
Randomized, placebo-controlled BPD trials have demonstrated striking improvements in patients in placebo groups, which may be attributed to the powerful therapeutic impact of regular, structured, nonjudgmental interactions within a research protocol. Prescribers can enhance a medication’s therapeutic effect by keeping in mind the same principles that apply to treatment of other common psychiatric disorders.
Patients with BPD respond well to validation of their symptoms and their experience. Tell patients you take their BPD symptoms seriously and acknowledge their distress. The goal is to partner with patients to improve function, decrease reactivity, and reduce emotional pain. When working with BPD patients, it is appropriate to communicate a sense of optimism and hopefulness about their prognosis and treatment. Performing this approach in a caring way will better preserve the therapeutic alliance.
Additional suggestions based on our clinical experience include:
- Provide regular medication management visits.
- Consider using a structured symptom rating scale to evaluate symptoms over time, such as the Zanarini Rating Scale for Borderline Personality Disorder33 or Borderline Evaluation of Severity Over Time.34
- Educate patients with BPD about the disorder by making the appropriate diagnosis and providing reputable educational materials (see Related Resources).
- Do not diagnose a patient with BPD as having bipolar disorder unless they clearly meet criteria for bipolar disorder.
- Communicate your limitations in advance.
- Orient the patient to the possibility of needing to try different medications to determine the most helpful agent or combination.
- Do not de-emphasize risks of medications or side effects. Serious symptoms require medications that bear a risk of side effects; communicate these risks to patients and carefully weigh the risk-benefit profile.
- Inform patients you will be responsive to making appropriate changes if problems arise that are associated with pharmacotherapy and outweigh the benefit of medication.
Multidisciplinary teamwork
Best outcomes for patients with BPD are facilitated by a collaborative team effort. Such an approach addresses both the psychological and biologic underpinnings of the disorder and can significantly decrease the possibility of “splitting” among team members. To determine ways in which a therapist and physician may work together, clinicians should discuss the:
- meaning of medication to the therapist, psychiatrist, and patient
- potential benefits and limitations of medication
- the role of medication in the patient’s overall treatment.35
Patients with BPD experience emotional crisis. At times, prescribing patterns unfortunately reflect the practice of adding medications to address emotional crisis. This practice may partially account for the high rates of polypharmacy in BPD patients.36 Patients with BPD will benefit from interacting with a clinician whose approach is responsive, validating, and non-reactive to the patient’s symptoms and experiences. A comprehensive treatment approach includes screening and treating comorbid conditions, providing education about the diagnosis, and multidisciplinary involvement combined with rational, targeted pharmacotherapy.
- Friedel RO. Borderline personality disorder demystified: an essential guide for understanding and living with BPD. New York, NY: Marlowe & Company; 2004.
- Chapman A, Gratz K. Borderline personality disorder survival guide: everything you need to know about living with BPD. Oakland, CA: New Harbinger Publications, Inc; 2007.
- National Education Alliance for Borderline Personality Disorder. www.borderlinepersonalitydisorder.com.
Drug Brand Names
- Alprazolam • Xanax
- Amitriptyline • Elavil
- Aripiprazole • Abilify
- Carbamazepine • Tegretol
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Haloperidol • Haldol
- Lamotrigine • Lamictal
- Olanzapine • Zyprexa
- Phenelzine • Nardil
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Thiothixene • Navane
- Topiramate • Topamax, Topiragen
- Tranylcypromine • Parnate
- Trifluoperazine • Stelazine
- Valproic acid • Depakote
- Ziprasidone • Geodon
Disclosure
Dr. Nelson receives research/grant support from the Minnesota Medical Foundation.
Dr. Schulz receives research/grant support from AstraZeneca, Otsuka, and Rules-Based Medicine and is a consultant to Bioavail, Bristol-Myers Squibb, and Eli Lilly and Company.
1. American Psychiatric Association Practice Guidelines. Practice guideline for the treatment of patients with borderline personality disorder. American Psychiatric Association. Am J Psychiatry. 2001;158(10 suppl):1-52.
2. Barrash J, Kroll J, Carey K, et al. Discriminating borderline disorder from other personality disorders. Cluster analysis of the diagnostic interview for borderlines. Arch Gen Psychiatry. 1983;40(12):1297-1302.
3. Kety SS, Rosenthal D, Wender PH, et al. Mental illness in the biological and adoptive families of adopted individuals who have become schizophrenic: a preliminary report based on psychiatric interviews. Proc Annu Meet Am Psychopathol Assoc. 1975;(63):147-165.
4. Diagnostic and statistical manual of mental disorders, 3rd ed. Washington DC: American Psychiatric Association; 1980.
5. Serban G, Siegel S. Response of borderline and schizotypal patients to small doses of thiothixene and haloperidol. Am J Psychiatry. 1984;141(11):1455-1458.
6. Goldberg SC, Schulz SC, Schulz PM, et al. Borderline and schizotypal personality disorders treated with low-dose thiothixene vs placebo. Arch Gen Psychiatry. 1986;43(7):680-686.
7. Soloff PH, George A, Nathan RS, et al. Progress in pharmacotherapy of borderline disorders. A double-blind study of amitriptyline, haloperidol, and placebo. Arch Gen Psychiatry. 1986;43(7):691-697.
8. Soloff PH, George A, Nathan RS, et al. Paradoxical effects of amitriptyline on borderline patients. Am J Psychiatry. 1986;143(12):1603-1635.
9. Cowdry RW, Gardner DL. Pharmacotherapy of borderline personality disorder. Alprazolam carbamazepine, trifluoperazine, and tranylcypromine. Arch Gen Psychiatry. 1988;45(2):111-119.
10. Markovitz PJ, Calabrese JR, Schulz SC, et al. Fluoxetine in the treatment of borderline and schizotypal personality disorders. Am J Psychiatry. 1991;148(8):1064-1067.
11. Coccaro EF, Kavoussi RJ. Fluoxetine and impulsive aggressive behavior in personality-disordered subjects. Arch Gen Psychiatry. 1997;54(12):1081-1088.
12. Salzman C, Wolfson AN, Schatzberg A, et al. Effect of fluoxetine on anger in symptomatic volunteers with borderline personality disorder. J Clin Psychopharmacol. 1995;15(1):23-29.
13. Hollander E, Tracy KA, Swann AC, et al. Divalproex in the treatment of impulsive aggression: efficacy in cluster B personality disorders. Neuropsychopharmacology. 2003;28(6):1186-1197.
14. Frankenburg FR, Zanarini MC. Divalproex sodium treatment of women with borderline personality disorder and bipolar II disorder: a double-blind placebo-controlled pilot study. J Clin Psychiatry. 2002;63(5):442-446.
15. Schulz SC, Camlin KL, Berry SA, et al. Olanzapine safety and efficacy in patients with borderline personality disorder and comorbid dysthymia. Biol Psychiatry. 1999;46(10):1429-1435.
16. Bogenschutz MP, George Nurnberg H. Olanzapine versus placebo in the treatment of borderline personality disorder. J Clin Psychiatry. 2004;65(1):104-109.
17. Zanarini MC, Frankenburg FR. Olanzapine treatment of female borderline personality disorder patients: a double-blind placebo-controlled pilot study. J Clin Psychiatry. 2001;62(11):849-854.
18. Schulz SC, Zanarini MC, Bateman A, et al. Olanzapine for the treatment of borderline personality disorder: variable dose 12-week randomised double-blind placebo-controlled study. Br J Psychiatry. 2008;193(6):485-492.
19. Nickel MK, Muehlbacher M, Nickel C, et al. Aripiprazole in the treatment of patients with borderline personality disorder: a double-blind, placebo-controlled study. Am J Psychiatry. 2006;163(5):833-838.
20. Adityanjee, Romine A, Brown E, et al. Quetiapine in patients with borderline personality disorder: an open-label trial. Ann Clin Psychiatry. 2008;20(4):219-226.
21. Villeneuve E, Lemelin S. Open-label study of atypical neuroleptic quetiapine for treatment of borderline personality disorder: impulsivity as main target. J Clin Psychiatry. 2005;66(10):1298-1303.
22. Rocca P, Marchiaro L, Cocuzza E, et al. Treatment of borderline personality disorder with risperidone. J Clin Psychiatry. 2002;63(3):241-244.
23. Zanarini MC, Frankenburg FR. Omega-3 fatty acid treatment of women with borderline personality disorder: a double-blind placebo-controlled pilot study. Am J Psychiatry. 2003;160(1):167-169.
24. Ingenhoven T, Lafay P, Rinne T, et al. Effectiveness of pharmacotherapy for severe personality disorders: meta-analyses of randomized controlled trials. J Clin Psychiatry. 2010;71(1):14-25.
25. Moen Moore R, Miller M, Lee S, et al. Extended release divalproex for borderline personality disorder. Poster presented at: U. S. Psychiatric and Mental Health Congress; October 13-16, 2007; Orlando, FL.
26. Nose M, Cipriani A, Biancosino B, et al. Efficacy of pharmacotherapy against core traits of borderline personality disorder: meta-analysis of randomized controlled trials. Int Clin Psychopharmacol. 2006;21(6):345-353.
27. Lieb K, Völlm B, Rücker G, et al. Pharmacotherapy for borderline personality disorder: Cochrane Systematic Review of Randomised Trials. Br J Psychiatry. 2010;196(1):4-12.
28. Stoffers J, Völlm BA, Rücker G, et al. Pharmacological interventions for borderline personality disorder. Cochrane Database Syst Rev. 2010;(6):CD005653.-
29. National Collaborating Centre for Mental Health. Borderline personality disorder: the NICE guideline on treatment and management. National clinical practice guideline no. 78. London United Kingdom: RCPsych Publications; 2009.
30. Linehan MM, McDavid JD, Brown MZ, et al. Olanzapine plus dialectical behavior therapy for women with high irritability who meet criteria for borderline personality disorder: a double-blind, placebo-controlled pilot study. J Clin Psychiatry. 2008;69(6):999-1005.
31. Soler J, Pascual JC, Campins J, et al. Double-blind, placebo-controlled study of dialectical behavior therapy plus olanzapine for borderline personality disorder. Am J Psychiatry. 2005;162(6):1221-1224.
32. Simpson EB, Yen S, Costello E, et al. Combined dialectical behavior therapy and fluoxetine in the treatment of borderline personality disorder. J Clin Psychiatry. 2004;65(3):379-385.
33. Zanarini MC, Vujanovic AA, Parachini EA, et al. Zanarini Rating Scale for Borderline Personality Disorder (ZAN-BPD): a continuous measure of DSM-IV borderline psychopathology. J Pers Disord. 2003;17(3):233-242.
34. Pfohl B, Blum N, St John D, et al. Reliability and validity of the Borderline Evaluation of Severity Over Time (BEST): a self-rated scale to measure severity and change in persons with borderline personality disorder. J Pers Disord. 2009;23(3):281-293.
35. Silk KR. Collaborative treatment for patients with personality disorders. In: Riba MB Balon R, eds. Psychopharmacology and psychotherapy: a collaborative approach. Washington, DC: American Psychiatric Press; 1999:221–277.
36. Zanarini MC. Update on pharmacotherapy of borderline personality disorder. Curr Psychiatry Rep. 2004;6(1):66-70.
As psychiatry’s understanding of borderline personality disorder (BPD) grows, the literature clearly describes the seriousness of BPD, as well as these patients’ high utilization of treatment. Pharmacotherapy for BPD remains controversial. The most recent American Psychiatric Association practice guidelines focus on using symptom domains of this heterogeneous illness to guide medication selection, yet when these guidelines were published, there was a lack of data to support this recommendation.1
This article evaluates medications for BPD and emerging data supporting matching medications to BPD symptom domains, with an emphasis on making choices that advance clinical practice. We conclude by reviewing studies of combined pharmacotherapy and dialectical behavior therapy (DBT) and describing how a multidisciplinary team approach can enhance BPD treatment.
Early research
Early studies of pharmacotherapy for BPD began after the development of the Diagnostic Interview for Borderlines2,3 and DSM-III criteria for BPD.4 Researchers recruited patients who fulfilled the diagnostic criteria; however, these participants’ symptom profiles were highly heterogeneous. Although such studies can be useful when starting to test new treatments—especially if they are able to show efficacy over placebo or explore safety—they are less helpful in guiding clinical practice.
During the 1980s, low doses of first-generation antipsychotics were evaluated based on hypotheses that BPD was related to schizophrenia. Case series5 and placebo-controlled trials6,7 pointed to symptom reduction over time and greater than placebo for BPD patients. Interestingly, in a small study of BPD inpatients, Soloff et al8 compared the first-generation antipsychotic haloperidol to amitriptyline and found amitriptyline led to symptom worsening in some patients. Cowdry and Gardner9 compared alprazolam, carbamazepine, trifluoperazine, and tranylcypromine in a double-blind, placebo-controlled crossover trial of 16 female BPD outpatients. They found antipsychotics were not useful. Further, the study found behavioral disinhibition when a benzodiazepine (alprazolam) was used alone in impulsive patients.
These studies provided a basis for the idea that medications could help reduce BPD symptoms. However, some early investigators noted that antipsychotics’ side effects led some patients to discontinue treatment.6
Next-generation studies
Antidepressants. Interest in exploring pharmacologic treatments for BPD diminished after the early efficacy trials. Several events led to a reemergence of this interest, including the FDA’s approval of the selective serotonin reuptake inhibitor fluoxetine for depression in 1987. Some investigators hypothesized fluoxetine’s antidepressant properties could help treat BPD symptoms and perhaps the serotonin reuptake action could diminish impulsivity.10 Case series and a double-blind, placebo-controlled trial11 demonstrated fluoxetine’s efficacy in BPD. In 1 study, Salzman et al12 found fluoxetine’s greatest impact was on “anger,” a major affective dimension of BPD.
Mood stabilizers. When valproic acid emerged as a successful treatment for bipolar disorder, researchers turned their attention to mood-stabilizing anticonvulsants for BPD. Numerous case series and controlled trials provided evidence of its efficacy.13,14 This was the first time subtypes of BPD patients were tested prospectively—with the hypothesis that the mood-stabilizing anticonvulsants would diminish impulsivity and aggression. The positive results of Hollander et al13 and Frankenburg and Zanarini14 in assessing divalproex in BPD patients with bipolar II disorder has implications for targeted treatment (discussed below).
Newer antipsychotics. The introduction of second-generation antipsychotics (SGA) led some researchers to explore whether these agents could decrease BPD symptoms. Case series15 and some (but not all) placebo-controlled trials have demonstrated benefit from SGAs such as olanzapine,16-18 aripiprazole,19 and quetiapine.20,21 Initial research on risperidone22 and ziprasidone also suggested efficacy for BPD. Two placebo-controlled studies of olanzapine examined which symptom groups were most helped; each reported a broad effect.16,17 However, not all studies of SGAs for BPD patients have been positive.18 Further, metabolic side effects have been noted for several SGAs, including olanzapine.18
Omega-3 fatty acids. Some studies examining omega-3 fatty acids have sparked an ongoing interest in this compound. In an 8-week, double-blind, pilot study of 30 women with BPD, Zanarini23 found omega-3 fatty acids demonstrated efficacy over placebo.
Most studies of BPD pharmacotherapy have used a classic clinical trial design, which does not easily translate into recommendations regarding medication selection for individual patients, especially those with BPD and comorbid illnesses. Also, existing trials have not fully explored starting doses, and no maintenance studies have been published. Therefore, many clinical application questions remain unresolved. However, some early treatment recommendations are supported by recent meta-analyses that demonstrate effects of medication classes for specific symptom domains.
Careful identification of comorbid psychiatric disorders is a rational first step. Diagnosing comorbid disorders, such as bipolar disorder, will determine medication choice and impact length of treatment. In a double-blind study of 30 women with BPD and comorbid bipolar II disorder, Frankenburg and Zanarini14 found divalproex had a statistically significant effect compared with placebo and could be considered for this specific population.
When treating a BPD patient who has a comorbid illness, it is important not to ignore BPD symptoms. The chronic emotional dysregulation and ongoing safety issues require psychiatrists to educate patients about these symptoms and to address them in a multidisciplinary manner.
Clarifying prominent symptom domains can help steer pharmacologic management. Many trials have attempted to focus on specific symptom domains, including cognitive-perceptual disturbances, impulsivity, and affective dysregulation. Table 124 lists BPD symptom domains and associated characteristics.
Table 1
Symptom domains of BPD
| Cognitive-perceptual symptoms |
| Suspiciousness |
| Referential thinking |
| Paranoid ideation |
| Illusions |
| Derealization |
| Depersonalization |
| Hallucination-like symptoms |
| Impulsive-behavioral dyscontrol |
| Impulsive aggression |
| Deliberate self-harm |
| Impulsive sexual behavior |
| Substance abuse |
| Impulsive spending |
| Affective dysregulation |
| Mood lability |
| Rejection sensitivity |
| Intense anger out of proportion to the stimuli |
| Sudden depressive mood episodes |
| BPD: borderline personality disorder Source: Reference 24 |
Dosing strategy
Developing a medication management strategy for BPD patients requires a thoughtful approach. When faced with a patient who has overwhelming distress, it is tempting to start with high medication doses; however, clinical experience suggests starting cautiously with lower doses will yield better tolerability and adherence. Based on our clinical experience, patients with BPD tend to be highly perceptive to physiologic stimuli and medication side effects.
Further research is needed to answer clinical questions regarding optimal dosing strategy and treatment, but some studies suggest when using SGAs, doses equivalent to one-third or one-half the dose used for treating schizophrenia may be appropriate.1,2,17,18 However, for fluoxetine, investigators have espoused using a dosage higher than generally used for depression.10 For mood-stabilizing anticonvulsants, almost all studies employed the same doses used for bipolar disorder.25 Some studies of valproic acid have verified appropriate blood levels—generally 50 to 100 μg/mL.
Controlled trials have not determined whether medications for patients with BPD should be used briefly during times of stress or for longer periods. Many studies of medication for BPD have been relatively brief trials that explored whether the drug has any potential efficacy. In our opinion, this issue currently is being addressed in clinical practice in a trial-and-error manner.
Clues to targeted treatment
Although pharmacotherapy for BPD subtypes remains controversial, recent meta-analyses by Ingenhoven24 and Nose26 and a Cochrane Review27 (with subsequent online update28) have identified evidence that supports the use of specific medications for treating BPD symptoms. These studies’ authors acknowledge replication studies are required because of the limited nature of the available data. In contrast, a meta-analysis conducted by the National Collaborating Centre for Mental Health29 did not identify sufficient evidence for medication use in BPD on which to base official guidelines to advise health care providers in the United Kingdom. The only medication recommendation in this meta-analysis is to consider prescribing short-term sedative antihistamines during crises; this recommendation is not supported by any clinical trial.
In a meta-analysis of 21 placebo-controlled trials of patients with BPD and/or schizotypal personality disorder, Inghoven et al24 used multiple domains and subdomains, including cognitive-perceptual symptoms, impulsive-behavioral dyscontrol, affective dysregulation, anger, and mood lability, to assess the efficacy of medication use (Table 2).24 They found:
- Antipsychotics seemed to have a moderate effect on cognitive-perceptual symptoms and a moderate-to-large effect on anger.
- Antidepressants had a small effect on anxiety, but no other domains.
- Mood stabilizers had a very large effect on impulsive-behavioral dyscontrol and anger, a large effect on anxiety, and a moderate effect on depressed mood.
- Regarding global functioning, mood stabilizers had a greater effect than antipsychotics. Both led to greater change than antidepressants.
A 2010 Cochrane Review meta-analysis initially conducted by Leib27 with subsequent online update by Stoffers28 included 28 studies with a total of 1,742 patients and also identified symptom-targeted BPD domains. This study analyzed pooled data and found support for the use of specific medications, including certain antipsychotics, mood stabilizers, and antidepressants, for specific BPD symptoms (Table 3).28 The authors recommended data be interpreted cautiously, however, because many of the clinical trials included in their meta-analysis have not been replicated and generalizability from research populations to clinical populations is not well understood.
Table 2
Which medications improve which BPD symptoms?
| Medication | Symptom domain | Effect |
|---|---|---|
| Antipsychotics | Cognitive-perceptual | Moderate |
| Anger | Moderate/large | |
| Antidepressants | Anxiety | Small |
| Anger | Small | |
| Mood stabilizers | Impulsive-behavioral dyscontrol | Very large |
| Anger | Very large | |
| Anxiety | Large | |
| Depressed mood | Moderate | |
| BPD: borderline personality disorder Source: Reference 24 | ||
Table 3
Pharmacotherapy for BPD: Results of a Cochrane review
| Class | Medication(s) |
|---|---|
| Cognitive-perceptual symptoms | |
| Antipsychotics | Olanzapine, aripiprazole |
| Impulsive-behavioral dyscontrol | |
| Mood stabilizers | Topiramate, lamotrigine |
| Antipsychotics | Aripiprazole |
| Affective dysregulation | |
| Antidepressants | Amitriptylinea (depressed mood) |
| Mood stabilizers | Topiramate, lamotrigine (anger), valproate (depressed mood) |
| Antipsychotics | Haloperidol (anger), olanzapine, aripiprazole |
| Omega-3 fatty acids | Fish oil (depression) |
| Suicidal behavior/suicidality | |
| Antipsychotics | Flupenthixol decanoate |
| Omega-3 fatty acids | Fish oil |
| Interpersonal problems | |
| Antipsychotics | Aripiprazole |
| Mood stabilizers | Valproate, topiramate |
| No improvement on any outcome: ziprasidone, thiothixene, phenelzine, fluoxetine, fluvoxamine, carbamazepine | |
| aDo not prescribe to suicidal patients BPD: borderline personality disorder Source: Reference 28 | |
DBT and pharmacotherapy
As is the case with many studies of psychiatric medications, early efficacy studies of pharmacotherapy for BPD did not include structured psychosocial treatment. In 2 double-blind, placebo-controlled trials with a total of 84 patients receiving DBT, those assigned to olanzapine had better outcomes on objective rating scales than those on placebo.30,31 Similar trials testing fluoxetine showed no advantage for the drug over placebo.32 In a pilot study by Moen et al,25 17 patients were assigned to “condensed DBT” before being randomized to divalproex extended release or placebo. Two patients remitted in the first 4 weeks and continued to improve without medication. If replicated, this finding may point to a targeted approach to the timing of medication initiation.
Clinical recommendations
Randomized, placebo-controlled BPD trials have demonstrated striking improvements in patients in placebo groups, which may be attributed to the powerful therapeutic impact of regular, structured, nonjudgmental interactions within a research protocol. Prescribers can enhance a medication’s therapeutic effect by keeping in mind the same principles that apply to treatment of other common psychiatric disorders.
Patients with BPD respond well to validation of their symptoms and their experience. Tell patients you take their BPD symptoms seriously and acknowledge their distress. The goal is to partner with patients to improve function, decrease reactivity, and reduce emotional pain. When working with BPD patients, it is appropriate to communicate a sense of optimism and hopefulness about their prognosis and treatment. Performing this approach in a caring way will better preserve the therapeutic alliance.
Additional suggestions based on our clinical experience include:
- Provide regular medication management visits.
- Consider using a structured symptom rating scale to evaluate symptoms over time, such as the Zanarini Rating Scale for Borderline Personality Disorder33 or Borderline Evaluation of Severity Over Time.34
- Educate patients with BPD about the disorder by making the appropriate diagnosis and providing reputable educational materials (see Related Resources).
- Do not diagnose a patient with BPD as having bipolar disorder unless they clearly meet criteria for bipolar disorder.
- Communicate your limitations in advance.
- Orient the patient to the possibility of needing to try different medications to determine the most helpful agent or combination.
- Do not de-emphasize risks of medications or side effects. Serious symptoms require medications that bear a risk of side effects; communicate these risks to patients and carefully weigh the risk-benefit profile.
- Inform patients you will be responsive to making appropriate changes if problems arise that are associated with pharmacotherapy and outweigh the benefit of medication.
Multidisciplinary teamwork
Best outcomes for patients with BPD are facilitated by a collaborative team effort. Such an approach addresses both the psychological and biologic underpinnings of the disorder and can significantly decrease the possibility of “splitting” among team members. To determine ways in which a therapist and physician may work together, clinicians should discuss the:
- meaning of medication to the therapist, psychiatrist, and patient
- potential benefits and limitations of medication
- the role of medication in the patient’s overall treatment.35
Patients with BPD experience emotional crisis. At times, prescribing patterns unfortunately reflect the practice of adding medications to address emotional crisis. This practice may partially account for the high rates of polypharmacy in BPD patients.36 Patients with BPD will benefit from interacting with a clinician whose approach is responsive, validating, and non-reactive to the patient’s symptoms and experiences. A comprehensive treatment approach includes screening and treating comorbid conditions, providing education about the diagnosis, and multidisciplinary involvement combined with rational, targeted pharmacotherapy.
- Friedel RO. Borderline personality disorder demystified: an essential guide for understanding and living with BPD. New York, NY: Marlowe & Company; 2004.
- Chapman A, Gratz K. Borderline personality disorder survival guide: everything you need to know about living with BPD. Oakland, CA: New Harbinger Publications, Inc; 2007.
- National Education Alliance for Borderline Personality Disorder. www.borderlinepersonalitydisorder.com.
Drug Brand Names
- Alprazolam • Xanax
- Amitriptyline • Elavil
- Aripiprazole • Abilify
- Carbamazepine • Tegretol
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Haloperidol • Haldol
- Lamotrigine • Lamictal
- Olanzapine • Zyprexa
- Phenelzine • Nardil
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Thiothixene • Navane
- Topiramate • Topamax, Topiragen
- Tranylcypromine • Parnate
- Trifluoperazine • Stelazine
- Valproic acid • Depakote
- Ziprasidone • Geodon
Disclosure
Dr. Nelson receives research/grant support from the Minnesota Medical Foundation.
Dr. Schulz receives research/grant support from AstraZeneca, Otsuka, and Rules-Based Medicine and is a consultant to Bioavail, Bristol-Myers Squibb, and Eli Lilly and Company.
As psychiatry’s understanding of borderline personality disorder (BPD) grows, the literature clearly describes the seriousness of BPD, as well as these patients’ high utilization of treatment. Pharmacotherapy for BPD remains controversial. The most recent American Psychiatric Association practice guidelines focus on using symptom domains of this heterogeneous illness to guide medication selection, yet when these guidelines were published, there was a lack of data to support this recommendation.1
This article evaluates medications for BPD and emerging data supporting matching medications to BPD symptom domains, with an emphasis on making choices that advance clinical practice. We conclude by reviewing studies of combined pharmacotherapy and dialectical behavior therapy (DBT) and describing how a multidisciplinary team approach can enhance BPD treatment.
Early research
Early studies of pharmacotherapy for BPD began after the development of the Diagnostic Interview for Borderlines2,3 and DSM-III criteria for BPD.4 Researchers recruited patients who fulfilled the diagnostic criteria; however, these participants’ symptom profiles were highly heterogeneous. Although such studies can be useful when starting to test new treatments—especially if they are able to show efficacy over placebo or explore safety—they are less helpful in guiding clinical practice.
During the 1980s, low doses of first-generation antipsychotics were evaluated based on hypotheses that BPD was related to schizophrenia. Case series5 and placebo-controlled trials6,7 pointed to symptom reduction over time and greater than placebo for BPD patients. Interestingly, in a small study of BPD inpatients, Soloff et al8 compared the first-generation antipsychotic haloperidol to amitriptyline and found amitriptyline led to symptom worsening in some patients. Cowdry and Gardner9 compared alprazolam, carbamazepine, trifluoperazine, and tranylcypromine in a double-blind, placebo-controlled crossover trial of 16 female BPD outpatients. They found antipsychotics were not useful. Further, the study found behavioral disinhibition when a benzodiazepine (alprazolam) was used alone in impulsive patients.
These studies provided a basis for the idea that medications could help reduce BPD symptoms. However, some early investigators noted that antipsychotics’ side effects led some patients to discontinue treatment.6
Next-generation studies
Antidepressants. Interest in exploring pharmacologic treatments for BPD diminished after the early efficacy trials. Several events led to a reemergence of this interest, including the FDA’s approval of the selective serotonin reuptake inhibitor fluoxetine for depression in 1987. Some investigators hypothesized fluoxetine’s antidepressant properties could help treat BPD symptoms and perhaps the serotonin reuptake action could diminish impulsivity.10 Case series and a double-blind, placebo-controlled trial11 demonstrated fluoxetine’s efficacy in BPD. In 1 study, Salzman et al12 found fluoxetine’s greatest impact was on “anger,” a major affective dimension of BPD.
Mood stabilizers. When valproic acid emerged as a successful treatment for bipolar disorder, researchers turned their attention to mood-stabilizing anticonvulsants for BPD. Numerous case series and controlled trials provided evidence of its efficacy.13,14 This was the first time subtypes of BPD patients were tested prospectively—with the hypothesis that the mood-stabilizing anticonvulsants would diminish impulsivity and aggression. The positive results of Hollander et al13 and Frankenburg and Zanarini14 in assessing divalproex in BPD patients with bipolar II disorder has implications for targeted treatment (discussed below).
Newer antipsychotics. The introduction of second-generation antipsychotics (SGA) led some researchers to explore whether these agents could decrease BPD symptoms. Case series15 and some (but not all) placebo-controlled trials have demonstrated benefit from SGAs such as olanzapine,16-18 aripiprazole,19 and quetiapine.20,21 Initial research on risperidone22 and ziprasidone also suggested efficacy for BPD. Two placebo-controlled studies of olanzapine examined which symptom groups were most helped; each reported a broad effect.16,17 However, not all studies of SGAs for BPD patients have been positive.18 Further, metabolic side effects have been noted for several SGAs, including olanzapine.18
Omega-3 fatty acids. Some studies examining omega-3 fatty acids have sparked an ongoing interest in this compound. In an 8-week, double-blind, pilot study of 30 women with BPD, Zanarini23 found omega-3 fatty acids demonstrated efficacy over placebo.
Most studies of BPD pharmacotherapy have used a classic clinical trial design, which does not easily translate into recommendations regarding medication selection for individual patients, especially those with BPD and comorbid illnesses. Also, existing trials have not fully explored starting doses, and no maintenance studies have been published. Therefore, many clinical application questions remain unresolved. However, some early treatment recommendations are supported by recent meta-analyses that demonstrate effects of medication classes for specific symptom domains.
Careful identification of comorbid psychiatric disorders is a rational first step. Diagnosing comorbid disorders, such as bipolar disorder, will determine medication choice and impact length of treatment. In a double-blind study of 30 women with BPD and comorbid bipolar II disorder, Frankenburg and Zanarini14 found divalproex had a statistically significant effect compared with placebo and could be considered for this specific population.
When treating a BPD patient who has a comorbid illness, it is important not to ignore BPD symptoms. The chronic emotional dysregulation and ongoing safety issues require psychiatrists to educate patients about these symptoms and to address them in a multidisciplinary manner.
Clarifying prominent symptom domains can help steer pharmacologic management. Many trials have attempted to focus on specific symptom domains, including cognitive-perceptual disturbances, impulsivity, and affective dysregulation. Table 124 lists BPD symptom domains and associated characteristics.
Table 1
Symptom domains of BPD
| Cognitive-perceptual symptoms |
| Suspiciousness |
| Referential thinking |
| Paranoid ideation |
| Illusions |
| Derealization |
| Depersonalization |
| Hallucination-like symptoms |
| Impulsive-behavioral dyscontrol |
| Impulsive aggression |
| Deliberate self-harm |
| Impulsive sexual behavior |
| Substance abuse |
| Impulsive spending |
| Affective dysregulation |
| Mood lability |
| Rejection sensitivity |
| Intense anger out of proportion to the stimuli |
| Sudden depressive mood episodes |
| BPD: borderline personality disorder Source: Reference 24 |
Dosing strategy
Developing a medication management strategy for BPD patients requires a thoughtful approach. When faced with a patient who has overwhelming distress, it is tempting to start with high medication doses; however, clinical experience suggests starting cautiously with lower doses will yield better tolerability and adherence. Based on our clinical experience, patients with BPD tend to be highly perceptive to physiologic stimuli and medication side effects.
Further research is needed to answer clinical questions regarding optimal dosing strategy and treatment, but some studies suggest when using SGAs, doses equivalent to one-third or one-half the dose used for treating schizophrenia may be appropriate.1,2,17,18 However, for fluoxetine, investigators have espoused using a dosage higher than generally used for depression.10 For mood-stabilizing anticonvulsants, almost all studies employed the same doses used for bipolar disorder.25 Some studies of valproic acid have verified appropriate blood levels—generally 50 to 100 μg/mL.
Controlled trials have not determined whether medications for patients with BPD should be used briefly during times of stress or for longer periods. Many studies of medication for BPD have been relatively brief trials that explored whether the drug has any potential efficacy. In our opinion, this issue currently is being addressed in clinical practice in a trial-and-error manner.
Clues to targeted treatment
Although pharmacotherapy for BPD subtypes remains controversial, recent meta-analyses by Ingenhoven24 and Nose26 and a Cochrane Review27 (with subsequent online update28) have identified evidence that supports the use of specific medications for treating BPD symptoms. These studies’ authors acknowledge replication studies are required because of the limited nature of the available data. In contrast, a meta-analysis conducted by the National Collaborating Centre for Mental Health29 did not identify sufficient evidence for medication use in BPD on which to base official guidelines to advise health care providers in the United Kingdom. The only medication recommendation in this meta-analysis is to consider prescribing short-term sedative antihistamines during crises; this recommendation is not supported by any clinical trial.
In a meta-analysis of 21 placebo-controlled trials of patients with BPD and/or schizotypal personality disorder, Inghoven et al24 used multiple domains and subdomains, including cognitive-perceptual symptoms, impulsive-behavioral dyscontrol, affective dysregulation, anger, and mood lability, to assess the efficacy of medication use (Table 2).24 They found:
- Antipsychotics seemed to have a moderate effect on cognitive-perceptual symptoms and a moderate-to-large effect on anger.
- Antidepressants had a small effect on anxiety, but no other domains.
- Mood stabilizers had a very large effect on impulsive-behavioral dyscontrol and anger, a large effect on anxiety, and a moderate effect on depressed mood.
- Regarding global functioning, mood stabilizers had a greater effect than antipsychotics. Both led to greater change than antidepressants.
A 2010 Cochrane Review meta-analysis initially conducted by Leib27 with subsequent online update by Stoffers28 included 28 studies with a total of 1,742 patients and also identified symptom-targeted BPD domains. This study analyzed pooled data and found support for the use of specific medications, including certain antipsychotics, mood stabilizers, and antidepressants, for specific BPD symptoms (Table 3).28 The authors recommended data be interpreted cautiously, however, because many of the clinical trials included in their meta-analysis have not been replicated and generalizability from research populations to clinical populations is not well understood.
Table 2
Which medications improve which BPD symptoms?
| Medication | Symptom domain | Effect |
|---|---|---|
| Antipsychotics | Cognitive-perceptual | Moderate |
| Anger | Moderate/large | |
| Antidepressants | Anxiety | Small |
| Anger | Small | |
| Mood stabilizers | Impulsive-behavioral dyscontrol | Very large |
| Anger | Very large | |
| Anxiety | Large | |
| Depressed mood | Moderate | |
| BPD: borderline personality disorder Source: Reference 24 | ||
Table 3
Pharmacotherapy for BPD: Results of a Cochrane review
| Class | Medication(s) |
|---|---|
| Cognitive-perceptual symptoms | |
| Antipsychotics | Olanzapine, aripiprazole |
| Impulsive-behavioral dyscontrol | |
| Mood stabilizers | Topiramate, lamotrigine |
| Antipsychotics | Aripiprazole |
| Affective dysregulation | |
| Antidepressants | Amitriptylinea (depressed mood) |
| Mood stabilizers | Topiramate, lamotrigine (anger), valproate (depressed mood) |
| Antipsychotics | Haloperidol (anger), olanzapine, aripiprazole |
| Omega-3 fatty acids | Fish oil (depression) |
| Suicidal behavior/suicidality | |
| Antipsychotics | Flupenthixol decanoate |
| Omega-3 fatty acids | Fish oil |
| Interpersonal problems | |
| Antipsychotics | Aripiprazole |
| Mood stabilizers | Valproate, topiramate |
| No improvement on any outcome: ziprasidone, thiothixene, phenelzine, fluoxetine, fluvoxamine, carbamazepine | |
| aDo not prescribe to suicidal patients BPD: borderline personality disorder Source: Reference 28 | |
DBT and pharmacotherapy
As is the case with many studies of psychiatric medications, early efficacy studies of pharmacotherapy for BPD did not include structured psychosocial treatment. In 2 double-blind, placebo-controlled trials with a total of 84 patients receiving DBT, those assigned to olanzapine had better outcomes on objective rating scales than those on placebo.30,31 Similar trials testing fluoxetine showed no advantage for the drug over placebo.32 In a pilot study by Moen et al,25 17 patients were assigned to “condensed DBT” before being randomized to divalproex extended release or placebo. Two patients remitted in the first 4 weeks and continued to improve without medication. If replicated, this finding may point to a targeted approach to the timing of medication initiation.
Clinical recommendations
Randomized, placebo-controlled BPD trials have demonstrated striking improvements in patients in placebo groups, which may be attributed to the powerful therapeutic impact of regular, structured, nonjudgmental interactions within a research protocol. Prescribers can enhance a medication’s therapeutic effect by keeping in mind the same principles that apply to treatment of other common psychiatric disorders.
Patients with BPD respond well to validation of their symptoms and their experience. Tell patients you take their BPD symptoms seriously and acknowledge their distress. The goal is to partner with patients to improve function, decrease reactivity, and reduce emotional pain. When working with BPD patients, it is appropriate to communicate a sense of optimism and hopefulness about their prognosis and treatment. Performing this approach in a caring way will better preserve the therapeutic alliance.
Additional suggestions based on our clinical experience include:
- Provide regular medication management visits.
- Consider using a structured symptom rating scale to evaluate symptoms over time, such as the Zanarini Rating Scale for Borderline Personality Disorder33 or Borderline Evaluation of Severity Over Time.34
- Educate patients with BPD about the disorder by making the appropriate diagnosis and providing reputable educational materials (see Related Resources).
- Do not diagnose a patient with BPD as having bipolar disorder unless they clearly meet criteria for bipolar disorder.
- Communicate your limitations in advance.
- Orient the patient to the possibility of needing to try different medications to determine the most helpful agent or combination.
- Do not de-emphasize risks of medications or side effects. Serious symptoms require medications that bear a risk of side effects; communicate these risks to patients and carefully weigh the risk-benefit profile.
- Inform patients you will be responsive to making appropriate changes if problems arise that are associated with pharmacotherapy and outweigh the benefit of medication.
Multidisciplinary teamwork
Best outcomes for patients with BPD are facilitated by a collaborative team effort. Such an approach addresses both the psychological and biologic underpinnings of the disorder and can significantly decrease the possibility of “splitting” among team members. To determine ways in which a therapist and physician may work together, clinicians should discuss the:
- meaning of medication to the therapist, psychiatrist, and patient
- potential benefits and limitations of medication
- the role of medication in the patient’s overall treatment.35
Patients with BPD experience emotional crisis. At times, prescribing patterns unfortunately reflect the practice of adding medications to address emotional crisis. This practice may partially account for the high rates of polypharmacy in BPD patients.36 Patients with BPD will benefit from interacting with a clinician whose approach is responsive, validating, and non-reactive to the patient’s symptoms and experiences. A comprehensive treatment approach includes screening and treating comorbid conditions, providing education about the diagnosis, and multidisciplinary involvement combined with rational, targeted pharmacotherapy.
- Friedel RO. Borderline personality disorder demystified: an essential guide for understanding and living with BPD. New York, NY: Marlowe & Company; 2004.
- Chapman A, Gratz K. Borderline personality disorder survival guide: everything you need to know about living with BPD. Oakland, CA: New Harbinger Publications, Inc; 2007.
- National Education Alliance for Borderline Personality Disorder. www.borderlinepersonalitydisorder.com.
Drug Brand Names
- Alprazolam • Xanax
- Amitriptyline • Elavil
- Aripiprazole • Abilify
- Carbamazepine • Tegretol
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Haloperidol • Haldol
- Lamotrigine • Lamictal
- Olanzapine • Zyprexa
- Phenelzine • Nardil
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Thiothixene • Navane
- Topiramate • Topamax, Topiragen
- Tranylcypromine • Parnate
- Trifluoperazine • Stelazine
- Valproic acid • Depakote
- Ziprasidone • Geodon
Disclosure
Dr. Nelson receives research/grant support from the Minnesota Medical Foundation.
Dr. Schulz receives research/grant support from AstraZeneca, Otsuka, and Rules-Based Medicine and is a consultant to Bioavail, Bristol-Myers Squibb, and Eli Lilly and Company.
1. American Psychiatric Association Practice Guidelines. Practice guideline for the treatment of patients with borderline personality disorder. American Psychiatric Association. Am J Psychiatry. 2001;158(10 suppl):1-52.
2. Barrash J, Kroll J, Carey K, et al. Discriminating borderline disorder from other personality disorders. Cluster analysis of the diagnostic interview for borderlines. Arch Gen Psychiatry. 1983;40(12):1297-1302.
3. Kety SS, Rosenthal D, Wender PH, et al. Mental illness in the biological and adoptive families of adopted individuals who have become schizophrenic: a preliminary report based on psychiatric interviews. Proc Annu Meet Am Psychopathol Assoc. 1975;(63):147-165.
4. Diagnostic and statistical manual of mental disorders, 3rd ed. Washington DC: American Psychiatric Association; 1980.
5. Serban G, Siegel S. Response of borderline and schizotypal patients to small doses of thiothixene and haloperidol. Am J Psychiatry. 1984;141(11):1455-1458.
6. Goldberg SC, Schulz SC, Schulz PM, et al. Borderline and schizotypal personality disorders treated with low-dose thiothixene vs placebo. Arch Gen Psychiatry. 1986;43(7):680-686.
7. Soloff PH, George A, Nathan RS, et al. Progress in pharmacotherapy of borderline disorders. A double-blind study of amitriptyline, haloperidol, and placebo. Arch Gen Psychiatry. 1986;43(7):691-697.
8. Soloff PH, George A, Nathan RS, et al. Paradoxical effects of amitriptyline on borderline patients. Am J Psychiatry. 1986;143(12):1603-1635.
9. Cowdry RW, Gardner DL. Pharmacotherapy of borderline personality disorder. Alprazolam carbamazepine, trifluoperazine, and tranylcypromine. Arch Gen Psychiatry. 1988;45(2):111-119.
10. Markovitz PJ, Calabrese JR, Schulz SC, et al. Fluoxetine in the treatment of borderline and schizotypal personality disorders. Am J Psychiatry. 1991;148(8):1064-1067.
11. Coccaro EF, Kavoussi RJ. Fluoxetine and impulsive aggressive behavior in personality-disordered subjects. Arch Gen Psychiatry. 1997;54(12):1081-1088.
12. Salzman C, Wolfson AN, Schatzberg A, et al. Effect of fluoxetine on anger in symptomatic volunteers with borderline personality disorder. J Clin Psychopharmacol. 1995;15(1):23-29.
13. Hollander E, Tracy KA, Swann AC, et al. Divalproex in the treatment of impulsive aggression: efficacy in cluster B personality disorders. Neuropsychopharmacology. 2003;28(6):1186-1197.
14. Frankenburg FR, Zanarini MC. Divalproex sodium treatment of women with borderline personality disorder and bipolar II disorder: a double-blind placebo-controlled pilot study. J Clin Psychiatry. 2002;63(5):442-446.
15. Schulz SC, Camlin KL, Berry SA, et al. Olanzapine safety and efficacy in patients with borderline personality disorder and comorbid dysthymia. Biol Psychiatry. 1999;46(10):1429-1435.
16. Bogenschutz MP, George Nurnberg H. Olanzapine versus placebo in the treatment of borderline personality disorder. J Clin Psychiatry. 2004;65(1):104-109.
17. Zanarini MC, Frankenburg FR. Olanzapine treatment of female borderline personality disorder patients: a double-blind placebo-controlled pilot study. J Clin Psychiatry. 2001;62(11):849-854.
18. Schulz SC, Zanarini MC, Bateman A, et al. Olanzapine for the treatment of borderline personality disorder: variable dose 12-week randomised double-blind placebo-controlled study. Br J Psychiatry. 2008;193(6):485-492.
19. Nickel MK, Muehlbacher M, Nickel C, et al. Aripiprazole in the treatment of patients with borderline personality disorder: a double-blind, placebo-controlled study. Am J Psychiatry. 2006;163(5):833-838.
20. Adityanjee, Romine A, Brown E, et al. Quetiapine in patients with borderline personality disorder: an open-label trial. Ann Clin Psychiatry. 2008;20(4):219-226.
21. Villeneuve E, Lemelin S. Open-label study of atypical neuroleptic quetiapine for treatment of borderline personality disorder: impulsivity as main target. J Clin Psychiatry. 2005;66(10):1298-1303.
22. Rocca P, Marchiaro L, Cocuzza E, et al. Treatment of borderline personality disorder with risperidone. J Clin Psychiatry. 2002;63(3):241-244.
23. Zanarini MC, Frankenburg FR. Omega-3 fatty acid treatment of women with borderline personality disorder: a double-blind placebo-controlled pilot study. Am J Psychiatry. 2003;160(1):167-169.
24. Ingenhoven T, Lafay P, Rinne T, et al. Effectiveness of pharmacotherapy for severe personality disorders: meta-analyses of randomized controlled trials. J Clin Psychiatry. 2010;71(1):14-25.
25. Moen Moore R, Miller M, Lee S, et al. Extended release divalproex for borderline personality disorder. Poster presented at: U. S. Psychiatric and Mental Health Congress; October 13-16, 2007; Orlando, FL.
26. Nose M, Cipriani A, Biancosino B, et al. Efficacy of pharmacotherapy against core traits of borderline personality disorder: meta-analysis of randomized controlled trials. Int Clin Psychopharmacol. 2006;21(6):345-353.
27. Lieb K, Völlm B, Rücker G, et al. Pharmacotherapy for borderline personality disorder: Cochrane Systematic Review of Randomised Trials. Br J Psychiatry. 2010;196(1):4-12.
28. Stoffers J, Völlm BA, Rücker G, et al. Pharmacological interventions for borderline personality disorder. Cochrane Database Syst Rev. 2010;(6):CD005653.-
29. National Collaborating Centre for Mental Health. Borderline personality disorder: the NICE guideline on treatment and management. National clinical practice guideline no. 78. London United Kingdom: RCPsych Publications; 2009.
30. Linehan MM, McDavid JD, Brown MZ, et al. Olanzapine plus dialectical behavior therapy for women with high irritability who meet criteria for borderline personality disorder: a double-blind, placebo-controlled pilot study. J Clin Psychiatry. 2008;69(6):999-1005.
31. Soler J, Pascual JC, Campins J, et al. Double-blind, placebo-controlled study of dialectical behavior therapy plus olanzapine for borderline personality disorder. Am J Psychiatry. 2005;162(6):1221-1224.
32. Simpson EB, Yen S, Costello E, et al. Combined dialectical behavior therapy and fluoxetine in the treatment of borderline personality disorder. J Clin Psychiatry. 2004;65(3):379-385.
33. Zanarini MC, Vujanovic AA, Parachini EA, et al. Zanarini Rating Scale for Borderline Personality Disorder (ZAN-BPD): a continuous measure of DSM-IV borderline psychopathology. J Pers Disord. 2003;17(3):233-242.
34. Pfohl B, Blum N, St John D, et al. Reliability and validity of the Borderline Evaluation of Severity Over Time (BEST): a self-rated scale to measure severity and change in persons with borderline personality disorder. J Pers Disord. 2009;23(3):281-293.
35. Silk KR. Collaborative treatment for patients with personality disorders. In: Riba MB Balon R, eds. Psychopharmacology and psychotherapy: a collaborative approach. Washington, DC: American Psychiatric Press; 1999:221–277.
36. Zanarini MC. Update on pharmacotherapy of borderline personality disorder. Curr Psychiatry Rep. 2004;6(1):66-70.
1. American Psychiatric Association Practice Guidelines. Practice guideline for the treatment of patients with borderline personality disorder. American Psychiatric Association. Am J Psychiatry. 2001;158(10 suppl):1-52.
2. Barrash J, Kroll J, Carey K, et al. Discriminating borderline disorder from other personality disorders. Cluster analysis of the diagnostic interview for borderlines. Arch Gen Psychiatry. 1983;40(12):1297-1302.
3. Kety SS, Rosenthal D, Wender PH, et al. Mental illness in the biological and adoptive families of adopted individuals who have become schizophrenic: a preliminary report based on psychiatric interviews. Proc Annu Meet Am Psychopathol Assoc. 1975;(63):147-165.
4. Diagnostic and statistical manual of mental disorders, 3rd ed. Washington DC: American Psychiatric Association; 1980.
5. Serban G, Siegel S. Response of borderline and schizotypal patients to small doses of thiothixene and haloperidol. Am J Psychiatry. 1984;141(11):1455-1458.
6. Goldberg SC, Schulz SC, Schulz PM, et al. Borderline and schizotypal personality disorders treated with low-dose thiothixene vs placebo. Arch Gen Psychiatry. 1986;43(7):680-686.
7. Soloff PH, George A, Nathan RS, et al. Progress in pharmacotherapy of borderline disorders. A double-blind study of amitriptyline, haloperidol, and placebo. Arch Gen Psychiatry. 1986;43(7):691-697.
8. Soloff PH, George A, Nathan RS, et al. Paradoxical effects of amitriptyline on borderline patients. Am J Psychiatry. 1986;143(12):1603-1635.
9. Cowdry RW, Gardner DL. Pharmacotherapy of borderline personality disorder. Alprazolam carbamazepine, trifluoperazine, and tranylcypromine. Arch Gen Psychiatry. 1988;45(2):111-119.
10. Markovitz PJ, Calabrese JR, Schulz SC, et al. Fluoxetine in the treatment of borderline and schizotypal personality disorders. Am J Psychiatry. 1991;148(8):1064-1067.
11. Coccaro EF, Kavoussi RJ. Fluoxetine and impulsive aggressive behavior in personality-disordered subjects. Arch Gen Psychiatry. 1997;54(12):1081-1088.
12. Salzman C, Wolfson AN, Schatzberg A, et al. Effect of fluoxetine on anger in symptomatic volunteers with borderline personality disorder. J Clin Psychopharmacol. 1995;15(1):23-29.
13. Hollander E, Tracy KA, Swann AC, et al. Divalproex in the treatment of impulsive aggression: efficacy in cluster B personality disorders. Neuropsychopharmacology. 2003;28(6):1186-1197.
14. Frankenburg FR, Zanarini MC. Divalproex sodium treatment of women with borderline personality disorder and bipolar II disorder: a double-blind placebo-controlled pilot study. J Clin Psychiatry. 2002;63(5):442-446.
15. Schulz SC, Camlin KL, Berry SA, et al. Olanzapine safety and efficacy in patients with borderline personality disorder and comorbid dysthymia. Biol Psychiatry. 1999;46(10):1429-1435.
16. Bogenschutz MP, George Nurnberg H. Olanzapine versus placebo in the treatment of borderline personality disorder. J Clin Psychiatry. 2004;65(1):104-109.
17. Zanarini MC, Frankenburg FR. Olanzapine treatment of female borderline personality disorder patients: a double-blind placebo-controlled pilot study. J Clin Psychiatry. 2001;62(11):849-854.
18. Schulz SC, Zanarini MC, Bateman A, et al. Olanzapine for the treatment of borderline personality disorder: variable dose 12-week randomised double-blind placebo-controlled study. Br J Psychiatry. 2008;193(6):485-492.
19. Nickel MK, Muehlbacher M, Nickel C, et al. Aripiprazole in the treatment of patients with borderline personality disorder: a double-blind, placebo-controlled study. Am J Psychiatry. 2006;163(5):833-838.
20. Adityanjee, Romine A, Brown E, et al. Quetiapine in patients with borderline personality disorder: an open-label trial. Ann Clin Psychiatry. 2008;20(4):219-226.
21. Villeneuve E, Lemelin S. Open-label study of atypical neuroleptic quetiapine for treatment of borderline personality disorder: impulsivity as main target. J Clin Psychiatry. 2005;66(10):1298-1303.
22. Rocca P, Marchiaro L, Cocuzza E, et al. Treatment of borderline personality disorder with risperidone. J Clin Psychiatry. 2002;63(3):241-244.
23. Zanarini MC, Frankenburg FR. Omega-3 fatty acid treatment of women with borderline personality disorder: a double-blind placebo-controlled pilot study. Am J Psychiatry. 2003;160(1):167-169.
24. Ingenhoven T, Lafay P, Rinne T, et al. Effectiveness of pharmacotherapy for severe personality disorders: meta-analyses of randomized controlled trials. J Clin Psychiatry. 2010;71(1):14-25.
25. Moen Moore R, Miller M, Lee S, et al. Extended release divalproex for borderline personality disorder. Poster presented at: U. S. Psychiatric and Mental Health Congress; October 13-16, 2007; Orlando, FL.
26. Nose M, Cipriani A, Biancosino B, et al. Efficacy of pharmacotherapy against core traits of borderline personality disorder: meta-analysis of randomized controlled trials. Int Clin Psychopharmacol. 2006;21(6):345-353.
27. Lieb K, Völlm B, Rücker G, et al. Pharmacotherapy for borderline personality disorder: Cochrane Systematic Review of Randomised Trials. Br J Psychiatry. 2010;196(1):4-12.
28. Stoffers J, Völlm BA, Rücker G, et al. Pharmacological interventions for borderline personality disorder. Cochrane Database Syst Rev. 2010;(6):CD005653.-
29. National Collaborating Centre for Mental Health. Borderline personality disorder: the NICE guideline on treatment and management. National clinical practice guideline no. 78. London United Kingdom: RCPsych Publications; 2009.
30. Linehan MM, McDavid JD, Brown MZ, et al. Olanzapine plus dialectical behavior therapy for women with high irritability who meet criteria for borderline personality disorder: a double-blind, placebo-controlled pilot study. J Clin Psychiatry. 2008;69(6):999-1005.
31. Soler J, Pascual JC, Campins J, et al. Double-blind, placebo-controlled study of dialectical behavior therapy plus olanzapine for borderline personality disorder. Am J Psychiatry. 2005;162(6):1221-1224.
32. Simpson EB, Yen S, Costello E, et al. Combined dialectical behavior therapy and fluoxetine in the treatment of borderline personality disorder. J Clin Psychiatry. 2004;65(3):379-385.
33. Zanarini MC, Vujanovic AA, Parachini EA, et al. Zanarini Rating Scale for Borderline Personality Disorder (ZAN-BPD): a continuous measure of DSM-IV borderline psychopathology. J Pers Disord. 2003;17(3):233-242.
34. Pfohl B, Blum N, St John D, et al. Reliability and validity of the Borderline Evaluation of Severity Over Time (BEST): a self-rated scale to measure severity and change in persons with borderline personality disorder. J Pers Disord. 2009;23(3):281-293.
35. Silk KR. Collaborative treatment for patients with personality disorders. In: Riba MB Balon R, eds. Psychopharmacology and psychotherapy: a collaborative approach. Washington, DC: American Psychiatric Press; 1999:221–277.
36. Zanarini MC. Update on pharmacotherapy of borderline personality disorder. Curr Psychiatry Rep. 2004;6(1):66-70.
Dissociative identity disorder: No excuse for criminal activity
Formerly called multiple personality disorder, dissociative identity disorder (DID) is a controversial diagnosis that challenges forensic psychiatrists, other mental health clinicians, legal professionals, the media, and the public. DID cases often present in the criminal justice system rather than in the mental health system, and the illness perplexes experts in both professions.
Individuals may commit criminal acts while in a dissociated state. A study that tracked 21 reported DID cases found that 47% of men and 35% of women reported engaging in criminal activity, including 19% of men and 7% of women who committed homicide.1 Defendants occasionally use DID as a basis for pleading not guilty by reason of insanity (NGRI). Controversy over the DID diagnosis has contributed to debates about the disorder’s role in criminal responsibility.
The DID diagnosis
An American Psychiatric Association Work Group has proposed new diagnostic criteria for DID for DSM-5, which is scheduled to be published in May 2013.2 Presently, DID is listed in DSM-IV-TR as an axis I disorder.3 Criteria for DID include the presence of ≥2 distinctive identities or personality states that recurrently take control of an individual’s behavior (Table 1).3 This is accompanied by an inability to recall important personal information to an extent that cannot be explained by ordinary forgetfulness. Patients with DID typically have a primary identity that is passive, dependent, guilty, and depressed, and alternate identities with characteristics that differ from the primary identity, commonly in reported age and gender, vocabulary, general knowledge, or predominant affect.3
Dissociative pathology may result from trauma, comorbid mental illness, or other medical issues, including complex partial seizures. Developmental theorists have proposed that severe sexual, physical, or psychological trauma in childhood predisposes an individual to develop DID.4 Theoretically, harm by a trusted caregiver forces a child to split off awareness and memory of the trauma to survive in the relationship. Later these memories and feelings are experienced as a separate personality. Because this process happens repeatedly, the patient develops multiple personalities; each has different memories and performs different functions, which may be helpful or destructive. Later, dissociation becomes a coping mechanism when individuals face stressful situations.5
Personality traits that may predispose patients to develop a dissociative disorder include mental absorption, suggestibility, ability to be easily hypnotized, and tendency to fantasize.6 Patients with dissociation also may meet criteria for posttraumatic stress disorder, borderline personality disorder, somatoform disorder, eating disorder, or substance use disorders.7
Table 1
DSM-IV-TR criteria for dissociative identity disorder
| The presence of ≥2 distinct identities or personality states, each with its own relatively enduring pattern of perceiving, relating to, and thinking about the environment and self |
| At least 2 of these identities or personality states must recurrently take control of the person’s behavior |
| An inability to recall important personal information that is too extensive to be explained by ordinary forgetfulness |
| The disturbance is not due to the direct physiological effects of substance or a general medical condition. In children, the symptoms are not attributable to imaginary playmates or other fantasy play |
| Source: Reference 3 |
DID and NGRI
An insanity defense is raised in <1% of felony cases, and is successful in only a fraction of those.8 A criminal defendant who claims NGRI asserts that he committed the offense and asks the court to find him not culpable because of his mental state when the offense occurred.
The legal approach used by the defense in cases of NGRI due to DID will be determined by the jurisdiction in which the case is tried. The “Alter-in-control” approach considers the key issue as which “alter” (personality) was in control at the time of the offense and whether he or she met the insanity standard, the “Each-alter” approach considers whether each personality met the insanity standard, and the “Host-alter” approach considers whether the dominant or primary personality met the insanity standard.9
Legal and mental health professionals are divided on whether DID warrants an acquittal for insanity. The first time DID was recognized as a mental disorder that could excuse criminal responsibility occurred in State v Milligan (1978).10 The court declared serial rapist Billy Milligan insane due to lack of one integrated personality and therefore not culpable of the crimes he committed. Public outrage was extraordinary. Since this case, most DID defenses have not been successful (Table 2).10-16
In a 1980 court case,11 a defendant charged with murder pleaded NGRI due to having multiple personalities. The court found that having alter personalities was not necessarily a mental disease that would preclude responsibility for the murder.
In State v Grimsley (1982),12 the defense used NGRI due to multiple personalities in a drunk driving case. The court ruled that it is immaterial what state of consciousness or personality the defendant was in as long as the personality controlling the behavior was conscious and aware of his or her actions.
In Kirkland v State (1983),13 attorneys for a woman who committed a bank robbery asserted an insanity defense based on a psychogenic fugue, which is sudden, unexpected travel away from home accompanied by inability to recall one’s past and confusion about identity or assumption of a new identity.3 The court found that the law adjudges criminal liability according to the person’s state of mind at the time of the act and will not inquire whether an individual possesses other personalities, fugues, or even moods in which he would not have performed the crime.
In State v Jones (1988),14 the court found the defendant guilty of murdering a woman he met at a bar despite expert testimony that his multiple personalities “paralyzed” him from knowing right from wrong.
More recently, courts have rejected the admissibility of DID evidence, including expert testimony, because the scientific evidence failed to meet reliability standards, and therefore is not ultimately useful to the judge or jury. In State v Greene (1998),15 the defendant claimed that 1 of his 24 alters was responsible for killing his therapist. The Supreme Court of Washington affirmed that evidence of Mr. Greene’s DID, including expert testimony, was not reliable and not admissible.
Similarly, in State v Lockhart (2000),16 Mr. Lockhart contested his conviction of first degree sexual assault on the basis that he was not permitted to present evidence of DID to support his insanity defense. The West Virginia Court held that the diagnosis of DID was speculative and therefore did not meet reliability standards for evidence.
Table 2
Using dissociative identity disorder* as a basis for not guilty by reason of insanity
| Case | Year | Charge | Defense | Court ruling |
|---|---|---|---|---|
| State v Milligan10 | 1978 | Rape | NGRI-MPD | Lack of an integrated personality meant the defendant was not culpable |
| State v Darnall11 | 1980 | Murder | NGRI-MPD | Multiple personalities do not preclude criminal responsibility |
| State v Grimsley12 | 1982 | Drunk driving | NGRI-MPD; primary personality had no control over the ‘alter’ | State of consciousness or personality of defendant is immaterial |
| Kirkland v State13 | 1983 | Bank robbery | NGRI-psychogenic fugue | Law does not inquire about other personalities, fugue states, or moods in cases of criminal liability |
| State v Jones14 | 1988 | Murder | NGRI-MPD | Alter personalities will not be an excuse for inability to distinguish right from wrong |
| State v Greene15 | 1998 | Murder | NGRI-DID; primary personality was ‘unconscious’ | Evidence of DID, including expert testimony, was not admissible because it did not meet reliability standards |
| State v Lockhart16 | 2000 | Sexual assault | NGRI-DID | DID was not allowed into evidence by the West Virginia Court due to lack of scientific evidence |
| *Dissociative identity disorder formerly was referred to as multiple personality disorder DID: dissociative identity disorder; MPD: multiple personality disorder; NGRI: not guilty by reason of insanity. | ||||
Evaluating DID
Because the courts may ask psychiatrists to provide expert opinion on DID to assist with legal rulings, clinicians must remain vigilant to the possibility of DID as well as to defendants who may malinger multiple personalities to evade punishment. In such situations, factors to consider include the mental status examination, data and history collection, collateral information, criminal background, mental health history, history of abuse, and objective assessment tools.
Extensive field testing has shown that the Structured Clinical Interview for Dissociative Disorders (SCID-D) has good reliability and excellent validity.17 The SCID-D allows a trained interviewer to assess the severity of 5 dissociative symptoms: amnesia, depersonalization, derealization, identity confusion, and identity alteration.17 Other tools that may help assess a patient with suspected DID are listed in Table 3.
Patients who commit criminal acts while in a dissociated state may assert a defense of NGRI due to DID, but rarely has this defense been successful. Although a patient may have distinct personalities that control his or her behavior, this condition does not preclude criminal responsibility.
The role of hypnosis in evaluating DID is controversial. The introduction of pseudo-memories and potential for iatrogenic DID may complicate the clinical presentation and subsequent diagnosis.18
Table 3
Tools for diagnosing dissociative identity disorder
| Structured Clinical Interview for Dissociative Disorders |
| Dissociative Disorder Interview Schedule |
| Dissociative Experiences Scale |
| Childhood Trauma Questionnaire |
Related Resource
- West S, Noffsinger S. Is this patient not guilty by reason of insanity? Current Psychiatry. 2006;5(8):54-62.
Disclosure
Dr. Farrell reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Putnam. Diagnosis and treatment of multiple personality disorder. New York, NY: The Guilford Press; 1989.
2. American Psychiatric Association. DSM-5 Development. 300. 14. Dissociative identity disorder. Proposed revision. Available at: http://www.dsm5.org/ProposedRevisions/Pages/proposedrevision.aspx?rid=57. Accessed April 22 2011.
3. Diagnostic and statistical manual of mental disorders. 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
4. Sadock BJ, Sadock VA. eds. Dissociative disorders. In: Sadock BJ, Sadock VA, eds. Kaplan & Sadock’s comprehensive textbook of psychiatry. 7th ed. New York, NY: Lippincott Williams & Wilkins; 2000:1544–1576.
5. Lyons-Ruth K, Dutra L, Schuder MR, et al. From infant attachment disorganization to adult dissociation: relational adaptations or traumatic experiences? Psychiatr Clin North Am. 2006;29(1):63-86, viii.
6. Brahams D. Automatism and post-traumatic stress disorder. Lancet. 1990;335(8701):1333.-
7. Simeon D, Guralnik O, Knutelska M, et al. Personality factors associated with dissociation: temperament, defenses, and cognitive schemata. Am J Psychiatry. 2002;159(3):489-491.
8. Perlin M. The jurisprudence of the insanity defense. Durham NC: Carolina Academic Press; 1994.
9. Steinberg M, Bancroft J, Buchanan J. Multiple personality disorder in criminal law. Bull Am Acad Psychiatry Law. 1993;21(3):345-356.
10. State v Milligan, No 77-CR-11-2908 (Franklin County, Ohio, December 4 1978).
11. State v Darnall, 47 Or App 161, 614 P2d 120 (1980).
12. State v Grimsley, 3 Ohio App 3d 165 444 NE2d 1071 (1982).
13. Kirkland v State, 166 Ga App 478, 304 SE2d 561 (1983).
14. State v Jones, 743 P2d 176 (Wash Ct App 1987) aff’d, 759 P2d 1183, 1185 (Wash 1998).
15. State v Greene, 92 Wn App 80, 960 P2d 980 (1998).
16. State v Lockhart, 208 W Va 622 (2000).
17. Steinberg M, Rounsaville B, Cicchetti D. Detection of dissociative disorders in psychiatric patients by a screening instrument and a structured diagnostic interview. Am J Psychiatry. 1991;148(8):1050-1054.
18. Putnam FW. Dissociative phenomena. In: Tasman A ed. Annual review of psychiatry. Washington, DC: American Psychiatric Press; 1991:145–160.
Formerly called multiple personality disorder, dissociative identity disorder (DID) is a controversial diagnosis that challenges forensic psychiatrists, other mental health clinicians, legal professionals, the media, and the public. DID cases often present in the criminal justice system rather than in the mental health system, and the illness perplexes experts in both professions.
Individuals may commit criminal acts while in a dissociated state. A study that tracked 21 reported DID cases found that 47% of men and 35% of women reported engaging in criminal activity, including 19% of men and 7% of women who committed homicide.1 Defendants occasionally use DID as a basis for pleading not guilty by reason of insanity (NGRI). Controversy over the DID diagnosis has contributed to debates about the disorder’s role in criminal responsibility.
The DID diagnosis
An American Psychiatric Association Work Group has proposed new diagnostic criteria for DID for DSM-5, which is scheduled to be published in May 2013.2 Presently, DID is listed in DSM-IV-TR as an axis I disorder.3 Criteria for DID include the presence of ≥2 distinctive identities or personality states that recurrently take control of an individual’s behavior (Table 1).3 This is accompanied by an inability to recall important personal information to an extent that cannot be explained by ordinary forgetfulness. Patients with DID typically have a primary identity that is passive, dependent, guilty, and depressed, and alternate identities with characteristics that differ from the primary identity, commonly in reported age and gender, vocabulary, general knowledge, or predominant affect.3
Dissociative pathology may result from trauma, comorbid mental illness, or other medical issues, including complex partial seizures. Developmental theorists have proposed that severe sexual, physical, or psychological trauma in childhood predisposes an individual to develop DID.4 Theoretically, harm by a trusted caregiver forces a child to split off awareness and memory of the trauma to survive in the relationship. Later these memories and feelings are experienced as a separate personality. Because this process happens repeatedly, the patient develops multiple personalities; each has different memories and performs different functions, which may be helpful or destructive. Later, dissociation becomes a coping mechanism when individuals face stressful situations.5
Personality traits that may predispose patients to develop a dissociative disorder include mental absorption, suggestibility, ability to be easily hypnotized, and tendency to fantasize.6 Patients with dissociation also may meet criteria for posttraumatic stress disorder, borderline personality disorder, somatoform disorder, eating disorder, or substance use disorders.7
Table 1
DSM-IV-TR criteria for dissociative identity disorder
| The presence of ≥2 distinct identities or personality states, each with its own relatively enduring pattern of perceiving, relating to, and thinking about the environment and self |
| At least 2 of these identities or personality states must recurrently take control of the person’s behavior |
| An inability to recall important personal information that is too extensive to be explained by ordinary forgetfulness |
| The disturbance is not due to the direct physiological effects of substance or a general medical condition. In children, the symptoms are not attributable to imaginary playmates or other fantasy play |
| Source: Reference 3 |
DID and NGRI
An insanity defense is raised in <1% of felony cases, and is successful in only a fraction of those.8 A criminal defendant who claims NGRI asserts that he committed the offense and asks the court to find him not culpable because of his mental state when the offense occurred.
The legal approach used by the defense in cases of NGRI due to DID will be determined by the jurisdiction in which the case is tried. The “Alter-in-control” approach considers the key issue as which “alter” (personality) was in control at the time of the offense and whether he or she met the insanity standard, the “Each-alter” approach considers whether each personality met the insanity standard, and the “Host-alter” approach considers whether the dominant or primary personality met the insanity standard.9
Legal and mental health professionals are divided on whether DID warrants an acquittal for insanity. The first time DID was recognized as a mental disorder that could excuse criminal responsibility occurred in State v Milligan (1978).10 The court declared serial rapist Billy Milligan insane due to lack of one integrated personality and therefore not culpable of the crimes he committed. Public outrage was extraordinary. Since this case, most DID defenses have not been successful (Table 2).10-16
In a 1980 court case,11 a defendant charged with murder pleaded NGRI due to having multiple personalities. The court found that having alter personalities was not necessarily a mental disease that would preclude responsibility for the murder.
In State v Grimsley (1982),12 the defense used NGRI due to multiple personalities in a drunk driving case. The court ruled that it is immaterial what state of consciousness or personality the defendant was in as long as the personality controlling the behavior was conscious and aware of his or her actions.
In Kirkland v State (1983),13 attorneys for a woman who committed a bank robbery asserted an insanity defense based on a psychogenic fugue, which is sudden, unexpected travel away from home accompanied by inability to recall one’s past and confusion about identity or assumption of a new identity.3 The court found that the law adjudges criminal liability according to the person’s state of mind at the time of the act and will not inquire whether an individual possesses other personalities, fugues, or even moods in which he would not have performed the crime.
In State v Jones (1988),14 the court found the defendant guilty of murdering a woman he met at a bar despite expert testimony that his multiple personalities “paralyzed” him from knowing right from wrong.
More recently, courts have rejected the admissibility of DID evidence, including expert testimony, because the scientific evidence failed to meet reliability standards, and therefore is not ultimately useful to the judge or jury. In State v Greene (1998),15 the defendant claimed that 1 of his 24 alters was responsible for killing his therapist. The Supreme Court of Washington affirmed that evidence of Mr. Greene’s DID, including expert testimony, was not reliable and not admissible.
Similarly, in State v Lockhart (2000),16 Mr. Lockhart contested his conviction of first degree sexual assault on the basis that he was not permitted to present evidence of DID to support his insanity defense. The West Virginia Court held that the diagnosis of DID was speculative and therefore did not meet reliability standards for evidence.
Table 2
Using dissociative identity disorder* as a basis for not guilty by reason of insanity
| Case | Year | Charge | Defense | Court ruling |
|---|---|---|---|---|
| State v Milligan10 | 1978 | Rape | NGRI-MPD | Lack of an integrated personality meant the defendant was not culpable |
| State v Darnall11 | 1980 | Murder | NGRI-MPD | Multiple personalities do not preclude criminal responsibility |
| State v Grimsley12 | 1982 | Drunk driving | NGRI-MPD; primary personality had no control over the ‘alter’ | State of consciousness or personality of defendant is immaterial |
| Kirkland v State13 | 1983 | Bank robbery | NGRI-psychogenic fugue | Law does not inquire about other personalities, fugue states, or moods in cases of criminal liability |
| State v Jones14 | 1988 | Murder | NGRI-MPD | Alter personalities will not be an excuse for inability to distinguish right from wrong |
| State v Greene15 | 1998 | Murder | NGRI-DID; primary personality was ‘unconscious’ | Evidence of DID, including expert testimony, was not admissible because it did not meet reliability standards |
| State v Lockhart16 | 2000 | Sexual assault | NGRI-DID | DID was not allowed into evidence by the West Virginia Court due to lack of scientific evidence |
| *Dissociative identity disorder formerly was referred to as multiple personality disorder DID: dissociative identity disorder; MPD: multiple personality disorder; NGRI: not guilty by reason of insanity. | ||||
Evaluating DID
Because the courts may ask psychiatrists to provide expert opinion on DID to assist with legal rulings, clinicians must remain vigilant to the possibility of DID as well as to defendants who may malinger multiple personalities to evade punishment. In such situations, factors to consider include the mental status examination, data and history collection, collateral information, criminal background, mental health history, history of abuse, and objective assessment tools.
Extensive field testing has shown that the Structured Clinical Interview for Dissociative Disorders (SCID-D) has good reliability and excellent validity.17 The SCID-D allows a trained interviewer to assess the severity of 5 dissociative symptoms: amnesia, depersonalization, derealization, identity confusion, and identity alteration.17 Other tools that may help assess a patient with suspected DID are listed in Table 3.
Patients who commit criminal acts while in a dissociated state may assert a defense of NGRI due to DID, but rarely has this defense been successful. Although a patient may have distinct personalities that control his or her behavior, this condition does not preclude criminal responsibility.
The role of hypnosis in evaluating DID is controversial. The introduction of pseudo-memories and potential for iatrogenic DID may complicate the clinical presentation and subsequent diagnosis.18
Table 3
Tools for diagnosing dissociative identity disorder
| Structured Clinical Interview for Dissociative Disorders |
| Dissociative Disorder Interview Schedule |
| Dissociative Experiences Scale |
| Childhood Trauma Questionnaire |
Related Resource
- West S, Noffsinger S. Is this patient not guilty by reason of insanity? Current Psychiatry. 2006;5(8):54-62.
Disclosure
Dr. Farrell reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Formerly called multiple personality disorder, dissociative identity disorder (DID) is a controversial diagnosis that challenges forensic psychiatrists, other mental health clinicians, legal professionals, the media, and the public. DID cases often present in the criminal justice system rather than in the mental health system, and the illness perplexes experts in both professions.
Individuals may commit criminal acts while in a dissociated state. A study that tracked 21 reported DID cases found that 47% of men and 35% of women reported engaging in criminal activity, including 19% of men and 7% of women who committed homicide.1 Defendants occasionally use DID as a basis for pleading not guilty by reason of insanity (NGRI). Controversy over the DID diagnosis has contributed to debates about the disorder’s role in criminal responsibility.
The DID diagnosis
An American Psychiatric Association Work Group has proposed new diagnostic criteria for DID for DSM-5, which is scheduled to be published in May 2013.2 Presently, DID is listed in DSM-IV-TR as an axis I disorder.3 Criteria for DID include the presence of ≥2 distinctive identities or personality states that recurrently take control of an individual’s behavior (Table 1).3 This is accompanied by an inability to recall important personal information to an extent that cannot be explained by ordinary forgetfulness. Patients with DID typically have a primary identity that is passive, dependent, guilty, and depressed, and alternate identities with characteristics that differ from the primary identity, commonly in reported age and gender, vocabulary, general knowledge, or predominant affect.3
Dissociative pathology may result from trauma, comorbid mental illness, or other medical issues, including complex partial seizures. Developmental theorists have proposed that severe sexual, physical, or psychological trauma in childhood predisposes an individual to develop DID.4 Theoretically, harm by a trusted caregiver forces a child to split off awareness and memory of the trauma to survive in the relationship. Later these memories and feelings are experienced as a separate personality. Because this process happens repeatedly, the patient develops multiple personalities; each has different memories and performs different functions, which may be helpful or destructive. Later, dissociation becomes a coping mechanism when individuals face stressful situations.5
Personality traits that may predispose patients to develop a dissociative disorder include mental absorption, suggestibility, ability to be easily hypnotized, and tendency to fantasize.6 Patients with dissociation also may meet criteria for posttraumatic stress disorder, borderline personality disorder, somatoform disorder, eating disorder, or substance use disorders.7
Table 1
DSM-IV-TR criteria for dissociative identity disorder
| The presence of ≥2 distinct identities or personality states, each with its own relatively enduring pattern of perceiving, relating to, and thinking about the environment and self |
| At least 2 of these identities or personality states must recurrently take control of the person’s behavior |
| An inability to recall important personal information that is too extensive to be explained by ordinary forgetfulness |
| The disturbance is not due to the direct physiological effects of substance or a general medical condition. In children, the symptoms are not attributable to imaginary playmates or other fantasy play |
| Source: Reference 3 |
DID and NGRI
An insanity defense is raised in <1% of felony cases, and is successful in only a fraction of those.8 A criminal defendant who claims NGRI asserts that he committed the offense and asks the court to find him not culpable because of his mental state when the offense occurred.
The legal approach used by the defense in cases of NGRI due to DID will be determined by the jurisdiction in which the case is tried. The “Alter-in-control” approach considers the key issue as which “alter” (personality) was in control at the time of the offense and whether he or she met the insanity standard, the “Each-alter” approach considers whether each personality met the insanity standard, and the “Host-alter” approach considers whether the dominant or primary personality met the insanity standard.9
Legal and mental health professionals are divided on whether DID warrants an acquittal for insanity. The first time DID was recognized as a mental disorder that could excuse criminal responsibility occurred in State v Milligan (1978).10 The court declared serial rapist Billy Milligan insane due to lack of one integrated personality and therefore not culpable of the crimes he committed. Public outrage was extraordinary. Since this case, most DID defenses have not been successful (Table 2).10-16
In a 1980 court case,11 a defendant charged with murder pleaded NGRI due to having multiple personalities. The court found that having alter personalities was not necessarily a mental disease that would preclude responsibility for the murder.
In State v Grimsley (1982),12 the defense used NGRI due to multiple personalities in a drunk driving case. The court ruled that it is immaterial what state of consciousness or personality the defendant was in as long as the personality controlling the behavior was conscious and aware of his or her actions.
In Kirkland v State (1983),13 attorneys for a woman who committed a bank robbery asserted an insanity defense based on a psychogenic fugue, which is sudden, unexpected travel away from home accompanied by inability to recall one’s past and confusion about identity or assumption of a new identity.3 The court found that the law adjudges criminal liability according to the person’s state of mind at the time of the act and will not inquire whether an individual possesses other personalities, fugues, or even moods in which he would not have performed the crime.
In State v Jones (1988),14 the court found the defendant guilty of murdering a woman he met at a bar despite expert testimony that his multiple personalities “paralyzed” him from knowing right from wrong.
More recently, courts have rejected the admissibility of DID evidence, including expert testimony, because the scientific evidence failed to meet reliability standards, and therefore is not ultimately useful to the judge or jury. In State v Greene (1998),15 the defendant claimed that 1 of his 24 alters was responsible for killing his therapist. The Supreme Court of Washington affirmed that evidence of Mr. Greene’s DID, including expert testimony, was not reliable and not admissible.
Similarly, in State v Lockhart (2000),16 Mr. Lockhart contested his conviction of first degree sexual assault on the basis that he was not permitted to present evidence of DID to support his insanity defense. The West Virginia Court held that the diagnosis of DID was speculative and therefore did not meet reliability standards for evidence.
Table 2
Using dissociative identity disorder* as a basis for not guilty by reason of insanity
| Case | Year | Charge | Defense | Court ruling |
|---|---|---|---|---|
| State v Milligan10 | 1978 | Rape | NGRI-MPD | Lack of an integrated personality meant the defendant was not culpable |
| State v Darnall11 | 1980 | Murder | NGRI-MPD | Multiple personalities do not preclude criminal responsibility |
| State v Grimsley12 | 1982 | Drunk driving | NGRI-MPD; primary personality had no control over the ‘alter’ | State of consciousness or personality of defendant is immaterial |
| Kirkland v State13 | 1983 | Bank robbery | NGRI-psychogenic fugue | Law does not inquire about other personalities, fugue states, or moods in cases of criminal liability |
| State v Jones14 | 1988 | Murder | NGRI-MPD | Alter personalities will not be an excuse for inability to distinguish right from wrong |
| State v Greene15 | 1998 | Murder | NGRI-DID; primary personality was ‘unconscious’ | Evidence of DID, including expert testimony, was not admissible because it did not meet reliability standards |
| State v Lockhart16 | 2000 | Sexual assault | NGRI-DID | DID was not allowed into evidence by the West Virginia Court due to lack of scientific evidence |
| *Dissociative identity disorder formerly was referred to as multiple personality disorder DID: dissociative identity disorder; MPD: multiple personality disorder; NGRI: not guilty by reason of insanity. | ||||
Evaluating DID
Because the courts may ask psychiatrists to provide expert opinion on DID to assist with legal rulings, clinicians must remain vigilant to the possibility of DID as well as to defendants who may malinger multiple personalities to evade punishment. In such situations, factors to consider include the mental status examination, data and history collection, collateral information, criminal background, mental health history, history of abuse, and objective assessment tools.
Extensive field testing has shown that the Structured Clinical Interview for Dissociative Disorders (SCID-D) has good reliability and excellent validity.17 The SCID-D allows a trained interviewer to assess the severity of 5 dissociative symptoms: amnesia, depersonalization, derealization, identity confusion, and identity alteration.17 Other tools that may help assess a patient with suspected DID are listed in Table 3.
Patients who commit criminal acts while in a dissociated state may assert a defense of NGRI due to DID, but rarely has this defense been successful. Although a patient may have distinct personalities that control his or her behavior, this condition does not preclude criminal responsibility.
The role of hypnosis in evaluating DID is controversial. The introduction of pseudo-memories and potential for iatrogenic DID may complicate the clinical presentation and subsequent diagnosis.18
Table 3
Tools for diagnosing dissociative identity disorder
| Structured Clinical Interview for Dissociative Disorders |
| Dissociative Disorder Interview Schedule |
| Dissociative Experiences Scale |
| Childhood Trauma Questionnaire |
Related Resource
- West S, Noffsinger S. Is this patient not guilty by reason of insanity? Current Psychiatry. 2006;5(8):54-62.
Disclosure
Dr. Farrell reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Putnam. Diagnosis and treatment of multiple personality disorder. New York, NY: The Guilford Press; 1989.
2. American Psychiatric Association. DSM-5 Development. 300. 14. Dissociative identity disorder. Proposed revision. Available at: http://www.dsm5.org/ProposedRevisions/Pages/proposedrevision.aspx?rid=57. Accessed April 22 2011.
3. Diagnostic and statistical manual of mental disorders. 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
4. Sadock BJ, Sadock VA. eds. Dissociative disorders. In: Sadock BJ, Sadock VA, eds. Kaplan & Sadock’s comprehensive textbook of psychiatry. 7th ed. New York, NY: Lippincott Williams & Wilkins; 2000:1544–1576.
5. Lyons-Ruth K, Dutra L, Schuder MR, et al. From infant attachment disorganization to adult dissociation: relational adaptations or traumatic experiences? Psychiatr Clin North Am. 2006;29(1):63-86, viii.
6. Brahams D. Automatism and post-traumatic stress disorder. Lancet. 1990;335(8701):1333.-
7. Simeon D, Guralnik O, Knutelska M, et al. Personality factors associated with dissociation: temperament, defenses, and cognitive schemata. Am J Psychiatry. 2002;159(3):489-491.
8. Perlin M. The jurisprudence of the insanity defense. Durham NC: Carolina Academic Press; 1994.
9. Steinberg M, Bancroft J, Buchanan J. Multiple personality disorder in criminal law. Bull Am Acad Psychiatry Law. 1993;21(3):345-356.
10. State v Milligan, No 77-CR-11-2908 (Franklin County, Ohio, December 4 1978).
11. State v Darnall, 47 Or App 161, 614 P2d 120 (1980).
12. State v Grimsley, 3 Ohio App 3d 165 444 NE2d 1071 (1982).
13. Kirkland v State, 166 Ga App 478, 304 SE2d 561 (1983).
14. State v Jones, 743 P2d 176 (Wash Ct App 1987) aff’d, 759 P2d 1183, 1185 (Wash 1998).
15. State v Greene, 92 Wn App 80, 960 P2d 980 (1998).
16. State v Lockhart, 208 W Va 622 (2000).
17. Steinberg M, Rounsaville B, Cicchetti D. Detection of dissociative disorders in psychiatric patients by a screening instrument and a structured diagnostic interview. Am J Psychiatry. 1991;148(8):1050-1054.
18. Putnam FW. Dissociative phenomena. In: Tasman A ed. Annual review of psychiatry. Washington, DC: American Psychiatric Press; 1991:145–160.
1. Putnam. Diagnosis and treatment of multiple personality disorder. New York, NY: The Guilford Press; 1989.
2. American Psychiatric Association. DSM-5 Development. 300. 14. Dissociative identity disorder. Proposed revision. Available at: http://www.dsm5.org/ProposedRevisions/Pages/proposedrevision.aspx?rid=57. Accessed April 22 2011.
3. Diagnostic and statistical manual of mental disorders. 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
4. Sadock BJ, Sadock VA. eds. Dissociative disorders. In: Sadock BJ, Sadock VA, eds. Kaplan & Sadock’s comprehensive textbook of psychiatry. 7th ed. New York, NY: Lippincott Williams & Wilkins; 2000:1544–1576.
5. Lyons-Ruth K, Dutra L, Schuder MR, et al. From infant attachment disorganization to adult dissociation: relational adaptations or traumatic experiences? Psychiatr Clin North Am. 2006;29(1):63-86, viii.
6. Brahams D. Automatism and post-traumatic stress disorder. Lancet. 1990;335(8701):1333.-
7. Simeon D, Guralnik O, Knutelska M, et al. Personality factors associated with dissociation: temperament, defenses, and cognitive schemata. Am J Psychiatry. 2002;159(3):489-491.
8. Perlin M. The jurisprudence of the insanity defense. Durham NC: Carolina Academic Press; 1994.
9. Steinberg M, Bancroft J, Buchanan J. Multiple personality disorder in criminal law. Bull Am Acad Psychiatry Law. 1993;21(3):345-356.
10. State v Milligan, No 77-CR-11-2908 (Franklin County, Ohio, December 4 1978).
11. State v Darnall, 47 Or App 161, 614 P2d 120 (1980).
12. State v Grimsley, 3 Ohio App 3d 165 444 NE2d 1071 (1982).
13. Kirkland v State, 166 Ga App 478, 304 SE2d 561 (1983).
14. State v Jones, 743 P2d 176 (Wash Ct App 1987) aff’d, 759 P2d 1183, 1185 (Wash 1998).
15. State v Greene, 92 Wn App 80, 960 P2d 980 (1998).
16. State v Lockhart, 208 W Va 622 (2000).
17. Steinberg M, Rounsaville B, Cicchetti D. Detection of dissociative disorders in psychiatric patients by a screening instrument and a structured diagnostic interview. Am J Psychiatry. 1991;148(8):1050-1054.
18. Putnam FW. Dissociative phenomena. In: Tasman A ed. Annual review of psychiatry. Washington, DC: American Psychiatric Press; 1991:145–160.
Teaching suicidal adolescents how to "walk the middle path"
Possession obsession: Help hoarders escape their own prisons
The popularity of TV shows such as A&E’s Hoarders,TLC’s Hoarding: buried alive,and Planet Green’s Gutted has increased public awareness of problems caused by hoarding. Seventy-five communities across the United States have coordinated hoarding task forces that include therapists, social workers, police, fire departments, and child protective services, and that number is rising quickly.1 Therefore, psychiatrists likely will be encountering growing numbers of hoarders and their families seeking treatment.
Hoarding behavior
Affecting 2% to 5% of the population, compulsive hoarding is persistent difficulty parting with possessions—even useless items or those of limited value—that results in cluttered personal surroundings and impaired functioning.2 Hoarders may be threatened with eviction or the possibility of losing custody of their children.1 Hoarding can create fire hazards, fall risks, and unsanitary environments.3
Causes
Hoarding behavior usually is a result of fear of losing items that may be needed later or making the “wrong” decision about what should be kept or discarded.4Symptoms generally start at age 12 or 13, begin interfering with daily functioning in the mid-30s, and increase in severity with age.2 Clutter can accumulate with or without excessive acquisition of goods, through buying, collecting, or stealing.2Hoarding often is ego-syntonic, and many patients do not believe their behaviors are problematic.3
A new diagnosis?
Hoarding often is associated with obsessive-compulsive disorder (OCD), and DSM-IV-TR lists hoarding behavior as a criterion for obsessive-compulsive personality disorder. However, hoarding behavior has been observed in other neuropsychiatric disorders, including schizophrenia, depression, social phobia, dementia, eating disorders, brain injury, and mental retardation, and in nonclinical populations.3,4
Most research has focused on the connections between hoarding and OCD, but genetics, brain lesions, neuroimaging, and neuropsychological studies suggest that “hoarding disorder” should be a separate entity in DSM-5.2A proposed set of diagnostic criteria states that the hoarding behavior not be restricted to the symptoms of another mental disorder.2 For example, the behavior is not caused by intrusive or recurrent thoughts from OCD or secondary to apathy in depression. The proposed criteria specify if the hoarding is associated with excessive acquisition of items, as well as how much insight the patient has into his or her problem.2
Treatment
Because hoarding behavior frequently is ego-syntonic, patients may be brought in by family members or friends. Treatment should begin with a thorough neuropsychiatric evaluation to determine the etiology of the behavior, such as another axis I disorder.4Assess the amount of clutter, types of items saved, usability of living and work spaces, potential health and safety hazards, beliefs about possessions, information processing deficits, avoidance behaviors, insight, motivation for treatment, social and occupational functioning, and activities of daily living.4
Studies of selective serotonin reuptake inhibitors and cognitive-behavioral therapy (CBT) in OCD patients with hoarding symptoms have produced mixed results.4 In some cases, paroxetine monotherapy, specialized CBT protocols, and combined treatments have proven effective.4 Studies examining those treatments’ efficacy for hoarding in the absence of OCD are underway. Whichever strategy is employed, it is important to involve family members or friends in treatment2 and to identify other available resources, such as community hoarding task forces.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Webley K. Cleaning house. How community task forces are dealing with hoarding one pile of junk at a time. Time. 2010;176:43-44.
2. Mataix-Cols D, Frost R, Pertussa A, et al. Hoarding disorder: a new diagnosis for DSM-V? Depress Anxiety. 2010;27:556-572.
3. Steketee G, Frost R. Compulsive hoarding: current status of the research. Clin Psychol Rev. 2003;23:905-927.
4. Saxena S. Neurobiology and treatment of compulsive hoarding. CNS Spectr. 2008;13:29-36.
The popularity of TV shows such as A&E’s Hoarders,TLC’s Hoarding: buried alive,and Planet Green’s Gutted has increased public awareness of problems caused by hoarding. Seventy-five communities across the United States have coordinated hoarding task forces that include therapists, social workers, police, fire departments, and child protective services, and that number is rising quickly.1 Therefore, psychiatrists likely will be encountering growing numbers of hoarders and their families seeking treatment.
Hoarding behavior
Affecting 2% to 5% of the population, compulsive hoarding is persistent difficulty parting with possessions—even useless items or those of limited value—that results in cluttered personal surroundings and impaired functioning.2 Hoarders may be threatened with eviction or the possibility of losing custody of their children.1 Hoarding can create fire hazards, fall risks, and unsanitary environments.3
Causes
Hoarding behavior usually is a result of fear of losing items that may be needed later or making the “wrong” decision about what should be kept or discarded.4Symptoms generally start at age 12 or 13, begin interfering with daily functioning in the mid-30s, and increase in severity with age.2 Clutter can accumulate with or without excessive acquisition of goods, through buying, collecting, or stealing.2Hoarding often is ego-syntonic, and many patients do not believe their behaviors are problematic.3
A new diagnosis?
Hoarding often is associated with obsessive-compulsive disorder (OCD), and DSM-IV-TR lists hoarding behavior as a criterion for obsessive-compulsive personality disorder. However, hoarding behavior has been observed in other neuropsychiatric disorders, including schizophrenia, depression, social phobia, dementia, eating disorders, brain injury, and mental retardation, and in nonclinical populations.3,4
Most research has focused on the connections between hoarding and OCD, but genetics, brain lesions, neuroimaging, and neuropsychological studies suggest that “hoarding disorder” should be a separate entity in DSM-5.2A proposed set of diagnostic criteria states that the hoarding behavior not be restricted to the symptoms of another mental disorder.2 For example, the behavior is not caused by intrusive or recurrent thoughts from OCD or secondary to apathy in depression. The proposed criteria specify if the hoarding is associated with excessive acquisition of items, as well as how much insight the patient has into his or her problem.2
Treatment
Because hoarding behavior frequently is ego-syntonic, patients may be brought in by family members or friends. Treatment should begin with a thorough neuropsychiatric evaluation to determine the etiology of the behavior, such as another axis I disorder.4Assess the amount of clutter, types of items saved, usability of living and work spaces, potential health and safety hazards, beliefs about possessions, information processing deficits, avoidance behaviors, insight, motivation for treatment, social and occupational functioning, and activities of daily living.4
Studies of selective serotonin reuptake inhibitors and cognitive-behavioral therapy (CBT) in OCD patients with hoarding symptoms have produced mixed results.4 In some cases, paroxetine monotherapy, specialized CBT protocols, and combined treatments have proven effective.4 Studies examining those treatments’ efficacy for hoarding in the absence of OCD are underway. Whichever strategy is employed, it is important to involve family members or friends in treatment2 and to identify other available resources, such as community hoarding task forces.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
The popularity of TV shows such as A&E’s Hoarders,TLC’s Hoarding: buried alive,and Planet Green’s Gutted has increased public awareness of problems caused by hoarding. Seventy-five communities across the United States have coordinated hoarding task forces that include therapists, social workers, police, fire departments, and child protective services, and that number is rising quickly.1 Therefore, psychiatrists likely will be encountering growing numbers of hoarders and their families seeking treatment.
Hoarding behavior
Affecting 2% to 5% of the population, compulsive hoarding is persistent difficulty parting with possessions—even useless items or those of limited value—that results in cluttered personal surroundings and impaired functioning.2 Hoarders may be threatened with eviction or the possibility of losing custody of their children.1 Hoarding can create fire hazards, fall risks, and unsanitary environments.3
Causes
Hoarding behavior usually is a result of fear of losing items that may be needed later or making the “wrong” decision about what should be kept or discarded.4Symptoms generally start at age 12 or 13, begin interfering with daily functioning in the mid-30s, and increase in severity with age.2 Clutter can accumulate with or without excessive acquisition of goods, through buying, collecting, or stealing.2Hoarding often is ego-syntonic, and many patients do not believe their behaviors are problematic.3
A new diagnosis?
Hoarding often is associated with obsessive-compulsive disorder (OCD), and DSM-IV-TR lists hoarding behavior as a criterion for obsessive-compulsive personality disorder. However, hoarding behavior has been observed in other neuropsychiatric disorders, including schizophrenia, depression, social phobia, dementia, eating disorders, brain injury, and mental retardation, and in nonclinical populations.3,4
Most research has focused on the connections between hoarding and OCD, but genetics, brain lesions, neuroimaging, and neuropsychological studies suggest that “hoarding disorder” should be a separate entity in DSM-5.2A proposed set of diagnostic criteria states that the hoarding behavior not be restricted to the symptoms of another mental disorder.2 For example, the behavior is not caused by intrusive or recurrent thoughts from OCD or secondary to apathy in depression. The proposed criteria specify if the hoarding is associated with excessive acquisition of items, as well as how much insight the patient has into his or her problem.2
Treatment
Because hoarding behavior frequently is ego-syntonic, patients may be brought in by family members or friends. Treatment should begin with a thorough neuropsychiatric evaluation to determine the etiology of the behavior, such as another axis I disorder.4Assess the amount of clutter, types of items saved, usability of living and work spaces, potential health and safety hazards, beliefs about possessions, information processing deficits, avoidance behaviors, insight, motivation for treatment, social and occupational functioning, and activities of daily living.4
Studies of selective serotonin reuptake inhibitors and cognitive-behavioral therapy (CBT) in OCD patients with hoarding symptoms have produced mixed results.4 In some cases, paroxetine monotherapy, specialized CBT protocols, and combined treatments have proven effective.4 Studies examining those treatments’ efficacy for hoarding in the absence of OCD are underway. Whichever strategy is employed, it is important to involve family members or friends in treatment2 and to identify other available resources, such as community hoarding task forces.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Webley K. Cleaning house. How community task forces are dealing with hoarding one pile of junk at a time. Time. 2010;176:43-44.
2. Mataix-Cols D, Frost R, Pertussa A, et al. Hoarding disorder: a new diagnosis for DSM-V? Depress Anxiety. 2010;27:556-572.
3. Steketee G, Frost R. Compulsive hoarding: current status of the research. Clin Psychol Rev. 2003;23:905-927.
4. Saxena S. Neurobiology and treatment of compulsive hoarding. CNS Spectr. 2008;13:29-36.
1. Webley K. Cleaning house. How community task forces are dealing with hoarding one pile of junk at a time. Time. 2010;176:43-44.
2. Mataix-Cols D, Frost R, Pertussa A, et al. Hoarding disorder: a new diagnosis for DSM-V? Depress Anxiety. 2010;27:556-572.
3. Steketee G, Frost R. Compulsive hoarding: current status of the research. Clin Psychol Rev. 2003;23:905-927.
4. Saxena S. Neurobiology and treatment of compulsive hoarding. CNS Spectr. 2008;13:29-36.