User login
Emergency department visits from adverse drug events
Clinical question: The purpose of this study was to describe emergency department (ED) visits for adverse drug events in year 2013-2014 compared to year 2005-2006 to learn changing patterns of ADEs and to help advance medication safety initiatives in outpatient settings.
Background: Adverse drug events (ADEs) are the most common cause of iatrogenic harm to patients and there have been significant national-level initiatives to prevent them as a part of patient safety. In the outpatient setting, where 90% of prescription drug expenditures occur, preventing ADEs remains a patient safety challenge because patients can have complex medication regimens, at times prescribed by multiple clinicians, with far less monitoring compared with hospitalized patients.
Setting and study design: Active, public health surveillance in 58 EDs in the United States that participate in the National Electronic Injury Surveillance System–Cooperative Adverse Drug Event Surveillance Project (NEISS-CADES). Trained data abstractors at each hospital reviewed each ED visit to identify any clinician-diagnosed ADEs that were the reason for the ED visit. Reports were coded by CDC and analyzed.
Synopsis: Based on 42,585 cases, 4.0 (95% CI, 3.1-5) ED visits for ADEs per 1,000 individuals occurred annually in the United States in 2013-2014 and 27.3% (22.2%-32.4%) of ED visits for ADEs resulted in hospitalization.
An estimated 34.5 % (95% CI, 30.3-38.8) of ED visits for ADEs occurred among adults aged 65 or older in 2013 compared with an estimated 25.6% (95% CI, 21-30) in 2005-2006. The population rate for adults older than 65 years was 9.7 visits per 1,000 individuals, compared with 3.1 visits per 1,000 individuals for those younger than 65 years. Older adults experienced higher hospitalization rates 43.6% (95% CI, 36.6-50.5). When adjusted for the U.S. population, the hospitalization rate for ADEs among older individuals was seven times higher compared with younger patients.
A single medication was implicated in most ED visits for ADEs (83.8%; 95% CI, 81.5-86.1). Supratherapeutic effects of ingestion of excess dose was the most common type of ADE (37.2%; 95% CI, 34.7-39.6). Medication errors were documented in 1 of 10 ED visits for ADEs (10.5%; 95% CI, 8.9-12.2).
The most commonly implicated drug classes were anticoagulants (17.6%), systemic antibiotics (16.1%), diabetes agents (13.3%), opioid analgesics (6.8%), antiplatelets (6.6%), renin-angiotensin system inhibitors (3.5%), antineoplastic agents (3%) and sedative/hypnotics (3%). Since 2005-2006, the proportions of ED visits for ADEs involving anticoagulants, antiplatelets, and diabetic agents have increased, whereas proportions involving antibiotics have decreased.
In children aged 5 years or younger, antibiotics were the most common drug class (56.4; 95% CI, 51.8-61). Among children and adolescents aged 6-19 years, antibiotics also were the most common class (31.8%; 95% CI, 28.7-34.9), followed by antipsychotics (4.5%; 95% CI, 3.3-5.6).
Among older adults, three drug classes recently targeted by federal patient safety initiatives (anticoagulants, diabetes agents, and opioid analgesics) were implicated in an estimated 59.9% (95% CI, 56.8-62.9) of ED visits. Four anticoagulants (warfarin, rivaroxaban, dabigatran, and enoxaparin) and five diabetes agents (insulin and four oral agents) were among the 15 most common drugs implicated. Medications to always avoid in older adults according to Beers criteria were implicated in 1.8% (95% CI, 1.5-2.1) of ED visits for adverse drug events.
Summary: The most common drug classes implicated in ED visits for ADEs in the United States are the same ones identified a decade ago – anticoagulants, antibiotics, diabetes agents, and opioid analgesics. The proportion of ED visits for ADEs involving anticoagulants has increased during the last decade with increased anticoagulant use. The prevalence of potentially inappropriate medication use in older patients also remains high.
Citation: JAMA. 2016;316(20):2115-25. doi: 10.1001/jama.2016.16201.
Dr. Patel is a hospitalist in the division of hospital medicine and assistant professor of medicine at Cooper Medical School of Rowan University, Camden, N.J. He is CMSRU’s associate residency program director and serves as codirector of the Foundation of Medical Practice curriculum.
Clinical question: The purpose of this study was to describe emergency department (ED) visits for adverse drug events in year 2013-2014 compared to year 2005-2006 to learn changing patterns of ADEs and to help advance medication safety initiatives in outpatient settings.
Background: Adverse drug events (ADEs) are the most common cause of iatrogenic harm to patients and there have been significant national-level initiatives to prevent them as a part of patient safety. In the outpatient setting, where 90% of prescription drug expenditures occur, preventing ADEs remains a patient safety challenge because patients can have complex medication regimens, at times prescribed by multiple clinicians, with far less monitoring compared with hospitalized patients.
Setting and study design: Active, public health surveillance in 58 EDs in the United States that participate in the National Electronic Injury Surveillance System–Cooperative Adverse Drug Event Surveillance Project (NEISS-CADES). Trained data abstractors at each hospital reviewed each ED visit to identify any clinician-diagnosed ADEs that were the reason for the ED visit. Reports were coded by CDC and analyzed.
Synopsis: Based on 42,585 cases, 4.0 (95% CI, 3.1-5) ED visits for ADEs per 1,000 individuals occurred annually in the United States in 2013-2014 and 27.3% (22.2%-32.4%) of ED visits for ADEs resulted in hospitalization.
An estimated 34.5 % (95% CI, 30.3-38.8) of ED visits for ADEs occurred among adults aged 65 or older in 2013 compared with an estimated 25.6% (95% CI, 21-30) in 2005-2006. The population rate for adults older than 65 years was 9.7 visits per 1,000 individuals, compared with 3.1 visits per 1,000 individuals for those younger than 65 years. Older adults experienced higher hospitalization rates 43.6% (95% CI, 36.6-50.5). When adjusted for the U.S. population, the hospitalization rate for ADEs among older individuals was seven times higher compared with younger patients.
A single medication was implicated in most ED visits for ADEs (83.8%; 95% CI, 81.5-86.1). Supratherapeutic effects of ingestion of excess dose was the most common type of ADE (37.2%; 95% CI, 34.7-39.6). Medication errors were documented in 1 of 10 ED visits for ADEs (10.5%; 95% CI, 8.9-12.2).
The most commonly implicated drug classes were anticoagulants (17.6%), systemic antibiotics (16.1%), diabetes agents (13.3%), opioid analgesics (6.8%), antiplatelets (6.6%), renin-angiotensin system inhibitors (3.5%), antineoplastic agents (3%) and sedative/hypnotics (3%). Since 2005-2006, the proportions of ED visits for ADEs involving anticoagulants, antiplatelets, and diabetic agents have increased, whereas proportions involving antibiotics have decreased.
In children aged 5 years or younger, antibiotics were the most common drug class (56.4; 95% CI, 51.8-61). Among children and adolescents aged 6-19 years, antibiotics also were the most common class (31.8%; 95% CI, 28.7-34.9), followed by antipsychotics (4.5%; 95% CI, 3.3-5.6).
Among older adults, three drug classes recently targeted by federal patient safety initiatives (anticoagulants, diabetes agents, and opioid analgesics) were implicated in an estimated 59.9% (95% CI, 56.8-62.9) of ED visits. Four anticoagulants (warfarin, rivaroxaban, dabigatran, and enoxaparin) and five diabetes agents (insulin and four oral agents) were among the 15 most common drugs implicated. Medications to always avoid in older adults according to Beers criteria were implicated in 1.8% (95% CI, 1.5-2.1) of ED visits for adverse drug events.
Summary: The most common drug classes implicated in ED visits for ADEs in the United States are the same ones identified a decade ago – anticoagulants, antibiotics, diabetes agents, and opioid analgesics. The proportion of ED visits for ADEs involving anticoagulants has increased during the last decade with increased anticoagulant use. The prevalence of potentially inappropriate medication use in older patients also remains high.
Citation: JAMA. 2016;316(20):2115-25. doi: 10.1001/jama.2016.16201.
Dr. Patel is a hospitalist in the division of hospital medicine and assistant professor of medicine at Cooper Medical School of Rowan University, Camden, N.J. He is CMSRU’s associate residency program director and serves as codirector of the Foundation of Medical Practice curriculum.
Clinical question: The purpose of this study was to describe emergency department (ED) visits for adverse drug events in year 2013-2014 compared to year 2005-2006 to learn changing patterns of ADEs and to help advance medication safety initiatives in outpatient settings.
Background: Adverse drug events (ADEs) are the most common cause of iatrogenic harm to patients and there have been significant national-level initiatives to prevent them as a part of patient safety. In the outpatient setting, where 90% of prescription drug expenditures occur, preventing ADEs remains a patient safety challenge because patients can have complex medication regimens, at times prescribed by multiple clinicians, with far less monitoring compared with hospitalized patients.
Setting and study design: Active, public health surveillance in 58 EDs in the United States that participate in the National Electronic Injury Surveillance System–Cooperative Adverse Drug Event Surveillance Project (NEISS-CADES). Trained data abstractors at each hospital reviewed each ED visit to identify any clinician-diagnosed ADEs that were the reason for the ED visit. Reports were coded by CDC and analyzed.
Synopsis: Based on 42,585 cases, 4.0 (95% CI, 3.1-5) ED visits for ADEs per 1,000 individuals occurred annually in the United States in 2013-2014 and 27.3% (22.2%-32.4%) of ED visits for ADEs resulted in hospitalization.
An estimated 34.5 % (95% CI, 30.3-38.8) of ED visits for ADEs occurred among adults aged 65 or older in 2013 compared with an estimated 25.6% (95% CI, 21-30) in 2005-2006. The population rate for adults older than 65 years was 9.7 visits per 1,000 individuals, compared with 3.1 visits per 1,000 individuals for those younger than 65 years. Older adults experienced higher hospitalization rates 43.6% (95% CI, 36.6-50.5). When adjusted for the U.S. population, the hospitalization rate for ADEs among older individuals was seven times higher compared with younger patients.
A single medication was implicated in most ED visits for ADEs (83.8%; 95% CI, 81.5-86.1). Supratherapeutic effects of ingestion of excess dose was the most common type of ADE (37.2%; 95% CI, 34.7-39.6). Medication errors were documented in 1 of 10 ED visits for ADEs (10.5%; 95% CI, 8.9-12.2).
The most commonly implicated drug classes were anticoagulants (17.6%), systemic antibiotics (16.1%), diabetes agents (13.3%), opioid analgesics (6.8%), antiplatelets (6.6%), renin-angiotensin system inhibitors (3.5%), antineoplastic agents (3%) and sedative/hypnotics (3%). Since 2005-2006, the proportions of ED visits for ADEs involving anticoagulants, antiplatelets, and diabetic agents have increased, whereas proportions involving antibiotics have decreased.
In children aged 5 years or younger, antibiotics were the most common drug class (56.4; 95% CI, 51.8-61). Among children and adolescents aged 6-19 years, antibiotics also were the most common class (31.8%; 95% CI, 28.7-34.9), followed by antipsychotics (4.5%; 95% CI, 3.3-5.6).
Among older adults, three drug classes recently targeted by federal patient safety initiatives (anticoagulants, diabetes agents, and opioid analgesics) were implicated in an estimated 59.9% (95% CI, 56.8-62.9) of ED visits. Four anticoagulants (warfarin, rivaroxaban, dabigatran, and enoxaparin) and five diabetes agents (insulin and four oral agents) were among the 15 most common drugs implicated. Medications to always avoid in older adults according to Beers criteria were implicated in 1.8% (95% CI, 1.5-2.1) of ED visits for adverse drug events.
Summary: The most common drug classes implicated in ED visits for ADEs in the United States are the same ones identified a decade ago – anticoagulants, antibiotics, diabetes agents, and opioid analgesics. The proportion of ED visits for ADEs involving anticoagulants has increased during the last decade with increased anticoagulant use. The prevalence of potentially inappropriate medication use in older patients also remains high.
Citation: JAMA. 2016;316(20):2115-25. doi: 10.1001/jama.2016.16201.
Dr. Patel is a hospitalist in the division of hospital medicine and assistant professor of medicine at Cooper Medical School of Rowan University, Camden, N.J. He is CMSRU’s associate residency program director and serves as codirector of the Foundation of Medical Practice curriculum.
Trending at SHM
Top 10 reasons to attend 2017 Quality and Safety Educators Academy
It’s your last chance to register for the 2017 Quality and Safety Educators Academy (QSEA), which will be held Feb. 26-28 in Tempe, Ariz. Looking for some reasons to attend? Here are the top 10:
- Education. Develop and refine your knowledge in quality and patient safety.
- Desert beauty. Enjoy sunny Tempe, or travel to nearby Phoenix or Scottsdale.
- Curriculum development. Return to your institution with a collection of new educational strategies and curriculum development tactics.
- Professional development. Hone your skills and be the best that you can be to meet the increasing demand for medical educators who are well versed in patient safety and quality.
- Relationships. Build your network with faculty mentors and colleagues who have similar career interests.
- Institutional backing. Engage your institutional leaders to support and implement a quality and patient safety curriculum to meet the Accreditation Council for Graduate Medical Education core competencies and improve patient care.
- Hands-on learning. Engage in an interactive learning environment, with a 10:1 student to faculty ratio, including facilitated large-group sessions, small-group exercises, and panel discussions.
- Variety. Each day has its own topic that breaks down into subtopics, covering the breadth of information you need to know to succeed.
- Faculty. All sessions are led by experienced physicians known for their ability to practice and teach quality improvement and patient safety, mentor junior faculty, and guide educators in curriculum development.
- Resources. Leave with a toolkit of educational resources and curricular tools for quality and safety education.
Reserve your spot today before the meeting sells out at www.shmqsea.org.
SHM committees address practice management topics
SHM’s Practice Management Committee has been researching, deliberating case studies, and authoring timely content to further define HM’s role in key health care innovations. As the specialty has grown and evolved, so have hospitalists’ involvement in comanagement relationships.
The committee recently released a white paper addressing the evolution of comanagement in hospital medicine. Be on the lookout for that in early 2017.
Similarly, telemedicine is rapidly expanding, and the committee found it imperative to clarify the who, what, when, where, why, and how of telemedicine programs in hospital medicine. You can also expect this white paper in early 2017.
The committee also has created guidelines on how to raise awareness of cultural humility in your HM group. Deemed the “5 R’s of Cultural Humility,” look for a campaign around the guidelines to launch at HM17 in May in Las Vegas.
SHM’s Health Information Technology Committee has been diligently analyzing and reporting on survey results that captured hospitalists’ attitudes toward electronic health records. The purpose of this white paper is to effect change on EHR systems by informing conversations with decision makers, and to provide HM a definitive voice in the landscape of the tumultuous world of EHRs. More information is coming soon.
Make a difference with SHM
Grow professionally, expand your curriculum vitae, and get involved in work you are passionate about with colleagues across the country with SHM’s volunteer experiences. New opportunities are constantly being added that will bolster your strengths, sharpen your professional acumen and enhance your profile in the hospital medicine community at www.hospitalmedicine.org/getinvolved.
Leadership Academy 2017 has a new look
Don’t miss out on the only leadership program designed specifically for hospitalists. SHM Leadership Academy 2017 will be at the JW Marriott Camelback Inn in Scottsdale, Ariz., on Oct. 23-26.
For the first time, the Leadership Academy prerequisite of attendance in the first-level, Foundations course has been removed. Essential Strategies (formerly Leadership Foundations), Influential Management, and Mastering Teamwork courses are available to all attendees, regardless of previous attendance. Prior participants have made recommendations to help interested registrants determine which course fits them best in their leadership journey.
All three courses run concurrently over the span of 4 days. This expanded meeting will provide attendees with world-class networking opportunities, creating opportunities for a more engaging, impactful educational experience.
Learn more about SHM’s Leadership Academy at www.shmleadershipacademy.org.
Earn dues credits with the Membership Ambassador Program
Help SHM grow its network of hospitalists and continue to provide education, networking, and career advancement for its members. Visit www.hospitalmedicine.org/refer today.
Brett Radler is SHM's communications specialist.
Top 10 reasons to attend 2017 Quality and Safety Educators Academy
It’s your last chance to register for the 2017 Quality and Safety Educators Academy (QSEA), which will be held Feb. 26-28 in Tempe, Ariz. Looking for some reasons to attend? Here are the top 10:
- Education. Develop and refine your knowledge in quality and patient safety.
- Desert beauty. Enjoy sunny Tempe, or travel to nearby Phoenix or Scottsdale.
- Curriculum development. Return to your institution with a collection of new educational strategies and curriculum development tactics.
- Professional development. Hone your skills and be the best that you can be to meet the increasing demand for medical educators who are well versed in patient safety and quality.
- Relationships. Build your network with faculty mentors and colleagues who have similar career interests.
- Institutional backing. Engage your institutional leaders to support and implement a quality and patient safety curriculum to meet the Accreditation Council for Graduate Medical Education core competencies and improve patient care.
- Hands-on learning. Engage in an interactive learning environment, with a 10:1 student to faculty ratio, including facilitated large-group sessions, small-group exercises, and panel discussions.
- Variety. Each day has its own topic that breaks down into subtopics, covering the breadth of information you need to know to succeed.
- Faculty. All sessions are led by experienced physicians known for their ability to practice and teach quality improvement and patient safety, mentor junior faculty, and guide educators in curriculum development.
- Resources. Leave with a toolkit of educational resources and curricular tools for quality and safety education.
Reserve your spot today before the meeting sells out at www.shmqsea.org.
SHM committees address practice management topics
SHM’s Practice Management Committee has been researching, deliberating case studies, and authoring timely content to further define HM’s role in key health care innovations. As the specialty has grown and evolved, so have hospitalists’ involvement in comanagement relationships.
The committee recently released a white paper addressing the evolution of comanagement in hospital medicine. Be on the lookout for that in early 2017.
Similarly, telemedicine is rapidly expanding, and the committee found it imperative to clarify the who, what, when, where, why, and how of telemedicine programs in hospital medicine. You can also expect this white paper in early 2017.
The committee also has created guidelines on how to raise awareness of cultural humility in your HM group. Deemed the “5 R’s of Cultural Humility,” look for a campaign around the guidelines to launch at HM17 in May in Las Vegas.
SHM’s Health Information Technology Committee has been diligently analyzing and reporting on survey results that captured hospitalists’ attitudes toward electronic health records. The purpose of this white paper is to effect change on EHR systems by informing conversations with decision makers, and to provide HM a definitive voice in the landscape of the tumultuous world of EHRs. More information is coming soon.
Make a difference with SHM
Grow professionally, expand your curriculum vitae, and get involved in work you are passionate about with colleagues across the country with SHM’s volunteer experiences. New opportunities are constantly being added that will bolster your strengths, sharpen your professional acumen and enhance your profile in the hospital medicine community at www.hospitalmedicine.org/getinvolved.
Leadership Academy 2017 has a new look
Don’t miss out on the only leadership program designed specifically for hospitalists. SHM Leadership Academy 2017 will be at the JW Marriott Camelback Inn in Scottsdale, Ariz., on Oct. 23-26.
For the first time, the Leadership Academy prerequisite of attendance in the first-level, Foundations course has been removed. Essential Strategies (formerly Leadership Foundations), Influential Management, and Mastering Teamwork courses are available to all attendees, regardless of previous attendance. Prior participants have made recommendations to help interested registrants determine which course fits them best in their leadership journey.
All three courses run concurrently over the span of 4 days. This expanded meeting will provide attendees with world-class networking opportunities, creating opportunities for a more engaging, impactful educational experience.
Learn more about SHM’s Leadership Academy at www.shmleadershipacademy.org.
Earn dues credits with the Membership Ambassador Program
Help SHM grow its network of hospitalists and continue to provide education, networking, and career advancement for its members. Visit www.hospitalmedicine.org/refer today.
Brett Radler is SHM's communications specialist.
Top 10 reasons to attend 2017 Quality and Safety Educators Academy
It’s your last chance to register for the 2017 Quality and Safety Educators Academy (QSEA), which will be held Feb. 26-28 in Tempe, Ariz. Looking for some reasons to attend? Here are the top 10:
- Education. Develop and refine your knowledge in quality and patient safety.
- Desert beauty. Enjoy sunny Tempe, or travel to nearby Phoenix or Scottsdale.
- Curriculum development. Return to your institution with a collection of new educational strategies and curriculum development tactics.
- Professional development. Hone your skills and be the best that you can be to meet the increasing demand for medical educators who are well versed in patient safety and quality.
- Relationships. Build your network with faculty mentors and colleagues who have similar career interests.
- Institutional backing. Engage your institutional leaders to support and implement a quality and patient safety curriculum to meet the Accreditation Council for Graduate Medical Education core competencies and improve patient care.
- Hands-on learning. Engage in an interactive learning environment, with a 10:1 student to faculty ratio, including facilitated large-group sessions, small-group exercises, and panel discussions.
- Variety. Each day has its own topic that breaks down into subtopics, covering the breadth of information you need to know to succeed.
- Faculty. All sessions are led by experienced physicians known for their ability to practice and teach quality improvement and patient safety, mentor junior faculty, and guide educators in curriculum development.
- Resources. Leave with a toolkit of educational resources and curricular tools for quality and safety education.
Reserve your spot today before the meeting sells out at www.shmqsea.org.
SHM committees address practice management topics
SHM’s Practice Management Committee has been researching, deliberating case studies, and authoring timely content to further define HM’s role in key health care innovations. As the specialty has grown and evolved, so have hospitalists’ involvement in comanagement relationships.
The committee recently released a white paper addressing the evolution of comanagement in hospital medicine. Be on the lookout for that in early 2017.
Similarly, telemedicine is rapidly expanding, and the committee found it imperative to clarify the who, what, when, where, why, and how of telemedicine programs in hospital medicine. You can also expect this white paper in early 2017.
The committee also has created guidelines on how to raise awareness of cultural humility in your HM group. Deemed the “5 R’s of Cultural Humility,” look for a campaign around the guidelines to launch at HM17 in May in Las Vegas.
SHM’s Health Information Technology Committee has been diligently analyzing and reporting on survey results that captured hospitalists’ attitudes toward electronic health records. The purpose of this white paper is to effect change on EHR systems by informing conversations with decision makers, and to provide HM a definitive voice in the landscape of the tumultuous world of EHRs. More information is coming soon.
Make a difference with SHM
Grow professionally, expand your curriculum vitae, and get involved in work you are passionate about with colleagues across the country with SHM’s volunteer experiences. New opportunities are constantly being added that will bolster your strengths, sharpen your professional acumen and enhance your profile in the hospital medicine community at www.hospitalmedicine.org/getinvolved.
Leadership Academy 2017 has a new look
Don’t miss out on the only leadership program designed specifically for hospitalists. SHM Leadership Academy 2017 will be at the JW Marriott Camelback Inn in Scottsdale, Ariz., on Oct. 23-26.
For the first time, the Leadership Academy prerequisite of attendance in the first-level, Foundations course has been removed. Essential Strategies (formerly Leadership Foundations), Influential Management, and Mastering Teamwork courses are available to all attendees, regardless of previous attendance. Prior participants have made recommendations to help interested registrants determine which course fits them best in their leadership journey.
All three courses run concurrently over the span of 4 days. This expanded meeting will provide attendees with world-class networking opportunities, creating opportunities for a more engaging, impactful educational experience.
Learn more about SHM’s Leadership Academy at www.shmleadershipacademy.org.
Earn dues credits with the Membership Ambassador Program
Help SHM grow its network of hospitalists and continue to provide education, networking, and career advancement for its members. Visit www.hospitalmedicine.org/refer today.
Brett Radler is SHM's communications specialist.
Female physicians, lower mortality, lower readmissions: A case study
Week in, week out for the past 25 years, I have had a front-row seat to the medical practice of a certain female physician: my wife, Heather. We met when we worked together on the wards during residency in 1991; spent a year in rural Montana working together in clinics, ERs, and hospitals; shared the care of one another’s patients as our practices grew in parallel – hers in skilled nursing facilities, mine in the hospital; and reunited in recent years to work together as part of the same practice.
When I saw the paper by Yusuke Tsugawa, MD, MPH, PhD, and his associates showing lower mortality and readmission rates for female physicians versus their male counterparts, I began to wonder if the case of Heather’s practice style, and my observations of it, could help to interpret the findings of the study (JAMA Intern Med. 2016 Dec 19. doi: 10.1001/jamainternmed.2016.7875). The authors suggested that female physicians may produce better outcomes than male physicians.
The study in question, which analyzed more than 1.5 million hospitalizations, looked at Medicare beneficiaries hospitalized with a medical condition treated by general internists between 2011 and 2014. The authors found that patients treated by female physicians had lower 30-day mortality (adjusted rate, 11.07% vs. 11.49%, P<.001) and readmissions (adjusted rate, 15.02% vs. 15.57%, P<.001) than those treated by male physicians within the same hospital. The differences were “modest but important,” coauthor Ashish K. Jha, MD, MPH, wrote in his blog. Numbers needed to treat to prevent one death and one readmission were 233 and 182, respectively.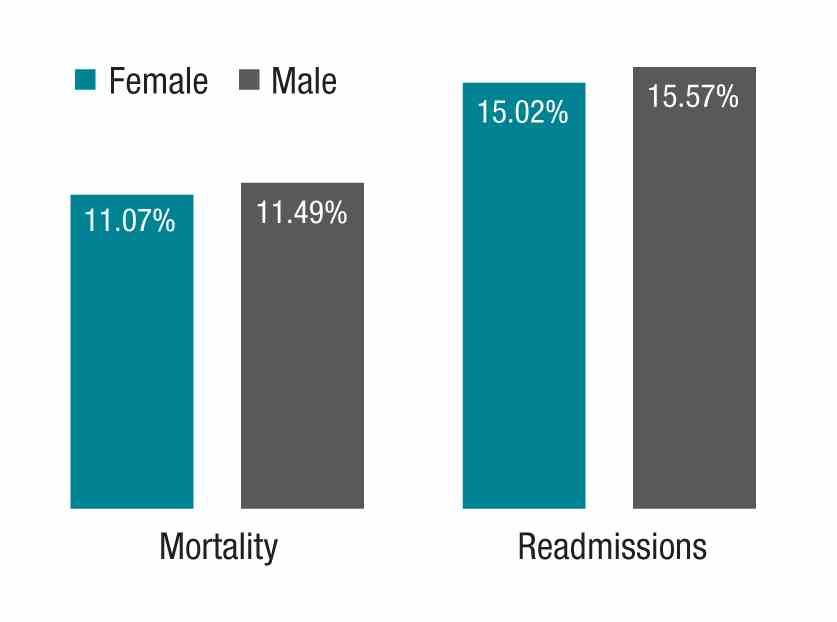
My observations of Heather’s practice approach, compared with my own, center around three main themes:
She spends more time considering her approach to a challenging case.
She has less urgency in deciding on a definitive course of action and more patience in sorting things out before proceeding with a diagnostic and therapeutic plan. She is more likely to leave open the possibility of changing her mind; she has less of a tendency to anchor on a particular diagnosis and treatment. Put another way, she is more willing to continue with ambiguous findings without lateralizing to one particular approach.
She brings more work-life balance to her professional responsibilities.
Despite being highly productive at work (and at home), she has worked less than full time throughout her career. This means that, during any given patient encounter, she is more likely to be unburdened by overwork and its negative consequences. It is my sense that many full-time physicians would be happier (and more effective) if they simply worked less. Heather has had the self-knowledge to take on a more manageable workload; the result is that she has remained joyous in practice for more than two decades.
She is less dogmatic and more willing to customize care based on the needs of the individual patient.
Although a good fund of knowledge is essential, if such knowledge obscures the physician’s ability to read the patient, then it is best abandoned, at least temporarily. Heather refers to the body of scientific evidence frequently, but she reserves an equal or greater portion of her cognitive bandwidth for the patient she is caring for at a particular moment.
How might the observations of this case study help to derive meaning from the study by Dr. Tsugawa and his associates, so that all patients may benefit from whatever it is that female physicians do to achieve better outcomes?
First, if physicians – regardless of gender – simply have an awareness of anchoring bias or rushing to land on a diagnosis or treatment, they will be less likely to do so in the future.
Next, we can learn that avoiding overwork can make for more joy in work, and if this is so, our patients may fare better. When I say “avoiding overwork,” that might mean rethinking our assumptions underlying the amount of work we take on.
Finally, while amassing a large fund of knowledge is a good thing, balancing medical knowledge with knowledge of the individual patient is crucial to good medical practice.
Dr. Whitcomb is Chief Medical Officer at Remedy Partners in Darien, CT. He is a cofounder and past president of SHM. Email him at wfwhit@comcast.net.
Week in, week out for the past 25 years, I have had a front-row seat to the medical practice of a certain female physician: my wife, Heather. We met when we worked together on the wards during residency in 1991; spent a year in rural Montana working together in clinics, ERs, and hospitals; shared the care of one another’s patients as our practices grew in parallel – hers in skilled nursing facilities, mine in the hospital; and reunited in recent years to work together as part of the same practice.
When I saw the paper by Yusuke Tsugawa, MD, MPH, PhD, and his associates showing lower mortality and readmission rates for female physicians versus their male counterparts, I began to wonder if the case of Heather’s practice style, and my observations of it, could help to interpret the findings of the study (JAMA Intern Med. 2016 Dec 19. doi: 10.1001/jamainternmed.2016.7875). The authors suggested that female physicians may produce better outcomes than male physicians.
The study in question, which analyzed more than 1.5 million hospitalizations, looked at Medicare beneficiaries hospitalized with a medical condition treated by general internists between 2011 and 2014. The authors found that patients treated by female physicians had lower 30-day mortality (adjusted rate, 11.07% vs. 11.49%, P<.001) and readmissions (adjusted rate, 15.02% vs. 15.57%, P<.001) than those treated by male physicians within the same hospital. The differences were “modest but important,” coauthor Ashish K. Jha, MD, MPH, wrote in his blog. Numbers needed to treat to prevent one death and one readmission were 233 and 182, respectively.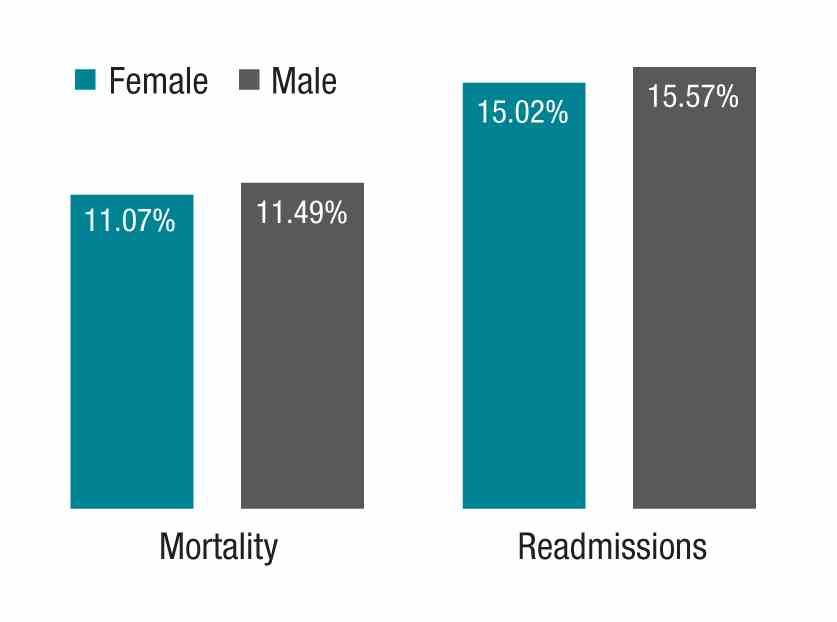
My observations of Heather’s practice approach, compared with my own, center around three main themes:
She spends more time considering her approach to a challenging case.
She has less urgency in deciding on a definitive course of action and more patience in sorting things out before proceeding with a diagnostic and therapeutic plan. She is more likely to leave open the possibility of changing her mind; she has less of a tendency to anchor on a particular diagnosis and treatment. Put another way, she is more willing to continue with ambiguous findings without lateralizing to one particular approach.
She brings more work-life balance to her professional responsibilities.
Despite being highly productive at work (and at home), she has worked less than full time throughout her career. This means that, during any given patient encounter, she is more likely to be unburdened by overwork and its negative consequences. It is my sense that many full-time physicians would be happier (and more effective) if they simply worked less. Heather has had the self-knowledge to take on a more manageable workload; the result is that she has remained joyous in practice for more than two decades.
She is less dogmatic and more willing to customize care based on the needs of the individual patient.
Although a good fund of knowledge is essential, if such knowledge obscures the physician’s ability to read the patient, then it is best abandoned, at least temporarily. Heather refers to the body of scientific evidence frequently, but she reserves an equal or greater portion of her cognitive bandwidth for the patient she is caring for at a particular moment.
How might the observations of this case study help to derive meaning from the study by Dr. Tsugawa and his associates, so that all patients may benefit from whatever it is that female physicians do to achieve better outcomes?
First, if physicians – regardless of gender – simply have an awareness of anchoring bias or rushing to land on a diagnosis or treatment, they will be less likely to do so in the future.
Next, we can learn that avoiding overwork can make for more joy in work, and if this is so, our patients may fare better. When I say “avoiding overwork,” that might mean rethinking our assumptions underlying the amount of work we take on.
Finally, while amassing a large fund of knowledge is a good thing, balancing medical knowledge with knowledge of the individual patient is crucial to good medical practice.
Dr. Whitcomb is Chief Medical Officer at Remedy Partners in Darien, CT. He is a cofounder and past president of SHM. Email him at wfwhit@comcast.net.
Week in, week out for the past 25 years, I have had a front-row seat to the medical practice of a certain female physician: my wife, Heather. We met when we worked together on the wards during residency in 1991; spent a year in rural Montana working together in clinics, ERs, and hospitals; shared the care of one another’s patients as our practices grew in parallel – hers in skilled nursing facilities, mine in the hospital; and reunited in recent years to work together as part of the same practice.
When I saw the paper by Yusuke Tsugawa, MD, MPH, PhD, and his associates showing lower mortality and readmission rates for female physicians versus their male counterparts, I began to wonder if the case of Heather’s practice style, and my observations of it, could help to interpret the findings of the study (JAMA Intern Med. 2016 Dec 19. doi: 10.1001/jamainternmed.2016.7875). The authors suggested that female physicians may produce better outcomes than male physicians.
The study in question, which analyzed more than 1.5 million hospitalizations, looked at Medicare beneficiaries hospitalized with a medical condition treated by general internists between 2011 and 2014. The authors found that patients treated by female physicians had lower 30-day mortality (adjusted rate, 11.07% vs. 11.49%, P<.001) and readmissions (adjusted rate, 15.02% vs. 15.57%, P<.001) than those treated by male physicians within the same hospital. The differences were “modest but important,” coauthor Ashish K. Jha, MD, MPH, wrote in his blog. Numbers needed to treat to prevent one death and one readmission were 233 and 182, respectively.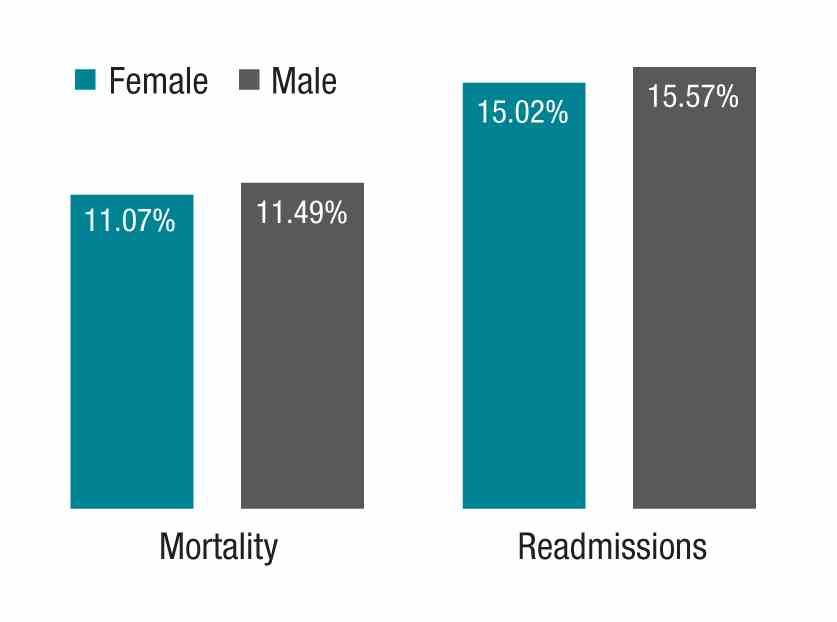
My observations of Heather’s practice approach, compared with my own, center around three main themes:
She spends more time considering her approach to a challenging case.
She has less urgency in deciding on a definitive course of action and more patience in sorting things out before proceeding with a diagnostic and therapeutic plan. She is more likely to leave open the possibility of changing her mind; she has less of a tendency to anchor on a particular diagnosis and treatment. Put another way, she is more willing to continue with ambiguous findings without lateralizing to one particular approach.
She brings more work-life balance to her professional responsibilities.
Despite being highly productive at work (and at home), she has worked less than full time throughout her career. This means that, during any given patient encounter, she is more likely to be unburdened by overwork and its negative consequences. It is my sense that many full-time physicians would be happier (and more effective) if they simply worked less. Heather has had the self-knowledge to take on a more manageable workload; the result is that she has remained joyous in practice for more than two decades.
She is less dogmatic and more willing to customize care based on the needs of the individual patient.
Although a good fund of knowledge is essential, if such knowledge obscures the physician’s ability to read the patient, then it is best abandoned, at least temporarily. Heather refers to the body of scientific evidence frequently, but she reserves an equal or greater portion of her cognitive bandwidth for the patient she is caring for at a particular moment.
How might the observations of this case study help to derive meaning from the study by Dr. Tsugawa and his associates, so that all patients may benefit from whatever it is that female physicians do to achieve better outcomes?
First, if physicians – regardless of gender – simply have an awareness of anchoring bias or rushing to land on a diagnosis or treatment, they will be less likely to do so in the future.
Next, we can learn that avoiding overwork can make for more joy in work, and if this is so, our patients may fare better. When I say “avoiding overwork,” that might mean rethinking our assumptions underlying the amount of work we take on.
Finally, while amassing a large fund of knowledge is a good thing, balancing medical knowledge with knowledge of the individual patient is crucial to good medical practice.
Dr. Whitcomb is Chief Medical Officer at Remedy Partners in Darien, CT. He is a cofounder and past president of SHM. Email him at wfwhit@comcast.net.
Hospital factors play key role in readmission risk after surgery
CORONADO, CALIF. – Variation in readmission risk across hospitals following certain surgical procedures is more attributable to hospital factors than to patient characteristics, results from a large analysis demonstrated.
Such is the impact of the care delivery macro environment (CDM), which Sarah A. Brownlee and coauthors defined as a series of complex interactions between patient characteristics and imposed hospital attributes than can impact patient outcomes postoperatively.
The purpose of the current study was to determine the relative contribution of various aspects of the CDM to 1-year readmission risk after surgery. Working with colleagues Anai Kothari, MD, and Paul Kuo MD, in the One:MAP Section of Clinical informatics and Analytics in the department of surgery at Loyola University Medical Center, Ms. Brownlee analyzed the Healthcare Cost and Utilization Project State Inpatient Databases from Florida, New York, and Washington between 2009 and 2013, which were linked to the American Hospital Association Annual Survey from that same time period.
The researchers used smoothed hazard estimates to determine all-cause readmission in the year after surgery, and multilevel survival models with shared frailty to determine the relative impact of hospital versus patient characteristics on the heterogeneity of readmission risk between hospitals. They limited the analysis to patients aged 18 years and older who underwent one the following procedures: abdominal aortic aneurysm repair, pancreatectomy, colectomy, coronary artery bypass graft, and total hip arthroplasty.
Ms. Brownlee reported results from 502,157 patients who underwent surgical procedures at 347 hospitals. The 1-year readmission rate was 23.5%, and ranged from 12% to 36% across procedures. After controlling for procedure, the researchers observed a 7.9% variation in readmission risk between hospitals. Staffing accounted for 9.8% of variance, followed by hospital structural characteristics such as teaching status and clinical programs (7.5%), patient ZIP code (3.8%), hospital perioperative resources such as inpatient rehab (2.9%), hospital volume (2.8%), and patient clinical characteristics (2.1%). The following hospital characteristics were significantly associated with a lower risk of 1-year readmission: high physician/bed ratio (hazard ratio 0.85; P = .00017); transplant status (HR 0.87; P = .022); high-income ZIP code (HR 0.89; P less than .001); high nurse bed/bed ratio (HR 0.90; P = .047), and cancer center designation (HR 0.93; P = .021).
“Compared to patient clinical characteristics, hospital factors such as staffing ratios, perioperative resources, and structural elements account for more variation in postoperative outcomes,” Ms. Brownlee concluded. “However, it’s important to note that in the present study, over 70% of variation in readmission rates is not explained by the covariates that we analyzed. It’s possible that there are other factors we need to consider. That’s where the direction of this research is going. Much of the variation in readmission risk across hospitals cannot be characterized with currently utilized administrative data.”
The National Institutes of Health provided funding for the study. Ms. Brownlee reported having no financial disclosures.
CORONADO, CALIF. – Variation in readmission risk across hospitals following certain surgical procedures is more attributable to hospital factors than to patient characteristics, results from a large analysis demonstrated.
Such is the impact of the care delivery macro environment (CDM), which Sarah A. Brownlee and coauthors defined as a series of complex interactions between patient characteristics and imposed hospital attributes than can impact patient outcomes postoperatively.
The purpose of the current study was to determine the relative contribution of various aspects of the CDM to 1-year readmission risk after surgery. Working with colleagues Anai Kothari, MD, and Paul Kuo MD, in the One:MAP Section of Clinical informatics and Analytics in the department of surgery at Loyola University Medical Center, Ms. Brownlee analyzed the Healthcare Cost and Utilization Project State Inpatient Databases from Florida, New York, and Washington between 2009 and 2013, which were linked to the American Hospital Association Annual Survey from that same time period.
The researchers used smoothed hazard estimates to determine all-cause readmission in the year after surgery, and multilevel survival models with shared frailty to determine the relative impact of hospital versus patient characteristics on the heterogeneity of readmission risk between hospitals. They limited the analysis to patients aged 18 years and older who underwent one the following procedures: abdominal aortic aneurysm repair, pancreatectomy, colectomy, coronary artery bypass graft, and total hip arthroplasty.
Ms. Brownlee reported results from 502,157 patients who underwent surgical procedures at 347 hospitals. The 1-year readmission rate was 23.5%, and ranged from 12% to 36% across procedures. After controlling for procedure, the researchers observed a 7.9% variation in readmission risk between hospitals. Staffing accounted for 9.8% of variance, followed by hospital structural characteristics such as teaching status and clinical programs (7.5%), patient ZIP code (3.8%), hospital perioperative resources such as inpatient rehab (2.9%), hospital volume (2.8%), and patient clinical characteristics (2.1%). The following hospital characteristics were significantly associated with a lower risk of 1-year readmission: high physician/bed ratio (hazard ratio 0.85; P = .00017); transplant status (HR 0.87; P = .022); high-income ZIP code (HR 0.89; P less than .001); high nurse bed/bed ratio (HR 0.90; P = .047), and cancer center designation (HR 0.93; P = .021).
“Compared to patient clinical characteristics, hospital factors such as staffing ratios, perioperative resources, and structural elements account for more variation in postoperative outcomes,” Ms. Brownlee concluded. “However, it’s important to note that in the present study, over 70% of variation in readmission rates is not explained by the covariates that we analyzed. It’s possible that there are other factors we need to consider. That’s where the direction of this research is going. Much of the variation in readmission risk across hospitals cannot be characterized with currently utilized administrative data.”
The National Institutes of Health provided funding for the study. Ms. Brownlee reported having no financial disclosures.
CORONADO, CALIF. – Variation in readmission risk across hospitals following certain surgical procedures is more attributable to hospital factors than to patient characteristics, results from a large analysis demonstrated.
Such is the impact of the care delivery macro environment (CDM), which Sarah A. Brownlee and coauthors defined as a series of complex interactions between patient characteristics and imposed hospital attributes than can impact patient outcomes postoperatively.
The purpose of the current study was to determine the relative contribution of various aspects of the CDM to 1-year readmission risk after surgery. Working with colleagues Anai Kothari, MD, and Paul Kuo MD, in the One:MAP Section of Clinical informatics and Analytics in the department of surgery at Loyola University Medical Center, Ms. Brownlee analyzed the Healthcare Cost and Utilization Project State Inpatient Databases from Florida, New York, and Washington between 2009 and 2013, which were linked to the American Hospital Association Annual Survey from that same time period.
The researchers used smoothed hazard estimates to determine all-cause readmission in the year after surgery, and multilevel survival models with shared frailty to determine the relative impact of hospital versus patient characteristics on the heterogeneity of readmission risk between hospitals. They limited the analysis to patients aged 18 years and older who underwent one the following procedures: abdominal aortic aneurysm repair, pancreatectomy, colectomy, coronary artery bypass graft, and total hip arthroplasty.
Ms. Brownlee reported results from 502,157 patients who underwent surgical procedures at 347 hospitals. The 1-year readmission rate was 23.5%, and ranged from 12% to 36% across procedures. After controlling for procedure, the researchers observed a 7.9% variation in readmission risk between hospitals. Staffing accounted for 9.8% of variance, followed by hospital structural characteristics such as teaching status and clinical programs (7.5%), patient ZIP code (3.8%), hospital perioperative resources such as inpatient rehab (2.9%), hospital volume (2.8%), and patient clinical characteristics (2.1%). The following hospital characteristics were significantly associated with a lower risk of 1-year readmission: high physician/bed ratio (hazard ratio 0.85; P = .00017); transplant status (HR 0.87; P = .022); high-income ZIP code (HR 0.89; P less than .001); high nurse bed/bed ratio (HR 0.90; P = .047), and cancer center designation (HR 0.93; P = .021).
“Compared to patient clinical characteristics, hospital factors such as staffing ratios, perioperative resources, and structural elements account for more variation in postoperative outcomes,” Ms. Brownlee concluded. “However, it’s important to note that in the present study, over 70% of variation in readmission rates is not explained by the covariates that we analyzed. It’s possible that there are other factors we need to consider. That’s where the direction of this research is going. Much of the variation in readmission risk across hospitals cannot be characterized with currently utilized administrative data.”
The National Institutes of Health provided funding for the study. Ms. Brownlee reported having no financial disclosures.
AT WSA 2016
Key clinical point:
Major finding: Staffing accounted for 9.8% of variance in readmission risk between hospitals, followed by hospital structural characteristics such as teaching status and clinical programs (7.5%).
Data source: Results from 502,157 patients who underwent surgical procedures at 347 hospitals in three states.
Disclosures: The National Institutes of Health provided funding for the study. Ms. Brownlee reported having no financial disclosures.
Tips for Improving Early Discharge Rates
Discharging patients before noon has many advantages: It creates open beds to accommodate the surge in admissions in the afternoon and helps minimize the bottleneck in system-wide patient flow, says Ragu P. Sanjeev, MD, unit-based medical director at Christiana Hospital in Newark, Del.
“Doing so can reduce ER wait times, reduce the percentage of patients leaving the ED without being seen—a safety issue for those patients—and also help to place the right patient in the right bed in a timely manner,” he says. “It’s a not just a patient flow issue; it’s a patient safety issue, as well.”
At his hospital, hospitalists developed a “Discharge by Appointment” process to address the issue systematically and completed a pilot project to test it. Their “‘Discharge by Appointment’ Improves Patient Flow, by Increasing Number of Discharges Before Noon,” was an abstract presented at HM16.1
“Giving patients that have a high predictability of being discharged next day, an appointment, and set off a series of steps to be completed the day before discharge including, notifying the transport team/family members of the appointment, helped improve the number of discharges before noon significantly,” according to the abstract.
Their successful pilot project has led to lasting changes, Dr. Sanjeev says. For about 16 months, the number of discharges before noon has been steadily increasing, helping the acute medicine service line perform better than its “Discharge by Noon” goal by 44.4% this fiscal year.
“As hospitalists, we have a great potential to positively impact the hospital-wide issues like patient flow and patient safety,” Dr. Sanjeev says. “By actively participating in important hospital committees, you can understand better and get inspired by the ongoing improvement efforts. By partnering with your care team, including bedside nurses, case managers, and social workers, we can make a big difference in early discharges. This success can be expanded to discharges throughout the day with appointments, thereby keeping the flow faucet open at all times.”
Reference
- Sanjeev R, McMillen J, Fedyk A. ‘discharge by Appointment’ Improves Patient Flow, by Increasing Number of Discharges Before Noon [abstract]. J Hosp Med. http://www.shmabstracts.com/abstract/discharge-by-appointment-improves-patient-flow-by-increasing-number-of-discharges-before-noon/. Accessed April 27, 2016.
Discharging patients before noon has many advantages: It creates open beds to accommodate the surge in admissions in the afternoon and helps minimize the bottleneck in system-wide patient flow, says Ragu P. Sanjeev, MD, unit-based medical director at Christiana Hospital in Newark, Del.
“Doing so can reduce ER wait times, reduce the percentage of patients leaving the ED without being seen—a safety issue for those patients—and also help to place the right patient in the right bed in a timely manner,” he says. “It’s a not just a patient flow issue; it’s a patient safety issue, as well.”
At his hospital, hospitalists developed a “Discharge by Appointment” process to address the issue systematically and completed a pilot project to test it. Their “‘Discharge by Appointment’ Improves Patient Flow, by Increasing Number of Discharges Before Noon,” was an abstract presented at HM16.1
“Giving patients that have a high predictability of being discharged next day, an appointment, and set off a series of steps to be completed the day before discharge including, notifying the transport team/family members of the appointment, helped improve the number of discharges before noon significantly,” according to the abstract.
Their successful pilot project has led to lasting changes, Dr. Sanjeev says. For about 16 months, the number of discharges before noon has been steadily increasing, helping the acute medicine service line perform better than its “Discharge by Noon” goal by 44.4% this fiscal year.
“As hospitalists, we have a great potential to positively impact the hospital-wide issues like patient flow and patient safety,” Dr. Sanjeev says. “By actively participating in important hospital committees, you can understand better and get inspired by the ongoing improvement efforts. By partnering with your care team, including bedside nurses, case managers, and social workers, we can make a big difference in early discharges. This success can be expanded to discharges throughout the day with appointments, thereby keeping the flow faucet open at all times.”
Reference
- Sanjeev R, McMillen J, Fedyk A. ‘discharge by Appointment’ Improves Patient Flow, by Increasing Number of Discharges Before Noon [abstract]. J Hosp Med. http://www.shmabstracts.com/abstract/discharge-by-appointment-improves-patient-flow-by-increasing-number-of-discharges-before-noon/. Accessed April 27, 2016.
Discharging patients before noon has many advantages: It creates open beds to accommodate the surge in admissions in the afternoon and helps minimize the bottleneck in system-wide patient flow, says Ragu P. Sanjeev, MD, unit-based medical director at Christiana Hospital in Newark, Del.
“Doing so can reduce ER wait times, reduce the percentage of patients leaving the ED without being seen—a safety issue for those patients—and also help to place the right patient in the right bed in a timely manner,” he says. “It’s a not just a patient flow issue; it’s a patient safety issue, as well.”
At his hospital, hospitalists developed a “Discharge by Appointment” process to address the issue systematically and completed a pilot project to test it. Their “‘Discharge by Appointment’ Improves Patient Flow, by Increasing Number of Discharges Before Noon,” was an abstract presented at HM16.1
“Giving patients that have a high predictability of being discharged next day, an appointment, and set off a series of steps to be completed the day before discharge including, notifying the transport team/family members of the appointment, helped improve the number of discharges before noon significantly,” according to the abstract.
Their successful pilot project has led to lasting changes, Dr. Sanjeev says. For about 16 months, the number of discharges before noon has been steadily increasing, helping the acute medicine service line perform better than its “Discharge by Noon” goal by 44.4% this fiscal year.
“As hospitalists, we have a great potential to positively impact the hospital-wide issues like patient flow and patient safety,” Dr. Sanjeev says. “By actively participating in important hospital committees, you can understand better and get inspired by the ongoing improvement efforts. By partnering with your care team, including bedside nurses, case managers, and social workers, we can make a big difference in early discharges. This success can be expanded to discharges throughout the day with appointments, thereby keeping the flow faucet open at all times.”
Reference
- Sanjeev R, McMillen J, Fedyk A. ‘discharge by Appointment’ Improves Patient Flow, by Increasing Number of Discharges Before Noon [abstract]. J Hosp Med. http://www.shmabstracts.com/abstract/discharge-by-appointment-improves-patient-flow-by-increasing-number-of-discharges-before-noon/. Accessed April 27, 2016.
Barriers to Achieving High Reliability
The conceptual models being used in healthcare’s efforts to achieve high reliability may have weaknesses, according to Marc T. Edwards, MD, MBA, author of “An Organizational Learning Framework for Patient Safety,” published in the American Journal of Medical Quality. Those weaknesses could explain why controversy over basic issues around the subject remain.
His paper analyzes those barriers to achieving high reliability in healthcare and points to a way forward—specifically, a different framework for identifying leverage points for improvement based on organizational learning theory.
“Organizations learn from others, from defects, from measurement, and from mindfulness,” he writes. “These learning modes correspond with contemporary themes of collaboration, no blame for human error, accountability for performance, and managing the unexpected. The collaborative model has dominated improvement efforts. Greater attention to the underdeveloped modes of organizational learning may foster more rapid progress in patient safety by increasing organizational capabilities, strengthening a culture of safety, and fixing more of the process problems that contribute to patient harm.”
To help bring this about, hospitalists can contribute by “embracing accountability for clinical performance, developing appropriate measures, and engaging in safety improvement activities — the most salient and important of which is reporting adverse events, near misses, and hazardous conditions affecting their own patients,” Dr. Edwards says. “This means taking responsibility for ending the culture of blame in healthcare, which currently blocks physicians from such self-reporting.”
He adds that hospitalists can do this by changing the model by which they conduct clinical peer review: Instead of focusing on whether individual physicians practiced according to standards, they could look broadly at learning opportunities for improvement in the system of care.
Reference
- Edwards MT. An organizational learning framework for patient safety [published online ahead of print February 25, 2016]. Am J Med Qual. pii:1062860616632295.
The conceptual models being used in healthcare’s efforts to achieve high reliability may have weaknesses, according to Marc T. Edwards, MD, MBA, author of “An Organizational Learning Framework for Patient Safety,” published in the American Journal of Medical Quality. Those weaknesses could explain why controversy over basic issues around the subject remain.
His paper analyzes those barriers to achieving high reliability in healthcare and points to a way forward—specifically, a different framework for identifying leverage points for improvement based on organizational learning theory.
“Organizations learn from others, from defects, from measurement, and from mindfulness,” he writes. “These learning modes correspond with contemporary themes of collaboration, no blame for human error, accountability for performance, and managing the unexpected. The collaborative model has dominated improvement efforts. Greater attention to the underdeveloped modes of organizational learning may foster more rapid progress in patient safety by increasing organizational capabilities, strengthening a culture of safety, and fixing more of the process problems that contribute to patient harm.”
To help bring this about, hospitalists can contribute by “embracing accountability for clinical performance, developing appropriate measures, and engaging in safety improvement activities — the most salient and important of which is reporting adverse events, near misses, and hazardous conditions affecting their own patients,” Dr. Edwards says. “This means taking responsibility for ending the culture of blame in healthcare, which currently blocks physicians from such self-reporting.”
He adds that hospitalists can do this by changing the model by which they conduct clinical peer review: Instead of focusing on whether individual physicians practiced according to standards, they could look broadly at learning opportunities for improvement in the system of care.
Reference
- Edwards MT. An organizational learning framework for patient safety [published online ahead of print February 25, 2016]. Am J Med Qual. pii:1062860616632295.
The conceptual models being used in healthcare’s efforts to achieve high reliability may have weaknesses, according to Marc T. Edwards, MD, MBA, author of “An Organizational Learning Framework for Patient Safety,” published in the American Journal of Medical Quality. Those weaknesses could explain why controversy over basic issues around the subject remain.
His paper analyzes those barriers to achieving high reliability in healthcare and points to a way forward—specifically, a different framework for identifying leverage points for improvement based on organizational learning theory.
“Organizations learn from others, from defects, from measurement, and from mindfulness,” he writes. “These learning modes correspond with contemporary themes of collaboration, no blame for human error, accountability for performance, and managing the unexpected. The collaborative model has dominated improvement efforts. Greater attention to the underdeveloped modes of organizational learning may foster more rapid progress in patient safety by increasing organizational capabilities, strengthening a culture of safety, and fixing more of the process problems that contribute to patient harm.”
To help bring this about, hospitalists can contribute by “embracing accountability for clinical performance, developing appropriate measures, and engaging in safety improvement activities — the most salient and important of which is reporting adverse events, near misses, and hazardous conditions affecting their own patients,” Dr. Edwards says. “This means taking responsibility for ending the culture of blame in healthcare, which currently blocks physicians from such self-reporting.”
He adds that hospitalists can do this by changing the model by which they conduct clinical peer review: Instead of focusing on whether individual physicians practiced according to standards, they could look broadly at learning opportunities for improvement in the system of care.
Reference
- Edwards MT. An organizational learning framework for patient safety [published online ahead of print February 25, 2016]. Am J Med Qual. pii:1062860616632295.
Video Feedback Can Be a Helpful Tool for QI, Patient Safety
Procedures are the most expensive item in healthcare, but tremendous variation remains in quality.
“In part that’ s because we have weak systems of peer support and in part because medicine sanctions a physician to do procedures, and then for the next 40 or 50 years, a surgeon can receive no input and not change their technique even though the field changes,” says Martin Makary, MD, MPH, professor of surgery and health policy and management at Johns Hopkins University in Baltimore.
Video could be used to address this, he suggests in an editorial called “Video Transparency: A Powerful Tool for Patient Safety and Quality Improvement” in the January 2016 BMJ Quality & Safety.
“In areas of excellence outside of medicine—football, aviation—they use video and video feedback for educational purposes. In healthcare, we can also use video to learn,” he says. “In surgical care, we can actually predict outcomes based on independent review of procedure video, but we just choose not to record videos because we don’ t have the infrastructure set up to provide feedback.”
When it has been done, he says, it’ s been received with enthusiasm. This doesn’ t mean cameras in primary-care clinics monitoring physicians.
“We’ re talking about the video-based procedures being recorded, not being erased with the next procedure that’ s done,” he says. “In the past, we couldn’ t do this with videotapes, but now with the capacity of memory and video data storage, there’ s an opportunity to leave the ‘ record’ button on on the video-based procedures that are already taking place.”
Reference
- Joo S, Xu T, Makary MA. Video transparency: a powerful tool for patient safety and quality improvement [published online ahead of print January 12, 2016]. BMJ Qual Saf,doi:10.1136/bmjqs-2015-005058.
Procedures are the most expensive item in healthcare, but tremendous variation remains in quality.
“In part that’ s because we have weak systems of peer support and in part because medicine sanctions a physician to do procedures, and then for the next 40 or 50 years, a surgeon can receive no input and not change their technique even though the field changes,” says Martin Makary, MD, MPH, professor of surgery and health policy and management at Johns Hopkins University in Baltimore.
Video could be used to address this, he suggests in an editorial called “Video Transparency: A Powerful Tool for Patient Safety and Quality Improvement” in the January 2016 BMJ Quality & Safety.
“In areas of excellence outside of medicine—football, aviation—they use video and video feedback for educational purposes. In healthcare, we can also use video to learn,” he says. “In surgical care, we can actually predict outcomes based on independent review of procedure video, but we just choose not to record videos because we don’ t have the infrastructure set up to provide feedback.”
When it has been done, he says, it’ s been received with enthusiasm. This doesn’ t mean cameras in primary-care clinics monitoring physicians.
“We’ re talking about the video-based procedures being recorded, not being erased with the next procedure that’ s done,” he says. “In the past, we couldn’ t do this with videotapes, but now with the capacity of memory and video data storage, there’ s an opportunity to leave the ‘ record’ button on on the video-based procedures that are already taking place.”
Reference
- Joo S, Xu T, Makary MA. Video transparency: a powerful tool for patient safety and quality improvement [published online ahead of print January 12, 2016]. BMJ Qual Saf,doi:10.1136/bmjqs-2015-005058.
Procedures are the most expensive item in healthcare, but tremendous variation remains in quality.
“In part that’ s because we have weak systems of peer support and in part because medicine sanctions a physician to do procedures, and then for the next 40 or 50 years, a surgeon can receive no input and not change their technique even though the field changes,” says Martin Makary, MD, MPH, professor of surgery and health policy and management at Johns Hopkins University in Baltimore.
Video could be used to address this, he suggests in an editorial called “Video Transparency: A Powerful Tool for Patient Safety and Quality Improvement” in the January 2016 BMJ Quality & Safety.
“In areas of excellence outside of medicine—football, aviation—they use video and video feedback for educational purposes. In healthcare, we can also use video to learn,” he says. “In surgical care, we can actually predict outcomes based on independent review of procedure video, but we just choose not to record videos because we don’ t have the infrastructure set up to provide feedback.”
When it has been done, he says, it’ s been received with enthusiasm. This doesn’ t mean cameras in primary-care clinics monitoring physicians.
“We’ re talking about the video-based procedures being recorded, not being erased with the next procedure that’ s done,” he says. “In the past, we couldn’ t do this with videotapes, but now with the capacity of memory and video data storage, there’ s an opportunity to leave the ‘ record’ button on on the video-based procedures that are already taking place.”
Reference
- Joo S, Xu T, Makary MA. Video transparency: a powerful tool for patient safety and quality improvement [published online ahead of print January 12, 2016]. BMJ Qual Saf,doi:10.1136/bmjqs-2015-005058.
Joint Commission Leaders Call on Physicians to Embrace Quality Improvement
In a May 12 JAMA “Viewpoint” article, Mark Chassin, MD, FACP, MPP, MPH, The Joint Commission’s president and CEO, and David Baker, MD, FACP, MPH, The Joint Commission’s vice president for healthcare quality evaluation, called on American physicians to acquire the necessary skills to take on new responsibilities to become leaders for QI and patient safety in an increasingly complex healthcare environment.1
The Joint Commission, they said, has embraced the tools, methods, and science of QI used in other industries, including Lean Six Sigma and change management, for all of its internal improvement functions and for its Center for Transforming Healthcare. They urge physicians to do the same or risk jeopardizing medicine’s long-standing self-governance status because of societal concerns about patient safety.
Drs. Chassin and Baker note that medicine has too often tolerated problematic behaviors and is viewed by some stakeholders as failing to address poor quality of care and safety, lack of access, and high costs of care.
“Physicians could make a much stronger case for continued self-government if they took a more visible and vigorous leadership role in efforts that led to major improvement in the quality and safety of patient care,” they said.
Reference
- Chassin MR, Baker DW. Aiming higher to enhance professionalism: beyond accreditation and certification. JAMA. 2015;313(18):1795-1796.
In a May 12 JAMA “Viewpoint” article, Mark Chassin, MD, FACP, MPP, MPH, The Joint Commission’s president and CEO, and David Baker, MD, FACP, MPH, The Joint Commission’s vice president for healthcare quality evaluation, called on American physicians to acquire the necessary skills to take on new responsibilities to become leaders for QI and patient safety in an increasingly complex healthcare environment.1
The Joint Commission, they said, has embraced the tools, methods, and science of QI used in other industries, including Lean Six Sigma and change management, for all of its internal improvement functions and for its Center for Transforming Healthcare. They urge physicians to do the same or risk jeopardizing medicine’s long-standing self-governance status because of societal concerns about patient safety.
Drs. Chassin and Baker note that medicine has too often tolerated problematic behaviors and is viewed by some stakeholders as failing to address poor quality of care and safety, lack of access, and high costs of care.
“Physicians could make a much stronger case for continued self-government if they took a more visible and vigorous leadership role in efforts that led to major improvement in the quality and safety of patient care,” they said.
Reference
- Chassin MR, Baker DW. Aiming higher to enhance professionalism: beyond accreditation and certification. JAMA. 2015;313(18):1795-1796.
In a May 12 JAMA “Viewpoint” article, Mark Chassin, MD, FACP, MPP, MPH, The Joint Commission’s president and CEO, and David Baker, MD, FACP, MPH, The Joint Commission’s vice president for healthcare quality evaluation, called on American physicians to acquire the necessary skills to take on new responsibilities to become leaders for QI and patient safety in an increasingly complex healthcare environment.1
The Joint Commission, they said, has embraced the tools, methods, and science of QI used in other industries, including Lean Six Sigma and change management, for all of its internal improvement functions and for its Center for Transforming Healthcare. They urge physicians to do the same or risk jeopardizing medicine’s long-standing self-governance status because of societal concerns about patient safety.
Drs. Chassin and Baker note that medicine has too often tolerated problematic behaviors and is viewed by some stakeholders as failing to address poor quality of care and safety, lack of access, and high costs of care.
“Physicians could make a much stronger case for continued self-government if they took a more visible and vigorous leadership role in efforts that led to major improvement in the quality and safety of patient care,” they said.
Reference
- Chassin MR, Baker DW. Aiming higher to enhance professionalism: beyond accreditation and certification. JAMA. 2015;313(18):1795-1796.
PHM15: New Quality Measures for Children with Medical Complexity
Pediatric Hospital Medicine 2015's keynote speaker, Rita Mangione-Smith, MD, MPH, reviewed quality measures being developed for medically complex patients by the Center of Excellence on Quality of Care Measures for Children with Complex Needs (COE4CCN). As one of the most challenging groups to not only provide care but to determine if the management provided brings value, the importance of quality measures was emphasized.
Dr. Mangione-Smith, of Seattle Children’s Hospital, reviewed the need for quality measures, as well as the process of developing these measures. Quality measures help to quantify outcomes from care practices, stated Dr. Mangione-Smith, to compare similar settings, and also to set possible benchmarks. The processes range from identifying and prioritizing measures to how they are validated as true value added outcomes. Data sources, sample size, and reliability/validity of the measures are considered important components to ensure that answers or results acquired are applicable and relevant to the population. Another important component is to clearly define a child with medical complexity.
Some reasons why medically complex patients require this focus:
- The low amount of information about their quality of care, investment, and need for coordination;
- Lack of understanding of which care practices make the biggest differences on their outcomes; and
- Their high rate of resource utilization.
The objective was to see which areas of care, such as care coordination, have the highest benefit/improvement on outcomes so as to prioritize resources more effectively. Dr. Mangione-Smith also touched on some obstacles and challenges, such as lack of insurance coverage leading to use of emergency resources as their primary care and its effect on increasing resource utilization.
Measures were determined via a multi-component methodology. Surveys using a binary and linear mean scoring tool were used. This provided multiple types of information such as assessing family’s perception of care, their understanding of medical information and care plans, and their accessibility to medical care services or information about their child.
Currently there is very little evidence on which management methods have the most significant, or any, effect on children with medical complexity. The use of quality measures to help guide which practices may have the highest positive impact on their outcomes greatly adds to the challenging care of this population and can be “used to assess quality of care coordination over time.” TH
Dr. Alvarez is a pediatric hospitalist and medical director of community hospital services at Children’s National Health System in Washington, D.C.
Pediatric Hospital Medicine 2015's keynote speaker, Rita Mangione-Smith, MD, MPH, reviewed quality measures being developed for medically complex patients by the Center of Excellence on Quality of Care Measures for Children with Complex Needs (COE4CCN). As one of the most challenging groups to not only provide care but to determine if the management provided brings value, the importance of quality measures was emphasized.
Dr. Mangione-Smith, of Seattle Children’s Hospital, reviewed the need for quality measures, as well as the process of developing these measures. Quality measures help to quantify outcomes from care practices, stated Dr. Mangione-Smith, to compare similar settings, and also to set possible benchmarks. The processes range from identifying and prioritizing measures to how they are validated as true value added outcomes. Data sources, sample size, and reliability/validity of the measures are considered important components to ensure that answers or results acquired are applicable and relevant to the population. Another important component is to clearly define a child with medical complexity.
Some reasons why medically complex patients require this focus:
- The low amount of information about their quality of care, investment, and need for coordination;
- Lack of understanding of which care practices make the biggest differences on their outcomes; and
- Their high rate of resource utilization.
The objective was to see which areas of care, such as care coordination, have the highest benefit/improvement on outcomes so as to prioritize resources more effectively. Dr. Mangione-Smith also touched on some obstacles and challenges, such as lack of insurance coverage leading to use of emergency resources as their primary care and its effect on increasing resource utilization.
Measures were determined via a multi-component methodology. Surveys using a binary and linear mean scoring tool were used. This provided multiple types of information such as assessing family’s perception of care, their understanding of medical information and care plans, and their accessibility to medical care services or information about their child.
Currently there is very little evidence on which management methods have the most significant, or any, effect on children with medical complexity. The use of quality measures to help guide which practices may have the highest positive impact on their outcomes greatly adds to the challenging care of this population and can be “used to assess quality of care coordination over time.” TH
Dr. Alvarez is a pediatric hospitalist and medical director of community hospital services at Children’s National Health System in Washington, D.C.
Pediatric Hospital Medicine 2015's keynote speaker, Rita Mangione-Smith, MD, MPH, reviewed quality measures being developed for medically complex patients by the Center of Excellence on Quality of Care Measures for Children with Complex Needs (COE4CCN). As one of the most challenging groups to not only provide care but to determine if the management provided brings value, the importance of quality measures was emphasized.
Dr. Mangione-Smith, of Seattle Children’s Hospital, reviewed the need for quality measures, as well as the process of developing these measures. Quality measures help to quantify outcomes from care practices, stated Dr. Mangione-Smith, to compare similar settings, and also to set possible benchmarks. The processes range from identifying and prioritizing measures to how they are validated as true value added outcomes. Data sources, sample size, and reliability/validity of the measures are considered important components to ensure that answers or results acquired are applicable and relevant to the population. Another important component is to clearly define a child with medical complexity.
Some reasons why medically complex patients require this focus:
- The low amount of information about their quality of care, investment, and need for coordination;
- Lack of understanding of which care practices make the biggest differences on their outcomes; and
- Their high rate of resource utilization.
The objective was to see which areas of care, such as care coordination, have the highest benefit/improvement on outcomes so as to prioritize resources more effectively. Dr. Mangione-Smith also touched on some obstacles and challenges, such as lack of insurance coverage leading to use of emergency resources as their primary care and its effect on increasing resource utilization.
Measures were determined via a multi-component methodology. Surveys using a binary and linear mean scoring tool were used. This provided multiple types of information such as assessing family’s perception of care, their understanding of medical information and care plans, and their accessibility to medical care services or information about their child.
Currently there is very little evidence on which management methods have the most significant, or any, effect on children with medical complexity. The use of quality measures to help guide which practices may have the highest positive impact on their outcomes greatly adds to the challenging care of this population and can be “used to assess quality of care coordination over time.” TH
Dr. Alvarez is a pediatric hospitalist and medical director of community hospital services at Children’s National Health System in Washington, D.C.
Startup Pharmacy Takes Mail-Order to Next Level, Could Solve Medication Management Issue for Millions
It only takes one idea to help change the face of medicine and, recently, Forbes posted an article outlining a small startup pharmacy that could change the way we get our medication. Manchester, N.H.-based Pill Pack takes the whole mail-order pharmacy to a new level.
Medication management can be a major issue for seniors and their caregivers. Seniors are at risk for such problems as overmedication and drug interactions, if medications are not properly managed.
An UpToDate article says that a survey for adults aged 57-85 shows:
- At least one prescription medication was used by 81%;
- Five or more prescription medications were used by 29% of the overall survey population and by 36% of people aged 75 to 85 years; and
- 46% of prescription users also took at least one over-the-counter medication.
Hospitalists see it every day; the readmit because prescribed medication isn’t taken correctly. Possibly, Pill Pack might be one step in the right direction. TH
Lisa Courtney is director of operations at Baptist Health Systems in Birmingham, Ala., and a member of Team Hospitalist.
It only takes one idea to help change the face of medicine and, recently, Forbes posted an article outlining a small startup pharmacy that could change the way we get our medication. Manchester, N.H.-based Pill Pack takes the whole mail-order pharmacy to a new level.
Medication management can be a major issue for seniors and their caregivers. Seniors are at risk for such problems as overmedication and drug interactions, if medications are not properly managed.
An UpToDate article says that a survey for adults aged 57-85 shows:
- At least one prescription medication was used by 81%;
- Five or more prescription medications were used by 29% of the overall survey population and by 36% of people aged 75 to 85 years; and
- 46% of prescription users also took at least one over-the-counter medication.
Hospitalists see it every day; the readmit because prescribed medication isn’t taken correctly. Possibly, Pill Pack might be one step in the right direction. TH
Lisa Courtney is director of operations at Baptist Health Systems in Birmingham, Ala., and a member of Team Hospitalist.
It only takes one idea to help change the face of medicine and, recently, Forbes posted an article outlining a small startup pharmacy that could change the way we get our medication. Manchester, N.H.-based Pill Pack takes the whole mail-order pharmacy to a new level.
Medication management can be a major issue for seniors and their caregivers. Seniors are at risk for such problems as overmedication and drug interactions, if medications are not properly managed.
An UpToDate article says that a survey for adults aged 57-85 shows:
- At least one prescription medication was used by 81%;
- Five or more prescription medications were used by 29% of the overall survey population and by 36% of people aged 75 to 85 years; and
- 46% of prescription users also took at least one over-the-counter medication.
Hospitalists see it every day; the readmit because prescribed medication isn’t taken correctly. Possibly, Pill Pack might be one step in the right direction. TH
Lisa Courtney is director of operations at Baptist Health Systems in Birmingham, Ala., and a member of Team Hospitalist.