User login
Novel options for treating hairy cell leukemia
NEW YORK – Ibrutinib, and now moxetumomab pasudotox, are two novel therapies that can be tried in patients with previously treated hairy cell leukemia, although data and experience with them are so far limited in this rare disease, experts said during a panel discussion at the National Comprehensive Cancer Network Hematologic Malignancies Annual Congress.
Since there are so few patients, data on the BTK inhibitor ibrutinib in hairy cell leukemia is largely “anecdotal,” said Andrew D. Zelenetz, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York.
The anti-CD22 monoclonal antibody moxetumomab pasudotox – approved for hairy cell leukemia in September – isn’t yet on the formulary at Memorial Sloan Kettering, Dr. Zelenetz added in a panel discussion of treatment options for a patient previously treated with purine analogueues and vemurafenib.
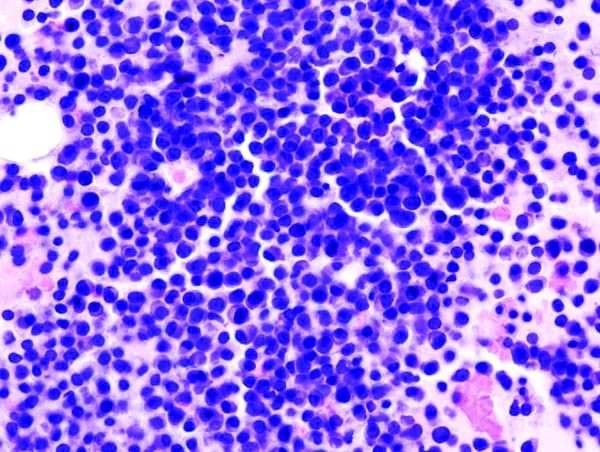
Between the two agents, moxetumomab pasudotox has more robust data in this disease, said John N. Allan, MD, of Weill Cornell Medicine, New York.
“I think if you can get access to the drug, that’s probably the best answer,” Dr. Allan said in the case discussion.
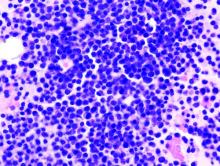
Hairy cell leukemia is an indolent B-cell lymphoma that makes up just 2% of all lymphoid leukemias, according to NCCN guidelines.
It is a chronic disease that requires long-term management, according to Dr. Allan.
First-line treatment is usually a purine analogue, either cladribine or pentostatin, and multiple treatments are possible as long as responses of greater than 2 years are achieved, he told attendees at the NCCN conference.
For relapses more than 2 years after first-line treatment, patients can be retreated with the same purine analogue, with or without rituximab, or can be switched to the alternative purine analogue, he said.
Vemurafenib, the BRAF inhibitor, is “surprisingly” effective in 90% of classic hairy cell leukemia patients with the BRAF V600E mutation, Dr. Allan added, though only about 40% of patients achieve complete response.
In discussing therapy options for a hairy cell leukemia patient previously treated with purine analogues and vemurafenib, Dr. Allan noted that the data behind ibrutinib includes case reports and early clinical investigations.
Several phase 1 studies with small numbers of patients show response rates “in the 50% range,” he said.
“This is an option,” he said. “It’s in the guidelines, and it’s something to consider.”
Moxetumomab pasudotox was recently approved for intravenous use in adults with relapsed or refractory hairy cell leukemia who have had at least two previous systemic treatments, including a purine nucleoside analogue. The CD22-directed cytotoxin is the first of its kind for treating patients with hairy cell leukemia, according to the Food and Drug Administration.
In a single-arm, open-label clinical trial including 80 patients with hairy cell leukemia who had previous treatment in line with that indication, 75% had a partial or complete response, of whom 30% had a durable complete response (CR), defined as maintaining hematologic remission for at least 180 days following CR.
Following the FDA’s approval of moxetumomab pasudotox, the NCCN updated its hairy cell leukemia clinical practice guidelines to include the drug as a category 2A recommendation for relapsed/refractory treatment. Other category 2A options in that setting include ibrutinib, vemurafenib with or without rituximab, or a clinical trial.
Along with that, NCCN guideline authors added a full page on special considerations for use of moxetumomab pasudotox. That includes advice on monitoring for capillary leak syndrome and hemolytic uremic syndrome, along with guidance on capillary leak syndrome grading and management by grade.
Dr. Zelenetz reported financial disclosures related to Adaptive Biotechnology, Amgen, AstraZeneca, Celgene, Genentech, Gilead, Hoffman La Roche, MEI Pharma, MorphoSys AG, Novartis, Pfizer, Pharmacyclics, Roche, and Verastem Oncology. Dr. Allan reported disclosures related to AbbVie, Acerta Pharma, Genentech, Pharmacyclics, Sunesis, and Verastem Oncology.
NEW YORK – Ibrutinib, and now moxetumomab pasudotox, are two novel therapies that can be tried in patients with previously treated hairy cell leukemia, although data and experience with them are so far limited in this rare disease, experts said during a panel discussion at the National Comprehensive Cancer Network Hematologic Malignancies Annual Congress.
Since there are so few patients, data on the BTK inhibitor ibrutinib in hairy cell leukemia is largely “anecdotal,” said Andrew D. Zelenetz, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York.
The anti-CD22 monoclonal antibody moxetumomab pasudotox – approved for hairy cell leukemia in September – isn’t yet on the formulary at Memorial Sloan Kettering, Dr. Zelenetz added in a panel discussion of treatment options for a patient previously treated with purine analogueues and vemurafenib.
Between the two agents, moxetumomab pasudotox has more robust data in this disease, said John N. Allan, MD, of Weill Cornell Medicine, New York.
“I think if you can get access to the drug, that’s probably the best answer,” Dr. Allan said in the case discussion.
Hairy cell leukemia is an indolent B-cell lymphoma that makes up just 2% of all lymphoid leukemias, according to NCCN guidelines.
It is a chronic disease that requires long-term management, according to Dr. Allan.
First-line treatment is usually a purine analogue, either cladribine or pentostatin, and multiple treatments are possible as long as responses of greater than 2 years are achieved, he told attendees at the NCCN conference.
For relapses more than 2 years after first-line treatment, patients can be retreated with the same purine analogue, with or without rituximab, or can be switched to the alternative purine analogue, he said.
Vemurafenib, the BRAF inhibitor, is “surprisingly” effective in 90% of classic hairy cell leukemia patients with the BRAF V600E mutation, Dr. Allan added, though only about 40% of patients achieve complete response.
In discussing therapy options for a hairy cell leukemia patient previously treated with purine analogues and vemurafenib, Dr. Allan noted that the data behind ibrutinib includes case reports and early clinical investigations.
Several phase 1 studies with small numbers of patients show response rates “in the 50% range,” he said.
“This is an option,” he said. “It’s in the guidelines, and it’s something to consider.”
Moxetumomab pasudotox was recently approved for intravenous use in adults with relapsed or refractory hairy cell leukemia who have had at least two previous systemic treatments, including a purine nucleoside analogue. The CD22-directed cytotoxin is the first of its kind for treating patients with hairy cell leukemia, according to the Food and Drug Administration.
In a single-arm, open-label clinical trial including 80 patients with hairy cell leukemia who had previous treatment in line with that indication, 75% had a partial or complete response, of whom 30% had a durable complete response (CR), defined as maintaining hematologic remission for at least 180 days following CR.
Following the FDA’s approval of moxetumomab pasudotox, the NCCN updated its hairy cell leukemia clinical practice guidelines to include the drug as a category 2A recommendation for relapsed/refractory treatment. Other category 2A options in that setting include ibrutinib, vemurafenib with or without rituximab, or a clinical trial.
Along with that, NCCN guideline authors added a full page on special considerations for use of moxetumomab pasudotox. That includes advice on monitoring for capillary leak syndrome and hemolytic uremic syndrome, along with guidance on capillary leak syndrome grading and management by grade.
Dr. Zelenetz reported financial disclosures related to Adaptive Biotechnology, Amgen, AstraZeneca, Celgene, Genentech, Gilead, Hoffman La Roche, MEI Pharma, MorphoSys AG, Novartis, Pfizer, Pharmacyclics, Roche, and Verastem Oncology. Dr. Allan reported disclosures related to AbbVie, Acerta Pharma, Genentech, Pharmacyclics, Sunesis, and Verastem Oncology.
NEW YORK – Ibrutinib, and now moxetumomab pasudotox, are two novel therapies that can be tried in patients with previously treated hairy cell leukemia, although data and experience with them are so far limited in this rare disease, experts said during a panel discussion at the National Comprehensive Cancer Network Hematologic Malignancies Annual Congress.
Since there are so few patients, data on the BTK inhibitor ibrutinib in hairy cell leukemia is largely “anecdotal,” said Andrew D. Zelenetz, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York.
The anti-CD22 monoclonal antibody moxetumomab pasudotox – approved for hairy cell leukemia in September – isn’t yet on the formulary at Memorial Sloan Kettering, Dr. Zelenetz added in a panel discussion of treatment options for a patient previously treated with purine analogueues and vemurafenib.
Between the two agents, moxetumomab pasudotox has more robust data in this disease, said John N. Allan, MD, of Weill Cornell Medicine, New York.
“I think if you can get access to the drug, that’s probably the best answer,” Dr. Allan said in the case discussion.
Hairy cell leukemia is an indolent B-cell lymphoma that makes up just 2% of all lymphoid leukemias, according to NCCN guidelines.
It is a chronic disease that requires long-term management, according to Dr. Allan.
First-line treatment is usually a purine analogue, either cladribine or pentostatin, and multiple treatments are possible as long as responses of greater than 2 years are achieved, he told attendees at the NCCN conference.
For relapses more than 2 years after first-line treatment, patients can be retreated with the same purine analogue, with or without rituximab, or can be switched to the alternative purine analogue, he said.
Vemurafenib, the BRAF inhibitor, is “surprisingly” effective in 90% of classic hairy cell leukemia patients with the BRAF V600E mutation, Dr. Allan added, though only about 40% of patients achieve complete response.
In discussing therapy options for a hairy cell leukemia patient previously treated with purine analogues and vemurafenib, Dr. Allan noted that the data behind ibrutinib includes case reports and early clinical investigations.
Several phase 1 studies with small numbers of patients show response rates “in the 50% range,” he said.
“This is an option,” he said. “It’s in the guidelines, and it’s something to consider.”
Moxetumomab pasudotox was recently approved for intravenous use in adults with relapsed or refractory hairy cell leukemia who have had at least two previous systemic treatments, including a purine nucleoside analogue. The CD22-directed cytotoxin is the first of its kind for treating patients with hairy cell leukemia, according to the Food and Drug Administration.
In a single-arm, open-label clinical trial including 80 patients with hairy cell leukemia who had previous treatment in line with that indication, 75% had a partial or complete response, of whom 30% had a durable complete response (CR), defined as maintaining hematologic remission for at least 180 days following CR.
Following the FDA’s approval of moxetumomab pasudotox, the NCCN updated its hairy cell leukemia clinical practice guidelines to include the drug as a category 2A recommendation for relapsed/refractory treatment. Other category 2A options in that setting include ibrutinib, vemurafenib with or without rituximab, or a clinical trial.
Along with that, NCCN guideline authors added a full page on special considerations for use of moxetumomab pasudotox. That includes advice on monitoring for capillary leak syndrome and hemolytic uremic syndrome, along with guidance on capillary leak syndrome grading and management by grade.
Dr. Zelenetz reported financial disclosures related to Adaptive Biotechnology, Amgen, AstraZeneca, Celgene, Genentech, Gilead, Hoffman La Roche, MEI Pharma, MorphoSys AG, Novartis, Pfizer, Pharmacyclics, Roche, and Verastem Oncology. Dr. Allan reported disclosures related to AbbVie, Acerta Pharma, Genentech, Pharmacyclics, Sunesis, and Verastem Oncology.
EXPERT ANALYSIS FROM NCCN HEMATOLOGIC MALIGNANCIES
B-cell maturation antigen targeted in myeloma trials
NEW YORK – Three novel treatment strategies that target B-cell maturation antigen (BCMA) have shown promise in recent multiple myeloma clinical trials, according to Shaji K. Kumar, MD, of the Mayo Clinic Cancer Center in Rochester, Minn.
These strategies include B-cell maturation antigen (BCMA)–specific chimeric antigen receptor (CAR) T-cell therapies, bispecific T-cell engagers (BiTEs), and a BCMA antibody–drug conjugate, Dr. Kumar said at the annual congress on Hematologic Malignancies held by the National Comprehensive Cancer Network.
“Clearly, there are a lot of exciting drugs that are currently in clinical trials, but these three platforms appear to be much more advanced than the others, and hopefully we will see that in the clinic in the near future,” Dr. Kumar said.
The antibody-drug conjugate, GSK2857916, is a humanized IgG1 anti-BCMA antibody conjugated to a microtubule-disrupting agent that has produced an overall response rate in 67% in a group of myeloma patients who had previously received multiple standard-of-care agents.
“Some of the responses were quite durable, lasting several months,” he said.
Now, GSK2857916 is being evaluated in a variety of different combinations, including in a phase 2 study of the antibody-drug conjugate in combination with lenalidomide plus dexamethasone, or bortezomib plus dexamethasone, in patients with relapsed or refractory disease.
Some of the most “exciting” data with anti-BCMA CAR T-cell therapy in myeloma involves bb2121, which showed durable clinical responses in heavily pretreated patients, according to data presented at the 2017 annual meeting of the American Society of Hematology.
“The overall response rate is quite significant,” said Dr. Kumar, who related a 94% rate of overall response that was even higher in patients treated with doses of 150 x 106 CAR+ T cells or more. Many of the response were lasting, he said, with five patients in ongoing response for more than 1 year.
“The results are exciting enough that this is actually moving forward with registration trials,” Dr. Kumar said.
Additionally, promising results have been presented on a novel CAR T-cell product, LCAR-B38M, which principally targets BCMA and led to a significant number of patients who achieved stringent complete response that lasted beyond 1 year.
Multiple BCMA-targeting CAR T-cell products that use different vectors and costimulatory molecules are currently undergoing clinical trials, Dr. Kumar said.
In contrast to CAR T-cell products that must be customized to each patient in a process that takes weeks, BiTEs are a ready-made approach to allow T cells to engage with tumor cells.
“In patients with advanced disease, a lot can change in that short time frame, so having an approach that is off the shelf, which is not patient specific, is quite attractive,” Dr. Kumar said.
BCMA-directed BiTE therapies under investigation include AMG 420 and PF-06863135, he added.
Dr. Kumar reported one disclosure related to Dr. Reddy’s Laboratories.
NEW YORK – Three novel treatment strategies that target B-cell maturation antigen (BCMA) have shown promise in recent multiple myeloma clinical trials, according to Shaji K. Kumar, MD, of the Mayo Clinic Cancer Center in Rochester, Minn.
These strategies include B-cell maturation antigen (BCMA)–specific chimeric antigen receptor (CAR) T-cell therapies, bispecific T-cell engagers (BiTEs), and a BCMA antibody–drug conjugate, Dr. Kumar said at the annual congress on Hematologic Malignancies held by the National Comprehensive Cancer Network.
“Clearly, there are a lot of exciting drugs that are currently in clinical trials, but these three platforms appear to be much more advanced than the others, and hopefully we will see that in the clinic in the near future,” Dr. Kumar said.
The antibody-drug conjugate, GSK2857916, is a humanized IgG1 anti-BCMA antibody conjugated to a microtubule-disrupting agent that has produced an overall response rate in 67% in a group of myeloma patients who had previously received multiple standard-of-care agents.
“Some of the responses were quite durable, lasting several months,” he said.
Now, GSK2857916 is being evaluated in a variety of different combinations, including in a phase 2 study of the antibody-drug conjugate in combination with lenalidomide plus dexamethasone, or bortezomib plus dexamethasone, in patients with relapsed or refractory disease.
Some of the most “exciting” data with anti-BCMA CAR T-cell therapy in myeloma involves bb2121, which showed durable clinical responses in heavily pretreated patients, according to data presented at the 2017 annual meeting of the American Society of Hematology.
“The overall response rate is quite significant,” said Dr. Kumar, who related a 94% rate of overall response that was even higher in patients treated with doses of 150 x 106 CAR+ T cells or more. Many of the response were lasting, he said, with five patients in ongoing response for more than 1 year.
“The results are exciting enough that this is actually moving forward with registration trials,” Dr. Kumar said.
Additionally, promising results have been presented on a novel CAR T-cell product, LCAR-B38M, which principally targets BCMA and led to a significant number of patients who achieved stringent complete response that lasted beyond 1 year.
Multiple BCMA-targeting CAR T-cell products that use different vectors and costimulatory molecules are currently undergoing clinical trials, Dr. Kumar said.
In contrast to CAR T-cell products that must be customized to each patient in a process that takes weeks, BiTEs are a ready-made approach to allow T cells to engage with tumor cells.
“In patients with advanced disease, a lot can change in that short time frame, so having an approach that is off the shelf, which is not patient specific, is quite attractive,” Dr. Kumar said.
BCMA-directed BiTE therapies under investigation include AMG 420 and PF-06863135, he added.
Dr. Kumar reported one disclosure related to Dr. Reddy’s Laboratories.
NEW YORK – Three novel treatment strategies that target B-cell maturation antigen (BCMA) have shown promise in recent multiple myeloma clinical trials, according to Shaji K. Kumar, MD, of the Mayo Clinic Cancer Center in Rochester, Minn.
These strategies include B-cell maturation antigen (BCMA)–specific chimeric antigen receptor (CAR) T-cell therapies, bispecific T-cell engagers (BiTEs), and a BCMA antibody–drug conjugate, Dr. Kumar said at the annual congress on Hematologic Malignancies held by the National Comprehensive Cancer Network.
“Clearly, there are a lot of exciting drugs that are currently in clinical trials, but these three platforms appear to be much more advanced than the others, and hopefully we will see that in the clinic in the near future,” Dr. Kumar said.
The antibody-drug conjugate, GSK2857916, is a humanized IgG1 anti-BCMA antibody conjugated to a microtubule-disrupting agent that has produced an overall response rate in 67% in a group of myeloma patients who had previously received multiple standard-of-care agents.
“Some of the responses were quite durable, lasting several months,” he said.
Now, GSK2857916 is being evaluated in a variety of different combinations, including in a phase 2 study of the antibody-drug conjugate in combination with lenalidomide plus dexamethasone, or bortezomib plus dexamethasone, in patients with relapsed or refractory disease.
Some of the most “exciting” data with anti-BCMA CAR T-cell therapy in myeloma involves bb2121, which showed durable clinical responses in heavily pretreated patients, according to data presented at the 2017 annual meeting of the American Society of Hematology.
“The overall response rate is quite significant,” said Dr. Kumar, who related a 94% rate of overall response that was even higher in patients treated with doses of 150 x 106 CAR+ T cells or more. Many of the response were lasting, he said, with five patients in ongoing response for more than 1 year.
“The results are exciting enough that this is actually moving forward with registration trials,” Dr. Kumar said.
Additionally, promising results have been presented on a novel CAR T-cell product, LCAR-B38M, which principally targets BCMA and led to a significant number of patients who achieved stringent complete response that lasted beyond 1 year.
Multiple BCMA-targeting CAR T-cell products that use different vectors and costimulatory molecules are currently undergoing clinical trials, Dr. Kumar said.
In contrast to CAR T-cell products that must be customized to each patient in a process that takes weeks, BiTEs are a ready-made approach to allow T cells to engage with tumor cells.
“In patients with advanced disease, a lot can change in that short time frame, so having an approach that is off the shelf, which is not patient specific, is quite attractive,” Dr. Kumar said.
BCMA-directed BiTE therapies under investigation include AMG 420 and PF-06863135, he added.
Dr. Kumar reported one disclosure related to Dr. Reddy’s Laboratories.
EXPERT ANALYSIS FROM THE NCCN HEMATOLOGIC MALIGNANCIES CONGRESS
Checkpoint inhibitor linked to antiphospholipid syndrome in melanoma patient
A patient with melanoma experienced antiphospholipid syndrome following multiple infusions of the PD-1 inhibitor pembrolizumab, according to authors of a recent case report.
Presence of Raynaud phenomenon and high levels of antiphospholipid antibodies led to the diagnosis of antiphospholipid syndrome in the patient, who had stage IIIB unresectable melanoma.
This report provides additional evidence that this syndrome is an immune-related adverse event associated with checkpoint inhibitor therapy, said Alexandra Picard, MD, of Hôpital Archet, Nice, France, and coauthors.
“Due to the increased use of anti PD-1 therapies, clinicians should be aware of this new potential immune-mediated toxic effect that manifests as antiphospholipid syndrome,” the researchers wrote. The report is in JAMA Dermatology.
“Great caution” should be exercised when considering use of immune checkpoint inhibitors in patients with a history of antiphospholipid syndrome, the authors added.
The woman in this report was over 60 years of age and had first presented with superficial melanoma on her right calf, followed by recurrent lymph node metastases over the next few years, all of which were surgically treated.
Following a PET-CT scan showing a new metastatic lymph node, the woman started pembrolizumab 2 mg/kg every 3 weeks and had a partial response within 3 months, the investigators reported.
After the tenth infusion, however, the patient developed bilateral secondary Raynaud phenomenon that followed a typical discoloration sequence and resulted in a necrotic lesion at the tip of one finger.
The patient had no personal or family history of Raynaud phenomenon.
While beta2-glycoprotein 1 antibodies were not elevated, laboratory tests did show anticardiolipin antibodies and lupus anticoagulants at elevated levels, the investigators said, noting that repeat testing at 12 weeks confirmed positivity of antiphospholipid antibodies.
The Raynaud phenomenon disappeared and the necrotic lesion healed after pembrolizumab was stopped and prednisolone treatment was started, they added.
No recurrence of either was noted at the last follow-up.
Previous reports have described antiphospholipid syndrome in advanced melanoma patients treated with alfa-2b interferon alone or in combination with anti-interleukin 2, the authors said in their discussion of the case.
In addition, there has been another recent report of antiphospholipid syndrome associated with the CTLA4 inhibitor ipilimumab and the PD-1 inhibitor nivolumab, they said. In that case, testing for antiphospholipid antibodies revealed elevated beta2-glycoprotein 1 antibody levels.
“We hypothesize that [antiphospholipid syndrome] is a kind of autoimmunity induced by anti–PD-1 due to the expansive expression of the immune system against tumor cells,” the researchers wrote.
Although a case of cancer-associated antiphospholipid syndrome could not be ruled out in the present report, the rapid and complete resolution of symptoms after treatment discontinuation suggested that pembrolizumab, a “known immunostimulant,” was the cause, they said.
While antibodies against PD-1 have improved melanoma prognosis, they are associated with a wide range of immune-related adverse effects in the skin, gastrointestinal tract, liver, and endocrine system, Dr. Picard and coauthors noted.
They reported having no conflicts of interest.
SOURCE: Sanchez A, et al. JAMA Derm. 2018 Sep 19. doi: 10.1001/jamadermatol.2018.2770.
A patient with melanoma experienced antiphospholipid syndrome following multiple infusions of the PD-1 inhibitor pembrolizumab, according to authors of a recent case report.
Presence of Raynaud phenomenon and high levels of antiphospholipid antibodies led to the diagnosis of antiphospholipid syndrome in the patient, who had stage IIIB unresectable melanoma.
This report provides additional evidence that this syndrome is an immune-related adverse event associated with checkpoint inhibitor therapy, said Alexandra Picard, MD, of Hôpital Archet, Nice, France, and coauthors.
“Due to the increased use of anti PD-1 therapies, clinicians should be aware of this new potential immune-mediated toxic effect that manifests as antiphospholipid syndrome,” the researchers wrote. The report is in JAMA Dermatology.
“Great caution” should be exercised when considering use of immune checkpoint inhibitors in patients with a history of antiphospholipid syndrome, the authors added.
The woman in this report was over 60 years of age and had first presented with superficial melanoma on her right calf, followed by recurrent lymph node metastases over the next few years, all of which were surgically treated.
Following a PET-CT scan showing a new metastatic lymph node, the woman started pembrolizumab 2 mg/kg every 3 weeks and had a partial response within 3 months, the investigators reported.
After the tenth infusion, however, the patient developed bilateral secondary Raynaud phenomenon that followed a typical discoloration sequence and resulted in a necrotic lesion at the tip of one finger.
The patient had no personal or family history of Raynaud phenomenon.
While beta2-glycoprotein 1 antibodies were not elevated, laboratory tests did show anticardiolipin antibodies and lupus anticoagulants at elevated levels, the investigators said, noting that repeat testing at 12 weeks confirmed positivity of antiphospholipid antibodies.
The Raynaud phenomenon disappeared and the necrotic lesion healed after pembrolizumab was stopped and prednisolone treatment was started, they added.
No recurrence of either was noted at the last follow-up.
Previous reports have described antiphospholipid syndrome in advanced melanoma patients treated with alfa-2b interferon alone or in combination with anti-interleukin 2, the authors said in their discussion of the case.
In addition, there has been another recent report of antiphospholipid syndrome associated with the CTLA4 inhibitor ipilimumab and the PD-1 inhibitor nivolumab, they said. In that case, testing for antiphospholipid antibodies revealed elevated beta2-glycoprotein 1 antibody levels.
“We hypothesize that [antiphospholipid syndrome] is a kind of autoimmunity induced by anti–PD-1 due to the expansive expression of the immune system against tumor cells,” the researchers wrote.
Although a case of cancer-associated antiphospholipid syndrome could not be ruled out in the present report, the rapid and complete resolution of symptoms after treatment discontinuation suggested that pembrolizumab, a “known immunostimulant,” was the cause, they said.
While antibodies against PD-1 have improved melanoma prognosis, they are associated with a wide range of immune-related adverse effects in the skin, gastrointestinal tract, liver, and endocrine system, Dr. Picard and coauthors noted.
They reported having no conflicts of interest.
SOURCE: Sanchez A, et al. JAMA Derm. 2018 Sep 19. doi: 10.1001/jamadermatol.2018.2770.
A patient with melanoma experienced antiphospholipid syndrome following multiple infusions of the PD-1 inhibitor pembrolizumab, according to authors of a recent case report.
Presence of Raynaud phenomenon and high levels of antiphospholipid antibodies led to the diagnosis of antiphospholipid syndrome in the patient, who had stage IIIB unresectable melanoma.
This report provides additional evidence that this syndrome is an immune-related adverse event associated with checkpoint inhibitor therapy, said Alexandra Picard, MD, of Hôpital Archet, Nice, France, and coauthors.
“Due to the increased use of anti PD-1 therapies, clinicians should be aware of this new potential immune-mediated toxic effect that manifests as antiphospholipid syndrome,” the researchers wrote. The report is in JAMA Dermatology.
“Great caution” should be exercised when considering use of immune checkpoint inhibitors in patients with a history of antiphospholipid syndrome, the authors added.
The woman in this report was over 60 years of age and had first presented with superficial melanoma on her right calf, followed by recurrent lymph node metastases over the next few years, all of which were surgically treated.
Following a PET-CT scan showing a new metastatic lymph node, the woman started pembrolizumab 2 mg/kg every 3 weeks and had a partial response within 3 months, the investigators reported.
After the tenth infusion, however, the patient developed bilateral secondary Raynaud phenomenon that followed a typical discoloration sequence and resulted in a necrotic lesion at the tip of one finger.
The patient had no personal or family history of Raynaud phenomenon.
While beta2-glycoprotein 1 antibodies were not elevated, laboratory tests did show anticardiolipin antibodies and lupus anticoagulants at elevated levels, the investigators said, noting that repeat testing at 12 weeks confirmed positivity of antiphospholipid antibodies.
The Raynaud phenomenon disappeared and the necrotic lesion healed after pembrolizumab was stopped and prednisolone treatment was started, they added.
No recurrence of either was noted at the last follow-up.
Previous reports have described antiphospholipid syndrome in advanced melanoma patients treated with alfa-2b interferon alone or in combination with anti-interleukin 2, the authors said in their discussion of the case.
In addition, there has been another recent report of antiphospholipid syndrome associated with the CTLA4 inhibitor ipilimumab and the PD-1 inhibitor nivolumab, they said. In that case, testing for antiphospholipid antibodies revealed elevated beta2-glycoprotein 1 antibody levels.
“We hypothesize that [antiphospholipid syndrome] is a kind of autoimmunity induced by anti–PD-1 due to the expansive expression of the immune system against tumor cells,” the researchers wrote.
Although a case of cancer-associated antiphospholipid syndrome could not be ruled out in the present report, the rapid and complete resolution of symptoms after treatment discontinuation suggested that pembrolizumab, a “known immunostimulant,” was the cause, they said.
While antibodies against PD-1 have improved melanoma prognosis, they are associated with a wide range of immune-related adverse effects in the skin, gastrointestinal tract, liver, and endocrine system, Dr. Picard and coauthors noted.
They reported having no conflicts of interest.
SOURCE: Sanchez A, et al. JAMA Derm. 2018 Sep 19. doi: 10.1001/jamadermatol.2018.2770.
FROM JAMA DERMATOLOGY
Key clinical point: Antiphospholipid syndrome appears to be an immune-related adverse event associated with anti-PD-1 therapy.
Major finding: A melanoma patient receiving pembrolizumab was diagnosed with antiphospholipid syndrome that resolved following discontinuation of that treatment.
Study details: Case report of a woman in her 60s with stage IIIB unresectable melanoma who was treated with pembrolizumab 2 mg/kg every 3 weeks.
Disclosures: The authors reported no conflicts of interest.
Source: Sanchez A et al. JAMA Derm. 2018 Sep 19. doi: 10.1001/jamadermatol.2018.2770.
Venetoclax promising in unfit elderly AML patients
New York – For unfit elderly patients with acute myeloid leukemia (AML), venetoclax may be one of the most promising potential options that is emerging, according to an expert in the field.
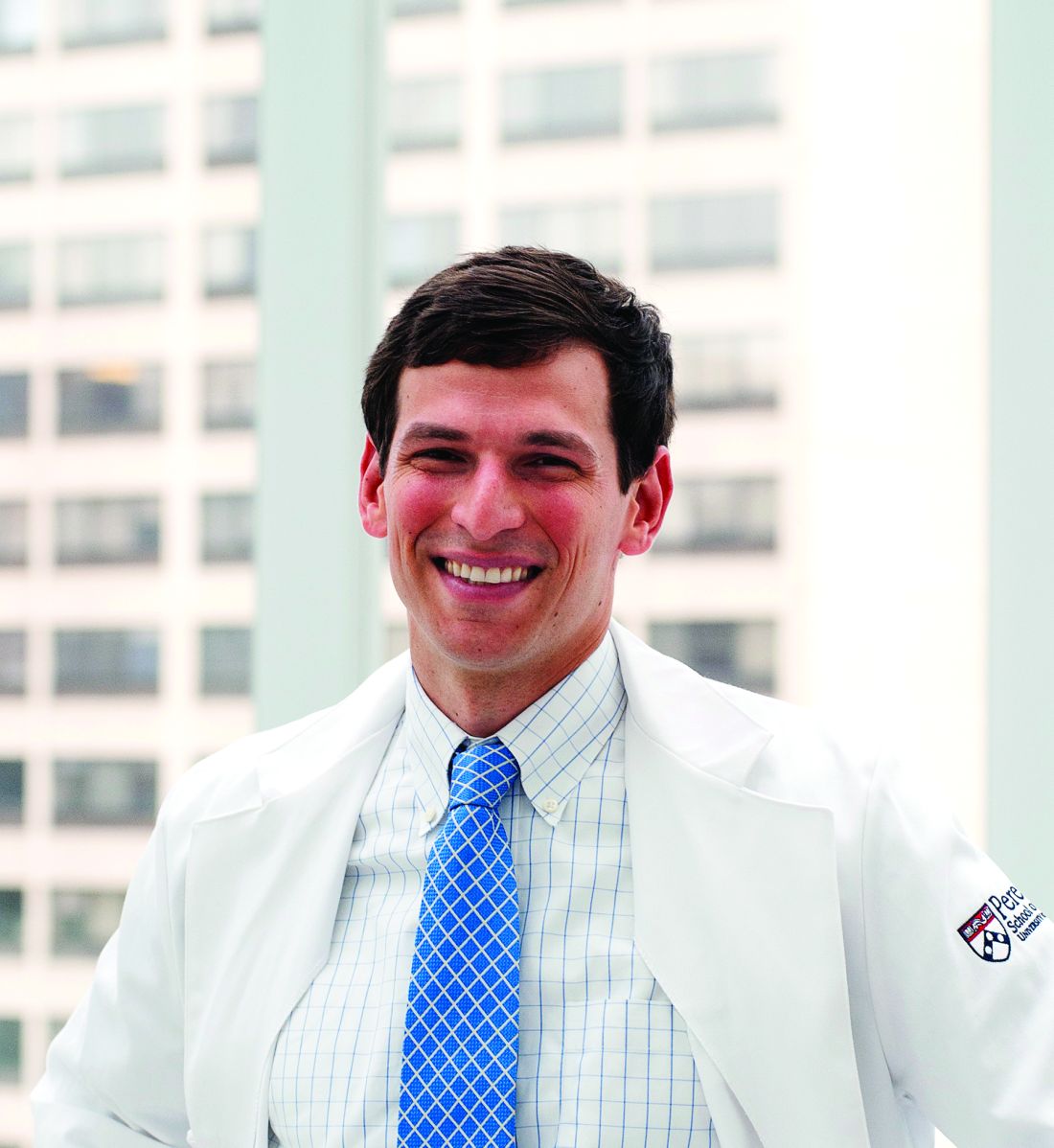
The oral B-cell lymphoma 2 (BCL-2) inhibitor is the treatment that some in the AML community are “most excited about” for this population, Eunice S. Wang, MD, of Roswell Park Comprehensive Cancer Center in Buffalo, N.Y., said at the National Comprehensive Cancer Network (NCCN) Annual Congress: Hematologic Malignancies.
Venetoclax is currently approved by the Food and Drug Administration for previously treated chronic lymphocytic leukemia (CLL), alone or in combination with rituximab. It has been granted four Breakthrough Therapy designations from the FDA in AML. In July 2018, AbbVie submitted a Supplemental New Drug Application to the FDA for its use in combination with a hypomethylating agent (HMA) or in combination with low-dose cytarabine (LDAC) for the treatment of newly diagnosed AML patients who are ineligible for intensive chemotherapy.
“This agent doesn’t work on its own but had worked in the refractory setting and can be a great option upfront,” Dr. Wang said.
About half the patients were alive at 1 year following treatment with venetoclax plus low-dose chemotherapy, whether that was LDAC or an HMA, she said, commenting on recently reported results.
In a phase 1b trial, venetoclax was evaluated in combination with either azacitidine or decitabine. In recently reported preliminary results that included 57 patients aged 65 years or older who were ineligible for standard induction therapy, the combination was well tolerated and had promising activity (Lancet Oncol. 2018 Feb;19[2]:216-28).
Overall, 35 patients (61%) had complete remission (CR) or complete remission with incomplete marrow recovery (CRi).
In another report on this same trial, which included 33 patients from a single participating center who received venetoclax and azacytidine, the overall response rate was 91%, including 19 (58%) with CR and 9 (27%) with CRi (Blood. 2017 Dec;130 [Suppl 1]:181).
A separate phase 1/2 trial examined venetoclax plus LDAC in treatment-naive elderly patients unfit for intensive chemotherapy. In the 1-year outcomes that have been reported, the observed CR/CRi rate was 62%, median overall survival was an “encouraging” 11.4 months, and the observed 12-month overall survival was 46% in 61 patients treated at a venetoclax dose of 600 mg (Blood. 2017 Dec;130 [Suppl 1]:890).
In those 61 patients, treatment-related grade 3/4 adverse events included thrombocytopenia in 59%, neutropenia in 46%, febrile neutropenia in 36%, anemia in 28%, decreased white blood cell count in 26%, and one case of tumor lysis syndrome, according to the report.
Based on those findings in a cohort of patients with poor risk features, venetoclax 600 mg plus LDAC was carried forward to be evaluated in an ongoing phase 3 study, investigators noted at the time.
Dr. Wang reported financial relationships with AbbVie, Amgen, ImmunoGen, Incyte, Novartis, and Otsuka.
New York – For unfit elderly patients with acute myeloid leukemia (AML), venetoclax may be one of the most promising potential options that is emerging, according to an expert in the field.
The oral B-cell lymphoma 2 (BCL-2) inhibitor is the treatment that some in the AML community are “most excited about” for this population, Eunice S. Wang, MD, of Roswell Park Comprehensive Cancer Center in Buffalo, N.Y., said at the National Comprehensive Cancer Network (NCCN) Annual Congress: Hematologic Malignancies.
Venetoclax is currently approved by the Food and Drug Administration for previously treated chronic lymphocytic leukemia (CLL), alone or in combination with rituximab. It has been granted four Breakthrough Therapy designations from the FDA in AML. In July 2018, AbbVie submitted a Supplemental New Drug Application to the FDA for its use in combination with a hypomethylating agent (HMA) or in combination with low-dose cytarabine (LDAC) for the treatment of newly diagnosed AML patients who are ineligible for intensive chemotherapy.
“This agent doesn’t work on its own but had worked in the refractory setting and can be a great option upfront,” Dr. Wang said.
About half the patients were alive at 1 year following treatment with venetoclax plus low-dose chemotherapy, whether that was LDAC or an HMA, she said, commenting on recently reported results.
In a phase 1b trial, venetoclax was evaluated in combination with either azacitidine or decitabine. In recently reported preliminary results that included 57 patients aged 65 years or older who were ineligible for standard induction therapy, the combination was well tolerated and had promising activity (Lancet Oncol. 2018 Feb;19[2]:216-28).
Overall, 35 patients (61%) had complete remission (CR) or complete remission with incomplete marrow recovery (CRi).
In another report on this same trial, which included 33 patients from a single participating center who received venetoclax and azacytidine, the overall response rate was 91%, including 19 (58%) with CR and 9 (27%) with CRi (Blood. 2017 Dec;130 [Suppl 1]:181).
A separate phase 1/2 trial examined venetoclax plus LDAC in treatment-naive elderly patients unfit for intensive chemotherapy. In the 1-year outcomes that have been reported, the observed CR/CRi rate was 62%, median overall survival was an “encouraging” 11.4 months, and the observed 12-month overall survival was 46% in 61 patients treated at a venetoclax dose of 600 mg (Blood. 2017 Dec;130 [Suppl 1]:890).
In those 61 patients, treatment-related grade 3/4 adverse events included thrombocytopenia in 59%, neutropenia in 46%, febrile neutropenia in 36%, anemia in 28%, decreased white blood cell count in 26%, and one case of tumor lysis syndrome, according to the report.
Based on those findings in a cohort of patients with poor risk features, venetoclax 600 mg plus LDAC was carried forward to be evaluated in an ongoing phase 3 study, investigators noted at the time.
Dr. Wang reported financial relationships with AbbVie, Amgen, ImmunoGen, Incyte, Novartis, and Otsuka.
New York – For unfit elderly patients with acute myeloid leukemia (AML), venetoclax may be one of the most promising potential options that is emerging, according to an expert in the field.
The oral B-cell lymphoma 2 (BCL-2) inhibitor is the treatment that some in the AML community are “most excited about” for this population, Eunice S. Wang, MD, of Roswell Park Comprehensive Cancer Center in Buffalo, N.Y., said at the National Comprehensive Cancer Network (NCCN) Annual Congress: Hematologic Malignancies.
Venetoclax is currently approved by the Food and Drug Administration for previously treated chronic lymphocytic leukemia (CLL), alone or in combination with rituximab. It has been granted four Breakthrough Therapy designations from the FDA in AML. In July 2018, AbbVie submitted a Supplemental New Drug Application to the FDA for its use in combination with a hypomethylating agent (HMA) or in combination with low-dose cytarabine (LDAC) for the treatment of newly diagnosed AML patients who are ineligible for intensive chemotherapy.
“This agent doesn’t work on its own but had worked in the refractory setting and can be a great option upfront,” Dr. Wang said.
About half the patients were alive at 1 year following treatment with venetoclax plus low-dose chemotherapy, whether that was LDAC or an HMA, she said, commenting on recently reported results.
In a phase 1b trial, venetoclax was evaluated in combination with either azacitidine or decitabine. In recently reported preliminary results that included 57 patients aged 65 years or older who were ineligible for standard induction therapy, the combination was well tolerated and had promising activity (Lancet Oncol. 2018 Feb;19[2]:216-28).
Overall, 35 patients (61%) had complete remission (CR) or complete remission with incomplete marrow recovery (CRi).
In another report on this same trial, which included 33 patients from a single participating center who received venetoclax and azacytidine, the overall response rate was 91%, including 19 (58%) with CR and 9 (27%) with CRi (Blood. 2017 Dec;130 [Suppl 1]:181).
A separate phase 1/2 trial examined venetoclax plus LDAC in treatment-naive elderly patients unfit for intensive chemotherapy. In the 1-year outcomes that have been reported, the observed CR/CRi rate was 62%, median overall survival was an “encouraging” 11.4 months, and the observed 12-month overall survival was 46% in 61 patients treated at a venetoclax dose of 600 mg (Blood. 2017 Dec;130 [Suppl 1]:890).
In those 61 patients, treatment-related grade 3/4 adverse events included thrombocytopenia in 59%, neutropenia in 46%, febrile neutropenia in 36%, anemia in 28%, decreased white blood cell count in 26%, and one case of tumor lysis syndrome, according to the report.
Based on those findings in a cohort of patients with poor risk features, venetoclax 600 mg plus LDAC was carried forward to be evaluated in an ongoing phase 3 study, investigators noted at the time.
Dr. Wang reported financial relationships with AbbVie, Amgen, ImmunoGen, Incyte, Novartis, and Otsuka.
EXPERT ANALYSIS FROM THE NCCN ANNUAL CONGRESS: HEMATOLOGIC MALIGNANCIES
Researchers share Nobel Prize for cancer immunotherapy discoveries
Two researchers who made groundbreaking discoveries leading to the development of immune checkpoint therapy have jointly received the 2018 Nobel Prize in Physiology or Medicine.
James P. Allison, PhD, and Tasuku Honjo, MD, PhD, share the prize for their work in showing how strategies for “inhibiting the brakes” on T cells can be used in the treatment of cancer, the Nobel Assembly at Karolinska Institutet, Stockholm, said in a news release.
The discoveries of Dr. Allison and Dr. Honjo represent a landmark in the fight against cancer, according to the Nobel Assembly.
“This new form of immunotherapy unleashes a vigorous, and often durable, immune response directed against essentially any tumor already recognized by the immune system,” members of the Nobel Committee and Assembly said in a simultaneously published manuscript explaining the scientific background behind the discovery.
The “unprecedented” research activity in the immune checkpoint field demonstrates how influential the discoveries of Dr. Allison and Dr. Honjo have been, molecular genetics professor C. I. Edvard Smith, MD, PhD, and coauthors said in the manuscript.
Their findings have “conferred great benefit on mankind” and add a “new pillar” to existing cancer treatments, Dr. Smith and coauthors said in their report.
Dr. Allison was one of several scientists to observe that the cytotoxic T-lymphocyte antigen 4 (CTLA4) protein functions as a brake on T cells, the Nobel Assembly said in the press release. He developed an antibody that could bind to CTLA4 and block its function, and demonstrated its activity in experiments taking place near the end of 1994.
The “spectacular” results showed that, in mice, the antibodies could inhibit the brake and unlock antitumor T-cell activity, according to the release.
Studies of CTLA-4 blockade in humans from several research groups yielded promising results, and in 2010, a major breakthrough came, according to the Nobel Assembly, when it was reported that the CTLA4 blocker ipilimumab improved survival in patients with metastatic melanoma.
Dr. Honjo discovered the programmed cell death protein (PD-1) in 1992, a few years before Dr. Allison’s discovery, and explored its function in experiments carried out over many years at his laboratory at Kyoto University.
Dr. Honjo’s experiments showed that PD-1 functioned as a T-cell brake, but by a different mechanism than CTLA4, paving the way for studying PD-1 as a target of cancer treatment.
That led to a considerable amount of clinical development, including a key 2012 study showing that patients treated with the anti-PD-1 antibody nivolumab led to long-term remissions and possible cures in some patients, the assembly said in their press release.
Scientists have attempted to harness the immune system in the fight against cancer for more than 100 years, according to the assembly. “Until the seminal discoveries by the two laureates, progress into clinical development was modest. Checkpoint therapy has now revolutionized cancer treatment and has fundamentally changed the way we view how cancer can be managed.”
Two researchers who made groundbreaking discoveries leading to the development of immune checkpoint therapy have jointly received the 2018 Nobel Prize in Physiology or Medicine.
James P. Allison, PhD, and Tasuku Honjo, MD, PhD, share the prize for their work in showing how strategies for “inhibiting the brakes” on T cells can be used in the treatment of cancer, the Nobel Assembly at Karolinska Institutet, Stockholm, said in a news release.
The discoveries of Dr. Allison and Dr. Honjo represent a landmark in the fight against cancer, according to the Nobel Assembly.
“This new form of immunotherapy unleashes a vigorous, and often durable, immune response directed against essentially any tumor already recognized by the immune system,” members of the Nobel Committee and Assembly said in a simultaneously published manuscript explaining the scientific background behind the discovery.
The “unprecedented” research activity in the immune checkpoint field demonstrates how influential the discoveries of Dr. Allison and Dr. Honjo have been, molecular genetics professor C. I. Edvard Smith, MD, PhD, and coauthors said in the manuscript.
Their findings have “conferred great benefit on mankind” and add a “new pillar” to existing cancer treatments, Dr. Smith and coauthors said in their report.
Dr. Allison was one of several scientists to observe that the cytotoxic T-lymphocyte antigen 4 (CTLA4) protein functions as a brake on T cells, the Nobel Assembly said in the press release. He developed an antibody that could bind to CTLA4 and block its function, and demonstrated its activity in experiments taking place near the end of 1994.
The “spectacular” results showed that, in mice, the antibodies could inhibit the brake and unlock antitumor T-cell activity, according to the release.
Studies of CTLA-4 blockade in humans from several research groups yielded promising results, and in 2010, a major breakthrough came, according to the Nobel Assembly, when it was reported that the CTLA4 blocker ipilimumab improved survival in patients with metastatic melanoma.
Dr. Honjo discovered the programmed cell death protein (PD-1) in 1992, a few years before Dr. Allison’s discovery, and explored its function in experiments carried out over many years at his laboratory at Kyoto University.
Dr. Honjo’s experiments showed that PD-1 functioned as a T-cell brake, but by a different mechanism than CTLA4, paving the way for studying PD-1 as a target of cancer treatment.
That led to a considerable amount of clinical development, including a key 2012 study showing that patients treated with the anti-PD-1 antibody nivolumab led to long-term remissions and possible cures in some patients, the assembly said in their press release.
Scientists have attempted to harness the immune system in the fight against cancer for more than 100 years, according to the assembly. “Until the seminal discoveries by the two laureates, progress into clinical development was modest. Checkpoint therapy has now revolutionized cancer treatment and has fundamentally changed the way we view how cancer can be managed.”
Two researchers who made groundbreaking discoveries leading to the development of immune checkpoint therapy have jointly received the 2018 Nobel Prize in Physiology or Medicine.
James P. Allison, PhD, and Tasuku Honjo, MD, PhD, share the prize for their work in showing how strategies for “inhibiting the brakes” on T cells can be used in the treatment of cancer, the Nobel Assembly at Karolinska Institutet, Stockholm, said in a news release.
The discoveries of Dr. Allison and Dr. Honjo represent a landmark in the fight against cancer, according to the Nobel Assembly.
“This new form of immunotherapy unleashes a vigorous, and often durable, immune response directed against essentially any tumor already recognized by the immune system,” members of the Nobel Committee and Assembly said in a simultaneously published manuscript explaining the scientific background behind the discovery.
The “unprecedented” research activity in the immune checkpoint field demonstrates how influential the discoveries of Dr. Allison and Dr. Honjo have been, molecular genetics professor C. I. Edvard Smith, MD, PhD, and coauthors said in the manuscript.
Their findings have “conferred great benefit on mankind” and add a “new pillar” to existing cancer treatments, Dr. Smith and coauthors said in their report.
Dr. Allison was one of several scientists to observe that the cytotoxic T-lymphocyte antigen 4 (CTLA4) protein functions as a brake on T cells, the Nobel Assembly said in the press release. He developed an antibody that could bind to CTLA4 and block its function, and demonstrated its activity in experiments taking place near the end of 1994.
The “spectacular” results showed that, in mice, the antibodies could inhibit the brake and unlock antitumor T-cell activity, according to the release.
Studies of CTLA-4 blockade in humans from several research groups yielded promising results, and in 2010, a major breakthrough came, according to the Nobel Assembly, when it was reported that the CTLA4 blocker ipilimumab improved survival in patients with metastatic melanoma.
Dr. Honjo discovered the programmed cell death protein (PD-1) in 1992, a few years before Dr. Allison’s discovery, and explored its function in experiments carried out over many years at his laboratory at Kyoto University.
Dr. Honjo’s experiments showed that PD-1 functioned as a T-cell brake, but by a different mechanism than CTLA4, paving the way for studying PD-1 as a target of cancer treatment.
That led to a considerable amount of clinical development, including a key 2012 study showing that patients treated with the anti-PD-1 antibody nivolumab led to long-term remissions and possible cures in some patients, the assembly said in their press release.
Scientists have attempted to harness the immune system in the fight against cancer for more than 100 years, according to the assembly. “Until the seminal discoveries by the two laureates, progress into clinical development was modest. Checkpoint therapy has now revolutionized cancer treatment and has fundamentally changed the way we view how cancer can be managed.”
BCMA-targeted platforms could alter MM therapy
New York—Three novel treatment strategies that target B-cell maturation antigen (BCMA) are showing promise in recent multiple myeloma (MM) clinical trials, according to Shaji K. Kumar, MD, of Mayo Clinic Cancer Center in Rochester, Minnesota.
The strategies include B-cell maturation antigen (BCMA) antibody-drug conjugate, BCMA-specific chimeric antigen receptor (CAR) T-cell therapies, and bispecific T-cell engagers (BiTEs).
“Clearly, there are a lot of exciting drugs that are currently in clinical trials, but these 3 platforms appear to be much more advanced than the others, and hopefully we will see that in the clinic in the near future,” Dr. Kumar told attendees at the NCCN 13th Annual Congress: Hematologic Malignancies.
BCMA is required for plasma cell survival and is broadly expressed on malignant plasma cells.
BCMA antibody-drug conjugate
The antibody-drug conjugate, GSK2857916, is a humanized IgG1 anti-BCMA antibody conjugated to a microtubule-disrupting agent. It produced an overall response rate of 67% at the 2 highest dose levels in 9 MM patients who had previously received multiple standard-of-care agents.
“Some of the responses were quite durable, lasting several months,” he said.
Now, GSK2857916 is being evaluated in a variety of different combinations, he said, including in an upcoming phase 2 study of the antibody-drug conjugate in combination with lenalidomide plus dexamethasone or bortezomib plus dexamethasone in patients with relapsed or refractory disease.
BCMA-specific CAR T-cell therapy
Some of the most “exciting” data with anti-BCMA CAR T-cell therapy in myeloma, according to Dr. Kumar, involves bb2121. bb2121 showed durable clinical responses in heavily pretreated patients, according to an ASH 2017 presentation.
“The overall response rate is quite significant,” Dr. Kumar said. He related a 94% rate of overall response that was even higher in patients treated with doses of 150 x 106 CAR+ T cells or more. Many of the responses were lasting, he said, with 5 patients in ongoing response for more than a year.
“The results are exciting enough that this is actually moving forward with registration trials,” Dr. Kumar added.
Another novel CAR T-cell product, LCAR-B38M, has demonstrated promising results. LCAR-B38M principally targets BCMA and has led to a significant number of patients achieving stringent complete response that lasted beyond 1 year.
Multiple BCMA-targeting CAR T-cell products that use different vectors and different costimulatory molecules are currently in clinical trials, Dr. Kumar said.
BiTEs
In contrast to CAR T-cell products that must be customized to each patient in a process that takes weeks, BiTEs are a ready-made approach to allow T cells to engage with tumor cells.
“In patients with advanced disease, a lot can change in that short timeframe, so having an approach that is off-the-shelf, which is not patient specific, is quite attractive,” Dr. Kumar said.
BCMA-directed BiTE therapies to watch that are under investigation include AMG 420 and PF-06863135, he said.
New York—Three novel treatment strategies that target B-cell maturation antigen (BCMA) are showing promise in recent multiple myeloma (MM) clinical trials, according to Shaji K. Kumar, MD, of Mayo Clinic Cancer Center in Rochester, Minnesota.
The strategies include B-cell maturation antigen (BCMA) antibody-drug conjugate, BCMA-specific chimeric antigen receptor (CAR) T-cell therapies, and bispecific T-cell engagers (BiTEs).
“Clearly, there are a lot of exciting drugs that are currently in clinical trials, but these 3 platforms appear to be much more advanced than the others, and hopefully we will see that in the clinic in the near future,” Dr. Kumar told attendees at the NCCN 13th Annual Congress: Hematologic Malignancies.
BCMA is required for plasma cell survival and is broadly expressed on malignant plasma cells.
BCMA antibody-drug conjugate
The antibody-drug conjugate, GSK2857916, is a humanized IgG1 anti-BCMA antibody conjugated to a microtubule-disrupting agent. It produced an overall response rate of 67% at the 2 highest dose levels in 9 MM patients who had previously received multiple standard-of-care agents.
“Some of the responses were quite durable, lasting several months,” he said.
Now, GSK2857916 is being evaluated in a variety of different combinations, he said, including in an upcoming phase 2 study of the antibody-drug conjugate in combination with lenalidomide plus dexamethasone or bortezomib plus dexamethasone in patients with relapsed or refractory disease.
BCMA-specific CAR T-cell therapy
Some of the most “exciting” data with anti-BCMA CAR T-cell therapy in myeloma, according to Dr. Kumar, involves bb2121. bb2121 showed durable clinical responses in heavily pretreated patients, according to an ASH 2017 presentation.
“The overall response rate is quite significant,” Dr. Kumar said. He related a 94% rate of overall response that was even higher in patients treated with doses of 150 x 106 CAR+ T cells or more. Many of the responses were lasting, he said, with 5 patients in ongoing response for more than a year.
“The results are exciting enough that this is actually moving forward with registration trials,” Dr. Kumar added.
Another novel CAR T-cell product, LCAR-B38M, has demonstrated promising results. LCAR-B38M principally targets BCMA and has led to a significant number of patients achieving stringent complete response that lasted beyond 1 year.
Multiple BCMA-targeting CAR T-cell products that use different vectors and different costimulatory molecules are currently in clinical trials, Dr. Kumar said.
BiTEs
In contrast to CAR T-cell products that must be customized to each patient in a process that takes weeks, BiTEs are a ready-made approach to allow T cells to engage with tumor cells.
“In patients with advanced disease, a lot can change in that short timeframe, so having an approach that is off-the-shelf, which is not patient specific, is quite attractive,” Dr. Kumar said.
BCMA-directed BiTE therapies to watch that are under investigation include AMG 420 and PF-06863135, he said.
New York—Three novel treatment strategies that target B-cell maturation antigen (BCMA) are showing promise in recent multiple myeloma (MM) clinical trials, according to Shaji K. Kumar, MD, of Mayo Clinic Cancer Center in Rochester, Minnesota.
The strategies include B-cell maturation antigen (BCMA) antibody-drug conjugate, BCMA-specific chimeric antigen receptor (CAR) T-cell therapies, and bispecific T-cell engagers (BiTEs).
“Clearly, there are a lot of exciting drugs that are currently in clinical trials, but these 3 platforms appear to be much more advanced than the others, and hopefully we will see that in the clinic in the near future,” Dr. Kumar told attendees at the NCCN 13th Annual Congress: Hematologic Malignancies.
BCMA is required for plasma cell survival and is broadly expressed on malignant plasma cells.
BCMA antibody-drug conjugate
The antibody-drug conjugate, GSK2857916, is a humanized IgG1 anti-BCMA antibody conjugated to a microtubule-disrupting agent. It produced an overall response rate of 67% at the 2 highest dose levels in 9 MM patients who had previously received multiple standard-of-care agents.
“Some of the responses were quite durable, lasting several months,” he said.
Now, GSK2857916 is being evaluated in a variety of different combinations, he said, including in an upcoming phase 2 study of the antibody-drug conjugate in combination with lenalidomide plus dexamethasone or bortezomib plus dexamethasone in patients with relapsed or refractory disease.
BCMA-specific CAR T-cell therapy
Some of the most “exciting” data with anti-BCMA CAR T-cell therapy in myeloma, according to Dr. Kumar, involves bb2121. bb2121 showed durable clinical responses in heavily pretreated patients, according to an ASH 2017 presentation.
“The overall response rate is quite significant,” Dr. Kumar said. He related a 94% rate of overall response that was even higher in patients treated with doses of 150 x 106 CAR+ T cells or more. Many of the responses were lasting, he said, with 5 patients in ongoing response for more than a year.
“The results are exciting enough that this is actually moving forward with registration trials,” Dr. Kumar added.
Another novel CAR T-cell product, LCAR-B38M, has demonstrated promising results. LCAR-B38M principally targets BCMA and has led to a significant number of patients achieving stringent complete response that lasted beyond 1 year.
Multiple BCMA-targeting CAR T-cell products that use different vectors and different costimulatory molecules are currently in clinical trials, Dr. Kumar said.
BiTEs
In contrast to CAR T-cell products that must be customized to each patient in a process that takes weeks, BiTEs are a ready-made approach to allow T cells to engage with tumor cells.
“In patients with advanced disease, a lot can change in that short timeframe, so having an approach that is off-the-shelf, which is not patient specific, is quite attractive,” Dr. Kumar said.
BCMA-directed BiTE therapies to watch that are under investigation include AMG 420 and PF-06863135, he said.
ASPREE: What to do now about aspirin for healthy elderly people
Across-the-board use of aspirin for primary prevention is “not justified” based on the results of ASPREE as well as the equivocal results from other recent primary prevention trials, according to Prakash C. Deedwania, MD, clinical professor of medicine and chief of the cardiology division at the Veterans Affairs Medical Center/University of California San Francisco Program in Fresno.
The importance of interpreting these studies lies in the recognition that while low-risk people don’t benefit, patients who are at mid to high cardiovascular (CV) risk clearly might. Aspirin’s role in secondary prevention after an initial CV event is clearly established, Dr. Deedwania added.
In ASPREE, a randomized, double-blind, placebo-controlled trial including nearly 20,000 participants, daily aspirin increased rates of major hemorrhage and did not significantly decrease risks of cardiovascular events, death, or other outcomes in healthy elderly individuals.
Aspirin did not prolong disability-free survival, a composite endpoint that included death, dementia, and permanent physical disability, according to one of three separate reports on ASPREE that were published in the New England Journal of Medicine.
Cardiovascular disease rates were likewise not significantly different between aspirin and placebo, with a hazard ratio that ruled out the possibility of a major protective effect, lead author John J. McNeil, MBBS, PhD, of Monash University, Melbourne, said in a second report on ASPREE.
All-cause mortality was actually higher in the aspirin arm versus the placebo arm, attributable largely to an excess of cancer-related deaths, Dr. McNeil and colleagues said in their third full report in the journal. However, that mortality finding needs to be interpreted with caution, they noted, given that previous investigations have shown a protective effect of aspirin on cancer-related death.
Potential harms of “innocuous” drug
The ASPREE (Aspirin in Reducing Events in the Elderly) study evaluated the use of aspirin as primary prevention in 19,114 healthy subjects, with a median age of 74 years, enrolled at 34 centers in Australia and the United States between 2010 and 2014.
The patients, who did not have cardiovascular disease, dementia, or disability at baseline, were randomized to daily 100-mg enteric-coated aspirin or placebo.
The rate of death, dementia, or disability was 21.5 events per 1,000 person-years in the aspirin group, and 21.2 events per 1,000 person-years in the placebo group, with a hazard ratio of 1.01 (95% confidence interval, 0.92-1.11; P = .79), Dr. McNeil and colleagues reported.
The rate of major hemorrhage was 8.6 events per 1,000 person-years for aspirin versus 6.2 events per 1,000 person years for placebo (HR, 1.38; 95% CI, 1.18-1.62; P less than .001), investigators found.
Cardiovascular outcomes: expectations vs. reality
Investigators said they thought they might see a significant cardiovascular benefit of aspirin in ASPREE based on earlier studies and meta-analyses that suggested a benefit in other populations. However, the rate of cardiovascular disease at 4.7 years of follow-up was 10.7 events per 1,000 person-years for aspirin, and 11.3 per 1,000 person years for placebo (HR, 0.95; 95% CI, 0.83-1.08).
That hazard ratio “rules out the possibility of a major protective effect of aspirin but is compatible with a more modest lowering of risk of up to 17%,” Dr. McNeil and colleagues wrote.
The results are consistent with those of a recent meta-analysis including eight primary prevention trials, mainly in adults under 70 years of age. That analysis found a 17% reduction in nonfatal myocardial infarction risk, a 14% reduction in stroke risk, and a higher risk of serious bleeding for aspirin versus control groups.
Results of ASPREE have to be interpreted in light of event rates, which were much lower than the expected 22.4 events per 1,000 person-years, they added. The low event rate probably reflects both the relatively good health of the study subjects, and the declining rates of cardiovascular disease in recent years, they said.
“Because of these factors, the absolute benefit that results from any proportionally lower rate of cardiovascular disease may be less than the benefit observed in studies from previous decades and is less likely than it had been to outweigh the risk of adverse events from aspirin,” investigators said in their report.
Current guidelines state that the evidence is limited for use of aspirin as primary prevention of cardiovascular disease in the elderly. “Nevertheless, many millions of relatively healthy older persons in the United States and Australia take low-dose aspirin with the assumption that it will reduce the likelihood of future cardiovascular disease and stroke,” study authors said in a discussion of the results.
Excess deaths explored
There were also no significant differences between arms for the endpoints of death, dementia, or disability evaluated separately. However, the rate of death by any cause was numerically higher in the aspirin group versus the placebo group, at 12.7 and 11.1 events per 1,000 person-years, respectively (HR, 1.14; 95% CI, 1.01-1.29).
Cancer was the major contributor to the imbalance in deaths, ASPREE results show, at 1.6 excess deaths per 1,000 person-years. A total of 3.1% of patients in the aspirin group had cancer-related deaths, compared with 2.3% in the placebo arm of the trial (HR, 1.31; 95% CI, 1.10-1.56).
Mortality related to major hemorrhage contributed “only minimally” to the excess in deaths, investigators added in their report.
The finding of excess deaths in the aspirin arm of ASPREE contrasts with meta-analyses of previous prevention trials. According to investigators, those studies show a protective effect of aspirin on cancer-related death that is apparent after 4-5 years of continuous treatment.
Various cellular and molecular pathways relevant to cancer development, progression, and spread are influenced by aspirin, previous studies show.
“Questions may therefore arise about whether the biology of cancer differs among age groups with regard to the frequency of common molecular patterns, metastatic behavior, and treatment responses,” Dr. McNeil and coauthors wrote in their report.
Dr. McNeil reported nonfinancial support from Bayer received during the conduct of the study.
SOURCE: McNeil JJ et al. N Engl J Med. 2018 Sep 16.
Across-the-board use of aspirin for primary prevention is “not justified” based on the results of ASPREE as well as the equivocal results from other recent primary prevention trials, according to Prakash C. Deedwania, MD, clinical professor of medicine and chief of the cardiology division at the Veterans Affairs Medical Center/University of California San Francisco Program in Fresno.
The importance of interpreting these studies lies in the recognition that while low-risk people don’t benefit, patients who are at mid to high cardiovascular (CV) risk clearly might. Aspirin’s role in secondary prevention after an initial CV event is clearly established, Dr. Deedwania added.
In ASPREE, a randomized, double-blind, placebo-controlled trial including nearly 20,000 participants, daily aspirin increased rates of major hemorrhage and did not significantly decrease risks of cardiovascular events, death, or other outcomes in healthy elderly individuals.
Aspirin did not prolong disability-free survival, a composite endpoint that included death, dementia, and permanent physical disability, according to one of three separate reports on ASPREE that were published in the New England Journal of Medicine.
Cardiovascular disease rates were likewise not significantly different between aspirin and placebo, with a hazard ratio that ruled out the possibility of a major protective effect, lead author John J. McNeil, MBBS, PhD, of Monash University, Melbourne, said in a second report on ASPREE.
All-cause mortality was actually higher in the aspirin arm versus the placebo arm, attributable largely to an excess of cancer-related deaths, Dr. McNeil and colleagues said in their third full report in the journal. However, that mortality finding needs to be interpreted with caution, they noted, given that previous investigations have shown a protective effect of aspirin on cancer-related death.
Potential harms of “innocuous” drug
The ASPREE (Aspirin in Reducing Events in the Elderly) study evaluated the use of aspirin as primary prevention in 19,114 healthy subjects, with a median age of 74 years, enrolled at 34 centers in Australia and the United States between 2010 and 2014.
The patients, who did not have cardiovascular disease, dementia, or disability at baseline, were randomized to daily 100-mg enteric-coated aspirin or placebo.
The rate of death, dementia, or disability was 21.5 events per 1,000 person-years in the aspirin group, and 21.2 events per 1,000 person-years in the placebo group, with a hazard ratio of 1.01 (95% confidence interval, 0.92-1.11; P = .79), Dr. McNeil and colleagues reported.
The rate of major hemorrhage was 8.6 events per 1,000 person-years for aspirin versus 6.2 events per 1,000 person years for placebo (HR, 1.38; 95% CI, 1.18-1.62; P less than .001), investigators found.
Cardiovascular outcomes: expectations vs. reality
Investigators said they thought they might see a significant cardiovascular benefit of aspirin in ASPREE based on earlier studies and meta-analyses that suggested a benefit in other populations. However, the rate of cardiovascular disease at 4.7 years of follow-up was 10.7 events per 1,000 person-years for aspirin, and 11.3 per 1,000 person years for placebo (HR, 0.95; 95% CI, 0.83-1.08).
That hazard ratio “rules out the possibility of a major protective effect of aspirin but is compatible with a more modest lowering of risk of up to 17%,” Dr. McNeil and colleagues wrote.
The results are consistent with those of a recent meta-analysis including eight primary prevention trials, mainly in adults under 70 years of age. That analysis found a 17% reduction in nonfatal myocardial infarction risk, a 14% reduction in stroke risk, and a higher risk of serious bleeding for aspirin versus control groups.
Results of ASPREE have to be interpreted in light of event rates, which were much lower than the expected 22.4 events per 1,000 person-years, they added. The low event rate probably reflects both the relatively good health of the study subjects, and the declining rates of cardiovascular disease in recent years, they said.
“Because of these factors, the absolute benefit that results from any proportionally lower rate of cardiovascular disease may be less than the benefit observed in studies from previous decades and is less likely than it had been to outweigh the risk of adverse events from aspirin,” investigators said in their report.
Current guidelines state that the evidence is limited for use of aspirin as primary prevention of cardiovascular disease in the elderly. “Nevertheless, many millions of relatively healthy older persons in the United States and Australia take low-dose aspirin with the assumption that it will reduce the likelihood of future cardiovascular disease and stroke,” study authors said in a discussion of the results.
Excess deaths explored
There were also no significant differences between arms for the endpoints of death, dementia, or disability evaluated separately. However, the rate of death by any cause was numerically higher in the aspirin group versus the placebo group, at 12.7 and 11.1 events per 1,000 person-years, respectively (HR, 1.14; 95% CI, 1.01-1.29).
Cancer was the major contributor to the imbalance in deaths, ASPREE results show, at 1.6 excess deaths per 1,000 person-years. A total of 3.1% of patients in the aspirin group had cancer-related deaths, compared with 2.3% in the placebo arm of the trial (HR, 1.31; 95% CI, 1.10-1.56).
Mortality related to major hemorrhage contributed “only minimally” to the excess in deaths, investigators added in their report.
The finding of excess deaths in the aspirin arm of ASPREE contrasts with meta-analyses of previous prevention trials. According to investigators, those studies show a protective effect of aspirin on cancer-related death that is apparent after 4-5 years of continuous treatment.
Various cellular and molecular pathways relevant to cancer development, progression, and spread are influenced by aspirin, previous studies show.
“Questions may therefore arise about whether the biology of cancer differs among age groups with regard to the frequency of common molecular patterns, metastatic behavior, and treatment responses,” Dr. McNeil and coauthors wrote in their report.
Dr. McNeil reported nonfinancial support from Bayer received during the conduct of the study.
SOURCE: McNeil JJ et al. N Engl J Med. 2018 Sep 16.
Across-the-board use of aspirin for primary prevention is “not justified” based on the results of ASPREE as well as the equivocal results from other recent primary prevention trials, according to Prakash C. Deedwania, MD, clinical professor of medicine and chief of the cardiology division at the Veterans Affairs Medical Center/University of California San Francisco Program in Fresno.
The importance of interpreting these studies lies in the recognition that while low-risk people don’t benefit, patients who are at mid to high cardiovascular (CV) risk clearly might. Aspirin’s role in secondary prevention after an initial CV event is clearly established, Dr. Deedwania added.
In ASPREE, a randomized, double-blind, placebo-controlled trial including nearly 20,000 participants, daily aspirin increased rates of major hemorrhage and did not significantly decrease risks of cardiovascular events, death, or other outcomes in healthy elderly individuals.
Aspirin did not prolong disability-free survival, a composite endpoint that included death, dementia, and permanent physical disability, according to one of three separate reports on ASPREE that were published in the New England Journal of Medicine.
Cardiovascular disease rates were likewise not significantly different between aspirin and placebo, with a hazard ratio that ruled out the possibility of a major protective effect, lead author John J. McNeil, MBBS, PhD, of Monash University, Melbourne, said in a second report on ASPREE.
All-cause mortality was actually higher in the aspirin arm versus the placebo arm, attributable largely to an excess of cancer-related deaths, Dr. McNeil and colleagues said in their third full report in the journal. However, that mortality finding needs to be interpreted with caution, they noted, given that previous investigations have shown a protective effect of aspirin on cancer-related death.
Potential harms of “innocuous” drug
The ASPREE (Aspirin in Reducing Events in the Elderly) study evaluated the use of aspirin as primary prevention in 19,114 healthy subjects, with a median age of 74 years, enrolled at 34 centers in Australia and the United States between 2010 and 2014.
The patients, who did not have cardiovascular disease, dementia, or disability at baseline, were randomized to daily 100-mg enteric-coated aspirin or placebo.
The rate of death, dementia, or disability was 21.5 events per 1,000 person-years in the aspirin group, and 21.2 events per 1,000 person-years in the placebo group, with a hazard ratio of 1.01 (95% confidence interval, 0.92-1.11; P = .79), Dr. McNeil and colleagues reported.
The rate of major hemorrhage was 8.6 events per 1,000 person-years for aspirin versus 6.2 events per 1,000 person years for placebo (HR, 1.38; 95% CI, 1.18-1.62; P less than .001), investigators found.
Cardiovascular outcomes: expectations vs. reality
Investigators said they thought they might see a significant cardiovascular benefit of aspirin in ASPREE based on earlier studies and meta-analyses that suggested a benefit in other populations. However, the rate of cardiovascular disease at 4.7 years of follow-up was 10.7 events per 1,000 person-years for aspirin, and 11.3 per 1,000 person years for placebo (HR, 0.95; 95% CI, 0.83-1.08).
That hazard ratio “rules out the possibility of a major protective effect of aspirin but is compatible with a more modest lowering of risk of up to 17%,” Dr. McNeil and colleagues wrote.
The results are consistent with those of a recent meta-analysis including eight primary prevention trials, mainly in adults under 70 years of age. That analysis found a 17% reduction in nonfatal myocardial infarction risk, a 14% reduction in stroke risk, and a higher risk of serious bleeding for aspirin versus control groups.
Results of ASPREE have to be interpreted in light of event rates, which were much lower than the expected 22.4 events per 1,000 person-years, they added. The low event rate probably reflects both the relatively good health of the study subjects, and the declining rates of cardiovascular disease in recent years, they said.
“Because of these factors, the absolute benefit that results from any proportionally lower rate of cardiovascular disease may be less than the benefit observed in studies from previous decades and is less likely than it had been to outweigh the risk of adverse events from aspirin,” investigators said in their report.
Current guidelines state that the evidence is limited for use of aspirin as primary prevention of cardiovascular disease in the elderly. “Nevertheless, many millions of relatively healthy older persons in the United States and Australia take low-dose aspirin with the assumption that it will reduce the likelihood of future cardiovascular disease and stroke,” study authors said in a discussion of the results.
Excess deaths explored
There were also no significant differences between arms for the endpoints of death, dementia, or disability evaluated separately. However, the rate of death by any cause was numerically higher in the aspirin group versus the placebo group, at 12.7 and 11.1 events per 1,000 person-years, respectively (HR, 1.14; 95% CI, 1.01-1.29).
Cancer was the major contributor to the imbalance in deaths, ASPREE results show, at 1.6 excess deaths per 1,000 person-years. A total of 3.1% of patients in the aspirin group had cancer-related deaths, compared with 2.3% in the placebo arm of the trial (HR, 1.31; 95% CI, 1.10-1.56).
Mortality related to major hemorrhage contributed “only minimally” to the excess in deaths, investigators added in their report.
The finding of excess deaths in the aspirin arm of ASPREE contrasts with meta-analyses of previous prevention trials. According to investigators, those studies show a protective effect of aspirin on cancer-related death that is apparent after 4-5 years of continuous treatment.
Various cellular and molecular pathways relevant to cancer development, progression, and spread are influenced by aspirin, previous studies show.
“Questions may therefore arise about whether the biology of cancer differs among age groups with regard to the frequency of common molecular patterns, metastatic behavior, and treatment responses,” Dr. McNeil and coauthors wrote in their report.
Dr. McNeil reported nonfinancial support from Bayer received during the conduct of the study.
SOURCE: McNeil JJ et al. N Engl J Med. 2018 Sep 16.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
New guidelines frame treatment options for Castleman disease
The (MCD), although adjuvant chemotherapy can be critical in severe cases, according to the first-ever consensus treatment guidelines based on symptom severity.
Early intervention with combination chemotherapy may prevent a fatal outcome in patients with severe idiopathic MCD, according to the guidelines, which are based on input from 42 experts from 10 countries.
The guidelines should help clinicians select therapy, evaluate response, and thereby improve outcomes for this difficult-to-treat disease, according to guideline co-author David C. Fajgenbaum, MD, who is himself an idiopathic MCD patient. Frits van Rhee, MD, PhD, is the first author of the guidelines.*
“Right now we recommend siltuximab first line for everyone,” Dr. Fajgenbaum said in an interview, “but if we continue to dig deeper, it may be that there are clinical cases within idiopathic MCD that we think are even better candidates than others, and there may be alternative therapies for other patients.”
Experts reviewed published literature and a series of 344 clinical cases to develop the guidelines, which are published in the journal Blood.
Treating idiopathic MCD is challenging because of the rarity and heterogeneity of the disease, among other factors, said Dr. Fajgenbaum, of the division of translational medicine and human genetics at the University of Pennsylvania, Philadelphia.
Some 6,000-7,000 cases of Castleman disease are diagnosed yearly, and of those, only about 1,000 cases are idiopathic MCD, according to Dr. Fajgenbaum.
“Even within idiopathic MCD, there is some heterogeneity,” he said. “Some patients present in the intensive care unit with life-threatening multiple organ failure and will die within weeks of presentation, whereas others will have a slower presentation and certainly not nearly as aggressive presentation.”
Although the exact etiology of idiopathic MCD is unknown, human interleukin (IL)-6 is the most common pathological driver, experts said in the guidelines.
Siltuximab and tocilizumab are two IL-6–directed therapies used to treat multicentric Castleman disease, with siltuximab targeting IL-6 itself and tocilizumab targeting the IL-6 receptor. Siltuximab is recommended as the first choice because of rigorous data supporting its use, including randomized clinical trial data, while tocilizumab is recommended if siltuximab is not available.
However, clinicians need to carefully monitor laboratory results and clinical features for patients on these drugs because about 50% of idiopathic MCD patients don’t have a satisfactory response to first-line anti–IL-6 treatments, Dr. Fajgenbaum said.
“Once you get to second-line therapies, that’s really where the level of evidence is lower,” he said.
Second-line therapy should include rituximab, and immunomodulatory/immunosuppressive agents or steroids may be added, according to the guidelines.
Third line therapy is “less well defined,” according to the guidelines, and experts generally recommended immunomodulatory/immunosuppressive agents such as cyclosporine A, sirolimus, thalidomide, and lenalidomide.
Cytotoxic chemotherapy has a high response rate but also a high rate of relapse and significant toxicities, according to the data analysis conducted as part of the guideline development process. Based on that, the experts said to avoid it unless the patient progresses to severe idiopathic MCD.
“Patients who are literally dying in the intensive care unit, given the right combination chemotherapy, can improve within days to weeks and can even leave the hospital,” Dr. Fajgenbaum said. “It’s not necessarily going to be the answer long term, but it can be life saving in the short term. So we recommended a really quite aggressive approach for these patients.”
To bolster the evidence base, investigators in the Castleman Disease Collaborative Network (CDCN) set up an international registry to collect treatment and outcome data for 500 patients. After the first year and a half, 150 patients were enrolled, and the investigators have identified more than 30 drugs that have been used off label to treat idiopathic MCD, according to Dr. Fajgenbaum.
“Some of the drugs are demonstrating efficacy in small numbers,” he said. “With the goal of 500 patients total, we can certainly hope to see some trends.”
Dr. Fajgenbaum was diagnosed with idiopathic MCD as a medical student.
“That certainly served as a very strong personal motivator for me to get involved in the disease,” he said. “But as I’ve gotten more and more involved, I’ve obviously met a lot of other patients, and that really is a huge motivator for all members of the CDCN. We want more options for more patients more quickly so we can help as many people as possible.”
Dr. Fajgenbaum reported research funding from Janssen. Coauthors reported disclosures related to Janssen, Bristol-Myers Squibb, Genentech, Merck, Celgene, Incyte, Pfizer, Sequenom, and Foundation Medicine, among others.
SOURCE: van Rhee F et al. Blood. 2018 Sep 4. doi: 10.1182/blood-2018-07-862334.
This story was updated 10/01/2018.
The (MCD), although adjuvant chemotherapy can be critical in severe cases, according to the first-ever consensus treatment guidelines based on symptom severity.
Early intervention with combination chemotherapy may prevent a fatal outcome in patients with severe idiopathic MCD, according to the guidelines, which are based on input from 42 experts from 10 countries.
The guidelines should help clinicians select therapy, evaluate response, and thereby improve outcomes for this difficult-to-treat disease, according to guideline co-author David C. Fajgenbaum, MD, who is himself an idiopathic MCD patient. Frits van Rhee, MD, PhD, is the first author of the guidelines.*
“Right now we recommend siltuximab first line for everyone,” Dr. Fajgenbaum said in an interview, “but if we continue to dig deeper, it may be that there are clinical cases within idiopathic MCD that we think are even better candidates than others, and there may be alternative therapies for other patients.”
Experts reviewed published literature and a series of 344 clinical cases to develop the guidelines, which are published in the journal Blood.
Treating idiopathic MCD is challenging because of the rarity and heterogeneity of the disease, among other factors, said Dr. Fajgenbaum, of the division of translational medicine and human genetics at the University of Pennsylvania, Philadelphia.
Some 6,000-7,000 cases of Castleman disease are diagnosed yearly, and of those, only about 1,000 cases are idiopathic MCD, according to Dr. Fajgenbaum.
“Even within idiopathic MCD, there is some heterogeneity,” he said. “Some patients present in the intensive care unit with life-threatening multiple organ failure and will die within weeks of presentation, whereas others will have a slower presentation and certainly not nearly as aggressive presentation.”
Although the exact etiology of idiopathic MCD is unknown, human interleukin (IL)-6 is the most common pathological driver, experts said in the guidelines.
Siltuximab and tocilizumab are two IL-6–directed therapies used to treat multicentric Castleman disease, with siltuximab targeting IL-6 itself and tocilizumab targeting the IL-6 receptor. Siltuximab is recommended as the first choice because of rigorous data supporting its use, including randomized clinical trial data, while tocilizumab is recommended if siltuximab is not available.
However, clinicians need to carefully monitor laboratory results and clinical features for patients on these drugs because about 50% of idiopathic MCD patients don’t have a satisfactory response to first-line anti–IL-6 treatments, Dr. Fajgenbaum said.
“Once you get to second-line therapies, that’s really where the level of evidence is lower,” he said.
Second-line therapy should include rituximab, and immunomodulatory/immunosuppressive agents or steroids may be added, according to the guidelines.
Third line therapy is “less well defined,” according to the guidelines, and experts generally recommended immunomodulatory/immunosuppressive agents such as cyclosporine A, sirolimus, thalidomide, and lenalidomide.
Cytotoxic chemotherapy has a high response rate but also a high rate of relapse and significant toxicities, according to the data analysis conducted as part of the guideline development process. Based on that, the experts said to avoid it unless the patient progresses to severe idiopathic MCD.
“Patients who are literally dying in the intensive care unit, given the right combination chemotherapy, can improve within days to weeks and can even leave the hospital,” Dr. Fajgenbaum said. “It’s not necessarily going to be the answer long term, but it can be life saving in the short term. So we recommended a really quite aggressive approach for these patients.”
To bolster the evidence base, investigators in the Castleman Disease Collaborative Network (CDCN) set up an international registry to collect treatment and outcome data for 500 patients. After the first year and a half, 150 patients were enrolled, and the investigators have identified more than 30 drugs that have been used off label to treat idiopathic MCD, according to Dr. Fajgenbaum.
“Some of the drugs are demonstrating efficacy in small numbers,” he said. “With the goal of 500 patients total, we can certainly hope to see some trends.”
Dr. Fajgenbaum was diagnosed with idiopathic MCD as a medical student.
“That certainly served as a very strong personal motivator for me to get involved in the disease,” he said. “But as I’ve gotten more and more involved, I’ve obviously met a lot of other patients, and that really is a huge motivator for all members of the CDCN. We want more options for more patients more quickly so we can help as many people as possible.”
Dr. Fajgenbaum reported research funding from Janssen. Coauthors reported disclosures related to Janssen, Bristol-Myers Squibb, Genentech, Merck, Celgene, Incyte, Pfizer, Sequenom, and Foundation Medicine, among others.
SOURCE: van Rhee F et al. Blood. 2018 Sep 4. doi: 10.1182/blood-2018-07-862334.
This story was updated 10/01/2018.
The (MCD), although adjuvant chemotherapy can be critical in severe cases, according to the first-ever consensus treatment guidelines based on symptom severity.
Early intervention with combination chemotherapy may prevent a fatal outcome in patients with severe idiopathic MCD, according to the guidelines, which are based on input from 42 experts from 10 countries.
The guidelines should help clinicians select therapy, evaluate response, and thereby improve outcomes for this difficult-to-treat disease, according to guideline co-author David C. Fajgenbaum, MD, who is himself an idiopathic MCD patient. Frits van Rhee, MD, PhD, is the first author of the guidelines.*
“Right now we recommend siltuximab first line for everyone,” Dr. Fajgenbaum said in an interview, “but if we continue to dig deeper, it may be that there are clinical cases within idiopathic MCD that we think are even better candidates than others, and there may be alternative therapies for other patients.”
Experts reviewed published literature and a series of 344 clinical cases to develop the guidelines, which are published in the journal Blood.
Treating idiopathic MCD is challenging because of the rarity and heterogeneity of the disease, among other factors, said Dr. Fajgenbaum, of the division of translational medicine and human genetics at the University of Pennsylvania, Philadelphia.
Some 6,000-7,000 cases of Castleman disease are diagnosed yearly, and of those, only about 1,000 cases are idiopathic MCD, according to Dr. Fajgenbaum.
“Even within idiopathic MCD, there is some heterogeneity,” he said. “Some patients present in the intensive care unit with life-threatening multiple organ failure and will die within weeks of presentation, whereas others will have a slower presentation and certainly not nearly as aggressive presentation.”
Although the exact etiology of idiopathic MCD is unknown, human interleukin (IL)-6 is the most common pathological driver, experts said in the guidelines.
Siltuximab and tocilizumab are two IL-6–directed therapies used to treat multicentric Castleman disease, with siltuximab targeting IL-6 itself and tocilizumab targeting the IL-6 receptor. Siltuximab is recommended as the first choice because of rigorous data supporting its use, including randomized clinical trial data, while tocilizumab is recommended if siltuximab is not available.
However, clinicians need to carefully monitor laboratory results and clinical features for patients on these drugs because about 50% of idiopathic MCD patients don’t have a satisfactory response to first-line anti–IL-6 treatments, Dr. Fajgenbaum said.
“Once you get to second-line therapies, that’s really where the level of evidence is lower,” he said.
Second-line therapy should include rituximab, and immunomodulatory/immunosuppressive agents or steroids may be added, according to the guidelines.
Third line therapy is “less well defined,” according to the guidelines, and experts generally recommended immunomodulatory/immunosuppressive agents such as cyclosporine A, sirolimus, thalidomide, and lenalidomide.
Cytotoxic chemotherapy has a high response rate but also a high rate of relapse and significant toxicities, according to the data analysis conducted as part of the guideline development process. Based on that, the experts said to avoid it unless the patient progresses to severe idiopathic MCD.
“Patients who are literally dying in the intensive care unit, given the right combination chemotherapy, can improve within days to weeks and can even leave the hospital,” Dr. Fajgenbaum said. “It’s not necessarily going to be the answer long term, but it can be life saving in the short term. So we recommended a really quite aggressive approach for these patients.”
To bolster the evidence base, investigators in the Castleman Disease Collaborative Network (CDCN) set up an international registry to collect treatment and outcome data for 500 patients. After the first year and a half, 150 patients were enrolled, and the investigators have identified more than 30 drugs that have been used off label to treat idiopathic MCD, according to Dr. Fajgenbaum.
“Some of the drugs are demonstrating efficacy in small numbers,” he said. “With the goal of 500 patients total, we can certainly hope to see some trends.”
Dr. Fajgenbaum was diagnosed with idiopathic MCD as a medical student.
“That certainly served as a very strong personal motivator for me to get involved in the disease,” he said. “But as I’ve gotten more and more involved, I’ve obviously met a lot of other patients, and that really is a huge motivator for all members of the CDCN. We want more options for more patients more quickly so we can help as many people as possible.”
Dr. Fajgenbaum reported research funding from Janssen. Coauthors reported disclosures related to Janssen, Bristol-Myers Squibb, Genentech, Merck, Celgene, Incyte, Pfizer, Sequenom, and Foundation Medicine, among others.
SOURCE: van Rhee F et al. Blood. 2018 Sep 4. doi: 10.1182/blood-2018-07-862334.
This story was updated 10/01/2018.
FROM BLOOD
Breast cancer patients getting unnecessary scans against recommendations
PHOENIX – Despite clear guidance on lack of benefit and potential harms, many patients with early-stage breast cancers at low metastasis risk have undergone imaging tests for staging, recent retrospective studies have shown.
Nearly one-third of early-stage breast cancer patients received the unnecessary and potentially harmful interventions in one of the two studies presented at a symposium on quality care sponsored by the American Society of Clinical Oncology (ASCO).
Low-risk patients in that study were more likely to undergo imaging if they were younger or had triple-negative disease, among other factors, said researcher Brett Barlow, of the University of Alabama at Birmingham.
Physicians should be further educated about the low-risk nature of early-stage breast cancer, even in subgroups that are perceived to be higher risk, Mr. Barlow said in an interview.
“I think we can reassure physicians that these patients will do well and that these guidelines are based on good data,” he said “There could potentially be an element of distrust in these guidelines in these higher-risk patients, and that may be what’s driving some of these extra tests.”
According to Mr. Barlow, imaging low-risk patients is inconsistent with guidance from Choosing Wisely, an initiative designed to promote discussions between clinicians and patients about medical tests or procedures that are unnecessary.
As part of that initiative, ASCO recommended that PET, CT, and radionuclide bone scans should not be performed for staging of early-stage breast cancer at low risk for metastasis.
There is a lack of evidence that demonstrates a benefit for those imaging modalities in patients with newly identified ductal carcinoma in situ (DCIS) or clinical stage I or II disease, the society said at the time.
Unnecessary imaging can result in unnecessary invasive procedures, overtreatment, radiation exposure, and misdiagnosis, the society said in the guidance, which was published in 2012.
Despite the guidance, 262 out of 872 patients with stage 0-II breast cancer (30%) seen during 2013-2015 underwent imaging, according to results of the single-center retrospective cohort study Mr. Barlow and his coauthors described in a poster presentation.
The median age of the patients who underwent unnecessary imaging was 55 years versus 60 years for patients who did not, according to the researchers.
Risk of inappropriate imaging was increased in younger patients, those with triple-negative disease versus those with any hormone receptor–positive disease, those with higher-stage breast cancer, and those without Medicare insurance, investigators found.
Although it’s unclear whether there were any formal, institution-level efforts to promote the ASCO recommendations during the 2013-2015 period, it was “definitely a topic of debate at the time,” Mr. Barlow said.
“Something we hope to evaluate further is whether we have improved,” he said. “It’s important to set a baseline and see how we did in this area. We look forward to reevaluating that in a few years to see.”
In a separate study, investigators reviewed records from Mount Sinai Health System in New York and found that unnecessary scans were performed in 19% of patients diagnosed with stage I-II breast cancer during 2014-2015.
No cases of metastatic disease were found in 733 patients included in the study, and 43% had false-positive findings, according to Ana I. Velazquez Manana, MD, MS, of Mount Sinai Beth Israel Foundation, New York, and her coinvestigators.
Imaging increased costs by $4,480 per patient, according to the investigators, who found in multivariate analysis that the unnecessary scans were associated with young age, presence of T2 tumor, positive lymph nodes, and triple-negative disease.
“Further educational efforts are needed to avoid unnecessary scans in patients with early-stage breast cancer,” the researchers wrote in an abstract describing the results.
Mr. Barlow reported no disclosures, while one coauthor reported disclosures related to Carevive Systems, Genentech/Roche, Medscape, Pack Health, and Pfizer. Dr. Velazquez Manana and her coauthors had no relationships to disclose, and their study was funded by the Medical Student Rotation for Underrepresented Populations.
SOURCE: Barlow B et al. Quality Care Symposium, Abstract 51. Velazquez Manana AI et al. Quality Care Symposium, Abstract 52.
PHOENIX – Despite clear guidance on lack of benefit and potential harms, many patients with early-stage breast cancers at low metastasis risk have undergone imaging tests for staging, recent retrospective studies have shown.
Nearly one-third of early-stage breast cancer patients received the unnecessary and potentially harmful interventions in one of the two studies presented at a symposium on quality care sponsored by the American Society of Clinical Oncology (ASCO).
Low-risk patients in that study were more likely to undergo imaging if they were younger or had triple-negative disease, among other factors, said researcher Brett Barlow, of the University of Alabama at Birmingham.
Physicians should be further educated about the low-risk nature of early-stage breast cancer, even in subgroups that are perceived to be higher risk, Mr. Barlow said in an interview.
“I think we can reassure physicians that these patients will do well and that these guidelines are based on good data,” he said “There could potentially be an element of distrust in these guidelines in these higher-risk patients, and that may be what’s driving some of these extra tests.”
According to Mr. Barlow, imaging low-risk patients is inconsistent with guidance from Choosing Wisely, an initiative designed to promote discussions between clinicians and patients about medical tests or procedures that are unnecessary.
As part of that initiative, ASCO recommended that PET, CT, and radionuclide bone scans should not be performed for staging of early-stage breast cancer at low risk for metastasis.
There is a lack of evidence that demonstrates a benefit for those imaging modalities in patients with newly identified ductal carcinoma in situ (DCIS) or clinical stage I or II disease, the society said at the time.
Unnecessary imaging can result in unnecessary invasive procedures, overtreatment, radiation exposure, and misdiagnosis, the society said in the guidance, which was published in 2012.
Despite the guidance, 262 out of 872 patients with stage 0-II breast cancer (30%) seen during 2013-2015 underwent imaging, according to results of the single-center retrospective cohort study Mr. Barlow and his coauthors described in a poster presentation.
The median age of the patients who underwent unnecessary imaging was 55 years versus 60 years for patients who did not, according to the researchers.
Risk of inappropriate imaging was increased in younger patients, those with triple-negative disease versus those with any hormone receptor–positive disease, those with higher-stage breast cancer, and those without Medicare insurance, investigators found.
Although it’s unclear whether there were any formal, institution-level efforts to promote the ASCO recommendations during the 2013-2015 period, it was “definitely a topic of debate at the time,” Mr. Barlow said.
“Something we hope to evaluate further is whether we have improved,” he said. “It’s important to set a baseline and see how we did in this area. We look forward to reevaluating that in a few years to see.”
In a separate study, investigators reviewed records from Mount Sinai Health System in New York and found that unnecessary scans were performed in 19% of patients diagnosed with stage I-II breast cancer during 2014-2015.
No cases of metastatic disease were found in 733 patients included in the study, and 43% had false-positive findings, according to Ana I. Velazquez Manana, MD, MS, of Mount Sinai Beth Israel Foundation, New York, and her coinvestigators.
Imaging increased costs by $4,480 per patient, according to the investigators, who found in multivariate analysis that the unnecessary scans were associated with young age, presence of T2 tumor, positive lymph nodes, and triple-negative disease.
“Further educational efforts are needed to avoid unnecessary scans in patients with early-stage breast cancer,” the researchers wrote in an abstract describing the results.
Mr. Barlow reported no disclosures, while one coauthor reported disclosures related to Carevive Systems, Genentech/Roche, Medscape, Pack Health, and Pfizer. Dr. Velazquez Manana and her coauthors had no relationships to disclose, and their study was funded by the Medical Student Rotation for Underrepresented Populations.
SOURCE: Barlow B et al. Quality Care Symposium, Abstract 51. Velazquez Manana AI et al. Quality Care Symposium, Abstract 52.
PHOENIX – Despite clear guidance on lack of benefit and potential harms, many patients with early-stage breast cancers at low metastasis risk have undergone imaging tests for staging, recent retrospective studies have shown.
Nearly one-third of early-stage breast cancer patients received the unnecessary and potentially harmful interventions in one of the two studies presented at a symposium on quality care sponsored by the American Society of Clinical Oncology (ASCO).
Low-risk patients in that study were more likely to undergo imaging if they were younger or had triple-negative disease, among other factors, said researcher Brett Barlow, of the University of Alabama at Birmingham.
Physicians should be further educated about the low-risk nature of early-stage breast cancer, even in subgroups that are perceived to be higher risk, Mr. Barlow said in an interview.
“I think we can reassure physicians that these patients will do well and that these guidelines are based on good data,” he said “There could potentially be an element of distrust in these guidelines in these higher-risk patients, and that may be what’s driving some of these extra tests.”
According to Mr. Barlow, imaging low-risk patients is inconsistent with guidance from Choosing Wisely, an initiative designed to promote discussions between clinicians and patients about medical tests or procedures that are unnecessary.
As part of that initiative, ASCO recommended that PET, CT, and radionuclide bone scans should not be performed for staging of early-stage breast cancer at low risk for metastasis.
There is a lack of evidence that demonstrates a benefit for those imaging modalities in patients with newly identified ductal carcinoma in situ (DCIS) or clinical stage I or II disease, the society said at the time.
Unnecessary imaging can result in unnecessary invasive procedures, overtreatment, radiation exposure, and misdiagnosis, the society said in the guidance, which was published in 2012.
Despite the guidance, 262 out of 872 patients with stage 0-II breast cancer (30%) seen during 2013-2015 underwent imaging, according to results of the single-center retrospective cohort study Mr. Barlow and his coauthors described in a poster presentation.
The median age of the patients who underwent unnecessary imaging was 55 years versus 60 years for patients who did not, according to the researchers.
Risk of inappropriate imaging was increased in younger patients, those with triple-negative disease versus those with any hormone receptor–positive disease, those with higher-stage breast cancer, and those without Medicare insurance, investigators found.
Although it’s unclear whether there were any formal, institution-level efforts to promote the ASCO recommendations during the 2013-2015 period, it was “definitely a topic of debate at the time,” Mr. Barlow said.
“Something we hope to evaluate further is whether we have improved,” he said. “It’s important to set a baseline and see how we did in this area. We look forward to reevaluating that in a few years to see.”
In a separate study, investigators reviewed records from Mount Sinai Health System in New York and found that unnecessary scans were performed in 19% of patients diagnosed with stage I-II breast cancer during 2014-2015.
No cases of metastatic disease were found in 733 patients included in the study, and 43% had false-positive findings, according to Ana I. Velazquez Manana, MD, MS, of Mount Sinai Beth Israel Foundation, New York, and her coinvestigators.
Imaging increased costs by $4,480 per patient, according to the investigators, who found in multivariate analysis that the unnecessary scans were associated with young age, presence of T2 tumor, positive lymph nodes, and triple-negative disease.
“Further educational efforts are needed to avoid unnecessary scans in patients with early-stage breast cancer,” the researchers wrote in an abstract describing the results.
Mr. Barlow reported no disclosures, while one coauthor reported disclosures related to Carevive Systems, Genentech/Roche, Medscape, Pack Health, and Pfizer. Dr. Velazquez Manana and her coauthors had no relationships to disclose, and their study was funded by the Medical Student Rotation for Underrepresented Populations.
SOURCE: Barlow B et al. Quality Care Symposium, Abstract 51. Velazquez Manana AI et al. Quality Care Symposium, Abstract 52.
REPORTING FROM THE QUALITY CARE SYMPOSIUM
Key clinical point: Many patients with early breast cancers at low metastasis risk received imaging tests for staging despite ASCO recommendations against such testing.
Major finding: In two studies, 30% and 19% of low-risk breast cancer patients underwent imaging for staging.
Study details: Two single-center, retrospective cohort studies that included 872 and 733 patients, respectively.
Disclosures: In one study, researchers reported disclosures related to Carevive Systems, Genentech/Roche, Medscape, Pack Health, and Pfizer. The second study was funded by the Medical Student Rotation for Underrepresented Populations.
Source: Barlow B et al. Quality Care Symposium, Abstract 51; Velazquez Manana AI et al. Quality Care Symposium, Abstract 52.
Infliximab biosimilar only moderately less expensive
The infliximab-dyyb biosimilar was only moderately less expensive than the originator infliximab product Remicade in the United States in 2017 under Medicare Part D, an analysis shows.
Infliximab-dyyb (Inflectra) cost 18% less than infliximab, with an annual cost exceeding $14,000 in an analysis published online in JAMA by Jinoos Yazdany, MD, of the division of rheumatology at the University of California, San Francisco, and her coauthors.
However, “without biosimilar gap discounts in 2017, beneficiaries would have paid more than $5,100 for infliximab-dyyb, or nearly $1,700 more in projected out-of-pocket costs than infliximab,” Dr. Yazdany and her coauthors wrote.
Biologics represent only 2% of U.S. prescriptions but made up 38% of drug spending in 2015 and accounted for 70% of growth in drug spending from 2010 to 2015, according to Dr. Yazdany and her colleagues.
Biologics for rheumatoid arthritis (RA) and gastroenterology cost more than $14,000 per year, and in 2015, 3 were among the top 15 drugs in terms of Medicare expenditures, they added.
While biosimilars are supposed to increase competition and lower prices, it’s an open question whether they actually reduce out-of-pocket expenditures for the 43 million individuals with drug benefits under Medicare Part D.
That uncertainty is due in part to the complex cost-sharing design of Part D, which includes an initial deductible, a coverage phase, a coverage gap, and catastrophic coverage.
In 2017, the plan included an initial $400 deductible, followed by the coverage phase, in which the patient paid 25% of drug costs. In the coverage gap, which started at $3,700 in total drug costs, the patient’s share of drug costs increased to 40% for biologics, and 51% for biosimilars. In the catastrophic coverage phase, triggered when out-of-pocket costs exceeded $4,950, the patient was responsible for 5% of drug costs.
“Currently, beneficiaries receive a 50% manufacturer discount during the gap for brand-name drugs and biologics, but not for biosimilars,” Dr. Yazdany and her coauthors noted.
To evaluate cost-sharing for infliximab-dyyb, the authors analyzed data for all Part D plans in the June 2017 Medicare Prescription Drug Plan Formulary, Pharmacy Network, and Pricing Information Files.
Out of 2,547 plans, only 10% covered the biosimilar, while 96% covered infliximab, the authors found.
The mean total cost of infliximab-dyyb was “modestly lower,” they reported. Eight-week prescription costs were $2,185 for infliximab-dyyb versus $2,667 for infliximab, while annual costs were $14,202 for the biosimilar and $17,335 for infliximab.
However, all plans required coinsurance cost-sharing for the biosimilar, they said. The mean coinsurance rate was 26.6% of the total drug cost for the biosimilar and 28.4% for infliximab.
For beneficiaries, projected annual out-of-pocket costs without the gap discount were $5,118 for infliximab-dyyb and $3,432 for infliximab, the researchers said.
Biosimilar gap discounts are set to start in 2019, according to the authors. However, they said those discounts may not substantially reduce out-of-pocket costs for Part D beneficiaries because of the high price of infliximab-dyyb and a coinsurance cost-sharing rate similar to that of infliximab. Because the RA starting dose is typically 3 mg/kg, compared with the 5-mg/kg starting dose for patients with inflammatory bowel disease, cost issues may be worse for GI patients.
“Further policies are needed to address affordability and access to specialty drugs,” Dr. Yazdany and her coauthors concluded.
The study was funded in part by grants from the Agency for Healthcare Research and Quality, the Robert L. Kroc Endowed Chair in Rheumatic and Connective Tissue Diseases, and other sources. Dr. Yazdany reported receiving an independent investigator award from Pfizer. Her coauthors reported no conflicts of interest.
The infliximab-dyyb biosimilar was only moderately less expensive than the originator infliximab product Remicade in the United States in 2017 under Medicare Part D, an analysis shows.
Infliximab-dyyb (Inflectra) cost 18% less than infliximab, with an annual cost exceeding $14,000 in an analysis published online in JAMA by Jinoos Yazdany, MD, of the division of rheumatology at the University of California, San Francisco, and her coauthors.
However, “without biosimilar gap discounts in 2017, beneficiaries would have paid more than $5,100 for infliximab-dyyb, or nearly $1,700 more in projected out-of-pocket costs than infliximab,” Dr. Yazdany and her coauthors wrote.
Biologics represent only 2% of U.S. prescriptions but made up 38% of drug spending in 2015 and accounted for 70% of growth in drug spending from 2010 to 2015, according to Dr. Yazdany and her colleagues.
Biologics for rheumatoid arthritis (RA) and gastroenterology cost more than $14,000 per year, and in 2015, 3 were among the top 15 drugs in terms of Medicare expenditures, they added.
While biosimilars are supposed to increase competition and lower prices, it’s an open question whether they actually reduce out-of-pocket expenditures for the 43 million individuals with drug benefits under Medicare Part D.
That uncertainty is due in part to the complex cost-sharing design of Part D, which includes an initial deductible, a coverage phase, a coverage gap, and catastrophic coverage.
In 2017, the plan included an initial $400 deductible, followed by the coverage phase, in which the patient paid 25% of drug costs. In the coverage gap, which started at $3,700 in total drug costs, the patient’s share of drug costs increased to 40% for biologics, and 51% for biosimilars. In the catastrophic coverage phase, triggered when out-of-pocket costs exceeded $4,950, the patient was responsible for 5% of drug costs.
“Currently, beneficiaries receive a 50% manufacturer discount during the gap for brand-name drugs and biologics, but not for biosimilars,” Dr. Yazdany and her coauthors noted.
To evaluate cost-sharing for infliximab-dyyb, the authors analyzed data for all Part D plans in the June 2017 Medicare Prescription Drug Plan Formulary, Pharmacy Network, and Pricing Information Files.
Out of 2,547 plans, only 10% covered the biosimilar, while 96% covered infliximab, the authors found.
The mean total cost of infliximab-dyyb was “modestly lower,” they reported. Eight-week prescription costs were $2,185 for infliximab-dyyb versus $2,667 for infliximab, while annual costs were $14,202 for the biosimilar and $17,335 for infliximab.
However, all plans required coinsurance cost-sharing for the biosimilar, they said. The mean coinsurance rate was 26.6% of the total drug cost for the biosimilar and 28.4% for infliximab.
For beneficiaries, projected annual out-of-pocket costs without the gap discount were $5,118 for infliximab-dyyb and $3,432 for infliximab, the researchers said.
Biosimilar gap discounts are set to start in 2019, according to the authors. However, they said those discounts may not substantially reduce out-of-pocket costs for Part D beneficiaries because of the high price of infliximab-dyyb and a coinsurance cost-sharing rate similar to that of infliximab. Because the RA starting dose is typically 3 mg/kg, compared with the 5-mg/kg starting dose for patients with inflammatory bowel disease, cost issues may be worse for GI patients.
“Further policies are needed to address affordability and access to specialty drugs,” Dr. Yazdany and her coauthors concluded.
The study was funded in part by grants from the Agency for Healthcare Research and Quality, the Robert L. Kroc Endowed Chair in Rheumatic and Connective Tissue Diseases, and other sources. Dr. Yazdany reported receiving an independent investigator award from Pfizer. Her coauthors reported no conflicts of interest.
The infliximab-dyyb biosimilar was only moderately less expensive than the originator infliximab product Remicade in the United States in 2017 under Medicare Part D, an analysis shows.
Infliximab-dyyb (Inflectra) cost 18% less than infliximab, with an annual cost exceeding $14,000 in an analysis published online in JAMA by Jinoos Yazdany, MD, of the division of rheumatology at the University of California, San Francisco, and her coauthors.
However, “without biosimilar gap discounts in 2017, beneficiaries would have paid more than $5,100 for infliximab-dyyb, or nearly $1,700 more in projected out-of-pocket costs than infliximab,” Dr. Yazdany and her coauthors wrote.
Biologics represent only 2% of U.S. prescriptions but made up 38% of drug spending in 2015 and accounted for 70% of growth in drug spending from 2010 to 2015, according to Dr. Yazdany and her colleagues.
Biologics for rheumatoid arthritis (RA) and gastroenterology cost more than $14,000 per year, and in 2015, 3 were among the top 15 drugs in terms of Medicare expenditures, they added.
While biosimilars are supposed to increase competition and lower prices, it’s an open question whether they actually reduce out-of-pocket expenditures for the 43 million individuals with drug benefits under Medicare Part D.
That uncertainty is due in part to the complex cost-sharing design of Part D, which includes an initial deductible, a coverage phase, a coverage gap, and catastrophic coverage.
In 2017, the plan included an initial $400 deductible, followed by the coverage phase, in which the patient paid 25% of drug costs. In the coverage gap, which started at $3,700 in total drug costs, the patient’s share of drug costs increased to 40% for biologics, and 51% for biosimilars. In the catastrophic coverage phase, triggered when out-of-pocket costs exceeded $4,950, the patient was responsible for 5% of drug costs.
“Currently, beneficiaries receive a 50% manufacturer discount during the gap for brand-name drugs and biologics, but not for biosimilars,” Dr. Yazdany and her coauthors noted.
To evaluate cost-sharing for infliximab-dyyb, the authors analyzed data for all Part D plans in the June 2017 Medicare Prescription Drug Plan Formulary, Pharmacy Network, and Pricing Information Files.
Out of 2,547 plans, only 10% covered the biosimilar, while 96% covered infliximab, the authors found.
The mean total cost of infliximab-dyyb was “modestly lower,” they reported. Eight-week prescription costs were $2,185 for infliximab-dyyb versus $2,667 for infliximab, while annual costs were $14,202 for the biosimilar and $17,335 for infliximab.
However, all plans required coinsurance cost-sharing for the biosimilar, they said. The mean coinsurance rate was 26.6% of the total drug cost for the biosimilar and 28.4% for infliximab.
For beneficiaries, projected annual out-of-pocket costs without the gap discount were $5,118 for infliximab-dyyb and $3,432 for infliximab, the researchers said.
Biosimilar gap discounts are set to start in 2019, according to the authors. However, they said those discounts may not substantially reduce out-of-pocket costs for Part D beneficiaries because of the high price of infliximab-dyyb and a coinsurance cost-sharing rate similar to that of infliximab. Because the RA starting dose is typically 3 mg/kg, compared with the 5-mg/kg starting dose for patients with inflammatory bowel disease, cost issues may be worse for GI patients.
“Further policies are needed to address affordability and access to specialty drugs,” Dr. Yazdany and her coauthors concluded.
The study was funded in part by grants from the Agency for Healthcare Research and Quality, the Robert L. Kroc Endowed Chair in Rheumatic and Connective Tissue Diseases, and other sources. Dr. Yazdany reported receiving an independent investigator award from Pfizer. Her coauthors reported no conflicts of interest.
JAMA