User login
Constructive Criticism
This is the first in a two-part series about how to provide constructive criticism to your hospitalist peers.
Part of improving your performance is learning from other hospitalists on a regular basis. You can do this through observation or discussion, and—when appropriate—by offering or receiving constructive criticism.
There are two types of physician-to-physician constructive criticism: When discussing perceived poor handling of a patient’s case, comments should take place within a formal peer review. Concerns about a physician’s non-clinical performance, such as communications problems or lack of availability, can be handled in a one-on-one conversation. Herein we’ll examine the peer review process; next month we’ll take a look at how and when to give constructive criticism to a peer informally.
Why Use Peer Review?
When a hospitalist notices a colleague’s clinical error or lack of judgment, it should be addressed in the program’s next peer review meeting, both for legal and procedural reasons.
“The key thing to understand is that ‘peer review’ offers certain protections for physicians and their colleagues,” explains Richard Rohr, MD, director, Hospitalist Service, Milford Hospital, Milford, Conn. “Ordinarily, if I discuss [another physician’s] case and render my opinion, then—in principle—if that patient were to file a lawsuit, they could subpoena me to testify about what I thought about their case. In the past, this had a chilling effect on peer review.”
Due to state laws passed years ago, peer review meetings now offer protection against subpoena. “Peer review meetings are protected,” says Dr. Rohr. “They can’t be used in court, and this makes it possible to have an organized peer review where you look at physicians’ work and provide an opinion about that work without fear of being drawn into a legal situation.”
The bottom line: “If you want to talk to another physician about their case, do so within [the peer review structure] so you’re legally protected,” says Dr. Rohr.
Focus on Improvement
When discussing a specific case or physician, remember that the reason for doing so is to improve quality of care. “Every practice should sit down, look at specific cases, and talk about possible areas of improvement,” says Dr. Rohr. “You need to take minutes of these meetings that are marked as confidential.”
The key to improvement is having an open discussion in each peer review meeting. “A good meeting is educational,” says Dr. Rohr. “The objective is to support each other and improve performance. A lot depends on the attitude that people bring to it. You have to not be afraid to say something; you must be willing to express opinions, or you’ll have a wasted meeting.”
Sometimes you may find that the problem goes beyond a single physician’s actions on a case. “If there is a problem with a case, find out whether it’s an aberration or if the problem needs to be addressed,” says Dr. Rohr. “Some things are not a physician’s fault, so much as [they are] signs that a medical system doesn’t work as effectively as it should or [that there is] a general lack of training. For example, an ER [emergency room] doctor misses a fracture. Was finding that fracture outside his competency? Does he need training reading X-rays, or can you manage to get radiologists in to check X-rays fast enough to become part of the process?”
Use a Set Structure
It’s up to the hospital medicine program director to set up a peer review process, which should be done within the structure established by the hospital. Peer review meetings “should be done on a regular basis,” advises Dr. Rohr. “How often depends on the volume of the program, but a typical group should meet monthly. You’ll probably look at three or four cases, which is a reasonable number to cover in one meeting. Look at unexpected mortalities or complications—you have a responsibility to the public to examine these.”
You might do best by bringing in an outside facilitator for the meetings. This creates an impartial atmosphere for discussions. “We bring in an external facilitator from a local teaching hospital,” says Dr. Rohr. “It’s good to have an educator lead the meeting; someone from academia will have a greater fund of knowledge and [a stronger] grasp of the medical literature, which helps bring the discussion to a more educational level. Everyone respects medical science.”
Note that the facilitator may need to be credentialed as a member of the medical staff in order for the proceedings to be protected from legal discovery.
“Peer review is difficult in smaller practices, because everyone knows everyone and they may be uncomfortable addressing problems,” explains Dr. Rohr. “Here, it’s especially helpful to have a leader from the outside who can render opinions and get everyone to chime in and render their own opinions.”
Remember that your peer review system is reportable. “As part of the hospital’s peer review structure, you’ll have to report findings from the meetings,” adds Dr. Rohr. “If someone is showing a pattern, these things have to be trended. Do they need training, or should they be dismissed?”
Giving Feedback through Peer Review
When you participate in a peer review discussion, don’t let your comments get too personal or subjective. “The most important thing is to keep it professional and make it educational to the greatest extent possible,” says Dr. Rohr. “Reference facts in the medical literature as often as possible. Point to something that’s been published to support your opinion. Base your comments on what’s known, and apply that to your analysis of the case.”
An evidence-based opinion doesn’t have to cite specific details; as long as you’re aware of major papers on the topic, you should have a grounded opinion.
Finally, as a physician participating in a peer review discussion, think before you speak. “Peer review works best when you have a basic respect for each other, as well as basic humility,” he says. TH
Jane Jerrard has written for The Hospitalist since 2005.
This is the first in a two-part series about how to provide constructive criticism to your hospitalist peers.
Part of improving your performance is learning from other hospitalists on a regular basis. You can do this through observation or discussion, and—when appropriate—by offering or receiving constructive criticism.
There are two types of physician-to-physician constructive criticism: When discussing perceived poor handling of a patient’s case, comments should take place within a formal peer review. Concerns about a physician’s non-clinical performance, such as communications problems or lack of availability, can be handled in a one-on-one conversation. Herein we’ll examine the peer review process; next month we’ll take a look at how and when to give constructive criticism to a peer informally.
Why Use Peer Review?
When a hospitalist notices a colleague’s clinical error or lack of judgment, it should be addressed in the program’s next peer review meeting, both for legal and procedural reasons.
“The key thing to understand is that ‘peer review’ offers certain protections for physicians and their colleagues,” explains Richard Rohr, MD, director, Hospitalist Service, Milford Hospital, Milford, Conn. “Ordinarily, if I discuss [another physician’s] case and render my opinion, then—in principle—if that patient were to file a lawsuit, they could subpoena me to testify about what I thought about their case. In the past, this had a chilling effect on peer review.”
Due to state laws passed years ago, peer review meetings now offer protection against subpoena. “Peer review meetings are protected,” says Dr. Rohr. “They can’t be used in court, and this makes it possible to have an organized peer review where you look at physicians’ work and provide an opinion about that work without fear of being drawn into a legal situation.”
The bottom line: “If you want to talk to another physician about their case, do so within [the peer review structure] so you’re legally protected,” says Dr. Rohr.
Focus on Improvement
When discussing a specific case or physician, remember that the reason for doing so is to improve quality of care. “Every practice should sit down, look at specific cases, and talk about possible areas of improvement,” says Dr. Rohr. “You need to take minutes of these meetings that are marked as confidential.”
The key to improvement is having an open discussion in each peer review meeting. “A good meeting is educational,” says Dr. Rohr. “The objective is to support each other and improve performance. A lot depends on the attitude that people bring to it. You have to not be afraid to say something; you must be willing to express opinions, or you’ll have a wasted meeting.”
Sometimes you may find that the problem goes beyond a single physician’s actions on a case. “If there is a problem with a case, find out whether it’s an aberration or if the problem needs to be addressed,” says Dr. Rohr. “Some things are not a physician’s fault, so much as [they are] signs that a medical system doesn’t work as effectively as it should or [that there is] a general lack of training. For example, an ER [emergency room] doctor misses a fracture. Was finding that fracture outside his competency? Does he need training reading X-rays, or can you manage to get radiologists in to check X-rays fast enough to become part of the process?”
Use a Set Structure
It’s up to the hospital medicine program director to set up a peer review process, which should be done within the structure established by the hospital. Peer review meetings “should be done on a regular basis,” advises Dr. Rohr. “How often depends on the volume of the program, but a typical group should meet monthly. You’ll probably look at three or four cases, which is a reasonable number to cover in one meeting. Look at unexpected mortalities or complications—you have a responsibility to the public to examine these.”
You might do best by bringing in an outside facilitator for the meetings. This creates an impartial atmosphere for discussions. “We bring in an external facilitator from a local teaching hospital,” says Dr. Rohr. “It’s good to have an educator lead the meeting; someone from academia will have a greater fund of knowledge and [a stronger] grasp of the medical literature, which helps bring the discussion to a more educational level. Everyone respects medical science.”
Note that the facilitator may need to be credentialed as a member of the medical staff in order for the proceedings to be protected from legal discovery.
“Peer review is difficult in smaller practices, because everyone knows everyone and they may be uncomfortable addressing problems,” explains Dr. Rohr. “Here, it’s especially helpful to have a leader from the outside who can render opinions and get everyone to chime in and render their own opinions.”
Remember that your peer review system is reportable. “As part of the hospital’s peer review structure, you’ll have to report findings from the meetings,” adds Dr. Rohr. “If someone is showing a pattern, these things have to be trended. Do they need training, or should they be dismissed?”
Giving Feedback through Peer Review
When you participate in a peer review discussion, don’t let your comments get too personal or subjective. “The most important thing is to keep it professional and make it educational to the greatest extent possible,” says Dr. Rohr. “Reference facts in the medical literature as often as possible. Point to something that’s been published to support your opinion. Base your comments on what’s known, and apply that to your analysis of the case.”
An evidence-based opinion doesn’t have to cite specific details; as long as you’re aware of major papers on the topic, you should have a grounded opinion.
Finally, as a physician participating in a peer review discussion, think before you speak. “Peer review works best when you have a basic respect for each other, as well as basic humility,” he says. TH
Jane Jerrard has written for The Hospitalist since 2005.
This is the first in a two-part series about how to provide constructive criticism to your hospitalist peers.
Part of improving your performance is learning from other hospitalists on a regular basis. You can do this through observation or discussion, and—when appropriate—by offering or receiving constructive criticism.
There are two types of physician-to-physician constructive criticism: When discussing perceived poor handling of a patient’s case, comments should take place within a formal peer review. Concerns about a physician’s non-clinical performance, such as communications problems or lack of availability, can be handled in a one-on-one conversation. Herein we’ll examine the peer review process; next month we’ll take a look at how and when to give constructive criticism to a peer informally.
Why Use Peer Review?
When a hospitalist notices a colleague’s clinical error or lack of judgment, it should be addressed in the program’s next peer review meeting, both for legal and procedural reasons.
“The key thing to understand is that ‘peer review’ offers certain protections for physicians and their colleagues,” explains Richard Rohr, MD, director, Hospitalist Service, Milford Hospital, Milford, Conn. “Ordinarily, if I discuss [another physician’s] case and render my opinion, then—in principle—if that patient were to file a lawsuit, they could subpoena me to testify about what I thought about their case. In the past, this had a chilling effect on peer review.”
Due to state laws passed years ago, peer review meetings now offer protection against subpoena. “Peer review meetings are protected,” says Dr. Rohr. “They can’t be used in court, and this makes it possible to have an organized peer review where you look at physicians’ work and provide an opinion about that work without fear of being drawn into a legal situation.”
The bottom line: “If you want to talk to another physician about their case, do so within [the peer review structure] so you’re legally protected,” says Dr. Rohr.
Focus on Improvement
When discussing a specific case or physician, remember that the reason for doing so is to improve quality of care. “Every practice should sit down, look at specific cases, and talk about possible areas of improvement,” says Dr. Rohr. “You need to take minutes of these meetings that are marked as confidential.”
The key to improvement is having an open discussion in each peer review meeting. “A good meeting is educational,” says Dr. Rohr. “The objective is to support each other and improve performance. A lot depends on the attitude that people bring to it. You have to not be afraid to say something; you must be willing to express opinions, or you’ll have a wasted meeting.”
Sometimes you may find that the problem goes beyond a single physician’s actions on a case. “If there is a problem with a case, find out whether it’s an aberration or if the problem needs to be addressed,” says Dr. Rohr. “Some things are not a physician’s fault, so much as [they are] signs that a medical system doesn’t work as effectively as it should or [that there is] a general lack of training. For example, an ER [emergency room] doctor misses a fracture. Was finding that fracture outside his competency? Does he need training reading X-rays, or can you manage to get radiologists in to check X-rays fast enough to become part of the process?”
Use a Set Structure
It’s up to the hospital medicine program director to set up a peer review process, which should be done within the structure established by the hospital. Peer review meetings “should be done on a regular basis,” advises Dr. Rohr. “How often depends on the volume of the program, but a typical group should meet monthly. You’ll probably look at three or four cases, which is a reasonable number to cover in one meeting. Look at unexpected mortalities or complications—you have a responsibility to the public to examine these.”
You might do best by bringing in an outside facilitator for the meetings. This creates an impartial atmosphere for discussions. “We bring in an external facilitator from a local teaching hospital,” says Dr. Rohr. “It’s good to have an educator lead the meeting; someone from academia will have a greater fund of knowledge and [a stronger] grasp of the medical literature, which helps bring the discussion to a more educational level. Everyone respects medical science.”
Note that the facilitator may need to be credentialed as a member of the medical staff in order for the proceedings to be protected from legal discovery.
“Peer review is difficult in smaller practices, because everyone knows everyone and they may be uncomfortable addressing problems,” explains Dr. Rohr. “Here, it’s especially helpful to have a leader from the outside who can render opinions and get everyone to chime in and render their own opinions.”
Remember that your peer review system is reportable. “As part of the hospital’s peer review structure, you’ll have to report findings from the meetings,” adds Dr. Rohr. “If someone is showing a pattern, these things have to be trended. Do they need training, or should they be dismissed?”
Giving Feedback through Peer Review
When you participate in a peer review discussion, don’t let your comments get too personal or subjective. “The most important thing is to keep it professional and make it educational to the greatest extent possible,” says Dr. Rohr. “Reference facts in the medical literature as often as possible. Point to something that’s been published to support your opinion. Base your comments on what’s known, and apply that to your analysis of the case.”
An evidence-based opinion doesn’t have to cite specific details; as long as you’re aware of major papers on the topic, you should have a grounded opinion.
Finally, as a physician participating in a peer review discussion, think before you speak. “Peer review works best when you have a basic respect for each other, as well as basic humility,” he says. TH
Jane Jerrard has written for The Hospitalist since 2005.
New Party in Power
Due to an overwhelming number of Democratic victories in last November’s midterm elections, the 110th Congress, which took office early this year, has new leaders and a new agenda that could bode well for healthcare legislation.
In this article, Laura Allendorf, SHM’s senior advisor for advocacy and government affairs, explains what the changes in Congress could mean for the near future of healthcare and for the legislation and issues that SHM strongly supports. Based in Washington, D.C., Allendorf is responsible for providing government relations services for SHM. She advises the organization on key legislative and regulatory healthcare issues before Congress and the Bush administration, and she works with SHM leaders and staff on policy development and advocacy strategies.
Majority Rules
The midterm elections brought about a shift in power that goes deeper than numbers of bodies on each side of the aisle. “The Democrats are now the majority in both chambers. This is significant, because they’ve been the minority since 1994, says Allendorf. “As the majority, they control the agenda now—on healthcare and other issues—and they also head the key committees.”
What can we expect to see from the Democratic Congress? “We should expect to see a more expansionist agenda” in general, according to Allendorf. “We’re going to see more activism in the area of healthcare, but whether anything gets done remains to be seen. There’s only a slim majority in the Senate, and President Bush can wield his veto pen. For example, the Democrats would like to give [the Department of] Health and Human Services the power to negotiate drug prices with pharmaceutical companies, specifically on Medicare Part D, but Bush won’t like that.”
Much depends on the issues at hand, as well as on how much bipartisan support exists for each specific bill.
Changing of the Guard
Anyone who glances at the newspaper knows that Democrat Nancy Pelosi (Calif.) is now the Speaker of the House. But Democratic leadership goes much deeper than that because the ruling party has also taken over leadership of Congressional committees. These committees shape the legislation introduced in the House and Senate.
As of press time, Congressional committee assignments had not been formally decided—at least not in the Senate—but many assignments were certain. “Typically, the highest-ranking Democrat [House or Senate] on a committee will become the new head, though Nancy Pelosi isn’t sticking to that,” explains Allendorf. “Pete Stark (D-Calif.) will likely chair the Ways and Means Committee’s Subcommittee on Health, and Charles Rangel (D-N.Y.) will head the House Ways and Means Committee. John Dingell (D-Mich.) will chair the House Energy and Commerce Committee.” (For more on committee chairs, visit http://media-newswire.com/release_1040623.html.)
For a complete list of committee members, visit SHM’s new Legislative Action Center at http://capwiz.com/hospitalmedicine/home/. See “New Advocacy Tool Available,” for more information on the Legislative Action Center, above.)
Starting Over on Key Issues
Many of the bills introduced in 2006—particularly spending bills—were not voted on by the end of the lame duck session last fall. That means that these bills must be reintroduced in the new year. Bills that recommend funding changes are frozen, so agencies continue to receive 2006 funding until the new Congress votes to change their budget.
“All bills have to be reintroduced in the 110th,” stresses Allendorf. “It will take some time—how much depends on the issue. The Democrats may want to hold hearings on legislation, or they may simply dust off legislation that was introduced last year.”
The Democrats are expected to move on many of the issues that SHM has been lobbying for. “They’ve said that they want to reform the healthcare system,” says Allendorf. “Top issues include providing coverage to the uninsured, reforming Medicare Part D, and resolving the physician payment issue.”
Allendorf believes that there will be a bipartisan effort to push through physician payment reform. “There are some 265 members of Congress who requested action on this issue this year [in 2006],” she points out. “There’s a genuine interest and desire to address physician payment reform and pay-for-performance as well. They may differ on how quickly they want to move on some of these.”
The news is not so good on the issue of gainsharing, where physicians are allowed to share the profits realized by a hospital’s cost reductions when linked to specific best practices. “Representative Nancy Johnson (R-Conn.) was a big proponent of this issue in the House, and she was not re-elected,” says Allendorf. “Stark is an opponent of gainsharing, so there may not be the same Congressional push behind it—at least in the House.”
However, the unexpected gainsharing demonstration projects approved in 2006 are underway, and Congress will hear reports on those in several years, once the projects have been analyzed.
Another issue that may not be addressed is liability. “Medical liability reform will be on the back burner,” warns Allendorf. “It’s generally not supported by the Democrats.”
In 2006, SHM supported increased funding for the Agency for Healthcare Research and Quality (AHRQ)—this was one of the major issues addressed by members during Legislative Advocacy Day during the Annual Meeting in Washington, D.C. Whether the next budget includes more money for the agency remains to be seen. “The Democrats support increased funding for NIH (National Institutes of Health), AHRQ, and other healthcare agencies,” says Allendorf. “There’s certainly political will, but where is the money going to come from?”
New Congress, New Issues
What about new issues? “Democrats have signaled that healthcare access for the uninsured will be a priority,” says Allendorf. “I think that we’ll see new legislation with a renewed emphasis on access to care.”
SHM’s Public Policy Committee will be waiting for the first legislation to be introduced regarding coverage for uninsured Americans. “This is an issue that SHM is strongly in favor of,” explains Allendorf. “SHM will look at any bills that come out on this issue and then form a policy.”
Regardless of which healthcare issues come to the forefront first, SHM’s Public Policy Committee, staff, and members are likely to be more active than ever. “I see a very busy year legislatively for SHM,” says Allendorf. TH
Jane Jerrard regularly writes “Public Policy” for The Hospitalist.
Due to an overwhelming number of Democratic victories in last November’s midterm elections, the 110th Congress, which took office early this year, has new leaders and a new agenda that could bode well for healthcare legislation.
In this article, Laura Allendorf, SHM’s senior advisor for advocacy and government affairs, explains what the changes in Congress could mean for the near future of healthcare and for the legislation and issues that SHM strongly supports. Based in Washington, D.C., Allendorf is responsible for providing government relations services for SHM. She advises the organization on key legislative and regulatory healthcare issues before Congress and the Bush administration, and she works with SHM leaders and staff on policy development and advocacy strategies.
Majority Rules
The midterm elections brought about a shift in power that goes deeper than numbers of bodies on each side of the aisle. “The Democrats are now the majority in both chambers. This is significant, because they’ve been the minority since 1994, says Allendorf. “As the majority, they control the agenda now—on healthcare and other issues—and they also head the key committees.”
What can we expect to see from the Democratic Congress? “We should expect to see a more expansionist agenda” in general, according to Allendorf. “We’re going to see more activism in the area of healthcare, but whether anything gets done remains to be seen. There’s only a slim majority in the Senate, and President Bush can wield his veto pen. For example, the Democrats would like to give [the Department of] Health and Human Services the power to negotiate drug prices with pharmaceutical companies, specifically on Medicare Part D, but Bush won’t like that.”
Much depends on the issues at hand, as well as on how much bipartisan support exists for each specific bill.
Changing of the Guard
Anyone who glances at the newspaper knows that Democrat Nancy Pelosi (Calif.) is now the Speaker of the House. But Democratic leadership goes much deeper than that because the ruling party has also taken over leadership of Congressional committees. These committees shape the legislation introduced in the House and Senate.
As of press time, Congressional committee assignments had not been formally decided—at least not in the Senate—but many assignments were certain. “Typically, the highest-ranking Democrat [House or Senate] on a committee will become the new head, though Nancy Pelosi isn’t sticking to that,” explains Allendorf. “Pete Stark (D-Calif.) will likely chair the Ways and Means Committee’s Subcommittee on Health, and Charles Rangel (D-N.Y.) will head the House Ways and Means Committee. John Dingell (D-Mich.) will chair the House Energy and Commerce Committee.” (For more on committee chairs, visit http://media-newswire.com/release_1040623.html.)
For a complete list of committee members, visit SHM’s new Legislative Action Center at http://capwiz.com/hospitalmedicine/home/. See “New Advocacy Tool Available,” for more information on the Legislative Action Center, above.)
Starting Over on Key Issues
Many of the bills introduced in 2006—particularly spending bills—were not voted on by the end of the lame duck session last fall. That means that these bills must be reintroduced in the new year. Bills that recommend funding changes are frozen, so agencies continue to receive 2006 funding until the new Congress votes to change their budget.
“All bills have to be reintroduced in the 110th,” stresses Allendorf. “It will take some time—how much depends on the issue. The Democrats may want to hold hearings on legislation, or they may simply dust off legislation that was introduced last year.”
The Democrats are expected to move on many of the issues that SHM has been lobbying for. “They’ve said that they want to reform the healthcare system,” says Allendorf. “Top issues include providing coverage to the uninsured, reforming Medicare Part D, and resolving the physician payment issue.”
Allendorf believes that there will be a bipartisan effort to push through physician payment reform. “There are some 265 members of Congress who requested action on this issue this year [in 2006],” she points out. “There’s a genuine interest and desire to address physician payment reform and pay-for-performance as well. They may differ on how quickly they want to move on some of these.”
The news is not so good on the issue of gainsharing, where physicians are allowed to share the profits realized by a hospital’s cost reductions when linked to specific best practices. “Representative Nancy Johnson (R-Conn.) was a big proponent of this issue in the House, and she was not re-elected,” says Allendorf. “Stark is an opponent of gainsharing, so there may not be the same Congressional push behind it—at least in the House.”
However, the unexpected gainsharing demonstration projects approved in 2006 are underway, and Congress will hear reports on those in several years, once the projects have been analyzed.
Another issue that may not be addressed is liability. “Medical liability reform will be on the back burner,” warns Allendorf. “It’s generally not supported by the Democrats.”
In 2006, SHM supported increased funding for the Agency for Healthcare Research and Quality (AHRQ)—this was one of the major issues addressed by members during Legislative Advocacy Day during the Annual Meeting in Washington, D.C. Whether the next budget includes more money for the agency remains to be seen. “The Democrats support increased funding for NIH (National Institutes of Health), AHRQ, and other healthcare agencies,” says Allendorf. “There’s certainly political will, but where is the money going to come from?”
New Congress, New Issues
What about new issues? “Democrats have signaled that healthcare access for the uninsured will be a priority,” says Allendorf. “I think that we’ll see new legislation with a renewed emphasis on access to care.”
SHM’s Public Policy Committee will be waiting for the first legislation to be introduced regarding coverage for uninsured Americans. “This is an issue that SHM is strongly in favor of,” explains Allendorf. “SHM will look at any bills that come out on this issue and then form a policy.”
Regardless of which healthcare issues come to the forefront first, SHM’s Public Policy Committee, staff, and members are likely to be more active than ever. “I see a very busy year legislatively for SHM,” says Allendorf. TH
Jane Jerrard regularly writes “Public Policy” for The Hospitalist.
Due to an overwhelming number of Democratic victories in last November’s midterm elections, the 110th Congress, which took office early this year, has new leaders and a new agenda that could bode well for healthcare legislation.
In this article, Laura Allendorf, SHM’s senior advisor for advocacy and government affairs, explains what the changes in Congress could mean for the near future of healthcare and for the legislation and issues that SHM strongly supports. Based in Washington, D.C., Allendorf is responsible for providing government relations services for SHM. She advises the organization on key legislative and regulatory healthcare issues before Congress and the Bush administration, and she works with SHM leaders and staff on policy development and advocacy strategies.
Majority Rules
The midterm elections brought about a shift in power that goes deeper than numbers of bodies on each side of the aisle. “The Democrats are now the majority in both chambers. This is significant, because they’ve been the minority since 1994, says Allendorf. “As the majority, they control the agenda now—on healthcare and other issues—and they also head the key committees.”
What can we expect to see from the Democratic Congress? “We should expect to see a more expansionist agenda” in general, according to Allendorf. “We’re going to see more activism in the area of healthcare, but whether anything gets done remains to be seen. There’s only a slim majority in the Senate, and President Bush can wield his veto pen. For example, the Democrats would like to give [the Department of] Health and Human Services the power to negotiate drug prices with pharmaceutical companies, specifically on Medicare Part D, but Bush won’t like that.”
Much depends on the issues at hand, as well as on how much bipartisan support exists for each specific bill.
Changing of the Guard
Anyone who glances at the newspaper knows that Democrat Nancy Pelosi (Calif.) is now the Speaker of the House. But Democratic leadership goes much deeper than that because the ruling party has also taken over leadership of Congressional committees. These committees shape the legislation introduced in the House and Senate.
As of press time, Congressional committee assignments had not been formally decided—at least not in the Senate—but many assignments were certain. “Typically, the highest-ranking Democrat [House or Senate] on a committee will become the new head, though Nancy Pelosi isn’t sticking to that,” explains Allendorf. “Pete Stark (D-Calif.) will likely chair the Ways and Means Committee’s Subcommittee on Health, and Charles Rangel (D-N.Y.) will head the House Ways and Means Committee. John Dingell (D-Mich.) will chair the House Energy and Commerce Committee.” (For more on committee chairs, visit http://media-newswire.com/release_1040623.html.)
For a complete list of committee members, visit SHM’s new Legislative Action Center at http://capwiz.com/hospitalmedicine/home/. See “New Advocacy Tool Available,” for more information on the Legislative Action Center, above.)
Starting Over on Key Issues
Many of the bills introduced in 2006—particularly spending bills—were not voted on by the end of the lame duck session last fall. That means that these bills must be reintroduced in the new year. Bills that recommend funding changes are frozen, so agencies continue to receive 2006 funding until the new Congress votes to change their budget.
“All bills have to be reintroduced in the 110th,” stresses Allendorf. “It will take some time—how much depends on the issue. The Democrats may want to hold hearings on legislation, or they may simply dust off legislation that was introduced last year.”
The Democrats are expected to move on many of the issues that SHM has been lobbying for. “They’ve said that they want to reform the healthcare system,” says Allendorf. “Top issues include providing coverage to the uninsured, reforming Medicare Part D, and resolving the physician payment issue.”
Allendorf believes that there will be a bipartisan effort to push through physician payment reform. “There are some 265 members of Congress who requested action on this issue this year [in 2006],” she points out. “There’s a genuine interest and desire to address physician payment reform and pay-for-performance as well. They may differ on how quickly they want to move on some of these.”
The news is not so good on the issue of gainsharing, where physicians are allowed to share the profits realized by a hospital’s cost reductions when linked to specific best practices. “Representative Nancy Johnson (R-Conn.) was a big proponent of this issue in the House, and she was not re-elected,” says Allendorf. “Stark is an opponent of gainsharing, so there may not be the same Congressional push behind it—at least in the House.”
However, the unexpected gainsharing demonstration projects approved in 2006 are underway, and Congress will hear reports on those in several years, once the projects have been analyzed.
Another issue that may not be addressed is liability. “Medical liability reform will be on the back burner,” warns Allendorf. “It’s generally not supported by the Democrats.”
In 2006, SHM supported increased funding for the Agency for Healthcare Research and Quality (AHRQ)—this was one of the major issues addressed by members during Legislative Advocacy Day during the Annual Meeting in Washington, D.C. Whether the next budget includes more money for the agency remains to be seen. “The Democrats support increased funding for NIH (National Institutes of Health), AHRQ, and other healthcare agencies,” says Allendorf. “There’s certainly political will, but where is the money going to come from?”
New Congress, New Issues
What about new issues? “Democrats have signaled that healthcare access for the uninsured will be a priority,” says Allendorf. “I think that we’ll see new legislation with a renewed emphasis on access to care.”
SHM’s Public Policy Committee will be waiting for the first legislation to be introduced regarding coverage for uninsured Americans. “This is an issue that SHM is strongly in favor of,” explains Allendorf. “SHM will look at any bills that come out on this issue and then form a policy.”
Regardless of which healthcare issues come to the forefront first, SHM’s Public Policy Committee, staff, and members are likely to be more active than ever. “I see a very busy year legislatively for SHM,” says Allendorf. TH
Jane Jerrard regularly writes “Public Policy” for The Hospitalist.
Train the Teacher
If you work at a teaching institution, an important part of your career track may be teaching residents the work of hospitalists. “Within academia, there are two major tracks: research[er] and clinical educator,” says Sanjay Saint, MD, MPH, hospitalist and professor of internal medicine at the Ann Arbor Veterans Affairs Medical Center and the University of Michigan Medical School, Ann Arbor. “We’re promoted based on our clinical work and on education evaluations; it’s helpful when we’re being reviewed if we’re seen as good teachers by our students.”
How are your teaching skills? How much thought and effort do you put into how you train your students? Do you take steps to improve your methods?
“Most of us have to work at being good teachers,” admits Dr. Saint. “We watch excellent teachers and learn as we go.” What follows is the advice of one excellent teacher.
Teachers: Champions for Hospital Medicine
Jeffrey Wiese, MD, FACP, is an SHM board member and associate professor of medicine at Tulane University Health Sciences Center in New Orleans, where he also serves as associate chairman of medicine, director of the Tulane Internal Medicine Residency Program, and associate director of student programs, internal medicine. “From an [SHM] board perspective, it’s been my agenda to better situate hospitalists as teachers,” he says.
One reason he’s committed to boosting the number of hospitalist-teachers is that Dr. Wiese believes the specialty is a perfect match for imparting knowledge. “Hospitalists are better instructors primarily because of their greater accessibility for supervision,” he says. “Because of the number of things they do and the consistent repetition with which they do them, they also have a better familiarity with what students need to know and how to do it.”
Another reason that hospitalists are excellent choices to train residents: “Hospitalists work at improving hospital systems and focus on quality of care,” says Dr. Wiese. “What better group of people to teach the systems of care and practice-based learning competencies?”
Coaching Versus Teaching
The basis of Dr. Wiese’s theory of teaching is that you should think and act as a coach—not a teacher. “A teacher is responsible for disseminating knowledge to his pupils; a coach is responsible for the performance of his pupils,” explains Dr. Wiese. “With a coach, the success of the job is contingent on the performance of the player—in this case, the student or resident.”
The coaching theory goes deeper than that distinction. “Components of coaching include [the following]: You have to teach the necessary skill, but you have to motivate the person to want to do it right, create a vision of how they’re going to do it, anticipate and prepare them for potential obstacles that might stand in the way of their performance, and provide feedback and evaluation when they do it,” says Dr. Wiese. “A football coach wouldn’t just tell you how to throw a ball. He would teach you the skill and then watch you do it, while providing feedback on your performance. He would tell you what the opposing team might do to oppose your performance of that skill and prepare you to overcome that opposition. And then he would instill a motivation such that you wanted to perform the skill well.”
Dr. Saint, who is familiar with Dr. Wiese’s theory, says, “I like the metaphor of coaching because a coach tries to make you better at what you’re learning. A coach may use techniques that make you uncomfortable at the time, but if you look back after a couple of years, you’ll be thankful that he pushed you.”
Another aspect of coaching that fits neatly into today’s clinical learning is the team aspect. “Medicine is no longer an individual event,” explains Dr. Wiese. “It’s a team activity, where the best patient care is provided by a team of healthcare professionals from doctors to nurses to physical therapists and others. Teaching the mentality of playing as part of a team will help residents perform better in this environment as they advance in their careers.”
Teaching in a “Vacum”
“I use the mnemonic VACUM [to describe coaching],” says Dr. Wiese. VACUM stands for:
- Visualization: To pique interest in a topic or procedure, start by asking students to visualize themselves using the skill. Repeatedly ask them how they think they will put the skill to use.
“Get the person to picture herself with a patient,” urges Dr. Wiese. This step both hooks learners at the beginning of a session and helps teach them the skill.
- Anticipation: If you’re an experienced teacher and know your students well, you know where they will struggle in the learning process. “Think about the common pitfalls,” says Dr. Wiese. “Alert the student to where she will get confused or make mistakes and spend time preparing the student for how she can avoid the pitfall. For example, if you’re teaching them about putting in a central line, tell them, ‘You [might] not think about the patient’s bleeding risk prior to procedure. Make sure you know his INR [international normalized ratio] and platelet count prior to starting the procedure.’ ”
- Content: “This is where most teachers go awry,” warns Dr. Wiese. “Medical educators try to teach too much, and students try to learn too much. Not every detail in a topic needs to be discussed. It’s far better to sacrifice details to preserve time to ensure that students have mastered the fundamental concepts of a disease or skill. They can pick up the details later—focus on what they need to know.”
How do you know what to focus on? “The guidelines of what students must learn during their internal medicine clerkship are voluminous,” says Dr. Wiese. “Find those that you think have utility in your practice or utility to the students. The best strategy is to stick to the fundamentals. With this strategy, they will walk away with the critical components that will empower them to pick up the details during subsequent teaching sessions.”
- Utility: “This goes with content,” says Dr. Wiese. “Teach them skills that they can utilize. Remember, utility varies from student to student. A student heading into a future career in orthopedics will find greater utility in learning about pre-operative care and management of atrial fibrillation than she will with a discourse on lupus.”
- Motivation: Motivation includes three subcategories. “Students or residents have to know that the coach is on their side,” says Dr. Wiese. One way to do this is to learn their names—and use them frequently. You should also use physical contact to show your support.
“Give a pat on the shoulder, or shake someone’s hand,” he advises. “If you’re in a classroom, move around the room. Show that you’re accessible.” Finally, find people’s hooks—that is, what interests them.
So how do you know you’ve become a good teacher? “The ultimate goal of coaching is successful student performance—not awards or approbation. The measure of your success is defined by seeing your students months or even years later, doing right by a patient because of what you taught them to do,” says Dr. Wiese. “Focus on that goal, and everything else will fall into place.” TH
Jane Jerrard regularly writes “Career Development.”
If you work at a teaching institution, an important part of your career track may be teaching residents the work of hospitalists. “Within academia, there are two major tracks: research[er] and clinical educator,” says Sanjay Saint, MD, MPH, hospitalist and professor of internal medicine at the Ann Arbor Veterans Affairs Medical Center and the University of Michigan Medical School, Ann Arbor. “We’re promoted based on our clinical work and on education evaluations; it’s helpful when we’re being reviewed if we’re seen as good teachers by our students.”
How are your teaching skills? How much thought and effort do you put into how you train your students? Do you take steps to improve your methods?
“Most of us have to work at being good teachers,” admits Dr. Saint. “We watch excellent teachers and learn as we go.” What follows is the advice of one excellent teacher.
Teachers: Champions for Hospital Medicine
Jeffrey Wiese, MD, FACP, is an SHM board member and associate professor of medicine at Tulane University Health Sciences Center in New Orleans, where he also serves as associate chairman of medicine, director of the Tulane Internal Medicine Residency Program, and associate director of student programs, internal medicine. “From an [SHM] board perspective, it’s been my agenda to better situate hospitalists as teachers,” he says.
One reason he’s committed to boosting the number of hospitalist-teachers is that Dr. Wiese believes the specialty is a perfect match for imparting knowledge. “Hospitalists are better instructors primarily because of their greater accessibility for supervision,” he says. “Because of the number of things they do and the consistent repetition with which they do them, they also have a better familiarity with what students need to know and how to do it.”
Another reason that hospitalists are excellent choices to train residents: “Hospitalists work at improving hospital systems and focus on quality of care,” says Dr. Wiese. “What better group of people to teach the systems of care and practice-based learning competencies?”
Coaching Versus Teaching
The basis of Dr. Wiese’s theory of teaching is that you should think and act as a coach—not a teacher. “A teacher is responsible for disseminating knowledge to his pupils; a coach is responsible for the performance of his pupils,” explains Dr. Wiese. “With a coach, the success of the job is contingent on the performance of the player—in this case, the student or resident.”
The coaching theory goes deeper than that distinction. “Components of coaching include [the following]: You have to teach the necessary skill, but you have to motivate the person to want to do it right, create a vision of how they’re going to do it, anticipate and prepare them for potential obstacles that might stand in the way of their performance, and provide feedback and evaluation when they do it,” says Dr. Wiese. “A football coach wouldn’t just tell you how to throw a ball. He would teach you the skill and then watch you do it, while providing feedback on your performance. He would tell you what the opposing team might do to oppose your performance of that skill and prepare you to overcome that opposition. And then he would instill a motivation such that you wanted to perform the skill well.”
Dr. Saint, who is familiar with Dr. Wiese’s theory, says, “I like the metaphor of coaching because a coach tries to make you better at what you’re learning. A coach may use techniques that make you uncomfortable at the time, but if you look back after a couple of years, you’ll be thankful that he pushed you.”
Another aspect of coaching that fits neatly into today’s clinical learning is the team aspect. “Medicine is no longer an individual event,” explains Dr. Wiese. “It’s a team activity, where the best patient care is provided by a team of healthcare professionals from doctors to nurses to physical therapists and others. Teaching the mentality of playing as part of a team will help residents perform better in this environment as they advance in their careers.”
Teaching in a “Vacum”
“I use the mnemonic VACUM [to describe coaching],” says Dr. Wiese. VACUM stands for:
- Visualization: To pique interest in a topic or procedure, start by asking students to visualize themselves using the skill. Repeatedly ask them how they think they will put the skill to use.
“Get the person to picture herself with a patient,” urges Dr. Wiese. This step both hooks learners at the beginning of a session and helps teach them the skill.
- Anticipation: If you’re an experienced teacher and know your students well, you know where they will struggle in the learning process. “Think about the common pitfalls,” says Dr. Wiese. “Alert the student to where she will get confused or make mistakes and spend time preparing the student for how she can avoid the pitfall. For example, if you’re teaching them about putting in a central line, tell them, ‘You [might] not think about the patient’s bleeding risk prior to procedure. Make sure you know his INR [international normalized ratio] and platelet count prior to starting the procedure.’ ”
- Content: “This is where most teachers go awry,” warns Dr. Wiese. “Medical educators try to teach too much, and students try to learn too much. Not every detail in a topic needs to be discussed. It’s far better to sacrifice details to preserve time to ensure that students have mastered the fundamental concepts of a disease or skill. They can pick up the details later—focus on what they need to know.”
How do you know what to focus on? “The guidelines of what students must learn during their internal medicine clerkship are voluminous,” says Dr. Wiese. “Find those that you think have utility in your practice or utility to the students. The best strategy is to stick to the fundamentals. With this strategy, they will walk away with the critical components that will empower them to pick up the details during subsequent teaching sessions.”
- Utility: “This goes with content,” says Dr. Wiese. “Teach them skills that they can utilize. Remember, utility varies from student to student. A student heading into a future career in orthopedics will find greater utility in learning about pre-operative care and management of atrial fibrillation than she will with a discourse on lupus.”
- Motivation: Motivation includes three subcategories. “Students or residents have to know that the coach is on their side,” says Dr. Wiese. One way to do this is to learn their names—and use them frequently. You should also use physical contact to show your support.
“Give a pat on the shoulder, or shake someone’s hand,” he advises. “If you’re in a classroom, move around the room. Show that you’re accessible.” Finally, find people’s hooks—that is, what interests them.
So how do you know you’ve become a good teacher? “The ultimate goal of coaching is successful student performance—not awards or approbation. The measure of your success is defined by seeing your students months or even years later, doing right by a patient because of what you taught them to do,” says Dr. Wiese. “Focus on that goal, and everything else will fall into place.” TH
Jane Jerrard regularly writes “Career Development.”
If you work at a teaching institution, an important part of your career track may be teaching residents the work of hospitalists. “Within academia, there are two major tracks: research[er] and clinical educator,” says Sanjay Saint, MD, MPH, hospitalist and professor of internal medicine at the Ann Arbor Veterans Affairs Medical Center and the University of Michigan Medical School, Ann Arbor. “We’re promoted based on our clinical work and on education evaluations; it’s helpful when we’re being reviewed if we’re seen as good teachers by our students.”
How are your teaching skills? How much thought and effort do you put into how you train your students? Do you take steps to improve your methods?
“Most of us have to work at being good teachers,” admits Dr. Saint. “We watch excellent teachers and learn as we go.” What follows is the advice of one excellent teacher.
Teachers: Champions for Hospital Medicine
Jeffrey Wiese, MD, FACP, is an SHM board member and associate professor of medicine at Tulane University Health Sciences Center in New Orleans, where he also serves as associate chairman of medicine, director of the Tulane Internal Medicine Residency Program, and associate director of student programs, internal medicine. “From an [SHM] board perspective, it’s been my agenda to better situate hospitalists as teachers,” he says.
One reason he’s committed to boosting the number of hospitalist-teachers is that Dr. Wiese believes the specialty is a perfect match for imparting knowledge. “Hospitalists are better instructors primarily because of their greater accessibility for supervision,” he says. “Because of the number of things they do and the consistent repetition with which they do them, they also have a better familiarity with what students need to know and how to do it.”
Another reason that hospitalists are excellent choices to train residents: “Hospitalists work at improving hospital systems and focus on quality of care,” says Dr. Wiese. “What better group of people to teach the systems of care and practice-based learning competencies?”
Coaching Versus Teaching
The basis of Dr. Wiese’s theory of teaching is that you should think and act as a coach—not a teacher. “A teacher is responsible for disseminating knowledge to his pupils; a coach is responsible for the performance of his pupils,” explains Dr. Wiese. “With a coach, the success of the job is contingent on the performance of the player—in this case, the student or resident.”
The coaching theory goes deeper than that distinction. “Components of coaching include [the following]: You have to teach the necessary skill, but you have to motivate the person to want to do it right, create a vision of how they’re going to do it, anticipate and prepare them for potential obstacles that might stand in the way of their performance, and provide feedback and evaluation when they do it,” says Dr. Wiese. “A football coach wouldn’t just tell you how to throw a ball. He would teach you the skill and then watch you do it, while providing feedback on your performance. He would tell you what the opposing team might do to oppose your performance of that skill and prepare you to overcome that opposition. And then he would instill a motivation such that you wanted to perform the skill well.”
Dr. Saint, who is familiar with Dr. Wiese’s theory, says, “I like the metaphor of coaching because a coach tries to make you better at what you’re learning. A coach may use techniques that make you uncomfortable at the time, but if you look back after a couple of years, you’ll be thankful that he pushed you.”
Another aspect of coaching that fits neatly into today’s clinical learning is the team aspect. “Medicine is no longer an individual event,” explains Dr. Wiese. “It’s a team activity, where the best patient care is provided by a team of healthcare professionals from doctors to nurses to physical therapists and others. Teaching the mentality of playing as part of a team will help residents perform better in this environment as they advance in their careers.”
Teaching in a “Vacum”
“I use the mnemonic VACUM [to describe coaching],” says Dr. Wiese. VACUM stands for:
- Visualization: To pique interest in a topic or procedure, start by asking students to visualize themselves using the skill. Repeatedly ask them how they think they will put the skill to use.
“Get the person to picture herself with a patient,” urges Dr. Wiese. This step both hooks learners at the beginning of a session and helps teach them the skill.
- Anticipation: If you’re an experienced teacher and know your students well, you know where they will struggle in the learning process. “Think about the common pitfalls,” says Dr. Wiese. “Alert the student to where she will get confused or make mistakes and spend time preparing the student for how she can avoid the pitfall. For example, if you’re teaching them about putting in a central line, tell them, ‘You [might] not think about the patient’s bleeding risk prior to procedure. Make sure you know his INR [international normalized ratio] and platelet count prior to starting the procedure.’ ”
- Content: “This is where most teachers go awry,” warns Dr. Wiese. “Medical educators try to teach too much, and students try to learn too much. Not every detail in a topic needs to be discussed. It’s far better to sacrifice details to preserve time to ensure that students have mastered the fundamental concepts of a disease or skill. They can pick up the details later—focus on what they need to know.”
How do you know what to focus on? “The guidelines of what students must learn during their internal medicine clerkship are voluminous,” says Dr. Wiese. “Find those that you think have utility in your practice or utility to the students. The best strategy is to stick to the fundamentals. With this strategy, they will walk away with the critical components that will empower them to pick up the details during subsequent teaching sessions.”
- Utility: “This goes with content,” says Dr. Wiese. “Teach them skills that they can utilize. Remember, utility varies from student to student. A student heading into a future career in orthopedics will find greater utility in learning about pre-operative care and management of atrial fibrillation than she will with a discourse on lupus.”
- Motivation: Motivation includes three subcategories. “Students or residents have to know that the coach is on their side,” says Dr. Wiese. One way to do this is to learn their names—and use them frequently. You should also use physical contact to show your support.
“Give a pat on the shoulder, or shake someone’s hand,” he advises. “If you’re in a classroom, move around the room. Show that you’re accessible.” Finally, find people’s hooks—that is, what interests them.
So how do you know you’ve become a good teacher? “The ultimate goal of coaching is successful student performance—not awards or approbation. The measure of your success is defined by seeing your students months or even years later, doing right by a patient because of what you taught them to do,” says Dr. Wiese. “Focus on that goal, and everything else will fall into place.” TH
Jane Jerrard regularly writes “Career Development.”
A Look inside Healthcare Transparency
One of the many trends in healthcare today is a move toward making specific quality and pricing information available to the public.
“When you’re buying a car, you can easily compare quality, features, and prices to make an educated guess,” points out Eric Siegal, MD, regional medical director, Cogent Healthcare, Madison, Wis., and chair of SHM’s Public Policy Committee. “In contrast, healthcare is completely opaque. People choose a doctor or a hospital—sometimes for a surgery that’s life threatening—by word of mouth or [based on] proximity. How do you make it possible to choose based on quality of care and on price?”
Known as healthcare transparency, this trend is driven by multiple sources. “The [CMS] Hospital Compare initiative was a first step in this, as were the Leapfrog initiative and the IHI [Institute for Health Improvement] Collaborative,” says Dr. Siegal. “In fact, the government is a little late to the game, but they’re quickly closing the gap.”
Mandate from the President
On August 22, 2006, President George W. Bush signed an executive order requiring key federal agencies to collect information about the quality and cost of the healthcare they provide and to share that data with each another—and with beneficiaries. Agencies included in the order are the Department of Health and Human Services (HHS), the Department of Defense (DoD), the Department of Veterans Affairs (VA), and the Office of Personnel Management (OPM).
The executive order directs these four agencies to work with the private sector and other government agencies to develop programs to measure quality of care. They were required by Jan. 1, 2007, to identify practices that promote high quality care and to compile information on the prices they pay for common services available to their members. Ultimately, the executive order calls for combining that data in a comprehensive source on providers’ quality and prices; this information will then be available to consumers.
President Bush has said that his order sends a message to healthcare providers that “in order to do business with the federal government, you’ve got to show us your prices.” The new requirements for transparency will affect healthcare providers across the country because treating about one-quarter of Americans covered by health insurance entails “doing business with the federal government.” That one-quarter includes Medicare beneficiaries, health insurance beneficiaries at the DoD and the VA, and federal employees. (The order clearly states that the directive does not apply to state-administered or -funded programs.)
House Legislation: Make Prices Public
Comprehensive pricing transparency may also be required on a state level. On Sept. 13, 2006, Representative Michael Burgess (R-Texas) introduced the Health Care Price Transparency Act of 2006 in the House. This American Hospital Association (AHA)-supported legislation would require states to publicly report hospital charges for specific inpatient and outpatient services and would require insurers to give patients, on request, an estimate of their expected out-of-pocket expenses.
—Eric Siegal, MD
The bill would also require the Agency for Healthcare Research and Quality to study what type of healthcare price information consumers would find useful and how that information could be made available in a timely, understandable form.
Thirty-two states already require hospitals to report pricing information, and six more are voluntarily doing so, but this legislation would likely change the information that hospitals and other providers are gathering and providing.
At press time, the legislation had been referred to the House Subcommittee on Health.
How Transparency Will Roll Out
While the House legislation is in limbo, the executive order will have an immediate effect on healthcare, starting this year. The quality measures to be included in reporting will be developed from private and government sources, including local providers, employers, and health plans and insurers.
After the data are gathered and the information technology (IT) infrastructure is set up, consumers will be able to access specific information on pricing and quality of services performed by doctors, hospitals, and other healthcare providers. This information may be available through a variety of sources, including insurance companies, employers, and Medicare-sponsored Web sites.
One of the keys to success will be in the collaboration among the agencies involved. “There’s a keen understanding among the major players that if everyone does their own thing, we’ll have chaos,” says Dr. Siegal. “There has to be a significant degree of harmonization [among] physician measures, hospital measures, inpatient measures, and outpatient measures.”
Where Hospitalists Fit in
Will healthcare transparency affect hospitalists? “It’s already impacting hospitalists,” says Dr. Siegal. “Not on pricing, but on quality reporting. The good news is that hospitalists may be the single best-prepared group of physicians [for transparency] because we’re already doing it. The question will be, as it becomes more pervasive, will it be done in a way that is thoughtful, measured, and practical?”
Hospitals are likely to look to their hospitalists to ensure that their quality measurements are competitive. Dr. Siegal explains, “Hospitals looking to improve quality will be most effective in getting results from the physicians whose financial incentives are aligned with theirs.”
However, additional—or more public—quality indicators will not necessarily create a huge source of income for hospital medicine. “The low-hanging fruit won’t be the patients that hospitalists see; it will be elective surgical cases,” predicts Dr. Siegal. “Those are cleanly defined procedures, with bundled payments and predictable outcomes, where a hospital can understand what happens and what’s included. Then they can say, ‘Why do we charge 20% more for a total elective hip [surgery] than the hospital down the road?’ ”
As transparency is rolled out in U.S. hospitals and healthcare systems, hospitalists will look good. “Hospitalists already live in a quality reporting world, more so than other doctors,” says Dr. Siegal. TH
Jane Jerrard writes “Public Policy” for The Hospitalist.
One of the many trends in healthcare today is a move toward making specific quality and pricing information available to the public.
“When you’re buying a car, you can easily compare quality, features, and prices to make an educated guess,” points out Eric Siegal, MD, regional medical director, Cogent Healthcare, Madison, Wis., and chair of SHM’s Public Policy Committee. “In contrast, healthcare is completely opaque. People choose a doctor or a hospital—sometimes for a surgery that’s life threatening—by word of mouth or [based on] proximity. How do you make it possible to choose based on quality of care and on price?”
Known as healthcare transparency, this trend is driven by multiple sources. “The [CMS] Hospital Compare initiative was a first step in this, as were the Leapfrog initiative and the IHI [Institute for Health Improvement] Collaborative,” says Dr. Siegal. “In fact, the government is a little late to the game, but they’re quickly closing the gap.”
Mandate from the President
On August 22, 2006, President George W. Bush signed an executive order requiring key federal agencies to collect information about the quality and cost of the healthcare they provide and to share that data with each another—and with beneficiaries. Agencies included in the order are the Department of Health and Human Services (HHS), the Department of Defense (DoD), the Department of Veterans Affairs (VA), and the Office of Personnel Management (OPM).
The executive order directs these four agencies to work with the private sector and other government agencies to develop programs to measure quality of care. They were required by Jan. 1, 2007, to identify practices that promote high quality care and to compile information on the prices they pay for common services available to their members. Ultimately, the executive order calls for combining that data in a comprehensive source on providers’ quality and prices; this information will then be available to consumers.
President Bush has said that his order sends a message to healthcare providers that “in order to do business with the federal government, you’ve got to show us your prices.” The new requirements for transparency will affect healthcare providers across the country because treating about one-quarter of Americans covered by health insurance entails “doing business with the federal government.” That one-quarter includes Medicare beneficiaries, health insurance beneficiaries at the DoD and the VA, and federal employees. (The order clearly states that the directive does not apply to state-administered or -funded programs.)
House Legislation: Make Prices Public
Comprehensive pricing transparency may also be required on a state level. On Sept. 13, 2006, Representative Michael Burgess (R-Texas) introduced the Health Care Price Transparency Act of 2006 in the House. This American Hospital Association (AHA)-supported legislation would require states to publicly report hospital charges for specific inpatient and outpatient services and would require insurers to give patients, on request, an estimate of their expected out-of-pocket expenses.
—Eric Siegal, MD
The bill would also require the Agency for Healthcare Research and Quality to study what type of healthcare price information consumers would find useful and how that information could be made available in a timely, understandable form.
Thirty-two states already require hospitals to report pricing information, and six more are voluntarily doing so, but this legislation would likely change the information that hospitals and other providers are gathering and providing.
At press time, the legislation had been referred to the House Subcommittee on Health.
How Transparency Will Roll Out
While the House legislation is in limbo, the executive order will have an immediate effect on healthcare, starting this year. The quality measures to be included in reporting will be developed from private and government sources, including local providers, employers, and health plans and insurers.
After the data are gathered and the information technology (IT) infrastructure is set up, consumers will be able to access specific information on pricing and quality of services performed by doctors, hospitals, and other healthcare providers. This information may be available through a variety of sources, including insurance companies, employers, and Medicare-sponsored Web sites.
One of the keys to success will be in the collaboration among the agencies involved. “There’s a keen understanding among the major players that if everyone does their own thing, we’ll have chaos,” says Dr. Siegal. “There has to be a significant degree of harmonization [among] physician measures, hospital measures, inpatient measures, and outpatient measures.”
Where Hospitalists Fit in
Will healthcare transparency affect hospitalists? “It’s already impacting hospitalists,” says Dr. Siegal. “Not on pricing, but on quality reporting. The good news is that hospitalists may be the single best-prepared group of physicians [for transparency] because we’re already doing it. The question will be, as it becomes more pervasive, will it be done in a way that is thoughtful, measured, and practical?”
Hospitals are likely to look to their hospitalists to ensure that their quality measurements are competitive. Dr. Siegal explains, “Hospitals looking to improve quality will be most effective in getting results from the physicians whose financial incentives are aligned with theirs.”
However, additional—or more public—quality indicators will not necessarily create a huge source of income for hospital medicine. “The low-hanging fruit won’t be the patients that hospitalists see; it will be elective surgical cases,” predicts Dr. Siegal. “Those are cleanly defined procedures, with bundled payments and predictable outcomes, where a hospital can understand what happens and what’s included. Then they can say, ‘Why do we charge 20% more for a total elective hip [surgery] than the hospital down the road?’ ”
As transparency is rolled out in U.S. hospitals and healthcare systems, hospitalists will look good. “Hospitalists already live in a quality reporting world, more so than other doctors,” says Dr. Siegal. TH
Jane Jerrard writes “Public Policy” for The Hospitalist.
One of the many trends in healthcare today is a move toward making specific quality and pricing information available to the public.
“When you’re buying a car, you can easily compare quality, features, and prices to make an educated guess,” points out Eric Siegal, MD, regional medical director, Cogent Healthcare, Madison, Wis., and chair of SHM’s Public Policy Committee. “In contrast, healthcare is completely opaque. People choose a doctor or a hospital—sometimes for a surgery that’s life threatening—by word of mouth or [based on] proximity. How do you make it possible to choose based on quality of care and on price?”
Known as healthcare transparency, this trend is driven by multiple sources. “The [CMS] Hospital Compare initiative was a first step in this, as were the Leapfrog initiative and the IHI [Institute for Health Improvement] Collaborative,” says Dr. Siegal. “In fact, the government is a little late to the game, but they’re quickly closing the gap.”
Mandate from the President
On August 22, 2006, President George W. Bush signed an executive order requiring key federal agencies to collect information about the quality and cost of the healthcare they provide and to share that data with each another—and with beneficiaries. Agencies included in the order are the Department of Health and Human Services (HHS), the Department of Defense (DoD), the Department of Veterans Affairs (VA), and the Office of Personnel Management (OPM).
The executive order directs these four agencies to work with the private sector and other government agencies to develop programs to measure quality of care. They were required by Jan. 1, 2007, to identify practices that promote high quality care and to compile information on the prices they pay for common services available to their members. Ultimately, the executive order calls for combining that data in a comprehensive source on providers’ quality and prices; this information will then be available to consumers.
President Bush has said that his order sends a message to healthcare providers that “in order to do business with the federal government, you’ve got to show us your prices.” The new requirements for transparency will affect healthcare providers across the country because treating about one-quarter of Americans covered by health insurance entails “doing business with the federal government.” That one-quarter includes Medicare beneficiaries, health insurance beneficiaries at the DoD and the VA, and federal employees. (The order clearly states that the directive does not apply to state-administered or -funded programs.)
House Legislation: Make Prices Public
Comprehensive pricing transparency may also be required on a state level. On Sept. 13, 2006, Representative Michael Burgess (R-Texas) introduced the Health Care Price Transparency Act of 2006 in the House. This American Hospital Association (AHA)-supported legislation would require states to publicly report hospital charges for specific inpatient and outpatient services and would require insurers to give patients, on request, an estimate of their expected out-of-pocket expenses.
—Eric Siegal, MD
The bill would also require the Agency for Healthcare Research and Quality to study what type of healthcare price information consumers would find useful and how that information could be made available in a timely, understandable form.
Thirty-two states already require hospitals to report pricing information, and six more are voluntarily doing so, but this legislation would likely change the information that hospitals and other providers are gathering and providing.
At press time, the legislation had been referred to the House Subcommittee on Health.
How Transparency Will Roll Out
While the House legislation is in limbo, the executive order will have an immediate effect on healthcare, starting this year. The quality measures to be included in reporting will be developed from private and government sources, including local providers, employers, and health plans and insurers.
After the data are gathered and the information technology (IT) infrastructure is set up, consumers will be able to access specific information on pricing and quality of services performed by doctors, hospitals, and other healthcare providers. This information may be available through a variety of sources, including insurance companies, employers, and Medicare-sponsored Web sites.
One of the keys to success will be in the collaboration among the agencies involved. “There’s a keen understanding among the major players that if everyone does their own thing, we’ll have chaos,” says Dr. Siegal. “There has to be a significant degree of harmonization [among] physician measures, hospital measures, inpatient measures, and outpatient measures.”
Where Hospitalists Fit in
Will healthcare transparency affect hospitalists? “It’s already impacting hospitalists,” says Dr. Siegal. “Not on pricing, but on quality reporting. The good news is that hospitalists may be the single best-prepared group of physicians [for transparency] because we’re already doing it. The question will be, as it becomes more pervasive, will it be done in a way that is thoughtful, measured, and practical?”
Hospitals are likely to look to their hospitalists to ensure that their quality measurements are competitive. Dr. Siegal explains, “Hospitals looking to improve quality will be most effective in getting results from the physicians whose financial incentives are aligned with theirs.”
However, additional—or more public—quality indicators will not necessarily create a huge source of income for hospital medicine. “The low-hanging fruit won’t be the patients that hospitalists see; it will be elective surgical cases,” predicts Dr. Siegal. “Those are cleanly defined procedures, with bundled payments and predictable outcomes, where a hospital can understand what happens and what’s included. Then they can say, ‘Why do we charge 20% more for a total elective hip [surgery] than the hospital down the road?’ ”
As transparency is rolled out in U.S. hospitals and healthcare systems, hospitalists will look good. “Hospitalists already live in a quality reporting world, more so than other doctors,” says Dr. Siegal. TH
Jane Jerrard writes “Public Policy” for The Hospitalist.
Pay Dirt
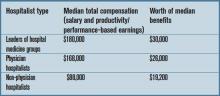
It’ s easy to find figures on what hospitalists earn these days, but if your own income doesn’t match up, does that mean you’re underpaid? Not necessarily.
The SHM Survey
There are several sources that provide figures on hospitalist income, but SHM offers an accurate, detailed—and the largest representative—picture of what hospitalists earn now. In spring 2006, SHM released its latest comprehensive survey of membership, “The 2005-2006 SHM Survey: The Authoritative Source on the State of the Hospitalist Movement.” The report is based on responses of 396 hospital medicine groups representing more than 2,500 hospitalists. However, Joseph A. Miller, senior vice president of SHM, warns that the survey’s salary figures may skew toward one or more specific demographics.
“In our survey, we have a number of respondents in each cell—academic, pediatric, etc.—as well as a range of geographic areas and other differences,” he says. “Anyone who looks at the metric needs to understand the factors behind it.”
John Nelson, MD, director, hospital practice, Overlake Hospital, Bellevue, Wash., and author of “Practice Management” for The Hospitalist, who has participated in developing and analyzing SHM surveys for years, agrees that the figures in the survey should be used as general guidelines only. “It’s easy to take individual metrics in a vacuum without considering the variables,” he warns.
With these caveats in mind, the basic information on hospitalist compensation from the survey breaks down as follows: (table right)
To put these numbers in perspective, the median number of patient encounters per hospitalist was 2,328 per year, and the median number of work RVUs was 3,213.
Both leader- and physician-hospitalists have enjoyed an 8% increase in compensation, as well as an 8% increase in benefits, compared with the 2003-2004 survey. Non-physician hospitalists have seen a whopping increase in median income of 26% since 2003-2004. (Their benefits increased 7%.)
Perhaps the main reason for steadily increasing hospitalist incomes is that demand for hospitalists continues to exceed supply. “I’ve been trying to recruit hospitalists to my group for years,” says Dr. Nelson. “I thought that by 2002 or 2003, the number of available physicians would exceed the demand—but that hasn’t happened. It’s true that the number of doctors interested in hospital medicine has gone up pretty dramatically, but the demand went up even faster.”
By some estimates, says Dr. Nelson, there are two or three open positions for every hospitalist jobseeker.
—John Nelson, MD
Forms of Payment
To break these figures down further, income varies with type of compensation. In other words, how you are paid can influence how much you’re paid. Physician hospitalists who are paid 100% salary had a median income of $150,000. Those who are 100% productivity/performance-based make more money—a median income of $165,000; and those with a mixed-compensation model make the most of all, with a median income of $170,000.
Currently, according to the SHM survey, only 28% of respondents are 100% salary-based and 5% are 100% productivity/performance-based. The remaining majority (67%) is compensated with a combination of the two. Compared to the 2003-2004 SHM survey, the mixed compensation model increased from 47%.
“The portion of hospitalists paid via straight salary or based solely on production has been declining in the last few years,” says Dr. Nelson. “I think [a] low base and high productivity component is ideal, but [a] lower base does impede recruiting even if the total income is very attractive.”
IPC—The Hospitalist Company, one of the largest employers of hospitalists, uses the same combination of base salary and incentives for all physicians, regardless of their level of experience.
“We might change the salary figures slightly for different geographic areas, says Tim Lary, vice president of physician staffing for IPC, “but within our company, the average physician earns a little bit north of $200,000. A large portion earn over $300,000 because of our incentive plan.” That figure includes a base salary of approximately $150,000; the rest is comprised of incentives based on “typical counters” that hospitalists see, according to Lary, including productivity, quality indicators, and compliance.
Lary postulates that compensation is higher at a large organization like IPC because those employers have an infrastructure in place that ensures cost-effectiveness. “We have a 99.9% collection rate because we have a good central business office,” he says. “Small groups don’t have resources like that. We also do a great deal of training in proper coding techniques so that we can bill appropriately.”
A Grain of Salt
Before you barge in to your director’s office and ask for a raise, you should understand that the salaries summarized here have severe limitations and should be seen only as rough guidelines. There are major factors that can boost annual compensation, including:
- A heavy load of on-call, night, or weekend work;
- Employment in a geographic region with a shortage of physicians;
- Employment in a geographic region with higher physician incomes (such as the southeast);
- The type of practice you work for; and
- New practices recruiting hospitalists.
Also keep in mind that compensation totals include all bonuses and incentives received during the year.
Find Your Figure
Hospitalist income—particularly productivity-based income—is also directly affected by workload. Dr. Nelson suggests using the information in the SHM survey to find a rough guideline for productivity and compensation.
“Take the compensation figure from the survey for your region, production type, etc. and take the average production numbers from that same subgroup,” he says. “Then do the math to find the number of dollars per encounter or per RVU, and gauge your own numbers. If you have 25% more encounters, your income should be 25% higher than the average.”
The best rule of thumb for estimating what you should make, says Dr. Nelson, is to aim for five to 15% more than physicians working in traditional practice in your market. Unfortunately, information on what other doctors earn may not be readily available. Some sources (including a few listed in the sidebar to this article) provide information on all physician incomes, but is broken down by region at best. “You have to ask around,” says Dr. Nelson. “And if you’re interviewing, ask what they’re offering—then go and interview at a private practice and ask what they’re offering.”
In other words, there’s no easy way to tell if what you make is exactly on the mark for other hospitalists in your area—unless you ask those other hospitalists. But the SHM survey information should provide enough information to give you an idea. You can view an executive summary of the survey or purchase a complete copy at www.hospitalmedicine.org. TH
Jane Jerrard is the monthly writer for “Career Development.”
It’ s easy to find figures on what hospitalists earn these days, but if your own income doesn’t match up, does that mean you’re underpaid? Not necessarily.
The SHM Survey
There are several sources that provide figures on hospitalist income, but SHM offers an accurate, detailed—and the largest representative—picture of what hospitalists earn now. In spring 2006, SHM released its latest comprehensive survey of membership, “The 2005-2006 SHM Survey: The Authoritative Source on the State of the Hospitalist Movement.” The report is based on responses of 396 hospital medicine groups representing more than 2,500 hospitalists. However, Joseph A. Miller, senior vice president of SHM, warns that the survey’s salary figures may skew toward one or more specific demographics.
“In our survey, we have a number of respondents in each cell—academic, pediatric, etc.—as well as a range of geographic areas and other differences,” he says. “Anyone who looks at the metric needs to understand the factors behind it.”
John Nelson, MD, director, hospital practice, Overlake Hospital, Bellevue, Wash., and author of “Practice Management” for The Hospitalist, who has participated in developing and analyzing SHM surveys for years, agrees that the figures in the survey should be used as general guidelines only. “It’s easy to take individual metrics in a vacuum without considering the variables,” he warns.
With these caveats in mind, the basic information on hospitalist compensation from the survey breaks down as follows: (table right)
To put these numbers in perspective, the median number of patient encounters per hospitalist was 2,328 per year, and the median number of work RVUs was 3,213.
Both leader- and physician-hospitalists have enjoyed an 8% increase in compensation, as well as an 8% increase in benefits, compared with the 2003-2004 survey. Non-physician hospitalists have seen a whopping increase in median income of 26% since 2003-2004. (Their benefits increased 7%.)
Perhaps the main reason for steadily increasing hospitalist incomes is that demand for hospitalists continues to exceed supply. “I’ve been trying to recruit hospitalists to my group for years,” says Dr. Nelson. “I thought that by 2002 or 2003, the number of available physicians would exceed the demand—but that hasn’t happened. It’s true that the number of doctors interested in hospital medicine has gone up pretty dramatically, but the demand went up even faster.”
By some estimates, says Dr. Nelson, there are two or three open positions for every hospitalist jobseeker.
—John Nelson, MD
Forms of Payment
To break these figures down further, income varies with type of compensation. In other words, how you are paid can influence how much you’re paid. Physician hospitalists who are paid 100% salary had a median income of $150,000. Those who are 100% productivity/performance-based make more money—a median income of $165,000; and those with a mixed-compensation model make the most of all, with a median income of $170,000.
Currently, according to the SHM survey, only 28% of respondents are 100% salary-based and 5% are 100% productivity/performance-based. The remaining majority (67%) is compensated with a combination of the two. Compared to the 2003-2004 SHM survey, the mixed compensation model increased from 47%.
“The portion of hospitalists paid via straight salary or based solely on production has been declining in the last few years,” says Dr. Nelson. “I think [a] low base and high productivity component is ideal, but [a] lower base does impede recruiting even if the total income is very attractive.”
IPC—The Hospitalist Company, one of the largest employers of hospitalists, uses the same combination of base salary and incentives for all physicians, regardless of their level of experience.
“We might change the salary figures slightly for different geographic areas, says Tim Lary, vice president of physician staffing for IPC, “but within our company, the average physician earns a little bit north of $200,000. A large portion earn over $300,000 because of our incentive plan.” That figure includes a base salary of approximately $150,000; the rest is comprised of incentives based on “typical counters” that hospitalists see, according to Lary, including productivity, quality indicators, and compliance.
Lary postulates that compensation is higher at a large organization like IPC because those employers have an infrastructure in place that ensures cost-effectiveness. “We have a 99.9% collection rate because we have a good central business office,” he says. “Small groups don’t have resources like that. We also do a great deal of training in proper coding techniques so that we can bill appropriately.”
A Grain of Salt
Before you barge in to your director’s office and ask for a raise, you should understand that the salaries summarized here have severe limitations and should be seen only as rough guidelines. There are major factors that can boost annual compensation, including:
- A heavy load of on-call, night, or weekend work;
- Employment in a geographic region with a shortage of physicians;
- Employment in a geographic region with higher physician incomes (such as the southeast);
- The type of practice you work for; and
- New practices recruiting hospitalists.
Also keep in mind that compensation totals include all bonuses and incentives received during the year.
Find Your Figure
Hospitalist income—particularly productivity-based income—is also directly affected by workload. Dr. Nelson suggests using the information in the SHM survey to find a rough guideline for productivity and compensation.
“Take the compensation figure from the survey for your region, production type, etc. and take the average production numbers from that same subgroup,” he says. “Then do the math to find the number of dollars per encounter or per RVU, and gauge your own numbers. If you have 25% more encounters, your income should be 25% higher than the average.”
The best rule of thumb for estimating what you should make, says Dr. Nelson, is to aim for five to 15% more than physicians working in traditional practice in your market. Unfortunately, information on what other doctors earn may not be readily available. Some sources (including a few listed in the sidebar to this article) provide information on all physician incomes, but is broken down by region at best. “You have to ask around,” says Dr. Nelson. “And if you’re interviewing, ask what they’re offering—then go and interview at a private practice and ask what they’re offering.”
In other words, there’s no easy way to tell if what you make is exactly on the mark for other hospitalists in your area—unless you ask those other hospitalists. But the SHM survey information should provide enough information to give you an idea. You can view an executive summary of the survey or purchase a complete copy at www.hospitalmedicine.org. TH
Jane Jerrard is the monthly writer for “Career Development.”
It’ s easy to find figures on what hospitalists earn these days, but if your own income doesn’t match up, does that mean you’re underpaid? Not necessarily.
The SHM Survey
There are several sources that provide figures on hospitalist income, but SHM offers an accurate, detailed—and the largest representative—picture of what hospitalists earn now. In spring 2006, SHM released its latest comprehensive survey of membership, “The 2005-2006 SHM Survey: The Authoritative Source on the State of the Hospitalist Movement.” The report is based on responses of 396 hospital medicine groups representing more than 2,500 hospitalists. However, Joseph A. Miller, senior vice president of SHM, warns that the survey’s salary figures may skew toward one or more specific demographics.
“In our survey, we have a number of respondents in each cell—academic, pediatric, etc.—as well as a range of geographic areas and other differences,” he says. “Anyone who looks at the metric needs to understand the factors behind it.”
John Nelson, MD, director, hospital practice, Overlake Hospital, Bellevue, Wash., and author of “Practice Management” for The Hospitalist, who has participated in developing and analyzing SHM surveys for years, agrees that the figures in the survey should be used as general guidelines only. “It’s easy to take individual metrics in a vacuum without considering the variables,” he warns.
With these caveats in mind, the basic information on hospitalist compensation from the survey breaks down as follows: (table right)
To put these numbers in perspective, the median number of patient encounters per hospitalist was 2,328 per year, and the median number of work RVUs was 3,213.
Both leader- and physician-hospitalists have enjoyed an 8% increase in compensation, as well as an 8% increase in benefits, compared with the 2003-2004 survey. Non-physician hospitalists have seen a whopping increase in median income of 26% since 2003-2004. (Their benefits increased 7%.)
Perhaps the main reason for steadily increasing hospitalist incomes is that demand for hospitalists continues to exceed supply. “I’ve been trying to recruit hospitalists to my group for years,” says Dr. Nelson. “I thought that by 2002 or 2003, the number of available physicians would exceed the demand—but that hasn’t happened. It’s true that the number of doctors interested in hospital medicine has gone up pretty dramatically, but the demand went up even faster.”
By some estimates, says Dr. Nelson, there are two or three open positions for every hospitalist jobseeker.
—John Nelson, MD
Forms of Payment
To break these figures down further, income varies with type of compensation. In other words, how you are paid can influence how much you’re paid. Physician hospitalists who are paid 100% salary had a median income of $150,000. Those who are 100% productivity/performance-based make more money—a median income of $165,000; and those with a mixed-compensation model make the most of all, with a median income of $170,000.
Currently, according to the SHM survey, only 28% of respondents are 100% salary-based and 5% are 100% productivity/performance-based. The remaining majority (67%) is compensated with a combination of the two. Compared to the 2003-2004 SHM survey, the mixed compensation model increased from 47%.
“The portion of hospitalists paid via straight salary or based solely on production has been declining in the last few years,” says Dr. Nelson. “I think [a] low base and high productivity component is ideal, but [a] lower base does impede recruiting even if the total income is very attractive.”
IPC—The Hospitalist Company, one of the largest employers of hospitalists, uses the same combination of base salary and incentives for all physicians, regardless of their level of experience.
“We might change the salary figures slightly for different geographic areas, says Tim Lary, vice president of physician staffing for IPC, “but within our company, the average physician earns a little bit north of $200,000. A large portion earn over $300,000 because of our incentive plan.” That figure includes a base salary of approximately $150,000; the rest is comprised of incentives based on “typical counters” that hospitalists see, according to Lary, including productivity, quality indicators, and compliance.
Lary postulates that compensation is higher at a large organization like IPC because those employers have an infrastructure in place that ensures cost-effectiveness. “We have a 99.9% collection rate because we have a good central business office,” he says. “Small groups don’t have resources like that. We also do a great deal of training in proper coding techniques so that we can bill appropriately.”
A Grain of Salt
Before you barge in to your director’s office and ask for a raise, you should understand that the salaries summarized here have severe limitations and should be seen only as rough guidelines. There are major factors that can boost annual compensation, including:
- A heavy load of on-call, night, or weekend work;
- Employment in a geographic region with a shortage of physicians;
- Employment in a geographic region with higher physician incomes (such as the southeast);
- The type of practice you work for; and
- New practices recruiting hospitalists.
Also keep in mind that compensation totals include all bonuses and incentives received during the year.
Find Your Figure
Hospitalist income—particularly productivity-based income—is also directly affected by workload. Dr. Nelson suggests using the information in the SHM survey to find a rough guideline for productivity and compensation.
“Take the compensation figure from the survey for your region, production type, etc. and take the average production numbers from that same subgroup,” he says. “Then do the math to find the number of dollars per encounter or per RVU, and gauge your own numbers. If you have 25% more encounters, your income should be 25% higher than the average.”
The best rule of thumb for estimating what you should make, says Dr. Nelson, is to aim for five to 15% more than physicians working in traditional practice in your market. Unfortunately, information on what other doctors earn may not be readily available. Some sources (including a few listed in the sidebar to this article) provide information on all physician incomes, but is broken down by region at best. “You have to ask around,” says Dr. Nelson. “And if you’re interviewing, ask what they’re offering—then go and interview at a private practice and ask what they’re offering.”
In other words, there’s no easy way to tell if what you make is exactly on the mark for other hospitalists in your area—unless you ask those other hospitalists. But the SHM survey information should provide enough information to give you an idea. You can view an executive summary of the survey or purchase a complete copy at www.hospitalmedicine.org. TH
Jane Jerrard is the monthly writer for “Career Development.”
Medicare, Money, and Quality Measures
The federal government—particularly the Centers for Medicare and Medicaid Services (CMS)—is moving faster than anyone thought possible to implement “value-based purchasing,” which ties payment to quality of care and other outcomes. CMS has a congressional mandate to make value-based purchasing a reality by fiscal year 2009.
“As Congress looks at cutting physician payments, they’re very open to alternative payment methods like pay-for-performance,” says Patrick Torcson, MD, MMM, FACP, chair of SHM’s Performance and Standards Task Force, medical director, hospital medicine, St. Tammany Parish Hospital, Covington, La. “There’s tremendous political will behind this.”
Here is an overview of three CMS demonstration programs in various stages that will determine which new payment models may shape your hospital budget—and your salary—in the future.
CMS Gainsharing Demo: An Update
As reported in the October issue of The Hospitalist, CMS has been charged with establishing six three-year gainsharing pilot programs, including two in rural settings, by January 1, 2007.
CMS invited applications for the programs in mid-September, and applications were due by November 17. The six participating hospitals will provide gainsharing payments to physicians who help to save costs. The gainsharing payments will be based on net savings. Each hospital will propose multiple approaches that will both save costs and improve quality and efficiency of care.
“Gainsharing could be a better quality incentive payment model for hospitalists, [but] maybe not for other specialties,” says Dr. Torcson.
New “Gainsharing Plus” Demo—Participation Encouraged!
During Legislative Advocacy Day at the SHM Annual Meeting in Washington, D.C., in May, SHM members personally urged policymakers to broaden the concept of gainsharing and initiate demonstration projects like this that promote physician and hospital collaboration in improving care.
Four months later (in early September) CMS surprised the healthcare community with the announcement of an additional three-year demonstration program that goes beyond the traditional concept of gainsharing—one that will examine whether allowing hospitals to provide financial incentives for physicians to support better care can improve patient outcomes without increasing costs.
“SHM was pleased to hear that CMS was offering this program because we support the development of these payment models,” says Dr. Torcson.
Under the program, known as the Physician-Hospital Collaboration Demonstration (PHCD), hospitals would be paid their usual inpatient rate for the patients’ care but would be allowed to pay physicians a portion of the savings resulting from quality improvement and efficiency initiatives.
In the CMS release announcing this demonstration, former CMS Administrator Mark B. McClellan, MD, PhD, was quoted as saying, “The most costly and intensive physician services are provided in hospitals, yet our payment systems do not support steps by hospitals and doctors to work together to improve care. This demonstration program will support efforts to track and improve the overall episode of patient care, including follow-up and longer-term outcomes.”
The program will begin in 2007, and applications are due by end of business on January 9, 2007. SHM encourages members to explore the possibility of applying for one of the demonstrations with their group and their hospital administrators. Details on the PHCD are available at www.cms.hhs.gov (go to the “Medicare” page and then click the “Demonstration Projects & Evaluation Reports” page. Then click “Medicare Demonstrations).”
Of particular interest is the fact that CMS will allow participating hospitals to set the indicators to be measured. “What they’re asking for are proposals from the hospitals as to what they’ll explore—basing the program on whatever quality indicators the hospital can [use to] measure and demonstrate cost savings,” says Dr. Torcson. “CMS is providing no details regarding specific performance measures.”
Organizations eligible for the PHCD include physician groups, integrated delivery systems (IDSs), and regional coalitions of physician groups. A hospital may be included if it has an affiliation agreement with an eligible physician group. CMS has stated that preference will be given to projects developed and implemented by a consortium of physician groups and their affiliated hospitals. No more than 72 hospitals across all projects will be included in the demonstration.
“This raises the bar that any physician group has to be pretty far along already in measuring quality indicators and performance reporting,” says Dr. Torcson. “It will take a lot of infrastructure to report, measure, [and so on]. I’ll be very impressed with any group that is that far along with performance measurement and reporting. I hope a hospitalist group can be among those that step up and apply.”
Dr. Torcson believes that, while CMS did not specify hospitalists, a hospital medicine group would be uniquely positioned to participate. “Hospitalists are perfect for this,” he emphasizes.
Premier Hospital Demo: Mission Accomplished!
CMS’ first pay-for-performance demonstration program is complete. The Premier Hospital Quality Incentive Demonstration officially ended in September. CMS partnered with Premier, Inc., a nationwide alliance of not-for-profit hospitals, for the three-year demo. At the end of each of the three years, CMS rewarded the top-performing hospitals with cash bonuses. Performance was based on 33 evidence-based quality measures for inpatients with heart attack, heart failure, pneumonia, coronary artery bypass graft, and hip and knee replacements. (The individual measures were compiled into an overall quality score for each clinical condition.)
“I wish all our projects went this well,” said Mark Wynn, director of the Division of Payment Policy Demonstrations, CMS. “We’re absolutely delighted. This program shows the efficacy [of] using pay-for-performance in hospitals.”
According to analysis from Premier, Inc., if every patient in the country with pneumonia, heart bypass, acute myocardial infarction, and hip and knee replacement in 2004 had received most or all (76% to 100%) of a set of widely accepted care processes, it could have resulted in nearly 5,700 fewer deaths, 8,100 fewer complications, 10,000 fewer readmissions, and 750,000 fewer days in the hospital. In addition, hospital costs could have been as much as $1.35 billion lower.
What’s next? Wynn says that CMS is “actively looking at lessons we can use” as the agency prepares a report to be presented to Congress in 2007. “We’ll make a specific recommendation regarding pay-for-performance.”
The Future Is Coming
“Value-based purchasing is here to stay,” says Dr. Torcson. “For the significant amount of money spent on healthcare, you have to see a certain level of quality in return. This hasn’t been so obvious in healthcare. Healthcare is just starting to look like the free market in this regard. There’s a place for both pay-for-performance and gainsharing. The CMS budget is big enough for both.”
SHM is involved in pushing for these changes and wants to prepare members for any new measurement criteria that develop. “We would like for the work of the SHM Performance and Standards Task Force to result in an SHM performance agenda,” says Dr. Torcson. “We want to be able to tell members what to expect when all of these demos become a reality and be able to provide relevant information on designing their programs so that they’re ready.” TH
Jane Jerrard regularly writes “Public Policy.”
The federal government—particularly the Centers for Medicare and Medicaid Services (CMS)—is moving faster than anyone thought possible to implement “value-based purchasing,” which ties payment to quality of care and other outcomes. CMS has a congressional mandate to make value-based purchasing a reality by fiscal year 2009.
“As Congress looks at cutting physician payments, they’re very open to alternative payment methods like pay-for-performance,” says Patrick Torcson, MD, MMM, FACP, chair of SHM’s Performance and Standards Task Force, medical director, hospital medicine, St. Tammany Parish Hospital, Covington, La. “There’s tremendous political will behind this.”
Here is an overview of three CMS demonstration programs in various stages that will determine which new payment models may shape your hospital budget—and your salary—in the future.
CMS Gainsharing Demo: An Update
As reported in the October issue of The Hospitalist, CMS has been charged with establishing six three-year gainsharing pilot programs, including two in rural settings, by January 1, 2007.
CMS invited applications for the programs in mid-September, and applications were due by November 17. The six participating hospitals will provide gainsharing payments to physicians who help to save costs. The gainsharing payments will be based on net savings. Each hospital will propose multiple approaches that will both save costs and improve quality and efficiency of care.
“Gainsharing could be a better quality incentive payment model for hospitalists, [but] maybe not for other specialties,” says Dr. Torcson.
New “Gainsharing Plus” Demo—Participation Encouraged!
During Legislative Advocacy Day at the SHM Annual Meeting in Washington, D.C., in May, SHM members personally urged policymakers to broaden the concept of gainsharing and initiate demonstration projects like this that promote physician and hospital collaboration in improving care.
Four months later (in early September) CMS surprised the healthcare community with the announcement of an additional three-year demonstration program that goes beyond the traditional concept of gainsharing—one that will examine whether allowing hospitals to provide financial incentives for physicians to support better care can improve patient outcomes without increasing costs.
“SHM was pleased to hear that CMS was offering this program because we support the development of these payment models,” says Dr. Torcson.
Under the program, known as the Physician-Hospital Collaboration Demonstration (PHCD), hospitals would be paid their usual inpatient rate for the patients’ care but would be allowed to pay physicians a portion of the savings resulting from quality improvement and efficiency initiatives.
In the CMS release announcing this demonstration, former CMS Administrator Mark B. McClellan, MD, PhD, was quoted as saying, “The most costly and intensive physician services are provided in hospitals, yet our payment systems do not support steps by hospitals and doctors to work together to improve care. This demonstration program will support efforts to track and improve the overall episode of patient care, including follow-up and longer-term outcomes.”
The program will begin in 2007, and applications are due by end of business on January 9, 2007. SHM encourages members to explore the possibility of applying for one of the demonstrations with their group and their hospital administrators. Details on the PHCD are available at www.cms.hhs.gov (go to the “Medicare” page and then click the “Demonstration Projects & Evaluation Reports” page. Then click “Medicare Demonstrations).”
Of particular interest is the fact that CMS will allow participating hospitals to set the indicators to be measured. “What they’re asking for are proposals from the hospitals as to what they’ll explore—basing the program on whatever quality indicators the hospital can [use to] measure and demonstrate cost savings,” says Dr. Torcson. “CMS is providing no details regarding specific performance measures.”
Organizations eligible for the PHCD include physician groups, integrated delivery systems (IDSs), and regional coalitions of physician groups. A hospital may be included if it has an affiliation agreement with an eligible physician group. CMS has stated that preference will be given to projects developed and implemented by a consortium of physician groups and their affiliated hospitals. No more than 72 hospitals across all projects will be included in the demonstration.
“This raises the bar that any physician group has to be pretty far along already in measuring quality indicators and performance reporting,” says Dr. Torcson. “It will take a lot of infrastructure to report, measure, [and so on]. I’ll be very impressed with any group that is that far along with performance measurement and reporting. I hope a hospitalist group can be among those that step up and apply.”
Dr. Torcson believes that, while CMS did not specify hospitalists, a hospital medicine group would be uniquely positioned to participate. “Hospitalists are perfect for this,” he emphasizes.
Premier Hospital Demo: Mission Accomplished!
CMS’ first pay-for-performance demonstration program is complete. The Premier Hospital Quality Incentive Demonstration officially ended in September. CMS partnered with Premier, Inc., a nationwide alliance of not-for-profit hospitals, for the three-year demo. At the end of each of the three years, CMS rewarded the top-performing hospitals with cash bonuses. Performance was based on 33 evidence-based quality measures for inpatients with heart attack, heart failure, pneumonia, coronary artery bypass graft, and hip and knee replacements. (The individual measures were compiled into an overall quality score for each clinical condition.)
“I wish all our projects went this well,” said Mark Wynn, director of the Division of Payment Policy Demonstrations, CMS. “We’re absolutely delighted. This program shows the efficacy [of] using pay-for-performance in hospitals.”
According to analysis from Premier, Inc., if every patient in the country with pneumonia, heart bypass, acute myocardial infarction, and hip and knee replacement in 2004 had received most or all (76% to 100%) of a set of widely accepted care processes, it could have resulted in nearly 5,700 fewer deaths, 8,100 fewer complications, 10,000 fewer readmissions, and 750,000 fewer days in the hospital. In addition, hospital costs could have been as much as $1.35 billion lower.
What’s next? Wynn says that CMS is “actively looking at lessons we can use” as the agency prepares a report to be presented to Congress in 2007. “We’ll make a specific recommendation regarding pay-for-performance.”
The Future Is Coming
“Value-based purchasing is here to stay,” says Dr. Torcson. “For the significant amount of money spent on healthcare, you have to see a certain level of quality in return. This hasn’t been so obvious in healthcare. Healthcare is just starting to look like the free market in this regard. There’s a place for both pay-for-performance and gainsharing. The CMS budget is big enough for both.”
SHM is involved in pushing for these changes and wants to prepare members for any new measurement criteria that develop. “We would like for the work of the SHM Performance and Standards Task Force to result in an SHM performance agenda,” says Dr. Torcson. “We want to be able to tell members what to expect when all of these demos become a reality and be able to provide relevant information on designing their programs so that they’re ready.” TH
Jane Jerrard regularly writes “Public Policy.”
The federal government—particularly the Centers for Medicare and Medicaid Services (CMS)—is moving faster than anyone thought possible to implement “value-based purchasing,” which ties payment to quality of care and other outcomes. CMS has a congressional mandate to make value-based purchasing a reality by fiscal year 2009.
“As Congress looks at cutting physician payments, they’re very open to alternative payment methods like pay-for-performance,” says Patrick Torcson, MD, MMM, FACP, chair of SHM’s Performance and Standards Task Force, medical director, hospital medicine, St. Tammany Parish Hospital, Covington, La. “There’s tremendous political will behind this.”
Here is an overview of three CMS demonstration programs in various stages that will determine which new payment models may shape your hospital budget—and your salary—in the future.
CMS Gainsharing Demo: An Update
As reported in the October issue of The Hospitalist, CMS has been charged with establishing six three-year gainsharing pilot programs, including two in rural settings, by January 1, 2007.
CMS invited applications for the programs in mid-September, and applications were due by November 17. The six participating hospitals will provide gainsharing payments to physicians who help to save costs. The gainsharing payments will be based on net savings. Each hospital will propose multiple approaches that will both save costs and improve quality and efficiency of care.
“Gainsharing could be a better quality incentive payment model for hospitalists, [but] maybe not for other specialties,” says Dr. Torcson.
New “Gainsharing Plus” Demo—Participation Encouraged!
During Legislative Advocacy Day at the SHM Annual Meeting in Washington, D.C., in May, SHM members personally urged policymakers to broaden the concept of gainsharing and initiate demonstration projects like this that promote physician and hospital collaboration in improving care.
Four months later (in early September) CMS surprised the healthcare community with the announcement of an additional three-year demonstration program that goes beyond the traditional concept of gainsharing—one that will examine whether allowing hospitals to provide financial incentives for physicians to support better care can improve patient outcomes without increasing costs.
“SHM was pleased to hear that CMS was offering this program because we support the development of these payment models,” says Dr. Torcson.
Under the program, known as the Physician-Hospital Collaboration Demonstration (PHCD), hospitals would be paid their usual inpatient rate for the patients’ care but would be allowed to pay physicians a portion of the savings resulting from quality improvement and efficiency initiatives.
In the CMS release announcing this demonstration, former CMS Administrator Mark B. McClellan, MD, PhD, was quoted as saying, “The most costly and intensive physician services are provided in hospitals, yet our payment systems do not support steps by hospitals and doctors to work together to improve care. This demonstration program will support efforts to track and improve the overall episode of patient care, including follow-up and longer-term outcomes.”
The program will begin in 2007, and applications are due by end of business on January 9, 2007. SHM encourages members to explore the possibility of applying for one of the demonstrations with their group and their hospital administrators. Details on the PHCD are available at www.cms.hhs.gov (go to the “Medicare” page and then click the “Demonstration Projects & Evaluation Reports” page. Then click “Medicare Demonstrations).”
Of particular interest is the fact that CMS will allow participating hospitals to set the indicators to be measured. “What they’re asking for are proposals from the hospitals as to what they’ll explore—basing the program on whatever quality indicators the hospital can [use to] measure and demonstrate cost savings,” says Dr. Torcson. “CMS is providing no details regarding specific performance measures.”
Organizations eligible for the PHCD include physician groups, integrated delivery systems (IDSs), and regional coalitions of physician groups. A hospital may be included if it has an affiliation agreement with an eligible physician group. CMS has stated that preference will be given to projects developed and implemented by a consortium of physician groups and their affiliated hospitals. No more than 72 hospitals across all projects will be included in the demonstration.
“This raises the bar that any physician group has to be pretty far along already in measuring quality indicators and performance reporting,” says Dr. Torcson. “It will take a lot of infrastructure to report, measure, [and so on]. I’ll be very impressed with any group that is that far along with performance measurement and reporting. I hope a hospitalist group can be among those that step up and apply.”
Dr. Torcson believes that, while CMS did not specify hospitalists, a hospital medicine group would be uniquely positioned to participate. “Hospitalists are perfect for this,” he emphasizes.
Premier Hospital Demo: Mission Accomplished!
CMS’ first pay-for-performance demonstration program is complete. The Premier Hospital Quality Incentive Demonstration officially ended in September. CMS partnered with Premier, Inc., a nationwide alliance of not-for-profit hospitals, for the three-year demo. At the end of each of the three years, CMS rewarded the top-performing hospitals with cash bonuses. Performance was based on 33 evidence-based quality measures for inpatients with heart attack, heart failure, pneumonia, coronary artery bypass graft, and hip and knee replacements. (The individual measures were compiled into an overall quality score for each clinical condition.)
“I wish all our projects went this well,” said Mark Wynn, director of the Division of Payment Policy Demonstrations, CMS. “We’re absolutely delighted. This program shows the efficacy [of] using pay-for-performance in hospitals.”
According to analysis from Premier, Inc., if every patient in the country with pneumonia, heart bypass, acute myocardial infarction, and hip and knee replacement in 2004 had received most or all (76% to 100%) of a set of widely accepted care processes, it could have resulted in nearly 5,700 fewer deaths, 8,100 fewer complications, 10,000 fewer readmissions, and 750,000 fewer days in the hospital. In addition, hospital costs could have been as much as $1.35 billion lower.
What’s next? Wynn says that CMS is “actively looking at lessons we can use” as the agency prepares a report to be presented to Congress in 2007. “We’ll make a specific recommendation regarding pay-for-performance.”
The Future Is Coming
“Value-based purchasing is here to stay,” says Dr. Torcson. “For the significant amount of money spent on healthcare, you have to see a certain level of quality in return. This hasn’t been so obvious in healthcare. Healthcare is just starting to look like the free market in this regard. There’s a place for both pay-for-performance and gainsharing. The CMS budget is big enough for both.”
SHM is involved in pushing for these changes and wants to prepare members for any new measurement criteria that develop. “We would like for the work of the SHM Performance and Standards Task Force to result in an SHM performance agenda,” says Dr. Torcson. “We want to be able to tell members what to expect when all of these demos become a reality and be able to provide relevant information on designing their programs so that they’re ready.” TH
Jane Jerrard regularly writes “Public Policy.”
Robot Pharmd
One way to reduce medication errors in your hospital pharmacy is to put a robot in charge of stocking and dispensing medication doses. Roughly 300 U.S. hospitals have done just that and have, as a result, seen their in-pharmacy errors drop significantly. In this instance, robots simply don’t make mistakes.
Manufactured by McKesson Automation of Pittsburgh, Pa., ROBOT-Rx is the lead robot: McKesson estimates that 97% to 98% of hospital pharmacies with a medication-dispensing robot are using their product. ROBOT-Rx units installed in hospitals collectively dispense a half billion bar-coded doses, error-free, every year.
Meet Ernie
Evergreen Hospital Medical Center in Kirkland, Wash., is a 235-bed facility with an average daily census of 175. In March 2004, their pharmacy acquired a ROBOT-Rx, which dispenses up to 93% of all patient medications. Called Ernie (short for Evergreen Robot Noticeably Improving Efficiency), the robot does indeed improve pharmacy efficiency.
“Pharmacists still have to review orders, but the robot saves us time in the pharmacy,” says Bob Blanchard, pharmacy director at Evergreen. “Now they can be out on the floor more, where the orders occur, before mistakes happen.”
The biggest benefit of having the robot is an ongoing reduction in errors. “A good hospital pharmacy might have a 0.5% to 1% error rate,” says Blanchard, “but you have to look at the number of doses dispensed. In a busy hospital—like here—the pharmacy dispenses 1,200-1,300 doses a day. Translate that error rate, and you’ve got five or six errors each day.” Since Ernie took over the job of dispensing drugs, the number of medication errors has been reduced by 25%. It’s worth noting, though, that hospitalists and other doctors at Evergreen Hospital have no interaction with Ernie.
What Does It Take to Start Up a Robot?
Ordering and installing the robot and implementing a new system called for an overhaul of the pharmacy—in more ways than one. “It takes a bit of planning to start up,” admits Blanchard. “Very few med[ication]s are sent from the manufacturer with readable barcodes, except for IVs. We bought a couple of packaging machines, which went into the robot.”
The packaging machines are actually part of the robot. The robot is huge and is actually multiple machines working from a single “brain.” The machines parcel the bulk meds into single doses and barcode them as this happens.
A recent Food and Drug Administration (FDA) mandate requires pharmaceutical companies to include a bar code on packaging for medications, but that applies to bulk packages received at a pharmacy, not single doses.
Ernie takes up about 100 square feet in an octagon-shaped room in the hospital pharmacy. The room has 22 computerized drug-dispensing cabinets. In the center is an electronic arm that can rotate and use suction cups to pick up drug packets. The robot will grab a packet and laser-scan the bar code to ensure that it has picked the correct medication. If the bar code doesn’t match, the arm drops the packet on the floor or puts it in a bin for a pharmacist to check.
After verifying the correct bar code, the robot will place the dose into an envelope marked for a specific patient. The robot also restocks packaged doses that have been checked by pharmacists. Ernie receives the latest patient information automatically. “The robot directly interfaces with the pharmacy information system,” explains Rodger Fletcher, ROBOT-Rx product marketing manager at McKesson. “The robot … seamlessly integrates with nearly every other pharmacy information system.”
Take It to the Next Level
Evergreen Hospital has plans to further reduce their medication error rate. “Most errors occur after the drugs leave the pharmacy, on the hospital floor,” states Blanchard. “We see errors with wrong medications, wrong patients, and wrong times.”
The solution for reducing these errors is to implement additional technology. “We want to get bar coding at the bedside, where we scan the patient, medication, and nurse,” he explains. “This will catch any problem at that time, whether it’s the wrong medication, the wrong dose, or the wrong time.”
Getting Ernie installed was an integral part of this solution. “With the robot, we’re partway there. By the end of next year, we hope to have the bedside piece in place. We have all our medications bar-coded; we need basic technology at the bedside,” says Blanchard. “The selection and correct patient information are taken care of by the robot.”
Bar code scanning of medications at bedside is becoming more common. “We’re seeing a lot of momentum for this,” says Fletcher. “Industry statistics show that 7.5% to 10% of all hospitals have implemented [a bedside medication system], and others are universally planning one. The robot was developed with this in mind.”
For now, Evergreen Hospital is happy with the first stage in reducing medication errors: having Ernie sort and dispense patient meds. “It’s been a long time coming,” says Blanchard. TH
Jane Jerrard is a frequent contributor to The Hospitalist.
One way to reduce medication errors in your hospital pharmacy is to put a robot in charge of stocking and dispensing medication doses. Roughly 300 U.S. hospitals have done just that and have, as a result, seen their in-pharmacy errors drop significantly. In this instance, robots simply don’t make mistakes.
Manufactured by McKesson Automation of Pittsburgh, Pa., ROBOT-Rx is the lead robot: McKesson estimates that 97% to 98% of hospital pharmacies with a medication-dispensing robot are using their product. ROBOT-Rx units installed in hospitals collectively dispense a half billion bar-coded doses, error-free, every year.
Meet Ernie
Evergreen Hospital Medical Center in Kirkland, Wash., is a 235-bed facility with an average daily census of 175. In March 2004, their pharmacy acquired a ROBOT-Rx, which dispenses up to 93% of all patient medications. Called Ernie (short for Evergreen Robot Noticeably Improving Efficiency), the robot does indeed improve pharmacy efficiency.
“Pharmacists still have to review orders, but the robot saves us time in the pharmacy,” says Bob Blanchard, pharmacy director at Evergreen. “Now they can be out on the floor more, where the orders occur, before mistakes happen.”
The biggest benefit of having the robot is an ongoing reduction in errors. “A good hospital pharmacy might have a 0.5% to 1% error rate,” says Blanchard, “but you have to look at the number of doses dispensed. In a busy hospital—like here—the pharmacy dispenses 1,200-1,300 doses a day. Translate that error rate, and you’ve got five or six errors each day.” Since Ernie took over the job of dispensing drugs, the number of medication errors has been reduced by 25%. It’s worth noting, though, that hospitalists and other doctors at Evergreen Hospital have no interaction with Ernie.
What Does It Take to Start Up a Robot?
Ordering and installing the robot and implementing a new system called for an overhaul of the pharmacy—in more ways than one. “It takes a bit of planning to start up,” admits Blanchard. “Very few med[ication]s are sent from the manufacturer with readable barcodes, except for IVs. We bought a couple of packaging machines, which went into the robot.”
The packaging machines are actually part of the robot. The robot is huge and is actually multiple machines working from a single “brain.” The machines parcel the bulk meds into single doses and barcode them as this happens.
A recent Food and Drug Administration (FDA) mandate requires pharmaceutical companies to include a bar code on packaging for medications, but that applies to bulk packages received at a pharmacy, not single doses.
Ernie takes up about 100 square feet in an octagon-shaped room in the hospital pharmacy. The room has 22 computerized drug-dispensing cabinets. In the center is an electronic arm that can rotate and use suction cups to pick up drug packets. The robot will grab a packet and laser-scan the bar code to ensure that it has picked the correct medication. If the bar code doesn’t match, the arm drops the packet on the floor or puts it in a bin for a pharmacist to check.
After verifying the correct bar code, the robot will place the dose into an envelope marked for a specific patient. The robot also restocks packaged doses that have been checked by pharmacists. Ernie receives the latest patient information automatically. “The robot directly interfaces with the pharmacy information system,” explains Rodger Fletcher, ROBOT-Rx product marketing manager at McKesson. “The robot … seamlessly integrates with nearly every other pharmacy information system.”
Take It to the Next Level
Evergreen Hospital has plans to further reduce their medication error rate. “Most errors occur after the drugs leave the pharmacy, on the hospital floor,” states Blanchard. “We see errors with wrong medications, wrong patients, and wrong times.”
The solution for reducing these errors is to implement additional technology. “We want to get bar coding at the bedside, where we scan the patient, medication, and nurse,” he explains. “This will catch any problem at that time, whether it’s the wrong medication, the wrong dose, or the wrong time.”
Getting Ernie installed was an integral part of this solution. “With the robot, we’re partway there. By the end of next year, we hope to have the bedside piece in place. We have all our medications bar-coded; we need basic technology at the bedside,” says Blanchard. “The selection and correct patient information are taken care of by the robot.”
Bar code scanning of medications at bedside is becoming more common. “We’re seeing a lot of momentum for this,” says Fletcher. “Industry statistics show that 7.5% to 10% of all hospitals have implemented [a bedside medication system], and others are universally planning one. The robot was developed with this in mind.”
For now, Evergreen Hospital is happy with the first stage in reducing medication errors: having Ernie sort and dispense patient meds. “It’s been a long time coming,” says Blanchard. TH
Jane Jerrard is a frequent contributor to The Hospitalist.
One way to reduce medication errors in your hospital pharmacy is to put a robot in charge of stocking and dispensing medication doses. Roughly 300 U.S. hospitals have done just that and have, as a result, seen their in-pharmacy errors drop significantly. In this instance, robots simply don’t make mistakes.
Manufactured by McKesson Automation of Pittsburgh, Pa., ROBOT-Rx is the lead robot: McKesson estimates that 97% to 98% of hospital pharmacies with a medication-dispensing robot are using their product. ROBOT-Rx units installed in hospitals collectively dispense a half billion bar-coded doses, error-free, every year.
Meet Ernie
Evergreen Hospital Medical Center in Kirkland, Wash., is a 235-bed facility with an average daily census of 175. In March 2004, their pharmacy acquired a ROBOT-Rx, which dispenses up to 93% of all patient medications. Called Ernie (short for Evergreen Robot Noticeably Improving Efficiency), the robot does indeed improve pharmacy efficiency.
“Pharmacists still have to review orders, but the robot saves us time in the pharmacy,” says Bob Blanchard, pharmacy director at Evergreen. “Now they can be out on the floor more, where the orders occur, before mistakes happen.”
The biggest benefit of having the robot is an ongoing reduction in errors. “A good hospital pharmacy might have a 0.5% to 1% error rate,” says Blanchard, “but you have to look at the number of doses dispensed. In a busy hospital—like here—the pharmacy dispenses 1,200-1,300 doses a day. Translate that error rate, and you’ve got five or six errors each day.” Since Ernie took over the job of dispensing drugs, the number of medication errors has been reduced by 25%. It’s worth noting, though, that hospitalists and other doctors at Evergreen Hospital have no interaction with Ernie.
What Does It Take to Start Up a Robot?
Ordering and installing the robot and implementing a new system called for an overhaul of the pharmacy—in more ways than one. “It takes a bit of planning to start up,” admits Blanchard. “Very few med[ication]s are sent from the manufacturer with readable barcodes, except for IVs. We bought a couple of packaging machines, which went into the robot.”
The packaging machines are actually part of the robot. The robot is huge and is actually multiple machines working from a single “brain.” The machines parcel the bulk meds into single doses and barcode them as this happens.
A recent Food and Drug Administration (FDA) mandate requires pharmaceutical companies to include a bar code on packaging for medications, but that applies to bulk packages received at a pharmacy, not single doses.
Ernie takes up about 100 square feet in an octagon-shaped room in the hospital pharmacy. The room has 22 computerized drug-dispensing cabinets. In the center is an electronic arm that can rotate and use suction cups to pick up drug packets. The robot will grab a packet and laser-scan the bar code to ensure that it has picked the correct medication. If the bar code doesn’t match, the arm drops the packet on the floor or puts it in a bin for a pharmacist to check.
After verifying the correct bar code, the robot will place the dose into an envelope marked for a specific patient. The robot also restocks packaged doses that have been checked by pharmacists. Ernie receives the latest patient information automatically. “The robot directly interfaces with the pharmacy information system,” explains Rodger Fletcher, ROBOT-Rx product marketing manager at McKesson. “The robot … seamlessly integrates with nearly every other pharmacy information system.”
Take It to the Next Level
Evergreen Hospital has plans to further reduce their medication error rate. “Most errors occur after the drugs leave the pharmacy, on the hospital floor,” states Blanchard. “We see errors with wrong medications, wrong patients, and wrong times.”
The solution for reducing these errors is to implement additional technology. “We want to get bar coding at the bedside, where we scan the patient, medication, and nurse,” he explains. “This will catch any problem at that time, whether it’s the wrong medication, the wrong dose, or the wrong time.”
Getting Ernie installed was an integral part of this solution. “With the robot, we’re partway there. By the end of next year, we hope to have the bedside piece in place. We have all our medications bar-coded; we need basic technology at the bedside,” says Blanchard. “The selection and correct patient information are taken care of by the robot.”
Bar code scanning of medications at bedside is becoming more common. “We’re seeing a lot of momentum for this,” says Fletcher. “Industry statistics show that 7.5% to 10% of all hospitals have implemented [a bedside medication system], and others are universally planning one. The robot was developed with this in mind.”
For now, Evergreen Hospital is happy with the first stage in reducing medication errors: having Ernie sort and dispense patient meds. “It’s been a long time coming,” says Blanchard. TH
Jane Jerrard is a frequent contributor to The Hospitalist.
You Can Always Get What You Want
How prepared are you to negotiate the best possible contract for your next position? Do you know what you can realistically ask for? If the salary offered seems too low, do other factors make the job a perfect fit?
In order to get the most beneficial contract with your next hospitalist position, you must have confidence in your negotiation skills. Here are some steps that may help.
1. Recognize Your Priorities
Before you set foot in your first interview with an organization, you must know your own mind—what exactly do you want to “win” in a contract negotiation?
“Your first step should be quiet reflection, where you figure out what you want and what [part] of that is non-negotiable,” advises Fred A. McCurdy, MD, PhD, MBA, FAAP, CPE, professor and regional chairman of the department of pediatrics, Texas Tech University Health Sciences Center at Amarillo. Most people focus on money when they anticipate negotiating employment, but there are other factors to consider, such as schedule (on-duty and on-call hours); opportunities for advancement, including research, project management, and teaching; and, of course, benefits, including insurance and retirement packages. Consider carefully which factors matter most to you, then rank them to organize your personal priorities.
Dr. McCurdy recommends the process he uses for all the negotiations he participates in as part of his job. “I think through the principles of each negotiation situation and write them out,” he says. “I pick out the non-negotiable items as well as the items I hope to achieve.”
2. Do Your Homework
It’s tough to negotiate your salary or your benefits when you don’t know the market. “Don’t walk in without knowing your facts,” warns Dr. McCurdy. “Do your homework to see what the market is and how payment systems work.”
Research the potential employer to find out what they’re paying other physicians and how they pay. “You can ask [the interviewers], ‘What are you currently paying your other hospitalists?’ ” says Dr. McCurdy. “You might get [them to tell you] a pay range.”
Ask questions in your interviews, and conduct independent research on the organization and on the market.
“You can obtain a lot of information on your own,” he explains. “The MGMA [Medical Group Management Association] and the Association of American Medical Colleges (AAMC) have salary scales available. Salaries are public information for people who work in public institutions like university hospitals.”
SHM also provides up-to-date salary information in its “Bi-Annual Survey on the State of the Hospital Medicine Movement,” available at www.hospitalmedicine.org.
3. Know Your Strengths
Another homework assignment before the interview process: Know your strongest selling points. Whether you have an excellent record as a faculty member or a strong background in heading up task forces, your unique strengths will be your strongest argument in negotiating your contract.
“The most effective way to negotiate is to talk about the value-added,” says Dr. McCurdy. “Find out what they want, and speak to that. You’ll have to figure that out as you go.”
It might be what you can do to improve the organization’s bottom line; it might be specific skills or expertise you bring to the table, such as teaching proficiency or research skills.
What about recent graduates who are seeking their first job as a hospitalist? “People right out of training seem to have distinct advantages that they don’t emphasize,” says Dr. McCurdy. “They’re young and have a high energy level, for one thing. Their knowledge base is very current, so they’re cutting edge, and they have quality of training—they were recently instructed by cutting-edge teachers.”
4. Look Beyond Salary
Of course you’ll want to negotiate for as much money as you can, but other factors may make a lower salary worthwhile to you. “Lots of organizations have a lot of non-tangibles to offer, but many physicians go into this ill informed” about what they can get, says Dr. McCurdy. You might ask for “some equity holding in the organization you’re looking to become part of” if it’s a privately held hospital medicine group.
“Think about various trade-offs,” urges Dr. McCurdy. “For example, you might accept a lower salary for less on-call time. Or if you’re considering a position in academic medicine, you know that your residents will take most of your night hours—is that worth a lower salary to you?”
You might also consider “access to a foundation that could help you leverage a project you want to do or a situation where you have a chance to spin off intellectual property where you keep the proceeds,” he suggests. “It all depends on the organization. What do they have that would be valuable to you?”
5. Practice Your Negotiation Skills
One last piece of homework before you walk into the final interview: Do a practice run of how the meeting might go.
Physicians don’t always practice negotiation conversations, says Dr. McCurdy. “Find someone who will practice with you, who will throw a lot of questions at you. I used a personal coach. She had me practicing ‘how to deal with Fred when he’s in conflict.’ I hated it, and I’m so glad I did it!”
So do your homework and be prepared to argue your strengths, stick up for your non-negotiables, and resign yourself to giving in on some of your other points. With insight, information, and practice, you’ll be in an excellent position to walk away from the table with most—if not all—of what you want in your next contract. TH
Jane Jerrard writes “Career Management” monthly for The Hospitalist.
How prepared are you to negotiate the best possible contract for your next position? Do you know what you can realistically ask for? If the salary offered seems too low, do other factors make the job a perfect fit?
In order to get the most beneficial contract with your next hospitalist position, you must have confidence in your negotiation skills. Here are some steps that may help.
1. Recognize Your Priorities
Before you set foot in your first interview with an organization, you must know your own mind—what exactly do you want to “win” in a contract negotiation?
“Your first step should be quiet reflection, where you figure out what you want and what [part] of that is non-negotiable,” advises Fred A. McCurdy, MD, PhD, MBA, FAAP, CPE, professor and regional chairman of the department of pediatrics, Texas Tech University Health Sciences Center at Amarillo. Most people focus on money when they anticipate negotiating employment, but there are other factors to consider, such as schedule (on-duty and on-call hours); opportunities for advancement, including research, project management, and teaching; and, of course, benefits, including insurance and retirement packages. Consider carefully which factors matter most to you, then rank them to organize your personal priorities.
Dr. McCurdy recommends the process he uses for all the negotiations he participates in as part of his job. “I think through the principles of each negotiation situation and write them out,” he says. “I pick out the non-negotiable items as well as the items I hope to achieve.”
2. Do Your Homework
It’s tough to negotiate your salary or your benefits when you don’t know the market. “Don’t walk in without knowing your facts,” warns Dr. McCurdy. “Do your homework to see what the market is and how payment systems work.”
Research the potential employer to find out what they’re paying other physicians and how they pay. “You can ask [the interviewers], ‘What are you currently paying your other hospitalists?’ ” says Dr. McCurdy. “You might get [them to tell you] a pay range.”
Ask questions in your interviews, and conduct independent research on the organization and on the market.
“You can obtain a lot of information on your own,” he explains. “The MGMA [Medical Group Management Association] and the Association of American Medical Colleges (AAMC) have salary scales available. Salaries are public information for people who work in public institutions like university hospitals.”
SHM also provides up-to-date salary information in its “Bi-Annual Survey on the State of the Hospital Medicine Movement,” available at www.hospitalmedicine.org.
3. Know Your Strengths
Another homework assignment before the interview process: Know your strongest selling points. Whether you have an excellent record as a faculty member or a strong background in heading up task forces, your unique strengths will be your strongest argument in negotiating your contract.
“The most effective way to negotiate is to talk about the value-added,” says Dr. McCurdy. “Find out what they want, and speak to that. You’ll have to figure that out as you go.”
It might be what you can do to improve the organization’s bottom line; it might be specific skills or expertise you bring to the table, such as teaching proficiency or research skills.
What about recent graduates who are seeking their first job as a hospitalist? “People right out of training seem to have distinct advantages that they don’t emphasize,” says Dr. McCurdy. “They’re young and have a high energy level, for one thing. Their knowledge base is very current, so they’re cutting edge, and they have quality of training—they were recently instructed by cutting-edge teachers.”
4. Look Beyond Salary
Of course you’ll want to negotiate for as much money as you can, but other factors may make a lower salary worthwhile to you. “Lots of organizations have a lot of non-tangibles to offer, but many physicians go into this ill informed” about what they can get, says Dr. McCurdy. You might ask for “some equity holding in the organization you’re looking to become part of” if it’s a privately held hospital medicine group.
“Think about various trade-offs,” urges Dr. McCurdy. “For example, you might accept a lower salary for less on-call time. Or if you’re considering a position in academic medicine, you know that your residents will take most of your night hours—is that worth a lower salary to you?”
You might also consider “access to a foundation that could help you leverage a project you want to do or a situation where you have a chance to spin off intellectual property where you keep the proceeds,” he suggests. “It all depends on the organization. What do they have that would be valuable to you?”
5. Practice Your Negotiation Skills
One last piece of homework before you walk into the final interview: Do a practice run of how the meeting might go.
Physicians don’t always practice negotiation conversations, says Dr. McCurdy. “Find someone who will practice with you, who will throw a lot of questions at you. I used a personal coach. She had me practicing ‘how to deal with Fred when he’s in conflict.’ I hated it, and I’m so glad I did it!”
So do your homework and be prepared to argue your strengths, stick up for your non-negotiables, and resign yourself to giving in on some of your other points. With insight, information, and practice, you’ll be in an excellent position to walk away from the table with most—if not all—of what you want in your next contract. TH
Jane Jerrard writes “Career Management” monthly for The Hospitalist.
How prepared are you to negotiate the best possible contract for your next position? Do you know what you can realistically ask for? If the salary offered seems too low, do other factors make the job a perfect fit?
In order to get the most beneficial contract with your next hospitalist position, you must have confidence in your negotiation skills. Here are some steps that may help.
1. Recognize Your Priorities
Before you set foot in your first interview with an organization, you must know your own mind—what exactly do you want to “win” in a contract negotiation?
“Your first step should be quiet reflection, where you figure out what you want and what [part] of that is non-negotiable,” advises Fred A. McCurdy, MD, PhD, MBA, FAAP, CPE, professor and regional chairman of the department of pediatrics, Texas Tech University Health Sciences Center at Amarillo. Most people focus on money when they anticipate negotiating employment, but there are other factors to consider, such as schedule (on-duty and on-call hours); opportunities for advancement, including research, project management, and teaching; and, of course, benefits, including insurance and retirement packages. Consider carefully which factors matter most to you, then rank them to organize your personal priorities.
Dr. McCurdy recommends the process he uses for all the negotiations he participates in as part of his job. “I think through the principles of each negotiation situation and write them out,” he says. “I pick out the non-negotiable items as well as the items I hope to achieve.”
2. Do Your Homework
It’s tough to negotiate your salary or your benefits when you don’t know the market. “Don’t walk in without knowing your facts,” warns Dr. McCurdy. “Do your homework to see what the market is and how payment systems work.”
Research the potential employer to find out what they’re paying other physicians and how they pay. “You can ask [the interviewers], ‘What are you currently paying your other hospitalists?’ ” says Dr. McCurdy. “You might get [them to tell you] a pay range.”
Ask questions in your interviews, and conduct independent research on the organization and on the market.
“You can obtain a lot of information on your own,” he explains. “The MGMA [Medical Group Management Association] and the Association of American Medical Colleges (AAMC) have salary scales available. Salaries are public information for people who work in public institutions like university hospitals.”
SHM also provides up-to-date salary information in its “Bi-Annual Survey on the State of the Hospital Medicine Movement,” available at www.hospitalmedicine.org.
3. Know Your Strengths
Another homework assignment before the interview process: Know your strongest selling points. Whether you have an excellent record as a faculty member or a strong background in heading up task forces, your unique strengths will be your strongest argument in negotiating your contract.
“The most effective way to negotiate is to talk about the value-added,” says Dr. McCurdy. “Find out what they want, and speak to that. You’ll have to figure that out as you go.”
It might be what you can do to improve the organization’s bottom line; it might be specific skills or expertise you bring to the table, such as teaching proficiency or research skills.
What about recent graduates who are seeking their first job as a hospitalist? “People right out of training seem to have distinct advantages that they don’t emphasize,” says Dr. McCurdy. “They’re young and have a high energy level, for one thing. Their knowledge base is very current, so they’re cutting edge, and they have quality of training—they were recently instructed by cutting-edge teachers.”
4. Look Beyond Salary
Of course you’ll want to negotiate for as much money as you can, but other factors may make a lower salary worthwhile to you. “Lots of organizations have a lot of non-tangibles to offer, but many physicians go into this ill informed” about what they can get, says Dr. McCurdy. You might ask for “some equity holding in the organization you’re looking to become part of” if it’s a privately held hospital medicine group.
“Think about various trade-offs,” urges Dr. McCurdy. “For example, you might accept a lower salary for less on-call time. Or if you’re considering a position in academic medicine, you know that your residents will take most of your night hours—is that worth a lower salary to you?”
You might also consider “access to a foundation that could help you leverage a project you want to do or a situation where you have a chance to spin off intellectual property where you keep the proceeds,” he suggests. “It all depends on the organization. What do they have that would be valuable to you?”
5. Practice Your Negotiation Skills
One last piece of homework before you walk into the final interview: Do a practice run of how the meeting might go.
Physicians don’t always practice negotiation conversations, says Dr. McCurdy. “Find someone who will practice with you, who will throw a lot of questions at you. I used a personal coach. She had me practicing ‘how to deal with Fred when he’s in conflict.’ I hated it, and I’m so glad I did it!”
So do your homework and be prepared to argue your strengths, stick up for your non-negotiables, and resign yourself to giving in on some of your other points. With insight, information, and practice, you’ll be in an excellent position to walk away from the table with most—if not all—of what you want in your next contract. TH
Jane Jerrard writes “Career Management” monthly for The Hospitalist.
Small Gains Made by Gainsharing
While pay-for-performance has become one of the hottest trends in healthcare, another program that would tie payment to performance is starting to get some notice. Gainsharing is on the horizon for hospitals and the physicians who work for them, but the advances made in this savings-sharing model are questionable.
Gainsharing Defined
What is gainsharing? It has to do with the sharing of gains—or of costs saved, to be more precise. Under a gainsharing model, a hospital will select specific best practices, including standard policies, procedures, and/or protocols that will improve quality of care and reduce financial costs. Any reduction in costs that results from physicians following these best practices is documented by the hospital over a specified period. After monitoring and noting that physicians met the predetermined benchmarks for quality of care, the hospital then pays a cash bonus to those who contributed to the cost reduction.
Gainsharing can take various forms, but generally the practice applies to services provided within a single clinical specialty such as oncology or cardiac surgery. “Gainsharing could affect anyone who cares for patients in a hospital if it became legal,” says Ron Greeno, MD, FCCP, chief medical officer, Cogent Healthcare, Irvine, Calif., “but hospitalists are the perfect group of doctors to take on projects like this.”
The most recent gainsharing programs have focused on the use of pre-approved medical devices, equipment, and supplies. For example, a hospital might recommend that physicians use less costly items with the same level of effectiveness, such as a knee-high sequential compression device rather than a thigh-high device.
How much money is involved in gainsharing? Of course, it depends on the program. “Gainsharing deals could include significant money depending on how they are structured,” explains Dr. Greeno, “if you did something that results in enough quality benefit.”
Example: A hospital asked a physician group to give an appropriate antibiotic to patients as soon as possible upon admission and was consequently able to show that they avoided a prolonged stay for five of those patients and that this saved the hospital $1 million in costs. “If the hospital gave 50% of that savings to 20 physicians who helped meet that goal, why would anyone want to regulate against that?” asks Dr. Greeno.
A Brief History of Gainsharing
There is a good reason you may not have heard much about gainsharing; the practice was banned in 1999 by the federal Office of Inspector General (OIG). The OIG was concerned that gainsharing could limit patient care and might lead to physicians “cherry picking” patients who are healthier, while sending seriously ill patients to a different hospital.
Only in September 2005 did the OIG carry out a half-hearted reversal, providing advisory opinions that allow pre-approved arrangements between individual hospitals and physician groups—as long as appropriate safeguards are adopted to protect against abuse.
“This was a very small change,” says Dr. Greeno. “Their approval is highly limited. They have basically agreed to very specific, very short trials of gainsharing, which they will approve one at a time.”
Dr. Greeno is frustrated by the baby step taken by the federal government. “The OIG equates gainsharing with denial of care,” he says. “Their limits are preventing a tremendous opportunity for hospitals and physicians to partner to provide quality care; they’re saying we can’t provide the right incentive scheme.”
The point that Dr. Greeno finds most frustrating is the vast difference of opinion on gainsharing versus another payment trend. “The irony is that all gainsharing is pay-for-performance,” says Dr. Greeno. “The difference is that instead of Medicare paying, it’s the individual hospital paying for performance. Even people who really understand healthcare haven’t connected the dots. They’re pushing for pay-for-performance, but telling hospitals they can’t do essentially the same thing. The hospital industry is developing a strategy to point that out to Capitol Hill, and in my opinion, SHM should develop a more formal approach to do the same.”
Current State of Gainsharing
There have been a few gainsharing programs that were approved by the OIG. “There are a couple of [pilot programs] that private hospitals have done,” says Dr. Greeno. “All the projects so far have targeted medical devices. One New Jersey hospital focused on the use of defibrillators. They spent a lot of money setting up the project, which only lasted one year. As I said, these [approved projects] are very limited.”
Gainsharing programs that focus on medical devices are simple because cost savings are easy to track; however, gainsharing could be built around quality indicators that are found in pay-for-performance programs. “Cutting costs is not the only way to improve quality,” says Dr. Greeno. “That’s not how you get the biggest bang for your buck. That comes when someone will invest in capabilities and processes that target the 30% of costs spent on each patient in the hospital that is waste.”
Pilot Programs Planned
Following the OIG reversal, Congress passed the Deficit Reduction Omnibus Reconciliation Act of 2005, which included funding for a gainsharing demonstration project. The Centers for Medicare and Medicaid Services (CMS) will establish six gainsharing pilot programs, including two in rural settings, by January 1, 2007. The bill states that these demonstration programs are intended to “test and evaluate methodologies and arrangements between hospitals and physicians designed to govern the utilization of inpatient hospital resources and physician work to improve quality and efficiency of care provided to Medicare beneficiaries.”
You can review details on the gainsharing demonstration on the CMS Web site at www.cms.hhs.gov/DemoProjectsEvalRpts/MD/itemdetail.asp?filterType=none&filterByDID=-99&sortByDID=3&sortOrder=ascending&itemID=CMS1186805.
A second new CMS demonstration program will go beyond the traditional concept of gainsharing. Under the program, known as the Physician-Hospital Collaboration Demonstration (PHCD), hospitals would be allowed to pay physicians a portion of the savings they reap from specific quality improvement and efficiency initiatives. This project, in particular, could eventually have direct implications for hospital medicine.
The SHM Public Policy Committee is urging members to consider soliciting involvement with PHCD, and possibly partnering with other physician groups and affiliated hospitals to compete for inclusion. You can find more on the PHCD online at www.cms.hhs.gov/DemoProjectsEvalRpts/MD/itemdetail.asp?filterType=none&filterByDID=99&sortByDID=3&sortOrder=ascending&itemID=CMS1186653. If you decide to submit a proposal to CMS for the PHCD, please let Joe Miller at SHM (jmiller@hospitalmedicine.org) know.
The Future of Gainsharing
Will the CMS gainsharing pilot programs lead to widespread trials? “Who knows?” asks Dr. Greeno. “It will be a slow crawl toward some type of application, but it will likely be too limited when it does happen.”
In the meantime, Dr. Greeno is urging SHM and individual physicians to keep pushing for some real advances in gainsharing. “Our best chance is to work with the hospital community to connect the dots for our federal lawmakers,” he says. “We want to work to allow hospitals to reward doctors for quality performance.” TH
Jane Jerrard regularly writes “Public Policy.”
While pay-for-performance has become one of the hottest trends in healthcare, another program that would tie payment to performance is starting to get some notice. Gainsharing is on the horizon for hospitals and the physicians who work for them, but the advances made in this savings-sharing model are questionable.
Gainsharing Defined
What is gainsharing? It has to do with the sharing of gains—or of costs saved, to be more precise. Under a gainsharing model, a hospital will select specific best practices, including standard policies, procedures, and/or protocols that will improve quality of care and reduce financial costs. Any reduction in costs that results from physicians following these best practices is documented by the hospital over a specified period. After monitoring and noting that physicians met the predetermined benchmarks for quality of care, the hospital then pays a cash bonus to those who contributed to the cost reduction.
Gainsharing can take various forms, but generally the practice applies to services provided within a single clinical specialty such as oncology or cardiac surgery. “Gainsharing could affect anyone who cares for patients in a hospital if it became legal,” says Ron Greeno, MD, FCCP, chief medical officer, Cogent Healthcare, Irvine, Calif., “but hospitalists are the perfect group of doctors to take on projects like this.”
The most recent gainsharing programs have focused on the use of pre-approved medical devices, equipment, and supplies. For example, a hospital might recommend that physicians use less costly items with the same level of effectiveness, such as a knee-high sequential compression device rather than a thigh-high device.
How much money is involved in gainsharing? Of course, it depends on the program. “Gainsharing deals could include significant money depending on how they are structured,” explains Dr. Greeno, “if you did something that results in enough quality benefit.”
Example: A hospital asked a physician group to give an appropriate antibiotic to patients as soon as possible upon admission and was consequently able to show that they avoided a prolonged stay for five of those patients and that this saved the hospital $1 million in costs. “If the hospital gave 50% of that savings to 20 physicians who helped meet that goal, why would anyone want to regulate against that?” asks Dr. Greeno.
A Brief History of Gainsharing
There is a good reason you may not have heard much about gainsharing; the practice was banned in 1999 by the federal Office of Inspector General (OIG). The OIG was concerned that gainsharing could limit patient care and might lead to physicians “cherry picking” patients who are healthier, while sending seriously ill patients to a different hospital.
Only in September 2005 did the OIG carry out a half-hearted reversal, providing advisory opinions that allow pre-approved arrangements between individual hospitals and physician groups—as long as appropriate safeguards are adopted to protect against abuse.
“This was a very small change,” says Dr. Greeno. “Their approval is highly limited. They have basically agreed to very specific, very short trials of gainsharing, which they will approve one at a time.”
Dr. Greeno is frustrated by the baby step taken by the federal government. “The OIG equates gainsharing with denial of care,” he says. “Their limits are preventing a tremendous opportunity for hospitals and physicians to partner to provide quality care; they’re saying we can’t provide the right incentive scheme.”
The point that Dr. Greeno finds most frustrating is the vast difference of opinion on gainsharing versus another payment trend. “The irony is that all gainsharing is pay-for-performance,” says Dr. Greeno. “The difference is that instead of Medicare paying, it’s the individual hospital paying for performance. Even people who really understand healthcare haven’t connected the dots. They’re pushing for pay-for-performance, but telling hospitals they can’t do essentially the same thing. The hospital industry is developing a strategy to point that out to Capitol Hill, and in my opinion, SHM should develop a more formal approach to do the same.”
Current State of Gainsharing
There have been a few gainsharing programs that were approved by the OIG. “There are a couple of [pilot programs] that private hospitals have done,” says Dr. Greeno. “All the projects so far have targeted medical devices. One New Jersey hospital focused on the use of defibrillators. They spent a lot of money setting up the project, which only lasted one year. As I said, these [approved projects] are very limited.”
Gainsharing programs that focus on medical devices are simple because cost savings are easy to track; however, gainsharing could be built around quality indicators that are found in pay-for-performance programs. “Cutting costs is not the only way to improve quality,” says Dr. Greeno. “That’s not how you get the biggest bang for your buck. That comes when someone will invest in capabilities and processes that target the 30% of costs spent on each patient in the hospital that is waste.”
Pilot Programs Planned
Following the OIG reversal, Congress passed the Deficit Reduction Omnibus Reconciliation Act of 2005, which included funding for a gainsharing demonstration project. The Centers for Medicare and Medicaid Services (CMS) will establish six gainsharing pilot programs, including two in rural settings, by January 1, 2007. The bill states that these demonstration programs are intended to “test and evaluate methodologies and arrangements between hospitals and physicians designed to govern the utilization of inpatient hospital resources and physician work to improve quality and efficiency of care provided to Medicare beneficiaries.”
You can review details on the gainsharing demonstration on the CMS Web site at www.cms.hhs.gov/DemoProjectsEvalRpts/MD/itemdetail.asp?filterType=none&filterByDID=-99&sortByDID=3&sortOrder=ascending&itemID=CMS1186805.
A second new CMS demonstration program will go beyond the traditional concept of gainsharing. Under the program, known as the Physician-Hospital Collaboration Demonstration (PHCD), hospitals would be allowed to pay physicians a portion of the savings they reap from specific quality improvement and efficiency initiatives. This project, in particular, could eventually have direct implications for hospital medicine.
The SHM Public Policy Committee is urging members to consider soliciting involvement with PHCD, and possibly partnering with other physician groups and affiliated hospitals to compete for inclusion. You can find more on the PHCD online at www.cms.hhs.gov/DemoProjectsEvalRpts/MD/itemdetail.asp?filterType=none&filterByDID=99&sortByDID=3&sortOrder=ascending&itemID=CMS1186653. If you decide to submit a proposal to CMS for the PHCD, please let Joe Miller at SHM (jmiller@hospitalmedicine.org) know.
The Future of Gainsharing
Will the CMS gainsharing pilot programs lead to widespread trials? “Who knows?” asks Dr. Greeno. “It will be a slow crawl toward some type of application, but it will likely be too limited when it does happen.”
In the meantime, Dr. Greeno is urging SHM and individual physicians to keep pushing for some real advances in gainsharing. “Our best chance is to work with the hospital community to connect the dots for our federal lawmakers,” he says. “We want to work to allow hospitals to reward doctors for quality performance.” TH
Jane Jerrard regularly writes “Public Policy.”
While pay-for-performance has become one of the hottest trends in healthcare, another program that would tie payment to performance is starting to get some notice. Gainsharing is on the horizon for hospitals and the physicians who work for them, but the advances made in this savings-sharing model are questionable.
Gainsharing Defined
What is gainsharing? It has to do with the sharing of gains—or of costs saved, to be more precise. Under a gainsharing model, a hospital will select specific best practices, including standard policies, procedures, and/or protocols that will improve quality of care and reduce financial costs. Any reduction in costs that results from physicians following these best practices is documented by the hospital over a specified period. After monitoring and noting that physicians met the predetermined benchmarks for quality of care, the hospital then pays a cash bonus to those who contributed to the cost reduction.
Gainsharing can take various forms, but generally the practice applies to services provided within a single clinical specialty such as oncology or cardiac surgery. “Gainsharing could affect anyone who cares for patients in a hospital if it became legal,” says Ron Greeno, MD, FCCP, chief medical officer, Cogent Healthcare, Irvine, Calif., “but hospitalists are the perfect group of doctors to take on projects like this.”
The most recent gainsharing programs have focused on the use of pre-approved medical devices, equipment, and supplies. For example, a hospital might recommend that physicians use less costly items with the same level of effectiveness, such as a knee-high sequential compression device rather than a thigh-high device.
How much money is involved in gainsharing? Of course, it depends on the program. “Gainsharing deals could include significant money depending on how they are structured,” explains Dr. Greeno, “if you did something that results in enough quality benefit.”
Example: A hospital asked a physician group to give an appropriate antibiotic to patients as soon as possible upon admission and was consequently able to show that they avoided a prolonged stay for five of those patients and that this saved the hospital $1 million in costs. “If the hospital gave 50% of that savings to 20 physicians who helped meet that goal, why would anyone want to regulate against that?” asks Dr. Greeno.
A Brief History of Gainsharing
There is a good reason you may not have heard much about gainsharing; the practice was banned in 1999 by the federal Office of Inspector General (OIG). The OIG was concerned that gainsharing could limit patient care and might lead to physicians “cherry picking” patients who are healthier, while sending seriously ill patients to a different hospital.
Only in September 2005 did the OIG carry out a half-hearted reversal, providing advisory opinions that allow pre-approved arrangements between individual hospitals and physician groups—as long as appropriate safeguards are adopted to protect against abuse.
“This was a very small change,” says Dr. Greeno. “Their approval is highly limited. They have basically agreed to very specific, very short trials of gainsharing, which they will approve one at a time.”
Dr. Greeno is frustrated by the baby step taken by the federal government. “The OIG equates gainsharing with denial of care,” he says. “Their limits are preventing a tremendous opportunity for hospitals and physicians to partner to provide quality care; they’re saying we can’t provide the right incentive scheme.”
The point that Dr. Greeno finds most frustrating is the vast difference of opinion on gainsharing versus another payment trend. “The irony is that all gainsharing is pay-for-performance,” says Dr. Greeno. “The difference is that instead of Medicare paying, it’s the individual hospital paying for performance. Even people who really understand healthcare haven’t connected the dots. They’re pushing for pay-for-performance, but telling hospitals they can’t do essentially the same thing. The hospital industry is developing a strategy to point that out to Capitol Hill, and in my opinion, SHM should develop a more formal approach to do the same.”
Current State of Gainsharing
There have been a few gainsharing programs that were approved by the OIG. “There are a couple of [pilot programs] that private hospitals have done,” says Dr. Greeno. “All the projects so far have targeted medical devices. One New Jersey hospital focused on the use of defibrillators. They spent a lot of money setting up the project, which only lasted one year. As I said, these [approved projects] are very limited.”
Gainsharing programs that focus on medical devices are simple because cost savings are easy to track; however, gainsharing could be built around quality indicators that are found in pay-for-performance programs. “Cutting costs is not the only way to improve quality,” says Dr. Greeno. “That’s not how you get the biggest bang for your buck. That comes when someone will invest in capabilities and processes that target the 30% of costs spent on each patient in the hospital that is waste.”
Pilot Programs Planned
Following the OIG reversal, Congress passed the Deficit Reduction Omnibus Reconciliation Act of 2005, which included funding for a gainsharing demonstration project. The Centers for Medicare and Medicaid Services (CMS) will establish six gainsharing pilot programs, including two in rural settings, by January 1, 2007. The bill states that these demonstration programs are intended to “test and evaluate methodologies and arrangements between hospitals and physicians designed to govern the utilization of inpatient hospital resources and physician work to improve quality and efficiency of care provided to Medicare beneficiaries.”
You can review details on the gainsharing demonstration on the CMS Web site at www.cms.hhs.gov/DemoProjectsEvalRpts/MD/itemdetail.asp?filterType=none&filterByDID=-99&sortByDID=3&sortOrder=ascending&itemID=CMS1186805.
A second new CMS demonstration program will go beyond the traditional concept of gainsharing. Under the program, known as the Physician-Hospital Collaboration Demonstration (PHCD), hospitals would be allowed to pay physicians a portion of the savings they reap from specific quality improvement and efficiency initiatives. This project, in particular, could eventually have direct implications for hospital medicine.
The SHM Public Policy Committee is urging members to consider soliciting involvement with PHCD, and possibly partnering with other physician groups and affiliated hospitals to compete for inclusion. You can find more on the PHCD online at www.cms.hhs.gov/DemoProjectsEvalRpts/MD/itemdetail.asp?filterType=none&filterByDID=99&sortByDID=3&sortOrder=ascending&itemID=CMS1186653. If you decide to submit a proposal to CMS for the PHCD, please let Joe Miller at SHM (jmiller@hospitalmedicine.org) know.
The Future of Gainsharing
Will the CMS gainsharing pilot programs lead to widespread trials? “Who knows?” asks Dr. Greeno. “It will be a slow crawl toward some type of application, but it will likely be too limited when it does happen.”
In the meantime, Dr. Greeno is urging SHM and individual physicians to keep pushing for some real advances in gainsharing. “Our best chance is to work with the hospital community to connect the dots for our federal lawmakers,” he says. “We want to work to allow hospitals to reward doctors for quality performance.” TH
Jane Jerrard regularly writes “Public Policy.”
Master Meetings
Meetings are a fact of life. They play an integral role in how our departments, committees, and hospitals make decisions, implement new projects and processes, convey information, and, unfortunately, take up our precious time.
Perhaps you’ve been thrust into the role of leading meetings—as the head of a quality initiative task force, or as facilitator of a brainstorming session on a quality of care issue—or maybe you’re just beginning to face that possibility. How can you hone your skills to ensure that your meetings are on track, fulfill their goals, and waste as little time as possible?
—Roger Schenke
Watch and Learn
Russell L. Holman, MD, senior vice president and national medical director, Cogent Healthcare, and president-elect, SHM, put a lot of effort into mastering his meeting leadership skills, beginning early in his career. “I was working in an organization that was meeting-rich,” recalls Dr. Holman. “It was important to me to learn that way of getting things done.”
He began with the simple act of watching how others led meetings, noting what some did right and others did wrong. “A lot of my work has been through observation, and through seeking out mentoring,” he says. It helps to have spent time sitting in many meetings before you become a leader. “You can see how things are done. When you observe someone who does well at leading a meeting, ask to sit down with them and ask how they set out to accomplish the goal of the meeting.”
Learn as You Go
As a hospitalist, you are likely to assume the role of meeting leader. You can then concentrate on refining your skills with each meeting. “Seek feedback of the senior people participating, as well as general participants,” suggests Dr. Holman. “Do a bit of analysis if there were conflicts in the meeting, or if you feel the group is not making progress.”
Tip: If you’re a clinical hospitalist without hierarchical authority and have been asked to lead a project or task force, use Dr. Holman’s “transfer of authority” method. Ask someone with recognizable importance, such as the hospital CEO or a department chair, to stop in your group’s first meeting for a few minutes. While they are there, they should offer their resources for any necessary support, and voice their confidence in you as the leader and in the group in general. This simple visit will transfer their authority to you as the group leader.
Structure Is Key
Roger Schenke, executive vice president of the American College of Physician Executives (ACPE), believes that when the right structure is imposed any meeting is easy to run—without personality conflicts or wasted time. Schenke, who teaches an introductory ACPE course on management that includes a section on meetings, explains, “A structure approach [to meetings] takes proven techniques and superimposes them on any group. Once you start using structure, you don’t have to manipulate the meeting; people will simply follow the structure. They’ll feel that they’re part of a process.”
Schenke outlines an ideal meeting scenario, which can take place as a single, long meeting within a pre-set room, or be broken into separate, sequential meetings:
- Briefing. This should last no more than 30 minutes. A single speaker or a select panel provides information to participants and then allows questions. “Everyone knows the rules for this type of meeting,” adds Schenke.
- Problem-solving or problem-identification meeting. “The room should be set up with small tables and a flip chart for each. Small groups are assigned a specific task,” says Schenke, such as solving the hospital’s nursing shortage. A committee or task force should be broken into small groups so “you can’t go above seven people when you want people to interact,” says Schenke. “Above that, and little subgroups and factions form.”
- Parliamentary meetings should take place at a conference table. “Everyone eligible to mandate policy hears recommendations from other groups, such as the problem-solving groups,” says Schenke.
Obviously, each of these meetings has a unique structure with a unique room setting. “Structure determines or controls behavior,” says Schenke. “When people are put in these situations, they understand the rules. The key is not preparation; all it takes is letting the group know the purpose of the meeting.”
Practice, Practice, Practice
There are many theories and styles regarding running successful meetings, and you’ll find a wealth of information on how to become a better meeting leader. Just as meetings are a fact of life, it’s also true that you can improve your facilitation skills with each new meeting you lead. TH
Jane Jerrard writes “Career Management” monthly for The Hospitalist.
Meetings are a fact of life. They play an integral role in how our departments, committees, and hospitals make decisions, implement new projects and processes, convey information, and, unfortunately, take up our precious time.
Perhaps you’ve been thrust into the role of leading meetings—as the head of a quality initiative task force, or as facilitator of a brainstorming session on a quality of care issue—or maybe you’re just beginning to face that possibility. How can you hone your skills to ensure that your meetings are on track, fulfill their goals, and waste as little time as possible?
—Roger Schenke
Watch and Learn
Russell L. Holman, MD, senior vice president and national medical director, Cogent Healthcare, and president-elect, SHM, put a lot of effort into mastering his meeting leadership skills, beginning early in his career. “I was working in an organization that was meeting-rich,” recalls Dr. Holman. “It was important to me to learn that way of getting things done.”
He began with the simple act of watching how others led meetings, noting what some did right and others did wrong. “A lot of my work has been through observation, and through seeking out mentoring,” he says. It helps to have spent time sitting in many meetings before you become a leader. “You can see how things are done. When you observe someone who does well at leading a meeting, ask to sit down with them and ask how they set out to accomplish the goal of the meeting.”
Learn as You Go
As a hospitalist, you are likely to assume the role of meeting leader. You can then concentrate on refining your skills with each meeting. “Seek feedback of the senior people participating, as well as general participants,” suggests Dr. Holman. “Do a bit of analysis if there were conflicts in the meeting, or if you feel the group is not making progress.”
Tip: If you’re a clinical hospitalist without hierarchical authority and have been asked to lead a project or task force, use Dr. Holman’s “transfer of authority” method. Ask someone with recognizable importance, such as the hospital CEO or a department chair, to stop in your group’s first meeting for a few minutes. While they are there, they should offer their resources for any necessary support, and voice their confidence in you as the leader and in the group in general. This simple visit will transfer their authority to you as the group leader.
Structure Is Key
Roger Schenke, executive vice president of the American College of Physician Executives (ACPE), believes that when the right structure is imposed any meeting is easy to run—without personality conflicts or wasted time. Schenke, who teaches an introductory ACPE course on management that includes a section on meetings, explains, “A structure approach [to meetings] takes proven techniques and superimposes them on any group. Once you start using structure, you don’t have to manipulate the meeting; people will simply follow the structure. They’ll feel that they’re part of a process.”
Schenke outlines an ideal meeting scenario, which can take place as a single, long meeting within a pre-set room, or be broken into separate, sequential meetings:
- Briefing. This should last no more than 30 minutes. A single speaker or a select panel provides information to participants and then allows questions. “Everyone knows the rules for this type of meeting,” adds Schenke.
- Problem-solving or problem-identification meeting. “The room should be set up with small tables and a flip chart for each. Small groups are assigned a specific task,” says Schenke, such as solving the hospital’s nursing shortage. A committee or task force should be broken into small groups so “you can’t go above seven people when you want people to interact,” says Schenke. “Above that, and little subgroups and factions form.”
- Parliamentary meetings should take place at a conference table. “Everyone eligible to mandate policy hears recommendations from other groups, such as the problem-solving groups,” says Schenke.
Obviously, each of these meetings has a unique structure with a unique room setting. “Structure determines or controls behavior,” says Schenke. “When people are put in these situations, they understand the rules. The key is not preparation; all it takes is letting the group know the purpose of the meeting.”
Practice, Practice, Practice
There are many theories and styles regarding running successful meetings, and you’ll find a wealth of information on how to become a better meeting leader. Just as meetings are a fact of life, it’s also true that you can improve your facilitation skills with each new meeting you lead. TH
Jane Jerrard writes “Career Management” monthly for The Hospitalist.
Meetings are a fact of life. They play an integral role in how our departments, committees, and hospitals make decisions, implement new projects and processes, convey information, and, unfortunately, take up our precious time.
Perhaps you’ve been thrust into the role of leading meetings—as the head of a quality initiative task force, or as facilitator of a brainstorming session on a quality of care issue—or maybe you’re just beginning to face that possibility. How can you hone your skills to ensure that your meetings are on track, fulfill their goals, and waste as little time as possible?
—Roger Schenke
Watch and Learn
Russell L. Holman, MD, senior vice president and national medical director, Cogent Healthcare, and president-elect, SHM, put a lot of effort into mastering his meeting leadership skills, beginning early in his career. “I was working in an organization that was meeting-rich,” recalls Dr. Holman. “It was important to me to learn that way of getting things done.”
He began with the simple act of watching how others led meetings, noting what some did right and others did wrong. “A lot of my work has been through observation, and through seeking out mentoring,” he says. It helps to have spent time sitting in many meetings before you become a leader. “You can see how things are done. When you observe someone who does well at leading a meeting, ask to sit down with them and ask how they set out to accomplish the goal of the meeting.”
Learn as You Go
As a hospitalist, you are likely to assume the role of meeting leader. You can then concentrate on refining your skills with each meeting. “Seek feedback of the senior people participating, as well as general participants,” suggests Dr. Holman. “Do a bit of analysis if there were conflicts in the meeting, or if you feel the group is not making progress.”
Tip: If you’re a clinical hospitalist without hierarchical authority and have been asked to lead a project or task force, use Dr. Holman’s “transfer of authority” method. Ask someone with recognizable importance, such as the hospital CEO or a department chair, to stop in your group’s first meeting for a few minutes. While they are there, they should offer their resources for any necessary support, and voice their confidence in you as the leader and in the group in general. This simple visit will transfer their authority to you as the group leader.
Structure Is Key
Roger Schenke, executive vice president of the American College of Physician Executives (ACPE), believes that when the right structure is imposed any meeting is easy to run—without personality conflicts or wasted time. Schenke, who teaches an introductory ACPE course on management that includes a section on meetings, explains, “A structure approach [to meetings] takes proven techniques and superimposes them on any group. Once you start using structure, you don’t have to manipulate the meeting; people will simply follow the structure. They’ll feel that they’re part of a process.”
Schenke outlines an ideal meeting scenario, which can take place as a single, long meeting within a pre-set room, or be broken into separate, sequential meetings:
- Briefing. This should last no more than 30 minutes. A single speaker or a select panel provides information to participants and then allows questions. “Everyone knows the rules for this type of meeting,” adds Schenke.
- Problem-solving or problem-identification meeting. “The room should be set up with small tables and a flip chart for each. Small groups are assigned a specific task,” says Schenke, such as solving the hospital’s nursing shortage. A committee or task force should be broken into small groups so “you can’t go above seven people when you want people to interact,” says Schenke. “Above that, and little subgroups and factions form.”
- Parliamentary meetings should take place at a conference table. “Everyone eligible to mandate policy hears recommendations from other groups, such as the problem-solving groups,” says Schenke.
Obviously, each of these meetings has a unique structure with a unique room setting. “Structure determines or controls behavior,” says Schenke. “When people are put in these situations, they understand the rules. The key is not preparation; all it takes is letting the group know the purpose of the meeting.”
Practice, Practice, Practice
There are many theories and styles regarding running successful meetings, and you’ll find a wealth of information on how to become a better meeting leader. Just as meetings are a fact of life, it’s also true that you can improve your facilitation skills with each new meeting you lead. TH
Jane Jerrard writes “Career Management” monthly for The Hospitalist.