User login
Investigational Drug Improves Maintenance of Wakefulness
DENVER—An investigational drug known as JZP-110 significantly improves the ability to stay awake, compared with placebo, in patients with narcolepsy, according to data presented at the 30th Anniversary Meeting of the Associated Professional Sleep Societies. The large effect sizes associated with the drug confirm the robustness of the results, according to the researchers.
JZP-110 is a selective dopamine and norepinephrine reuptake inhibitor in development as a treatment for excessive sleepiness and impaired wakefulness associated with narcolepsy and obstructive sleep apnea. In phase II trials, the drug improved wakefulness, compared with placebo, on the 40-minute Maintenance of Wakefulness Test (MWT). Studies of other agents, however, have reported sleep latency results using a 20-minute MWT.
Chad Ruoff, MD, Clinical Assistant Professor of Psychiatry and Behavioral Sciences at the Stanford Center for Sleep Sciences and Medicine in California, and colleagues conducted a post hoc analysis of data from two phase II trials to evaluate changes from baseline in mean MWT sleep latency associated with JZP-110, censoring data to include only the first 20 minutes of the 40-minute MWT. In one study, 33 adults with narcolepsy (with or without cataplexy) were randomized to receive two weeks of treatment with placebo or JZP-110. Active treatment was administered at a dose of 150 mg/day during the first week and at a dose of 300 mg/day during the second week. In the second study, 93 adults with narcolepsy (with or without cataplexy) were randomized to receive placebo or JZP-110 for 12 weeks. The dose of drug was 150 mg/day during the first four weeks and 300 mg/day for the remaining eight weeks.
Regardless of whether the data were censored at 20 minutes or at 40 minutes, JZP-110 resulted in a statistically significant increase from baseline in MWT sleep latency, compared with placebo, in both studies. In the first study, mean changes in sleep latency were 12.7 minutes with the drug versus 0.9 minutes with placebo when censored at 40 minutes. The changes were 8.9 minutes with drug and 0.4 minutes with placebo when data were censored at 20 minutes. In the second study, mean changes in MWT were 12.8 minutes with JZP-110 and 2.1 minutes with placebo when data were censored at 40 minutes. Mean changes were 8.9 minutes for drug and 1.1 minutes for placebo when data were censored at 20 minutes.
Effect sizes were large and slightly greater for 20-minute censored data (1.54 in the first study and 1.41 in the second study) than for 40-minute censored data (1.37 in the first study and 1.17 in the second study). Researchers observed two serious adverse events--one case of conversion disorder and one case of acute cholecystitis--that they considered unrelated to the study drug. Few discontinuations resulted from adverse events.
—Erik Greb
DENVER—An investigational drug known as JZP-110 significantly improves the ability to stay awake, compared with placebo, in patients with narcolepsy, according to data presented at the 30th Anniversary Meeting of the Associated Professional Sleep Societies. The large effect sizes associated with the drug confirm the robustness of the results, according to the researchers.
JZP-110 is a selective dopamine and norepinephrine reuptake inhibitor in development as a treatment for excessive sleepiness and impaired wakefulness associated with narcolepsy and obstructive sleep apnea. In phase II trials, the drug improved wakefulness, compared with placebo, on the 40-minute Maintenance of Wakefulness Test (MWT). Studies of other agents, however, have reported sleep latency results using a 20-minute MWT.
Chad Ruoff, MD, Clinical Assistant Professor of Psychiatry and Behavioral Sciences at the Stanford Center for Sleep Sciences and Medicine in California, and colleagues conducted a post hoc analysis of data from two phase II trials to evaluate changes from baseline in mean MWT sleep latency associated with JZP-110, censoring data to include only the first 20 minutes of the 40-minute MWT. In one study, 33 adults with narcolepsy (with or without cataplexy) were randomized to receive two weeks of treatment with placebo or JZP-110. Active treatment was administered at a dose of 150 mg/day during the first week and at a dose of 300 mg/day during the second week. In the second study, 93 adults with narcolepsy (with or without cataplexy) were randomized to receive placebo or JZP-110 for 12 weeks. The dose of drug was 150 mg/day during the first four weeks and 300 mg/day for the remaining eight weeks.
Regardless of whether the data were censored at 20 minutes or at 40 minutes, JZP-110 resulted in a statistically significant increase from baseline in MWT sleep latency, compared with placebo, in both studies. In the first study, mean changes in sleep latency were 12.7 minutes with the drug versus 0.9 minutes with placebo when censored at 40 minutes. The changes were 8.9 minutes with drug and 0.4 minutes with placebo when data were censored at 20 minutes. In the second study, mean changes in MWT were 12.8 minutes with JZP-110 and 2.1 minutes with placebo when data were censored at 40 minutes. Mean changes were 8.9 minutes for drug and 1.1 minutes for placebo when data were censored at 20 minutes.
Effect sizes were large and slightly greater for 20-minute censored data (1.54 in the first study and 1.41 in the second study) than for 40-minute censored data (1.37 in the first study and 1.17 in the second study). Researchers observed two serious adverse events--one case of conversion disorder and one case of acute cholecystitis--that they considered unrelated to the study drug. Few discontinuations resulted from adverse events.
—Erik Greb
DENVER—An investigational drug known as JZP-110 significantly improves the ability to stay awake, compared with placebo, in patients with narcolepsy, according to data presented at the 30th Anniversary Meeting of the Associated Professional Sleep Societies. The large effect sizes associated with the drug confirm the robustness of the results, according to the researchers.
JZP-110 is a selective dopamine and norepinephrine reuptake inhibitor in development as a treatment for excessive sleepiness and impaired wakefulness associated with narcolepsy and obstructive sleep apnea. In phase II trials, the drug improved wakefulness, compared with placebo, on the 40-minute Maintenance of Wakefulness Test (MWT). Studies of other agents, however, have reported sleep latency results using a 20-minute MWT.
Chad Ruoff, MD, Clinical Assistant Professor of Psychiatry and Behavioral Sciences at the Stanford Center for Sleep Sciences and Medicine in California, and colleagues conducted a post hoc analysis of data from two phase II trials to evaluate changes from baseline in mean MWT sleep latency associated with JZP-110, censoring data to include only the first 20 minutes of the 40-minute MWT. In one study, 33 adults with narcolepsy (with or without cataplexy) were randomized to receive two weeks of treatment with placebo or JZP-110. Active treatment was administered at a dose of 150 mg/day during the first week and at a dose of 300 mg/day during the second week. In the second study, 93 adults with narcolepsy (with or without cataplexy) were randomized to receive placebo or JZP-110 for 12 weeks. The dose of drug was 150 mg/day during the first four weeks and 300 mg/day for the remaining eight weeks.
Regardless of whether the data were censored at 20 minutes or at 40 minutes, JZP-110 resulted in a statistically significant increase from baseline in MWT sleep latency, compared with placebo, in both studies. In the first study, mean changes in sleep latency were 12.7 minutes with the drug versus 0.9 minutes with placebo when censored at 40 minutes. The changes were 8.9 minutes with drug and 0.4 minutes with placebo when data were censored at 20 minutes. In the second study, mean changes in MWT were 12.8 minutes with JZP-110 and 2.1 minutes with placebo when data were censored at 40 minutes. Mean changes were 8.9 minutes for drug and 1.1 minutes for placebo when data were censored at 20 minutes.
Effect sizes were large and slightly greater for 20-minute censored data (1.54 in the first study and 1.41 in the second study) than for 40-minute censored data (1.37 in the first study and 1.17 in the second study). Researchers observed two serious adverse events--one case of conversion disorder and one case of acute cholecystitis--that they considered unrelated to the study drug. Few discontinuations resulted from adverse events.
—Erik Greb
What Are the Next-Morning Effects of Hypnotic Drugs?
DENVER—Sleep medication, when administered in recommended dosages at bedtime, can significantly impair next-morning short- and long-term memory, according to data presented at the 30th Anniversary Meeting of the Associated Professional Sleep Societies. Additionally, the medication significantly impairs psychomotor speed in healthy adults, but not in the elderly.
Joris C. Verster, PhD, Associate Professor in the Division of Pharmacology at Utrecht University in the Netherlands, and colleagues conducted two meta-analyses on the next-morning effects of hypnotic drugs. In one analysis, they looked at the drugs’ effects on short- and long-term memory functioning in healthy adults and in the elderly. In another study, they examined the next-morning effects on psychomotor speed and motor control in the same two age groups. For these meta-analyses, Dr. Verster and colleagues identified 33,969 potentially relevant articles.
Morning-After Effects on Memory
Studies were included if they assessed next-morning short- and long-term memory after bedtime administration of recommended dosages of hypnotic drugs and were double-blind, placebo-controlled, and conducted in healthy volunteers, and if sufficient data were reported. Separate analyses were performed for adults (ages 18 to 65) and for elderly healthy volunteers (age 65 or older).
In adults, eight studies assessing next-morning short-term memory (after bedtime administration of nitrazepam, triazolam, temazepam, flurazepam, melatonin, zaleplon, lormetazepam, or zolpidem) and five studies assessing long-term memory (after bedtime administration of triazolam, nitrazepam, zopiclone, flurazepam, or zolpidem) were included in the meta-analysis. The analysis revealed that next-morning short- and long-term memory were significantly impaired.
In the elderly, three studies assessing next-morning short-term memory (after bedtime administration of flurazepam, zolpidem, or temazepam) and three studies assessing long-term memory (after bedtime administration of flurazepam, zolpidem, or temazepam) were included in the meta-analysis. This analysis revealed that in the elderly, next-morning short-term memory was significantly impaired, but no significant impairment was detected in long-term memory.
Morning-After Effects on Psychomotor Speed and Motor Control
Studies were included in the analysis if they assessed next-morning effects on psychomotor speed or motor control after bedtime administration of recommended dosages of hypnotic drugs. As in the meta-analyses described above, studies also had to be double-blind, placebo-controlled, and conducted in healthy subjects, and to provide sufficient data.
In adults, 15 studies assessing next-morning psychomotor speed and five studies assessing next-morning motor control were included in the meta-analysis. This analysis revealed that next-morning psychomotor speed was significantly impaired, whereas next-morning motor control was not.
In the elderly, six studies assessing next-morning psychomotor speed and three studies assessing next-morning motor control were included in the meta-analysis. This analysis revealed that in the elderly, next-morning psychomotor speed and motor control were not significantly impaired. Taken together, the analyses show that skills and abilities that are relevant to daily activities such as driving a car or job performance may be impaired the day after using hypnotic drugs.
—Glenn S. Williams
DENVER—Sleep medication, when administered in recommended dosages at bedtime, can significantly impair next-morning short- and long-term memory, according to data presented at the 30th Anniversary Meeting of the Associated Professional Sleep Societies. Additionally, the medication significantly impairs psychomotor speed in healthy adults, but not in the elderly.
Joris C. Verster, PhD, Associate Professor in the Division of Pharmacology at Utrecht University in the Netherlands, and colleagues conducted two meta-analyses on the next-morning effects of hypnotic drugs. In one analysis, they looked at the drugs’ effects on short- and long-term memory functioning in healthy adults and in the elderly. In another study, they examined the next-morning effects on psychomotor speed and motor control in the same two age groups. For these meta-analyses, Dr. Verster and colleagues identified 33,969 potentially relevant articles.
Morning-After Effects on Memory
Studies were included if they assessed next-morning short- and long-term memory after bedtime administration of recommended dosages of hypnotic drugs and were double-blind, placebo-controlled, and conducted in healthy volunteers, and if sufficient data were reported. Separate analyses were performed for adults (ages 18 to 65) and for elderly healthy volunteers (age 65 or older).
In adults, eight studies assessing next-morning short-term memory (after bedtime administration of nitrazepam, triazolam, temazepam, flurazepam, melatonin, zaleplon, lormetazepam, or zolpidem) and five studies assessing long-term memory (after bedtime administration of triazolam, nitrazepam, zopiclone, flurazepam, or zolpidem) were included in the meta-analysis. The analysis revealed that next-morning short- and long-term memory were significantly impaired.
In the elderly, three studies assessing next-morning short-term memory (after bedtime administration of flurazepam, zolpidem, or temazepam) and three studies assessing long-term memory (after bedtime administration of flurazepam, zolpidem, or temazepam) were included in the meta-analysis. This analysis revealed that in the elderly, next-morning short-term memory was significantly impaired, but no significant impairment was detected in long-term memory.
Morning-After Effects on Psychomotor Speed and Motor Control
Studies were included in the analysis if they assessed next-morning effects on psychomotor speed or motor control after bedtime administration of recommended dosages of hypnotic drugs. As in the meta-analyses described above, studies also had to be double-blind, placebo-controlled, and conducted in healthy subjects, and to provide sufficient data.
In adults, 15 studies assessing next-morning psychomotor speed and five studies assessing next-morning motor control were included in the meta-analysis. This analysis revealed that next-morning psychomotor speed was significantly impaired, whereas next-morning motor control was not.
In the elderly, six studies assessing next-morning psychomotor speed and three studies assessing next-morning motor control were included in the meta-analysis. This analysis revealed that in the elderly, next-morning psychomotor speed and motor control were not significantly impaired. Taken together, the analyses show that skills and abilities that are relevant to daily activities such as driving a car or job performance may be impaired the day after using hypnotic drugs.
—Glenn S. Williams
DENVER—Sleep medication, when administered in recommended dosages at bedtime, can significantly impair next-morning short- and long-term memory, according to data presented at the 30th Anniversary Meeting of the Associated Professional Sleep Societies. Additionally, the medication significantly impairs psychomotor speed in healthy adults, but not in the elderly.
Joris C. Verster, PhD, Associate Professor in the Division of Pharmacology at Utrecht University in the Netherlands, and colleagues conducted two meta-analyses on the next-morning effects of hypnotic drugs. In one analysis, they looked at the drugs’ effects on short- and long-term memory functioning in healthy adults and in the elderly. In another study, they examined the next-morning effects on psychomotor speed and motor control in the same two age groups. For these meta-analyses, Dr. Verster and colleagues identified 33,969 potentially relevant articles.
Morning-After Effects on Memory
Studies were included if they assessed next-morning short- and long-term memory after bedtime administration of recommended dosages of hypnotic drugs and were double-blind, placebo-controlled, and conducted in healthy volunteers, and if sufficient data were reported. Separate analyses were performed for adults (ages 18 to 65) and for elderly healthy volunteers (age 65 or older).
In adults, eight studies assessing next-morning short-term memory (after bedtime administration of nitrazepam, triazolam, temazepam, flurazepam, melatonin, zaleplon, lormetazepam, or zolpidem) and five studies assessing long-term memory (after bedtime administration of triazolam, nitrazepam, zopiclone, flurazepam, or zolpidem) were included in the meta-analysis. The analysis revealed that next-morning short- and long-term memory were significantly impaired.
In the elderly, three studies assessing next-morning short-term memory (after bedtime administration of flurazepam, zolpidem, or temazepam) and three studies assessing long-term memory (after bedtime administration of flurazepam, zolpidem, or temazepam) were included in the meta-analysis. This analysis revealed that in the elderly, next-morning short-term memory was significantly impaired, but no significant impairment was detected in long-term memory.
Morning-After Effects on Psychomotor Speed and Motor Control
Studies were included in the analysis if they assessed next-morning effects on psychomotor speed or motor control after bedtime administration of recommended dosages of hypnotic drugs. As in the meta-analyses described above, studies also had to be double-blind, placebo-controlled, and conducted in healthy subjects, and to provide sufficient data.
In adults, 15 studies assessing next-morning psychomotor speed and five studies assessing next-morning motor control were included in the meta-analysis. This analysis revealed that next-morning psychomotor speed was significantly impaired, whereas next-morning motor control was not.
In the elderly, six studies assessing next-morning psychomotor speed and three studies assessing next-morning motor control were included in the meta-analysis. This analysis revealed that in the elderly, next-morning psychomotor speed and motor control were not significantly impaired. Taken together, the analyses show that skills and abilities that are relevant to daily activities such as driving a car or job performance may be impaired the day after using hypnotic drugs.
—Glenn S. Williams
Sleep doctor: Less than 7 hours can worsen diabetes
SAN DIEGO – A sleep specialist told an audience of diabetes educators that quality sleep is “profoundly important” to the health of their patients, and regularly sleeping fewer than 7 hours a night can wreak havoc on glucose levels and insulin resistance.
There’s even evidence of a link between lack of sleep, diabetes, and heart disease, according to Terese C. Hammond, MD, medical director of the Keck Hospital of the University of Southern California Sleep Disorders Center in Los Angeles. “We don’t know which way the cause goes, but we know there’s a connection,” she said.
Dr. Hammond, who spoke at the annual meeting of the American Association of Diabetes Educators, noted that the vast majority of adults need 7-9 hours of sleep a night.
If you repeatedly don’t reach 7 hours, “there is ample evidence that some metabolic and biologic things happen to your body. Glucose goes up and insulin is secreted. Leptin decreases – the protein that tells us when we’re sated, when our hunger is satisfied. It’s a pretty potent combination, and this is associated with increases in weight and carbohydrate intake,” Dr. Hammond said.
Indeed, findings from one small study suggest a link between chronic insufficient sleep to consumption of more calories, mostly carbohydrates. The study authors speculated this may be because people eat extra food to account for being awake more but take in more than they need (Proc Natl Acad Sci USA. 2013 Apr;110[14]:5695-700).
It is possible for people to pay off a “sleep debt” by catching up on sleep, Dr. Hammond said, but only if the sleep is lost temporarily, as during a heavy medical rotation or after a personal tragedy. When sleep loss is chronic, she said, “it’s becoming apparent that the end-organ consequences are not fully recoverable.”
In regard to diabetes specifically, she said, research has linked insufficient sleep to higher rates of central obesity, higher rates of diabetes in blacks and whites, impaired glucose tolerance, decreased insulin, metabolic syndrome, and high lipids. Too much sleep has also been linked to poor health outcomes.
How can medical professionals help patients improve sleep? “The most important thing to remember about sleep is that it’s a very primitive process,” according to Dr. Hammond. “You can’t think yourself into better sleep. You have to act yourself into better sleep through light, temperature, sound, and repetitive behaviors.”
Controversial research has linked sleeping pills to higher mortality rates, she says.“I try to avoid them long term for insomnia, and not only because there’s probably an increased risk. They stop working eventually.”
Another approach, cognitive behavioral therapy (CBT), is “the most potent way to change behavior,” she said.
“CBT improves sleep efficiency in a vast majority of chronic medical diseases,” she said. “It does just as well as drugs and better than most sleeping pills.”
According to Dr. Hammond, CBT focuses on several strategies:
• Education about sleep hygiene, such as limiting the bedroom to nighttime sleep and intimacy, going to bed at the same time every night, and focusing on a dark, cool, quiet environment.
• Increasing the “sleep drive” through temporary sleep deprivation.
• Relaxation training through techniques like guided imagery, biofeedback, progressive muscle relaxation, and self-hypnosis.
Dr. Hammond reported having no relevant financial disclosures.
SAN DIEGO – A sleep specialist told an audience of diabetes educators that quality sleep is “profoundly important” to the health of their patients, and regularly sleeping fewer than 7 hours a night can wreak havoc on glucose levels and insulin resistance.
There’s even evidence of a link between lack of sleep, diabetes, and heart disease, according to Terese C. Hammond, MD, medical director of the Keck Hospital of the University of Southern California Sleep Disorders Center in Los Angeles. “We don’t know which way the cause goes, but we know there’s a connection,” she said.
Dr. Hammond, who spoke at the annual meeting of the American Association of Diabetes Educators, noted that the vast majority of adults need 7-9 hours of sleep a night.
If you repeatedly don’t reach 7 hours, “there is ample evidence that some metabolic and biologic things happen to your body. Glucose goes up and insulin is secreted. Leptin decreases – the protein that tells us when we’re sated, when our hunger is satisfied. It’s a pretty potent combination, and this is associated with increases in weight and carbohydrate intake,” Dr. Hammond said.
Indeed, findings from one small study suggest a link between chronic insufficient sleep to consumption of more calories, mostly carbohydrates. The study authors speculated this may be because people eat extra food to account for being awake more but take in more than they need (Proc Natl Acad Sci USA. 2013 Apr;110[14]:5695-700).
It is possible for people to pay off a “sleep debt” by catching up on sleep, Dr. Hammond said, but only if the sleep is lost temporarily, as during a heavy medical rotation or after a personal tragedy. When sleep loss is chronic, she said, “it’s becoming apparent that the end-organ consequences are not fully recoverable.”
In regard to diabetes specifically, she said, research has linked insufficient sleep to higher rates of central obesity, higher rates of diabetes in blacks and whites, impaired glucose tolerance, decreased insulin, metabolic syndrome, and high lipids. Too much sleep has also been linked to poor health outcomes.
How can medical professionals help patients improve sleep? “The most important thing to remember about sleep is that it’s a very primitive process,” according to Dr. Hammond. “You can’t think yourself into better sleep. You have to act yourself into better sleep through light, temperature, sound, and repetitive behaviors.”
Controversial research has linked sleeping pills to higher mortality rates, she says.“I try to avoid them long term for insomnia, and not only because there’s probably an increased risk. They stop working eventually.”
Another approach, cognitive behavioral therapy (CBT), is “the most potent way to change behavior,” she said.
“CBT improves sleep efficiency in a vast majority of chronic medical diseases,” she said. “It does just as well as drugs and better than most sleeping pills.”
According to Dr. Hammond, CBT focuses on several strategies:
• Education about sleep hygiene, such as limiting the bedroom to nighttime sleep and intimacy, going to bed at the same time every night, and focusing on a dark, cool, quiet environment.
• Increasing the “sleep drive” through temporary sleep deprivation.
• Relaxation training through techniques like guided imagery, biofeedback, progressive muscle relaxation, and self-hypnosis.
Dr. Hammond reported having no relevant financial disclosures.
SAN DIEGO – A sleep specialist told an audience of diabetes educators that quality sleep is “profoundly important” to the health of their patients, and regularly sleeping fewer than 7 hours a night can wreak havoc on glucose levels and insulin resistance.
There’s even evidence of a link between lack of sleep, diabetes, and heart disease, according to Terese C. Hammond, MD, medical director of the Keck Hospital of the University of Southern California Sleep Disorders Center in Los Angeles. “We don’t know which way the cause goes, but we know there’s a connection,” she said.
Dr. Hammond, who spoke at the annual meeting of the American Association of Diabetes Educators, noted that the vast majority of adults need 7-9 hours of sleep a night.
If you repeatedly don’t reach 7 hours, “there is ample evidence that some metabolic and biologic things happen to your body. Glucose goes up and insulin is secreted. Leptin decreases – the protein that tells us when we’re sated, when our hunger is satisfied. It’s a pretty potent combination, and this is associated with increases in weight and carbohydrate intake,” Dr. Hammond said.
Indeed, findings from one small study suggest a link between chronic insufficient sleep to consumption of more calories, mostly carbohydrates. The study authors speculated this may be because people eat extra food to account for being awake more but take in more than they need (Proc Natl Acad Sci USA. 2013 Apr;110[14]:5695-700).
It is possible for people to pay off a “sleep debt” by catching up on sleep, Dr. Hammond said, but only if the sleep is lost temporarily, as during a heavy medical rotation or after a personal tragedy. When sleep loss is chronic, she said, “it’s becoming apparent that the end-organ consequences are not fully recoverable.”
In regard to diabetes specifically, she said, research has linked insufficient sleep to higher rates of central obesity, higher rates of diabetes in blacks and whites, impaired glucose tolerance, decreased insulin, metabolic syndrome, and high lipids. Too much sleep has also been linked to poor health outcomes.
How can medical professionals help patients improve sleep? “The most important thing to remember about sleep is that it’s a very primitive process,” according to Dr. Hammond. “You can’t think yourself into better sleep. You have to act yourself into better sleep through light, temperature, sound, and repetitive behaviors.”
Controversial research has linked sleeping pills to higher mortality rates, she says.“I try to avoid them long term for insomnia, and not only because there’s probably an increased risk. They stop working eventually.”
Another approach, cognitive behavioral therapy (CBT), is “the most potent way to change behavior,” she said.
“CBT improves sleep efficiency in a vast majority of chronic medical diseases,” she said. “It does just as well as drugs and better than most sleeping pills.”
According to Dr. Hammond, CBT focuses on several strategies:
• Education about sleep hygiene, such as limiting the bedroom to nighttime sleep and intimacy, going to bed at the same time every night, and focusing on a dark, cool, quiet environment.
• Increasing the “sleep drive” through temporary sleep deprivation.
• Relaxation training through techniques like guided imagery, biofeedback, progressive muscle relaxation, and self-hypnosis.
Dr. Hammond reported having no relevant financial disclosures.
AT AADE 16
Hypoxia of obstructive sleep apnea aggravates NAFLD, NASH in adolescents
A new study has found that a strong association exists in adolescents who have obstructive sleep apnea, and their risks of developing more highly progressed forms of nonalcoholic fatty liver disease (NAFLD) or nonalcoholic steatohepatitis (NASH).
“Substantial evidence suggests oxidative stress is a central mediator in NAFLD pathogenesis and progression, although the specific trigger for reactive oxygen species (ROS) generation has not been clearly delineated,” wrote the authors, led by Shikha S. Sundaram, MD of the University of Colorado at Denver, Aurora, adding that “Emerging evidence demonstrates that obesity-related obstructive sleep apnea (OSA) and intermittent nocturnal hypoxia are associated with NAFLD progression.”
Dr. Sundaram and her coinvestigators looked at patients admitted to the Children’s Hospital Colorado Pediatric Liver Center from June 2009 through January 2014. Subjects included were children ages 8-18 years, male and female, who were classified as Tanner stage 2-4 with liver biopsy evidence of NAFLD.
“In our center, a clinical liver biopsy for suspected NAFLD is performed in overweight or obese children (body mass index greater than 85% for age and gender) with chronically elevated aminotransferases in whom a diagnosis is unclear based on serologic testing,” Dr. Sundaram and her coauthors clarified regarding the screening process.
Additionally, age-matched “lean” children, that is, those with a body mass index lower than 85%, were also enrolled as controls; these subjects were included if they had no evidence of hepatomegaly or liver disease – translated to AST and ALT levels of 640 IU/L – and were also Tanner stage 2-4. The authors explained that this Tanner stage range was chosen in order to “minimize variations in insulin sensitivity that may confound the interpretation of potential associations between OSA/hypoxia and NAFLD.”
Ultimately, 36 NAFLD adolescent subjects and 14 controls completed the study. A total of 25 of the 36 NAFLD subjects (69.4%) had OSA and/or nocturnal hypoxia; of these, 15 were classified as having isolated OSA, 9 had both OSA and hypoxia, and 1 had isolated hypoxia. Polysomnograms found that all NAFLD subjects spent more than 12% of their total time asleep in REM sleep, which was deemed adequate enough to consider the findings valid.
Based on liver histology scoring, laboratory testing, urine F2-isoprostanes, and 4-hydroxynonenal liver immunohistochemistry tests that were conducted on all subjects, Dr. Sundaram and her coinvestigators found that subjects with OSA or hypoxia had more severe fibrosis than did those without. While the latter cohort were 100% stage 0-2, only 64% of those with OSA/hypoxia were stage 0-2, while the remaining 36% were stage 3 (P = .03). Additionally, higher F2-isoprostanes – used to measure lipid peroxidation – correlated with apnea/hypoxia index (r = 0.39; P = .03), and the most severe OSA/hypoxia occurred in subjects that had the greatest 4-hydroxynonenal staining (P = .03). Furthermore, an increase in both F2-isoprostanes and 4-hydroxynonenal hepatic staining was shown to lead to a higher risk of worse steatosis: r = 0.32 and r = 0.47, respectively (P = .04 and P = .007).
“These data support sleep disordered breathing as an important trigger of oxidative stress that promotes progression of pediatric NAFLD to NASH,” the authors concluded, adding that “this study confirms that OSA/hypoxia is common in pediatric NAFLD and that more severe OSA/hypoxia is associated with elevated aminotransferases, hepatic steatosis, inflammation, NAS [NAFLD activity score], and fibrosis.”
Dr. Sundaram and her coauthors call for further research to examine if “prevention or reversal of NASH following effective therapy of OSA and nocturnal hypoxia in obese patients” is viable.
This study was supported by funding from the National Institutes of Health. Dr. Sundaram and her coinvestigators did not report any relevant financial disclosures.
A new study has found that a strong association exists in adolescents who have obstructive sleep apnea, and their risks of developing more highly progressed forms of nonalcoholic fatty liver disease (NAFLD) or nonalcoholic steatohepatitis (NASH).
“Substantial evidence suggests oxidative stress is a central mediator in NAFLD pathogenesis and progression, although the specific trigger for reactive oxygen species (ROS) generation has not been clearly delineated,” wrote the authors, led by Shikha S. Sundaram, MD of the University of Colorado at Denver, Aurora, adding that “Emerging evidence demonstrates that obesity-related obstructive sleep apnea (OSA) and intermittent nocturnal hypoxia are associated with NAFLD progression.”
Dr. Sundaram and her coinvestigators looked at patients admitted to the Children’s Hospital Colorado Pediatric Liver Center from June 2009 through January 2014. Subjects included were children ages 8-18 years, male and female, who were classified as Tanner stage 2-4 with liver biopsy evidence of NAFLD.
“In our center, a clinical liver biopsy for suspected NAFLD is performed in overweight or obese children (body mass index greater than 85% for age and gender) with chronically elevated aminotransferases in whom a diagnosis is unclear based on serologic testing,” Dr. Sundaram and her coauthors clarified regarding the screening process.
Additionally, age-matched “lean” children, that is, those with a body mass index lower than 85%, were also enrolled as controls; these subjects were included if they had no evidence of hepatomegaly or liver disease – translated to AST and ALT levels of 640 IU/L – and were also Tanner stage 2-4. The authors explained that this Tanner stage range was chosen in order to “minimize variations in insulin sensitivity that may confound the interpretation of potential associations between OSA/hypoxia and NAFLD.”
Ultimately, 36 NAFLD adolescent subjects and 14 controls completed the study. A total of 25 of the 36 NAFLD subjects (69.4%) had OSA and/or nocturnal hypoxia; of these, 15 were classified as having isolated OSA, 9 had both OSA and hypoxia, and 1 had isolated hypoxia. Polysomnograms found that all NAFLD subjects spent more than 12% of their total time asleep in REM sleep, which was deemed adequate enough to consider the findings valid.
Based on liver histology scoring, laboratory testing, urine F2-isoprostanes, and 4-hydroxynonenal liver immunohistochemistry tests that were conducted on all subjects, Dr. Sundaram and her coinvestigators found that subjects with OSA or hypoxia had more severe fibrosis than did those without. While the latter cohort were 100% stage 0-2, only 64% of those with OSA/hypoxia were stage 0-2, while the remaining 36% were stage 3 (P = .03). Additionally, higher F2-isoprostanes – used to measure lipid peroxidation – correlated with apnea/hypoxia index (r = 0.39; P = .03), and the most severe OSA/hypoxia occurred in subjects that had the greatest 4-hydroxynonenal staining (P = .03). Furthermore, an increase in both F2-isoprostanes and 4-hydroxynonenal hepatic staining was shown to lead to a higher risk of worse steatosis: r = 0.32 and r = 0.47, respectively (P = .04 and P = .007).
“These data support sleep disordered breathing as an important trigger of oxidative stress that promotes progression of pediatric NAFLD to NASH,” the authors concluded, adding that “this study confirms that OSA/hypoxia is common in pediatric NAFLD and that more severe OSA/hypoxia is associated with elevated aminotransferases, hepatic steatosis, inflammation, NAS [NAFLD activity score], and fibrosis.”
Dr. Sundaram and her coauthors call for further research to examine if “prevention or reversal of NASH following effective therapy of OSA and nocturnal hypoxia in obese patients” is viable.
This study was supported by funding from the National Institutes of Health. Dr. Sundaram and her coinvestigators did not report any relevant financial disclosures.
A new study has found that a strong association exists in adolescents who have obstructive sleep apnea, and their risks of developing more highly progressed forms of nonalcoholic fatty liver disease (NAFLD) or nonalcoholic steatohepatitis (NASH).
“Substantial evidence suggests oxidative stress is a central mediator in NAFLD pathogenesis and progression, although the specific trigger for reactive oxygen species (ROS) generation has not been clearly delineated,” wrote the authors, led by Shikha S. Sundaram, MD of the University of Colorado at Denver, Aurora, adding that “Emerging evidence demonstrates that obesity-related obstructive sleep apnea (OSA) and intermittent nocturnal hypoxia are associated with NAFLD progression.”
Dr. Sundaram and her coinvestigators looked at patients admitted to the Children’s Hospital Colorado Pediatric Liver Center from June 2009 through January 2014. Subjects included were children ages 8-18 years, male and female, who were classified as Tanner stage 2-4 with liver biopsy evidence of NAFLD.
“In our center, a clinical liver biopsy for suspected NAFLD is performed in overweight or obese children (body mass index greater than 85% for age and gender) with chronically elevated aminotransferases in whom a diagnosis is unclear based on serologic testing,” Dr. Sundaram and her coauthors clarified regarding the screening process.
Additionally, age-matched “lean” children, that is, those with a body mass index lower than 85%, were also enrolled as controls; these subjects were included if they had no evidence of hepatomegaly or liver disease – translated to AST and ALT levels of 640 IU/L – and were also Tanner stage 2-4. The authors explained that this Tanner stage range was chosen in order to “minimize variations in insulin sensitivity that may confound the interpretation of potential associations between OSA/hypoxia and NAFLD.”
Ultimately, 36 NAFLD adolescent subjects and 14 controls completed the study. A total of 25 of the 36 NAFLD subjects (69.4%) had OSA and/or nocturnal hypoxia; of these, 15 were classified as having isolated OSA, 9 had both OSA and hypoxia, and 1 had isolated hypoxia. Polysomnograms found that all NAFLD subjects spent more than 12% of their total time asleep in REM sleep, which was deemed adequate enough to consider the findings valid.
Based on liver histology scoring, laboratory testing, urine F2-isoprostanes, and 4-hydroxynonenal liver immunohistochemistry tests that were conducted on all subjects, Dr. Sundaram and her coinvestigators found that subjects with OSA or hypoxia had more severe fibrosis than did those without. While the latter cohort were 100% stage 0-2, only 64% of those with OSA/hypoxia were stage 0-2, while the remaining 36% were stage 3 (P = .03). Additionally, higher F2-isoprostanes – used to measure lipid peroxidation – correlated with apnea/hypoxia index (r = 0.39; P = .03), and the most severe OSA/hypoxia occurred in subjects that had the greatest 4-hydroxynonenal staining (P = .03). Furthermore, an increase in both F2-isoprostanes and 4-hydroxynonenal hepatic staining was shown to lead to a higher risk of worse steatosis: r = 0.32 and r = 0.47, respectively (P = .04 and P = .007).
“These data support sleep disordered breathing as an important trigger of oxidative stress that promotes progression of pediatric NAFLD to NASH,” the authors concluded, adding that “this study confirms that OSA/hypoxia is common in pediatric NAFLD and that more severe OSA/hypoxia is associated with elevated aminotransferases, hepatic steatosis, inflammation, NAS [NAFLD activity score], and fibrosis.”
Dr. Sundaram and her coauthors call for further research to examine if “prevention or reversal of NASH following effective therapy of OSA and nocturnal hypoxia in obese patients” is viable.
This study was supported by funding from the National Institutes of Health. Dr. Sundaram and her coinvestigators did not report any relevant financial disclosures.
FROM THE JOURNAL OF HEPATOLOGY
Key clinical point: Adolescents with obstructive sleep apnea have a higher risk for nonalcoholic fatty liver disease, because of liver tissue scarring.
Major finding: The cohort of subjects with OSA had more severe fibrosis (64%, stages 0-2; 36% stage 3) than those without OSA (100%, stages 0-2) (P = .03).
Data source: Prospective cohort study of 36 adolescents with NAFLD and 14 lean controls.
Disclosures: Funding provided by the NIH. Authors reported no relevant financial disclosures.
CPAP May Be Vasculoprotective in Stroke and TIA
DENVER—Long-term continuous positive airway pressure (CPAP) for treatment of sleep apnea in patients with a recent mild stroke or transient ischemic attack (TIA) resulted in improved cardiovascular and metabolic risk factors, better neurologic function, and a reduction in the recurrent vascular event rate, compared with usual care, in the SLEEP TIGHT study.
“Up to 25% of patients will have a stroke, cardiovascular event, or death within 90 days after a minor stroke or TIA despite current preventive strategies. And, importantly, patients with a TIA or stroke have a high prevalence of obstructive sleep apnea—on the order of 60% to 80%,” explained H. Klar Yaggi, MD, MPH, at the 30th Anniversary Meeting of the Associated Professional Sleep Societies.
H. Klar Yaggi, MD, MPH
SLEEP TIGHT’s findings support the hypothesis that diagnosis and treatment of sleep apnea in patients with a recent minor stroke or TIA will address a major unmet need for better methods of reducing the high vascular risk present in this population, said Dr. Yaggi, Associate Professor of Medicine and Director of the Program in Sleep Medicine at Yale University in New Haven, Connecticut.
A High-Risk Population
SLEEP TIGHT was a National Heart, Lung, and Blood Institute–sponsored phase II, 12-month, multicenter, single-blind, randomized, proof-of-concept study. It included 252 patients, 80% of whom had a recent minor stroke, and the rest had a TIA. Patients had high levels of cardiovascular risk factors; two-thirds had hypertension, half were hyperlipidemic, 40% had diabetes, 15% had a prior myocardial infarction, 10% had atrial fibrillation, and the group’s mean BMI was 30. Polysomnography revealed that 76% of subjects had sleep apnea, as defined by an apnea–hypopnea index of at least five events per hour. In fact, they averaged about 23 events per hour, putting them in the moderate-severity range. As is common among patients with stroke or TIA and sleep apnea, they experienced less daytime sleepiness than is typical in a sleep clinic population, with a mean baseline Epworth Sleepiness Scale score of 7.
Participants were randomized to one of three groups: a usual care control group, a CPAP arm, or an enhanced CPAP arm. The enhanced intervention protocol was designed to boost CPAP adherence; it included targeted education, a customized cognitive intervention, and additional CPAP support beyond the standard CPAP protocols used in sleep medicine clinics. Patients with sleep apnea in the two intervention arms were then placed on CPAP.
At one year of follow-up, the stroke rate was 8.7 per 100 patient-years in the usual care group, compared with 5.5 per 100 person-years in the combined intervention arms. The composite cardiovascular event rate, composed of all-cause mortality, acute myocardial infarction, stroke, hospitalization for unstable angina, or urgent coronary revascularization, was 13.1 per 100 person-years with usual care and 11.0 in the CPAP intervention arms. While these results are encouraging, SLEEP TIGHT wasn’t powered to show significant differences in these events.
Patient Adherence
Outcomes across the board didn’t differ significantly between the CPAP and enhanced CPAP groups. And since the mean number of hours of CPAP use per night was also similar in the two groups—3.9 hours with standard CPAP and 4.3 hours with enhanced CPAP—it’s likely that the phase III trial will rely upon the much simpler standard CPAP intervention, according to Dr. Yaggi.
He deemed CPAP adherence in this stroke or TIA population to be similar to the rates typically seen in routine sleep medicine practice. Roughly 40% of the patients with stroke or TIA were rated as having good adherence, 30% made some use of the therapy, and 30% had no or poor adherence.
Nonetheless, patients in the two intervention arms did significantly better than the usual care group, in terms of one-year changes in insulin resistance and glycosylated hemoglobin. They also had lower 24-hour mean systolic blood pressure and were more likely to convert to a favorable pattern of nocturnal blood pressure dipping. However, no differences between the intervention and usual care groups were seen in levels of high-sensitivity C-reactive protein and interleukin-6, the two markers of systemic inflammation analyzed. Nor did the CPAP intervention provide any benefit in terms of heart rate variability and other measures of autonomic function.
Fifty-eight percent of patients in the intervention arms had a desirable NIH Stroke Scale score of 0 to 1, compared with 38% of the usual care group. In addition, daytime sleepiness, as reflected in Epworth Sleepiness Scale scores, was reduced at last follow-up to a significantly greater extent in the CPAP groups, Dr. Yaggi noted.
Greater CPAP use was associated with a favorable trend for improvement in the modified Rankin score: a 0.3-point reduction with no or poor CPAP use, a 0.4-point reduction with some use, and a 0.9-point reduction with good use.
The encouraging results will be helpful in designing a larger, event-driven, definitive phase III trial, Dr. Yaggi said.
—Bruce Jancin
Suggested Reading
Yaggi HK, Mittleman MA, Bravata DM, et al. Reducing cardiovascular risk through treatment of obstructive sleep apnea: 2 methodological approaches. Am Heart J. 2016;172:135-143.
DENVER—Long-term continuous positive airway pressure (CPAP) for treatment of sleep apnea in patients with a recent mild stroke or transient ischemic attack (TIA) resulted in improved cardiovascular and metabolic risk factors, better neurologic function, and a reduction in the recurrent vascular event rate, compared with usual care, in the SLEEP TIGHT study.
“Up to 25% of patients will have a stroke, cardiovascular event, or death within 90 days after a minor stroke or TIA despite current preventive strategies. And, importantly, patients with a TIA or stroke have a high prevalence of obstructive sleep apnea—on the order of 60% to 80%,” explained H. Klar Yaggi, MD, MPH, at the 30th Anniversary Meeting of the Associated Professional Sleep Societies.
H. Klar Yaggi, MD, MPH
SLEEP TIGHT’s findings support the hypothesis that diagnosis and treatment of sleep apnea in patients with a recent minor stroke or TIA will address a major unmet need for better methods of reducing the high vascular risk present in this population, said Dr. Yaggi, Associate Professor of Medicine and Director of the Program in Sleep Medicine at Yale University in New Haven, Connecticut.
A High-Risk Population
SLEEP TIGHT was a National Heart, Lung, and Blood Institute–sponsored phase II, 12-month, multicenter, single-blind, randomized, proof-of-concept study. It included 252 patients, 80% of whom had a recent minor stroke, and the rest had a TIA. Patients had high levels of cardiovascular risk factors; two-thirds had hypertension, half were hyperlipidemic, 40% had diabetes, 15% had a prior myocardial infarction, 10% had atrial fibrillation, and the group’s mean BMI was 30. Polysomnography revealed that 76% of subjects had sleep apnea, as defined by an apnea–hypopnea index of at least five events per hour. In fact, they averaged about 23 events per hour, putting them in the moderate-severity range. As is common among patients with stroke or TIA and sleep apnea, they experienced less daytime sleepiness than is typical in a sleep clinic population, with a mean baseline Epworth Sleepiness Scale score of 7.
Participants were randomized to one of three groups: a usual care control group, a CPAP arm, or an enhanced CPAP arm. The enhanced intervention protocol was designed to boost CPAP adherence; it included targeted education, a customized cognitive intervention, and additional CPAP support beyond the standard CPAP protocols used in sleep medicine clinics. Patients with sleep apnea in the two intervention arms were then placed on CPAP.
At one year of follow-up, the stroke rate was 8.7 per 100 patient-years in the usual care group, compared with 5.5 per 100 person-years in the combined intervention arms. The composite cardiovascular event rate, composed of all-cause mortality, acute myocardial infarction, stroke, hospitalization for unstable angina, or urgent coronary revascularization, was 13.1 per 100 person-years with usual care and 11.0 in the CPAP intervention arms. While these results are encouraging, SLEEP TIGHT wasn’t powered to show significant differences in these events.
Patient Adherence
Outcomes across the board didn’t differ significantly between the CPAP and enhanced CPAP groups. And since the mean number of hours of CPAP use per night was also similar in the two groups—3.9 hours with standard CPAP and 4.3 hours with enhanced CPAP—it’s likely that the phase III trial will rely upon the much simpler standard CPAP intervention, according to Dr. Yaggi.
He deemed CPAP adherence in this stroke or TIA population to be similar to the rates typically seen in routine sleep medicine practice. Roughly 40% of the patients with stroke or TIA were rated as having good adherence, 30% made some use of the therapy, and 30% had no or poor adherence.
Nonetheless, patients in the two intervention arms did significantly better than the usual care group, in terms of one-year changes in insulin resistance and glycosylated hemoglobin. They also had lower 24-hour mean systolic blood pressure and were more likely to convert to a favorable pattern of nocturnal blood pressure dipping. However, no differences between the intervention and usual care groups were seen in levels of high-sensitivity C-reactive protein and interleukin-6, the two markers of systemic inflammation analyzed. Nor did the CPAP intervention provide any benefit in terms of heart rate variability and other measures of autonomic function.
Fifty-eight percent of patients in the intervention arms had a desirable NIH Stroke Scale score of 0 to 1, compared with 38% of the usual care group. In addition, daytime sleepiness, as reflected in Epworth Sleepiness Scale scores, was reduced at last follow-up to a significantly greater extent in the CPAP groups, Dr. Yaggi noted.
Greater CPAP use was associated with a favorable trend for improvement in the modified Rankin score: a 0.3-point reduction with no or poor CPAP use, a 0.4-point reduction with some use, and a 0.9-point reduction with good use.
The encouraging results will be helpful in designing a larger, event-driven, definitive phase III trial, Dr. Yaggi said.
—Bruce Jancin
DENVER—Long-term continuous positive airway pressure (CPAP) for treatment of sleep apnea in patients with a recent mild stroke or transient ischemic attack (TIA) resulted in improved cardiovascular and metabolic risk factors, better neurologic function, and a reduction in the recurrent vascular event rate, compared with usual care, in the SLEEP TIGHT study.
“Up to 25% of patients will have a stroke, cardiovascular event, or death within 90 days after a minor stroke or TIA despite current preventive strategies. And, importantly, patients with a TIA or stroke have a high prevalence of obstructive sleep apnea—on the order of 60% to 80%,” explained H. Klar Yaggi, MD, MPH, at the 30th Anniversary Meeting of the Associated Professional Sleep Societies.
H. Klar Yaggi, MD, MPH
SLEEP TIGHT’s findings support the hypothesis that diagnosis and treatment of sleep apnea in patients with a recent minor stroke or TIA will address a major unmet need for better methods of reducing the high vascular risk present in this population, said Dr. Yaggi, Associate Professor of Medicine and Director of the Program in Sleep Medicine at Yale University in New Haven, Connecticut.
A High-Risk Population
SLEEP TIGHT was a National Heart, Lung, and Blood Institute–sponsored phase II, 12-month, multicenter, single-blind, randomized, proof-of-concept study. It included 252 patients, 80% of whom had a recent minor stroke, and the rest had a TIA. Patients had high levels of cardiovascular risk factors; two-thirds had hypertension, half were hyperlipidemic, 40% had diabetes, 15% had a prior myocardial infarction, 10% had atrial fibrillation, and the group’s mean BMI was 30. Polysomnography revealed that 76% of subjects had sleep apnea, as defined by an apnea–hypopnea index of at least five events per hour. In fact, they averaged about 23 events per hour, putting them in the moderate-severity range. As is common among patients with stroke or TIA and sleep apnea, they experienced less daytime sleepiness than is typical in a sleep clinic population, with a mean baseline Epworth Sleepiness Scale score of 7.
Participants were randomized to one of three groups: a usual care control group, a CPAP arm, or an enhanced CPAP arm. The enhanced intervention protocol was designed to boost CPAP adherence; it included targeted education, a customized cognitive intervention, and additional CPAP support beyond the standard CPAP protocols used in sleep medicine clinics. Patients with sleep apnea in the two intervention arms were then placed on CPAP.
At one year of follow-up, the stroke rate was 8.7 per 100 patient-years in the usual care group, compared with 5.5 per 100 person-years in the combined intervention arms. The composite cardiovascular event rate, composed of all-cause mortality, acute myocardial infarction, stroke, hospitalization for unstable angina, or urgent coronary revascularization, was 13.1 per 100 person-years with usual care and 11.0 in the CPAP intervention arms. While these results are encouraging, SLEEP TIGHT wasn’t powered to show significant differences in these events.
Patient Adherence
Outcomes across the board didn’t differ significantly between the CPAP and enhanced CPAP groups. And since the mean number of hours of CPAP use per night was also similar in the two groups—3.9 hours with standard CPAP and 4.3 hours with enhanced CPAP—it’s likely that the phase III trial will rely upon the much simpler standard CPAP intervention, according to Dr. Yaggi.
He deemed CPAP adherence in this stroke or TIA population to be similar to the rates typically seen in routine sleep medicine practice. Roughly 40% of the patients with stroke or TIA were rated as having good adherence, 30% made some use of the therapy, and 30% had no or poor adherence.
Nonetheless, patients in the two intervention arms did significantly better than the usual care group, in terms of one-year changes in insulin resistance and glycosylated hemoglobin. They also had lower 24-hour mean systolic blood pressure and were more likely to convert to a favorable pattern of nocturnal blood pressure dipping. However, no differences between the intervention and usual care groups were seen in levels of high-sensitivity C-reactive protein and interleukin-6, the two markers of systemic inflammation analyzed. Nor did the CPAP intervention provide any benefit in terms of heart rate variability and other measures of autonomic function.
Fifty-eight percent of patients in the intervention arms had a desirable NIH Stroke Scale score of 0 to 1, compared with 38% of the usual care group. In addition, daytime sleepiness, as reflected in Epworth Sleepiness Scale scores, was reduced at last follow-up to a significantly greater extent in the CPAP groups, Dr. Yaggi noted.
Greater CPAP use was associated with a favorable trend for improvement in the modified Rankin score: a 0.3-point reduction with no or poor CPAP use, a 0.4-point reduction with some use, and a 0.9-point reduction with good use.
The encouraging results will be helpful in designing a larger, event-driven, definitive phase III trial, Dr. Yaggi said.
—Bruce Jancin
Suggested Reading
Yaggi HK, Mittleman MA, Bravata DM, et al. Reducing cardiovascular risk through treatment of obstructive sleep apnea: 2 methodological approaches. Am Heart J. 2016;172:135-143.
Suggested Reading
Yaggi HK, Mittleman MA, Bravata DM, et al. Reducing cardiovascular risk through treatment of obstructive sleep apnea: 2 methodological approaches. Am Heart J. 2016;172:135-143.
Sleep Apnea in Later Life More Than Doubles Subsequent Alzheimer’s Disease Risk
DENVER—Obstructive sleep apnea (OSA) diagnosed later in life is associated with an increased likelihood of subsequent Alzheimer’s disease, Omonigho Bubu, MD, MPH, said at the 2016 Annual Meeting of the Associated Professional Sleep Societies.
He presented a retrospective cohort study in which a dose-response relationship was apparent. The more severe an individual’s OSA, as reflected in a higher apnea–hypopnea index on polysomnography, the greater the risk of later being diagnosed with Alzheimer’s disease, compared with matched controls during up to 13 years of follow-up.
Researchers identified several possible contributing factors for the observed relationship between OSA and Alzheimer’s disease. Patients with OSA and more severe sleep fragmentation, nocturnal hypoxia, and abnormal sleep duration were significantly more likely to subsequently develop Alzheimer’s disease than were patients with OSA and less severely disrupted sleep measures, added Dr. Bubu, a PhD candidate at the University of South Florida in Tampa.
The study included 756 patients age 65 and older with no history of cognitive decline when diagnosed with OSA by polysomnography at Tampa General Hospital during 2001–2005. They were matched by age, race, sex, BMI, and zip code to two control groups totaling 3,780 subjects. The controls, drawn from outpatient medical clinics at the hospital, had various medical problems, but no sleep disorders or cognitive impairment.
During a mean 10.5-year follow-up period, 513 subjects were diagnosed with Alzheimer’s disease, according to Medicare data. In a Cox proportional hazards analysis adjusted for age, sex, race, BMI, and education level, OSA was independently associated with a 2.2-fold increased risk of Alzheimer’s disease. Further adjustment for alcohol intake, smoking, use of sleep medications, and chronic medical conditions didn’t substantially change the results.
However, the investigators were not able to control for APOE ε4 allele status, which is a known risk factor for OSA and Alzheimer’s disease, so it remains unclear whether the association is “all related to APOE,” said Richard J. Caselli, MD, Professor of Neurology at the Mayo Clinic in Scottsdale, Arizona.
Time to onset of Alzheimer’s disease was shorter in patients with OSA. The mean time to diagnosis was 60.8 months after diagnosis of OSA, compared with 73 and 78 months in members of the two control groups who developed the dementia.
When the risk of developing Alzheimer’s disease was stratified according to baseline OSA severity, a dose-response effect was seen. Mild OSA, defined as 5–14 apnea–hypopnea events per hour of sleep, was associated with a 1.67-fold greater risk than in controls. The moderate OSA group, which had 15–29 events per hour, had a 1.81-fold increased risk. Patients with severe OSA, with 30 or more events per hour, had a 2.63-fold increased risk.
Gender, race, and education modified the relationship between OSA and Alzheimer’s disease, Dr. Bubu said. Women with OSA had a 2.28-fold greater risk of later developing the disease, compared with controls; men had a 1.42-fold increased risk. African-Americans with OSA were at 2.56-fold greater risk than were controls, while Hispanics with OSA were at 1.8-fold increased risk, and non-Hispanic whites were at 1.87-fold increased risk. Patients with OSA and a high school education or less were at 2.73 times greater risk of Alzheimer’s disease than were controls; those with at least some college or technical school were at 1.82-fold risk, and patients with OSA who had attended graduate school had a 1.31-fold increased risk.
“Our results definitely show that OSA precedes the onset of Alzheimer’s disease. But we cannot say that’s causation. That will be left to future research examining the potential mechanisms we’ve identified,” Dr. Bubu said.
A key missing link in establishing a causal relationship is the lack of data on how many of the older patients diagnosed with OSA accepted treatment for the condition, and what their response rates were. In other words, it remains to be seen whether OSA occurring later in life is a modifiable risk factor for Alzheimer’s disease, as opposed to an early expression of the dementing disease process, whereby treatment of the sleep disorder doesn’t affect the progressive cognitive decline.
Short sleep duration of less than six hours as well as a mean total sleep time greater than nine hours in patients with OSA were associated with significantly increased risk of Alzheimer’s disease, compared with a sleep time of six to nine hours. Patients with high sleep-onset latency in the sleep lab, a high REM latency from sleep onset, a low percentage of time spent in REM, an oxygen saturation level of less than 90% for at least 1% of sleep time, or a high number of arousals per hour of sleep were also at increased risk of subsequent Alzheimer’s disease.
The study was supported by the Byrd Alzheimer’s Institute. Dr. Bubu reported having no financial conflicts.
—Bruce Jancin
Suggested Reading
Kheirandish-Gozal L, Philby ME, Alonso-Álvarez ML, et al. Biomarkers of Alzheimer disease in children with obstructive sleep apnea: effect of adenotonsillectomty. Sleep. 2016;39(6):1225-1232.
DENVER—Obstructive sleep apnea (OSA) diagnosed later in life is associated with an increased likelihood of subsequent Alzheimer’s disease, Omonigho Bubu, MD, MPH, said at the 2016 Annual Meeting of the Associated Professional Sleep Societies.
He presented a retrospective cohort study in which a dose-response relationship was apparent. The more severe an individual’s OSA, as reflected in a higher apnea–hypopnea index on polysomnography, the greater the risk of later being diagnosed with Alzheimer’s disease, compared with matched controls during up to 13 years of follow-up.
Researchers identified several possible contributing factors for the observed relationship between OSA and Alzheimer’s disease. Patients with OSA and more severe sleep fragmentation, nocturnal hypoxia, and abnormal sleep duration were significantly more likely to subsequently develop Alzheimer’s disease than were patients with OSA and less severely disrupted sleep measures, added Dr. Bubu, a PhD candidate at the University of South Florida in Tampa.
The study included 756 patients age 65 and older with no history of cognitive decline when diagnosed with OSA by polysomnography at Tampa General Hospital during 2001–2005. They were matched by age, race, sex, BMI, and zip code to two control groups totaling 3,780 subjects. The controls, drawn from outpatient medical clinics at the hospital, had various medical problems, but no sleep disorders or cognitive impairment.
During a mean 10.5-year follow-up period, 513 subjects were diagnosed with Alzheimer’s disease, according to Medicare data. In a Cox proportional hazards analysis adjusted for age, sex, race, BMI, and education level, OSA was independently associated with a 2.2-fold increased risk of Alzheimer’s disease. Further adjustment for alcohol intake, smoking, use of sleep medications, and chronic medical conditions didn’t substantially change the results.
However, the investigators were not able to control for APOE ε4 allele status, which is a known risk factor for OSA and Alzheimer’s disease, so it remains unclear whether the association is “all related to APOE,” said Richard J. Caselli, MD, Professor of Neurology at the Mayo Clinic in Scottsdale, Arizona.
Time to onset of Alzheimer’s disease was shorter in patients with OSA. The mean time to diagnosis was 60.8 months after diagnosis of OSA, compared with 73 and 78 months in members of the two control groups who developed the dementia.
When the risk of developing Alzheimer’s disease was stratified according to baseline OSA severity, a dose-response effect was seen. Mild OSA, defined as 5–14 apnea–hypopnea events per hour of sleep, was associated with a 1.67-fold greater risk than in controls. The moderate OSA group, which had 15–29 events per hour, had a 1.81-fold increased risk. Patients with severe OSA, with 30 or more events per hour, had a 2.63-fold increased risk.
Gender, race, and education modified the relationship between OSA and Alzheimer’s disease, Dr. Bubu said. Women with OSA had a 2.28-fold greater risk of later developing the disease, compared with controls; men had a 1.42-fold increased risk. African-Americans with OSA were at 2.56-fold greater risk than were controls, while Hispanics with OSA were at 1.8-fold increased risk, and non-Hispanic whites were at 1.87-fold increased risk. Patients with OSA and a high school education or less were at 2.73 times greater risk of Alzheimer’s disease than were controls; those with at least some college or technical school were at 1.82-fold risk, and patients with OSA who had attended graduate school had a 1.31-fold increased risk.
“Our results definitely show that OSA precedes the onset of Alzheimer’s disease. But we cannot say that’s causation. That will be left to future research examining the potential mechanisms we’ve identified,” Dr. Bubu said.
A key missing link in establishing a causal relationship is the lack of data on how many of the older patients diagnosed with OSA accepted treatment for the condition, and what their response rates were. In other words, it remains to be seen whether OSA occurring later in life is a modifiable risk factor for Alzheimer’s disease, as opposed to an early expression of the dementing disease process, whereby treatment of the sleep disorder doesn’t affect the progressive cognitive decline.
Short sleep duration of less than six hours as well as a mean total sleep time greater than nine hours in patients with OSA were associated with significantly increased risk of Alzheimer’s disease, compared with a sleep time of six to nine hours. Patients with high sleep-onset latency in the sleep lab, a high REM latency from sleep onset, a low percentage of time spent in REM, an oxygen saturation level of less than 90% for at least 1% of sleep time, or a high number of arousals per hour of sleep were also at increased risk of subsequent Alzheimer’s disease.
The study was supported by the Byrd Alzheimer’s Institute. Dr. Bubu reported having no financial conflicts.
—Bruce Jancin
DENVER—Obstructive sleep apnea (OSA) diagnosed later in life is associated with an increased likelihood of subsequent Alzheimer’s disease, Omonigho Bubu, MD, MPH, said at the 2016 Annual Meeting of the Associated Professional Sleep Societies.
He presented a retrospective cohort study in which a dose-response relationship was apparent. The more severe an individual’s OSA, as reflected in a higher apnea–hypopnea index on polysomnography, the greater the risk of later being diagnosed with Alzheimer’s disease, compared with matched controls during up to 13 years of follow-up.
Researchers identified several possible contributing factors for the observed relationship between OSA and Alzheimer’s disease. Patients with OSA and more severe sleep fragmentation, nocturnal hypoxia, and abnormal sleep duration were significantly more likely to subsequently develop Alzheimer’s disease than were patients with OSA and less severely disrupted sleep measures, added Dr. Bubu, a PhD candidate at the University of South Florida in Tampa.
The study included 756 patients age 65 and older with no history of cognitive decline when diagnosed with OSA by polysomnography at Tampa General Hospital during 2001–2005. They were matched by age, race, sex, BMI, and zip code to two control groups totaling 3,780 subjects. The controls, drawn from outpatient medical clinics at the hospital, had various medical problems, but no sleep disorders or cognitive impairment.
During a mean 10.5-year follow-up period, 513 subjects were diagnosed with Alzheimer’s disease, according to Medicare data. In a Cox proportional hazards analysis adjusted for age, sex, race, BMI, and education level, OSA was independently associated with a 2.2-fold increased risk of Alzheimer’s disease. Further adjustment for alcohol intake, smoking, use of sleep medications, and chronic medical conditions didn’t substantially change the results.
However, the investigators were not able to control for APOE ε4 allele status, which is a known risk factor for OSA and Alzheimer’s disease, so it remains unclear whether the association is “all related to APOE,” said Richard J. Caselli, MD, Professor of Neurology at the Mayo Clinic in Scottsdale, Arizona.
Time to onset of Alzheimer’s disease was shorter in patients with OSA. The mean time to diagnosis was 60.8 months after diagnosis of OSA, compared with 73 and 78 months in members of the two control groups who developed the dementia.
When the risk of developing Alzheimer’s disease was stratified according to baseline OSA severity, a dose-response effect was seen. Mild OSA, defined as 5–14 apnea–hypopnea events per hour of sleep, was associated with a 1.67-fold greater risk than in controls. The moderate OSA group, which had 15–29 events per hour, had a 1.81-fold increased risk. Patients with severe OSA, with 30 or more events per hour, had a 2.63-fold increased risk.
Gender, race, and education modified the relationship between OSA and Alzheimer’s disease, Dr. Bubu said. Women with OSA had a 2.28-fold greater risk of later developing the disease, compared with controls; men had a 1.42-fold increased risk. African-Americans with OSA were at 2.56-fold greater risk than were controls, while Hispanics with OSA were at 1.8-fold increased risk, and non-Hispanic whites were at 1.87-fold increased risk. Patients with OSA and a high school education or less were at 2.73 times greater risk of Alzheimer’s disease than were controls; those with at least some college or technical school were at 1.82-fold risk, and patients with OSA who had attended graduate school had a 1.31-fold increased risk.
“Our results definitely show that OSA precedes the onset of Alzheimer’s disease. But we cannot say that’s causation. That will be left to future research examining the potential mechanisms we’ve identified,” Dr. Bubu said.
A key missing link in establishing a causal relationship is the lack of data on how many of the older patients diagnosed with OSA accepted treatment for the condition, and what their response rates were. In other words, it remains to be seen whether OSA occurring later in life is a modifiable risk factor for Alzheimer’s disease, as opposed to an early expression of the dementing disease process, whereby treatment of the sleep disorder doesn’t affect the progressive cognitive decline.
Short sleep duration of less than six hours as well as a mean total sleep time greater than nine hours in patients with OSA were associated with significantly increased risk of Alzheimer’s disease, compared with a sleep time of six to nine hours. Patients with high sleep-onset latency in the sleep lab, a high REM latency from sleep onset, a low percentage of time spent in REM, an oxygen saturation level of less than 90% for at least 1% of sleep time, or a high number of arousals per hour of sleep were also at increased risk of subsequent Alzheimer’s disease.
The study was supported by the Byrd Alzheimer’s Institute. Dr. Bubu reported having no financial conflicts.
—Bruce Jancin
Suggested Reading
Kheirandish-Gozal L, Philby ME, Alonso-Álvarez ML, et al. Biomarkers of Alzheimer disease in children with obstructive sleep apnea: effect of adenotonsillectomty. Sleep. 2016;39(6):1225-1232.
Suggested Reading
Kheirandish-Gozal L, Philby ME, Alonso-Álvarez ML, et al. Biomarkers of Alzheimer disease in children with obstructive sleep apnea: effect of adenotonsillectomty. Sleep. 2016;39(6):1225-1232.
Disordered sleep: Ask the right questions to reveal this hidden confounder
It seems like common sense: Sleeping poorly results in not feeling good. The truth is that many of our patients are sleep deprived but are either unaware of, or unwilling to acknowledge, their problem. The busy life that many patients have does not allow adequate time for sleep. In fact, I have encountered patients who think of sleep as an inconvenience that takes away time from other pursuits.
Sleep deprivation in psychiatric disorders
Sleep deprivation occurs when the duration or quality of sleep is inadequate. Inadequate sleep duration can be caused by insomnia or simply not allowing enough time for sleep (1 aspect of poor sleep hygiene). Poor sleep quality often is caused by sleep-disordered breathing.
Sleep deprivation can result in either sleepiness or fatigue. Sleepiness is a propensity to fall asleep; fatigue is a lack of energy that is not alleviated by additional sleep. Fatigue is more likely to be associated with a psychiatric disorder; sleepiness is more predominant in sleep disorders (although there is significant overlap). For example, patients with a major depressive disorder can experience fatigue as much as patients with sleep deprivation, but the latter also is more likely to result in sleepiness. Trouble concentrating is seen in anxiety, depression, attention-deficit/hyperactivity disorder (ADHD), and sleep deprivation.1
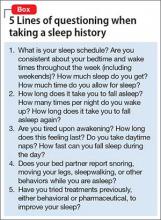
Insomnia or poor sleep hygiene can be diagnosed with a thorough sleep history. I take special care to consider sleep problems by presenting 5 groups of questions to the patient (Box).
Sleep-disordered breathing
A sleep study is required to accurately diagnose sleep-disordered breathing. Unless this diagnosis is specifically looked for, it remains hidden from both physicians and patients. Clues to the presence of sleep-disordered breathing include snorting, snoring, and gasping for air during sleep; witnessed apnea during sleep; nighttime awakening; daytime fatigue; nocturia; mouth breathing or dry mouth; acid reflux; irritability; morning headache; nighttime sweating; and low libido. Risk factors for sleep-disordered breathing include obesity; smoking; menopause; family history; increasing age; and anatomical factors (eg, deviation of the nasal septum; retrognathia; long face syndrome; high-arched narrow hard palate; large tonsils, uvula, or tongue).2
Measuring sleep quality
Some patients are unaware of the extent to which they are sleepy. The most widely used scale to measure sleepiness is the Epworth Sleepiness Scale.3 Sleep specialists view a score of ≥10 on the Epworth scale as indicative of daytime sleepiness. In addition, a patient’s daily consumption of caffeinated beverages can be a clue to excessive sleepiness or, at least, fatigue. If the degree of sleepiness cannot be determined subjectively, objective measures, such as the Multiple Sleep Latency Test (MSLT), can quantify it. In a randomly selected sample from the general population, 13.4% had excessive daytime sleepiness as measured by the MSLT.4
Adult ADHD and sleep deprivation
In my practice, sleep problems confound both the diagnosis and treatment of psychiatric disorders, especially ADHD. Often, patients who report ADHD symptoms have no clear history of ADHD during childhood. In these cases, I always consider the possibility that their ADHD symptoms are due to sleep deprivation. Sleep deprivation can mimic the poor executive function and difficulty concentrating that is often seen in ADHD, because such deprivation is associated with decreased activity in the prefrontal cortex during wakefulness.5
In patients who provide a clear history of ADHD symptoms during childhood, it is possible that inadequate sleep exacerbates ADHD symptoms as adults. Unless sleep deprivation is diagnosed and treated in these patients, they can end up taking a higher-than-necessary dosage of a stimulant. Also, patients who have ADHD might have a difficult time managing their sleep schedule because of poor executive functioning. This, in turn, can result in additional sleep deprivation, thus worsening their ADHD symptoms, creating a vicious circle.
Psychotropics and sedation
Many psychiatric medications list sedation as a side effect. Patients with untreated sleep problems might be more likely to notice this side effect because sleep problems contribute to their fatigue. I have had patients who were unable to tolerate sedative medications until their sleep apnea was treated.
In conclusion
It is important to consider sleep deprivation in your differential diagnosis of psychiatric patients. This will allow for more accurate diagnosis and treatment and, in some cases, can avoid treatment resistance.
1. Stahl SM. Excessive sleepiness. San Diego, CA: NEI Press; 2005.
2. Jordan AS, McSharry DG, Malhotra A. Adult obstructive sleep apnoea. Lancet. 2014;383(9918):736-747.
3. Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540-545.
4. Drake CL, Roehrs TA, Richardson GS, et al. Epidemiology and morbidity of excessive daytime sleepiness. Sleep. 2002;25:A91-A92.
5. Thomas M, Sing H, Belenky G, et al. Neural basis of alertness and cognitive performance impairments during sleepiness. I. Effects of 24 h of sleep deprivation on waking human regional brain activity. J Sleep Res. 2000;9(4):335-352.
It seems like common sense: Sleeping poorly results in not feeling good. The truth is that many of our patients are sleep deprived but are either unaware of, or unwilling to acknowledge, their problem. The busy life that many patients have does not allow adequate time for sleep. In fact, I have encountered patients who think of sleep as an inconvenience that takes away time from other pursuits.
Sleep deprivation in psychiatric disorders
Sleep deprivation occurs when the duration or quality of sleep is inadequate. Inadequate sleep duration can be caused by insomnia or simply not allowing enough time for sleep (1 aspect of poor sleep hygiene). Poor sleep quality often is caused by sleep-disordered breathing.
Sleep deprivation can result in either sleepiness or fatigue. Sleepiness is a propensity to fall asleep; fatigue is a lack of energy that is not alleviated by additional sleep. Fatigue is more likely to be associated with a psychiatric disorder; sleepiness is more predominant in sleep disorders (although there is significant overlap). For example, patients with a major depressive disorder can experience fatigue as much as patients with sleep deprivation, but the latter also is more likely to result in sleepiness. Trouble concentrating is seen in anxiety, depression, attention-deficit/hyperactivity disorder (ADHD), and sleep deprivation.1
Insomnia or poor sleep hygiene can be diagnosed with a thorough sleep history. I take special care to consider sleep problems by presenting 5 groups of questions to the patient (Box).
Sleep-disordered breathing
A sleep study is required to accurately diagnose sleep-disordered breathing. Unless this diagnosis is specifically looked for, it remains hidden from both physicians and patients. Clues to the presence of sleep-disordered breathing include snorting, snoring, and gasping for air during sleep; witnessed apnea during sleep; nighttime awakening; daytime fatigue; nocturia; mouth breathing or dry mouth; acid reflux; irritability; morning headache; nighttime sweating; and low libido. Risk factors for sleep-disordered breathing include obesity; smoking; menopause; family history; increasing age; and anatomical factors (eg, deviation of the nasal septum; retrognathia; long face syndrome; high-arched narrow hard palate; large tonsils, uvula, or tongue).2
Measuring sleep quality
Some patients are unaware of the extent to which they are sleepy. The most widely used scale to measure sleepiness is the Epworth Sleepiness Scale.3 Sleep specialists view a score of ≥10 on the Epworth scale as indicative of daytime sleepiness. In addition, a patient’s daily consumption of caffeinated beverages can be a clue to excessive sleepiness or, at least, fatigue. If the degree of sleepiness cannot be determined subjectively, objective measures, such as the Multiple Sleep Latency Test (MSLT), can quantify it. In a randomly selected sample from the general population, 13.4% had excessive daytime sleepiness as measured by the MSLT.4
Adult ADHD and sleep deprivation
In my practice, sleep problems confound both the diagnosis and treatment of psychiatric disorders, especially ADHD. Often, patients who report ADHD symptoms have no clear history of ADHD during childhood. In these cases, I always consider the possibility that their ADHD symptoms are due to sleep deprivation. Sleep deprivation can mimic the poor executive function and difficulty concentrating that is often seen in ADHD, because such deprivation is associated with decreased activity in the prefrontal cortex during wakefulness.5
In patients who provide a clear history of ADHD symptoms during childhood, it is possible that inadequate sleep exacerbates ADHD symptoms as adults. Unless sleep deprivation is diagnosed and treated in these patients, they can end up taking a higher-than-necessary dosage of a stimulant. Also, patients who have ADHD might have a difficult time managing their sleep schedule because of poor executive functioning. This, in turn, can result in additional sleep deprivation, thus worsening their ADHD symptoms, creating a vicious circle.
Psychotropics and sedation
Many psychiatric medications list sedation as a side effect. Patients with untreated sleep problems might be more likely to notice this side effect because sleep problems contribute to their fatigue. I have had patients who were unable to tolerate sedative medications until their sleep apnea was treated.
In conclusion
It is important to consider sleep deprivation in your differential diagnosis of psychiatric patients. This will allow for more accurate diagnosis and treatment and, in some cases, can avoid treatment resistance.
It seems like common sense: Sleeping poorly results in not feeling good. The truth is that many of our patients are sleep deprived but are either unaware of, or unwilling to acknowledge, their problem. The busy life that many patients have does not allow adequate time for sleep. In fact, I have encountered patients who think of sleep as an inconvenience that takes away time from other pursuits.
Sleep deprivation in psychiatric disorders
Sleep deprivation occurs when the duration or quality of sleep is inadequate. Inadequate sleep duration can be caused by insomnia or simply not allowing enough time for sleep (1 aspect of poor sleep hygiene). Poor sleep quality often is caused by sleep-disordered breathing.
Sleep deprivation can result in either sleepiness or fatigue. Sleepiness is a propensity to fall asleep; fatigue is a lack of energy that is not alleviated by additional sleep. Fatigue is more likely to be associated with a psychiatric disorder; sleepiness is more predominant in sleep disorders (although there is significant overlap). For example, patients with a major depressive disorder can experience fatigue as much as patients with sleep deprivation, but the latter also is more likely to result in sleepiness. Trouble concentrating is seen in anxiety, depression, attention-deficit/hyperactivity disorder (ADHD), and sleep deprivation.1
Insomnia or poor sleep hygiene can be diagnosed with a thorough sleep history. I take special care to consider sleep problems by presenting 5 groups of questions to the patient (Box).
Sleep-disordered breathing
A sleep study is required to accurately diagnose sleep-disordered breathing. Unless this diagnosis is specifically looked for, it remains hidden from both physicians and patients. Clues to the presence of sleep-disordered breathing include snorting, snoring, and gasping for air during sleep; witnessed apnea during sleep; nighttime awakening; daytime fatigue; nocturia; mouth breathing or dry mouth; acid reflux; irritability; morning headache; nighttime sweating; and low libido. Risk factors for sleep-disordered breathing include obesity; smoking; menopause; family history; increasing age; and anatomical factors (eg, deviation of the nasal septum; retrognathia; long face syndrome; high-arched narrow hard palate; large tonsils, uvula, or tongue).2
Measuring sleep quality
Some patients are unaware of the extent to which they are sleepy. The most widely used scale to measure sleepiness is the Epworth Sleepiness Scale.3 Sleep specialists view a score of ≥10 on the Epworth scale as indicative of daytime sleepiness. In addition, a patient’s daily consumption of caffeinated beverages can be a clue to excessive sleepiness or, at least, fatigue. If the degree of sleepiness cannot be determined subjectively, objective measures, such as the Multiple Sleep Latency Test (MSLT), can quantify it. In a randomly selected sample from the general population, 13.4% had excessive daytime sleepiness as measured by the MSLT.4
Adult ADHD and sleep deprivation
In my practice, sleep problems confound both the diagnosis and treatment of psychiatric disorders, especially ADHD. Often, patients who report ADHD symptoms have no clear history of ADHD during childhood. In these cases, I always consider the possibility that their ADHD symptoms are due to sleep deprivation. Sleep deprivation can mimic the poor executive function and difficulty concentrating that is often seen in ADHD, because such deprivation is associated with decreased activity in the prefrontal cortex during wakefulness.5
In patients who provide a clear history of ADHD symptoms during childhood, it is possible that inadequate sleep exacerbates ADHD symptoms as adults. Unless sleep deprivation is diagnosed and treated in these patients, they can end up taking a higher-than-necessary dosage of a stimulant. Also, patients who have ADHD might have a difficult time managing their sleep schedule because of poor executive functioning. This, in turn, can result in additional sleep deprivation, thus worsening their ADHD symptoms, creating a vicious circle.
Psychotropics and sedation
Many psychiatric medications list sedation as a side effect. Patients with untreated sleep problems might be more likely to notice this side effect because sleep problems contribute to their fatigue. I have had patients who were unable to tolerate sedative medications until their sleep apnea was treated.
In conclusion
It is important to consider sleep deprivation in your differential diagnosis of psychiatric patients. This will allow for more accurate diagnosis and treatment and, in some cases, can avoid treatment resistance.
1. Stahl SM. Excessive sleepiness. San Diego, CA: NEI Press; 2005.
2. Jordan AS, McSharry DG, Malhotra A. Adult obstructive sleep apnoea. Lancet. 2014;383(9918):736-747.
3. Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540-545.
4. Drake CL, Roehrs TA, Richardson GS, et al. Epidemiology and morbidity of excessive daytime sleepiness. Sleep. 2002;25:A91-A92.
5. Thomas M, Sing H, Belenky G, et al. Neural basis of alertness and cognitive performance impairments during sleepiness. I. Effects of 24 h of sleep deprivation on waking human regional brain activity. J Sleep Res. 2000;9(4):335-352.
1. Stahl SM. Excessive sleepiness. San Diego, CA: NEI Press; 2005.
2. Jordan AS, McSharry DG, Malhotra A. Adult obstructive sleep apnoea. Lancet. 2014;383(9918):736-747.
3. Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540-545.
4. Drake CL, Roehrs TA, Richardson GS, et al. Epidemiology and morbidity of excessive daytime sleepiness. Sleep. 2002;25:A91-A92.
5. Thomas M, Sing H, Belenky G, et al. Neural basis of alertness and cognitive performance impairments during sleepiness. I. Effects of 24 h of sleep deprivation on waking human regional brain activity. J Sleep Res. 2000;9(4):335-352.
GERD and sleep disorders often go hand in glove
Gastroesophageal reflux disease (GERD) is fertile soil for medical and psychiatric comorbid conditions, with sleep disorders leading the way, according to Maurice M. Ohayon, MD, who presented the findings of a longitudinal, population-based study on GERD and its "fellow travelers" at the annual meeting of the Associated Professional Sleep Societies. Insomnia, obstructive sleep apnea, and restless legs syndrome were among the most prevalent comorbidities of GERD. However, one sleep disorder symptom was reported to be a problem in up to 46% of those with the digestive disease. To learn more, see Family Practice News at: http://www.familypracticenews.com/specialty-focus/pulmonary-sleep-medicine/single-article-page/gerd-and-sleep-disorders-often-go-hand-in-glove/1dc81a99b64d296e03b86aa28893fbc7.html.
Gastroesophageal reflux disease (GERD) is fertile soil for medical and psychiatric comorbid conditions, with sleep disorders leading the way, according to Maurice M. Ohayon, MD, who presented the findings of a longitudinal, population-based study on GERD and its "fellow travelers" at the annual meeting of the Associated Professional Sleep Societies. Insomnia, obstructive sleep apnea, and restless legs syndrome were among the most prevalent comorbidities of GERD. However, one sleep disorder symptom was reported to be a problem in up to 46% of those with the digestive disease. To learn more, see Family Practice News at: http://www.familypracticenews.com/specialty-focus/pulmonary-sleep-medicine/single-article-page/gerd-and-sleep-disorders-often-go-hand-in-glove/1dc81a99b64d296e03b86aa28893fbc7.html.
Gastroesophageal reflux disease (GERD) is fertile soil for medical and psychiatric comorbid conditions, with sleep disorders leading the way, according to Maurice M. Ohayon, MD, who presented the findings of a longitudinal, population-based study on GERD and its "fellow travelers" at the annual meeting of the Associated Professional Sleep Societies. Insomnia, obstructive sleep apnea, and restless legs syndrome were among the most prevalent comorbidities of GERD. However, one sleep disorder symptom was reported to be a problem in up to 46% of those with the digestive disease. To learn more, see Family Practice News at: http://www.familypracticenews.com/specialty-focus/pulmonary-sleep-medicine/single-article-page/gerd-and-sleep-disorders-often-go-hand-in-glove/1dc81a99b64d296e03b86aa28893fbc7.html.
Flumazenil effective in refractory hypersomnolence
DENVER – Transdermal or sublingual flumazenil is well worth considering for treatment of carefully selected patients with hypersomnolence refractory to conventional wake-promoting medications, Lynn Marie Trotti, MD, said at the annual meeting of the Associated Professional Sleep Societies.
Her retrospective chart review of 153 consecutive patients treated with flumazenil (Romazicon) showed that 63% derived symptomatic benefit, and 39% of patients remained on the drug at the end of the review period, which averaged 6.8 months, reported Dr. Trotti, a neurologist and sleep scientist at Emory University in Atlanta.
Make no mistake: This is off-label therapy. Flumazenil’s approved indication is as intravenous therapy for benzodiazepine sedation. Given orally, the drug is almost entirely eliminated on first-pass metabolism, so she and her coinvestigators had flumazenil compounded at a pharmacy in two formulations: a 6-mg sublingual lozenge and a transcutaneous lotion in a dispenser providing 3 mg of flumazenil per click of the device.
This novel therapy is supported by a plausible mechanistic rationale. Dr. Trotti and colleagues have previously shown that most patients with central hypersomnolence have abnormal potentiation of GABA-A receptors in their cerebrospinal fluid (CSF).
“Functionally speaking, it’s as though they’re producing an endogenous benzodiazepinelike substance,” she explained.
The investigators showed further that the macrolide antibiotic clarithromycin, a negative allosteric modulator of GABA-A receptors, reduced sleepiness in patients with central hypersomnolence syndromes in a randomized, double-blind, crossover trial (Ann Neurol. 2015 Sep;78[3]:454-65).
“It’s not great to use an antibiotic to treat people who don’t have a bacterial infection, so it would be really lovely if we had a GABA antagonist or negative allosteric modulator of GABA-A receptors that was not clarithromycin. And that’s where flumazenil comes into the picture,” according to Dr. Trotti.
As a requirement for receiving flumazenil at the Emory sleep disorders center, patients had to have been refractory to all conventional therapies. Indeed, they had been refractory to an average of 4.6 medications for excessive sleepiness. Also, their hypersomnolence had to have a serious impact on their daily life, for example a job at risk because of inability to drive to and from work safely. Initially, it was further required as a condition for treatment that patients had to show abnormal CSF potentiation of GABA-A receptors; however, the investigators quit requiring a CSF sample after roughly the first 100 candidates proved positive.
Dosing of the sublingual flumazenil lozenges began at one 6-mg lozenge four times daily, titrating up by adding an extra lozenge every 4-5 days until reaching a maximum of 12 per day. The lotion is rubbed on the inside of the forearm at a dose of 3 mg on each arm up to four times per day.
Among the 40 treatment responders who completed the Epworth Sleepiness Scale at baseline and after an average of 6.8 months on flumazenil, the average score improved from 15 to 10.3.
Fifty-seven patients obtained no benefit from flumazenil, 10 stopped the drug because of side effects, 3 quit because they preferred clarithromycin, 8 stopped owing to the cost, and the rest dropped the drug for an assortment of reasons, including planned pregnancy.
The most common treatment-emergent adverse events included dizziness in 13% of subjects, anxiety in 7%, and other mood disturbances in 6%.
Two serious adverse events occurred. One patient with a history of atrial fibrillation experienced a transient ischemic attack. And a patient with systemic lupus erythematous developed asymptomatic CNS lupus vasculopathy. It’s not possible to say whether these events were treatment related because the experience with chronic flumazenil therapy is so limited. After all, the drug is given for its approved indication for no longer than a few days, Dr. Trotti observed.
“This is all clinical data. Obviously I’m not suggesting that everybody should start prescribing flumazenil. That being said, we really need better treatment options,” she said.
The long-term treatment continuation rate with modafinil for hypersomnolence is about 50%, anywhere from 29% to 66% for amphetamines, 38% for clarithromycin, and 37% for pitolisant.
“If you look globally at how likely people with idiopathic hypersomnolence or narcolepsy are to get a satisfactory response to conventional therapies, probably 15%-20% do not get satisfactorily treated with what we currently have available. Prospective controlled studies of flumazenil for treatment of hypersomnolence are certainly needed, but in the absence of those data there’s at least a rationale for people who are severely affected and have nowhere else to turn to consider flumazenil,” Dr. Trotti concluded.
She reported having no financial conflicts regarding her study, supported by the National Institutes of Health.
DENVER – Transdermal or sublingual flumazenil is well worth considering for treatment of carefully selected patients with hypersomnolence refractory to conventional wake-promoting medications, Lynn Marie Trotti, MD, said at the annual meeting of the Associated Professional Sleep Societies.
Her retrospective chart review of 153 consecutive patients treated with flumazenil (Romazicon) showed that 63% derived symptomatic benefit, and 39% of patients remained on the drug at the end of the review period, which averaged 6.8 months, reported Dr. Trotti, a neurologist and sleep scientist at Emory University in Atlanta.
Make no mistake: This is off-label therapy. Flumazenil’s approved indication is as intravenous therapy for benzodiazepine sedation. Given orally, the drug is almost entirely eliminated on first-pass metabolism, so she and her coinvestigators had flumazenil compounded at a pharmacy in two formulations: a 6-mg sublingual lozenge and a transcutaneous lotion in a dispenser providing 3 mg of flumazenil per click of the device.
This novel therapy is supported by a plausible mechanistic rationale. Dr. Trotti and colleagues have previously shown that most patients with central hypersomnolence have abnormal potentiation of GABA-A receptors in their cerebrospinal fluid (CSF).
“Functionally speaking, it’s as though they’re producing an endogenous benzodiazepinelike substance,” she explained.
The investigators showed further that the macrolide antibiotic clarithromycin, a negative allosteric modulator of GABA-A receptors, reduced sleepiness in patients with central hypersomnolence syndromes in a randomized, double-blind, crossover trial (Ann Neurol. 2015 Sep;78[3]:454-65).
“It’s not great to use an antibiotic to treat people who don’t have a bacterial infection, so it would be really lovely if we had a GABA antagonist or negative allosteric modulator of GABA-A receptors that was not clarithromycin. And that’s where flumazenil comes into the picture,” according to Dr. Trotti.
As a requirement for receiving flumazenil at the Emory sleep disorders center, patients had to have been refractory to all conventional therapies. Indeed, they had been refractory to an average of 4.6 medications for excessive sleepiness. Also, their hypersomnolence had to have a serious impact on their daily life, for example a job at risk because of inability to drive to and from work safely. Initially, it was further required as a condition for treatment that patients had to show abnormal CSF potentiation of GABA-A receptors; however, the investigators quit requiring a CSF sample after roughly the first 100 candidates proved positive.
Dosing of the sublingual flumazenil lozenges began at one 6-mg lozenge four times daily, titrating up by adding an extra lozenge every 4-5 days until reaching a maximum of 12 per day. The lotion is rubbed on the inside of the forearm at a dose of 3 mg on each arm up to four times per day.
Among the 40 treatment responders who completed the Epworth Sleepiness Scale at baseline and after an average of 6.8 months on flumazenil, the average score improved from 15 to 10.3.
Fifty-seven patients obtained no benefit from flumazenil, 10 stopped the drug because of side effects, 3 quit because they preferred clarithromycin, 8 stopped owing to the cost, and the rest dropped the drug for an assortment of reasons, including planned pregnancy.
The most common treatment-emergent adverse events included dizziness in 13% of subjects, anxiety in 7%, and other mood disturbances in 6%.
Two serious adverse events occurred. One patient with a history of atrial fibrillation experienced a transient ischemic attack. And a patient with systemic lupus erythematous developed asymptomatic CNS lupus vasculopathy. It’s not possible to say whether these events were treatment related because the experience with chronic flumazenil therapy is so limited. After all, the drug is given for its approved indication for no longer than a few days, Dr. Trotti observed.
“This is all clinical data. Obviously I’m not suggesting that everybody should start prescribing flumazenil. That being said, we really need better treatment options,” she said.
The long-term treatment continuation rate with modafinil for hypersomnolence is about 50%, anywhere from 29% to 66% for amphetamines, 38% for clarithromycin, and 37% for pitolisant.
“If you look globally at how likely people with idiopathic hypersomnolence or narcolepsy are to get a satisfactory response to conventional therapies, probably 15%-20% do not get satisfactorily treated with what we currently have available. Prospective controlled studies of flumazenil for treatment of hypersomnolence are certainly needed, but in the absence of those data there’s at least a rationale for people who are severely affected and have nowhere else to turn to consider flumazenil,” Dr. Trotti concluded.
She reported having no financial conflicts regarding her study, supported by the National Institutes of Health.
DENVER – Transdermal or sublingual flumazenil is well worth considering for treatment of carefully selected patients with hypersomnolence refractory to conventional wake-promoting medications, Lynn Marie Trotti, MD, said at the annual meeting of the Associated Professional Sleep Societies.
Her retrospective chart review of 153 consecutive patients treated with flumazenil (Romazicon) showed that 63% derived symptomatic benefit, and 39% of patients remained on the drug at the end of the review period, which averaged 6.8 months, reported Dr. Trotti, a neurologist and sleep scientist at Emory University in Atlanta.
Make no mistake: This is off-label therapy. Flumazenil’s approved indication is as intravenous therapy for benzodiazepine sedation. Given orally, the drug is almost entirely eliminated on first-pass metabolism, so she and her coinvestigators had flumazenil compounded at a pharmacy in two formulations: a 6-mg sublingual lozenge and a transcutaneous lotion in a dispenser providing 3 mg of flumazenil per click of the device.
This novel therapy is supported by a plausible mechanistic rationale. Dr. Trotti and colleagues have previously shown that most patients with central hypersomnolence have abnormal potentiation of GABA-A receptors in their cerebrospinal fluid (CSF).
“Functionally speaking, it’s as though they’re producing an endogenous benzodiazepinelike substance,” she explained.
The investigators showed further that the macrolide antibiotic clarithromycin, a negative allosteric modulator of GABA-A receptors, reduced sleepiness in patients with central hypersomnolence syndromes in a randomized, double-blind, crossover trial (Ann Neurol. 2015 Sep;78[3]:454-65).
“It’s not great to use an antibiotic to treat people who don’t have a bacterial infection, so it would be really lovely if we had a GABA antagonist or negative allosteric modulator of GABA-A receptors that was not clarithromycin. And that’s where flumazenil comes into the picture,” according to Dr. Trotti.
As a requirement for receiving flumazenil at the Emory sleep disorders center, patients had to have been refractory to all conventional therapies. Indeed, they had been refractory to an average of 4.6 medications for excessive sleepiness. Also, their hypersomnolence had to have a serious impact on their daily life, for example a job at risk because of inability to drive to and from work safely. Initially, it was further required as a condition for treatment that patients had to show abnormal CSF potentiation of GABA-A receptors; however, the investigators quit requiring a CSF sample after roughly the first 100 candidates proved positive.
Dosing of the sublingual flumazenil lozenges began at one 6-mg lozenge four times daily, titrating up by adding an extra lozenge every 4-5 days until reaching a maximum of 12 per day. The lotion is rubbed on the inside of the forearm at a dose of 3 mg on each arm up to four times per day.
Among the 40 treatment responders who completed the Epworth Sleepiness Scale at baseline and after an average of 6.8 months on flumazenil, the average score improved from 15 to 10.3.
Fifty-seven patients obtained no benefit from flumazenil, 10 stopped the drug because of side effects, 3 quit because they preferred clarithromycin, 8 stopped owing to the cost, and the rest dropped the drug for an assortment of reasons, including planned pregnancy.
The most common treatment-emergent adverse events included dizziness in 13% of subjects, anxiety in 7%, and other mood disturbances in 6%.
Two serious adverse events occurred. One patient with a history of atrial fibrillation experienced a transient ischemic attack. And a patient with systemic lupus erythematous developed asymptomatic CNS lupus vasculopathy. It’s not possible to say whether these events were treatment related because the experience with chronic flumazenil therapy is so limited. After all, the drug is given for its approved indication for no longer than a few days, Dr. Trotti observed.
“This is all clinical data. Obviously I’m not suggesting that everybody should start prescribing flumazenil. That being said, we really need better treatment options,” she said.
The long-term treatment continuation rate with modafinil for hypersomnolence is about 50%, anywhere from 29% to 66% for amphetamines, 38% for clarithromycin, and 37% for pitolisant.
“If you look globally at how likely people with idiopathic hypersomnolence or narcolepsy are to get a satisfactory response to conventional therapies, probably 15%-20% do not get satisfactorily treated with what we currently have available. Prospective controlled studies of flumazenil for treatment of hypersomnolence are certainly needed, but in the absence of those data there’s at least a rationale for people who are severely affected and have nowhere else to turn to consider flumazenil,” Dr. Trotti concluded.
She reported having no financial conflicts regarding her study, supported by the National Institutes of Health.
AT SLEEP 2016
Key clinical point: Flumazenil offers a new option for refractory hypersomnolence.
Major finding: Sixty-three percent of patients with highly refractory hypersomnolence derived symptomatic benefit from flumazenil, and 39% of treated patients remained on the drug at a mean 6.8 months of follow-up.
Data source: This was a retrospective chart review of 153 consecutive patients with severe hypersomnolence refractory to all standard therapies who were treated with sublingual or topical flumazenil.
Disclosures: The presenter reported having no financial conflicts regarding her study, supported by the National Institutes of Health.
GERD and Sleep Disorders Often Go Hand in Glove
DENVER – Gastroesophageal reflux disease is fertile soil for medical and psychiatric comorbid conditions, with sleep disorders leading the way, Maurice M. Ohayon, MD, reported at the annual meeting of the Associated Professional Sleep Societies.
He presented a very large, longitudinal, population-based study of gastroesophageal reflux disease (GERD) and its fellow travelers. The study entailed telephone interviews with 12,218 nationally representative subjects in 8 states at time 1, and reinterviews with 10,830 of them 3 years later. The interviews were guided by Sleep-EVAL, a validated computerized diagnostic interview system.
At time 1, 10.6% of subjects reported that they were told by a physician they have GERD and/or they were taking a medication for it. At time 2 (3 years later), the prevalence had increased to 12.4%, according to Dr. Ohayon, professor of psychiatry and behavioral sciences, chief of the division of public mental health and population sciences, and director of the sleep epidemiology research center at Stanford (Calif.) University.
Chronic GERD – that is, GERD at both time points – was present in 3.9% of subjects; 6% of subjects were remitters, meaning that they had GERD at time 1 but not at time 2. Another 8.5% of the total sample had incident GERD, meaning they had GERD at time 2 but not time 1.
The prevalence of GERD rose stepwise with increasing age, from the low single digits in 18- to 34-year-olds to a peak in the 55- to 64-year-old age group, where the prevalence was 13.5% at time 1 and 17% at time 2.
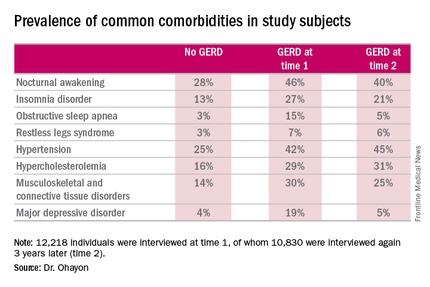
GERD was significantly more common in women. At time 2, the prevalence was 10% in men and 14.4% in women.
Nocturnal awakening was the sleep disorder symptom most commonly associated with GERD. It was a complaint in 28% of subjects who never had GERD, 46% of those with GERD at time 1, and 40% of those with GERD at time 2.
Insomnia, obstructive sleep apnea, and restless legs syndrome were also significantly more common among subjects with GERD. So were musculoskeletal and connective tissue diseases, hypertension, hypercholesterolemia, and major depressive disorder.
The study was supported by the John Arrillaga Foundation and Takeda Pharmaceuticals. Dr. Ohayon reported no financial conflicts of interest.
DENVER – Gastroesophageal reflux disease is fertile soil for medical and psychiatric comorbid conditions, with sleep disorders leading the way, Maurice M. Ohayon, MD, reported at the annual meeting of the Associated Professional Sleep Societies.
He presented a very large, longitudinal, population-based study of gastroesophageal reflux disease (GERD) and its fellow travelers. The study entailed telephone interviews with 12,218 nationally representative subjects in 8 states at time 1, and reinterviews with 10,830 of them 3 years later. The interviews were guided by Sleep-EVAL, a validated computerized diagnostic interview system.
At time 1, 10.6% of subjects reported that they were told by a physician they have GERD and/or they were taking a medication for it. At time 2 (3 years later), the prevalence had increased to 12.4%, according to Dr. Ohayon, professor of psychiatry and behavioral sciences, chief of the division of public mental health and population sciences, and director of the sleep epidemiology research center at Stanford (Calif.) University.
Chronic GERD – that is, GERD at both time points – was present in 3.9% of subjects; 6% of subjects were remitters, meaning that they had GERD at time 1 but not at time 2. Another 8.5% of the total sample had incident GERD, meaning they had GERD at time 2 but not time 1.
The prevalence of GERD rose stepwise with increasing age, from the low single digits in 18- to 34-year-olds to a peak in the 55- to 64-year-old age group, where the prevalence was 13.5% at time 1 and 17% at time 2.
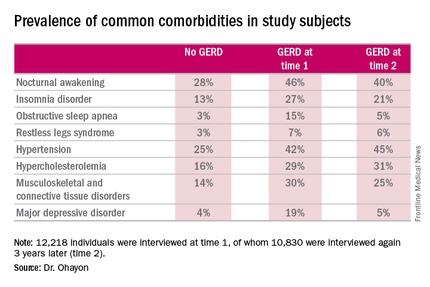
GERD was significantly more common in women. At time 2, the prevalence was 10% in men and 14.4% in women.
Nocturnal awakening was the sleep disorder symptom most commonly associated with GERD. It was a complaint in 28% of subjects who never had GERD, 46% of those with GERD at time 1, and 40% of those with GERD at time 2.
Insomnia, obstructive sleep apnea, and restless legs syndrome were also significantly more common among subjects with GERD. So were musculoskeletal and connective tissue diseases, hypertension, hypercholesterolemia, and major depressive disorder.
The study was supported by the John Arrillaga Foundation and Takeda Pharmaceuticals. Dr. Ohayon reported no financial conflicts of interest.
DENVER – Gastroesophageal reflux disease is fertile soil for medical and psychiatric comorbid conditions, with sleep disorders leading the way, Maurice M. Ohayon, MD, reported at the annual meeting of the Associated Professional Sleep Societies.
He presented a very large, longitudinal, population-based study of gastroesophageal reflux disease (GERD) and its fellow travelers. The study entailed telephone interviews with 12,218 nationally representative subjects in 8 states at time 1, and reinterviews with 10,830 of them 3 years later. The interviews were guided by Sleep-EVAL, a validated computerized diagnostic interview system.
At time 1, 10.6% of subjects reported that they were told by a physician they have GERD and/or they were taking a medication for it. At time 2 (3 years later), the prevalence had increased to 12.4%, according to Dr. Ohayon, professor of psychiatry and behavioral sciences, chief of the division of public mental health and population sciences, and director of the sleep epidemiology research center at Stanford (Calif.) University.
Chronic GERD – that is, GERD at both time points – was present in 3.9% of subjects; 6% of subjects were remitters, meaning that they had GERD at time 1 but not at time 2. Another 8.5% of the total sample had incident GERD, meaning they had GERD at time 2 but not time 1.
The prevalence of GERD rose stepwise with increasing age, from the low single digits in 18- to 34-year-olds to a peak in the 55- to 64-year-old age group, where the prevalence was 13.5% at time 1 and 17% at time 2.
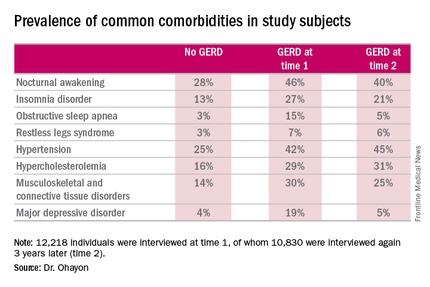
GERD was significantly more common in women. At time 2, the prevalence was 10% in men and 14.4% in women.
Nocturnal awakening was the sleep disorder symptom most commonly associated with GERD. It was a complaint in 28% of subjects who never had GERD, 46% of those with GERD at time 1, and 40% of those with GERD at time 2.
Insomnia, obstructive sleep apnea, and restless legs syndrome were also significantly more common among subjects with GERD. So were musculoskeletal and connective tissue diseases, hypertension, hypercholesterolemia, and major depressive disorder.
The study was supported by the John Arrillaga Foundation and Takeda Pharmaceuticals. Dr. Ohayon reported no financial conflicts of interest.
AT SLEEP 2016