User login
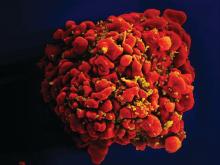
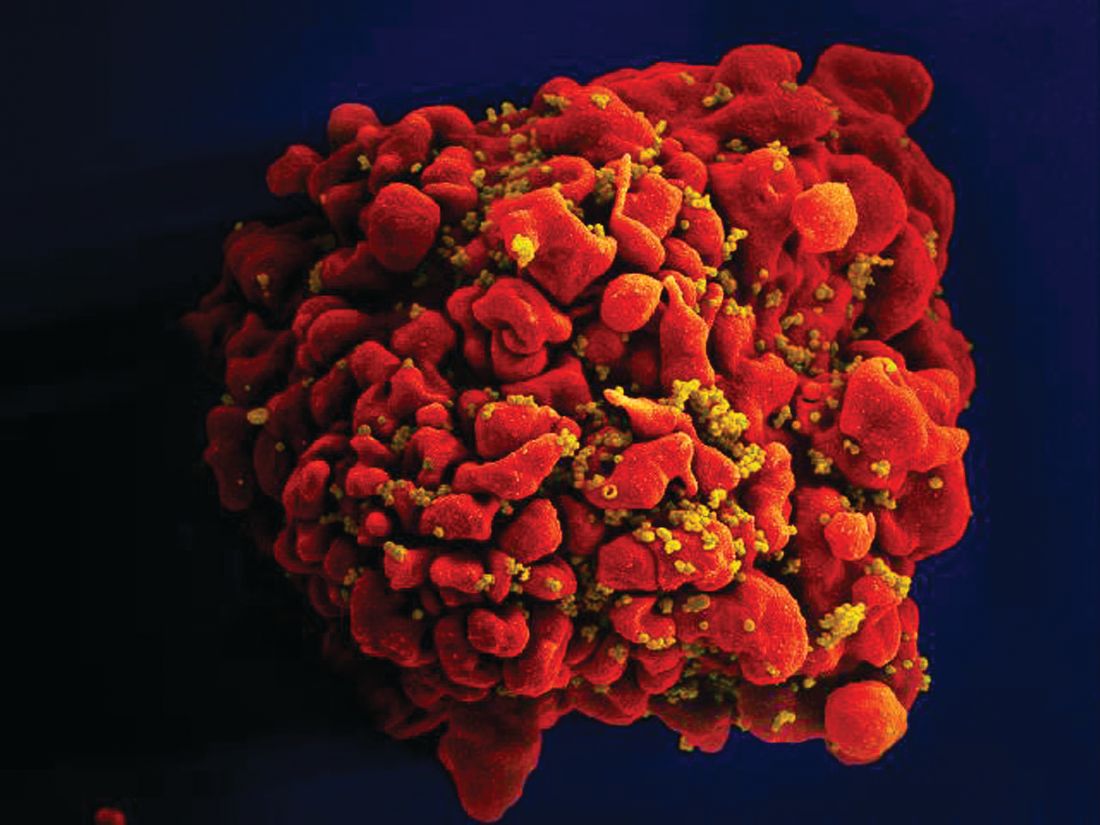
Zero HIV transmission rate when viral load suppressed
according to a new paper published in the Lancet.
The prospective observational PARTNER2 study (Lancet 2019 May 2. doi: 10.1016/S0140-6736[19]304018-0) followed 782 serodiscordant gay couples from 14 European countries, where the HIV-positive partner had to be virally suppressed to below 200 copies of HIV-1 RNA per milliliter, and the couple was engaging in condomless sex without using pre- or postexposure prophylaxis.
After a median follow-up of 2 years, there was not a single case of HIV transmission between couples, representing a transmission rate of zero. The study did record 15 new HIV infections during follow-up but these were all phylogenetically linked to sources other than the HIV-positive partner.
The HIV-positive partners had been on antiretroviral therapy for a median of 4.3 years – most on regimens of three or more drugs – with high levels of adherence. During the follow-up period, 37 HIV-positive partners (5%) reported missing their antiretroviral therapy for more than 4 consecutive days.
“Our results give equivalence of evidence for gay men as for heterosexual couples and indicate that the risk of HIV transmission when HIV viral load is suppressed is effectively zero for both anal and vaginal sex,” wrote Dr. Alison J. Rodger of the Institute for Global Health at University College London, and coauthors. “These findings emphasize the importance of regular monitoring to ensure HIV viral load remains suppressed and supporting HIV-positive people with long-term adherence.”
Around one-quarter of the HIV-negative men and 27% of the HIV-positive men reported a sexually-transmitted infection during follow-up; the most common infections were syphilis, gonorrhea, and chlamydia.
The study noted six additional cases of seroconversion of HIV-negative partners. However, these occurred outside the eligible couple-years of the follow-up period. They were ineligible due to no questionnaire about sexual behavior having been completed by either partner in the couple, a lack of condomless sex between the couple, use of postexposure prophylaxis, or a lack of viral load measurement for the HIV-positive partner in the past year.
The authors did note that the study population was predominantly white and with a median age of 38 years, while most HIV transmission occurs in young people aged under 25 years.
“The results from the PARTNER studies support wider dissemination of the message of the U=U [Undetectable equals Untransmittable] campaign that risk of transmission of HIV in the context of virally suppressive ART is zero,” they wrote.
The study was supported by the National Institute for Health Research, the British HIV Association, the Danish National Research Foundation, ViiV Healthcare, Gilead Sciences, Augustinus Fonden, and A P Møller Fonden. Fourteen authors declared grants, personal fees and other support from the pharmaceutical sector.
SOURCE: Rodger A et al. Lancet 2019, May 2. doi: 10.1016/S0140-6736[19]304018-0.
The results of the PARTNER and PARTNER2 trials show that timely diagnosis and effective treatment can virtually eliminate the risk of HIV transmission. However, access to HIV testing and care is not always easy, and fear, stigma, homophobia, and other forces continue to limit access to HIV treatment. This study also highlights the impact of sexual relations outside the bounds of a couple’s relationship.
While the use of preexposure prophylaxis was a criterion for exclusion from this study, this intervention should also be recognized as an important part of HIV prevention. A recent survey found that men who have sex with men are more likely to trust preexposure prophylaxis for HIV prevention than antiretroviral therapy.
Dr. Myron S Cohen is from the departments of medicine, microbiology, immunology, and epidemiology, University of North Carolina at Chapel Hill, and the UNC Institute for Global Health and Infectious Diseases in Chapel Hill. These comments are adapted from an editorial (Lancet 2019, May 2. doi: 10.1016/S0140-6736[19]30701-9). Dr. Cohen reported advisory board travel fees from Merck and Gilead unrelated to this work.
The results of the PARTNER and PARTNER2 trials show that timely diagnosis and effective treatment can virtually eliminate the risk of HIV transmission. However, access to HIV testing and care is not always easy, and fear, stigma, homophobia, and other forces continue to limit access to HIV treatment. This study also highlights the impact of sexual relations outside the bounds of a couple’s relationship.
While the use of preexposure prophylaxis was a criterion for exclusion from this study, this intervention should also be recognized as an important part of HIV prevention. A recent survey found that men who have sex with men are more likely to trust preexposure prophylaxis for HIV prevention than antiretroviral therapy.
Dr. Myron S Cohen is from the departments of medicine, microbiology, immunology, and epidemiology, University of North Carolina at Chapel Hill, and the UNC Institute for Global Health and Infectious Diseases in Chapel Hill. These comments are adapted from an editorial (Lancet 2019, May 2. doi: 10.1016/S0140-6736[19]30701-9). Dr. Cohen reported advisory board travel fees from Merck and Gilead unrelated to this work.
The results of the PARTNER and PARTNER2 trials show that timely diagnosis and effective treatment can virtually eliminate the risk of HIV transmission. However, access to HIV testing and care is not always easy, and fear, stigma, homophobia, and other forces continue to limit access to HIV treatment. This study also highlights the impact of sexual relations outside the bounds of a couple’s relationship.
While the use of preexposure prophylaxis was a criterion for exclusion from this study, this intervention should also be recognized as an important part of HIV prevention. A recent survey found that men who have sex with men are more likely to trust preexposure prophylaxis for HIV prevention than antiretroviral therapy.
Dr. Myron S Cohen is from the departments of medicine, microbiology, immunology, and epidemiology, University of North Carolina at Chapel Hill, and the UNC Institute for Global Health and Infectious Diseases in Chapel Hill. These comments are adapted from an editorial (Lancet 2019, May 2. doi: 10.1016/S0140-6736[19]30701-9). Dr. Cohen reported advisory board travel fees from Merck and Gilead unrelated to this work.
according to a new paper published in the Lancet.
The prospective observational PARTNER2 study (Lancet 2019 May 2. doi: 10.1016/S0140-6736[19]304018-0) followed 782 serodiscordant gay couples from 14 European countries, where the HIV-positive partner had to be virally suppressed to below 200 copies of HIV-1 RNA per milliliter, and the couple was engaging in condomless sex without using pre- or postexposure prophylaxis.
After a median follow-up of 2 years, there was not a single case of HIV transmission between couples, representing a transmission rate of zero. The study did record 15 new HIV infections during follow-up but these were all phylogenetically linked to sources other than the HIV-positive partner.
The HIV-positive partners had been on antiretroviral therapy for a median of 4.3 years – most on regimens of three or more drugs – with high levels of adherence. During the follow-up period, 37 HIV-positive partners (5%) reported missing their antiretroviral therapy for more than 4 consecutive days.
“Our results give equivalence of evidence for gay men as for heterosexual couples and indicate that the risk of HIV transmission when HIV viral load is suppressed is effectively zero for both anal and vaginal sex,” wrote Dr. Alison J. Rodger of the Institute for Global Health at University College London, and coauthors. “These findings emphasize the importance of regular monitoring to ensure HIV viral load remains suppressed and supporting HIV-positive people with long-term adherence.”
Around one-quarter of the HIV-negative men and 27% of the HIV-positive men reported a sexually-transmitted infection during follow-up; the most common infections were syphilis, gonorrhea, and chlamydia.
The study noted six additional cases of seroconversion of HIV-negative partners. However, these occurred outside the eligible couple-years of the follow-up period. They were ineligible due to no questionnaire about sexual behavior having been completed by either partner in the couple, a lack of condomless sex between the couple, use of postexposure prophylaxis, or a lack of viral load measurement for the HIV-positive partner in the past year.
The authors did note that the study population was predominantly white and with a median age of 38 years, while most HIV transmission occurs in young people aged under 25 years.
“The results from the PARTNER studies support wider dissemination of the message of the U=U [Undetectable equals Untransmittable] campaign that risk of transmission of HIV in the context of virally suppressive ART is zero,” they wrote.
The study was supported by the National Institute for Health Research, the British HIV Association, the Danish National Research Foundation, ViiV Healthcare, Gilead Sciences, Augustinus Fonden, and A P Møller Fonden. Fourteen authors declared grants, personal fees and other support from the pharmaceutical sector.
SOURCE: Rodger A et al. Lancet 2019, May 2. doi: 10.1016/S0140-6736[19]304018-0.
according to a new paper published in the Lancet.
The prospective observational PARTNER2 study (Lancet 2019 May 2. doi: 10.1016/S0140-6736[19]304018-0) followed 782 serodiscordant gay couples from 14 European countries, where the HIV-positive partner had to be virally suppressed to below 200 copies of HIV-1 RNA per milliliter, and the couple was engaging in condomless sex without using pre- or postexposure prophylaxis.
After a median follow-up of 2 years, there was not a single case of HIV transmission between couples, representing a transmission rate of zero. The study did record 15 new HIV infections during follow-up but these were all phylogenetically linked to sources other than the HIV-positive partner.
The HIV-positive partners had been on antiretroviral therapy for a median of 4.3 years – most on regimens of three or more drugs – with high levels of adherence. During the follow-up period, 37 HIV-positive partners (5%) reported missing their antiretroviral therapy for more than 4 consecutive days.
“Our results give equivalence of evidence for gay men as for heterosexual couples and indicate that the risk of HIV transmission when HIV viral load is suppressed is effectively zero for both anal and vaginal sex,” wrote Dr. Alison J. Rodger of the Institute for Global Health at University College London, and coauthors. “These findings emphasize the importance of regular monitoring to ensure HIV viral load remains suppressed and supporting HIV-positive people with long-term adherence.”
Around one-quarter of the HIV-negative men and 27% of the HIV-positive men reported a sexually-transmitted infection during follow-up; the most common infections were syphilis, gonorrhea, and chlamydia.
The study noted six additional cases of seroconversion of HIV-negative partners. However, these occurred outside the eligible couple-years of the follow-up period. They were ineligible due to no questionnaire about sexual behavior having been completed by either partner in the couple, a lack of condomless sex between the couple, use of postexposure prophylaxis, or a lack of viral load measurement for the HIV-positive partner in the past year.
The authors did note that the study population was predominantly white and with a median age of 38 years, while most HIV transmission occurs in young people aged under 25 years.
“The results from the PARTNER studies support wider dissemination of the message of the U=U [Undetectable equals Untransmittable] campaign that risk of transmission of HIV in the context of virally suppressive ART is zero,” they wrote.
The study was supported by the National Institute for Health Research, the British HIV Association, the Danish National Research Foundation, ViiV Healthcare, Gilead Sciences, Augustinus Fonden, and A P Møller Fonden. Fourteen authors declared grants, personal fees and other support from the pharmaceutical sector.
SOURCE: Rodger A et al. Lancet 2019, May 2. doi: 10.1016/S0140-6736[19]304018-0.
FROM THE LANCET
Racial, economic disparities found in buprenorphine prescriptions
Buprenorphine for opioid use disorder is much less likely to be prescribed to patients who are black or who do not have health insurance, an analysis of two national surveys shows.
Researchers analyzed data from the National Ambulatory Medical Care Survey and the National Hospital Ambulatory Medical Care Survey from 2004 to 2015, including 13.4 million visits in which buprenorphine was prescribed. The analysis was published as a research letter in JAMA Psychiatry.
From 2012 to 2015, the number of ambulatory visits involving buprenorphine rose from 0.04% to 0.36%. Black patients were 77% less likely to receive a prescription for buprenorphine at their visit – even after adjustment for payment method, sex, and age – while the number of prescription received by white patients was considerably higher than for patients of any other ethnicity, wrote Pooja A. Lagisetty, MD, and coauthors.
, and the age group with the highest incidence of buprenorphine prescriptions was 30-50 years.
Self-pay and private health insurance were the most common payment methods, but the number of self-paying patients receiving buprenorphine prescriptions dramatically increased from 585,568 in 2004-2007 to 5.3 million in 2012-2015.
“This finding in nationally representative data builds on a previous study that reported buprenorphine treatment disparities on the basis of race/ethnicity and income in New York City,” said Dr. Lagisetty of the department of medicine at the University of Michigan, Ann Arbor, and coauthors.
However, they acknowledged that it was unclear whether the treatment disparity might in fact reflect a difference in the prevalence of opioid use disorder across ethnicities.
Commenting on the differences in payment methods, the authors noted that, despite the enactment of mental health parity legislation and the expansion of Medicaid, the proportion of self-pay visits remained relatively unchanged across the study period.
“A recent study demonstrated that half of the physicians prescribing buprenorphine in Ohio accepted cash alone, and our findings suggest that this practice may be widespread and may be associated with additional financial barriers for low-income populations,” the researchers wrote. “With rising rates of opioid overdoses, it is imperative that policy and research efforts specifically address racial/ethnic and economic differences in treatment access and engagement.”
No conflicts of interest were declared.
SOURCE: Lagisetty P et al. JAMA Psychiatry. 2019 May 8. doi: 10.1001/jamapsychiatry.2019.0876.
Buprenorphine for opioid use disorder is much less likely to be prescribed to patients who are black or who do not have health insurance, an analysis of two national surveys shows.
Researchers analyzed data from the National Ambulatory Medical Care Survey and the National Hospital Ambulatory Medical Care Survey from 2004 to 2015, including 13.4 million visits in which buprenorphine was prescribed. The analysis was published as a research letter in JAMA Psychiatry.
From 2012 to 2015, the number of ambulatory visits involving buprenorphine rose from 0.04% to 0.36%. Black patients were 77% less likely to receive a prescription for buprenorphine at their visit – even after adjustment for payment method, sex, and age – while the number of prescription received by white patients was considerably higher than for patients of any other ethnicity, wrote Pooja A. Lagisetty, MD, and coauthors.
, and the age group with the highest incidence of buprenorphine prescriptions was 30-50 years.
Self-pay and private health insurance were the most common payment methods, but the number of self-paying patients receiving buprenorphine prescriptions dramatically increased from 585,568 in 2004-2007 to 5.3 million in 2012-2015.
“This finding in nationally representative data builds on a previous study that reported buprenorphine treatment disparities on the basis of race/ethnicity and income in New York City,” said Dr. Lagisetty of the department of medicine at the University of Michigan, Ann Arbor, and coauthors.
However, they acknowledged that it was unclear whether the treatment disparity might in fact reflect a difference in the prevalence of opioid use disorder across ethnicities.
Commenting on the differences in payment methods, the authors noted that, despite the enactment of mental health parity legislation and the expansion of Medicaid, the proportion of self-pay visits remained relatively unchanged across the study period.
“A recent study demonstrated that half of the physicians prescribing buprenorphine in Ohio accepted cash alone, and our findings suggest that this practice may be widespread and may be associated with additional financial barriers for low-income populations,” the researchers wrote. “With rising rates of opioid overdoses, it is imperative that policy and research efforts specifically address racial/ethnic and economic differences in treatment access and engagement.”
No conflicts of interest were declared.
SOURCE: Lagisetty P et al. JAMA Psychiatry. 2019 May 8. doi: 10.1001/jamapsychiatry.2019.0876.
Buprenorphine for opioid use disorder is much less likely to be prescribed to patients who are black or who do not have health insurance, an analysis of two national surveys shows.
Researchers analyzed data from the National Ambulatory Medical Care Survey and the National Hospital Ambulatory Medical Care Survey from 2004 to 2015, including 13.4 million visits in which buprenorphine was prescribed. The analysis was published as a research letter in JAMA Psychiatry.
From 2012 to 2015, the number of ambulatory visits involving buprenorphine rose from 0.04% to 0.36%. Black patients were 77% less likely to receive a prescription for buprenorphine at their visit – even after adjustment for payment method, sex, and age – while the number of prescription received by white patients was considerably higher than for patients of any other ethnicity, wrote Pooja A. Lagisetty, MD, and coauthors.
, and the age group with the highest incidence of buprenorphine prescriptions was 30-50 years.
Self-pay and private health insurance were the most common payment methods, but the number of self-paying patients receiving buprenorphine prescriptions dramatically increased from 585,568 in 2004-2007 to 5.3 million in 2012-2015.
“This finding in nationally representative data builds on a previous study that reported buprenorphine treatment disparities on the basis of race/ethnicity and income in New York City,” said Dr. Lagisetty of the department of medicine at the University of Michigan, Ann Arbor, and coauthors.
However, they acknowledged that it was unclear whether the treatment disparity might in fact reflect a difference in the prevalence of opioid use disorder across ethnicities.
Commenting on the differences in payment methods, the authors noted that, despite the enactment of mental health parity legislation and the expansion of Medicaid, the proportion of self-pay visits remained relatively unchanged across the study period.
“A recent study demonstrated that half of the physicians prescribing buprenorphine in Ohio accepted cash alone, and our findings suggest that this practice may be widespread and may be associated with additional financial barriers for low-income populations,” the researchers wrote. “With rising rates of opioid overdoses, it is imperative that policy and research efforts specifically address racial/ethnic and economic differences in treatment access and engagement.”
No conflicts of interest were declared.
SOURCE: Lagisetty P et al. JAMA Psychiatry. 2019 May 8. doi: 10.1001/jamapsychiatry.2019.0876.
FROM JAMA PSYCHIATRY
Liraglutide seems safe, effective in children already on metformin
The addition of liraglutide to metformin shows significantly improved glycemic control in children and adolescents with type 2 diabetes, compared with metformin alone, according to data presented at the Pediatric Academic Societies annual meeting in Baltimore.
The phase 3 study, which was simultaneously published in the New England Journal of Medicine, involved 134 patients aged 10-17 years with type 2 diabetes who were managing their diabetes with diet and exercise, metformin, or insulin.
Participants were randomized either to subcutaneous liraglutide – dose-escalated up to 1.8 mg/day, depending on efficacy and side effects – or placebo for 52 weeks. The first 26 weeks were double blind and the second 26 weeks were an open-label extension period.
At 26 weeks, mean glycated hemoglobin levels in the liraglutide group had decreased by 0.64 percentage points from baseline, but in the placebo group they had increased by 0.42 percentage points, representing a treatment difference of –1.06 percentage points (P less than .001). By week 52, the treatment difference between the two groups had increased to –1.30 percentage points.
William V. Tamborlane, MD, from the department of pediatrics at Yale University, New Haven, Conn., and his coauthors wrote that metformin is the approved drug of choice for pediatric patients with type 2 diabetes, and that insulin currently is the only approved option for those who do not have an adequate response to metformin monotherapy.
“This discrepancy in available treatments for youth as compared with adults persists because of a lack of successfully completed trials needed for approval of new drugs for the treatment of type 2 diabetes in children since a trial of metformin was completed in 1999,” they wrote.
The study showed that significantly more patients in the liraglutide group (63.7%) achieved glycated hemoglobin levels below 7%, compared with 36.5% of patients in the placebo group. Fasting plasma glucose levels were decreased in the liraglutide group at both 26 and 52 weeks, but had increased in the placebo group.
Although the number of reported adverse events were similar between the two groups, there were significantly more reports of gastrointestinal adverse events – particularly nausea – in patients taking liraglutide, compared with those on placebo.
However, the study did not show a difference between liraglutide and placebo in lowering body mass index, although mean body weight decreases – which were seen in both groups – were maintained at week 52 only in the liraglutide group. The authors suggested this might be owing to the relatively small number of patients enrolled in the study and that some of the children were still growing.
Novo Nordisk, which manufactures liraglutide, supported the study. Twelve authors reported grants or support from Novo Nordisk in relation to the trial. Three authors were employees of Novo Nordisk. Eight authors reported unrelated grants and fees from Novo Nordisk and other pharmaceutical companies.
SOURCE: Tamborlane WV et al. N Engl J Med. 2019 Apr 28. doi: 10.1056/NEJMoa1903822.
The addition of liraglutide to metformin shows significantly improved glycemic control in children and adolescents with type 2 diabetes, compared with metformin alone, according to data presented at the Pediatric Academic Societies annual meeting in Baltimore.
The phase 3 study, which was simultaneously published in the New England Journal of Medicine, involved 134 patients aged 10-17 years with type 2 diabetes who were managing their diabetes with diet and exercise, metformin, or insulin.
Participants were randomized either to subcutaneous liraglutide – dose-escalated up to 1.8 mg/day, depending on efficacy and side effects – or placebo for 52 weeks. The first 26 weeks were double blind and the second 26 weeks were an open-label extension period.
At 26 weeks, mean glycated hemoglobin levels in the liraglutide group had decreased by 0.64 percentage points from baseline, but in the placebo group they had increased by 0.42 percentage points, representing a treatment difference of –1.06 percentage points (P less than .001). By week 52, the treatment difference between the two groups had increased to –1.30 percentage points.
William V. Tamborlane, MD, from the department of pediatrics at Yale University, New Haven, Conn., and his coauthors wrote that metformin is the approved drug of choice for pediatric patients with type 2 diabetes, and that insulin currently is the only approved option for those who do not have an adequate response to metformin monotherapy.
“This discrepancy in available treatments for youth as compared with adults persists because of a lack of successfully completed trials needed for approval of new drugs for the treatment of type 2 diabetes in children since a trial of metformin was completed in 1999,” they wrote.
The study showed that significantly more patients in the liraglutide group (63.7%) achieved glycated hemoglobin levels below 7%, compared with 36.5% of patients in the placebo group. Fasting plasma glucose levels were decreased in the liraglutide group at both 26 and 52 weeks, but had increased in the placebo group.
Although the number of reported adverse events were similar between the two groups, there were significantly more reports of gastrointestinal adverse events – particularly nausea – in patients taking liraglutide, compared with those on placebo.
However, the study did not show a difference between liraglutide and placebo in lowering body mass index, although mean body weight decreases – which were seen in both groups – were maintained at week 52 only in the liraglutide group. The authors suggested this might be owing to the relatively small number of patients enrolled in the study and that some of the children were still growing.
Novo Nordisk, which manufactures liraglutide, supported the study. Twelve authors reported grants or support from Novo Nordisk in relation to the trial. Three authors were employees of Novo Nordisk. Eight authors reported unrelated grants and fees from Novo Nordisk and other pharmaceutical companies.
SOURCE: Tamborlane WV et al. N Engl J Med. 2019 Apr 28. doi: 10.1056/NEJMoa1903822.
The addition of liraglutide to metformin shows significantly improved glycemic control in children and adolescents with type 2 diabetes, compared with metformin alone, according to data presented at the Pediatric Academic Societies annual meeting in Baltimore.
The phase 3 study, which was simultaneously published in the New England Journal of Medicine, involved 134 patients aged 10-17 years with type 2 diabetes who were managing their diabetes with diet and exercise, metformin, or insulin.
Participants were randomized either to subcutaneous liraglutide – dose-escalated up to 1.8 mg/day, depending on efficacy and side effects – or placebo for 52 weeks. The first 26 weeks were double blind and the second 26 weeks were an open-label extension period.
At 26 weeks, mean glycated hemoglobin levels in the liraglutide group had decreased by 0.64 percentage points from baseline, but in the placebo group they had increased by 0.42 percentage points, representing a treatment difference of –1.06 percentage points (P less than .001). By week 52, the treatment difference between the two groups had increased to –1.30 percentage points.
William V. Tamborlane, MD, from the department of pediatrics at Yale University, New Haven, Conn., and his coauthors wrote that metformin is the approved drug of choice for pediatric patients with type 2 diabetes, and that insulin currently is the only approved option for those who do not have an adequate response to metformin monotherapy.
“This discrepancy in available treatments for youth as compared with adults persists because of a lack of successfully completed trials needed for approval of new drugs for the treatment of type 2 diabetes in children since a trial of metformin was completed in 1999,” they wrote.
The study showed that significantly more patients in the liraglutide group (63.7%) achieved glycated hemoglobin levels below 7%, compared with 36.5% of patients in the placebo group. Fasting plasma glucose levels were decreased in the liraglutide group at both 26 and 52 weeks, but had increased in the placebo group.
Although the number of reported adverse events were similar between the two groups, there were significantly more reports of gastrointestinal adverse events – particularly nausea – in patients taking liraglutide, compared with those on placebo.
However, the study did not show a difference between liraglutide and placebo in lowering body mass index, although mean body weight decreases – which were seen in both groups – were maintained at week 52 only in the liraglutide group. The authors suggested this might be owing to the relatively small number of patients enrolled in the study and that some of the children were still growing.
Novo Nordisk, which manufactures liraglutide, supported the study. Twelve authors reported grants or support from Novo Nordisk in relation to the trial. Three authors were employees of Novo Nordisk. Eight authors reported unrelated grants and fees from Novo Nordisk and other pharmaceutical companies.
SOURCE: Tamborlane WV et al. N Engl J Med. 2019 Apr 28. doi: 10.1056/NEJMoa1903822.
FROM PAS 2019
Version success more likely in lower BMI, multiparous breech pregnancies
according to results of a single-center retrospective study.
Writing in Obstetrics & Gynecology, Ofer Isakov, MD, PhD, and colleagues from the Sourasky Medical Center, Tel Aviv, reported the results of a study of 250 women with singleton pregnancies and breech presentation who underwent external cephalic version (ECV) to turn the baby at 36-41 weeks’ gestation.
The overall success rate of the procedure was 65%. However, women with no forebag – the pocket of amniotic fluid in front of the fetal presenting part – had a 3%-10% chance of successful version, while those with a forebag size greater than 1 cm had a 96%-97% probability of success.
Women with a BMI greater than 29 had a very low chance of success, which the authors suggested was likely attributable to a thicker abdominal wall that made manipulation more difficult. However, among women with a BMI of 29 or below, success was significantly associated with forebag size.
Among women with a forebag of 1 cm in size, multiparous women had a significantly higher chance of success than nulliparous women (81%-91% vs. 0%-24%, respectively).
Dr. Isakov and colleagues suggested that the impact of multiparity could relate to late engagement or the relative laxity of the abdomen in women who had experienced previous births.
The authors then developed a decision tree predictive model of success for ECV, which had a prediction accuracy of 92%.
“External version is a simple and effective procedure that can reduce the cesarean delivery rate, but counseling patients on the risks and success rates of version is challenging owing to the lack of validated models to predict success,” Dr. Isakov and colleagues wrote. “The ability to predict the outcome of an ECV attempt may improve the rates of patient consent and prevent the performance of many unpleasant procedures with low chance for success.”
They noted that their success rate was higher than that seen in other studies of ECV and suggested this may be because all the procedures were performed by a single experienced practitioner, and the mean BMI of the cohort was lower than that in earlier studies.
None of the authors declared any relevant financial disclosures, and there was no external funding.
SOURCE: Isakov O et al. Obstet Gynecol. 2019;133:869-78.
With cesarean delivery rates rising, there is a need for vigilance to prevent them from returning to the 2009 peak of 33% of deliveries, and ECV is one strategy to help reduce cesarean rates. While there are some risks associated with ECV, which could contribute to negative attitudes, the lack of acceptance of this procedure may be improved if clinicians can provide an individualized estimate for the chance of success. This study proposes creating a predictive model that discriminates between poor and good changes of ECV success.
The fact that this study is a single-center study with a single physician performing all the procedures does limit its generalizability. However the authors’ use of ultrasound measurements of the forebag is a novel contribution that provides an objective measure of this factor, as well as an objective estimate of the engagement of the breech, which has been lacking.
Dr. Gayle Olson Koutrouvelis is a professor of obstetrics, gynecology, and maternal-fetal medicine at the University of Texas Medical Branch in Galveston. These comments are adapted from an editorial accompanying the article by Isakov et al. (Obstet Gynecol. 2019; 133:855-6.). She declared no conflicts of interest.
With cesarean delivery rates rising, there is a need for vigilance to prevent them from returning to the 2009 peak of 33% of deliveries, and ECV is one strategy to help reduce cesarean rates. While there are some risks associated with ECV, which could contribute to negative attitudes, the lack of acceptance of this procedure may be improved if clinicians can provide an individualized estimate for the chance of success. This study proposes creating a predictive model that discriminates between poor and good changes of ECV success.
The fact that this study is a single-center study with a single physician performing all the procedures does limit its generalizability. However the authors’ use of ultrasound measurements of the forebag is a novel contribution that provides an objective measure of this factor, as well as an objective estimate of the engagement of the breech, which has been lacking.
Dr. Gayle Olson Koutrouvelis is a professor of obstetrics, gynecology, and maternal-fetal medicine at the University of Texas Medical Branch in Galveston. These comments are adapted from an editorial accompanying the article by Isakov et al. (Obstet Gynecol. 2019; 133:855-6.). She declared no conflicts of interest.
With cesarean delivery rates rising, there is a need for vigilance to prevent them from returning to the 2009 peak of 33% of deliveries, and ECV is one strategy to help reduce cesarean rates. While there are some risks associated with ECV, which could contribute to negative attitudes, the lack of acceptance of this procedure may be improved if clinicians can provide an individualized estimate for the chance of success. This study proposes creating a predictive model that discriminates between poor and good changes of ECV success.
The fact that this study is a single-center study with a single physician performing all the procedures does limit its generalizability. However the authors’ use of ultrasound measurements of the forebag is a novel contribution that provides an objective measure of this factor, as well as an objective estimate of the engagement of the breech, which has been lacking.
Dr. Gayle Olson Koutrouvelis is a professor of obstetrics, gynecology, and maternal-fetal medicine at the University of Texas Medical Branch in Galveston. These comments are adapted from an editorial accompanying the article by Isakov et al. (Obstet Gynecol. 2019; 133:855-6.). She declared no conflicts of interest.
according to results of a single-center retrospective study.
Writing in Obstetrics & Gynecology, Ofer Isakov, MD, PhD, and colleagues from the Sourasky Medical Center, Tel Aviv, reported the results of a study of 250 women with singleton pregnancies and breech presentation who underwent external cephalic version (ECV) to turn the baby at 36-41 weeks’ gestation.
The overall success rate of the procedure was 65%. However, women with no forebag – the pocket of amniotic fluid in front of the fetal presenting part – had a 3%-10% chance of successful version, while those with a forebag size greater than 1 cm had a 96%-97% probability of success.
Women with a BMI greater than 29 had a very low chance of success, which the authors suggested was likely attributable to a thicker abdominal wall that made manipulation more difficult. However, among women with a BMI of 29 or below, success was significantly associated with forebag size.
Among women with a forebag of 1 cm in size, multiparous women had a significantly higher chance of success than nulliparous women (81%-91% vs. 0%-24%, respectively).
Dr. Isakov and colleagues suggested that the impact of multiparity could relate to late engagement or the relative laxity of the abdomen in women who had experienced previous births.
The authors then developed a decision tree predictive model of success for ECV, which had a prediction accuracy of 92%.
“External version is a simple and effective procedure that can reduce the cesarean delivery rate, but counseling patients on the risks and success rates of version is challenging owing to the lack of validated models to predict success,” Dr. Isakov and colleagues wrote. “The ability to predict the outcome of an ECV attempt may improve the rates of patient consent and prevent the performance of many unpleasant procedures with low chance for success.”
They noted that their success rate was higher than that seen in other studies of ECV and suggested this may be because all the procedures were performed by a single experienced practitioner, and the mean BMI of the cohort was lower than that in earlier studies.
None of the authors declared any relevant financial disclosures, and there was no external funding.
SOURCE: Isakov O et al. Obstet Gynecol. 2019;133:869-78.
according to results of a single-center retrospective study.
Writing in Obstetrics & Gynecology, Ofer Isakov, MD, PhD, and colleagues from the Sourasky Medical Center, Tel Aviv, reported the results of a study of 250 women with singleton pregnancies and breech presentation who underwent external cephalic version (ECV) to turn the baby at 36-41 weeks’ gestation.
The overall success rate of the procedure was 65%. However, women with no forebag – the pocket of amniotic fluid in front of the fetal presenting part – had a 3%-10% chance of successful version, while those with a forebag size greater than 1 cm had a 96%-97% probability of success.
Women with a BMI greater than 29 had a very low chance of success, which the authors suggested was likely attributable to a thicker abdominal wall that made manipulation more difficult. However, among women with a BMI of 29 or below, success was significantly associated with forebag size.
Among women with a forebag of 1 cm in size, multiparous women had a significantly higher chance of success than nulliparous women (81%-91% vs. 0%-24%, respectively).
Dr. Isakov and colleagues suggested that the impact of multiparity could relate to late engagement or the relative laxity of the abdomen in women who had experienced previous births.
The authors then developed a decision tree predictive model of success for ECV, which had a prediction accuracy of 92%.
“External version is a simple and effective procedure that can reduce the cesarean delivery rate, but counseling patients on the risks and success rates of version is challenging owing to the lack of validated models to predict success,” Dr. Isakov and colleagues wrote. “The ability to predict the outcome of an ECV attempt may improve the rates of patient consent and prevent the performance of many unpleasant procedures with low chance for success.”
They noted that their success rate was higher than that seen in other studies of ECV and suggested this may be because all the procedures were performed by a single experienced practitioner, and the mean BMI of the cohort was lower than that in earlier studies.
None of the authors declared any relevant financial disclosures, and there was no external funding.
SOURCE: Isakov O et al. Obstet Gynecol. 2019;133:869-78.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point: Multiparity, larger forebag size, and lower BMI are predictors of external cephalic version success.
Major finding: Model of external cephalic version success shows prediction accuracy of 92%.
Study details: A single-center retrospective cohort study in 250 women with breech presentation.
Disclosures: None of the authors declared any relevant financial disclosures, and there was no external funding.
Source: Isakov O et al. Obstet Gynecol. 2019;133:869-78.
Few stroke patients undergo osteoporosis screening, treatment
Although stroke is a risk factor for osteoporosis, falls, and fractures, very few people who have experienced a recent stroke are either screened for osteoporosis or treated, research suggests.
Writing in Stroke, researchers presented an analysis of Ontario registry data from 16,581 patients who were aged 65 years or older and presented with stroke between 2003 and 2013.
Overall, just 5.1% of patients underwent bone mineral density testing. Of the 1,577 patients who had experienced a prior fracture, 71 (4.7%) had bone mineral density testing, and only 2.9% of those who had not had prior bone mineral density testing were tested after their stroke. Bone mineral density testing was more likely in patients who were younger, who were female, and who experienced a low-trauma fracture in the year after their stroke.
In total, 15.5% of patients were prescribed osteoporosis drugs in the first year after their stroke. However, only 7.8% of those who had fractures before the stroke and 14.8% of those with fractures after the stroke received osteoporosis treatment after the stroke. Patients who were female, had prior osteoporosis, had experienced prior fracture, had previously undergone bone mineral density testing, or had experienced a fracture or fall after their stroke were more likely to receive osteoporosis pharmacotherapy.
The authors found that the neither the severity of stroke nor the presence of other comorbidities was associated with an increased likelihood of screening or treatment of osteoporosis after the stroke.
Stroke is associated with up to a fourfold increased risk of osteoporosis and fracture, compared with healthy controls, most probably because of reduced mobility and an increased risk of falls, wrote Eshita Kapoor of the department of medicine at the University of Toronto and her coauthors.
“Screening and treatment may be particularly low poststroke because of under-recognition of osteoporosis as a consequence of stroke, a selective focus on the management of cardiovascular risk and stroke recovery, or factors such as dysphagia precluding use of oral bisphosphonates,” the authors wrote.
While the association is noted in U.S. stroke guidelines, there are few recommendations for treatment aside from fall prevention strategies, which the authors noted was a missed opportunity for prevention.
“Use of a risk prediction score to identify those at particularly high short-term risk of fractures after stroke may help to prioritize patients for osteoporosis testing and treatment,” they suggested.
The study was funded by the Heart and Stroke Foundation of Canada and was supported by ICES (Institute for Clinical Evaluative Sciences) and the Ontario Ministry of Health and Long-Term Care. One author declared consultancies for the pharmaceutical sector. No other conflicts of interest were declared.
SOURCE: Kapoor E et al. Stroke. 2019 April 25. doi: 10.1161/STROKEAHA.118.024685
Although stroke is a risk factor for osteoporosis, falls, and fractures, very few people who have experienced a recent stroke are either screened for osteoporosis or treated, research suggests.
Writing in Stroke, researchers presented an analysis of Ontario registry data from 16,581 patients who were aged 65 years or older and presented with stroke between 2003 and 2013.
Overall, just 5.1% of patients underwent bone mineral density testing. Of the 1,577 patients who had experienced a prior fracture, 71 (4.7%) had bone mineral density testing, and only 2.9% of those who had not had prior bone mineral density testing were tested after their stroke. Bone mineral density testing was more likely in patients who were younger, who were female, and who experienced a low-trauma fracture in the year after their stroke.
In total, 15.5% of patients were prescribed osteoporosis drugs in the first year after their stroke. However, only 7.8% of those who had fractures before the stroke and 14.8% of those with fractures after the stroke received osteoporosis treatment after the stroke. Patients who were female, had prior osteoporosis, had experienced prior fracture, had previously undergone bone mineral density testing, or had experienced a fracture or fall after their stroke were more likely to receive osteoporosis pharmacotherapy.
The authors found that the neither the severity of stroke nor the presence of other comorbidities was associated with an increased likelihood of screening or treatment of osteoporosis after the stroke.
Stroke is associated with up to a fourfold increased risk of osteoporosis and fracture, compared with healthy controls, most probably because of reduced mobility and an increased risk of falls, wrote Eshita Kapoor of the department of medicine at the University of Toronto and her coauthors.
“Screening and treatment may be particularly low poststroke because of under-recognition of osteoporosis as a consequence of stroke, a selective focus on the management of cardiovascular risk and stroke recovery, or factors such as dysphagia precluding use of oral bisphosphonates,” the authors wrote.
While the association is noted in U.S. stroke guidelines, there are few recommendations for treatment aside from fall prevention strategies, which the authors noted was a missed opportunity for prevention.
“Use of a risk prediction score to identify those at particularly high short-term risk of fractures after stroke may help to prioritize patients for osteoporosis testing and treatment,” they suggested.
The study was funded by the Heart and Stroke Foundation of Canada and was supported by ICES (Institute for Clinical Evaluative Sciences) and the Ontario Ministry of Health and Long-Term Care. One author declared consultancies for the pharmaceutical sector. No other conflicts of interest were declared.
SOURCE: Kapoor E et al. Stroke. 2019 April 25. doi: 10.1161/STROKEAHA.118.024685
Although stroke is a risk factor for osteoporosis, falls, and fractures, very few people who have experienced a recent stroke are either screened for osteoporosis or treated, research suggests.
Writing in Stroke, researchers presented an analysis of Ontario registry data from 16,581 patients who were aged 65 years or older and presented with stroke between 2003 and 2013.
Overall, just 5.1% of patients underwent bone mineral density testing. Of the 1,577 patients who had experienced a prior fracture, 71 (4.7%) had bone mineral density testing, and only 2.9% of those who had not had prior bone mineral density testing were tested after their stroke. Bone mineral density testing was more likely in patients who were younger, who were female, and who experienced a low-trauma fracture in the year after their stroke.
In total, 15.5% of patients were prescribed osteoporosis drugs in the first year after their stroke. However, only 7.8% of those who had fractures before the stroke and 14.8% of those with fractures after the stroke received osteoporosis treatment after the stroke. Patients who were female, had prior osteoporosis, had experienced prior fracture, had previously undergone bone mineral density testing, or had experienced a fracture or fall after their stroke were more likely to receive osteoporosis pharmacotherapy.
The authors found that the neither the severity of stroke nor the presence of other comorbidities was associated with an increased likelihood of screening or treatment of osteoporosis after the stroke.
Stroke is associated with up to a fourfold increased risk of osteoporosis and fracture, compared with healthy controls, most probably because of reduced mobility and an increased risk of falls, wrote Eshita Kapoor of the department of medicine at the University of Toronto and her coauthors.
“Screening and treatment may be particularly low poststroke because of under-recognition of osteoporosis as a consequence of stroke, a selective focus on the management of cardiovascular risk and stroke recovery, or factors such as dysphagia precluding use of oral bisphosphonates,” the authors wrote.
While the association is noted in U.S. stroke guidelines, there are few recommendations for treatment aside from fall prevention strategies, which the authors noted was a missed opportunity for prevention.
“Use of a risk prediction score to identify those at particularly high short-term risk of fractures after stroke may help to prioritize patients for osteoporosis testing and treatment,” they suggested.
The study was funded by the Heart and Stroke Foundation of Canada and was supported by ICES (Institute for Clinical Evaluative Sciences) and the Ontario Ministry of Health and Long-Term Care. One author declared consultancies for the pharmaceutical sector. No other conflicts of interest were declared.
SOURCE: Kapoor E et al. Stroke. 2019 April 25. doi: 10.1161/STROKEAHA.118.024685
FROM STROKE
CD40 ligand–binding protein safely lowered RA disease activity
A nonantibody scaffold protein that targets the CD40 ligand appears to dampen down autoimmune responses without the thromboembolic complications seen in trials of monoclonal antibodies against the CD40 ligand.
In a paper published in Science Translational Medicine, researchers presented the results of a phase 1a study in 59 healthy volunteers and phase 1b proof-of-concept study in 57 individuals with rheumatoid arthritis. Participants received either varying dosages of CD40 ligand (CD40L)–binding protein VIB4920 – a single dose in the healthy volunteers and seven doses in the phase 1b study – or placebo.
Jodi L. Karnell, PhD, of Viela Bio in Gaithersburg, Md., and coauthors, wrote that the CD40/CD40L pathway is known to play a key role in humoral immune responses and in the pathogenesis of several autoimmune diseases.
However, previous clinical trials of compounds targeting CD40L were stopped early because of an increased risk of adverse thromboembolic events related to platelet aggregation, despite showing potential benefits in lupus and immune thrombocytopenic purpura.
Preclinical studies of VIB4920 found that it blocked the expansion of CD40L-dependent human B cells without showing any signs of platelet aggregation. The authors said the platelet aggregation had been linked to a particular region of anti-CD40L monoclonal antibodies, but VIB4920 was engineered using a protein scaffold that did not contain that region.
In healthy volunteers, researchers saw a dose-dependent suppression of antibody production and reductions in B-cell proliferation, in recall response to a T cell–dependent antigen.
In individuals with rheumatoid arthritis, more than half of those treated with the two highest dosages of VIB4920 achieved low disease activity state or clinical remission by 12 weeks. Overall, there was also a significant decrease in disease activity, and dose-dependent decreases in rheumatoid factor autoantibodies and Vectra DA biomarker score, which is a composite of twelve rheumatoid arthritis–related biomarkers.
“The consistency of improvement across a variety of clinical and laboratory outcome measures further supports the potential clinical efficacy of VIB4920,” the authors wrote.
Researchers saw a similar rate of adverse events in the placebo and treatment arms of the study.
“VIB4920 represents an alternative to monoclonal antibody–based targeting of CD40L, which does not induce platelet aggregation in vitro and demonstrates a favorable safety profile in early clinical evaluation.”
The study was funded by MedImmune. All but one author were employees of MedImmune/AstraZeneca or of Viela Bio.
SOURCE: Karnell J et al. Sci Transl Med. 2019 April 24. doi: 10.1126/scitranslmed.aar6584
A nonantibody scaffold protein that targets the CD40 ligand appears to dampen down autoimmune responses without the thromboembolic complications seen in trials of monoclonal antibodies against the CD40 ligand.
In a paper published in Science Translational Medicine, researchers presented the results of a phase 1a study in 59 healthy volunteers and phase 1b proof-of-concept study in 57 individuals with rheumatoid arthritis. Participants received either varying dosages of CD40 ligand (CD40L)–binding protein VIB4920 – a single dose in the healthy volunteers and seven doses in the phase 1b study – or placebo.
Jodi L. Karnell, PhD, of Viela Bio in Gaithersburg, Md., and coauthors, wrote that the CD40/CD40L pathway is known to play a key role in humoral immune responses and in the pathogenesis of several autoimmune diseases.
However, previous clinical trials of compounds targeting CD40L were stopped early because of an increased risk of adverse thromboembolic events related to platelet aggregation, despite showing potential benefits in lupus and immune thrombocytopenic purpura.
Preclinical studies of VIB4920 found that it blocked the expansion of CD40L-dependent human B cells without showing any signs of platelet aggregation. The authors said the platelet aggregation had been linked to a particular region of anti-CD40L monoclonal antibodies, but VIB4920 was engineered using a protein scaffold that did not contain that region.
In healthy volunteers, researchers saw a dose-dependent suppression of antibody production and reductions in B-cell proliferation, in recall response to a T cell–dependent antigen.
In individuals with rheumatoid arthritis, more than half of those treated with the two highest dosages of VIB4920 achieved low disease activity state or clinical remission by 12 weeks. Overall, there was also a significant decrease in disease activity, and dose-dependent decreases in rheumatoid factor autoantibodies and Vectra DA biomarker score, which is a composite of twelve rheumatoid arthritis–related biomarkers.
“The consistency of improvement across a variety of clinical and laboratory outcome measures further supports the potential clinical efficacy of VIB4920,” the authors wrote.
Researchers saw a similar rate of adverse events in the placebo and treatment arms of the study.
“VIB4920 represents an alternative to monoclonal antibody–based targeting of CD40L, which does not induce platelet aggregation in vitro and demonstrates a favorable safety profile in early clinical evaluation.”
The study was funded by MedImmune. All but one author were employees of MedImmune/AstraZeneca or of Viela Bio.
SOURCE: Karnell J et al. Sci Transl Med. 2019 April 24. doi: 10.1126/scitranslmed.aar6584
A nonantibody scaffold protein that targets the CD40 ligand appears to dampen down autoimmune responses without the thromboembolic complications seen in trials of monoclonal antibodies against the CD40 ligand.
In a paper published in Science Translational Medicine, researchers presented the results of a phase 1a study in 59 healthy volunteers and phase 1b proof-of-concept study in 57 individuals with rheumatoid arthritis. Participants received either varying dosages of CD40 ligand (CD40L)–binding protein VIB4920 – a single dose in the healthy volunteers and seven doses in the phase 1b study – or placebo.
Jodi L. Karnell, PhD, of Viela Bio in Gaithersburg, Md., and coauthors, wrote that the CD40/CD40L pathway is known to play a key role in humoral immune responses and in the pathogenesis of several autoimmune diseases.
However, previous clinical trials of compounds targeting CD40L were stopped early because of an increased risk of adverse thromboembolic events related to platelet aggregation, despite showing potential benefits in lupus and immune thrombocytopenic purpura.
Preclinical studies of VIB4920 found that it blocked the expansion of CD40L-dependent human B cells without showing any signs of platelet aggregation. The authors said the platelet aggregation had been linked to a particular region of anti-CD40L monoclonal antibodies, but VIB4920 was engineered using a protein scaffold that did not contain that region.
In healthy volunteers, researchers saw a dose-dependent suppression of antibody production and reductions in B-cell proliferation, in recall response to a T cell–dependent antigen.
In individuals with rheumatoid arthritis, more than half of those treated with the two highest dosages of VIB4920 achieved low disease activity state or clinical remission by 12 weeks. Overall, there was also a significant decrease in disease activity, and dose-dependent decreases in rheumatoid factor autoantibodies and Vectra DA biomarker score, which is a composite of twelve rheumatoid arthritis–related biomarkers.
“The consistency of improvement across a variety of clinical and laboratory outcome measures further supports the potential clinical efficacy of VIB4920,” the authors wrote.
Researchers saw a similar rate of adverse events in the placebo and treatment arms of the study.
“VIB4920 represents an alternative to monoclonal antibody–based targeting of CD40L, which does not induce platelet aggregation in vitro and demonstrates a favorable safety profile in early clinical evaluation.”
The study was funded by MedImmune. All but one author were employees of MedImmune/AstraZeneca or of Viela Bio.
SOURCE: Karnell J et al. Sci Transl Med. 2019 April 24. doi: 10.1126/scitranslmed.aar6584
FROM SCIENCE TRANSLATIONAL MEDICINE
Key clinical point:
Major finding: Treatment with higher doses of VIB4920 is associated with low disease activity or remission in 50% of rheumatoid arthritis patients.
Study details: Phase 1a and 1b study in 59 healthy individuals and 57 people with rheumatoid arthritis.
Disclosures: The study was funded by MedImmune. All but one author were employees of MedImmune/AstraZeneca or Viela Bio.
Source: Karnell J et al. Sci Transl Med. 2019 April 24. doi: 10.1126/scitranslmed.aar6584.
Decline in CIN2+ in younger women after HPV vaccine introduced
The introduction of human papillomavirus vaccination in the United States in 2006 was associated with a significant decrease in the rates of cervical intraepithelial neoplasia grades 2 and above (CIN2+) in younger women.
The overall rate of CIN2+ declined from an estimated 216,000 cases in 2008 – 55% of which were in women aged 18-29 years – to 196,000 cases in 2016, of which 36% were in women aged 18-29 years, according to analysis of data from the Human Papillomavirus Vaccine Impact Monitoring Program (MMWR. 2019 Apr 19;68:337-43.
In 2008, the highest rates of CIN2+ were seen in women aged 20-24 years and decreased with age, but in 2016, the highest rates were in women aged 25-29 years. The rates of CIN2+ declined significantly in women aged 18-19 years from 2008-2016, but increased in women aged 40-64 years.
In 2008 and 2016, around three-quarters of all CIN2+ cases were attributable to HPV types that are targeted by the HPV vaccine. However the rates of vaccine-preventable CIN2+ declined among women aged 18-24 years, from 52% in 2008 to 30% in 2016.
“Both the estimated number and rates of U.S. CIN2+ cases in this report must be interpreted in the context of cervical cancer prevention strategies, including HPV vaccination and cervical cancer screening,” wrote Nancy M. McClung, PhD, of the Epidemic Intelligence Service at the Centers for Disease Control and Prevention and coauthors.
Notably, the screening interval for cervical cancer was increased from yearly in 2008 to once in 3 years with cytology alone or once in 5 years with cytology plus HPV testing for women aged 30 or above in 2016.
“Older age at screening initiation, longer screening intervals, and more conservative management in young women might be expected to reduce the number of CIN2+ cases detected in younger age groups in whom lesions are most likely to regress and shift detection of some CIN2+ to older age groups, resulting in a transient increase in rates,” Dr. McClung and colleagues wrote.
However they noted that the decrease in HPV 16/18–attributable CIN2+ rates among younger age groups was likely a reflection of the impact of the introduction of the quadrivalent vaccine immunization program.
One author declared personal fees from Merck during the course of the study. No other conflicts of interest were declared.
SOURCE: McClung N et al. MMWR. 2019 Apr 19;68:337-43.
The introduction of human papillomavirus vaccination in the United States in 2006 was associated with a significant decrease in the rates of cervical intraepithelial neoplasia grades 2 and above (CIN2+) in younger women.
The overall rate of CIN2+ declined from an estimated 216,000 cases in 2008 – 55% of which were in women aged 18-29 years – to 196,000 cases in 2016, of which 36% were in women aged 18-29 years, according to analysis of data from the Human Papillomavirus Vaccine Impact Monitoring Program (MMWR. 2019 Apr 19;68:337-43.
In 2008, the highest rates of CIN2+ were seen in women aged 20-24 years and decreased with age, but in 2016, the highest rates were in women aged 25-29 years. The rates of CIN2+ declined significantly in women aged 18-19 years from 2008-2016, but increased in women aged 40-64 years.
In 2008 and 2016, around three-quarters of all CIN2+ cases were attributable to HPV types that are targeted by the HPV vaccine. However the rates of vaccine-preventable CIN2+ declined among women aged 18-24 years, from 52% in 2008 to 30% in 2016.
“Both the estimated number and rates of U.S. CIN2+ cases in this report must be interpreted in the context of cervical cancer prevention strategies, including HPV vaccination and cervical cancer screening,” wrote Nancy M. McClung, PhD, of the Epidemic Intelligence Service at the Centers for Disease Control and Prevention and coauthors.
Notably, the screening interval for cervical cancer was increased from yearly in 2008 to once in 3 years with cytology alone or once in 5 years with cytology plus HPV testing for women aged 30 or above in 2016.
“Older age at screening initiation, longer screening intervals, and more conservative management in young women might be expected to reduce the number of CIN2+ cases detected in younger age groups in whom lesions are most likely to regress and shift detection of some CIN2+ to older age groups, resulting in a transient increase in rates,” Dr. McClung and colleagues wrote.
However they noted that the decrease in HPV 16/18–attributable CIN2+ rates among younger age groups was likely a reflection of the impact of the introduction of the quadrivalent vaccine immunization program.
One author declared personal fees from Merck during the course of the study. No other conflicts of interest were declared.
SOURCE: McClung N et al. MMWR. 2019 Apr 19;68:337-43.
The introduction of human papillomavirus vaccination in the United States in 2006 was associated with a significant decrease in the rates of cervical intraepithelial neoplasia grades 2 and above (CIN2+) in younger women.
The overall rate of CIN2+ declined from an estimated 216,000 cases in 2008 – 55% of which were in women aged 18-29 years – to 196,000 cases in 2016, of which 36% were in women aged 18-29 years, according to analysis of data from the Human Papillomavirus Vaccine Impact Monitoring Program (MMWR. 2019 Apr 19;68:337-43.
In 2008, the highest rates of CIN2+ were seen in women aged 20-24 years and decreased with age, but in 2016, the highest rates were in women aged 25-29 years. The rates of CIN2+ declined significantly in women aged 18-19 years from 2008-2016, but increased in women aged 40-64 years.
In 2008 and 2016, around three-quarters of all CIN2+ cases were attributable to HPV types that are targeted by the HPV vaccine. However the rates of vaccine-preventable CIN2+ declined among women aged 18-24 years, from 52% in 2008 to 30% in 2016.
“Both the estimated number and rates of U.S. CIN2+ cases in this report must be interpreted in the context of cervical cancer prevention strategies, including HPV vaccination and cervical cancer screening,” wrote Nancy M. McClung, PhD, of the Epidemic Intelligence Service at the Centers for Disease Control and Prevention and coauthors.
Notably, the screening interval for cervical cancer was increased from yearly in 2008 to once in 3 years with cytology alone or once in 5 years with cytology plus HPV testing for women aged 30 or above in 2016.
“Older age at screening initiation, longer screening intervals, and more conservative management in young women might be expected to reduce the number of CIN2+ cases detected in younger age groups in whom lesions are most likely to regress and shift detection of some CIN2+ to older age groups, resulting in a transient increase in rates,” Dr. McClung and colleagues wrote.
However they noted that the decrease in HPV 16/18–attributable CIN2+ rates among younger age groups was likely a reflection of the impact of the introduction of the quadrivalent vaccine immunization program.
One author declared personal fees from Merck during the course of the study. No other conflicts of interest were declared.
SOURCE: McClung N et al. MMWR. 2019 Apr 19;68:337-43.
FROM MMWR
Most CBT delivery methods effective for depression
Most modes of delivery for cognitive-behavioral therapy appear to be effective interventions for the acute symptoms of depression, with the exception of unguided self-help therapy, a study has found.
In the study, published in JAMA Psychiatry, : individual, group, telephone, guided, and unguided self-help.
In general, CBT delivered individually, in a group, by guided self-help, or by telephone were all significantly more effective at improving the severity of depression than unguided, self-administered CBT, and significantly more effective than the controls of waiting list or usual care.
However, even unguided self-help CBT was more effective than the waiting list, although not more effective than care as usual.
“This study suggests that group, telephone, and guided self-help treatments are effective interventions that may be considered as alternatives to individual CBT,” wrote Pim Cuijpers, PhD, who is affiliated with the Amsterdam Public Health Research Institute at the Vrije Universiteit Amsterdam, and his coauthors. “Applying effective and acceptable CBT in a range of different formats will make CBT easier to implement, disseminate, and deliver across different settings and diverse patient populations.”
In terms of acceptability, individual-, group-, and telephone-delivered CBT were all equally acceptable. The analysis showed that guided self-help had lower acceptability than individual or group therapy, care as usual, and the waiting list, while unguided self-help therapy was less acceptable than being on a waiting list.
The authors said it was not clear why guided self-help CBT showed lower acceptability, compared with the other CBT formats.
“Maybe the absence of direct contact with a professional makes it easier to stop the treatment because there is less personal relationship pressure to continue with the treatment or the study,” they wrote.
The analysis also explored the long-term effectiveness of different delivery methods, although the authors cautioned that this was based on small numbers of comparisons. They found significantly greater long-term effectiveness associated with individual, group, guided self-help, and telephone CBT, compared with usual care, but telephone CBT was less effective than individual CBT.
Two authors reported receiving personal fees from private industry outside of the submitted work, and one reported receiving grants and support from the National Institute for Health Research.
SOURCE: Cuijpers P et al. JAMA Psychiatry. 2019 Apr 17. doi: 10.1001/jamapsychiatry.2019.0268.
Most modes of delivery for cognitive-behavioral therapy appear to be effective interventions for the acute symptoms of depression, with the exception of unguided self-help therapy, a study has found.
In the study, published in JAMA Psychiatry, : individual, group, telephone, guided, and unguided self-help.
In general, CBT delivered individually, in a group, by guided self-help, or by telephone were all significantly more effective at improving the severity of depression than unguided, self-administered CBT, and significantly more effective than the controls of waiting list or usual care.
However, even unguided self-help CBT was more effective than the waiting list, although not more effective than care as usual.
“This study suggests that group, telephone, and guided self-help treatments are effective interventions that may be considered as alternatives to individual CBT,” wrote Pim Cuijpers, PhD, who is affiliated with the Amsterdam Public Health Research Institute at the Vrije Universiteit Amsterdam, and his coauthors. “Applying effective and acceptable CBT in a range of different formats will make CBT easier to implement, disseminate, and deliver across different settings and diverse patient populations.”
In terms of acceptability, individual-, group-, and telephone-delivered CBT were all equally acceptable. The analysis showed that guided self-help had lower acceptability than individual or group therapy, care as usual, and the waiting list, while unguided self-help therapy was less acceptable than being on a waiting list.
The authors said it was not clear why guided self-help CBT showed lower acceptability, compared with the other CBT formats.
“Maybe the absence of direct contact with a professional makes it easier to stop the treatment because there is less personal relationship pressure to continue with the treatment or the study,” they wrote.
The analysis also explored the long-term effectiveness of different delivery methods, although the authors cautioned that this was based on small numbers of comparisons. They found significantly greater long-term effectiveness associated with individual, group, guided self-help, and telephone CBT, compared with usual care, but telephone CBT was less effective than individual CBT.
Two authors reported receiving personal fees from private industry outside of the submitted work, and one reported receiving grants and support from the National Institute for Health Research.
SOURCE: Cuijpers P et al. JAMA Psychiatry. 2019 Apr 17. doi: 10.1001/jamapsychiatry.2019.0268.
Most modes of delivery for cognitive-behavioral therapy appear to be effective interventions for the acute symptoms of depression, with the exception of unguided self-help therapy, a study has found.
In the study, published in JAMA Psychiatry, : individual, group, telephone, guided, and unguided self-help.
In general, CBT delivered individually, in a group, by guided self-help, or by telephone were all significantly more effective at improving the severity of depression than unguided, self-administered CBT, and significantly more effective than the controls of waiting list or usual care.
However, even unguided self-help CBT was more effective than the waiting list, although not more effective than care as usual.
“This study suggests that group, telephone, and guided self-help treatments are effective interventions that may be considered as alternatives to individual CBT,” wrote Pim Cuijpers, PhD, who is affiliated with the Amsterdam Public Health Research Institute at the Vrije Universiteit Amsterdam, and his coauthors. “Applying effective and acceptable CBT in a range of different formats will make CBT easier to implement, disseminate, and deliver across different settings and diverse patient populations.”
In terms of acceptability, individual-, group-, and telephone-delivered CBT were all equally acceptable. The analysis showed that guided self-help had lower acceptability than individual or group therapy, care as usual, and the waiting list, while unguided self-help therapy was less acceptable than being on a waiting list.
The authors said it was not clear why guided self-help CBT showed lower acceptability, compared with the other CBT formats.
“Maybe the absence of direct contact with a professional makes it easier to stop the treatment because there is less personal relationship pressure to continue with the treatment or the study,” they wrote.
The analysis also explored the long-term effectiveness of different delivery methods, although the authors cautioned that this was based on small numbers of comparisons. They found significantly greater long-term effectiveness associated with individual, group, guided self-help, and telephone CBT, compared with usual care, but telephone CBT was less effective than individual CBT.
Two authors reported receiving personal fees from private industry outside of the submitted work, and one reported receiving grants and support from the National Institute for Health Research.
SOURCE: Cuijpers P et al. JAMA Psychiatry. 2019 Apr 17. doi: 10.1001/jamapsychiatry.2019.0268.
FROM JAMA PSYCHIATRY
PCI reduces mortality after STEMI in older adults
The use of percutaneous coronary intervention after ST-segment elevation myocardial infarction is increasing in older adults, and is associated with significantly lower in-hospital mortality, new research has found.
“Our study shows that the rates of utilization of PCI in older patients with STEMI and cardiogenic shock is rising. This rise has been paralleled by an equivalent decline in unadjusted mortality rates,” Abdulla A. Damluji, MD, and his coinvestigators wrote in an analysis published in the Journal of the American College of Cardiology.
They looked at outcomes of 317,728 cases of STEMI with cardiogenic shock during 1999-2013, of which 35% occurred in individuals aged 75 years or above.
Over the study period, the proportion of adults aged 75 years and over who underwent percutaneous coronary intervention after STEMI increased from 27% in 1999 to 56% in 2013. At the same time, in-hospital mortality rates in those patients declined from 64% in 1999 to 46% in 2013. Both differences were significant at P less than 0.001.
PCI more than halved the mortality associated with STEMI in older adults, even after adjustment for propensity score, and this was seen across all four U.S. Census Bureau regions in the analysis.
However, mortality rates were slightly higher in patients who underwent percutaneous coronary intervention and had a bleeding event, compared with those who did not have a bleeding event.
There were some significant differences in the prevalence of cardiovascular risk factors and noncardiovascular diagnoses between those who underwent percutaneous coronary intervention and those who did not. There was around a 20% higher prevalence of obesity, but a lower prevalence of valvular heart disease and heart failure, in individuals who were treated with percutaneous coronary intervention than among those who were not.
Older adults who received percutaneous coronary intervention also had a significantly lower disease burden compared with older adults who did not, and were more likely to be younger, male, and not an underrepresented minority.
“Despite the improvement in survival associated with early revascularization as reported by these studies, many older adults with multiple chronic conditions, worse disease burden, and possibly limited life expectancy as assessed by interventional cardiologists do not receive early revascularization with PCI,” wrote Dr. Damluji of Sinai Hospital of Baltimore and Johns Hopkins University, and his coauthors.
“This study was aimed to address this important selection bias by implementing different methods of propensity matching to understand the influence of early revascularization adjusting for demographic, clinical, and hospital characteristics between older adults with early revascularization versus those without revascularization.”
The study was partly supported by the Jane and Stanley F. Rodbell family. Three authors declared support from the National Institute on Aging. Two authors declared funding from private industry and one declared pharmaceutical stocks. No other conflicts of interest were declared.
SOURCE: Damluji A et al. J Am Coll Cardiol. 2019 Apr;73(15):1890-900.
Despite recent advances in early revascularization approaches, such as increasing availability and improved safety profile, which have seen a decrease in mortality rates after cardiogenic shock, many of the studies of these advances have excluded elderly patients. This limits the generalizability of the results.
This study is the largest analysis so far to explore the outcomes of cardiogenic shock and percutaneous coronary intervention in older adults. The authors have used a propensity score adjustment in an attempt to account for potentially confounding baseline characteristics, and shown significantly lower mortality after PCI.
However, the analysis is subject to the usual limitations of observational studies. In particular is the fact that patients with cardiogenic shock represent a spectrum of risk, comorbidities, degrees of disease, and coronary anatomy. These comorbid conditions could therefore have affected the selection decision for revascularization, and therefore outcomes. The challenge still remains also to identify older patients who are more likely to benefit from revascularization after STEMI.
Dr. Eliano P. Navarese is from Interventional Cardiology and Cardiovascular Medicine, Mater Dei Hospital and SIRIO MEDICINE Research Network, Italy. Dr. Sunil V. Rao is from the faculty of medicine at the University of Alberta, Edmonton. Dr. Mitchell W. Krucoff is from Duke University Medical Center/Duke Clinical Research Institute, Durham, N.C. These comments are adapted from their editorial (J Am Coll Cardiol. 2019 Apr;73(15):1901-4). No conflicts of interest were declared.
Despite recent advances in early revascularization approaches, such as increasing availability and improved safety profile, which have seen a decrease in mortality rates after cardiogenic shock, many of the studies of these advances have excluded elderly patients. This limits the generalizability of the results.
This study is the largest analysis so far to explore the outcomes of cardiogenic shock and percutaneous coronary intervention in older adults. The authors have used a propensity score adjustment in an attempt to account for potentially confounding baseline characteristics, and shown significantly lower mortality after PCI.
However, the analysis is subject to the usual limitations of observational studies. In particular is the fact that patients with cardiogenic shock represent a spectrum of risk, comorbidities, degrees of disease, and coronary anatomy. These comorbid conditions could therefore have affected the selection decision for revascularization, and therefore outcomes. The challenge still remains also to identify older patients who are more likely to benefit from revascularization after STEMI.
Dr. Eliano P. Navarese is from Interventional Cardiology and Cardiovascular Medicine, Mater Dei Hospital and SIRIO MEDICINE Research Network, Italy. Dr. Sunil V. Rao is from the faculty of medicine at the University of Alberta, Edmonton. Dr. Mitchell W. Krucoff is from Duke University Medical Center/Duke Clinical Research Institute, Durham, N.C. These comments are adapted from their editorial (J Am Coll Cardiol. 2019 Apr;73(15):1901-4). No conflicts of interest were declared.
Despite recent advances in early revascularization approaches, such as increasing availability and improved safety profile, which have seen a decrease in mortality rates after cardiogenic shock, many of the studies of these advances have excluded elderly patients. This limits the generalizability of the results.
This study is the largest analysis so far to explore the outcomes of cardiogenic shock and percutaneous coronary intervention in older adults. The authors have used a propensity score adjustment in an attempt to account for potentially confounding baseline characteristics, and shown significantly lower mortality after PCI.
However, the analysis is subject to the usual limitations of observational studies. In particular is the fact that patients with cardiogenic shock represent a spectrum of risk, comorbidities, degrees of disease, and coronary anatomy. These comorbid conditions could therefore have affected the selection decision for revascularization, and therefore outcomes. The challenge still remains also to identify older patients who are more likely to benefit from revascularization after STEMI.
Dr. Eliano P. Navarese is from Interventional Cardiology and Cardiovascular Medicine, Mater Dei Hospital and SIRIO MEDICINE Research Network, Italy. Dr. Sunil V. Rao is from the faculty of medicine at the University of Alberta, Edmonton. Dr. Mitchell W. Krucoff is from Duke University Medical Center/Duke Clinical Research Institute, Durham, N.C. These comments are adapted from their editorial (J Am Coll Cardiol. 2019 Apr;73(15):1901-4). No conflicts of interest were declared.
The use of percutaneous coronary intervention after ST-segment elevation myocardial infarction is increasing in older adults, and is associated with significantly lower in-hospital mortality, new research has found.
“Our study shows that the rates of utilization of PCI in older patients with STEMI and cardiogenic shock is rising. This rise has been paralleled by an equivalent decline in unadjusted mortality rates,” Abdulla A. Damluji, MD, and his coinvestigators wrote in an analysis published in the Journal of the American College of Cardiology.
They looked at outcomes of 317,728 cases of STEMI with cardiogenic shock during 1999-2013, of which 35% occurred in individuals aged 75 years or above.
Over the study period, the proportion of adults aged 75 years and over who underwent percutaneous coronary intervention after STEMI increased from 27% in 1999 to 56% in 2013. At the same time, in-hospital mortality rates in those patients declined from 64% in 1999 to 46% in 2013. Both differences were significant at P less than 0.001.
PCI more than halved the mortality associated with STEMI in older adults, even after adjustment for propensity score, and this was seen across all four U.S. Census Bureau regions in the analysis.
However, mortality rates were slightly higher in patients who underwent percutaneous coronary intervention and had a bleeding event, compared with those who did not have a bleeding event.
There were some significant differences in the prevalence of cardiovascular risk factors and noncardiovascular diagnoses between those who underwent percutaneous coronary intervention and those who did not. There was around a 20% higher prevalence of obesity, but a lower prevalence of valvular heart disease and heart failure, in individuals who were treated with percutaneous coronary intervention than among those who were not.
Older adults who received percutaneous coronary intervention also had a significantly lower disease burden compared with older adults who did not, and were more likely to be younger, male, and not an underrepresented minority.
“Despite the improvement in survival associated with early revascularization as reported by these studies, many older adults with multiple chronic conditions, worse disease burden, and possibly limited life expectancy as assessed by interventional cardiologists do not receive early revascularization with PCI,” wrote Dr. Damluji of Sinai Hospital of Baltimore and Johns Hopkins University, and his coauthors.
“This study was aimed to address this important selection bias by implementing different methods of propensity matching to understand the influence of early revascularization adjusting for demographic, clinical, and hospital characteristics between older adults with early revascularization versus those without revascularization.”
The study was partly supported by the Jane and Stanley F. Rodbell family. Three authors declared support from the National Institute on Aging. Two authors declared funding from private industry and one declared pharmaceutical stocks. No other conflicts of interest were declared.
SOURCE: Damluji A et al. J Am Coll Cardiol. 2019 Apr;73(15):1890-900.
The use of percutaneous coronary intervention after ST-segment elevation myocardial infarction is increasing in older adults, and is associated with significantly lower in-hospital mortality, new research has found.
“Our study shows that the rates of utilization of PCI in older patients with STEMI and cardiogenic shock is rising. This rise has been paralleled by an equivalent decline in unadjusted mortality rates,” Abdulla A. Damluji, MD, and his coinvestigators wrote in an analysis published in the Journal of the American College of Cardiology.
They looked at outcomes of 317,728 cases of STEMI with cardiogenic shock during 1999-2013, of which 35% occurred in individuals aged 75 years or above.
Over the study period, the proportion of adults aged 75 years and over who underwent percutaneous coronary intervention after STEMI increased from 27% in 1999 to 56% in 2013. At the same time, in-hospital mortality rates in those patients declined from 64% in 1999 to 46% in 2013. Both differences were significant at P less than 0.001.
PCI more than halved the mortality associated with STEMI in older adults, even after adjustment for propensity score, and this was seen across all four U.S. Census Bureau regions in the analysis.
However, mortality rates were slightly higher in patients who underwent percutaneous coronary intervention and had a bleeding event, compared with those who did not have a bleeding event.
There were some significant differences in the prevalence of cardiovascular risk factors and noncardiovascular diagnoses between those who underwent percutaneous coronary intervention and those who did not. There was around a 20% higher prevalence of obesity, but a lower prevalence of valvular heart disease and heart failure, in individuals who were treated with percutaneous coronary intervention than among those who were not.
Older adults who received percutaneous coronary intervention also had a significantly lower disease burden compared with older adults who did not, and were more likely to be younger, male, and not an underrepresented minority.
“Despite the improvement in survival associated with early revascularization as reported by these studies, many older adults with multiple chronic conditions, worse disease burden, and possibly limited life expectancy as assessed by interventional cardiologists do not receive early revascularization with PCI,” wrote Dr. Damluji of Sinai Hospital of Baltimore and Johns Hopkins University, and his coauthors.
“This study was aimed to address this important selection bias by implementing different methods of propensity matching to understand the influence of early revascularization adjusting for demographic, clinical, and hospital characteristics between older adults with early revascularization versus those without revascularization.”
The study was partly supported by the Jane and Stanley F. Rodbell family. Three authors declared support from the National Institute on Aging. Two authors declared funding from private industry and one declared pharmaceutical stocks. No other conflicts of interest were declared.
SOURCE: Damluji A et al. J Am Coll Cardiol. 2019 Apr;73(15):1890-900.
FROM JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Canagliflozin lowers kidney failure risk in T2D: CREDENCE
Patients with type 2 diabetes and chronic kidney disease (CKD) show significantly lower incidence of kidney failure and cardiovascular events after treatment with the sodium-glucose cotransporter 2 inhibitor canagliflozin, in the CREDENCE trial.
CREDENCE (Evaluation of the Effects of Canagliflozin on Renal and Cardiovascular Outcomes in Participants With Diabetic Nephropathy) is a double-blind, placebo-controlled trial involving 4,401 patients with type 2 diabetes and albuminuric CKD, who were randomized to either 100 mg of canagliflozin daily or placebo.
After a median follow-up of 2.62 years, there was a significant 30% lower risk of the primary outcome, which was a composite of end-stage kidney disease, a doubling of serum creatinine, or death from renal or cardiovascular causes, a highly significant difference at P = .00001.
Separately, there was a 32% lower risk of end-stage kidney disease, a 20% lower risk of cardiovascular death, MI, or stroke, and a 39% lower risk of hospitalization for heart failure, both significant differences. Patients treated with canagliflozin also had a 40% lower risk of a doubling of serum creatinine, and a 28% lower risk of dialysis, kidney transplantation, or renal death.
“These findings were observed despite very modest between-group differences in blood glucose level, weight, and blood pressure, and in contrast to previous concern about the initial acute reduction in the estimated GFR [glomerular filtration rate] observed with SGLT2 inhibitors,” wrote Vlado Perkovic, MD, from the George Institute for Global Health, University of New South Wales Sydney, and his coauthors. “This suggests that the mechanism of benefit is likely to be independent of glucose levels and may possibly stem from a reduction in intraglomerular pressure, with other possible mechanisms presently being studied.”
The trial was stopped early after reaching the prespecified efficacy criteria for early cessation. The authors estimated that 21.2 patients would need to be treated with canagliflozin to prevent one primary outcome.
There were no significant differences between the two groups in the rate of adverse and serious adverse events, including the risk of lower limb amputation and fracture.
The study was supported by Janssen Research and Development. Eighteen authors declared steering committee, support and consultancies with Janssen, and thirteen also declared personal fees from other pharmaceutical and private industry. Five authors were employees of Janssen.
SOURCE: Perkovic V et al. N Engl J Med. 2019 Apr 14. doi: 10.1056/NEJMoa1811744.
Sodium-glucose cotransporter 2 inhibitors are the most promising of a number of diabetes medications that have shown potential in renoprotection through a mechanism other than glucose homeostasis.
The study suggests canagliflozin’s effects are felt both in the renal system and systemically. The initial decrease in glomerular filtration rate in the first few weeks of treatment could be the result of decreases in glomerular perfusion and intraglomerular pressure, but this effect does stabilize. Levels of angiotensin II and atrial natriuretic peptide decrease, and there is also a decrease in inflammation and an increase in intrarenal oxygenation.
These findings are good news for patients with diabetes and chronic kidney disease, and their importance cannot be overstated.
Julie R. Ingelfinger, MD, is from the Tufts University in Boston, and Clifford J. Rosen, MD, is from the Center for Clinical and Translational Research, Maine Medical Center Research Institute, Scarborough. These comments are adapted from an accompanying editorial (N Engl J Med. 2019 Apr 14. doi: 10.1056/NEJMe1904740).
Sodium-glucose cotransporter 2 inhibitors are the most promising of a number of diabetes medications that have shown potential in renoprotection through a mechanism other than glucose homeostasis.
The study suggests canagliflozin’s effects are felt both in the renal system and systemically. The initial decrease in glomerular filtration rate in the first few weeks of treatment could be the result of decreases in glomerular perfusion and intraglomerular pressure, but this effect does stabilize. Levels of angiotensin II and atrial natriuretic peptide decrease, and there is also a decrease in inflammation and an increase in intrarenal oxygenation.
These findings are good news for patients with diabetes and chronic kidney disease, and their importance cannot be overstated.
Julie R. Ingelfinger, MD, is from the Tufts University in Boston, and Clifford J. Rosen, MD, is from the Center for Clinical and Translational Research, Maine Medical Center Research Institute, Scarborough. These comments are adapted from an accompanying editorial (N Engl J Med. 2019 Apr 14. doi: 10.1056/NEJMe1904740).
Sodium-glucose cotransporter 2 inhibitors are the most promising of a number of diabetes medications that have shown potential in renoprotection through a mechanism other than glucose homeostasis.
The study suggests canagliflozin’s effects are felt both in the renal system and systemically. The initial decrease in glomerular filtration rate in the first few weeks of treatment could be the result of decreases in glomerular perfusion and intraglomerular pressure, but this effect does stabilize. Levels of angiotensin II and atrial natriuretic peptide decrease, and there is also a decrease in inflammation and an increase in intrarenal oxygenation.
These findings are good news for patients with diabetes and chronic kidney disease, and their importance cannot be overstated.
Julie R. Ingelfinger, MD, is from the Tufts University in Boston, and Clifford J. Rosen, MD, is from the Center for Clinical and Translational Research, Maine Medical Center Research Institute, Scarborough. These comments are adapted from an accompanying editorial (N Engl J Med. 2019 Apr 14. doi: 10.1056/NEJMe1904740).
Patients with type 2 diabetes and chronic kidney disease (CKD) show significantly lower incidence of kidney failure and cardiovascular events after treatment with the sodium-glucose cotransporter 2 inhibitor canagliflozin, in the CREDENCE trial.
CREDENCE (Evaluation of the Effects of Canagliflozin on Renal and Cardiovascular Outcomes in Participants With Diabetic Nephropathy) is a double-blind, placebo-controlled trial involving 4,401 patients with type 2 diabetes and albuminuric CKD, who were randomized to either 100 mg of canagliflozin daily or placebo.
After a median follow-up of 2.62 years, there was a significant 30% lower risk of the primary outcome, which was a composite of end-stage kidney disease, a doubling of serum creatinine, or death from renal or cardiovascular causes, a highly significant difference at P = .00001.
Separately, there was a 32% lower risk of end-stage kidney disease, a 20% lower risk of cardiovascular death, MI, or stroke, and a 39% lower risk of hospitalization for heart failure, both significant differences. Patients treated with canagliflozin also had a 40% lower risk of a doubling of serum creatinine, and a 28% lower risk of dialysis, kidney transplantation, or renal death.
“These findings were observed despite very modest between-group differences in blood glucose level, weight, and blood pressure, and in contrast to previous concern about the initial acute reduction in the estimated GFR [glomerular filtration rate] observed with SGLT2 inhibitors,” wrote Vlado Perkovic, MD, from the George Institute for Global Health, University of New South Wales Sydney, and his coauthors. “This suggests that the mechanism of benefit is likely to be independent of glucose levels and may possibly stem from a reduction in intraglomerular pressure, with other possible mechanisms presently being studied.”
The trial was stopped early after reaching the prespecified efficacy criteria for early cessation. The authors estimated that 21.2 patients would need to be treated with canagliflozin to prevent one primary outcome.
There were no significant differences between the two groups in the rate of adverse and serious adverse events, including the risk of lower limb amputation and fracture.
The study was supported by Janssen Research and Development. Eighteen authors declared steering committee, support and consultancies with Janssen, and thirteen also declared personal fees from other pharmaceutical and private industry. Five authors were employees of Janssen.
SOURCE: Perkovic V et al. N Engl J Med. 2019 Apr 14. doi: 10.1056/NEJMoa1811744.
Patients with type 2 diabetes and chronic kidney disease (CKD) show significantly lower incidence of kidney failure and cardiovascular events after treatment with the sodium-glucose cotransporter 2 inhibitor canagliflozin, in the CREDENCE trial.
CREDENCE (Evaluation of the Effects of Canagliflozin on Renal and Cardiovascular Outcomes in Participants With Diabetic Nephropathy) is a double-blind, placebo-controlled trial involving 4,401 patients with type 2 diabetes and albuminuric CKD, who were randomized to either 100 mg of canagliflozin daily or placebo.
After a median follow-up of 2.62 years, there was a significant 30% lower risk of the primary outcome, which was a composite of end-stage kidney disease, a doubling of serum creatinine, or death from renal or cardiovascular causes, a highly significant difference at P = .00001.
Separately, there was a 32% lower risk of end-stage kidney disease, a 20% lower risk of cardiovascular death, MI, or stroke, and a 39% lower risk of hospitalization for heart failure, both significant differences. Patients treated with canagliflozin also had a 40% lower risk of a doubling of serum creatinine, and a 28% lower risk of dialysis, kidney transplantation, or renal death.
“These findings were observed despite very modest between-group differences in blood glucose level, weight, and blood pressure, and in contrast to previous concern about the initial acute reduction in the estimated GFR [glomerular filtration rate] observed with SGLT2 inhibitors,” wrote Vlado Perkovic, MD, from the George Institute for Global Health, University of New South Wales Sydney, and his coauthors. “This suggests that the mechanism of benefit is likely to be independent of glucose levels and may possibly stem from a reduction in intraglomerular pressure, with other possible mechanisms presently being studied.”
The trial was stopped early after reaching the prespecified efficacy criteria for early cessation. The authors estimated that 21.2 patients would need to be treated with canagliflozin to prevent one primary outcome.
There were no significant differences between the two groups in the rate of adverse and serious adverse events, including the risk of lower limb amputation and fracture.
The study was supported by Janssen Research and Development. Eighteen authors declared steering committee, support and consultancies with Janssen, and thirteen also declared personal fees from other pharmaceutical and private industry. Five authors were employees of Janssen.
SOURCE: Perkovic V et al. N Engl J Med. 2019 Apr 14. doi: 10.1056/NEJMoa1811744.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE