User login
Medicaid youth suicides include more females, younger kids, hanging deaths
Young people enrolled in Medicaid who commit suicide are disproportionately female, younger, and more likely to die by hanging, compared with non-Medicaid youth, results of a large, observational, population-based study suggest.
Nearly 40% of young people in the study who died by suicide were covered by Medicaid, according to study lead author Cynthia A. Fontanella, PhD, of the department of psychiatry and behavioral health at the Ohio State University, Columbus. Those findings, in addition to those of other studies indicating that youth enrolled in Medicaid endure more maltreatment and poverty-related adversity, suggest a need for health care delivery systems to develop “trauma-informed approaches” and implement them, Dr. Fontanella and her coauthors reported in the American Journal of Preventive Medicine.
“Effective suicide screening of enrollees could substantially decrease suicide mortality in the United States,” they wrote.
Dr. Fontanella and her coauthors reviewed death certificate data from the 16 most populous states to identify all youth aged 10-18 who committed suicide during 2009-2013. They identified 4,045 deaths from suicide based on state death certificate data in California, Florida, Georgia, Illinois, Indiana, Massachusetts, Michigan, Minnesota, New York, North Carolina, Ohio, Oregon, Texas, Virginia, Washington, and Wisconsin. To identify the subset of youth who were enrolled in Medicaid, they used Social Security numbers to link the death certificate data to data from a Medicaid database.
Out of 4,045 youth suicide deaths that occurred during that time period, 39% were among youth enrolled in Medicaid, the investigators found.
Although the overall suicide rate did not differ significantly between the Medicaid and non-Medicaid groups, investigators said they did identify significant differences in age and sex subgroups. Specifically, those in the Medicaid group had a 28% increased risk of suicide among the 10- to 14-year age subgroup, and a 14% increased risk of suicide among females, the findings showed. Moreover, the risk of death by hanging was 26% greater among the Medicare youth.
Dr. Fontanella and her coauthors reported several limitations. One is that the findings might not be generalizable to all 50 states. Also, they said, because suicide is underreported as a cause of death, the prevalence of suicide found in the study might have been underreported.
Nevertheless, , Dr. Fontanella and her associates wrote. Boundaried populations are those defined by a service setting or organizational function. In other words, they wrote, findings based on an analysis of service use patterns captured in Medicaid claims “could prove helpful in identifying periods known to be associated with heightened suicide risk, such as that immediately following discharge from inpatient psychiatric care.”
The National Action Alliance for Suicide Prevention’s Research Prioritization Task Force has recommended that those populations be targeted for research on interventions designed to reduce suicide deaths, Dr. Fontanella and her coauthors wrote.
This is the first-ever study to evaluate suicide-related mortality among Medicaid-covered youth, the investigators said. Previous studies of suicide in Medicaid have focused on adults – specifically those in the Veterans Health Administration, specific state Medicaid programs, or health maintenance organization networks.
The American Foundation for Suicide Prevention and the National Institutes of Health funded the study. Dr. Fontanella and her coauthors reported no other financial conflicts of interest.
SOURCE: Fontanella CA et al. Am J Prev Med. 2019 Jan 17. doi: 10.1016/j.amepre.2018.10.008.
Young people enrolled in Medicaid who commit suicide are disproportionately female, younger, and more likely to die by hanging, compared with non-Medicaid youth, results of a large, observational, population-based study suggest.
Nearly 40% of young people in the study who died by suicide were covered by Medicaid, according to study lead author Cynthia A. Fontanella, PhD, of the department of psychiatry and behavioral health at the Ohio State University, Columbus. Those findings, in addition to those of other studies indicating that youth enrolled in Medicaid endure more maltreatment and poverty-related adversity, suggest a need for health care delivery systems to develop “trauma-informed approaches” and implement them, Dr. Fontanella and her coauthors reported in the American Journal of Preventive Medicine.
“Effective suicide screening of enrollees could substantially decrease suicide mortality in the United States,” they wrote.
Dr. Fontanella and her coauthors reviewed death certificate data from the 16 most populous states to identify all youth aged 10-18 who committed suicide during 2009-2013. They identified 4,045 deaths from suicide based on state death certificate data in California, Florida, Georgia, Illinois, Indiana, Massachusetts, Michigan, Minnesota, New York, North Carolina, Ohio, Oregon, Texas, Virginia, Washington, and Wisconsin. To identify the subset of youth who were enrolled in Medicaid, they used Social Security numbers to link the death certificate data to data from a Medicaid database.
Out of 4,045 youth suicide deaths that occurred during that time period, 39% were among youth enrolled in Medicaid, the investigators found.
Although the overall suicide rate did not differ significantly between the Medicaid and non-Medicaid groups, investigators said they did identify significant differences in age and sex subgroups. Specifically, those in the Medicaid group had a 28% increased risk of suicide among the 10- to 14-year age subgroup, and a 14% increased risk of suicide among females, the findings showed. Moreover, the risk of death by hanging was 26% greater among the Medicare youth.
Dr. Fontanella and her coauthors reported several limitations. One is that the findings might not be generalizable to all 50 states. Also, they said, because suicide is underreported as a cause of death, the prevalence of suicide found in the study might have been underreported.
Nevertheless, , Dr. Fontanella and her associates wrote. Boundaried populations are those defined by a service setting or organizational function. In other words, they wrote, findings based on an analysis of service use patterns captured in Medicaid claims “could prove helpful in identifying periods known to be associated with heightened suicide risk, such as that immediately following discharge from inpatient psychiatric care.”
The National Action Alliance for Suicide Prevention’s Research Prioritization Task Force has recommended that those populations be targeted for research on interventions designed to reduce suicide deaths, Dr. Fontanella and her coauthors wrote.
This is the first-ever study to evaluate suicide-related mortality among Medicaid-covered youth, the investigators said. Previous studies of suicide in Medicaid have focused on adults – specifically those in the Veterans Health Administration, specific state Medicaid programs, or health maintenance organization networks.
The American Foundation for Suicide Prevention and the National Institutes of Health funded the study. Dr. Fontanella and her coauthors reported no other financial conflicts of interest.
SOURCE: Fontanella CA et al. Am J Prev Med. 2019 Jan 17. doi: 10.1016/j.amepre.2018.10.008.
Young people enrolled in Medicaid who commit suicide are disproportionately female, younger, and more likely to die by hanging, compared with non-Medicaid youth, results of a large, observational, population-based study suggest.
Nearly 40% of young people in the study who died by suicide were covered by Medicaid, according to study lead author Cynthia A. Fontanella, PhD, of the department of psychiatry and behavioral health at the Ohio State University, Columbus. Those findings, in addition to those of other studies indicating that youth enrolled in Medicaid endure more maltreatment and poverty-related adversity, suggest a need for health care delivery systems to develop “trauma-informed approaches” and implement them, Dr. Fontanella and her coauthors reported in the American Journal of Preventive Medicine.
“Effective suicide screening of enrollees could substantially decrease suicide mortality in the United States,” they wrote.
Dr. Fontanella and her coauthors reviewed death certificate data from the 16 most populous states to identify all youth aged 10-18 who committed suicide during 2009-2013. They identified 4,045 deaths from suicide based on state death certificate data in California, Florida, Georgia, Illinois, Indiana, Massachusetts, Michigan, Minnesota, New York, North Carolina, Ohio, Oregon, Texas, Virginia, Washington, and Wisconsin. To identify the subset of youth who were enrolled in Medicaid, they used Social Security numbers to link the death certificate data to data from a Medicaid database.
Out of 4,045 youth suicide deaths that occurred during that time period, 39% were among youth enrolled in Medicaid, the investigators found.
Although the overall suicide rate did not differ significantly between the Medicaid and non-Medicaid groups, investigators said they did identify significant differences in age and sex subgroups. Specifically, those in the Medicaid group had a 28% increased risk of suicide among the 10- to 14-year age subgroup, and a 14% increased risk of suicide among females, the findings showed. Moreover, the risk of death by hanging was 26% greater among the Medicare youth.
Dr. Fontanella and her coauthors reported several limitations. One is that the findings might not be generalizable to all 50 states. Also, they said, because suicide is underreported as a cause of death, the prevalence of suicide found in the study might have been underreported.
Nevertheless, , Dr. Fontanella and her associates wrote. Boundaried populations are those defined by a service setting or organizational function. In other words, they wrote, findings based on an analysis of service use patterns captured in Medicaid claims “could prove helpful in identifying periods known to be associated with heightened suicide risk, such as that immediately following discharge from inpatient psychiatric care.”
The National Action Alliance for Suicide Prevention’s Research Prioritization Task Force has recommended that those populations be targeted for research on interventions designed to reduce suicide deaths, Dr. Fontanella and her coauthors wrote.
This is the first-ever study to evaluate suicide-related mortality among Medicaid-covered youth, the investigators said. Previous studies of suicide in Medicaid have focused on adults – specifically those in the Veterans Health Administration, specific state Medicaid programs, or health maintenance organization networks.
The American Foundation for Suicide Prevention and the National Institutes of Health funded the study. Dr. Fontanella and her coauthors reported no other financial conflicts of interest.
SOURCE: Fontanella CA et al. Am J Prev Med. 2019 Jan 17. doi: 10.1016/j.amepre.2018.10.008.
FROM THE AMERICAN JOURNAL OF PREVENTIVE MEDICINE
Key clinical point: Youth enrolled in Medicaid who commit suicide are disproportionately female, younger, and more likely to die by hanging, compared with non-Medicaid youth.
Major finding: The Medicaid group had a 28% increased risk of suicide among the 10- to 14-year age subgroup, a 14% increased risk of suicide among females, and a 26% greater risk of death by hanging.
Study details: An observational study from the 16 most populous states that includes 4,045 youth who committed suicide during 2009-2013.
Disclosures: The authors reported no financial conflicts. The study was funded by the American Foundation for Suicide Prevention and the National Institutes of Health.
Source: Fontanella CA et al. Am J Prev Med. 2019 Jan 17. doi: 10.1016/j.amepre.2018.10.008.
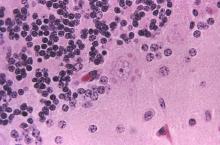
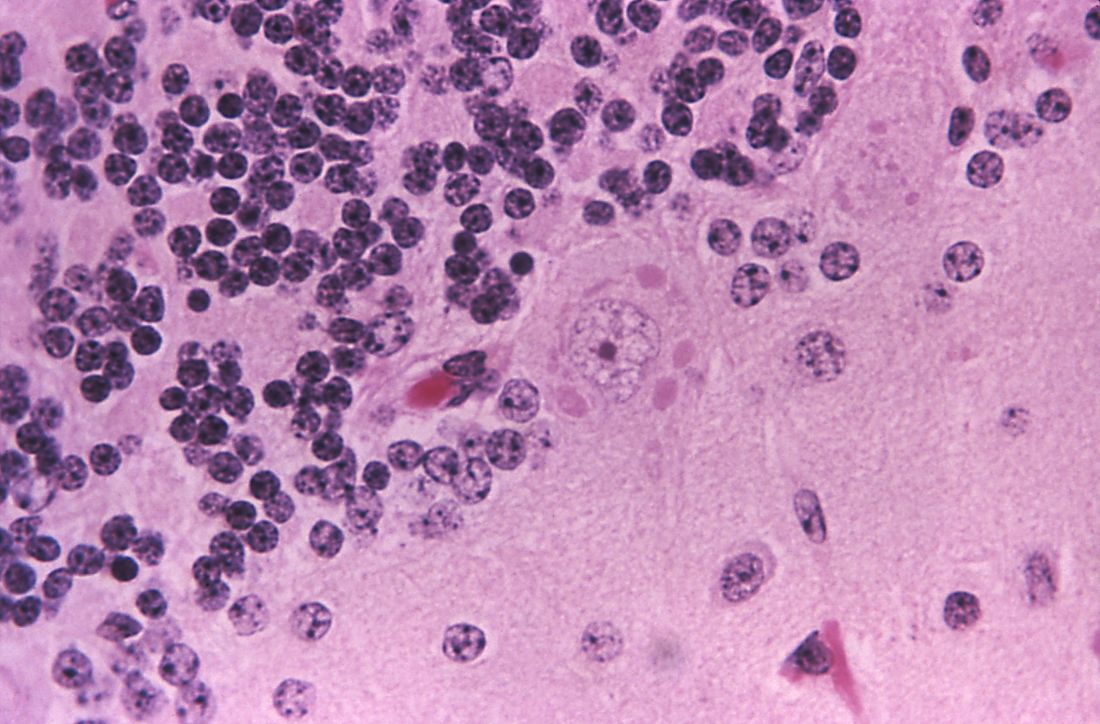
Obinutuzumab-based regimens yield durable remissions in CLL
Two different obinutuzumab-based chemoimmunotherapy regimens resulted in excellent long-term disease control as front-line therapy for chronic lymphocytic leukemia (CLL), investigators said in a follow-up report on a phase 1b study.
Both obinutuzumab plus fludarabine/cyclophosphamide (G-FC) and obinutuzumab plus bendamustine (G-B) were well tolerated, with adverse events similar to what has been reported in rituximab-containing immunotherapy regimens, they said in the report of final results from the GALTON trial.
Most evaluable patients had B-cell recovery by 36 months in the study, which included a population of CLL patients largely without 17p deletions, said Jennifer R. Brown, MD, PhD, of Dana-Farber Cancer Institute, Boston, and her coinvestigators.
“These data support moving forward with these regimens in subsequent trials, which are currently ongoing,” they said in their report on the study, which appears in Blood.
The open-label, parallel-arm, multicenter phase 1b GALTON study included 41 patients with CLL, of whom 21 received G-FC and 20 received G-B for up to six cycles of 28 days each. The median age was 60 years, and about one-third of patients had Rai stage III or IV disease. Only one patient had del(17p), and nearly half of patients tested (17 of 38 patients) had unmutated immunoglobulin heavy-chain variable region gene (IGHV). Six patients had del(11q), including four in the G-FC arm and two in the G-B arm.
Both G-FC and G-B had manageable toxicities, with infusion-related reactions being the most common adverse event, occurring in 88% (20% grade 3 or 4), Dr. Brown and her colleagues reported, adding that grade 3 or 4 neutropenia was seen in 48% of the G-FC arm and 55% of the G-B arm.
The objective response rate (ORR) was 62% for G-FC and 90% for GB.
“The ORR in the G-FC arm likely does not reflect the true activity of the regimen, as it is based on an intent-to-treat analysis,” the investigators said.
With a median observation time of 40.4 months, 95% of patients were alive, and 90% had not experienced a progression-free survival event.
Nine patients in the G-FC arm underwent minimal residual disease (MRD) testing in peripheral blood; 100% had undetectable MRD, according to the report.
“With the caveat of small patient numbers and inevitable differences in patient populations across studies, these results suggest that G-FC may clear residual disease more effectively than rituximab plus FC,” the investigators wrote.
Previous studies of R-FC showed an undetectable MRD rate of 45% or less, they said.
The study was sponsored by Genentech. The investigators reported disclosures related to Genentech/Roche and other companies.
SOURCE: Brown JR et al. Blood. 2018 Dec 28. doi: 10.1182/blood-2018-06-857714.
Two different obinutuzumab-based chemoimmunotherapy regimens resulted in excellent long-term disease control as front-line therapy for chronic lymphocytic leukemia (CLL), investigators said in a follow-up report on a phase 1b study.
Both obinutuzumab plus fludarabine/cyclophosphamide (G-FC) and obinutuzumab plus bendamustine (G-B) were well tolerated, with adverse events similar to what has been reported in rituximab-containing immunotherapy regimens, they said in the report of final results from the GALTON trial.
Most evaluable patients had B-cell recovery by 36 months in the study, which included a population of CLL patients largely without 17p deletions, said Jennifer R. Brown, MD, PhD, of Dana-Farber Cancer Institute, Boston, and her coinvestigators.
“These data support moving forward with these regimens in subsequent trials, which are currently ongoing,” they said in their report on the study, which appears in Blood.
The open-label, parallel-arm, multicenter phase 1b GALTON study included 41 patients with CLL, of whom 21 received G-FC and 20 received G-B for up to six cycles of 28 days each. The median age was 60 years, and about one-third of patients had Rai stage III or IV disease. Only one patient had del(17p), and nearly half of patients tested (17 of 38 patients) had unmutated immunoglobulin heavy-chain variable region gene (IGHV). Six patients had del(11q), including four in the G-FC arm and two in the G-B arm.
Both G-FC and G-B had manageable toxicities, with infusion-related reactions being the most common adverse event, occurring in 88% (20% grade 3 or 4), Dr. Brown and her colleagues reported, adding that grade 3 or 4 neutropenia was seen in 48% of the G-FC arm and 55% of the G-B arm.
The objective response rate (ORR) was 62% for G-FC and 90% for GB.
“The ORR in the G-FC arm likely does not reflect the true activity of the regimen, as it is based on an intent-to-treat analysis,” the investigators said.
With a median observation time of 40.4 months, 95% of patients were alive, and 90% had not experienced a progression-free survival event.
Nine patients in the G-FC arm underwent minimal residual disease (MRD) testing in peripheral blood; 100% had undetectable MRD, according to the report.
“With the caveat of small patient numbers and inevitable differences in patient populations across studies, these results suggest that G-FC may clear residual disease more effectively than rituximab plus FC,” the investigators wrote.
Previous studies of R-FC showed an undetectable MRD rate of 45% or less, they said.
The study was sponsored by Genentech. The investigators reported disclosures related to Genentech/Roche and other companies.
SOURCE: Brown JR et al. Blood. 2018 Dec 28. doi: 10.1182/blood-2018-06-857714.
Two different obinutuzumab-based chemoimmunotherapy regimens resulted in excellent long-term disease control as front-line therapy for chronic lymphocytic leukemia (CLL), investigators said in a follow-up report on a phase 1b study.
Both obinutuzumab plus fludarabine/cyclophosphamide (G-FC) and obinutuzumab plus bendamustine (G-B) were well tolerated, with adverse events similar to what has been reported in rituximab-containing immunotherapy regimens, they said in the report of final results from the GALTON trial.
Most evaluable patients had B-cell recovery by 36 months in the study, which included a population of CLL patients largely without 17p deletions, said Jennifer R. Brown, MD, PhD, of Dana-Farber Cancer Institute, Boston, and her coinvestigators.
“These data support moving forward with these regimens in subsequent trials, which are currently ongoing,” they said in their report on the study, which appears in Blood.
The open-label, parallel-arm, multicenter phase 1b GALTON study included 41 patients with CLL, of whom 21 received G-FC and 20 received G-B for up to six cycles of 28 days each. The median age was 60 years, and about one-third of patients had Rai stage III or IV disease. Only one patient had del(17p), and nearly half of patients tested (17 of 38 patients) had unmutated immunoglobulin heavy-chain variable region gene (IGHV). Six patients had del(11q), including four in the G-FC arm and two in the G-B arm.
Both G-FC and G-B had manageable toxicities, with infusion-related reactions being the most common adverse event, occurring in 88% (20% grade 3 or 4), Dr. Brown and her colleagues reported, adding that grade 3 or 4 neutropenia was seen in 48% of the G-FC arm and 55% of the G-B arm.
The objective response rate (ORR) was 62% for G-FC and 90% for GB.
“The ORR in the G-FC arm likely does not reflect the true activity of the regimen, as it is based on an intent-to-treat analysis,” the investigators said.
With a median observation time of 40.4 months, 95% of patients were alive, and 90% had not experienced a progression-free survival event.
Nine patients in the G-FC arm underwent minimal residual disease (MRD) testing in peripheral blood; 100% had undetectable MRD, according to the report.
“With the caveat of small patient numbers and inevitable differences in patient populations across studies, these results suggest that G-FC may clear residual disease more effectively than rituximab plus FC,” the investigators wrote.
Previous studies of R-FC showed an undetectable MRD rate of 45% or less, they said.
The study was sponsored by Genentech. The investigators reported disclosures related to Genentech/Roche and other companies.
SOURCE: Brown JR et al. Blood. 2018 Dec 28. doi: 10.1182/blood-2018-06-857714.
FROM BLOOD
Key clinical point:
Major finding: With a median observation time of 40.4 months, 95% of patients were alive, and 90% had not experienced a progression-free survival event.
Study details: Long-term follow-up of the phase 1b GALTON trial, including 41 patients with CLL.
Disclosures: The study was sponsored by Genentech. The study authors reported disclosures related to Genentech/Roche and other companies.
Source: Brown JR et al. Blood. 2018 Dec 28. doi: 10.1182/blood-2018-06-857714.
Online tools support hemophilia A prophylaxis changes
Online applications designed to facilitate tailoring of hemophilia A prophylaxis supported a regimen change in nearly half of patients enrolled in a recent study, investigators report.
The development of individualized pharmacokinetic profiles using those online tools may have contributed to improved adherence and decreased bleeding, according to Azusa Nagao, MD, a researcher in the department of blood coagulation at Ogikubo Hospital, Tokyo, and colleagues.
Dr. Nagao and colleagues calculated individual pharmacokinetic profiles for the 39 patients using myPKFiT for those patients receiving antihemophilic factor (recombinant) and the Web-Accessible Population Pharmacokinetic Service-Hemophilia (WAPPS-Hemo) for those using other factor concentrates.
Based on profiling results, changes to prophylaxis regimens were warranted for 20 of the 39 patients, Dr. Nagao and coresearchers reported in Thrombosis Research.
Those changes included a higher dosage of factor concentrate in eight patients, a shorter infusion interval in five patients, a change from a standard half-life product to an extended half-life product in five patients, and a reduction in prophylaxis dose for two patients.
Adherence stayed the same in patients who had a dose increase and improved for those who switched to a shorter infusion interval and for those who switched to an extended half-life product, according to the researchers.
Annualized bleeding rate significantly decreased for patients who switched to an extended half-life product (P less than .05), and there was a trend toward decrease in annualized joint bleeding rate in this group, the researchers reported.
The annualized joint bleeding rate did significantly decrease in patients without end-stage arthropathy (P less than .05), with no significant change in this outcome for those with end-stage arthropathy.
“The impact of adopting population pharmacokinetics-based treatment as measured by changes in treatment adherence and bleeding rate was modest, but the study power was limited by the characteristics of the study population,” the researchers wrote.
The myPKFiT and WAPPS-Hemo tools are designed to simplify the development of individual pharmacokinetic profiles to guide prophylaxis dosing in patients with hemophilia A, according to the researchers.
“Full [pharmacokinetic] analysis poses a big burden, especially on children and their families,” they wrote.
A full pharmacokinetic study requires a 72-hour washout period and sample collection at 10 time points over the course of about 48 hours, along with associated hospital admissions or outpatient clinic visits, they noted.
The myPKFiT application, cleared by the Food and Drug Administration for use in hemophilia A patients being treated with antihemophilic factor (recombinant), can generate an individual’s pharmacokinetic profile based on as few as two blood samples, according to a news release from Shire.
Nagao reported receiving a research grant from Shire unrelated to this study. One coauthor also reported disclosures related to Shire, Bayer, Pfizer, Novo Nordisk, CSL Behring, and others.
SOURCE: Nagao A et al. Thromb Res. 2019 Jan;173:79-84.
Online applications designed to facilitate tailoring of hemophilia A prophylaxis supported a regimen change in nearly half of patients enrolled in a recent study, investigators report.
The development of individualized pharmacokinetic profiles using those online tools may have contributed to improved adherence and decreased bleeding, according to Azusa Nagao, MD, a researcher in the department of blood coagulation at Ogikubo Hospital, Tokyo, and colleagues.
Dr. Nagao and colleagues calculated individual pharmacokinetic profiles for the 39 patients using myPKFiT for those patients receiving antihemophilic factor (recombinant) and the Web-Accessible Population Pharmacokinetic Service-Hemophilia (WAPPS-Hemo) for those using other factor concentrates.
Based on profiling results, changes to prophylaxis regimens were warranted for 20 of the 39 patients, Dr. Nagao and coresearchers reported in Thrombosis Research.
Those changes included a higher dosage of factor concentrate in eight patients, a shorter infusion interval in five patients, a change from a standard half-life product to an extended half-life product in five patients, and a reduction in prophylaxis dose for two patients.
Adherence stayed the same in patients who had a dose increase and improved for those who switched to a shorter infusion interval and for those who switched to an extended half-life product, according to the researchers.
Annualized bleeding rate significantly decreased for patients who switched to an extended half-life product (P less than .05), and there was a trend toward decrease in annualized joint bleeding rate in this group, the researchers reported.
The annualized joint bleeding rate did significantly decrease in patients without end-stage arthropathy (P less than .05), with no significant change in this outcome for those with end-stage arthropathy.
“The impact of adopting population pharmacokinetics-based treatment as measured by changes in treatment adherence and bleeding rate was modest, but the study power was limited by the characteristics of the study population,” the researchers wrote.
The myPKFiT and WAPPS-Hemo tools are designed to simplify the development of individual pharmacokinetic profiles to guide prophylaxis dosing in patients with hemophilia A, according to the researchers.
“Full [pharmacokinetic] analysis poses a big burden, especially on children and their families,” they wrote.
A full pharmacokinetic study requires a 72-hour washout period and sample collection at 10 time points over the course of about 48 hours, along with associated hospital admissions or outpatient clinic visits, they noted.
The myPKFiT application, cleared by the Food and Drug Administration for use in hemophilia A patients being treated with antihemophilic factor (recombinant), can generate an individual’s pharmacokinetic profile based on as few as two blood samples, according to a news release from Shire.
Nagao reported receiving a research grant from Shire unrelated to this study. One coauthor also reported disclosures related to Shire, Bayer, Pfizer, Novo Nordisk, CSL Behring, and others.
SOURCE: Nagao A et al. Thromb Res. 2019 Jan;173:79-84.
Online applications designed to facilitate tailoring of hemophilia A prophylaxis supported a regimen change in nearly half of patients enrolled in a recent study, investigators report.
The development of individualized pharmacokinetic profiles using those online tools may have contributed to improved adherence and decreased bleeding, according to Azusa Nagao, MD, a researcher in the department of blood coagulation at Ogikubo Hospital, Tokyo, and colleagues.
Dr. Nagao and colleagues calculated individual pharmacokinetic profiles for the 39 patients using myPKFiT for those patients receiving antihemophilic factor (recombinant) and the Web-Accessible Population Pharmacokinetic Service-Hemophilia (WAPPS-Hemo) for those using other factor concentrates.
Based on profiling results, changes to prophylaxis regimens were warranted for 20 of the 39 patients, Dr. Nagao and coresearchers reported in Thrombosis Research.
Those changes included a higher dosage of factor concentrate in eight patients, a shorter infusion interval in five patients, a change from a standard half-life product to an extended half-life product in five patients, and a reduction in prophylaxis dose for two patients.
Adherence stayed the same in patients who had a dose increase and improved for those who switched to a shorter infusion interval and for those who switched to an extended half-life product, according to the researchers.
Annualized bleeding rate significantly decreased for patients who switched to an extended half-life product (P less than .05), and there was a trend toward decrease in annualized joint bleeding rate in this group, the researchers reported.
The annualized joint bleeding rate did significantly decrease in patients without end-stage arthropathy (P less than .05), with no significant change in this outcome for those with end-stage arthropathy.
“The impact of adopting population pharmacokinetics-based treatment as measured by changes in treatment adherence and bleeding rate was modest, but the study power was limited by the characteristics of the study population,” the researchers wrote.
The myPKFiT and WAPPS-Hemo tools are designed to simplify the development of individual pharmacokinetic profiles to guide prophylaxis dosing in patients with hemophilia A, according to the researchers.
“Full [pharmacokinetic] analysis poses a big burden, especially on children and their families,” they wrote.
A full pharmacokinetic study requires a 72-hour washout period and sample collection at 10 time points over the course of about 48 hours, along with associated hospital admissions or outpatient clinic visits, they noted.
The myPKFiT application, cleared by the Food and Drug Administration for use in hemophilia A patients being treated with antihemophilic factor (recombinant), can generate an individual’s pharmacokinetic profile based on as few as two blood samples, according to a news release from Shire.
Nagao reported receiving a research grant from Shire unrelated to this study. One coauthor also reported disclosures related to Shire, Bayer, Pfizer, Novo Nordisk, CSL Behring, and others.
SOURCE: Nagao A et al. Thromb Res. 2019 Jan;173:79-84.
FROM THROMBOSIS RESEARCH
Key clinical point:
Major finding: Adherence stayed the same or improved in patients whose prophylaxis regimens were changed based on the tool results, while bleeding rates improved for specific patient subsets.
Study details: Prospective study including 39 patients receiving hemophilia A prophylaxis.
Disclosures: Study authors reported disclosures related to Shire, Bayer, Pfizer, Novo Nordisk, CSL Behring, and others.
Source: Nagao A et al. Thromb Res. 2019 Jan;173:79-84.
HDL-P subfractions may be prognostic in heart failure
In heart failure, derangements in HDL cholesterol particle (HDL-P) subfractions have prognostic implications beyond those of conventional cardiovascular risk factors, according to investigators who analyzed plasma samples from more than 6,500 patients.
The study revealed derangements that were shared and more severe in heart failure with reduced ejection fraction (HFrEF) as compared to heart failure with preserved ejection fraction (HFpEF), according to the researchers, who said their study is the largest to date of HDL-P subfractions in heart failure.
Both total HDL-P and small HDL-P had a strong inverse association with adverse outcomes, consistent with the conclusions of previous studies, they said in a report on their study in the Journal of the American College of Cardiology.
“Altogether, our findings support total and small HDL-P as important markers of residual risk in both HFrEF and HFpEF,” said the investigators, led by Wynn G. Hunter, MD, of Duke University, Durham, N.C.
Dr. Hunter and colleagues used the CATHGEN (Catheterization Genetics) biorepository to identify plasma samples obtained at catheterization for 782 patients with HFrEF, 1,004 with HFpEF, and 4,742 with no heart failure.
Lipoprotein profiling of the samples revealed that mean HDL-P size was greater in HFrEF than in HFpEF, and in both of those cases, mean HDL-P size was greater than in patients with no heart failure (P less than .0001), investigators reported.
Concentrations of small HDL-P and total HDL-P were by contrast lower in HFrEF versus HFpEF, and again, the values for both HFrEF and HFpEF were lower than in patients without heart failure (P less than .0001), they added.
Small HDL-P and total HDL-P had an inverse association with time to adverse events and all-cause mortality for both the HFrEF and HFpEF groups, according to investigators, who said those links remained robust even after multivariate adjustment for 14 cardiovascular risk factors, including diabetes, LDL particle, and GlycA, a marker of inflammation.
For example, small HDL-P and total HDL-P were inversely associated with all-cause mortality risk, with adjusted hazard ratios of 0.69-0.79 (P less than .0001), they reported. Similarly, a greater mean HDL-P size was associated with increased risk of all-cause mortality, yielding adjusted hazard ratios of 1.23-1.46 (P less than .0001).
Further studies are needed to clarify the role of HDL-P in the pathophysiology of heart failure, and to identify treatments that might increase total and small HDL-P in heart failure patients, Dr. Hunter and coauthors concluded.
Dr. Hunter reported no disclosures related to the study. Coauthors provided disclosures related to Amgen, Ostuka, Roche Diagnostics, Novartis, Trevena, Singulex, Medtronic, AstraZeneca, Bristol-Myers Squibb, Janssen, Portola, Boston Scientific, Gilead, GlaxoSmithKline, Merck, Alnylam, Ikaria Pharmaceuticals, Pfizer, Philips, LipoScience, and Pfizer, among others.
SOURCE: Hunter WG et al. J Am Coll Cardiol. 2019 Jan 22;73(2):177-86.
Although the study by Dr. Hunter and colleagues confirms the role of HDL cholesterol and HDL-P subfractions in heart failure, the immediate clinical implications of their findings are uncertain.
However, clinical use as a biomarker remains a “distant vision,” in part because a useful biomarker must be proven to provide an incremental benefit in terms of reducing disease-associated morbidity or mortality.
Even so, the present study could begin to inform future therapeutic studies looking at increasing specific HDL-P subfractions, rather than increasing HDL cholesterol across the board.
“Perhaps, this study will possibly serve to spur investigation into therapies designed to reduce derangements of [HDL cholesterol] metabolism and primarily target HDL-P as a regulator molecule, a promise that may keep the HDL story alive into the near future of scientific excursion.”
These comments were taken from an accompanying editorial by Hector O. Ventura, MD, and Carl J. Lavie, MD, of the University of Queensland Ochsner Clinical School, Brisbane, Australia, and New Orleans; and Mandeep R. Mehra, MD, of the Center of Advanced Heart Disease, Harvard University, Boston (J Am Coll Cardiol 2019 Jan 22;73[2]:187-9). Dr. Mehra reported that he is a consultant for Abbott, Medtronic, nupulseCV, Portola, Bayer, and FineHeart.
Although the study by Dr. Hunter and colleagues confirms the role of HDL cholesterol and HDL-P subfractions in heart failure, the immediate clinical implications of their findings are uncertain.
However, clinical use as a biomarker remains a “distant vision,” in part because a useful biomarker must be proven to provide an incremental benefit in terms of reducing disease-associated morbidity or mortality.
Even so, the present study could begin to inform future therapeutic studies looking at increasing specific HDL-P subfractions, rather than increasing HDL cholesterol across the board.
“Perhaps, this study will possibly serve to spur investigation into therapies designed to reduce derangements of [HDL cholesterol] metabolism and primarily target HDL-P as a regulator molecule, a promise that may keep the HDL story alive into the near future of scientific excursion.”
These comments were taken from an accompanying editorial by Hector O. Ventura, MD, and Carl J. Lavie, MD, of the University of Queensland Ochsner Clinical School, Brisbane, Australia, and New Orleans; and Mandeep R. Mehra, MD, of the Center of Advanced Heart Disease, Harvard University, Boston (J Am Coll Cardiol 2019 Jan 22;73[2]:187-9). Dr. Mehra reported that he is a consultant for Abbott, Medtronic, nupulseCV, Portola, Bayer, and FineHeart.
Although the study by Dr. Hunter and colleagues confirms the role of HDL cholesterol and HDL-P subfractions in heart failure, the immediate clinical implications of their findings are uncertain.
However, clinical use as a biomarker remains a “distant vision,” in part because a useful biomarker must be proven to provide an incremental benefit in terms of reducing disease-associated morbidity or mortality.
Even so, the present study could begin to inform future therapeutic studies looking at increasing specific HDL-P subfractions, rather than increasing HDL cholesterol across the board.
“Perhaps, this study will possibly serve to spur investigation into therapies designed to reduce derangements of [HDL cholesterol] metabolism and primarily target HDL-P as a regulator molecule, a promise that may keep the HDL story alive into the near future of scientific excursion.”
These comments were taken from an accompanying editorial by Hector O. Ventura, MD, and Carl J. Lavie, MD, of the University of Queensland Ochsner Clinical School, Brisbane, Australia, and New Orleans; and Mandeep R. Mehra, MD, of the Center of Advanced Heart Disease, Harvard University, Boston (J Am Coll Cardiol 2019 Jan 22;73[2]:187-9). Dr. Mehra reported that he is a consultant for Abbott, Medtronic, nupulseCV, Portola, Bayer, and FineHeart.
In heart failure, derangements in HDL cholesterol particle (HDL-P) subfractions have prognostic implications beyond those of conventional cardiovascular risk factors, according to investigators who analyzed plasma samples from more than 6,500 patients.
The study revealed derangements that were shared and more severe in heart failure with reduced ejection fraction (HFrEF) as compared to heart failure with preserved ejection fraction (HFpEF), according to the researchers, who said their study is the largest to date of HDL-P subfractions in heart failure.
Both total HDL-P and small HDL-P had a strong inverse association with adverse outcomes, consistent with the conclusions of previous studies, they said in a report on their study in the Journal of the American College of Cardiology.
“Altogether, our findings support total and small HDL-P as important markers of residual risk in both HFrEF and HFpEF,” said the investigators, led by Wynn G. Hunter, MD, of Duke University, Durham, N.C.
Dr. Hunter and colleagues used the CATHGEN (Catheterization Genetics) biorepository to identify plasma samples obtained at catheterization for 782 patients with HFrEF, 1,004 with HFpEF, and 4,742 with no heart failure.
Lipoprotein profiling of the samples revealed that mean HDL-P size was greater in HFrEF than in HFpEF, and in both of those cases, mean HDL-P size was greater than in patients with no heart failure (P less than .0001), investigators reported.
Concentrations of small HDL-P and total HDL-P were by contrast lower in HFrEF versus HFpEF, and again, the values for both HFrEF and HFpEF were lower than in patients without heart failure (P less than .0001), they added.
Small HDL-P and total HDL-P had an inverse association with time to adverse events and all-cause mortality for both the HFrEF and HFpEF groups, according to investigators, who said those links remained robust even after multivariate adjustment for 14 cardiovascular risk factors, including diabetes, LDL particle, and GlycA, a marker of inflammation.
For example, small HDL-P and total HDL-P were inversely associated with all-cause mortality risk, with adjusted hazard ratios of 0.69-0.79 (P less than .0001), they reported. Similarly, a greater mean HDL-P size was associated with increased risk of all-cause mortality, yielding adjusted hazard ratios of 1.23-1.46 (P less than .0001).
Further studies are needed to clarify the role of HDL-P in the pathophysiology of heart failure, and to identify treatments that might increase total and small HDL-P in heart failure patients, Dr. Hunter and coauthors concluded.
Dr. Hunter reported no disclosures related to the study. Coauthors provided disclosures related to Amgen, Ostuka, Roche Diagnostics, Novartis, Trevena, Singulex, Medtronic, AstraZeneca, Bristol-Myers Squibb, Janssen, Portola, Boston Scientific, Gilead, GlaxoSmithKline, Merck, Alnylam, Ikaria Pharmaceuticals, Pfizer, Philips, LipoScience, and Pfizer, among others.
SOURCE: Hunter WG et al. J Am Coll Cardiol. 2019 Jan 22;73(2):177-86.
In heart failure, derangements in HDL cholesterol particle (HDL-P) subfractions have prognostic implications beyond those of conventional cardiovascular risk factors, according to investigators who analyzed plasma samples from more than 6,500 patients.
The study revealed derangements that were shared and more severe in heart failure with reduced ejection fraction (HFrEF) as compared to heart failure with preserved ejection fraction (HFpEF), according to the researchers, who said their study is the largest to date of HDL-P subfractions in heart failure.
Both total HDL-P and small HDL-P had a strong inverse association with adverse outcomes, consistent with the conclusions of previous studies, they said in a report on their study in the Journal of the American College of Cardiology.
“Altogether, our findings support total and small HDL-P as important markers of residual risk in both HFrEF and HFpEF,” said the investigators, led by Wynn G. Hunter, MD, of Duke University, Durham, N.C.
Dr. Hunter and colleagues used the CATHGEN (Catheterization Genetics) biorepository to identify plasma samples obtained at catheterization for 782 patients with HFrEF, 1,004 with HFpEF, and 4,742 with no heart failure.
Lipoprotein profiling of the samples revealed that mean HDL-P size was greater in HFrEF than in HFpEF, and in both of those cases, mean HDL-P size was greater than in patients with no heart failure (P less than .0001), investigators reported.
Concentrations of small HDL-P and total HDL-P were by contrast lower in HFrEF versus HFpEF, and again, the values for both HFrEF and HFpEF were lower than in patients without heart failure (P less than .0001), they added.
Small HDL-P and total HDL-P had an inverse association with time to adverse events and all-cause mortality for both the HFrEF and HFpEF groups, according to investigators, who said those links remained robust even after multivariate adjustment for 14 cardiovascular risk factors, including diabetes, LDL particle, and GlycA, a marker of inflammation.
For example, small HDL-P and total HDL-P were inversely associated with all-cause mortality risk, with adjusted hazard ratios of 0.69-0.79 (P less than .0001), they reported. Similarly, a greater mean HDL-P size was associated with increased risk of all-cause mortality, yielding adjusted hazard ratios of 1.23-1.46 (P less than .0001).
Further studies are needed to clarify the role of HDL-P in the pathophysiology of heart failure, and to identify treatments that might increase total and small HDL-P in heart failure patients, Dr. Hunter and coauthors concluded.
Dr. Hunter reported no disclosures related to the study. Coauthors provided disclosures related to Amgen, Ostuka, Roche Diagnostics, Novartis, Trevena, Singulex, Medtronic, AstraZeneca, Bristol-Myers Squibb, Janssen, Portola, Boston Scientific, Gilead, GlaxoSmithKline, Merck, Alnylam, Ikaria Pharmaceuticals, Pfizer, Philips, LipoScience, and Pfizer, among others.
SOURCE: Hunter WG et al. J Am Coll Cardiol. 2019 Jan 22;73(2):177-86.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Key clinical point: Derangements in HDL particle (HDL-P) subfractions may have prognostic implications in patients with heart failure with reduced or preserved ejection fraction.
Major finding: (P less than .0001).
Study details: Study based on lipid profiling of more than 6,500 plasma samples obtained at catheterization.
Disclosures: Study authors provided disclosures related to Amgen, Ostuka, Roche Diagnostics, Novartis, Medtronic, and others.
Source: Hunter WG et al. J Am Coll Cardiol. 2019 Jan 22;73(2):177-86.
Lung screening complications costly, more prevalent than in trial setting
The real-world rate of is substantially higher than in clinical trials, a study suggests.
Those complications related to low-dose computed tomography (LDCT) screening are potentially costly, according to the analysis of commercial and Medicare claims data for nearly 350,000 individuals.
While tentative, these results emphasize the need to discuss the risk of adverse events and their costs as part of the shared decision-making process between physicians and patients, researchers said in a report on their study in JAMA Internal Medicine.
“As the number of individuals seeking lung cancer screening with LDCT increases, so too will the number of individuals undergoing invasive diagnostic procedures as a results of abnormal findings,” said Jinhai Huo, MD, PhD, of the department of health services research, management, and policy at the University of Florida, Gainesville.
The retrospective cohort study included 174,702 individuals who underwent an invasive diagnostic procedure related to lung cancer screening and 169,808 control subjects.
All individuals studied were between 55 and 77 years old, the targeted age range for lung cancer screening specified by the Centers for Medicare & Medicaid Services.
Complication rates were about twice as high as they were in the landmark National Lung Screening Trial (NLST), both for a younger cohort of individuals aged 55-64 years, and an older Medicare age group of individuals aged 65 to 77 years, Dr. Huo and coinvestigators reported.
The estimated rate of complications was 22.0% (95% confidence interval, 21.7%-22.7%) in the younger age group, and even higher in the older age group, at 23.8% (95% CI, 23.0%-24.6%), according to investigators. By contrast, complication rates in the NLST were 9.8% and 8.5% for younger and older age cohorts, respectively.
The cost of managing postprocedural complications was higher than the cost of the diagnostic procedures, investigators said.
Mean costs ranged from $6,320 for minor complications to $56,845 for major complications, they reported.
The most common invasive diagnostic procedure in the study cohort was cytology test or biopsy in 26.1%, followed by bronchoscopy in 25.6%, according to study data. Another 5.4% underwent thoracic surgery.
In a previous Medicare advisory committee meeting, some experts expressed concern that complication rates in settings outside of the NLST would be higher than what was reported in that study, Dr. Huo and coauthors noted in their report.
“Our findings echoed this concern,” they said in a discussion of their results.
Dr. Huo and coauthors reported no conflicts of interest related to the research, which was supported in part by grants or fellowships from the University of Texas MD Anderson Cancer Center, the University of Florida, the National Cancer Institute, and the National Institutes of Health.
SOURCE: Huo J et al. JAMA Intern Med. 2019 Jan 14.
“The conversations that are occurring about lung cancer screening are woefully inadequate and do not discuss harms,” wrote Rita F. Redberg, MD, in an editorial note. Shared decision-making visits were made mandatory prior to lung cancer screening by the Centers for Medicare & Medicaid Services. That decision was made because of an evidence review suggesting a “low likelihood” that benefits of lung cancer screening would exceed harms in the Medicare population, Dr. Redberg wrote. Despite that, most Medicare beneficiaries are not having the required visit for shared decision making before they undergo the CT scan.
“It is likely that patients’ decisions not to undergo low-dose computed tomography for lung cancer screening are driven by the high false-positive rate, high chance of incidental findings, and subsequent need for invasive procedures, and small chance of benefit,” she said in her comment.
Shared decision-making visits are also rarely happening in the privately insured population, as shown in previous research, Dr. Redberg noted.
She reported no conflicts of interest related to her Editor’s Note, which appears in JAMA Internal Medicine (2019 Jan 14).
Dr. Redberg is with the department of medicine, University of California, San Francisco.
“The conversations that are occurring about lung cancer screening are woefully inadequate and do not discuss harms,” wrote Rita F. Redberg, MD, in an editorial note. Shared decision-making visits were made mandatory prior to lung cancer screening by the Centers for Medicare & Medicaid Services. That decision was made because of an evidence review suggesting a “low likelihood” that benefits of lung cancer screening would exceed harms in the Medicare population, Dr. Redberg wrote. Despite that, most Medicare beneficiaries are not having the required visit for shared decision making before they undergo the CT scan.
“It is likely that patients’ decisions not to undergo low-dose computed tomography for lung cancer screening are driven by the high false-positive rate, high chance of incidental findings, and subsequent need for invasive procedures, and small chance of benefit,” she said in her comment.
Shared decision-making visits are also rarely happening in the privately insured population, as shown in previous research, Dr. Redberg noted.
She reported no conflicts of interest related to her Editor’s Note, which appears in JAMA Internal Medicine (2019 Jan 14).
Dr. Redberg is with the department of medicine, University of California, San Francisco.
“The conversations that are occurring about lung cancer screening are woefully inadequate and do not discuss harms,” wrote Rita F. Redberg, MD, in an editorial note. Shared decision-making visits were made mandatory prior to lung cancer screening by the Centers for Medicare & Medicaid Services. That decision was made because of an evidence review suggesting a “low likelihood” that benefits of lung cancer screening would exceed harms in the Medicare population, Dr. Redberg wrote. Despite that, most Medicare beneficiaries are not having the required visit for shared decision making before they undergo the CT scan.
“It is likely that patients’ decisions not to undergo low-dose computed tomography for lung cancer screening are driven by the high false-positive rate, high chance of incidental findings, and subsequent need for invasive procedures, and small chance of benefit,” she said in her comment.
Shared decision-making visits are also rarely happening in the privately insured population, as shown in previous research, Dr. Redberg noted.
She reported no conflicts of interest related to her Editor’s Note, which appears in JAMA Internal Medicine (2019 Jan 14).
Dr. Redberg is with the department of medicine, University of California, San Francisco.
The real-world rate of is substantially higher than in clinical trials, a study suggests.
Those complications related to low-dose computed tomography (LDCT) screening are potentially costly, according to the analysis of commercial and Medicare claims data for nearly 350,000 individuals.
While tentative, these results emphasize the need to discuss the risk of adverse events and their costs as part of the shared decision-making process between physicians and patients, researchers said in a report on their study in JAMA Internal Medicine.
“As the number of individuals seeking lung cancer screening with LDCT increases, so too will the number of individuals undergoing invasive diagnostic procedures as a results of abnormal findings,” said Jinhai Huo, MD, PhD, of the department of health services research, management, and policy at the University of Florida, Gainesville.
The retrospective cohort study included 174,702 individuals who underwent an invasive diagnostic procedure related to lung cancer screening and 169,808 control subjects.
All individuals studied were between 55 and 77 years old, the targeted age range for lung cancer screening specified by the Centers for Medicare & Medicaid Services.
Complication rates were about twice as high as they were in the landmark National Lung Screening Trial (NLST), both for a younger cohort of individuals aged 55-64 years, and an older Medicare age group of individuals aged 65 to 77 years, Dr. Huo and coinvestigators reported.
The estimated rate of complications was 22.0% (95% confidence interval, 21.7%-22.7%) in the younger age group, and even higher in the older age group, at 23.8% (95% CI, 23.0%-24.6%), according to investigators. By contrast, complication rates in the NLST were 9.8% and 8.5% for younger and older age cohorts, respectively.
The cost of managing postprocedural complications was higher than the cost of the diagnostic procedures, investigators said.
Mean costs ranged from $6,320 for minor complications to $56,845 for major complications, they reported.
The most common invasive diagnostic procedure in the study cohort was cytology test or biopsy in 26.1%, followed by bronchoscopy in 25.6%, according to study data. Another 5.4% underwent thoracic surgery.
In a previous Medicare advisory committee meeting, some experts expressed concern that complication rates in settings outside of the NLST would be higher than what was reported in that study, Dr. Huo and coauthors noted in their report.
“Our findings echoed this concern,” they said in a discussion of their results.
Dr. Huo and coauthors reported no conflicts of interest related to the research, which was supported in part by grants or fellowships from the University of Texas MD Anderson Cancer Center, the University of Florida, the National Cancer Institute, and the National Institutes of Health.
SOURCE: Huo J et al. JAMA Intern Med. 2019 Jan 14.
The real-world rate of is substantially higher than in clinical trials, a study suggests.
Those complications related to low-dose computed tomography (LDCT) screening are potentially costly, according to the analysis of commercial and Medicare claims data for nearly 350,000 individuals.
While tentative, these results emphasize the need to discuss the risk of adverse events and their costs as part of the shared decision-making process between physicians and patients, researchers said in a report on their study in JAMA Internal Medicine.
“As the number of individuals seeking lung cancer screening with LDCT increases, so too will the number of individuals undergoing invasive diagnostic procedures as a results of abnormal findings,” said Jinhai Huo, MD, PhD, of the department of health services research, management, and policy at the University of Florida, Gainesville.
The retrospective cohort study included 174,702 individuals who underwent an invasive diagnostic procedure related to lung cancer screening and 169,808 control subjects.
All individuals studied were between 55 and 77 years old, the targeted age range for lung cancer screening specified by the Centers for Medicare & Medicaid Services.
Complication rates were about twice as high as they were in the landmark National Lung Screening Trial (NLST), both for a younger cohort of individuals aged 55-64 years, and an older Medicare age group of individuals aged 65 to 77 years, Dr. Huo and coinvestigators reported.
The estimated rate of complications was 22.0% (95% confidence interval, 21.7%-22.7%) in the younger age group, and even higher in the older age group, at 23.8% (95% CI, 23.0%-24.6%), according to investigators. By contrast, complication rates in the NLST were 9.8% and 8.5% for younger and older age cohorts, respectively.
The cost of managing postprocedural complications was higher than the cost of the diagnostic procedures, investigators said.
Mean costs ranged from $6,320 for minor complications to $56,845 for major complications, they reported.
The most common invasive diagnostic procedure in the study cohort was cytology test or biopsy in 26.1%, followed by bronchoscopy in 25.6%, according to study data. Another 5.4% underwent thoracic surgery.
In a previous Medicare advisory committee meeting, some experts expressed concern that complication rates in settings outside of the NLST would be higher than what was reported in that study, Dr. Huo and coauthors noted in their report.
“Our findings echoed this concern,” they said in a discussion of their results.
Dr. Huo and coauthors reported no conflicts of interest related to the research, which was supported in part by grants or fellowships from the University of Texas MD Anderson Cancer Center, the University of Florida, the National Cancer Institute, and the National Institutes of Health.
SOURCE: Huo J et al. JAMA Intern Med. 2019 Jan 14.
FROM JAMA INTERNAL MEDICINE
Key clinical point: The risk of complications following lung cancer screening is higher in a real-world setting as compared with the landmark National Lung Screening Trial (NLST).
Major finding: Estimated complication rates were 22.0%-23.8%, compared with 8.5%-9.8% in the NLST.
Study details: A retrospective cohort study including 174,702 individuals who underwent an invasive diagnostic procedure related to lung cancer screening and 169,808 controls.
Disclosures: Authors reported no conflicts of interest. The research was supported in part by grants or fellowships from the University of Texas MD Anderson Cancer Center, the University of Florida, the National Cancer Institute, and the National Institutes of Health.
Source: Huo J et al. JAMA Intern Med. 2019 Jan 14.
New hypopnea criteria ID unique OSA patient subset
The latest recommended criteria for hypopnea define a distinct group of patients who report substantial daytime sleepiness but with no significant cardiovascular risk, investigators reported in a retrospective, cross-sectional analysis.
The number of obstructive sleep apnea (OSA) diagnoses increased by nearly 13% when using the 2012 American Academy of Sleep Medicine (AASM) criteria of ≥ 3% desaturation or arousal, instead of the 2007 criteria of ≥ 4% desaturation, according to investigators.
While cardiovascular disease risk did not appear to be elevated in those with an OSA diagnosis based on the newer, more inclusive criteria, reported lead author Christine H.J. Won, MD, of Yale University, New Haven, Conn., and her coinvestigators.
“Our findings suggest [that] a more inclusive hypopnea definition alters OSA severity categorization, identifies a new symptomatic group of patients with predominantly mild OSA without increased cardiovascular odds, and does not ameliorate the increased odds predicted by severe OSA for arrhythmias,” the investigators wrote in the Journal of Clinical Sleep Medicine.
The analysis by Dr. Won and her colleagues included 1,400 veterans who had polysomnography for suspected sleep-disordered breathing. Of those veterans, two-thirds (932; 66%) had an OSA diagnosis based on the ≥ 4% desaturation criteria.
With the newer criteria of ≥ 3% desaturation or arousal, another 175 OSA diagnoses were captured out of the remaining 468 previously negative studies, meaning that more than 37% of those patients would be recategorized as having OSA, Dr. Won and her coauthors said.
Compared with individuals with OSA classified by the older, more restrictive criteria, the 175 individuals in this “new OSA” group were younger and less likely to be obese, though they were still more likely to be obese, compared with individuals with no OSA diagnosis, according to the authors.
The new OSA group had more disrupted sleep architecture, significantly worse oxygen saturations, and more self-reported sleepiness on the Epworth Sleepiness Scale as compared with those with no OSA, they added.
Adding in the new OSA group redistributed disease severity, with a relative increase of 21.4% for mild and 21.3% for moderate OSA, but just 15.3% for severe OSA. “Most of the [new OSA] category consisted of mild sleep-disordered breathing,” said Dr. Won and her coauthors in the report.
While there was a statistically significant increase in odds ratio for arrhythmias using the older criteria, reclassifying OSA severity using the newer definition meant that mild and moderate disease lost predictive value. However, severe OSA by the new criteria remained a significant predictor of arrhythmias, the authors said.
Odds ratios for ischemic heart disease and heart failure were numerically higher in the new OSA group versus the no OSA group, though no statistically significant differences were found, according to investigators.
This is thought to be the first study to describe a unique group of patients who escape OSA diagnosis based on the ≥ 4% desaturation criteria but are captured ≥ 3% desaturation or arousal criteria, Dr. Won and her coauthors said.
Further studies would be helpful to evaluate other polysomnographic features in this group to see how they affect cardiovascular or other health risks, they added.
“It would also be important to assess whether treatment in any of these groups leads to improved cardiovascular health, or whether treatment of the [new OSA] group leads to improved daytime sleepiness or quality of life,” they said in the report.
The researchers reported no conflicts of interest related to their work, which was performed at the Veterans Affairs Healthcare System in West Haven, Conn.; Indianapolis; and Cleveland.
SOURCE: Won CHJ et al. J Clin Sleep Med. 2018 Dec 15;14[12]:1987-94.
The study by Won and colleagues provides a “useful perspective” on how hypopnea is defined by including outcome data based on the two different scoring criteria, according to Kenneth R. Casey, MD, MPH, and Rachna Tiwari, MBBS.
Results of the study suggest a rationale for using both the 2007 American Academy of Sleep Medicine hypopnea criteria based on ≥ 4% desaturation, and the updated 2012 AASM criteria based on ≥ 3% desaturation or arousal in the evaluation of polysomnography results, Dr. Casey and Dr. Tiwari said in a commentary accompanying the study.
“This perspective may ultimately be the solution to the confusion caused by competing functional definitions of hypopnea,” they said in the commentary published in the Journal of Clinical Sleep Medicine.
The 2007 recommended criteria of ≥ 4% desaturation seemed reasonable based on available evidence at the time, but was not rigorously based by today’s standards, the authors said.
At that time, they also proposed the new alternative criteria based on ≥ 3% desaturation or an arousal, which in 2012 became elevated to a recommended rule. However, the previous recommended rule was kept to accommodate patients who required Centers for Medicare & Medicaid Services reimbursement, according to Dr. Casey and Dr. Tiwari.
Subsequent studies demonstrated “significant differences” in apnea-hypopnea index results, depending on which scoring criteria were used, they added.
“This confusing, vacillating definition has created a rather bizarre, and perhaps unsettling, situation wherein the severity of the diagnosis of sleep-disordered breathing, and perhaps its presence or absence, is determined by the patient’s insurance coverage,” they said in the commentary.
Dr. Casey and Dr. Tiwari are with the University of Wisconsin and William S. Middleton Memorial Veterans Hospital, both in Madison. They reported no conflicts of interest related to their editorial, which appears in the Journal of Clinical Sleep Medicine.
The study by Won and colleagues provides a “useful perspective” on how hypopnea is defined by including outcome data based on the two different scoring criteria, according to Kenneth R. Casey, MD, MPH, and Rachna Tiwari, MBBS.
Results of the study suggest a rationale for using both the 2007 American Academy of Sleep Medicine hypopnea criteria based on ≥ 4% desaturation, and the updated 2012 AASM criteria based on ≥ 3% desaturation or arousal in the evaluation of polysomnography results, Dr. Casey and Dr. Tiwari said in a commentary accompanying the study.
“This perspective may ultimately be the solution to the confusion caused by competing functional definitions of hypopnea,” they said in the commentary published in the Journal of Clinical Sleep Medicine.
The 2007 recommended criteria of ≥ 4% desaturation seemed reasonable based on available evidence at the time, but was not rigorously based by today’s standards, the authors said.
At that time, they also proposed the new alternative criteria based on ≥ 3% desaturation or an arousal, which in 2012 became elevated to a recommended rule. However, the previous recommended rule was kept to accommodate patients who required Centers for Medicare & Medicaid Services reimbursement, according to Dr. Casey and Dr. Tiwari.
Subsequent studies demonstrated “significant differences” in apnea-hypopnea index results, depending on which scoring criteria were used, they added.
“This confusing, vacillating definition has created a rather bizarre, and perhaps unsettling, situation wherein the severity of the diagnosis of sleep-disordered breathing, and perhaps its presence or absence, is determined by the patient’s insurance coverage,” they said in the commentary.
Dr. Casey and Dr. Tiwari are with the University of Wisconsin and William S. Middleton Memorial Veterans Hospital, both in Madison. They reported no conflicts of interest related to their editorial, which appears in the Journal of Clinical Sleep Medicine.
The study by Won and colleagues provides a “useful perspective” on how hypopnea is defined by including outcome data based on the two different scoring criteria, according to Kenneth R. Casey, MD, MPH, and Rachna Tiwari, MBBS.
Results of the study suggest a rationale for using both the 2007 American Academy of Sleep Medicine hypopnea criteria based on ≥ 4% desaturation, and the updated 2012 AASM criteria based on ≥ 3% desaturation or arousal in the evaluation of polysomnography results, Dr. Casey and Dr. Tiwari said in a commentary accompanying the study.
“This perspective may ultimately be the solution to the confusion caused by competing functional definitions of hypopnea,” they said in the commentary published in the Journal of Clinical Sleep Medicine.
The 2007 recommended criteria of ≥ 4% desaturation seemed reasonable based on available evidence at the time, but was not rigorously based by today’s standards, the authors said.
At that time, they also proposed the new alternative criteria based on ≥ 3% desaturation or an arousal, which in 2012 became elevated to a recommended rule. However, the previous recommended rule was kept to accommodate patients who required Centers for Medicare & Medicaid Services reimbursement, according to Dr. Casey and Dr. Tiwari.
Subsequent studies demonstrated “significant differences” in apnea-hypopnea index results, depending on which scoring criteria were used, they added.
“This confusing, vacillating definition has created a rather bizarre, and perhaps unsettling, situation wherein the severity of the diagnosis of sleep-disordered breathing, and perhaps its presence or absence, is determined by the patient’s insurance coverage,” they said in the commentary.
Dr. Casey and Dr. Tiwari are with the University of Wisconsin and William S. Middleton Memorial Veterans Hospital, both in Madison. They reported no conflicts of interest related to their editorial, which appears in the Journal of Clinical Sleep Medicine.
The latest recommended criteria for hypopnea define a distinct group of patients who report substantial daytime sleepiness but with no significant cardiovascular risk, investigators reported in a retrospective, cross-sectional analysis.
The number of obstructive sleep apnea (OSA) diagnoses increased by nearly 13% when using the 2012 American Academy of Sleep Medicine (AASM) criteria of ≥ 3% desaturation or arousal, instead of the 2007 criteria of ≥ 4% desaturation, according to investigators.
While cardiovascular disease risk did not appear to be elevated in those with an OSA diagnosis based on the newer, more inclusive criteria, reported lead author Christine H.J. Won, MD, of Yale University, New Haven, Conn., and her coinvestigators.
“Our findings suggest [that] a more inclusive hypopnea definition alters OSA severity categorization, identifies a new symptomatic group of patients with predominantly mild OSA without increased cardiovascular odds, and does not ameliorate the increased odds predicted by severe OSA for arrhythmias,” the investigators wrote in the Journal of Clinical Sleep Medicine.
The analysis by Dr. Won and her colleagues included 1,400 veterans who had polysomnography for suspected sleep-disordered breathing. Of those veterans, two-thirds (932; 66%) had an OSA diagnosis based on the ≥ 4% desaturation criteria.
With the newer criteria of ≥ 3% desaturation or arousal, another 175 OSA diagnoses were captured out of the remaining 468 previously negative studies, meaning that more than 37% of those patients would be recategorized as having OSA, Dr. Won and her coauthors said.
Compared with individuals with OSA classified by the older, more restrictive criteria, the 175 individuals in this “new OSA” group were younger and less likely to be obese, though they were still more likely to be obese, compared with individuals with no OSA diagnosis, according to the authors.
The new OSA group had more disrupted sleep architecture, significantly worse oxygen saturations, and more self-reported sleepiness on the Epworth Sleepiness Scale as compared with those with no OSA, they added.
Adding in the new OSA group redistributed disease severity, with a relative increase of 21.4% for mild and 21.3% for moderate OSA, but just 15.3% for severe OSA. “Most of the [new OSA] category consisted of mild sleep-disordered breathing,” said Dr. Won and her coauthors in the report.
While there was a statistically significant increase in odds ratio for arrhythmias using the older criteria, reclassifying OSA severity using the newer definition meant that mild and moderate disease lost predictive value. However, severe OSA by the new criteria remained a significant predictor of arrhythmias, the authors said.
Odds ratios for ischemic heart disease and heart failure were numerically higher in the new OSA group versus the no OSA group, though no statistically significant differences were found, according to investigators.
This is thought to be the first study to describe a unique group of patients who escape OSA diagnosis based on the ≥ 4% desaturation criteria but are captured ≥ 3% desaturation or arousal criteria, Dr. Won and her coauthors said.
Further studies would be helpful to evaluate other polysomnographic features in this group to see how they affect cardiovascular or other health risks, they added.
“It would also be important to assess whether treatment in any of these groups leads to improved cardiovascular health, or whether treatment of the [new OSA] group leads to improved daytime sleepiness or quality of life,” they said in the report.
The researchers reported no conflicts of interest related to their work, which was performed at the Veterans Affairs Healthcare System in West Haven, Conn.; Indianapolis; and Cleveland.
SOURCE: Won CHJ et al. J Clin Sleep Med. 2018 Dec 15;14[12]:1987-94.
The latest recommended criteria for hypopnea define a distinct group of patients who report substantial daytime sleepiness but with no significant cardiovascular risk, investigators reported in a retrospective, cross-sectional analysis.
The number of obstructive sleep apnea (OSA) diagnoses increased by nearly 13% when using the 2012 American Academy of Sleep Medicine (AASM) criteria of ≥ 3% desaturation or arousal, instead of the 2007 criteria of ≥ 4% desaturation, according to investigators.
While cardiovascular disease risk did not appear to be elevated in those with an OSA diagnosis based on the newer, more inclusive criteria, reported lead author Christine H.J. Won, MD, of Yale University, New Haven, Conn., and her coinvestigators.
“Our findings suggest [that] a more inclusive hypopnea definition alters OSA severity categorization, identifies a new symptomatic group of patients with predominantly mild OSA without increased cardiovascular odds, and does not ameliorate the increased odds predicted by severe OSA for arrhythmias,” the investigators wrote in the Journal of Clinical Sleep Medicine.
The analysis by Dr. Won and her colleagues included 1,400 veterans who had polysomnography for suspected sleep-disordered breathing. Of those veterans, two-thirds (932; 66%) had an OSA diagnosis based on the ≥ 4% desaturation criteria.
With the newer criteria of ≥ 3% desaturation or arousal, another 175 OSA diagnoses were captured out of the remaining 468 previously negative studies, meaning that more than 37% of those patients would be recategorized as having OSA, Dr. Won and her coauthors said.
Compared with individuals with OSA classified by the older, more restrictive criteria, the 175 individuals in this “new OSA” group were younger and less likely to be obese, though they were still more likely to be obese, compared with individuals with no OSA diagnosis, according to the authors.
The new OSA group had more disrupted sleep architecture, significantly worse oxygen saturations, and more self-reported sleepiness on the Epworth Sleepiness Scale as compared with those with no OSA, they added.
Adding in the new OSA group redistributed disease severity, with a relative increase of 21.4% for mild and 21.3% for moderate OSA, but just 15.3% for severe OSA. “Most of the [new OSA] category consisted of mild sleep-disordered breathing,” said Dr. Won and her coauthors in the report.
While there was a statistically significant increase in odds ratio for arrhythmias using the older criteria, reclassifying OSA severity using the newer definition meant that mild and moderate disease lost predictive value. However, severe OSA by the new criteria remained a significant predictor of arrhythmias, the authors said.
Odds ratios for ischemic heart disease and heart failure were numerically higher in the new OSA group versus the no OSA group, though no statistically significant differences were found, according to investigators.
This is thought to be the first study to describe a unique group of patients who escape OSA diagnosis based on the ≥ 4% desaturation criteria but are captured ≥ 3% desaturation or arousal criteria, Dr. Won and her coauthors said.
Further studies would be helpful to evaluate other polysomnographic features in this group to see how they affect cardiovascular or other health risks, they added.
“It would also be important to assess whether treatment in any of these groups leads to improved cardiovascular health, or whether treatment of the [new OSA] group leads to improved daytime sleepiness or quality of life,” they said in the report.
The researchers reported no conflicts of interest related to their work, which was performed at the Veterans Affairs Healthcare System in West Haven, Conn.; Indianapolis; and Cleveland.
SOURCE: Won CHJ et al. J Clin Sleep Med. 2018 Dec 15;14[12]:1987-94.
FROM THE CLINICAL JOURNAL OF SLEEP MEDICINE
Key clinical point: The latest AASM criteria for hypopnea identify a subset of obstructive sleep apnea patients with substantial daytime sleepiness but no apparent significant increase in cardiovascular risk.
Major finding: The number of obstructive sleep apnea (OSA) diagnoses increased by nearly 13% when using the 2012 AASM criteria of ≥ 3% desaturation or an arousal, instead of the 2007 criteria of ≥ 4% desaturation.
Study details: Retrospective, cross-sectional, observational study that includes 1,400 veterans evaluated for suspected sleep-disordered breathing.
Disclosures: Authors reported no conflicts of interest.
Source: Won CHJ et al. J Clin Sleep Med. 2018 Dec 15;14(12):1987-94.
Neoadjuvant degarelix more effective than triptorelin for ovarian suppression
Degarelix, the gonadotropin-releasing hormone (GnRH) antagonist approved for prostate cancer, was more effective than a GnRH agonist in achieving ovarian function suppression in women with breast cancer, results of a randomized trial show.
Ovarian function suppression was achieved more rapidly and maintained more effectively with degarelix, compared with triptorelin, in the premenopausal women who were receiving letrozole for neoadjuvant endocrine therapy, investigators said.
Adverse events including hot flashes and injection site reactions were reported more often with degarelix versus the GnRH agonist in this randomized, phase 2 trial of 51 subjects.
Additional research is needed to determine whether degarelix results in superior disease control versus the current standard of care, reported Silvia Dellapasqua, MD, of the European Institute of Oncology IRCCS in Milan, Italy, and coinvestigators.
“The study is hypothesis-generating, and supports later studies to assess whether maintenance of ovarian function suppression with degarelix translates into a better clinical outcome and is worth a trade-off of increased rate of some adverse events,” the researchers wrote. The report is in the Journal of Clinical Oncology.
Patients were randomly assigned to receive degarelix plus letrozole or triptorelin plus letrozole for six 28-day cycles. Degarelix was administered subcutaneously on day 1 of each cycle, while triptorelin was administered intramuscularly on day 1 of each cycle, and oral letrozole was to be taken daily. Surgery was performed a few weeks after the last injection.
All patients achieved optimal ovarian function suppression by the end of the first cycle. However, that endpoint was achieved significantly faster among patients in the degarelix arm, at a median of 3 days, versus a median of 14 days for the GnRH agonist, the investigators reported.
The optimal ovarian function suppression was seen three times faster with degarelix (hazard ratio, 3.05; 95% confidence interval, 1.65-5.65; P less than 001), they added.
One hundred percent of patients receiving degarelix and letrozole maintained optimal ovarian function suppression throughout the study, while about 15% of patients assigned to triptorelin had suboptimal suppression after that first cycle.
The group of patients receiving degarelix had a higher rate of node-negative disease at surgery, and a higher rate of breast-conserving surgery compared with the triptorelin group, the investigators said.
There were two grade 3 adverse events, hypertension and anemia, which both occurred in the triptorelin group, and no grade 4 adverse events. The most common adverse events reported were hot flashes, occurring in 80.0% and 69.2% of the degarelix and triptorelin groups, respectively; arthralgias in 32.0% and 53.8%; insomnia in 24.0% and 11.5%; injection site reactions in 24.0% and 0%; and nausea in 16.0% and 3.8%.
The study was supported by Ferring, and by the International Breast Cancer Study Group via Frontier Science and Technology Research Foundation, Swiss Group for Clinical Cancer Research, Cancer Research Switzerland, Oncosuisse, Swiss Cancer League, and the Foundation for Clinical Cancer Research of Eastern Switzerland. The authors reported disclosures related to Ferring, Novartis, Ipsen, DVAX, Roche, Genentech, Pfizer, Celgene, and Merck, among others.
SOURCE: Dellapasqua S et al. J Clin Oncol. 2018 Dec 27. doi: 10.1200/JCO.18.00296.
Degarelix, the gonadotropin-releasing hormone (GnRH) antagonist approved for prostate cancer, was more effective than a GnRH agonist in achieving ovarian function suppression in women with breast cancer, results of a randomized trial show.
Ovarian function suppression was achieved more rapidly and maintained more effectively with degarelix, compared with triptorelin, in the premenopausal women who were receiving letrozole for neoadjuvant endocrine therapy, investigators said.
Adverse events including hot flashes and injection site reactions were reported more often with degarelix versus the GnRH agonist in this randomized, phase 2 trial of 51 subjects.
Additional research is needed to determine whether degarelix results in superior disease control versus the current standard of care, reported Silvia Dellapasqua, MD, of the European Institute of Oncology IRCCS in Milan, Italy, and coinvestigators.
“The study is hypothesis-generating, and supports later studies to assess whether maintenance of ovarian function suppression with degarelix translates into a better clinical outcome and is worth a trade-off of increased rate of some adverse events,” the researchers wrote. The report is in the Journal of Clinical Oncology.
Patients were randomly assigned to receive degarelix plus letrozole or triptorelin plus letrozole for six 28-day cycles. Degarelix was administered subcutaneously on day 1 of each cycle, while triptorelin was administered intramuscularly on day 1 of each cycle, and oral letrozole was to be taken daily. Surgery was performed a few weeks after the last injection.
All patients achieved optimal ovarian function suppression by the end of the first cycle. However, that endpoint was achieved significantly faster among patients in the degarelix arm, at a median of 3 days, versus a median of 14 days for the GnRH agonist, the investigators reported.
The optimal ovarian function suppression was seen three times faster with degarelix (hazard ratio, 3.05; 95% confidence interval, 1.65-5.65; P less than 001), they added.
One hundred percent of patients receiving degarelix and letrozole maintained optimal ovarian function suppression throughout the study, while about 15% of patients assigned to triptorelin had suboptimal suppression after that first cycle.
The group of patients receiving degarelix had a higher rate of node-negative disease at surgery, and a higher rate of breast-conserving surgery compared with the triptorelin group, the investigators said.
There were two grade 3 adverse events, hypertension and anemia, which both occurred in the triptorelin group, and no grade 4 adverse events. The most common adverse events reported were hot flashes, occurring in 80.0% and 69.2% of the degarelix and triptorelin groups, respectively; arthralgias in 32.0% and 53.8%; insomnia in 24.0% and 11.5%; injection site reactions in 24.0% and 0%; and nausea in 16.0% and 3.8%.
The study was supported by Ferring, and by the International Breast Cancer Study Group via Frontier Science and Technology Research Foundation, Swiss Group for Clinical Cancer Research, Cancer Research Switzerland, Oncosuisse, Swiss Cancer League, and the Foundation for Clinical Cancer Research of Eastern Switzerland. The authors reported disclosures related to Ferring, Novartis, Ipsen, DVAX, Roche, Genentech, Pfizer, Celgene, and Merck, among others.
SOURCE: Dellapasqua S et al. J Clin Oncol. 2018 Dec 27. doi: 10.1200/JCO.18.00296.
Degarelix, the gonadotropin-releasing hormone (GnRH) antagonist approved for prostate cancer, was more effective than a GnRH agonist in achieving ovarian function suppression in women with breast cancer, results of a randomized trial show.
Ovarian function suppression was achieved more rapidly and maintained more effectively with degarelix, compared with triptorelin, in the premenopausal women who were receiving letrozole for neoadjuvant endocrine therapy, investigators said.
Adverse events including hot flashes and injection site reactions were reported more often with degarelix versus the GnRH agonist in this randomized, phase 2 trial of 51 subjects.
Additional research is needed to determine whether degarelix results in superior disease control versus the current standard of care, reported Silvia Dellapasqua, MD, of the European Institute of Oncology IRCCS in Milan, Italy, and coinvestigators.
“The study is hypothesis-generating, and supports later studies to assess whether maintenance of ovarian function suppression with degarelix translates into a better clinical outcome and is worth a trade-off of increased rate of some adverse events,” the researchers wrote. The report is in the Journal of Clinical Oncology.
Patients were randomly assigned to receive degarelix plus letrozole or triptorelin plus letrozole for six 28-day cycles. Degarelix was administered subcutaneously on day 1 of each cycle, while triptorelin was administered intramuscularly on day 1 of each cycle, and oral letrozole was to be taken daily. Surgery was performed a few weeks after the last injection.
All patients achieved optimal ovarian function suppression by the end of the first cycle. However, that endpoint was achieved significantly faster among patients in the degarelix arm, at a median of 3 days, versus a median of 14 days for the GnRH agonist, the investigators reported.
The optimal ovarian function suppression was seen three times faster with degarelix (hazard ratio, 3.05; 95% confidence interval, 1.65-5.65; P less than 001), they added.
One hundred percent of patients receiving degarelix and letrozole maintained optimal ovarian function suppression throughout the study, while about 15% of patients assigned to triptorelin had suboptimal suppression after that first cycle.
The group of patients receiving degarelix had a higher rate of node-negative disease at surgery, and a higher rate of breast-conserving surgery compared with the triptorelin group, the investigators said.
There were two grade 3 adverse events, hypertension and anemia, which both occurred in the triptorelin group, and no grade 4 adverse events. The most common adverse events reported were hot flashes, occurring in 80.0% and 69.2% of the degarelix and triptorelin groups, respectively; arthralgias in 32.0% and 53.8%; insomnia in 24.0% and 11.5%; injection site reactions in 24.0% and 0%; and nausea in 16.0% and 3.8%.
The study was supported by Ferring, and by the International Breast Cancer Study Group via Frontier Science and Technology Research Foundation, Swiss Group for Clinical Cancer Research, Cancer Research Switzerland, Oncosuisse, Swiss Cancer League, and the Foundation for Clinical Cancer Research of Eastern Switzerland. The authors reported disclosures related to Ferring, Novartis, Ipsen, DVAX, Roche, Genentech, Pfizer, Celgene, and Merck, among others.
SOURCE: Dellapasqua S et al. J Clin Oncol. 2018 Dec 27. doi: 10.1200/JCO.18.00296.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Degarelix, the gonadotropin-releasing hormone (GnRH) antagonist approved for prostate cancer, was more effective than the GnRH agonist triptorelin in achieving ovarian function suppression.
Major finding: Ovarian function suppression occurred three times faster with degarelix (hazard ratio, 3.05; 95% confidence interval, 1.65-5.65; P less than .001) and in contrast to the triptorelin group, none had suboptimal suppression on subsequent cycles.
Study details: A randomized phase 2 trial including 51 premenopausal women receiving letrozole for locally advanced, endocrine-responsive breast cancer.
Disclosures: The study was supported in part by Ferring. Authors reported disclosures related to Ferring, Novartis, Ipsen, DVAX, Roche, Genentech, Pfizer, Celgene, and Merck, among others.
Source: Dellapasqua S et al. J Clin Oncol. 2018 Dec 27. doi: 10.1200/JCO.18.00296.
Puppy bite at yoga retreat leads to rabies death: Prompts health warning
Individuals going to rabies-endemic countries should have a pretrip consultation with a travel health specialist, say authors of a case report describing the death of a woman who sustained a bite from a rabid puppy during a 2017 yoga retreat in rural India.
Preexposure prophylaxis is warranted, especially for individuals expected to be in those countries for long durations, those planning to go to remote areas, or if they plan activities that may put them at risk for rabies exposure, the authors wrote in Morbidity and Mortality Weekly Report.
“In the case of the yoga retreat tour, given the extended length of the tour and the rural and community activities involved, pretravel rabies vaccination should have been considered,” said Julia Murphy, DVM, a veterinarian with the Virginia Department of Health, and her coauthors in the recently published report.
The case also underscores the importance of prompt rabies diagnosis, according to Dr. Murphy and her colleagues: 250 health care workers were assessed for exposure to the patient, 72 (29%) of whom were advised to initiate postexposure prophylaxis and were treated at a cost of nearly a quarter million dollars.
The Virginia woman described in the case report was aged 65 years and had no preexisting health conditions. She had spent more than 2 months on a yoga retreat tour in India and was bitten by a puppy near her hotel in Rishikesh in northern India, according to results of a public health investigation.
That retreat ended on April 7, 2017, according to the report, and on May 3, 2017, the woman started to have pain and paresthesia in her right arm during gardening.
On May 6, she sought care at an urgent care facility, resulting in a diagnosis of carpal tunnel syndrome and a prescription for an NSAID.
The next day, she was evaluated at a hospital for anxiety, insomnia, shortness of breath, and difficulty swallowing water and was given lorazepam for a presumed panic attack. She was discharged and, in her car, experienced claustrophobia and shortness of breath. She returned to the hospital’s ED, received more lorazepam, and was again discharged.
The day after that, she was transported by ambulance to another hospital with increased anxiety, shortness of breath, chest discomfort, and progressive paresthesia; she was found to have elevated cardiac enzymes and underwent emergency cardiac catheterization, which revealed normal arteries.
That evening, the patient became “progressively agitated and combative,” according to the report, and was found to be gasping for air while trying to drink water. When family were questioned about animal exposures, the woman’s husband indicated that she had been bitten on the right hand by a puppy during the yoga retreat, about 6 weeks before the symptoms started.
Once a diagnosis of rabies was confirmed, the woman was started on aggressive treatment but eventually died, according to Dr. Murphy and her coauthors, which made this patient the ninth person in the United States to die from rabies exposure while overseas since 2008. Canine rabies has been eliminated in the United States because of the strict vaccination laws.
“These events underscore the importance of obtaining a thorough pretravel health consultation, particularly when visiting countries with high incidence of emerging or zoonotic pathogens, to ensure awareness of health risks and appropriate pretravel and postexposure health care actions,” they concluded in their report.
Dr. Murphy and her coauthors reported no potential conflicts of interest related to the case report.
SOURCE: Murphy J et al. MMWR Morb Mortal Wkly Rep. 2019 Jan 4;67(5152):1410-4.
Individuals going to rabies-endemic countries should have a pretrip consultation with a travel health specialist, say authors of a case report describing the death of a woman who sustained a bite from a rabid puppy during a 2017 yoga retreat in rural India.
Preexposure prophylaxis is warranted, especially for individuals expected to be in those countries for long durations, those planning to go to remote areas, or if they plan activities that may put them at risk for rabies exposure, the authors wrote in Morbidity and Mortality Weekly Report.
“In the case of the yoga retreat tour, given the extended length of the tour and the rural and community activities involved, pretravel rabies vaccination should have been considered,” said Julia Murphy, DVM, a veterinarian with the Virginia Department of Health, and her coauthors in the recently published report.
The case also underscores the importance of prompt rabies diagnosis, according to Dr. Murphy and her colleagues: 250 health care workers were assessed for exposure to the patient, 72 (29%) of whom were advised to initiate postexposure prophylaxis and were treated at a cost of nearly a quarter million dollars.
The Virginia woman described in the case report was aged 65 years and had no preexisting health conditions. She had spent more than 2 months on a yoga retreat tour in India and was bitten by a puppy near her hotel in Rishikesh in northern India, according to results of a public health investigation.
That retreat ended on April 7, 2017, according to the report, and on May 3, 2017, the woman started to have pain and paresthesia in her right arm during gardening.
On May 6, she sought care at an urgent care facility, resulting in a diagnosis of carpal tunnel syndrome and a prescription for an NSAID.
The next day, she was evaluated at a hospital for anxiety, insomnia, shortness of breath, and difficulty swallowing water and was given lorazepam for a presumed panic attack. She was discharged and, in her car, experienced claustrophobia and shortness of breath. She returned to the hospital’s ED, received more lorazepam, and was again discharged.
The day after that, she was transported by ambulance to another hospital with increased anxiety, shortness of breath, chest discomfort, and progressive paresthesia; she was found to have elevated cardiac enzymes and underwent emergency cardiac catheterization, which revealed normal arteries.
That evening, the patient became “progressively agitated and combative,” according to the report, and was found to be gasping for air while trying to drink water. When family were questioned about animal exposures, the woman’s husband indicated that she had been bitten on the right hand by a puppy during the yoga retreat, about 6 weeks before the symptoms started.
Once a diagnosis of rabies was confirmed, the woman was started on aggressive treatment but eventually died, according to Dr. Murphy and her coauthors, which made this patient the ninth person in the United States to die from rabies exposure while overseas since 2008. Canine rabies has been eliminated in the United States because of the strict vaccination laws.
“These events underscore the importance of obtaining a thorough pretravel health consultation, particularly when visiting countries with high incidence of emerging or zoonotic pathogens, to ensure awareness of health risks and appropriate pretravel and postexposure health care actions,” they concluded in their report.
Dr. Murphy and her coauthors reported no potential conflicts of interest related to the case report.
SOURCE: Murphy J et al. MMWR Morb Mortal Wkly Rep. 2019 Jan 4;67(5152):1410-4.
Individuals going to rabies-endemic countries should have a pretrip consultation with a travel health specialist, say authors of a case report describing the death of a woman who sustained a bite from a rabid puppy during a 2017 yoga retreat in rural India.
Preexposure prophylaxis is warranted, especially for individuals expected to be in those countries for long durations, those planning to go to remote areas, or if they plan activities that may put them at risk for rabies exposure, the authors wrote in Morbidity and Mortality Weekly Report.
“In the case of the yoga retreat tour, given the extended length of the tour and the rural and community activities involved, pretravel rabies vaccination should have been considered,” said Julia Murphy, DVM, a veterinarian with the Virginia Department of Health, and her coauthors in the recently published report.
The case also underscores the importance of prompt rabies diagnosis, according to Dr. Murphy and her colleagues: 250 health care workers were assessed for exposure to the patient, 72 (29%) of whom were advised to initiate postexposure prophylaxis and were treated at a cost of nearly a quarter million dollars.
The Virginia woman described in the case report was aged 65 years and had no preexisting health conditions. She had spent more than 2 months on a yoga retreat tour in India and was bitten by a puppy near her hotel in Rishikesh in northern India, according to results of a public health investigation.
That retreat ended on April 7, 2017, according to the report, and on May 3, 2017, the woman started to have pain and paresthesia in her right arm during gardening.
On May 6, she sought care at an urgent care facility, resulting in a diagnosis of carpal tunnel syndrome and a prescription for an NSAID.
The next day, she was evaluated at a hospital for anxiety, insomnia, shortness of breath, and difficulty swallowing water and was given lorazepam for a presumed panic attack. She was discharged and, in her car, experienced claustrophobia and shortness of breath. She returned to the hospital’s ED, received more lorazepam, and was again discharged.
The day after that, she was transported by ambulance to another hospital with increased anxiety, shortness of breath, chest discomfort, and progressive paresthesia; she was found to have elevated cardiac enzymes and underwent emergency cardiac catheterization, which revealed normal arteries.
That evening, the patient became “progressively agitated and combative,” according to the report, and was found to be gasping for air while trying to drink water. When family were questioned about animal exposures, the woman’s husband indicated that she had been bitten on the right hand by a puppy during the yoga retreat, about 6 weeks before the symptoms started.
Once a diagnosis of rabies was confirmed, the woman was started on aggressive treatment but eventually died, according to Dr. Murphy and her coauthors, which made this patient the ninth person in the United States to die from rabies exposure while overseas since 2008. Canine rabies has been eliminated in the United States because of the strict vaccination laws.
“These events underscore the importance of obtaining a thorough pretravel health consultation, particularly when visiting countries with high incidence of emerging or zoonotic pathogens, to ensure awareness of health risks and appropriate pretravel and postexposure health care actions,” they concluded in their report.
Dr. Murphy and her coauthors reported no potential conflicts of interest related to the case report.
SOURCE: Murphy J et al. MMWR Morb Mortal Wkly Rep. 2019 Jan 4;67(5152):1410-4.
FROM MMWR
Key clinical point: depending on length of trip, location, and activities involved.
Major finding: A Virginia woman died after sustaining a bite from a rabid puppy during a 2017 yoga retreat in rural India.
Study details: Case report including details of the 65-year-old woman’s trip, rabies exposure, symptoms, diagnosis, and eventual death.
Disclosures: Authors reported no potential conflicts of interest.
Source: Murphy J et al. MMWR Morb Mortal Wkly Rep. 2019 Jan 4;67(5152):1410-4.
Actionable mutations more likely in women with both breast and uterine cancer
Women with both breast and uterine cancer are more likely to carry genetic mutations than women with either breast or uterine cancer alone, according to results of a retrospective analysis of test results.
The majority of the mutations identified were actionable, suggesting that women with breast and uterine cancer should be offered expanded genetic testing, authors of the analysis wrote in Gynecologic Oncology.
“Expanded testing for patients with breast and uterine cancer can help guide management by identifying more patients who may benefit from additional surveillance, along with at-risk family members,” said Kelly Fulk, an oncology genetic specialist at Ambry Genetics, and her coauthors.
The analysis by Ms. Fulk and her colleagues at St. Thomas Health, Nashville, and the University of California, Irvine, was based on a cohort of 52,000 women who had undergone multigene panel testing.
That cohort included 1,650 women with both breast and uterine cancer, of whom about 70% were white, and more than 94% were older than age 50 years at the time of testing. Their median age at first diagnosis was 56 years for breast cancer and 58 years for uterine cancer.
A total of 231 women with breast and uterine cancer, or 14.0%, carried at least one pathogenic mutation or likely pathogenic variant, Ms. Fulk and her colleagues reported. By comparison, mutations were seen in 9.3% of women with breast cancer only (P less than .001), 11.5% of women with uterine cancer only (P = 4.63 x 10–3), and 6.8% of women with no personal cancer history (P less than .001).
Women with both breast and uterine cancer more often had mutations in ATM, BARD1, BRCA2, MSH2, MSH6, PALB2, PMS2, and PTEN, when compared with those women with no personal cancer history, according to the report by Ms. Fulk and her coauthors.
When compared with women with just breast cancer, the women with both breast and uterine cancer more often had mutations in BRCA1, MLH1, MSH2, MSH6, PMS2 and PTEN, they added, noting that women with both cancers were twice as likely to have a BRCA1 mutation (odds ratio, 2.01; 95% confidence interval, 1.08-3.39, P = .016).
While this study had limitations, including its retrospective nature and use of genetic tests with varying numbers of genes analyzed, authors said the results nonetheless support expanded testing in women with both breast and uterine cancers to help guide therapy and cancer surveillance.
“Mutations associated with hereditary breast and ovarian cancer, Lynch syndrome, Cowden syndrome, and Li-Fraumeni syndrome have clear guidelines regarding management and surveillance for other cancers, which can benefit patients and their at-risk family members,” the investigators said.
Ms. Fulk and five coauthors reported that they are paid employees of Ambry Genetics. No other disclosures were provided.
SOURCE: Fulk K et al. Gynecol Oncol. 2019 Jan 3. doi: 10.1016/j.ygyno.2018.12.021.
Women with both breast and uterine cancer are more likely to carry genetic mutations than women with either breast or uterine cancer alone, according to results of a retrospective analysis of test results.
The majority of the mutations identified were actionable, suggesting that women with breast and uterine cancer should be offered expanded genetic testing, authors of the analysis wrote in Gynecologic Oncology.
“Expanded testing for patients with breast and uterine cancer can help guide management by identifying more patients who may benefit from additional surveillance, along with at-risk family members,” said Kelly Fulk, an oncology genetic specialist at Ambry Genetics, and her coauthors.
The analysis by Ms. Fulk and her colleagues at St. Thomas Health, Nashville, and the University of California, Irvine, was based on a cohort of 52,000 women who had undergone multigene panel testing.
That cohort included 1,650 women with both breast and uterine cancer, of whom about 70% were white, and more than 94% were older than age 50 years at the time of testing. Their median age at first diagnosis was 56 years for breast cancer and 58 years for uterine cancer.
A total of 231 women with breast and uterine cancer, or 14.0%, carried at least one pathogenic mutation or likely pathogenic variant, Ms. Fulk and her colleagues reported. By comparison, mutations were seen in 9.3% of women with breast cancer only (P less than .001), 11.5% of women with uterine cancer only (P = 4.63 x 10–3), and 6.8% of women with no personal cancer history (P less than .001).
Women with both breast and uterine cancer more often had mutations in ATM, BARD1, BRCA2, MSH2, MSH6, PALB2, PMS2, and PTEN, when compared with those women with no personal cancer history, according to the report by Ms. Fulk and her coauthors.
When compared with women with just breast cancer, the women with both breast and uterine cancer more often had mutations in BRCA1, MLH1, MSH2, MSH6, PMS2 and PTEN, they added, noting that women with both cancers were twice as likely to have a BRCA1 mutation (odds ratio, 2.01; 95% confidence interval, 1.08-3.39, P = .016).
While this study had limitations, including its retrospective nature and use of genetic tests with varying numbers of genes analyzed, authors said the results nonetheless support expanded testing in women with both breast and uterine cancers to help guide therapy and cancer surveillance.
“Mutations associated with hereditary breast and ovarian cancer, Lynch syndrome, Cowden syndrome, and Li-Fraumeni syndrome have clear guidelines regarding management and surveillance for other cancers, which can benefit patients and their at-risk family members,” the investigators said.
Ms. Fulk and five coauthors reported that they are paid employees of Ambry Genetics. No other disclosures were provided.
SOURCE: Fulk K et al. Gynecol Oncol. 2019 Jan 3. doi: 10.1016/j.ygyno.2018.12.021.
Women with both breast and uterine cancer are more likely to carry genetic mutations than women with either breast or uterine cancer alone, according to results of a retrospective analysis of test results.
The majority of the mutations identified were actionable, suggesting that women with breast and uterine cancer should be offered expanded genetic testing, authors of the analysis wrote in Gynecologic Oncology.
“Expanded testing for patients with breast and uterine cancer can help guide management by identifying more patients who may benefit from additional surveillance, along with at-risk family members,” said Kelly Fulk, an oncology genetic specialist at Ambry Genetics, and her coauthors.
The analysis by Ms. Fulk and her colleagues at St. Thomas Health, Nashville, and the University of California, Irvine, was based on a cohort of 52,000 women who had undergone multigene panel testing.
That cohort included 1,650 women with both breast and uterine cancer, of whom about 70% were white, and more than 94% were older than age 50 years at the time of testing. Their median age at first diagnosis was 56 years for breast cancer and 58 years for uterine cancer.
A total of 231 women with breast and uterine cancer, or 14.0%, carried at least one pathogenic mutation or likely pathogenic variant, Ms. Fulk and her colleagues reported. By comparison, mutations were seen in 9.3% of women with breast cancer only (P less than .001), 11.5% of women with uterine cancer only (P = 4.63 x 10–3), and 6.8% of women with no personal cancer history (P less than .001).
Women with both breast and uterine cancer more often had mutations in ATM, BARD1, BRCA2, MSH2, MSH6, PALB2, PMS2, and PTEN, when compared with those women with no personal cancer history, according to the report by Ms. Fulk and her coauthors.
When compared with women with just breast cancer, the women with both breast and uterine cancer more often had mutations in BRCA1, MLH1, MSH2, MSH6, PMS2 and PTEN, they added, noting that women with both cancers were twice as likely to have a BRCA1 mutation (odds ratio, 2.01; 95% confidence interval, 1.08-3.39, P = .016).
While this study had limitations, including its retrospective nature and use of genetic tests with varying numbers of genes analyzed, authors said the results nonetheless support expanded testing in women with both breast and uterine cancers to help guide therapy and cancer surveillance.
“Mutations associated with hereditary breast and ovarian cancer, Lynch syndrome, Cowden syndrome, and Li-Fraumeni syndrome have clear guidelines regarding management and surveillance for other cancers, which can benefit patients and their at-risk family members,” the investigators said.
Ms. Fulk and five coauthors reported that they are paid employees of Ambry Genetics. No other disclosures were provided.
SOURCE: Fulk K et al. Gynecol Oncol. 2019 Jan 3. doi: 10.1016/j.ygyno.2018.12.021.
FROM GYNECOLOGIC ONCOLOGY
Key clinical point: Women with both breast and uterine cancer are more likely to carry actionable mutations than do women with breast or uterine cancer alone.
Major finding: At least one actionable mutation was seen in 14% of women with breast and uterine cancer, compared with 9.3% of women with breast cancer only, 11.5% of women with uterine cancer only, and 6.8% of women with no personal cancer history.
Study details: A retrospective analysis of a cohort of nearly 52,000 patients who underwent multigene panel testing.
Disclosures: Ms. Fulk and five coauthors reported that they are paid employees of Ambry Genetics.
Source: Fulk K et al. Gynecol Oncol. 2019 Jan 3. doi: 10.1016/j.ygyno.2018.12.021.
Poor-prognosis cancers linked to highest suicide risk in first year
Suicide risk significantly increases within the first year of a cancer diagnosis, with risk varying by type of cancer, according to investigators who conducted a retrospective analysis representing nearly 4.7 million patients.
Risk of suicide in that first year after diagnosis was especially high in pancreatic and lung cancers, while by contrast, breast and prostate cancer did not increase suicide risk, reported the researchers, led by Hesham Hamoda, MD, MPH, of Boston Children’s Hospital/Harvard Medical School, and Ahmad Alfaar, MBBCh, MSc, of Charité–Universitätsmedizin Berlin.
That variation in suicide risk by cancer type suggests that prognosis and 5-year relative survival play a role in increasing suicide rates, according to Dr. Hamoda, Dr. Alfaar, and their coauthors.
“After the diagnosis, it is important that health care providers be vigilant in screening for suicide and ensuring that patients have access to social and emotional support,” they wrote in a report published in Cancer. Their analysis was based on 4,671,989 patients with a diagnosis of cancer in the Surveillance, Epidemiology, and End Results (SEER) database between 2000 and 2014. Out of 1,005,825 of those patients who died within the first year of diagnosis, the cause of death was suicide for 1,585, or 0.16%.
Overall, the risk of suicide increased significantly among cancer patients versus the general population, with an observed-to-expected (O/E) ratio of 2.51 per 10,000 person-years, the investigators found. The risk was highest in the first 6 months, with an O/E mortality of 3.13 versus 1.8 in the latter 6 months.
The highest ratios were seen for pancreatic cancer, with an O/E ratio of 8.01, and lung cancer, with a ratio of 6.05, the researchers found in further analysis.
Significant increases in suicide risk were also seen for colorectal cancer (2.08) and melanoma (1.45), though rates were not significantly different versus the general population for breast (1.23) and prostate (0.99), according to the reported data.
Suicide risk was relatively high for any cancer with distant metastases (5.63), though still significantly higher at 1.65 in persons with localized/regional disease, the data show.
The increased suicide risk persisted more than 1 year after the cancer diagnosis, though not to the degree observed within that first year, they added.
Most patients with suicide as a cause of death were white (90.2%) and male (87%). Nearly 60% were between the ages of 65 and 84 at the time of suicide.
Social support plays an integral role in suicide prevention among cancer patients, the researchers noted.
Previous studies suggest that support programs may decrease suicide risk by making patients better aware of their prognosis, receptive to decreased social stigma, or less likely to have stress related to cost of care, they said.
“Discussing the quality of life after diagnosis, the effectiveness of therapy, and the prognosis of the disease and maintaining a trusting relationship with health care professionals all decrease the likelihood of suicide immediately after a diagnosis of cancer,” they said.
Dr. Hamoda, Dr. Alfaar, and their coauthors reported no conflicts of interest. Funding for the study came in part from the German Academic Exchange Service (Dr. Alfaar).
SOURCE: Saad AM, et al. Cancer 2019 Jan 7. doi: 10.1002/cncr.31876.
Suicide risk significantly increases within the first year of a cancer diagnosis, with risk varying by type of cancer, according to investigators who conducted a retrospective analysis representing nearly 4.7 million patients.
Risk of suicide in that first year after diagnosis was especially high in pancreatic and lung cancers, while by contrast, breast and prostate cancer did not increase suicide risk, reported the researchers, led by Hesham Hamoda, MD, MPH, of Boston Children’s Hospital/Harvard Medical School, and Ahmad Alfaar, MBBCh, MSc, of Charité–Universitätsmedizin Berlin.
That variation in suicide risk by cancer type suggests that prognosis and 5-year relative survival play a role in increasing suicide rates, according to Dr. Hamoda, Dr. Alfaar, and their coauthors.
“After the diagnosis, it is important that health care providers be vigilant in screening for suicide and ensuring that patients have access to social and emotional support,” they wrote in a report published in Cancer. Their analysis was based on 4,671,989 patients with a diagnosis of cancer in the Surveillance, Epidemiology, and End Results (SEER) database between 2000 and 2014. Out of 1,005,825 of those patients who died within the first year of diagnosis, the cause of death was suicide for 1,585, or 0.16%.
Overall, the risk of suicide increased significantly among cancer patients versus the general population, with an observed-to-expected (O/E) ratio of 2.51 per 10,000 person-years, the investigators found. The risk was highest in the first 6 months, with an O/E mortality of 3.13 versus 1.8 in the latter 6 months.
The highest ratios were seen for pancreatic cancer, with an O/E ratio of 8.01, and lung cancer, with a ratio of 6.05, the researchers found in further analysis.
Significant increases in suicide risk were also seen for colorectal cancer (2.08) and melanoma (1.45), though rates were not significantly different versus the general population for breast (1.23) and prostate (0.99), according to the reported data.
Suicide risk was relatively high for any cancer with distant metastases (5.63), though still significantly higher at 1.65 in persons with localized/regional disease, the data show.
The increased suicide risk persisted more than 1 year after the cancer diagnosis, though not to the degree observed within that first year, they added.
Most patients with suicide as a cause of death were white (90.2%) and male (87%). Nearly 60% were between the ages of 65 and 84 at the time of suicide.
Social support plays an integral role in suicide prevention among cancer patients, the researchers noted.
Previous studies suggest that support programs may decrease suicide risk by making patients better aware of their prognosis, receptive to decreased social stigma, or less likely to have stress related to cost of care, they said.
“Discussing the quality of life after diagnosis, the effectiveness of therapy, and the prognosis of the disease and maintaining a trusting relationship with health care professionals all decrease the likelihood of suicide immediately after a diagnosis of cancer,” they said.
Dr. Hamoda, Dr. Alfaar, and their coauthors reported no conflicts of interest. Funding for the study came in part from the German Academic Exchange Service (Dr. Alfaar).
SOURCE: Saad AM, et al. Cancer 2019 Jan 7. doi: 10.1002/cncr.31876.
Suicide risk significantly increases within the first year of a cancer diagnosis, with risk varying by type of cancer, according to investigators who conducted a retrospective analysis representing nearly 4.7 million patients.
Risk of suicide in that first year after diagnosis was especially high in pancreatic and lung cancers, while by contrast, breast and prostate cancer did not increase suicide risk, reported the researchers, led by Hesham Hamoda, MD, MPH, of Boston Children’s Hospital/Harvard Medical School, and Ahmad Alfaar, MBBCh, MSc, of Charité–Universitätsmedizin Berlin.
That variation in suicide risk by cancer type suggests that prognosis and 5-year relative survival play a role in increasing suicide rates, according to Dr. Hamoda, Dr. Alfaar, and their coauthors.
“After the diagnosis, it is important that health care providers be vigilant in screening for suicide and ensuring that patients have access to social and emotional support,” they wrote in a report published in Cancer. Their analysis was based on 4,671,989 patients with a diagnosis of cancer in the Surveillance, Epidemiology, and End Results (SEER) database between 2000 and 2014. Out of 1,005,825 of those patients who died within the first year of diagnosis, the cause of death was suicide for 1,585, or 0.16%.
Overall, the risk of suicide increased significantly among cancer patients versus the general population, with an observed-to-expected (O/E) ratio of 2.51 per 10,000 person-years, the investigators found. The risk was highest in the first 6 months, with an O/E mortality of 3.13 versus 1.8 in the latter 6 months.
The highest ratios were seen for pancreatic cancer, with an O/E ratio of 8.01, and lung cancer, with a ratio of 6.05, the researchers found in further analysis.
Significant increases in suicide risk were also seen for colorectal cancer (2.08) and melanoma (1.45), though rates were not significantly different versus the general population for breast (1.23) and prostate (0.99), according to the reported data.
Suicide risk was relatively high for any cancer with distant metastases (5.63), though still significantly higher at 1.65 in persons with localized/regional disease, the data show.
The increased suicide risk persisted more than 1 year after the cancer diagnosis, though not to the degree observed within that first year, they added.
Most patients with suicide as a cause of death were white (90.2%) and male (87%). Nearly 60% were between the ages of 65 and 84 at the time of suicide.
Social support plays an integral role in suicide prevention among cancer patients, the researchers noted.
Previous studies suggest that support programs may decrease suicide risk by making patients better aware of their prognosis, receptive to decreased social stigma, or less likely to have stress related to cost of care, they said.
“Discussing the quality of life after diagnosis, the effectiveness of therapy, and the prognosis of the disease and maintaining a trusting relationship with health care professionals all decrease the likelihood of suicide immediately after a diagnosis of cancer,” they said.
Dr. Hamoda, Dr. Alfaar, and their coauthors reported no conflicts of interest. Funding for the study came in part from the German Academic Exchange Service (Dr. Alfaar).
SOURCE: Saad AM, et al. Cancer 2019 Jan 7. doi: 10.1002/cncr.31876.
FROM CANCER
Key clinical point: A cancer diagnosis significantly increases risk of suicide in comparison to the general population, particularly for poorer-prognosis cancers.
Major finding: The observed-to-expected mortality ratio was substantially higher for pancreatic cancer (8.01), and lung cancer (6.05), but not significantly increased for breast (1.23) and prostate (0.99).
Study details: A retrospective population-based study of 4,671,989 cancer patients.
Disclosures: The authors reported no conflicts of interest. Funding for the study came in part from the German Academic Exchange Service.
Source: Saad AM et al. Cancer. 2019 Jan 7. doi: 10.1002/cncr.31876.