User login
FDA: Don't Give Revatio to Children With PAH
The Food and Drug Administration is warning physicians not to use off-label Revatio (sildenafil) to treat pulmonary arterial hypertension in children younger than 18 years.
The FDA made the announcement after a pediatric trial revealed high doses of Revatio increased mortality, and low doses failed to improve exercise ability among young PAH patients.
Revatio is a phosphodiesterase-5 inhibitor approved by the FDA to improve exercise ability and delay the progression of PAH in adults. However, the drug is not approved for treatment in children.
Results from a recent randomized, controlled study of Revatio use in 234 children aged 1-17 years with mild to moderate PAH demonstrated that low doses of the drug didn’t improve patients’ exercise ability. In addition, the mortality rate among children taking high doses of Revatio was 3.5 times greater than that of children taking low doses, a statistically significant difference.
The FDA has added a warning to Revatio’s labeling stating that the drug is not recommended for pediatric patients. The agency also has required the drug’s manufacturer, Pfizer, to evaluate Revatio’s mortality risk in adults.
Physicians can report adverse side effects involving Revatio to the FDA MedWatch program.
The Food and Drug Administration is warning physicians not to use off-label Revatio (sildenafil) to treat pulmonary arterial hypertension in children younger than 18 years.
The FDA made the announcement after a pediatric trial revealed high doses of Revatio increased mortality, and low doses failed to improve exercise ability among young PAH patients.
Revatio is a phosphodiesterase-5 inhibitor approved by the FDA to improve exercise ability and delay the progression of PAH in adults. However, the drug is not approved for treatment in children.
Results from a recent randomized, controlled study of Revatio use in 234 children aged 1-17 years with mild to moderate PAH demonstrated that low doses of the drug didn’t improve patients’ exercise ability. In addition, the mortality rate among children taking high doses of Revatio was 3.5 times greater than that of children taking low doses, a statistically significant difference.
The FDA has added a warning to Revatio’s labeling stating that the drug is not recommended for pediatric patients. The agency also has required the drug’s manufacturer, Pfizer, to evaluate Revatio’s mortality risk in adults.
Physicians can report adverse side effects involving Revatio to the FDA MedWatch program.
The Food and Drug Administration is warning physicians not to use off-label Revatio (sildenafil) to treat pulmonary arterial hypertension in children younger than 18 years.
The FDA made the announcement after a pediatric trial revealed high doses of Revatio increased mortality, and low doses failed to improve exercise ability among young PAH patients.
Revatio is a phosphodiesterase-5 inhibitor approved by the FDA to improve exercise ability and delay the progression of PAH in adults. However, the drug is not approved for treatment in children.
Results from a recent randomized, controlled study of Revatio use in 234 children aged 1-17 years with mild to moderate PAH demonstrated that low doses of the drug didn’t improve patients’ exercise ability. In addition, the mortality rate among children taking high doses of Revatio was 3.5 times greater than that of children taking low doses, a statistically significant difference.
The FDA has added a warning to Revatio’s labeling stating that the drug is not recommended for pediatric patients. The agency also has required the drug’s manufacturer, Pfizer, to evaluate Revatio’s mortality risk in adults.
Physicians can report adverse side effects involving Revatio to the FDA MedWatch program.
Docs See Slight Raise; Revenues Fall for Groups
Nearly 80% of physicians saw a modest increase in compensation in 2011, with a 4% average increase for primary care and 2.8% for specialists, according to findings from the American Medical Groups Association’s 2012 Medical Group Compensation and Financial Survey. Hospitalists saw a 3.1% raise.
The most significant pay increases were for hematology & medical oncology (7.1%), hypertension and nephrology (6.9%), urgent care (5.2%) and family medicine (5.1%). Despite the increases, provider organizations across the country saw operating revenues run in the red, with a national average margin of -$1,235 per physician. Donald Fisher, Ph.D, president and CEO of AMGA, said the findings provide further evidence to support the campaign to reform physician reimbursement.
"AMGA continues to advocate for changes in the Medicare reimbursement system, including a shift from volume-based to value-base payment models," he said in a statement.
Additional findings showed a slight decrease in relative value units (RVUs, –.5% on average). However, that decrease is normal, according to Brad Vaudrey, a principal with Sullivan, Cotter, and Assoc., an independent consulting firm specializing in physician compensation.
"It is fairly typical to see only small changes annually to the RVU numbers so an overall -.5% is not alarming, it just indicates overall physicians continue to maintain the work effort level," Mr. Vaudrey said in an interview. "We are watching so see if the implementation of [electronic medical records], medical home, push for quality, and other factors that may change the role of the [physician] will have an impact on the RVU output." Hospitalists were among the group who had a slight increase of 2.8% in RVUs.
The survey was conducted by Sullivan, Cotter. Data were collected from 225 medical groups, representing 55,800 physicians. Of the 178 medical groups responding to a survey question about type of ownership, 68 (38%) said they were physician owned. An additional 53% of respondents reported being with a health system or a hospital, as compared with 51% in 2010.
Nearly 80% of physicians saw a modest increase in compensation in 2011, with a 4% average increase for primary care and 2.8% for specialists, according to findings from the American Medical Groups Association’s 2012 Medical Group Compensation and Financial Survey. Hospitalists saw a 3.1% raise.
The most significant pay increases were for hematology & medical oncology (7.1%), hypertension and nephrology (6.9%), urgent care (5.2%) and family medicine (5.1%). Despite the increases, provider organizations across the country saw operating revenues run in the red, with a national average margin of -$1,235 per physician. Donald Fisher, Ph.D, president and CEO of AMGA, said the findings provide further evidence to support the campaign to reform physician reimbursement.
"AMGA continues to advocate for changes in the Medicare reimbursement system, including a shift from volume-based to value-base payment models," he said in a statement.
Additional findings showed a slight decrease in relative value units (RVUs, –.5% on average). However, that decrease is normal, according to Brad Vaudrey, a principal with Sullivan, Cotter, and Assoc., an independent consulting firm specializing in physician compensation.
"It is fairly typical to see only small changes annually to the RVU numbers so an overall -.5% is not alarming, it just indicates overall physicians continue to maintain the work effort level," Mr. Vaudrey said in an interview. "We are watching so see if the implementation of [electronic medical records], medical home, push for quality, and other factors that may change the role of the [physician] will have an impact on the RVU output." Hospitalists were among the group who had a slight increase of 2.8% in RVUs.
The survey was conducted by Sullivan, Cotter. Data were collected from 225 medical groups, representing 55,800 physicians. Of the 178 medical groups responding to a survey question about type of ownership, 68 (38%) said they were physician owned. An additional 53% of respondents reported being with a health system or a hospital, as compared with 51% in 2010.
Nearly 80% of physicians saw a modest increase in compensation in 2011, with a 4% average increase for primary care and 2.8% for specialists, according to findings from the American Medical Groups Association’s 2012 Medical Group Compensation and Financial Survey. Hospitalists saw a 3.1% raise.
The most significant pay increases were for hematology & medical oncology (7.1%), hypertension and nephrology (6.9%), urgent care (5.2%) and family medicine (5.1%). Despite the increases, provider organizations across the country saw operating revenues run in the red, with a national average margin of -$1,235 per physician. Donald Fisher, Ph.D, president and CEO of AMGA, said the findings provide further evidence to support the campaign to reform physician reimbursement.
"AMGA continues to advocate for changes in the Medicare reimbursement system, including a shift from volume-based to value-base payment models," he said in a statement.
Additional findings showed a slight decrease in relative value units (RVUs, –.5% on average). However, that decrease is normal, according to Brad Vaudrey, a principal with Sullivan, Cotter, and Assoc., an independent consulting firm specializing in physician compensation.
"It is fairly typical to see only small changes annually to the RVU numbers so an overall -.5% is not alarming, it just indicates overall physicians continue to maintain the work effort level," Mr. Vaudrey said in an interview. "We are watching so see if the implementation of [electronic medical records], medical home, push for quality, and other factors that may change the role of the [physician] will have an impact on the RVU output." Hospitalists were among the group who had a slight increase of 2.8% in RVUs.
The survey was conducted by Sullivan, Cotter. Data were collected from 225 medical groups, representing 55,800 physicians. Of the 178 medical groups responding to a survey question about type of ownership, 68 (38%) said they were physician owned. An additional 53% of respondents reported being with a health system or a hospital, as compared with 51% in 2010.
FROM A SURVEY BY THE AMERICAN MEDICAL GROUP ASSOCIATION
Major Finding: Nearly 80% of physicians saw a modest increase in compensation in 2011, with a 4% average increase for primary care and 2.8% for specialists
Data Source: A nationwide survey of 225 medical groups, representing 55,800 physicians across the nation
Disclosures: The sponsor of study, Sullivan, Cotter, and Assoc., had no relevant financial disclosures.
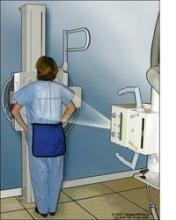
FDA Recommends X-Ray for ICD Patients With Riata Leads
The Food and Drug Administration is recommending that all patients with implanted cardioverter defibrillators or cardiac resynchronization therapy defibrillators with Riata or Riata ST leads get an x-ray to check for abnormalities. St. Jude Medical voluntarily recalled those leads in November 2011 after reports of insulation failure or premature erosion of the insulation surrounding the electrical conductor wires. While the company stopped selling the Riata leads in 2010, they estimate that 79,000 leads are still implanted in patients across the country.
The leads, which connect the defibrillator to the heart to monitor its rhythms, are typically made with layers of insulation around them to protect the electrical wiring within the lead. However, insulation failure can cause inappropriate impulses, no impulses at all, or life-threatening abnormal heart beats. The FDA is ordering St. Jude Medical to conduct 3-year postmarket surveillance studies to learn more about what patients and physicians should expect.
"The majority of Riata and Riata ST leads, including those that show signs of electrical conductor migration or externalization, continue to function normally and provide life-saving support for patients," said Dr. Jeffrey Shuren, director of FDA’s Center for Devices and Radiology Health, in a statement. However, "The agency does not have enough information to determine the frequency and timing of insulation failure in these leads; therefore, the postmarket surveillance studies will ensure that health care professionals and patients get the data they need to better guide clinical management decisions."
The postmarket studies will address issues including the timing of lead insulation failure, serious side effects associated with treatment for malfunctioning leads, and whether the insulation failure can be detected with an x-ray.
St. Jude Medical has also voluntarily recalled two other sets of leads, QuickSite LV CRT leads and QuickFlex LV CRT leads, because of insulation abrasion. CRT leads are battery-powered units implanted in patients with heart failure to keep the left and right sides of the heart beating in unison. Like the Riata leads, CRT leads are insulated to monitor health rhythm and deliver electrical impulses.
The Food and Drug Administration is recommending that all patients with implanted cardioverter defibrillators or cardiac resynchronization therapy defibrillators with Riata or Riata ST leads get an x-ray to check for abnormalities. St. Jude Medical voluntarily recalled those leads in November 2011 after reports of insulation failure or premature erosion of the insulation surrounding the electrical conductor wires. While the company stopped selling the Riata leads in 2010, they estimate that 79,000 leads are still implanted in patients across the country.
The leads, which connect the defibrillator to the heart to monitor its rhythms, are typically made with layers of insulation around them to protect the electrical wiring within the lead. However, insulation failure can cause inappropriate impulses, no impulses at all, or life-threatening abnormal heart beats. The FDA is ordering St. Jude Medical to conduct 3-year postmarket surveillance studies to learn more about what patients and physicians should expect.
"The majority of Riata and Riata ST leads, including those that show signs of electrical conductor migration or externalization, continue to function normally and provide life-saving support for patients," said Dr. Jeffrey Shuren, director of FDA’s Center for Devices and Radiology Health, in a statement. However, "The agency does not have enough information to determine the frequency and timing of insulation failure in these leads; therefore, the postmarket surveillance studies will ensure that health care professionals and patients get the data they need to better guide clinical management decisions."
The postmarket studies will address issues including the timing of lead insulation failure, serious side effects associated with treatment for malfunctioning leads, and whether the insulation failure can be detected with an x-ray.
St. Jude Medical has also voluntarily recalled two other sets of leads, QuickSite LV CRT leads and QuickFlex LV CRT leads, because of insulation abrasion. CRT leads are battery-powered units implanted in patients with heart failure to keep the left and right sides of the heart beating in unison. Like the Riata leads, CRT leads are insulated to monitor health rhythm and deliver electrical impulses.
The Food and Drug Administration is recommending that all patients with implanted cardioverter defibrillators or cardiac resynchronization therapy defibrillators with Riata or Riata ST leads get an x-ray to check for abnormalities. St. Jude Medical voluntarily recalled those leads in November 2011 after reports of insulation failure or premature erosion of the insulation surrounding the electrical conductor wires. While the company stopped selling the Riata leads in 2010, they estimate that 79,000 leads are still implanted in patients across the country.
The leads, which connect the defibrillator to the heart to monitor its rhythms, are typically made with layers of insulation around them to protect the electrical wiring within the lead. However, insulation failure can cause inappropriate impulses, no impulses at all, or life-threatening abnormal heart beats. The FDA is ordering St. Jude Medical to conduct 3-year postmarket surveillance studies to learn more about what patients and physicians should expect.
"The majority of Riata and Riata ST leads, including those that show signs of electrical conductor migration or externalization, continue to function normally and provide life-saving support for patients," said Dr. Jeffrey Shuren, director of FDA’s Center for Devices and Radiology Health, in a statement. However, "The agency does not have enough information to determine the frequency and timing of insulation failure in these leads; therefore, the postmarket surveillance studies will ensure that health care professionals and patients get the data they need to better guide clinical management decisions."
The postmarket studies will address issues including the timing of lead insulation failure, serious side effects associated with treatment for malfunctioning leads, and whether the insulation failure can be detected with an x-ray.
St. Jude Medical has also voluntarily recalled two other sets of leads, QuickSite LV CRT leads and QuickFlex LV CRT leads, because of insulation abrasion. CRT leads are battery-powered units implanted in patients with heart failure to keep the left and right sides of the heart beating in unison. Like the Riata leads, CRT leads are insulated to monitor health rhythm and deliver electrical impulses.
EM Doc Sees Hope in Disney's 'Doc McStuffins'
When the Disney show "Doc McStuffins" premiered this year, Dr. Myiesha Taylor – and her 4-year-old daughter Hana – could not get enough. The show chronicles the life of 6-year-old African American Dottie "Doc" McStuffins, who cures the ouchies, oopsies, and uh-ohs that plague her stuffed animal friends. Dottie McStuffins wants to be a doctor just like her mother. Similarly, Dr. Taylor remembers using play medical equipment and medical records to treat her own stuffed companions.
As one of the first Disney shows to feature an African American female central character, "Doc McStuffins" sends a much-needed message to minority youth, who traditionally lack strong minority role models, said Dr. Taylor, an emergency physician in Fort Worth, Tex.
Children should be taught from an early age that they can do whatever they want to do if they work hard enough, Dr. Taylor said in an interview. "Then, when they’re in sixth grade, they’re already on a trajectory to greatness and they’re not aspiring necessarily to be a rock star [or] an athlete. They know that they can find success if they work hard in this intellectual field of medicine, as opposed to a performing field," she said.
To show her appreciation, Dr. Taylor created a collage of the image of Doc McStuffins surrounded by more than 130 photographs of African American female physicians across the country. She said her collage was her way of thanking Disney for shining a light on the diversity in America.
"In 20 or 30 years, you’ll have a different look in America, so you need to start addressing those issues now, and the way you address it is not intervention in high school. That’s too late," she said.
Dr. Taylor remembers feeling called to medicine at a young age, inspired by her mother and grandmother, who were both nurses. But after her father’s tragic death during the Los Angeles riots in 1992, her calling to emergency medicine became clear. Dwight Taylor died at age 42, just hours after he was transported to an emergency department that did not have a trauma center. Dr. Taylor, then a senior in high school, remembers wanting to make a difference for people in their most desperate hours.
"As I continued in my training, I said, ‘You know, I think that I want to be the type of doctor that can make an immediate change,’ " she recalled. "Motivated by what happened to my father, it just felt like the natural thing for me to go into."
While the kind of family tragedy that inspired Dr. Taylor is thankfully rare, she emphasized that if provided with inspiration from the adults around them, minority children can be drawn to emergency medicine and other medical careers. She added that as the minority population in the United States grows, it’s more important than ever that the physician population reflect the image of the people they serve. And emergency physicians should work to make that a reality in their field.
"Our patients don’t look like our group, so we need to reach out," she said. "I know you can’t just go and pick a doctor off a tree. So, that means that my colleagues need to recognize that it’s important for more students to be ready for medical school ... and then once they’re in medical school, you want to try to recruit them into your specialty so that they don’t all end up in a specialty that is less competitive, for instance, because they just have so many spots."
Embracing diversity is not just about race, but gender as well, Dr. Taylor added. Even a pretend doctor like Doc McStuffins can help children understand that a black woman can be an accomplished physician, she said.
"You need that leading lady to show she’s in charge, she’s the doctor, so that when I walk in to the patients’ rooms, they’re not thinking that it’s weird and I must be the nurse. Or the medical student that’s with me must be the doctor because he’s a man. These types of shows dispel some of those stereotypes and make it easier for all female physicians and people of color."
When the Disney show "Doc McStuffins" premiered this year, Dr. Myiesha Taylor – and her 4-year-old daughter Hana – could not get enough. The show chronicles the life of 6-year-old African American Dottie "Doc" McStuffins, who cures the ouchies, oopsies, and uh-ohs that plague her stuffed animal friends. Dottie McStuffins wants to be a doctor just like her mother. Similarly, Dr. Taylor remembers using play medical equipment and medical records to treat her own stuffed companions.
As one of the first Disney shows to feature an African American female central character, "Doc McStuffins" sends a much-needed message to minority youth, who traditionally lack strong minority role models, said Dr. Taylor, an emergency physician in Fort Worth, Tex.
Children should be taught from an early age that they can do whatever they want to do if they work hard enough, Dr. Taylor said in an interview. "Then, when they’re in sixth grade, they’re already on a trajectory to greatness and they’re not aspiring necessarily to be a rock star [or] an athlete. They know that they can find success if they work hard in this intellectual field of medicine, as opposed to a performing field," she said.
To show her appreciation, Dr. Taylor created a collage of the image of Doc McStuffins surrounded by more than 130 photographs of African American female physicians across the country. She said her collage was her way of thanking Disney for shining a light on the diversity in America.
"In 20 or 30 years, you’ll have a different look in America, so you need to start addressing those issues now, and the way you address it is not intervention in high school. That’s too late," she said.
Dr. Taylor remembers feeling called to medicine at a young age, inspired by her mother and grandmother, who were both nurses. But after her father’s tragic death during the Los Angeles riots in 1992, her calling to emergency medicine became clear. Dwight Taylor died at age 42, just hours after he was transported to an emergency department that did not have a trauma center. Dr. Taylor, then a senior in high school, remembers wanting to make a difference for people in their most desperate hours.
"As I continued in my training, I said, ‘You know, I think that I want to be the type of doctor that can make an immediate change,’ " she recalled. "Motivated by what happened to my father, it just felt like the natural thing for me to go into."
While the kind of family tragedy that inspired Dr. Taylor is thankfully rare, she emphasized that if provided with inspiration from the adults around them, minority children can be drawn to emergency medicine and other medical careers. She added that as the minority population in the United States grows, it’s more important than ever that the physician population reflect the image of the people they serve. And emergency physicians should work to make that a reality in their field.
"Our patients don’t look like our group, so we need to reach out," she said. "I know you can’t just go and pick a doctor off a tree. So, that means that my colleagues need to recognize that it’s important for more students to be ready for medical school ... and then once they’re in medical school, you want to try to recruit them into your specialty so that they don’t all end up in a specialty that is less competitive, for instance, because they just have so many spots."
Embracing diversity is not just about race, but gender as well, Dr. Taylor added. Even a pretend doctor like Doc McStuffins can help children understand that a black woman can be an accomplished physician, she said.
"You need that leading lady to show she’s in charge, she’s the doctor, so that when I walk in to the patients’ rooms, they’re not thinking that it’s weird and I must be the nurse. Or the medical student that’s with me must be the doctor because he’s a man. These types of shows dispel some of those stereotypes and make it easier for all female physicians and people of color."
When the Disney show "Doc McStuffins" premiered this year, Dr. Myiesha Taylor – and her 4-year-old daughter Hana – could not get enough. The show chronicles the life of 6-year-old African American Dottie "Doc" McStuffins, who cures the ouchies, oopsies, and uh-ohs that plague her stuffed animal friends. Dottie McStuffins wants to be a doctor just like her mother. Similarly, Dr. Taylor remembers using play medical equipment and medical records to treat her own stuffed companions.
As one of the first Disney shows to feature an African American female central character, "Doc McStuffins" sends a much-needed message to minority youth, who traditionally lack strong minority role models, said Dr. Taylor, an emergency physician in Fort Worth, Tex.
Children should be taught from an early age that they can do whatever they want to do if they work hard enough, Dr. Taylor said in an interview. "Then, when they’re in sixth grade, they’re already on a trajectory to greatness and they’re not aspiring necessarily to be a rock star [or] an athlete. They know that they can find success if they work hard in this intellectual field of medicine, as opposed to a performing field," she said.
To show her appreciation, Dr. Taylor created a collage of the image of Doc McStuffins surrounded by more than 130 photographs of African American female physicians across the country. She said her collage was her way of thanking Disney for shining a light on the diversity in America.
"In 20 or 30 years, you’ll have a different look in America, so you need to start addressing those issues now, and the way you address it is not intervention in high school. That’s too late," she said.
Dr. Taylor remembers feeling called to medicine at a young age, inspired by her mother and grandmother, who were both nurses. But after her father’s tragic death during the Los Angeles riots in 1992, her calling to emergency medicine became clear. Dwight Taylor died at age 42, just hours after he was transported to an emergency department that did not have a trauma center. Dr. Taylor, then a senior in high school, remembers wanting to make a difference for people in their most desperate hours.
"As I continued in my training, I said, ‘You know, I think that I want to be the type of doctor that can make an immediate change,’ " she recalled. "Motivated by what happened to my father, it just felt like the natural thing for me to go into."
While the kind of family tragedy that inspired Dr. Taylor is thankfully rare, she emphasized that if provided with inspiration from the adults around them, minority children can be drawn to emergency medicine and other medical careers. She added that as the minority population in the United States grows, it’s more important than ever that the physician population reflect the image of the people they serve. And emergency physicians should work to make that a reality in their field.
"Our patients don’t look like our group, so we need to reach out," she said. "I know you can’t just go and pick a doctor off a tree. So, that means that my colleagues need to recognize that it’s important for more students to be ready for medical school ... and then once they’re in medical school, you want to try to recruit them into your specialty so that they don’t all end up in a specialty that is less competitive, for instance, because they just have so many spots."
Embracing diversity is not just about race, but gender as well, Dr. Taylor added. Even a pretend doctor like Doc McStuffins can help children understand that a black woman can be an accomplished physician, she said.
"You need that leading lady to show she’s in charge, she’s the doctor, so that when I walk in to the patients’ rooms, they’re not thinking that it’s weird and I must be the nurse. Or the medical student that’s with me must be the doctor because he’s a man. These types of shows dispel some of those stereotypes and make it easier for all female physicians and people of color."
Study: ACA Will Up Health Spending
WASHINGTON – The major expansions in health care coverage in 2014 called for by the Affordable Care Act will cause health care spending to grow by 7.4% that year alone – a rate two percentage points higher than would have occurred without the law, according to an analysis by economists from the Centers for Medicare and Medicaid Services.
Much of that growth will be driven by increased use of physician services (projected to grow by 8.5%) and prescription drugs (projected to grow by 8.8%) as an estimated additional 30 million Americans gain health coverage under the law, Sean P. Keehan and his colleagues from the CMS Office of the Actuary said at a press briefing sponsored by the journal Health Affairs.
Their analysis was published online in the journal Health Affairs (2012 June [doi:10.1377/hlthaff.2012.0404]).
The coming growth in health spending is tempered by the current economic climate, according to the analysis. Estimated spending growth for 2011 is 3.9% – the same rate seen in 2010 and just above the historically slow growth rate of 3.8% in 2009.
"The recent recession and the modest economic recovery have played a role in our projection of near historic lows in health spending growth through 2013," Mr. Keehan said.
The economists noted, however, that once the health care system absorbs those newly insured via the state health insurance exchanges and Medicaid expansion in 2014, growth in spending is projected to stabilize.
"Once you have [the population from the coverage expansion] in, the growth rate of national health spending is projected to be fairly similar with or without the Affordable Care Act," Mr. Keehan said.
The projections also assume the approximate 30% cut in Medicare physician payment under the Sustainable Growth Rate formula will go into effect Jan. 1, 2013, and will remain in effect thereafter. This would bring the growth in Medicare spending down to 1.3%, from 5.9% in 2012. Previously Congress has generally prevented these SGR cuts.
Medicare costs are projected to grow every year, as more baby boomers qualify for benefits. Those costs will be offset partially by cost-saving provisions under the ACA, said CMS economist Gigi Cuckler.
"The growth rate in 2014 is largely influenced by the coverage expansions, but once you go into 2015 through 2021, you still have continuing effects of the coverage expansions," she said.
"However, you have a lot of Medicare cost-savings provisions also in play here that are bringing down the costs at this time."
The analysis is similar to that released last July by CMS.
The projections are based on economic and demographic assumptions that were obtained from the 2012 Medicare Trustees Report.
As everyone knows by now, in essence, the Supreme Court upheld the Accountable Care Act in its entirety on June 28th. Unless repealed by Congress, all or in part, the fiscal projections outlined in this article will become reality. I must say, I find it difficult to believe that growth in spending, as predicted in the article, will stabilize anytime soon. In balance, the law is good for patients who otherwise would go without coverage. In the short run, it may even be good for doctors (absent the 30% cut we face based on the SGR formulation). I am quite sure it will be good for many hospitals. However, over the long haul, the impending increase in healthcare spending, unless truly offset by improvements in prevention and quality, will likely be disastrous for this country, placing an insurmountable burden on our children and their children. An added fiscal note and a plea to call your legislators ...with sequestration, an additional 2% cut for physicians is scheduled to take effect on January 1, 2013.
Mark D. Morasch, M.D., is a vascular surgeon at The Heart and Vascular Center, St. Vincent's Hospital, Billings, Montana, and an associate medical editor of Vascular Specialist.
As everyone knows by now, in essence, the Supreme Court upheld the Accountable Care Act in its entirety on June 28th. Unless repealed by Congress, all or in part, the fiscal projections outlined in this article will become reality. I must say, I find it difficult to believe that growth in spending, as predicted in the article, will stabilize anytime soon. In balance, the law is good for patients who otherwise would go without coverage. In the short run, it may even be good for doctors (absent the 30% cut we face based on the SGR formulation). I am quite sure it will be good for many hospitals. However, over the long haul, the impending increase in healthcare spending, unless truly offset by improvements in prevention and quality, will likely be disastrous for this country, placing an insurmountable burden on our children and their children. An added fiscal note and a plea to call your legislators ...with sequestration, an additional 2% cut for physicians is scheduled to take effect on January 1, 2013.
Mark D. Morasch, M.D., is a vascular surgeon at The Heart and Vascular Center, St. Vincent's Hospital, Billings, Montana, and an associate medical editor of Vascular Specialist.
As everyone knows by now, in essence, the Supreme Court upheld the Accountable Care Act in its entirety on June 28th. Unless repealed by Congress, all or in part, the fiscal projections outlined in this article will become reality. I must say, I find it difficult to believe that growth in spending, as predicted in the article, will stabilize anytime soon. In balance, the law is good for patients who otherwise would go without coverage. In the short run, it may even be good for doctors (absent the 30% cut we face based on the SGR formulation). I am quite sure it will be good for many hospitals. However, over the long haul, the impending increase in healthcare spending, unless truly offset by improvements in prevention and quality, will likely be disastrous for this country, placing an insurmountable burden on our children and their children. An added fiscal note and a plea to call your legislators ...with sequestration, an additional 2% cut for physicians is scheduled to take effect on January 1, 2013.
Mark D. Morasch, M.D., is a vascular surgeon at The Heart and Vascular Center, St. Vincent's Hospital, Billings, Montana, and an associate medical editor of Vascular Specialist.
WASHINGTON – The major expansions in health care coverage in 2014 called for by the Affordable Care Act will cause health care spending to grow by 7.4% that year alone – a rate two percentage points higher than would have occurred without the law, according to an analysis by economists from the Centers for Medicare and Medicaid Services.
Much of that growth will be driven by increased use of physician services (projected to grow by 8.5%) and prescription drugs (projected to grow by 8.8%) as an estimated additional 30 million Americans gain health coverage under the law, Sean P. Keehan and his colleagues from the CMS Office of the Actuary said at a press briefing sponsored by the journal Health Affairs.
Their analysis was published online in the journal Health Affairs (2012 June [doi:10.1377/hlthaff.2012.0404]).
The coming growth in health spending is tempered by the current economic climate, according to the analysis. Estimated spending growth for 2011 is 3.9% – the same rate seen in 2010 and just above the historically slow growth rate of 3.8% in 2009.
"The recent recession and the modest economic recovery have played a role in our projection of near historic lows in health spending growth through 2013," Mr. Keehan said.
The economists noted, however, that once the health care system absorbs those newly insured via the state health insurance exchanges and Medicaid expansion in 2014, growth in spending is projected to stabilize.
"Once you have [the population from the coverage expansion] in, the growth rate of national health spending is projected to be fairly similar with or without the Affordable Care Act," Mr. Keehan said.
The projections also assume the approximate 30% cut in Medicare physician payment under the Sustainable Growth Rate formula will go into effect Jan. 1, 2013, and will remain in effect thereafter. This would bring the growth in Medicare spending down to 1.3%, from 5.9% in 2012. Previously Congress has generally prevented these SGR cuts.
Medicare costs are projected to grow every year, as more baby boomers qualify for benefits. Those costs will be offset partially by cost-saving provisions under the ACA, said CMS economist Gigi Cuckler.
"The growth rate in 2014 is largely influenced by the coverage expansions, but once you go into 2015 through 2021, you still have continuing effects of the coverage expansions," she said.
"However, you have a lot of Medicare cost-savings provisions also in play here that are bringing down the costs at this time."
The analysis is similar to that released last July by CMS.
The projections are based on economic and demographic assumptions that were obtained from the 2012 Medicare Trustees Report.
WASHINGTON – The major expansions in health care coverage in 2014 called for by the Affordable Care Act will cause health care spending to grow by 7.4% that year alone – a rate two percentage points higher than would have occurred without the law, according to an analysis by economists from the Centers for Medicare and Medicaid Services.
Much of that growth will be driven by increased use of physician services (projected to grow by 8.5%) and prescription drugs (projected to grow by 8.8%) as an estimated additional 30 million Americans gain health coverage under the law, Sean P. Keehan and his colleagues from the CMS Office of the Actuary said at a press briefing sponsored by the journal Health Affairs.
Their analysis was published online in the journal Health Affairs (2012 June [doi:10.1377/hlthaff.2012.0404]).
The coming growth in health spending is tempered by the current economic climate, according to the analysis. Estimated spending growth for 2011 is 3.9% – the same rate seen in 2010 and just above the historically slow growth rate of 3.8% in 2009.
"The recent recession and the modest economic recovery have played a role in our projection of near historic lows in health spending growth through 2013," Mr. Keehan said.
The economists noted, however, that once the health care system absorbs those newly insured via the state health insurance exchanges and Medicaid expansion in 2014, growth in spending is projected to stabilize.
"Once you have [the population from the coverage expansion] in, the growth rate of national health spending is projected to be fairly similar with or without the Affordable Care Act," Mr. Keehan said.
The projections also assume the approximate 30% cut in Medicare physician payment under the Sustainable Growth Rate formula will go into effect Jan. 1, 2013, and will remain in effect thereafter. This would bring the growth in Medicare spending down to 1.3%, from 5.9% in 2012. Previously Congress has generally prevented these SGR cuts.
Medicare costs are projected to grow every year, as more baby boomers qualify for benefits. Those costs will be offset partially by cost-saving provisions under the ACA, said CMS economist Gigi Cuckler.
"The growth rate in 2014 is largely influenced by the coverage expansions, but once you go into 2015 through 2021, you still have continuing effects of the coverage expansions," she said.
"However, you have a lot of Medicare cost-savings provisions also in play here that are bringing down the costs at this time."
The analysis is similar to that released last July by CMS.
The projections are based on economic and demographic assumptions that were obtained from the 2012 Medicare Trustees Report.
A PRESS BRIEFING SPONSORED BY THE JOURNAL HEALTH AFFAIRS
MedPAC Suggests EHR Incentives May Not Cover True Costs
WASHINGTON – Members of the Medicare Payment Advisory Commission expressed concern about the burden placed on smaller practices by the requirements of the Health Information Technology for Economic and Clinical Health (HITECH) Act.
Physicians who meet requirements for the meaningful use of an electronic health record (EHR) can earn incentive payments of up to $44,000 under HITECH. Starting in 2015, physicians who do not participate will be penalized.
One thing the incentive pay does not cover, said Commissioner Peter Butler, is the time needed to manage all the additional data requirements."What [incentives] do not do is provide dollars for decision support, for data repositories, data warehouses, which are really the heart of managing in an [accountable care organization] capitated world. It kind of ignores some of the real tools that ultimately you need to kind of make a difference," said Mr. Butler, Rush University Medical Center, Chicago.
As data requirements increase, the commission should consider how to address that concern in terms of patient satisfaction, noted Dr. Borman, a surgeon at Abington (Pa.) Memorial Hospital.
Despite the flaws in the EHR incentive program, commissioners agreed that, if it’s done right, EHRs would benefit both physicians and patients.
MedPAC Commissioner Dr. William Hall of the University of Rochester (N.Y.), noted that EHR systems support a higher level of coding, which would mean higher payments to physicians than even incentive payments could offer.
Joanna Kim, senior associate director of the American Hospital Association, Washington, testified to the commission that EHR requirements are too challenging, even for hospitals.
"[Incentive payments] are slow to come because the stage one requirements were set entirely too high," Ms. Kim said. She added that certain elements, like the patient portal are too expensive, cause major security concerns, and carry uncertain benefits.
CMS penalties for failing to meet meaningful use requirements will begin in 2015, but they’ll be based on 2013 performances. As well as examining the EHR incentive program, the commission unanimously recommended changes to Medicare fee-for-service benefit design, including:
• Establishing a limit for out-of-pocket expenses to protect beneficiaries who reach catastrophic levels of Medicare costs. The commission recognized that a small group of beneficiaries would reach the out-of-pocket cap in any given year, they said many more would benefit from the cap.
PIReplacing coinsurance (where the beneficiary pays a percentage of the fee) with copayments (where the beneficiary pays a proscribed fee per service) that vary according to the type of service and provider. MedPAC staffers stated copayments are more predictable, easier to budget for, and easier to understand than is coinsurance.
• Placing an additional charge on private supplemental insurance, or Medigap, that pays for services not covered under Medicare. The commission said the charge would help recoup some of the added costs of Medicare.
• Allow the HHS secretary to determine cost sharing based on evidence of service value.
• Maintaining a deductible for Part A and Part B services.
The recommendations were included in the commission’s June report.☐
WASHINGTON – Members of the Medicare Payment Advisory Commission expressed concern about the burden placed on smaller practices by the requirements of the Health Information Technology for Economic and Clinical Health (HITECH) Act.
Physicians who meet requirements for the meaningful use of an electronic health record (EHR) can earn incentive payments of up to $44,000 under HITECH. Starting in 2015, physicians who do not participate will be penalized.
One thing the incentive pay does not cover, said Commissioner Peter Butler, is the time needed to manage all the additional data requirements."What [incentives] do not do is provide dollars for decision support, for data repositories, data warehouses, which are really the heart of managing in an [accountable care organization] capitated world. It kind of ignores some of the real tools that ultimately you need to kind of make a difference," said Mr. Butler, Rush University Medical Center, Chicago.
As data requirements increase, the commission should consider how to address that concern in terms of patient satisfaction, noted Dr. Borman, a surgeon at Abington (Pa.) Memorial Hospital.
Despite the flaws in the EHR incentive program, commissioners agreed that, if it’s done right, EHRs would benefit both physicians and patients.
MedPAC Commissioner Dr. William Hall of the University of Rochester (N.Y.), noted that EHR systems support a higher level of coding, which would mean higher payments to physicians than even incentive payments could offer.
Joanna Kim, senior associate director of the American Hospital Association, Washington, testified to the commission that EHR requirements are too challenging, even for hospitals.
"[Incentive payments] are slow to come because the stage one requirements were set entirely too high," Ms. Kim said. She added that certain elements, like the patient portal are too expensive, cause major security concerns, and carry uncertain benefits.
CMS penalties for failing to meet meaningful use requirements will begin in 2015, but they’ll be based on 2013 performances. As well as examining the EHR incentive program, the commission unanimously recommended changes to Medicare fee-for-service benefit design, including:
• Establishing a limit for out-of-pocket expenses to protect beneficiaries who reach catastrophic levels of Medicare costs. The commission recognized that a small group of beneficiaries would reach the out-of-pocket cap in any given year, they said many more would benefit from the cap.
PIReplacing coinsurance (where the beneficiary pays a percentage of the fee) with copayments (where the beneficiary pays a proscribed fee per service) that vary according to the type of service and provider. MedPAC staffers stated copayments are more predictable, easier to budget for, and easier to understand than is coinsurance.
• Placing an additional charge on private supplemental insurance, or Medigap, that pays for services not covered under Medicare. The commission said the charge would help recoup some of the added costs of Medicare.
• Allow the HHS secretary to determine cost sharing based on evidence of service value.
• Maintaining a deductible for Part A and Part B services.
The recommendations were included in the commission’s June report.☐
WASHINGTON – Members of the Medicare Payment Advisory Commission expressed concern about the burden placed on smaller practices by the requirements of the Health Information Technology for Economic and Clinical Health (HITECH) Act.
Physicians who meet requirements for the meaningful use of an electronic health record (EHR) can earn incentive payments of up to $44,000 under HITECH. Starting in 2015, physicians who do not participate will be penalized.
One thing the incentive pay does not cover, said Commissioner Peter Butler, is the time needed to manage all the additional data requirements."What [incentives] do not do is provide dollars for decision support, for data repositories, data warehouses, which are really the heart of managing in an [accountable care organization] capitated world. It kind of ignores some of the real tools that ultimately you need to kind of make a difference," said Mr. Butler, Rush University Medical Center, Chicago.
As data requirements increase, the commission should consider how to address that concern in terms of patient satisfaction, noted Dr. Borman, a surgeon at Abington (Pa.) Memorial Hospital.
Despite the flaws in the EHR incentive program, commissioners agreed that, if it’s done right, EHRs would benefit both physicians and patients.
MedPAC Commissioner Dr. William Hall of the University of Rochester (N.Y.), noted that EHR systems support a higher level of coding, which would mean higher payments to physicians than even incentive payments could offer.
Joanna Kim, senior associate director of the American Hospital Association, Washington, testified to the commission that EHR requirements are too challenging, even for hospitals.
"[Incentive payments] are slow to come because the stage one requirements were set entirely too high," Ms. Kim said. She added that certain elements, like the patient portal are too expensive, cause major security concerns, and carry uncertain benefits.
CMS penalties for failing to meet meaningful use requirements will begin in 2015, but they’ll be based on 2013 performances. As well as examining the EHR incentive program, the commission unanimously recommended changes to Medicare fee-for-service benefit design, including:
• Establishing a limit for out-of-pocket expenses to protect beneficiaries who reach catastrophic levels of Medicare costs. The commission recognized that a small group of beneficiaries would reach the out-of-pocket cap in any given year, they said many more would benefit from the cap.
PIReplacing coinsurance (where the beneficiary pays a percentage of the fee) with copayments (where the beneficiary pays a proscribed fee per service) that vary according to the type of service and provider. MedPAC staffers stated copayments are more predictable, easier to budget for, and easier to understand than is coinsurance.
• Placing an additional charge on private supplemental insurance, or Medigap, that pays for services not covered under Medicare. The commission said the charge would help recoup some of the added costs of Medicare.
• Allow the HHS secretary to determine cost sharing based on evidence of service value.
• Maintaining a deductible for Part A and Part B services.
The recommendations were included in the commission’s June report.☐
States in Medicaid Limbo After Court's Ruling
Questions and uncertainty abound as state governments begin deciding whether they will participate in the expansion of Medicaid that was called for by the Affordable Care Act.
In light of the Supreme Court’s decision that the federal government cannot penalize states that don’t participate, the governors of Texas, South Carolina, Nebraska, Iowa, Louisiana, Mississippi, and Florida have said that their states will opt out.
Leaders in other states say they need more information.
"The original act was very punitive for states that didn’t expand Medicaid. [The Supreme Court decision] now gives some options which, honestly, I don’t think a lot of us expected," Gov. Bob McDonnell (R-Va.) said at a press conference held at the National Governors Association annual meeting. "I don’t think it’s responsible fully for my state to make a decision now, because there’s still more information I need."
"I think this is a really historic opportunity to align the health care system for health."
Gov. Jack Markell (D-Del.) said he sees the expansion as a "good deal for Delaware taxpayers," but agreed that most states will need more guidance from the federal government before making a decision.
As the ruling allows states to opt out of Medicaid expansion without losing existing federal monies, health care reform likely will look very different from state to state, said Sheila Burke of the John F. Kennedy School of Government at Harvard University, Cambridge, Massachusetts.
"These states are going to respond to this very differently, and they are very different in terms of their preparation and their capacity to take on these changes. Governors, state legislators, exchange directors, and insurance commissioners all may have a different view," Ms. Burke said at a briefing held by the Alliance for Health Reform. She pointed out that many states legislatures won’t meet again until next year, so meaningful decision making may be on hold until then.
Prior to passage of the ACA, Medicaid provided health care coverage for the indigent, especially those who were dependent children, pregnant women, disabled, or elderly. Under the expansion, Medicaid would also cover anyone younger than age 65 years with an annual income less than 133% of the federal poverty level. The law also provides tax credits for people with incomes between 100% and 400% of the federal poverty level to purchase insurance.
If a state decides to opt out of Medicaid expansion, people whose income is above the federal poverty level, those who are single, childless, or don’t live with their children would not be covered. In addition, those who qualify for premium subsidies under the law but can’t find affordable coverage (that is, mostly low-wage workers) would not be covered.
States that opt out of the expansion also could have a harder time balancing impending cuts to providers and hospitals, according to Chris Jennings, president of Jennings Policy Strategies and former top health aide to President Clinton.
Physicians face a 27% Medicare pay cut in January according to the Sustainable Growth Rate (SGR) formula; hospitals, too, face cuts to their Disproportionate Share Hospital (DSH) payments.
Although there may be other ways to balance the cuts, the easiest is expanding Medicaid to get the extra funding, said Mr. Jennings. "It’s a harder road to go than just taking the money."
While an influx of federal funding would help states offset other cuts, it’s unlikely that it would be enough for physicians to rebound from a huge SGR cut, according to Dr. Glen R. Stream, president of the American Academy of Family Physicians.
"If the SGR-indicated payment cut was to go into place, there’s no way that the expansion of Medicaid is going to offset the devastating financial impact that that’s going to have for practices," he said in an interview. But he added that expanding Medicaid is currently the best option for providing much-needed care for low-income Americans.
"I don’t think anyone necessarily envisions expansion of Medicaid as the ideal means to expand coverage, but it is the one that’s on the table. My hope would be that if states chose to opt out of the Medicaid expansion, they would do so with some other plan to meet the needs of their citizens. The challenge would be that the plan wouldn’t be coming with any federal dollars," Dr. Stream said.
Officials with the American College of Physicians said that states should move forward with expansion as soon as possible.
The "ACP also strongly urges states to move forward on expanding Medicaid to all persons with incomes up to 133% of the federal poverty level, notwithstanding the court’s ruling that states may not be denied existing Medicaid dollars for failing to do so," ACP president David L. Bronson said in a statement following the court’s ruling.
Even as states weigh their options, Mr. Jennings speculated that more will participate in the Medicaid expansion than most people currently think.
Dr. Stream agreed. "I suspect, at the end of the day, that we’ll have a lot more states coming in than we currently are hearing, primarily because I have some confidence in stakeholders’ abilities to encourage legislatures and governors to move ahead," he said.
Maryland is one of those states. Dr. Joshua Sharfstein, the state Secretary of Health and Mental Hygiene, said that implementing the law will give states an edge over those that opt out.
"I’ve heard [Gov. Martin O’Malley (D-Md.)] say that he ultimately sees successful implementation of the law as a competitive advantage for Maryland [and] for businesses to locate in the state if there’s real investment in the workforce," Dr. Sharfstein said at the briefing. "I think this is a really historic opportunity to align the health care system for health and I think it’s those types of things that are going to get the job done."
Questions and uncertainty abound as state governments begin deciding whether they will participate in the expansion of Medicaid that was called for by the Affordable Care Act.
In light of the Supreme Court’s decision that the federal government cannot penalize states that don’t participate, the governors of Texas, South Carolina, Nebraska, Iowa, Louisiana, Mississippi, and Florida have said that their states will opt out.
Leaders in other states say they need more information.
"The original act was very punitive for states that didn’t expand Medicaid. [The Supreme Court decision] now gives some options which, honestly, I don’t think a lot of us expected," Gov. Bob McDonnell (R-Va.) said at a press conference held at the National Governors Association annual meeting. "I don’t think it’s responsible fully for my state to make a decision now, because there’s still more information I need."
"I think this is a really historic opportunity to align the health care system for health."
Gov. Jack Markell (D-Del.) said he sees the expansion as a "good deal for Delaware taxpayers," but agreed that most states will need more guidance from the federal government before making a decision.
As the ruling allows states to opt out of Medicaid expansion without losing existing federal monies, health care reform likely will look very different from state to state, said Sheila Burke of the John F. Kennedy School of Government at Harvard University, Cambridge, Massachusetts.
"These states are going to respond to this very differently, and they are very different in terms of their preparation and their capacity to take on these changes. Governors, state legislators, exchange directors, and insurance commissioners all may have a different view," Ms. Burke said at a briefing held by the Alliance for Health Reform. She pointed out that many states legislatures won’t meet again until next year, so meaningful decision making may be on hold until then.
Prior to passage of the ACA, Medicaid provided health care coverage for the indigent, especially those who were dependent children, pregnant women, disabled, or elderly. Under the expansion, Medicaid would also cover anyone younger than age 65 years with an annual income less than 133% of the federal poverty level. The law also provides tax credits for people with incomes between 100% and 400% of the federal poverty level to purchase insurance.
If a state decides to opt out of Medicaid expansion, people whose income is above the federal poverty level, those who are single, childless, or don’t live with their children would not be covered. In addition, those who qualify for premium subsidies under the law but can’t find affordable coverage (that is, mostly low-wage workers) would not be covered.
States that opt out of the expansion also could have a harder time balancing impending cuts to providers and hospitals, according to Chris Jennings, president of Jennings Policy Strategies and former top health aide to President Clinton.
Physicians face a 27% Medicare pay cut in January according to the Sustainable Growth Rate (SGR) formula; hospitals, too, face cuts to their Disproportionate Share Hospital (DSH) payments.
Although there may be other ways to balance the cuts, the easiest is expanding Medicaid to get the extra funding, said Mr. Jennings. "It’s a harder road to go than just taking the money."
While an influx of federal funding would help states offset other cuts, it’s unlikely that it would be enough for physicians to rebound from a huge SGR cut, according to Dr. Glen R. Stream, president of the American Academy of Family Physicians.
"If the SGR-indicated payment cut was to go into place, there’s no way that the expansion of Medicaid is going to offset the devastating financial impact that that’s going to have for practices," he said in an interview. But he added that expanding Medicaid is currently the best option for providing much-needed care for low-income Americans.
"I don’t think anyone necessarily envisions expansion of Medicaid as the ideal means to expand coverage, but it is the one that’s on the table. My hope would be that if states chose to opt out of the Medicaid expansion, they would do so with some other plan to meet the needs of their citizens. The challenge would be that the plan wouldn’t be coming with any federal dollars," Dr. Stream said.
Officials with the American College of Physicians said that states should move forward with expansion as soon as possible.
The "ACP also strongly urges states to move forward on expanding Medicaid to all persons with incomes up to 133% of the federal poverty level, notwithstanding the court’s ruling that states may not be denied existing Medicaid dollars for failing to do so," ACP president David L. Bronson said in a statement following the court’s ruling.
Even as states weigh their options, Mr. Jennings speculated that more will participate in the Medicaid expansion than most people currently think.
Dr. Stream agreed. "I suspect, at the end of the day, that we’ll have a lot more states coming in than we currently are hearing, primarily because I have some confidence in stakeholders’ abilities to encourage legislatures and governors to move ahead," he said.
Maryland is one of those states. Dr. Joshua Sharfstein, the state Secretary of Health and Mental Hygiene, said that implementing the law will give states an edge over those that opt out.
"I’ve heard [Gov. Martin O’Malley (D-Md.)] say that he ultimately sees successful implementation of the law as a competitive advantage for Maryland [and] for businesses to locate in the state if there’s real investment in the workforce," Dr. Sharfstein said at the briefing. "I think this is a really historic opportunity to align the health care system for health and I think it’s those types of things that are going to get the job done."
Questions and uncertainty abound as state governments begin deciding whether they will participate in the expansion of Medicaid that was called for by the Affordable Care Act.
In light of the Supreme Court’s decision that the federal government cannot penalize states that don’t participate, the governors of Texas, South Carolina, Nebraska, Iowa, Louisiana, Mississippi, and Florida have said that their states will opt out.
Leaders in other states say they need more information.
"The original act was very punitive for states that didn’t expand Medicaid. [The Supreme Court decision] now gives some options which, honestly, I don’t think a lot of us expected," Gov. Bob McDonnell (R-Va.) said at a press conference held at the National Governors Association annual meeting. "I don’t think it’s responsible fully for my state to make a decision now, because there’s still more information I need."
"I think this is a really historic opportunity to align the health care system for health."
Gov. Jack Markell (D-Del.) said he sees the expansion as a "good deal for Delaware taxpayers," but agreed that most states will need more guidance from the federal government before making a decision.
As the ruling allows states to opt out of Medicaid expansion without losing existing federal monies, health care reform likely will look very different from state to state, said Sheila Burke of the John F. Kennedy School of Government at Harvard University, Cambridge, Massachusetts.
"These states are going to respond to this very differently, and they are very different in terms of their preparation and their capacity to take on these changes. Governors, state legislators, exchange directors, and insurance commissioners all may have a different view," Ms. Burke said at a briefing held by the Alliance for Health Reform. She pointed out that many states legislatures won’t meet again until next year, so meaningful decision making may be on hold until then.
Prior to passage of the ACA, Medicaid provided health care coverage for the indigent, especially those who were dependent children, pregnant women, disabled, or elderly. Under the expansion, Medicaid would also cover anyone younger than age 65 years with an annual income less than 133% of the federal poverty level. The law also provides tax credits for people with incomes between 100% and 400% of the federal poverty level to purchase insurance.
If a state decides to opt out of Medicaid expansion, people whose income is above the federal poverty level, those who are single, childless, or don’t live with their children would not be covered. In addition, those who qualify for premium subsidies under the law but can’t find affordable coverage (that is, mostly low-wage workers) would not be covered.
States that opt out of the expansion also could have a harder time balancing impending cuts to providers and hospitals, according to Chris Jennings, president of Jennings Policy Strategies and former top health aide to President Clinton.
Physicians face a 27% Medicare pay cut in January according to the Sustainable Growth Rate (SGR) formula; hospitals, too, face cuts to their Disproportionate Share Hospital (DSH) payments.
Although there may be other ways to balance the cuts, the easiest is expanding Medicaid to get the extra funding, said Mr. Jennings. "It’s a harder road to go than just taking the money."
While an influx of federal funding would help states offset other cuts, it’s unlikely that it would be enough for physicians to rebound from a huge SGR cut, according to Dr. Glen R. Stream, president of the American Academy of Family Physicians.
"If the SGR-indicated payment cut was to go into place, there’s no way that the expansion of Medicaid is going to offset the devastating financial impact that that’s going to have for practices," he said in an interview. But he added that expanding Medicaid is currently the best option for providing much-needed care for low-income Americans.
"I don’t think anyone necessarily envisions expansion of Medicaid as the ideal means to expand coverage, but it is the one that’s on the table. My hope would be that if states chose to opt out of the Medicaid expansion, they would do so with some other plan to meet the needs of their citizens. The challenge would be that the plan wouldn’t be coming with any federal dollars," Dr. Stream said.
Officials with the American College of Physicians said that states should move forward with expansion as soon as possible.
The "ACP also strongly urges states to move forward on expanding Medicaid to all persons with incomes up to 133% of the federal poverty level, notwithstanding the court’s ruling that states may not be denied existing Medicaid dollars for failing to do so," ACP president David L. Bronson said in a statement following the court’s ruling.
Even as states weigh their options, Mr. Jennings speculated that more will participate in the Medicaid expansion than most people currently think.
Dr. Stream agreed. "I suspect, at the end of the day, that we’ll have a lot more states coming in than we currently are hearing, primarily because I have some confidence in stakeholders’ abilities to encourage legislatures and governors to move ahead," he said.
Maryland is one of those states. Dr. Joshua Sharfstein, the state Secretary of Health and Mental Hygiene, said that implementing the law will give states an edge over those that opt out.
"I’ve heard [Gov. Martin O’Malley (D-Md.)] say that he ultimately sees successful implementation of the law as a competitive advantage for Maryland [and] for businesses to locate in the state if there’s real investment in the workforce," Dr. Sharfstein said at the briefing. "I think this is a really historic opportunity to align the health care system for health and I think it’s those types of things that are going to get the job done."
MedPAC Suggests EHR Incentives May Not Cover True Costs
WASHINGTON – Members of the Medicare Payment Advisory Commission expressed concern about the burden placed on smaller practices by the requirements of the Health Information Technology for Economic and Clinical Health (HITECH) Act.
Physicians who meet requirements for the meaningful use of an electronic health record (EHR) can earn incentive payments of up to $44,000 under HITECH. Starting in 2015, physicians who do not participate will be penalized.
One thing the incentive pay does not cover, according to Commissioner Peter Butler, is the time necessary to manage all the additional data requirements."What [incentives] do not do is provide dollars for decision support, for data repositories, data warehouses, which are really the heart of managing in an [accountable care organization] capitated world. It kind of ignores some of the real tools that ultimately you need to kind of make a difference," said Mr. Butler, president and chief operating officer at Rush University Medical Center, Chicago.
Dr. Karen Borman, a MedPAC commissioner, added that the additional data requirements are also forcing physicians to spend more time in front of the computer instead of interacting with the patient.
As data requirements increase, the commission should consider how to address that concern in terms of patient satisfaction, noted Dr. Borman, a surgeon at Abington (Pa.) Memorial Hospital.
Despite the flaws in the EHR incentive program, commissioners agreed that, if it’s done right, EHRs would benefit both physicians and patients.
MedPAC Commissioner Dr. William Hall of the University of Rochester (N.Y.), noted that EHR systems support a higher level of coding, which would mean higher payments to physicians than even incentive payments could offer.
Joanna Kim, senior associate director of the American Hospital Association, Washington, testified to the commission that EHR requirements are too challenging, even for hospitals.
"[Incentive payments] are slow to come because the stage one requirements were set entirely too high," Ms. Kim said. She added that certain elements, like the patient portal are too expensive to implement, cause major security concerns, and carry uncertain benefits.
CMS penalties for failing to meet meaningful use requirements will not hit until 2015, but they’ll be based on 2013 performances. As well as examining the EHR incentive program, the commission unanimously recommended changes to Medicare fee-for-service benefit design, including:
• Establishing a limit for out-of-pocket expenses to protect beneficiaries who reach catastrophic levels of Medicare costs. Although the commission recognized that a small group of beneficiaries would reach the out-of-pocket cap in any given year, they said many more would benefit from the cap.
• Replacing coinsurance (where the beneficiary pays a percentage of the fee) with copayments (where the beneficiary pays a proscribed fee per service) that vary according to the type of service and provider. According to MedPAC staffers, copayments are more predictable, easier to budget for, and easier to understand than is coinsurance.
• Placing an additional charge on private supplemental insurance, or Medigap, that pays for services not covered under Medicare. The commission said the charge would help recoup some of the added costs of Medicare.
• Allow the HHS secretary to determine cost sharing based on evidence of service value.
• Maintaining a deductible for Part A and Part B services.
The recommendations were included in the commission’s June report.
WASHINGTON – Members of the Medicare Payment Advisory Commission expressed concern about the burden placed on smaller practices by the requirements of the Health Information Technology for Economic and Clinical Health (HITECH) Act.
Physicians who meet requirements for the meaningful use of an electronic health record (EHR) can earn incentive payments of up to $44,000 under HITECH. Starting in 2015, physicians who do not participate will be penalized.
One thing the incentive pay does not cover, according to Commissioner Peter Butler, is the time necessary to manage all the additional data requirements."What [incentives] do not do is provide dollars for decision support, for data repositories, data warehouses, which are really the heart of managing in an [accountable care organization] capitated world. It kind of ignores some of the real tools that ultimately you need to kind of make a difference," said Mr. Butler, president and chief operating officer at Rush University Medical Center, Chicago.
Dr. Karen Borman, a MedPAC commissioner, added that the additional data requirements are also forcing physicians to spend more time in front of the computer instead of interacting with the patient.
As data requirements increase, the commission should consider how to address that concern in terms of patient satisfaction, noted Dr. Borman, a surgeon at Abington (Pa.) Memorial Hospital.
Despite the flaws in the EHR incentive program, commissioners agreed that, if it’s done right, EHRs would benefit both physicians and patients.
MedPAC Commissioner Dr. William Hall of the University of Rochester (N.Y.), noted that EHR systems support a higher level of coding, which would mean higher payments to physicians than even incentive payments could offer.
Joanna Kim, senior associate director of the American Hospital Association, Washington, testified to the commission that EHR requirements are too challenging, even for hospitals.
"[Incentive payments] are slow to come because the stage one requirements were set entirely too high," Ms. Kim said. She added that certain elements, like the patient portal are too expensive to implement, cause major security concerns, and carry uncertain benefits.
CMS penalties for failing to meet meaningful use requirements will not hit until 2015, but they’ll be based on 2013 performances. As well as examining the EHR incentive program, the commission unanimously recommended changes to Medicare fee-for-service benefit design, including:
• Establishing a limit for out-of-pocket expenses to protect beneficiaries who reach catastrophic levels of Medicare costs. Although the commission recognized that a small group of beneficiaries would reach the out-of-pocket cap in any given year, they said many more would benefit from the cap.
• Replacing coinsurance (where the beneficiary pays a percentage of the fee) with copayments (where the beneficiary pays a proscribed fee per service) that vary according to the type of service and provider. According to MedPAC staffers, copayments are more predictable, easier to budget for, and easier to understand than is coinsurance.
• Placing an additional charge on private supplemental insurance, or Medigap, that pays for services not covered under Medicare. The commission said the charge would help recoup some of the added costs of Medicare.
• Allow the HHS secretary to determine cost sharing based on evidence of service value.
• Maintaining a deductible for Part A and Part B services.
The recommendations were included in the commission’s June report.
WASHINGTON – Members of the Medicare Payment Advisory Commission expressed concern about the burden placed on smaller practices by the requirements of the Health Information Technology for Economic and Clinical Health (HITECH) Act.
Physicians who meet requirements for the meaningful use of an electronic health record (EHR) can earn incentive payments of up to $44,000 under HITECH. Starting in 2015, physicians who do not participate will be penalized.
One thing the incentive pay does not cover, according to Commissioner Peter Butler, is the time necessary to manage all the additional data requirements."What [incentives] do not do is provide dollars for decision support, for data repositories, data warehouses, which are really the heart of managing in an [accountable care organization] capitated world. It kind of ignores some of the real tools that ultimately you need to kind of make a difference," said Mr. Butler, president and chief operating officer at Rush University Medical Center, Chicago.
Dr. Karen Borman, a MedPAC commissioner, added that the additional data requirements are also forcing physicians to spend more time in front of the computer instead of interacting with the patient.
As data requirements increase, the commission should consider how to address that concern in terms of patient satisfaction, noted Dr. Borman, a surgeon at Abington (Pa.) Memorial Hospital.
Despite the flaws in the EHR incentive program, commissioners agreed that, if it’s done right, EHRs would benefit both physicians and patients.
MedPAC Commissioner Dr. William Hall of the University of Rochester (N.Y.), noted that EHR systems support a higher level of coding, which would mean higher payments to physicians than even incentive payments could offer.
Joanna Kim, senior associate director of the American Hospital Association, Washington, testified to the commission that EHR requirements are too challenging, even for hospitals.
"[Incentive payments] are slow to come because the stage one requirements were set entirely too high," Ms. Kim said. She added that certain elements, like the patient portal are too expensive to implement, cause major security concerns, and carry uncertain benefits.
CMS penalties for failing to meet meaningful use requirements will not hit until 2015, but they’ll be based on 2013 performances. As well as examining the EHR incentive program, the commission unanimously recommended changes to Medicare fee-for-service benefit design, including:
• Establishing a limit for out-of-pocket expenses to protect beneficiaries who reach catastrophic levels of Medicare costs. Although the commission recognized that a small group of beneficiaries would reach the out-of-pocket cap in any given year, they said many more would benefit from the cap.
• Replacing coinsurance (where the beneficiary pays a percentage of the fee) with copayments (where the beneficiary pays a proscribed fee per service) that vary according to the type of service and provider. According to MedPAC staffers, copayments are more predictable, easier to budget for, and easier to understand than is coinsurance.
• Placing an additional charge on private supplemental insurance, or Medigap, that pays for services not covered under Medicare. The commission said the charge would help recoup some of the added costs of Medicare.
• Allow the HHS secretary to determine cost sharing based on evidence of service value.
• Maintaining a deductible for Part A and Part B services.
The recommendations were included in the commission’s June report.
FDA Approves Over-the-Counter Test for HIV
The first over-the-counter, self-administered test for human immunodeficiency virus infection has been approved by the U.S. Food and Drug Administration. The OraQuick In-Home HIV test detects antibodies to HIV-1 and HIV-2 using oral fluid obtained by swabbing the upper and lower gums of the mouth. The sample swab is placed in a developer vial and yields results within 20 to 40 minutes, the FDA said in a statement.
In clinical studies of self-testing, the OraQuick In-Home HIV Test had 92% sensitivity (one false negative result would be expected out of every 12 test results in HIV-infected individuals). Test specificity was 99.98% (one false positive would be expected out of every 5,000 test results in uninfected individuals). The agency warns that a negative test result does not mean that an individual is definitely not infected with HIV, particularly when HIV exposure may have occurred within 3 months of testing and before antibody production could be detected. Also, positive test results should prompt confirmatory testing with a health care professional.
"The availability of a home-use HIV test kit provides another option for individuals to get tested so that they can seek medical care, if appropriate," Dr. Karen Midthun, director of the FDA’s Center for Biologics Evaluation and Research said in a statement. OraSure Technologies expects to release the test for use starting in early October. They will provide a retail price closer to the date of release, according to Doug Michels, OraSure president and CEO. They also have a professional version of the test available for $17.50 for clinics and physician offices.
The Centers for Disease Control and Prevention estimates that 1.2 million people in the United States are infected with HIV and that nearly 1 in 5 don’t know they have it.
The first over-the-counter, self-administered test for human immunodeficiency virus infection has been approved by the U.S. Food and Drug Administration. The OraQuick In-Home HIV test detects antibodies to HIV-1 and HIV-2 using oral fluid obtained by swabbing the upper and lower gums of the mouth. The sample swab is placed in a developer vial and yields results within 20 to 40 minutes, the FDA said in a statement.
In clinical studies of self-testing, the OraQuick In-Home HIV Test had 92% sensitivity (one false negative result would be expected out of every 12 test results in HIV-infected individuals). Test specificity was 99.98% (one false positive would be expected out of every 5,000 test results in uninfected individuals). The agency warns that a negative test result does not mean that an individual is definitely not infected with HIV, particularly when HIV exposure may have occurred within 3 months of testing and before antibody production could be detected. Also, positive test results should prompt confirmatory testing with a health care professional.
"The availability of a home-use HIV test kit provides another option for individuals to get tested so that they can seek medical care, if appropriate," Dr. Karen Midthun, director of the FDA’s Center for Biologics Evaluation and Research said in a statement. OraSure Technologies expects to release the test for use starting in early October. They will provide a retail price closer to the date of release, according to Doug Michels, OraSure president and CEO. They also have a professional version of the test available for $17.50 for clinics and physician offices.
The Centers for Disease Control and Prevention estimates that 1.2 million people in the United States are infected with HIV and that nearly 1 in 5 don’t know they have it.
The first over-the-counter, self-administered test for human immunodeficiency virus infection has been approved by the U.S. Food and Drug Administration. The OraQuick In-Home HIV test detects antibodies to HIV-1 and HIV-2 using oral fluid obtained by swabbing the upper and lower gums of the mouth. The sample swab is placed in a developer vial and yields results within 20 to 40 minutes, the FDA said in a statement.
In clinical studies of self-testing, the OraQuick In-Home HIV Test had 92% sensitivity (one false negative result would be expected out of every 12 test results in HIV-infected individuals). Test specificity was 99.98% (one false positive would be expected out of every 5,000 test results in uninfected individuals). The agency warns that a negative test result does not mean that an individual is definitely not infected with HIV, particularly when HIV exposure may have occurred within 3 months of testing and before antibody production could be detected. Also, positive test results should prompt confirmatory testing with a health care professional.
"The availability of a home-use HIV test kit provides another option for individuals to get tested so that they can seek medical care, if appropriate," Dr. Karen Midthun, director of the FDA’s Center for Biologics Evaluation and Research said in a statement. OraSure Technologies expects to release the test for use starting in early October. They will provide a retail price closer to the date of release, according to Doug Michels, OraSure president and CEO. They also have a professional version of the test available for $17.50 for clinics and physician offices.
The Centers for Disease Control and Prevention estimates that 1.2 million people in the United States are infected with HIV and that nearly 1 in 5 don’t know they have it.
Head for the Hill: ACA Pushes More Doctors onto the Ballot
Increasingly, it’s not Mr. Smith who goes to Washington – it’s Dr. Smith.
Currently, 20 physicians serve in the 112th Congress: 3 in the Senate and 17 in the House.
This year, 42 doctors are running for a seat in the next Congress; 17 of those are seeking reelection, according to the American Medical Association.
While their reasons for suspending their medical careers in favor of public service vary, many say the steady increase of physician legislators is largely because of the Affordable Care Act.
"This is likely a tectonic shift that has now occurred," said Rep. Michael Burgess (R-Tex.), a gynecologist seeking reelection in that state’s 26th district. "Historically, doctors have been so busy taking care of their patients, raising their families, running their offices that they haven’t paid a lot of attention to politics. But [it’s the] issues surrounding the Affordable Care Act, [that have] driven this."
Dr. John McGoff, an emergency physician running to represent Indiana’s 5th congressional district, said that he believes doctors running for office think the ACA allows for too much government control of health care and threatens the doctor-patient relationship.
"I think most people would like to get back to how it was in the old days, where there was a patient-physician relationship and you didn’t have an insurance company or some type of government entity in between," Dr. McGoff, a Republican, said in an interview.
Emergency physician Randy Jotte wants to represent Missouri’s 2nd congressional district. Dr. Jotte, also a Republican, said that he decided to run to address increasing demands on emergency physicians with limited resources, as well as fighting to repeal the ACA.
The health reform law doesn’t give physicians enough resources to handle a growing number of patients and increasing demand to improve quality and to lower costs, Dr. Jotte said, adding that as health reform took the national stage, the general public became more aware of the issues at stake, and now they’re looking to those who understand the system to help shape it.
"People are much more cognizant of some of the needs and weaknesses in the health care system. ... They look to physicians, both the physicians that are in their offices as well as physicians in Congress and saying ‘how can we do this better.’ "
Most physicians (90%) serving in Congress are Republicans; of the 42 doctors running for Congress this year, 25 are Republicans, 16 are Democrats, and 1 is Libertarian.
Dr. McGoff speculated as to why. "Physicians tend to be somewhat conservative," he said. "Less government, low taxes, individual responsibility, [and] strong national defense; those are the core principles of the Republican Party and I think that resonates well with a lot of physicians."
Rep. Phil Gingrey (R-Ga.), a gynecologist seeking reelection to the House representing Georgia’s 11th district, pointed out that many doctors are also small business owners.
"They’re running these small businesses and they’re seeing the burdens of rules and regulations run amok ... and they’re railing against that ... realizing that a federal government that can give everything can also take away everything from you," he said in an interview.
While Dr. James Buckmaster is a Democrat, he too opposes the ACA. The family physician seeks to represent Kentucky’s 1st district in Congress.
If elected, Dr. Buckmaster said he’d like to see a full repeal and replacement of the health law with a more affordable option that includes fewer regulations on health care professionals. He added that his medical peers are not only passionate about the issues, but are also hard wired to make tough decisions.
"We tend to respond to problems ... we tend to want to interact with them, fix them before they get out of control. I think that’s just the basic way that we’re wired," Dr. Buckmaster said in an interview.
"We’re intelligent people, and we’re confident and rather autonomous; we make decisions each day and we stick by them. Those are the characteristics that we want in our elected officials, and we just aren’t seeing it," he added.
Dr. Evan Saulino, who serves on the board of directors for Doctors for America, noted that research over the last decade has highlighted issues in health care delivery and outcomes. That data, coupled with disappointment with the original model of managed care, fueled discussions about how to improve health care delivery, which motivated doctors to get involved, according to Dr. Saulino, a family physician in Portland, Ore. That involvement has only snowballed with the implementation of health care reform.
"It’s a passion that people recognize that this is something that can shape the future of health care so they’re jumping in to play a role," Dr. Saulino said in an interview.
But the transition from doctor to representative can be a little rocky, Rep. Burgess noted.
"It’s pretty frustrating to work here because you’re in a big, large, slow-moving body. Not everyone will do what you say ... most physicians are used to being pretty much in command of their surroundings, whether it be the operating room, their office, their hospital, or the hospital board," he said in an interview. Regardless, Rep. Burgess doesn’t regret his choice; and neither does Rep. Gingrey, who said he decided to serve in Congress after he realized the difference he could make.
"I realized that I would be giving up my medical practice, something that I dearly loved, but that on a larger scale, I would be helping [million of] patients rather than just 3,000 or 4,000," Rep. Gingrey said.
Rep. Gingrey serves as cochair of the Republican Doctors Caucus, a Congressional interest group made up of 13 physicians and eight other health professionals including dentists and nurses. The group was formed in 2009 to protest the Affordable Care Act, among other aims. He said that more physicians in the House means greater clout for health care issues on Capitol Hill.
"We’re just bringing more in numbers and in clinical experience in dealing with patients and health care issues in the private sector," Rep. Gingery said in an interview. "To bring that to Washington, I think, has been a tremendous asset for us." As of yet, Democrats have no organization or committee similar to the group.
Many believe that the number of physician-legislators will only continue to grow. Health care issues, such as Medicare, will affect generations to come, Dr. Jotte said. "Even if we [repeal the ACA] we still have all the same problems that frustrate physicians ... and that gets you emotionally. Emotion is what draws people to action."
Increasingly, it’s not Mr. Smith who goes to Washington – it’s Dr. Smith.
Currently, 20 physicians serve in the 112th Congress: 3 in the Senate and 17 in the House.
This year, 42 doctors are running for a seat in the next Congress; 17 of those are seeking reelection, according to the American Medical Association.
While their reasons for suspending their medical careers in favor of public service vary, many say the steady increase of physician legislators is largely because of the Affordable Care Act.
"This is likely a tectonic shift that has now occurred," said Rep. Michael Burgess (R-Tex.), a gynecologist seeking reelection in that state’s 26th district. "Historically, doctors have been so busy taking care of their patients, raising their families, running their offices that they haven’t paid a lot of attention to politics. But [it’s the] issues surrounding the Affordable Care Act, [that have] driven this."
Dr. John McGoff, an emergency physician running to represent Indiana’s 5th congressional district, said that he believes doctors running for office think the ACA allows for too much government control of health care and threatens the doctor-patient relationship.
"I think most people would like to get back to how it was in the old days, where there was a patient-physician relationship and you didn’t have an insurance company or some type of government entity in between," Dr. McGoff, a Republican, said in an interview.
Emergency physician Randy Jotte wants to represent Missouri’s 2nd congressional district. Dr. Jotte, also a Republican, said that he decided to run to address increasing demands on emergency physicians with limited resources, as well as fighting to repeal the ACA.
The health reform law doesn’t give physicians enough resources to handle a growing number of patients and increasing demand to improve quality and to lower costs, Dr. Jotte said, adding that as health reform took the national stage, the general public became more aware of the issues at stake, and now they’re looking to those who understand the system to help shape it.
"People are much more cognizant of some of the needs and weaknesses in the health care system. ... They look to physicians, both the physicians that are in their offices as well as physicians in Congress and saying ‘how can we do this better.’ "
Most physicians (90%) serving in Congress are Republicans; of the 42 doctors running for Congress this year, 25 are Republicans, 16 are Democrats, and 1 is Libertarian.
Dr. McGoff speculated as to why. "Physicians tend to be somewhat conservative," he said. "Less government, low taxes, individual responsibility, [and] strong national defense; those are the core principles of the Republican Party and I think that resonates well with a lot of physicians."
Rep. Phil Gingrey (R-Ga.), a gynecologist seeking reelection to the House representing Georgia’s 11th district, pointed out that many doctors are also small business owners.
"They’re running these small businesses and they’re seeing the burdens of rules and regulations run amok ... and they’re railing against that ... realizing that a federal government that can give everything can also take away everything from you," he said in an interview.
While Dr. James Buckmaster is a Democrat, he too opposes the ACA. The family physician seeks to represent Kentucky’s 1st district in Congress.
If elected, Dr. Buckmaster said he’d like to see a full repeal and replacement of the health law with a more affordable option that includes fewer regulations on health care professionals. He added that his medical peers are not only passionate about the issues, but are also hard wired to make tough decisions.
"We tend to respond to problems ... we tend to want to interact with them, fix them before they get out of control. I think that’s just the basic way that we’re wired," Dr. Buckmaster said in an interview.
"We’re intelligent people, and we’re confident and rather autonomous; we make decisions each day and we stick by them. Those are the characteristics that we want in our elected officials, and we just aren’t seeing it," he added.
Dr. Evan Saulino, who serves on the board of directors for Doctors for America, noted that research over the last decade has highlighted issues in health care delivery and outcomes. That data, coupled with disappointment with the original model of managed care, fueled discussions about how to improve health care delivery, which motivated doctors to get involved, according to Dr. Saulino, a family physician in Portland, Ore. That involvement has only snowballed with the implementation of health care reform.
"It’s a passion that people recognize that this is something that can shape the future of health care so they’re jumping in to play a role," Dr. Saulino said in an interview.
But the transition from doctor to representative can be a little rocky, Rep. Burgess noted.
"It’s pretty frustrating to work here because you’re in a big, large, slow-moving body. Not everyone will do what you say ... most physicians are used to being pretty much in command of their surroundings, whether it be the operating room, their office, their hospital, or the hospital board," he said in an interview. Regardless, Rep. Burgess doesn’t regret his choice; and neither does Rep. Gingrey, who said he decided to serve in Congress after he realized the difference he could make.
"I realized that I would be giving up my medical practice, something that I dearly loved, but that on a larger scale, I would be helping [million of] patients rather than just 3,000 or 4,000," Rep. Gingrey said.
Rep. Gingrey serves as cochair of the Republican Doctors Caucus, a Congressional interest group made up of 13 physicians and eight other health professionals including dentists and nurses. The group was formed in 2009 to protest the Affordable Care Act, among other aims. He said that more physicians in the House means greater clout for health care issues on Capitol Hill.
"We’re just bringing more in numbers and in clinical experience in dealing with patients and health care issues in the private sector," Rep. Gingery said in an interview. "To bring that to Washington, I think, has been a tremendous asset for us." As of yet, Democrats have no organization or committee similar to the group.
Many believe that the number of physician-legislators will only continue to grow. Health care issues, such as Medicare, will affect generations to come, Dr. Jotte said. "Even if we [repeal the ACA] we still have all the same problems that frustrate physicians ... and that gets you emotionally. Emotion is what draws people to action."
Increasingly, it’s not Mr. Smith who goes to Washington – it’s Dr. Smith.
Currently, 20 physicians serve in the 112th Congress: 3 in the Senate and 17 in the House.
This year, 42 doctors are running for a seat in the next Congress; 17 of those are seeking reelection, according to the American Medical Association.
While their reasons for suspending their medical careers in favor of public service vary, many say the steady increase of physician legislators is largely because of the Affordable Care Act.
"This is likely a tectonic shift that has now occurred," said Rep. Michael Burgess (R-Tex.), a gynecologist seeking reelection in that state’s 26th district. "Historically, doctors have been so busy taking care of their patients, raising their families, running their offices that they haven’t paid a lot of attention to politics. But [it’s the] issues surrounding the Affordable Care Act, [that have] driven this."
Dr. John McGoff, an emergency physician running to represent Indiana’s 5th congressional district, said that he believes doctors running for office think the ACA allows for too much government control of health care and threatens the doctor-patient relationship.
"I think most people would like to get back to how it was in the old days, where there was a patient-physician relationship and you didn’t have an insurance company or some type of government entity in between," Dr. McGoff, a Republican, said in an interview.
Emergency physician Randy Jotte wants to represent Missouri’s 2nd congressional district. Dr. Jotte, also a Republican, said that he decided to run to address increasing demands on emergency physicians with limited resources, as well as fighting to repeal the ACA.
The health reform law doesn’t give physicians enough resources to handle a growing number of patients and increasing demand to improve quality and to lower costs, Dr. Jotte said, adding that as health reform took the national stage, the general public became more aware of the issues at stake, and now they’re looking to those who understand the system to help shape it.
"People are much more cognizant of some of the needs and weaknesses in the health care system. ... They look to physicians, both the physicians that are in their offices as well as physicians in Congress and saying ‘how can we do this better.’ "
Most physicians (90%) serving in Congress are Republicans; of the 42 doctors running for Congress this year, 25 are Republicans, 16 are Democrats, and 1 is Libertarian.
Dr. McGoff speculated as to why. "Physicians tend to be somewhat conservative," he said. "Less government, low taxes, individual responsibility, [and] strong national defense; those are the core principles of the Republican Party and I think that resonates well with a lot of physicians."
Rep. Phil Gingrey (R-Ga.), a gynecologist seeking reelection to the House representing Georgia’s 11th district, pointed out that many doctors are also small business owners.
"They’re running these small businesses and they’re seeing the burdens of rules and regulations run amok ... and they’re railing against that ... realizing that a federal government that can give everything can also take away everything from you," he said in an interview.
While Dr. James Buckmaster is a Democrat, he too opposes the ACA. The family physician seeks to represent Kentucky’s 1st district in Congress.
If elected, Dr. Buckmaster said he’d like to see a full repeal and replacement of the health law with a more affordable option that includes fewer regulations on health care professionals. He added that his medical peers are not only passionate about the issues, but are also hard wired to make tough decisions.
"We tend to respond to problems ... we tend to want to interact with them, fix them before they get out of control. I think that’s just the basic way that we’re wired," Dr. Buckmaster said in an interview.
"We’re intelligent people, and we’re confident and rather autonomous; we make decisions each day and we stick by them. Those are the characteristics that we want in our elected officials, and we just aren’t seeing it," he added.
Dr. Evan Saulino, who serves on the board of directors for Doctors for America, noted that research over the last decade has highlighted issues in health care delivery and outcomes. That data, coupled with disappointment with the original model of managed care, fueled discussions about how to improve health care delivery, which motivated doctors to get involved, according to Dr. Saulino, a family physician in Portland, Ore. That involvement has only snowballed with the implementation of health care reform.
"It’s a passion that people recognize that this is something that can shape the future of health care so they’re jumping in to play a role," Dr. Saulino said in an interview.
But the transition from doctor to representative can be a little rocky, Rep. Burgess noted.
"It’s pretty frustrating to work here because you’re in a big, large, slow-moving body. Not everyone will do what you say ... most physicians are used to being pretty much in command of their surroundings, whether it be the operating room, their office, their hospital, or the hospital board," he said in an interview. Regardless, Rep. Burgess doesn’t regret his choice; and neither does Rep. Gingrey, who said he decided to serve in Congress after he realized the difference he could make.
"I realized that I would be giving up my medical practice, something that I dearly loved, but that on a larger scale, I would be helping [million of] patients rather than just 3,000 or 4,000," Rep. Gingrey said.
Rep. Gingrey serves as cochair of the Republican Doctors Caucus, a Congressional interest group made up of 13 physicians and eight other health professionals including dentists and nurses. The group was formed in 2009 to protest the Affordable Care Act, among other aims. He said that more physicians in the House means greater clout for health care issues on Capitol Hill.
"We’re just bringing more in numbers and in clinical experience in dealing with patients and health care issues in the private sector," Rep. Gingery said in an interview. "To bring that to Washington, I think, has been a tremendous asset for us." As of yet, Democrats have no organization or committee similar to the group.
Many believe that the number of physician-legislators will only continue to grow. Health care issues, such as Medicare, will affect generations to come, Dr. Jotte said. "Even if we [repeal the ACA] we still have all the same problems that frustrate physicians ... and that gets you emotionally. Emotion is what draws people to action."