User login
Anecdotal Failures in the Diagnosis of Serotonin Syndrome
Clinical Question: What is the validity of commonly held beliefs regarding serotonin syndrome (SS)?
Background: SS is a potentially life-threatening condition caused by serotonin excess in the central nervous system. The authors tested the validity of four widely accepted tenets about SS: that the Hunter criteria are superior, that the onset of SS is rapid compared to neuroleptic malignant syndrome (NMS), that hyperthermia is common with SS, and that SS can be distinguished from NMS based on medication history.
Study Design: Systematic review and meta-analysis.
Setting: PubMed and Web of Science.
Synopsis: Researchers identified 299 case reports from 2004 to 2014 in which SS was the most likely diagnosis based on one of three available diagnostic systems. Rhabdomyolysis with creatine kinase >1,500 and ICU treatment were used as proxies for SS severity. The Hunter criteria (the current gold standard) identified fewer overdoses, episodes of rhabdomyolysis, and ICU cases than the Sternbach or Radomski criteria. Combinations of antidepressants with methylene blue, opiates, or linezolid were the most common reasons for ICU admission. Symptom onset was within six hours in only 27.5% of cases. Hyperthermia was present in only 9.2% of patients with SS.
Hospitalists cannot rely on any one set of criteria to diagnose SS. The typical combinations of opiates or linezolid with antidepressants should raise the level of suspicion for SS. Rigidity and rhabdomyolysis occur commonly in both NMS and SS. Hyperthermia and timing of onset are not good indicators to the diagnosis of SS.
Bottom line: A high index of suspicion rather than reliance on classification systems or anecdotal key symptoms is necessary when considering SS.
Citation: Werneke U, Jamshidi F, Taylor DM, Ott M. Conundrums in neurology: diagnosing serotonin syndrome – a meta-analysis of cases. BMC Neurol. 2016;16:97.
Clinical Question: What is the validity of commonly held beliefs regarding serotonin syndrome (SS)?
Background: SS is a potentially life-threatening condition caused by serotonin excess in the central nervous system. The authors tested the validity of four widely accepted tenets about SS: that the Hunter criteria are superior, that the onset of SS is rapid compared to neuroleptic malignant syndrome (NMS), that hyperthermia is common with SS, and that SS can be distinguished from NMS based on medication history.
Study Design: Systematic review and meta-analysis.
Setting: PubMed and Web of Science.
Synopsis: Researchers identified 299 case reports from 2004 to 2014 in which SS was the most likely diagnosis based on one of three available diagnostic systems. Rhabdomyolysis with creatine kinase >1,500 and ICU treatment were used as proxies for SS severity. The Hunter criteria (the current gold standard) identified fewer overdoses, episodes of rhabdomyolysis, and ICU cases than the Sternbach or Radomski criteria. Combinations of antidepressants with methylene blue, opiates, or linezolid were the most common reasons for ICU admission. Symptom onset was within six hours in only 27.5% of cases. Hyperthermia was present in only 9.2% of patients with SS.
Hospitalists cannot rely on any one set of criteria to diagnose SS. The typical combinations of opiates or linezolid with antidepressants should raise the level of suspicion for SS. Rigidity and rhabdomyolysis occur commonly in both NMS and SS. Hyperthermia and timing of onset are not good indicators to the diagnosis of SS.
Bottom line: A high index of suspicion rather than reliance on classification systems or anecdotal key symptoms is necessary when considering SS.
Citation: Werneke U, Jamshidi F, Taylor DM, Ott M. Conundrums in neurology: diagnosing serotonin syndrome – a meta-analysis of cases. BMC Neurol. 2016;16:97.
Clinical Question: What is the validity of commonly held beliefs regarding serotonin syndrome (SS)?
Background: SS is a potentially life-threatening condition caused by serotonin excess in the central nervous system. The authors tested the validity of four widely accepted tenets about SS: that the Hunter criteria are superior, that the onset of SS is rapid compared to neuroleptic malignant syndrome (NMS), that hyperthermia is common with SS, and that SS can be distinguished from NMS based on medication history.
Study Design: Systematic review and meta-analysis.
Setting: PubMed and Web of Science.
Synopsis: Researchers identified 299 case reports from 2004 to 2014 in which SS was the most likely diagnosis based on one of three available diagnostic systems. Rhabdomyolysis with creatine kinase >1,500 and ICU treatment were used as proxies for SS severity. The Hunter criteria (the current gold standard) identified fewer overdoses, episodes of rhabdomyolysis, and ICU cases than the Sternbach or Radomski criteria. Combinations of antidepressants with methylene blue, opiates, or linezolid were the most common reasons for ICU admission. Symptom onset was within six hours in only 27.5% of cases. Hyperthermia was present in only 9.2% of patients with SS.
Hospitalists cannot rely on any one set of criteria to diagnose SS. The typical combinations of opiates or linezolid with antidepressants should raise the level of suspicion for SS. Rigidity and rhabdomyolysis occur commonly in both NMS and SS. Hyperthermia and timing of onset are not good indicators to the diagnosis of SS.
Bottom line: A high index of suspicion rather than reliance on classification systems or anecdotal key symptoms is necessary when considering SS.
Citation: Werneke U, Jamshidi F, Taylor DM, Ott M. Conundrums in neurology: diagnosing serotonin syndrome – a meta-analysis of cases. BMC Neurol. 2016;16:97.
Restrictive Blood Transfusion Strategies May Increase the Risk of Mortality, Morbidity for Elderly Patients Undergoing Orthopedic Surgery
Clinical Question: Are there particular groups of patients in which lower transfusion thresholds (transfusion only at lower hemoglobin levels) may be harmful?
Background: Previously published meta-analyses have examined transfusion thresholds for critically ill, surgical, and medical patients. By combining these patients, previous meta-analyses are limited in the identification of intervention effects. A more refined understanding of how transfusion thresholds impact outcomes for a variety of patients in different clinical settings is needed.
Study Design: Context-specific systematic review and meta-analysis of randomized clinical trials.
Setting: Adult patients in perioperative, emergency, or intensive-care settings.
Synopsis: Patient information was extracted from 31 randomized clinical trials. The authors found that among 3,465 elderly patients undergoing orthopedic surgery, those given restrictive transfusion strategies had significantly more events reflecting inadequate oxygen supply (relative risk, 1.41; 95% CI, 1.03–1.92). No statistically significant effect from restrictive transfusions was seen in 3,322 patients with cardiovascular disease undergoing cardiac or vascular procedures; 3,590 mixed medical-surgical patients in emergency and intensive-care settings; and 823 patients in a combined group of postpartum women, hematologic malignancy patients, and younger patients with neurologic injury.
The authors argue that even statistically nonsignificant differences in morbidity and mortality should encourage more liberal transfusion; apart from orthopedic surgery patients, this argument is not well-supported by the available data.
Bottom Line: It remains unclear whether restrictive transfusion strategies have a negative impact on certain types of patients, although the authors argue that there may be a trend in that direction. Further study is needed for specific patient populations.
Citation: Hovaguimian F, Myles PS. Restrictive versus liberal transfusion strategy in the perioperative and acute care settings: a context-specific systematic review and meta-analysis of randomized clinical trials. Anesthesiology. 2016;125(1):46-61.
Clinical Question: Are there particular groups of patients in which lower transfusion thresholds (transfusion only at lower hemoglobin levels) may be harmful?
Background: Previously published meta-analyses have examined transfusion thresholds for critically ill, surgical, and medical patients. By combining these patients, previous meta-analyses are limited in the identification of intervention effects. A more refined understanding of how transfusion thresholds impact outcomes for a variety of patients in different clinical settings is needed.
Study Design: Context-specific systematic review and meta-analysis of randomized clinical trials.
Setting: Adult patients in perioperative, emergency, or intensive-care settings.
Synopsis: Patient information was extracted from 31 randomized clinical trials. The authors found that among 3,465 elderly patients undergoing orthopedic surgery, those given restrictive transfusion strategies had significantly more events reflecting inadequate oxygen supply (relative risk, 1.41; 95% CI, 1.03–1.92). No statistically significant effect from restrictive transfusions was seen in 3,322 patients with cardiovascular disease undergoing cardiac or vascular procedures; 3,590 mixed medical-surgical patients in emergency and intensive-care settings; and 823 patients in a combined group of postpartum women, hematologic malignancy patients, and younger patients with neurologic injury.
The authors argue that even statistically nonsignificant differences in morbidity and mortality should encourage more liberal transfusion; apart from orthopedic surgery patients, this argument is not well-supported by the available data.
Bottom Line: It remains unclear whether restrictive transfusion strategies have a negative impact on certain types of patients, although the authors argue that there may be a trend in that direction. Further study is needed for specific patient populations.
Citation: Hovaguimian F, Myles PS. Restrictive versus liberal transfusion strategy in the perioperative and acute care settings: a context-specific systematic review and meta-analysis of randomized clinical trials. Anesthesiology. 2016;125(1):46-61.
Clinical Question: Are there particular groups of patients in which lower transfusion thresholds (transfusion only at lower hemoglobin levels) may be harmful?
Background: Previously published meta-analyses have examined transfusion thresholds for critically ill, surgical, and medical patients. By combining these patients, previous meta-analyses are limited in the identification of intervention effects. A more refined understanding of how transfusion thresholds impact outcomes for a variety of patients in different clinical settings is needed.
Study Design: Context-specific systematic review and meta-analysis of randomized clinical trials.
Setting: Adult patients in perioperative, emergency, or intensive-care settings.
Synopsis: Patient information was extracted from 31 randomized clinical trials. The authors found that among 3,465 elderly patients undergoing orthopedic surgery, those given restrictive transfusion strategies had significantly more events reflecting inadequate oxygen supply (relative risk, 1.41; 95% CI, 1.03–1.92). No statistically significant effect from restrictive transfusions was seen in 3,322 patients with cardiovascular disease undergoing cardiac or vascular procedures; 3,590 mixed medical-surgical patients in emergency and intensive-care settings; and 823 patients in a combined group of postpartum women, hematologic malignancy patients, and younger patients with neurologic injury.
The authors argue that even statistically nonsignificant differences in morbidity and mortality should encourage more liberal transfusion; apart from orthopedic surgery patients, this argument is not well-supported by the available data.
Bottom Line: It remains unclear whether restrictive transfusion strategies have a negative impact on certain types of patients, although the authors argue that there may be a trend in that direction. Further study is needed for specific patient populations.
Citation: Hovaguimian F, Myles PS. Restrictive versus liberal transfusion strategy in the perioperative and acute care settings: a context-specific systematic review and meta-analysis of randomized clinical trials. Anesthesiology. 2016;125(1):46-61.
Loss of Independence after Surgery and Subsequent Outcomes in Older Patients
Clinical Question: What is the incidence of loss of independence (LOI) for older adults after surgery, and is there an association between LOI and readmission or death?
Background: LOI is being increasingly recognized as an important measure of patient-centered care and a potential opportunity for intervention to prevent disablement. This study is the first to examine links between LOI and rates of readmission or death following surgery.
Study Design: Retrospective cohort.
Setting: 26 U.S. hospitals participating in a national quality improvement project.
Synopsis: The authors examined data from 5,077 patients age 65 or older undergoing an inpatient surgical procedure. They examined ability to perform activities of daily living (ADLs), mobility, and living situation before and after surgery, and they defined LOI as a change in one or more of these factors at the time of discharge.
They found that LOI increased with age, with 49.9% of patients ages 65–74, 67.3% of patients ages 75–84, and 83.9% of patients age 85 or older experiencing LOI. The study also showed an association between LOI and negative outcomes, including readmission (odds ratio, 1.7) and death after discharge (odds ratio, 6.7).
Although this study was retrospective, the findings indicate that LOI is strongly correlated with negative short-term outcomes, especially in older populations. LOI related to surgery is a measure that deserves closer attention and greater future study as a potential target for clinical initiatives and intervention.
Bottom Line: LOI (functional ability, mobility, and living situation) after surgery increases with age and is associated with negative short-term outcomes including readmission and death.
Citation: Berian JR, Mohanty S, Ko CY, Rosenthal RA, Robinson TN. Association of loss of independence with readmission and death after discharge in older patients after surgical procedures. JAMA Surg. 2016;151(9):e161689.
Short Take
Transition to New Electronic Health Records Systems Does Not Increase Adverse Outcomes
An observational study comparing 17 hospitals implementing new electronic health records systems with 399 control hospitals showed no difference in the rate of adverse safety events or readmissions following implementation.
Citation: Barnett ML, Mehrotra A, Jena AB. Adverse inpatient outcomes during the transition to a new electronic health record system: observational study. BMJ. 2016;354:i3835.
Clinical Question: What is the incidence of loss of independence (LOI) for older adults after surgery, and is there an association between LOI and readmission or death?
Background: LOI is being increasingly recognized as an important measure of patient-centered care and a potential opportunity for intervention to prevent disablement. This study is the first to examine links between LOI and rates of readmission or death following surgery.
Study Design: Retrospective cohort.
Setting: 26 U.S. hospitals participating in a national quality improvement project.
Synopsis: The authors examined data from 5,077 patients age 65 or older undergoing an inpatient surgical procedure. They examined ability to perform activities of daily living (ADLs), mobility, and living situation before and after surgery, and they defined LOI as a change in one or more of these factors at the time of discharge.
They found that LOI increased with age, with 49.9% of patients ages 65–74, 67.3% of patients ages 75–84, and 83.9% of patients age 85 or older experiencing LOI. The study also showed an association between LOI and negative outcomes, including readmission (odds ratio, 1.7) and death after discharge (odds ratio, 6.7).
Although this study was retrospective, the findings indicate that LOI is strongly correlated with negative short-term outcomes, especially in older populations. LOI related to surgery is a measure that deserves closer attention and greater future study as a potential target for clinical initiatives and intervention.
Bottom Line: LOI (functional ability, mobility, and living situation) after surgery increases with age and is associated with negative short-term outcomes including readmission and death.
Citation: Berian JR, Mohanty S, Ko CY, Rosenthal RA, Robinson TN. Association of loss of independence with readmission and death after discharge in older patients after surgical procedures. JAMA Surg. 2016;151(9):e161689.
Short Take
Transition to New Electronic Health Records Systems Does Not Increase Adverse Outcomes
An observational study comparing 17 hospitals implementing new electronic health records systems with 399 control hospitals showed no difference in the rate of adverse safety events or readmissions following implementation.
Citation: Barnett ML, Mehrotra A, Jena AB. Adverse inpatient outcomes during the transition to a new electronic health record system: observational study. BMJ. 2016;354:i3835.
Clinical Question: What is the incidence of loss of independence (LOI) for older adults after surgery, and is there an association between LOI and readmission or death?
Background: LOI is being increasingly recognized as an important measure of patient-centered care and a potential opportunity for intervention to prevent disablement. This study is the first to examine links between LOI and rates of readmission or death following surgery.
Study Design: Retrospective cohort.
Setting: 26 U.S. hospitals participating in a national quality improvement project.
Synopsis: The authors examined data from 5,077 patients age 65 or older undergoing an inpatient surgical procedure. They examined ability to perform activities of daily living (ADLs), mobility, and living situation before and after surgery, and they defined LOI as a change in one or more of these factors at the time of discharge.
They found that LOI increased with age, with 49.9% of patients ages 65–74, 67.3% of patients ages 75–84, and 83.9% of patients age 85 or older experiencing LOI. The study also showed an association between LOI and negative outcomes, including readmission (odds ratio, 1.7) and death after discharge (odds ratio, 6.7).
Although this study was retrospective, the findings indicate that LOI is strongly correlated with negative short-term outcomes, especially in older populations. LOI related to surgery is a measure that deserves closer attention and greater future study as a potential target for clinical initiatives and intervention.
Bottom Line: LOI (functional ability, mobility, and living situation) after surgery increases with age and is associated with negative short-term outcomes including readmission and death.
Citation: Berian JR, Mohanty S, Ko CY, Rosenthal RA, Robinson TN. Association of loss of independence with readmission and death after discharge in older patients after surgical procedures. JAMA Surg. 2016;151(9):e161689.
Short Take
Transition to New Electronic Health Records Systems Does Not Increase Adverse Outcomes
An observational study comparing 17 hospitals implementing new electronic health records systems with 399 control hospitals showed no difference in the rate of adverse safety events or readmissions following implementation.
Citation: Barnett ML, Mehrotra A, Jena AB. Adverse inpatient outcomes during the transition to a new electronic health record system: observational study. BMJ. 2016;354:i3835.
Euthanasia and Physician-Assisted Suicide Remain Rare and Primarily Involve Cancer Patients
Clinical Question: What data are available regarding the attitudes toward and the practice of euthanasia and physician-assisted suicide (PAS)?
Background: Although controversial, euthanasia and PAS are currently legal in the Netherlands, Belgium, Luxembourg, Colombia, and Canada, while PAS (but not euthanasia) is legal in Switzerland and five states (Oregon, Washington, Montana, Vermont, and California). Knowledge about current practices is limited as only a portion of these jurisdictions have reporting requirements.
Study Design: Literature review with a focus on original data.
Setting: Data from United States, Canada, and Europe.
Synopsis: Published data from 1947 to 2016 were reviewed. U.S. public opinion surveys show a recent decline in support of PAS, from a peak of 75% in 2005 to 64% in 2012. With the exception of the Netherlands and Belgium, physicians in the U.S., Europe, and Australia are less supportive than the general public.
In the U.S., <20% of physicians reported receiving a request for euthanasia or PAS, and <5% complied. Oncologists are most likely to receive a patient request. The typical patient is older, white, insured, well-educated, and enrolled in hospice. Seventy-five percent have cancer, while 15% have neurodegenerative conditions. Loss of autonomy and dignity are common motivators, while <33% of patients cite uncontrolled pain. PAS remains rare, accounting for <0.4% of all deaths. Existing data do not indicate abuse of these practices.
The authors emphasize that existing data are limited and recommend that all countries, not just those where euthanasia and/or PAS are legal, should formally collect information on end-of-life practices.
Bottom Line: Euthanasia and PAS remain relatively rare and primarily involve oncology patients despite increasing legalization.
Citation: Emanuel EJ, Onwuteaka-Philipsen BD, Urwin JW, Cohen J. Attitudes and practices of euthanasia and physician-assisted suicide in the United States, Canada, and Europe. JAMA. 2016;316(1):79-90.
Short Take
Peer Support for Physicians May Curb Burnout
This perspective piece outlines a program of one-to-one peer outreach for physicians as a way to mitigate stress especially when dealing with adverse events or litigation, but no data are provided.
Citation: Shapiro J, Galowitz P. Peer support for clinicians: a programmatic approach. Acad Med. 2016;91(9):1200-1204.
Clinical Question: What data are available regarding the attitudes toward and the practice of euthanasia and physician-assisted suicide (PAS)?
Background: Although controversial, euthanasia and PAS are currently legal in the Netherlands, Belgium, Luxembourg, Colombia, and Canada, while PAS (but not euthanasia) is legal in Switzerland and five states (Oregon, Washington, Montana, Vermont, and California). Knowledge about current practices is limited as only a portion of these jurisdictions have reporting requirements.
Study Design: Literature review with a focus on original data.
Setting: Data from United States, Canada, and Europe.
Synopsis: Published data from 1947 to 2016 were reviewed. U.S. public opinion surveys show a recent decline in support of PAS, from a peak of 75% in 2005 to 64% in 2012. With the exception of the Netherlands and Belgium, physicians in the U.S., Europe, and Australia are less supportive than the general public.
In the U.S., <20% of physicians reported receiving a request for euthanasia or PAS, and <5% complied. Oncologists are most likely to receive a patient request. The typical patient is older, white, insured, well-educated, and enrolled in hospice. Seventy-five percent have cancer, while 15% have neurodegenerative conditions. Loss of autonomy and dignity are common motivators, while <33% of patients cite uncontrolled pain. PAS remains rare, accounting for <0.4% of all deaths. Existing data do not indicate abuse of these practices.
The authors emphasize that existing data are limited and recommend that all countries, not just those where euthanasia and/or PAS are legal, should formally collect information on end-of-life practices.
Bottom Line: Euthanasia and PAS remain relatively rare and primarily involve oncology patients despite increasing legalization.
Citation: Emanuel EJ, Onwuteaka-Philipsen BD, Urwin JW, Cohen J. Attitudes and practices of euthanasia and physician-assisted suicide in the United States, Canada, and Europe. JAMA. 2016;316(1):79-90.
Short Take
Peer Support for Physicians May Curb Burnout
This perspective piece outlines a program of one-to-one peer outreach for physicians as a way to mitigate stress especially when dealing with adverse events or litigation, but no data are provided.
Citation: Shapiro J, Galowitz P. Peer support for clinicians: a programmatic approach. Acad Med. 2016;91(9):1200-1204.
Clinical Question: What data are available regarding the attitudes toward and the practice of euthanasia and physician-assisted suicide (PAS)?
Background: Although controversial, euthanasia and PAS are currently legal in the Netherlands, Belgium, Luxembourg, Colombia, and Canada, while PAS (but not euthanasia) is legal in Switzerland and five states (Oregon, Washington, Montana, Vermont, and California). Knowledge about current practices is limited as only a portion of these jurisdictions have reporting requirements.
Study Design: Literature review with a focus on original data.
Setting: Data from United States, Canada, and Europe.
Synopsis: Published data from 1947 to 2016 were reviewed. U.S. public opinion surveys show a recent decline in support of PAS, from a peak of 75% in 2005 to 64% in 2012. With the exception of the Netherlands and Belgium, physicians in the U.S., Europe, and Australia are less supportive than the general public.
In the U.S., <20% of physicians reported receiving a request for euthanasia or PAS, and <5% complied. Oncologists are most likely to receive a patient request. The typical patient is older, white, insured, well-educated, and enrolled in hospice. Seventy-five percent have cancer, while 15% have neurodegenerative conditions. Loss of autonomy and dignity are common motivators, while <33% of patients cite uncontrolled pain. PAS remains rare, accounting for <0.4% of all deaths. Existing data do not indicate abuse of these practices.
The authors emphasize that existing data are limited and recommend that all countries, not just those where euthanasia and/or PAS are legal, should formally collect information on end-of-life practices.
Bottom Line: Euthanasia and PAS remain relatively rare and primarily involve oncology patients despite increasing legalization.
Citation: Emanuel EJ, Onwuteaka-Philipsen BD, Urwin JW, Cohen J. Attitudes and practices of euthanasia and physician-assisted suicide in the United States, Canada, and Europe. JAMA. 2016;316(1):79-90.
Short Take
Peer Support for Physicians May Curb Burnout
This perspective piece outlines a program of one-to-one peer outreach for physicians as a way to mitigate stress especially when dealing with adverse events or litigation, but no data are provided.
Citation: Shapiro J, Galowitz P. Peer support for clinicians: a programmatic approach. Acad Med. 2016;91(9):1200-1204.
Goals of Care Infrequently Discussed among Hospitalized Long-Term Care Residents
Clinical Question: How often are goals of care (GOC) discussed during hospitalization of long-term care residents, and what patient characteristics make this more likely to occur?
Background: GOC discussions during hospitalization have the potential to better align patient wishes with care received and to reduce unwanted care. Previous studies have examined barriers to GOC discussions, but less is known about factors associated with GOC discussions occurring and the outcomes of these discussions.
Study Design: Retrospective chart review.
Setting: Two academic hospitals in Toronto.
Synopsis: In the review, 665 hospitalized patients during a one-year period were identified as being >65 years old and from a long-term care facility. Of the 665 patients, a random sampling of 200 unique patients was reviewed. Of these, 37.5% had a documented GOC discussion. Lower Glasgow Coma Scale scores and higher respiratory rates were correlated with a higher incidence of GOC discussions. Patients with GOC discussions had higher rates of no resuscitation and comfort care orders; these patients also had higher odds of in-hospital death and one-year mortality. Of patients that had a change in their GOC, 74% did not have this change reflected in the discharge summary.
Although this study is a retrospective review and limited to two Canadian teaching hospitals, there is likely an opportunity for hospitalists to more frequently discuss and document GOC in hospitalized long-term care patients.
Bottom Line: In hospitalized long-term care patients, GOC are infrequently discussed and documented. Frequency of discussions is correlated with illness severity.
Citation: Wong HJ, Wang J, Grinman M, Wu RC. Goals of care discussions among hospitalized long-term care residents: predictors and associated outcomes of care [published online ahead of print July 21, 2016]. J Hosp Med.
Short Take
Sleep-Promoting Interventions Improve Sleep in Hospitalized Patients
A non-blinded, quasi-randomized pilot study of 112 patients demonstrated that sleep-promoting interventions, including education and environmental control to minimize sleep disruption, improved total nighttime sleep time as well as qualitative measures of sleep.
Citation: Gathecha E, Rios R, Buenaver LF, Landis R, Howell E, Wright S. Pilot study aiming to support sleep quality and duration during hospitalizations. J Hosp Med. 2016;11(7):467-472.
Clinical Question: How often are goals of care (GOC) discussed during hospitalization of long-term care residents, and what patient characteristics make this more likely to occur?
Background: GOC discussions during hospitalization have the potential to better align patient wishes with care received and to reduce unwanted care. Previous studies have examined barriers to GOC discussions, but less is known about factors associated with GOC discussions occurring and the outcomes of these discussions.
Study Design: Retrospective chart review.
Setting: Two academic hospitals in Toronto.
Synopsis: In the review, 665 hospitalized patients during a one-year period were identified as being >65 years old and from a long-term care facility. Of the 665 patients, a random sampling of 200 unique patients was reviewed. Of these, 37.5% had a documented GOC discussion. Lower Glasgow Coma Scale scores and higher respiratory rates were correlated with a higher incidence of GOC discussions. Patients with GOC discussions had higher rates of no resuscitation and comfort care orders; these patients also had higher odds of in-hospital death and one-year mortality. Of patients that had a change in their GOC, 74% did not have this change reflected in the discharge summary.
Although this study is a retrospective review and limited to two Canadian teaching hospitals, there is likely an opportunity for hospitalists to more frequently discuss and document GOC in hospitalized long-term care patients.
Bottom Line: In hospitalized long-term care patients, GOC are infrequently discussed and documented. Frequency of discussions is correlated with illness severity.
Citation: Wong HJ, Wang J, Grinman M, Wu RC. Goals of care discussions among hospitalized long-term care residents: predictors and associated outcomes of care [published online ahead of print July 21, 2016]. J Hosp Med.
Short Take
Sleep-Promoting Interventions Improve Sleep in Hospitalized Patients
A non-blinded, quasi-randomized pilot study of 112 patients demonstrated that sleep-promoting interventions, including education and environmental control to minimize sleep disruption, improved total nighttime sleep time as well as qualitative measures of sleep.
Citation: Gathecha E, Rios R, Buenaver LF, Landis R, Howell E, Wright S. Pilot study aiming to support sleep quality and duration during hospitalizations. J Hosp Med. 2016;11(7):467-472.
Clinical Question: How often are goals of care (GOC) discussed during hospitalization of long-term care residents, and what patient characteristics make this more likely to occur?
Background: GOC discussions during hospitalization have the potential to better align patient wishes with care received and to reduce unwanted care. Previous studies have examined barriers to GOC discussions, but less is known about factors associated with GOC discussions occurring and the outcomes of these discussions.
Study Design: Retrospective chart review.
Setting: Two academic hospitals in Toronto.
Synopsis: In the review, 665 hospitalized patients during a one-year period were identified as being >65 years old and from a long-term care facility. Of the 665 patients, a random sampling of 200 unique patients was reviewed. Of these, 37.5% had a documented GOC discussion. Lower Glasgow Coma Scale scores and higher respiratory rates were correlated with a higher incidence of GOC discussions. Patients with GOC discussions had higher rates of no resuscitation and comfort care orders; these patients also had higher odds of in-hospital death and one-year mortality. Of patients that had a change in their GOC, 74% did not have this change reflected in the discharge summary.
Although this study is a retrospective review and limited to two Canadian teaching hospitals, there is likely an opportunity for hospitalists to more frequently discuss and document GOC in hospitalized long-term care patients.
Bottom Line: In hospitalized long-term care patients, GOC are infrequently discussed and documented. Frequency of discussions is correlated with illness severity.
Citation: Wong HJ, Wang J, Grinman M, Wu RC. Goals of care discussions among hospitalized long-term care residents: predictors and associated outcomes of care [published online ahead of print July 21, 2016]. J Hosp Med.
Short Take
Sleep-Promoting Interventions Improve Sleep in Hospitalized Patients
A non-blinded, quasi-randomized pilot study of 112 patients demonstrated that sleep-promoting interventions, including education and environmental control to minimize sleep disruption, improved total nighttime sleep time as well as qualitative measures of sleep.
Citation: Gathecha E, Rios R, Buenaver LF, Landis R, Howell E, Wright S. Pilot study aiming to support sleep quality and duration during hospitalizations. J Hosp Med. 2016;11(7):467-472.
Hand Hygiene Improves Patient Safety
Clinical Question: Does improving hand hygiene compliance from a high level (>80%) to a very high level (>95%) reduce healthcare-associated infections?
Background: Hand hygiene compliance remains an elusive infection prevention parameter to master. Studies show a correlation in reduction of healthcare-associated infections with improved hand hygiene compliance from a low to medium level, but little data exist on very high rates of hand hygiene compliance.
Study Design: Prospective observational.
Setting: University of North Carolina Hospitals.
Synopsis: Researchers recruited all hospital staff to be hand hygiene monitors, thereby using the Hawthorne effect to drive hand hygiene compliance rates. Over a 17-month period, >4,000 unique observers made >140,000 observations. Data showed a significant increase in hand hygiene compliance rates of about 10% (P<0.001) and a significant decrease in overall healthcare-associated infection rates of about 6% (P=0.0066). A reduction in healthcare-associated Clostridium difficile infection of 14% was observed in association with the improved hand hygiene compliance. No association with multidrug-resistant organisms was found.
Bottom Line: There is continued correlation between improved hand hygiene compliance and reduced healthcare-associated infection rates even at very high levels (>95%) of hand hygiene compliance.
Citation: Sickbert-Bennett EE, DiBiase LM, Willis TM, Wolak ES, Weber DJ, Rutala WA. Reduction of healthcare-associated infections by exceeding high compliance with hand hygiene practices. Emerg Infect Dis. 2016;22(9):1628-1630.
Short Take
Avoid Fluoroquinolones in Acute Sinusitis, Acute Exacerbations of Bronchitis, and Uncomplicated Urinary Tract Infections If Other Treatment Options Exist
Because fluoroquinolones have been associated with potentially permanent side effects involving tendons, muscles, joints, and nerves, the FDA recently updated the boxed warning to state that the risk of use likely outweighs the benefit for uncomplicated infections.
Citation: Fluoroquinolone Antibacterial Drugs for Systemic Use: Drug Safety Communication - Warnings Updated Due to Disabling Side Effects. FDA website. Accessed September 9, 2016.
Clinical Question: Does improving hand hygiene compliance from a high level (>80%) to a very high level (>95%) reduce healthcare-associated infections?
Background: Hand hygiene compliance remains an elusive infection prevention parameter to master. Studies show a correlation in reduction of healthcare-associated infections with improved hand hygiene compliance from a low to medium level, but little data exist on very high rates of hand hygiene compliance.
Study Design: Prospective observational.
Setting: University of North Carolina Hospitals.
Synopsis: Researchers recruited all hospital staff to be hand hygiene monitors, thereby using the Hawthorne effect to drive hand hygiene compliance rates. Over a 17-month period, >4,000 unique observers made >140,000 observations. Data showed a significant increase in hand hygiene compliance rates of about 10% (P<0.001) and a significant decrease in overall healthcare-associated infection rates of about 6% (P=0.0066). A reduction in healthcare-associated Clostridium difficile infection of 14% was observed in association with the improved hand hygiene compliance. No association with multidrug-resistant organisms was found.
Bottom Line: There is continued correlation between improved hand hygiene compliance and reduced healthcare-associated infection rates even at very high levels (>95%) of hand hygiene compliance.
Citation: Sickbert-Bennett EE, DiBiase LM, Willis TM, Wolak ES, Weber DJ, Rutala WA. Reduction of healthcare-associated infections by exceeding high compliance with hand hygiene practices. Emerg Infect Dis. 2016;22(9):1628-1630.
Short Take
Avoid Fluoroquinolones in Acute Sinusitis, Acute Exacerbations of Bronchitis, and Uncomplicated Urinary Tract Infections If Other Treatment Options Exist
Because fluoroquinolones have been associated with potentially permanent side effects involving tendons, muscles, joints, and nerves, the FDA recently updated the boxed warning to state that the risk of use likely outweighs the benefit for uncomplicated infections.
Citation: Fluoroquinolone Antibacterial Drugs for Systemic Use: Drug Safety Communication - Warnings Updated Due to Disabling Side Effects. FDA website. Accessed September 9, 2016.
Clinical Question: Does improving hand hygiene compliance from a high level (>80%) to a very high level (>95%) reduce healthcare-associated infections?
Background: Hand hygiene compliance remains an elusive infection prevention parameter to master. Studies show a correlation in reduction of healthcare-associated infections with improved hand hygiene compliance from a low to medium level, but little data exist on very high rates of hand hygiene compliance.
Study Design: Prospective observational.
Setting: University of North Carolina Hospitals.
Synopsis: Researchers recruited all hospital staff to be hand hygiene monitors, thereby using the Hawthorne effect to drive hand hygiene compliance rates. Over a 17-month period, >4,000 unique observers made >140,000 observations. Data showed a significant increase in hand hygiene compliance rates of about 10% (P<0.001) and a significant decrease in overall healthcare-associated infection rates of about 6% (P=0.0066). A reduction in healthcare-associated Clostridium difficile infection of 14% was observed in association with the improved hand hygiene compliance. No association with multidrug-resistant organisms was found.
Bottom Line: There is continued correlation between improved hand hygiene compliance and reduced healthcare-associated infection rates even at very high levels (>95%) of hand hygiene compliance.
Citation: Sickbert-Bennett EE, DiBiase LM, Willis TM, Wolak ES, Weber DJ, Rutala WA. Reduction of healthcare-associated infections by exceeding high compliance with hand hygiene practices. Emerg Infect Dis. 2016;22(9):1628-1630.
Short Take
Avoid Fluoroquinolones in Acute Sinusitis, Acute Exacerbations of Bronchitis, and Uncomplicated Urinary Tract Infections If Other Treatment Options Exist
Because fluoroquinolones have been associated with potentially permanent side effects involving tendons, muscles, joints, and nerves, the FDA recently updated the boxed warning to state that the risk of use likely outweighs the benefit for uncomplicated infections.
Citation: Fluoroquinolone Antibacterial Drugs for Systemic Use: Drug Safety Communication - Warnings Updated Due to Disabling Side Effects. FDA website. Accessed September 9, 2016.
Traditional Hand Hygiene Audits Can Lead to Inaccurate Conclusions about Physician Performance
Clinical Question: Does direct observation underestimate physician compliance with hand hygiene (HH) compared to other professional groups due to the Hawthorne effect?
Background: Although it is well-known that HH is imperative to infection control, physician compliance remains suboptimal and is often reported to be below that of nurses. The Hawthorne effect may be contributing to this perceived difference because nurses, who work on the same unit consistently, may more readily recognize hospital auditors.
Study Design: Observational.
Setting: 800-bed acute-care academic hospital in Canada.
Synopsis: Two students were trained to covertly observe physician and nursing HH compliance on inpatient units. For two months, students rotated units every week to minimize risk of discovery. Their findings were compared with data gathered by hospital auditors over the same time period.
Covertly observed HH compliance was 50% (799/1,597 opportunities) compared with 83.7% (2,769/3,309) reported by hospital auditors (P<0.0002). The difference in physician compliance was 19% (73.2% compliance with overt observation versus 54.2% with covert observation). The difference was much higher for nurses at 40.7% (85.8% compliance with overt observation versus 45.1% with covert observation). Attending physician behaviors heavily influenced team behaviors—79.5% of trainees were compliant if their attending was compliant compared with 18.9% if attending was not (P<0.0002).
Bottom Line: Traditional HH audit findings that physicians are less compliant than nurses may be at least partially due to the Hawthorne effect. Nonetheless, all healthcare providers have substantial room for improvement, and attending physicians are powerful role models to effect this change.
Citation: Kovacs-Litman A, Wong K, Shojania KJ, Callery S, Vearncombe M, Leis J. Do physicians clean their hands? Insights from a covert observational study [published online ahead of print July 5, 2016]. J Hosp Med.
Clinical Question: Does direct observation underestimate physician compliance with hand hygiene (HH) compared to other professional groups due to the Hawthorne effect?
Background: Although it is well-known that HH is imperative to infection control, physician compliance remains suboptimal and is often reported to be below that of nurses. The Hawthorne effect may be contributing to this perceived difference because nurses, who work on the same unit consistently, may more readily recognize hospital auditors.
Study Design: Observational.
Setting: 800-bed acute-care academic hospital in Canada.
Synopsis: Two students were trained to covertly observe physician and nursing HH compliance on inpatient units. For two months, students rotated units every week to minimize risk of discovery. Their findings were compared with data gathered by hospital auditors over the same time period.
Covertly observed HH compliance was 50% (799/1,597 opportunities) compared with 83.7% (2,769/3,309) reported by hospital auditors (P<0.0002). The difference in physician compliance was 19% (73.2% compliance with overt observation versus 54.2% with covert observation). The difference was much higher for nurses at 40.7% (85.8% compliance with overt observation versus 45.1% with covert observation). Attending physician behaviors heavily influenced team behaviors—79.5% of trainees were compliant if their attending was compliant compared with 18.9% if attending was not (P<0.0002).
Bottom Line: Traditional HH audit findings that physicians are less compliant than nurses may be at least partially due to the Hawthorne effect. Nonetheless, all healthcare providers have substantial room for improvement, and attending physicians are powerful role models to effect this change.
Citation: Kovacs-Litman A, Wong K, Shojania KJ, Callery S, Vearncombe M, Leis J. Do physicians clean their hands? Insights from a covert observational study [published online ahead of print July 5, 2016]. J Hosp Med.
Clinical Question: Does direct observation underestimate physician compliance with hand hygiene (HH) compared to other professional groups due to the Hawthorne effect?
Background: Although it is well-known that HH is imperative to infection control, physician compliance remains suboptimal and is often reported to be below that of nurses. The Hawthorne effect may be contributing to this perceived difference because nurses, who work on the same unit consistently, may more readily recognize hospital auditors.
Study Design: Observational.
Setting: 800-bed acute-care academic hospital in Canada.
Synopsis: Two students were trained to covertly observe physician and nursing HH compliance on inpatient units. For two months, students rotated units every week to minimize risk of discovery. Their findings were compared with data gathered by hospital auditors over the same time period.
Covertly observed HH compliance was 50% (799/1,597 opportunities) compared with 83.7% (2,769/3,309) reported by hospital auditors (P<0.0002). The difference in physician compliance was 19% (73.2% compliance with overt observation versus 54.2% with covert observation). The difference was much higher for nurses at 40.7% (85.8% compliance with overt observation versus 45.1% with covert observation). Attending physician behaviors heavily influenced team behaviors—79.5% of trainees were compliant if their attending was compliant compared with 18.9% if attending was not (P<0.0002).
Bottom Line: Traditional HH audit findings that physicians are less compliant than nurses may be at least partially due to the Hawthorne effect. Nonetheless, all healthcare providers have substantial room for improvement, and attending physicians are powerful role models to effect this change.
Citation: Kovacs-Litman A, Wong K, Shojania KJ, Callery S, Vearncombe M, Leis J. Do physicians clean their hands? Insights from a covert observational study [published online ahead of print July 5, 2016]. J Hosp Med.
Long-Term Mortality in Nondiabetic Patients Favors Coronary Artery Bypass Over Intervention with Drug-Eluting Stents
Clinical Question: Is there a mortality difference in nondiabetic patients with multivessel coronary artery disease (CAD) treated with coronary artery bypass graft (CABG) versus percutaneous coronary intervention (PCI)?
Background: Randomized clinical trials have shown a mortality benefit of CABG over PCI with drug-eluting stents (DES) for diabetic patients. The best strategy for nondiabetics, however, has not been well established.
Study Design: Pooled individual patient data from two large randomized clinical trials.
Setting: Multicenter, multinational (Europe, United States, Asia).
Synopsis: Excluding patients with left main disease, a total of 1,275 nondiabetic patients with two- or three-vessel CAD were analyzed. After median follow-up of 61 months, the CABG group had significantly fewer deaths from any cause (hazard ratio [HR], 0.65; 95% CI, 0.43–0.98; P=0.039) as well as fewer deaths from cardiac causes (HR, 0.41; 95% CI, 0.25–0.78; P=0.005) when compared to PCI with DES. The benefit was primarily seen at five-year follow-up in patients with intermediate to severe disease, with a nonsignificant difference detected in patients with less severe disease.
Despite the increasing popularity of DES, this study suggests that for nondiabetic patients with CAD, there is a mortality benefit at five years favoring CABG over PCI with DES. However, in this study stents used for PCI included both older and newer generation DES; a study using only newer DES may reduce the differences in outcomes between the groups.
Bottom Line: Five-year mortality is lower in nondiabetic patients with multivessel CAD treated with CABG compared with PCI with DES.
Citation: Chang M, Ahn JM, Lee CW, et al. Long-term mortality after coronary revascularization in nondiabetic patients with multivessel disease. J Am Coll Cardiol. 2016;68(1):29-36.
Clinical Question: Is there a mortality difference in nondiabetic patients with multivessel coronary artery disease (CAD) treated with coronary artery bypass graft (CABG) versus percutaneous coronary intervention (PCI)?
Background: Randomized clinical trials have shown a mortality benefit of CABG over PCI with drug-eluting stents (DES) for diabetic patients. The best strategy for nondiabetics, however, has not been well established.
Study Design: Pooled individual patient data from two large randomized clinical trials.
Setting: Multicenter, multinational (Europe, United States, Asia).
Synopsis: Excluding patients with left main disease, a total of 1,275 nondiabetic patients with two- or three-vessel CAD were analyzed. After median follow-up of 61 months, the CABG group had significantly fewer deaths from any cause (hazard ratio [HR], 0.65; 95% CI, 0.43–0.98; P=0.039) as well as fewer deaths from cardiac causes (HR, 0.41; 95% CI, 0.25–0.78; P=0.005) when compared to PCI with DES. The benefit was primarily seen at five-year follow-up in patients with intermediate to severe disease, with a nonsignificant difference detected in patients with less severe disease.
Despite the increasing popularity of DES, this study suggests that for nondiabetic patients with CAD, there is a mortality benefit at five years favoring CABG over PCI with DES. However, in this study stents used for PCI included both older and newer generation DES; a study using only newer DES may reduce the differences in outcomes between the groups.
Bottom Line: Five-year mortality is lower in nondiabetic patients with multivessel CAD treated with CABG compared with PCI with DES.
Citation: Chang M, Ahn JM, Lee CW, et al. Long-term mortality after coronary revascularization in nondiabetic patients with multivessel disease. J Am Coll Cardiol. 2016;68(1):29-36.
Clinical Question: Is there a mortality difference in nondiabetic patients with multivessel coronary artery disease (CAD) treated with coronary artery bypass graft (CABG) versus percutaneous coronary intervention (PCI)?
Background: Randomized clinical trials have shown a mortality benefit of CABG over PCI with drug-eluting stents (DES) for diabetic patients. The best strategy for nondiabetics, however, has not been well established.
Study Design: Pooled individual patient data from two large randomized clinical trials.
Setting: Multicenter, multinational (Europe, United States, Asia).
Synopsis: Excluding patients with left main disease, a total of 1,275 nondiabetic patients with two- or three-vessel CAD were analyzed. After median follow-up of 61 months, the CABG group had significantly fewer deaths from any cause (hazard ratio [HR], 0.65; 95% CI, 0.43–0.98; P=0.039) as well as fewer deaths from cardiac causes (HR, 0.41; 95% CI, 0.25–0.78; P=0.005) when compared to PCI with DES. The benefit was primarily seen at five-year follow-up in patients with intermediate to severe disease, with a nonsignificant difference detected in patients with less severe disease.
Despite the increasing popularity of DES, this study suggests that for nondiabetic patients with CAD, there is a mortality benefit at five years favoring CABG over PCI with DES. However, in this study stents used for PCI included both older and newer generation DES; a study using only newer DES may reduce the differences in outcomes between the groups.
Bottom Line: Five-year mortality is lower in nondiabetic patients with multivessel CAD treated with CABG compared with PCI with DES.
Citation: Chang M, Ahn JM, Lee CW, et al. Long-term mortality after coronary revascularization in nondiabetic patients with multivessel disease. J Am Coll Cardiol. 2016;68(1):29-36.
Prolonged Ceftaroline Exposure Associated with High Incidence of Neutropenia
Clinical Question: What is the incidence of neutropenia in patients treated with prolonged courses of ceftaroline?
Background: Ceftaroline, a new broad-spectrum cephalosporin antibiotic, is FDA approved for the treatment of skin and soft-tissue infections and community-acquired pneumonia (CAP). Other than a few case reports, previous studies have not assessed the incidence of neutropenia in patients receiving ceftaroline for off-label indications or for prolonged courses.
Study Design: Retrospective chart review.
Setting: Brigham and Women’s Hospital and Massachusetts General Hospital in Boston.
Synopsis: The authors identified 67 patients who received ceftaroline for seven or more consecutive days. Overall, ceftaroline exposure for two or more weeks was associated with a 10%–14% incidence of neutropenia (absolute neutrophil count less than 1,800 cells/mm3), and ceftaroline exposure for three or more weeks was associated with a 21% incidence of neutropenia. Both the mean duration of ceftaroline exposure and the total number of ceftaroline doses were associated with incident neutropenia.
This is the first study to systematically assess the incidence of ceftaroline-associated neutropenia. The data support a correlation between cumulative ceftaroline exposure and neutropenia. Hospitalists managing patients with prolonged courses of ceftaroline should carefully monitor hematologic studies during treatment.
Bottom Line: The overall rate of neutropenia in patients receiving prolonged courses of ceftaroline is significant, and it is associated with duration of ceftaroline exposure and total number of doses received.
Citation: Furtek KJ, Kubiak DW, Barra M, Varughese C, Ashbaugh CD, Koo S. High incidence of neutropenia in patients with prolonged ceftaroline exposure. J Antimicrob Chemother. 2016;71(7):2010-2013.
Short Take
New Guidelines from IDSA/ATS for Patients with Community-Acquired Pneumonia Can Safely Be Implemented for Hospitalized Patients
A multicenter, non-inferiority randomized clinical trial of 312 patients with community-acquired pneumonia (CAP) found that stopping antibiotics after five days was not associated with worse outcomes and may reduce readmissions.
Citation: Uranga A, España PP, Bilbao A, et al. Duration of antibiotic treatment in community-acquired pneumonia: a multicenter randomized clinical trial. JAMA Intern Med. 2016;176(9):1257-1265.
Clinical Question: What is the incidence of neutropenia in patients treated with prolonged courses of ceftaroline?
Background: Ceftaroline, a new broad-spectrum cephalosporin antibiotic, is FDA approved for the treatment of skin and soft-tissue infections and community-acquired pneumonia (CAP). Other than a few case reports, previous studies have not assessed the incidence of neutropenia in patients receiving ceftaroline for off-label indications or for prolonged courses.
Study Design: Retrospective chart review.
Setting: Brigham and Women’s Hospital and Massachusetts General Hospital in Boston.
Synopsis: The authors identified 67 patients who received ceftaroline for seven or more consecutive days. Overall, ceftaroline exposure for two or more weeks was associated with a 10%–14% incidence of neutropenia (absolute neutrophil count less than 1,800 cells/mm3), and ceftaroline exposure for three or more weeks was associated with a 21% incidence of neutropenia. Both the mean duration of ceftaroline exposure and the total number of ceftaroline doses were associated with incident neutropenia.
This is the first study to systematically assess the incidence of ceftaroline-associated neutropenia. The data support a correlation between cumulative ceftaroline exposure and neutropenia. Hospitalists managing patients with prolonged courses of ceftaroline should carefully monitor hematologic studies during treatment.
Bottom Line: The overall rate of neutropenia in patients receiving prolonged courses of ceftaroline is significant, and it is associated with duration of ceftaroline exposure and total number of doses received.
Citation: Furtek KJ, Kubiak DW, Barra M, Varughese C, Ashbaugh CD, Koo S. High incidence of neutropenia in patients with prolonged ceftaroline exposure. J Antimicrob Chemother. 2016;71(7):2010-2013.
Short Take
New Guidelines from IDSA/ATS for Patients with Community-Acquired Pneumonia Can Safely Be Implemented for Hospitalized Patients
A multicenter, non-inferiority randomized clinical trial of 312 patients with community-acquired pneumonia (CAP) found that stopping antibiotics after five days was not associated with worse outcomes and may reduce readmissions.
Citation: Uranga A, España PP, Bilbao A, et al. Duration of antibiotic treatment in community-acquired pneumonia: a multicenter randomized clinical trial. JAMA Intern Med. 2016;176(9):1257-1265.
Clinical Question: What is the incidence of neutropenia in patients treated with prolonged courses of ceftaroline?
Background: Ceftaroline, a new broad-spectrum cephalosporin antibiotic, is FDA approved for the treatment of skin and soft-tissue infections and community-acquired pneumonia (CAP). Other than a few case reports, previous studies have not assessed the incidence of neutropenia in patients receiving ceftaroline for off-label indications or for prolonged courses.
Study Design: Retrospective chart review.
Setting: Brigham and Women’s Hospital and Massachusetts General Hospital in Boston.
Synopsis: The authors identified 67 patients who received ceftaroline for seven or more consecutive days. Overall, ceftaroline exposure for two or more weeks was associated with a 10%–14% incidence of neutropenia (absolute neutrophil count less than 1,800 cells/mm3), and ceftaroline exposure for three or more weeks was associated with a 21% incidence of neutropenia. Both the mean duration of ceftaroline exposure and the total number of ceftaroline doses were associated with incident neutropenia.
This is the first study to systematically assess the incidence of ceftaroline-associated neutropenia. The data support a correlation between cumulative ceftaroline exposure and neutropenia. Hospitalists managing patients with prolonged courses of ceftaroline should carefully monitor hematologic studies during treatment.
Bottom Line: The overall rate of neutropenia in patients receiving prolonged courses of ceftaroline is significant, and it is associated with duration of ceftaroline exposure and total number of doses received.
Citation: Furtek KJ, Kubiak DW, Barra M, Varughese C, Ashbaugh CD, Koo S. High incidence of neutropenia in patients with prolonged ceftaroline exposure. J Antimicrob Chemother. 2016;71(7):2010-2013.
Short Take
New Guidelines from IDSA/ATS for Patients with Community-Acquired Pneumonia Can Safely Be Implemented for Hospitalized Patients
A multicenter, non-inferiority randomized clinical trial of 312 patients with community-acquired pneumonia (CAP) found that stopping antibiotics after five days was not associated with worse outcomes and may reduce readmissions.
Citation: Uranga A, España PP, Bilbao A, et al. Duration of antibiotic treatment in community-acquired pneumonia: a multicenter randomized clinical trial. JAMA Intern Med. 2016;176(9):1257-1265.
How Should a Hospitalized Patient with Newly Diagnosed Cirrhosis Be Evaluated and Managed?
The Case
A 50-year-old man with no known medical history presents with two months of increasing abdominal distension. Exam is notable for scleral icterus, telangiectasias on the upper chest, abdominal distention with a positive fluid wave, and bilateral pitting lower-extremity edema. An abdominal ultrasound shows large ascites and a nodular liver consistent with cirrhosis. How should this patient with newly diagnosed cirrhosis be evaluated and managed?
Background
Cirrhosis is a leading cause of death among people ages 25–64 and associated with a mortality rate of 11.5 per 100,000 people.1 In 2010, 101,000 people were discharged from the hospital with chronic liver disease and cirrhosis as the first-listed diagnosis.2 Given the myriad etiologies and the asymptomatic nature of many of these conditions, hospitalists frequently encounter patients presenting with advanced disease.
Evaluation
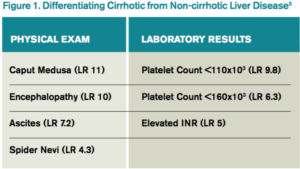
The gold standard for diagnosis is liver biopsy, although this is now usually reserved for atypical cases or where the etiology of cirrhosis is unclear. Alcohol and viral hepatitis (B and C) are the most common causes of chronic liver disease, with nonalcoholic steatohepatitis (NASH) increasing in prevalence. Other less common etiologies and characteristic test findings are listed in Figure 2.
Recently, the Centers for Disease Control and Prevention (CDC) recommended that adults born between 1945 and 1965 receive one-time testing for hepatitis C virus (HCV) infection, regardless of other risk factors, given the higher prevalence in this birth cohort and the introduction of newer oral treatments that achieve sustained virologic response.3
Management
The three classic complications of cirrhosis that will typically prompt inpatient admission are volume overload/ascites, gastrointestinal variceal bleeding, and hepatic encephalopathy.
Volume overload/ascites. Ascites is the most common major complication of cirrhosis, with roughly 50% of patients with asymptomatic cirrhosis developing ascites within 10 years.4 Ascites development portends a poor prognosis, with a mortality of 15% within one year and 44% within five years of diagnosis.4 Patients presenting with new-onset ascites should have a diagnostic paracentesis performed to determine the etiology and evaluate for infection.
Ascitic fluid should be sent for an albumin level and a cell count with differential. A serum-ascites albumin gradient (SAAG) of greater than or equal to 1.1 g/dL is consistent with portal hypertension and cirrhosis, while values less than 1.1 g/dL suggest a non-cirrhotic cause, such as infection or malignancy. Due to the high prevalence of spontaneous bacterial peritonitis (SBP) in hospitalized patients, fluid should also be immediately inoculated in aerobic and anaerobic culture bottles at the bedside, as this has been shown to improve the yield compared to inoculation of culture bottles in the laboratory. Other testing (such as cytology for the evaluation of malignancy) should only be performed if there is significant concern for a particular disease since the vast majority of cases are secondary to uncomplicated cirrhosis.4
In patients with a large amount of ascites and related symptoms (eg, abdominal pain, shortness of breath), therapeutic paracentesis should be performed. Although there is controversy over the need for routine albumin administration, guidelines currently recommend the infusion of 6–8 g of albumin per liter of ascites removed for paracentesis volumes of greater than 4–5 liters.4
No data support the routine administration of fresh frozen plasma (FFP) or platelets prior to paracentesis. Although significant complications of paracentesis (including bowel perforation and hemorrhage) may occur, these are exceedingly rare. Ultrasonography can be used to decrease risks and identify suitable pockets of fluid to tap, even when fluid is not obvious on physical exam alone.5
For patients with significant edema or ascites that is due to portal hypertension (SAAG >1.1 g/dL), the first-line therapy is sodium restriction to less than 2,000 mg/day. Consulting a nutritionist may be beneficial for patient education.
For patients with significant natriuresis (>78 mmol daily urine sodium excretion), dietary restriction alone can manage fluid retention. Most patients (85%–90%), however, require diuretics to increase sodium output. Single-agent spironolactone is more efficacious than single-agent furosemide, but diuresis is improved when both agents are used.4 A dosing regimen of once-daily 40 mg furosemide and 100 mg spironolactone is the recommended starting regimen to promote diuresis while maintaining normokalemia. Due to the long half-life of spironolactone, the dose can be increased every three to five days if needed for diuresis.4
Gastroesophageal variceal bleeding. Approximately 50% of patients with cirrhosis have gastroesophageal varices as a consequence of portal hypertension, with prevalence increasing in those with more severe disease.6 As many patients with cirrhosis have advanced disease at the time of diagnosis, it is recommended that patients be referred for endoscopic screening when diagnosed.6 Nonselective beta-blockers decrease the risk of bleeding in patients with known varices but should not be initiated empirically in all patients with cirrhosis given significant side effects, including worsening of ascites.
There is increasing evidence that there is a “window” period for beta-blocker use in cirrhosis with the window opening after the diagnosis of varices and the window closing at advanced stages of disease (marked by an episode of spontaneous bacterial peritonitis, refractory ascites, or hepatorenal syndrome, for example).7
Hepatic encephalopathy. Hepatic encephalopathy (HE) is another complication of portal hypertension and is seen in 10%–14% of patients at the time of cirrhosis diagnosis.8 Overt HE is estimated to occur in 30%–40% of patients with cirrhosis at some point during their disease course, and more subtle forms (minimal or covert HE) are seen in up to 80%.8 HE can cause numerous neurologic and psychiatric issues including personality changes, poor memory, sleep-wake disturbances, and alterations in consciousness.
In patients with an episode of encephalopathy, precipitating factors should be evaluated. Typical precipitants include infections, bleeding, electrolyte disorders, and constipation. Ammonia levels are frequently drawn as part of the evaluation of hepatic encephalopathy, but elevated levels do not significantly change diagnostic probabilities or add prognostic information.8 A low ammonia level, on the other hand, may be useful in lowering the probability of hepatic encephalopathy in a patient with altered mental status of unknown etiology.8
Routine primary prophylaxis of HE in all patients with cirrhosis is not currently recommended. Treatment is only recommended in patients with overt HE, with secondary prophylaxis administered following an episode due to the high risk for recurrence.
Other Issues
VTE prophylaxis. Although patients with cirrhosis are often presumed to be “auto-anticoagulated” due to an elevated international normalized ratio (INR), they experience thrombotic complications during hospitalization at the same rate or higher than patients with other chronic illnesses.9 Unfortunately, studies examining venous thromboembolism (VTE) prophylaxis in hospitalized patients have generally excluded cirrhotics. Therefore, risks/benefits of prophylaxis need to be considered on an individual basis, taking into account the presence of varices (if known), platelet count, and other VTE risk factors.
Drugs to avoid. As detailed above, nonselective beta-blockers should be avoided when outside the “window” period of benefit. Patients with cirrhosis should be counseled to avoid nonsteroidal anti-inflammatory drugs (NSAIDs) due to an increased risk of bleeding and renal dysfunction. ACE inhibitors (ACE-Is) and angiotensin-receptor blockers (ARBs) can also precipitate renal dysfunction and should generally be avoided unless strongly indicated for another diagnosis.
There is conflicting evidence with regard to whether the use of proton-pump inhibitors (PPIs) in cirrhotics increases the risk of SBP.10,11 Nevertheless, it is prudent to reevaluate the need for PPIs in patients with cirrhosis to determine where a true indication exists.
Post-hospitalization care. Patients with a new diagnosis of cirrhosis require screening for esophageal varices and hepatocellular carcinoma (HCC), with frequency of subsequent testing based on initial results. They should also be immunized against hepatitis A (HAV) and hepatitis B (HBV), if not already immune. Specific treatments are available for many causes of cirrhosis, including new antiviral agents against hepatitis C (HCV), and liver transplantation is an option for select patients. Given the complexity of subsequent diagnostic and treatment options, patients with new cirrhosis should be referred to a gastroenterologist or hepatologist, if possible.
Back to the Case
The patient is hospitalized, and a large-volume paracentesis is performed. Four liters are removed without the administration of albumin. Ascitic fluid analysis reveals a SAAG of greater than 1.1 g/dL and a polymorphonuclear cell count of 50 cell/mm3, suggesting ascites due to portal hypertension and ruling out infection. Nutrition is consulted and educates the patient on a restricted-sodium diet. Furosemide is started at 40 mg daily; spironolactone is started at 100 mg daily. Initial workup and serologies demonstrate active HCV infection (HCV RNA positive), with immunity to HBV due to vaccination. HAV vaccination is administered given lack of seropositivity. The patient is screened for alcohol and found not to drink alcohol. By the time of discharge, the patient is experiencing daily 0.5 kg weight loss due to diuretics and has stable renal function. The patient is referred to outpatient gastroenterology for gastroesophageal variceal screening and consideration of HCV treatment and/or liver transplantation.
Bottom Line
Workup and management of cirrhosis should focus on revealing the underlying etiology, managing complications, and discharging patients with a comprehensive follow-up plan. TH
Dr. Sehgal and Dr. Hanson are hospitalists in the division of hospital medicine at the University of Texas Health Science Center at San Antonio and the South Texas Veterans Health Care System.
References
- Heron M. Deaths: leading causes for 2012. Natl Vital Stat Rep. 2015;64(10):1-93.
- Chronic liver disease and cirrhosis. Centers for Disease Control and Prevention website. Accessed March 17, 2016.
- Smith BD, Morgan RL, Beckett GA, Falck-Ytter Y, Holtzman D, Ward JW. Hepatitis C virus testing of persons born during 1945-1965: recommendations from the Centers for Disease Control and Prevention. Ann Intern Med. 2012;157(11):817-822. doi:10.7326/0003-4819-157-9-201211060-00529.
- Runyon BA, AASLD. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013;57(4):1651-1653. doi:10.1002/hep.26359.
- Udell JA, Wang CS, Tinmouth J, et al. Does this patient with liver disease have cirrhosis? JAMA. 2012;307(8):832-842. doi:10.1001/jama.2012.186.
- Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W, Practice Guidelines Committee of the American Association for the Study of Liver Diseases, Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46(3):922-938. doi:10.1002/hep.21907.
- Mandorfer M, Bota S, Schwabl P, et al. Nonselective β blockers increase risk for hepatorenal syndrome and death in patients with cirrhosis and spontaneous bacterial peritonitis. Gastroenterology. 2014;146(7):1680-90.e1. doi:10.1053/j.gastro.2014.03.005.
- Vilstrup H, Amodio P, Bajaj J, et al. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology. 2014;60(2):715-735. doi:10.1002/hep.27210.
- Khoury T, Ayman AR, Cohen J, Daher S, Shmuel C, Mizrahi M. The complex role of anticoagulation in cirrhosis: an updated review of where we are and where we are going. Digestion. 2016;93(2):149-159. doi:10.1159/000442877.
- Terg R, Casciato P, Garbe C, et al. Proton pump inhibitor therapy does not increase the incidence of spontaneous bacterial peritonitis in cirrhosis: a multicenter prospective study. J Hepatol. 2015;62(5):1056-1060. doi:10.1016/j.jhep.2014.11.036.
- Deshpande A, Pasupuleti V, Thota P, et al. Acid-suppressive therapy is associated with spontaneous bacterial peritonitis in cirrhotic patients: a meta-analysis. J Gastroenterol Hepatol. 2013;28(2):235-242. doi:10.1111/jgh.12065.
Key Points
- Cirrhosis has many etiologies, and new diagnoses require further investigation as to the underlying etiology.
- Initial management should focus on evaluation and treatment of complications, including ascites, esophageal varices, and hepatic encephalopathy.
- A diagnostic paracentesis, salt restriction, and a nutrition consult are the initial therapies for ascites although most patients will also require diuretics to increase sodium excretion.
- Once stabilized, the cirrhotic patient will require specialty care for possible liver biopsy (if etiology remains unclear), treatment (eg, HCV antivirals), and/or referral for liver transplantation.
The Case
A 50-year-old man with no known medical history presents with two months of increasing abdominal distension. Exam is notable for scleral icterus, telangiectasias on the upper chest, abdominal distention with a positive fluid wave, and bilateral pitting lower-extremity edema. An abdominal ultrasound shows large ascites and a nodular liver consistent with cirrhosis. How should this patient with newly diagnosed cirrhosis be evaluated and managed?
Background
Cirrhosis is a leading cause of death among people ages 25–64 and associated with a mortality rate of 11.5 per 100,000 people.1 In 2010, 101,000 people were discharged from the hospital with chronic liver disease and cirrhosis as the first-listed diagnosis.2 Given the myriad etiologies and the asymptomatic nature of many of these conditions, hospitalists frequently encounter patients presenting with advanced disease.
Evaluation
The gold standard for diagnosis is liver biopsy, although this is now usually reserved for atypical cases or where the etiology of cirrhosis is unclear. Alcohol and viral hepatitis (B and C) are the most common causes of chronic liver disease, with nonalcoholic steatohepatitis (NASH) increasing in prevalence. Other less common etiologies and characteristic test findings are listed in Figure 2.
Recently, the Centers for Disease Control and Prevention (CDC) recommended that adults born between 1945 and 1965 receive one-time testing for hepatitis C virus (HCV) infection, regardless of other risk factors, given the higher prevalence in this birth cohort and the introduction of newer oral treatments that achieve sustained virologic response.3
Management
The three classic complications of cirrhosis that will typically prompt inpatient admission are volume overload/ascites, gastrointestinal variceal bleeding, and hepatic encephalopathy.
Volume overload/ascites. Ascites is the most common major complication of cirrhosis, with roughly 50% of patients with asymptomatic cirrhosis developing ascites within 10 years.4 Ascites development portends a poor prognosis, with a mortality of 15% within one year and 44% within five years of diagnosis.4 Patients presenting with new-onset ascites should have a diagnostic paracentesis performed to determine the etiology and evaluate for infection.
Ascitic fluid should be sent for an albumin level and a cell count with differential. A serum-ascites albumin gradient (SAAG) of greater than or equal to 1.1 g/dL is consistent with portal hypertension and cirrhosis, while values less than 1.1 g/dL suggest a non-cirrhotic cause, such as infection or malignancy. Due to the high prevalence of spontaneous bacterial peritonitis (SBP) in hospitalized patients, fluid should also be immediately inoculated in aerobic and anaerobic culture bottles at the bedside, as this has been shown to improve the yield compared to inoculation of culture bottles in the laboratory. Other testing (such as cytology for the evaluation of malignancy) should only be performed if there is significant concern for a particular disease since the vast majority of cases are secondary to uncomplicated cirrhosis.4
In patients with a large amount of ascites and related symptoms (eg, abdominal pain, shortness of breath), therapeutic paracentesis should be performed. Although there is controversy over the need for routine albumin administration, guidelines currently recommend the infusion of 6–8 g of albumin per liter of ascites removed for paracentesis volumes of greater than 4–5 liters.4
No data support the routine administration of fresh frozen plasma (FFP) or platelets prior to paracentesis. Although significant complications of paracentesis (including bowel perforation and hemorrhage) may occur, these are exceedingly rare. Ultrasonography can be used to decrease risks and identify suitable pockets of fluid to tap, even when fluid is not obvious on physical exam alone.5
For patients with significant edema or ascites that is due to portal hypertension (SAAG >1.1 g/dL), the first-line therapy is sodium restriction to less than 2,000 mg/day. Consulting a nutritionist may be beneficial for patient education.
For patients with significant natriuresis (>78 mmol daily urine sodium excretion), dietary restriction alone can manage fluid retention. Most patients (85%–90%), however, require diuretics to increase sodium output. Single-agent spironolactone is more efficacious than single-agent furosemide, but diuresis is improved when both agents are used.4 A dosing regimen of once-daily 40 mg furosemide and 100 mg spironolactone is the recommended starting regimen to promote diuresis while maintaining normokalemia. Due to the long half-life of spironolactone, the dose can be increased every three to five days if needed for diuresis.4
Gastroesophageal variceal bleeding. Approximately 50% of patients with cirrhosis have gastroesophageal varices as a consequence of portal hypertension, with prevalence increasing in those with more severe disease.6 As many patients with cirrhosis have advanced disease at the time of diagnosis, it is recommended that patients be referred for endoscopic screening when diagnosed.6 Nonselective beta-blockers decrease the risk of bleeding in patients with known varices but should not be initiated empirically in all patients with cirrhosis given significant side effects, including worsening of ascites.
There is increasing evidence that there is a “window” period for beta-blocker use in cirrhosis with the window opening after the diagnosis of varices and the window closing at advanced stages of disease (marked by an episode of spontaneous bacterial peritonitis, refractory ascites, or hepatorenal syndrome, for example).7
Hepatic encephalopathy. Hepatic encephalopathy (HE) is another complication of portal hypertension and is seen in 10%–14% of patients at the time of cirrhosis diagnosis.8 Overt HE is estimated to occur in 30%–40% of patients with cirrhosis at some point during their disease course, and more subtle forms (minimal or covert HE) are seen in up to 80%.8 HE can cause numerous neurologic and psychiatric issues including personality changes, poor memory, sleep-wake disturbances, and alterations in consciousness.
In patients with an episode of encephalopathy, precipitating factors should be evaluated. Typical precipitants include infections, bleeding, electrolyte disorders, and constipation. Ammonia levels are frequently drawn as part of the evaluation of hepatic encephalopathy, but elevated levels do not significantly change diagnostic probabilities or add prognostic information.8 A low ammonia level, on the other hand, may be useful in lowering the probability of hepatic encephalopathy in a patient with altered mental status of unknown etiology.8
Routine primary prophylaxis of HE in all patients with cirrhosis is not currently recommended. Treatment is only recommended in patients with overt HE, with secondary prophylaxis administered following an episode due to the high risk for recurrence.
Other Issues
VTE prophylaxis. Although patients with cirrhosis are often presumed to be “auto-anticoagulated” due to an elevated international normalized ratio (INR), they experience thrombotic complications during hospitalization at the same rate or higher than patients with other chronic illnesses.9 Unfortunately, studies examining venous thromboembolism (VTE) prophylaxis in hospitalized patients have generally excluded cirrhotics. Therefore, risks/benefits of prophylaxis need to be considered on an individual basis, taking into account the presence of varices (if known), platelet count, and other VTE risk factors.
Drugs to avoid. As detailed above, nonselective beta-blockers should be avoided when outside the “window” period of benefit. Patients with cirrhosis should be counseled to avoid nonsteroidal anti-inflammatory drugs (NSAIDs) due to an increased risk of bleeding and renal dysfunction. ACE inhibitors (ACE-Is) and angiotensin-receptor blockers (ARBs) can also precipitate renal dysfunction and should generally be avoided unless strongly indicated for another diagnosis.
There is conflicting evidence with regard to whether the use of proton-pump inhibitors (PPIs) in cirrhotics increases the risk of SBP.10,11 Nevertheless, it is prudent to reevaluate the need for PPIs in patients with cirrhosis to determine where a true indication exists.
Post-hospitalization care. Patients with a new diagnosis of cirrhosis require screening for esophageal varices and hepatocellular carcinoma (HCC), with frequency of subsequent testing based on initial results. They should also be immunized against hepatitis A (HAV) and hepatitis B (HBV), if not already immune. Specific treatments are available for many causes of cirrhosis, including new antiviral agents against hepatitis C (HCV), and liver transplantation is an option for select patients. Given the complexity of subsequent diagnostic and treatment options, patients with new cirrhosis should be referred to a gastroenterologist or hepatologist, if possible.
Back to the Case
The patient is hospitalized, and a large-volume paracentesis is performed. Four liters are removed without the administration of albumin. Ascitic fluid analysis reveals a SAAG of greater than 1.1 g/dL and a polymorphonuclear cell count of 50 cell/mm3, suggesting ascites due to portal hypertension and ruling out infection. Nutrition is consulted and educates the patient on a restricted-sodium diet. Furosemide is started at 40 mg daily; spironolactone is started at 100 mg daily. Initial workup and serologies demonstrate active HCV infection (HCV RNA positive), with immunity to HBV due to vaccination. HAV vaccination is administered given lack of seropositivity. The patient is screened for alcohol and found not to drink alcohol. By the time of discharge, the patient is experiencing daily 0.5 kg weight loss due to diuretics and has stable renal function. The patient is referred to outpatient gastroenterology for gastroesophageal variceal screening and consideration of HCV treatment and/or liver transplantation.
Bottom Line
Workup and management of cirrhosis should focus on revealing the underlying etiology, managing complications, and discharging patients with a comprehensive follow-up plan. TH
Dr. Sehgal and Dr. Hanson are hospitalists in the division of hospital medicine at the University of Texas Health Science Center at San Antonio and the South Texas Veterans Health Care System.
References
- Heron M. Deaths: leading causes for 2012. Natl Vital Stat Rep. 2015;64(10):1-93.
- Chronic liver disease and cirrhosis. Centers for Disease Control and Prevention website. Accessed March 17, 2016.
- Smith BD, Morgan RL, Beckett GA, Falck-Ytter Y, Holtzman D, Ward JW. Hepatitis C virus testing of persons born during 1945-1965: recommendations from the Centers for Disease Control and Prevention. Ann Intern Med. 2012;157(11):817-822. doi:10.7326/0003-4819-157-9-201211060-00529.
- Runyon BA, AASLD. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013;57(4):1651-1653. doi:10.1002/hep.26359.
- Udell JA, Wang CS, Tinmouth J, et al. Does this patient with liver disease have cirrhosis? JAMA. 2012;307(8):832-842. doi:10.1001/jama.2012.186.
- Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W, Practice Guidelines Committee of the American Association for the Study of Liver Diseases, Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46(3):922-938. doi:10.1002/hep.21907.
- Mandorfer M, Bota S, Schwabl P, et al. Nonselective β blockers increase risk for hepatorenal syndrome and death in patients with cirrhosis and spontaneous bacterial peritonitis. Gastroenterology. 2014;146(7):1680-90.e1. doi:10.1053/j.gastro.2014.03.005.
- Vilstrup H, Amodio P, Bajaj J, et al. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology. 2014;60(2):715-735. doi:10.1002/hep.27210.
- Khoury T, Ayman AR, Cohen J, Daher S, Shmuel C, Mizrahi M. The complex role of anticoagulation in cirrhosis: an updated review of where we are and where we are going. Digestion. 2016;93(2):149-159. doi:10.1159/000442877.
- Terg R, Casciato P, Garbe C, et al. Proton pump inhibitor therapy does not increase the incidence of spontaneous bacterial peritonitis in cirrhosis: a multicenter prospective study. J Hepatol. 2015;62(5):1056-1060. doi:10.1016/j.jhep.2014.11.036.
- Deshpande A, Pasupuleti V, Thota P, et al. Acid-suppressive therapy is associated with spontaneous bacterial peritonitis in cirrhotic patients: a meta-analysis. J Gastroenterol Hepatol. 2013;28(2):235-242. doi:10.1111/jgh.12065.
Key Points
- Cirrhosis has many etiologies, and new diagnoses require further investigation as to the underlying etiology.
- Initial management should focus on evaluation and treatment of complications, including ascites, esophageal varices, and hepatic encephalopathy.
- A diagnostic paracentesis, salt restriction, and a nutrition consult are the initial therapies for ascites although most patients will also require diuretics to increase sodium excretion.
- Once stabilized, the cirrhotic patient will require specialty care for possible liver biopsy (if etiology remains unclear), treatment (eg, HCV antivirals), and/or referral for liver transplantation.
The Case
A 50-year-old man with no known medical history presents with two months of increasing abdominal distension. Exam is notable for scleral icterus, telangiectasias on the upper chest, abdominal distention with a positive fluid wave, and bilateral pitting lower-extremity edema. An abdominal ultrasound shows large ascites and a nodular liver consistent with cirrhosis. How should this patient with newly diagnosed cirrhosis be evaluated and managed?
Background
Cirrhosis is a leading cause of death among people ages 25–64 and associated with a mortality rate of 11.5 per 100,000 people.1 In 2010, 101,000 people were discharged from the hospital with chronic liver disease and cirrhosis as the first-listed diagnosis.2 Given the myriad etiologies and the asymptomatic nature of many of these conditions, hospitalists frequently encounter patients presenting with advanced disease.
Evaluation
The gold standard for diagnosis is liver biopsy, although this is now usually reserved for atypical cases or where the etiology of cirrhosis is unclear. Alcohol and viral hepatitis (B and C) are the most common causes of chronic liver disease, with nonalcoholic steatohepatitis (NASH) increasing in prevalence. Other less common etiologies and characteristic test findings are listed in Figure 2.
Recently, the Centers for Disease Control and Prevention (CDC) recommended that adults born between 1945 and 1965 receive one-time testing for hepatitis C virus (HCV) infection, regardless of other risk factors, given the higher prevalence in this birth cohort and the introduction of newer oral treatments that achieve sustained virologic response.3
Management
The three classic complications of cirrhosis that will typically prompt inpatient admission are volume overload/ascites, gastrointestinal variceal bleeding, and hepatic encephalopathy.
Volume overload/ascites. Ascites is the most common major complication of cirrhosis, with roughly 50% of patients with asymptomatic cirrhosis developing ascites within 10 years.4 Ascites development portends a poor prognosis, with a mortality of 15% within one year and 44% within five years of diagnosis.4 Patients presenting with new-onset ascites should have a diagnostic paracentesis performed to determine the etiology and evaluate for infection.
Ascitic fluid should be sent for an albumin level and a cell count with differential. A serum-ascites albumin gradient (SAAG) of greater than or equal to 1.1 g/dL is consistent with portal hypertension and cirrhosis, while values less than 1.1 g/dL suggest a non-cirrhotic cause, such as infection or malignancy. Due to the high prevalence of spontaneous bacterial peritonitis (SBP) in hospitalized patients, fluid should also be immediately inoculated in aerobic and anaerobic culture bottles at the bedside, as this has been shown to improve the yield compared to inoculation of culture bottles in the laboratory. Other testing (such as cytology for the evaluation of malignancy) should only be performed if there is significant concern for a particular disease since the vast majority of cases are secondary to uncomplicated cirrhosis.4
In patients with a large amount of ascites and related symptoms (eg, abdominal pain, shortness of breath), therapeutic paracentesis should be performed. Although there is controversy over the need for routine albumin administration, guidelines currently recommend the infusion of 6–8 g of albumin per liter of ascites removed for paracentesis volumes of greater than 4–5 liters.4
No data support the routine administration of fresh frozen plasma (FFP) or platelets prior to paracentesis. Although significant complications of paracentesis (including bowel perforation and hemorrhage) may occur, these are exceedingly rare. Ultrasonography can be used to decrease risks and identify suitable pockets of fluid to tap, even when fluid is not obvious on physical exam alone.5
For patients with significant edema or ascites that is due to portal hypertension (SAAG >1.1 g/dL), the first-line therapy is sodium restriction to less than 2,000 mg/day. Consulting a nutritionist may be beneficial for patient education.
For patients with significant natriuresis (>78 mmol daily urine sodium excretion), dietary restriction alone can manage fluid retention. Most patients (85%–90%), however, require diuretics to increase sodium output. Single-agent spironolactone is more efficacious than single-agent furosemide, but diuresis is improved when both agents are used.4 A dosing regimen of once-daily 40 mg furosemide and 100 mg spironolactone is the recommended starting regimen to promote diuresis while maintaining normokalemia. Due to the long half-life of spironolactone, the dose can be increased every three to five days if needed for diuresis.4
Gastroesophageal variceal bleeding. Approximately 50% of patients with cirrhosis have gastroesophageal varices as a consequence of portal hypertension, with prevalence increasing in those with more severe disease.6 As many patients with cirrhosis have advanced disease at the time of diagnosis, it is recommended that patients be referred for endoscopic screening when diagnosed.6 Nonselective beta-blockers decrease the risk of bleeding in patients with known varices but should not be initiated empirically in all patients with cirrhosis given significant side effects, including worsening of ascites.
There is increasing evidence that there is a “window” period for beta-blocker use in cirrhosis with the window opening after the diagnosis of varices and the window closing at advanced stages of disease (marked by an episode of spontaneous bacterial peritonitis, refractory ascites, or hepatorenal syndrome, for example).7
Hepatic encephalopathy. Hepatic encephalopathy (HE) is another complication of portal hypertension and is seen in 10%–14% of patients at the time of cirrhosis diagnosis.8 Overt HE is estimated to occur in 30%–40% of patients with cirrhosis at some point during their disease course, and more subtle forms (minimal or covert HE) are seen in up to 80%.8 HE can cause numerous neurologic and psychiatric issues including personality changes, poor memory, sleep-wake disturbances, and alterations in consciousness.
In patients with an episode of encephalopathy, precipitating factors should be evaluated. Typical precipitants include infections, bleeding, electrolyte disorders, and constipation. Ammonia levels are frequently drawn as part of the evaluation of hepatic encephalopathy, but elevated levels do not significantly change diagnostic probabilities or add prognostic information.8 A low ammonia level, on the other hand, may be useful in lowering the probability of hepatic encephalopathy in a patient with altered mental status of unknown etiology.8
Routine primary prophylaxis of HE in all patients with cirrhosis is not currently recommended. Treatment is only recommended in patients with overt HE, with secondary prophylaxis administered following an episode due to the high risk for recurrence.
Other Issues
VTE prophylaxis. Although patients with cirrhosis are often presumed to be “auto-anticoagulated” due to an elevated international normalized ratio (INR), they experience thrombotic complications during hospitalization at the same rate or higher than patients with other chronic illnesses.9 Unfortunately, studies examining venous thromboembolism (VTE) prophylaxis in hospitalized patients have generally excluded cirrhotics. Therefore, risks/benefits of prophylaxis need to be considered on an individual basis, taking into account the presence of varices (if known), platelet count, and other VTE risk factors.
Drugs to avoid. As detailed above, nonselective beta-blockers should be avoided when outside the “window” period of benefit. Patients with cirrhosis should be counseled to avoid nonsteroidal anti-inflammatory drugs (NSAIDs) due to an increased risk of bleeding and renal dysfunction. ACE inhibitors (ACE-Is) and angiotensin-receptor blockers (ARBs) can also precipitate renal dysfunction and should generally be avoided unless strongly indicated for another diagnosis.
There is conflicting evidence with regard to whether the use of proton-pump inhibitors (PPIs) in cirrhotics increases the risk of SBP.10,11 Nevertheless, it is prudent to reevaluate the need for PPIs in patients with cirrhosis to determine where a true indication exists.
Post-hospitalization care. Patients with a new diagnosis of cirrhosis require screening for esophageal varices and hepatocellular carcinoma (HCC), with frequency of subsequent testing based on initial results. They should also be immunized against hepatitis A (HAV) and hepatitis B (HBV), if not already immune. Specific treatments are available for many causes of cirrhosis, including new antiviral agents against hepatitis C (HCV), and liver transplantation is an option for select patients. Given the complexity of subsequent diagnostic and treatment options, patients with new cirrhosis should be referred to a gastroenterologist or hepatologist, if possible.
Back to the Case
The patient is hospitalized, and a large-volume paracentesis is performed. Four liters are removed without the administration of albumin. Ascitic fluid analysis reveals a SAAG of greater than 1.1 g/dL and a polymorphonuclear cell count of 50 cell/mm3, suggesting ascites due to portal hypertension and ruling out infection. Nutrition is consulted and educates the patient on a restricted-sodium diet. Furosemide is started at 40 mg daily; spironolactone is started at 100 mg daily. Initial workup and serologies demonstrate active HCV infection (HCV RNA positive), with immunity to HBV due to vaccination. HAV vaccination is administered given lack of seropositivity. The patient is screened for alcohol and found not to drink alcohol. By the time of discharge, the patient is experiencing daily 0.5 kg weight loss due to diuretics and has stable renal function. The patient is referred to outpatient gastroenterology for gastroesophageal variceal screening and consideration of HCV treatment and/or liver transplantation.
Bottom Line
Workup and management of cirrhosis should focus on revealing the underlying etiology, managing complications, and discharging patients with a comprehensive follow-up plan. TH
Dr. Sehgal and Dr. Hanson are hospitalists in the division of hospital medicine at the University of Texas Health Science Center at San Antonio and the South Texas Veterans Health Care System.
References
- Heron M. Deaths: leading causes for 2012. Natl Vital Stat Rep. 2015;64(10):1-93.
- Chronic liver disease and cirrhosis. Centers for Disease Control and Prevention website. Accessed March 17, 2016.
- Smith BD, Morgan RL, Beckett GA, Falck-Ytter Y, Holtzman D, Ward JW. Hepatitis C virus testing of persons born during 1945-1965: recommendations from the Centers for Disease Control and Prevention. Ann Intern Med. 2012;157(11):817-822. doi:10.7326/0003-4819-157-9-201211060-00529.
- Runyon BA, AASLD. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013;57(4):1651-1653. doi:10.1002/hep.26359.
- Udell JA, Wang CS, Tinmouth J, et al. Does this patient with liver disease have cirrhosis? JAMA. 2012;307(8):832-842. doi:10.1001/jama.2012.186.
- Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W, Practice Guidelines Committee of the American Association for the Study of Liver Diseases, Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46(3):922-938. doi:10.1002/hep.21907.
- Mandorfer M, Bota S, Schwabl P, et al. Nonselective β blockers increase risk for hepatorenal syndrome and death in patients with cirrhosis and spontaneous bacterial peritonitis. Gastroenterology. 2014;146(7):1680-90.e1. doi:10.1053/j.gastro.2014.03.005.
- Vilstrup H, Amodio P, Bajaj J, et al. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology. 2014;60(2):715-735. doi:10.1002/hep.27210.
- Khoury T, Ayman AR, Cohen J, Daher S, Shmuel C, Mizrahi M. The complex role of anticoagulation in cirrhosis: an updated review of where we are and where we are going. Digestion. 2016;93(2):149-159. doi:10.1159/000442877.
- Terg R, Casciato P, Garbe C, et al. Proton pump inhibitor therapy does not increase the incidence of spontaneous bacterial peritonitis in cirrhosis: a multicenter prospective study. J Hepatol. 2015;62(5):1056-1060. doi:10.1016/j.jhep.2014.11.036.
- Deshpande A, Pasupuleti V, Thota P, et al. Acid-suppressive therapy is associated with spontaneous bacterial peritonitis in cirrhotic patients: a meta-analysis. J Gastroenterol Hepatol. 2013;28(2):235-242. doi:10.1111/jgh.12065.
Key Points
- Cirrhosis has many etiologies, and new diagnoses require further investigation as to the underlying etiology.
- Initial management should focus on evaluation and treatment of complications, including ascites, esophageal varices, and hepatic encephalopathy.
- A diagnostic paracentesis, salt restriction, and a nutrition consult are the initial therapies for ascites although most patients will also require diuretics to increase sodium excretion.
- Once stabilized, the cirrhotic patient will require specialty care for possible liver biopsy (if etiology remains unclear), treatment (eg, HCV antivirals), and/or referral for liver transplantation.