User login
Phase 2 studies show potential of FcRn blockade in primary ITP
ORLANDO – Treatments targeted to the neonatal Fc receptor are showing promise in phase 2 studies in primary immune thrombocytopenia, investigators reported at the annual meeting of the American Society of Hematology.
Encouraging outcomes support the continued phase 3 development of these agents, which are designed to block the neonatal Fc receptor (FcRn) in patients with this IgG-mediated disease.
Blocking FcRN is intended to prevent recycling of IgG, resulting in IgG degradation, according to the authors of studies evaluating rozanolixizumab, a subcutaneously administered monoclonal antibody, and efgartigimod, an intravenously administered antibody fragment, in primary immune thrombocytopenia (ITP).
Rozanolixizumab
Results of the phase 2 study of rozanolixizumab demonstrated that this agent reduced IgG levels and improved platelet counts at all doses tested, according to the investigators, led by Tadeusz Robak, MD, of the department of hematology at the Medical University of Lodz (Poland).
Efficacy endpoints were seen more quickly – by day 8 of treatment – with single subcutaneous infusions at higher doses, according to the researchers.
Headaches of mild to moderate severity were noted at higher doses, and no patients left the study because of adverse events, they reported.
“These safety, tolerability, and efficacy data support phase 3 development of rozanolixizumab in patients with primary ITP,” wrote Dr. Robak and coauthors in the abstract for their study.
A total of 66 adult patients with primary ITP were enrolled and treated with single or multiple subcutaneous doses of rozanolixizumab administered at 1-week intervals.
Baseline characteristics suggested a “difficult-to-treat” patient cohort that had a median ITP duration of nearly 6 years and a median of four prior therapies, including thrombopoietin receptor agonists in about one-third of patients, according to the investigators.
Platelet counts of at least 50 x 109/L were achieved by day 8 in more than half of patients who received single doses of rozanolixizumab at higher dose levels of 15 mg/kg (58.3%) and 20 mg/kg (54.5%), Dr. Robak and colleagues reported.
Mild to moderate headaches were seen in about 40% of patients over an 8-week observation period. There were no serious infections and, of four serious adverse events occurring during the study, none were deemed to be treatment related, according to the investigators.
“People who have primary ITP may experience low platelet count that can put them at risk for severe bleeding, and there are limited options that provide a rapid increase in platelet count to reduce this risk,” Dr. Robak said in an interview. “These data build on the growing body of evidence that suggest targeting the FcRn pathway could have the potential to transform the treatment experience for people with rare IgG autoantibody–mediated diseases such as primary ITP.”
Efgartigimod
Substantial reductions in IgG levels and clinically relevant increases in platelet counts were seen following a 3-week treatment cycle with efgartigimod in patients with treatment-refractory ITP, according to investigator Adrian C. Newland, MB, BCh, of the Royal London Hospital and coinvestigators.
The human IgG1 antibody Fc-fragment, a natural ligand of FcRN, is engineered to have increased affinity to FcRn, while preserving its pH‐dependent binding, according to the investigators.
Efgartigimod treatment was well tolerated and reduced the proportion of patients with bleeding in the phase 2 study presented at ASH 2019.
“This suggests that targeted IgG reduction with efgartigimod is a potential new treatment modality in primary ITP, and warrants evaluation of longer-term treatment in a larger phase 3 study,” the investigators reported in the abstract for their study.
The report described 38 patients randomized to four weekly intravenous infusions of placebo or efgartigimod at one of two dosing levels. Patients had long-standing ITP, with a median 4.8 years disease duration, and all had either failed splenectomy or had inadequate response to prior treatment.
Efgartigimod treatment rapidly reduced total IgG in all patients who received it, with a mean change from baseline of up to 63.7%, according to investigators.
Platelet counts favored the investigational treatment over placebo by several measures. Platelet counts of at least 50 x 109/L on two or more occasions were seen in 46% of efgartigimod-treated patients and 25% of the placebo group; that platelet count was achieved for 10 or more days in 38% and 0% of the efgartigimod and placebo groups, respectively.
Treatment was well tolerated, according to the investigators, who said there were “no dose-related safety observations.” Full results of the phase 2 investigation were published in the American Journal of Hematology, concurrent with the meeting (2019 Dec 10. doi.org/10.1002/ajh.25680).
The study of rozanolixizumab was supported by UCB; Dr. Robak reported disclosures related to UCB (honoraria, research funding), as well as Takeda, Janssen, Amgen, Roche, AbbVie, Gilead, BeiGene, Acerta, and MorphoSys. The study of efgartigimod was supported by argenx; Dr. Newland reported disclosures related to argenx, Novartis, Angle, Amgen, Ono Pharmaceutical, Shionogi, Rigel, and Dova Pharmaceuticals.
SOURCEs: Robak T et al. ASH 2019, Abstract 897; Newland AC et al. ASH 2019, Abstract 895.
ORLANDO – Treatments targeted to the neonatal Fc receptor are showing promise in phase 2 studies in primary immune thrombocytopenia, investigators reported at the annual meeting of the American Society of Hematology.
Encouraging outcomes support the continued phase 3 development of these agents, which are designed to block the neonatal Fc receptor (FcRn) in patients with this IgG-mediated disease.
Blocking FcRN is intended to prevent recycling of IgG, resulting in IgG degradation, according to the authors of studies evaluating rozanolixizumab, a subcutaneously administered monoclonal antibody, and efgartigimod, an intravenously administered antibody fragment, in primary immune thrombocytopenia (ITP).
Rozanolixizumab
Results of the phase 2 study of rozanolixizumab demonstrated that this agent reduced IgG levels and improved platelet counts at all doses tested, according to the investigators, led by Tadeusz Robak, MD, of the department of hematology at the Medical University of Lodz (Poland).
Efficacy endpoints were seen more quickly – by day 8 of treatment – with single subcutaneous infusions at higher doses, according to the researchers.
Headaches of mild to moderate severity were noted at higher doses, and no patients left the study because of adverse events, they reported.
“These safety, tolerability, and efficacy data support phase 3 development of rozanolixizumab in patients with primary ITP,” wrote Dr. Robak and coauthors in the abstract for their study.
A total of 66 adult patients with primary ITP were enrolled and treated with single or multiple subcutaneous doses of rozanolixizumab administered at 1-week intervals.
Baseline characteristics suggested a “difficult-to-treat” patient cohort that had a median ITP duration of nearly 6 years and a median of four prior therapies, including thrombopoietin receptor agonists in about one-third of patients, according to the investigators.
Platelet counts of at least 50 x 109/L were achieved by day 8 in more than half of patients who received single doses of rozanolixizumab at higher dose levels of 15 mg/kg (58.3%) and 20 mg/kg (54.5%), Dr. Robak and colleagues reported.
Mild to moderate headaches were seen in about 40% of patients over an 8-week observation period. There were no serious infections and, of four serious adverse events occurring during the study, none were deemed to be treatment related, according to the investigators.
“People who have primary ITP may experience low platelet count that can put them at risk for severe bleeding, and there are limited options that provide a rapid increase in platelet count to reduce this risk,” Dr. Robak said in an interview. “These data build on the growing body of evidence that suggest targeting the FcRn pathway could have the potential to transform the treatment experience for people with rare IgG autoantibody–mediated diseases such as primary ITP.”
Efgartigimod
Substantial reductions in IgG levels and clinically relevant increases in platelet counts were seen following a 3-week treatment cycle with efgartigimod in patients with treatment-refractory ITP, according to investigator Adrian C. Newland, MB, BCh, of the Royal London Hospital and coinvestigators.
The human IgG1 antibody Fc-fragment, a natural ligand of FcRN, is engineered to have increased affinity to FcRn, while preserving its pH‐dependent binding, according to the investigators.
Efgartigimod treatment was well tolerated and reduced the proportion of patients with bleeding in the phase 2 study presented at ASH 2019.
“This suggests that targeted IgG reduction with efgartigimod is a potential new treatment modality in primary ITP, and warrants evaluation of longer-term treatment in a larger phase 3 study,” the investigators reported in the abstract for their study.
The report described 38 patients randomized to four weekly intravenous infusions of placebo or efgartigimod at one of two dosing levels. Patients had long-standing ITP, with a median 4.8 years disease duration, and all had either failed splenectomy or had inadequate response to prior treatment.
Efgartigimod treatment rapidly reduced total IgG in all patients who received it, with a mean change from baseline of up to 63.7%, according to investigators.
Platelet counts favored the investigational treatment over placebo by several measures. Platelet counts of at least 50 x 109/L on two or more occasions were seen in 46% of efgartigimod-treated patients and 25% of the placebo group; that platelet count was achieved for 10 or more days in 38% and 0% of the efgartigimod and placebo groups, respectively.
Treatment was well tolerated, according to the investigators, who said there were “no dose-related safety observations.” Full results of the phase 2 investigation were published in the American Journal of Hematology, concurrent with the meeting (2019 Dec 10. doi.org/10.1002/ajh.25680).
The study of rozanolixizumab was supported by UCB; Dr. Robak reported disclosures related to UCB (honoraria, research funding), as well as Takeda, Janssen, Amgen, Roche, AbbVie, Gilead, BeiGene, Acerta, and MorphoSys. The study of efgartigimod was supported by argenx; Dr. Newland reported disclosures related to argenx, Novartis, Angle, Amgen, Ono Pharmaceutical, Shionogi, Rigel, and Dova Pharmaceuticals.
SOURCEs: Robak T et al. ASH 2019, Abstract 897; Newland AC et al. ASH 2019, Abstract 895.
ORLANDO – Treatments targeted to the neonatal Fc receptor are showing promise in phase 2 studies in primary immune thrombocytopenia, investigators reported at the annual meeting of the American Society of Hematology.
Encouraging outcomes support the continued phase 3 development of these agents, which are designed to block the neonatal Fc receptor (FcRn) in patients with this IgG-mediated disease.
Blocking FcRN is intended to prevent recycling of IgG, resulting in IgG degradation, according to the authors of studies evaluating rozanolixizumab, a subcutaneously administered monoclonal antibody, and efgartigimod, an intravenously administered antibody fragment, in primary immune thrombocytopenia (ITP).
Rozanolixizumab
Results of the phase 2 study of rozanolixizumab demonstrated that this agent reduced IgG levels and improved platelet counts at all doses tested, according to the investigators, led by Tadeusz Robak, MD, of the department of hematology at the Medical University of Lodz (Poland).
Efficacy endpoints were seen more quickly – by day 8 of treatment – with single subcutaneous infusions at higher doses, according to the researchers.
Headaches of mild to moderate severity were noted at higher doses, and no patients left the study because of adverse events, they reported.
“These safety, tolerability, and efficacy data support phase 3 development of rozanolixizumab in patients with primary ITP,” wrote Dr. Robak and coauthors in the abstract for their study.
A total of 66 adult patients with primary ITP were enrolled and treated with single or multiple subcutaneous doses of rozanolixizumab administered at 1-week intervals.
Baseline characteristics suggested a “difficult-to-treat” patient cohort that had a median ITP duration of nearly 6 years and a median of four prior therapies, including thrombopoietin receptor agonists in about one-third of patients, according to the investigators.
Platelet counts of at least 50 x 109/L were achieved by day 8 in more than half of patients who received single doses of rozanolixizumab at higher dose levels of 15 mg/kg (58.3%) and 20 mg/kg (54.5%), Dr. Robak and colleagues reported.
Mild to moderate headaches were seen in about 40% of patients over an 8-week observation period. There were no serious infections and, of four serious adverse events occurring during the study, none were deemed to be treatment related, according to the investigators.
“People who have primary ITP may experience low platelet count that can put them at risk for severe bleeding, and there are limited options that provide a rapid increase in platelet count to reduce this risk,” Dr. Robak said in an interview. “These data build on the growing body of evidence that suggest targeting the FcRn pathway could have the potential to transform the treatment experience for people with rare IgG autoantibody–mediated diseases such as primary ITP.”
Efgartigimod
Substantial reductions in IgG levels and clinically relevant increases in platelet counts were seen following a 3-week treatment cycle with efgartigimod in patients with treatment-refractory ITP, according to investigator Adrian C. Newland, MB, BCh, of the Royal London Hospital and coinvestigators.
The human IgG1 antibody Fc-fragment, a natural ligand of FcRN, is engineered to have increased affinity to FcRn, while preserving its pH‐dependent binding, according to the investigators.
Efgartigimod treatment was well tolerated and reduced the proportion of patients with bleeding in the phase 2 study presented at ASH 2019.
“This suggests that targeted IgG reduction with efgartigimod is a potential new treatment modality in primary ITP, and warrants evaluation of longer-term treatment in a larger phase 3 study,” the investigators reported in the abstract for their study.
The report described 38 patients randomized to four weekly intravenous infusions of placebo or efgartigimod at one of two dosing levels. Patients had long-standing ITP, with a median 4.8 years disease duration, and all had either failed splenectomy or had inadequate response to prior treatment.
Efgartigimod treatment rapidly reduced total IgG in all patients who received it, with a mean change from baseline of up to 63.7%, according to investigators.
Platelet counts favored the investigational treatment over placebo by several measures. Platelet counts of at least 50 x 109/L on two or more occasions were seen in 46% of efgartigimod-treated patients and 25% of the placebo group; that platelet count was achieved for 10 or more days in 38% and 0% of the efgartigimod and placebo groups, respectively.
Treatment was well tolerated, according to the investigators, who said there were “no dose-related safety observations.” Full results of the phase 2 investigation were published in the American Journal of Hematology, concurrent with the meeting (2019 Dec 10. doi.org/10.1002/ajh.25680).
The study of rozanolixizumab was supported by UCB; Dr. Robak reported disclosures related to UCB (honoraria, research funding), as well as Takeda, Janssen, Amgen, Roche, AbbVie, Gilead, BeiGene, Acerta, and MorphoSys. The study of efgartigimod was supported by argenx; Dr. Newland reported disclosures related to argenx, Novartis, Angle, Amgen, Ono Pharmaceutical, Shionogi, Rigel, and Dova Pharmaceuticals.
SOURCEs: Robak T et al. ASH 2019, Abstract 897; Newland AC et al. ASH 2019, Abstract 895.
REPORTING FROM ASH 2019
New ASH guideline: VTE prophylaxis after major surgery
ORLANDO – The latest American Society of Hematology guideline on venous thromboembolism (VTE) tackles 30 key questions regarding prophylaxis in hospitalized patients undergoing surgery, according to the chair of the guideline panel, who highlighted 9 of those questions during a special session at the society’s annual meeting.
The clinical practice guideline, published just about a week before the annual meeting of the American Society of Hematology, focuses mainly on pharmacologic prophylaxis in specific surgical settings, said David R. Anderson, MD, dean of the faculty of medicine of Dalhousie University, Halifax, N.S.
“Our guidelines focused upon clinically important symptomatic outcomes, with less emphasis being placed on asymptomatic deep vein thrombosis detected by screening tests,” Dr. Anderson said.
At the special education session, Dr. Anderson highlighted several specific recommendations on prophylaxis in surgical patients.
Pharmacologic prophylaxis is not recommended for patients experiencing major trauma deemed to be at high risk of bleeding. Its use does reduce risk of symptomatic pulmonary embolism (PE) and deep vein thrombosis (DVT) by about 10 events per 1,000 patients treated; however, Dr. Anderson said, the panel’s opinion was that this benefit was outweighed by increased risk of major bleeding, at 24 events per 1,000 patients treated.
“We do recommend, however that this risk of bleeding must be reevaluated over the course of recovery of patients, and this may change the decision around this intervention over time,” Dr. Anderson told attendees at the special session.
That’s because pharmacologic prophylaxis is recommended in surgical patients at low to moderate risk of bleeding. In this scenario, the incremental risk of major bleeding (14 events per 1,000 patients treated) is outweighed by the benefit of the reduction of symptomatic VTE events, according to Dr. Anderson.
When pharmacologic prophylaxis is used, the panel recommends combined prophylaxis – mechanical prophylaxis in addition to pharmacologic prophylaxis – especially in those patients at high or very high risk of VTE. Evidence shows that the combination approach significantly reduces risk of PE, and strongly suggests it may also reduce risk of symptomatic proximal DVT, Dr. Anderson said.
In surgical patients not receiving pharmacologic prophylaxis, mechanical prophylaxis is recommended over no mechanical prophylaxis, he added. Moreover, in those patients receiving mechanical prophylaxis, the ASH panel recommends use of intermittent compression devices over graduated compression stockings.
The panel comes out against prophylactic inferior vena cava (IVC) filter insertion in the guidelines. Dr. Anderson said that the “small reduction” in PE risk seen in observational studies is outweighed by increased risk of DVT, and a resulting trend for increased mortality, associated with insertion of the devices.
“We did not consider other risks of IVC filters such as filter embolization or perforation, which again would be complications that would support our recommendation against routine use of these devices in patients undergoing major surgery,” he said.
In terms of the type of pharmacologic prophylaxis to use, the panel said low-molecular-weight heparin or unfractionated heparin would be reasonable choices in this setting. Available data do not demonstrate any significant differences between these choices for major clinical outcomes, Dr. Anderson added.
The guideline also addresses duration of pharmacologic prophylaxis, stating that extended prophylaxis – of at least 3 weeks – is favored over short-term prophylaxis, or up to 2 weeks of treatment. The extended approach significantly reduces risk of symptomatic PE and proximal DVT, though most of the supporting data come from studies of major joint arthroplasty and major general surgical procedures for patients with cancer. “We need more studies in other clinical areas to examine this particular question,” Dr. Anderson said.
The guideline on prophylaxis in surgical patients was published in Blood Advances (2019 Dec 3;3[23]:3898-944). Six other ASH VTE guidelines, all published in 2018, covered prophylaxis in medical patients, diagnosis, VTE in pregnancy, optimal anticoagulation, heparin-induced thrombocytopenia, and pediatric considerations. The guidelines are available on the ASH website.
Dr. Anderson reported having no relevant conflicts of interest.
ORLANDO – The latest American Society of Hematology guideline on venous thromboembolism (VTE) tackles 30 key questions regarding prophylaxis in hospitalized patients undergoing surgery, according to the chair of the guideline panel, who highlighted 9 of those questions during a special session at the society’s annual meeting.
The clinical practice guideline, published just about a week before the annual meeting of the American Society of Hematology, focuses mainly on pharmacologic prophylaxis in specific surgical settings, said David R. Anderson, MD, dean of the faculty of medicine of Dalhousie University, Halifax, N.S.
“Our guidelines focused upon clinically important symptomatic outcomes, with less emphasis being placed on asymptomatic deep vein thrombosis detected by screening tests,” Dr. Anderson said.
At the special education session, Dr. Anderson highlighted several specific recommendations on prophylaxis in surgical patients.
Pharmacologic prophylaxis is not recommended for patients experiencing major trauma deemed to be at high risk of bleeding. Its use does reduce risk of symptomatic pulmonary embolism (PE) and deep vein thrombosis (DVT) by about 10 events per 1,000 patients treated; however, Dr. Anderson said, the panel’s opinion was that this benefit was outweighed by increased risk of major bleeding, at 24 events per 1,000 patients treated.
“We do recommend, however that this risk of bleeding must be reevaluated over the course of recovery of patients, and this may change the decision around this intervention over time,” Dr. Anderson told attendees at the special session.
That’s because pharmacologic prophylaxis is recommended in surgical patients at low to moderate risk of bleeding. In this scenario, the incremental risk of major bleeding (14 events per 1,000 patients treated) is outweighed by the benefit of the reduction of symptomatic VTE events, according to Dr. Anderson.
When pharmacologic prophylaxis is used, the panel recommends combined prophylaxis – mechanical prophylaxis in addition to pharmacologic prophylaxis – especially in those patients at high or very high risk of VTE. Evidence shows that the combination approach significantly reduces risk of PE, and strongly suggests it may also reduce risk of symptomatic proximal DVT, Dr. Anderson said.
In surgical patients not receiving pharmacologic prophylaxis, mechanical prophylaxis is recommended over no mechanical prophylaxis, he added. Moreover, in those patients receiving mechanical prophylaxis, the ASH panel recommends use of intermittent compression devices over graduated compression stockings.
The panel comes out against prophylactic inferior vena cava (IVC) filter insertion in the guidelines. Dr. Anderson said that the “small reduction” in PE risk seen in observational studies is outweighed by increased risk of DVT, and a resulting trend for increased mortality, associated with insertion of the devices.
“We did not consider other risks of IVC filters such as filter embolization or perforation, which again would be complications that would support our recommendation against routine use of these devices in patients undergoing major surgery,” he said.
In terms of the type of pharmacologic prophylaxis to use, the panel said low-molecular-weight heparin or unfractionated heparin would be reasonable choices in this setting. Available data do not demonstrate any significant differences between these choices for major clinical outcomes, Dr. Anderson added.
The guideline also addresses duration of pharmacologic prophylaxis, stating that extended prophylaxis – of at least 3 weeks – is favored over short-term prophylaxis, or up to 2 weeks of treatment. The extended approach significantly reduces risk of symptomatic PE and proximal DVT, though most of the supporting data come from studies of major joint arthroplasty and major general surgical procedures for patients with cancer. “We need more studies in other clinical areas to examine this particular question,” Dr. Anderson said.
The guideline on prophylaxis in surgical patients was published in Blood Advances (2019 Dec 3;3[23]:3898-944). Six other ASH VTE guidelines, all published in 2018, covered prophylaxis in medical patients, diagnosis, VTE in pregnancy, optimal anticoagulation, heparin-induced thrombocytopenia, and pediatric considerations. The guidelines are available on the ASH website.
Dr. Anderson reported having no relevant conflicts of interest.
ORLANDO – The latest American Society of Hematology guideline on venous thromboembolism (VTE) tackles 30 key questions regarding prophylaxis in hospitalized patients undergoing surgery, according to the chair of the guideline panel, who highlighted 9 of those questions during a special session at the society’s annual meeting.
The clinical practice guideline, published just about a week before the annual meeting of the American Society of Hematology, focuses mainly on pharmacologic prophylaxis in specific surgical settings, said David R. Anderson, MD, dean of the faculty of medicine of Dalhousie University, Halifax, N.S.
“Our guidelines focused upon clinically important symptomatic outcomes, with less emphasis being placed on asymptomatic deep vein thrombosis detected by screening tests,” Dr. Anderson said.
At the special education session, Dr. Anderson highlighted several specific recommendations on prophylaxis in surgical patients.
Pharmacologic prophylaxis is not recommended for patients experiencing major trauma deemed to be at high risk of bleeding. Its use does reduce risk of symptomatic pulmonary embolism (PE) and deep vein thrombosis (DVT) by about 10 events per 1,000 patients treated; however, Dr. Anderson said, the panel’s opinion was that this benefit was outweighed by increased risk of major bleeding, at 24 events per 1,000 patients treated.
“We do recommend, however that this risk of bleeding must be reevaluated over the course of recovery of patients, and this may change the decision around this intervention over time,” Dr. Anderson told attendees at the special session.
That’s because pharmacologic prophylaxis is recommended in surgical patients at low to moderate risk of bleeding. In this scenario, the incremental risk of major bleeding (14 events per 1,000 patients treated) is outweighed by the benefit of the reduction of symptomatic VTE events, according to Dr. Anderson.
When pharmacologic prophylaxis is used, the panel recommends combined prophylaxis – mechanical prophylaxis in addition to pharmacologic prophylaxis – especially in those patients at high or very high risk of VTE. Evidence shows that the combination approach significantly reduces risk of PE, and strongly suggests it may also reduce risk of symptomatic proximal DVT, Dr. Anderson said.
In surgical patients not receiving pharmacologic prophylaxis, mechanical prophylaxis is recommended over no mechanical prophylaxis, he added. Moreover, in those patients receiving mechanical prophylaxis, the ASH panel recommends use of intermittent compression devices over graduated compression stockings.
The panel comes out against prophylactic inferior vena cava (IVC) filter insertion in the guidelines. Dr. Anderson said that the “small reduction” in PE risk seen in observational studies is outweighed by increased risk of DVT, and a resulting trend for increased mortality, associated with insertion of the devices.
“We did not consider other risks of IVC filters such as filter embolization or perforation, which again would be complications that would support our recommendation against routine use of these devices in patients undergoing major surgery,” he said.
In terms of the type of pharmacologic prophylaxis to use, the panel said low-molecular-weight heparin or unfractionated heparin would be reasonable choices in this setting. Available data do not demonstrate any significant differences between these choices for major clinical outcomes, Dr. Anderson added.
The guideline also addresses duration of pharmacologic prophylaxis, stating that extended prophylaxis – of at least 3 weeks – is favored over short-term prophylaxis, or up to 2 weeks of treatment. The extended approach significantly reduces risk of symptomatic PE and proximal DVT, though most of the supporting data come from studies of major joint arthroplasty and major general surgical procedures for patients with cancer. “We need more studies in other clinical areas to examine this particular question,” Dr. Anderson said.
The guideline on prophylaxis in surgical patients was published in Blood Advances (2019 Dec 3;3[23]:3898-944). Six other ASH VTE guidelines, all published in 2018, covered prophylaxis in medical patients, diagnosis, VTE in pregnancy, optimal anticoagulation, heparin-induced thrombocytopenia, and pediatric considerations. The guidelines are available on the ASH website.
Dr. Anderson reported having no relevant conflicts of interest.
EXPERT ANALYSIS FROM ASH 2019
Fibrosis scoring systems have ‘modest’ predictive value in general population
Currently available fibrosis scoring systems appear to have only a modest predictive ability for development of severe liver disease in the general population, according to authors of a large, retrospective cohort study.
Of five noninvasive scoring systems evaluated, all did have high negative predictive value in the general population, according to authors of the study, which included data on more than 800,000 individuals in Sweden. However, their sensitivities were low, with most of the individuals who developed severe liver disease over a 10-year follow-up period initially classified as being at low risk for advanced fibrosis, according to the study authors, led by Hannes Hagström, MD, PhD, of the division of hepatology, Karolinska University Hospital, Stockholm.
The scoring systems tended to perform better in patients at higher risk for nonalcoholic fatty liver disease (NAFLD) at baseline, suggesting the best use of the tools is in patients at increased risk or who have liver disease indications, Dr. Hagström and coauthors wrote in a report on the study.
“Although useful in populations with a high prevalence of advanced fibrosis, current scores lack precision for usage in the general population for which the prevalence of advanced fibrosis is much lower,” Dr. Hagström and colleagues said.
The scoring systems were derived from high-risk cohorts with liver diseases, the authors noted, stating that the disease prevalence in any given population will affect the performance of a test that’s intended to diagnose that specific disease.
“New and improved” scoring systems should be developed to more effectively pinpoint patients with NAFLD who are at higher risk of a severe liver event, they added in the report, which appears in Gastroenterology.
The population-based cohort study by Dr. Hagström and colleagues was based on data from 812,073 patients enrolled in the Swedish Apolipoprotein Mortality Risk (AMORIS) cohort between 1985 and 1996. Investigators said they excluded patients under 35 and over 79 years of age, patients with severe liver disease at baseline, and those with a prior diagnosis of alcohol or drug abuse.
Investigators used available data to calculate five scores, including the AST to Platelet Ratio Index (APRI); the body mass index, AST/ALT ratio, and diabetes (BARD) score; the Fibrosis-4 (FIB-4) score; Forns Index; and NAFLD Fibrosis Score (NFS).
At baseline, 0.5%-8.0% of patients were considered to be at high risk for advanced fibrosis, depending on the test used, investigators said. With up to 10 years of follow-up, the proportion of individuals who developed severe liver diseases (cirrhosis, liver failure, hepatocellular carcinoma, liver transplantation, or decompensated liver disease) was 0.3%-0.6%, and with the maximum 27 years of follow-up, the incidence ranged from 1.0% to 1.4%.
There was a “strong association” between baseline risk of fibrosis and development of severe liver diseases; however, the majority of cases occurred in patients deemed low risk at baseline, Dr. Hagström and colleagues noted in their report.
For example, 12.4% of individuals classified as high risk by APRI developed severe liver diseases over 10 years, compared to just 0.4% of the low-risk group, yet out of 723 cases, 502 (69%) occurred in the low-risk patients, the data show.
Hazard ratios did increase with risk level, and at the high-risk level, adjusted hazard ratios ranged from 1.7 (95% confidence interval [CI], 1.1-2.5) for the high-risk BARD patients to 45.9 (95% CI, 36.1-58.3) for the high-risk APRI patients, investigators reported.
Taken together, results of this study demonstrate that the performance of all scores was low in an unselected population, according to investigators.
Of all tests, APRI was least likely to falsely classify patients who never developed severe liver diseases and had an intermediate-risk group of 4%, the lowest of any test, which are findings that may have implications for routine primary care, according to investigators.
“APRI could be the currently best score to exclude a high risk of liver-related events in the near future, and thereby reduce unnecessary testing in a general population,” they said in a discussion of their results.
The study was supported by an independent grant from AstraZeneca. Dr. Hagström reported disclosures related to that company, as well as Novo Nordisk, Gilead Sciences, IQVIA, Intercept, and Bristol Myers-Squibb.
SOURCE: Hagström H et al. Gastroenterology. 2019 Sep 26. doi: 10.1053/j.gastro.2019.09.008.
Currently available fibrosis scoring systems appear to have only a modest predictive ability for development of severe liver disease in the general population, according to authors of a large, retrospective cohort study.
Of five noninvasive scoring systems evaluated, all did have high negative predictive value in the general population, according to authors of the study, which included data on more than 800,000 individuals in Sweden. However, their sensitivities were low, with most of the individuals who developed severe liver disease over a 10-year follow-up period initially classified as being at low risk for advanced fibrosis, according to the study authors, led by Hannes Hagström, MD, PhD, of the division of hepatology, Karolinska University Hospital, Stockholm.
The scoring systems tended to perform better in patients at higher risk for nonalcoholic fatty liver disease (NAFLD) at baseline, suggesting the best use of the tools is in patients at increased risk or who have liver disease indications, Dr. Hagström and coauthors wrote in a report on the study.
“Although useful in populations with a high prevalence of advanced fibrosis, current scores lack precision for usage in the general population for which the prevalence of advanced fibrosis is much lower,” Dr. Hagström and colleagues said.
The scoring systems were derived from high-risk cohorts with liver diseases, the authors noted, stating that the disease prevalence in any given population will affect the performance of a test that’s intended to diagnose that specific disease.
“New and improved” scoring systems should be developed to more effectively pinpoint patients with NAFLD who are at higher risk of a severe liver event, they added in the report, which appears in Gastroenterology.
The population-based cohort study by Dr. Hagström and colleagues was based on data from 812,073 patients enrolled in the Swedish Apolipoprotein Mortality Risk (AMORIS) cohort between 1985 and 1996. Investigators said they excluded patients under 35 and over 79 years of age, patients with severe liver disease at baseline, and those with a prior diagnosis of alcohol or drug abuse.
Investigators used available data to calculate five scores, including the AST to Platelet Ratio Index (APRI); the body mass index, AST/ALT ratio, and diabetes (BARD) score; the Fibrosis-4 (FIB-4) score; Forns Index; and NAFLD Fibrosis Score (NFS).
At baseline, 0.5%-8.0% of patients were considered to be at high risk for advanced fibrosis, depending on the test used, investigators said. With up to 10 years of follow-up, the proportion of individuals who developed severe liver diseases (cirrhosis, liver failure, hepatocellular carcinoma, liver transplantation, or decompensated liver disease) was 0.3%-0.6%, and with the maximum 27 years of follow-up, the incidence ranged from 1.0% to 1.4%.
There was a “strong association” between baseline risk of fibrosis and development of severe liver diseases; however, the majority of cases occurred in patients deemed low risk at baseline, Dr. Hagström and colleagues noted in their report.
For example, 12.4% of individuals classified as high risk by APRI developed severe liver diseases over 10 years, compared to just 0.4% of the low-risk group, yet out of 723 cases, 502 (69%) occurred in the low-risk patients, the data show.
Hazard ratios did increase with risk level, and at the high-risk level, adjusted hazard ratios ranged from 1.7 (95% confidence interval [CI], 1.1-2.5) for the high-risk BARD patients to 45.9 (95% CI, 36.1-58.3) for the high-risk APRI patients, investigators reported.
Taken together, results of this study demonstrate that the performance of all scores was low in an unselected population, according to investigators.
Of all tests, APRI was least likely to falsely classify patients who never developed severe liver diseases and had an intermediate-risk group of 4%, the lowest of any test, which are findings that may have implications for routine primary care, according to investigators.
“APRI could be the currently best score to exclude a high risk of liver-related events in the near future, and thereby reduce unnecessary testing in a general population,” they said in a discussion of their results.
The study was supported by an independent grant from AstraZeneca. Dr. Hagström reported disclosures related to that company, as well as Novo Nordisk, Gilead Sciences, IQVIA, Intercept, and Bristol Myers-Squibb.
SOURCE: Hagström H et al. Gastroenterology. 2019 Sep 26. doi: 10.1053/j.gastro.2019.09.008.
Currently available fibrosis scoring systems appear to have only a modest predictive ability for development of severe liver disease in the general population, according to authors of a large, retrospective cohort study.
Of five noninvasive scoring systems evaluated, all did have high negative predictive value in the general population, according to authors of the study, which included data on more than 800,000 individuals in Sweden. However, their sensitivities were low, with most of the individuals who developed severe liver disease over a 10-year follow-up period initially classified as being at low risk for advanced fibrosis, according to the study authors, led by Hannes Hagström, MD, PhD, of the division of hepatology, Karolinska University Hospital, Stockholm.
The scoring systems tended to perform better in patients at higher risk for nonalcoholic fatty liver disease (NAFLD) at baseline, suggesting the best use of the tools is in patients at increased risk or who have liver disease indications, Dr. Hagström and coauthors wrote in a report on the study.
“Although useful in populations with a high prevalence of advanced fibrosis, current scores lack precision for usage in the general population for which the prevalence of advanced fibrosis is much lower,” Dr. Hagström and colleagues said.
The scoring systems were derived from high-risk cohorts with liver diseases, the authors noted, stating that the disease prevalence in any given population will affect the performance of a test that’s intended to diagnose that specific disease.
“New and improved” scoring systems should be developed to more effectively pinpoint patients with NAFLD who are at higher risk of a severe liver event, they added in the report, which appears in Gastroenterology.
The population-based cohort study by Dr. Hagström and colleagues was based on data from 812,073 patients enrolled in the Swedish Apolipoprotein Mortality Risk (AMORIS) cohort between 1985 and 1996. Investigators said they excluded patients under 35 and over 79 years of age, patients with severe liver disease at baseline, and those with a prior diagnosis of alcohol or drug abuse.
Investigators used available data to calculate five scores, including the AST to Platelet Ratio Index (APRI); the body mass index, AST/ALT ratio, and diabetes (BARD) score; the Fibrosis-4 (FIB-4) score; Forns Index; and NAFLD Fibrosis Score (NFS).
At baseline, 0.5%-8.0% of patients were considered to be at high risk for advanced fibrosis, depending on the test used, investigators said. With up to 10 years of follow-up, the proportion of individuals who developed severe liver diseases (cirrhosis, liver failure, hepatocellular carcinoma, liver transplantation, or decompensated liver disease) was 0.3%-0.6%, and with the maximum 27 years of follow-up, the incidence ranged from 1.0% to 1.4%.
There was a “strong association” between baseline risk of fibrosis and development of severe liver diseases; however, the majority of cases occurred in patients deemed low risk at baseline, Dr. Hagström and colleagues noted in their report.
For example, 12.4% of individuals classified as high risk by APRI developed severe liver diseases over 10 years, compared to just 0.4% of the low-risk group, yet out of 723 cases, 502 (69%) occurred in the low-risk patients, the data show.
Hazard ratios did increase with risk level, and at the high-risk level, adjusted hazard ratios ranged from 1.7 (95% confidence interval [CI], 1.1-2.5) for the high-risk BARD patients to 45.9 (95% CI, 36.1-58.3) for the high-risk APRI patients, investigators reported.
Taken together, results of this study demonstrate that the performance of all scores was low in an unselected population, according to investigators.
Of all tests, APRI was least likely to falsely classify patients who never developed severe liver diseases and had an intermediate-risk group of 4%, the lowest of any test, which are findings that may have implications for routine primary care, according to investigators.
“APRI could be the currently best score to exclude a high risk of liver-related events in the near future, and thereby reduce unnecessary testing in a general population,” they said in a discussion of their results.
The study was supported by an independent grant from AstraZeneca. Dr. Hagström reported disclosures related to that company, as well as Novo Nordisk, Gilead Sciences, IQVIA, Intercept, and Bristol Myers-Squibb.
SOURCE: Hagström H et al. Gastroenterology. 2019 Sep 26. doi: 10.1053/j.gastro.2019.09.008.
FROM GASTROENTEROLOGY
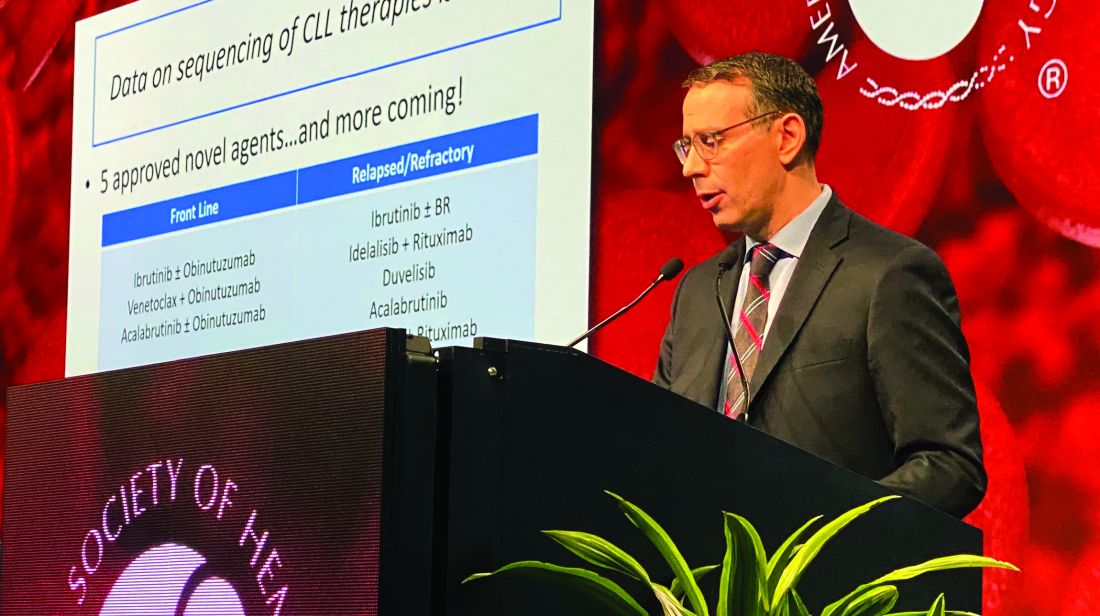
Efficacy of postvenetoclax therapy may depend on prior agent exposure in CLL
ORLANDO – For a patient with chronic lymphocytic leukemia (CLL) who has discontinued venetoclax, choosing the best next therapy may depend on what novel agents the patient was exposed to and why they discontinued them, according to Anthony R. Mato, MD, with the Center for CLL at Memorial Sloan Kettering Cancer Center in New York.
If the patient is Bruton tyrosine kinase (BTK) inhibitor naive, then use of a BTK inhibitor after venetoclax would be supported, Dr. Mato said, by the high overall response rates and durable remissions that he and his coinvestigators documented in a retrospective, multicenter study designed specifically to address the gap in knowledge regarding what to use after venetoclax.
If the patient is BTK inhibitor exposed, then the reason for discontinuation needs to be considered before going with that venetoclax-to-BTK inhibitor sequence, Dr. Mato said during an oral presentation at the annual meeting of the American Society of Hematology.
“In patients with resistance to a BTK inhibitor, the sequence was not supported – it did not appear to be effective,” he said. “However, in the setting of intolerance, an alternate BTK inhibitor could be considered.”
The study did not support a venetoclax-to-PI3K inhibitor sequence in PI3K-naive patients, he added, noting that remissions did not appear to be durable, suggesting a potential overlap in resistance mechanisms between agents.
All told, the most effective therapies for in the postvenetoclax setting included the use of a BTK inhibitor in BTK inhibitor–naive or previously responsive patients, and allogeneic transplant following double novel-agent exposure.
“These data may provide support for venetoclax’s earlier use in the course of CLL, and may guide clinical practice and aid in the design of future clinical trials to address sequencing of novel agents,” Dr. Mato told attendees.
While prospective and real-world data clearly show that venetoclax is active in ibrutinib- or idelalisib-exposed patients, data are conversely “variable and limited” with regard to outcomes for next therapies following venetoclax.
“Current data addressing this key sequencing question, I feel, is a major limitation in supporting the sequence of venetoclax to a BTK inhibitor,” Dr. Mato said.
Accordingly, Dr. Mato and colleagues at 31 centers internationally planned and conducted this study, which included data on 326 patients treated with venetoclax who then discontinued for any reason.
“I wanted to highlight that 50% of the sites for this trial were recruited by a single tweet,” said Dr. Mato, adding that he and his coauthors received no funding to conduct this study and volunteered their time to complete it.
They found that, in BTK inhibitor–naive patients who discontinued venetoclax, subsequent BTK inhibitor treatment was associated with a high overall response rate and durable remissions, with a median progression-free survival (PFS) of 32 months.
In BTK inhibitor–exposed patients, response to postvenetoclax BTK inhibitor treatment depended on the reason for discontinuation, with a favorable result (PFS not reached with a mean follow-up of 7.7 months) in patients who were intolerant of the prior BTK inhibitor. By contrast, median PFS was only about 4 months for patients who were resistant to the prior BTK inhibitor.
PI3K inhibitors did not produce durable remissions after venetoclax, with a median PFS also of just 4 months, Dr. Mato reported.
However, cellular therapies appeared to be effective after venetoclax. Allogeneic hematopoietic stem cell transplantation was particularly effective, with the median PFS not reached, while chimeric antigen receptor T-cell therapy produced a PFS of 9 months.
Dr. Mato emphasized that the results of the retrospective trial were “hypothesis generating” and noted that patients in the study had received a median of 3, and up to 11, prior therapies. “This population are probably not our patients receiving venetoclax in clinical practice. They’re more heavily pretreated.”
Dr. Mato reported disclosures related to Gilead, AstraZeneca, AbbVie, Sunesis, Johnson & Johnson, TG Therapeutics, Loxo Oncology, DTRM Biopharma, Genentech, Janssen, Acerta Pharma, Pharmacyclics, and Celgene.
SOURCE: Mato AR et al. ASH 2019, Abstract 502.
ORLANDO – For a patient with chronic lymphocytic leukemia (CLL) who has discontinued venetoclax, choosing the best next therapy may depend on what novel agents the patient was exposed to and why they discontinued them, according to Anthony R. Mato, MD, with the Center for CLL at Memorial Sloan Kettering Cancer Center in New York.
If the patient is Bruton tyrosine kinase (BTK) inhibitor naive, then use of a BTK inhibitor after venetoclax would be supported, Dr. Mato said, by the high overall response rates and durable remissions that he and his coinvestigators documented in a retrospective, multicenter study designed specifically to address the gap in knowledge regarding what to use after venetoclax.
If the patient is BTK inhibitor exposed, then the reason for discontinuation needs to be considered before going with that venetoclax-to-BTK inhibitor sequence, Dr. Mato said during an oral presentation at the annual meeting of the American Society of Hematology.
“In patients with resistance to a BTK inhibitor, the sequence was not supported – it did not appear to be effective,” he said. “However, in the setting of intolerance, an alternate BTK inhibitor could be considered.”
The study did not support a venetoclax-to-PI3K inhibitor sequence in PI3K-naive patients, he added, noting that remissions did not appear to be durable, suggesting a potential overlap in resistance mechanisms between agents.
All told, the most effective therapies for in the postvenetoclax setting included the use of a BTK inhibitor in BTK inhibitor–naive or previously responsive patients, and allogeneic transplant following double novel-agent exposure.
“These data may provide support for venetoclax’s earlier use in the course of CLL, and may guide clinical practice and aid in the design of future clinical trials to address sequencing of novel agents,” Dr. Mato told attendees.
While prospective and real-world data clearly show that venetoclax is active in ibrutinib- or idelalisib-exposed patients, data are conversely “variable and limited” with regard to outcomes for next therapies following venetoclax.
“Current data addressing this key sequencing question, I feel, is a major limitation in supporting the sequence of venetoclax to a BTK inhibitor,” Dr. Mato said.
Accordingly, Dr. Mato and colleagues at 31 centers internationally planned and conducted this study, which included data on 326 patients treated with venetoclax who then discontinued for any reason.
“I wanted to highlight that 50% of the sites for this trial were recruited by a single tweet,” said Dr. Mato, adding that he and his coauthors received no funding to conduct this study and volunteered their time to complete it.
They found that, in BTK inhibitor–naive patients who discontinued venetoclax, subsequent BTK inhibitor treatment was associated with a high overall response rate and durable remissions, with a median progression-free survival (PFS) of 32 months.
In BTK inhibitor–exposed patients, response to postvenetoclax BTK inhibitor treatment depended on the reason for discontinuation, with a favorable result (PFS not reached with a mean follow-up of 7.7 months) in patients who were intolerant of the prior BTK inhibitor. By contrast, median PFS was only about 4 months for patients who were resistant to the prior BTK inhibitor.
PI3K inhibitors did not produce durable remissions after venetoclax, with a median PFS also of just 4 months, Dr. Mato reported.
However, cellular therapies appeared to be effective after venetoclax. Allogeneic hematopoietic stem cell transplantation was particularly effective, with the median PFS not reached, while chimeric antigen receptor T-cell therapy produced a PFS of 9 months.
Dr. Mato emphasized that the results of the retrospective trial were “hypothesis generating” and noted that patients in the study had received a median of 3, and up to 11, prior therapies. “This population are probably not our patients receiving venetoclax in clinical practice. They’re more heavily pretreated.”
Dr. Mato reported disclosures related to Gilead, AstraZeneca, AbbVie, Sunesis, Johnson & Johnson, TG Therapeutics, Loxo Oncology, DTRM Biopharma, Genentech, Janssen, Acerta Pharma, Pharmacyclics, and Celgene.
SOURCE: Mato AR et al. ASH 2019, Abstract 502.
ORLANDO – For a patient with chronic lymphocytic leukemia (CLL) who has discontinued venetoclax, choosing the best next therapy may depend on what novel agents the patient was exposed to and why they discontinued them, according to Anthony R. Mato, MD, with the Center for CLL at Memorial Sloan Kettering Cancer Center in New York.
If the patient is Bruton tyrosine kinase (BTK) inhibitor naive, then use of a BTK inhibitor after venetoclax would be supported, Dr. Mato said, by the high overall response rates and durable remissions that he and his coinvestigators documented in a retrospective, multicenter study designed specifically to address the gap in knowledge regarding what to use after venetoclax.
If the patient is BTK inhibitor exposed, then the reason for discontinuation needs to be considered before going with that venetoclax-to-BTK inhibitor sequence, Dr. Mato said during an oral presentation at the annual meeting of the American Society of Hematology.
“In patients with resistance to a BTK inhibitor, the sequence was not supported – it did not appear to be effective,” he said. “However, in the setting of intolerance, an alternate BTK inhibitor could be considered.”
The study did not support a venetoclax-to-PI3K inhibitor sequence in PI3K-naive patients, he added, noting that remissions did not appear to be durable, suggesting a potential overlap in resistance mechanisms between agents.
All told, the most effective therapies for in the postvenetoclax setting included the use of a BTK inhibitor in BTK inhibitor–naive or previously responsive patients, and allogeneic transplant following double novel-agent exposure.
“These data may provide support for venetoclax’s earlier use in the course of CLL, and may guide clinical practice and aid in the design of future clinical trials to address sequencing of novel agents,” Dr. Mato told attendees.
While prospective and real-world data clearly show that venetoclax is active in ibrutinib- or idelalisib-exposed patients, data are conversely “variable and limited” with regard to outcomes for next therapies following venetoclax.
“Current data addressing this key sequencing question, I feel, is a major limitation in supporting the sequence of venetoclax to a BTK inhibitor,” Dr. Mato said.
Accordingly, Dr. Mato and colleagues at 31 centers internationally planned and conducted this study, which included data on 326 patients treated with venetoclax who then discontinued for any reason.
“I wanted to highlight that 50% of the sites for this trial were recruited by a single tweet,” said Dr. Mato, adding that he and his coauthors received no funding to conduct this study and volunteered their time to complete it.
They found that, in BTK inhibitor–naive patients who discontinued venetoclax, subsequent BTK inhibitor treatment was associated with a high overall response rate and durable remissions, with a median progression-free survival (PFS) of 32 months.
In BTK inhibitor–exposed patients, response to postvenetoclax BTK inhibitor treatment depended on the reason for discontinuation, with a favorable result (PFS not reached with a mean follow-up of 7.7 months) in patients who were intolerant of the prior BTK inhibitor. By contrast, median PFS was only about 4 months for patients who were resistant to the prior BTK inhibitor.
PI3K inhibitors did not produce durable remissions after venetoclax, with a median PFS also of just 4 months, Dr. Mato reported.
However, cellular therapies appeared to be effective after venetoclax. Allogeneic hematopoietic stem cell transplantation was particularly effective, with the median PFS not reached, while chimeric antigen receptor T-cell therapy produced a PFS of 9 months.
Dr. Mato emphasized that the results of the retrospective trial were “hypothesis generating” and noted that patients in the study had received a median of 3, and up to 11, prior therapies. “This population are probably not our patients receiving venetoclax in clinical practice. They’re more heavily pretreated.”
Dr. Mato reported disclosures related to Gilead, AstraZeneca, AbbVie, Sunesis, Johnson & Johnson, TG Therapeutics, Loxo Oncology, DTRM Biopharma, Genentech, Janssen, Acerta Pharma, Pharmacyclics, and Celgene.
SOURCE: Mato AR et al. ASH 2019, Abstract 502.
REPORTING FROM ASH 2019
Fragmentation of sickle cell disease care starts in young adulthood
ORLANDO – While over time, results of a retrospective study suggest.
Nearly 60% of children between aged10-17 years were seen at just one facility over the course of 7 years in the analysis, which was based on analysis of data for nearly 7,000 patients seen in California during 1991-2016.
That contrasted sharply with young adults, aged 18-25 years, only about 20% of whom were admitted to one facility, said senior study author Anjlee Mahajan, MD, of the University of California, Davis, adding that another 20% were seen at five or more centers over a 7-year follow-up period.
Fragmentation of care didn’t increase the risk of death in this study, as investigators hypothesized it might. However, the outcomes and the quality of care among young adults with SCD who received inpatient care at multiple facilities nevertheless was likely to be affected, Dr. Mahajan said at the annual meeting of the American Society of Hematology.
“Imagine what that would be like to have a chronic, debilitating illness and to have to go to multiple different hospitals, during this vulnerable time period in your life, and being seen by different care providers who may not know you and may not have all of your records as well,” she said in a press conference at the meeting.
Providers and the health care system need to work harder to ensure young adults receive comprehensive and coordinated care, especially at a time when therapeutic advances are improving the treatment of this disease, according to the investigator.
“When you’re seen at one center, you can have a specific pain plan, and maybe when you are going into the emergency room and being admitted, your sickle cell care provider might come and visit you in the hospital or at least be in contact with your team,” Dr. Mahajan said in an interview. “That may not happen if you’re going to be seen at five different hospitals in 7 years.”
Encouraging the concept of “medical home” for SCD may be help ease transition from pediatric to adult care, thereby reducing fragmentation of care for young adults, according to Julie A. Panepinto, MD, professor of pediatric hematology and the director of the center for clinical effectiveness research at the Children’s Research Institute, Medical College of Wisconsin, Milwaukee.
“That 18- to 30-year-old age group historically and repeatedly over time is shown to be the age that relies on the emergency department and that has a higher mortality as they transition,” Dr. Panepinto said in an interview. “So ideally, you would have a pediatric program that’s comprehensive and that can transition an adult patient to a very similar setting with knowledgeable providers in SCD across the spectrum, from the emergency department to the hospital to the outpatient clinic.”
Dr. Mahajan reported no disclosures related to her group’s study. Coauthors provided disclosures related to Pfizer and Janssen.
SOURCE: Shatola A et al. ASH 2019. Abstract 4667.
ORLANDO – While over time, results of a retrospective study suggest.
Nearly 60% of children between aged10-17 years were seen at just one facility over the course of 7 years in the analysis, which was based on analysis of data for nearly 7,000 patients seen in California during 1991-2016.
That contrasted sharply with young adults, aged 18-25 years, only about 20% of whom were admitted to one facility, said senior study author Anjlee Mahajan, MD, of the University of California, Davis, adding that another 20% were seen at five or more centers over a 7-year follow-up period.
Fragmentation of care didn’t increase the risk of death in this study, as investigators hypothesized it might. However, the outcomes and the quality of care among young adults with SCD who received inpatient care at multiple facilities nevertheless was likely to be affected, Dr. Mahajan said at the annual meeting of the American Society of Hematology.
“Imagine what that would be like to have a chronic, debilitating illness and to have to go to multiple different hospitals, during this vulnerable time period in your life, and being seen by different care providers who may not know you and may not have all of your records as well,” she said in a press conference at the meeting.
Providers and the health care system need to work harder to ensure young adults receive comprehensive and coordinated care, especially at a time when therapeutic advances are improving the treatment of this disease, according to the investigator.
“When you’re seen at one center, you can have a specific pain plan, and maybe when you are going into the emergency room and being admitted, your sickle cell care provider might come and visit you in the hospital or at least be in contact with your team,” Dr. Mahajan said in an interview. “That may not happen if you’re going to be seen at five different hospitals in 7 years.”
Encouraging the concept of “medical home” for SCD may be help ease transition from pediatric to adult care, thereby reducing fragmentation of care for young adults, according to Julie A. Panepinto, MD, professor of pediatric hematology and the director of the center for clinical effectiveness research at the Children’s Research Institute, Medical College of Wisconsin, Milwaukee.
“That 18- to 30-year-old age group historically and repeatedly over time is shown to be the age that relies on the emergency department and that has a higher mortality as they transition,” Dr. Panepinto said in an interview. “So ideally, you would have a pediatric program that’s comprehensive and that can transition an adult patient to a very similar setting with knowledgeable providers in SCD across the spectrum, from the emergency department to the hospital to the outpatient clinic.”
Dr. Mahajan reported no disclosures related to her group’s study. Coauthors provided disclosures related to Pfizer and Janssen.
SOURCE: Shatola A et al. ASH 2019. Abstract 4667.
ORLANDO – While over time, results of a retrospective study suggest.
Nearly 60% of children between aged10-17 years were seen at just one facility over the course of 7 years in the analysis, which was based on analysis of data for nearly 7,000 patients seen in California during 1991-2016.
That contrasted sharply with young adults, aged 18-25 years, only about 20% of whom were admitted to one facility, said senior study author Anjlee Mahajan, MD, of the University of California, Davis, adding that another 20% were seen at five or more centers over a 7-year follow-up period.
Fragmentation of care didn’t increase the risk of death in this study, as investigators hypothesized it might. However, the outcomes and the quality of care among young adults with SCD who received inpatient care at multiple facilities nevertheless was likely to be affected, Dr. Mahajan said at the annual meeting of the American Society of Hematology.
“Imagine what that would be like to have a chronic, debilitating illness and to have to go to multiple different hospitals, during this vulnerable time period in your life, and being seen by different care providers who may not know you and may not have all of your records as well,” she said in a press conference at the meeting.
Providers and the health care system need to work harder to ensure young adults receive comprehensive and coordinated care, especially at a time when therapeutic advances are improving the treatment of this disease, according to the investigator.
“When you’re seen at one center, you can have a specific pain plan, and maybe when you are going into the emergency room and being admitted, your sickle cell care provider might come and visit you in the hospital or at least be in contact with your team,” Dr. Mahajan said in an interview. “That may not happen if you’re going to be seen at five different hospitals in 7 years.”
Encouraging the concept of “medical home” for SCD may be help ease transition from pediatric to adult care, thereby reducing fragmentation of care for young adults, according to Julie A. Panepinto, MD, professor of pediatric hematology and the director of the center for clinical effectiveness research at the Children’s Research Institute, Medical College of Wisconsin, Milwaukee.
“That 18- to 30-year-old age group historically and repeatedly over time is shown to be the age that relies on the emergency department and that has a higher mortality as they transition,” Dr. Panepinto said in an interview. “So ideally, you would have a pediatric program that’s comprehensive and that can transition an adult patient to a very similar setting with knowledgeable providers in SCD across the spectrum, from the emergency department to the hospital to the outpatient clinic.”
Dr. Mahajan reported no disclosures related to her group’s study. Coauthors provided disclosures related to Pfizer and Janssen.
SOURCE: Shatola A et al. ASH 2019. Abstract 4667.
REPORTING FROM ASH 2019
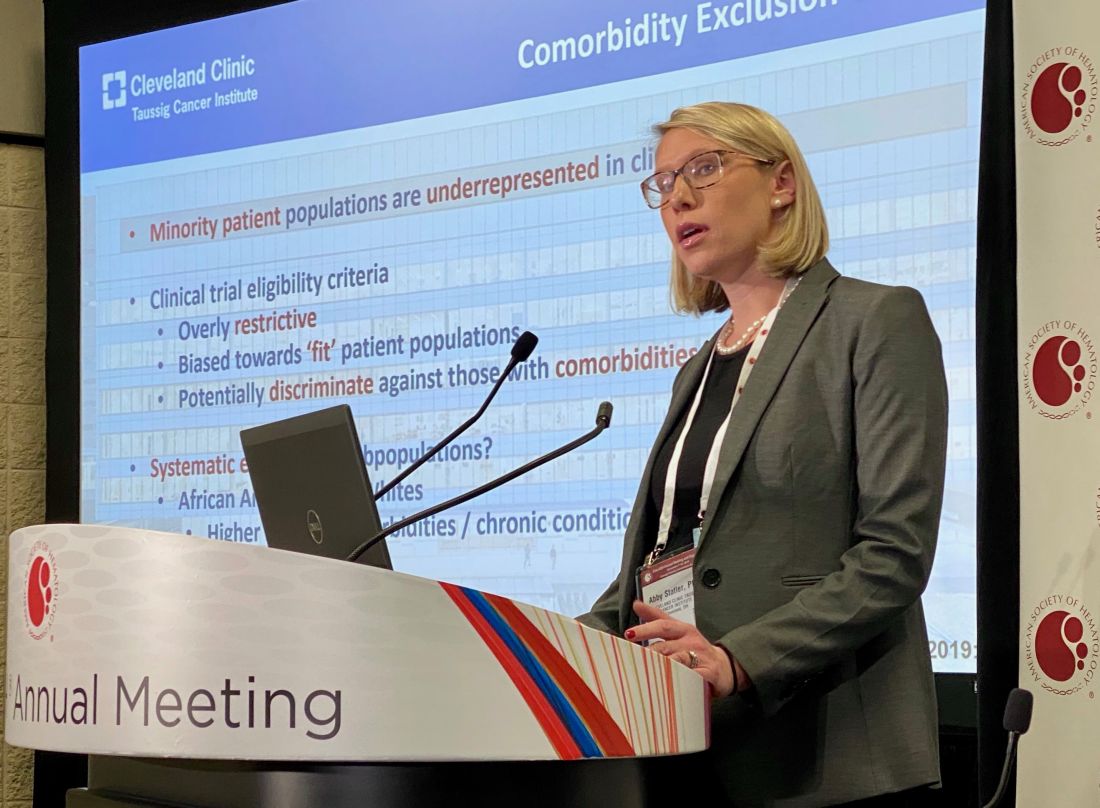
Kidney function in African American AML patients not linked to reduced survival compared with whites
ORLANDO – While African Americans with acute myeloid leukemia were more likely to have evidence of abnormal kidney function, the excess of this comorbidity didn’t affect overall survival, compared with whites, according to a study of more than 1,000 patients.
A total of 63% of African Americans with acute myeloid leukemia (AML) presented with a renal function abnormality that could have excluded them from a clinical trial, compared with 56% in the overall cohort; however, analysis of outcomes data suggested that renal function abnormalities were not associated with decreased survival in African Americans versus whites, said Abby Statler, PhD, MPH, of the Cleveland Clinic.
The findings may have implications for the design of clinical trials that might exclude patients on the basis of comorbidities that don’t actually affect survival, according to Dr. Statler.
“If we’re able to liberalize renal function eligibility criteria ... this may reduce racial disparities in clinical trial enrollment, which might be a major step in improving the diversity of cancer patient populations,” Dr. Statler said in a press conference at the annual meeting of the American Society of Hematology.
Overly restrictive criteria could be a significant barrier to clinical trial enrollment among minority patient populations, according to Dr. Statler.
Eligibility criteria are generally biased toward “fit” patient populations, which means they may discriminate against less-fit groups, such as African Americans who, compared with whites, have higher rates of comorbidities and report poorer overall health, according to Dr. Statler.
Laura Michaelis, MD, who chaired the press conference, said these findings suggest current clinical trial designs may be “too restrictive.”
“Once it’s published and validated, [these] data should definitely make us think twice about when you limit a patient’s enrollment in a trial,” Dr. Michaelis said in an interview.
Restrictive eligibility criteria may not only limit access to minority populations, but also may slow clinical trial accrual and completion, and make it harder to generalize clinical trial findings to the overall population, said Dr. Michaelis, associate professor of medicine in the division of hematology and oncology, Medical College of Wisconsin, Milwaukee.
The study by Dr. Statler and colleagues included 1,040 AML patients who received chemotherapy at Cleveland Clinic between 2003 and 2019. About 10% of the patients in the analysis were African American and 90% were white.
Median overall survival was not significantly different by race, at 13.7 months for African Americans and 14.9 months for whites (P = 0.89), according to results published in the study abstract.
Mild creatinine elevation did not appear to affect survival in this study, according to the investigator. Survival was not significantly different between patients with normal creatinine and those with creatinine up to 1.5 times the upper limit of normal. However, higher levels of creatinine were significantly associated with worse survival, Dr. Statler said.
Further analyses showed that these survival findings by creatinine level held up specifically in the African American subgroup as well, Dr. Statler said in the press conference.
Dr. Statler provided no disclosures related to the presentation. Study coauthors described disclosures related to Amgen, SimulStat, Bristol-Myers Squibb, Takeda, Pfizer, Novartis, Celgene Corporation, Abbvie, and Incyte, among others.
SOURCE: Statler A et al. ASH 2019, Abstract 381.
ORLANDO – While African Americans with acute myeloid leukemia were more likely to have evidence of abnormal kidney function, the excess of this comorbidity didn’t affect overall survival, compared with whites, according to a study of more than 1,000 patients.
A total of 63% of African Americans with acute myeloid leukemia (AML) presented with a renal function abnormality that could have excluded them from a clinical trial, compared with 56% in the overall cohort; however, analysis of outcomes data suggested that renal function abnormalities were not associated with decreased survival in African Americans versus whites, said Abby Statler, PhD, MPH, of the Cleveland Clinic.
The findings may have implications for the design of clinical trials that might exclude patients on the basis of comorbidities that don’t actually affect survival, according to Dr. Statler.
“If we’re able to liberalize renal function eligibility criteria ... this may reduce racial disparities in clinical trial enrollment, which might be a major step in improving the diversity of cancer patient populations,” Dr. Statler said in a press conference at the annual meeting of the American Society of Hematology.
Overly restrictive criteria could be a significant barrier to clinical trial enrollment among minority patient populations, according to Dr. Statler.
Eligibility criteria are generally biased toward “fit” patient populations, which means they may discriminate against less-fit groups, such as African Americans who, compared with whites, have higher rates of comorbidities and report poorer overall health, according to Dr. Statler.
Laura Michaelis, MD, who chaired the press conference, said these findings suggest current clinical trial designs may be “too restrictive.”
“Once it’s published and validated, [these] data should definitely make us think twice about when you limit a patient’s enrollment in a trial,” Dr. Michaelis said in an interview.
Restrictive eligibility criteria may not only limit access to minority populations, but also may slow clinical trial accrual and completion, and make it harder to generalize clinical trial findings to the overall population, said Dr. Michaelis, associate professor of medicine in the division of hematology and oncology, Medical College of Wisconsin, Milwaukee.
The study by Dr. Statler and colleagues included 1,040 AML patients who received chemotherapy at Cleveland Clinic between 2003 and 2019. About 10% of the patients in the analysis were African American and 90% were white.
Median overall survival was not significantly different by race, at 13.7 months for African Americans and 14.9 months for whites (P = 0.89), according to results published in the study abstract.
Mild creatinine elevation did not appear to affect survival in this study, according to the investigator. Survival was not significantly different between patients with normal creatinine and those with creatinine up to 1.5 times the upper limit of normal. However, higher levels of creatinine were significantly associated with worse survival, Dr. Statler said.
Further analyses showed that these survival findings by creatinine level held up specifically in the African American subgroup as well, Dr. Statler said in the press conference.
Dr. Statler provided no disclosures related to the presentation. Study coauthors described disclosures related to Amgen, SimulStat, Bristol-Myers Squibb, Takeda, Pfizer, Novartis, Celgene Corporation, Abbvie, and Incyte, among others.
SOURCE: Statler A et al. ASH 2019, Abstract 381.
ORLANDO – While African Americans with acute myeloid leukemia were more likely to have evidence of abnormal kidney function, the excess of this comorbidity didn’t affect overall survival, compared with whites, according to a study of more than 1,000 patients.
A total of 63% of African Americans with acute myeloid leukemia (AML) presented with a renal function abnormality that could have excluded them from a clinical trial, compared with 56% in the overall cohort; however, analysis of outcomes data suggested that renal function abnormalities were not associated with decreased survival in African Americans versus whites, said Abby Statler, PhD, MPH, of the Cleveland Clinic.
The findings may have implications for the design of clinical trials that might exclude patients on the basis of comorbidities that don’t actually affect survival, according to Dr. Statler.
“If we’re able to liberalize renal function eligibility criteria ... this may reduce racial disparities in clinical trial enrollment, which might be a major step in improving the diversity of cancer patient populations,” Dr. Statler said in a press conference at the annual meeting of the American Society of Hematology.
Overly restrictive criteria could be a significant barrier to clinical trial enrollment among minority patient populations, according to Dr. Statler.
Eligibility criteria are generally biased toward “fit” patient populations, which means they may discriminate against less-fit groups, such as African Americans who, compared with whites, have higher rates of comorbidities and report poorer overall health, according to Dr. Statler.
Laura Michaelis, MD, who chaired the press conference, said these findings suggest current clinical trial designs may be “too restrictive.”
“Once it’s published and validated, [these] data should definitely make us think twice about when you limit a patient’s enrollment in a trial,” Dr. Michaelis said in an interview.
Restrictive eligibility criteria may not only limit access to minority populations, but also may slow clinical trial accrual and completion, and make it harder to generalize clinical trial findings to the overall population, said Dr. Michaelis, associate professor of medicine in the division of hematology and oncology, Medical College of Wisconsin, Milwaukee.
The study by Dr. Statler and colleagues included 1,040 AML patients who received chemotherapy at Cleveland Clinic between 2003 and 2019. About 10% of the patients in the analysis were African American and 90% were white.
Median overall survival was not significantly different by race, at 13.7 months for African Americans and 14.9 months for whites (P = 0.89), according to results published in the study abstract.
Mild creatinine elevation did not appear to affect survival in this study, according to the investigator. Survival was not significantly different between patients with normal creatinine and those with creatinine up to 1.5 times the upper limit of normal. However, higher levels of creatinine were significantly associated with worse survival, Dr. Statler said.
Further analyses showed that these survival findings by creatinine level held up specifically in the African American subgroup as well, Dr. Statler said in the press conference.
Dr. Statler provided no disclosures related to the presentation. Study coauthors described disclosures related to Amgen, SimulStat, Bristol-Myers Squibb, Takeda, Pfizer, Novartis, Celgene Corporation, Abbvie, and Incyte, among others.
SOURCE: Statler A et al. ASH 2019, Abstract 381.
REPORTING FROM ASH 2019
Bispecific CAR T-cells yield high response rate in relapsed/refractory myeloma
ORLANDO – A dual-targeted chimeric antigen receptor (CAR) T-cell therapy has demonstrated a high overall response rate, a long response duration, and manageable safety in patients with relapsed or refractory multiple myeloma, according to an investigator in a phase 1 study.
The overall response rate exceeded 90%, and about three-quarters of patients remained progression-free at 9 months after treatment with the CAR T-cell therapy, which targets both B-cell maturation antigen (BCMA) and CD38, the study investigator reported.
Grade 3 or greater cytokine release syndrome (CRS) occurred in about one-quarter of the patients, and no neurotoxicity was observed, according to investigator Yu Hu, MD, of Tongji Medical College in Hubei, China.
“,” Dr. Hu said in a press conference.
Short-term relapse has been a “major challenge” with current CAR T-cell therapies currently under investigation for myeloma, most of which target BCMA, according to Dr. Hu.
He said the bispecific CAR T-cell therapy under investigation, known as BM38, was designed to target antigen loss and increase persistence of effector cells. According to the investigator, this was the first study to focus on an anti-BCMA and CD38 dual-targeted CAR T-cell therapy for patients with relapsed or refractory multiple myeloma.
Gary J. Schiller, MD, of UCLA Health, who moderated the press conference, said that while dual-targeting is a potentially “attractive” approach in these hard-to-treat patients, further follow-up is needed to see duration of response and to see if antigen escape re-emerges.
“Cellular therapy is costly, in terms of toxicity as well as financial costs, so you would like to see what the durability of responses is before engaging in that as a late-stage therapy, not to mention moving it up front,” Dr. Schiller said in an interview.
The median progression-free survival (PFS) duration had not been reached at the time of this report, though the 9-month PFS rate was 78.87%, according to the data presented by Dr. Hu.
In the phase 1 study, 22 patients received BM38 CAR T-cell infusions following a fludarabine and cyclophosphamide preconditioning regimen. The median patient age was 59 years, and 50% were male. Nearly three-quarters (72%) had a cytogenetic abnormality, and the median number of prior therapies approached four (range, two to nine prior therapies).
Twenty of the patients (90.9%) had a response: 12 who achieved stringent complete remission, 2 with very good partial response, 5 with partial responses, and 1 with a minimal response.
Of 9 patients with extramedullary disease, 8 achieved partial or complete elimination of tumors, Dr. Hu said in his presentation.
Cytokine release syndrome occurred in 20 patients (90.91%), 5 of whom experienced severe cases (22.73%), according to the reported data. There was no observed neurotoxicity, according to the report, while almost all had hematologic toxicities. Three experienced hepatotoxicity and one had nephrotoxicity, according to Dr. Hu.
The phase 1 study was supported by the National Natural Science Foundation of China, the Major Technological Innovation Special Project Fund of Hubei Province of China, and Cellyan Therapeutics. The senior author of the study was affiliated with Cellyan Therapeutics. Dr. Hu and coauthors reported that they had no relevant conflicts of interest to declare.
SOURCE: Li C et al. ASH 2019. Abstract 930.
ORLANDO – A dual-targeted chimeric antigen receptor (CAR) T-cell therapy has demonstrated a high overall response rate, a long response duration, and manageable safety in patients with relapsed or refractory multiple myeloma, according to an investigator in a phase 1 study.
The overall response rate exceeded 90%, and about three-quarters of patients remained progression-free at 9 months after treatment with the CAR T-cell therapy, which targets both B-cell maturation antigen (BCMA) and CD38, the study investigator reported.
Grade 3 or greater cytokine release syndrome (CRS) occurred in about one-quarter of the patients, and no neurotoxicity was observed, according to investigator Yu Hu, MD, of Tongji Medical College in Hubei, China.
“,” Dr. Hu said in a press conference.
Short-term relapse has been a “major challenge” with current CAR T-cell therapies currently under investigation for myeloma, most of which target BCMA, according to Dr. Hu.
He said the bispecific CAR T-cell therapy under investigation, known as BM38, was designed to target antigen loss and increase persistence of effector cells. According to the investigator, this was the first study to focus on an anti-BCMA and CD38 dual-targeted CAR T-cell therapy for patients with relapsed or refractory multiple myeloma.
Gary J. Schiller, MD, of UCLA Health, who moderated the press conference, said that while dual-targeting is a potentially “attractive” approach in these hard-to-treat patients, further follow-up is needed to see duration of response and to see if antigen escape re-emerges.
“Cellular therapy is costly, in terms of toxicity as well as financial costs, so you would like to see what the durability of responses is before engaging in that as a late-stage therapy, not to mention moving it up front,” Dr. Schiller said in an interview.
The median progression-free survival (PFS) duration had not been reached at the time of this report, though the 9-month PFS rate was 78.87%, according to the data presented by Dr. Hu.
In the phase 1 study, 22 patients received BM38 CAR T-cell infusions following a fludarabine and cyclophosphamide preconditioning regimen. The median patient age was 59 years, and 50% were male. Nearly three-quarters (72%) had a cytogenetic abnormality, and the median number of prior therapies approached four (range, two to nine prior therapies).
Twenty of the patients (90.9%) had a response: 12 who achieved stringent complete remission, 2 with very good partial response, 5 with partial responses, and 1 with a minimal response.
Of 9 patients with extramedullary disease, 8 achieved partial or complete elimination of tumors, Dr. Hu said in his presentation.
Cytokine release syndrome occurred in 20 patients (90.91%), 5 of whom experienced severe cases (22.73%), according to the reported data. There was no observed neurotoxicity, according to the report, while almost all had hematologic toxicities. Three experienced hepatotoxicity and one had nephrotoxicity, according to Dr. Hu.
The phase 1 study was supported by the National Natural Science Foundation of China, the Major Technological Innovation Special Project Fund of Hubei Province of China, and Cellyan Therapeutics. The senior author of the study was affiliated with Cellyan Therapeutics. Dr. Hu and coauthors reported that they had no relevant conflicts of interest to declare.
SOURCE: Li C et al. ASH 2019. Abstract 930.
ORLANDO – A dual-targeted chimeric antigen receptor (CAR) T-cell therapy has demonstrated a high overall response rate, a long response duration, and manageable safety in patients with relapsed or refractory multiple myeloma, according to an investigator in a phase 1 study.
The overall response rate exceeded 90%, and about three-quarters of patients remained progression-free at 9 months after treatment with the CAR T-cell therapy, which targets both B-cell maturation antigen (BCMA) and CD38, the study investigator reported.
Grade 3 or greater cytokine release syndrome (CRS) occurred in about one-quarter of the patients, and no neurotoxicity was observed, according to investigator Yu Hu, MD, of Tongji Medical College in Hubei, China.
“,” Dr. Hu said in a press conference.
Short-term relapse has been a “major challenge” with current CAR T-cell therapies currently under investigation for myeloma, most of which target BCMA, according to Dr. Hu.
He said the bispecific CAR T-cell therapy under investigation, known as BM38, was designed to target antigen loss and increase persistence of effector cells. According to the investigator, this was the first study to focus on an anti-BCMA and CD38 dual-targeted CAR T-cell therapy for patients with relapsed or refractory multiple myeloma.
Gary J. Schiller, MD, of UCLA Health, who moderated the press conference, said that while dual-targeting is a potentially “attractive” approach in these hard-to-treat patients, further follow-up is needed to see duration of response and to see if antigen escape re-emerges.
“Cellular therapy is costly, in terms of toxicity as well as financial costs, so you would like to see what the durability of responses is before engaging in that as a late-stage therapy, not to mention moving it up front,” Dr. Schiller said in an interview.
The median progression-free survival (PFS) duration had not been reached at the time of this report, though the 9-month PFS rate was 78.87%, according to the data presented by Dr. Hu.
In the phase 1 study, 22 patients received BM38 CAR T-cell infusions following a fludarabine and cyclophosphamide preconditioning regimen. The median patient age was 59 years, and 50% were male. Nearly three-quarters (72%) had a cytogenetic abnormality, and the median number of prior therapies approached four (range, two to nine prior therapies).
Twenty of the patients (90.9%) had a response: 12 who achieved stringent complete remission, 2 with very good partial response, 5 with partial responses, and 1 with a minimal response.
Of 9 patients with extramedullary disease, 8 achieved partial or complete elimination of tumors, Dr. Hu said in his presentation.
Cytokine release syndrome occurred in 20 patients (90.91%), 5 of whom experienced severe cases (22.73%), according to the reported data. There was no observed neurotoxicity, according to the report, while almost all had hematologic toxicities. Three experienced hepatotoxicity and one had nephrotoxicity, according to Dr. Hu.
The phase 1 study was supported by the National Natural Science Foundation of China, the Major Technological Innovation Special Project Fund of Hubei Province of China, and Cellyan Therapeutics. The senior author of the study was affiliated with Cellyan Therapeutics. Dr. Hu and coauthors reported that they had no relevant conflicts of interest to declare.
SOURCE: Li C et al. ASH 2019. Abstract 930.
REPORTING FROM ASH 2019
UC: Tofacitinib tied to modest, reversible lipid increases, infrequent CV events
according to results of an analysis including more than 1,000 patients.
Major adverse cardiac events (MACE) were “infrequent” following treatment, according to the authors of the analysis, with an incidence rate similar to what has been reported for tofacitinib in rheumatoid arthritis and for other agents in ulcerative colitis.
That said, the period of observation in the analysis is “relatively short,” and so may not provide an accurate risk estimate for MACE, noted the investigators, led by Bruce E. Sands, MD, of the division of gastroenterology at the Icahn School of Medicine at Mount Sinai, New York.
“Longer-term studies, involving a larger number of patients, will be needed to further assess MACE risk in patients with ulcerative colitis,” Dr. Sands and coinvestigators wrote in their report on the observational analysis, which appears in Clinical Gastroenterology and Hepatology.
“It is noteworthy that no increase in MACE risk and no dose relationship with tofacitinib have been observed in a larger rheumatoid arthritis cohort with over 8.5 years of observation and more than 19,000 patient-years of collective exposure,” they continued.
The present analysis included 1,157 patients with ulcerative colitis who participated in 8-week phase 2 and 3 tofacitinib induction studies, a phase 3 maintenance study, and a long-term extension study that is ongoing.
Reversible and dose-dependent increases in both LDL cholesterol and HDL cholesterol were observed after 8 weeks of treatment with tofacitinib at the recommended induction dose of 10 mg twice daily, the investigators found.
Increases in LDL cholesterol, HDL cholesterol, and total cholesterol correlated with decreases in high-sensitivity C-reactive protein, suggesting any potential impact of lipid increases on cardiovascular events might be offset by reduced inflammation, according to the investigators.
“Previous studies in RA and inflammatory bowel disease have shown an inverse relationship between active inflammation and serum lipid profiles, suggesting that inflammation lowers lipid concentrations, and that treatment of the underlying inflammatory disease may, therefore, increase them,” Dr. Sands and colleagues wrote.
The lipid changes also correlated with increases in body mass index, possibly because of better nutrition, reduced protein loss, and less catabolism following tofacitinib treatment, along with the corticosteroid taper required in these studies of the drug, they added.
Lipid increases generally stayed elevated through 61 weeks of treatment, while in patients randomized to placebo after 8 weeks of tofacitinib treatment, lipid levels fell back toward baseline, which suggests a reversal of the increases after tofacitinib withdrawal, the investigators wrote.
A total of 4 MACEs were seen among the 1,157 patients in the analysis, for an incidence rate of 0.24 (95% confidence interval, 0.07-0.62), according to the report. Those events included an acute coronary syndrome, an MI, an aortic dissection, and a hemorrhagic stroke. All four occurred in tofacitinib-treated patients, though the investigators noted that the aortic dissection and hemorrhagic stroke are events typically associated with genetics or other nonlipid factors.
In any case, that MACE incidence rate was “similar” to infliximab (Remicade) for what has been observed in tumor necrosis factor antagonist treatment of ulcerative colitis within a U.S. claims database study. In that analysis, including patients treated with infliximab, golimumab, and adalimumab, the incidence rate was 0.51 (95% CI, 0.31-0.79), the investigators noted.
These findings, taken together, support recommendations in tofacitinib prescribing information that call for monitoring of lipid concentrations 4-8 weeks after treatment is started, according to Dr. Sands and coauthors.
Funding for the study came from Pfizer. The study authors disclosed potential conflicts of interest related to Pfizer, AbbVie, Amgen, Bristol-Myers Squibb, Celgene, Janssen, MedImmune (AstraZeneca), Millennium Pharmaceuticals, Prometheus Laboratories, Takeda, and 4D Pharma, among others.
SOURCE: Sands BE et al. Clin Gastroenterol Hepatol. 2019 May 8. doi: 10.1016/j.cgh.2019.04.059.
Tofacitinib has several well-described effects on lipid metabolism, increasing levels of LDL cholesterol, HDL cholesterol, and total cholesterol. The clinical consequences of these lipid changes remains uncertain in ulcerative colitis (UC), for which there may be an increased risk of cardiovascular events.
In this study, Sands and colleagues used the largest cohort to date to quantify the effect of tofacitinib-associated lipid profile changes, their association with inflammatory markers, and the risk of major adverse cardiovascular events (MACEs). Using pooled data from multiple controlled, open-label studies of tofacitinib in UC, the authors appreciated a significant association between the rise in HDL cholesterol, LDL cholesterol, and total cholesterol levels and declines in C-reactive protein. They noted only four MACEs, an incidence rate similar to that seen in prior anti–tumor necrosis factor trials, and no change in a commonly used risk score for cardiovascular events.
These results are an important initial step in quantifying the cardiovascular risk associated with tofacitinib, but should be interpreted with caution. A significant proportion of individuals evaluated were from induction studies, with only 8 weeks of exposure. Only one dose of tofacitinib was required for inclusion. The median age in the OCTAVE trials, which contributed the majority of the data for this cohort, was only 41 years, and the baseline cardiovascular risk was low. While these data and rheumatologic literature are reassuring, further research with longitudinal follow-up, the assessment of time-varying exposures, and stratification by baseline cardiovascular risk will be required to better understand the association between tofacitinib and MACEs.
Frank I. Scott, MD, MSCE, assistant professor of medicine, Crohn’s and Colitis Center, codirector of clinical research/DART, director of GI fellowship research, division of gastroenterology and hepatology, University of Colorado at Denver, Aurora. He has received research funding and consulting fees from Takeda, and Janssen, and consulting fees from Merck.
Tofacitinib has several well-described effects on lipid metabolism, increasing levels of LDL cholesterol, HDL cholesterol, and total cholesterol. The clinical consequences of these lipid changes remains uncertain in ulcerative colitis (UC), for which there may be an increased risk of cardiovascular events.
In this study, Sands and colleagues used the largest cohort to date to quantify the effect of tofacitinib-associated lipid profile changes, their association with inflammatory markers, and the risk of major adverse cardiovascular events (MACEs). Using pooled data from multiple controlled, open-label studies of tofacitinib in UC, the authors appreciated a significant association between the rise in HDL cholesterol, LDL cholesterol, and total cholesterol levels and declines in C-reactive protein. They noted only four MACEs, an incidence rate similar to that seen in prior anti–tumor necrosis factor trials, and no change in a commonly used risk score for cardiovascular events.
These results are an important initial step in quantifying the cardiovascular risk associated with tofacitinib, but should be interpreted with caution. A significant proportion of individuals evaluated were from induction studies, with only 8 weeks of exposure. Only one dose of tofacitinib was required for inclusion. The median age in the OCTAVE trials, which contributed the majority of the data for this cohort, was only 41 years, and the baseline cardiovascular risk was low. While these data and rheumatologic literature are reassuring, further research with longitudinal follow-up, the assessment of time-varying exposures, and stratification by baseline cardiovascular risk will be required to better understand the association between tofacitinib and MACEs.
Frank I. Scott, MD, MSCE, assistant professor of medicine, Crohn’s and Colitis Center, codirector of clinical research/DART, director of GI fellowship research, division of gastroenterology and hepatology, University of Colorado at Denver, Aurora. He has received research funding and consulting fees from Takeda, and Janssen, and consulting fees from Merck.
Tofacitinib has several well-described effects on lipid metabolism, increasing levels of LDL cholesterol, HDL cholesterol, and total cholesterol. The clinical consequences of these lipid changes remains uncertain in ulcerative colitis (UC), for which there may be an increased risk of cardiovascular events.
In this study, Sands and colleagues used the largest cohort to date to quantify the effect of tofacitinib-associated lipid profile changes, their association with inflammatory markers, and the risk of major adverse cardiovascular events (MACEs). Using pooled data from multiple controlled, open-label studies of tofacitinib in UC, the authors appreciated a significant association between the rise in HDL cholesterol, LDL cholesterol, and total cholesterol levels and declines in C-reactive protein. They noted only four MACEs, an incidence rate similar to that seen in prior anti–tumor necrosis factor trials, and no change in a commonly used risk score for cardiovascular events.
These results are an important initial step in quantifying the cardiovascular risk associated with tofacitinib, but should be interpreted with caution. A significant proportion of individuals evaluated were from induction studies, with only 8 weeks of exposure. Only one dose of tofacitinib was required for inclusion. The median age in the OCTAVE trials, which contributed the majority of the data for this cohort, was only 41 years, and the baseline cardiovascular risk was low. While these data and rheumatologic literature are reassuring, further research with longitudinal follow-up, the assessment of time-varying exposures, and stratification by baseline cardiovascular risk will be required to better understand the association between tofacitinib and MACEs.
Frank I. Scott, MD, MSCE, assistant professor of medicine, Crohn’s and Colitis Center, codirector of clinical research/DART, director of GI fellowship research, division of gastroenterology and hepatology, University of Colorado at Denver, Aurora. He has received research funding and consulting fees from Takeda, and Janssen, and consulting fees from Merck.
according to results of an analysis including more than 1,000 patients.
Major adverse cardiac events (MACE) were “infrequent” following treatment, according to the authors of the analysis, with an incidence rate similar to what has been reported for tofacitinib in rheumatoid arthritis and for other agents in ulcerative colitis.
That said, the period of observation in the analysis is “relatively short,” and so may not provide an accurate risk estimate for MACE, noted the investigators, led by Bruce E. Sands, MD, of the division of gastroenterology at the Icahn School of Medicine at Mount Sinai, New York.
“Longer-term studies, involving a larger number of patients, will be needed to further assess MACE risk in patients with ulcerative colitis,” Dr. Sands and coinvestigators wrote in their report on the observational analysis, which appears in Clinical Gastroenterology and Hepatology.
“It is noteworthy that no increase in MACE risk and no dose relationship with tofacitinib have been observed in a larger rheumatoid arthritis cohort with over 8.5 years of observation and more than 19,000 patient-years of collective exposure,” they continued.
The present analysis included 1,157 patients with ulcerative colitis who participated in 8-week phase 2 and 3 tofacitinib induction studies, a phase 3 maintenance study, and a long-term extension study that is ongoing.
Reversible and dose-dependent increases in both LDL cholesterol and HDL cholesterol were observed after 8 weeks of treatment with tofacitinib at the recommended induction dose of 10 mg twice daily, the investigators found.
Increases in LDL cholesterol, HDL cholesterol, and total cholesterol correlated with decreases in high-sensitivity C-reactive protein, suggesting any potential impact of lipid increases on cardiovascular events might be offset by reduced inflammation, according to the investigators.
“Previous studies in RA and inflammatory bowel disease have shown an inverse relationship between active inflammation and serum lipid profiles, suggesting that inflammation lowers lipid concentrations, and that treatment of the underlying inflammatory disease may, therefore, increase them,” Dr. Sands and colleagues wrote.
The lipid changes also correlated with increases in body mass index, possibly because of better nutrition, reduced protein loss, and less catabolism following tofacitinib treatment, along with the corticosteroid taper required in these studies of the drug, they added.
Lipid increases generally stayed elevated through 61 weeks of treatment, while in patients randomized to placebo after 8 weeks of tofacitinib treatment, lipid levels fell back toward baseline, which suggests a reversal of the increases after tofacitinib withdrawal, the investigators wrote.
A total of 4 MACEs were seen among the 1,157 patients in the analysis, for an incidence rate of 0.24 (95% confidence interval, 0.07-0.62), according to the report. Those events included an acute coronary syndrome, an MI, an aortic dissection, and a hemorrhagic stroke. All four occurred in tofacitinib-treated patients, though the investigators noted that the aortic dissection and hemorrhagic stroke are events typically associated with genetics or other nonlipid factors.
In any case, that MACE incidence rate was “similar” to infliximab (Remicade) for what has been observed in tumor necrosis factor antagonist treatment of ulcerative colitis within a U.S. claims database study. In that analysis, including patients treated with infliximab, golimumab, and adalimumab, the incidence rate was 0.51 (95% CI, 0.31-0.79), the investigators noted.
These findings, taken together, support recommendations in tofacitinib prescribing information that call for monitoring of lipid concentrations 4-8 weeks after treatment is started, according to Dr. Sands and coauthors.
Funding for the study came from Pfizer. The study authors disclosed potential conflicts of interest related to Pfizer, AbbVie, Amgen, Bristol-Myers Squibb, Celgene, Janssen, MedImmune (AstraZeneca), Millennium Pharmaceuticals, Prometheus Laboratories, Takeda, and 4D Pharma, among others.
SOURCE: Sands BE et al. Clin Gastroenterol Hepatol. 2019 May 8. doi: 10.1016/j.cgh.2019.04.059.
according to results of an analysis including more than 1,000 patients.
Major adverse cardiac events (MACE) were “infrequent” following treatment, according to the authors of the analysis, with an incidence rate similar to what has been reported for tofacitinib in rheumatoid arthritis and for other agents in ulcerative colitis.
That said, the period of observation in the analysis is “relatively short,” and so may not provide an accurate risk estimate for MACE, noted the investigators, led by Bruce E. Sands, MD, of the division of gastroenterology at the Icahn School of Medicine at Mount Sinai, New York.
“Longer-term studies, involving a larger number of patients, will be needed to further assess MACE risk in patients with ulcerative colitis,” Dr. Sands and coinvestigators wrote in their report on the observational analysis, which appears in Clinical Gastroenterology and Hepatology.
“It is noteworthy that no increase in MACE risk and no dose relationship with tofacitinib have been observed in a larger rheumatoid arthritis cohort with over 8.5 years of observation and more than 19,000 patient-years of collective exposure,” they continued.
The present analysis included 1,157 patients with ulcerative colitis who participated in 8-week phase 2 and 3 tofacitinib induction studies, a phase 3 maintenance study, and a long-term extension study that is ongoing.
Reversible and dose-dependent increases in both LDL cholesterol and HDL cholesterol were observed after 8 weeks of treatment with tofacitinib at the recommended induction dose of 10 mg twice daily, the investigators found.
Increases in LDL cholesterol, HDL cholesterol, and total cholesterol correlated with decreases in high-sensitivity C-reactive protein, suggesting any potential impact of lipid increases on cardiovascular events might be offset by reduced inflammation, according to the investigators.
“Previous studies in RA and inflammatory bowel disease have shown an inverse relationship between active inflammation and serum lipid profiles, suggesting that inflammation lowers lipid concentrations, and that treatment of the underlying inflammatory disease may, therefore, increase them,” Dr. Sands and colleagues wrote.
The lipid changes also correlated with increases in body mass index, possibly because of better nutrition, reduced protein loss, and less catabolism following tofacitinib treatment, along with the corticosteroid taper required in these studies of the drug, they added.
Lipid increases generally stayed elevated through 61 weeks of treatment, while in patients randomized to placebo after 8 weeks of tofacitinib treatment, lipid levels fell back toward baseline, which suggests a reversal of the increases after tofacitinib withdrawal, the investigators wrote.
A total of 4 MACEs were seen among the 1,157 patients in the analysis, for an incidence rate of 0.24 (95% confidence interval, 0.07-0.62), according to the report. Those events included an acute coronary syndrome, an MI, an aortic dissection, and a hemorrhagic stroke. All four occurred in tofacitinib-treated patients, though the investigators noted that the aortic dissection and hemorrhagic stroke are events typically associated with genetics or other nonlipid factors.
In any case, that MACE incidence rate was “similar” to infliximab (Remicade) for what has been observed in tumor necrosis factor antagonist treatment of ulcerative colitis within a U.S. claims database study. In that analysis, including patients treated with infliximab, golimumab, and adalimumab, the incidence rate was 0.51 (95% CI, 0.31-0.79), the investigators noted.
These findings, taken together, support recommendations in tofacitinib prescribing information that call for monitoring of lipid concentrations 4-8 weeks after treatment is started, according to Dr. Sands and coauthors.
Funding for the study came from Pfizer. The study authors disclosed potential conflicts of interest related to Pfizer, AbbVie, Amgen, Bristol-Myers Squibb, Celgene, Janssen, MedImmune (AstraZeneca), Millennium Pharmaceuticals, Prometheus Laboratories, Takeda, and 4D Pharma, among others.
SOURCE: Sands BE et al. Clin Gastroenterol Hepatol. 2019 May 8. doi: 10.1016/j.cgh.2019.04.059.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
No clear-cut evidence of vedolizumab effect in retrospective study of primary sclerosing cholangitis
While initial case reports and series provided preliminarily encouraging results, a larger retrospective study has provided no clear-cut evidence of biochemical response to vedolizumab in patients with primary sclerosing cholangitis (PSC) and inflammatory bowel disease, investigators report.
A subset of patients in the retrospective analysis did experience a substantial drop in alkaline phosphatase (ALP), according to investigators with the International Primary Sclerosing Cholangitis Study Group.
Overall, however, levels of that cholestasis marker rose by a small but statistically significant amount in this study, which included more than 100 patients with PSC and inflammatory bowel disease (IBD).
Responses were more likely in patients with cirrhosis and in those with elevated ALP at baseline, both of which are indicators of more aggressive disease, according to investigator Kate D. Lynch, MD, PhD, of the University of Oxford (England) and her coauthors.
The rate of liver outcomes was in line with the natural history of the disease, according to Dr. Lynch and coinvestigators, who added that most patients had an endoscopic IBD response, as might be expected based on studies of IBD-only patients treated with vedolizumab.
“Despite the disappointment with lack of a uniform response, further evaluation of vedolizumab as a beneficial treatment in PSC may be warranted in a subset of patients via a stratified randomized clinical trial,” Dr. Lynch and coauthors said in their report, which was published in Clinical Gastroenterology and Hepatology.
Vedolizumab, a monoclonal antibody against integrin alpha4beta7, is effective in Crohn’s disease and ulcerative colitis, according to investigators, who added that the “gut-homing pathway” it targets has also been implicated in the pathophysiology of PSC.
“It is possible that vedolizumab may play a role in reducing lymphocyte infiltration into the liver in patients with PSC and thereby in reducing hepatic and biliary inflammation, authors of the retrospective analysis said.
Their analysis included 102 patients with PSC and IBD at 20 centers in Europe and North America. All patients had received at least three doses of vedolizumab for their IBD, given according to the usual dosing schedule. Most of the patients were male (64 patients, or 62.8%) and about 90% had classical large-duct PSC. About one-fifth had cirrhosis, and the majority (about 65%) had ulcerative colitis. Patients were followed until death, liver transplant, or 56 days after the last vedolizumab dose.
The median ALP increased from 1.53 times the upper limit of normal at baseline to 1.64 times the upper limit of normal by the last follow-up, an increase that was statistically significant (P = .018) but not clinically significant, according to investigators. Likewise, they said, statistically significant increases were seen overall in median alanine transaminase and aspartate aminotransferase levels.
However, 21 patients (20.6%) had a drop in ALP of at least 20% from baseline to last follow-up, and another 39 patients (38.2%) had stable ALP over that period, data show, while the remaining 42 (41.2%) had an increase of 20% or more.
Cirrhosis was associated with a near fivefold odds of a 20% or greater ALP drop from baseline to follow-up (odds ratio, 4.70, 95% confidence interval, 1.61-13.76), according to results of univariate analysis, which investigators said were “reproduced” in multivariate analysis.
While no other variables were so clearly linked to a 20% or greater drop in ALP, Dr. Lynch and colleagues said there was a “trend toward an association” in patients with ALP raised at baseline, and in those who had Crohn’s disease or IBD-unspecified instead of ulcerative colitis.
Endoscopic IBD responses were seen in 42 out of 74 patients (56.8%) for whom those data were available, investigators added.
A total of 22 patients (20.9%) had a liver-related outcome over median follow-up of 561 days; however, that outcome may be “slightly overrepresented” by an incidence of cholangitis in 8.8%, which in and of itself is not necessarily an indicator of advanced liver disease, said Dr. Lynch and coauthors in their report.
“This proportion of liver-related outcomes is consistent with the natural history of PSC and does not by itself indicate that vedolizumab treatment is harmful in PSC,” they said, adding that the findings were similar to a study of simtuzumab, a monoclonal antibody directed against lysyl oxidase-like 2, in patients with PSC, of whom 20.1% had a PSC-related event and the incidence of cholangitis was 13.2%.
The retrospective study was supported by the Birmingham National Institute for Health Research (NIHR) Biomedical Research Centre in the United Kingdom. Authors of the report provided disclosures related to Takeda, AbbVie, Dr. Falk Pharma, Intercept, MSD, Janssen, Vifor, Gilead, and Novartis, among others.
SOURCE: Lynch KD et al. Clin Gastroenterol Hepatol. 2019 May 14. doi: 10.1016/j.cgh.2019.05.013.
While initial case reports and series provided preliminarily encouraging results, a larger retrospective study has provided no clear-cut evidence of biochemical response to vedolizumab in patients with primary sclerosing cholangitis (PSC) and inflammatory bowel disease, investigators report.
A subset of patients in the retrospective analysis did experience a substantial drop in alkaline phosphatase (ALP), according to investigators with the International Primary Sclerosing Cholangitis Study Group.
Overall, however, levels of that cholestasis marker rose by a small but statistically significant amount in this study, which included more than 100 patients with PSC and inflammatory bowel disease (IBD).
Responses were more likely in patients with cirrhosis and in those with elevated ALP at baseline, both of which are indicators of more aggressive disease, according to investigator Kate D. Lynch, MD, PhD, of the University of Oxford (England) and her coauthors.
The rate of liver outcomes was in line with the natural history of the disease, according to Dr. Lynch and coinvestigators, who added that most patients had an endoscopic IBD response, as might be expected based on studies of IBD-only patients treated with vedolizumab.
“Despite the disappointment with lack of a uniform response, further evaluation of vedolizumab as a beneficial treatment in PSC may be warranted in a subset of patients via a stratified randomized clinical trial,” Dr. Lynch and coauthors said in their report, which was published in Clinical Gastroenterology and Hepatology.
Vedolizumab, a monoclonal antibody against integrin alpha4beta7, is effective in Crohn’s disease and ulcerative colitis, according to investigators, who added that the “gut-homing pathway” it targets has also been implicated in the pathophysiology of PSC.
“It is possible that vedolizumab may play a role in reducing lymphocyte infiltration into the liver in patients with PSC and thereby in reducing hepatic and biliary inflammation, authors of the retrospective analysis said.
Their analysis included 102 patients with PSC and IBD at 20 centers in Europe and North America. All patients had received at least three doses of vedolizumab for their IBD, given according to the usual dosing schedule. Most of the patients were male (64 patients, or 62.8%) and about 90% had classical large-duct PSC. About one-fifth had cirrhosis, and the majority (about 65%) had ulcerative colitis. Patients were followed until death, liver transplant, or 56 days after the last vedolizumab dose.
The median ALP increased from 1.53 times the upper limit of normal at baseline to 1.64 times the upper limit of normal by the last follow-up, an increase that was statistically significant (P = .018) but not clinically significant, according to investigators. Likewise, they said, statistically significant increases were seen overall in median alanine transaminase and aspartate aminotransferase levels.
However, 21 patients (20.6%) had a drop in ALP of at least 20% from baseline to last follow-up, and another 39 patients (38.2%) had stable ALP over that period, data show, while the remaining 42 (41.2%) had an increase of 20% or more.
Cirrhosis was associated with a near fivefold odds of a 20% or greater ALP drop from baseline to follow-up (odds ratio, 4.70, 95% confidence interval, 1.61-13.76), according to results of univariate analysis, which investigators said were “reproduced” in multivariate analysis.
While no other variables were so clearly linked to a 20% or greater drop in ALP, Dr. Lynch and colleagues said there was a “trend toward an association” in patients with ALP raised at baseline, and in those who had Crohn’s disease or IBD-unspecified instead of ulcerative colitis.
Endoscopic IBD responses were seen in 42 out of 74 patients (56.8%) for whom those data were available, investigators added.
A total of 22 patients (20.9%) had a liver-related outcome over median follow-up of 561 days; however, that outcome may be “slightly overrepresented” by an incidence of cholangitis in 8.8%, which in and of itself is not necessarily an indicator of advanced liver disease, said Dr. Lynch and coauthors in their report.
“This proportion of liver-related outcomes is consistent with the natural history of PSC and does not by itself indicate that vedolizumab treatment is harmful in PSC,” they said, adding that the findings were similar to a study of simtuzumab, a monoclonal antibody directed against lysyl oxidase-like 2, in patients with PSC, of whom 20.1% had a PSC-related event and the incidence of cholangitis was 13.2%.
The retrospective study was supported by the Birmingham National Institute for Health Research (NIHR) Biomedical Research Centre in the United Kingdom. Authors of the report provided disclosures related to Takeda, AbbVie, Dr. Falk Pharma, Intercept, MSD, Janssen, Vifor, Gilead, and Novartis, among others.
SOURCE: Lynch KD et al. Clin Gastroenterol Hepatol. 2019 May 14. doi: 10.1016/j.cgh.2019.05.013.
While initial case reports and series provided preliminarily encouraging results, a larger retrospective study has provided no clear-cut evidence of biochemical response to vedolizumab in patients with primary sclerosing cholangitis (PSC) and inflammatory bowel disease, investigators report.
A subset of patients in the retrospective analysis did experience a substantial drop in alkaline phosphatase (ALP), according to investigators with the International Primary Sclerosing Cholangitis Study Group.
Overall, however, levels of that cholestasis marker rose by a small but statistically significant amount in this study, which included more than 100 patients with PSC and inflammatory bowel disease (IBD).
Responses were more likely in patients with cirrhosis and in those with elevated ALP at baseline, both of which are indicators of more aggressive disease, according to investigator Kate D. Lynch, MD, PhD, of the University of Oxford (England) and her coauthors.
The rate of liver outcomes was in line with the natural history of the disease, according to Dr. Lynch and coinvestigators, who added that most patients had an endoscopic IBD response, as might be expected based on studies of IBD-only patients treated with vedolizumab.
“Despite the disappointment with lack of a uniform response, further evaluation of vedolizumab as a beneficial treatment in PSC may be warranted in a subset of patients via a stratified randomized clinical trial,” Dr. Lynch and coauthors said in their report, which was published in Clinical Gastroenterology and Hepatology.
Vedolizumab, a monoclonal antibody against integrin alpha4beta7, is effective in Crohn’s disease and ulcerative colitis, according to investigators, who added that the “gut-homing pathway” it targets has also been implicated in the pathophysiology of PSC.
“It is possible that vedolizumab may play a role in reducing lymphocyte infiltration into the liver in patients with PSC and thereby in reducing hepatic and biliary inflammation, authors of the retrospective analysis said.
Their analysis included 102 patients with PSC and IBD at 20 centers in Europe and North America. All patients had received at least three doses of vedolizumab for their IBD, given according to the usual dosing schedule. Most of the patients were male (64 patients, or 62.8%) and about 90% had classical large-duct PSC. About one-fifth had cirrhosis, and the majority (about 65%) had ulcerative colitis. Patients were followed until death, liver transplant, or 56 days after the last vedolizumab dose.
The median ALP increased from 1.53 times the upper limit of normal at baseline to 1.64 times the upper limit of normal by the last follow-up, an increase that was statistically significant (P = .018) but not clinically significant, according to investigators. Likewise, they said, statistically significant increases were seen overall in median alanine transaminase and aspartate aminotransferase levels.
However, 21 patients (20.6%) had a drop in ALP of at least 20% from baseline to last follow-up, and another 39 patients (38.2%) had stable ALP over that period, data show, while the remaining 42 (41.2%) had an increase of 20% or more.
Cirrhosis was associated with a near fivefold odds of a 20% or greater ALP drop from baseline to follow-up (odds ratio, 4.70, 95% confidence interval, 1.61-13.76), according to results of univariate analysis, which investigators said were “reproduced” in multivariate analysis.
While no other variables were so clearly linked to a 20% or greater drop in ALP, Dr. Lynch and colleagues said there was a “trend toward an association” in patients with ALP raised at baseline, and in those who had Crohn’s disease or IBD-unspecified instead of ulcerative colitis.
Endoscopic IBD responses were seen in 42 out of 74 patients (56.8%) for whom those data were available, investigators added.
A total of 22 patients (20.9%) had a liver-related outcome over median follow-up of 561 days; however, that outcome may be “slightly overrepresented” by an incidence of cholangitis in 8.8%, which in and of itself is not necessarily an indicator of advanced liver disease, said Dr. Lynch and coauthors in their report.
“This proportion of liver-related outcomes is consistent with the natural history of PSC and does not by itself indicate that vedolizumab treatment is harmful in PSC,” they said, adding that the findings were similar to a study of simtuzumab, a monoclonal antibody directed against lysyl oxidase-like 2, in patients with PSC, of whom 20.1% had a PSC-related event and the incidence of cholangitis was 13.2%.
The retrospective study was supported by the Birmingham National Institute for Health Research (NIHR) Biomedical Research Centre in the United Kingdom. Authors of the report provided disclosures related to Takeda, AbbVie, Dr. Falk Pharma, Intercept, MSD, Janssen, Vifor, Gilead, and Novartis, among others.
SOURCE: Lynch KD et al. Clin Gastroenterol Hepatol. 2019 May 14. doi: 10.1016/j.cgh.2019.05.013.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Early colonoscopy for acute lower GI bleeding fails to improve diagnostic yield or reduce rebleeding rate
While generally recommended for diagnosis and treatment of severe bleeding, early colonoscopy did not improve stigmata identification or reduce rebleeding rates in patients admitted for acute lower gastrointestinal bleeding in a relatively large, multicenter randomized trial, investigators report.
The proportion of patients with identified stigmata of recent hemorrhage (SRH) was not statistically significantly different between groups of patients who had early colonoscopy versus those who had a procedure 24 hours or more after admission, according to results of the 170-patient randomized study.
Although rebleeding rate was only a secondary endpoint, a larger study would be “unlikely to show a benefit” of the urgent approach, said investigators led by Ryota Niikura, MD, PhD, of the department of gastroenterology in the graduate school of medicine at the University of Tokyo.
“Our results for rebleeding suggested that early colonoscopy does not improve rebleeding outcomes, even if we chose rebleeding as the primary outcome,” Dr. Niikura and colleagues said in a discussion of the results, which appear in Gastroenterology.
Leading up to this trial, there was “controversy” over whether early colonoscopy could improve significant clinical outcomes such as rebleeding, transfusion need, and mortality, according to the authors, who said this is the largest of four randomized, controlled trials reported on the subject to date, and the first multicenter trial among that group.
One of those randomized studies, reported by Green and colleagues in the American Journal of Gastroenterology in 2005, found no differences in mortality, hospital stay, intensive care unit stay, transfusion requirements, rebleeding, or surgery for urgent colonoscopy versus care provided according to a standard algorithm.
Similarly, Laine and Shah said urgent colonoscopy had no edge over routine elective colonoscopy in terms of clinical outcomes or lowering costs, in a randomized study reported in 2010, also in the American Journal of Gastroenterology.
In September 2019, van Rongen and colleagues reported results of the BLEED study of early versus standard colonoscopy. Length of hospital stay was significantly shorter among patients randomized to the urgent approach; however, the rate of recurrent bleeding and hospital readmission was significantly higher in that group, according to results published in the Journal of Clinical Gastroenterology.
Two out of three of the previous randomized trials also showed no improvement in diagnostic yield with early colonoscopy, though “some meta-analyses” do suggest such a benefit, Dr. Niikura and coauthors said.
The latest reported randomized trial by Dr. Niikura and coinvestigators included patients 20 years of age or older who had moderate to severe hematochezia or melena within 24 hours of admission. A total of 162 adult patients at 15 hospitals in Japan were randomized to undergo early colonoscopy within 24 hours, or elective colonoscopy between 24 and 72 hours.
The primary outcome, identification of SRH, was not significantly different for the early versus later colonoscopy. Investigators said SRH was observed in 17 of 79 patients undergoing early colonoscopy or 21.5%, and in 17 of 80 patients in the elective colonoscopy group, or 21.3% (P = .967).
Similar rates of SRH between early and elective colonoscopy is a finding “in line” with the two of three previous randomized trials that found no increase in diagnostic yield, Dr. Niikura and coinvestigators noted in their report.
Rebleeding within 30 days, the “key secondary outcome” of the study according to investigators, was seen in 11 of 72 patients in the early colonoscopy group, or 15.3%, and in 5 of 75 patients in the elective colonoscopy group, or 6.7%, for a difference of 8.6 percentage points (95% confidence interval, –1.4 to 18.7).
Taken together, these findings suggest that early colonoscopy did not improve the SRH identification rate and that the 30-day rebleeding rate was not different, the authors said in a discussion of the results.
“Guidelines and prior studies often recommend that early colonoscopy be performed within 8-24 hours of admission to increase diagnostic yield and the likelihood of a therapeutic intervention,” they added in their discussion.
Dr. Niikura and coauthors acknowledged receiving grant funding from the Japanese Gastroenterological Association. Study coauthor Mitsuhiro Fujishiro, MD, PhD, reported disclosures related to Takeda, AstraZeneca, Zeria, Daiichi-Sankyo, and EA Pharma. The remaining authors did not declare competing interests.
SOURCE: Niikura R et al. Gastroenterology. 2019. doi: 10.1053/j.gastro.2019.09.010.
When to perform colonoscopy for the evaluation of acute lower gastrointestinal bleeding (LGIB) is controversial. Multiple observational studies, three small, single center randomized controlled trials, and several meta-analyses have produced mixed results. Therefore, a large, multicenter trial is of high priority.
Overall, the results suggest that in most patients presenting with acute LGIB, we do not need to perform colonoscopy within 24 hours of admission. However, the mean time to colonoscopy in the elective group was 41 hours from presentation. Therefore, colonoscopy should be performed on a next available basis. Further delays add unnecessary hospital days and increase cost of care. Future studies are needed to identify alternative ways to improve outcomes in LGIB, define the management of unstable patients with acute LGIB, and perfect the approach to endoscopic hemostasis in the colon.
Lisa L. Strate, MD, is professor of medicine, University of Washington, and section chief, gastroenterology, Harborview Medical Center, Seattle.
When to perform colonoscopy for the evaluation of acute lower gastrointestinal bleeding (LGIB) is controversial. Multiple observational studies, three small, single center randomized controlled trials, and several meta-analyses have produced mixed results. Therefore, a large, multicenter trial is of high priority.
Overall, the results suggest that in most patients presenting with acute LGIB, we do not need to perform colonoscopy within 24 hours of admission. However, the mean time to colonoscopy in the elective group was 41 hours from presentation. Therefore, colonoscopy should be performed on a next available basis. Further delays add unnecessary hospital days and increase cost of care. Future studies are needed to identify alternative ways to improve outcomes in LGIB, define the management of unstable patients with acute LGIB, and perfect the approach to endoscopic hemostasis in the colon.
Lisa L. Strate, MD, is professor of medicine, University of Washington, and section chief, gastroenterology, Harborview Medical Center, Seattle.
When to perform colonoscopy for the evaluation of acute lower gastrointestinal bleeding (LGIB) is controversial. Multiple observational studies, three small, single center randomized controlled trials, and several meta-analyses have produced mixed results. Therefore, a large, multicenter trial is of high priority.
Overall, the results suggest that in most patients presenting with acute LGIB, we do not need to perform colonoscopy within 24 hours of admission. However, the mean time to colonoscopy in the elective group was 41 hours from presentation. Therefore, colonoscopy should be performed on a next available basis. Further delays add unnecessary hospital days and increase cost of care. Future studies are needed to identify alternative ways to improve outcomes in LGIB, define the management of unstable patients with acute LGIB, and perfect the approach to endoscopic hemostasis in the colon.
Lisa L. Strate, MD, is professor of medicine, University of Washington, and section chief, gastroenterology, Harborview Medical Center, Seattle.
While generally recommended for diagnosis and treatment of severe bleeding, early colonoscopy did not improve stigmata identification or reduce rebleeding rates in patients admitted for acute lower gastrointestinal bleeding in a relatively large, multicenter randomized trial, investigators report.
The proportion of patients with identified stigmata of recent hemorrhage (SRH) was not statistically significantly different between groups of patients who had early colonoscopy versus those who had a procedure 24 hours or more after admission, according to results of the 170-patient randomized study.
Although rebleeding rate was only a secondary endpoint, a larger study would be “unlikely to show a benefit” of the urgent approach, said investigators led by Ryota Niikura, MD, PhD, of the department of gastroenterology in the graduate school of medicine at the University of Tokyo.
“Our results for rebleeding suggested that early colonoscopy does not improve rebleeding outcomes, even if we chose rebleeding as the primary outcome,” Dr. Niikura and colleagues said in a discussion of the results, which appear in Gastroenterology.
Leading up to this trial, there was “controversy” over whether early colonoscopy could improve significant clinical outcomes such as rebleeding, transfusion need, and mortality, according to the authors, who said this is the largest of four randomized, controlled trials reported on the subject to date, and the first multicenter trial among that group.
One of those randomized studies, reported by Green and colleagues in the American Journal of Gastroenterology in 2005, found no differences in mortality, hospital stay, intensive care unit stay, transfusion requirements, rebleeding, or surgery for urgent colonoscopy versus care provided according to a standard algorithm.
Similarly, Laine and Shah said urgent colonoscopy had no edge over routine elective colonoscopy in terms of clinical outcomes or lowering costs, in a randomized study reported in 2010, also in the American Journal of Gastroenterology.
In September 2019, van Rongen and colleagues reported results of the BLEED study of early versus standard colonoscopy. Length of hospital stay was significantly shorter among patients randomized to the urgent approach; however, the rate of recurrent bleeding and hospital readmission was significantly higher in that group, according to results published in the Journal of Clinical Gastroenterology.
Two out of three of the previous randomized trials also showed no improvement in diagnostic yield with early colonoscopy, though “some meta-analyses” do suggest such a benefit, Dr. Niikura and coauthors said.
The latest reported randomized trial by Dr. Niikura and coinvestigators included patients 20 years of age or older who had moderate to severe hematochezia or melena within 24 hours of admission. A total of 162 adult patients at 15 hospitals in Japan were randomized to undergo early colonoscopy within 24 hours, or elective colonoscopy between 24 and 72 hours.
The primary outcome, identification of SRH, was not significantly different for the early versus later colonoscopy. Investigators said SRH was observed in 17 of 79 patients undergoing early colonoscopy or 21.5%, and in 17 of 80 patients in the elective colonoscopy group, or 21.3% (P = .967).
Similar rates of SRH between early and elective colonoscopy is a finding “in line” with the two of three previous randomized trials that found no increase in diagnostic yield, Dr. Niikura and coinvestigators noted in their report.
Rebleeding within 30 days, the “key secondary outcome” of the study according to investigators, was seen in 11 of 72 patients in the early colonoscopy group, or 15.3%, and in 5 of 75 patients in the elective colonoscopy group, or 6.7%, for a difference of 8.6 percentage points (95% confidence interval, –1.4 to 18.7).
Taken together, these findings suggest that early colonoscopy did not improve the SRH identification rate and that the 30-day rebleeding rate was not different, the authors said in a discussion of the results.
“Guidelines and prior studies often recommend that early colonoscopy be performed within 8-24 hours of admission to increase diagnostic yield and the likelihood of a therapeutic intervention,” they added in their discussion.
Dr. Niikura and coauthors acknowledged receiving grant funding from the Japanese Gastroenterological Association. Study coauthor Mitsuhiro Fujishiro, MD, PhD, reported disclosures related to Takeda, AstraZeneca, Zeria, Daiichi-Sankyo, and EA Pharma. The remaining authors did not declare competing interests.
SOURCE: Niikura R et al. Gastroenterology. 2019. doi: 10.1053/j.gastro.2019.09.010.
While generally recommended for diagnosis and treatment of severe bleeding, early colonoscopy did not improve stigmata identification or reduce rebleeding rates in patients admitted for acute lower gastrointestinal bleeding in a relatively large, multicenter randomized trial, investigators report.
The proportion of patients with identified stigmata of recent hemorrhage (SRH) was not statistically significantly different between groups of patients who had early colonoscopy versus those who had a procedure 24 hours or more after admission, according to results of the 170-patient randomized study.
Although rebleeding rate was only a secondary endpoint, a larger study would be “unlikely to show a benefit” of the urgent approach, said investigators led by Ryota Niikura, MD, PhD, of the department of gastroenterology in the graduate school of medicine at the University of Tokyo.
“Our results for rebleeding suggested that early colonoscopy does not improve rebleeding outcomes, even if we chose rebleeding as the primary outcome,” Dr. Niikura and colleagues said in a discussion of the results, which appear in Gastroenterology.
Leading up to this trial, there was “controversy” over whether early colonoscopy could improve significant clinical outcomes such as rebleeding, transfusion need, and mortality, according to the authors, who said this is the largest of four randomized, controlled trials reported on the subject to date, and the first multicenter trial among that group.
One of those randomized studies, reported by Green and colleagues in the American Journal of Gastroenterology in 2005, found no differences in mortality, hospital stay, intensive care unit stay, transfusion requirements, rebleeding, or surgery for urgent colonoscopy versus care provided according to a standard algorithm.
Similarly, Laine and Shah said urgent colonoscopy had no edge over routine elective colonoscopy in terms of clinical outcomes or lowering costs, in a randomized study reported in 2010, also in the American Journal of Gastroenterology.
In September 2019, van Rongen and colleagues reported results of the BLEED study of early versus standard colonoscopy. Length of hospital stay was significantly shorter among patients randomized to the urgent approach; however, the rate of recurrent bleeding and hospital readmission was significantly higher in that group, according to results published in the Journal of Clinical Gastroenterology.
Two out of three of the previous randomized trials also showed no improvement in diagnostic yield with early colonoscopy, though “some meta-analyses” do suggest such a benefit, Dr. Niikura and coauthors said.
The latest reported randomized trial by Dr. Niikura and coinvestigators included patients 20 years of age or older who had moderate to severe hematochezia or melena within 24 hours of admission. A total of 162 adult patients at 15 hospitals in Japan were randomized to undergo early colonoscopy within 24 hours, or elective colonoscopy between 24 and 72 hours.
The primary outcome, identification of SRH, was not significantly different for the early versus later colonoscopy. Investigators said SRH was observed in 17 of 79 patients undergoing early colonoscopy or 21.5%, and in 17 of 80 patients in the elective colonoscopy group, or 21.3% (P = .967).
Similar rates of SRH between early and elective colonoscopy is a finding “in line” with the two of three previous randomized trials that found no increase in diagnostic yield, Dr. Niikura and coinvestigators noted in their report.
Rebleeding within 30 days, the “key secondary outcome” of the study according to investigators, was seen in 11 of 72 patients in the early colonoscopy group, or 15.3%, and in 5 of 75 patients in the elective colonoscopy group, or 6.7%, for a difference of 8.6 percentage points (95% confidence interval, –1.4 to 18.7).
Taken together, these findings suggest that early colonoscopy did not improve the SRH identification rate and that the 30-day rebleeding rate was not different, the authors said in a discussion of the results.
“Guidelines and prior studies often recommend that early colonoscopy be performed within 8-24 hours of admission to increase diagnostic yield and the likelihood of a therapeutic intervention,” they added in their discussion.
Dr. Niikura and coauthors acknowledged receiving grant funding from the Japanese Gastroenterological Association. Study coauthor Mitsuhiro Fujishiro, MD, PhD, reported disclosures related to Takeda, AstraZeneca, Zeria, Daiichi-Sankyo, and EA Pharma. The remaining authors did not declare competing interests.
SOURCE: Niikura R et al. Gastroenterology. 2019. doi: 10.1053/j.gastro.2019.09.010.
FROM GASTROENTEROLOGY