User login
That’s What They Said
I stare; a brimming audience stares back. Two eyeballs battling thousands. Slightly uncomfortable, I shift my weight, trying to hide behind the glass podium. Two microphones snake out of the podium slithering together inches from my mouth. The attendees squirm, sidle to the edge of their seats, restless to depart. HM11 is trying to close; only I stand in its way.
A Herculean task lies before me—summarize the annual meeting in a 10-minute wrap-up session titled “What We’ve Learned.” How do you summarize four days, eight pre-courses, nine breakout tracks, and more than 100 presentations in a few minutes? A bead of forehead sweat forms; I clear my throat. Memories of the past few days slide-show across my mind. It occurs to me that the essence of the meeting is not contained in the data, the information, or the PowerPoint slides that were presented. Rather, the story of HM11 is best told through its quotes.
Patient Caps: Your Grandmother and Professionalism
“I worry about patient caps because the next patient could be your grandmother.”
—Joe Li, MD, SFHM, new president of SHM
“Patient caps are the greatest threat to the professionalism of the field.”
—Rob Bessler, MD, CEO, Sound Inpatient Physicians
These two quotes from the opening plenary focused on the 2011 HM compensation and productivity survey particularly stuck out. The most noteworthy exchange came when Drs. Li and Bressler commented on the appropriate number of daily encounters for a hospitalist. The quotes highlight two important points about patient volume, especially in the wake of the training regulations that limit the number of resident physician encounters, which can engender a “cap mentality.” One is that it matters; there is a safe amount of encounters that shouldn’t routinely be breached. Two is that in the heat of the moment, Patient 19 is as important as Patient 11 and should be treated as such. Contingency plans are essential, but our field is built on the moorings of professionalism—the focus needs to be on humans, not numbers.
Hospitalist Compensation: Increasing but Not as Juicy
“It’s not going to get less anytime soon.”
—Dr. Bressler
In commenting on the data showing that the average community hospitalist makes about $220,000 annually—a 3% increase over last year—while producing around 4,000 work RVUs—flat over last year—and that their academic counterparts made $173,000 on about 3,400 wRVUs, Dr. Bressler opined that the laws of supply and demand would dictate that salaries would continue to rise for the near term. Although I agree with Dr. Bressler, my guess is that future salary increases will be driven more by quality than quantity (more to follow below).
“Juice-to-squeeze ratio”
—John Nelson, MD, MHM, SHM cofounder
Dr. Nelson highlighted interesting data showing that the average pay per wRVU was approximately $54. However, he noted that the compensation per wRVU tends to peak at a certain level, after which compensation per wRVU falls. In other words, after, say, 4,000 wRVUs, the amount of compensation per wRVU diminishes such that seeing more patients benefits an individual hospitalist less. That is, lots of squeeze, little juice at the high end.
Reform: Variety, Change, and Waste
“Variety is about choice; change is not.”
—Cecil Wilson, MD, AMA president
“You won’t have many more conferences where you start by talking about work RVUs.”
—Bob Kocher, MD, former special assistant to President Obama
The highlight of the conference for me was Dr. Kocher’s behind-the-scenes look at what was a very publicly muddy event—the passage of ACA. Coming from a D.C. insider, this under-the-covers peek at the machinations that went into passing the healthcare reform bill was fascinating.
The key message, summarized in this comment referring to the opening plenary about hospitalist compensation and productivity, was that the future is quality and the future is now. In the very near future, we will be measured and paid based on our ability to effect quality outcomes, not patient encounters. The message was simple: It’s about quality, not quantity.
“It costs $7.50 for a healthcare transaction, versus 2 cents for a VISA transaction.”
—Dr. Kocher
A statistic I had not heard before, this quote sums up one of the major problems with American healthcare: waste. The $7.50 transaction he was referring to was the amount of money it takes to file a healthcare claim. We certainly feel it in the challenges of documentation, billing, and denials, but the system feels it in terms of high cost of capturing what in many ways should be as simple as swiping your credit card at Starbucks.
Duty-Hour Restrictions: Harbinger of The Future?
“Don’t begrudge the ACGME—begrudge us.”
—Jeff Wiese, MD, SFHM, SHM past president
In a much-anticipated session on the impact of the new ACGME residency work-hour rules commencing in July—notably limiting intern (16-hour) and resident (28-hour) shift duration—Dr. Wiese aptly pointed out that a lot of the angst toward residency work environment regulation could have been avoided if physician leadership had better reacted to the issues of sleep deprivation and resident fatigue following Libby Zion’s death in 1984. Had we put our energy into improving work conditions rather than debate the impact of sleep deprivation on the outcome in this one case, we might be in a different place today.
I couldn’t help but wonder if the message here could also be applied to society’s push for higher quality, lower cost, and safer care. Either we regulate ourselves or someone else will. In other words, we need to embrace quality and safety, or it will be thrust upon us from external sources in ways we might not like.
A Mariner Calls
“I love you, Papi. Come home and take some baseball cuts.”
—Greyson Glasheen, future Major League Baseball shortstop
I wrote in a column leading up to the annual meeting (see “Annual Meeting Mariner,” April 2011, p. 45) that I was looking forward to the meeting because it was a professional mariner of sorts, a way for me to refresh, reset, and reinvigorate. Indeed, reflecting from the podium, it had been a fantastic meeting that served its purpose well. I had learned a ton, caught up with colleagues I hadn’t seen since the last meeting, saw old medical school friends, and met future old friends. I’d led a committee, given a talk, presented a poster, met up with a mentor, and had a reunion with past attendees of the Academic Hospitalist Academy.
Yet I was ready to get back to normalcy. On the last night of the meeting, I was therefore drawn by a different, more personal mariner—this time, a 14-second voicemail message from a 3-year-old boy waiting impatiently for Dad to come home, to make him his center, to simply play a little tee ball in the backyard. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado at Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
I stare; a brimming audience stares back. Two eyeballs battling thousands. Slightly uncomfortable, I shift my weight, trying to hide behind the glass podium. Two microphones snake out of the podium slithering together inches from my mouth. The attendees squirm, sidle to the edge of their seats, restless to depart. HM11 is trying to close; only I stand in its way.
A Herculean task lies before me—summarize the annual meeting in a 10-minute wrap-up session titled “What We’ve Learned.” How do you summarize four days, eight pre-courses, nine breakout tracks, and more than 100 presentations in a few minutes? A bead of forehead sweat forms; I clear my throat. Memories of the past few days slide-show across my mind. It occurs to me that the essence of the meeting is not contained in the data, the information, or the PowerPoint slides that were presented. Rather, the story of HM11 is best told through its quotes.
Patient Caps: Your Grandmother and Professionalism
“I worry about patient caps because the next patient could be your grandmother.”
—Joe Li, MD, SFHM, new president of SHM
“Patient caps are the greatest threat to the professionalism of the field.”
—Rob Bessler, MD, CEO, Sound Inpatient Physicians
These two quotes from the opening plenary focused on the 2011 HM compensation and productivity survey particularly stuck out. The most noteworthy exchange came when Drs. Li and Bressler commented on the appropriate number of daily encounters for a hospitalist. The quotes highlight two important points about patient volume, especially in the wake of the training regulations that limit the number of resident physician encounters, which can engender a “cap mentality.” One is that it matters; there is a safe amount of encounters that shouldn’t routinely be breached. Two is that in the heat of the moment, Patient 19 is as important as Patient 11 and should be treated as such. Contingency plans are essential, but our field is built on the moorings of professionalism—the focus needs to be on humans, not numbers.
Hospitalist Compensation: Increasing but Not as Juicy
“It’s not going to get less anytime soon.”
—Dr. Bressler
In commenting on the data showing that the average community hospitalist makes about $220,000 annually—a 3% increase over last year—while producing around 4,000 work RVUs—flat over last year—and that their academic counterparts made $173,000 on about 3,400 wRVUs, Dr. Bressler opined that the laws of supply and demand would dictate that salaries would continue to rise for the near term. Although I agree with Dr. Bressler, my guess is that future salary increases will be driven more by quality than quantity (more to follow below).
“Juice-to-squeeze ratio”
—John Nelson, MD, MHM, SHM cofounder
Dr. Nelson highlighted interesting data showing that the average pay per wRVU was approximately $54. However, he noted that the compensation per wRVU tends to peak at a certain level, after which compensation per wRVU falls. In other words, after, say, 4,000 wRVUs, the amount of compensation per wRVU diminishes such that seeing more patients benefits an individual hospitalist less. That is, lots of squeeze, little juice at the high end.
Reform: Variety, Change, and Waste
“Variety is about choice; change is not.”
—Cecil Wilson, MD, AMA president
“You won’t have many more conferences where you start by talking about work RVUs.”
—Bob Kocher, MD, former special assistant to President Obama
The highlight of the conference for me was Dr. Kocher’s behind-the-scenes look at what was a very publicly muddy event—the passage of ACA. Coming from a D.C. insider, this under-the-covers peek at the machinations that went into passing the healthcare reform bill was fascinating.
The key message, summarized in this comment referring to the opening plenary about hospitalist compensation and productivity, was that the future is quality and the future is now. In the very near future, we will be measured and paid based on our ability to effect quality outcomes, not patient encounters. The message was simple: It’s about quality, not quantity.
“It costs $7.50 for a healthcare transaction, versus 2 cents for a VISA transaction.”
—Dr. Kocher
A statistic I had not heard before, this quote sums up one of the major problems with American healthcare: waste. The $7.50 transaction he was referring to was the amount of money it takes to file a healthcare claim. We certainly feel it in the challenges of documentation, billing, and denials, but the system feels it in terms of high cost of capturing what in many ways should be as simple as swiping your credit card at Starbucks.
Duty-Hour Restrictions: Harbinger of The Future?
“Don’t begrudge the ACGME—begrudge us.”
—Jeff Wiese, MD, SFHM, SHM past president
In a much-anticipated session on the impact of the new ACGME residency work-hour rules commencing in July—notably limiting intern (16-hour) and resident (28-hour) shift duration—Dr. Wiese aptly pointed out that a lot of the angst toward residency work environment regulation could have been avoided if physician leadership had better reacted to the issues of sleep deprivation and resident fatigue following Libby Zion’s death in 1984. Had we put our energy into improving work conditions rather than debate the impact of sleep deprivation on the outcome in this one case, we might be in a different place today.
I couldn’t help but wonder if the message here could also be applied to society’s push for higher quality, lower cost, and safer care. Either we regulate ourselves or someone else will. In other words, we need to embrace quality and safety, or it will be thrust upon us from external sources in ways we might not like.
A Mariner Calls
“I love you, Papi. Come home and take some baseball cuts.”
—Greyson Glasheen, future Major League Baseball shortstop
I wrote in a column leading up to the annual meeting (see “Annual Meeting Mariner,” April 2011, p. 45) that I was looking forward to the meeting because it was a professional mariner of sorts, a way for me to refresh, reset, and reinvigorate. Indeed, reflecting from the podium, it had been a fantastic meeting that served its purpose well. I had learned a ton, caught up with colleagues I hadn’t seen since the last meeting, saw old medical school friends, and met future old friends. I’d led a committee, given a talk, presented a poster, met up with a mentor, and had a reunion with past attendees of the Academic Hospitalist Academy.
Yet I was ready to get back to normalcy. On the last night of the meeting, I was therefore drawn by a different, more personal mariner—this time, a 14-second voicemail message from a 3-year-old boy waiting impatiently for Dad to come home, to make him his center, to simply play a little tee ball in the backyard. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado at Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
I stare; a brimming audience stares back. Two eyeballs battling thousands. Slightly uncomfortable, I shift my weight, trying to hide behind the glass podium. Two microphones snake out of the podium slithering together inches from my mouth. The attendees squirm, sidle to the edge of their seats, restless to depart. HM11 is trying to close; only I stand in its way.
A Herculean task lies before me—summarize the annual meeting in a 10-minute wrap-up session titled “What We’ve Learned.” How do you summarize four days, eight pre-courses, nine breakout tracks, and more than 100 presentations in a few minutes? A bead of forehead sweat forms; I clear my throat. Memories of the past few days slide-show across my mind. It occurs to me that the essence of the meeting is not contained in the data, the information, or the PowerPoint slides that were presented. Rather, the story of HM11 is best told through its quotes.
Patient Caps: Your Grandmother and Professionalism
“I worry about patient caps because the next patient could be your grandmother.”
—Joe Li, MD, SFHM, new president of SHM
“Patient caps are the greatest threat to the professionalism of the field.”
—Rob Bessler, MD, CEO, Sound Inpatient Physicians
These two quotes from the opening plenary focused on the 2011 HM compensation and productivity survey particularly stuck out. The most noteworthy exchange came when Drs. Li and Bressler commented on the appropriate number of daily encounters for a hospitalist. The quotes highlight two important points about patient volume, especially in the wake of the training regulations that limit the number of resident physician encounters, which can engender a “cap mentality.” One is that it matters; there is a safe amount of encounters that shouldn’t routinely be breached. Two is that in the heat of the moment, Patient 19 is as important as Patient 11 and should be treated as such. Contingency plans are essential, but our field is built on the moorings of professionalism—the focus needs to be on humans, not numbers.
Hospitalist Compensation: Increasing but Not as Juicy
“It’s not going to get less anytime soon.”
—Dr. Bressler
In commenting on the data showing that the average community hospitalist makes about $220,000 annually—a 3% increase over last year—while producing around 4,000 work RVUs—flat over last year—and that their academic counterparts made $173,000 on about 3,400 wRVUs, Dr. Bressler opined that the laws of supply and demand would dictate that salaries would continue to rise for the near term. Although I agree with Dr. Bressler, my guess is that future salary increases will be driven more by quality than quantity (more to follow below).
“Juice-to-squeeze ratio”
—John Nelson, MD, MHM, SHM cofounder
Dr. Nelson highlighted interesting data showing that the average pay per wRVU was approximately $54. However, he noted that the compensation per wRVU tends to peak at a certain level, after which compensation per wRVU falls. In other words, after, say, 4,000 wRVUs, the amount of compensation per wRVU diminishes such that seeing more patients benefits an individual hospitalist less. That is, lots of squeeze, little juice at the high end.
Reform: Variety, Change, and Waste
“Variety is about choice; change is not.”
—Cecil Wilson, MD, AMA president
“You won’t have many more conferences where you start by talking about work RVUs.”
—Bob Kocher, MD, former special assistant to President Obama
The highlight of the conference for me was Dr. Kocher’s behind-the-scenes look at what was a very publicly muddy event—the passage of ACA. Coming from a D.C. insider, this under-the-covers peek at the machinations that went into passing the healthcare reform bill was fascinating.
The key message, summarized in this comment referring to the opening plenary about hospitalist compensation and productivity, was that the future is quality and the future is now. In the very near future, we will be measured and paid based on our ability to effect quality outcomes, not patient encounters. The message was simple: It’s about quality, not quantity.
“It costs $7.50 for a healthcare transaction, versus 2 cents for a VISA transaction.”
—Dr. Kocher
A statistic I had not heard before, this quote sums up one of the major problems with American healthcare: waste. The $7.50 transaction he was referring to was the amount of money it takes to file a healthcare claim. We certainly feel it in the challenges of documentation, billing, and denials, but the system feels it in terms of high cost of capturing what in many ways should be as simple as swiping your credit card at Starbucks.
Duty-Hour Restrictions: Harbinger of The Future?
“Don’t begrudge the ACGME—begrudge us.”
—Jeff Wiese, MD, SFHM, SHM past president
In a much-anticipated session on the impact of the new ACGME residency work-hour rules commencing in July—notably limiting intern (16-hour) and resident (28-hour) shift duration—Dr. Wiese aptly pointed out that a lot of the angst toward residency work environment regulation could have been avoided if physician leadership had better reacted to the issues of sleep deprivation and resident fatigue following Libby Zion’s death in 1984. Had we put our energy into improving work conditions rather than debate the impact of sleep deprivation on the outcome in this one case, we might be in a different place today.
I couldn’t help but wonder if the message here could also be applied to society’s push for higher quality, lower cost, and safer care. Either we regulate ourselves or someone else will. In other words, we need to embrace quality and safety, or it will be thrust upon us from external sources in ways we might not like.
A Mariner Calls
“I love you, Papi. Come home and take some baseball cuts.”
—Greyson Glasheen, future Major League Baseball shortstop
I wrote in a column leading up to the annual meeting (see “Annual Meeting Mariner,” April 2011, p. 45) that I was looking forward to the meeting because it was a professional mariner of sorts, a way for me to refresh, reset, and reinvigorate. Indeed, reflecting from the podium, it had been a fantastic meeting that served its purpose well. I had learned a ton, caught up with colleagues I hadn’t seen since the last meeting, saw old medical school friends, and met future old friends. I’d led a committee, given a talk, presented a poster, met up with a mentor, and had a reunion with past attendees of the Academic Hospitalist Academy.
Yet I was ready to get back to normalcy. On the last night of the meeting, I was therefore drawn by a different, more personal mariner—this time, a 14-second voicemail message from a 3-year-old boy waiting impatiently for Dad to come home, to make him his center, to simply play a little tee ball in the backyard. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado at Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
Annual Meeting Mariner
It’s been one of those days. It all started at 4:30 this morning, when my 3-year-old son crawled into our bed, naked except for the diarrhea dripping down his leg. Turns out, this was his way—quite effective, I might add—of telling my wife and me that he had had an “accident.” After an hour of carrying soiled sheets to the washer, child-bathing, and Weimaraner coat-scrubbing, we relaxed to the sound of our 1-year-old daughter’s blood-curdling screams.
Upon examination, we found that the night had mysteriously transformed our precious little button-nosed bundle of joy into a tangle-haired, snot-nosed bundle of melancholy. Where her face used to be, there now hung something approximating the mask from that Scream movie. Additionally, her throat was raw, olive-sized lymph nodes populated her neck, and her nose had taken to perpetual booger-manufacturing. A rapid strep swab would later reveal the culprit, but at the moment, our differential tilted toward demonic possession.
That Dripping Feeling
Moments later, my wife and I picked 6:15 a.m. as the time to discover that we both had 7 a.m. meetings and no time to drop the kids off at daycare, especially when factoring in the 10-minute “discussion” we had about who was going to drop the kids off at daycare. All of this preceded my 7:10 a.m. arrival time for the 7 o’clock meeting with a hospital executive team to discuss our HM group funding for the next year—an encounter that left me feeling as my son must have just prior to crawling into bed with us that morning.
Now 8 a.m., I had to meet with a surgeon eager to unveil his “great idea” for our hospitalists to admit all of his patients. “It solves our problem of no interns, and allows you to play a meaningful role in the hospital!” he exclaimed.
“The meaningful role of intern?” I replied. Again, I had that dripping feeling.
It was 8:30 a.m. and I was ready to round on my patients. The first patient, a lovely woman, was stricken with un-insure-ia and a deep-seated belief that the inequitable health system that rendered her unable to get her surgery was clearly the result of some moral failing on my part. Next up was a spectacularly intoxicated male who welcomed my caring touch by belching a bit of breakfast burrito onto my cheek. Then it was a floridly bipolar patient whose apparent life mission was to drop her pants to show me her new mesh thong.
Burnout, Respect, Satisfaction
And so it continued until 1 p.m., when I had a meeting with a resident mentee of mine. It turns out that he wanted to tell me that despite his desire to be a hospitalist since his fourth year of medical school, he instead was going to apply to a rheumatology fellowship. After talking to several practicing hospitalists, he’d decided it just wasn’t for him—discussions he summarized as too much burnout, too little respect, and not enough satisfaction. Again, that dripping feeling.
Stuffing my face with a vending-machine carb-load that doubled as both breakfast and lunch, I sat down for a few minutes of e-mail. First up, a journal rejection of a research paper we’d recently submitted. Oh, the fulfillment of academics. Next were two e-mails that enzymatically trebled my “to do” list for the day. Sandwiched between those e-mails and one from a friend reminding me not to be late for a dinner that night that I was clearly going to be late for was an e-mail from a nice-appearing Nigerian man wanting to give me millions of dollars; at last, my day was turning around.
Alas, this was not the case. Checking my voicemail, I found out that my uncle was in the hospital, my dog’s lab tests were abnormal, my mom was angry about something, and I had missed a dentist appointment that morning. Finally, our group assistant came with a message that our prized hospitalist recruit had accepted a job at another institution. Drip … drip … drip…
Self-Reflection
Now 2:30 p.m., I took stock of my day and reflected on what my resident mentee had said about hospitalists. Trying to balance the rigors of patient care, academic requirements, life, friends, family, and being a boss, I was most definitely feeling a bit downtrodden, unsated, and crispy around the edges. What, exactly, did I like about this job? Was this what I wanted professionally? Would I ever find balance? Perhaps, too, a rheumatology application could salve my problems.
It was at that point that the notice for the SHM annual meeting appeared, oracle-like, on my desk. Picking it up, I realized this, not a two-year sojourn through the world of creaky joints, was the tonic to my problems.
Meeting Hierarchy
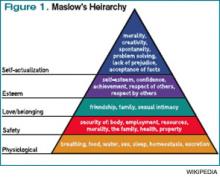
Every year since I began going to the SHM annual meeting in 2003, the meeting has helped me rejuvenate and grow. Much like Maslow’s Hierarchy of Needs, which posits that humans develop in stages that build on each other, I’ve found stepwise growth in the annual meeting.
Before my first meeting, I had been wandering nomadically through a hospitalist job for three years, wondering what, exactly, I was doing. I was the only hospitalist in my group, had few days off, with no support system around me. I had just agreed to take a job at another institution to build a new 10-person hospitalist group and had no idea how to do this. In Maslow terms, I was trying to satisfy my “physiologic needs” to survive. I needed to find, metaphorically, “food, water, clothes, and shelter.”
I found them at the annual meeting. The practice-management pre-course taught me how to build a hospitalist group, the mentorship breakfast introduced me to a veteran I still turn to, and the educational offerings helped improve my patient-care skills. I had conquered the base of Maslow’s pyramid.
The next year, I became involved in an SHM committee, and our gathering at the annual meeting helped set the course for our group’s future endeavors. I also met up with many friends I hadn’t seen since medical school and even recruited a person to my new group. In Maslow-speak, the meeting was helping me achieve my “safety needs” by providing control, well-being, and predictability.
By the third year, I was beginning to look forward to meeting up with national colleagues I had met at prior annual meetings, fulfilling Maslow’s third-stage need of “belonging.” During the ensuing years, I presented research projects, gave talks, and helped develop and lead forums and summits, thus quenching Maslow’s “self-esteem” need.
I wonder, as I leave my office to go back to see my afternoon complement of new patients, what my ninth annual meeting will bring. I’m not sure if I’ll ever achieve Maslow’s final phase of “self-actualization,” mostly because I’m not entirely sure what that means. However, I do know this: This job can be tough. We all feel it regardless of our age, gender, or practice setting. It is easy to get knocked out of balance, to get beaten down, to lose our focus. It is at those times that we all need a mariner to right the course. To remind us why we do this, to allow us to recharge, to facilitate our growth, to fulfill our needs.
For me, that mariner is the annual meeting. I look forward to seeing you all in Dallas next month. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado at Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
It’s been one of those days. It all started at 4:30 this morning, when my 3-year-old son crawled into our bed, naked except for the diarrhea dripping down his leg. Turns out, this was his way—quite effective, I might add—of telling my wife and me that he had had an “accident.” After an hour of carrying soiled sheets to the washer, child-bathing, and Weimaraner coat-scrubbing, we relaxed to the sound of our 1-year-old daughter’s blood-curdling screams.
Upon examination, we found that the night had mysteriously transformed our precious little button-nosed bundle of joy into a tangle-haired, snot-nosed bundle of melancholy. Where her face used to be, there now hung something approximating the mask from that Scream movie. Additionally, her throat was raw, olive-sized lymph nodes populated her neck, and her nose had taken to perpetual booger-manufacturing. A rapid strep swab would later reveal the culprit, but at the moment, our differential tilted toward demonic possession.
That Dripping Feeling
Moments later, my wife and I picked 6:15 a.m. as the time to discover that we both had 7 a.m. meetings and no time to drop the kids off at daycare, especially when factoring in the 10-minute “discussion” we had about who was going to drop the kids off at daycare. All of this preceded my 7:10 a.m. arrival time for the 7 o’clock meeting with a hospital executive team to discuss our HM group funding for the next year—an encounter that left me feeling as my son must have just prior to crawling into bed with us that morning.
Now 8 a.m., I had to meet with a surgeon eager to unveil his “great idea” for our hospitalists to admit all of his patients. “It solves our problem of no interns, and allows you to play a meaningful role in the hospital!” he exclaimed.
“The meaningful role of intern?” I replied. Again, I had that dripping feeling.
It was 8:30 a.m. and I was ready to round on my patients. The first patient, a lovely woman, was stricken with un-insure-ia and a deep-seated belief that the inequitable health system that rendered her unable to get her surgery was clearly the result of some moral failing on my part. Next up was a spectacularly intoxicated male who welcomed my caring touch by belching a bit of breakfast burrito onto my cheek. Then it was a floridly bipolar patient whose apparent life mission was to drop her pants to show me her new mesh thong.
Burnout, Respect, Satisfaction
And so it continued until 1 p.m., when I had a meeting with a resident mentee of mine. It turns out that he wanted to tell me that despite his desire to be a hospitalist since his fourth year of medical school, he instead was going to apply to a rheumatology fellowship. After talking to several practicing hospitalists, he’d decided it just wasn’t for him—discussions he summarized as too much burnout, too little respect, and not enough satisfaction. Again, that dripping feeling.
Stuffing my face with a vending-machine carb-load that doubled as both breakfast and lunch, I sat down for a few minutes of e-mail. First up, a journal rejection of a research paper we’d recently submitted. Oh, the fulfillment of academics. Next were two e-mails that enzymatically trebled my “to do” list for the day. Sandwiched between those e-mails and one from a friend reminding me not to be late for a dinner that night that I was clearly going to be late for was an e-mail from a nice-appearing Nigerian man wanting to give me millions of dollars; at last, my day was turning around.
Alas, this was not the case. Checking my voicemail, I found out that my uncle was in the hospital, my dog’s lab tests were abnormal, my mom was angry about something, and I had missed a dentist appointment that morning. Finally, our group assistant came with a message that our prized hospitalist recruit had accepted a job at another institution. Drip … drip … drip…
Self-Reflection
Now 2:30 p.m., I took stock of my day and reflected on what my resident mentee had said about hospitalists. Trying to balance the rigors of patient care, academic requirements, life, friends, family, and being a boss, I was most definitely feeling a bit downtrodden, unsated, and crispy around the edges. What, exactly, did I like about this job? Was this what I wanted professionally? Would I ever find balance? Perhaps, too, a rheumatology application could salve my problems.
It was at that point that the notice for the SHM annual meeting appeared, oracle-like, on my desk. Picking it up, I realized this, not a two-year sojourn through the world of creaky joints, was the tonic to my problems.
Meeting Hierarchy
Every year since I began going to the SHM annual meeting in 2003, the meeting has helped me rejuvenate and grow. Much like Maslow’s Hierarchy of Needs, which posits that humans develop in stages that build on each other, I’ve found stepwise growth in the annual meeting.
Before my first meeting, I had been wandering nomadically through a hospitalist job for three years, wondering what, exactly, I was doing. I was the only hospitalist in my group, had few days off, with no support system around me. I had just agreed to take a job at another institution to build a new 10-person hospitalist group and had no idea how to do this. In Maslow terms, I was trying to satisfy my “physiologic needs” to survive. I needed to find, metaphorically, “food, water, clothes, and shelter.”
I found them at the annual meeting. The practice-management pre-course taught me how to build a hospitalist group, the mentorship breakfast introduced me to a veteran I still turn to, and the educational offerings helped improve my patient-care skills. I had conquered the base of Maslow’s pyramid.
The next year, I became involved in an SHM committee, and our gathering at the annual meeting helped set the course for our group’s future endeavors. I also met up with many friends I hadn’t seen since medical school and even recruited a person to my new group. In Maslow-speak, the meeting was helping me achieve my “safety needs” by providing control, well-being, and predictability.
By the third year, I was beginning to look forward to meeting up with national colleagues I had met at prior annual meetings, fulfilling Maslow’s third-stage need of “belonging.” During the ensuing years, I presented research projects, gave talks, and helped develop and lead forums and summits, thus quenching Maslow’s “self-esteem” need.
I wonder, as I leave my office to go back to see my afternoon complement of new patients, what my ninth annual meeting will bring. I’m not sure if I’ll ever achieve Maslow’s final phase of “self-actualization,” mostly because I’m not entirely sure what that means. However, I do know this: This job can be tough. We all feel it regardless of our age, gender, or practice setting. It is easy to get knocked out of balance, to get beaten down, to lose our focus. It is at those times that we all need a mariner to right the course. To remind us why we do this, to allow us to recharge, to facilitate our growth, to fulfill our needs.
For me, that mariner is the annual meeting. I look forward to seeing you all in Dallas next month. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado at Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
It’s been one of those days. It all started at 4:30 this morning, when my 3-year-old son crawled into our bed, naked except for the diarrhea dripping down his leg. Turns out, this was his way—quite effective, I might add—of telling my wife and me that he had had an “accident.” After an hour of carrying soiled sheets to the washer, child-bathing, and Weimaraner coat-scrubbing, we relaxed to the sound of our 1-year-old daughter’s blood-curdling screams.
Upon examination, we found that the night had mysteriously transformed our precious little button-nosed bundle of joy into a tangle-haired, snot-nosed bundle of melancholy. Where her face used to be, there now hung something approximating the mask from that Scream movie. Additionally, her throat was raw, olive-sized lymph nodes populated her neck, and her nose had taken to perpetual booger-manufacturing. A rapid strep swab would later reveal the culprit, but at the moment, our differential tilted toward demonic possession.
That Dripping Feeling
Moments later, my wife and I picked 6:15 a.m. as the time to discover that we both had 7 a.m. meetings and no time to drop the kids off at daycare, especially when factoring in the 10-minute “discussion” we had about who was going to drop the kids off at daycare. All of this preceded my 7:10 a.m. arrival time for the 7 o’clock meeting with a hospital executive team to discuss our HM group funding for the next year—an encounter that left me feeling as my son must have just prior to crawling into bed with us that morning.
Now 8 a.m., I had to meet with a surgeon eager to unveil his “great idea” for our hospitalists to admit all of his patients. “It solves our problem of no interns, and allows you to play a meaningful role in the hospital!” he exclaimed.
“The meaningful role of intern?” I replied. Again, I had that dripping feeling.
It was 8:30 a.m. and I was ready to round on my patients. The first patient, a lovely woman, was stricken with un-insure-ia and a deep-seated belief that the inequitable health system that rendered her unable to get her surgery was clearly the result of some moral failing on my part. Next up was a spectacularly intoxicated male who welcomed my caring touch by belching a bit of breakfast burrito onto my cheek. Then it was a floridly bipolar patient whose apparent life mission was to drop her pants to show me her new mesh thong.
Burnout, Respect, Satisfaction
And so it continued until 1 p.m., when I had a meeting with a resident mentee of mine. It turns out that he wanted to tell me that despite his desire to be a hospitalist since his fourth year of medical school, he instead was going to apply to a rheumatology fellowship. After talking to several practicing hospitalists, he’d decided it just wasn’t for him—discussions he summarized as too much burnout, too little respect, and not enough satisfaction. Again, that dripping feeling.
Stuffing my face with a vending-machine carb-load that doubled as both breakfast and lunch, I sat down for a few minutes of e-mail. First up, a journal rejection of a research paper we’d recently submitted. Oh, the fulfillment of academics. Next were two e-mails that enzymatically trebled my “to do” list for the day. Sandwiched between those e-mails and one from a friend reminding me not to be late for a dinner that night that I was clearly going to be late for was an e-mail from a nice-appearing Nigerian man wanting to give me millions of dollars; at last, my day was turning around.
Alas, this was not the case. Checking my voicemail, I found out that my uncle was in the hospital, my dog’s lab tests were abnormal, my mom was angry about something, and I had missed a dentist appointment that morning. Finally, our group assistant came with a message that our prized hospitalist recruit had accepted a job at another institution. Drip … drip … drip…
Self-Reflection
Now 2:30 p.m., I took stock of my day and reflected on what my resident mentee had said about hospitalists. Trying to balance the rigors of patient care, academic requirements, life, friends, family, and being a boss, I was most definitely feeling a bit downtrodden, unsated, and crispy around the edges. What, exactly, did I like about this job? Was this what I wanted professionally? Would I ever find balance? Perhaps, too, a rheumatology application could salve my problems.
It was at that point that the notice for the SHM annual meeting appeared, oracle-like, on my desk. Picking it up, I realized this, not a two-year sojourn through the world of creaky joints, was the tonic to my problems.
Meeting Hierarchy
Every year since I began going to the SHM annual meeting in 2003, the meeting has helped me rejuvenate and grow. Much like Maslow’s Hierarchy of Needs, which posits that humans develop in stages that build on each other, I’ve found stepwise growth in the annual meeting.
Before my first meeting, I had been wandering nomadically through a hospitalist job for three years, wondering what, exactly, I was doing. I was the only hospitalist in my group, had few days off, with no support system around me. I had just agreed to take a job at another institution to build a new 10-person hospitalist group and had no idea how to do this. In Maslow terms, I was trying to satisfy my “physiologic needs” to survive. I needed to find, metaphorically, “food, water, clothes, and shelter.”
I found them at the annual meeting. The practice-management pre-course taught me how to build a hospitalist group, the mentorship breakfast introduced me to a veteran I still turn to, and the educational offerings helped improve my patient-care skills. I had conquered the base of Maslow’s pyramid.
The next year, I became involved in an SHM committee, and our gathering at the annual meeting helped set the course for our group’s future endeavors. I also met up with many friends I hadn’t seen since medical school and even recruited a person to my new group. In Maslow-speak, the meeting was helping me achieve my “safety needs” by providing control, well-being, and predictability.
By the third year, I was beginning to look forward to meeting up with national colleagues I had met at prior annual meetings, fulfilling Maslow’s third-stage need of “belonging.” During the ensuing years, I presented research projects, gave talks, and helped develop and lead forums and summits, thus quenching Maslow’s “self-esteem” need.
I wonder, as I leave my office to go back to see my afternoon complement of new patients, what my ninth annual meeting will bring. I’m not sure if I’ll ever achieve Maslow’s final phase of “self-actualization,” mostly because I’m not entirely sure what that means. However, I do know this: This job can be tough. We all feel it regardless of our age, gender, or practice setting. It is easy to get knocked out of balance, to get beaten down, to lose our focus. It is at those times that we all need a mariner to right the course. To remind us why we do this, to allow us to recharge, to facilitate our growth, to fulfill our needs.
For me, that mariner is the annual meeting. I look forward to seeing you all in Dallas next month. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado at Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
Minivan, Major Lesson
I recently visited my parents in my ancestral home of Wisconsin. As parents of a certain age, they inexplicably are genetically predisposed to owning a minivan. Another quirk of their DNA is that they must own a new minivan. No sooner has the last wisp of new-car smell osmosed from the burled walnut interior than they are trading up to the newest, tricked-out minivan. Perhaps more puzzling is the manner of pride they display in their minivan.
Now, my dad, as if not readily apparent, is not cool. And to see him folded into the driver’s seat, his furry-ear-to-furry-ear grin signaling a self-satisfaction customarily reserved for his grandchildren, painstakingly recounting glory-day stories and 4:30 p.m. dinner buffets, further solidifies his place in the Annals of Uncool.
When I’m home, they tend to employ my chauffeur services (most likely in retribution for my peri-pubescent years), and on the first day back home, I stopped their newest ride near the back door of the house, foot idling on the brake while this exchange occurred: “That’s a fascinating story about how much more challenging the world was when you were my age, Dad. You are a true American hero. Would you like to get out here or in the garage?”
“Here,” he replied.
“OK, then get out,” I countered.
“I can’t,” he responded knowingly.
“Why not?” I queried, the patience seeping from my voice.
“Because the door’s not open,” he answered, seemingly mocking me.
“Then open it,” I replied, silently recounting the evidence for his institutionalization.
“I can’t,” he responded.
“Why not?” I replied again, this time calculating the likelihood that I was adopted.
“Because it’s locked,” came his retort.
“Then unlock it,” I answered, reconfirming my decision to move away for college.
“I can’t,” he replied, ostensibly encouraging parenticide.
“Why not?” I queried, strongly contemplating parenticide.
“Because you haven’t put the car in park,” he responded triumphantly.
A System So Safe
As a safety feature, the minivan needed to be in park before you could open the door to exit. I’ve never heard of anyone actually falling out of a moving car, but recollecting high school, I can fathom the right mix, type, and number of teenagers where possibility would meet inevitability. But, apparently, enough people are falling out of moving vehicles that car engineers have built a system that is so safe, this can’t happen. So no matter how hard someone tries, it just isn’t possible to fall out of a moving car (believe me, toward the end of a week of my father’s car stories, my mind had worked every possible angle).
Likewise, newer vehicles employ occupant-sensitive sensors that detect the weight, size, and position of the passenger to determine if the airbag should deploy. Rather than depending on the driver to turn the passenger-side airbag on or off, the car does it for you: heavy enough to trigger the sensor, and the airbag will deploy; too light, and the car assumes you are a child and doesn’t deploy. It’s a system that is so safe because it doesn’t depend on the operator to get it right.
Ditto motion sensors that detect objects behind the car while reversing (avoiding accidental back-overs), antilock brakes (to maintain control during panicked braking), traction control (improves stability during acceleration), electronic stability control (foils spinouts), tire-pressure-monitoring systems (avoids blowouts), daytime running lights (ensures others see you), rollover airbags (they stay inflated to keep you in the car), lane-departure warning (alerts you if you stray from your lane), and doors that automatically lock after the car starts (again, falling out of cars).
For all the negative press of late, car manufacturers understand safety.
A System Not So Safe
Contrast this to healthcare, in which 10% of patients will suffer a serious, preventable, adverse event during their hospital stay.1 Read that sentence again. That’s 10%; that’s preventable; that’s a number that has largely remained unchanged in the past decade. If 1 in 10 drivers suffered a serious adverse preventable auto accident, Congress would do nothing but hold automotive safety hearings.
In medicine, we still largely employ unsafe systems in which even the best doctors can, and do, hurt patients. Sure, we have made strides in this arena (oxygen tubing that only works if hooked up properly, smart pumps that avert IV dosing errors, CO2 monitors to detect proper endotracheal tube placement), but remarkably, in this era of patient safety, we still utilize systems that largely depend on the heroism of the individual.
As physicians, we are famously autonomous and value our professional independence, even to the degree that it might harm patients. We generally eschew standardization, believing that each patient is inherently different. In fact, the thrill of the improvisational theater that follows every patient’s chief compliant is one of the great satisfiers in medicine. We love that feeling that comes from sleuthing each case, deftly enacting a plan of action to shepherd the patient to health.
To suggest following protocols, guidelines, and checklists is derisively dismissed as “cookbook medicine.” To work in teams in which certain tasks are delegated to others is seen as weakness—we don’t need a system that utilizes a pharmacist; rather, we should know the doses of all medicines, their interactions, and the effect of renal and liver impairment on their clearance. To suggest otherwise is an insult to our Oslerian roots. To examine our errors, our system breakdowns, our patient harms is anathema to our practice, an admission of failure.
The result is that most of us continue to toil in systems that have become exponentially unsafe as healthcare has become more complex. Today, we still have a system that will more or less allow us to kill a patient by doing nothing more than forgetting the letter “g.” I can go to my hospital today and intend to write “4 grams of magnesium sulfate (MgSO4)” and inadvertently forget the “g” in “Mg.” This could result in an order for a lethal dose of morphine sulfate (MSO4). It’s that easy to hurt a patient. Now, you might say that would never happen, because the pharmacy would catch it. And this is likely. But is it guaranteed? Can you 100% ensure it wouldn’t happen? Consider that nearly 20% of medication doses administered in a hospital are done so incorrectly.2 Nearly 1 in 5. This is the type of system we are employing to stop this lethal overdose. Is this system, which depends on another human to prevent an error, foolproof, or just a snare waiting to prove you the fool?
This represents our opportunity. As hospitalists, the hospital is our tapestry, our system of care, our responsibility. Few others are as well-positioned to ensure that the systems that envelop our patients are highly functional, reliable, and safe. This will take work—work that will feel burdensome, underappreciated, undercompensated. And, fully recognizing that none of us went into medicine to become systems engineers, this will be hard.
However, if not us, who? Who will ensure that our fathers, our mothers, our children will be as safe in the hospital as they are on the drive to the hospital? TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
References
- Global health leaders join the World Health Organization to announce accelerated efforts to improve patient safety. World Health Organization website. Available at: www.who.int/mediacentre/news/releases/2004/pr74/en/. Accessed Feb. 14, 2011.
- Barker KN, Flynn EA, Pepper GA, Bates DW, Mikeal RL. Medication errors observed in 36 health care facilities. Arch Intern Med. 2002;162(16):1897-1903.
I recently visited my parents in my ancestral home of Wisconsin. As parents of a certain age, they inexplicably are genetically predisposed to owning a minivan. Another quirk of their DNA is that they must own a new minivan. No sooner has the last wisp of new-car smell osmosed from the burled walnut interior than they are trading up to the newest, tricked-out minivan. Perhaps more puzzling is the manner of pride they display in their minivan.
Now, my dad, as if not readily apparent, is not cool. And to see him folded into the driver’s seat, his furry-ear-to-furry-ear grin signaling a self-satisfaction customarily reserved for his grandchildren, painstakingly recounting glory-day stories and 4:30 p.m. dinner buffets, further solidifies his place in the Annals of Uncool.
When I’m home, they tend to employ my chauffeur services (most likely in retribution for my peri-pubescent years), and on the first day back home, I stopped their newest ride near the back door of the house, foot idling on the brake while this exchange occurred: “That’s a fascinating story about how much more challenging the world was when you were my age, Dad. You are a true American hero. Would you like to get out here or in the garage?”
“Here,” he replied.
“OK, then get out,” I countered.
“I can’t,” he responded knowingly.
“Why not?” I queried, the patience seeping from my voice.
“Because the door’s not open,” he answered, seemingly mocking me.
“Then open it,” I replied, silently recounting the evidence for his institutionalization.
“I can’t,” he responded.
“Why not?” I replied again, this time calculating the likelihood that I was adopted.
“Because it’s locked,” came his retort.
“Then unlock it,” I answered, reconfirming my decision to move away for college.
“I can’t,” he replied, ostensibly encouraging parenticide.
“Why not?” I queried, strongly contemplating parenticide.
“Because you haven’t put the car in park,” he responded triumphantly.
A System So Safe
As a safety feature, the minivan needed to be in park before you could open the door to exit. I’ve never heard of anyone actually falling out of a moving car, but recollecting high school, I can fathom the right mix, type, and number of teenagers where possibility would meet inevitability. But, apparently, enough people are falling out of moving vehicles that car engineers have built a system that is so safe, this can’t happen. So no matter how hard someone tries, it just isn’t possible to fall out of a moving car (believe me, toward the end of a week of my father’s car stories, my mind had worked every possible angle).
Likewise, newer vehicles employ occupant-sensitive sensors that detect the weight, size, and position of the passenger to determine if the airbag should deploy. Rather than depending on the driver to turn the passenger-side airbag on or off, the car does it for you: heavy enough to trigger the sensor, and the airbag will deploy; too light, and the car assumes you are a child and doesn’t deploy. It’s a system that is so safe because it doesn’t depend on the operator to get it right.
Ditto motion sensors that detect objects behind the car while reversing (avoiding accidental back-overs), antilock brakes (to maintain control during panicked braking), traction control (improves stability during acceleration), electronic stability control (foils spinouts), tire-pressure-monitoring systems (avoids blowouts), daytime running lights (ensures others see you), rollover airbags (they stay inflated to keep you in the car), lane-departure warning (alerts you if you stray from your lane), and doors that automatically lock after the car starts (again, falling out of cars).
For all the negative press of late, car manufacturers understand safety.
A System Not So Safe
Contrast this to healthcare, in which 10% of patients will suffer a serious, preventable, adverse event during their hospital stay.1 Read that sentence again. That’s 10%; that’s preventable; that’s a number that has largely remained unchanged in the past decade. If 1 in 10 drivers suffered a serious adverse preventable auto accident, Congress would do nothing but hold automotive safety hearings.
In medicine, we still largely employ unsafe systems in which even the best doctors can, and do, hurt patients. Sure, we have made strides in this arena (oxygen tubing that only works if hooked up properly, smart pumps that avert IV dosing errors, CO2 monitors to detect proper endotracheal tube placement), but remarkably, in this era of patient safety, we still utilize systems that largely depend on the heroism of the individual.
As physicians, we are famously autonomous and value our professional independence, even to the degree that it might harm patients. We generally eschew standardization, believing that each patient is inherently different. In fact, the thrill of the improvisational theater that follows every patient’s chief compliant is one of the great satisfiers in medicine. We love that feeling that comes from sleuthing each case, deftly enacting a plan of action to shepherd the patient to health.
To suggest following protocols, guidelines, and checklists is derisively dismissed as “cookbook medicine.” To work in teams in which certain tasks are delegated to others is seen as weakness—we don’t need a system that utilizes a pharmacist; rather, we should know the doses of all medicines, their interactions, and the effect of renal and liver impairment on their clearance. To suggest otherwise is an insult to our Oslerian roots. To examine our errors, our system breakdowns, our patient harms is anathema to our practice, an admission of failure.
The result is that most of us continue to toil in systems that have become exponentially unsafe as healthcare has become more complex. Today, we still have a system that will more or less allow us to kill a patient by doing nothing more than forgetting the letter “g.” I can go to my hospital today and intend to write “4 grams of magnesium sulfate (MgSO4)” and inadvertently forget the “g” in “Mg.” This could result in an order for a lethal dose of morphine sulfate (MSO4). It’s that easy to hurt a patient. Now, you might say that would never happen, because the pharmacy would catch it. And this is likely. But is it guaranteed? Can you 100% ensure it wouldn’t happen? Consider that nearly 20% of medication doses administered in a hospital are done so incorrectly.2 Nearly 1 in 5. This is the type of system we are employing to stop this lethal overdose. Is this system, which depends on another human to prevent an error, foolproof, or just a snare waiting to prove you the fool?
This represents our opportunity. As hospitalists, the hospital is our tapestry, our system of care, our responsibility. Few others are as well-positioned to ensure that the systems that envelop our patients are highly functional, reliable, and safe. This will take work—work that will feel burdensome, underappreciated, undercompensated. And, fully recognizing that none of us went into medicine to become systems engineers, this will be hard.
However, if not us, who? Who will ensure that our fathers, our mothers, our children will be as safe in the hospital as they are on the drive to the hospital? TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
References
- Global health leaders join the World Health Organization to announce accelerated efforts to improve patient safety. World Health Organization website. Available at: www.who.int/mediacentre/news/releases/2004/pr74/en/. Accessed Feb. 14, 2011.
- Barker KN, Flynn EA, Pepper GA, Bates DW, Mikeal RL. Medication errors observed in 36 health care facilities. Arch Intern Med. 2002;162(16):1897-1903.
I recently visited my parents in my ancestral home of Wisconsin. As parents of a certain age, they inexplicably are genetically predisposed to owning a minivan. Another quirk of their DNA is that they must own a new minivan. No sooner has the last wisp of new-car smell osmosed from the burled walnut interior than they are trading up to the newest, tricked-out minivan. Perhaps more puzzling is the manner of pride they display in their minivan.
Now, my dad, as if not readily apparent, is not cool. And to see him folded into the driver’s seat, his furry-ear-to-furry-ear grin signaling a self-satisfaction customarily reserved for his grandchildren, painstakingly recounting glory-day stories and 4:30 p.m. dinner buffets, further solidifies his place in the Annals of Uncool.
When I’m home, they tend to employ my chauffeur services (most likely in retribution for my peri-pubescent years), and on the first day back home, I stopped their newest ride near the back door of the house, foot idling on the brake while this exchange occurred: “That’s a fascinating story about how much more challenging the world was when you were my age, Dad. You are a true American hero. Would you like to get out here or in the garage?”
“Here,” he replied.
“OK, then get out,” I countered.
“I can’t,” he responded knowingly.
“Why not?” I queried, the patience seeping from my voice.
“Because the door’s not open,” he answered, seemingly mocking me.
“Then open it,” I replied, silently recounting the evidence for his institutionalization.
“I can’t,” he responded.
“Why not?” I replied again, this time calculating the likelihood that I was adopted.
“Because it’s locked,” came his retort.
“Then unlock it,” I answered, reconfirming my decision to move away for college.
“I can’t,” he replied, ostensibly encouraging parenticide.
“Why not?” I queried, strongly contemplating parenticide.
“Because you haven’t put the car in park,” he responded triumphantly.
A System So Safe
As a safety feature, the minivan needed to be in park before you could open the door to exit. I’ve never heard of anyone actually falling out of a moving car, but recollecting high school, I can fathom the right mix, type, and number of teenagers where possibility would meet inevitability. But, apparently, enough people are falling out of moving vehicles that car engineers have built a system that is so safe, this can’t happen. So no matter how hard someone tries, it just isn’t possible to fall out of a moving car (believe me, toward the end of a week of my father’s car stories, my mind had worked every possible angle).
Likewise, newer vehicles employ occupant-sensitive sensors that detect the weight, size, and position of the passenger to determine if the airbag should deploy. Rather than depending on the driver to turn the passenger-side airbag on or off, the car does it for you: heavy enough to trigger the sensor, and the airbag will deploy; too light, and the car assumes you are a child and doesn’t deploy. It’s a system that is so safe because it doesn’t depend on the operator to get it right.
Ditto motion sensors that detect objects behind the car while reversing (avoiding accidental back-overs), antilock brakes (to maintain control during panicked braking), traction control (improves stability during acceleration), electronic stability control (foils spinouts), tire-pressure-monitoring systems (avoids blowouts), daytime running lights (ensures others see you), rollover airbags (they stay inflated to keep you in the car), lane-departure warning (alerts you if you stray from your lane), and doors that automatically lock after the car starts (again, falling out of cars).
For all the negative press of late, car manufacturers understand safety.
A System Not So Safe
Contrast this to healthcare, in which 10% of patients will suffer a serious, preventable, adverse event during their hospital stay.1 Read that sentence again. That’s 10%; that’s preventable; that’s a number that has largely remained unchanged in the past decade. If 1 in 10 drivers suffered a serious adverse preventable auto accident, Congress would do nothing but hold automotive safety hearings.
In medicine, we still largely employ unsafe systems in which even the best doctors can, and do, hurt patients. Sure, we have made strides in this arena (oxygen tubing that only works if hooked up properly, smart pumps that avert IV dosing errors, CO2 monitors to detect proper endotracheal tube placement), but remarkably, in this era of patient safety, we still utilize systems that largely depend on the heroism of the individual.
As physicians, we are famously autonomous and value our professional independence, even to the degree that it might harm patients. We generally eschew standardization, believing that each patient is inherently different. In fact, the thrill of the improvisational theater that follows every patient’s chief compliant is one of the great satisfiers in medicine. We love that feeling that comes from sleuthing each case, deftly enacting a plan of action to shepherd the patient to health.
To suggest following protocols, guidelines, and checklists is derisively dismissed as “cookbook medicine.” To work in teams in which certain tasks are delegated to others is seen as weakness—we don’t need a system that utilizes a pharmacist; rather, we should know the doses of all medicines, their interactions, and the effect of renal and liver impairment on their clearance. To suggest otherwise is an insult to our Oslerian roots. To examine our errors, our system breakdowns, our patient harms is anathema to our practice, an admission of failure.
The result is that most of us continue to toil in systems that have become exponentially unsafe as healthcare has become more complex. Today, we still have a system that will more or less allow us to kill a patient by doing nothing more than forgetting the letter “g.” I can go to my hospital today and intend to write “4 grams of magnesium sulfate (MgSO4)” and inadvertently forget the “g” in “Mg.” This could result in an order for a lethal dose of morphine sulfate (MSO4). It’s that easy to hurt a patient. Now, you might say that would never happen, because the pharmacy would catch it. And this is likely. But is it guaranteed? Can you 100% ensure it wouldn’t happen? Consider that nearly 20% of medication doses administered in a hospital are done so incorrectly.2 Nearly 1 in 5. This is the type of system we are employing to stop this lethal overdose. Is this system, which depends on another human to prevent an error, foolproof, or just a snare waiting to prove you the fool?
This represents our opportunity. As hospitalists, the hospital is our tapestry, our system of care, our responsibility. Few others are as well-positioned to ensure that the systems that envelop our patients are highly functional, reliable, and safe. This will take work—work that will feel burdensome, underappreciated, undercompensated. And, fully recognizing that none of us went into medicine to become systems engineers, this will be hard.
However, if not us, who? Who will ensure that our fathers, our mothers, our children will be as safe in the hospital as they are on the drive to the hospital? TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
References
- Global health leaders join the World Health Organization to announce accelerated efforts to improve patient safety. World Health Organization website. Available at: www.who.int/mediacentre/news/releases/2004/pr74/en/. Accessed Feb. 14, 2011.
- Barker KN, Flynn EA, Pepper GA, Bates DW, Mikeal RL. Medication errors observed in 36 health care facilities. Arch Intern Med. 2002;162(16):1897-1903.
Surgery’s Waterboys
The query came from the audience: “But isn’t comanagement really about us becoming the surgeon’s waterboy?” Encouraged by the chortling crowd, he furthered, “I mean, think about it: How much more demeaning can it get than to be the admit-ologist and discharge-ologist for the surgeon? They make all the coin and we just follow after them picking up their jock straps.”
Slack-jawed, I mustered what was, under the circumstances, a rather confident “Umm … ?”
This comment, from a talk I gave a couple of years ago at an SHM annual meeting about comanagement, took me a bit by surprise. Not because of the sentiment; that I get. It’s easy to feel that the comanagement we do suffices only to sate the surgeon at the hospitalist’s expense. Rather, I was taken aback because of its indication of the distance with which we’ve missed the comanagement bull’s-eye.
New Comanagement Data
A recent article regarding the comanagement of neurosurgical patients drudged this oratorical memory from its peaceful cerebral resting place between the 1982 Milwaukee Brewers’ starting outfield (Ogilvie, Thomas, Moore), my wife’s least favorite Beatle (Ringo), and the number of macaroni noodles my grade-school friend Mike could stuff into his nostril and cough up through his mouth (nine with aspiration, five without). In the paper, Auerbach et al report a retrospective, before-and-after study of 7,596 patients admitted to the neurosurgery service at the University of California at San Francisco Medical Center.1 The authors compared administrative, financial, and survey data for 4,203 patients before a hospitalist-neurosurgery comanagement arrangement to 3,393 patients after the program implementation—by far the largest trial of hospitalist comanagement to date.
They found:
- Shockingly, surgeons (“hospitalists make it easier for me to do my job”) and nurses (“I can easily and promptly reach a physician”) liked having us around.
- Curiously, patients were rather indifferent (measured via patient satisfaction indicators) to our presence.
- The cost of care decreased by about $1,500 per patient after the intercalation of hospitalists—this despite the fact that the length of stay was unchanged before and after model implementation.
- Unfortunately, such traditional markers of quality as mortality and readmission rate remained stubbornly unchanged.
- Encouragingly, nontraditional-but-likely-important indicators of quality (e.g. nursing and physician perception of improvements in care provision) were achieved.
Perspective
This study adds significantly to our understanding of the comanagement model. The finding of costs savings is as expected (nearly all studies of hospitalist programs have shown cost savings) as it is unexpected (prior studies of comanagement models reported no cost savings).2 Likewise, the lack of improvement of hard quality endpoints (mortality and readmission rates) is consistent with most studies of hospitalist programs, including a previous report of comanagement of orthopedic patients that showed improvements only in minor complications, such as rates of electrolyte abnormalities, while improvement in the softer quality endpoints—nursing and surgeon satisfaction and perceptions of quality—is consistent with most reports and conventional wisdom.2
Within hours of publication, the blogs were throbbing with discussion of what this meant for the field of hospital medicine. Did this prove comanagement to be the godsend many believe (perceptions of improved quality), the complete farce that many believe (no evidence of mortality benefit), or was this just further confirmation that hospitalists are really nothing more than cost reduction-ists?
My opinion? This is just the comanagement MacGuffin.
MacGuffin Explained
Fans of film will know that the MacGuffin is a Hitchcockian plot device that uses a meaningless but often mysterious and intriguing element to drive the plot. So while everyone, it seems, is concerned with the MacGuffin, the MacGuffin exists only to help the story unfold. Think of the “government secrets” driving the plot in Hitchcock’s North by Northwest, or “unobtainium” in the movie Avatar. In both cases, the MacGuffin preoccupied the cast (they had to have it, or defend it), but in the end, the MacGuffin was insignificant except to move the plot forward.
In much the same way, the debate about whether the shared-care model of surgical patients is a good thing is comanagment’s MacGuffin; it definitely drives the plot but ultimately it misses the point. The real comanagement story—indeed, the story of the whole of hospital medicine—is our need to fundamentally improve outcomes through systems improvements. The true benefit of comanagement is not in one doctor (hospitalist) taking over the medical care of another doctor (surgeon). That will only slightly improve outcomes of the medical issues at which the hospitalist is more expert (e.g. minor electrolyte disorders). Meanwhile, this model continues to allow the same harms that the underlying unsafe hospital system imparts. The comanagement model itself won’t fix this. Rather, the model simply acts as a mechanism for us to accomplish our desired goals of system redesign.
Put another way, I am better at internal-medicine care than a neurosurgeon is. As such, I have no doubt that if I manage the medical issues of neurosurgical patients, I will do it better. However, this system of hospitalist provision of internal-medicine care can ultimately only lead to the type of marginal, not meaningful, improvements these comanagement studies have shown.
The real potential for the comanagement model comes when I take off my internal-medicine hat (diabetes care, electrolyte management, etc.) and put on my HM hat (ability to execute systematic quality and process improvements that result in safer systems that effect ALL patients, ALL the time, and is not dependent on the individual provider to do the right thing).
In doing this, the MacGuffin—the comanagement model that cohorts a lot of patients in the hands of a relatively few hospitalists—affords us the opportunity to truly advance the patient-safety plot by building better systems, the type of systems that ensure that every patient systematically gets appropriate VTE prophylaxis, avoids medication errors, has unnecessary urinary and central venous catheters removed, avoids pressure ulcers, doesn’t fall or get delirious, and has expert transitions of care. I have no doubt that if we achieved these kinds of interventions, rather than just managing patients’ medical issues, we’d see the kind of profound changes the comanagement model can offer.
MacGuffin or not, comanagement is likely here to stay. The challenge, then, is to find a way in which these care arrangements can go beyond scut to systematically and comprehensively improve the flawed systems of care that envelop our surgical patients.
Doing this will vastly improve patient outcomes, add significant value to the care we provide, and clearly signal to the surgeon that it’s time to bring us the water bottle. TH
Dr. Glasheen is physician editor of The Hospitalist. He is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
References
- Auerbach AD, Wachter RM, Cheng HQ, et al. Comanagement of surgical patients between neurosurgeons and hospitalists. Arch Intern Med. 2010;170(22):2004-2010.
- Huddleston JM, Long KH, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141(1):28-38.
The query came from the audience: “But isn’t comanagement really about us becoming the surgeon’s waterboy?” Encouraged by the chortling crowd, he furthered, “I mean, think about it: How much more demeaning can it get than to be the admit-ologist and discharge-ologist for the surgeon? They make all the coin and we just follow after them picking up their jock straps.”
Slack-jawed, I mustered what was, under the circumstances, a rather confident “Umm … ?”
This comment, from a talk I gave a couple of years ago at an SHM annual meeting about comanagement, took me a bit by surprise. Not because of the sentiment; that I get. It’s easy to feel that the comanagement we do suffices only to sate the surgeon at the hospitalist’s expense. Rather, I was taken aback because of its indication of the distance with which we’ve missed the comanagement bull’s-eye.
New Comanagement Data
A recent article regarding the comanagement of neurosurgical patients drudged this oratorical memory from its peaceful cerebral resting place between the 1982 Milwaukee Brewers’ starting outfield (Ogilvie, Thomas, Moore), my wife’s least favorite Beatle (Ringo), and the number of macaroni noodles my grade-school friend Mike could stuff into his nostril and cough up through his mouth (nine with aspiration, five without). In the paper, Auerbach et al report a retrospective, before-and-after study of 7,596 patients admitted to the neurosurgery service at the University of California at San Francisco Medical Center.1 The authors compared administrative, financial, and survey data for 4,203 patients before a hospitalist-neurosurgery comanagement arrangement to 3,393 patients after the program implementation—by far the largest trial of hospitalist comanagement to date.
They found:
- Shockingly, surgeons (“hospitalists make it easier for me to do my job”) and nurses (“I can easily and promptly reach a physician”) liked having us around.
- Curiously, patients were rather indifferent (measured via patient satisfaction indicators) to our presence.
- The cost of care decreased by about $1,500 per patient after the intercalation of hospitalists—this despite the fact that the length of stay was unchanged before and after model implementation.
- Unfortunately, such traditional markers of quality as mortality and readmission rate remained stubbornly unchanged.
- Encouragingly, nontraditional-but-likely-important indicators of quality (e.g. nursing and physician perception of improvements in care provision) were achieved.
Perspective
This study adds significantly to our understanding of the comanagement model. The finding of costs savings is as expected (nearly all studies of hospitalist programs have shown cost savings) as it is unexpected (prior studies of comanagement models reported no cost savings).2 Likewise, the lack of improvement of hard quality endpoints (mortality and readmission rates) is consistent with most studies of hospitalist programs, including a previous report of comanagement of orthopedic patients that showed improvements only in minor complications, such as rates of electrolyte abnormalities, while improvement in the softer quality endpoints—nursing and surgeon satisfaction and perceptions of quality—is consistent with most reports and conventional wisdom.2
Within hours of publication, the blogs were throbbing with discussion of what this meant for the field of hospital medicine. Did this prove comanagement to be the godsend many believe (perceptions of improved quality), the complete farce that many believe (no evidence of mortality benefit), or was this just further confirmation that hospitalists are really nothing more than cost reduction-ists?
My opinion? This is just the comanagement MacGuffin.
MacGuffin Explained
Fans of film will know that the MacGuffin is a Hitchcockian plot device that uses a meaningless but often mysterious and intriguing element to drive the plot. So while everyone, it seems, is concerned with the MacGuffin, the MacGuffin exists only to help the story unfold. Think of the “government secrets” driving the plot in Hitchcock’s North by Northwest, or “unobtainium” in the movie Avatar. In both cases, the MacGuffin preoccupied the cast (they had to have it, or defend it), but in the end, the MacGuffin was insignificant except to move the plot forward.
In much the same way, the debate about whether the shared-care model of surgical patients is a good thing is comanagment’s MacGuffin; it definitely drives the plot but ultimately it misses the point. The real comanagement story—indeed, the story of the whole of hospital medicine—is our need to fundamentally improve outcomes through systems improvements. The true benefit of comanagement is not in one doctor (hospitalist) taking over the medical care of another doctor (surgeon). That will only slightly improve outcomes of the medical issues at which the hospitalist is more expert (e.g. minor electrolyte disorders). Meanwhile, this model continues to allow the same harms that the underlying unsafe hospital system imparts. The comanagement model itself won’t fix this. Rather, the model simply acts as a mechanism for us to accomplish our desired goals of system redesign.
Put another way, I am better at internal-medicine care than a neurosurgeon is. As such, I have no doubt that if I manage the medical issues of neurosurgical patients, I will do it better. However, this system of hospitalist provision of internal-medicine care can ultimately only lead to the type of marginal, not meaningful, improvements these comanagement studies have shown.
The real potential for the comanagement model comes when I take off my internal-medicine hat (diabetes care, electrolyte management, etc.) and put on my HM hat (ability to execute systematic quality and process improvements that result in safer systems that effect ALL patients, ALL the time, and is not dependent on the individual provider to do the right thing).
In doing this, the MacGuffin—the comanagement model that cohorts a lot of patients in the hands of a relatively few hospitalists—affords us the opportunity to truly advance the patient-safety plot by building better systems, the type of systems that ensure that every patient systematically gets appropriate VTE prophylaxis, avoids medication errors, has unnecessary urinary and central venous catheters removed, avoids pressure ulcers, doesn’t fall or get delirious, and has expert transitions of care. I have no doubt that if we achieved these kinds of interventions, rather than just managing patients’ medical issues, we’d see the kind of profound changes the comanagement model can offer.
MacGuffin or not, comanagement is likely here to stay. The challenge, then, is to find a way in which these care arrangements can go beyond scut to systematically and comprehensively improve the flawed systems of care that envelop our surgical patients.
Doing this will vastly improve patient outcomes, add significant value to the care we provide, and clearly signal to the surgeon that it’s time to bring us the water bottle. TH
Dr. Glasheen is physician editor of The Hospitalist. He is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
References
- Auerbach AD, Wachter RM, Cheng HQ, et al. Comanagement of surgical patients between neurosurgeons and hospitalists. Arch Intern Med. 2010;170(22):2004-2010.
- Huddleston JM, Long KH, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141(1):28-38.
The query came from the audience: “But isn’t comanagement really about us becoming the surgeon’s waterboy?” Encouraged by the chortling crowd, he furthered, “I mean, think about it: How much more demeaning can it get than to be the admit-ologist and discharge-ologist for the surgeon? They make all the coin and we just follow after them picking up their jock straps.”
Slack-jawed, I mustered what was, under the circumstances, a rather confident “Umm … ?”
This comment, from a talk I gave a couple of years ago at an SHM annual meeting about comanagement, took me a bit by surprise. Not because of the sentiment; that I get. It’s easy to feel that the comanagement we do suffices only to sate the surgeon at the hospitalist’s expense. Rather, I was taken aback because of its indication of the distance with which we’ve missed the comanagement bull’s-eye.
New Comanagement Data
A recent article regarding the comanagement of neurosurgical patients drudged this oratorical memory from its peaceful cerebral resting place between the 1982 Milwaukee Brewers’ starting outfield (Ogilvie, Thomas, Moore), my wife’s least favorite Beatle (Ringo), and the number of macaroni noodles my grade-school friend Mike could stuff into his nostril and cough up through his mouth (nine with aspiration, five without). In the paper, Auerbach et al report a retrospective, before-and-after study of 7,596 patients admitted to the neurosurgery service at the University of California at San Francisco Medical Center.1 The authors compared administrative, financial, and survey data for 4,203 patients before a hospitalist-neurosurgery comanagement arrangement to 3,393 patients after the program implementation—by far the largest trial of hospitalist comanagement to date.
They found:
- Shockingly, surgeons (“hospitalists make it easier for me to do my job”) and nurses (“I can easily and promptly reach a physician”) liked having us around.
- Curiously, patients were rather indifferent (measured via patient satisfaction indicators) to our presence.
- The cost of care decreased by about $1,500 per patient after the intercalation of hospitalists—this despite the fact that the length of stay was unchanged before and after model implementation.
- Unfortunately, such traditional markers of quality as mortality and readmission rate remained stubbornly unchanged.
- Encouragingly, nontraditional-but-likely-important indicators of quality (e.g. nursing and physician perception of improvements in care provision) were achieved.
Perspective
This study adds significantly to our understanding of the comanagement model. The finding of costs savings is as expected (nearly all studies of hospitalist programs have shown cost savings) as it is unexpected (prior studies of comanagement models reported no cost savings).2 Likewise, the lack of improvement of hard quality endpoints (mortality and readmission rates) is consistent with most studies of hospitalist programs, including a previous report of comanagement of orthopedic patients that showed improvements only in minor complications, such as rates of electrolyte abnormalities, while improvement in the softer quality endpoints—nursing and surgeon satisfaction and perceptions of quality—is consistent with most reports and conventional wisdom.2
Within hours of publication, the blogs were throbbing with discussion of what this meant for the field of hospital medicine. Did this prove comanagement to be the godsend many believe (perceptions of improved quality), the complete farce that many believe (no evidence of mortality benefit), or was this just further confirmation that hospitalists are really nothing more than cost reduction-ists?
My opinion? This is just the comanagement MacGuffin.
MacGuffin Explained
Fans of film will know that the MacGuffin is a Hitchcockian plot device that uses a meaningless but often mysterious and intriguing element to drive the plot. So while everyone, it seems, is concerned with the MacGuffin, the MacGuffin exists only to help the story unfold. Think of the “government secrets” driving the plot in Hitchcock’s North by Northwest, or “unobtainium” in the movie Avatar. In both cases, the MacGuffin preoccupied the cast (they had to have it, or defend it), but in the end, the MacGuffin was insignificant except to move the plot forward.
In much the same way, the debate about whether the shared-care model of surgical patients is a good thing is comanagment’s MacGuffin; it definitely drives the plot but ultimately it misses the point. The real comanagement story—indeed, the story of the whole of hospital medicine—is our need to fundamentally improve outcomes through systems improvements. The true benefit of comanagement is not in one doctor (hospitalist) taking over the medical care of another doctor (surgeon). That will only slightly improve outcomes of the medical issues at which the hospitalist is more expert (e.g. minor electrolyte disorders). Meanwhile, this model continues to allow the same harms that the underlying unsafe hospital system imparts. The comanagement model itself won’t fix this. Rather, the model simply acts as a mechanism for us to accomplish our desired goals of system redesign.
Put another way, I am better at internal-medicine care than a neurosurgeon is. As such, I have no doubt that if I manage the medical issues of neurosurgical patients, I will do it better. However, this system of hospitalist provision of internal-medicine care can ultimately only lead to the type of marginal, not meaningful, improvements these comanagement studies have shown.
The real potential for the comanagement model comes when I take off my internal-medicine hat (diabetes care, electrolyte management, etc.) and put on my HM hat (ability to execute systematic quality and process improvements that result in safer systems that effect ALL patients, ALL the time, and is not dependent on the individual provider to do the right thing).
In doing this, the MacGuffin—the comanagement model that cohorts a lot of patients in the hands of a relatively few hospitalists—affords us the opportunity to truly advance the patient-safety plot by building better systems, the type of systems that ensure that every patient systematically gets appropriate VTE prophylaxis, avoids medication errors, has unnecessary urinary and central venous catheters removed, avoids pressure ulcers, doesn’t fall or get delirious, and has expert transitions of care. I have no doubt that if we achieved these kinds of interventions, rather than just managing patients’ medical issues, we’d see the kind of profound changes the comanagement model can offer.
MacGuffin or not, comanagement is likely here to stay. The challenge, then, is to find a way in which these care arrangements can go beyond scut to systematically and comprehensively improve the flawed systems of care that envelop our surgical patients.
Doing this will vastly improve patient outcomes, add significant value to the care we provide, and clearly signal to the surgeon that it’s time to bring us the water bottle. TH
Dr. Glasheen is physician editor of The Hospitalist. He is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
References
- Auerbach AD, Wachter RM, Cheng HQ, et al. Comanagement of surgical patients between neurosurgeons and hospitalists. Arch Intern Med. 2010;170(22):2004-2010.
- Huddleston JM, Long KH, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141(1):28-38.
Words Forever Lost
She couldn’t have been more than two weeks old, a newborn. Tussling in her mother’s arms just outside the patient’s room, she let out a gurgle of a cry. Her two brothers, twins by the look of it, clung to Mom’s pant leg for answers. Mom was speechless, tears burning lava tracks down her face. Her husband lay splayed as the centerpiece on display. Cords draped his chest, radioing green tachycardia to an overhead monitor. The man’s breathing was a tangle of labored dyspnea, harsh coughing and raw panic. A nurse suctioned his mouth while an intern vultured over his wrist, eagerly attempting his first arterial line.
I surveyed this scene through the unsullied eyes of a medical student, figuratively clinging to my resident’s pant leg for answers. I was young, confused, and scared by the drama. I didn’t know it yet, but by morning light, this “great case” would morph from “a 29-year-old with acute lymphoblastic leukemia complicated by severe community-acquired pneumonia” to one of the most powerful lessons of my career.
A lesson I wasn’t intended to learn.
Hidden Curriculum
For those of you unfamiliar with the term, the “hidden curriculum” is the things we are “taught” when no one thinks they are teaching. It’s not what teachers necessarily say; it’s how they say it, how they act, what they do. It’s nearly always unconscious, unintentional. We learn these things by watching people interact, the inflections and tone of their voices, their bedside manner, the way they treat staff and patients.
This is not just an issue for teaching hospitalists who are imparting these unwitting lessons daily. Rather, it is important to recognize that all of us have been exposed to, and our careers and practices shaped by, these hidden messages. Sometimes these lessons impart such helpful tools as noting how a skilled clinician puts a patient at ease before palpating their abdomen. Other times, the tutorial is less beneficial (e.g. subconsciously teaching bias or impatience). And sometimes the message conveyed is much more malignant.
I, unfortunately, was about to be taught the latter.
Room 118
The man, stripped of his shirt, his pants, his dignity, winced with the pain of the third radial art-line attempt. He tried to hitch himself up in bed, drawing a scowl from the intern who had to readjust his sterile field—a rebuke from the nurse who got lubricant on her shirt. “Can’t you see that I’m trying to place a catheter in your penis?” she implored. Of course he could—as could I, his family, and much of the ICU. That was part of the lesson.
To be fair, I honestly doubt that anyone in room 118 intended to treat Mr. Davis in such a callous way. They didn’t intend to depersonalize the situation—make him an object, another cog in the wheel of their daily grind. They simply were trying to do their jobs—to save this new admission’s life. A noble intention, indeed.
However, in doing this, they employed a career’s worth of defense mechanisms aimed at fending off the stress of a life-threatening situation. And each of these actions moved them ever so slightly away from the compassion that defines our field and toward the seemingly uncaring automatons they had become.
The Lesson Continues
By now, Mr. Davis was breathing 40 times a minute. A neb of medications, a drip of antibiotics, and a facemask of oxygen did little to prevent his slide. Exposed, shivering, lights reflecting off the paunch of his naked stomach, he cried out for his wife. Coming to him, she was halted by the icy stare of the grizzled charge nurse called in to hold the combatant down. “You’re lucky we even allow you in the ICU with those kids,” she thundered.
The ABG was still pending, but the critical-care fellow was confident of its results. To nobody, he declared, “We have to tube this guy.” Terror was etched in the “guy’s” eyes as he searched the room for answers. What does “tubing” mean? he must have wondered. Am I going to die? Would my sons remember me? Would my daughter be OK? How will my wife do it without me?
Again, he called out for his wife.
It didn’t take long for the excitement to reverberate throughout the hospital. A surgical intern stopped by room 118 to see if he could put in any lines, while the respiratory therapist prepared a vent and a few more medical students rubbernecked in the hall. The oncology fellow took a moment to teach us about a recent article she read that showed that pneumonia was uniformly fatal in acute leukemic patients who got intubated. “Do you mean tubing him is essentially a death sentence?” I asked, death confronting me for the first time in my career. Meeting the patient’s eyes, she turned and lowered her voice to reply, leaving me to wonder if this was the kind of thing we should keep secret.
The wife, managing to momentarily penetrate the critical-care zone defense, was holding Mr. Davis’ hand while she filled his ear with whispers. With his daughter’s face mere inches from his, he appeared calmer. He tried to speak but was drowned out by the charge nurse who demanded he remove his wedding band. “But … I … don’t … want … ”
“I know you don’t want to take it off, sir, but you have to,” she demanded, shooing the wife from the bedside. “Your hands are going to get edematous in the next few days and you don’t want me to have to cut it off, do you?” she asked rhetorically. Crestfallen, he extended his ring finger to his wife, as he no doubt did years earlier, an understanding of his fate crossing his face. Missing the cue, the nurse deftly intercepted the ring off his finger, placing it in her pocket as she swooped out of the room to get the intubation kit, leaving Mr. Davis further agitated.
The critical-care fellow lowered the head of the bed, leaving Mr. Davis upright and calling for his wife. “My … ring … ” he panted, his breathing worsening by the breath. “I … need … to tell … my … wife … ” he gasped as the charge nurse thrust him a bit too harshly to the bed, adding that there wasn’t time to talk now—his message would have to wait. “But … ” the patient protested as the sedative coursed into this vein. “I need … her … to … know … ”
“Quiet now, sir, you have to calm down, you’re just making this harder.” The wife tore closer to him, no doubt wondering what could possibly make this harder. “I love you, John,” she said. “I … ” he replied.
The tube slipped in.
Reflections
It’s been 15 years, but I think of this night often. In some ways, I am haunted by it; in many ways, my practice style was fashioned by it; in all ways, I was changed by it. I wonder if the same can be said for the other providers.
I also wonder about Mr. Davis. How did the world look through his eyes? Did he see us as his saviors or his tormentors? Did he worry for his well-being, or was he too absorbed in the welfare of his kids and wife to fret about himself? Did he worry about his kids seeing him sick, the impact that might have on them? Was he scared? How must he have felt to be left so powerless? To have no control over his situation. To have his wedding band taken by a complete stranger. To not be able to give his wife an urgent message.
Did it have to be this way? Could we have better balanced the urgency of the situation with the humanity it required? In doing our jobs, did we have to dismiss the one person who entrusted us to help him?
I also think about how that night influenced me. How it shaped my approach to the patients who privilege me to care for them during their most vulnerable times. I wonder what came of the Davis family. That newborn daughter is learning to drive, the boys preparing for college. And I also wonder what it was John so urgently wanted to tell his wife that night. As, no doubt, does she.
For Mr. Davis died that night, his words forever lost. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado at Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
She couldn’t have been more than two weeks old, a newborn. Tussling in her mother’s arms just outside the patient’s room, she let out a gurgle of a cry. Her two brothers, twins by the look of it, clung to Mom’s pant leg for answers. Mom was speechless, tears burning lava tracks down her face. Her husband lay splayed as the centerpiece on display. Cords draped his chest, radioing green tachycardia to an overhead monitor. The man’s breathing was a tangle of labored dyspnea, harsh coughing and raw panic. A nurse suctioned his mouth while an intern vultured over his wrist, eagerly attempting his first arterial line.
I surveyed this scene through the unsullied eyes of a medical student, figuratively clinging to my resident’s pant leg for answers. I was young, confused, and scared by the drama. I didn’t know it yet, but by morning light, this “great case” would morph from “a 29-year-old with acute lymphoblastic leukemia complicated by severe community-acquired pneumonia” to one of the most powerful lessons of my career.
A lesson I wasn’t intended to learn.
Hidden Curriculum
For those of you unfamiliar with the term, the “hidden curriculum” is the things we are “taught” when no one thinks they are teaching. It’s not what teachers necessarily say; it’s how they say it, how they act, what they do. It’s nearly always unconscious, unintentional. We learn these things by watching people interact, the inflections and tone of their voices, their bedside manner, the way they treat staff and patients.
This is not just an issue for teaching hospitalists who are imparting these unwitting lessons daily. Rather, it is important to recognize that all of us have been exposed to, and our careers and practices shaped by, these hidden messages. Sometimes these lessons impart such helpful tools as noting how a skilled clinician puts a patient at ease before palpating their abdomen. Other times, the tutorial is less beneficial (e.g. subconsciously teaching bias or impatience). And sometimes the message conveyed is much more malignant.
I, unfortunately, was about to be taught the latter.
Room 118
The man, stripped of his shirt, his pants, his dignity, winced with the pain of the third radial art-line attempt. He tried to hitch himself up in bed, drawing a scowl from the intern who had to readjust his sterile field—a rebuke from the nurse who got lubricant on her shirt. “Can’t you see that I’m trying to place a catheter in your penis?” she implored. Of course he could—as could I, his family, and much of the ICU. That was part of the lesson.
To be fair, I honestly doubt that anyone in room 118 intended to treat Mr. Davis in such a callous way. They didn’t intend to depersonalize the situation—make him an object, another cog in the wheel of their daily grind. They simply were trying to do their jobs—to save this new admission’s life. A noble intention, indeed.
However, in doing this, they employed a career’s worth of defense mechanisms aimed at fending off the stress of a life-threatening situation. And each of these actions moved them ever so slightly away from the compassion that defines our field and toward the seemingly uncaring automatons they had become.
The Lesson Continues
By now, Mr. Davis was breathing 40 times a minute. A neb of medications, a drip of antibiotics, and a facemask of oxygen did little to prevent his slide. Exposed, shivering, lights reflecting off the paunch of his naked stomach, he cried out for his wife. Coming to him, she was halted by the icy stare of the grizzled charge nurse called in to hold the combatant down. “You’re lucky we even allow you in the ICU with those kids,” she thundered.
The ABG was still pending, but the critical-care fellow was confident of its results. To nobody, he declared, “We have to tube this guy.” Terror was etched in the “guy’s” eyes as he searched the room for answers. What does “tubing” mean? he must have wondered. Am I going to die? Would my sons remember me? Would my daughter be OK? How will my wife do it without me?
Again, he called out for his wife.
It didn’t take long for the excitement to reverberate throughout the hospital. A surgical intern stopped by room 118 to see if he could put in any lines, while the respiratory therapist prepared a vent and a few more medical students rubbernecked in the hall. The oncology fellow took a moment to teach us about a recent article she read that showed that pneumonia was uniformly fatal in acute leukemic patients who got intubated. “Do you mean tubing him is essentially a death sentence?” I asked, death confronting me for the first time in my career. Meeting the patient’s eyes, she turned and lowered her voice to reply, leaving me to wonder if this was the kind of thing we should keep secret.
The wife, managing to momentarily penetrate the critical-care zone defense, was holding Mr. Davis’ hand while she filled his ear with whispers. With his daughter’s face mere inches from his, he appeared calmer. He tried to speak but was drowned out by the charge nurse who demanded he remove his wedding band. “But … I … don’t … want … ”
“I know you don’t want to take it off, sir, but you have to,” she demanded, shooing the wife from the bedside. “Your hands are going to get edematous in the next few days and you don’t want me to have to cut it off, do you?” she asked rhetorically. Crestfallen, he extended his ring finger to his wife, as he no doubt did years earlier, an understanding of his fate crossing his face. Missing the cue, the nurse deftly intercepted the ring off his finger, placing it in her pocket as she swooped out of the room to get the intubation kit, leaving Mr. Davis further agitated.
The critical-care fellow lowered the head of the bed, leaving Mr. Davis upright and calling for his wife. “My … ring … ” he panted, his breathing worsening by the breath. “I … need … to tell … my … wife … ” he gasped as the charge nurse thrust him a bit too harshly to the bed, adding that there wasn’t time to talk now—his message would have to wait. “But … ” the patient protested as the sedative coursed into this vein. “I need … her … to … know … ”
“Quiet now, sir, you have to calm down, you’re just making this harder.” The wife tore closer to him, no doubt wondering what could possibly make this harder. “I love you, John,” she said. “I … ” he replied.
The tube slipped in.
Reflections
It’s been 15 years, but I think of this night often. In some ways, I am haunted by it; in many ways, my practice style was fashioned by it; in all ways, I was changed by it. I wonder if the same can be said for the other providers.
I also wonder about Mr. Davis. How did the world look through his eyes? Did he see us as his saviors or his tormentors? Did he worry for his well-being, or was he too absorbed in the welfare of his kids and wife to fret about himself? Did he worry about his kids seeing him sick, the impact that might have on them? Was he scared? How must he have felt to be left so powerless? To have no control over his situation. To have his wedding band taken by a complete stranger. To not be able to give his wife an urgent message.
Did it have to be this way? Could we have better balanced the urgency of the situation with the humanity it required? In doing our jobs, did we have to dismiss the one person who entrusted us to help him?
I also think about how that night influenced me. How it shaped my approach to the patients who privilege me to care for them during their most vulnerable times. I wonder what came of the Davis family. That newborn daughter is learning to drive, the boys preparing for college. And I also wonder what it was John so urgently wanted to tell his wife that night. As, no doubt, does she.
For Mr. Davis died that night, his words forever lost. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado at Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
She couldn’t have been more than two weeks old, a newborn. Tussling in her mother’s arms just outside the patient’s room, she let out a gurgle of a cry. Her two brothers, twins by the look of it, clung to Mom’s pant leg for answers. Mom was speechless, tears burning lava tracks down her face. Her husband lay splayed as the centerpiece on display. Cords draped his chest, radioing green tachycardia to an overhead monitor. The man’s breathing was a tangle of labored dyspnea, harsh coughing and raw panic. A nurse suctioned his mouth while an intern vultured over his wrist, eagerly attempting his first arterial line.
I surveyed this scene through the unsullied eyes of a medical student, figuratively clinging to my resident’s pant leg for answers. I was young, confused, and scared by the drama. I didn’t know it yet, but by morning light, this “great case” would morph from “a 29-year-old with acute lymphoblastic leukemia complicated by severe community-acquired pneumonia” to one of the most powerful lessons of my career.
A lesson I wasn’t intended to learn.
Hidden Curriculum
For those of you unfamiliar with the term, the “hidden curriculum” is the things we are “taught” when no one thinks they are teaching. It’s not what teachers necessarily say; it’s how they say it, how they act, what they do. It’s nearly always unconscious, unintentional. We learn these things by watching people interact, the inflections and tone of their voices, their bedside manner, the way they treat staff and patients.
This is not just an issue for teaching hospitalists who are imparting these unwitting lessons daily. Rather, it is important to recognize that all of us have been exposed to, and our careers and practices shaped by, these hidden messages. Sometimes these lessons impart such helpful tools as noting how a skilled clinician puts a patient at ease before palpating their abdomen. Other times, the tutorial is less beneficial (e.g. subconsciously teaching bias or impatience). And sometimes the message conveyed is much more malignant.
I, unfortunately, was about to be taught the latter.
Room 118
The man, stripped of his shirt, his pants, his dignity, winced with the pain of the third radial art-line attempt. He tried to hitch himself up in bed, drawing a scowl from the intern who had to readjust his sterile field—a rebuke from the nurse who got lubricant on her shirt. “Can’t you see that I’m trying to place a catheter in your penis?” she implored. Of course he could—as could I, his family, and much of the ICU. That was part of the lesson.
To be fair, I honestly doubt that anyone in room 118 intended to treat Mr. Davis in such a callous way. They didn’t intend to depersonalize the situation—make him an object, another cog in the wheel of their daily grind. They simply were trying to do their jobs—to save this new admission’s life. A noble intention, indeed.
However, in doing this, they employed a career’s worth of defense mechanisms aimed at fending off the stress of a life-threatening situation. And each of these actions moved them ever so slightly away from the compassion that defines our field and toward the seemingly uncaring automatons they had become.
The Lesson Continues
By now, Mr. Davis was breathing 40 times a minute. A neb of medications, a drip of antibiotics, and a facemask of oxygen did little to prevent his slide. Exposed, shivering, lights reflecting off the paunch of his naked stomach, he cried out for his wife. Coming to him, she was halted by the icy stare of the grizzled charge nurse called in to hold the combatant down. “You’re lucky we even allow you in the ICU with those kids,” she thundered.
The ABG was still pending, but the critical-care fellow was confident of its results. To nobody, he declared, “We have to tube this guy.” Terror was etched in the “guy’s” eyes as he searched the room for answers. What does “tubing” mean? he must have wondered. Am I going to die? Would my sons remember me? Would my daughter be OK? How will my wife do it without me?
Again, he called out for his wife.
It didn’t take long for the excitement to reverberate throughout the hospital. A surgical intern stopped by room 118 to see if he could put in any lines, while the respiratory therapist prepared a vent and a few more medical students rubbernecked in the hall. The oncology fellow took a moment to teach us about a recent article she read that showed that pneumonia was uniformly fatal in acute leukemic patients who got intubated. “Do you mean tubing him is essentially a death sentence?” I asked, death confronting me for the first time in my career. Meeting the patient’s eyes, she turned and lowered her voice to reply, leaving me to wonder if this was the kind of thing we should keep secret.
The wife, managing to momentarily penetrate the critical-care zone defense, was holding Mr. Davis’ hand while she filled his ear with whispers. With his daughter’s face mere inches from his, he appeared calmer. He tried to speak but was drowned out by the charge nurse who demanded he remove his wedding band. “But … I … don’t … want … ”
“I know you don’t want to take it off, sir, but you have to,” she demanded, shooing the wife from the bedside. “Your hands are going to get edematous in the next few days and you don’t want me to have to cut it off, do you?” she asked rhetorically. Crestfallen, he extended his ring finger to his wife, as he no doubt did years earlier, an understanding of his fate crossing his face. Missing the cue, the nurse deftly intercepted the ring off his finger, placing it in her pocket as she swooped out of the room to get the intubation kit, leaving Mr. Davis further agitated.
The critical-care fellow lowered the head of the bed, leaving Mr. Davis upright and calling for his wife. “My … ring … ” he panted, his breathing worsening by the breath. “I … need … to tell … my … wife … ” he gasped as the charge nurse thrust him a bit too harshly to the bed, adding that there wasn’t time to talk now—his message would have to wait. “But … ” the patient protested as the sedative coursed into this vein. “I need … her … to … know … ”
“Quiet now, sir, you have to calm down, you’re just making this harder.” The wife tore closer to him, no doubt wondering what could possibly make this harder. “I love you, John,” she said. “I … ” he replied.
The tube slipped in.
Reflections
It’s been 15 years, but I think of this night often. In some ways, I am haunted by it; in many ways, my practice style was fashioned by it; in all ways, I was changed by it. I wonder if the same can be said for the other providers.
I also wonder about Mr. Davis. How did the world look through his eyes? Did he see us as his saviors or his tormentors? Did he worry for his well-being, or was he too absorbed in the welfare of his kids and wife to fret about himself? Did he worry about his kids seeing him sick, the impact that might have on them? Was he scared? How must he have felt to be left so powerless? To have no control over his situation. To have his wedding band taken by a complete stranger. To not be able to give his wife an urgent message.
Did it have to be this way? Could we have better balanced the urgency of the situation with the humanity it required? In doing our jobs, did we have to dismiss the one person who entrusted us to help him?
I also think about how that night influenced me. How it shaped my approach to the patients who privilege me to care for them during their most vulnerable times. I wonder what came of the Davis family. That newborn daughter is learning to drive, the boys preparing for college. And I also wonder what it was John so urgently wanted to tell his wife that night. As, no doubt, does she.
For Mr. Davis died that night, his words forever lost. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado at Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
Designed to Harm
If every system is perfectly designed to get the results it gets …
And if 15 million patients are harmed every year from medical care …
And if as many as 98,000 people die every year due to medical errors in hospitals …
Then what does that say about the system we have designed?
A System Designed to Competently Hurt Many
By now you’ve no doubt heard, read, and possibly even uttered the above facts and figures yourself. I think we all have our opinions about the veracity of these numbers, but I don’t think any of us would argue with the sentiment. The U.S. healthcare system comprises the most competent, compassionate, well-meaning, and caring professionals on this planet—who harm, maim, and kill countless people every year.
What a discomforting paradox.
Equity: The Overlooked Quality Domain
Many years back, the Institute of Medicine (IOM) published a list of six “domains” of healthcare quality. You’ve no doubt stumbled across the IOM’s Safe … Timely … Effective … Efficient … Equitable … Patient-Centered mnemonic recipe—STEEEP—for high-quality care.1 In fact, it’s hard to read a journal, attend a medical presentation, or open a local newspaper without finding reference to these domains. It’s all the rage to talk about wrong-site surgery (safe), access to care (timely), comparative-effectiveness research (effective), lean concepts (efficient), and individualized medicine (patient-centered). However, the sixth domain often seems to get the Jan Brady treatment—minimized, marginalized, and oft-forgotten.
The IOM defines equitable care as that which “does not vary in quality because of personal characteristics such as gender, ethnicity, geographic location, and socioeconomic status.”1 To be sure, there is some hum at the national level about issues of equity, especially around healthcare coverage for all. And this is important. However, what appears lost in the rant surrounding the inherent inequities in our tiered health insurance system is that we have blantant inequalities baked into the everyday machinery of our hospitals. And they affect all, regardless of skin color, gender, or insurance status.
Think for a moment about your hospital. Are the type, level, and access to care equal at all times? Does the level of care change when the streetlights come on? How about on weekends and holidays? Do your operating rooms run on Saturdays and Sundays? Can patients get chemotherapy on the weekends? Does your hospital alter its nursing staff ratios after hours? Can you get an ultrasound at midnight? How about a urology or neurosurgery consult at 2 a.m.? How about getting interventional radiology to place an IVC filter on a holiday?
Now scratch a bit closer to home. Does your hospitalist group downstaff on weekends and holidays, even though the volumes probably warrant more coverage? Are your night providers part of your group, or are they moonlighters? Do your after-hours providers cross-cover and admit a reasonable number of patients, or are they frequently overwhelmed? Do they cover patients or admit for services that they don’t typically care for during the day (e.g. ICU, neurosurgical, subspecialty cardiology or oncology patients)? For the intensely ill patients admitted to U.S. hospitals today, should the type and availability of care differ when it’s delivered at 3 p.m. or 3 a.m., Sunday or Monday?
Disregarding the macro-inequities in our societal approach to healthcare, can we even ensure equitable care within our own hospital walls 24 hours a day, seven days a week?
The Answer: An Unfortunate “No”
For the record, I hate working nights, abhor working weekends, and resent working holidays. But the thing I’d hate even more than working nights, weekends, and holidays would be being a patient admitted during a night, weekend, or holiday. To understand why, I have to look no further than my hospital parking lot. During bankers’ hours, I can barely find a parking spot on the top floor of our multilevel parking structure.
Fast-forward to Saturday, and I have my pick of empty football fields’ worth of spots on all floors. Ditto Sundays, nights, and holidays.
Why is it that nationally, a collectively near-trillion-dollar hospital enterprise finds it acceptable to effectively shutter itself for a quarter to a third of the week? Especially when doing so seems to counter their primary mission of providing safe, timely, effective, efficient, equitable, and patient-centered care.
The Weekend Effect
There are, of course, economic and operational reasons to downshift during off hours—some hospitals don’t have the elective procedures to run operating rooms seven days a week, and very few patients want to have their elective colonoscopy at 11 p.m. or their chemotherapy during Thanksgiving dinner. However, in most cases, the reasons for doing so center on hospital staff and physician satisfaction. Most us of just don’t like working off hours. As a result, studies have shown significantly less access to such high-level care as coronary angiography and percutaneous coronary intervention on weekends.2,3
And the effects of this “weekend effect” can be devastating.
A recent paper in the New England Journal of Medicine reported that for every 1,000 patients admitted with a myocardial infarction on a weekend, nine more would die than a comparable group admitted during the week.4 Their offense? Having the misfortune to get ill on a Saturday morning. The authors concluded that this higher mortality was secondary to a lower rate of invasive cardiac procedures, presumably because they were less available. And the weekend effect isn’t just limited to coronary care. Poorer outcomes, including higher mortality rates, have been reported for weekend admissions to the neonatal ICU and adult ICU, as well as admission for epiglottitis, ruptured abdominal aortic aneurysms, and pulmonary embolism.5,6,7
So let’s connect the dots: A system designed with inequal access to lifesaving therapies and appropriate staffing results in worse outcomes, more harm, more deaths.
To be clear, 98,000 people don’t die every year because of my disdain for working nights and weekends. This is a much deeper problem that hinges on many unsatisfactory systems working unsatisfactorily in tandem (e.g. see the other five IOM domains of quality care). Furthermore, I don’t mean to suggest that hospitalists necessarily have a lot of say in cardiac catheterization schedules. Yet we do control our own systems of care—how many patients we admit and cover during a shift, how strongly we advocate for timely testing and consultation, how we staff weekends and cover patients at night.
And, more and more, we are in a position to enhance the care delivery systems of the hospital and its providers that surround us. With that comes a responsibility to ensure that these systems are highly functioning and equitable, regardless of the time of day, day of the week.
If we are going to fundamentally enhance the quality of care, then we have to design safer systems of care. It will take time and resources to alter many of our bruised systems of care, but we can begin by at least ensuring equity in how we deliver care at our own institutions. That is, unless we are comfortable with a system perfectly designed to harm. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
References
- Institute of Medicine (IOM). Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C.: National Academy Press; 2001.
- Bell CM, Redelmeier DA. Waiting for urgent procedures on the weekend among emergently hospitalized patients. Am J Med. 2004:117(3):175-181.
- Magid DJ, Wang Y, Herrin J, et al. Relationship between time of day, day of week, timeliness of reperfusion, and in-hospital mortality for patients with acute ST-segment elevation myocardial infarction. JAMA. 2005;294(7):803-812.
- Kostis WJ, Demissie K, Marcella SW, Shao YH, Wilson AC, Moreyra AE. Weekend versus weekday admission and mortality from myocardial infarction. N Eng J Med. 2007;356 (11):1099-1109.
- Hendry RA. The weekend—a dangerous time to be born? Br J Obstet Gynaecol. 1981;88(12):1200-1203.
- Barnett MJ, Kaboli PJ, Sirio CA, Rosenthal GE. Day of the week of intensive care admission and patient outcomes: a multisite regional evaluation. Med Care. 2002;40(6):530-539.
- Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Eng J Med. 2001;345(9):663-668.
If every system is perfectly designed to get the results it gets …
And if 15 million patients are harmed every year from medical care …
And if as many as 98,000 people die every year due to medical errors in hospitals …
Then what does that say about the system we have designed?
A System Designed to Competently Hurt Many
By now you’ve no doubt heard, read, and possibly even uttered the above facts and figures yourself. I think we all have our opinions about the veracity of these numbers, but I don’t think any of us would argue with the sentiment. The U.S. healthcare system comprises the most competent, compassionate, well-meaning, and caring professionals on this planet—who harm, maim, and kill countless people every year.
What a discomforting paradox.
Equity: The Overlooked Quality Domain
Many years back, the Institute of Medicine (IOM) published a list of six “domains” of healthcare quality. You’ve no doubt stumbled across the IOM’s Safe … Timely … Effective … Efficient … Equitable … Patient-Centered mnemonic recipe—STEEEP—for high-quality care.1 In fact, it’s hard to read a journal, attend a medical presentation, or open a local newspaper without finding reference to these domains. It’s all the rage to talk about wrong-site surgery (safe), access to care (timely), comparative-effectiveness research (effective), lean concepts (efficient), and individualized medicine (patient-centered). However, the sixth domain often seems to get the Jan Brady treatment—minimized, marginalized, and oft-forgotten.
The IOM defines equitable care as that which “does not vary in quality because of personal characteristics such as gender, ethnicity, geographic location, and socioeconomic status.”1 To be sure, there is some hum at the national level about issues of equity, especially around healthcare coverage for all. And this is important. However, what appears lost in the rant surrounding the inherent inequities in our tiered health insurance system is that we have blantant inequalities baked into the everyday machinery of our hospitals. And they affect all, regardless of skin color, gender, or insurance status.
Think for a moment about your hospital. Are the type, level, and access to care equal at all times? Does the level of care change when the streetlights come on? How about on weekends and holidays? Do your operating rooms run on Saturdays and Sundays? Can patients get chemotherapy on the weekends? Does your hospital alter its nursing staff ratios after hours? Can you get an ultrasound at midnight? How about a urology or neurosurgery consult at 2 a.m.? How about getting interventional radiology to place an IVC filter on a holiday?
Now scratch a bit closer to home. Does your hospitalist group downstaff on weekends and holidays, even though the volumes probably warrant more coverage? Are your night providers part of your group, or are they moonlighters? Do your after-hours providers cross-cover and admit a reasonable number of patients, or are they frequently overwhelmed? Do they cover patients or admit for services that they don’t typically care for during the day (e.g. ICU, neurosurgical, subspecialty cardiology or oncology patients)? For the intensely ill patients admitted to U.S. hospitals today, should the type and availability of care differ when it’s delivered at 3 p.m. or 3 a.m., Sunday or Monday?
Disregarding the macro-inequities in our societal approach to healthcare, can we even ensure equitable care within our own hospital walls 24 hours a day, seven days a week?
The Answer: An Unfortunate “No”
For the record, I hate working nights, abhor working weekends, and resent working holidays. But the thing I’d hate even more than working nights, weekends, and holidays would be being a patient admitted during a night, weekend, or holiday. To understand why, I have to look no further than my hospital parking lot. During bankers’ hours, I can barely find a parking spot on the top floor of our multilevel parking structure.
Fast-forward to Saturday, and I have my pick of empty football fields’ worth of spots on all floors. Ditto Sundays, nights, and holidays.
Why is it that nationally, a collectively near-trillion-dollar hospital enterprise finds it acceptable to effectively shutter itself for a quarter to a third of the week? Especially when doing so seems to counter their primary mission of providing safe, timely, effective, efficient, equitable, and patient-centered care.
The Weekend Effect
There are, of course, economic and operational reasons to downshift during off hours—some hospitals don’t have the elective procedures to run operating rooms seven days a week, and very few patients want to have their elective colonoscopy at 11 p.m. or their chemotherapy during Thanksgiving dinner. However, in most cases, the reasons for doing so center on hospital staff and physician satisfaction. Most us of just don’t like working off hours. As a result, studies have shown significantly less access to such high-level care as coronary angiography and percutaneous coronary intervention on weekends.2,3
And the effects of this “weekend effect” can be devastating.
A recent paper in the New England Journal of Medicine reported that for every 1,000 patients admitted with a myocardial infarction on a weekend, nine more would die than a comparable group admitted during the week.4 Their offense? Having the misfortune to get ill on a Saturday morning. The authors concluded that this higher mortality was secondary to a lower rate of invasive cardiac procedures, presumably because they were less available. And the weekend effect isn’t just limited to coronary care. Poorer outcomes, including higher mortality rates, have been reported for weekend admissions to the neonatal ICU and adult ICU, as well as admission for epiglottitis, ruptured abdominal aortic aneurysms, and pulmonary embolism.5,6,7
So let’s connect the dots: A system designed with inequal access to lifesaving therapies and appropriate staffing results in worse outcomes, more harm, more deaths.
To be clear, 98,000 people don’t die every year because of my disdain for working nights and weekends. This is a much deeper problem that hinges on many unsatisfactory systems working unsatisfactorily in tandem (e.g. see the other five IOM domains of quality care). Furthermore, I don’t mean to suggest that hospitalists necessarily have a lot of say in cardiac catheterization schedules. Yet we do control our own systems of care—how many patients we admit and cover during a shift, how strongly we advocate for timely testing and consultation, how we staff weekends and cover patients at night.
And, more and more, we are in a position to enhance the care delivery systems of the hospital and its providers that surround us. With that comes a responsibility to ensure that these systems are highly functioning and equitable, regardless of the time of day, day of the week.
If we are going to fundamentally enhance the quality of care, then we have to design safer systems of care. It will take time and resources to alter many of our bruised systems of care, but we can begin by at least ensuring equity in how we deliver care at our own institutions. That is, unless we are comfortable with a system perfectly designed to harm. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
References
- Institute of Medicine (IOM). Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C.: National Academy Press; 2001.
- Bell CM, Redelmeier DA. Waiting for urgent procedures on the weekend among emergently hospitalized patients. Am J Med. 2004:117(3):175-181.
- Magid DJ, Wang Y, Herrin J, et al. Relationship between time of day, day of week, timeliness of reperfusion, and in-hospital mortality for patients with acute ST-segment elevation myocardial infarction. JAMA. 2005;294(7):803-812.
- Kostis WJ, Demissie K, Marcella SW, Shao YH, Wilson AC, Moreyra AE. Weekend versus weekday admission and mortality from myocardial infarction. N Eng J Med. 2007;356 (11):1099-1109.
- Hendry RA. The weekend—a dangerous time to be born? Br J Obstet Gynaecol. 1981;88(12):1200-1203.
- Barnett MJ, Kaboli PJ, Sirio CA, Rosenthal GE. Day of the week of intensive care admission and patient outcomes: a multisite regional evaluation. Med Care. 2002;40(6):530-539.
- Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Eng J Med. 2001;345(9):663-668.
If every system is perfectly designed to get the results it gets …
And if 15 million patients are harmed every year from medical care …
And if as many as 98,000 people die every year due to medical errors in hospitals …
Then what does that say about the system we have designed?
A System Designed to Competently Hurt Many
By now you’ve no doubt heard, read, and possibly even uttered the above facts and figures yourself. I think we all have our opinions about the veracity of these numbers, but I don’t think any of us would argue with the sentiment. The U.S. healthcare system comprises the most competent, compassionate, well-meaning, and caring professionals on this planet—who harm, maim, and kill countless people every year.
What a discomforting paradox.
Equity: The Overlooked Quality Domain
Many years back, the Institute of Medicine (IOM) published a list of six “domains” of healthcare quality. You’ve no doubt stumbled across the IOM’s Safe … Timely … Effective … Efficient … Equitable … Patient-Centered mnemonic recipe—STEEEP—for high-quality care.1 In fact, it’s hard to read a journal, attend a medical presentation, or open a local newspaper without finding reference to these domains. It’s all the rage to talk about wrong-site surgery (safe), access to care (timely), comparative-effectiveness research (effective), lean concepts (efficient), and individualized medicine (patient-centered). However, the sixth domain often seems to get the Jan Brady treatment—minimized, marginalized, and oft-forgotten.
The IOM defines equitable care as that which “does not vary in quality because of personal characteristics such as gender, ethnicity, geographic location, and socioeconomic status.”1 To be sure, there is some hum at the national level about issues of equity, especially around healthcare coverage for all. And this is important. However, what appears lost in the rant surrounding the inherent inequities in our tiered health insurance system is that we have blantant inequalities baked into the everyday machinery of our hospitals. And they affect all, regardless of skin color, gender, or insurance status.
Think for a moment about your hospital. Are the type, level, and access to care equal at all times? Does the level of care change when the streetlights come on? How about on weekends and holidays? Do your operating rooms run on Saturdays and Sundays? Can patients get chemotherapy on the weekends? Does your hospital alter its nursing staff ratios after hours? Can you get an ultrasound at midnight? How about a urology or neurosurgery consult at 2 a.m.? How about getting interventional radiology to place an IVC filter on a holiday?
Now scratch a bit closer to home. Does your hospitalist group downstaff on weekends and holidays, even though the volumes probably warrant more coverage? Are your night providers part of your group, or are they moonlighters? Do your after-hours providers cross-cover and admit a reasonable number of patients, or are they frequently overwhelmed? Do they cover patients or admit for services that they don’t typically care for during the day (e.g. ICU, neurosurgical, subspecialty cardiology or oncology patients)? For the intensely ill patients admitted to U.S. hospitals today, should the type and availability of care differ when it’s delivered at 3 p.m. or 3 a.m., Sunday or Monday?
Disregarding the macro-inequities in our societal approach to healthcare, can we even ensure equitable care within our own hospital walls 24 hours a day, seven days a week?
The Answer: An Unfortunate “No”
For the record, I hate working nights, abhor working weekends, and resent working holidays. But the thing I’d hate even more than working nights, weekends, and holidays would be being a patient admitted during a night, weekend, or holiday. To understand why, I have to look no further than my hospital parking lot. During bankers’ hours, I can barely find a parking spot on the top floor of our multilevel parking structure.
Fast-forward to Saturday, and I have my pick of empty football fields’ worth of spots on all floors. Ditto Sundays, nights, and holidays.
Why is it that nationally, a collectively near-trillion-dollar hospital enterprise finds it acceptable to effectively shutter itself for a quarter to a third of the week? Especially when doing so seems to counter their primary mission of providing safe, timely, effective, efficient, equitable, and patient-centered care.
The Weekend Effect
There are, of course, economic and operational reasons to downshift during off hours—some hospitals don’t have the elective procedures to run operating rooms seven days a week, and very few patients want to have their elective colonoscopy at 11 p.m. or their chemotherapy during Thanksgiving dinner. However, in most cases, the reasons for doing so center on hospital staff and physician satisfaction. Most us of just don’t like working off hours. As a result, studies have shown significantly less access to such high-level care as coronary angiography and percutaneous coronary intervention on weekends.2,3
And the effects of this “weekend effect” can be devastating.
A recent paper in the New England Journal of Medicine reported that for every 1,000 patients admitted with a myocardial infarction on a weekend, nine more would die than a comparable group admitted during the week.4 Their offense? Having the misfortune to get ill on a Saturday morning. The authors concluded that this higher mortality was secondary to a lower rate of invasive cardiac procedures, presumably because they were less available. And the weekend effect isn’t just limited to coronary care. Poorer outcomes, including higher mortality rates, have been reported for weekend admissions to the neonatal ICU and adult ICU, as well as admission for epiglottitis, ruptured abdominal aortic aneurysms, and pulmonary embolism.5,6,7
So let’s connect the dots: A system designed with inequal access to lifesaving therapies and appropriate staffing results in worse outcomes, more harm, more deaths.
To be clear, 98,000 people don’t die every year because of my disdain for working nights and weekends. This is a much deeper problem that hinges on many unsatisfactory systems working unsatisfactorily in tandem (e.g. see the other five IOM domains of quality care). Furthermore, I don’t mean to suggest that hospitalists necessarily have a lot of say in cardiac catheterization schedules. Yet we do control our own systems of care—how many patients we admit and cover during a shift, how strongly we advocate for timely testing and consultation, how we staff weekends and cover patients at night.
And, more and more, we are in a position to enhance the care delivery systems of the hospital and its providers that surround us. With that comes a responsibility to ensure that these systems are highly functioning and equitable, regardless of the time of day, day of the week.
If we are going to fundamentally enhance the quality of care, then we have to design safer systems of care. It will take time and resources to alter many of our bruised systems of care, but we can begin by at least ensuring equity in how we deliver care at our own institutions. That is, unless we are comfortable with a system perfectly designed to harm. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
References
- Institute of Medicine (IOM). Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C.: National Academy Press; 2001.
- Bell CM, Redelmeier DA. Waiting for urgent procedures on the weekend among emergently hospitalized patients. Am J Med. 2004:117(3):175-181.
- Magid DJ, Wang Y, Herrin J, et al. Relationship between time of day, day of week, timeliness of reperfusion, and in-hospital mortality for patients with acute ST-segment elevation myocardial infarction. JAMA. 2005;294(7):803-812.
- Kostis WJ, Demissie K, Marcella SW, Shao YH, Wilson AC, Moreyra AE. Weekend versus weekday admission and mortality from myocardial infarction. N Eng J Med. 2007;356 (11):1099-1109.
- Hendry RA. The weekend—a dangerous time to be born? Br J Obstet Gynaecol. 1981;88(12):1200-1203.
- Barnett MJ, Kaboli PJ, Sirio CA, Rosenthal GE. Day of the week of intensive care admission and patient outcomes: a multisite regional evaluation. Med Care. 2002;40(6):530-539.
- Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Eng J Med. 2001;345(9):663-668.
Underwater Breathing
It’s fall. I know that because the leaves are turning, the nights are chillier, and my dogs have migrated back to the bed from a hot summer on the floor. Oh, and I again need to fill four positions for my hospitalist group.
A lot has changed in HM recruiting in the past few years. There was a feeding frenzy in the early part of the century, when I often joked that group leaders were so desperate for boots on the ground that my mom (who is not a physician, is retired, and struggles somewhat with the triple acid-base disorder) could have gotten a job as a hospitalist. I saw it in the number of reference calls for the residents in our program, their ever-increasing salary offers, and the breathless e-mails I’d receive from headhunters. Improbably, on occasion, their froth would even boil over to an offer for me, an academic. Now that’s desperation.
But things seem to be changing. The number of calls per resident is down and my inbox is filled with slightly less-winded recruiters. Maybe groups have finally matured and don’t need to hire; maybe the recession has induced an air of caution around growth; or maybe groups have uncovered the secret tonic to seeing more patients with fewer providers. Whatever it is, it seems that the job market has tightened ever so slightly.
And the job market has changed, especially on the academic side.
Work Harder for Less
In academics, we hire into jobs we describe as “clinician-something,” with the something reflecting what you do when you are not seeing patients, the thing that in most cases will get you promoted from instructor to assistant to associate to professor. Because HM is not a fellowship-driven field, primary researchers, called clinician-researchers, are rare. Most of the folks we hire fall into the clinician-educator mold—that is, they see patients and teach, develop curriculums, and produce scholarship, often around education.
And therein lies the problem.
We’re running out of educational opportunities. The demand for clinical work long ago outstripped the supply of teaching opportunities, resulting in many academic HM groups hiring hospitalists for clinical jobs without residents to teach. Much like a deep-sea diver miles below the surface who finds his oxygen tank is running low, we now find ourselves looking up at an ocean of patients and realize that our educational lifeline has been severed. And the dyspnea is becoming ever more uncomfortable.
Increasingly, here is the sell for many academic HM groups: “Come work for us, do the same work you’d do at a community hospital, in a less-efficient system, without residents, for a lot less money.” And because you are primarily a clinician, you probably won’t have protected time to develop an academic interest and, therefore, you won’t get promoted beyond the “instructor” level because you haven’t contributed to advancing your field of medicine.
Even my mom wouldn’t apply for that job.
Failure Does Matter
The academic hospitalist job circa 2010 is heavy on the hospitalist and light on the academic. This is bad. And it matters to all of us, community hospitalists included. Without a strong frontline of academic hospitalists, we will not develop this field beyond “doctors who work in a hospital.”
There is a science to our field and it needs to be further developed. It can be seen in the comparative-effectiveness research, which tells us the best way to manage common diagnoses, the translational research (i.e. getting that new drug from the bench to the bedside), and the systems-based improvements (e.g. ensuring every stroke patient gets thrombolytics within three hours).
Take readmissions. There is a lot of dyspepsia swirling around this issue, and it’s clear that we have to reduce them. In fact, without such reductions, our hospitals (and likely us) won’t get paid. How will we do that? Maybe Project RED, maybe Project BOOST, maybe the best solution hasn’t been found yet. We don’t know, and we won’t until academic hospitalists have studied it.
Moreover, if we don’t present learners with talented, satisfied, respected hospitalist role models, I guarantee you that the quantity and quality of residents graduating to academic and community HM programs will suffer. Think back to those people who lured you into your specialty. Were you inspired to pediatrics, family medicine, or internal medicine because you saw those providers toiling away unsated by themselves on the wards?
Academic HM has a problem. And we are working toward the solution.
Six months ago, 90 academic hospitalist leaders convened in Washington, D.C., for the first Academic Hospital Medicine Leadership Summit. The goal was to develop a vision and action plan for the future of academic HM. Three work groups tackled the research, educational, and clinical issues facing our field. The recommendations of these sessions were then transferred to SHM’s Academic Committee and its subcommittees for operationalization.
A Pipeline of Quality
The education work group identified a need to establish hospitalists as the teachers of quality and safety for students and residents. This included increasing the number of hospitalists in such educational leadership positions as program and clerkship directors, where they can visibly lead the educational infrastructure. In response, SHM will unfurl the Quality and Safety Educators Academy this spring with the goal of providing academic hospitalists the construct to teach quality and safety.
Additionally, SHM’s Education Committee is developing a “plug and play” quality-improvement (QI) curriculum for use by any hospitalist educator. These initiatives will build on the success of the Academic Hospitalist Academy, developed two years ago to provide early career direction to academic hospitalists.
The education work group also prioritized the development of a strong pipeline of interest in HM starting at the medical-student level. This recommendation was turned over to the newly minted Pipeline Committee, which has been working feverishly to develop and expand medical student Hospital Medicine Interest Groups, the development of HM residency tracks, and an extension of our partnerships with other educational groups.
Answers to Future Questions
On the research front, goals were set to better develop and support clinician-researchers. This includes better delineating HM core research strengths, devising methods to partner with other medical subspecialties to perform quality and safety research in their areas of content expertise, and to develop a pipeline of future researchers.
To this last point, SHM awarded its first set of $50,000 research awards to two burgeoning researchers earlier this year.
SHM also is partnering with the Association of Specialty Professors to offer career development grants in geriatric medicine through the new Grants for Early Medical and Surgical Subspecialists’ Transitions to Aging Research (GEMSSTAR) program. And for the rest of us, SHM has devised free, Web-based forums for young researchers to present their work to their peers nationally.
Productivity, Efficiency, and Promotion
On the clinical side, the needs addressed include identification of benchmarks for academic clinical productivity, pathways for academic promotion, a methodology to garner more support for nonclinical work, and expectations to improve workflow and efficiency in academic medical centers.
These important tasks were assigned to a newly created Academic Practice and Promotions Task Force. This group is actively developing a quantitative survey to evaluate these needs and plans to publish a white paper of their findings, along with recommendations for hospitalist program directors, their department chairs and deans, and the hospitals that fund their programs. The findings will be presented at the next summit—at HM11 on May 10, 2011, in Dallas—as we continue to chart the course for success in academic hospital medicine.
Until then, I need to get my tank refilled. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
It’s fall. I know that because the leaves are turning, the nights are chillier, and my dogs have migrated back to the bed from a hot summer on the floor. Oh, and I again need to fill four positions for my hospitalist group.
A lot has changed in HM recruiting in the past few years. There was a feeding frenzy in the early part of the century, when I often joked that group leaders were so desperate for boots on the ground that my mom (who is not a physician, is retired, and struggles somewhat with the triple acid-base disorder) could have gotten a job as a hospitalist. I saw it in the number of reference calls for the residents in our program, their ever-increasing salary offers, and the breathless e-mails I’d receive from headhunters. Improbably, on occasion, their froth would even boil over to an offer for me, an academic. Now that’s desperation.
But things seem to be changing. The number of calls per resident is down and my inbox is filled with slightly less-winded recruiters. Maybe groups have finally matured and don’t need to hire; maybe the recession has induced an air of caution around growth; or maybe groups have uncovered the secret tonic to seeing more patients with fewer providers. Whatever it is, it seems that the job market has tightened ever so slightly.
And the job market has changed, especially on the academic side.
Work Harder for Less
In academics, we hire into jobs we describe as “clinician-something,” with the something reflecting what you do when you are not seeing patients, the thing that in most cases will get you promoted from instructor to assistant to associate to professor. Because HM is not a fellowship-driven field, primary researchers, called clinician-researchers, are rare. Most of the folks we hire fall into the clinician-educator mold—that is, they see patients and teach, develop curriculums, and produce scholarship, often around education.
And therein lies the problem.
We’re running out of educational opportunities. The demand for clinical work long ago outstripped the supply of teaching opportunities, resulting in many academic HM groups hiring hospitalists for clinical jobs without residents to teach. Much like a deep-sea diver miles below the surface who finds his oxygen tank is running low, we now find ourselves looking up at an ocean of patients and realize that our educational lifeline has been severed. And the dyspnea is becoming ever more uncomfortable.
Increasingly, here is the sell for many academic HM groups: “Come work for us, do the same work you’d do at a community hospital, in a less-efficient system, without residents, for a lot less money.” And because you are primarily a clinician, you probably won’t have protected time to develop an academic interest and, therefore, you won’t get promoted beyond the “instructor” level because you haven’t contributed to advancing your field of medicine.
Even my mom wouldn’t apply for that job.
Failure Does Matter
The academic hospitalist job circa 2010 is heavy on the hospitalist and light on the academic. This is bad. And it matters to all of us, community hospitalists included. Without a strong frontline of academic hospitalists, we will not develop this field beyond “doctors who work in a hospital.”
There is a science to our field and it needs to be further developed. It can be seen in the comparative-effectiveness research, which tells us the best way to manage common diagnoses, the translational research (i.e. getting that new drug from the bench to the bedside), and the systems-based improvements (e.g. ensuring every stroke patient gets thrombolytics within three hours).
Take readmissions. There is a lot of dyspepsia swirling around this issue, and it’s clear that we have to reduce them. In fact, without such reductions, our hospitals (and likely us) won’t get paid. How will we do that? Maybe Project RED, maybe Project BOOST, maybe the best solution hasn’t been found yet. We don’t know, and we won’t until academic hospitalists have studied it.
Moreover, if we don’t present learners with talented, satisfied, respected hospitalist role models, I guarantee you that the quantity and quality of residents graduating to academic and community HM programs will suffer. Think back to those people who lured you into your specialty. Were you inspired to pediatrics, family medicine, or internal medicine because you saw those providers toiling away unsated by themselves on the wards?
Academic HM has a problem. And we are working toward the solution.
Six months ago, 90 academic hospitalist leaders convened in Washington, D.C., for the first Academic Hospital Medicine Leadership Summit. The goal was to develop a vision and action plan for the future of academic HM. Three work groups tackled the research, educational, and clinical issues facing our field. The recommendations of these sessions were then transferred to SHM’s Academic Committee and its subcommittees for operationalization.
A Pipeline of Quality
The education work group identified a need to establish hospitalists as the teachers of quality and safety for students and residents. This included increasing the number of hospitalists in such educational leadership positions as program and clerkship directors, where they can visibly lead the educational infrastructure. In response, SHM will unfurl the Quality and Safety Educators Academy this spring with the goal of providing academic hospitalists the construct to teach quality and safety.
Additionally, SHM’s Education Committee is developing a “plug and play” quality-improvement (QI) curriculum for use by any hospitalist educator. These initiatives will build on the success of the Academic Hospitalist Academy, developed two years ago to provide early career direction to academic hospitalists.
The education work group also prioritized the development of a strong pipeline of interest in HM starting at the medical-student level. This recommendation was turned over to the newly minted Pipeline Committee, which has been working feverishly to develop and expand medical student Hospital Medicine Interest Groups, the development of HM residency tracks, and an extension of our partnerships with other educational groups.
Answers to Future Questions
On the research front, goals were set to better develop and support clinician-researchers. This includes better delineating HM core research strengths, devising methods to partner with other medical subspecialties to perform quality and safety research in their areas of content expertise, and to develop a pipeline of future researchers.
To this last point, SHM awarded its first set of $50,000 research awards to two burgeoning researchers earlier this year.
SHM also is partnering with the Association of Specialty Professors to offer career development grants in geriatric medicine through the new Grants for Early Medical and Surgical Subspecialists’ Transitions to Aging Research (GEMSSTAR) program. And for the rest of us, SHM has devised free, Web-based forums for young researchers to present their work to their peers nationally.
Productivity, Efficiency, and Promotion
On the clinical side, the needs addressed include identification of benchmarks for academic clinical productivity, pathways for academic promotion, a methodology to garner more support for nonclinical work, and expectations to improve workflow and efficiency in academic medical centers.
These important tasks were assigned to a newly created Academic Practice and Promotions Task Force. This group is actively developing a quantitative survey to evaluate these needs and plans to publish a white paper of their findings, along with recommendations for hospitalist program directors, their department chairs and deans, and the hospitals that fund their programs. The findings will be presented at the next summit—at HM11 on May 10, 2011, in Dallas—as we continue to chart the course for success in academic hospital medicine.
Until then, I need to get my tank refilled. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
It’s fall. I know that because the leaves are turning, the nights are chillier, and my dogs have migrated back to the bed from a hot summer on the floor. Oh, and I again need to fill four positions for my hospitalist group.
A lot has changed in HM recruiting in the past few years. There was a feeding frenzy in the early part of the century, when I often joked that group leaders were so desperate for boots on the ground that my mom (who is not a physician, is retired, and struggles somewhat with the triple acid-base disorder) could have gotten a job as a hospitalist. I saw it in the number of reference calls for the residents in our program, their ever-increasing salary offers, and the breathless e-mails I’d receive from headhunters. Improbably, on occasion, their froth would even boil over to an offer for me, an academic. Now that’s desperation.
But things seem to be changing. The number of calls per resident is down and my inbox is filled with slightly less-winded recruiters. Maybe groups have finally matured and don’t need to hire; maybe the recession has induced an air of caution around growth; or maybe groups have uncovered the secret tonic to seeing more patients with fewer providers. Whatever it is, it seems that the job market has tightened ever so slightly.
And the job market has changed, especially on the academic side.
Work Harder for Less
In academics, we hire into jobs we describe as “clinician-something,” with the something reflecting what you do when you are not seeing patients, the thing that in most cases will get you promoted from instructor to assistant to associate to professor. Because HM is not a fellowship-driven field, primary researchers, called clinician-researchers, are rare. Most of the folks we hire fall into the clinician-educator mold—that is, they see patients and teach, develop curriculums, and produce scholarship, often around education.
And therein lies the problem.
We’re running out of educational opportunities. The demand for clinical work long ago outstripped the supply of teaching opportunities, resulting in many academic HM groups hiring hospitalists for clinical jobs without residents to teach. Much like a deep-sea diver miles below the surface who finds his oxygen tank is running low, we now find ourselves looking up at an ocean of patients and realize that our educational lifeline has been severed. And the dyspnea is becoming ever more uncomfortable.
Increasingly, here is the sell for many academic HM groups: “Come work for us, do the same work you’d do at a community hospital, in a less-efficient system, without residents, for a lot less money.” And because you are primarily a clinician, you probably won’t have protected time to develop an academic interest and, therefore, you won’t get promoted beyond the “instructor” level because you haven’t contributed to advancing your field of medicine.
Even my mom wouldn’t apply for that job.
Failure Does Matter
The academic hospitalist job circa 2010 is heavy on the hospitalist and light on the academic. This is bad. And it matters to all of us, community hospitalists included. Without a strong frontline of academic hospitalists, we will not develop this field beyond “doctors who work in a hospital.”
There is a science to our field and it needs to be further developed. It can be seen in the comparative-effectiveness research, which tells us the best way to manage common diagnoses, the translational research (i.e. getting that new drug from the bench to the bedside), and the systems-based improvements (e.g. ensuring every stroke patient gets thrombolytics within three hours).
Take readmissions. There is a lot of dyspepsia swirling around this issue, and it’s clear that we have to reduce them. In fact, without such reductions, our hospitals (and likely us) won’t get paid. How will we do that? Maybe Project RED, maybe Project BOOST, maybe the best solution hasn’t been found yet. We don’t know, and we won’t until academic hospitalists have studied it.
Moreover, if we don’t present learners with talented, satisfied, respected hospitalist role models, I guarantee you that the quantity and quality of residents graduating to academic and community HM programs will suffer. Think back to those people who lured you into your specialty. Were you inspired to pediatrics, family medicine, or internal medicine because you saw those providers toiling away unsated by themselves on the wards?
Academic HM has a problem. And we are working toward the solution.
Six months ago, 90 academic hospitalist leaders convened in Washington, D.C., for the first Academic Hospital Medicine Leadership Summit. The goal was to develop a vision and action plan for the future of academic HM. Three work groups tackled the research, educational, and clinical issues facing our field. The recommendations of these sessions were then transferred to SHM’s Academic Committee and its subcommittees for operationalization.
A Pipeline of Quality
The education work group identified a need to establish hospitalists as the teachers of quality and safety for students and residents. This included increasing the number of hospitalists in such educational leadership positions as program and clerkship directors, where they can visibly lead the educational infrastructure. In response, SHM will unfurl the Quality and Safety Educators Academy this spring with the goal of providing academic hospitalists the construct to teach quality and safety.
Additionally, SHM’s Education Committee is developing a “plug and play” quality-improvement (QI) curriculum for use by any hospitalist educator. These initiatives will build on the success of the Academic Hospitalist Academy, developed two years ago to provide early career direction to academic hospitalists.
The education work group also prioritized the development of a strong pipeline of interest in HM starting at the medical-student level. This recommendation was turned over to the newly minted Pipeline Committee, which has been working feverishly to develop and expand medical student Hospital Medicine Interest Groups, the development of HM residency tracks, and an extension of our partnerships with other educational groups.
Answers to Future Questions
On the research front, goals were set to better develop and support clinician-researchers. This includes better delineating HM core research strengths, devising methods to partner with other medical subspecialties to perform quality and safety research in their areas of content expertise, and to develop a pipeline of future researchers.
To this last point, SHM awarded its first set of $50,000 research awards to two burgeoning researchers earlier this year.
SHM also is partnering with the Association of Specialty Professors to offer career development grants in geriatric medicine through the new Grants for Early Medical and Surgical Subspecialists’ Transitions to Aging Research (GEMSSTAR) program. And for the rest of us, SHM has devised free, Web-based forums for young researchers to present their work to their peers nationally.
Productivity, Efficiency, and Promotion
On the clinical side, the needs addressed include identification of benchmarks for academic clinical productivity, pathways for academic promotion, a methodology to garner more support for nonclinical work, and expectations to improve workflow and efficiency in academic medical centers.
These important tasks were assigned to a newly created Academic Practice and Promotions Task Force. This group is actively developing a quantitative survey to evaluate these needs and plans to publish a white paper of their findings, along with recommendations for hospitalist program directors, their department chairs and deans, and the hospitals that fund their programs. The findings will be presented at the next summit—at HM11 on May 10, 2011, in Dallas—as we continue to chart the course for success in academic hospital medicine.
Until then, I need to get my tank refilled. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
28,999 and Me
How many people have to die before you’ll pay attention? Like many of you, I read the article but it didn’t really stick. Rather, I filed it in the “interesting tidbits” folder on my brain’s hard drive. Somehow 29,000 people with cancer just didn’t register as a big number.
Until I thought I could be one of them.
The Number
I was harried, running late for a meeting, questioning my decision to try to shoehorn a PCP appointment into my lunch break. Then again, this was a routine follow-up of some labs and I, of course, am the picture of health. Well, I am if you exclude my LDL. It turns out that on a check 12 months earlier, my LDL was found to be running a few heart attacks higher than normal. I took this as a sign, combined with my ballooning waist, middle-ish age, and nagging wife, that I needed to do something.
Still, I wasn’t ready for “something” to include an anticholesterol medication. Instead, I chose the masochistic route and hit the treadmill. And the bike. And a little less of the dinner plate. As a result, I had lost 30 pounds, a handful of pant sizes and, while I wasn’t exactly “in shape,” I did find myself shaped a little less like the Michelin Man.
Triumphantly, I was returning to vanquish my tormentor—the PCP who foolhardily recommended I start a medication.
Sitting in the office awaiting the news of my post-weight-loss cholesterol, my grin was wide and smug—and apparently still overflowing with LDL. I was devastated. 259? I lose weight and my LDL actually goes up!?! I could feel the foam cells in my coronary plaques twitch with delight as they mockingly gorged on chylomicrons.
Undeterred, I inquired what my options were, secretly hoping the answer would be more red wine. Emboldened by my supersaturated serum, my PCP declared it was time for a statin. Alternatively, he noted that I could get a CT angiogram of my coronaries and, if they were clean, I potentially could bypass drug therapy. Thoughts of avoided myalgias happily flittered across my mind until they stumbled onto the number 29,000. It was then that I recalled the recent Archives of Internal Medicine paper.1
The Study
Using risk models based on the known biological effects of radiation, researchers estimated that approximately 29,000 people would develop cancer from the radiation associated with CT scans in 2007 alone. To arrive at this number, the authors used data showing that 1.5% to 2% of all U.S. cancers could be traced to the radiation from CT scans.
Not surprisingly, the most commonly utilized CT scans—namely, abdominal (14,000 a year), chest (4,100 a year), and head (4,000 a year)—accounted for the most morbidity. However, CT angiography, with its super-high dose of radiation, was projected to contribute 2,700 cancers a year. Apparently, my PCP didn’t read this article.
In terms of types of malignancy, lung cancer leads the list with 6,200 projected CT-induced cancers per year, followed by colon cancer (3,500 a year) and leukemia (2,800 a year).
The Names
If the numbers from this study hold, then about 1 in every 2,000 CT scans results in a new cancer. That would mean that I’ve dished out several cancers during my practice. In fact, I’ve ordered many thousand CT scans over my career—give or take a cancer. So my pen has, statistically, caused approximately three cancers.
I wondered which three patients it was. Was it Mr. Reynolds, who would’ve very likely died had we not diagnosed his post-operative abdominal abscess? Perhaps it was Mr. Jenson, who surely would have fared poorly if his pulmonary embolism had not been diagnosed and treated. Maybe it was Mrs. Hernandez, who wouldn’t have received thrombolytics for her stroke without a head CT.
Yes, I might have played a role in causing cancer in these three patients, but I did so knowing that I also saved, or at least improved, their lives. Most patients would accept that calculus.
But what if it were a different three? What if my cancer was that head CT I ordered for Mr. Davidson’s confusion, even though I know that head scans are rarely helpful in the evaluation of delirium? Perhaps my cancer-causer was that abdominal CT scan for Mrs. Ramirez’s chronic pain, which was clearly referable to her irritable bowel syndrome. Maybe it will be that CT scan I ordered last week because the patient insisted it be done, even though I strongly suspected, correctly, that it wouldn’t alter my management.
Which three would it be?
The Questions
This triggered more questions. How many of the 70 million-plus CT scans we order every year really are necessary? How many could be avoided by a robust physical examination, crisper clinical reasoning, or an alternate test? Do our patients really know the risk of these “innocuous” tests? Do we?
And, more personally, what if my PCP was still sitting on two? Would I be his number three?
Moving forward, I vow to remember 29,000. It will remain in the forefront of my mind, constantly badgering me about the next CT scan I order. To be sure, I will continue to order CTs—a lot of CTs. However, I will do so through the prism of the following query. If a patient developed a cancer from the CT scan I was about to order, could I sincerely look them in the eye and tell them I would do the test again?
And I’m agitated by one final question. How is that it took my own carcinogenic brush with CT scans for me to realize the gravity of 29,000? It’s not that 29,000 is not a big number. In fact, it’s precisely because it is a big number that we miss its importance. It’s too easy to hide behind the anonymity of the number. Because in the end, numbers don’t have names until the name is yours. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
Reference
- Berrington de González A, Mahesh M, Kim KP, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009;169(22):2071-2077.
How many people have to die before you’ll pay attention? Like many of you, I read the article but it didn’t really stick. Rather, I filed it in the “interesting tidbits” folder on my brain’s hard drive. Somehow 29,000 people with cancer just didn’t register as a big number.
Until I thought I could be one of them.
The Number
I was harried, running late for a meeting, questioning my decision to try to shoehorn a PCP appointment into my lunch break. Then again, this was a routine follow-up of some labs and I, of course, am the picture of health. Well, I am if you exclude my LDL. It turns out that on a check 12 months earlier, my LDL was found to be running a few heart attacks higher than normal. I took this as a sign, combined with my ballooning waist, middle-ish age, and nagging wife, that I needed to do something.
Still, I wasn’t ready for “something” to include an anticholesterol medication. Instead, I chose the masochistic route and hit the treadmill. And the bike. And a little less of the dinner plate. As a result, I had lost 30 pounds, a handful of pant sizes and, while I wasn’t exactly “in shape,” I did find myself shaped a little less like the Michelin Man.
Triumphantly, I was returning to vanquish my tormentor—the PCP who foolhardily recommended I start a medication.
Sitting in the office awaiting the news of my post-weight-loss cholesterol, my grin was wide and smug—and apparently still overflowing with LDL. I was devastated. 259? I lose weight and my LDL actually goes up!?! I could feel the foam cells in my coronary plaques twitch with delight as they mockingly gorged on chylomicrons.
Undeterred, I inquired what my options were, secretly hoping the answer would be more red wine. Emboldened by my supersaturated serum, my PCP declared it was time for a statin. Alternatively, he noted that I could get a CT angiogram of my coronaries and, if they were clean, I potentially could bypass drug therapy. Thoughts of avoided myalgias happily flittered across my mind until they stumbled onto the number 29,000. It was then that I recalled the recent Archives of Internal Medicine paper.1
The Study
Using risk models based on the known biological effects of radiation, researchers estimated that approximately 29,000 people would develop cancer from the radiation associated with CT scans in 2007 alone. To arrive at this number, the authors used data showing that 1.5% to 2% of all U.S. cancers could be traced to the radiation from CT scans.
Not surprisingly, the most commonly utilized CT scans—namely, abdominal (14,000 a year), chest (4,100 a year), and head (4,000 a year)—accounted for the most morbidity. However, CT angiography, with its super-high dose of radiation, was projected to contribute 2,700 cancers a year. Apparently, my PCP didn’t read this article.
In terms of types of malignancy, lung cancer leads the list with 6,200 projected CT-induced cancers per year, followed by colon cancer (3,500 a year) and leukemia (2,800 a year).
The Names
If the numbers from this study hold, then about 1 in every 2,000 CT scans results in a new cancer. That would mean that I’ve dished out several cancers during my practice. In fact, I’ve ordered many thousand CT scans over my career—give or take a cancer. So my pen has, statistically, caused approximately three cancers.
I wondered which three patients it was. Was it Mr. Reynolds, who would’ve very likely died had we not diagnosed his post-operative abdominal abscess? Perhaps it was Mr. Jenson, who surely would have fared poorly if his pulmonary embolism had not been diagnosed and treated. Maybe it was Mrs. Hernandez, who wouldn’t have received thrombolytics for her stroke without a head CT.
Yes, I might have played a role in causing cancer in these three patients, but I did so knowing that I also saved, or at least improved, their lives. Most patients would accept that calculus.
But what if it were a different three? What if my cancer was that head CT I ordered for Mr. Davidson’s confusion, even though I know that head scans are rarely helpful in the evaluation of delirium? Perhaps my cancer-causer was that abdominal CT scan for Mrs. Ramirez’s chronic pain, which was clearly referable to her irritable bowel syndrome. Maybe it will be that CT scan I ordered last week because the patient insisted it be done, even though I strongly suspected, correctly, that it wouldn’t alter my management.
Which three would it be?
The Questions
This triggered more questions. How many of the 70 million-plus CT scans we order every year really are necessary? How many could be avoided by a robust physical examination, crisper clinical reasoning, or an alternate test? Do our patients really know the risk of these “innocuous” tests? Do we?
And, more personally, what if my PCP was still sitting on two? Would I be his number three?
Moving forward, I vow to remember 29,000. It will remain in the forefront of my mind, constantly badgering me about the next CT scan I order. To be sure, I will continue to order CTs—a lot of CTs. However, I will do so through the prism of the following query. If a patient developed a cancer from the CT scan I was about to order, could I sincerely look them in the eye and tell them I would do the test again?
And I’m agitated by one final question. How is that it took my own carcinogenic brush with CT scans for me to realize the gravity of 29,000? It’s not that 29,000 is not a big number. In fact, it’s precisely because it is a big number that we miss its importance. It’s too easy to hide behind the anonymity of the number. Because in the end, numbers don’t have names until the name is yours. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
Reference
- Berrington de González A, Mahesh M, Kim KP, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009;169(22):2071-2077.
How many people have to die before you’ll pay attention? Like many of you, I read the article but it didn’t really stick. Rather, I filed it in the “interesting tidbits” folder on my brain’s hard drive. Somehow 29,000 people with cancer just didn’t register as a big number.
Until I thought I could be one of them.
The Number
I was harried, running late for a meeting, questioning my decision to try to shoehorn a PCP appointment into my lunch break. Then again, this was a routine follow-up of some labs and I, of course, am the picture of health. Well, I am if you exclude my LDL. It turns out that on a check 12 months earlier, my LDL was found to be running a few heart attacks higher than normal. I took this as a sign, combined with my ballooning waist, middle-ish age, and nagging wife, that I needed to do something.
Still, I wasn’t ready for “something” to include an anticholesterol medication. Instead, I chose the masochistic route and hit the treadmill. And the bike. And a little less of the dinner plate. As a result, I had lost 30 pounds, a handful of pant sizes and, while I wasn’t exactly “in shape,” I did find myself shaped a little less like the Michelin Man.
Triumphantly, I was returning to vanquish my tormentor—the PCP who foolhardily recommended I start a medication.
Sitting in the office awaiting the news of my post-weight-loss cholesterol, my grin was wide and smug—and apparently still overflowing with LDL. I was devastated. 259? I lose weight and my LDL actually goes up!?! I could feel the foam cells in my coronary plaques twitch with delight as they mockingly gorged on chylomicrons.
Undeterred, I inquired what my options were, secretly hoping the answer would be more red wine. Emboldened by my supersaturated serum, my PCP declared it was time for a statin. Alternatively, he noted that I could get a CT angiogram of my coronaries and, if they were clean, I potentially could bypass drug therapy. Thoughts of avoided myalgias happily flittered across my mind until they stumbled onto the number 29,000. It was then that I recalled the recent Archives of Internal Medicine paper.1
The Study
Using risk models based on the known biological effects of radiation, researchers estimated that approximately 29,000 people would develop cancer from the radiation associated with CT scans in 2007 alone. To arrive at this number, the authors used data showing that 1.5% to 2% of all U.S. cancers could be traced to the radiation from CT scans.
Not surprisingly, the most commonly utilized CT scans—namely, abdominal (14,000 a year), chest (4,100 a year), and head (4,000 a year)—accounted for the most morbidity. However, CT angiography, with its super-high dose of radiation, was projected to contribute 2,700 cancers a year. Apparently, my PCP didn’t read this article.
In terms of types of malignancy, lung cancer leads the list with 6,200 projected CT-induced cancers per year, followed by colon cancer (3,500 a year) and leukemia (2,800 a year).
The Names
If the numbers from this study hold, then about 1 in every 2,000 CT scans results in a new cancer. That would mean that I’ve dished out several cancers during my practice. In fact, I’ve ordered many thousand CT scans over my career—give or take a cancer. So my pen has, statistically, caused approximately three cancers.
I wondered which three patients it was. Was it Mr. Reynolds, who would’ve very likely died had we not diagnosed his post-operative abdominal abscess? Perhaps it was Mr. Jenson, who surely would have fared poorly if his pulmonary embolism had not been diagnosed and treated. Maybe it was Mrs. Hernandez, who wouldn’t have received thrombolytics for her stroke without a head CT.
Yes, I might have played a role in causing cancer in these three patients, but I did so knowing that I also saved, or at least improved, their lives. Most patients would accept that calculus.
But what if it were a different three? What if my cancer was that head CT I ordered for Mr. Davidson’s confusion, even though I know that head scans are rarely helpful in the evaluation of delirium? Perhaps my cancer-causer was that abdominal CT scan for Mrs. Ramirez’s chronic pain, which was clearly referable to her irritable bowel syndrome. Maybe it will be that CT scan I ordered last week because the patient insisted it be done, even though I strongly suspected, correctly, that it wouldn’t alter my management.
Which three would it be?
The Questions
This triggered more questions. How many of the 70 million-plus CT scans we order every year really are necessary? How many could be avoided by a robust physical examination, crisper clinical reasoning, or an alternate test? Do our patients really know the risk of these “innocuous” tests? Do we?
And, more personally, what if my PCP was still sitting on two? Would I be his number three?
Moving forward, I vow to remember 29,000. It will remain in the forefront of my mind, constantly badgering me about the next CT scan I order. To be sure, I will continue to order CTs—a lot of CTs. However, I will do so through the prism of the following query. If a patient developed a cancer from the CT scan I was about to order, could I sincerely look them in the eye and tell them I would do the test again?
And I’m agitated by one final question. How is that it took my own carcinogenic brush with CT scans for me to realize the gravity of 29,000? It’s not that 29,000 is not a big number. In fact, it’s precisely because it is a big number that we miss its importance. It’s too easy to hide behind the anonymity of the number. Because in the end, numbers don’t have names until the name is yours. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
Reference
- Berrington de González A, Mahesh M, Kim KP, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009;169(22):2071-2077.
The Devil & the Details
Act I: The Negotiation
(A barren academic office, dimly lit, the pall of difficult negotiations afloat, backlit like dust in the air. Seated, under a strangely intense incandescent bulb, a man, who looks eerily like a good-looking version of me, sits uncomfortably adjusting himself in his seat. His eyes constrict on his counterpart, a miserly sort peering out from behind wire-rim glasses and a shock of hair improbably combed over from ear to ear. The tension crests.)
GOOD-LOOKING ME
(Voice cracking)
I’ve come to ask for a raise for our hospitalist group.
MISER
(Adjusts his clip-on tie)
We just gave you a raise in 2004.
GOOD-LOOKING ME
(Smiles uncomfortably)
That was very gracious, sir, but I think the numbers support another.
MISER
(Incredulous look at his watch)
But your work RVUs are thousands below what I’d like to see.
GOOD-LOOKING ME
(Dabs bead of sweat away from chiseled chin)
That’s because you’ve set your benchmark thousands above a reasonable number.
MISER
(Voice flitting with child-like condescension)
But those are the numbers my finance guy gave me. It’s the benchmark.
(Blackout and end of Act I.)
Mutual Agreement
Tony Award-winning stuff for sure—and based on a true story! In fact, this scene no doubt plays out annually for those of you unfortunate enough to have to negotiate with hospital executives for programmatic support. To be fair, hospital administrators deserve to know that they are getting what they pay for. Thus, the concepts of a benchmark are reasonable. The problem lies in setting mutually-agreed-upon standards.
Act II: Disbelief and Confusion
GOOD-LOOKING ME
(Unsteadily hands document to Miser)
Sir, I’ve highlighted the national benchmarks for you to see. Column four of this 2007-2008 SHM survey clearly shows that the average academic hospitalist should make $168,800 and achieve 2,813 work RVUs. We achieve the latter benchmark but are severely underpaid.
MISER
(Produces a folded cocktail napkin from his shirt pocket)
But look at this: My executive-friends-at-other-medical-centers-who-overwork-and-underpay-their-hospitalists benchmark shows that you should be well over 4,500 work RVUs. And besides, the SHM numbers are skewed; it’s a survey of hospitalists done by a group that represents hospitalists. I don’t believe them.
GOOD-LOOKING ME
(Eyes averted, adopts a tone of trepidation)
But sir, with all due respect, don’t your numbers reflect a survey of hospital administrators who might have a bias toward more expected productivity? Which benchmark should we believe?
(Blackout and end of Act II.)
A New HM Benchmark Arises
It’s all about the benchmark you choose to believe. For years, the best source of data regarding hospitalist compensation and productivity was that published every other year by SHM. It is a fair, but unfounded, concern that these data might tilt toward the benefit of hospitalists. Likewise, the hospital administrator I work most closely with (who, for the record, reads this publication and IS NOT miserly, has a FULL HEAD of hair, and is, for innumerable reasons, a TRULY GREAT man) will produce benchmarks from organizations like the Association of American Medical Colleges (AAMC) or the University HealthSystems Consortium (UHC), all of which show surprisingly disparate numbers dripping with a similar tilt toward the medical center.
Thus, the importance of the 2010 SHM/MGMA report. The Medical Group Management Association (MGMA) consists of administrators and leaders of medical group practices. Since 1926, they’ve been providing accurate, independent data on physician practice metrics. For most hospital administrators, it is the benchmark. The problem is that in the past, MGMA has struggled to identify hospitalists; the MGMA data were always underpowered and, therefore, suspect.
Enter SHM and its large database of HM groups. What has resulted in the new survey rivals those old commercials in which a person walking with a piece of chocolate slams into another with a jar of peanut butter, resulting in the creation of the Reese’s Peanut Butter Cup (apologies to those readers under the age of 35).
Act III: No Raise; Children Go Hungry
GOOD-LOOKING ME
(Unsheathing haloed document from his portfolio)
Perhaps we could agree to use these new SHM/MGMA numbers as our benchmark. It includes data from more than 440 HM groups and 4,200 hospitalists. And it appears to be fair and balanced.
MISER
(Eyes alight, peering through a shroud of compromise)
MGMA, huh? Let’s take a look. Hmmm. Well. But wait—this says the average hospitalist makes $215,000! That’s outrageous.
GOOD-LOOKING ME
(Smugly retorts)
Yes, sir, we are severely underpaid.
MISER
(Reading; a weasel-like countenance overtakes his face)
Let me take a closer look at this. Aha! Here it is. You see, this only included community hospitalist practices. You will be getting no raise!
(Blackout and end of Act III.)
A Cautionary Tale
Alas, the miser is right. It’s not always what the data say but also what they don’t say.
The one snag with the new data is that it only included a handful of academic HM groups (only 1% of respondents). In fact, the survey actively instructed academic HM practices to not complete the survey. Rather, we academic types were instructed to await the MGMA survey of academic practices completed every fall to be reported early next year.
This is emblematic of the need to dig deep when interpreting these data. As tempting as it is to use a sound bite or two of these data to your advantage, the truth lies in the details. It’s easy to say that all hospitalists should make $215,000, see 2,229 encounters, and achieve 4,107 wRVUs annually.
However, just as there is no average hospitalist, there are no average numbers. There are just too many variables (e.g., practice ownership, geography, group size, night coverage, staffing model, compensation structure) to say definitively what an individual hospitalist should look like or achieve. Rather, these numbers should be used as a guide, adapted to each individual situation.
Act IV: See You This Spring
(Standing, Good-Looking Me shakes his foe’s shriveled claw of a hand while looking him intensely in the eye—a look that says, “I’ll see you this spring.” In his rival’s eyes, the Miser sees his future—a future that involves another meeting, more practice-appropriate data, and a dusting off of his checkbook.)
(Blackout and end of Act IV.) TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
Act I: The Negotiation
(A barren academic office, dimly lit, the pall of difficult negotiations afloat, backlit like dust in the air. Seated, under a strangely intense incandescent bulb, a man, who looks eerily like a good-looking version of me, sits uncomfortably adjusting himself in his seat. His eyes constrict on his counterpart, a miserly sort peering out from behind wire-rim glasses and a shock of hair improbably combed over from ear to ear. The tension crests.)
GOOD-LOOKING ME
(Voice cracking)
I’ve come to ask for a raise for our hospitalist group.
MISER
(Adjusts his clip-on tie)
We just gave you a raise in 2004.
GOOD-LOOKING ME
(Smiles uncomfortably)
That was very gracious, sir, but I think the numbers support another.
MISER
(Incredulous look at his watch)
But your work RVUs are thousands below what I’d like to see.
GOOD-LOOKING ME
(Dabs bead of sweat away from chiseled chin)
That’s because you’ve set your benchmark thousands above a reasonable number.
MISER
(Voice flitting with child-like condescension)
But those are the numbers my finance guy gave me. It’s the benchmark.
(Blackout and end of Act I.)
Mutual Agreement
Tony Award-winning stuff for sure—and based on a true story! In fact, this scene no doubt plays out annually for those of you unfortunate enough to have to negotiate with hospital executives for programmatic support. To be fair, hospital administrators deserve to know that they are getting what they pay for. Thus, the concepts of a benchmark are reasonable. The problem lies in setting mutually-agreed-upon standards.
Act II: Disbelief and Confusion
GOOD-LOOKING ME
(Unsteadily hands document to Miser)
Sir, I’ve highlighted the national benchmarks for you to see. Column four of this 2007-2008 SHM survey clearly shows that the average academic hospitalist should make $168,800 and achieve 2,813 work RVUs. We achieve the latter benchmark but are severely underpaid.
MISER
(Produces a folded cocktail napkin from his shirt pocket)
But look at this: My executive-friends-at-other-medical-centers-who-overwork-and-underpay-their-hospitalists benchmark shows that you should be well over 4,500 work RVUs. And besides, the SHM numbers are skewed; it’s a survey of hospitalists done by a group that represents hospitalists. I don’t believe them.
GOOD-LOOKING ME
(Eyes averted, adopts a tone of trepidation)
But sir, with all due respect, don’t your numbers reflect a survey of hospital administrators who might have a bias toward more expected productivity? Which benchmark should we believe?
(Blackout and end of Act II.)
A New HM Benchmark Arises
It’s all about the benchmark you choose to believe. For years, the best source of data regarding hospitalist compensation and productivity was that published every other year by SHM. It is a fair, but unfounded, concern that these data might tilt toward the benefit of hospitalists. Likewise, the hospital administrator I work most closely with (who, for the record, reads this publication and IS NOT miserly, has a FULL HEAD of hair, and is, for innumerable reasons, a TRULY GREAT man) will produce benchmarks from organizations like the Association of American Medical Colleges (AAMC) or the University HealthSystems Consortium (UHC), all of which show surprisingly disparate numbers dripping with a similar tilt toward the medical center.
Thus, the importance of the 2010 SHM/MGMA report. The Medical Group Management Association (MGMA) consists of administrators and leaders of medical group practices. Since 1926, they’ve been providing accurate, independent data on physician practice metrics. For most hospital administrators, it is the benchmark. The problem is that in the past, MGMA has struggled to identify hospitalists; the MGMA data were always underpowered and, therefore, suspect.
Enter SHM and its large database of HM groups. What has resulted in the new survey rivals those old commercials in which a person walking with a piece of chocolate slams into another with a jar of peanut butter, resulting in the creation of the Reese’s Peanut Butter Cup (apologies to those readers under the age of 35).
Act III: No Raise; Children Go Hungry
GOOD-LOOKING ME
(Unsheathing haloed document from his portfolio)
Perhaps we could agree to use these new SHM/MGMA numbers as our benchmark. It includes data from more than 440 HM groups and 4,200 hospitalists. And it appears to be fair and balanced.
MISER
(Eyes alight, peering through a shroud of compromise)
MGMA, huh? Let’s take a look. Hmmm. Well. But wait—this says the average hospitalist makes $215,000! That’s outrageous.
GOOD-LOOKING ME
(Smugly retorts)
Yes, sir, we are severely underpaid.
MISER
(Reading; a weasel-like countenance overtakes his face)
Let me take a closer look at this. Aha! Here it is. You see, this only included community hospitalist practices. You will be getting no raise!
(Blackout and end of Act III.)
A Cautionary Tale
Alas, the miser is right. It’s not always what the data say but also what they don’t say.
The one snag with the new data is that it only included a handful of academic HM groups (only 1% of respondents). In fact, the survey actively instructed academic HM practices to not complete the survey. Rather, we academic types were instructed to await the MGMA survey of academic practices completed every fall to be reported early next year.
This is emblematic of the need to dig deep when interpreting these data. As tempting as it is to use a sound bite or two of these data to your advantage, the truth lies in the details. It’s easy to say that all hospitalists should make $215,000, see 2,229 encounters, and achieve 4,107 wRVUs annually.
However, just as there is no average hospitalist, there are no average numbers. There are just too many variables (e.g., practice ownership, geography, group size, night coverage, staffing model, compensation structure) to say definitively what an individual hospitalist should look like or achieve. Rather, these numbers should be used as a guide, adapted to each individual situation.
Act IV: See You This Spring
(Standing, Good-Looking Me shakes his foe’s shriveled claw of a hand while looking him intensely in the eye—a look that says, “I’ll see you this spring.” In his rival’s eyes, the Miser sees his future—a future that involves another meeting, more practice-appropriate data, and a dusting off of his checkbook.)
(Blackout and end of Act IV.) TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
Act I: The Negotiation
(A barren academic office, dimly lit, the pall of difficult negotiations afloat, backlit like dust in the air. Seated, under a strangely intense incandescent bulb, a man, who looks eerily like a good-looking version of me, sits uncomfortably adjusting himself in his seat. His eyes constrict on his counterpart, a miserly sort peering out from behind wire-rim glasses and a shock of hair improbably combed over from ear to ear. The tension crests.)
GOOD-LOOKING ME
(Voice cracking)
I’ve come to ask for a raise for our hospitalist group.
MISER
(Adjusts his clip-on tie)
We just gave you a raise in 2004.
GOOD-LOOKING ME
(Smiles uncomfortably)
That was very gracious, sir, but I think the numbers support another.
MISER
(Incredulous look at his watch)
But your work RVUs are thousands below what I’d like to see.
GOOD-LOOKING ME
(Dabs bead of sweat away from chiseled chin)
That’s because you’ve set your benchmark thousands above a reasonable number.
MISER
(Voice flitting with child-like condescension)
But those are the numbers my finance guy gave me. It’s the benchmark.
(Blackout and end of Act I.)
Mutual Agreement
Tony Award-winning stuff for sure—and based on a true story! In fact, this scene no doubt plays out annually for those of you unfortunate enough to have to negotiate with hospital executives for programmatic support. To be fair, hospital administrators deserve to know that they are getting what they pay for. Thus, the concepts of a benchmark are reasonable. The problem lies in setting mutually-agreed-upon standards.
Act II: Disbelief and Confusion
GOOD-LOOKING ME
(Unsteadily hands document to Miser)
Sir, I’ve highlighted the national benchmarks for you to see. Column four of this 2007-2008 SHM survey clearly shows that the average academic hospitalist should make $168,800 and achieve 2,813 work RVUs. We achieve the latter benchmark but are severely underpaid.
MISER
(Produces a folded cocktail napkin from his shirt pocket)
But look at this: My executive-friends-at-other-medical-centers-who-overwork-and-underpay-their-hospitalists benchmark shows that you should be well over 4,500 work RVUs. And besides, the SHM numbers are skewed; it’s a survey of hospitalists done by a group that represents hospitalists. I don’t believe them.
GOOD-LOOKING ME
(Eyes averted, adopts a tone of trepidation)
But sir, with all due respect, don’t your numbers reflect a survey of hospital administrators who might have a bias toward more expected productivity? Which benchmark should we believe?
(Blackout and end of Act II.)
A New HM Benchmark Arises
It’s all about the benchmark you choose to believe. For years, the best source of data regarding hospitalist compensation and productivity was that published every other year by SHM. It is a fair, but unfounded, concern that these data might tilt toward the benefit of hospitalists. Likewise, the hospital administrator I work most closely with (who, for the record, reads this publication and IS NOT miserly, has a FULL HEAD of hair, and is, for innumerable reasons, a TRULY GREAT man) will produce benchmarks from organizations like the Association of American Medical Colleges (AAMC) or the University HealthSystems Consortium (UHC), all of which show surprisingly disparate numbers dripping with a similar tilt toward the medical center.
Thus, the importance of the 2010 SHM/MGMA report. The Medical Group Management Association (MGMA) consists of administrators and leaders of medical group practices. Since 1926, they’ve been providing accurate, independent data on physician practice metrics. For most hospital administrators, it is the benchmark. The problem is that in the past, MGMA has struggled to identify hospitalists; the MGMA data were always underpowered and, therefore, suspect.
Enter SHM and its large database of HM groups. What has resulted in the new survey rivals those old commercials in which a person walking with a piece of chocolate slams into another with a jar of peanut butter, resulting in the creation of the Reese’s Peanut Butter Cup (apologies to those readers under the age of 35).
Act III: No Raise; Children Go Hungry
GOOD-LOOKING ME
(Unsheathing haloed document from his portfolio)
Perhaps we could agree to use these new SHM/MGMA numbers as our benchmark. It includes data from more than 440 HM groups and 4,200 hospitalists. And it appears to be fair and balanced.
MISER
(Eyes alight, peering through a shroud of compromise)
MGMA, huh? Let’s take a look. Hmmm. Well. But wait—this says the average hospitalist makes $215,000! That’s outrageous.
GOOD-LOOKING ME
(Smugly retorts)
Yes, sir, we are severely underpaid.
MISER
(Reading; a weasel-like countenance overtakes his face)
Let me take a closer look at this. Aha! Here it is. You see, this only included community hospitalist practices. You will be getting no raise!
(Blackout and end of Act III.)
A Cautionary Tale
Alas, the miser is right. It’s not always what the data say but also what they don’t say.
The one snag with the new data is that it only included a handful of academic HM groups (only 1% of respondents). In fact, the survey actively instructed academic HM practices to not complete the survey. Rather, we academic types were instructed to await the MGMA survey of academic practices completed every fall to be reported early next year.
This is emblematic of the need to dig deep when interpreting these data. As tempting as it is to use a sound bite or two of these data to your advantage, the truth lies in the details. It’s easy to say that all hospitalists should make $215,000, see 2,229 encounters, and achieve 4,107 wRVUs annually.
However, just as there is no average hospitalist, there are no average numbers. There are just too many variables (e.g., practice ownership, geography, group size, night coverage, staffing model, compensation structure) to say definitively what an individual hospitalist should look like or achieve. Rather, these numbers should be used as a guide, adapted to each individual situation.
Act IV: See You This Spring
(Standing, Good-Looking Me shakes his foe’s shriveled claw of a hand while looking him intensely in the eye—a look that says, “I’ll see you this spring.” In his rival’s eyes, the Miser sees his future—a future that involves another meeting, more practice-appropriate data, and a dusting off of his checkbook.)
(Blackout and end of Act IV.) TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
Rise of the Napturnist
The best sleep I ever got was in the winter of 1996. I remember it vividly. It was effortless, natural, blissful. I had swiftly slipped through the early phases of non-REM sleep, skillfully side-stepping alpha and theta waves, leaving myoclonic jerks in my wake. There was a brief hypnagogic dream involving sun-swept landscapes, playful butterflies, and a field of rhythmically blowing lavender that waved me further along on my slumbering voyage. And then, magically, I was basking in the pillowy splendor of stage 4 sleep, delta waves soothingly serenading me into hibernation.
I had found the celebrated state of suspended sensory and motor activity characterized by unconsciousness and loss of voluntary muscle movement.1 I was asleep.
I was an intern, had just worked 36 continuous hours, and was driving a car.
ACGME Outlines Resident Duty-Hours Changes
I was reminded of this incident on June 23, when I reviewed the freshly minted recommendations from the Accreditation Council for Graduate Medical Education (ACGME) task force regarding duty hours.2 This proposal follows on ACGME’s 2003 report, which enacted such national resident duty-hour standards as the 80-hour work week, the maximum 24-hour shift (plus six hours for administrative time), and the requirement for 10 hours off between shifts.
Like the 2003 report, which has played a large role in the rise of academic HM, the 2010 recommendations have major implications for academic hospitalists and our community brethren who will receive our residency graduates. As such, the reaction within the hospitalist community was immediate. Within minutes of ACGME’s notification, I was inundated with e-mail from colleagues both locally and nationally. Everyone was struggling with the repercussions. Was this good for resident education, a boon or bust for HM, a death knell for teaching hospitals?
So What’s in There?
This hotly anticipated report focuses its energy on four key elements of what the ACGME has morphed from “duty hours” into the resident “work environment”: resident supervision, handoffs of patient care, use of systems to enhance patient safety, and the effects of sleep on performance. Much of this is not really controversial and likely good for both residents and HM—an emphasis on systems-based practice, transitions of care, and expectations around communication.
The most discussed and controversial changes regard the move toward supervision and work hours that are customized to trainees’ levels. Unlike in the past, when the intern bore the brunt of the hours and patient duties, this proposal emphasizes graded supervision and duty-hour expectations. Practically, this means first-year residents will require closer supervision (whether by a resident or an attending has yet to be delineated) than more senior residents. Likewise, although all residents can only work a maximum of 80 hours averaged over four weeks (no change from 2003), the maximum shift length for interns will be limited to 16 hours. Upper-level residents will be limited to no more than 24 consecutive hours with an additional four hours for administrative work, but it is “strongly suggested” that residents working longer than 16 hours be provided with opportunities for “strategic napping.”
Read the Tea Leaves
I think these recommendations are rational and reasonable. To be sure, when these go into effect on July 1, 2011, they will have a tremendous impact on my residency program, my hospital, and my hospitalist faculty. My program, like most, likely will move toward a shift system of patient care, instead of overnight call. My hospital likely will have to expend millions of dollars annually to back-fill the work that residents would have done. My hospitalist group likely will have to expand our nonresident coverage both during the day and at night, inducing one of my partners to query, “Does this mean we’ll have to hire napturnists to cover the residents’ strategic nap time?”
It’s easy to deride these work environment changes, especially if we see the world through the uphill-in-the-snow-both-ways lenses most of us use to recollect (fondly?) our residency days. Yes, the field of medicine is losing a rite of passage many of us endured, and I too retrospectively feel the nostalgic tug of the long shifts, the seemingly insurmountable avalanche of admissions, and the autonomy in resident decision-making that made my training so valuable. But are we really against ensuring that residents are properly supervised, handoffs are more standardized, and systems are in place to protect the safety of our patients?
Sleep = Safety
The push behind limiting the maximum duration of work to 16 and 24 hours for interns and residents, respectively, stems from the growing body of literature regarding the detrimental effects of the fatigue and sleep deprivation that comes with long shifts. Not so shockingly, the data show that residents are sleepy. When administered the Epworth Sleepiness Score, residents appear sleepier than sleep apneic patients and nearly as sleepy as narcoleptics.3,4 In fact, they are so sleepy they often don’t even recognize when they are sleeping. One study showed that nearly half the time that anesthesia residents were asleep, they were unaware that they were actually sleeping.5
Further data suggest that residents who sleep less than five hours per night are twice as likely to be sued, and significantly more likely to report adverse events and errors in patient care.6 When comparing traditional, every-third-night call and 24- to 30-hour shifts with 16-hour shifts, the former staffing model is associated with 36% more serious errors than the latter.
Furthermore, there is a five-fold increase in the rate of serious diagnostic errors in the residents in the longer-shift group.7 And to finish where I began, residents who worked shifts that lasted more than 24 hours are more than twice as likely to crash their cars as those working less than 24-hour shifts. In fact, every additional extended-duration shift per month increases the chances of a car crash while commuting by 16%.8
So ask yourself this: If you were designing, from scratch, residency training today, would you really design a system similar to what we had 10 years ago? Like the one we have now? Would you ask residents, many just months out of medical school, to admit a dozen or more patients a day, stay awake for more than 30 hours, and care for the sickest, most frail patients without the assistance of more senior physicians?
The field of medicine is at a crossroads, and it faces many questions, not the least of which is how best to train our future physicians. The ACGME has published its proposal and given the public, including you, until Aug. 9 to voice your comments. These are big issues to ponder.
Maybe you should sleep on it. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
References
- Sleep. Wikipedia website. Available at: http://en.wikipedia.org/wiki/Sleep. Accessed July 10, 2010.
- Nasca TJ, Day SH, Amis S. The new recommendations on duty hours from the ACGME task force. New England Journal of Medicine website. Available at: content.nejm.org/cgi/content/full/NEJMsb1005800. Accessed July 2, 2010.
- Mustafa M, Erokwu N, Ebose I, Strohl K. Sleep problems and the risk for sleep disorders in an outpatient veteran population. Sleep & Breathing. 2005;9:57-63.
- Papp KK, Stoller EP, Sage P, et al. The effects of sleep loss and fatigue on resident-physicians: a multi-institutional, mixed-method study. Acad Med. 2005; 79:394-406.
- Howard SK, Gaba DM, Rosekind MR, Zaracone VP. The risks and implications of excessive daytime sleepiness in resident physicians. Acad Med. 2002; 77:1019-1025.
- Baldwin DC, Daugherty SR. Sleep deprivation and fatigue in residency training: results of a national survey of 1st- and 2nd-year residents. Sleep. 2004;27:371-372.
- Landrigan CP, Rothschild JM, Cronin JW, et al. Effect of reducing interns’ work hours on serious medical errors in intensive care units. N Engl J Med. 2004;18:1838-1848.
- Barger LK, Cade BE, Ayas NT, et al. Extended work shifts and the risk of motor vehicle crashes among interns. N Engl J Med. 2005;352:125-134.
The best sleep I ever got was in the winter of 1996. I remember it vividly. It was effortless, natural, blissful. I had swiftly slipped through the early phases of non-REM sleep, skillfully side-stepping alpha and theta waves, leaving myoclonic jerks in my wake. There was a brief hypnagogic dream involving sun-swept landscapes, playful butterflies, and a field of rhythmically blowing lavender that waved me further along on my slumbering voyage. And then, magically, I was basking in the pillowy splendor of stage 4 sleep, delta waves soothingly serenading me into hibernation.
I had found the celebrated state of suspended sensory and motor activity characterized by unconsciousness and loss of voluntary muscle movement.1 I was asleep.
I was an intern, had just worked 36 continuous hours, and was driving a car.
ACGME Outlines Resident Duty-Hours Changes
I was reminded of this incident on June 23, when I reviewed the freshly minted recommendations from the Accreditation Council for Graduate Medical Education (ACGME) task force regarding duty hours.2 This proposal follows on ACGME’s 2003 report, which enacted such national resident duty-hour standards as the 80-hour work week, the maximum 24-hour shift (plus six hours for administrative time), and the requirement for 10 hours off between shifts.
Like the 2003 report, which has played a large role in the rise of academic HM, the 2010 recommendations have major implications for academic hospitalists and our community brethren who will receive our residency graduates. As such, the reaction within the hospitalist community was immediate. Within minutes of ACGME’s notification, I was inundated with e-mail from colleagues both locally and nationally. Everyone was struggling with the repercussions. Was this good for resident education, a boon or bust for HM, a death knell for teaching hospitals?
So What’s in There?
This hotly anticipated report focuses its energy on four key elements of what the ACGME has morphed from “duty hours” into the resident “work environment”: resident supervision, handoffs of patient care, use of systems to enhance patient safety, and the effects of sleep on performance. Much of this is not really controversial and likely good for both residents and HM—an emphasis on systems-based practice, transitions of care, and expectations around communication.
The most discussed and controversial changes regard the move toward supervision and work hours that are customized to trainees’ levels. Unlike in the past, when the intern bore the brunt of the hours and patient duties, this proposal emphasizes graded supervision and duty-hour expectations. Practically, this means first-year residents will require closer supervision (whether by a resident or an attending has yet to be delineated) than more senior residents. Likewise, although all residents can only work a maximum of 80 hours averaged over four weeks (no change from 2003), the maximum shift length for interns will be limited to 16 hours. Upper-level residents will be limited to no more than 24 consecutive hours with an additional four hours for administrative work, but it is “strongly suggested” that residents working longer than 16 hours be provided with opportunities for “strategic napping.”
Read the Tea Leaves
I think these recommendations are rational and reasonable. To be sure, when these go into effect on July 1, 2011, they will have a tremendous impact on my residency program, my hospital, and my hospitalist faculty. My program, like most, likely will move toward a shift system of patient care, instead of overnight call. My hospital likely will have to expend millions of dollars annually to back-fill the work that residents would have done. My hospitalist group likely will have to expand our nonresident coverage both during the day and at night, inducing one of my partners to query, “Does this mean we’ll have to hire napturnists to cover the residents’ strategic nap time?”
It’s easy to deride these work environment changes, especially if we see the world through the uphill-in-the-snow-both-ways lenses most of us use to recollect (fondly?) our residency days. Yes, the field of medicine is losing a rite of passage many of us endured, and I too retrospectively feel the nostalgic tug of the long shifts, the seemingly insurmountable avalanche of admissions, and the autonomy in resident decision-making that made my training so valuable. But are we really against ensuring that residents are properly supervised, handoffs are more standardized, and systems are in place to protect the safety of our patients?
Sleep = Safety
The push behind limiting the maximum duration of work to 16 and 24 hours for interns and residents, respectively, stems from the growing body of literature regarding the detrimental effects of the fatigue and sleep deprivation that comes with long shifts. Not so shockingly, the data show that residents are sleepy. When administered the Epworth Sleepiness Score, residents appear sleepier than sleep apneic patients and nearly as sleepy as narcoleptics.3,4 In fact, they are so sleepy they often don’t even recognize when they are sleeping. One study showed that nearly half the time that anesthesia residents were asleep, they were unaware that they were actually sleeping.5
Further data suggest that residents who sleep less than five hours per night are twice as likely to be sued, and significantly more likely to report adverse events and errors in patient care.6 When comparing traditional, every-third-night call and 24- to 30-hour shifts with 16-hour shifts, the former staffing model is associated with 36% more serious errors than the latter.
Furthermore, there is a five-fold increase in the rate of serious diagnostic errors in the residents in the longer-shift group.7 And to finish where I began, residents who worked shifts that lasted more than 24 hours are more than twice as likely to crash their cars as those working less than 24-hour shifts. In fact, every additional extended-duration shift per month increases the chances of a car crash while commuting by 16%.8
So ask yourself this: If you were designing, from scratch, residency training today, would you really design a system similar to what we had 10 years ago? Like the one we have now? Would you ask residents, many just months out of medical school, to admit a dozen or more patients a day, stay awake for more than 30 hours, and care for the sickest, most frail patients without the assistance of more senior physicians?
The field of medicine is at a crossroads, and it faces many questions, not the least of which is how best to train our future physicians. The ACGME has published its proposal and given the public, including you, until Aug. 9 to voice your comments. These are big issues to ponder.
Maybe you should sleep on it. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
References
- Sleep. Wikipedia website. Available at: http://en.wikipedia.org/wiki/Sleep. Accessed July 10, 2010.
- Nasca TJ, Day SH, Amis S. The new recommendations on duty hours from the ACGME task force. New England Journal of Medicine website. Available at: content.nejm.org/cgi/content/full/NEJMsb1005800. Accessed July 2, 2010.
- Mustafa M, Erokwu N, Ebose I, Strohl K. Sleep problems and the risk for sleep disorders in an outpatient veteran population. Sleep & Breathing. 2005;9:57-63.
- Papp KK, Stoller EP, Sage P, et al. The effects of sleep loss and fatigue on resident-physicians: a multi-institutional, mixed-method study. Acad Med. 2005; 79:394-406.
- Howard SK, Gaba DM, Rosekind MR, Zaracone VP. The risks and implications of excessive daytime sleepiness in resident physicians. Acad Med. 2002; 77:1019-1025.
- Baldwin DC, Daugherty SR. Sleep deprivation and fatigue in residency training: results of a national survey of 1st- and 2nd-year residents. Sleep. 2004;27:371-372.
- Landrigan CP, Rothschild JM, Cronin JW, et al. Effect of reducing interns’ work hours on serious medical errors in intensive care units. N Engl J Med. 2004;18:1838-1848.
- Barger LK, Cade BE, Ayas NT, et al. Extended work shifts and the risk of motor vehicle crashes among interns. N Engl J Med. 2005;352:125-134.
The best sleep I ever got was in the winter of 1996. I remember it vividly. It was effortless, natural, blissful. I had swiftly slipped through the early phases of non-REM sleep, skillfully side-stepping alpha and theta waves, leaving myoclonic jerks in my wake. There was a brief hypnagogic dream involving sun-swept landscapes, playful butterflies, and a field of rhythmically blowing lavender that waved me further along on my slumbering voyage. And then, magically, I was basking in the pillowy splendor of stage 4 sleep, delta waves soothingly serenading me into hibernation.
I had found the celebrated state of suspended sensory and motor activity characterized by unconsciousness and loss of voluntary muscle movement.1 I was asleep.
I was an intern, had just worked 36 continuous hours, and was driving a car.
ACGME Outlines Resident Duty-Hours Changes
I was reminded of this incident on June 23, when I reviewed the freshly minted recommendations from the Accreditation Council for Graduate Medical Education (ACGME) task force regarding duty hours.2 This proposal follows on ACGME’s 2003 report, which enacted such national resident duty-hour standards as the 80-hour work week, the maximum 24-hour shift (plus six hours for administrative time), and the requirement for 10 hours off between shifts.
Like the 2003 report, which has played a large role in the rise of academic HM, the 2010 recommendations have major implications for academic hospitalists and our community brethren who will receive our residency graduates. As such, the reaction within the hospitalist community was immediate. Within minutes of ACGME’s notification, I was inundated with e-mail from colleagues both locally and nationally. Everyone was struggling with the repercussions. Was this good for resident education, a boon or bust for HM, a death knell for teaching hospitals?
So What’s in There?
This hotly anticipated report focuses its energy on four key elements of what the ACGME has morphed from “duty hours” into the resident “work environment”: resident supervision, handoffs of patient care, use of systems to enhance patient safety, and the effects of sleep on performance. Much of this is not really controversial and likely good for both residents and HM—an emphasis on systems-based practice, transitions of care, and expectations around communication.
The most discussed and controversial changes regard the move toward supervision and work hours that are customized to trainees’ levels. Unlike in the past, when the intern bore the brunt of the hours and patient duties, this proposal emphasizes graded supervision and duty-hour expectations. Practically, this means first-year residents will require closer supervision (whether by a resident or an attending has yet to be delineated) than more senior residents. Likewise, although all residents can only work a maximum of 80 hours averaged over four weeks (no change from 2003), the maximum shift length for interns will be limited to 16 hours. Upper-level residents will be limited to no more than 24 consecutive hours with an additional four hours for administrative work, but it is “strongly suggested” that residents working longer than 16 hours be provided with opportunities for “strategic napping.”
Read the Tea Leaves
I think these recommendations are rational and reasonable. To be sure, when these go into effect on July 1, 2011, they will have a tremendous impact on my residency program, my hospital, and my hospitalist faculty. My program, like most, likely will move toward a shift system of patient care, instead of overnight call. My hospital likely will have to expend millions of dollars annually to back-fill the work that residents would have done. My hospitalist group likely will have to expand our nonresident coverage both during the day and at night, inducing one of my partners to query, “Does this mean we’ll have to hire napturnists to cover the residents’ strategic nap time?”
It’s easy to deride these work environment changes, especially if we see the world through the uphill-in-the-snow-both-ways lenses most of us use to recollect (fondly?) our residency days. Yes, the field of medicine is losing a rite of passage many of us endured, and I too retrospectively feel the nostalgic tug of the long shifts, the seemingly insurmountable avalanche of admissions, and the autonomy in resident decision-making that made my training so valuable. But are we really against ensuring that residents are properly supervised, handoffs are more standardized, and systems are in place to protect the safety of our patients?
Sleep = Safety
The push behind limiting the maximum duration of work to 16 and 24 hours for interns and residents, respectively, stems from the growing body of literature regarding the detrimental effects of the fatigue and sleep deprivation that comes with long shifts. Not so shockingly, the data show that residents are sleepy. When administered the Epworth Sleepiness Score, residents appear sleepier than sleep apneic patients and nearly as sleepy as narcoleptics.3,4 In fact, they are so sleepy they often don’t even recognize when they are sleeping. One study showed that nearly half the time that anesthesia residents were asleep, they were unaware that they were actually sleeping.5
Further data suggest that residents who sleep less than five hours per night are twice as likely to be sued, and significantly more likely to report adverse events and errors in patient care.6 When comparing traditional, every-third-night call and 24- to 30-hour shifts with 16-hour shifts, the former staffing model is associated with 36% more serious errors than the latter.
Furthermore, there is a five-fold increase in the rate of serious diagnostic errors in the residents in the longer-shift group.7 And to finish where I began, residents who worked shifts that lasted more than 24 hours are more than twice as likely to crash their cars as those working less than 24-hour shifts. In fact, every additional extended-duration shift per month increases the chances of a car crash while commuting by 16%.8
So ask yourself this: If you were designing, from scratch, residency training today, would you really design a system similar to what we had 10 years ago? Like the one we have now? Would you ask residents, many just months out of medical school, to admit a dozen or more patients a day, stay awake for more than 30 hours, and care for the sickest, most frail patients without the assistance of more senior physicians?
The field of medicine is at a crossroads, and it faces many questions, not the least of which is how best to train our future physicians. The ACGME has published its proposal and given the public, including you, until Aug. 9 to voice your comments. These are big issues to ponder.
Maybe you should sleep on it. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
References
- Sleep. Wikipedia website. Available at: http://en.wikipedia.org/wiki/Sleep. Accessed July 10, 2010.
- Nasca TJ, Day SH, Amis S. The new recommendations on duty hours from the ACGME task force. New England Journal of Medicine website. Available at: content.nejm.org/cgi/content/full/NEJMsb1005800. Accessed July 2, 2010.
- Mustafa M, Erokwu N, Ebose I, Strohl K. Sleep problems and the risk for sleep disorders in an outpatient veteran population. Sleep & Breathing. 2005;9:57-63.
- Papp KK, Stoller EP, Sage P, et al. The effects of sleep loss and fatigue on resident-physicians: a multi-institutional, mixed-method study. Acad Med. 2005; 79:394-406.
- Howard SK, Gaba DM, Rosekind MR, Zaracone VP. The risks and implications of excessive daytime sleepiness in resident physicians. Acad Med. 2002; 77:1019-1025.
- Baldwin DC, Daugherty SR. Sleep deprivation and fatigue in residency training: results of a national survey of 1st- and 2nd-year residents. Sleep. 2004;27:371-372.
- Landrigan CP, Rothschild JM, Cronin JW, et al. Effect of reducing interns’ work hours on serious medical errors in intensive care units. N Engl J Med. 2004;18:1838-1848.
- Barger LK, Cade BE, Ayas NT, et al. Extended work shifts and the risk of motor vehicle crashes among interns. N Engl J Med. 2005;352:125-134.