News
New options emerge for primary biliary cholangitis
- Author:
- Andrew D. Bowser
LAS VEGAS – Fibrates and other peroxisome proliferator-activated receptor agonists are emerging.
News

Spine fracture risk may be increased in IBD patients
- Author:
- Andrew D. Bowser
Fracture risk appears to be higher among IBD patients who use steroids.
News

Use these two questions to simplify H. pylori treatment choice
- Author:
- Andrew D. Bowser
New guidelines recommend two different treatment regimens, depending on the answers.
News

Women’s representation in CV drug trials still lagging
- Author:
- Andrew D. Bowser
We’ve come a long way in clinical trial representation of women, but there’s more work to do.
News

Hep B therapy: Indefinite or FINITE for e-negative patients?
- Author:
- Andrew D. Bowser
LAS VEGAS –
News
Dasatinib activity prominent in subset of GIST patients
- Author:
- Andrew D. Bowser
The estimated rate of 6-month progression-free survival was 29% overall, though it was 50% in one biomarker-defined patient subset.
News

Early breast cancer: Patients report favorable quality of life after partial breast irradiation
- Author:
- Andrew D. Bowser
Moreover, breast symptom scores were worse for whole breast radiation in the study.
News

Stroke patients benefited from CPAP
- Author:
- Andrew D. Bowser
Significantly more OSA patients with a recent history of stroke experienced an improvement in their Modified Rankin Scale score after using CPAP,...
News
CVD risk high in individuals who once had metabolically healthy obesity
- Author:
- Andrew D. Bowser
“Those with MHO may experience a lag in risk while they progress to metabolic syndrome.”
News
Meta-analysis finds no link between stroke and sickle cell trait
- Author:
- Andrew D. Bowser
Neither crude stroke incidence rates nor regression analysis indicated a link between sickle cell trait in African Americans and stroke.
News
Artificial pancreas treatment improves glycemic control in T1DM: Meta-analysis
- Author:
- Andrew D. Bowser
Closed-loop glucose control systems increase the time in normoglycemia for type 1 diabetic patients, but is it enough?
News

24-hour ambulatory BP measurements strongly predict mortality
- Author:
- Andrew D. Bowser
Masked hypertension identified by 24-hour monitoring carried the greatest risk of death.
News
Ibrutinib plus carfilzomib active in relapsed multiple myeloma
- Author:
- Andrew D. Bowser
Most of the study discontinuations were because of comorbidities, toxicity from prior treatment, or underlying disease factors.
News
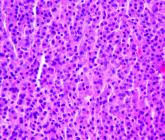
Statin plus chemo yields encouraging results in poor-risk AML
- Author:
- Andrew D. Bowser
Pravastatin may also have a therapeutic advantage in patients with FLT3 mutations.
Video

VIDEO: Meta-analysis: Mortality, safety data may favor SGLT2 inhibitors in T2DM
- Author:
- Andrew D. Bowser
GLP-1 agonists were associated with a higher risk of adverse events that led to study withdrawal, compared with SGLT2 inhibitors.
