User login
Sprout Pregnancy Essentials
An app to help your patient with chronic pelvic pain (February 2013)
An app to help your patient remember to take her OC (July 2012)
An app to help your patient lose weight (May 2012)
This handy toolkit helps mothers-to-be record important details like weight gain, kicks, and contraction times, with personalized timelines, checklists, comprehensive information about fetal development, and a journaling option.
In this series, I review what I call prescription apps—apps that you might consider recommending to your patient to enhance her medical care. Many patients are already looking at medical apps and want to hear your opinion. Often the free apps I recommend to patients are downloaded before they leave my office. When recommending apps, their cost (not necessarily a measure of quality or utility) and platform (device that the app has been designed for) should be taken into account. It is important to know whether the app you are recommending is supported by your patient’s smartphone.

For moms-to-be: quality information and a tracking tool
When I practiced obstetrics, my group provided patients with a pocket-sized, trifold pregnancy tracker at their first prenatal visit for them to bring to each subsequent appointment. In addition to data such as Rh status and estimated due date, blood pressure, weight, and fundal height were also recorded. The pregnancy tracker served two purposes: 1) a backup mini medical record in case their chart didn’t make it from the medical records department to the clinic on a particular day and 2) a keepsake.
Pregnancy apps take the concept of that little piece of cardboard to a whole new level. One highly rated pregnancy app is Sprout™ Pregnancy Essentials (recommended by Consumer Reports2 and named one of the 50 Best iPhone Apps in 2012 by Time magazine3) from Med ART Studios.4
With Sprout, the user enters her due date and the app automatically tracks the pregnancy week by week. Each time the app is accessed, the screen shows a realistic image of a developing fetus at the appropriate gestational age along with a pregnancy timeline. Tools allow the user to track her weight at each Ob visit. There is also a kick counter as well as a contraction timer for when the time comes.
Each week of the pregnancy is linked to medical information appropriate for the gestational age, such as second trimester screening at week 15 and group B streptococcus testing at week 35. The information is brief, but high-quality, and covers everything from prenatal testing and screening for gestational diabetes to stretch marks and carpal tunnel syndrome. From each topic, the user seamlessly can add preloaded questions to an “M.D. visit planner” or pregnancy-related tasks (such as making an appointment for a glucose challenge test) to a “to do” list.
A free version called Sprout Lite comes in English and Japanese. The premium version for $3.99 is available in English, Spanish, Chinese, German, Italian, Japanese, and Portuguese. The premium version is free of ads; has more advanced images of a developing fetus, with striking graphics; allows the user to share information via Facebook and e-mail; and has a timeline that adjusts to the baby’s gestational age. Both Sprout apps are currently only available for the iPhone and iPad.
Pros. Sprout is easy to use, has beautiful graphics, and the medical information is accurate and accessible. Sprout Lite contains the same high-quality information.
Cons. There is no way to track other medical data in addition to weight, such as fundal height, Rh status, or vaccinations. There is also a price tag to have the app be free of advertisements, get the best graphics, and have a more interactive user experience.
Verdict. It is always nice to be able to recommend a product with high-quality medical information. Sprout Lite always can be road tested first, but for those who live on Facebook, enjoy a more interactive product, hate advertisements, or love impressive graphics, the $3.99 may very well be worth it.
Keep a journal and create a book
While leaving the app with its data on the iPhone or iPad may be enough of a keepsake for some women, those who want to create a pregnancy book can obtain a separate Sprout Pregnancy Journal app-to-book™.5
This app allows the user to write journal entries, upload photos, and then, if desired, download a PDF of the journal or incorporate the beautiful images from the Sprout app to create a bound pregnancy journal (softcover: $19.95 for the first 40 pages; hardcover: $34.95 for the first 40 pages; additional charge for added pages).
The journal app is free to download for a 2-week trial. At the end of 2 weeks there is a choice:
- $4.99 to continue to use the app; includes cloud backup of data
- $7.99 to get cloud backup plus the PDF download (includes a discount for prepaying for the PDF plus $7.99 discount for a print book)
- If the $7.99 prepaid option isn’t chosen at the end of the 2-week trial, the PDF is $9.95.
The Sprout Pregnancy Journal app is available for iPhone, iPad Touch, and iPad.
We want to hear from you! Tell us what you think.
Why (and how) you should encourage your patients’ search for health information on the Web
(December 2011)
To blog or not to blog? What’s the answer for you and your practice?
(August 2011)
For better or, maybe worse, patients are judging your care online
(March 2011)
Twitter 101 for ObGyns: Pearls, pitfalls, and potential
(September 2010)
1. Smith A. Nearly half of American adults are Smartphone owners. Pew Internet & American Life Project. http://pewinternet.org/Reports/2012/Smartphone-Update-2012/Findings.aspx. Published March 1, 2012. Accessed August 14, 2012.
2. Morris N. App review: Sprout for iPad and iPhone. Consumer Reports Web site. http://news.consumerreports.org/baby/2011/10/app-review-sprout-for-ipad-and-iphone.html. Published October 10, 2011. Accessed August 13, 2012.
3. Peckham M. 50 best iPhone apps 2012: Pregnancy (Sprout). http://techland.time.com/2012/02/15/50-best-iphone-apps-2012/?iid=tl-article-mostpop1#all. Published February 15, 2012. Accessed August 13, 2012.
4. Sprout Pregnancy Essentials. Med ART Studios Web site. http://medart-studios.com/sprout-pregnancy-iphone-app/. Accessed August 13, 2012.
5. Sprout Pregnancy Journal. Med ART Studios Web site. http://medart-studios.com/sprout-pregnancy-journal-iphone-app/. Accessed August 13, 2012.
An app to help your patient with chronic pelvic pain (February 2013)
An app to help your patient remember to take her OC (July 2012)
An app to help your patient lose weight (May 2012)
This handy toolkit helps mothers-to-be record important details like weight gain, kicks, and contraction times, with personalized timelines, checklists, comprehensive information about fetal development, and a journaling option.
In this series, I review what I call prescription apps—apps that you might consider recommending to your patient to enhance her medical care. Many patients are already looking at medical apps and want to hear your opinion. Often the free apps I recommend to patients are downloaded before they leave my office. When recommending apps, their cost (not necessarily a measure of quality or utility) and platform (device that the app has been designed for) should be taken into account. It is important to know whether the app you are recommending is supported by your patient’s smartphone.

For moms-to-be: quality information and a tracking tool
When I practiced obstetrics, my group provided patients with a pocket-sized, trifold pregnancy tracker at their first prenatal visit for them to bring to each subsequent appointment. In addition to data such as Rh status and estimated due date, blood pressure, weight, and fundal height were also recorded. The pregnancy tracker served two purposes: 1) a backup mini medical record in case their chart didn’t make it from the medical records department to the clinic on a particular day and 2) a keepsake.
Pregnancy apps take the concept of that little piece of cardboard to a whole new level. One highly rated pregnancy app is Sprout™ Pregnancy Essentials (recommended by Consumer Reports2 and named one of the 50 Best iPhone Apps in 2012 by Time magazine3) from Med ART Studios.4
With Sprout, the user enters her due date and the app automatically tracks the pregnancy week by week. Each time the app is accessed, the screen shows a realistic image of a developing fetus at the appropriate gestational age along with a pregnancy timeline. Tools allow the user to track her weight at each Ob visit. There is also a kick counter as well as a contraction timer for when the time comes.
Each week of the pregnancy is linked to medical information appropriate for the gestational age, such as second trimester screening at week 15 and group B streptococcus testing at week 35. The information is brief, but high-quality, and covers everything from prenatal testing and screening for gestational diabetes to stretch marks and carpal tunnel syndrome. From each topic, the user seamlessly can add preloaded questions to an “M.D. visit planner” or pregnancy-related tasks (such as making an appointment for a glucose challenge test) to a “to do” list.
A free version called Sprout Lite comes in English and Japanese. The premium version for $3.99 is available in English, Spanish, Chinese, German, Italian, Japanese, and Portuguese. The premium version is free of ads; has more advanced images of a developing fetus, with striking graphics; allows the user to share information via Facebook and e-mail; and has a timeline that adjusts to the baby’s gestational age. Both Sprout apps are currently only available for the iPhone and iPad.
Pros. Sprout is easy to use, has beautiful graphics, and the medical information is accurate and accessible. Sprout Lite contains the same high-quality information.
Cons. There is no way to track other medical data in addition to weight, such as fundal height, Rh status, or vaccinations. There is also a price tag to have the app be free of advertisements, get the best graphics, and have a more interactive user experience.
Verdict. It is always nice to be able to recommend a product with high-quality medical information. Sprout Lite always can be road tested first, but for those who live on Facebook, enjoy a more interactive product, hate advertisements, or love impressive graphics, the $3.99 may very well be worth it.
Keep a journal and create a book
While leaving the app with its data on the iPhone or iPad may be enough of a keepsake for some women, those who want to create a pregnancy book can obtain a separate Sprout Pregnancy Journal app-to-book™.5
This app allows the user to write journal entries, upload photos, and then, if desired, download a PDF of the journal or incorporate the beautiful images from the Sprout app to create a bound pregnancy journal (softcover: $19.95 for the first 40 pages; hardcover: $34.95 for the first 40 pages; additional charge for added pages).
The journal app is free to download for a 2-week trial. At the end of 2 weeks there is a choice:
- $4.99 to continue to use the app; includes cloud backup of data
- $7.99 to get cloud backup plus the PDF download (includes a discount for prepaying for the PDF plus $7.99 discount for a print book)
- If the $7.99 prepaid option isn’t chosen at the end of the 2-week trial, the PDF is $9.95.
The Sprout Pregnancy Journal app is available for iPhone, iPad Touch, and iPad.
We want to hear from you! Tell us what you think.
Why (and how) you should encourage your patients’ search for health information on the Web
(December 2011)
To blog or not to blog? What’s the answer for you and your practice?
(August 2011)
For better or, maybe worse, patients are judging your care online
(March 2011)
Twitter 101 for ObGyns: Pearls, pitfalls, and potential
(September 2010)
An app to help your patient with chronic pelvic pain (February 2013)
An app to help your patient remember to take her OC (July 2012)
An app to help your patient lose weight (May 2012)
This handy toolkit helps mothers-to-be record important details like weight gain, kicks, and contraction times, with personalized timelines, checklists, comprehensive information about fetal development, and a journaling option.
In this series, I review what I call prescription apps—apps that you might consider recommending to your patient to enhance her medical care. Many patients are already looking at medical apps and want to hear your opinion. Often the free apps I recommend to patients are downloaded before they leave my office. When recommending apps, their cost (not necessarily a measure of quality or utility) and platform (device that the app has been designed for) should be taken into account. It is important to know whether the app you are recommending is supported by your patient’s smartphone.

For moms-to-be: quality information and a tracking tool
When I practiced obstetrics, my group provided patients with a pocket-sized, trifold pregnancy tracker at their first prenatal visit for them to bring to each subsequent appointment. In addition to data such as Rh status and estimated due date, blood pressure, weight, and fundal height were also recorded. The pregnancy tracker served two purposes: 1) a backup mini medical record in case their chart didn’t make it from the medical records department to the clinic on a particular day and 2) a keepsake.
Pregnancy apps take the concept of that little piece of cardboard to a whole new level. One highly rated pregnancy app is Sprout™ Pregnancy Essentials (recommended by Consumer Reports2 and named one of the 50 Best iPhone Apps in 2012 by Time magazine3) from Med ART Studios.4
With Sprout, the user enters her due date and the app automatically tracks the pregnancy week by week. Each time the app is accessed, the screen shows a realistic image of a developing fetus at the appropriate gestational age along with a pregnancy timeline. Tools allow the user to track her weight at each Ob visit. There is also a kick counter as well as a contraction timer for when the time comes.
Each week of the pregnancy is linked to medical information appropriate for the gestational age, such as second trimester screening at week 15 and group B streptococcus testing at week 35. The information is brief, but high-quality, and covers everything from prenatal testing and screening for gestational diabetes to stretch marks and carpal tunnel syndrome. From each topic, the user seamlessly can add preloaded questions to an “M.D. visit planner” or pregnancy-related tasks (such as making an appointment for a glucose challenge test) to a “to do” list.
A free version called Sprout Lite comes in English and Japanese. The premium version for $3.99 is available in English, Spanish, Chinese, German, Italian, Japanese, and Portuguese. The premium version is free of ads; has more advanced images of a developing fetus, with striking graphics; allows the user to share information via Facebook and e-mail; and has a timeline that adjusts to the baby’s gestational age. Both Sprout apps are currently only available for the iPhone and iPad.
Pros. Sprout is easy to use, has beautiful graphics, and the medical information is accurate and accessible. Sprout Lite contains the same high-quality information.
Cons. There is no way to track other medical data in addition to weight, such as fundal height, Rh status, or vaccinations. There is also a price tag to have the app be free of advertisements, get the best graphics, and have a more interactive user experience.
Verdict. It is always nice to be able to recommend a product with high-quality medical information. Sprout Lite always can be road tested first, but for those who live on Facebook, enjoy a more interactive product, hate advertisements, or love impressive graphics, the $3.99 may very well be worth it.
Keep a journal and create a book
While leaving the app with its data on the iPhone or iPad may be enough of a keepsake for some women, those who want to create a pregnancy book can obtain a separate Sprout Pregnancy Journal app-to-book™.5
This app allows the user to write journal entries, upload photos, and then, if desired, download a PDF of the journal or incorporate the beautiful images from the Sprout app to create a bound pregnancy journal (softcover: $19.95 for the first 40 pages; hardcover: $34.95 for the first 40 pages; additional charge for added pages).
The journal app is free to download for a 2-week trial. At the end of 2 weeks there is a choice:
- $4.99 to continue to use the app; includes cloud backup of data
- $7.99 to get cloud backup plus the PDF download (includes a discount for prepaying for the PDF plus $7.99 discount for a print book)
- If the $7.99 prepaid option isn’t chosen at the end of the 2-week trial, the PDF is $9.95.
The Sprout Pregnancy Journal app is available for iPhone, iPad Touch, and iPad.
We want to hear from you! Tell us what you think.
Why (and how) you should encourage your patients’ search for health information on the Web
(December 2011)
To blog or not to blog? What’s the answer for you and your practice?
(August 2011)
For better or, maybe worse, patients are judging your care online
(March 2011)
Twitter 101 for ObGyns: Pearls, pitfalls, and potential
(September 2010)
1. Smith A. Nearly half of American adults are Smartphone owners. Pew Internet & American Life Project. http://pewinternet.org/Reports/2012/Smartphone-Update-2012/Findings.aspx. Published March 1, 2012. Accessed August 14, 2012.
2. Morris N. App review: Sprout for iPad and iPhone. Consumer Reports Web site. http://news.consumerreports.org/baby/2011/10/app-review-sprout-for-ipad-and-iphone.html. Published October 10, 2011. Accessed August 13, 2012.
3. Peckham M. 50 best iPhone apps 2012: Pregnancy (Sprout). http://techland.time.com/2012/02/15/50-best-iphone-apps-2012/?iid=tl-article-mostpop1#all. Published February 15, 2012. Accessed August 13, 2012.
4. Sprout Pregnancy Essentials. Med ART Studios Web site. http://medart-studios.com/sprout-pregnancy-iphone-app/. Accessed August 13, 2012.
5. Sprout Pregnancy Journal. Med ART Studios Web site. http://medart-studios.com/sprout-pregnancy-journal-iphone-app/. Accessed August 13, 2012.
1. Smith A. Nearly half of American adults are Smartphone owners. Pew Internet & American Life Project. http://pewinternet.org/Reports/2012/Smartphone-Update-2012/Findings.aspx. Published March 1, 2012. Accessed August 14, 2012.
2. Morris N. App review: Sprout for iPad and iPhone. Consumer Reports Web site. http://news.consumerreports.org/baby/2011/10/app-review-sprout-for-ipad-and-iphone.html. Published October 10, 2011. Accessed August 13, 2012.
3. Peckham M. 50 best iPhone apps 2012: Pregnancy (Sprout). http://techland.time.com/2012/02/15/50-best-iphone-apps-2012/?iid=tl-article-mostpop1#all. Published February 15, 2012. Accessed August 13, 2012.
4. Sprout Pregnancy Essentials. Med ART Studios Web site. http://medart-studios.com/sprout-pregnancy-iphone-app/. Accessed August 13, 2012.
5. Sprout Pregnancy Journal. Med ART Studios Web site. http://medart-studios.com/sprout-pregnancy-journal-iphone-app/. Accessed August 13, 2012.
An app to help your patient lose weight
HAVE YOU SEEN THESE OTHER APP REVIEWS BY DR. GUNTER?
An app to help your patient with chronic pelvic pain (February 2013)
Sprout Pregnancy Essentials: An app to help your patient track her pregnancy (September 2012)
An app to help your patient remember to take her OC (July 2012)
The increasing use of smartphones among women presents an opportunity to address health issues, such as obesity.
Forty-four percent of US women own a smartphone, according to the latest data.1 Ownership is highest among younger women, with more than 60% of women between the ages of 18 and 34 owning one of these devices.1
One of the features that makes a smartphone, well, smart is the ability to run apps (short for software “applications”). Apps started out as ways to enhance access to email or calendars, but the market has ex-ploded—both demand and supply—so that there are now apps for essentially anything you might ever need. Apple’s app store, the largest, boasts more than 500,000 apps, and more than 25 billion apps had been downloaded by March 2012.2 Medical app developers are keen to capitalize on our ever-increasing “app”-etite.
Medical apps can be divided into two categories: those that can help the patient and those that can help the provider. This series will review what I call prescription apps—in other words, apps that you might consider recommending to your patient to enhance her medical care.
Apps are not new to your patients
Many of your patients are already looking at medical apps and want to hear your opinion. I know that my smartphone users are uniformly interested in hearing my recommendations, and it is not uncommon that the free apps I recommend are downloaded before my patient leaves the office.
If you are not an app user yourself, there are two basic things that you should know. First, some apps are free and others are not, although that is not necessarily a measure of quality or utility. Second, apps must be written for the particular device, so it is important to know whether the app you are recommending is supported by your patient’s smartphone. As of February 2012, the most common devices are the Android (20% of cell phone users), iPhone (19%), and Blackberry (6%).1 Some apps can also be used on tablets (e.g., iPad, Galaxy) and e-book readers (e.g., Nook, Kindle). Use of these devices is also increasing; currently, 29% of Americans own either a tablet or an e-book reader.3

When the clinical need is weight loss
Lose It! is a weight-management app that tracks calories, exercise, and weight. Considering that more than 30% of US women are obese, working toward a healthy weight is a common office discussion and any additional tool is wel-come.4 Journaling, or recording every single thing that is eaten, is a key component of successful dieting. Smartphone users tend to have their phones with them wherever they are, so an app is an ideal tool for the journaling commitment needed for weight loss.
Lose It! is free and works on the following platforms:
- Android
- iPhone
- iPad
- Nook Color
- Nook Tablet.
Advantages include ease of use
The patient need only enter her current weight and height (measure your patient during the visit to ensure that she gets started with accurate numbers), the weight she hopes to attain (you can discuss this as well), and how many pounds she hopes to lose each week, and the app calculates the recommended calorie intake to achieve this goal. The app comes preloaded with thousands of foods, and it enables barcode scanning to upload the food and nutritional content with just a click of the phone’s camera.
The database can be expanded by adding unlisted foods and even recipes. Synchronizing the phone with Loseit.com allows for emailed summaries and reminders when the patient forgets to log a meal. There is also a wide repository of exercises to choose from when logging an activity.
A couple of cons
There is no Lose It! app for the Blackberry—and no plans to write one.
Another disadvantage is the extremely basic exercise journaling (no weekly or review function), and exercise calories are automatically added into the user’s daily allotment—not every dieter wants their calories set up this way.
This is the app I used to journal my 50-lb weight loss (and 6 months of maintenance). I think that testimonial speaks for itself.
In the next installment: an app that reminds your patient to take her birth control pills.
- Why (and how) you should encourage your patients' search for health information on the Web (December 2011)
- Does the risk of unplanned pregnancy outweight the risk of VTE from hormonal contraception? (Guest Editorial, October 2012)
- To blog or not to blog? What's the answer for you and your practice? (August 2011)
- For better or, maybe worse, patients are judging your care online (March 2011)
- Twitter 101 for ObGyns: Pearls, pitfalls, and potential (September 2010)
We want to hear from you! Tell us what you think.
1. Pew Internet & American Life Project. Nearly half of American adults are Smartphone owners. http://pewinternet.org/Reports/2012/Smartphone-Update-2012/Findings.aspx. Accessed April 9, 2012.
2. Apple app store downloads top 25 billion [press release]. http://www.apple.com/pr/library/2012/03/05Apples-App-Store-Downloads-Top-25-Billion.html. Accessed April 9, 2012 .
3. Pew Internet & American Life Project. Tablet and e-book reader ownership nearly doubled over the holiday gift-giving period. http://libraries.pewinternet.org/2012/01/23/tablet-and-e-book-reader-ownership-nearly-double-over-the-holiday-gift-giving-period/. Accessed April 9, 2012.
4. National Center for Health Statistics. Obesity in the United States, 2009–2010. NCHS Data Brief No. 82; January 2012.
HAVE YOU SEEN THESE OTHER APP REVIEWS BY DR. GUNTER?
An app to help your patient with chronic pelvic pain (February 2013)
Sprout Pregnancy Essentials: An app to help your patient track her pregnancy (September 2012)
An app to help your patient remember to take her OC (July 2012)
The increasing use of smartphones among women presents an opportunity to address health issues, such as obesity.
Forty-four percent of US women own a smartphone, according to the latest data.1 Ownership is highest among younger women, with more than 60% of women between the ages of 18 and 34 owning one of these devices.1
One of the features that makes a smartphone, well, smart is the ability to run apps (short for software “applications”). Apps started out as ways to enhance access to email or calendars, but the market has ex-ploded—both demand and supply—so that there are now apps for essentially anything you might ever need. Apple’s app store, the largest, boasts more than 500,000 apps, and more than 25 billion apps had been downloaded by March 2012.2 Medical app developers are keen to capitalize on our ever-increasing “app”-etite.
Medical apps can be divided into two categories: those that can help the patient and those that can help the provider. This series will review what I call prescription apps—in other words, apps that you might consider recommending to your patient to enhance her medical care.
Apps are not new to your patients
Many of your patients are already looking at medical apps and want to hear your opinion. I know that my smartphone users are uniformly interested in hearing my recommendations, and it is not uncommon that the free apps I recommend are downloaded before my patient leaves the office.
If you are not an app user yourself, there are two basic things that you should know. First, some apps are free and others are not, although that is not necessarily a measure of quality or utility. Second, apps must be written for the particular device, so it is important to know whether the app you are recommending is supported by your patient’s smartphone. As of February 2012, the most common devices are the Android (20% of cell phone users), iPhone (19%), and Blackberry (6%).1 Some apps can also be used on tablets (e.g., iPad, Galaxy) and e-book readers (e.g., Nook, Kindle). Use of these devices is also increasing; currently, 29% of Americans own either a tablet or an e-book reader.3

When the clinical need is weight loss
Lose It! is a weight-management app that tracks calories, exercise, and weight. Considering that more than 30% of US women are obese, working toward a healthy weight is a common office discussion and any additional tool is wel-come.4 Journaling, or recording every single thing that is eaten, is a key component of successful dieting. Smartphone users tend to have their phones with them wherever they are, so an app is an ideal tool for the journaling commitment needed for weight loss.
Lose It! is free and works on the following platforms:
- Android
- iPhone
- iPad
- Nook Color
- Nook Tablet.
Advantages include ease of use
The patient need only enter her current weight and height (measure your patient during the visit to ensure that she gets started with accurate numbers), the weight she hopes to attain (you can discuss this as well), and how many pounds she hopes to lose each week, and the app calculates the recommended calorie intake to achieve this goal. The app comes preloaded with thousands of foods, and it enables barcode scanning to upload the food and nutritional content with just a click of the phone’s camera.
The database can be expanded by adding unlisted foods and even recipes. Synchronizing the phone with Loseit.com allows for emailed summaries and reminders when the patient forgets to log a meal. There is also a wide repository of exercises to choose from when logging an activity.
A couple of cons
There is no Lose It! app for the Blackberry—and no plans to write one.
Another disadvantage is the extremely basic exercise journaling (no weekly or review function), and exercise calories are automatically added into the user’s daily allotment—not every dieter wants their calories set up this way.
This is the app I used to journal my 50-lb weight loss (and 6 months of maintenance). I think that testimonial speaks for itself.
In the next installment: an app that reminds your patient to take her birth control pills.
- Why (and how) you should encourage your patients' search for health information on the Web (December 2011)
- Does the risk of unplanned pregnancy outweight the risk of VTE from hormonal contraception? (Guest Editorial, October 2012)
- To blog or not to blog? What's the answer for you and your practice? (August 2011)
- For better or, maybe worse, patients are judging your care online (March 2011)
- Twitter 101 for ObGyns: Pearls, pitfalls, and potential (September 2010)
We want to hear from you! Tell us what you think.
HAVE YOU SEEN THESE OTHER APP REVIEWS BY DR. GUNTER?
An app to help your patient with chronic pelvic pain (February 2013)
Sprout Pregnancy Essentials: An app to help your patient track her pregnancy (September 2012)
An app to help your patient remember to take her OC (July 2012)
The increasing use of smartphones among women presents an opportunity to address health issues, such as obesity.
Forty-four percent of US women own a smartphone, according to the latest data.1 Ownership is highest among younger women, with more than 60% of women between the ages of 18 and 34 owning one of these devices.1
One of the features that makes a smartphone, well, smart is the ability to run apps (short for software “applications”). Apps started out as ways to enhance access to email or calendars, but the market has ex-ploded—both demand and supply—so that there are now apps for essentially anything you might ever need. Apple’s app store, the largest, boasts more than 500,000 apps, and more than 25 billion apps had been downloaded by March 2012.2 Medical app developers are keen to capitalize on our ever-increasing “app”-etite.
Medical apps can be divided into two categories: those that can help the patient and those that can help the provider. This series will review what I call prescription apps—in other words, apps that you might consider recommending to your patient to enhance her medical care.
Apps are not new to your patients
Many of your patients are already looking at medical apps and want to hear your opinion. I know that my smartphone users are uniformly interested in hearing my recommendations, and it is not uncommon that the free apps I recommend are downloaded before my patient leaves the office.
If you are not an app user yourself, there are two basic things that you should know. First, some apps are free and others are not, although that is not necessarily a measure of quality or utility. Second, apps must be written for the particular device, so it is important to know whether the app you are recommending is supported by your patient’s smartphone. As of February 2012, the most common devices are the Android (20% of cell phone users), iPhone (19%), and Blackberry (6%).1 Some apps can also be used on tablets (e.g., iPad, Galaxy) and e-book readers (e.g., Nook, Kindle). Use of these devices is also increasing; currently, 29% of Americans own either a tablet or an e-book reader.3

When the clinical need is weight loss
Lose It! is a weight-management app that tracks calories, exercise, and weight. Considering that more than 30% of US women are obese, working toward a healthy weight is a common office discussion and any additional tool is wel-come.4 Journaling, or recording every single thing that is eaten, is a key component of successful dieting. Smartphone users tend to have their phones with them wherever they are, so an app is an ideal tool for the journaling commitment needed for weight loss.
Lose It! is free and works on the following platforms:
- Android
- iPhone
- iPad
- Nook Color
- Nook Tablet.
Advantages include ease of use
The patient need only enter her current weight and height (measure your patient during the visit to ensure that she gets started with accurate numbers), the weight she hopes to attain (you can discuss this as well), and how many pounds she hopes to lose each week, and the app calculates the recommended calorie intake to achieve this goal. The app comes preloaded with thousands of foods, and it enables barcode scanning to upload the food and nutritional content with just a click of the phone’s camera.
The database can be expanded by adding unlisted foods and even recipes. Synchronizing the phone with Loseit.com allows for emailed summaries and reminders when the patient forgets to log a meal. There is also a wide repository of exercises to choose from when logging an activity.
A couple of cons
There is no Lose It! app for the Blackberry—and no plans to write one.
Another disadvantage is the extremely basic exercise journaling (no weekly or review function), and exercise calories are automatically added into the user’s daily allotment—not every dieter wants their calories set up this way.
This is the app I used to journal my 50-lb weight loss (and 6 months of maintenance). I think that testimonial speaks for itself.
In the next installment: an app that reminds your patient to take her birth control pills.
- Why (and how) you should encourage your patients' search for health information on the Web (December 2011)
- Does the risk of unplanned pregnancy outweight the risk of VTE from hormonal contraception? (Guest Editorial, October 2012)
- To blog or not to blog? What's the answer for you and your practice? (August 2011)
- For better or, maybe worse, patients are judging your care online (March 2011)
- Twitter 101 for ObGyns: Pearls, pitfalls, and potential (September 2010)
We want to hear from you! Tell us what you think.
1. Pew Internet & American Life Project. Nearly half of American adults are Smartphone owners. http://pewinternet.org/Reports/2012/Smartphone-Update-2012/Findings.aspx. Accessed April 9, 2012.
2. Apple app store downloads top 25 billion [press release]. http://www.apple.com/pr/library/2012/03/05Apples-App-Store-Downloads-Top-25-Billion.html. Accessed April 9, 2012 .
3. Pew Internet & American Life Project. Tablet and e-book reader ownership nearly doubled over the holiday gift-giving period. http://libraries.pewinternet.org/2012/01/23/tablet-and-e-book-reader-ownership-nearly-double-over-the-holiday-gift-giving-period/. Accessed April 9, 2012.
4. National Center for Health Statistics. Obesity in the United States, 2009–2010. NCHS Data Brief No. 82; January 2012.
1. Pew Internet & American Life Project. Nearly half of American adults are Smartphone owners. http://pewinternet.org/Reports/2012/Smartphone-Update-2012/Findings.aspx. Accessed April 9, 2012.
2. Apple app store downloads top 25 billion [press release]. http://www.apple.com/pr/library/2012/03/05Apples-App-Store-Downloads-Top-25-Billion.html. Accessed April 9, 2012 .
3. Pew Internet & American Life Project. Tablet and e-book reader ownership nearly doubled over the holiday gift-giving period. http://libraries.pewinternet.org/2012/01/23/tablet-and-e-book-reader-ownership-nearly-double-over-the-holiday-gift-giving-period/. Accessed April 9, 2012.
4. National Center for Health Statistics. Obesity in the United States, 2009–2010. NCHS Data Brief No. 82; January 2012.
Does the risk of unplanned pregnancy outweigh the risk of VTE from hormonal contraception?
Let’s increase our use of IUDs and improve contraceptive effectiveness in this country
Robert L. Barbieri, MD (Editorial, August 2012)
Let’s increase our use of implants and DMPA and improve contraceptive effectiveness in this country
Robert L. Barbieri, MD (Editorial, September 2012)
It is well established that combined hormonal contraception increases the risk of venous thromboembolism (VTE), both deep venous thrombosis (DVT) and pulmonary embolism (PE).1 Concerns exist that drospirenone-containing combined oral contraceptives (OCs), the norelgestromin patch, and the etonogestrel vaginal ring may increase the risk of VTE, compared with second-generation OCs, although results from studies evaluating the thromboembolic risk of these products are conflicting.1,2
An April 2012 safety communication from the US Food and Drug Administration (FDA) reported that “drospirenone-containing birth control pills may be associated with a higher risk for blood clots than other progestin-containing pills.”3 These pills now carry revised drug labels stating that epidemiologic studies that compared the risk of VTE reported that the risk ranged from no increase to a three-fold increase.3
Together, these studies and the FDA warning have garnered a lot of publicity and caused confusion and concern, leading both patients and providers to ask, “Are these specific products really safe?”
What is the baseline risk?
For nonusers of hormonal contraception, the baseline risk of VTE is 1 to 5 events per 10,000 woman-years.1,3-5 Variables that increase a woman’s risk of VTE include1:
- advanced age
- obesity
- immobility
- hematologic disorders
- pregnancy.
Estrogen-containing OCs with second-generation progestins (levonorgestrel, norgestimate, and norethindrone) have a risk of VTE of approximately 3 to 9 events per 10,000 woman-years.1,3-5
When study results conflict
The relative risk of VTE associated with drospirenone-containing OCs, compared with second-generation pills, ranges from 0.9 to 3.3. The relative risk is 1.2 to 2.2 for the norelgestromin patch, and 1.6 to 1.9 for the etonogestrel ring.1-4
All of the studies addressing the increased risk of VTE with drospirenone, the patch, and the ring have some limitations, such as the use of retrospective data, selection bias, study design, or inclusion of multiple pill regimens. However, most of the studies that found no association between these methods and VTE were industry-funded.2 Criticisms of these studies have led to disagreement about the risk; it is unclear whether a definitive study ever can be designed and performed.2
Worst-case scenario. Using data from only those studies that show an increased risk of VTE, the increased number of VTE events above that conferred by a second-generation progestin would be approximately2:
- ring: 3–5/10,000 woman-years
- patch: 3–8/10,000 woman-years
- drospirenone pill: 5–10/10,000 woman-years (risk may be highest in the first year of use3).
Adding perspective
The risks of hormonal contraception must be weighed against the consequences of using no contraception: 43 million women in the United States are sexually active but do not wish to become pregnant. Without contraception, 85% will be pregnant within 1 year.6 The risk of mortality during pregnancy in the United States is 1.8 deaths per 10,000 live births (5.5 deaths per 10,000 live births for women older than 39 years).7The prevalence of VTE during pregnancy is 5 to 29 events per 10,000 women; during the postpartum period, the prevalence is 40 to 65 events per 10,000 women (although some quote the VTE risk during the postpartum period to be as high as 200 to 400 events per 10,000 women).3,5,8
An unplanned pregnancy is more likely than a planned pregnancy to have a poor perinatal outcome or to end in abortion. The socioeconomic benefits of planning pregnancies must also be considered.

Hormonal contraception confers benefits beyond the prevention of pregnancy. In addition to a 50% reduction in the rate of endometrial cancer and a 27% reduction in the rate of ovarian cancer (and an even greater reduction for women who take OCs longer than 5 years), there are other benefits to hormonal contraception, such as reduced acne, dysmenorrhea, and menorrhagia.9
Individualize your care
When choosing a method of contraception, it is important not only to consider thromboembolic risk but also:
- previous contraceptive experiences
- previous pregnancies
- patient preference
- efficacy
- individual health factors
- cost.
For instance, even though the risk of VTE may be slightly increased among women using the norelgestromin patch, compliance rates are higher with the patch than with the pill.10 A woman with two unplanned pregnancies while taking the pill who reports having difficulty adhering to a daily regimen is a different patch candidate than a woman who has successfully planned two pregnancies using OCs.
For many women, a weekly or monthly reversible contraceptive is the most desirable method. In addition to these more quantifiable factors, some women prefer a specific brand of pill or delivery method—and satisfaction is a key component of contraception adherence.
Educate your patient
I favor the approach of providing as much data as possible. Patients may read the black box warning in the package inserts for drospirenone-containing pills or the norelgestromin patch, find news sources that inaccurately report risk to garner the most compelling headline, or stumble across plaintiff’s lawyers advertising lawsuits for drospirenone-containing pills, the contraceptive ring, and the patch. I can best counter confusion or misinformation by providing accurate information and putting possible risks into perspective up front. I now explain that the risk for VTE may be higher with certain pills, the ring, and the patch, but there just aren’t enough high-quality data to be certain. I also explain that risk may mean different things for different patients, based on medical history and previous experiences. I have found that my patients appreciate the full disclosure.
Overall, the benefits of combined hormonal contraception with all methods outweigh the risk of VTE. In addition, issues related to switching contraceptive methods may increase the risk of an unplanned pregnancy. In 1995, when the United Kingdom warned that desogestrel pills carried an increased risk of VTE but were still “safe,” the incidence of unplanned pregnancies and abortions increased.2,11 The data regarding the risk of VTE associated with drospirenone, the patch, and the ring should not be an impetus for sweeping generalizations, but rather an opportunity to educate our patients (and ourselves) and to further individualize care.
Do you agree that the benefits of combined hormonal contraception with all methods outweigh the VTE risk? Why or why not? What do you do in your practice? Click here
Click here to find additional articles on contraception published in OBG Management
in 2012.
1. Lidegaard Ø, Milsom I, Geirsson R, Skjeldestad F. Hormonal contraception and venous thromboembolism. Acta Obstet Gynecol Scand. 2012;91(7):769-778.
2. Raymond EG, Burke AE, Espey E. Combined hormonal contraceptives and venous thromboembolism: putting the risks into perspective. Obstet Gynecol. 2012;119(5):1039-1044.
3. US Food and Drug Administration. Safety Announcement. Updated information about the risk of blood clots in women taking birth control pills containing drospirenone. http://www.fda.gov/Drugs/DrugSafety/ucm299305.htm. Published April 10 2012. Accessed September 11, 2012.
4. Lidegaard Ø, Nielsen L, Skovlund C, Løkkegaard E. Venous thrombosis in users of non-oral hormonal contraception: follow-up study Denmark 2001-10 [published online ahead of print May 10, 2012]. BMJ. 2012:344-353:e2990. doi: 10.1136 /bmj.e2990.
5. Oral contraceptives and the risk of thromboembolism: an update. Clinical practice Guideline No. 252. Society of Obstetricians and Gynaecologists of Canada. 2010;252. http://www.sogc.org/guidelines/documents/gui252CPG1012E.pdf. Accessed September 5, 2012.
6. Fact Sheet Contraceptive use in the United States. Guttmacher Institute. http://www.guttmacher.org/pubs/fb_contr_use.html. Published July 2012. Accessed September 5 2012.
7. Berg CJ, Callaghan WM, Syverson C, Henderson Z. Pregnancy related mortality in the United States 1998 to 2005. Obstet Gynecol. 2010;116(6):1302-1309.
8. James A. Committee on Practice Bulletins-Obstetrics. ACOG Practice Bulletin No. 123. Thromboembolism in pregnancy. Obstet Gynecol. 2011;118(3):718-729.
9. Committee on Practice Bulletins-Gynecology. ACOG Practice Bulletin No. 110. Noncontraceptive uses of hormonal contraception. Obstet Gynecol. 2010;115(1):206-218.
10. Archer DF, Bigrigg A, Smallwood GH, Shangold GA, Creasy GW, Fisher AC. Assessment of compliance with a weekly contraceptive patch (OrthoEvra/Evra) among North American women. Fertil Steril. 2002;77(2 suppl 2):S27-S31.
11. Furedi A. The public health implications of the 1995 ‘pill scare.’ Hum Reprod Update. 1999;5(6):621-626.
Let’s increase our use of IUDs and improve contraceptive effectiveness in this country
Robert L. Barbieri, MD (Editorial, August 2012)
Let’s increase our use of implants and DMPA and improve contraceptive effectiveness in this country
Robert L. Barbieri, MD (Editorial, September 2012)
It is well established that combined hormonal contraception increases the risk of venous thromboembolism (VTE), both deep venous thrombosis (DVT) and pulmonary embolism (PE).1 Concerns exist that drospirenone-containing combined oral contraceptives (OCs), the norelgestromin patch, and the etonogestrel vaginal ring may increase the risk of VTE, compared with second-generation OCs, although results from studies evaluating the thromboembolic risk of these products are conflicting.1,2
An April 2012 safety communication from the US Food and Drug Administration (FDA) reported that “drospirenone-containing birth control pills may be associated with a higher risk for blood clots than other progestin-containing pills.”3 These pills now carry revised drug labels stating that epidemiologic studies that compared the risk of VTE reported that the risk ranged from no increase to a three-fold increase.3
Together, these studies and the FDA warning have garnered a lot of publicity and caused confusion and concern, leading both patients and providers to ask, “Are these specific products really safe?”
What is the baseline risk?
For nonusers of hormonal contraception, the baseline risk of VTE is 1 to 5 events per 10,000 woman-years.1,3-5 Variables that increase a woman’s risk of VTE include1:
- advanced age
- obesity
- immobility
- hematologic disorders
- pregnancy.
Estrogen-containing OCs with second-generation progestins (levonorgestrel, norgestimate, and norethindrone) have a risk of VTE of approximately 3 to 9 events per 10,000 woman-years.1,3-5
When study results conflict
The relative risk of VTE associated with drospirenone-containing OCs, compared with second-generation pills, ranges from 0.9 to 3.3. The relative risk is 1.2 to 2.2 for the norelgestromin patch, and 1.6 to 1.9 for the etonogestrel ring.1-4
All of the studies addressing the increased risk of VTE with drospirenone, the patch, and the ring have some limitations, such as the use of retrospective data, selection bias, study design, or inclusion of multiple pill regimens. However, most of the studies that found no association between these methods and VTE were industry-funded.2 Criticisms of these studies have led to disagreement about the risk; it is unclear whether a definitive study ever can be designed and performed.2
Worst-case scenario. Using data from only those studies that show an increased risk of VTE, the increased number of VTE events above that conferred by a second-generation progestin would be approximately2:
- ring: 3–5/10,000 woman-years
- patch: 3–8/10,000 woman-years
- drospirenone pill: 5–10/10,000 woman-years (risk may be highest in the first year of use3).
Adding perspective
The risks of hormonal contraception must be weighed against the consequences of using no contraception: 43 million women in the United States are sexually active but do not wish to become pregnant. Without contraception, 85% will be pregnant within 1 year.6 The risk of mortality during pregnancy in the United States is 1.8 deaths per 10,000 live births (5.5 deaths per 10,000 live births for women older than 39 years).7The prevalence of VTE during pregnancy is 5 to 29 events per 10,000 women; during the postpartum period, the prevalence is 40 to 65 events per 10,000 women (although some quote the VTE risk during the postpartum period to be as high as 200 to 400 events per 10,000 women).3,5,8
An unplanned pregnancy is more likely than a planned pregnancy to have a poor perinatal outcome or to end in abortion. The socioeconomic benefits of planning pregnancies must also be considered.

Hormonal contraception confers benefits beyond the prevention of pregnancy. In addition to a 50% reduction in the rate of endometrial cancer and a 27% reduction in the rate of ovarian cancer (and an even greater reduction for women who take OCs longer than 5 years), there are other benefits to hormonal contraception, such as reduced acne, dysmenorrhea, and menorrhagia.9
Individualize your care
When choosing a method of contraception, it is important not only to consider thromboembolic risk but also:
- previous contraceptive experiences
- previous pregnancies
- patient preference
- efficacy
- individual health factors
- cost.
For instance, even though the risk of VTE may be slightly increased among women using the norelgestromin patch, compliance rates are higher with the patch than with the pill.10 A woman with two unplanned pregnancies while taking the pill who reports having difficulty adhering to a daily regimen is a different patch candidate than a woman who has successfully planned two pregnancies using OCs.
For many women, a weekly or monthly reversible contraceptive is the most desirable method. In addition to these more quantifiable factors, some women prefer a specific brand of pill or delivery method—and satisfaction is a key component of contraception adherence.
Educate your patient
I favor the approach of providing as much data as possible. Patients may read the black box warning in the package inserts for drospirenone-containing pills or the norelgestromin patch, find news sources that inaccurately report risk to garner the most compelling headline, or stumble across plaintiff’s lawyers advertising lawsuits for drospirenone-containing pills, the contraceptive ring, and the patch. I can best counter confusion or misinformation by providing accurate information and putting possible risks into perspective up front. I now explain that the risk for VTE may be higher with certain pills, the ring, and the patch, but there just aren’t enough high-quality data to be certain. I also explain that risk may mean different things for different patients, based on medical history and previous experiences. I have found that my patients appreciate the full disclosure.
Overall, the benefits of combined hormonal contraception with all methods outweigh the risk of VTE. In addition, issues related to switching contraceptive methods may increase the risk of an unplanned pregnancy. In 1995, when the United Kingdom warned that desogestrel pills carried an increased risk of VTE but were still “safe,” the incidence of unplanned pregnancies and abortions increased.2,11 The data regarding the risk of VTE associated with drospirenone, the patch, and the ring should not be an impetus for sweeping generalizations, but rather an opportunity to educate our patients (and ourselves) and to further individualize care.
Do you agree that the benefits of combined hormonal contraception with all methods outweigh the VTE risk? Why or why not? What do you do in your practice? Click here
Click here to find additional articles on contraception published in OBG Management
in 2012.
Let’s increase our use of IUDs and improve contraceptive effectiveness in this country
Robert L. Barbieri, MD (Editorial, August 2012)
Let’s increase our use of implants and DMPA and improve contraceptive effectiveness in this country
Robert L. Barbieri, MD (Editorial, September 2012)
It is well established that combined hormonal contraception increases the risk of venous thromboembolism (VTE), both deep venous thrombosis (DVT) and pulmonary embolism (PE).1 Concerns exist that drospirenone-containing combined oral contraceptives (OCs), the norelgestromin patch, and the etonogestrel vaginal ring may increase the risk of VTE, compared with second-generation OCs, although results from studies evaluating the thromboembolic risk of these products are conflicting.1,2
An April 2012 safety communication from the US Food and Drug Administration (FDA) reported that “drospirenone-containing birth control pills may be associated with a higher risk for blood clots than other progestin-containing pills.”3 These pills now carry revised drug labels stating that epidemiologic studies that compared the risk of VTE reported that the risk ranged from no increase to a three-fold increase.3
Together, these studies and the FDA warning have garnered a lot of publicity and caused confusion and concern, leading both patients and providers to ask, “Are these specific products really safe?”
What is the baseline risk?
For nonusers of hormonal contraception, the baseline risk of VTE is 1 to 5 events per 10,000 woman-years.1,3-5 Variables that increase a woman’s risk of VTE include1:
- advanced age
- obesity
- immobility
- hematologic disorders
- pregnancy.
Estrogen-containing OCs with second-generation progestins (levonorgestrel, norgestimate, and norethindrone) have a risk of VTE of approximately 3 to 9 events per 10,000 woman-years.1,3-5
When study results conflict
The relative risk of VTE associated with drospirenone-containing OCs, compared with second-generation pills, ranges from 0.9 to 3.3. The relative risk is 1.2 to 2.2 for the norelgestromin patch, and 1.6 to 1.9 for the etonogestrel ring.1-4
All of the studies addressing the increased risk of VTE with drospirenone, the patch, and the ring have some limitations, such as the use of retrospective data, selection bias, study design, or inclusion of multiple pill regimens. However, most of the studies that found no association between these methods and VTE were industry-funded.2 Criticisms of these studies have led to disagreement about the risk; it is unclear whether a definitive study ever can be designed and performed.2
Worst-case scenario. Using data from only those studies that show an increased risk of VTE, the increased number of VTE events above that conferred by a second-generation progestin would be approximately2:
- ring: 3–5/10,000 woman-years
- patch: 3–8/10,000 woman-years
- drospirenone pill: 5–10/10,000 woman-years (risk may be highest in the first year of use3).
Adding perspective
The risks of hormonal contraception must be weighed against the consequences of using no contraception: 43 million women in the United States are sexually active but do not wish to become pregnant. Without contraception, 85% will be pregnant within 1 year.6 The risk of mortality during pregnancy in the United States is 1.8 deaths per 10,000 live births (5.5 deaths per 10,000 live births for women older than 39 years).7The prevalence of VTE during pregnancy is 5 to 29 events per 10,000 women; during the postpartum period, the prevalence is 40 to 65 events per 10,000 women (although some quote the VTE risk during the postpartum period to be as high as 200 to 400 events per 10,000 women).3,5,8
An unplanned pregnancy is more likely than a planned pregnancy to have a poor perinatal outcome or to end in abortion. The socioeconomic benefits of planning pregnancies must also be considered.

Hormonal contraception confers benefits beyond the prevention of pregnancy. In addition to a 50% reduction in the rate of endometrial cancer and a 27% reduction in the rate of ovarian cancer (and an even greater reduction for women who take OCs longer than 5 years), there are other benefits to hormonal contraception, such as reduced acne, dysmenorrhea, and menorrhagia.9
Individualize your care
When choosing a method of contraception, it is important not only to consider thromboembolic risk but also:
- previous contraceptive experiences
- previous pregnancies
- patient preference
- efficacy
- individual health factors
- cost.
For instance, even though the risk of VTE may be slightly increased among women using the norelgestromin patch, compliance rates are higher with the patch than with the pill.10 A woman with two unplanned pregnancies while taking the pill who reports having difficulty adhering to a daily regimen is a different patch candidate than a woman who has successfully planned two pregnancies using OCs.
For many women, a weekly or monthly reversible contraceptive is the most desirable method. In addition to these more quantifiable factors, some women prefer a specific brand of pill or delivery method—and satisfaction is a key component of contraception adherence.
Educate your patient
I favor the approach of providing as much data as possible. Patients may read the black box warning in the package inserts for drospirenone-containing pills or the norelgestromin patch, find news sources that inaccurately report risk to garner the most compelling headline, or stumble across plaintiff’s lawyers advertising lawsuits for drospirenone-containing pills, the contraceptive ring, and the patch. I can best counter confusion or misinformation by providing accurate information and putting possible risks into perspective up front. I now explain that the risk for VTE may be higher with certain pills, the ring, and the patch, but there just aren’t enough high-quality data to be certain. I also explain that risk may mean different things for different patients, based on medical history and previous experiences. I have found that my patients appreciate the full disclosure.
Overall, the benefits of combined hormonal contraception with all methods outweigh the risk of VTE. In addition, issues related to switching contraceptive methods may increase the risk of an unplanned pregnancy. In 1995, when the United Kingdom warned that desogestrel pills carried an increased risk of VTE but were still “safe,” the incidence of unplanned pregnancies and abortions increased.2,11 The data regarding the risk of VTE associated with drospirenone, the patch, and the ring should not be an impetus for sweeping generalizations, but rather an opportunity to educate our patients (and ourselves) and to further individualize care.
Do you agree that the benefits of combined hormonal contraception with all methods outweigh the VTE risk? Why or why not? What do you do in your practice? Click here
Click here to find additional articles on contraception published in OBG Management
in 2012.
1. Lidegaard Ø, Milsom I, Geirsson R, Skjeldestad F. Hormonal contraception and venous thromboembolism. Acta Obstet Gynecol Scand. 2012;91(7):769-778.
2. Raymond EG, Burke AE, Espey E. Combined hormonal contraceptives and venous thromboembolism: putting the risks into perspective. Obstet Gynecol. 2012;119(5):1039-1044.
3. US Food and Drug Administration. Safety Announcement. Updated information about the risk of blood clots in women taking birth control pills containing drospirenone. http://www.fda.gov/Drugs/DrugSafety/ucm299305.htm. Published April 10 2012. Accessed September 11, 2012.
4. Lidegaard Ø, Nielsen L, Skovlund C, Løkkegaard E. Venous thrombosis in users of non-oral hormonal contraception: follow-up study Denmark 2001-10 [published online ahead of print May 10, 2012]. BMJ. 2012:344-353:e2990. doi: 10.1136 /bmj.e2990.
5. Oral contraceptives and the risk of thromboembolism: an update. Clinical practice Guideline No. 252. Society of Obstetricians and Gynaecologists of Canada. 2010;252. http://www.sogc.org/guidelines/documents/gui252CPG1012E.pdf. Accessed September 5, 2012.
6. Fact Sheet Contraceptive use in the United States. Guttmacher Institute. http://www.guttmacher.org/pubs/fb_contr_use.html. Published July 2012. Accessed September 5 2012.
7. Berg CJ, Callaghan WM, Syverson C, Henderson Z. Pregnancy related mortality in the United States 1998 to 2005. Obstet Gynecol. 2010;116(6):1302-1309.
8. James A. Committee on Practice Bulletins-Obstetrics. ACOG Practice Bulletin No. 123. Thromboembolism in pregnancy. Obstet Gynecol. 2011;118(3):718-729.
9. Committee on Practice Bulletins-Gynecology. ACOG Practice Bulletin No. 110. Noncontraceptive uses of hormonal contraception. Obstet Gynecol. 2010;115(1):206-218.
10. Archer DF, Bigrigg A, Smallwood GH, Shangold GA, Creasy GW, Fisher AC. Assessment of compliance with a weekly contraceptive patch (OrthoEvra/Evra) among North American women. Fertil Steril. 2002;77(2 suppl 2):S27-S31.
11. Furedi A. The public health implications of the 1995 ‘pill scare.’ Hum Reprod Update. 1999;5(6):621-626.
1. Lidegaard Ø, Milsom I, Geirsson R, Skjeldestad F. Hormonal contraception and venous thromboembolism. Acta Obstet Gynecol Scand. 2012;91(7):769-778.
2. Raymond EG, Burke AE, Espey E. Combined hormonal contraceptives and venous thromboembolism: putting the risks into perspective. Obstet Gynecol. 2012;119(5):1039-1044.
3. US Food and Drug Administration. Safety Announcement. Updated information about the risk of blood clots in women taking birth control pills containing drospirenone. http://www.fda.gov/Drugs/DrugSafety/ucm299305.htm. Published April 10 2012. Accessed September 11, 2012.
4. Lidegaard Ø, Nielsen L, Skovlund C, Løkkegaard E. Venous thrombosis in users of non-oral hormonal contraception: follow-up study Denmark 2001-10 [published online ahead of print May 10, 2012]. BMJ. 2012:344-353:e2990. doi: 10.1136 /bmj.e2990.
5. Oral contraceptives and the risk of thromboembolism: an update. Clinical practice Guideline No. 252. Society of Obstetricians and Gynaecologists of Canada. 2010;252. http://www.sogc.org/guidelines/documents/gui252CPG1012E.pdf. Accessed September 5, 2012.
6. Fact Sheet Contraceptive use in the United States. Guttmacher Institute. http://www.guttmacher.org/pubs/fb_contr_use.html. Published July 2012. Accessed September 5 2012.
7. Berg CJ, Callaghan WM, Syverson C, Henderson Z. Pregnancy related mortality in the United States 1998 to 2005. Obstet Gynecol. 2010;116(6):1302-1309.
8. James A. Committee on Practice Bulletins-Obstetrics. ACOG Practice Bulletin No. 123. Thromboembolism in pregnancy. Obstet Gynecol. 2011;118(3):718-729.
9. Committee on Practice Bulletins-Gynecology. ACOG Practice Bulletin No. 110. Noncontraceptive uses of hormonal contraception. Obstet Gynecol. 2010;115(1):206-218.
10. Archer DF, Bigrigg A, Smallwood GH, Shangold GA, Creasy GW, Fisher AC. Assessment of compliance with a weekly contraceptive patch (OrthoEvra/Evra) among North American women. Fertil Steril. 2002;77(2 suppl 2):S27-S31.
11. Furedi A. The public health implications of the 1995 ‘pill scare.’ Hum Reprod Update. 1999;5(6):621-626.
Vulvar pain syndromes: Making the correct diagnosis
Although the incidence of vulvar pain has increased over the past decade—thanks to both greater awareness and increasing numbers of affected women—the phenomenon is not a recent development. As early as 1874, T. Galliard Thomas wrote, “[T]his disorder, although fortunately not very frequent, is by no means very rare.”1 He went on to express “surprise” that it had not been “more generally and fully described.”
Despite the focus Thomas directed to the issue, vulvar pain did not get much attention until the 21st century, when a number of studies began to gauge its prevalence. For example, in a study in Boston of about 5,000 women, the lifetime prevalence of chronic vulvar pain was 16%.2 And in a study in Texas, the prevalence of vulvar pain in an urban, largely minority population was estimated to be 11%.3 The Boston study also reported that “nearly 40% of women chose not to seek treatment, and, of those who did, 60% saw three or more doctors, many of whom could not provide a diagnosis.”2
Clearly, there is a need for comprehensive information on vulvar pain and its causes, symptoms, diagnosis, and treatment. To address the lack of guidance, OBG Management Contributing Editor Neal M. Lonky, MD, assembled a panel of experts on vulvar pain syndromes and invited them to share their considerable knowledge. The ensuing discussion, presented in three parts, offers a gold mine of information. In this opening article, the panel focuses on causes, symptomatology, and diagnosis of this common complaint.
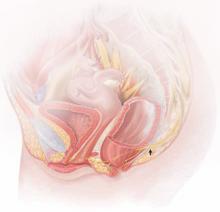
|
The lower vagina and vulva are richly supplied with peripheral nerves and are, therefore, sensitive to pain, particularly the region of the hymeneal ring. Although the pudendal nerve (arrow) courses through the area, it is an uncommon source of vulvar pain. |
![]()
Dr. Lonky: What are the most common diagnoses when vulvar pain is the complaint?
Dr. Gunter: The most common cause of chronic vulvar pain is vulvodynia, although lichen simplex chronicus, chronic yeast infections, and non-neoplastic epithelial disorders, such as lichen sclerosus and lichen planus, can also produce irritation and pain. In postmenopausal women, atrophic vaginitis can also cause a burning pain, although symptoms are typically more vaginal than vulvar. Yeast and lichen simplex chronicus typically produce itching, although sometimes they can present with irritation and pain, so they must be considered in the differential diagnosis. It is important to remember that many women with vulvodynia have used multiple topical agents and may have developed complex hygiene rituals in an attempt to treat their symptoms, which can result in a secondary lichen simplex chronicus.
That said, there is a high frequency of misdiagnosis with yeast. For example, in a study by Nyirjesy and colleagues, two thirds of women who were referred to a tertiary clinic for chronic vulvovaginal candidiasis were found to have a noninfectious entity instead—most commonly lichen simplex chronicus and vulvodynia.4
Dr. Edwards: The most common “diagnosis” for vulvar pain is vulvodynia. However, the definition of vulvodynia is pain—i.e., burning, rawness, irritation, soreness, aching, or stabbing or stinging sensations—in the absence of skin disease, infection, or specific neurologic disease. Therefore, even though the usual cause of vulvar pain is vulvodynia, it is a diagnosis of exclusion, and skin disease, infection, and neurologic disease must be ruled out.
In regard to infection, Candida albicans and bacterial vaginosis (BV) are usually the first conditions that are considered when a patient complains of vulvar pain, but they are not common causes of vulvar pain and are never causes of chronic vulvar pain. Very rarely they may cause recurrent pain that clears, at least briefly, with treatment.
Candida albicans is usually primarily pruritic, and BV produces discharge and odor, sometimes with minor symptoms. Non-albicans Candida (e.g., Candida glabrata) is nearly always asymptomatic, but it occasionally causes irritation and burning.
Group B streptococcus is another infectious entity that very, very occasionally causes irritation and dyspareunia but is usually only a colonizer.
Herpes simplex virus is a cause of recurrent but not chronic pain.
Chronic pain is more likely to be caused by skin disease than by infection. Lichen simplex chronicus causes itching; any pain is due to erosions from scratching.
Dr. Haefner: Several other infectious conditions or their treatments can cause vulvar pain. For example, herpes (particularly primary herpes infection) is classically associated with vulvar pain. The pain is so great that, at times, the patient requires admission for pain control. Surprisingly, despite the known pain of herpes, approximately 80% of patients who have it are unaware of their diagnosis.
Although condyloma is generally a painless condition, many patients complain of pain following treatment for it, whether treatment involves topical medications or laser surgery.
Chancroid is a painful vulvar ulcer. Trichomonas can sometimes be associated with vulvar pain.
Dr. Lonky: What terminology do we use when we discuss vulvar pain?
Dr. Haefner: The current terminology used to describe vulvar pain was published in 2004, after years of debate over nomenclature within the International Society for the Study of Vulvovaginal Disease.5 The terminology lists two major categories of vulvar pain:
-
pain related to a specific disorder. This category encompasses numerous conditions that feature an abnormal appearance of the vulva (Table 1).
TABLE 1
Terminology and classification of vulvar pain from the International Society for the Study of Vulvovaginal Disease
| SOURCE: Moyal-Barracco and Lynch.5 Reproduced with permission from the Journal of Reproductive Medicine. |
|
-
vulvodynia, in which the vulva appears normal, other than occasional erythema, which is most prominent at the duct openings (vestibular ducts—Bartholin’s and Skene’s).
As for vulvar pain, there are two major forms:
-
hyperalgesia (a low threshold for pain)
-
allodynia (pain in response to light touch).
Some diseases that are associated with vulvar pain do not qualify for the diagnosis of vulvodynia (Table 2) because they are associated with an abnormal appearance of the vulva.
TABLE 2
Conditions other than vulvodynia that are associated with vulvar pain
| Acute irritant contact dermatitis (e.g., erosion due to podofilox, imiquimod, cantharidin, fluorouracil, or podophyllin toxin) |
| Aphthous ulcer |
| Atrophy |
| Bartholin’s abscess |
| Candidiasis |
| Carcinoma |
| Chronic irritant contact dermatitis |
| Endometriosis |
| Herpes (simplex and zoster) |
| Immunobullous diseases (including cicatricial pemphigoid, pemphigus vulgaris, linear immunoglobulin A disease, etc.) |
| Lichen planus |
| Lichen sclerosus |
| Podophyllin overdose (see above) |
| Prolapsed urethra |
| Sjögren’s syndrome |
| Trauma |
| Trichomoniasis |
| Vulvar intraepithelial neoplasia |
![]()
Dr. Lonky: What skin diseases need to be ruled out before vulvodynia can be diagnosed?
Dr. Edwards: Skin diseases that affect the vulva are usually pruritic—pain is a later sign. Lichen simplex chronicus (also known as eczema) is pruritus caused by any irritant; any pain that arises is produced by visible excoriations from scratching.
Lichen sclerosus manifests as white epithelium that has a crinkling, shiny, or waxy texture. It can produce pain, especially dyspareunia. The pain is caused by erosions that arise from fragility and introital narrowing and inelasticity.
Vulvovaginal lichen planus is usually erosive and preferentially affects mucous membranes, especially the vestibule; it sometimes affects the vagina and mouth, as well.
Desquamative inflammatory vaginitis is most likely a skin disease that affects only the vagina. It involves introital redness and a clinically and microscopically purulent vaginal discharge that also reveals parabasal cells and absent lactobacilli.
Dr. Lonky: You mentioned that neurologic diseases can sometimes cause vulvar pain. Which ones?
Dr. Edwards: Pudendal neuralgia, diabetic neuropathy, and post-herpetic neuralgia are the most common specific neurologic causes of vulvar pain. Multiple sclerosis can also produce pain syndromes. Post-herpetic neuralgia follows herpes zoster—not herpes simplex—virus infection.
Dr. Lonky: Any other conditions that can cause vulvar pain?
Dr. Haefner: Aphthous ulcers are common and are often flared by stress.
Non-neoplastic epithelial disorders are also seen frequently in health-care providers’ offices; many patients who experience them report pain on the vulva.
It is always important to consider cancer when a patient has an abnormal vulvar appearance and pain that has persisted despite treatment.
![]()
Dr. Lonky: If you were to rank vulvar pain syndromes according to their prevalence, what would the most common syndromes be?
Dr. Gunter: Given the misdiagnosis of many women, who are told they have chronic yeast infection, as I mentioned, it’s hard to know which vulvar pain syndromes are most prevalent. I suspect that lichen simplex chronicus is most common, followed by vulvodynia, with chronic yeast infection a distant third.
My experience reflects what Nyirjesy and colleagues4 found: 65% to 75% of women referred to my clinic with chronic yeast actually have lichen simplex chronicus or vulvodynia. In postmenopausal women, atrophic vaginitis is also a consideration; it’s becoming more common now that the use of systemic hormone replacement therapy is decreasing.
Dr. Lonky: What about subsets of vulvodynia? Which ones are most common?
Dr. Edwards: There is good evidence of marked overlap among subsets of vulvodynia. The vast majority of women who have vulvodynia experience primarily provoked vestibular pain, regardless of age. However, I find that almost all patients also report pain that extends beyond the vestibule at times, as well as occasional unprovoked pain.
The diagnosis requires the exclusion of other causes of vulvar pain, and the subset is identified by the location of pain (that is, is it strictly localized or generalized or even migratory?) and its provoked or unprovoked nature.
Localized clitoral pain and vulvar pain localized to one side of the vulva are extremely uncommon, but they do occur. And although I rarely encounter teenagers and prepubertal children who have vulvodynia, I do have patients in both age groups who have vulvodynia.
Dr. Lonky: Are there racial differences in the prevalence of vulvodynia?
Dr. Edwards: Although several good studies show that women of African descent and white patients are equally likely to experience vulvodynia, the vast majority (99%) of my patients who have vulvodynia are white. My patients of African descent consult me primarily for itching or discharge.
My local demographics prevent me from judging the likelihood of Asians having vulvodynia, and our Hispanic population has limited access to health care.
In general, I don’t think that demographics are useful in making the diagnosis of vulvodynia.
![]()
Dr. Lonky: Do your patients who have vulvodynia or another vulvar pain syndrome tend to have comorbidities? If so, is this information helpful in establishing the diagnosis and planning therapy?
Dr. Haefner: Women who have vulvodynia often have other medical problems as well. In my practice, when new patients who have vulvodynia complete their intake survey, they often report a history of headache, irritable bowel syndrome, interstitial cystitis, fibromyalgia,6 chronic fatigue syndrome, back pain, and temporomandibular joint (TMJ) disorder. These comorbidities are not particularly helpful in establishing the diagnosis of vulvodynia, but they are an important consideration when choosing therapy for the patient. Often, the medications chosen to treat one condition will also benefit another condition. However, it’s important to check for potential interactions between drugs before prescribing a new treatment.
Dr. Gunter: A significant number of women who have vulvodynia also have other chronic pain syndromes. For example, the incidence of bladder pain syndrome–interstitial cystitis is 68% to 82% among women who have vulvodynia, compared with a baseline rate among all women of 6% to 11%.7-10 The rate of irritable bowel syndrome is more than doubled among women who have vulvodynia, compared with the general population (27% versus 12%).8 Another common comorbidity, hypertonic somatic dysfunction of the pelvic floor, is identified in 10% to 90% of women who have chronic vulvar pain.8,11,12 These women also have a higher incidence of nongenital pain syndromes, such as fibromyalgia, migraine, and TMJ dysfunction, than the general population, as Dr. Haefner noted.8,12,13
Many studies have evaluated psychological and emotional contributions to chronic vulvar pain. Pain and depression are intimately related—the incidence of depression among all people who experience chronic pain ranges from 27% to 54%, compared with 5% to 17% among the general population.14-16 The relationship is complex because chronic illness in general is associated with depression. Nevertheless, several studies have noted an increase in anxiety, stress, and depression among women who have vulvodynia.17-19
I screen every patient for depression using a Patient Health Questionnaire (PHQ-9); I also screen for anxiety. I find that a significant percentage of patients in my clinic are depressed or have an anxiety disorder. Failure to address these comorbidities makes treatment very difficult. I typically prescribe citalopram (Celexa), although there is some question whether it can safely be combined with a tricyclic antidepressant. We also offer stress-reduction classes, teach every patient the value of diaphragmatic breathing, offer mind-body classes for anxiety and stress, and provide intensive programs where the patient can learn important self-care skills, such as pacing (spacing activities throughout the day in a manner that avoids aggravating the pain), and address her anxiety and stress in a more guided manner. We also have a psychologist who specializes in pain for any patient who may need one-on-one counseling.
Dr. Edwards: The presence of comorbidities is somewhat useful in making the diagnosis of vulvodynia. I question my diagnosis, in fact, when a patient who has vulvodynia does not have headaches, low energy, depression, anxiety, irritable bowel syndrome, constipation, fibromyalgia, chronic fatigue, sensitivity to medications, TMJ dysfunction, or urinary symptoms.
![]()
Dr. Lonky: How prevalent is a finding of pudendal neuralgia?
Dr. Edwards: The prevalence and incidence of pudendal neuralgia are not known. Those who specialize in this condition think it is relatively common. I do not identify or suspect it very often. Its definitive diagnosis and management are outside the purview of the general gynecologist, but the general gynecologist should recognize the symptoms of pudendal neuralgia and refer the patient for evaluation and therapy.
Dr. Lonky: What are those symptoms?
Dr. Haefner: Pudendal neuralgia often occurs following trauma to the pudendal nerve. The pudendal nerve arises from sacral nerves, generally sacral nerves 2 to 4. Several tests can be utilized to diagnose this condition, including quantitative sensor tests, pudendal nerve motor latency tests, electromyography (EMG), and pudendal nerve blocks.20
Nantes Criteria allow for making a diagnosis of pudendal neuralgia (Table 3).21
TABLE 3
Nantes Criteria for pudendal neuralgia by pudendal nerve entrapment
| SOURCE: Labat et al.21 Reproduced with permission from Neurology and Urodynamics. |
Essential criteria
|
Complementary diagnostic criteria
|
Exclusion criteria
|
Associated signs not excluding the diagnosis
|
Initial treatments for pudendal neuralgia should be conservative. Treatments consist of lifestyle changes to prevent flare of disease. Physical therapy, medical management, nerve blocks, and alternative treatments may be beneficial.
Pudendal nerve entrapment is often exacerbated by sitting (not on a toilet seat, however) and is reduced in a standing position. It tends to increase in intensity throughout the day.22 The final treatment for pudendal nerve entrapment is surgery if the nerve is compressed. By this time, the generalist is not generally the provider who performs the surgery.
Dr. Gunter: I believe pudendal neuralgia is sometimes overdiagnosed. EMG studies of the pudendal nerve, often touted as a diagnostic tool, are unreliable (they can be abnormal after vaginal delivery or vaginal hysterectomy, for example). In my experience, bilateral pain is less likely to be pudendal neuralgia; spontaneous bilateral compression neuropathy at exactly the same level is not a common phenomenon in chronic pain.
I reserve the diagnosis of pudendal neuralgia for women who have allodynia in the distribution of the pudendal nerve with severe pain on sitting, and who have exquisite tenderness when pressure is applied over the pudendal nerve (at the level of the ischial spine on vaginal examination). Typically, the vaginal sidewall on the affected side is very sensitive to light touch. I do see pudendal nerve pain after vaginal surgery when there has been some compromise of the pudendal nerve or the sacral plexus. This is typically unilateral pain.
Dr. Lonky: Thank you all. We’ll continue our discussion, with a focus on treatment.
|
MORE TO COME
|
References
1. Thomas TG. Practical Treatise on the Diseases of Women. Philadelphia Pa: Henry C. Lea; 1874.
2. Harlow BL, Stewart EG. A population-based assessment of chronic unexplained vulvar pain: have we underestimated the prevalence of vulvodynia? J Am Med Womens Assoc. 2003;58(2):82–88.
3. Lavy RJ, Hynan LS, Haley RW. Prevalence of vulvar pain in an urban minority population. J Reprod Med. 2007;52(1):59–62.
4. Nyirjesy P, Peyton C, Weitz MV, Mathew L, Culhane JF. Causes of chronic vaginitis: analysis of a prospective database of affected women. Obstet Gynecol. 2006;108(5):1185–1191.
5. Moyal-Barracco M, Lynch PJ. 2003 ISSVD terminology and classification of vulvodynia: a historical perspective. J Reprod Med. 2004;49(10):772–777.
6. Yunas MB. Fibromyalgia and overlapping disorders: the unifying concept of central sensitivity syndromes. Semin Arthritis Rheum. 2007;36(6):339–356.
7. Kahn BS, Tatro C, Parsons CL, Willems JJ. Prevalence of interstitial cystitis in vulvodynia patients detected by bladder potassium sensitivity. J Sex Med. 2010;7(2 Pt 2):996–1002.
8. Arnold JD, Bachman GS, Rosen R, Kelly S, Rhoads GG. Vulvodynia: characteristics and associations with comorbidities and quality of life. Obstet Gynecol. 2006;107(3):617–624.
9. Parsons CL, Dell J, Stanford EJ, et al. The prevalence of interstitial cystitis in gynecologic patients with pelvic pain, as detected by intravesical potassium sensitivity. Am J Obstet Gynecol. 2002;187(5):1395–1400.
10. Clemens JQ, Meenan RT, O’Keefe Rosetti MC, et al. Prevalence of interstitial cystitis symptoms in a managed care population. J Urol. 2005;174(2):576–580.
11. Engman M, Lindehammar H, Wijma B. Surface electromyography diagnostics in women with partial vaginismus with or without vulvar vestibulitis and in asymptomatic women. J Psychosom Obstet Gynecol. 2004;25(3-4):281–294.
12. Gunter J. Vulvodynia: new thoughts on a devastating condition. Obstet Gynecol Surv. 2007;62(12):812–819.
13. Gordon AS, Panahlan-Jand M, McComb F, Melegari C, Sharp S. Characteristics of women with vulvar pain disorders: a Web-based survey. J Sex Marital Ther. 2003;29(suppl 1):45.
14. Whitten CE, Cristobal K. Chronic pain is a chronic condition not just a symptom. Permanente J. 2005;9(3):43.
15. Manchikanti L, Fellows B, Pampati V, et al. Comparison of psychological status of chronic pain patients and the general population. Pain Physician. 2002;5(1):40–48.
16. Banks SM, Kerns RD. Explaining the high rates of depression in chronic pain: a diathesis-stress framework. Psychological Bulletin. 1996;119(1):95–110.
17. Sadownik LA. Clinical correlates of vulvodynia patients. A prospective study of 300 patients. J Reprod Med. 2000;5:40–48. Editor found in PubMed: Sadownik LA. Clinical profile of vulvodynia patients. A prospective study of 300 patients. J Reprod Med. 2000;45(8):679–684. Could not find the citation listed. Please confirm.
18. Reed BD, Haefner HK, Punch MR, Roth RS, Gorenflo DW, Gillespie BW. Psychosocial and sexual functioning in women with vulvodynia and chronic pelvic pain. A comparative evaluation. J Reprod Med. 2000;45(8):624–632.
19. Landry T, Bergeron S. Biopsychosocial factors associated with dyspareunia in a community sample of adolescent girls. Arch Sex Behav. 2011; June 22.
20. Goldstein A, Pukall C, Goldstein I. When Sex Hurts: A Woman’s Guide to Banishing Sexual Pain. Cambridge Mass: Da Capo Lifelong Books; 2011;117–126.
21. Labat JJ, Riant T, Robert R, Amarenco G, Lefaucheur JP, Rigaud J. Diagnostic criteria for pudendal neuralgia by pudendal nerve entrapment (Nantes criteria). Neurol Urodyn. 2008;27(4):306–310.
22. Popeney C, Answell V, Renney K. Pudendal entrapment as an etiology of chronic perineal pain: Diagnosis and treatment. Neurol Urodyn. 2007;26(6):820–827.
Although the incidence of vulvar pain has increased over the past decade—thanks to both greater awareness and increasing numbers of affected women—the phenomenon is not a recent development. As early as 1874, T. Galliard Thomas wrote, “[T]his disorder, although fortunately not very frequent, is by no means very rare.”1 He went on to express “surprise” that it had not been “more generally and fully described.”
Despite the focus Thomas directed to the issue, vulvar pain did not get much attention until the 21st century, when a number of studies began to gauge its prevalence. For example, in a study in Boston of about 5,000 women, the lifetime prevalence of chronic vulvar pain was 16%.2 And in a study in Texas, the prevalence of vulvar pain in an urban, largely minority population was estimated to be 11%.3 The Boston study also reported that “nearly 40% of women chose not to seek treatment, and, of those who did, 60% saw three or more doctors, many of whom could not provide a diagnosis.”2
Clearly, there is a need for comprehensive information on vulvar pain and its causes, symptoms, diagnosis, and treatment. To address the lack of guidance, OBG Management Contributing Editor Neal M. Lonky, MD, assembled a panel of experts on vulvar pain syndromes and invited them to share their considerable knowledge. The ensuing discussion, presented in three parts, offers a gold mine of information. In this opening article, the panel focuses on causes, symptomatology, and diagnosis of this common complaint.
|
The lower vagina and vulva are richly supplied with peripheral nerves and are, therefore, sensitive to pain, particularly the region of the hymeneal ring. Although the pudendal nerve (arrow) courses through the area, it is an uncommon source of vulvar pain. |
![]()
Dr. Lonky: What are the most common diagnoses when vulvar pain is the complaint?
Dr. Gunter: The most common cause of chronic vulvar pain is vulvodynia, although lichen simplex chronicus, chronic yeast infections, and non-neoplastic epithelial disorders, such as lichen sclerosus and lichen planus, can also produce irritation and pain. In postmenopausal women, atrophic vaginitis can also cause a burning pain, although symptoms are typically more vaginal than vulvar. Yeast and lichen simplex chronicus typically produce itching, although sometimes they can present with irritation and pain, so they must be considered in the differential diagnosis. It is important to remember that many women with vulvodynia have used multiple topical agents and may have developed complex hygiene rituals in an attempt to treat their symptoms, which can result in a secondary lichen simplex chronicus.
That said, there is a high frequency of misdiagnosis with yeast. For example, in a study by Nyirjesy and colleagues, two thirds of women who were referred to a tertiary clinic for chronic vulvovaginal candidiasis were found to have a noninfectious entity instead—most commonly lichen simplex chronicus and vulvodynia.4
Dr. Edwards: The most common “diagnosis” for vulvar pain is vulvodynia. However, the definition of vulvodynia is pain—i.e., burning, rawness, irritation, soreness, aching, or stabbing or stinging sensations—in the absence of skin disease, infection, or specific neurologic disease. Therefore, even though the usual cause of vulvar pain is vulvodynia, it is a diagnosis of exclusion, and skin disease, infection, and neurologic disease must be ruled out.
In regard to infection, Candida albicans and bacterial vaginosis (BV) are usually the first conditions that are considered when a patient complains of vulvar pain, but they are not common causes of vulvar pain and are never causes of chronic vulvar pain. Very rarely they may cause recurrent pain that clears, at least briefly, with treatment.
Candida albicans is usually primarily pruritic, and BV produces discharge and odor, sometimes with minor symptoms. Non-albicans Candida (e.g., Candida glabrata) is nearly always asymptomatic, but it occasionally causes irritation and burning.
Group B streptococcus is another infectious entity that very, very occasionally causes irritation and dyspareunia but is usually only a colonizer.
Herpes simplex virus is a cause of recurrent but not chronic pain.
Chronic pain is more likely to be caused by skin disease than by infection. Lichen simplex chronicus causes itching; any pain is due to erosions from scratching.
Dr. Haefner: Several other infectious conditions or their treatments can cause vulvar pain. For example, herpes (particularly primary herpes infection) is classically associated with vulvar pain. The pain is so great that, at times, the patient requires admission for pain control. Surprisingly, despite the known pain of herpes, approximately 80% of patients who have it are unaware of their diagnosis.
Although condyloma is generally a painless condition, many patients complain of pain following treatment for it, whether treatment involves topical medications or laser surgery.
Chancroid is a painful vulvar ulcer. Trichomonas can sometimes be associated with vulvar pain.
Dr. Lonky: What terminology do we use when we discuss vulvar pain?
Dr. Haefner: The current terminology used to describe vulvar pain was published in 2004, after years of debate over nomenclature within the International Society for the Study of Vulvovaginal Disease.5 The terminology lists two major categories of vulvar pain:
-
pain related to a specific disorder. This category encompasses numerous conditions that feature an abnormal appearance of the vulva (Table 1).
TABLE 1
Terminology and classification of vulvar pain from the International Society for the Study of Vulvovaginal Disease
| SOURCE: Moyal-Barracco and Lynch.5 Reproduced with permission from the Journal of Reproductive Medicine. |
|
-
vulvodynia, in which the vulva appears normal, other than occasional erythema, which is most prominent at the duct openings (vestibular ducts—Bartholin’s and Skene’s).
As for vulvar pain, there are two major forms:
-
hyperalgesia (a low threshold for pain)
-
allodynia (pain in response to light touch).
Some diseases that are associated with vulvar pain do not qualify for the diagnosis of vulvodynia (Table 2) because they are associated with an abnormal appearance of the vulva.
TABLE 2
Conditions other than vulvodynia that are associated with vulvar pain
| Acute irritant contact dermatitis (e.g., erosion due to podofilox, imiquimod, cantharidin, fluorouracil, or podophyllin toxin) |
| Aphthous ulcer |
| Atrophy |
| Bartholin’s abscess |
| Candidiasis |
| Carcinoma |
| Chronic irritant contact dermatitis |
| Endometriosis |
| Herpes (simplex and zoster) |
| Immunobullous diseases (including cicatricial pemphigoid, pemphigus vulgaris, linear immunoglobulin A disease, etc.) |
| Lichen planus |
| Lichen sclerosus |
| Podophyllin overdose (see above) |
| Prolapsed urethra |
| Sjögren’s syndrome |
| Trauma |
| Trichomoniasis |
| Vulvar intraepithelial neoplasia |
![]()
Dr. Lonky: What skin diseases need to be ruled out before vulvodynia can be diagnosed?
Dr. Edwards: Skin diseases that affect the vulva are usually pruritic—pain is a later sign. Lichen simplex chronicus (also known as eczema) is pruritus caused by any irritant; any pain that arises is produced by visible excoriations from scratching.
Lichen sclerosus manifests as white epithelium that has a crinkling, shiny, or waxy texture. It can produce pain, especially dyspareunia. The pain is caused by erosions that arise from fragility and introital narrowing and inelasticity.
Vulvovaginal lichen planus is usually erosive and preferentially affects mucous membranes, especially the vestibule; it sometimes affects the vagina and mouth, as well.
Desquamative inflammatory vaginitis is most likely a skin disease that affects only the vagina. It involves introital redness and a clinically and microscopically purulent vaginal discharge that also reveals parabasal cells and absent lactobacilli.
Dr. Lonky: You mentioned that neurologic diseases can sometimes cause vulvar pain. Which ones?
Dr. Edwards: Pudendal neuralgia, diabetic neuropathy, and post-herpetic neuralgia are the most common specific neurologic causes of vulvar pain. Multiple sclerosis can also produce pain syndromes. Post-herpetic neuralgia follows herpes zoster—not herpes simplex—virus infection.
Dr. Lonky: Any other conditions that can cause vulvar pain?
Dr. Haefner: Aphthous ulcers are common and are often flared by stress.
Non-neoplastic epithelial disorders are also seen frequently in health-care providers’ offices; many patients who experience them report pain on the vulva.
It is always important to consider cancer when a patient has an abnormal vulvar appearance and pain that has persisted despite treatment.
![]()
Dr. Lonky: If you were to rank vulvar pain syndromes according to their prevalence, what would the most common syndromes be?
Dr. Gunter: Given the misdiagnosis of many women, who are told they have chronic yeast infection, as I mentioned, it’s hard to know which vulvar pain syndromes are most prevalent. I suspect that lichen simplex chronicus is most common, followed by vulvodynia, with chronic yeast infection a distant third.
My experience reflects what Nyirjesy and colleagues4 found: 65% to 75% of women referred to my clinic with chronic yeast actually have lichen simplex chronicus or vulvodynia. In postmenopausal women, atrophic vaginitis is also a consideration; it’s becoming more common now that the use of systemic hormone replacement therapy is decreasing.
Dr. Lonky: What about subsets of vulvodynia? Which ones are most common?
Dr. Edwards: There is good evidence of marked overlap among subsets of vulvodynia. The vast majority of women who have vulvodynia experience primarily provoked vestibular pain, regardless of age. However, I find that almost all patients also report pain that extends beyond the vestibule at times, as well as occasional unprovoked pain.
The diagnosis requires the exclusion of other causes of vulvar pain, and the subset is identified by the location of pain (that is, is it strictly localized or generalized or even migratory?) and its provoked or unprovoked nature.
Localized clitoral pain and vulvar pain localized to one side of the vulva are extremely uncommon, but they do occur. And although I rarely encounter teenagers and prepubertal children who have vulvodynia, I do have patients in both age groups who have vulvodynia.
Dr. Lonky: Are there racial differences in the prevalence of vulvodynia?
Dr. Edwards: Although several good studies show that women of African descent and white patients are equally likely to experience vulvodynia, the vast majority (99%) of my patients who have vulvodynia are white. My patients of African descent consult me primarily for itching or discharge.
My local demographics prevent me from judging the likelihood of Asians having vulvodynia, and our Hispanic population has limited access to health care.
In general, I don’t think that demographics are useful in making the diagnosis of vulvodynia.
![]()
Dr. Lonky: Do your patients who have vulvodynia or another vulvar pain syndrome tend to have comorbidities? If so, is this information helpful in establishing the diagnosis and planning therapy?
Dr. Haefner: Women who have vulvodynia often have other medical problems as well. In my practice, when new patients who have vulvodynia complete their intake survey, they often report a history of headache, irritable bowel syndrome, interstitial cystitis, fibromyalgia,6 chronic fatigue syndrome, back pain, and temporomandibular joint (TMJ) disorder. These comorbidities are not particularly helpful in establishing the diagnosis of vulvodynia, but they are an important consideration when choosing therapy for the patient. Often, the medications chosen to treat one condition will also benefit another condition. However, it’s important to check for potential interactions between drugs before prescribing a new treatment.
Dr. Gunter: A significant number of women who have vulvodynia also have other chronic pain syndromes. For example, the incidence of bladder pain syndrome–interstitial cystitis is 68% to 82% among women who have vulvodynia, compared with a baseline rate among all women of 6% to 11%.7-10 The rate of irritable bowel syndrome is more than doubled among women who have vulvodynia, compared with the general population (27% versus 12%).8 Another common comorbidity, hypertonic somatic dysfunction of the pelvic floor, is identified in 10% to 90% of women who have chronic vulvar pain.8,11,12 These women also have a higher incidence of nongenital pain syndromes, such as fibromyalgia, migraine, and TMJ dysfunction, than the general population, as Dr. Haefner noted.8,12,13
Many studies have evaluated psychological and emotional contributions to chronic vulvar pain. Pain and depression are intimately related—the incidence of depression among all people who experience chronic pain ranges from 27% to 54%, compared with 5% to 17% among the general population.14-16 The relationship is complex because chronic illness in general is associated with depression. Nevertheless, several studies have noted an increase in anxiety, stress, and depression among women who have vulvodynia.17-19
I screen every patient for depression using a Patient Health Questionnaire (PHQ-9); I also screen for anxiety. I find that a significant percentage of patients in my clinic are depressed or have an anxiety disorder. Failure to address these comorbidities makes treatment very difficult. I typically prescribe citalopram (Celexa), although there is some question whether it can safely be combined with a tricyclic antidepressant. We also offer stress-reduction classes, teach every patient the value of diaphragmatic breathing, offer mind-body classes for anxiety and stress, and provide intensive programs where the patient can learn important self-care skills, such as pacing (spacing activities throughout the day in a manner that avoids aggravating the pain), and address her anxiety and stress in a more guided manner. We also have a psychologist who specializes in pain for any patient who may need one-on-one counseling.
Dr. Edwards: The presence of comorbidities is somewhat useful in making the diagnosis of vulvodynia. I question my diagnosis, in fact, when a patient who has vulvodynia does not have headaches, low energy, depression, anxiety, irritable bowel syndrome, constipation, fibromyalgia, chronic fatigue, sensitivity to medications, TMJ dysfunction, or urinary symptoms.
![]()
Dr. Lonky: How prevalent is a finding of pudendal neuralgia?
Dr. Edwards: The prevalence and incidence of pudendal neuralgia are not known. Those who specialize in this condition think it is relatively common. I do not identify or suspect it very often. Its definitive diagnosis and management are outside the purview of the general gynecologist, but the general gynecologist should recognize the symptoms of pudendal neuralgia and refer the patient for evaluation and therapy.
Dr. Lonky: What are those symptoms?
Dr. Haefner: Pudendal neuralgia often occurs following trauma to the pudendal nerve. The pudendal nerve arises from sacral nerves, generally sacral nerves 2 to 4. Several tests can be utilized to diagnose this condition, including quantitative sensor tests, pudendal nerve motor latency tests, electromyography (EMG), and pudendal nerve blocks.20
Nantes Criteria allow for making a diagnosis of pudendal neuralgia (Table 3).21
TABLE 3
Nantes Criteria for pudendal neuralgia by pudendal nerve entrapment
| SOURCE: Labat et al.21 Reproduced with permission from Neurology and Urodynamics. |
Essential criteria
|
Complementary diagnostic criteria
|
Exclusion criteria
|
Associated signs not excluding the diagnosis
|
Initial treatments for pudendal neuralgia should be conservative. Treatments consist of lifestyle changes to prevent flare of disease. Physical therapy, medical management, nerve blocks, and alternative treatments may be beneficial.
Pudendal nerve entrapment is often exacerbated by sitting (not on a toilet seat, however) and is reduced in a standing position. It tends to increase in intensity throughout the day.22 The final treatment for pudendal nerve entrapment is surgery if the nerve is compressed. By this time, the generalist is not generally the provider who performs the surgery.
Dr. Gunter: I believe pudendal neuralgia is sometimes overdiagnosed. EMG studies of the pudendal nerve, often touted as a diagnostic tool, are unreliable (they can be abnormal after vaginal delivery or vaginal hysterectomy, for example). In my experience, bilateral pain is less likely to be pudendal neuralgia; spontaneous bilateral compression neuropathy at exactly the same level is not a common phenomenon in chronic pain.
I reserve the diagnosis of pudendal neuralgia for women who have allodynia in the distribution of the pudendal nerve with severe pain on sitting, and who have exquisite tenderness when pressure is applied over the pudendal nerve (at the level of the ischial spine on vaginal examination). Typically, the vaginal sidewall on the affected side is very sensitive to light touch. I do see pudendal nerve pain after vaginal surgery when there has been some compromise of the pudendal nerve or the sacral plexus. This is typically unilateral pain.
Dr. Lonky: Thank you all. We’ll continue our discussion, with a focus on treatment.
|
MORE TO COME
|
References
1. Thomas TG. Practical Treatise on the Diseases of Women. Philadelphia Pa: Henry C. Lea; 1874.
2. Harlow BL, Stewart EG. A population-based assessment of chronic unexplained vulvar pain: have we underestimated the prevalence of vulvodynia? J Am Med Womens Assoc. 2003;58(2):82–88.
3. Lavy RJ, Hynan LS, Haley RW. Prevalence of vulvar pain in an urban minority population. J Reprod Med. 2007;52(1):59–62.
4. Nyirjesy P, Peyton C, Weitz MV, Mathew L, Culhane JF. Causes of chronic vaginitis: analysis of a prospective database of affected women. Obstet Gynecol. 2006;108(5):1185–1191.
5. Moyal-Barracco M, Lynch PJ. 2003 ISSVD terminology and classification of vulvodynia: a historical perspective. J Reprod Med. 2004;49(10):772–777.
6. Yunas MB. Fibromyalgia and overlapping disorders: the unifying concept of central sensitivity syndromes. Semin Arthritis Rheum. 2007;36(6):339–356.
7. Kahn BS, Tatro C, Parsons CL, Willems JJ. Prevalence of interstitial cystitis in vulvodynia patients detected by bladder potassium sensitivity. J Sex Med. 2010;7(2 Pt 2):996–1002.
8. Arnold JD, Bachman GS, Rosen R, Kelly S, Rhoads GG. Vulvodynia: characteristics and associations with comorbidities and quality of life. Obstet Gynecol. 2006;107(3):617–624.
9. Parsons CL, Dell J, Stanford EJ, et al. The prevalence of interstitial cystitis in gynecologic patients with pelvic pain, as detected by intravesical potassium sensitivity. Am J Obstet Gynecol. 2002;187(5):1395–1400.
10. Clemens JQ, Meenan RT, O’Keefe Rosetti MC, et al. Prevalence of interstitial cystitis symptoms in a managed care population. J Urol. 2005;174(2):576–580.
11. Engman M, Lindehammar H, Wijma B. Surface electromyography diagnostics in women with partial vaginismus with or without vulvar vestibulitis and in asymptomatic women. J Psychosom Obstet Gynecol. 2004;25(3-4):281–294.
12. Gunter J. Vulvodynia: new thoughts on a devastating condition. Obstet Gynecol Surv. 2007;62(12):812–819.
13. Gordon AS, Panahlan-Jand M, McComb F, Melegari C, Sharp S. Characteristics of women with vulvar pain disorders: a Web-based survey. J Sex Marital Ther. 2003;29(suppl 1):45.
14. Whitten CE, Cristobal K. Chronic pain is a chronic condition not just a symptom. Permanente J. 2005;9(3):43.
15. Manchikanti L, Fellows B, Pampati V, et al. Comparison of psychological status of chronic pain patients and the general population. Pain Physician. 2002;5(1):40–48.
16. Banks SM, Kerns RD. Explaining the high rates of depression in chronic pain: a diathesis-stress framework. Psychological Bulletin. 1996;119(1):95–110.
17. Sadownik LA. Clinical correlates of vulvodynia patients. A prospective study of 300 patients. J Reprod Med. 2000;5:40–48. Editor found in PubMed: Sadownik LA. Clinical profile of vulvodynia patients. A prospective study of 300 patients. J Reprod Med. 2000;45(8):679–684. Could not find the citation listed. Please confirm.
18. Reed BD, Haefner HK, Punch MR, Roth RS, Gorenflo DW, Gillespie BW. Psychosocial and sexual functioning in women with vulvodynia and chronic pelvic pain. A comparative evaluation. J Reprod Med. 2000;45(8):624–632.
19. Landry T, Bergeron S. Biopsychosocial factors associated with dyspareunia in a community sample of adolescent girls. Arch Sex Behav. 2011; June 22.
20. Goldstein A, Pukall C, Goldstein I. When Sex Hurts: A Woman’s Guide to Banishing Sexual Pain. Cambridge Mass: Da Capo Lifelong Books; 2011;117–126.
21. Labat JJ, Riant T, Robert R, Amarenco G, Lefaucheur JP, Rigaud J. Diagnostic criteria for pudendal neuralgia by pudendal nerve entrapment (Nantes criteria). Neurol Urodyn. 2008;27(4):306–310.
22. Popeney C, Answell V, Renney K. Pudendal entrapment as an etiology of chronic perineal pain: Diagnosis and treatment. Neurol Urodyn. 2007;26(6):820–827.
Although the incidence of vulvar pain has increased over the past decade—thanks to both greater awareness and increasing numbers of affected women—the phenomenon is not a recent development. As early as 1874, T. Galliard Thomas wrote, “[T]his disorder, although fortunately not very frequent, is by no means very rare.”1 He went on to express “surprise” that it had not been “more generally and fully described.”
Despite the focus Thomas directed to the issue, vulvar pain did not get much attention until the 21st century, when a number of studies began to gauge its prevalence. For example, in a study in Boston of about 5,000 women, the lifetime prevalence of chronic vulvar pain was 16%.2 And in a study in Texas, the prevalence of vulvar pain in an urban, largely minority population was estimated to be 11%.3 The Boston study also reported that “nearly 40% of women chose not to seek treatment, and, of those who did, 60% saw three or more doctors, many of whom could not provide a diagnosis.”2
Clearly, there is a need for comprehensive information on vulvar pain and its causes, symptoms, diagnosis, and treatment. To address the lack of guidance, OBG Management Contributing Editor Neal M. Lonky, MD, assembled a panel of experts on vulvar pain syndromes and invited them to share their considerable knowledge. The ensuing discussion, presented in three parts, offers a gold mine of information. In this opening article, the panel focuses on causes, symptomatology, and diagnosis of this common complaint.
|
The lower vagina and vulva are richly supplied with peripheral nerves and are, therefore, sensitive to pain, particularly the region of the hymeneal ring. Although the pudendal nerve (arrow) courses through the area, it is an uncommon source of vulvar pain. |
![]()
Dr. Lonky: What are the most common diagnoses when vulvar pain is the complaint?
Dr. Gunter: The most common cause of chronic vulvar pain is vulvodynia, although lichen simplex chronicus, chronic yeast infections, and non-neoplastic epithelial disorders, such as lichen sclerosus and lichen planus, can also produce irritation and pain. In postmenopausal women, atrophic vaginitis can also cause a burning pain, although symptoms are typically more vaginal than vulvar. Yeast and lichen simplex chronicus typically produce itching, although sometimes they can present with irritation and pain, so they must be considered in the differential diagnosis. It is important to remember that many women with vulvodynia have used multiple topical agents and may have developed complex hygiene rituals in an attempt to treat their symptoms, which can result in a secondary lichen simplex chronicus.
That said, there is a high frequency of misdiagnosis with yeast. For example, in a study by Nyirjesy and colleagues, two thirds of women who were referred to a tertiary clinic for chronic vulvovaginal candidiasis were found to have a noninfectious entity instead—most commonly lichen simplex chronicus and vulvodynia.4
Dr. Edwards: The most common “diagnosis” for vulvar pain is vulvodynia. However, the definition of vulvodynia is pain—i.e., burning, rawness, irritation, soreness, aching, or stabbing or stinging sensations—in the absence of skin disease, infection, or specific neurologic disease. Therefore, even though the usual cause of vulvar pain is vulvodynia, it is a diagnosis of exclusion, and skin disease, infection, and neurologic disease must be ruled out.
In regard to infection, Candida albicans and bacterial vaginosis (BV) are usually the first conditions that are considered when a patient complains of vulvar pain, but they are not common causes of vulvar pain and are never causes of chronic vulvar pain. Very rarely they may cause recurrent pain that clears, at least briefly, with treatment.
Candida albicans is usually primarily pruritic, and BV produces discharge and odor, sometimes with minor symptoms. Non-albicans Candida (e.g., Candida glabrata) is nearly always asymptomatic, but it occasionally causes irritation and burning.
Group B streptococcus is another infectious entity that very, very occasionally causes irritation and dyspareunia but is usually only a colonizer.
Herpes simplex virus is a cause of recurrent but not chronic pain.
Chronic pain is more likely to be caused by skin disease than by infection. Lichen simplex chronicus causes itching; any pain is due to erosions from scratching.
Dr. Haefner: Several other infectious conditions or their treatments can cause vulvar pain. For example, herpes (particularly primary herpes infection) is classically associated with vulvar pain. The pain is so great that, at times, the patient requires admission for pain control. Surprisingly, despite the known pain of herpes, approximately 80% of patients who have it are unaware of their diagnosis.
Although condyloma is generally a painless condition, many patients complain of pain following treatment for it, whether treatment involves topical medications or laser surgery.
Chancroid is a painful vulvar ulcer. Trichomonas can sometimes be associated with vulvar pain.
Dr. Lonky: What terminology do we use when we discuss vulvar pain?
Dr. Haefner: The current terminology used to describe vulvar pain was published in 2004, after years of debate over nomenclature within the International Society for the Study of Vulvovaginal Disease.5 The terminology lists two major categories of vulvar pain:
-
pain related to a specific disorder. This category encompasses numerous conditions that feature an abnormal appearance of the vulva (Table 1).
TABLE 1
Terminology and classification of vulvar pain from the International Society for the Study of Vulvovaginal Disease
| SOURCE: Moyal-Barracco and Lynch.5 Reproduced with permission from the Journal of Reproductive Medicine. |
|
-
vulvodynia, in which the vulva appears normal, other than occasional erythema, which is most prominent at the duct openings (vestibular ducts—Bartholin’s and Skene’s).
As for vulvar pain, there are two major forms:
-
hyperalgesia (a low threshold for pain)
-
allodynia (pain in response to light touch).
Some diseases that are associated with vulvar pain do not qualify for the diagnosis of vulvodynia (Table 2) because they are associated with an abnormal appearance of the vulva.
TABLE 2
Conditions other than vulvodynia that are associated with vulvar pain
| Acute irritant contact dermatitis (e.g., erosion due to podofilox, imiquimod, cantharidin, fluorouracil, or podophyllin toxin) |
| Aphthous ulcer |
| Atrophy |
| Bartholin’s abscess |
| Candidiasis |
| Carcinoma |
| Chronic irritant contact dermatitis |
| Endometriosis |
| Herpes (simplex and zoster) |
| Immunobullous diseases (including cicatricial pemphigoid, pemphigus vulgaris, linear immunoglobulin A disease, etc.) |
| Lichen planus |
| Lichen sclerosus |
| Podophyllin overdose (see above) |
| Prolapsed urethra |
| Sjögren’s syndrome |
| Trauma |
| Trichomoniasis |
| Vulvar intraepithelial neoplasia |
![]()
Dr. Lonky: What skin diseases need to be ruled out before vulvodynia can be diagnosed?
Dr. Edwards: Skin diseases that affect the vulva are usually pruritic—pain is a later sign. Lichen simplex chronicus (also known as eczema) is pruritus caused by any irritant; any pain that arises is produced by visible excoriations from scratching.
Lichen sclerosus manifests as white epithelium that has a crinkling, shiny, or waxy texture. It can produce pain, especially dyspareunia. The pain is caused by erosions that arise from fragility and introital narrowing and inelasticity.
Vulvovaginal lichen planus is usually erosive and preferentially affects mucous membranes, especially the vestibule; it sometimes affects the vagina and mouth, as well.
Desquamative inflammatory vaginitis is most likely a skin disease that affects only the vagina. It involves introital redness and a clinically and microscopically purulent vaginal discharge that also reveals parabasal cells and absent lactobacilli.
Dr. Lonky: You mentioned that neurologic diseases can sometimes cause vulvar pain. Which ones?
Dr. Edwards: Pudendal neuralgia, diabetic neuropathy, and post-herpetic neuralgia are the most common specific neurologic causes of vulvar pain. Multiple sclerosis can also produce pain syndromes. Post-herpetic neuralgia follows herpes zoster—not herpes simplex—virus infection.
Dr. Lonky: Any other conditions that can cause vulvar pain?
Dr. Haefner: Aphthous ulcers are common and are often flared by stress.
Non-neoplastic epithelial disorders are also seen frequently in health-care providers’ offices; many patients who experience them report pain on the vulva.
It is always important to consider cancer when a patient has an abnormal vulvar appearance and pain that has persisted despite treatment.
![]()
Dr. Lonky: If you were to rank vulvar pain syndromes according to their prevalence, what would the most common syndromes be?
Dr. Gunter: Given the misdiagnosis of many women, who are told they have chronic yeast infection, as I mentioned, it’s hard to know which vulvar pain syndromes are most prevalent. I suspect that lichen simplex chronicus is most common, followed by vulvodynia, with chronic yeast infection a distant third.
My experience reflects what Nyirjesy and colleagues4 found: 65% to 75% of women referred to my clinic with chronic yeast actually have lichen simplex chronicus or vulvodynia. In postmenopausal women, atrophic vaginitis is also a consideration; it’s becoming more common now that the use of systemic hormone replacement therapy is decreasing.
Dr. Lonky: What about subsets of vulvodynia? Which ones are most common?
Dr. Edwards: There is good evidence of marked overlap among subsets of vulvodynia. The vast majority of women who have vulvodynia experience primarily provoked vestibular pain, regardless of age. However, I find that almost all patients also report pain that extends beyond the vestibule at times, as well as occasional unprovoked pain.
The diagnosis requires the exclusion of other causes of vulvar pain, and the subset is identified by the location of pain (that is, is it strictly localized or generalized or even migratory?) and its provoked or unprovoked nature.
Localized clitoral pain and vulvar pain localized to one side of the vulva are extremely uncommon, but they do occur. And although I rarely encounter teenagers and prepubertal children who have vulvodynia, I do have patients in both age groups who have vulvodynia.
Dr. Lonky: Are there racial differences in the prevalence of vulvodynia?
Dr. Edwards: Although several good studies show that women of African descent and white patients are equally likely to experience vulvodynia, the vast majority (99%) of my patients who have vulvodynia are white. My patients of African descent consult me primarily for itching or discharge.
My local demographics prevent me from judging the likelihood of Asians having vulvodynia, and our Hispanic population has limited access to health care.
In general, I don’t think that demographics are useful in making the diagnosis of vulvodynia.
![]()
Dr. Lonky: Do your patients who have vulvodynia or another vulvar pain syndrome tend to have comorbidities? If so, is this information helpful in establishing the diagnosis and planning therapy?
Dr. Haefner: Women who have vulvodynia often have other medical problems as well. In my practice, when new patients who have vulvodynia complete their intake survey, they often report a history of headache, irritable bowel syndrome, interstitial cystitis, fibromyalgia,6 chronic fatigue syndrome, back pain, and temporomandibular joint (TMJ) disorder. These comorbidities are not particularly helpful in establishing the diagnosis of vulvodynia, but they are an important consideration when choosing therapy for the patient. Often, the medications chosen to treat one condition will also benefit another condition. However, it’s important to check for potential interactions between drugs before prescribing a new treatment.
Dr. Gunter: A significant number of women who have vulvodynia also have other chronic pain syndromes. For example, the incidence of bladder pain syndrome–interstitial cystitis is 68% to 82% among women who have vulvodynia, compared with a baseline rate among all women of 6% to 11%.7-10 The rate of irritable bowel syndrome is more than doubled among women who have vulvodynia, compared with the general population (27% versus 12%).8 Another common comorbidity, hypertonic somatic dysfunction of the pelvic floor, is identified in 10% to 90% of women who have chronic vulvar pain.8,11,12 These women also have a higher incidence of nongenital pain syndromes, such as fibromyalgia, migraine, and TMJ dysfunction, than the general population, as Dr. Haefner noted.8,12,13
Many studies have evaluated psychological and emotional contributions to chronic vulvar pain. Pain and depression are intimately related—the incidence of depression among all people who experience chronic pain ranges from 27% to 54%, compared with 5% to 17% among the general population.14-16 The relationship is complex because chronic illness in general is associated with depression. Nevertheless, several studies have noted an increase in anxiety, stress, and depression among women who have vulvodynia.17-19
I screen every patient for depression using a Patient Health Questionnaire (PHQ-9); I also screen for anxiety. I find that a significant percentage of patients in my clinic are depressed or have an anxiety disorder. Failure to address these comorbidities makes treatment very difficult. I typically prescribe citalopram (Celexa), although there is some question whether it can safely be combined with a tricyclic antidepressant. We also offer stress-reduction classes, teach every patient the value of diaphragmatic breathing, offer mind-body classes for anxiety and stress, and provide intensive programs where the patient can learn important self-care skills, such as pacing (spacing activities throughout the day in a manner that avoids aggravating the pain), and address her anxiety and stress in a more guided manner. We also have a psychologist who specializes in pain for any patient who may need one-on-one counseling.
Dr. Edwards: The presence of comorbidities is somewhat useful in making the diagnosis of vulvodynia. I question my diagnosis, in fact, when a patient who has vulvodynia does not have headaches, low energy, depression, anxiety, irritable bowel syndrome, constipation, fibromyalgia, chronic fatigue, sensitivity to medications, TMJ dysfunction, or urinary symptoms.
![]()
Dr. Lonky: How prevalent is a finding of pudendal neuralgia?
Dr. Edwards: The prevalence and incidence of pudendal neuralgia are not known. Those who specialize in this condition think it is relatively common. I do not identify or suspect it very often. Its definitive diagnosis and management are outside the purview of the general gynecologist, but the general gynecologist should recognize the symptoms of pudendal neuralgia and refer the patient for evaluation and therapy.
Dr. Lonky: What are those symptoms?
Dr. Haefner: Pudendal neuralgia often occurs following trauma to the pudendal nerve. The pudendal nerve arises from sacral nerves, generally sacral nerves 2 to 4. Several tests can be utilized to diagnose this condition, including quantitative sensor tests, pudendal nerve motor latency tests, electromyography (EMG), and pudendal nerve blocks.20
Nantes Criteria allow for making a diagnosis of pudendal neuralgia (Table 3).21
TABLE 3
Nantes Criteria for pudendal neuralgia by pudendal nerve entrapment
| SOURCE: Labat et al.21 Reproduced with permission from Neurology and Urodynamics. |
Essential criteria
|
Complementary diagnostic criteria
|
Exclusion criteria
|
Associated signs not excluding the diagnosis
|
Initial treatments for pudendal neuralgia should be conservative. Treatments consist of lifestyle changes to prevent flare of disease. Physical therapy, medical management, nerve blocks, and alternative treatments may be beneficial.
Pudendal nerve entrapment is often exacerbated by sitting (not on a toilet seat, however) and is reduced in a standing position. It tends to increase in intensity throughout the day.22 The final treatment for pudendal nerve entrapment is surgery if the nerve is compressed. By this time, the generalist is not generally the provider who performs the surgery.
Dr. Gunter: I believe pudendal neuralgia is sometimes overdiagnosed. EMG studies of the pudendal nerve, often touted as a diagnostic tool, are unreliable (they can be abnormal after vaginal delivery or vaginal hysterectomy, for example). In my experience, bilateral pain is less likely to be pudendal neuralgia; spontaneous bilateral compression neuropathy at exactly the same level is not a common phenomenon in chronic pain.
I reserve the diagnosis of pudendal neuralgia for women who have allodynia in the distribution of the pudendal nerve with severe pain on sitting, and who have exquisite tenderness when pressure is applied over the pudendal nerve (at the level of the ischial spine on vaginal examination). Typically, the vaginal sidewall on the affected side is very sensitive to light touch. I do see pudendal nerve pain after vaginal surgery when there has been some compromise of the pudendal nerve or the sacral plexus. This is typically unilateral pain.
Dr. Lonky: Thank you all. We’ll continue our discussion, with a focus on treatment.
|
MORE TO COME
|
References
1. Thomas TG. Practical Treatise on the Diseases of Women. Philadelphia Pa: Henry C. Lea; 1874.
2. Harlow BL, Stewart EG. A population-based assessment of chronic unexplained vulvar pain: have we underestimated the prevalence of vulvodynia? J Am Med Womens Assoc. 2003;58(2):82–88.
3. Lavy RJ, Hynan LS, Haley RW. Prevalence of vulvar pain in an urban minority population. J Reprod Med. 2007;52(1):59–62.
4. Nyirjesy P, Peyton C, Weitz MV, Mathew L, Culhane JF. Causes of chronic vaginitis: analysis of a prospective database of affected women. Obstet Gynecol. 2006;108(5):1185–1191.
5. Moyal-Barracco M, Lynch PJ. 2003 ISSVD terminology and classification of vulvodynia: a historical perspective. J Reprod Med. 2004;49(10):772–777.
6. Yunas MB. Fibromyalgia and overlapping disorders: the unifying concept of central sensitivity syndromes. Semin Arthritis Rheum. 2007;36(6):339–356.
7. Kahn BS, Tatro C, Parsons CL, Willems JJ. Prevalence of interstitial cystitis in vulvodynia patients detected by bladder potassium sensitivity. J Sex Med. 2010;7(2 Pt 2):996–1002.
8. Arnold JD, Bachman GS, Rosen R, Kelly S, Rhoads GG. Vulvodynia: characteristics and associations with comorbidities and quality of life. Obstet Gynecol. 2006;107(3):617–624.
9. Parsons CL, Dell J, Stanford EJ, et al. The prevalence of interstitial cystitis in gynecologic patients with pelvic pain, as detected by intravesical potassium sensitivity. Am J Obstet Gynecol. 2002;187(5):1395–1400.
10. Clemens JQ, Meenan RT, O’Keefe Rosetti MC, et al. Prevalence of interstitial cystitis symptoms in a managed care population. J Urol. 2005;174(2):576–580.
11. Engman M, Lindehammar H, Wijma B. Surface electromyography diagnostics in women with partial vaginismus with or without vulvar vestibulitis and in asymptomatic women. J Psychosom Obstet Gynecol. 2004;25(3-4):281–294.
12. Gunter J. Vulvodynia: new thoughts on a devastating condition. Obstet Gynecol Surv. 2007;62(12):812–819.
13. Gordon AS, Panahlan-Jand M, McComb F, Melegari C, Sharp S. Characteristics of women with vulvar pain disorders: a Web-based survey. J Sex Marital Ther. 2003;29(suppl 1):45.
14. Whitten CE, Cristobal K. Chronic pain is a chronic condition not just a symptom. Permanente J. 2005;9(3):43.
15. Manchikanti L, Fellows B, Pampati V, et al. Comparison of psychological status of chronic pain patients and the general population. Pain Physician. 2002;5(1):40–48.
16. Banks SM, Kerns RD. Explaining the high rates of depression in chronic pain: a diathesis-stress framework. Psychological Bulletin. 1996;119(1):95–110.
17. Sadownik LA. Clinical correlates of vulvodynia patients. A prospective study of 300 patients. J Reprod Med. 2000;5:40–48. Editor found in PubMed: Sadownik LA. Clinical profile of vulvodynia patients. A prospective study of 300 patients. J Reprod Med. 2000;45(8):679–684. Could not find the citation listed. Please confirm.
18. Reed BD, Haefner HK, Punch MR, Roth RS, Gorenflo DW, Gillespie BW. Psychosocial and sexual functioning in women with vulvodynia and chronic pelvic pain. A comparative evaluation. J Reprod Med. 2000;45(8):624–632.
19. Landry T, Bergeron S. Biopsychosocial factors associated with dyspareunia in a community sample of adolescent girls. Arch Sex Behav. 2011; June 22.
20. Goldstein A, Pukall C, Goldstein I. When Sex Hurts: A Woman’s Guide to Banishing Sexual Pain. Cambridge Mass: Da Capo Lifelong Books; 2011;117–126.
21. Labat JJ, Riant T, Robert R, Amarenco G, Lefaucheur JP, Rigaud J. Diagnostic criteria for pudendal neuralgia by pudendal nerve entrapment (Nantes criteria). Neurol Urodyn. 2008;27(4):306–310.
22. Popeney C, Answell V, Renney K. Pudendal entrapment as an etiology of chronic perineal pain: Diagnosis and treatment. Neurol Urodyn. 2007;26(6):820–827.
Why (and how) you should encourage your patients’ search for health information on the Web
CASE: The Internet has (at least) two faces
Both Patient A and Patient B are 8 weeks pregnant with their first baby. At an office visit, you discuss influenza vaccination.
Patient A tells you: “I was undecided about the vaccine until I read all these horror stories about the H1N1 vaccine. A Web site, organichealthadviser.com, says vaccines and pregnancies don’t mix safely.1 It says that if the flu vaccine isn’t safe for a baby less than 6 months old, how can it be safe during pregnancy?1 I read story after story of women who got the vaccine and miscarried. Why would I want to be injected with a toxin?”
Patient B explains: “I was undecided about the vaccine until I read the information on the Centers for Disease Control and Prevention (CDC) Web site.2 I didn’t know that pregnant women are more likely to get really sick from the flu. The CDC says the vaccine is safe during pregnancy, will not harm my baby, and not only reduces my chance of getting sick from the flu, but will give my baby protection for 6 months after she is born.2 When and where can I get my shot?”
Sixty-nine percent of Americans (80% of those who have Internet access) turn to the Web for information about their health care, and 23% of people who have a major medical illness or other health condition report that the Internet plays a major role in helping them deal with their health issue.3,4 They might research symptoms, diagnosis, tests, and therapies before a visit to your office; many come armed with questions, sometimes bringing reams of pages downloaded from various sites. Among women receiving ObGyn care, almost 60% have accessed Web-based information before their visit.5 Others take to the Internet after their appointment to confirm or refute what they have heard in the office.
Regardless of what a patient researches or when she does it, the why is because she wants to be an active participant in her medical care. That is a good thing because participatory medicine (shared decision-making) leads to improved outcomes. However, the key to truly informed decision-making is content: A patient can be fully empowered to participate in her health care only if she has information that is accurate, understandable, and current.
Web-based health information: Entirely factual?
Not only do patients research health online, 60% of people believe what they read to be factual and at least as good as the information they receive from you in your office. In fact, there is evidence that only 6% believe the health information they gather online is lacking in quality.5,6
However, studies reveal that the accuracy of medical content on the Web varies greatly from site to site. For example, among women seeking information on the Internet about potential teratogenic agents, 40% found incorrect information, some of which was potentially harmful.7
In addition to the problem of potentially suspect content, more than 50% of patients don’t disclose with you the information that they find online.7 Ever encounter a patient you just couldn’t sway from a diagnosis she believed she had but you knew she didn’t? If your patient tells you where she got the information, you can walk her through the diagnosis and treatment step by step, pointing out where her information might not be accurate (or, sometimes, even medically plausible)—but it’s hard to undo what you don’t know about.
The ideal scenario. Discuss Web-based information as part of your visit, thereby acknowledging that the Internet is a valid place to investigate personal health care. You can also preemptively provide tools for tracking down the most accurate and understandable content. See, for example, the patient handout.
Let’s face it: Physicians have an advantage when it comes to weeding out the wisdom from the woo. To supplement our baseline knowledge, we can easily research facts on PubMed, check our medical societies for guidelines, or, simply, ask a colleague. Our patients don’t have these same resources, but with some guidance from you, their Internet health experience can be greatly enhanced.
Are your searches on the Internet turning up reliable health advice? Watch for these 10 red flags of bad information
- Sensationalized content Is the information on the site presented in an alarmist tone? Is it loaded with scary stories and extreme outcomes? Are the issues presented in terms of black and white, with no shades of gray? If the answer to any of these questions is “Yes,” the author may have an axe to grind or a hidden leaning. Suspect the accuracy of the information you obtain!
- No date This may seem like a minor problem, but the world of health care moves swiftly. Treatments and approaches that are reliable one day can be discredited in the blink of an eye. If the site does not date its content, or indicate when it was last updated, you have no way of knowing how current it is. Move on!
- No author credentials The author or authors of material on the Web site should clearly, and visibly, present their credentials—that is, their education and training, their title, and where they work. If they do not, it is impossible to judge their expertise—in fact, expertise may be lacking.
- Buzz words The use of quasi-scientific buzz words such as “toxins,” “heavy metals,” and “detoxification” should draw your attention. These words have no meaning, so they should lead to you question what else on the site might be fiction.
- Patient testimonials Three people may have improved with a particular drug, but what about those who haven’t? Using unverified personal experiences is a sign of advertising, not good medicine.
- For sale sign If you can’t easily tell the difference between the medical content and products for sale, move along. Even when products don’t appear prominently, chances are that the bottom line of the Web site is profit, not education.
- All benefits and no risks Sites that have a stake in a particular treatment—be it monetary, emotional, or some other involvement—usually provide a lot of information on benefits but not so much about risks. Every treatment has risks.
- No sources When physicians scrutinize an article or study, they make it a point to check the list of sources at the end, to ensure that it contains legitimate information, such as reports from a medical journal or government publication. A Web site that presents detailed medical information without providing links to the references or comparable detail about the sources of that information is highly suspect.
- Conflict of interest Most reputable health sites not only provide information from experts, they list any so-called potential conflicts of interest that those experts may have. For example, if a medication made by XYZ Pharmaceuticals is recommended by Dr. Smith, who is also a consultant to XYZ, you should know. Articles and presentations at scientific meetings require these disclosures for a reason: Financial ties can produce bias.
- The Web site or product is listed on QuackWatch This Web site is dedicated to exposing unproven and scientifically questionable medical claims (http://www.quackwatch.com).
Where can you turn for help?
- An excellent starting place is the National Medical Library Web site at http://www.mlanet.org/resources/userguide.html, which provides resources for obtaining reliable health information.
- The National Library of Medicine and National Institutes of Health also provide an outstanding 16-minute lesson on how you can evaluate online health information. Find it at http://www.nlm.nih.gov/medlineplus/webeval/webeval.html.
- healthfinder.gov is a Web “encyclopedia” offering entries on more than 1,600 health topics.
© Copyright 2011 Quadrant HealthCom, Inc. This “Guide” may be reproduced by clinicians without permission or fee for single-copy distribution to patients. All other uses require the written permission of the publisher.
To obtain a PDF of this Patient Guide, click here .
Four tips for evaluating online content
Consider the source
The very first thing to consider is the domain name—e.g., “.gov,” “.org,” “.edu,” “.com,” or .anythingelse.
.gov sites are owned and maintained by the US government. From a medical standpoint, the .gov designation means that a site contains evidence-based information maintained by medical librarians that is written at a level that most people can read.
It’s a common misperception that the .org designation indicates a not-for-profit site that is therefore “looking out for the public’s best interest.” But anyone can purchase an .org domain. Even if a particular site really is administered by a not-for-profit organization, that status does not ensure that the content is of high quality.
.edu sites are affiliated with academic institutions.
.com and .anythingelse are, like .org, free for anyone to purchase.
Evidence-based medicine tells us that .gov sites are the most accurate for content—anything else is buyer beware (interestingly, .edu sites fared the worst in one study for accuracy).7,8 This doesn’t mean that sites that are not .gov have no value! On the contrary, non-governmental Web sites, blogs, and news articles are often the first place a search starts. That’s because current content, such as a new site, is more likely to feature prominently in a search engine response. But non-governmental sites do require an additional level of scrutiny. For example, in one study, only 55% of health information on news Web sites was medically accurate.8
Who is the author? Does she have financial ties or bias?
Think about who is running the Web site, why they are doing it, and what they are trying to achieve. Is the author a doctor, a health reporter, an advocate, or a drug company? The credentials of any physicians associated with the site should be listed as well as credentials and affiliations of authors, if they are non-physicians. Sites that list physician credentials tend to rate higher in accuracy of content.7
Talk with your patients about the importance of financial ties. The sponsor of the Web site should be listed (drug company, university, or a physician blogging without reimbursement). Bias and money go hand in hand, so be careful in evaluating whether the information provided favors the sponsor. If there are products for sale that are recommended by the medical content, bias is implied and, in my opinion, that site is not informational but commercial.
Bias can also be non-commercial, which is why authors of academic papers are not only supposed to report financial ties but also any real or perceived conflict of interest. This can be hard to discern at times, but the Web site should disclose why it exists. If the message is muddied by advertising and other commercial content, it’s best to just move along.
How current is the content?
We all know that new studies constantly reshape the way we practice (and sometimes guidelines from professional societies seem to change with the wind), and what is new quickly becomes out of date. The good and bad with online information is that it is always there. A permanent record is in many ways a good thing, but content from 2004 may not be applicable in 2011. This is a particular issue with news sites. They may report on a fascinating study in 2007, but if a retraction later appears or a new study refutes the findings, that information may not warrant an article on the Web. A good rule of thumb: Anything older than 2 years requires an additional level of scrutiny.
Be wary when the subject is complementary and alternative medicine
Online content related to complementary and alternative medicine (CAM) should be approached with a higher degree of caution. One study found that 25% of CAM sites presented information that could cause physical harm if acted upon, and almost all CAM sites omitted vital warnings, such as drug interactions, contraindications, and adverse reactions. The quality of CAM sites doesn’t improve even when they meet three or four of the JAMA benchmarks for information quality (see page 40).9 In one study of breast cancer sites, Web pages with CAM content were 15 times more likely to contain inaccurate content, compared with sites without CAM content.7

Instruments and tools for evaluating online content
Three tools are available to help patients and providers judge the quality of written online information:
Discern is a 16-question tool designed to assess the quality of online health information. You will find it at http://www.discern.org.uk/discern_instrument.php. I recommend that you mention this tool to patients, even if you are uncertain whether they will use it. Certainly, any patient wedded to what seems like questionable content from a specific Web site should be encouraged to evaluate the site using the Discern tool. In addition, if you have Web sites other than .gov sites that you like to share with patients, it might be wise to personally review them with Discern so that you can reaffirm that you are directing patients to reliable content rather than a quagmire of misinformation.10
The Health on the Net Foundation (HON) is an independent, seven-person, Geneva-based panel that evaluates accuracy of medical Web sites based on specific guiding principles. It can be accessed at http://www.hon.ch/. Web sites that meet these criteria are awarded seals of approval. Only one problem: Not all sites that carry the seal are compliant with HON, and sites that don’t carry the seal can nevertheless be complete and accurate.11,12
JAMA benchmarks are four disclosures intended to help ensure the quality of a Web site: authorship, references, conflict of interest, and currency of content. Some research suggests that sites that have three or four of the benchmarks are more likely to have accurate content, but there is also evidence to suggest that JAMA benchmarks may not always reliably identify inaccurate information.7,13
Recommend a mini-course
Because these tools may be difficult to use or unreliable at identifying quality content, I recommend that every patient spend time on the National Medical Library Web site learning how to look up information. The other benefit of this site is that it lists top 10 Web sites for content, so it is a great launching point for a multitude of searches. It can be found at http://www.mlanet.org/resources/userguide.html.
If the patient finds the information at this portal too dry, there is a fantastic 16-minute tutorial about evaluating online health information; it’s a service of the National Library of Medicine and the National Institutes of Health. I recommend that every provider do this tutorial. Why? So you can better educate yourself on how to use the Internet and so you can tell your patients how great it is. It’s available at http://www.nlm.nih.gov/medlineplus/webeval/webeval.html.
Take the bull by the horns
Discuss the Internet with every one of your patients. Specifically, ask if she has read any information online and, if she has, how it stacks up with what you have just discussed during her office visit. That’s what I do. Explain that accurate content is critical in health-care decisions, guide your patient to sites that are more likely to be accurate, and teach her how to maximize the Internet to enhance her health care.
In my experience, patients are thrilled to be pointed in the right direction.
We want to hear from you! Tell us what you think.
1. H1N1 vaccine and pregnancy. Organic Health Adviser. http://organichealthadviser.com/archives/h1n1-vaccine-and-pregnancy. Accessed November 12 2011.
2. Pregnant women and influenza. Centers for Disease Control and Prevention. http://www.cdc.gov/flu/protect/vaccine/pregnant.htm. Accessed November 12 2011.
3. Fox S. The social life of health information 2011. Pew Internet and American Life Project. http://pewresearch.org/pubs/1989/health-care-online-social-network-users. Accessed November 12, 2011.
4. Horrigan J, Rainie L. The Internet’s growing role in life’s major moments. Decision-making Communities, Health. Pew Internet and American Life Project. http://www.pewinternet.org/Reports/2006/The-Internets-Growing-Role-in-Lifes-Major-Moments.aspx. Accessed November 12, 2011.
5. Neelapala P, Duvvi SK, Kumar G, Kumar BN. Do gynaecology outpatients use the Internet to seek health information? A questionnaire survey. J Eval Clin Pract. 2008;14(2):300-304.
6. Diaz JA, Griffith RA, Ng JJ, Reinert SE, Friedmann PD, Moulton AW. Patients’ use of the Internet for medical information. J Gen Intern Med. 2001;17(3):180-185.
7. Bernstam EV, Walji MF, Sagaram S, Sagaram D, Johnson CW, Meric-Bernstam F. Commonly cited website quality criteria are not effective at identifying inaccurate online information about breast cancer. Cancer. 2008;112(6):1206-1213.
8. Scullard P, Peacock C, Davies P. Googling children’s health: reliability of medical information on the Internet. Arch Dis Child. 2010;95(8):580-582.
9. Walji M, Sagaram S, Sagaram D, et al. Efficacy of quality criteria to identify potentially harmful information: a cross-sectional survey of complementary and alternative medicine web sites. J Med Internet Res. 2004;6(2):e21.-
10. Charnock D, Shepperd S, Needham G, Gann R. Discern: an instrument for judging the quality of written consumer health information on treatment choices. J Epidemiol Community Health. 1999;53(2):105-111.
11. Hardwick JC, MacKenzie FM. Information contained in miscarriage-related websites and the predictive value of website scoring systems. Eur J Gynecol Reprod Biol. 2003;106(1):60-63.
12. Khazaal Y, Chatton A, Zullino D. HON label and Discern as content quality indicators of health-related websites [published online ahead of print May 2011]. Psychiatr Q. doi: 10.1007/s11126-011-9179-x.
13. Meric F, Bernstam EV, Mirza NQ, et al. Breast cancer on the world wide web: cross sectional survey of quality of information and popularity of websites. BMJ. 2002;324(7337):577-581.
CASE: The Internet has (at least) two faces
Both Patient A and Patient B are 8 weeks pregnant with their first baby. At an office visit, you discuss influenza vaccination.
Patient A tells you: “I was undecided about the vaccine until I read all these horror stories about the H1N1 vaccine. A Web site, organichealthadviser.com, says vaccines and pregnancies don’t mix safely.1 It says that if the flu vaccine isn’t safe for a baby less than 6 months old, how can it be safe during pregnancy?1 I read story after story of women who got the vaccine and miscarried. Why would I want to be injected with a toxin?”
Patient B explains: “I was undecided about the vaccine until I read the information on the Centers for Disease Control and Prevention (CDC) Web site.2 I didn’t know that pregnant women are more likely to get really sick from the flu. The CDC says the vaccine is safe during pregnancy, will not harm my baby, and not only reduces my chance of getting sick from the flu, but will give my baby protection for 6 months after she is born.2 When and where can I get my shot?”
Sixty-nine percent of Americans (80% of those who have Internet access) turn to the Web for information about their health care, and 23% of people who have a major medical illness or other health condition report that the Internet plays a major role in helping them deal with their health issue.3,4 They might research symptoms, diagnosis, tests, and therapies before a visit to your office; many come armed with questions, sometimes bringing reams of pages downloaded from various sites. Among women receiving ObGyn care, almost 60% have accessed Web-based information before their visit.5 Others take to the Internet after their appointment to confirm or refute what they have heard in the office.
Regardless of what a patient researches or when she does it, the why is because she wants to be an active participant in her medical care. That is a good thing because participatory medicine (shared decision-making) leads to improved outcomes. However, the key to truly informed decision-making is content: A patient can be fully empowered to participate in her health care only if she has information that is accurate, understandable, and current.
Web-based health information: Entirely factual?
Not only do patients research health online, 60% of people believe what they read to be factual and at least as good as the information they receive from you in your office. In fact, there is evidence that only 6% believe the health information they gather online is lacking in quality.5,6
However, studies reveal that the accuracy of medical content on the Web varies greatly from site to site. For example, among women seeking information on the Internet about potential teratogenic agents, 40% found incorrect information, some of which was potentially harmful.7
In addition to the problem of potentially suspect content, more than 50% of patients don’t disclose with you the information that they find online.7 Ever encounter a patient you just couldn’t sway from a diagnosis she believed she had but you knew she didn’t? If your patient tells you where she got the information, you can walk her through the diagnosis and treatment step by step, pointing out where her information might not be accurate (or, sometimes, even medically plausible)—but it’s hard to undo what you don’t know about.
The ideal scenario. Discuss Web-based information as part of your visit, thereby acknowledging that the Internet is a valid place to investigate personal health care. You can also preemptively provide tools for tracking down the most accurate and understandable content. See, for example, the patient handout.
Let’s face it: Physicians have an advantage when it comes to weeding out the wisdom from the woo. To supplement our baseline knowledge, we can easily research facts on PubMed, check our medical societies for guidelines, or, simply, ask a colleague. Our patients don’t have these same resources, but with some guidance from you, their Internet health experience can be greatly enhanced.
Are your searches on the Internet turning up reliable health advice? Watch for these 10 red flags of bad information
- Sensationalized content Is the information on the site presented in an alarmist tone? Is it loaded with scary stories and extreme outcomes? Are the issues presented in terms of black and white, with no shades of gray? If the answer to any of these questions is “Yes,” the author may have an axe to grind or a hidden leaning. Suspect the accuracy of the information you obtain!
- No date This may seem like a minor problem, but the world of health care moves swiftly. Treatments and approaches that are reliable one day can be discredited in the blink of an eye. If the site does not date its content, or indicate when it was last updated, you have no way of knowing how current it is. Move on!
- No author credentials The author or authors of material on the Web site should clearly, and visibly, present their credentials—that is, their education and training, their title, and where they work. If they do not, it is impossible to judge their expertise—in fact, expertise may be lacking.
- Buzz words The use of quasi-scientific buzz words such as “toxins,” “heavy metals,” and “detoxification” should draw your attention. These words have no meaning, so they should lead to you question what else on the site might be fiction.
- Patient testimonials Three people may have improved with a particular drug, but what about those who haven’t? Using unverified personal experiences is a sign of advertising, not good medicine.
- For sale sign If you can’t easily tell the difference between the medical content and products for sale, move along. Even when products don’t appear prominently, chances are that the bottom line of the Web site is profit, not education.
- All benefits and no risks Sites that have a stake in a particular treatment—be it monetary, emotional, or some other involvement—usually provide a lot of information on benefits but not so much about risks. Every treatment has risks.
- No sources When physicians scrutinize an article or study, they make it a point to check the list of sources at the end, to ensure that it contains legitimate information, such as reports from a medical journal or government publication. A Web site that presents detailed medical information without providing links to the references or comparable detail about the sources of that information is highly suspect.
- Conflict of interest Most reputable health sites not only provide information from experts, they list any so-called potential conflicts of interest that those experts may have. For example, if a medication made by XYZ Pharmaceuticals is recommended by Dr. Smith, who is also a consultant to XYZ, you should know. Articles and presentations at scientific meetings require these disclosures for a reason: Financial ties can produce bias.
- The Web site or product is listed on QuackWatch This Web site is dedicated to exposing unproven and scientifically questionable medical claims (http://www.quackwatch.com).
Where can you turn for help?
- An excellent starting place is the National Medical Library Web site at http://www.mlanet.org/resources/userguide.html, which provides resources for obtaining reliable health information.
- The National Library of Medicine and National Institutes of Health also provide an outstanding 16-minute lesson on how you can evaluate online health information. Find it at http://www.nlm.nih.gov/medlineplus/webeval/webeval.html.
- healthfinder.gov is a Web “encyclopedia” offering entries on more than 1,600 health topics.
© Copyright 2011 Quadrant HealthCom, Inc. This “Guide” may be reproduced by clinicians without permission or fee for single-copy distribution to patients. All other uses require the written permission of the publisher.
To obtain a PDF of this Patient Guide, click here .
Four tips for evaluating online content
Consider the source
The very first thing to consider is the domain name—e.g., “.gov,” “.org,” “.edu,” “.com,” or .anythingelse.
.gov sites are owned and maintained by the US government. From a medical standpoint, the .gov designation means that a site contains evidence-based information maintained by medical librarians that is written at a level that most people can read.
It’s a common misperception that the .org designation indicates a not-for-profit site that is therefore “looking out for the public’s best interest.” But anyone can purchase an .org domain. Even if a particular site really is administered by a not-for-profit organization, that status does not ensure that the content is of high quality.
.edu sites are affiliated with academic institutions.
.com and .anythingelse are, like .org, free for anyone to purchase.
Evidence-based medicine tells us that .gov sites are the most accurate for content—anything else is buyer beware (interestingly, .edu sites fared the worst in one study for accuracy).7,8 This doesn’t mean that sites that are not .gov have no value! On the contrary, non-governmental Web sites, blogs, and news articles are often the first place a search starts. That’s because current content, such as a new site, is more likely to feature prominently in a search engine response. But non-governmental sites do require an additional level of scrutiny. For example, in one study, only 55% of health information on news Web sites was medically accurate.8
Who is the author? Does she have financial ties or bias?
Think about who is running the Web site, why they are doing it, and what they are trying to achieve. Is the author a doctor, a health reporter, an advocate, or a drug company? The credentials of any physicians associated with the site should be listed as well as credentials and affiliations of authors, if they are non-physicians. Sites that list physician credentials tend to rate higher in accuracy of content.7
Talk with your patients about the importance of financial ties. The sponsor of the Web site should be listed (drug company, university, or a physician blogging without reimbursement). Bias and money go hand in hand, so be careful in evaluating whether the information provided favors the sponsor. If there are products for sale that are recommended by the medical content, bias is implied and, in my opinion, that site is not informational but commercial.
Bias can also be non-commercial, which is why authors of academic papers are not only supposed to report financial ties but also any real or perceived conflict of interest. This can be hard to discern at times, but the Web site should disclose why it exists. If the message is muddied by advertising and other commercial content, it’s best to just move along.
How current is the content?
We all know that new studies constantly reshape the way we practice (and sometimes guidelines from professional societies seem to change with the wind), and what is new quickly becomes out of date. The good and bad with online information is that it is always there. A permanent record is in many ways a good thing, but content from 2004 may not be applicable in 2011. This is a particular issue with news sites. They may report on a fascinating study in 2007, but if a retraction later appears or a new study refutes the findings, that information may not warrant an article on the Web. A good rule of thumb: Anything older than 2 years requires an additional level of scrutiny.
Be wary when the subject is complementary and alternative medicine
Online content related to complementary and alternative medicine (CAM) should be approached with a higher degree of caution. One study found that 25% of CAM sites presented information that could cause physical harm if acted upon, and almost all CAM sites omitted vital warnings, such as drug interactions, contraindications, and adverse reactions. The quality of CAM sites doesn’t improve even when they meet three or four of the JAMA benchmarks for information quality (see page 40).9 In one study of breast cancer sites, Web pages with CAM content were 15 times more likely to contain inaccurate content, compared with sites without CAM content.7

Instruments and tools for evaluating online content
Three tools are available to help patients and providers judge the quality of written online information:
Discern is a 16-question tool designed to assess the quality of online health information. You will find it at http://www.discern.org.uk/discern_instrument.php. I recommend that you mention this tool to patients, even if you are uncertain whether they will use it. Certainly, any patient wedded to what seems like questionable content from a specific Web site should be encouraged to evaluate the site using the Discern tool. In addition, if you have Web sites other than .gov sites that you like to share with patients, it might be wise to personally review them with Discern so that you can reaffirm that you are directing patients to reliable content rather than a quagmire of misinformation.10
The Health on the Net Foundation (HON) is an independent, seven-person, Geneva-based panel that evaluates accuracy of medical Web sites based on specific guiding principles. It can be accessed at http://www.hon.ch/. Web sites that meet these criteria are awarded seals of approval. Only one problem: Not all sites that carry the seal are compliant with HON, and sites that don’t carry the seal can nevertheless be complete and accurate.11,12
JAMA benchmarks are four disclosures intended to help ensure the quality of a Web site: authorship, references, conflict of interest, and currency of content. Some research suggests that sites that have three or four of the benchmarks are more likely to have accurate content, but there is also evidence to suggest that JAMA benchmarks may not always reliably identify inaccurate information.7,13
Recommend a mini-course
Because these tools may be difficult to use or unreliable at identifying quality content, I recommend that every patient spend time on the National Medical Library Web site learning how to look up information. The other benefit of this site is that it lists top 10 Web sites for content, so it is a great launching point for a multitude of searches. It can be found at http://www.mlanet.org/resources/userguide.html.
If the patient finds the information at this portal too dry, there is a fantastic 16-minute tutorial about evaluating online health information; it’s a service of the National Library of Medicine and the National Institutes of Health. I recommend that every provider do this tutorial. Why? So you can better educate yourself on how to use the Internet and so you can tell your patients how great it is. It’s available at http://www.nlm.nih.gov/medlineplus/webeval/webeval.html.
Take the bull by the horns
Discuss the Internet with every one of your patients. Specifically, ask if she has read any information online and, if she has, how it stacks up with what you have just discussed during her office visit. That’s what I do. Explain that accurate content is critical in health-care decisions, guide your patient to sites that are more likely to be accurate, and teach her how to maximize the Internet to enhance her health care.
In my experience, patients are thrilled to be pointed in the right direction.
We want to hear from you! Tell us what you think.
CASE: The Internet has (at least) two faces
Both Patient A and Patient B are 8 weeks pregnant with their first baby. At an office visit, you discuss influenza vaccination.
Patient A tells you: “I was undecided about the vaccine until I read all these horror stories about the H1N1 vaccine. A Web site, organichealthadviser.com, says vaccines and pregnancies don’t mix safely.1 It says that if the flu vaccine isn’t safe for a baby less than 6 months old, how can it be safe during pregnancy?1 I read story after story of women who got the vaccine and miscarried. Why would I want to be injected with a toxin?”
Patient B explains: “I was undecided about the vaccine until I read the information on the Centers for Disease Control and Prevention (CDC) Web site.2 I didn’t know that pregnant women are more likely to get really sick from the flu. The CDC says the vaccine is safe during pregnancy, will not harm my baby, and not only reduces my chance of getting sick from the flu, but will give my baby protection for 6 months after she is born.2 When and where can I get my shot?”
Sixty-nine percent of Americans (80% of those who have Internet access) turn to the Web for information about their health care, and 23% of people who have a major medical illness or other health condition report that the Internet plays a major role in helping them deal with their health issue.3,4 They might research symptoms, diagnosis, tests, and therapies before a visit to your office; many come armed with questions, sometimes bringing reams of pages downloaded from various sites. Among women receiving ObGyn care, almost 60% have accessed Web-based information before their visit.5 Others take to the Internet after their appointment to confirm or refute what they have heard in the office.
Regardless of what a patient researches or when she does it, the why is because she wants to be an active participant in her medical care. That is a good thing because participatory medicine (shared decision-making) leads to improved outcomes. However, the key to truly informed decision-making is content: A patient can be fully empowered to participate in her health care only if she has information that is accurate, understandable, and current.
Web-based health information: Entirely factual?
Not only do patients research health online, 60% of people believe what they read to be factual and at least as good as the information they receive from you in your office. In fact, there is evidence that only 6% believe the health information they gather online is lacking in quality.5,6
However, studies reveal that the accuracy of medical content on the Web varies greatly from site to site. For example, among women seeking information on the Internet about potential teratogenic agents, 40% found incorrect information, some of which was potentially harmful.7
In addition to the problem of potentially suspect content, more than 50% of patients don’t disclose with you the information that they find online.7 Ever encounter a patient you just couldn’t sway from a diagnosis she believed she had but you knew she didn’t? If your patient tells you where she got the information, you can walk her through the diagnosis and treatment step by step, pointing out where her information might not be accurate (or, sometimes, even medically plausible)—but it’s hard to undo what you don’t know about.
The ideal scenario. Discuss Web-based information as part of your visit, thereby acknowledging that the Internet is a valid place to investigate personal health care. You can also preemptively provide tools for tracking down the most accurate and understandable content. See, for example, the patient handout.
Let’s face it: Physicians have an advantage when it comes to weeding out the wisdom from the woo. To supplement our baseline knowledge, we can easily research facts on PubMed, check our medical societies for guidelines, or, simply, ask a colleague. Our patients don’t have these same resources, but with some guidance from you, their Internet health experience can be greatly enhanced.
Are your searches on the Internet turning up reliable health advice? Watch for these 10 red flags of bad information
- Sensationalized content Is the information on the site presented in an alarmist tone? Is it loaded with scary stories and extreme outcomes? Are the issues presented in terms of black and white, with no shades of gray? If the answer to any of these questions is “Yes,” the author may have an axe to grind or a hidden leaning. Suspect the accuracy of the information you obtain!
- No date This may seem like a minor problem, but the world of health care moves swiftly. Treatments and approaches that are reliable one day can be discredited in the blink of an eye. If the site does not date its content, or indicate when it was last updated, you have no way of knowing how current it is. Move on!
- No author credentials The author or authors of material on the Web site should clearly, and visibly, present their credentials—that is, their education and training, their title, and where they work. If they do not, it is impossible to judge their expertise—in fact, expertise may be lacking.
- Buzz words The use of quasi-scientific buzz words such as “toxins,” “heavy metals,” and “detoxification” should draw your attention. These words have no meaning, so they should lead to you question what else on the site might be fiction.
- Patient testimonials Three people may have improved with a particular drug, but what about those who haven’t? Using unverified personal experiences is a sign of advertising, not good medicine.
- For sale sign If you can’t easily tell the difference between the medical content and products for sale, move along. Even when products don’t appear prominently, chances are that the bottom line of the Web site is profit, not education.
- All benefits and no risks Sites that have a stake in a particular treatment—be it monetary, emotional, or some other involvement—usually provide a lot of information on benefits but not so much about risks. Every treatment has risks.
- No sources When physicians scrutinize an article or study, they make it a point to check the list of sources at the end, to ensure that it contains legitimate information, such as reports from a medical journal or government publication. A Web site that presents detailed medical information without providing links to the references or comparable detail about the sources of that information is highly suspect.
- Conflict of interest Most reputable health sites not only provide information from experts, they list any so-called potential conflicts of interest that those experts may have. For example, if a medication made by XYZ Pharmaceuticals is recommended by Dr. Smith, who is also a consultant to XYZ, you should know. Articles and presentations at scientific meetings require these disclosures for a reason: Financial ties can produce bias.
- The Web site or product is listed on QuackWatch This Web site is dedicated to exposing unproven and scientifically questionable medical claims (http://www.quackwatch.com).
Where can you turn for help?
- An excellent starting place is the National Medical Library Web site at http://www.mlanet.org/resources/userguide.html, which provides resources for obtaining reliable health information.
- The National Library of Medicine and National Institutes of Health also provide an outstanding 16-minute lesson on how you can evaluate online health information. Find it at http://www.nlm.nih.gov/medlineplus/webeval/webeval.html.
- healthfinder.gov is a Web “encyclopedia” offering entries on more than 1,600 health topics.
© Copyright 2011 Quadrant HealthCom, Inc. This “Guide” may be reproduced by clinicians without permission or fee for single-copy distribution to patients. All other uses require the written permission of the publisher.
To obtain a PDF of this Patient Guide, click here .
Four tips for evaluating online content
Consider the source
The very first thing to consider is the domain name—e.g., “.gov,” “.org,” “.edu,” “.com,” or .anythingelse.
.gov sites are owned and maintained by the US government. From a medical standpoint, the .gov designation means that a site contains evidence-based information maintained by medical librarians that is written at a level that most people can read.
It’s a common misperception that the .org designation indicates a not-for-profit site that is therefore “looking out for the public’s best interest.” But anyone can purchase an .org domain. Even if a particular site really is administered by a not-for-profit organization, that status does not ensure that the content is of high quality.
.edu sites are affiliated with academic institutions.
.com and .anythingelse are, like .org, free for anyone to purchase.
Evidence-based medicine tells us that .gov sites are the most accurate for content—anything else is buyer beware (interestingly, .edu sites fared the worst in one study for accuracy).7,8 This doesn’t mean that sites that are not .gov have no value! On the contrary, non-governmental Web sites, blogs, and news articles are often the first place a search starts. That’s because current content, such as a new site, is more likely to feature prominently in a search engine response. But non-governmental sites do require an additional level of scrutiny. For example, in one study, only 55% of health information on news Web sites was medically accurate.8
Who is the author? Does she have financial ties or bias?
Think about who is running the Web site, why they are doing it, and what they are trying to achieve. Is the author a doctor, a health reporter, an advocate, or a drug company? The credentials of any physicians associated with the site should be listed as well as credentials and affiliations of authors, if they are non-physicians. Sites that list physician credentials tend to rate higher in accuracy of content.7
Talk with your patients about the importance of financial ties. The sponsor of the Web site should be listed (drug company, university, or a physician blogging without reimbursement). Bias and money go hand in hand, so be careful in evaluating whether the information provided favors the sponsor. If there are products for sale that are recommended by the medical content, bias is implied and, in my opinion, that site is not informational but commercial.
Bias can also be non-commercial, which is why authors of academic papers are not only supposed to report financial ties but also any real or perceived conflict of interest. This can be hard to discern at times, but the Web site should disclose why it exists. If the message is muddied by advertising and other commercial content, it’s best to just move along.
How current is the content?
We all know that new studies constantly reshape the way we practice (and sometimes guidelines from professional societies seem to change with the wind), and what is new quickly becomes out of date. The good and bad with online information is that it is always there. A permanent record is in many ways a good thing, but content from 2004 may not be applicable in 2011. This is a particular issue with news sites. They may report on a fascinating study in 2007, but if a retraction later appears or a new study refutes the findings, that information may not warrant an article on the Web. A good rule of thumb: Anything older than 2 years requires an additional level of scrutiny.
Be wary when the subject is complementary and alternative medicine
Online content related to complementary and alternative medicine (CAM) should be approached with a higher degree of caution. One study found that 25% of CAM sites presented information that could cause physical harm if acted upon, and almost all CAM sites omitted vital warnings, such as drug interactions, contraindications, and adverse reactions. The quality of CAM sites doesn’t improve even when they meet three or four of the JAMA benchmarks for information quality (see page 40).9 In one study of breast cancer sites, Web pages with CAM content were 15 times more likely to contain inaccurate content, compared with sites without CAM content.7

Instruments and tools for evaluating online content
Three tools are available to help patients and providers judge the quality of written online information:
Discern is a 16-question tool designed to assess the quality of online health information. You will find it at http://www.discern.org.uk/discern_instrument.php. I recommend that you mention this tool to patients, even if you are uncertain whether they will use it. Certainly, any patient wedded to what seems like questionable content from a specific Web site should be encouraged to evaluate the site using the Discern tool. In addition, if you have Web sites other than .gov sites that you like to share with patients, it might be wise to personally review them with Discern so that you can reaffirm that you are directing patients to reliable content rather than a quagmire of misinformation.10
The Health on the Net Foundation (HON) is an independent, seven-person, Geneva-based panel that evaluates accuracy of medical Web sites based on specific guiding principles. It can be accessed at http://www.hon.ch/. Web sites that meet these criteria are awarded seals of approval. Only one problem: Not all sites that carry the seal are compliant with HON, and sites that don’t carry the seal can nevertheless be complete and accurate.11,12
JAMA benchmarks are four disclosures intended to help ensure the quality of a Web site: authorship, references, conflict of interest, and currency of content. Some research suggests that sites that have three or four of the benchmarks are more likely to have accurate content, but there is also evidence to suggest that JAMA benchmarks may not always reliably identify inaccurate information.7,13
Recommend a mini-course
Because these tools may be difficult to use or unreliable at identifying quality content, I recommend that every patient spend time on the National Medical Library Web site learning how to look up information. The other benefit of this site is that it lists top 10 Web sites for content, so it is a great launching point for a multitude of searches. It can be found at http://www.mlanet.org/resources/userguide.html.
If the patient finds the information at this portal too dry, there is a fantastic 16-minute tutorial about evaluating online health information; it’s a service of the National Library of Medicine and the National Institutes of Health. I recommend that every provider do this tutorial. Why? So you can better educate yourself on how to use the Internet and so you can tell your patients how great it is. It’s available at http://www.nlm.nih.gov/medlineplus/webeval/webeval.html.
Take the bull by the horns
Discuss the Internet with every one of your patients. Specifically, ask if she has read any information online and, if she has, how it stacks up with what you have just discussed during her office visit. That’s what I do. Explain that accurate content is critical in health-care decisions, guide your patient to sites that are more likely to be accurate, and teach her how to maximize the Internet to enhance her health care.
In my experience, patients are thrilled to be pointed in the right direction.
We want to hear from you! Tell us what you think.
1. H1N1 vaccine and pregnancy. Organic Health Adviser. http://organichealthadviser.com/archives/h1n1-vaccine-and-pregnancy. Accessed November 12 2011.
2. Pregnant women and influenza. Centers for Disease Control and Prevention. http://www.cdc.gov/flu/protect/vaccine/pregnant.htm. Accessed November 12 2011.
3. Fox S. The social life of health information 2011. Pew Internet and American Life Project. http://pewresearch.org/pubs/1989/health-care-online-social-network-users. Accessed November 12, 2011.
4. Horrigan J, Rainie L. The Internet’s growing role in life’s major moments. Decision-making Communities, Health. Pew Internet and American Life Project. http://www.pewinternet.org/Reports/2006/The-Internets-Growing-Role-in-Lifes-Major-Moments.aspx. Accessed November 12, 2011.
5. Neelapala P, Duvvi SK, Kumar G, Kumar BN. Do gynaecology outpatients use the Internet to seek health information? A questionnaire survey. J Eval Clin Pract. 2008;14(2):300-304.
6. Diaz JA, Griffith RA, Ng JJ, Reinert SE, Friedmann PD, Moulton AW. Patients’ use of the Internet for medical information. J Gen Intern Med. 2001;17(3):180-185.
7. Bernstam EV, Walji MF, Sagaram S, Sagaram D, Johnson CW, Meric-Bernstam F. Commonly cited website quality criteria are not effective at identifying inaccurate online information about breast cancer. Cancer. 2008;112(6):1206-1213.
8. Scullard P, Peacock C, Davies P. Googling children’s health: reliability of medical information on the Internet. Arch Dis Child. 2010;95(8):580-582.
9. Walji M, Sagaram S, Sagaram D, et al. Efficacy of quality criteria to identify potentially harmful information: a cross-sectional survey of complementary and alternative medicine web sites. J Med Internet Res. 2004;6(2):e21.-
10. Charnock D, Shepperd S, Needham G, Gann R. Discern: an instrument for judging the quality of written consumer health information on treatment choices. J Epidemiol Community Health. 1999;53(2):105-111.
11. Hardwick JC, MacKenzie FM. Information contained in miscarriage-related websites and the predictive value of website scoring systems. Eur J Gynecol Reprod Biol. 2003;106(1):60-63.
12. Khazaal Y, Chatton A, Zullino D. HON label and Discern as content quality indicators of health-related websites [published online ahead of print May 2011]. Psychiatr Q. doi: 10.1007/s11126-011-9179-x.
13. Meric F, Bernstam EV, Mirza NQ, et al. Breast cancer on the world wide web: cross sectional survey of quality of information and popularity of websites. BMJ. 2002;324(7337):577-581.
1. H1N1 vaccine and pregnancy. Organic Health Adviser. http://organichealthadviser.com/archives/h1n1-vaccine-and-pregnancy. Accessed November 12 2011.
2. Pregnant women and influenza. Centers for Disease Control and Prevention. http://www.cdc.gov/flu/protect/vaccine/pregnant.htm. Accessed November 12 2011.
3. Fox S. The social life of health information 2011. Pew Internet and American Life Project. http://pewresearch.org/pubs/1989/health-care-online-social-network-users. Accessed November 12, 2011.
4. Horrigan J, Rainie L. The Internet’s growing role in life’s major moments. Decision-making Communities, Health. Pew Internet and American Life Project. http://www.pewinternet.org/Reports/2006/The-Internets-Growing-Role-in-Lifes-Major-Moments.aspx. Accessed November 12, 2011.
5. Neelapala P, Duvvi SK, Kumar G, Kumar BN. Do gynaecology outpatients use the Internet to seek health information? A questionnaire survey. J Eval Clin Pract. 2008;14(2):300-304.
6. Diaz JA, Griffith RA, Ng JJ, Reinert SE, Friedmann PD, Moulton AW. Patients’ use of the Internet for medical information. J Gen Intern Med. 2001;17(3):180-185.
7. Bernstam EV, Walji MF, Sagaram S, Sagaram D, Johnson CW, Meric-Bernstam F. Commonly cited website quality criteria are not effective at identifying inaccurate online information about breast cancer. Cancer. 2008;112(6):1206-1213.
8. Scullard P, Peacock C, Davies P. Googling children’s health: reliability of medical information on the Internet. Arch Dis Child. 2010;95(8):580-582.
9. Walji M, Sagaram S, Sagaram D, et al. Efficacy of quality criteria to identify potentially harmful information: a cross-sectional survey of complementary and alternative medicine web sites. J Med Internet Res. 2004;6(2):e21.-
10. Charnock D, Shepperd S, Needham G, Gann R. Discern: an instrument for judging the quality of written consumer health information on treatment choices. J Epidemiol Community Health. 1999;53(2):105-111.
11. Hardwick JC, MacKenzie FM. Information contained in miscarriage-related websites and the predictive value of website scoring systems. Eur J Gynecol Reprod Biol. 2003;106(1):60-63.
12. Khazaal Y, Chatton A, Zullino D. HON label and Discern as content quality indicators of health-related websites [published online ahead of print May 2011]. Psychiatr Q. doi: 10.1007/s11126-011-9179-x.
13. Meric F, Bernstam EV, Mirza NQ, et al. Breast cancer on the world wide web: cross sectional survey of quality of information and popularity of websites. BMJ. 2002;324(7337):577-581.
To blog or not to blog? What’s the answer for you and your practice?
CASE
Your gyn practice decides to publish an electronic newsletter for patients. You and your office manager spend a lot of time deciding on a format and writing content that you think is relevant to your patients. Everyone in the office agrees: It looks great.
But there’s a problem.
After your newsletter has been “live” for 6 months, fewer than 5% of your patients have signed up to receive it by e-mail (even though you’re sure that a lot more of them are on-line).
You’re perplexed: Why the poor response? The newsletter contains important information that your patients have told you they want—answers to the same questions that you get asked day in, day out.
Why does everyone seem so interested in getting answers to their questions when they’re in the office but not ahead of time and without a co-pay?
CASE: Resolved
The diagnosis: Newsletters are so 1990s.
Offering a Web-savvy patient a newsletter is like presenting her with a VHS tape of a surgical procedure you’re recommending. She will look at you and think, “Huh?”
It’s not that your patients don’t want health information—they are clearly eager for it: 80% of Americans who have Internet access look for health information on-line.1 The quest for health information is the third most popular on-line activity (behind e-mail and using a search engine), and women are more likely to search for health information on-line than men are.2 Nineteen percent of all Internet users search on-line for information about pregnancy and childbirth, and on WebMD (www.webmd.com, the second most popular Internet health site), hysterectomy was the fifth most commonly searched treatment in 2010.1
But getting health information from the Internet today does not mean another e-mail message in the in-box, where it sits waiting to be read or, more likely, deleted without having been opened. For most patients, looking for health information on-line entails 1) general searches (via Google, for example) for symptoms, specific diagnoses, or therapies or 2) searches on specific health-related Web sites (the top two for traffic in November 2010 were the National Institutes of Health and WebMD).1,3
More and more patients, however, are craving a dialogue about their health; 40% of on-line health-related activities involve interactive, user-generated content of social media, the most popular sources being Facebook, Twitter, and the Web-site tool known as blogs that I discuss in this article—with the aim of helping you determine whether placing your professional voice on the Web in a blog is workable, valuable, and respectable.1,3,4

Blog (noun, singular); blogs (plural)
What is it? A shortened form of “web log.” Has a different functional meaning for different people: A journal. A place to rant. A collaborative archive. A source of breaking news.
Whatever shape a blog takes, at its core it is an ongoing chronicle of information plus opinion. For a medical blog, that description typically refers to the perspective of the consumer/patient or the health-care professional who writes the “posts,” or entries.
The Web has thousands upon thousands of medical blogs. Some support an academic institution or a government agency (even the Centers for Disease Control and Prevention has a blog); many describe the experiences of an individual with one or another aspect of health care (from a patient’s or provider’s perspective). With one third of Americans reading blogs, they are an excellent way to disseminate information.1,3,4
Here are what I consider several good reasons to start a medical blog—reasons that, in part, motivated me to begin blogging (see “Why I blog,”):
- A blog is an ideal platform to deliver content to your patients and like-minded medical professionals. A blog allows your patients (and everyone else) to see information that you think is valuable and to hear your opinion on important health topics. Patients really like to know what their physician’s opinion is—how many times have you been asked, in the office, “What do you think I should do, doctor?”
- Blogging is good advertising for your practice. Your blog will appear in Web-search results, which may lead new patients to your doorstep. Reporters and other media workers troll the Web, fact-checking and looking for “angles” for news stories; you may be called to give your opinion about something you blogged about. Remember: Being mentioned in the local newspaper is free advertising (yes, people still read newspapers, though often on-line); ask the reporter to include a link to your blog in any story in which you’re quoted.
- Blogging helps you learn from your readers. Given the interactive nature of a blog (comments are encouraged), you might find feedback that is interesting at the least, possibly educational. Many people take commenting on blogs very seriously, and often post valuable links to other content.
- Contributing credible content drowns out garbage medical information that circulates widely on-line. The Internet is a powerhouse repository of medical knowledge, but it’s only as good as the content provided to it; in fact, 65% of Web pages contain inaccurate medical information.6 Regrettably, most people do not verify the medical information they find on-line.
- Blogging helps keep you relevant. Medicine is still trying to figure out how to best integrate itself with the user-centered operation and experience of Web 2.0. If you aren’t engaged here on some level, you risk being left behind.

I started blogging about prematurity 2 years ago, at my Web site, www.preemieprimer.com. I saw this as a way to support my book, The Preemie Primer, and to add content that I just didn’t have enough space for in the print edition.
Recently, I started a more general medical blog geared to women’s health (see an excerpt of a post below). I set up this blog myself, using WordPress (see the description in the main text), in under an hour (I’m of sub-average intelligence when it comes to computers, but I can follow directions). I paid a Web-savvy person to change the domain name to www.drjengunter.com.
Some days, my posts appeal to 20,000 people
Other days, I captivate, oh, a dozen. For me, the most important reasons for blogging are to use my voice (I really do write as I speak) and to add good content to the Web.
Like many of you, I was sick and tired of seeing page after page of what I can only describe as drivel that my unsuspecting patients were spending hours downloading and reading. I decided to stop just bemoaning this reality and to do something about it because—like most of my patients—I also research my own children’s medical conditions on the Web.
Let me tell you: If my son’s pediatric cardiologist had a blog, I’d be reading it every day.
—Jennifer Gunter, MD
Excerpt: “Are condoms with spermicide a good idea?”
“You are standing in the grocery store staring at the overwhelming selection of condoms. The last time you had sex, there was an unfortunate incident involving breakage and you are eager to avoid the pregnancy panic and STD scare that ensued. You look at the condoms with spermicide thinking that extra-protection sounds like a good idea right now.
After all, condoms without spermicide reduce your chance of getting gonorrhea and chlamydia by almost 100%, reduce your risk of catching HIV by 87%, reduce your chance of getting HPV (the virus that causes cervical cancer and genital warts) by 70%, and reduce your chance of getting herpes by 30%. Condoms with spermicide must be even better, right?
Wrong. Condoms with spermicide are no more effective than condoms with regular lube at preventing STDs. Condoms with spermicide are also more expensive and have a shorter shelf-life.
And here’s the big kicker. Spermicide damages the ecosystem and delicate skin of the vagina (it’s a secret garden in there, boys). Because of this, condoms with spermicide actually increase a woman’s risk of getting a bladder infection and can damage local defense mechanisms enough that the risk of catching an STD actually increases!
Source: Gunter J. Are condoms with spermicide a good idea? http://www.drjengunter.com. Accessed July 21, 2011.
The mechanics of starting a blog take little time and minimal technical knowledge. If you, or your practice, already have a Web site and a webmaster, he (she) can easily add a blog to the site for you. But you can also get a blog up and running yourself quite easily—at minimal or no cost to you (again, see “Why I blog”).
Two popular blog publishing platforms are WordPress (start at: https://en.wordpress.com/signup/) and Blogger (a service of Google; start at: https://www.blogger.com/signup.g). Both are free, although WordPress also sells a variety of upgrades that allow you to customize your site (if you have time and patience, you can navigate most of the upgrades on your own). Unless your blog needs a very specific look, however, you probably won’t need any of these options.
WordPress exacts an annual fee to keep third-party advertisements off your blog. Blogger does not charge to block advertising.
WordPress and Blogger both offer a variety of different templates so that you can trick out your blog to suit your style. You can delete the comments left by visitors with either platform. (Note: In 2 years of blogging, I’ve never had anyone post a comment that I thought needed deleting. But, you never know….)
So you’re not a writer. That’s OK—you aren’t chasing a Pulitzer.
People don’t linger on a blog. You want to make one or two points, not offer a dissertation. There is so much information on the Web that the only way to digest it is in small bites (think appetizers, not a four-course meal). Here are some pearls to consider for writing a blog successfully.
- Take the content that you might publish in a newsletter and simply cut it up into smaller pieces. Instead of a full page about the human papillomavirus (HPV) vaccine, divide what you’ve written into three or four discrete posts: for example, one post on the incidence of HPV; one on transmission; another on the vaccine schedule; and one on other means to prevent HPV (you can never have too many posts on the importance of using a condom, considering that almost 40% of sexually active high-school students did not use one the last time they had sexual intercourse).7
- Do some research. Read popular medical (and non-medical) blogs and decide what style suits you and your needs. A useful place to start is Dr. Kevin Pho’s blog at www.KevinMD.com" target="_blank">www.KevinMD.com. This is the most popular medical blog; in addition to his own writing, Dr. Pho posts content from an array of other physicians (including me), so you can find a number of different writing styles and viewpoints on a single blog.
- Post links to information from other blogs and traditional news sources (CNN, MSNBC, and so on) and add your brief comment to their reporting. This is an easy way to start a blog—just provide attribution and be careful not to infringe on your sources’ copyright.
- Answer the questions that you’re asked day in and day out in the office.
- Post on topics that are relevant to the moment. In autumn, for example, add information about the influenza vaccine in pregnancy, a link to the CDC Web page on influenza, and the date on which your office will begin offering shots.
- Add links to reputable sites; at the least, mention where you obtained specific information. This adds credibility, and people interested in learning more will appreciate knowing which sites are your sources.
- State that what you posted isn’t intended as individual medical advice. Given the medicolegal climate, I highly advise you to say this somewhere on your blog.
- End every post with a question. Doing so encourages comments.
- Stay true to your voice, whatever else you do. Insincerity is obvious. Painfully so.
Within your practice. Tell your patients that you have a blog. Consider listing the url of the blog on your business card.
And beyond. If you don’t want to promote your blog outside the practice, that’s fine. But if you like the idea of reaching more people, promote your posts on Twitter and Facebook and on information-sharing sites, such as reddit (http://www.reddit.com" target="_blank">http://www.reddit.com) and Digg (http://digg.com" target="_blank">http://digg.com). Note that Facebook and reddit are currently more popular among women; these two tools may be better suited to your needs if you’re looking to get the most promotion for a blog that’s geared to women’s health.
Promotion takes some work but, if what you write has value, you’ll be surprised at the viral life that a blog post can take on. Example: Recently, on my blog, I wrote a post that I titled “Oprah signs off and doctors everywhere rejoice.” The post went viral thanks to multiple re-postings on Twitter and Facebook and to views from reddit. In 3 days, the post was viewed more than 30,000 times.
This kind of traffic increases a blog’s ranking with search engines; it helped my blog stay at the top of the first “Results” page on various search engines for a while.
A blog can be a great tool for you and your practice
Blogging doesn’t have to take hours a day (although the public is fickle, and people will drift away if you don’t post at least three or four times a week); with only a little time and effort, you can have the satisfaction of self-expression. And, if you’re committed to good content, you will raise the quality of health information on the Web.
We want to hear from you! Tell us what you think.
1. Fox S. Health Topics. Pew Internet & American Life Project. http://pewinternet.org/Reports/2011/HealthTopics.aspx. Published February 1 2011. Accessed May 20, 2011.
2. Pew Research Center. Pew Internet & American Life Project Tracking Surveys: Trend data. http://www.pewinternet.org/Static-Pages/Trend-Data/Online-Activites-Total.aspx. Updated May 2011. Accessed June 1 2011.
3. McDaid D, Park A-la. Online health: Untangling the web. BUPA Health Pulse 2010. http://www.bupa.com/healthpulse. Published January 4 2011. Accessed June 1, 2010.
4. Pew Research Center. Generational differences in online activities. Pew Internet & American Life Project. http://www.pewinternet.org/Infographics/Generational-differences-in-online-activities.aspx. Published January 28 2009. Accessed June 1, 2011.
5. Gunter J. For better or maybe, worse, your patients are judging your care online. OBG Manage. 2011;23(3):47-51.
6. Thompson LA, Dawson K, Ferdig R, et al. The intersection of online social networking with medical professionalism. J Gen Intern Med. 2008;23(7):954-957.
7. Eaton DK, Kann L, Kinchen S, et al. Centers for Disease Control and Prevention. Youth risk behavior surveillance—United States 2009. MMWR Surveill Summ. 2010;59(5):1-142.
CASE
Your gyn practice decides to publish an electronic newsletter for patients. You and your office manager spend a lot of time deciding on a format and writing content that you think is relevant to your patients. Everyone in the office agrees: It looks great.
But there’s a problem.
After your newsletter has been “live” for 6 months, fewer than 5% of your patients have signed up to receive it by e-mail (even though you’re sure that a lot more of them are on-line).
You’re perplexed: Why the poor response? The newsletter contains important information that your patients have told you they want—answers to the same questions that you get asked day in, day out.
Why does everyone seem so interested in getting answers to their questions when they’re in the office but not ahead of time and without a co-pay?
CASE: Resolved
The diagnosis: Newsletters are so 1990s.
Offering a Web-savvy patient a newsletter is like presenting her with a VHS tape of a surgical procedure you’re recommending. She will look at you and think, “Huh?”
It’s not that your patients don’t want health information—they are clearly eager for it: 80% of Americans who have Internet access look for health information on-line.1 The quest for health information is the third most popular on-line activity (behind e-mail and using a search engine), and women are more likely to search for health information on-line than men are.2 Nineteen percent of all Internet users search on-line for information about pregnancy and childbirth, and on WebMD (www.webmd.com, the second most popular Internet health site), hysterectomy was the fifth most commonly searched treatment in 2010.1
But getting health information from the Internet today does not mean another e-mail message in the in-box, where it sits waiting to be read or, more likely, deleted without having been opened. For most patients, looking for health information on-line entails 1) general searches (via Google, for example) for symptoms, specific diagnoses, or therapies or 2) searches on specific health-related Web sites (the top two for traffic in November 2010 were the National Institutes of Health and WebMD).1,3
More and more patients, however, are craving a dialogue about their health; 40% of on-line health-related activities involve interactive, user-generated content of social media, the most popular sources being Facebook, Twitter, and the Web-site tool known as blogs that I discuss in this article—with the aim of helping you determine whether placing your professional voice on the Web in a blog is workable, valuable, and respectable.1,3,4

Blog (noun, singular); blogs (plural)
What is it? A shortened form of “web log.” Has a different functional meaning for different people: A journal. A place to rant. A collaborative archive. A source of breaking news.
Whatever shape a blog takes, at its core it is an ongoing chronicle of information plus opinion. For a medical blog, that description typically refers to the perspective of the consumer/patient or the health-care professional who writes the “posts,” or entries.
The Web has thousands upon thousands of medical blogs. Some support an academic institution or a government agency (even the Centers for Disease Control and Prevention has a blog); many describe the experiences of an individual with one or another aspect of health care (from a patient’s or provider’s perspective). With one third of Americans reading blogs, they are an excellent way to disseminate information.1,3,4
Here are what I consider several good reasons to start a medical blog—reasons that, in part, motivated me to begin blogging (see “Why I blog,”):
- A blog is an ideal platform to deliver content to your patients and like-minded medical professionals. A blog allows your patients (and everyone else) to see information that you think is valuable and to hear your opinion on important health topics. Patients really like to know what their physician’s opinion is—how many times have you been asked, in the office, “What do you think I should do, doctor?”
- Blogging is good advertising for your practice. Your blog will appear in Web-search results, which may lead new patients to your doorstep. Reporters and other media workers troll the Web, fact-checking and looking for “angles” for news stories; you may be called to give your opinion about something you blogged about. Remember: Being mentioned in the local newspaper is free advertising (yes, people still read newspapers, though often on-line); ask the reporter to include a link to your blog in any story in which you’re quoted.
- Blogging helps you learn from your readers. Given the interactive nature of a blog (comments are encouraged), you might find feedback that is interesting at the least, possibly educational. Many people take commenting on blogs very seriously, and often post valuable links to other content.
- Contributing credible content drowns out garbage medical information that circulates widely on-line. The Internet is a powerhouse repository of medical knowledge, but it’s only as good as the content provided to it; in fact, 65% of Web pages contain inaccurate medical information.6 Regrettably, most people do not verify the medical information they find on-line.
- Blogging helps keep you relevant. Medicine is still trying to figure out how to best integrate itself with the user-centered operation and experience of Web 2.0. If you aren’t engaged here on some level, you risk being left behind.

I started blogging about prematurity 2 years ago, at my Web site, www.preemieprimer.com. I saw this as a way to support my book, The Preemie Primer, and to add content that I just didn’t have enough space for in the print edition.
Recently, I started a more general medical blog geared to women’s health (see an excerpt of a post below). I set up this blog myself, using WordPress (see the description in the main text), in under an hour (I’m of sub-average intelligence when it comes to computers, but I can follow directions). I paid a Web-savvy person to change the domain name to www.drjengunter.com.
Some days, my posts appeal to 20,000 people
Other days, I captivate, oh, a dozen. For me, the most important reasons for blogging are to use my voice (I really do write as I speak) and to add good content to the Web.
Like many of you, I was sick and tired of seeing page after page of what I can only describe as drivel that my unsuspecting patients were spending hours downloading and reading. I decided to stop just bemoaning this reality and to do something about it because—like most of my patients—I also research my own children’s medical conditions on the Web.
Let me tell you: If my son’s pediatric cardiologist had a blog, I’d be reading it every day.
—Jennifer Gunter, MD
Excerpt: “Are condoms with spermicide a good idea?”
“You are standing in the grocery store staring at the overwhelming selection of condoms. The last time you had sex, there was an unfortunate incident involving breakage and you are eager to avoid the pregnancy panic and STD scare that ensued. You look at the condoms with spermicide thinking that extra-protection sounds like a good idea right now.
After all, condoms without spermicide reduce your chance of getting gonorrhea and chlamydia by almost 100%, reduce your risk of catching HIV by 87%, reduce your chance of getting HPV (the virus that causes cervical cancer and genital warts) by 70%, and reduce your chance of getting herpes by 30%. Condoms with spermicide must be even better, right?
Wrong. Condoms with spermicide are no more effective than condoms with regular lube at preventing STDs. Condoms with spermicide are also more expensive and have a shorter shelf-life.
And here’s the big kicker. Spermicide damages the ecosystem and delicate skin of the vagina (it’s a secret garden in there, boys). Because of this, condoms with spermicide actually increase a woman’s risk of getting a bladder infection and can damage local defense mechanisms enough that the risk of catching an STD actually increases!
Source: Gunter J. Are condoms with spermicide a good idea? http://www.drjengunter.com. Accessed July 21, 2011.
The mechanics of starting a blog take little time and minimal technical knowledge. If you, or your practice, already have a Web site and a webmaster, he (she) can easily add a blog to the site for you. But you can also get a blog up and running yourself quite easily—at minimal or no cost to you (again, see “Why I blog”).
Two popular blog publishing platforms are WordPress (start at: https://en.wordpress.com/signup/) and Blogger (a service of Google; start at: https://www.blogger.com/signup.g). Both are free, although WordPress also sells a variety of upgrades that allow you to customize your site (if you have time and patience, you can navigate most of the upgrades on your own). Unless your blog needs a very specific look, however, you probably won’t need any of these options.
WordPress exacts an annual fee to keep third-party advertisements off your blog. Blogger does not charge to block advertising.
WordPress and Blogger both offer a variety of different templates so that you can trick out your blog to suit your style. You can delete the comments left by visitors with either platform. (Note: In 2 years of blogging, I’ve never had anyone post a comment that I thought needed deleting. But, you never know….)
So you’re not a writer. That’s OK—you aren’t chasing a Pulitzer.
People don’t linger on a blog. You want to make one or two points, not offer a dissertation. There is so much information on the Web that the only way to digest it is in small bites (think appetizers, not a four-course meal). Here are some pearls to consider for writing a blog successfully.
- Take the content that you might publish in a newsletter and simply cut it up into smaller pieces. Instead of a full page about the human papillomavirus (HPV) vaccine, divide what you’ve written into three or four discrete posts: for example, one post on the incidence of HPV; one on transmission; another on the vaccine schedule; and one on other means to prevent HPV (you can never have too many posts on the importance of using a condom, considering that almost 40% of sexually active high-school students did not use one the last time they had sexual intercourse).7
- Do some research. Read popular medical (and non-medical) blogs and decide what style suits you and your needs. A useful place to start is Dr. Kevin Pho’s blog at www.KevinMD.com" target="_blank">www.KevinMD.com. This is the most popular medical blog; in addition to his own writing, Dr. Pho posts content from an array of other physicians (including me), so you can find a number of different writing styles and viewpoints on a single blog.
- Post links to information from other blogs and traditional news sources (CNN, MSNBC, and so on) and add your brief comment to their reporting. This is an easy way to start a blog—just provide attribution and be careful not to infringe on your sources’ copyright.
- Answer the questions that you’re asked day in and day out in the office.
- Post on topics that are relevant to the moment. In autumn, for example, add information about the influenza vaccine in pregnancy, a link to the CDC Web page on influenza, and the date on which your office will begin offering shots.
- Add links to reputable sites; at the least, mention where you obtained specific information. This adds credibility, and people interested in learning more will appreciate knowing which sites are your sources.
- State that what you posted isn’t intended as individual medical advice. Given the medicolegal climate, I highly advise you to say this somewhere on your blog.
- End every post with a question. Doing so encourages comments.
- Stay true to your voice, whatever else you do. Insincerity is obvious. Painfully so.
Within your practice. Tell your patients that you have a blog. Consider listing the url of the blog on your business card.
And beyond. If you don’t want to promote your blog outside the practice, that’s fine. But if you like the idea of reaching more people, promote your posts on Twitter and Facebook and on information-sharing sites, such as reddit (http://www.reddit.com" target="_blank">http://www.reddit.com) and Digg (http://digg.com" target="_blank">http://digg.com). Note that Facebook and reddit are currently more popular among women; these two tools may be better suited to your needs if you’re looking to get the most promotion for a blog that’s geared to women’s health.
Promotion takes some work but, if what you write has value, you’ll be surprised at the viral life that a blog post can take on. Example: Recently, on my blog, I wrote a post that I titled “Oprah signs off and doctors everywhere rejoice.” The post went viral thanks to multiple re-postings on Twitter and Facebook and to views from reddit. In 3 days, the post was viewed more than 30,000 times.
This kind of traffic increases a blog’s ranking with search engines; it helped my blog stay at the top of the first “Results” page on various search engines for a while.
A blog can be a great tool for you and your practice
Blogging doesn’t have to take hours a day (although the public is fickle, and people will drift away if you don’t post at least three or four times a week); with only a little time and effort, you can have the satisfaction of self-expression. And, if you’re committed to good content, you will raise the quality of health information on the Web.
We want to hear from you! Tell us what you think.
CASE
Your gyn practice decides to publish an electronic newsletter for patients. You and your office manager spend a lot of time deciding on a format and writing content that you think is relevant to your patients. Everyone in the office agrees: It looks great.
But there’s a problem.
After your newsletter has been “live” for 6 months, fewer than 5% of your patients have signed up to receive it by e-mail (even though you’re sure that a lot more of them are on-line).
You’re perplexed: Why the poor response? The newsletter contains important information that your patients have told you they want—answers to the same questions that you get asked day in, day out.
Why does everyone seem so interested in getting answers to their questions when they’re in the office but not ahead of time and without a co-pay?
CASE: Resolved
The diagnosis: Newsletters are so 1990s.
Offering a Web-savvy patient a newsletter is like presenting her with a VHS tape of a surgical procedure you’re recommending. She will look at you and think, “Huh?”
It’s not that your patients don’t want health information—they are clearly eager for it: 80% of Americans who have Internet access look for health information on-line.1 The quest for health information is the third most popular on-line activity (behind e-mail and using a search engine), and women are more likely to search for health information on-line than men are.2 Nineteen percent of all Internet users search on-line for information about pregnancy and childbirth, and on WebMD (www.webmd.com, the second most popular Internet health site), hysterectomy was the fifth most commonly searched treatment in 2010.1
But getting health information from the Internet today does not mean another e-mail message in the in-box, where it sits waiting to be read or, more likely, deleted without having been opened. For most patients, looking for health information on-line entails 1) general searches (via Google, for example) for symptoms, specific diagnoses, or therapies or 2) searches on specific health-related Web sites (the top two for traffic in November 2010 were the National Institutes of Health and WebMD).1,3
More and more patients, however, are craving a dialogue about their health; 40% of on-line health-related activities involve interactive, user-generated content of social media, the most popular sources being Facebook, Twitter, and the Web-site tool known as blogs that I discuss in this article—with the aim of helping you determine whether placing your professional voice on the Web in a blog is workable, valuable, and respectable.1,3,4

Blog (noun, singular); blogs (plural)
What is it? A shortened form of “web log.” Has a different functional meaning for different people: A journal. A place to rant. A collaborative archive. A source of breaking news.
Whatever shape a blog takes, at its core it is an ongoing chronicle of information plus opinion. For a medical blog, that description typically refers to the perspective of the consumer/patient or the health-care professional who writes the “posts,” or entries.
The Web has thousands upon thousands of medical blogs. Some support an academic institution or a government agency (even the Centers for Disease Control and Prevention has a blog); many describe the experiences of an individual with one or another aspect of health care (from a patient’s or provider’s perspective). With one third of Americans reading blogs, they are an excellent way to disseminate information.1,3,4
Here are what I consider several good reasons to start a medical blog—reasons that, in part, motivated me to begin blogging (see “Why I blog,”):
- A blog is an ideal platform to deliver content to your patients and like-minded medical professionals. A blog allows your patients (and everyone else) to see information that you think is valuable and to hear your opinion on important health topics. Patients really like to know what their physician’s opinion is—how many times have you been asked, in the office, “What do you think I should do, doctor?”
- Blogging is good advertising for your practice. Your blog will appear in Web-search results, which may lead new patients to your doorstep. Reporters and other media workers troll the Web, fact-checking and looking for “angles” for news stories; you may be called to give your opinion about something you blogged about. Remember: Being mentioned in the local newspaper is free advertising (yes, people still read newspapers, though often on-line); ask the reporter to include a link to your blog in any story in which you’re quoted.
- Blogging helps you learn from your readers. Given the interactive nature of a blog (comments are encouraged), you might find feedback that is interesting at the least, possibly educational. Many people take commenting on blogs very seriously, and often post valuable links to other content.
- Contributing credible content drowns out garbage medical information that circulates widely on-line. The Internet is a powerhouse repository of medical knowledge, but it’s only as good as the content provided to it; in fact, 65% of Web pages contain inaccurate medical information.6 Regrettably, most people do not verify the medical information they find on-line.
- Blogging helps keep you relevant. Medicine is still trying to figure out how to best integrate itself with the user-centered operation and experience of Web 2.0. If you aren’t engaged here on some level, you risk being left behind.

I started blogging about prematurity 2 years ago, at my Web site, www.preemieprimer.com. I saw this as a way to support my book, The Preemie Primer, and to add content that I just didn’t have enough space for in the print edition.
Recently, I started a more general medical blog geared to women’s health (see an excerpt of a post below). I set up this blog myself, using WordPress (see the description in the main text), in under an hour (I’m of sub-average intelligence when it comes to computers, but I can follow directions). I paid a Web-savvy person to change the domain name to www.drjengunter.com.
Some days, my posts appeal to 20,000 people
Other days, I captivate, oh, a dozen. For me, the most important reasons for blogging are to use my voice (I really do write as I speak) and to add good content to the Web.
Like many of you, I was sick and tired of seeing page after page of what I can only describe as drivel that my unsuspecting patients were spending hours downloading and reading. I decided to stop just bemoaning this reality and to do something about it because—like most of my patients—I also research my own children’s medical conditions on the Web.
Let me tell you: If my son’s pediatric cardiologist had a blog, I’d be reading it every day.
—Jennifer Gunter, MD
Excerpt: “Are condoms with spermicide a good idea?”
“You are standing in the grocery store staring at the overwhelming selection of condoms. The last time you had sex, there was an unfortunate incident involving breakage and you are eager to avoid the pregnancy panic and STD scare that ensued. You look at the condoms with spermicide thinking that extra-protection sounds like a good idea right now.
After all, condoms without spermicide reduce your chance of getting gonorrhea and chlamydia by almost 100%, reduce your risk of catching HIV by 87%, reduce your chance of getting HPV (the virus that causes cervical cancer and genital warts) by 70%, and reduce your chance of getting herpes by 30%. Condoms with spermicide must be even better, right?
Wrong. Condoms with spermicide are no more effective than condoms with regular lube at preventing STDs. Condoms with spermicide are also more expensive and have a shorter shelf-life.
And here’s the big kicker. Spermicide damages the ecosystem and delicate skin of the vagina (it’s a secret garden in there, boys). Because of this, condoms with spermicide actually increase a woman’s risk of getting a bladder infection and can damage local defense mechanisms enough that the risk of catching an STD actually increases!
Source: Gunter J. Are condoms with spermicide a good idea? http://www.drjengunter.com. Accessed July 21, 2011.
The mechanics of starting a blog take little time and minimal technical knowledge. If you, or your practice, already have a Web site and a webmaster, he (she) can easily add a blog to the site for you. But you can also get a blog up and running yourself quite easily—at minimal or no cost to you (again, see “Why I blog”).
Two popular blog publishing platforms are WordPress (start at: https://en.wordpress.com/signup/) and Blogger (a service of Google; start at: https://www.blogger.com/signup.g). Both are free, although WordPress also sells a variety of upgrades that allow you to customize your site (if you have time and patience, you can navigate most of the upgrades on your own). Unless your blog needs a very specific look, however, you probably won’t need any of these options.
WordPress exacts an annual fee to keep third-party advertisements off your blog. Blogger does not charge to block advertising.
WordPress and Blogger both offer a variety of different templates so that you can trick out your blog to suit your style. You can delete the comments left by visitors with either platform. (Note: In 2 years of blogging, I’ve never had anyone post a comment that I thought needed deleting. But, you never know….)
So you’re not a writer. That’s OK—you aren’t chasing a Pulitzer.
People don’t linger on a blog. You want to make one or two points, not offer a dissertation. There is so much information on the Web that the only way to digest it is in small bites (think appetizers, not a four-course meal). Here are some pearls to consider for writing a blog successfully.
- Take the content that you might publish in a newsletter and simply cut it up into smaller pieces. Instead of a full page about the human papillomavirus (HPV) vaccine, divide what you’ve written into three or four discrete posts: for example, one post on the incidence of HPV; one on transmission; another on the vaccine schedule; and one on other means to prevent HPV (you can never have too many posts on the importance of using a condom, considering that almost 40% of sexually active high-school students did not use one the last time they had sexual intercourse).7
- Do some research. Read popular medical (and non-medical) blogs and decide what style suits you and your needs. A useful place to start is Dr. Kevin Pho’s blog at www.KevinMD.com" target="_blank">www.KevinMD.com. This is the most popular medical blog; in addition to his own writing, Dr. Pho posts content from an array of other physicians (including me), so you can find a number of different writing styles and viewpoints on a single blog.
- Post links to information from other blogs and traditional news sources (CNN, MSNBC, and so on) and add your brief comment to their reporting. This is an easy way to start a blog—just provide attribution and be careful not to infringe on your sources’ copyright.
- Answer the questions that you’re asked day in and day out in the office.
- Post on topics that are relevant to the moment. In autumn, for example, add information about the influenza vaccine in pregnancy, a link to the CDC Web page on influenza, and the date on which your office will begin offering shots.
- Add links to reputable sites; at the least, mention where you obtained specific information. This adds credibility, and people interested in learning more will appreciate knowing which sites are your sources.
- State that what you posted isn’t intended as individual medical advice. Given the medicolegal climate, I highly advise you to say this somewhere on your blog.
- End every post with a question. Doing so encourages comments.
- Stay true to your voice, whatever else you do. Insincerity is obvious. Painfully so.
Within your practice. Tell your patients that you have a blog. Consider listing the url of the blog on your business card.
And beyond. If you don’t want to promote your blog outside the practice, that’s fine. But if you like the idea of reaching more people, promote your posts on Twitter and Facebook and on information-sharing sites, such as reddit (http://www.reddit.com" target="_blank">http://www.reddit.com) and Digg (http://digg.com" target="_blank">http://digg.com). Note that Facebook and reddit are currently more popular among women; these two tools may be better suited to your needs if you’re looking to get the most promotion for a blog that’s geared to women’s health.
Promotion takes some work but, if what you write has value, you’ll be surprised at the viral life that a blog post can take on. Example: Recently, on my blog, I wrote a post that I titled “Oprah signs off and doctors everywhere rejoice.” The post went viral thanks to multiple re-postings on Twitter and Facebook and to views from reddit. In 3 days, the post was viewed more than 30,000 times.
This kind of traffic increases a blog’s ranking with search engines; it helped my blog stay at the top of the first “Results” page on various search engines for a while.
A blog can be a great tool for you and your practice
Blogging doesn’t have to take hours a day (although the public is fickle, and people will drift away if you don’t post at least three or four times a week); with only a little time and effort, you can have the satisfaction of self-expression. And, if you’re committed to good content, you will raise the quality of health information on the Web.
We want to hear from you! Tell us what you think.
1. Fox S. Health Topics. Pew Internet & American Life Project. http://pewinternet.org/Reports/2011/HealthTopics.aspx. Published February 1 2011. Accessed May 20, 2011.
2. Pew Research Center. Pew Internet & American Life Project Tracking Surveys: Trend data. http://www.pewinternet.org/Static-Pages/Trend-Data/Online-Activites-Total.aspx. Updated May 2011. Accessed June 1 2011.
3. McDaid D, Park A-la. Online health: Untangling the web. BUPA Health Pulse 2010. http://www.bupa.com/healthpulse. Published January 4 2011. Accessed June 1, 2010.
4. Pew Research Center. Generational differences in online activities. Pew Internet & American Life Project. http://www.pewinternet.org/Infographics/Generational-differences-in-online-activities.aspx. Published January 28 2009. Accessed June 1, 2011.
5. Gunter J. For better or maybe, worse, your patients are judging your care online. OBG Manage. 2011;23(3):47-51.
6. Thompson LA, Dawson K, Ferdig R, et al. The intersection of online social networking with medical professionalism. J Gen Intern Med. 2008;23(7):954-957.
7. Eaton DK, Kann L, Kinchen S, et al. Centers for Disease Control and Prevention. Youth risk behavior surveillance—United States 2009. MMWR Surveill Summ. 2010;59(5):1-142.
1. Fox S. Health Topics. Pew Internet & American Life Project. http://pewinternet.org/Reports/2011/HealthTopics.aspx. Published February 1 2011. Accessed May 20, 2011.
2. Pew Research Center. Pew Internet & American Life Project Tracking Surveys: Trend data. http://www.pewinternet.org/Static-Pages/Trend-Data/Online-Activites-Total.aspx. Updated May 2011. Accessed June 1 2011.
3. McDaid D, Park A-la. Online health: Untangling the web. BUPA Health Pulse 2010. http://www.bupa.com/healthpulse. Published January 4 2011. Accessed June 1, 2010.
4. Pew Research Center. Generational differences in online activities. Pew Internet & American Life Project. http://www.pewinternet.org/Infographics/Generational-differences-in-online-activities.aspx. Published January 28 2009. Accessed June 1, 2011.
5. Gunter J. For better or maybe, worse, your patients are judging your care online. OBG Manage. 2011;23(3):47-51.
6. Thompson LA, Dawson K, Ferdig R, et al. The intersection of online social networking with medical professionalism. J Gen Intern Med. 2008;23(7):954-957.
7. Eaton DK, Kann L, Kinchen S, et al. Centers for Disease Control and Prevention. Youth risk behavior surveillance—United States 2009. MMWR Surveill Summ. 2010;59(5):1-142.
For better or, maybe, worse, patients are judging your care online
- Twitter 101 for ObGyns: Pearls, pitfalls, and potential
(September 2011)
CASE: Unfairly labeled and now unnerved
Dr. Y, your colleague, calls you; she’s distraught. She performed a Google search of her name and found what she describes as a hateful review on a physician-rating Web site from someone claiming to be her patient. The reviewer declared that Dr. Y. was “rude” and interested only in “pushing one drug.”
“She must be a shill for a drug company….”
You’ve referred many patients to Dr. Y, and you’ve always heard wonderful things about her care. You know that she has never accepted pharma money for lectures or research.
“What should I do?” Dr. Y pleads with you.
We physicians probably don’t think twice about looking up reviews and ratings of hotels and restaurants. But many of us balk at the thought of our professional services being reviewed in such a manner. We’re aware that patients discuss their care, of course, but the Internet— well, that provides a megaphone of global reach for what was once mere water-cooler chat.
And reading angry words in print hurts more than hearing them secondhand.
With the Internet hosting more than 30 sites that rate health-care providers and hospitals, most of us can expect to be reviewed at some point. Only about 15% of people report consulting online physician reviews, however, and fewer than 5% have posted an online review themselves.1,2
What do you need to know about these sites and their potential to have an impact on your practice? Here are some important observations and pearls from the literature and from my experience at the receiving end of ratings.
Types of physician online rating
The first step in navigating the morass of Internet review and rating sites is to understand the types of sites that you’ll encounter.
Angie’s List. This site rates all kinds of services, including physicians. Membership requires registration and a fee. A member can post a review of a given physician every 6 months. Although the names of reviewers are not posted, they are available to the physicians being reviewed—if they ask.
Free Web sites that require registration of some kind. These are general review sites, such as www.yelp.com or specific sites for physicians, such as www.DoctorScorecard.com, which states that a reviewer is allowed to rate a given physician only once.
Free Web sites that don’t require registration. One simply finds the physician’s name and either clicks on the number of stars or writes a review, or both. Two examples: www.vitals.com and www.drscore.com. These sites claim to limit the number of reviews: vitals.com, one review a month; drscore.com, one a quarter. A spokesperson for drscore.com, claiming that such information is proprietary, declined to tell me how, without the controls offered by registration, the site prevents a physician or an angry patient from stuffing the ballot box.

How valid are online reviews?
You might think that the patients most likely to rate a physician or post a comment about her (or his) care are ones who are unhappy with their medical care. You would be wrong: 70% to 90% of online ratings of physicians are positive.3,4 It’s unclear if the positive-negative division of ratings varies between Web sites that require registration (and therefore have a greater degree of accountability) and those that do not. A recent informal sampling of sites reveals that most physicians have five or fewer reviews on any one site—a sample far too small for the rating to be considered valid or to offer meaningful feedback to a physician.
What can I do to protect my reputation?”
Good question. The answer is multifaceted.
- Give your patients an opportunity to provide feedback after an appointment. If they can off-load to you at, or immediately after, their visit, they may be less inclined to post damaging comments elsewhere. And you might actually learn valuable information about your practice and your staff— and how convenient parking is.
- Consider an anonymous survey for the patient to complete before leaving the office or to mail back in a stamped envelope.
- Does the idea of a third-party Internet ranking site appeal to you? Find one that allows you to create a profile and have your staff direct patients to that site.
- Develop a robust Internet presence. Web content that is under your control is more likely to appear at the top of the first search-engine response page (SERP)—thereby pushing potentially negative reviews out of this prime real estate (links that appear on the bottom half of the first page of search results, and beyond, are far less likely to be viewed or clicked). If your Web site isn’t listed first, consult with a search engine optimization specialist about trying to change that. Other ways to generate positive hits on the first SERP? Use Twitter (as long as you are using a version of your name as the username); start a blog; and write guest posts on other Web sites.
- It’s possible to register with all the physician rating sites and receive alerts when you are mentioned, but that could be time-consuming. This strategy is also unlikely to be productive: First, not all sites allow rebuttal or other feedback from physicians. Second, even if you were able to respond, what you can say is limited by HIPAA. Last, although you can flag malicious content for removal, what you consider malicious and what the site administrator considers malicious could differ.
For the fictional Dr. Y., whose story was told at the beginning of this article, this is the best possible answer to her dilemma: Leave the review alone. It’s an opinion, and while hurtful, it isn’t slander and is unlikely to meet the requirements for removal. However, it might be wise to follow up with the bullet-point recommendations I’ve made, above.
Can you muzzle your patient population? One company, Medical Justice, Greensboro, N.C., provides practices with a patient contract that allows the physician to retain copyright to patients’ online comments. The contract doesn’t preclude posting, but the physician is free to remove negative comments. The company’s product was described by its founder and chief executive officer in an article in the December 2009 issue of OBG Management (“Should you worry that patients will use the Web to grade you?,” at www.obgmanagement.com).
Even if—and that’s a big “if”—patients are willing to sign on the dotted line, it’s unclear how such a contract could stop anonymous posting. And, by analogy, would you eat at a restaurant where you were required to turn over copyright to your online comments before you saw the menu?
I’m a believer in physician ratings: If I’m doing a good job for my patients, I like to know that. And, if there’s room for improvement, I can change or fix something I do only if I know about it.
My physician group has had a patient survey in place for several years. It’s similar to the CHECKBOOK/CSS program, although it is accomplished by mail.
I’m proud that I receive high scores from my patients. Whenever I find that some facet of my ratings is slipping, I redouble my efforts. Online, 70% to 90% of my reviews are positive, which is in line with physicians’ experiences reported in the literature that I cited for this article.
Most negative opinions in medicine stem from communication difficulties
As a parent of two medically fragile children who has spent a greater part of 7 years at the other end of the stethoscope, I understand this only too well. So I strive to provide the kind of service that I would want from my providers. I ask my patients if:
- they understand my recommendations
- they agree with the management plan
- there is anything else I have not addressed (and not while I have my hand on the doorknob!).
If I sense that my patient is unhappy, I ask her what’s wrong, and I do my best to allay her fears or mitigate her problems that are under my control. last, I’m not afraid of online reviews—although my preference is for a scientifically valid questionnaire with a focus on achieving adequate numbers.
I believe that, when patients search for health information, they deserve accurate content not only about their health condition but about their physician, too.—Jennifer Gunter, MD
Other models that are worth considering
The United Kingdom’s National Health Service (NHS) operates a health-care rating site (NHS Choices; http://www.nhs.uk), where, among many other services, patients can provide feedback about both physicians and hospitals (anonymous if desired, although an e-mail address is required for validation).1 What’s unique about NHS Choices is that it is moderated; there are specific ground rules for providing ratings; and physicians are encouraged to respond to individual ratings.
In several geographic markets in the United States, Consumer’s CHECKBOOK/ Center for the Study of Services (CHECKBOOK/CSS), a not-for-profit consumer education organization, has piloted an online survey of physicians. Patients are sampled randomly from the enrollment of a list of insurers and invited to participate. The system verifies that the patient being surveyed has made a visit to the physician in question during the past year.
CHECKBOOK/CSS uses questions developed by the US Agency for Healthcare Research and Quality. The reports generated by the system are based on a statistically valid number of surveys (on average, 49 completed surveys for one physician). They are available without charge to the public at the organization’s Web site (http://www.checkbook.org/patientcentral).
A recent perusal of CHECKBOOK/CSS in one market easily found an “above average” rating for a member of the OBG Management Board of Editors….
Let’s make this a useful thing
Here is what we can say with reasonable certainty, based on observation:
- Most online reviews are positive
- Most physicians have far too few ratings on any one Web site to approach a meaningful degree of scientific validity
- Lack of accountability on many ratings Web sites raises the specter of sham negative or positive reviews. The CHECKBOOK/CSS model that I described appears to address many of these concerns.
Most patients have valuable comments and opinions about their medical care; we should remember that listening is our most important clinical skill. Finding a way to make online feedback valid and productive for both patients and physicians should be a goal for our professional societies.
We want to hear from you! Tell us what you think.
1. Lagu T, Lindenauer PK. Putting the public back in public reporting of health care quality. JAMA. 2010;304(15):1711-1712.
2. Fox S, Jones S. The social life of health information. Pew Internet and American Life Project Web site. http://www.pewinternet.org/Reports/2009/8-The-Social-Life-of-Health-Information. aspx. Published June 11, 2009. Accessed January 12, 2011.
3. Lagu T, Hannon NS, Rothberg MB, Lindenauer PK. Patients’ evaluations of health care providers in the era of social networking: an analysis of physician rating websites. J Gen Intern Med. 2010;25(9):942-946.
4. Lopez A, Detz A, Ratanawongsa N, Schillinger D, Sarkar U. What do your patients say about you on the internet? A thematic analysis of online reviews of primary care physicians [abstract]. Presented at: 33rd Annual Society of General Internal Medicine Meeting; May 1, 2010; Minneapolis, MN.
- Twitter 101 for ObGyns: Pearls, pitfalls, and potential
(September 2011)
CASE: Unfairly labeled and now unnerved
Dr. Y, your colleague, calls you; she’s distraught. She performed a Google search of her name and found what she describes as a hateful review on a physician-rating Web site from someone claiming to be her patient. The reviewer declared that Dr. Y. was “rude” and interested only in “pushing one drug.”
“She must be a shill for a drug company….”
You’ve referred many patients to Dr. Y, and you’ve always heard wonderful things about her care. You know that she has never accepted pharma money for lectures or research.
“What should I do?” Dr. Y pleads with you.
We physicians probably don’t think twice about looking up reviews and ratings of hotels and restaurants. But many of us balk at the thought of our professional services being reviewed in such a manner. We’re aware that patients discuss their care, of course, but the Internet— well, that provides a megaphone of global reach for what was once mere water-cooler chat.
And reading angry words in print hurts more than hearing them secondhand.
With the Internet hosting more than 30 sites that rate health-care providers and hospitals, most of us can expect to be reviewed at some point. Only about 15% of people report consulting online physician reviews, however, and fewer than 5% have posted an online review themselves.1,2
What do you need to know about these sites and their potential to have an impact on your practice? Here are some important observations and pearls from the literature and from my experience at the receiving end of ratings.
Types of physician online rating
The first step in navigating the morass of Internet review and rating sites is to understand the types of sites that you’ll encounter.
Angie’s List. This site rates all kinds of services, including physicians. Membership requires registration and a fee. A member can post a review of a given physician every 6 months. Although the names of reviewers are not posted, they are available to the physicians being reviewed—if they ask.
Free Web sites that require registration of some kind. These are general review sites, such as www.yelp.com or specific sites for physicians, such as www.DoctorScorecard.com, which states that a reviewer is allowed to rate a given physician only once.
Free Web sites that don’t require registration. One simply finds the physician’s name and either clicks on the number of stars or writes a review, or both. Two examples: www.vitals.com and www.drscore.com. These sites claim to limit the number of reviews: vitals.com, one review a month; drscore.com, one a quarter. A spokesperson for drscore.com, claiming that such information is proprietary, declined to tell me how, without the controls offered by registration, the site prevents a physician or an angry patient from stuffing the ballot box.

How valid are online reviews?
You might think that the patients most likely to rate a physician or post a comment about her (or his) care are ones who are unhappy with their medical care. You would be wrong: 70% to 90% of online ratings of physicians are positive.3,4 It’s unclear if the positive-negative division of ratings varies between Web sites that require registration (and therefore have a greater degree of accountability) and those that do not. A recent informal sampling of sites reveals that most physicians have five or fewer reviews on any one site—a sample far too small for the rating to be considered valid or to offer meaningful feedback to a physician.
What can I do to protect my reputation?”
Good question. The answer is multifaceted.
- Give your patients an opportunity to provide feedback after an appointment. If they can off-load to you at, or immediately after, their visit, they may be less inclined to post damaging comments elsewhere. And you might actually learn valuable information about your practice and your staff— and how convenient parking is.
- Consider an anonymous survey for the patient to complete before leaving the office or to mail back in a stamped envelope.
- Does the idea of a third-party Internet ranking site appeal to you? Find one that allows you to create a profile and have your staff direct patients to that site.
- Develop a robust Internet presence. Web content that is under your control is more likely to appear at the top of the first search-engine response page (SERP)—thereby pushing potentially negative reviews out of this prime real estate (links that appear on the bottom half of the first page of search results, and beyond, are far less likely to be viewed or clicked). If your Web site isn’t listed first, consult with a search engine optimization specialist about trying to change that. Other ways to generate positive hits on the first SERP? Use Twitter (as long as you are using a version of your name as the username); start a blog; and write guest posts on other Web sites.
- It’s possible to register with all the physician rating sites and receive alerts when you are mentioned, but that could be time-consuming. This strategy is also unlikely to be productive: First, not all sites allow rebuttal or other feedback from physicians. Second, even if you were able to respond, what you can say is limited by HIPAA. Last, although you can flag malicious content for removal, what you consider malicious and what the site administrator considers malicious could differ.
For the fictional Dr. Y., whose story was told at the beginning of this article, this is the best possible answer to her dilemma: Leave the review alone. It’s an opinion, and while hurtful, it isn’t slander and is unlikely to meet the requirements for removal. However, it might be wise to follow up with the bullet-point recommendations I’ve made, above.
Can you muzzle your patient population? One company, Medical Justice, Greensboro, N.C., provides practices with a patient contract that allows the physician to retain copyright to patients’ online comments. The contract doesn’t preclude posting, but the physician is free to remove negative comments. The company’s product was described by its founder and chief executive officer in an article in the December 2009 issue of OBG Management (“Should you worry that patients will use the Web to grade you?,” at www.obgmanagement.com).
Even if—and that’s a big “if”—patients are willing to sign on the dotted line, it’s unclear how such a contract could stop anonymous posting. And, by analogy, would you eat at a restaurant where you were required to turn over copyright to your online comments before you saw the menu?
I’m a believer in physician ratings: If I’m doing a good job for my patients, I like to know that. And, if there’s room for improvement, I can change or fix something I do only if I know about it.
My physician group has had a patient survey in place for several years. It’s similar to the CHECKBOOK/CSS program, although it is accomplished by mail.
I’m proud that I receive high scores from my patients. Whenever I find that some facet of my ratings is slipping, I redouble my efforts. Online, 70% to 90% of my reviews are positive, which is in line with physicians’ experiences reported in the literature that I cited for this article.
Most negative opinions in medicine stem from communication difficulties
As a parent of two medically fragile children who has spent a greater part of 7 years at the other end of the stethoscope, I understand this only too well. So I strive to provide the kind of service that I would want from my providers. I ask my patients if:
- they understand my recommendations
- they agree with the management plan
- there is anything else I have not addressed (and not while I have my hand on the doorknob!).
If I sense that my patient is unhappy, I ask her what’s wrong, and I do my best to allay her fears or mitigate her problems that are under my control. last, I’m not afraid of online reviews—although my preference is for a scientifically valid questionnaire with a focus on achieving adequate numbers.
I believe that, when patients search for health information, they deserve accurate content not only about their health condition but about their physician, too.—Jennifer Gunter, MD
Other models that are worth considering
The United Kingdom’s National Health Service (NHS) operates a health-care rating site (NHS Choices; http://www.nhs.uk), where, among many other services, patients can provide feedback about both physicians and hospitals (anonymous if desired, although an e-mail address is required for validation).1 What’s unique about NHS Choices is that it is moderated; there are specific ground rules for providing ratings; and physicians are encouraged to respond to individual ratings.
In several geographic markets in the United States, Consumer’s CHECKBOOK/ Center for the Study of Services (CHECKBOOK/CSS), a not-for-profit consumer education organization, has piloted an online survey of physicians. Patients are sampled randomly from the enrollment of a list of insurers and invited to participate. The system verifies that the patient being surveyed has made a visit to the physician in question during the past year.
CHECKBOOK/CSS uses questions developed by the US Agency for Healthcare Research and Quality. The reports generated by the system are based on a statistically valid number of surveys (on average, 49 completed surveys for one physician). They are available without charge to the public at the organization’s Web site (http://www.checkbook.org/patientcentral).
A recent perusal of CHECKBOOK/CSS in one market easily found an “above average” rating for a member of the OBG Management Board of Editors….
Let’s make this a useful thing
Here is what we can say with reasonable certainty, based on observation:
- Most online reviews are positive
- Most physicians have far too few ratings on any one Web site to approach a meaningful degree of scientific validity
- Lack of accountability on many ratings Web sites raises the specter of sham negative or positive reviews. The CHECKBOOK/CSS model that I described appears to address many of these concerns.
Most patients have valuable comments and opinions about their medical care; we should remember that listening is our most important clinical skill. Finding a way to make online feedback valid and productive for both patients and physicians should be a goal for our professional societies.
We want to hear from you! Tell us what you think.
- Twitter 101 for ObGyns: Pearls, pitfalls, and potential
(September 2011)
CASE: Unfairly labeled and now unnerved
Dr. Y, your colleague, calls you; she’s distraught. She performed a Google search of her name and found what she describes as a hateful review on a physician-rating Web site from someone claiming to be her patient. The reviewer declared that Dr. Y. was “rude” and interested only in “pushing one drug.”
“She must be a shill for a drug company….”
You’ve referred many patients to Dr. Y, and you’ve always heard wonderful things about her care. You know that she has never accepted pharma money for lectures or research.
“What should I do?” Dr. Y pleads with you.
We physicians probably don’t think twice about looking up reviews and ratings of hotels and restaurants. But many of us balk at the thought of our professional services being reviewed in such a manner. We’re aware that patients discuss their care, of course, but the Internet— well, that provides a megaphone of global reach for what was once mere water-cooler chat.
And reading angry words in print hurts more than hearing them secondhand.
With the Internet hosting more than 30 sites that rate health-care providers and hospitals, most of us can expect to be reviewed at some point. Only about 15% of people report consulting online physician reviews, however, and fewer than 5% have posted an online review themselves.1,2
What do you need to know about these sites and their potential to have an impact on your practice? Here are some important observations and pearls from the literature and from my experience at the receiving end of ratings.
Types of physician online rating
The first step in navigating the morass of Internet review and rating sites is to understand the types of sites that you’ll encounter.
Angie’s List. This site rates all kinds of services, including physicians. Membership requires registration and a fee. A member can post a review of a given physician every 6 months. Although the names of reviewers are not posted, they are available to the physicians being reviewed—if they ask.
Free Web sites that require registration of some kind. These are general review sites, such as www.yelp.com or specific sites for physicians, such as www.DoctorScorecard.com, which states that a reviewer is allowed to rate a given physician only once.
Free Web sites that don’t require registration. One simply finds the physician’s name and either clicks on the number of stars or writes a review, or both. Two examples: www.vitals.com and www.drscore.com. These sites claim to limit the number of reviews: vitals.com, one review a month; drscore.com, one a quarter. A spokesperson for drscore.com, claiming that such information is proprietary, declined to tell me how, without the controls offered by registration, the site prevents a physician or an angry patient from stuffing the ballot box.

How valid are online reviews?
You might think that the patients most likely to rate a physician or post a comment about her (or his) care are ones who are unhappy with their medical care. You would be wrong: 70% to 90% of online ratings of physicians are positive.3,4 It’s unclear if the positive-negative division of ratings varies between Web sites that require registration (and therefore have a greater degree of accountability) and those that do not. A recent informal sampling of sites reveals that most physicians have five or fewer reviews on any one site—a sample far too small for the rating to be considered valid or to offer meaningful feedback to a physician.
What can I do to protect my reputation?”
Good question. The answer is multifaceted.
- Give your patients an opportunity to provide feedback after an appointment. If they can off-load to you at, or immediately after, their visit, they may be less inclined to post damaging comments elsewhere. And you might actually learn valuable information about your practice and your staff— and how convenient parking is.
- Consider an anonymous survey for the patient to complete before leaving the office or to mail back in a stamped envelope.
- Does the idea of a third-party Internet ranking site appeal to you? Find one that allows you to create a profile and have your staff direct patients to that site.
- Develop a robust Internet presence. Web content that is under your control is more likely to appear at the top of the first search-engine response page (SERP)—thereby pushing potentially negative reviews out of this prime real estate (links that appear on the bottom half of the first page of search results, and beyond, are far less likely to be viewed or clicked). If your Web site isn’t listed first, consult with a search engine optimization specialist about trying to change that. Other ways to generate positive hits on the first SERP? Use Twitter (as long as you are using a version of your name as the username); start a blog; and write guest posts on other Web sites.
- It’s possible to register with all the physician rating sites and receive alerts when you are mentioned, but that could be time-consuming. This strategy is also unlikely to be productive: First, not all sites allow rebuttal or other feedback from physicians. Second, even if you were able to respond, what you can say is limited by HIPAA. Last, although you can flag malicious content for removal, what you consider malicious and what the site administrator considers malicious could differ.
For the fictional Dr. Y., whose story was told at the beginning of this article, this is the best possible answer to her dilemma: Leave the review alone. It’s an opinion, and while hurtful, it isn’t slander and is unlikely to meet the requirements for removal. However, it might be wise to follow up with the bullet-point recommendations I’ve made, above.
Can you muzzle your patient population? One company, Medical Justice, Greensboro, N.C., provides practices with a patient contract that allows the physician to retain copyright to patients’ online comments. The contract doesn’t preclude posting, but the physician is free to remove negative comments. The company’s product was described by its founder and chief executive officer in an article in the December 2009 issue of OBG Management (“Should you worry that patients will use the Web to grade you?,” at www.obgmanagement.com).
Even if—and that’s a big “if”—patients are willing to sign on the dotted line, it’s unclear how such a contract could stop anonymous posting. And, by analogy, would you eat at a restaurant where you were required to turn over copyright to your online comments before you saw the menu?
I’m a believer in physician ratings: If I’m doing a good job for my patients, I like to know that. And, if there’s room for improvement, I can change or fix something I do only if I know about it.
My physician group has had a patient survey in place for several years. It’s similar to the CHECKBOOK/CSS program, although it is accomplished by mail.
I’m proud that I receive high scores from my patients. Whenever I find that some facet of my ratings is slipping, I redouble my efforts. Online, 70% to 90% of my reviews are positive, which is in line with physicians’ experiences reported in the literature that I cited for this article.
Most negative opinions in medicine stem from communication difficulties
As a parent of two medically fragile children who has spent a greater part of 7 years at the other end of the stethoscope, I understand this only too well. So I strive to provide the kind of service that I would want from my providers. I ask my patients if:
- they understand my recommendations
- they agree with the management plan
- there is anything else I have not addressed (and not while I have my hand on the doorknob!).
If I sense that my patient is unhappy, I ask her what’s wrong, and I do my best to allay her fears or mitigate her problems that are under my control. last, I’m not afraid of online reviews—although my preference is for a scientifically valid questionnaire with a focus on achieving adequate numbers.
I believe that, when patients search for health information, they deserve accurate content not only about their health condition but about their physician, too.—Jennifer Gunter, MD
Other models that are worth considering
The United Kingdom’s National Health Service (NHS) operates a health-care rating site (NHS Choices; http://www.nhs.uk), where, among many other services, patients can provide feedback about both physicians and hospitals (anonymous if desired, although an e-mail address is required for validation).1 What’s unique about NHS Choices is that it is moderated; there are specific ground rules for providing ratings; and physicians are encouraged to respond to individual ratings.
In several geographic markets in the United States, Consumer’s CHECKBOOK/ Center for the Study of Services (CHECKBOOK/CSS), a not-for-profit consumer education organization, has piloted an online survey of physicians. Patients are sampled randomly from the enrollment of a list of insurers and invited to participate. The system verifies that the patient being surveyed has made a visit to the physician in question during the past year.
CHECKBOOK/CSS uses questions developed by the US Agency for Healthcare Research and Quality. The reports generated by the system are based on a statistically valid number of surveys (on average, 49 completed surveys for one physician). They are available without charge to the public at the organization’s Web site (http://www.checkbook.org/patientcentral).
A recent perusal of CHECKBOOK/CSS in one market easily found an “above average” rating for a member of the OBG Management Board of Editors….
Let’s make this a useful thing
Here is what we can say with reasonable certainty, based on observation:
- Most online reviews are positive
- Most physicians have far too few ratings on any one Web site to approach a meaningful degree of scientific validity
- Lack of accountability on many ratings Web sites raises the specter of sham negative or positive reviews. The CHECKBOOK/CSS model that I described appears to address many of these concerns.
Most patients have valuable comments and opinions about their medical care; we should remember that listening is our most important clinical skill. Finding a way to make online feedback valid and productive for both patients and physicians should be a goal for our professional societies.
We want to hear from you! Tell us what you think.
1. Lagu T, Lindenauer PK. Putting the public back in public reporting of health care quality. JAMA. 2010;304(15):1711-1712.
2. Fox S, Jones S. The social life of health information. Pew Internet and American Life Project Web site. http://www.pewinternet.org/Reports/2009/8-The-Social-Life-of-Health-Information. aspx. Published June 11, 2009. Accessed January 12, 2011.
3. Lagu T, Hannon NS, Rothberg MB, Lindenauer PK. Patients’ evaluations of health care providers in the era of social networking: an analysis of physician rating websites. J Gen Intern Med. 2010;25(9):942-946.
4. Lopez A, Detz A, Ratanawongsa N, Schillinger D, Sarkar U. What do your patients say about you on the internet? A thematic analysis of online reviews of primary care physicians [abstract]. Presented at: 33rd Annual Society of General Internal Medicine Meeting; May 1, 2010; Minneapolis, MN.
1. Lagu T, Lindenauer PK. Putting the public back in public reporting of health care quality. JAMA. 2010;304(15):1711-1712.
2. Fox S, Jones S. The social life of health information. Pew Internet and American Life Project Web site. http://www.pewinternet.org/Reports/2009/8-The-Social-Life-of-Health-Information. aspx. Published June 11, 2009. Accessed January 12, 2011.
3. Lagu T, Hannon NS, Rothberg MB, Lindenauer PK. Patients’ evaluations of health care providers in the era of social networking: an analysis of physician rating websites. J Gen Intern Med. 2010;25(9):942-946.
4. Lopez A, Detz A, Ratanawongsa N, Schillinger D, Sarkar U. What do your patients say about you on the internet? A thematic analysis of online reviews of primary care physicians [abstract]. Presented at: 33rd Annual Society of General Internal Medicine Meeting; May 1, 2010; Minneapolis, MN.
Twitter 101 for ObGyns: Pearls, pitfalls, and potential
CASE: An acute episode of “evidence-baseless” medicine
You are discussing routine gyn care with a 20-year-old new patient. When you mention the value of being vaccinated against human papillomavirus, she says that she’s heard cervical cancer is caused by a weak immune system, not by HPV—and that she knows that a lot of girls have died from the vaccine.
You listen to her concerns and respond systematically, pointing out that the Nobel Prize in medicine in 2008 was awarded for the discovery of the link between HPV and cervical cancer and that 23 million doses of the HPV vaccine have been administered in the United States with 32 reported associated deaths—none attributable to the vaccine. You refer her to the Centers for Disease Control and Prevention Web site for more information.
You wrap up by asking her where she learned about the HPV vaccine.
“Twitter.”
Later that day, while you catch up on charting, you wonder: Exactly what is this Twitter? And why is it dispensing medical advice?
The answer to your first question, if you were not already clued in, is that Twitter is a social network that spreads information and links in messages (from individual and group subscribers) known as tweets, of 140 characters or fewer characters each. Because the number of characters is limited, tweeting is also known as microblogging.
Twitter is for what’s happening now, so it fits right into the 24/7 nature of the news and information cycle that increasingly characterizes our culture. You can tweet from your Twitter home page through a third-party application on your computer; or on the go by means of instant messaging or applications on a smart phone (iPhone, BlackBerry, Palm Treo, etc.). Subscribers who are interested sign on to follow your tweets, and you, in turn, sign on to follow the tweets of others—of your choosing and in unlimited numbers and potential variety.
The numbers are persuasive
Introduced in 2006, Twitter has evolved into a powerful social networking tool. According to information released at Chirp, the official Twitter developer conference held in San Francisco this past April, Twitter has more than 105 million registered users, more than 180 million unique visitors to the twitterverse each month, and, on average, 55 million tweets and 600 million search queries each day.
Four percent of news stories posted on Twitter are on health and medicine topics; compare this to 11% of stories in the traditional press. However, more and more, Twitter is becoming a legitimate source of medical information, as government agencies, organizations, hospitals, universities, medical societies, and journals use the service to disseminate information.1
That rising legitimacy means that you may want to consider becoming part of the twitterverse, for the good of your practice and your professional standing. Here are the basics of how to jump in, sensibly and usefully.
First, let me disclose myself: I tweet professionally as @DrJenGunter. I’ve met many fascinating people on Twitter—and only a few weirdoes, whom I’ve quickly blocked from having access to what I write (you can easily do that). I’m certainly not alone in our specialty: “We tweet, too,” describes the experiences of two ObGyns who use Twitter in their practice.
Twitter promotes the spread of good medical information when reputable voices utilize it. Sixty percent of patients look for health information on the Web; more than 50% of them believe that what they find there is essentially correct2,3—even though no entity controls accuracy or detects bias. In one study, high-school students were asked to research vaccines on the Web using the search terms “vaccine danger” and “vaccine safety”: On average, 65% of links identified on the first page of each search contained inaccurate information.4
Your presence on Twitter can be a powerful antidote to whatever misinformation is posted there. (Recall the hypothetical case at the beginning of this article?)
Twitter expands your on-line presence, at no cost. Like it or not, your patients are looking you up on-line.
Twitter connects you with other like-minded physicians—and with nurses, researchers, and health-care advocates.
Twitter attracts the interest of reporters and writers. Journalists use the service as a source of contacts.
Twitter can help you expand your practice and your “brand.”
An express tutorial
With Twitter, you find tweeps (people) who interest you; once you opt to “follow” them, their tweets appear real-time in your Twitter stream. You use the Twitter search function to peruse names, organizations, and subject matter, and to browse through lists of other people’s favorite tweeps. (One of the most comprehensive lists of tweeting physicians is twitter-doctors, maintained by “@hrana,” an internist who lists his location as 221b Baker Street.
The “@” before the username signals a reply to a tweet. Search these replies to find out who is sending you information in the public twitter stream; use “@” to reply in return so that the recipient knows you are talking to them. At http://tweetoclock.com, you can determine what time a given person is most likely to be active on Twitter, and then tweet accordingly; this is especially useful if you are trying to get the attention of someone who is not following you.
One goal is to get your tweets retweeted—meaning that your tweet is re-sent out by your followers to their followers, and so on, allowing your message to exponentially reach more people (if it’s interesting or funny enough, that is). Then, when non-followers read your message, they may be tempted to check out your home page and follow you if they like what they read.
There is some cloak of privacy on Twitter. You can communicate on Twitter using a direct message (a DM) that is seen only by its recipient. To send a DM, however, the person on the receiving end must be following you back.
In addition:
- If you decide you don’t want a person seeing what you have to say, you can block them from following you (although they can still see your tweets in searches, just not real-time)
- You can protect your profile from searches and make your tweets visible only to followers you have approved. Doing so ensures a higher degree of privacy but reduces the number of your followers; that’s because people like to check you out before they sign up to follow you and your tweets.
You can learn much more about how Twitter functions, and how to establish an account, under “Twitter Basics” at http://support.twitter.com. First, however, read “Steps 1 through 8 to get yourself started with Twitter.”
- First, think about how, and why, you plan to establish an identity on Twitter. Are you a health care professional, or a bass player or a closet comedian—or all three?1 The point is: Decide now what your goal is in taking the next step.
- Visit www.twitter.com and click on the yellow “Get Started Now” button
- Enter your name. What you enter will appear on your Twitter home page, but not on your tweets. Many people choose their real name; some pick a pseudonym. Don’t count on a pseudonym to provide anonymity, however—it’s not hard for someone to figure out who you are on Twitter.
- Choose a username (15 or fewer characters). Consider using a version of your name or the name of your practice, or a creative identity that supports your professional message. Make the username professional, accessible, and identifiable—think “business casual.” (Your Twitter homepage will be twitter.com/[username].)
- Upload a photograph of yourself for your home page. People (tweeps) are more likely to engage with you on Twitter when there’s a face behind the messages.
- Add a biographical statement to your home page. In capsule form, describe who you are and what you bring to the “Twitter table.”
- If your practice has a Web site, include a link to it.
- Follow some people, jump into the Twitter stream, and start swimming!
Reference
1. Grindrod KA, Gavura S. Pharmacy 2.0. Canadian Pharmacists J. 2010;143(3):122-125.
Twitter is like a…giant cocktail party
You know: You circle the room, and you have social permission to drop in on any conversation. You show your personality; you’re willing to engage. And you absolutely have something interesting to say, because no one wants to listen if you are only talking about yourself or only have one thing to talk about.
In short, you’re here to try to forge relationships.
For physicians interested in promoting their medical practice or “brand,” one strategy on Twitter is to divide your tweets into four (roughly equal in terms of volume, as a guide) categories:
- General medical information that’s related to your interests (although, if you read a fascinating article on a medical topic out of your left field, like keratoconus, send it along). You can tweet facts from your experience or from journals, or tweet links to authoritative, reputable Web sites that offer relevant medical information. Ask other experts whom you follow for their opinion on breaking stories in the media and medical literature. Follow organizations, associations, and journals so that you have instant access to breaking news to retweet to followers.
- Your specific message. Talk about topics on which you’re an expert; give information that’s exclusively yours. Provide a link to your practice blog or Web site, and to relevant articles in your area of interest. Tweet about what makes you, or your practice or your “brand,” special.
- General conversation—anything but medicine. Demonstrate that you have other interests; that you’re not one-dimensional. Tweet about top news stories, sports, last book read, or a favorite TV program. If you are less interested in Twitter for business purposes, then increase your general conversation.
- Retweeting. This is definitely a “do-unto-others” thing. Add a comment to the retweet to make it personal.
There may be a lot of fluff on Twitter, but there’s a lot of substance, too—and you get to decide which category enters your “stream.” Using Twitter can be a helpful way to learn about interesting research and breaking news that might otherwise pass you by. And it can broaden your professional and personal network.
These and other benefits are what hooked Ruth Ann Crystal, MD, an ObGyn in solo private practice in Palo Alto, Calif. Crystal tweets under the handle @CatchThe-Baby and has roughly 560 followers.
“I have been able to share with other doctors what I think about certain medical subjects and to compare it to what they have found in their practice experience,” she says.
“I follow the tweets of physicians, residents, medical students, and nurses from the United States and even from England and India. I follow the links to some great medical blogs like SCOPE (@SUMedicine), KevinMD.com (@KevinMD), ACOG (@acognews), NPR (@NPRHealth), Reuters (@Reuters_Health), etc. I can pick and choose which tweets (headlines) are most interesting to me so I don’t need to check each blog every day.”
“In addition, I follow tweeple (people who tweet, or tweeps) in other subjects that are interesting to me, such as food bloggers, high tech people, mama bloggers, and even a few silly sites to make me smile.”
“For me, Twitter is like having my own personal news channel. I get updated by those whose stories matter to me most. I learn every day.”
Communication is the thing
Although he uses Twitter for a slightly different purpose, Nicholas Fogelson, MD, finds great value in it. He tweets under @academicobgyn and, at last count, has 570 followers.
“My primary use of Twitter is as a second methodology for communicating with fans of my blog and podcast” (http://www.academicobgyn.com), he says. “I do not tweet directly to my patients or use it in direct conjunction with my practice.”
“Twitter has allowed me to network with ObGyns and other physicians from around the country and the world. Through Twitter and my blog, I have many contacts and friends who would have been inaccessible without them. I have also engaged in dialogue with thousands of nonphysicians about various issues that concern patients and physicians.” He adds: “I have met many talented and exciting people who are in completely different fields that I would never have run into in my normal physician life!”
Tangible benefits
Networking with other medical professionals is one of the biggest benefits Crystal has gained by using Twitter.
“For example, several of us docs were discussing the importance of vitamin D. We talked about the latest research data but also about the correct ICD-9 code to use on lab slips,” she says.
Fogelson’s focus is on branding. “Twitter allows a physician to develop a personal brand that carries beyond his or her employer,” he says. “Many physicians change jobs from time to time, and as such, lose their branding. Twitter and blogging allows one to brand oneself separately from the brand of the practice. At the same time, this self-branding can improve the super-brand of the practice, and bring in patients who otherwise might not have known about the practice.”
Caveats
“I find Twitter to be a bit addictive,” warns Crystal. “Therefore, I limit how much time I spend in this virtual world.”
“It is also extremely important that doctors not tweet personal information about patients without their consent. Sometimes I tweet the first name of the baby I just delivered (e.g., ‘Welcome to the world, Baby Jacob!’), but I always get consent first from both parents. Patient confidentiality and patient consent are paramount.”
For physicians on Twitter, what not to say, and do
Do not reveal HIPAA-protected information. In fact, be careful not to be too specific about your day. Don’t say “nasty case of gonorrhea this afternoon”; instead, if gonorrhea is on your mind, offer some statistics and a link to the Web site of the Centers for Disease Control and Prevention. You never know if that patient from “this afternoon,” or her mother, is following you.
Do not post a statement or picture that you wouldn’t want to see on the front page of a newspaper. In one study of medical students and residents who created an identity on Facebook, 70% had posted photographs of themselves with alcohol; in many of those photos, what was shown implied drinking to excess.5 Imagine the impact of that picture, poster-sized, when displayed to a jury at a malpractice trial….
Be wary of using Doc-speak. Your tweets, private or otherwise, are fair game for misinterpretation. Tweeting “Labor and delivery was crazy” may mean simply that there was a steady stream of patients and you didn’t get to eat dinner, but an attorney may, based on that statement, be able to convince a jury that L&D was understaffed.
Likewise, tweeting “Just finished a tough hysterectomy” may mean a complication-free laparoscopic procedure on an obese patient who had a 16-week-size uterus and dense adhesions but, to a jury, that might translate as, “I was in over my head and should have called for back-up.”
Don’t dispense medical advice. Ever. If people tweet you for advice, refer them to their physician in reply. Many physicians (including me) include a disclaimer in their Twitter biographical statement emphasizing that their tweets do not constitute medical advice.
Have you tried Twitter? Do you have a story to tell about it? Tweet me about it!—@DrJenGunter
Follow OBG ManaGeMent on Twitter: @obgmanagement.com
1. Fox S, Jones S. The social life of health information. Pew Internet & American Life Project. http://www.pewinternet.org/Reports/2009/8-The-Social-Life-of-Health-Information.aspx. Published June 11, 2009. Accessed June 1, 2010.
2. Fox S, Rainie L, Horrigan J, et al. The online health care revolution: how the Web helps Americans take better care of themselves. Pew Internet & American Life Project. http://www.pewinternet.org/Reports/2000/The-Online-Health-Care-Revolution.aspx. Published November 26, 2000. Accessed June 1, 2010.
3. How blogs and social media agendas relate and differ from the traditional press. Journalism.org Web site. http://www.journalism.org/node/20621. Published May 23, 2010. Accessed June 1, 2010.
4. Thompson LA, Dawson K, Ferdig R, et al. The intersection of online social networking with medical professionalism. J Gen Intern Med. 2008;23(7):954-957.
CASE: An acute episode of “evidence-baseless” medicine
You are discussing routine gyn care with a 20-year-old new patient. When you mention the value of being vaccinated against human papillomavirus, she says that she’s heard cervical cancer is caused by a weak immune system, not by HPV—and that she knows that a lot of girls have died from the vaccine.
You listen to her concerns and respond systematically, pointing out that the Nobel Prize in medicine in 2008 was awarded for the discovery of the link between HPV and cervical cancer and that 23 million doses of the HPV vaccine have been administered in the United States with 32 reported associated deaths—none attributable to the vaccine. You refer her to the Centers for Disease Control and Prevention Web site for more information.
You wrap up by asking her where she learned about the HPV vaccine.
“Twitter.”
Later that day, while you catch up on charting, you wonder: Exactly what is this Twitter? And why is it dispensing medical advice?
The answer to your first question, if you were not already clued in, is that Twitter is a social network that spreads information and links in messages (from individual and group subscribers) known as tweets, of 140 characters or fewer characters each. Because the number of characters is limited, tweeting is also known as microblogging.
Twitter is for what’s happening now, so it fits right into the 24/7 nature of the news and information cycle that increasingly characterizes our culture. You can tweet from your Twitter home page through a third-party application on your computer; or on the go by means of instant messaging or applications on a smart phone (iPhone, BlackBerry, Palm Treo, etc.). Subscribers who are interested sign on to follow your tweets, and you, in turn, sign on to follow the tweets of others—of your choosing and in unlimited numbers and potential variety.
The numbers are persuasive
Introduced in 2006, Twitter has evolved into a powerful social networking tool. According to information released at Chirp, the official Twitter developer conference held in San Francisco this past April, Twitter has more than 105 million registered users, more than 180 million unique visitors to the twitterverse each month, and, on average, 55 million tweets and 600 million search queries each day.
Four percent of news stories posted on Twitter are on health and medicine topics; compare this to 11% of stories in the traditional press. However, more and more, Twitter is becoming a legitimate source of medical information, as government agencies, organizations, hospitals, universities, medical societies, and journals use the service to disseminate information.1
That rising legitimacy means that you may want to consider becoming part of the twitterverse, for the good of your practice and your professional standing. Here are the basics of how to jump in, sensibly and usefully.
First, let me disclose myself: I tweet professionally as @DrJenGunter. I’ve met many fascinating people on Twitter—and only a few weirdoes, whom I’ve quickly blocked from having access to what I write (you can easily do that). I’m certainly not alone in our specialty: “We tweet, too,” describes the experiences of two ObGyns who use Twitter in their practice.
Twitter promotes the spread of good medical information when reputable voices utilize it. Sixty percent of patients look for health information on the Web; more than 50% of them believe that what they find there is essentially correct2,3—even though no entity controls accuracy or detects bias. In one study, high-school students were asked to research vaccines on the Web using the search terms “vaccine danger” and “vaccine safety”: On average, 65% of links identified on the first page of each search contained inaccurate information.4
Your presence on Twitter can be a powerful antidote to whatever misinformation is posted there. (Recall the hypothetical case at the beginning of this article?)
Twitter expands your on-line presence, at no cost. Like it or not, your patients are looking you up on-line.
Twitter connects you with other like-minded physicians—and with nurses, researchers, and health-care advocates.
Twitter attracts the interest of reporters and writers. Journalists use the service as a source of contacts.
Twitter can help you expand your practice and your “brand.”
An express tutorial
With Twitter, you find tweeps (people) who interest you; once you opt to “follow” them, their tweets appear real-time in your Twitter stream. You use the Twitter search function to peruse names, organizations, and subject matter, and to browse through lists of other people’s favorite tweeps. (One of the most comprehensive lists of tweeting physicians is twitter-doctors, maintained by “@hrana,” an internist who lists his location as 221b Baker Street.
The “@” before the username signals a reply to a tweet. Search these replies to find out who is sending you information in the public twitter stream; use “@” to reply in return so that the recipient knows you are talking to them. At http://tweetoclock.com, you can determine what time a given person is most likely to be active on Twitter, and then tweet accordingly; this is especially useful if you are trying to get the attention of someone who is not following you.
One goal is to get your tweets retweeted—meaning that your tweet is re-sent out by your followers to their followers, and so on, allowing your message to exponentially reach more people (if it’s interesting or funny enough, that is). Then, when non-followers read your message, they may be tempted to check out your home page and follow you if they like what they read.
There is some cloak of privacy on Twitter. You can communicate on Twitter using a direct message (a DM) that is seen only by its recipient. To send a DM, however, the person on the receiving end must be following you back.
In addition:
- If you decide you don’t want a person seeing what you have to say, you can block them from following you (although they can still see your tweets in searches, just not real-time)
- You can protect your profile from searches and make your tweets visible only to followers you have approved. Doing so ensures a higher degree of privacy but reduces the number of your followers; that’s because people like to check you out before they sign up to follow you and your tweets.
You can learn much more about how Twitter functions, and how to establish an account, under “Twitter Basics” at http://support.twitter.com. First, however, read “Steps 1 through 8 to get yourself started with Twitter.”
- First, think about how, and why, you plan to establish an identity on Twitter. Are you a health care professional, or a bass player or a closet comedian—or all three?1 The point is: Decide now what your goal is in taking the next step.
- Visit www.twitter.com and click on the yellow “Get Started Now” button
- Enter your name. What you enter will appear on your Twitter home page, but not on your tweets. Many people choose their real name; some pick a pseudonym. Don’t count on a pseudonym to provide anonymity, however—it’s not hard for someone to figure out who you are on Twitter.
- Choose a username (15 or fewer characters). Consider using a version of your name or the name of your practice, or a creative identity that supports your professional message. Make the username professional, accessible, and identifiable—think “business casual.” (Your Twitter homepage will be twitter.com/[username].)
- Upload a photograph of yourself for your home page. People (tweeps) are more likely to engage with you on Twitter when there’s a face behind the messages.
- Add a biographical statement to your home page. In capsule form, describe who you are and what you bring to the “Twitter table.”
- If your practice has a Web site, include a link to it.
- Follow some people, jump into the Twitter stream, and start swimming!
Reference
1. Grindrod KA, Gavura S. Pharmacy 2.0. Canadian Pharmacists J. 2010;143(3):122-125.
Twitter is like a…giant cocktail party
You know: You circle the room, and you have social permission to drop in on any conversation. You show your personality; you’re willing to engage. And you absolutely have something interesting to say, because no one wants to listen if you are only talking about yourself or only have one thing to talk about.
In short, you’re here to try to forge relationships.
For physicians interested in promoting their medical practice or “brand,” one strategy on Twitter is to divide your tweets into four (roughly equal in terms of volume, as a guide) categories:
- General medical information that’s related to your interests (although, if you read a fascinating article on a medical topic out of your left field, like keratoconus, send it along). You can tweet facts from your experience or from journals, or tweet links to authoritative, reputable Web sites that offer relevant medical information. Ask other experts whom you follow for their opinion on breaking stories in the media and medical literature. Follow organizations, associations, and journals so that you have instant access to breaking news to retweet to followers.
- Your specific message. Talk about topics on which you’re an expert; give information that’s exclusively yours. Provide a link to your practice blog or Web site, and to relevant articles in your area of interest. Tweet about what makes you, or your practice or your “brand,” special.
- General conversation—anything but medicine. Demonstrate that you have other interests; that you’re not one-dimensional. Tweet about top news stories, sports, last book read, or a favorite TV program. If you are less interested in Twitter for business purposes, then increase your general conversation.
- Retweeting. This is definitely a “do-unto-others” thing. Add a comment to the retweet to make it personal.
There may be a lot of fluff on Twitter, but there’s a lot of substance, too—and you get to decide which category enters your “stream.” Using Twitter can be a helpful way to learn about interesting research and breaking news that might otherwise pass you by. And it can broaden your professional and personal network.
These and other benefits are what hooked Ruth Ann Crystal, MD, an ObGyn in solo private practice in Palo Alto, Calif. Crystal tweets under the handle @CatchThe-Baby and has roughly 560 followers.
“I have been able to share with other doctors what I think about certain medical subjects and to compare it to what they have found in their practice experience,” she says.
“I follow the tweets of physicians, residents, medical students, and nurses from the United States and even from England and India. I follow the links to some great medical blogs like SCOPE (@SUMedicine), KevinMD.com (@KevinMD), ACOG (@acognews), NPR (@NPRHealth), Reuters (@Reuters_Health), etc. I can pick and choose which tweets (headlines) are most interesting to me so I don’t need to check each blog every day.”
“In addition, I follow tweeple (people who tweet, or tweeps) in other subjects that are interesting to me, such as food bloggers, high tech people, mama bloggers, and even a few silly sites to make me smile.”
“For me, Twitter is like having my own personal news channel. I get updated by those whose stories matter to me most. I learn every day.”
Communication is the thing
Although he uses Twitter for a slightly different purpose, Nicholas Fogelson, MD, finds great value in it. He tweets under @academicobgyn and, at last count, has 570 followers.
“My primary use of Twitter is as a second methodology for communicating with fans of my blog and podcast” (http://www.academicobgyn.com), he says. “I do not tweet directly to my patients or use it in direct conjunction with my practice.”
“Twitter has allowed me to network with ObGyns and other physicians from around the country and the world. Through Twitter and my blog, I have many contacts and friends who would have been inaccessible without them. I have also engaged in dialogue with thousands of nonphysicians about various issues that concern patients and physicians.” He adds: “I have met many talented and exciting people who are in completely different fields that I would never have run into in my normal physician life!”
Tangible benefits
Networking with other medical professionals is one of the biggest benefits Crystal has gained by using Twitter.
“For example, several of us docs were discussing the importance of vitamin D. We talked about the latest research data but also about the correct ICD-9 code to use on lab slips,” she says.
Fogelson’s focus is on branding. “Twitter allows a physician to develop a personal brand that carries beyond his or her employer,” he says. “Many physicians change jobs from time to time, and as such, lose their branding. Twitter and blogging allows one to brand oneself separately from the brand of the practice. At the same time, this self-branding can improve the super-brand of the practice, and bring in patients who otherwise might not have known about the practice.”
Caveats
“I find Twitter to be a bit addictive,” warns Crystal. “Therefore, I limit how much time I spend in this virtual world.”
“It is also extremely important that doctors not tweet personal information about patients without their consent. Sometimes I tweet the first name of the baby I just delivered (e.g., ‘Welcome to the world, Baby Jacob!’), but I always get consent first from both parents. Patient confidentiality and patient consent are paramount.”
For physicians on Twitter, what not to say, and do
Do not reveal HIPAA-protected information. In fact, be careful not to be too specific about your day. Don’t say “nasty case of gonorrhea this afternoon”; instead, if gonorrhea is on your mind, offer some statistics and a link to the Web site of the Centers for Disease Control and Prevention. You never know if that patient from “this afternoon,” or her mother, is following you.
Do not post a statement or picture that you wouldn’t want to see on the front page of a newspaper. In one study of medical students and residents who created an identity on Facebook, 70% had posted photographs of themselves with alcohol; in many of those photos, what was shown implied drinking to excess.5 Imagine the impact of that picture, poster-sized, when displayed to a jury at a malpractice trial….
Be wary of using Doc-speak. Your tweets, private or otherwise, are fair game for misinterpretation. Tweeting “Labor and delivery was crazy” may mean simply that there was a steady stream of patients and you didn’t get to eat dinner, but an attorney may, based on that statement, be able to convince a jury that L&D was understaffed.
Likewise, tweeting “Just finished a tough hysterectomy” may mean a complication-free laparoscopic procedure on an obese patient who had a 16-week-size uterus and dense adhesions but, to a jury, that might translate as, “I was in over my head and should have called for back-up.”
Don’t dispense medical advice. Ever. If people tweet you for advice, refer them to their physician in reply. Many physicians (including me) include a disclaimer in their Twitter biographical statement emphasizing that their tweets do not constitute medical advice.
Have you tried Twitter? Do you have a story to tell about it? Tweet me about it!—@DrJenGunter
Follow OBG ManaGeMent on Twitter: @obgmanagement.com
CASE: An acute episode of “evidence-baseless” medicine
You are discussing routine gyn care with a 20-year-old new patient. When you mention the value of being vaccinated against human papillomavirus, she says that she’s heard cervical cancer is caused by a weak immune system, not by HPV—and that she knows that a lot of girls have died from the vaccine.
You listen to her concerns and respond systematically, pointing out that the Nobel Prize in medicine in 2008 was awarded for the discovery of the link between HPV and cervical cancer and that 23 million doses of the HPV vaccine have been administered in the United States with 32 reported associated deaths—none attributable to the vaccine. You refer her to the Centers for Disease Control and Prevention Web site for more information.
You wrap up by asking her where she learned about the HPV vaccine.
“Twitter.”
Later that day, while you catch up on charting, you wonder: Exactly what is this Twitter? And why is it dispensing medical advice?
The answer to your first question, if you were not already clued in, is that Twitter is a social network that spreads information and links in messages (from individual and group subscribers) known as tweets, of 140 characters or fewer characters each. Because the number of characters is limited, tweeting is also known as microblogging.
Twitter is for what’s happening now, so it fits right into the 24/7 nature of the news and information cycle that increasingly characterizes our culture. You can tweet from your Twitter home page through a third-party application on your computer; or on the go by means of instant messaging or applications on a smart phone (iPhone, BlackBerry, Palm Treo, etc.). Subscribers who are interested sign on to follow your tweets, and you, in turn, sign on to follow the tweets of others—of your choosing and in unlimited numbers and potential variety.
The numbers are persuasive
Introduced in 2006, Twitter has evolved into a powerful social networking tool. According to information released at Chirp, the official Twitter developer conference held in San Francisco this past April, Twitter has more than 105 million registered users, more than 180 million unique visitors to the twitterverse each month, and, on average, 55 million tweets and 600 million search queries each day.
Four percent of news stories posted on Twitter are on health and medicine topics; compare this to 11% of stories in the traditional press. However, more and more, Twitter is becoming a legitimate source of medical information, as government agencies, organizations, hospitals, universities, medical societies, and journals use the service to disseminate information.1
That rising legitimacy means that you may want to consider becoming part of the twitterverse, for the good of your practice and your professional standing. Here are the basics of how to jump in, sensibly and usefully.
First, let me disclose myself: I tweet professionally as @DrJenGunter. I’ve met many fascinating people on Twitter—and only a few weirdoes, whom I’ve quickly blocked from having access to what I write (you can easily do that). I’m certainly not alone in our specialty: “We tweet, too,” describes the experiences of two ObGyns who use Twitter in their practice.
Twitter promotes the spread of good medical information when reputable voices utilize it. Sixty percent of patients look for health information on the Web; more than 50% of them believe that what they find there is essentially correct2,3—even though no entity controls accuracy or detects bias. In one study, high-school students were asked to research vaccines on the Web using the search terms “vaccine danger” and “vaccine safety”: On average, 65% of links identified on the first page of each search contained inaccurate information.4
Your presence on Twitter can be a powerful antidote to whatever misinformation is posted there. (Recall the hypothetical case at the beginning of this article?)
Twitter expands your on-line presence, at no cost. Like it or not, your patients are looking you up on-line.
Twitter connects you with other like-minded physicians—and with nurses, researchers, and health-care advocates.
Twitter attracts the interest of reporters and writers. Journalists use the service as a source of contacts.
Twitter can help you expand your practice and your “brand.”
An express tutorial
With Twitter, you find tweeps (people) who interest you; once you opt to “follow” them, their tweets appear real-time in your Twitter stream. You use the Twitter search function to peruse names, organizations, and subject matter, and to browse through lists of other people’s favorite tweeps. (One of the most comprehensive lists of tweeting physicians is twitter-doctors, maintained by “@hrana,” an internist who lists his location as 221b Baker Street.
The “@” before the username signals a reply to a tweet. Search these replies to find out who is sending you information in the public twitter stream; use “@” to reply in return so that the recipient knows you are talking to them. At http://tweetoclock.com, you can determine what time a given person is most likely to be active on Twitter, and then tweet accordingly; this is especially useful if you are trying to get the attention of someone who is not following you.
One goal is to get your tweets retweeted—meaning that your tweet is re-sent out by your followers to their followers, and so on, allowing your message to exponentially reach more people (if it’s interesting or funny enough, that is). Then, when non-followers read your message, they may be tempted to check out your home page and follow you if they like what they read.
There is some cloak of privacy on Twitter. You can communicate on Twitter using a direct message (a DM) that is seen only by its recipient. To send a DM, however, the person on the receiving end must be following you back.
In addition:
- If you decide you don’t want a person seeing what you have to say, you can block them from following you (although they can still see your tweets in searches, just not real-time)
- You can protect your profile from searches and make your tweets visible only to followers you have approved. Doing so ensures a higher degree of privacy but reduces the number of your followers; that’s because people like to check you out before they sign up to follow you and your tweets.
You can learn much more about how Twitter functions, and how to establish an account, under “Twitter Basics” at http://support.twitter.com. First, however, read “Steps 1 through 8 to get yourself started with Twitter.”
- First, think about how, and why, you plan to establish an identity on Twitter. Are you a health care professional, or a bass player or a closet comedian—or all three?1 The point is: Decide now what your goal is in taking the next step.
- Visit www.twitter.com and click on the yellow “Get Started Now” button
- Enter your name. What you enter will appear on your Twitter home page, but not on your tweets. Many people choose their real name; some pick a pseudonym. Don’t count on a pseudonym to provide anonymity, however—it’s not hard for someone to figure out who you are on Twitter.
- Choose a username (15 or fewer characters). Consider using a version of your name or the name of your practice, or a creative identity that supports your professional message. Make the username professional, accessible, and identifiable—think “business casual.” (Your Twitter homepage will be twitter.com/[username].)
- Upload a photograph of yourself for your home page. People (tweeps) are more likely to engage with you on Twitter when there’s a face behind the messages.
- Add a biographical statement to your home page. In capsule form, describe who you are and what you bring to the “Twitter table.”
- If your practice has a Web site, include a link to it.
- Follow some people, jump into the Twitter stream, and start swimming!
Reference
1. Grindrod KA, Gavura S. Pharmacy 2.0. Canadian Pharmacists J. 2010;143(3):122-125.
Twitter is like a…giant cocktail party
You know: You circle the room, and you have social permission to drop in on any conversation. You show your personality; you’re willing to engage. And you absolutely have something interesting to say, because no one wants to listen if you are only talking about yourself or only have one thing to talk about.
In short, you’re here to try to forge relationships.
For physicians interested in promoting their medical practice or “brand,” one strategy on Twitter is to divide your tweets into four (roughly equal in terms of volume, as a guide) categories:
- General medical information that’s related to your interests (although, if you read a fascinating article on a medical topic out of your left field, like keratoconus, send it along). You can tweet facts from your experience or from journals, or tweet links to authoritative, reputable Web sites that offer relevant medical information. Ask other experts whom you follow for their opinion on breaking stories in the media and medical literature. Follow organizations, associations, and journals so that you have instant access to breaking news to retweet to followers.
- Your specific message. Talk about topics on which you’re an expert; give information that’s exclusively yours. Provide a link to your practice blog or Web site, and to relevant articles in your area of interest. Tweet about what makes you, or your practice or your “brand,” special.
- General conversation—anything but medicine. Demonstrate that you have other interests; that you’re not one-dimensional. Tweet about top news stories, sports, last book read, or a favorite TV program. If you are less interested in Twitter for business purposes, then increase your general conversation.
- Retweeting. This is definitely a “do-unto-others” thing. Add a comment to the retweet to make it personal.
There may be a lot of fluff on Twitter, but there’s a lot of substance, too—and you get to decide which category enters your “stream.” Using Twitter can be a helpful way to learn about interesting research and breaking news that might otherwise pass you by. And it can broaden your professional and personal network.
These and other benefits are what hooked Ruth Ann Crystal, MD, an ObGyn in solo private practice in Palo Alto, Calif. Crystal tweets under the handle @CatchThe-Baby and has roughly 560 followers.
“I have been able to share with other doctors what I think about certain medical subjects and to compare it to what they have found in their practice experience,” she says.
“I follow the tweets of physicians, residents, medical students, and nurses from the United States and even from England and India. I follow the links to some great medical blogs like SCOPE (@SUMedicine), KevinMD.com (@KevinMD), ACOG (@acognews), NPR (@NPRHealth), Reuters (@Reuters_Health), etc. I can pick and choose which tweets (headlines) are most interesting to me so I don’t need to check each blog every day.”
“In addition, I follow tweeple (people who tweet, or tweeps) in other subjects that are interesting to me, such as food bloggers, high tech people, mama bloggers, and even a few silly sites to make me smile.”
“For me, Twitter is like having my own personal news channel. I get updated by those whose stories matter to me most. I learn every day.”
Communication is the thing
Although he uses Twitter for a slightly different purpose, Nicholas Fogelson, MD, finds great value in it. He tweets under @academicobgyn and, at last count, has 570 followers.
“My primary use of Twitter is as a second methodology for communicating with fans of my blog and podcast” (http://www.academicobgyn.com), he says. “I do not tweet directly to my patients or use it in direct conjunction with my practice.”
“Twitter has allowed me to network with ObGyns and other physicians from around the country and the world. Through Twitter and my blog, I have many contacts and friends who would have been inaccessible without them. I have also engaged in dialogue with thousands of nonphysicians about various issues that concern patients and physicians.” He adds: “I have met many talented and exciting people who are in completely different fields that I would never have run into in my normal physician life!”
Tangible benefits
Networking with other medical professionals is one of the biggest benefits Crystal has gained by using Twitter.
“For example, several of us docs were discussing the importance of vitamin D. We talked about the latest research data but also about the correct ICD-9 code to use on lab slips,” she says.
Fogelson’s focus is on branding. “Twitter allows a physician to develop a personal brand that carries beyond his or her employer,” he says. “Many physicians change jobs from time to time, and as such, lose their branding. Twitter and blogging allows one to brand oneself separately from the brand of the practice. At the same time, this self-branding can improve the super-brand of the practice, and bring in patients who otherwise might not have known about the practice.”
Caveats
“I find Twitter to be a bit addictive,” warns Crystal. “Therefore, I limit how much time I spend in this virtual world.”
“It is also extremely important that doctors not tweet personal information about patients without their consent. Sometimes I tweet the first name of the baby I just delivered (e.g., ‘Welcome to the world, Baby Jacob!’), but I always get consent first from both parents. Patient confidentiality and patient consent are paramount.”
For physicians on Twitter, what not to say, and do
Do not reveal HIPAA-protected information. In fact, be careful not to be too specific about your day. Don’t say “nasty case of gonorrhea this afternoon”; instead, if gonorrhea is on your mind, offer some statistics and a link to the Web site of the Centers for Disease Control and Prevention. You never know if that patient from “this afternoon,” or her mother, is following you.
Do not post a statement or picture that you wouldn’t want to see on the front page of a newspaper. In one study of medical students and residents who created an identity on Facebook, 70% had posted photographs of themselves with alcohol; in many of those photos, what was shown implied drinking to excess.5 Imagine the impact of that picture, poster-sized, when displayed to a jury at a malpractice trial….
Be wary of using Doc-speak. Your tweets, private or otherwise, are fair game for misinterpretation. Tweeting “Labor and delivery was crazy” may mean simply that there was a steady stream of patients and you didn’t get to eat dinner, but an attorney may, based on that statement, be able to convince a jury that L&D was understaffed.
Likewise, tweeting “Just finished a tough hysterectomy” may mean a complication-free laparoscopic procedure on an obese patient who had a 16-week-size uterus and dense adhesions but, to a jury, that might translate as, “I was in over my head and should have called for back-up.”
Don’t dispense medical advice. Ever. If people tweet you for advice, refer them to their physician in reply. Many physicians (including me) include a disclaimer in their Twitter biographical statement emphasizing that their tweets do not constitute medical advice.
Have you tried Twitter? Do you have a story to tell about it? Tweet me about it!—@DrJenGunter
Follow OBG ManaGeMent on Twitter: @obgmanagement.com
1. Fox S, Jones S. The social life of health information. Pew Internet & American Life Project. http://www.pewinternet.org/Reports/2009/8-The-Social-Life-of-Health-Information.aspx. Published June 11, 2009. Accessed June 1, 2010.
2. Fox S, Rainie L, Horrigan J, et al. The online health care revolution: how the Web helps Americans take better care of themselves. Pew Internet & American Life Project. http://www.pewinternet.org/Reports/2000/The-Online-Health-Care-Revolution.aspx. Published November 26, 2000. Accessed June 1, 2010.
3. How blogs and social media agendas relate and differ from the traditional press. Journalism.org Web site. http://www.journalism.org/node/20621. Published May 23, 2010. Accessed June 1, 2010.
4. Thompson LA, Dawson K, Ferdig R, et al. The intersection of online social networking with medical professionalism. J Gen Intern Med. 2008;23(7):954-957.
1. Fox S, Jones S. The social life of health information. Pew Internet & American Life Project. http://www.pewinternet.org/Reports/2009/8-The-Social-Life-of-Health-Information.aspx. Published June 11, 2009. Accessed June 1, 2010.
2. Fox S, Rainie L, Horrigan J, et al. The online health care revolution: how the Web helps Americans take better care of themselves. Pew Internet & American Life Project. http://www.pewinternet.org/Reports/2000/The-Online-Health-Care-Revolution.aspx. Published November 26, 2000. Accessed June 1, 2010.
3. How blogs and social media agendas relate and differ from the traditional press. Journalism.org Web site. http://www.journalism.org/node/20621. Published May 23, 2010. Accessed June 1, 2010.
4. Thompson LA, Dawson K, Ferdig R, et al. The intersection of online social networking with medical professionalism. J Gen Intern Med. 2008;23(7):954-957.