User login
Hospitalist Reviews on Healthcare-associated Infections, Mortality Benefit with Single Peripheral Pulmonary Emboli, Oral Anticoagulants to Treat Atrial Fibrillation
In This Edition
Literature At A Glance
A guide to this month’s studies
- Healthcare-associated infections financially impact the U.S. system
- No mortality benefit with treatment of single peripheral pulmonary emboli
- Modified (shorter) IV acetylcysteine infusion reduces adverse effects
- Comorbidities contribute to potentially avoidable hospital readmissions
- Resident handoff bundle reduces medical errors and adverse events, improves handoff quality
- Uncomplicated skin infections in the ambulatory setting commonly involve avoidable antibiotic exposure
- Warfarin initiation in atrial fibrillation associated with increased short-term risk of stroke
- Multifaceted discharge interventions reduce rates of pediatric readmission and post-hospital ED utilization
- Sepsis diagnoses are common, but many septic patients in ED do not receive antibiotics
- New oral anticoagulants safe, effective for atrial fibrillation treatment
Healthcare-Associated Infections Continue to Impact the U.S. Healthcare System Financially
Clinical question: What is the estimated cost of healthcare-associated infections (HAI) to the U.S. healthcare system?
Background: In spite of education efforts, HAIs occur frequently and contribute to high healthcare costs in the U.S. This study sought to estimate the costs of HAIs to the U.S. system using statistical analyses of published data.
Study design: Simulations of published data.
Setting: Published studies on five major HAIs.
Synopsis: Monte Carlo simulations based upon published point estimates were used to estimate per-case cost and confidence intervals, with extrapolation to total costs to the U.S. healthcare system. Overall, five major HAIs occur approximately 440,000 times annually and cost the healthcare system an estimated $9.78 billion (range $8.28 to $11.5 billion) in 2009.
Surgical site infections (36.0%) were the most common of the studied HAIs, with increased per-case cost of $20,785, equating to an estimated $3.30 billion annually (33.7% of total HAI costs). Clostridium difficile infection accounted for 30.3% of HAI but only 15.4% of costs ($1.51 billion). Central line-associated bloodstream infections were most costly per case ($45,814), with total costs of $1.85 billion (18.9% of costs). Ventilator-associated pneumonia accounted for $3.09 billion, or 31.7% of total costs. Catheter-associated urinary tract infection only represented 0.3% of total costs, or $27.9 million annually.
The authors suggest that changes in payment reform likely will drive hospitals to further invest in HAI reduction efforts.
Bottom line: HAIs remain frequent and expensive complications of hospitalization, in spite of improvement efforts to date.
Citation: Zimlichman E, Henderson D, Tamir O, et al. Health care-associated infections: a meta-analysis of costs and financial impact on the US health care system. JAMA Intern Med. 2013;173(22):2039-2046.
No Mortality Benefit with Treatment of Single Peripheral Pulmonary Emboli
Clinical question: Does treatment of single peripheral pulmonary emboli impact mortality and rates of post-discharge venous thromboembolism (VTE)?
Background: With the increase in CT pulmonary angiography (CTPA) use the past decade, there has been an increased rate of detection of peripheral filling defects. When confronted with a single peripheral filling defect (SPFD), clinicians face the dilemma of whether treatment is necessary, given the risks associated with anticoagulation.
Study design: Retrospective cohort.
Setting: Community teaching hospital in Norwalk, Conn.
Synopsis: A total of 4,906 CTPAs were screened, revealing 153 scans with an SPFD. Primary analysis included 134 patients 18 years or older. Of these patients, 61 (45.5%) received treatment with anticoagulation (n=51) or IVC filter alone (n=10).
This study revealed no difference in adjusted 90-day mortality between treated and untreated groups. No statistically significant difference was found in the rate of post-discharge VTE within 90 days.
Characteristics associated with treatment for SPFD were patient immobility, previous VTE, and radiology labeling the filling defect as a pulmonary embolus. It is important to note that none of the patients who had a normal second imaging study (e.g. V/Q scan or ultrasound) were treated; therefore, the use of secondary studies could mitigate some of the uncertainty around SPFD management, though this is not recommended in current diagnostic algorithms. Because this is a single-center study with a modest sample size, the comparability of findings to other centers might be limited. Larger studies are needed to help clarify these findings.
Bottom line: Treatment of SPFD was not associated with a difference in mortality or post-discharge VTE within 90 days.
Citation: Green O, Lempel J, Kolodziej A, et al. Treatment of single peripheral pulmonary emboli: patient outcomes and factors associated with decision to treat. J Hosp Med. 2014;9(1):42-47.
Modified IV Acetylcysteine Infusion Reduces Adverse Effects
Clinical question: Does a shorter regimen of IV acetylcysteine reduce adverse effects compared to the standard regimen?
Background: Acetaminophen poisoning is common, and recommended treatment is IV acetylcysteine; however, the standard regimen has many adverse effects, including vomiting and anaphylactoid reactions. Although studies have outlined these side effects, no published trials have compared their frequency to that of a shorter protocol.
Study design: Double-blinded, randomized controlled trial.
Setting: Three acute care hospitals in the United Kingdom.
Synopsis: Of 3,311 patients who presented with acetaminophen overdose, 222 underwent randomization to the standard (duration 20-25 hours) or modified (12 hours) acetylcysteine regimen, with or without pre-treatment with IV ondansetron 4 mg. The primary outcome of vomiting, retching, or need for rescue antiemetic treatment within two hours of acetylcysteine initiation was significantly less frequent in patients who received the shorter regimen, compared to those allocated to the standard regimen.
Specifically, the adjusted odds ratio was 0.26 with the modified regimen (97.5% CI, 0.13-0.52; P<0.0001). The primary outcome was significantly less in patients pre-treated with ondansetron compared to placebo (OR 0.41, 97.5% CI 0.2-0.8; P=0.003). Anaphylactic reactions were significantly reduced with the shorter protocol; no significant difference in hepatotoxicity was noted.
It is reasonable to infer that the shorter acetylcysteine regimen substantially reduces the frequency of vomiting and serious anaphylactoid reactions when compared with the standard schedule; however, hospitalists should note that this study was not powered to assess for non-inferiority of the shorter regimen with regard to prevention of acetaminophen’s hepatotoxic effects. Further studies are needed to confirm the efficacy and safety of the modified regimen before widespread adoption into clinical practice.
Bottom line: A shorter acetylcysteine regimen is associated with decreased occurrence of vomiting and anaphylactoid reactions compared to the standard protocol for treating acetaminophen toxicity. Additional research is needed to assess non-inferiority of this modified regimen for prevention of hepatotoxic effects.
Citation: Bateman DN, Dear JW, Thanacoody HK, et al. Reduction of adverse effects from intravenous acetylcysteine treatment for paracetamol poisoning: a randomized controlled trial. Lancet. 2014;383(9918):697-704.
Comorbidities Contribute to Potentially Avoidable Hospital Readmissions
Clinical question: What is the role of comorbidities in 30-day potentially avoidable readmissions?
Background: Higher comorbidity burden has been associated with 30-day readmissions. This study evaluated the role of comorbidities in the 30-day rate of potentially avoidable readmissions from a tertiary-care medical center.
Study design: Retrospective cohort.
Setting: Tertiary-care teaching hospital and affiliated network.
Synopsis: Investigators tested the hypothesis that comorbidities significantly contribute to 30-day, potentially avoidable readmissions in a cohort of consecutively discharged medical patients at an academic medical center over a 12-month period. Out of a total of 10,731 discharges, there were 2,398 readmissions to hospitals in the same health system. Of those 2,398 readmissions, 858 (35.8%) were judged potentially avoidable using a validated algorithm. Frequently, the reason for readmission was not related to the index discharge diagnosis but to a complication of known comorbidities.
The authors identified the top five diagnoses for readmission as infection, neoplasm, heart failure, gastrointestinal disorder, and liver disorder. Among those patients who had a readmission diagnosis different from the index-case discharge diagnosis, the comorbidities of neoplastic disease, heart failure, and chronic kidney disease significantly contributed to readmission as compared to those without similar comorbidities.
Bottom line: The reason for readmission often is not related to the index hospitalization diagnosis but, rather, to comorbidities present at the index episode of care; thus, attention to management of comorbidities in the post-discharge period is important in circumventing potentially avoidable readmissions.
Citation: Donzé J, Lipsitz S, Bates DW, Schnipper JL. Causes and patterns of readmissions in patients with common comorbidities: retrospective cohort study. BMJ. 2013;347:F7171.
Resident Handoff Bundle Reduces Medical Errors and Adverse Events, Improves Handoff Quality
Clinical question: In a pediatric inpatient setting, is the use of a handoff program associated with improved patient safety measures and handoff quality?
Background: Sentinel events related to errors in communication are a significant patient safety dilemma and an impetus for ongoing efforts to improve handoffs in postgraduate medical education. Various strategies to be incorporated into the handoff process have been suggested in the literature, but research is limited with regard to the relationship between handoffs and patient safety.
Study design: Prospective, pre-post study.
Setting: Academic, pediatric hospital in an urban setting.
Synopsis: Overall, 1,255 patient admissions (642 pre-/613 post-handoff intervention) were evaluated on two inpatient units during the periods of July 2009-September 2009 (pre-intervention) and November 2009-January 2010 (post-intervention). The intervention was a handoff “bundle” consisting of a standardized communication and handoff training session, a verbal mnemonic to standardize handoffs, and a new unified resident-intern handoff structure in a private, quiet setting. A computerized handoff tool was also added in one unit. Primary outcomes were a comparison of the rate of medical errors per 100 admissions and rates of preventable adverse events before and after the intervention.
Implementation of the bundle resulted in a significant decrease in medical errors (18.3 from 33.8 per 100 admissions, P<0.001) and preventable adverse events (1.5 from 3.3 per 100 admissions, P=0.04). Secondary outcomes included reductions in omissions of key data in the written handoff (even greater in the group using the computerized tool) and increased percentage of time spent in direct patient care, with no change in handoff duration. Additionally, handoffs were more likely to occur in a quiet, private location.
Limitations included the potential for confounding in a pre-post intervention design, the difficulty in ascertaining the value of the individual components of the bundle, and the potential lack of generalizability.
Bottom line: In a pediatric hospital setting, a multifaceted handoff bundle is associated with improved handoff quality and reductions in medical errors and preventable adverse events.
Citation: Starmer AJ, Sectish TC, Simon DW, et al. Rates of medical errors and preventable adverse events among hospitalized children following implementation of a resident handoff bundle. JAMA. 2013;310(21):2262-2270.
Uncomplicated Skin Infections in Ambulatory Setting Commonly Involve Avoidable Antibiotic Exposure
Clinical question: What are the current prescribing practices for antibiotics used to treat skin and soft tissue infections in the outpatient setting?
Background: Uncomplicated skin and soft tissue infections are among the most frequent indications for outpatient antibiotic use. Because antibiotic use is associated with bacterial resistance and adverse events, understanding antibiotic prescribing practices is necessary to minimize these types of complications.
Study design: Retrospective cohort.
Setting: Ambulatory care setting in the Denver Health System.
Synopsis: Data from 364 adults and children who presented to an ambulatory setting with a primary diagnosis of skin and soft tissue infection were analyzed using a stepwise multivariate logistic regression in order to determine factors associated with avoidable antibiotic exposure. Among cellulitis cases, 61% of patients were prescribed antibiotics to treat methicillin-resistant Staphylococcus aureus. Avoidable antibiotic exposure occurred in 46% of cases, including use of antibiotics with broad Gram-negative activity (4%), combination therapy (12%), and treatment for ≥10 days (42%). Use of short-course, single-antibiotic treatment approaches consistent with national guidelines would have reduced prescribed antibiotic days by 19%, to 55%.
Bottom line: Avoidable antibiotic exposure frequently occurs in the treatment of uncomplicated skin infections; using short-course, single-antibiotic treatment strategies could significantly reduce total antibiotic use.
Citation: Hurley HJ, Knepper BC, Price CS, Mehler PS, Burman WJ, Jenkins TC. Avoidable antibiotic exposure for uncomplicated skin and soft tissue infections in the ambulatory care setting. Am J Med. 2013;126(12):1099-1106.
Warfarin Initiation in Atrial Fibrillation Associated with Increased Short-Term Risk of Stroke
Clinical question: Is the initiation of warfarin associated with an increased risk of ischemic stroke in patients with atrial fibrillation (Afib)?
Background: Two Afib trials of oral factor Xa inhibitors showed an increased risk of stroke when patients were transitioned to open label warfarin at the end of the study. Warfarin can, theoretically, lead to a transient hypercoagulable state upon treatment initiation, so further study is indicated to determine if the initiation of warfarin is associated with increased stroke risk among Afib patients.
Study design: Population-based, nested case-control.
Setting: UK Clinical Practice Research Datalink.
Synopsis: A cohort of 70,766 patients with newly diagnosed Afib was identified from a large primary care database. Conditional logistic regression was used to estimate adjusted rate ratios (RR) of stroke associated with warfarin monotherapy, classified according to time since initiation of treatment when compared to patients not on antithrombotic therapy.
Warfarin was associated with a 71% increased risk of stroke in the first 30 days of use (RR 1.71, 95% CI 1.39-2.12). Risk was highest in the first week of warfarin treatment, which is consistent with the known transient pro-coagulant effect of warfarin. Decreased risks were observed with warfarin initiation >30 days before the ischemic event (31-90 days: RR 0.50, 95% CI 0.34-0.75; >90 days: RR 0.55, 95% CI 0.50-0.61).
Limitations included the extraction of data from a database, which could lead to misclassification of diagnosis or therapy, and the observational nature of the study.
Bottom line: There may be an increased risk of ischemic stroke during the first 30 days of treatment with warfarin in patients with Afib.
Citation: Azoulay L, Dell-Aniello S, Simon T, Renoux C, Suissa S. Initiation of warfarin in patients with atrial fibrillation: early effects on ischaemic strokes [published online ahead of print December 18, 2013]. Eur Heart J.
Multifaceted Discharge Interventions Reduce Rates of Pediatric Readmission and Post-Hospital ED Utilization
Clinical question: Do interventions at discharge reduce the rate of readmissions and post-hospitalization ED visits among pediatric patients?
Background: Readmissions are a high-priority quality measure in both the adult and pediatric settings. Although a broadening body of literature is evaluating the impact of interventions on readmissions in adult populations, the literature does not contain a similar breadth of assessments of interventions in the pediatric setting.
Study design: Systematic review.
Setting: English-language articles studying pediatric inpatient discharge interventions.
Synopsis: A total of 1,296 unique articles were identified from PubMed and the Cumulative Index to Nursing and Allied Health Literature. Additional articles were identified on review of references, yielding 14 articles that met inclusion criteria. Included studies evaluated the effect of pediatric discharge interventions on the primary outcomes of hospital readmission or post-hospitalization ED visits. Interventions focused on three main patient populations: asthma, cancer, and prematurity.
Six studies demonstrated statistically significant reductions in readmissions and/or ED visits, while two studies actually demonstrated an increase in post-discharge utilization. All successful interventions began in the inpatient setting and were multifaceted, with four of six studies including an educational component and a post-discharge follow-up component.
While all of the studies evaluated sought to enhance the transitional care from the inpatient to outpatient setting, only the interventions that included one responsible party (individual or team) with expertise in the medical condition providing oversight and support were successful in reducing the specified outcomes. A significant limitation was that many of the studies identified were not sufficiently powered to detect either outcome of interest.
Bottom line: A multifaceted intervention involving educational and post-discharge follow-up components with an experienced individual or team supporting the transition is associated with a reduction in hospital readmissions and post-discharge ED utilization.
Citation: Auger KA, Kenyon CC, Feudtner C, Davis MM. Pediatric hospital discharge interventions to reduce subsequent utilization: a systematic review [published online ahead of print December 20, 2013]. J Hosp Med.
Sepsis Diagnoses Are Common in ED, but Many Septic Patients in the ED Do Not Receive Antibiotics
Clinical question: Has the frequency of sepsis rates, along with administration of antibiotics in U.S. emergency departments (EDs), changed over time?
Background: Prior studies reviewing discharge data from hospitals suggest an increase of sepsis over time; however, little epidemiological research has evaluated the diagnosis of sepsis and antibiotic use in ED settings.
Study design: Retrospective, four-stage probability sample.
Setting: National Hospital Ambulatory Medical Care Survey (NHAMCS).
Synopsis: The NHAMCS includes a sample of all U.S. ED visits, except federal, military, and VA hospitals. According to NHAMCS data, an estimated 1.3 billion visits by adults to U.S. EDs occurred from 1994-2009, or approximately 81 million visits per year. Explicit sepsis was defined by the presence of the following, with ICD-9 codes: septicemia (038), sepsis (995.91), severe sepsis (995.92), or septic shock (785.52). Implicit sepsis was defined as a code indicating infection plus a code indicting organ dysfunction.
In U.S. EDs, explicit sepsis did not become more prevalent from 1994-2009; however, implicitly diagnosed sepsis increased by 7% every two years. There were 260,000 explicit sepsis-related ED visits per year, or 1.23 visits per 1,000 U.S. population. In-hospital mortality was 17% and 9% for the explicit and implicit diagnosis groups, respectively. On review of the explicit sepsis group, only 61% of the patients were found to have received antibiotics in the ED. The rate did increase over the time studied, from 52% in 1994-1997 to 69% in 2006-2009.
The study was limited by the retrospective analysis of data not designed to track sepsis or antibiotic use.
Bottom Line: Explicitly recognized sepsis remained stable in the ED setting from 1994-2009, and early antibiotic use has improved during this time, but there is still much opportunity for improvement.
Citation: Filbin MR, Arias SA, Camargo CA Jr, Barche A, Pallin DJ. Sepsis visits and antibiotic utilization in the U.S. emergency departments. Crit Care Med. 2014;42(3):528-535.
New Oral Anticoagulants Safe and Effective for Atrial Fibrillation Treatment
Clinical question: Is there a difference in efficacy and safety among new oral anticoagulants compared to warfarin in subgroups of patients with atrial fibrillation (Afib)?
Background: Studies of new oral anticoagulants have demonstrated that these agents are at least as safe and effective as warfarin for prevention of stroke and systemic embolism in Afib. This study was designed to look at available phase 3 randomized trials, with the goal of subgroup analysis for both efficacy and bleeding risks.
Study design: Meta-analysis.
Setting: Phase 3 randomized controlled trials of patients with Afib.
Synopsis: The analysis included four trials of Afib patients randomized to receive warfarin or a novel oral anticoagulant (NOAC), including dabigatran, rivaroxaban, apixaban, and edoxaban. In total, 42,411 patients received an NOAC and 29,272 patients received warfarin. Separate analyses were performed for high-dose and low-dose NOACs.
The high-dose NOAC demonstrated a 19% reduction in stroke and systemic embolic events as compared to warfarin, largely due to the reduction of hemorrhagic strokes by the NOAC. The low-dose NOAC showed similar efficacy to warfarin for reduction of stroke and systemic embolic events, with an increase noted in the subset of ischemic stroke in low-dose NOAC. Both doses of NOAC demonstrated a significant reduction in all-cause mortality. NOAC showed a non-significant reduction in bleeding compared to warfarin; however, subset analysis demonstrated an increase in gastrointestinal bleeding with high-dose NOAC and a significant reduction in intracranial hemorrhage with low-dose NOAC.
A notable limitation of the study is that it only included clinical trials in the analysis.
Bottom line: In relation to stroke, systemic embolic events, and all-cause mortality, new oral anticoagulants showed a favorable efficacy and safety profile as compared to warfarin in Afib patients.
Citation: Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383(9921):955-962.
In This Edition
Literature At A Glance
A guide to this month’s studies
- Healthcare-associated infections financially impact the U.S. system
- No mortality benefit with treatment of single peripheral pulmonary emboli
- Modified (shorter) IV acetylcysteine infusion reduces adverse effects
- Comorbidities contribute to potentially avoidable hospital readmissions
- Resident handoff bundle reduces medical errors and adverse events, improves handoff quality
- Uncomplicated skin infections in the ambulatory setting commonly involve avoidable antibiotic exposure
- Warfarin initiation in atrial fibrillation associated with increased short-term risk of stroke
- Multifaceted discharge interventions reduce rates of pediatric readmission and post-hospital ED utilization
- Sepsis diagnoses are common, but many septic patients in ED do not receive antibiotics
- New oral anticoagulants safe, effective for atrial fibrillation treatment
Healthcare-Associated Infections Continue to Impact the U.S. Healthcare System Financially
Clinical question: What is the estimated cost of healthcare-associated infections (HAI) to the U.S. healthcare system?
Background: In spite of education efforts, HAIs occur frequently and contribute to high healthcare costs in the U.S. This study sought to estimate the costs of HAIs to the U.S. system using statistical analyses of published data.
Study design: Simulations of published data.
Setting: Published studies on five major HAIs.
Synopsis: Monte Carlo simulations based upon published point estimates were used to estimate per-case cost and confidence intervals, with extrapolation to total costs to the U.S. healthcare system. Overall, five major HAIs occur approximately 440,000 times annually and cost the healthcare system an estimated $9.78 billion (range $8.28 to $11.5 billion) in 2009.
Surgical site infections (36.0%) were the most common of the studied HAIs, with increased per-case cost of $20,785, equating to an estimated $3.30 billion annually (33.7% of total HAI costs). Clostridium difficile infection accounted for 30.3% of HAI but only 15.4% of costs ($1.51 billion). Central line-associated bloodstream infections were most costly per case ($45,814), with total costs of $1.85 billion (18.9% of costs). Ventilator-associated pneumonia accounted for $3.09 billion, or 31.7% of total costs. Catheter-associated urinary tract infection only represented 0.3% of total costs, or $27.9 million annually.
The authors suggest that changes in payment reform likely will drive hospitals to further invest in HAI reduction efforts.
Bottom line: HAIs remain frequent and expensive complications of hospitalization, in spite of improvement efforts to date.
Citation: Zimlichman E, Henderson D, Tamir O, et al. Health care-associated infections: a meta-analysis of costs and financial impact on the US health care system. JAMA Intern Med. 2013;173(22):2039-2046.
No Mortality Benefit with Treatment of Single Peripheral Pulmonary Emboli
Clinical question: Does treatment of single peripheral pulmonary emboli impact mortality and rates of post-discharge venous thromboembolism (VTE)?
Background: With the increase in CT pulmonary angiography (CTPA) use the past decade, there has been an increased rate of detection of peripheral filling defects. When confronted with a single peripheral filling defect (SPFD), clinicians face the dilemma of whether treatment is necessary, given the risks associated with anticoagulation.
Study design: Retrospective cohort.
Setting: Community teaching hospital in Norwalk, Conn.
Synopsis: A total of 4,906 CTPAs were screened, revealing 153 scans with an SPFD. Primary analysis included 134 patients 18 years or older. Of these patients, 61 (45.5%) received treatment with anticoagulation (n=51) or IVC filter alone (n=10).
This study revealed no difference in adjusted 90-day mortality between treated and untreated groups. No statistically significant difference was found in the rate of post-discharge VTE within 90 days.
Characteristics associated with treatment for SPFD were patient immobility, previous VTE, and radiology labeling the filling defect as a pulmonary embolus. It is important to note that none of the patients who had a normal second imaging study (e.g. V/Q scan or ultrasound) were treated; therefore, the use of secondary studies could mitigate some of the uncertainty around SPFD management, though this is not recommended in current diagnostic algorithms. Because this is a single-center study with a modest sample size, the comparability of findings to other centers might be limited. Larger studies are needed to help clarify these findings.
Bottom line: Treatment of SPFD was not associated with a difference in mortality or post-discharge VTE within 90 days.
Citation: Green O, Lempel J, Kolodziej A, et al. Treatment of single peripheral pulmonary emboli: patient outcomes and factors associated with decision to treat. J Hosp Med. 2014;9(1):42-47.
Modified IV Acetylcysteine Infusion Reduces Adverse Effects
Clinical question: Does a shorter regimen of IV acetylcysteine reduce adverse effects compared to the standard regimen?
Background: Acetaminophen poisoning is common, and recommended treatment is IV acetylcysteine; however, the standard regimen has many adverse effects, including vomiting and anaphylactoid reactions. Although studies have outlined these side effects, no published trials have compared their frequency to that of a shorter protocol.
Study design: Double-blinded, randomized controlled trial.
Setting: Three acute care hospitals in the United Kingdom.
Synopsis: Of 3,311 patients who presented with acetaminophen overdose, 222 underwent randomization to the standard (duration 20-25 hours) or modified (12 hours) acetylcysteine regimen, with or without pre-treatment with IV ondansetron 4 mg. The primary outcome of vomiting, retching, or need for rescue antiemetic treatment within two hours of acetylcysteine initiation was significantly less frequent in patients who received the shorter regimen, compared to those allocated to the standard regimen.
Specifically, the adjusted odds ratio was 0.26 with the modified regimen (97.5% CI, 0.13-0.52; P<0.0001). The primary outcome was significantly less in patients pre-treated with ondansetron compared to placebo (OR 0.41, 97.5% CI 0.2-0.8; P=0.003). Anaphylactic reactions were significantly reduced with the shorter protocol; no significant difference in hepatotoxicity was noted.
It is reasonable to infer that the shorter acetylcysteine regimen substantially reduces the frequency of vomiting and serious anaphylactoid reactions when compared with the standard schedule; however, hospitalists should note that this study was not powered to assess for non-inferiority of the shorter regimen with regard to prevention of acetaminophen’s hepatotoxic effects. Further studies are needed to confirm the efficacy and safety of the modified regimen before widespread adoption into clinical practice.
Bottom line: A shorter acetylcysteine regimen is associated with decreased occurrence of vomiting and anaphylactoid reactions compared to the standard protocol for treating acetaminophen toxicity. Additional research is needed to assess non-inferiority of this modified regimen for prevention of hepatotoxic effects.
Citation: Bateman DN, Dear JW, Thanacoody HK, et al. Reduction of adverse effects from intravenous acetylcysteine treatment for paracetamol poisoning: a randomized controlled trial. Lancet. 2014;383(9918):697-704.
Comorbidities Contribute to Potentially Avoidable Hospital Readmissions
Clinical question: What is the role of comorbidities in 30-day potentially avoidable readmissions?
Background: Higher comorbidity burden has been associated with 30-day readmissions. This study evaluated the role of comorbidities in the 30-day rate of potentially avoidable readmissions from a tertiary-care medical center.
Study design: Retrospective cohort.
Setting: Tertiary-care teaching hospital and affiliated network.
Synopsis: Investigators tested the hypothesis that comorbidities significantly contribute to 30-day, potentially avoidable readmissions in a cohort of consecutively discharged medical patients at an academic medical center over a 12-month period. Out of a total of 10,731 discharges, there were 2,398 readmissions to hospitals in the same health system. Of those 2,398 readmissions, 858 (35.8%) were judged potentially avoidable using a validated algorithm. Frequently, the reason for readmission was not related to the index discharge diagnosis but to a complication of known comorbidities.
The authors identified the top five diagnoses for readmission as infection, neoplasm, heart failure, gastrointestinal disorder, and liver disorder. Among those patients who had a readmission diagnosis different from the index-case discharge diagnosis, the comorbidities of neoplastic disease, heart failure, and chronic kidney disease significantly contributed to readmission as compared to those without similar comorbidities.
Bottom line: The reason for readmission often is not related to the index hospitalization diagnosis but, rather, to comorbidities present at the index episode of care; thus, attention to management of comorbidities in the post-discharge period is important in circumventing potentially avoidable readmissions.
Citation: Donzé J, Lipsitz S, Bates DW, Schnipper JL. Causes and patterns of readmissions in patients with common comorbidities: retrospective cohort study. BMJ. 2013;347:F7171.
Resident Handoff Bundle Reduces Medical Errors and Adverse Events, Improves Handoff Quality
Clinical question: In a pediatric inpatient setting, is the use of a handoff program associated with improved patient safety measures and handoff quality?
Background: Sentinel events related to errors in communication are a significant patient safety dilemma and an impetus for ongoing efforts to improve handoffs in postgraduate medical education. Various strategies to be incorporated into the handoff process have been suggested in the literature, but research is limited with regard to the relationship between handoffs and patient safety.
Study design: Prospective, pre-post study.
Setting: Academic, pediatric hospital in an urban setting.
Synopsis: Overall, 1,255 patient admissions (642 pre-/613 post-handoff intervention) were evaluated on two inpatient units during the periods of July 2009-September 2009 (pre-intervention) and November 2009-January 2010 (post-intervention). The intervention was a handoff “bundle” consisting of a standardized communication and handoff training session, a verbal mnemonic to standardize handoffs, and a new unified resident-intern handoff structure in a private, quiet setting. A computerized handoff tool was also added in one unit. Primary outcomes were a comparison of the rate of medical errors per 100 admissions and rates of preventable adverse events before and after the intervention.
Implementation of the bundle resulted in a significant decrease in medical errors (18.3 from 33.8 per 100 admissions, P<0.001) and preventable adverse events (1.5 from 3.3 per 100 admissions, P=0.04). Secondary outcomes included reductions in omissions of key data in the written handoff (even greater in the group using the computerized tool) and increased percentage of time spent in direct patient care, with no change in handoff duration. Additionally, handoffs were more likely to occur in a quiet, private location.
Limitations included the potential for confounding in a pre-post intervention design, the difficulty in ascertaining the value of the individual components of the bundle, and the potential lack of generalizability.
Bottom line: In a pediatric hospital setting, a multifaceted handoff bundle is associated with improved handoff quality and reductions in medical errors and preventable adverse events.
Citation: Starmer AJ, Sectish TC, Simon DW, et al. Rates of medical errors and preventable adverse events among hospitalized children following implementation of a resident handoff bundle. JAMA. 2013;310(21):2262-2270.
Uncomplicated Skin Infections in Ambulatory Setting Commonly Involve Avoidable Antibiotic Exposure
Clinical question: What are the current prescribing practices for antibiotics used to treat skin and soft tissue infections in the outpatient setting?
Background: Uncomplicated skin and soft tissue infections are among the most frequent indications for outpatient antibiotic use. Because antibiotic use is associated with bacterial resistance and adverse events, understanding antibiotic prescribing practices is necessary to minimize these types of complications.
Study design: Retrospective cohort.
Setting: Ambulatory care setting in the Denver Health System.
Synopsis: Data from 364 adults and children who presented to an ambulatory setting with a primary diagnosis of skin and soft tissue infection were analyzed using a stepwise multivariate logistic regression in order to determine factors associated with avoidable antibiotic exposure. Among cellulitis cases, 61% of patients were prescribed antibiotics to treat methicillin-resistant Staphylococcus aureus. Avoidable antibiotic exposure occurred in 46% of cases, including use of antibiotics with broad Gram-negative activity (4%), combination therapy (12%), and treatment for ≥10 days (42%). Use of short-course, single-antibiotic treatment approaches consistent with national guidelines would have reduced prescribed antibiotic days by 19%, to 55%.
Bottom line: Avoidable antibiotic exposure frequently occurs in the treatment of uncomplicated skin infections; using short-course, single-antibiotic treatment strategies could significantly reduce total antibiotic use.
Citation: Hurley HJ, Knepper BC, Price CS, Mehler PS, Burman WJ, Jenkins TC. Avoidable antibiotic exposure for uncomplicated skin and soft tissue infections in the ambulatory care setting. Am J Med. 2013;126(12):1099-1106.
Warfarin Initiation in Atrial Fibrillation Associated with Increased Short-Term Risk of Stroke
Clinical question: Is the initiation of warfarin associated with an increased risk of ischemic stroke in patients with atrial fibrillation (Afib)?
Background: Two Afib trials of oral factor Xa inhibitors showed an increased risk of stroke when patients were transitioned to open label warfarin at the end of the study. Warfarin can, theoretically, lead to a transient hypercoagulable state upon treatment initiation, so further study is indicated to determine if the initiation of warfarin is associated with increased stroke risk among Afib patients.
Study design: Population-based, nested case-control.
Setting: UK Clinical Practice Research Datalink.
Synopsis: A cohort of 70,766 patients with newly diagnosed Afib was identified from a large primary care database. Conditional logistic regression was used to estimate adjusted rate ratios (RR) of stroke associated with warfarin monotherapy, classified according to time since initiation of treatment when compared to patients not on antithrombotic therapy.
Warfarin was associated with a 71% increased risk of stroke in the first 30 days of use (RR 1.71, 95% CI 1.39-2.12). Risk was highest in the first week of warfarin treatment, which is consistent with the known transient pro-coagulant effect of warfarin. Decreased risks were observed with warfarin initiation >30 days before the ischemic event (31-90 days: RR 0.50, 95% CI 0.34-0.75; >90 days: RR 0.55, 95% CI 0.50-0.61).
Limitations included the extraction of data from a database, which could lead to misclassification of diagnosis or therapy, and the observational nature of the study.
Bottom line: There may be an increased risk of ischemic stroke during the first 30 days of treatment with warfarin in patients with Afib.
Citation: Azoulay L, Dell-Aniello S, Simon T, Renoux C, Suissa S. Initiation of warfarin in patients with atrial fibrillation: early effects on ischaemic strokes [published online ahead of print December 18, 2013]. Eur Heart J.
Multifaceted Discharge Interventions Reduce Rates of Pediatric Readmission and Post-Hospital ED Utilization
Clinical question: Do interventions at discharge reduce the rate of readmissions and post-hospitalization ED visits among pediatric patients?
Background: Readmissions are a high-priority quality measure in both the adult and pediatric settings. Although a broadening body of literature is evaluating the impact of interventions on readmissions in adult populations, the literature does not contain a similar breadth of assessments of interventions in the pediatric setting.
Study design: Systematic review.
Setting: English-language articles studying pediatric inpatient discharge interventions.
Synopsis: A total of 1,296 unique articles were identified from PubMed and the Cumulative Index to Nursing and Allied Health Literature. Additional articles were identified on review of references, yielding 14 articles that met inclusion criteria. Included studies evaluated the effect of pediatric discharge interventions on the primary outcomes of hospital readmission or post-hospitalization ED visits. Interventions focused on three main patient populations: asthma, cancer, and prematurity.
Six studies demonstrated statistically significant reductions in readmissions and/or ED visits, while two studies actually demonstrated an increase in post-discharge utilization. All successful interventions began in the inpatient setting and were multifaceted, with four of six studies including an educational component and a post-discharge follow-up component.
While all of the studies evaluated sought to enhance the transitional care from the inpatient to outpatient setting, only the interventions that included one responsible party (individual or team) with expertise in the medical condition providing oversight and support were successful in reducing the specified outcomes. A significant limitation was that many of the studies identified were not sufficiently powered to detect either outcome of interest.
Bottom line: A multifaceted intervention involving educational and post-discharge follow-up components with an experienced individual or team supporting the transition is associated with a reduction in hospital readmissions and post-discharge ED utilization.
Citation: Auger KA, Kenyon CC, Feudtner C, Davis MM. Pediatric hospital discharge interventions to reduce subsequent utilization: a systematic review [published online ahead of print December 20, 2013]. J Hosp Med.
Sepsis Diagnoses Are Common in ED, but Many Septic Patients in the ED Do Not Receive Antibiotics
Clinical question: Has the frequency of sepsis rates, along with administration of antibiotics in U.S. emergency departments (EDs), changed over time?
Background: Prior studies reviewing discharge data from hospitals suggest an increase of sepsis over time; however, little epidemiological research has evaluated the diagnosis of sepsis and antibiotic use in ED settings.
Study design: Retrospective, four-stage probability sample.
Setting: National Hospital Ambulatory Medical Care Survey (NHAMCS).
Synopsis: The NHAMCS includes a sample of all U.S. ED visits, except federal, military, and VA hospitals. According to NHAMCS data, an estimated 1.3 billion visits by adults to U.S. EDs occurred from 1994-2009, or approximately 81 million visits per year. Explicit sepsis was defined by the presence of the following, with ICD-9 codes: septicemia (038), sepsis (995.91), severe sepsis (995.92), or septic shock (785.52). Implicit sepsis was defined as a code indicating infection plus a code indicting organ dysfunction.
In U.S. EDs, explicit sepsis did not become more prevalent from 1994-2009; however, implicitly diagnosed sepsis increased by 7% every two years. There were 260,000 explicit sepsis-related ED visits per year, or 1.23 visits per 1,000 U.S. population. In-hospital mortality was 17% and 9% for the explicit and implicit diagnosis groups, respectively. On review of the explicit sepsis group, only 61% of the patients were found to have received antibiotics in the ED. The rate did increase over the time studied, from 52% in 1994-1997 to 69% in 2006-2009.
The study was limited by the retrospective analysis of data not designed to track sepsis or antibiotic use.
Bottom Line: Explicitly recognized sepsis remained stable in the ED setting from 1994-2009, and early antibiotic use has improved during this time, but there is still much opportunity for improvement.
Citation: Filbin MR, Arias SA, Camargo CA Jr, Barche A, Pallin DJ. Sepsis visits and antibiotic utilization in the U.S. emergency departments. Crit Care Med. 2014;42(3):528-535.
New Oral Anticoagulants Safe and Effective for Atrial Fibrillation Treatment
Clinical question: Is there a difference in efficacy and safety among new oral anticoagulants compared to warfarin in subgroups of patients with atrial fibrillation (Afib)?
Background: Studies of new oral anticoagulants have demonstrated that these agents are at least as safe and effective as warfarin for prevention of stroke and systemic embolism in Afib. This study was designed to look at available phase 3 randomized trials, with the goal of subgroup analysis for both efficacy and bleeding risks.
Study design: Meta-analysis.
Setting: Phase 3 randomized controlled trials of patients with Afib.
Synopsis: The analysis included four trials of Afib patients randomized to receive warfarin or a novel oral anticoagulant (NOAC), including dabigatran, rivaroxaban, apixaban, and edoxaban. In total, 42,411 patients received an NOAC and 29,272 patients received warfarin. Separate analyses were performed for high-dose and low-dose NOACs.
The high-dose NOAC demonstrated a 19% reduction in stroke and systemic embolic events as compared to warfarin, largely due to the reduction of hemorrhagic strokes by the NOAC. The low-dose NOAC showed similar efficacy to warfarin for reduction of stroke and systemic embolic events, with an increase noted in the subset of ischemic stroke in low-dose NOAC. Both doses of NOAC demonstrated a significant reduction in all-cause mortality. NOAC showed a non-significant reduction in bleeding compared to warfarin; however, subset analysis demonstrated an increase in gastrointestinal bleeding with high-dose NOAC and a significant reduction in intracranial hemorrhage with low-dose NOAC.
A notable limitation of the study is that it only included clinical trials in the analysis.
Bottom line: In relation to stroke, systemic embolic events, and all-cause mortality, new oral anticoagulants showed a favorable efficacy and safety profile as compared to warfarin in Afib patients.
Citation: Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383(9921):955-962.
In This Edition
Literature At A Glance
A guide to this month’s studies
- Healthcare-associated infections financially impact the U.S. system
- No mortality benefit with treatment of single peripheral pulmonary emboli
- Modified (shorter) IV acetylcysteine infusion reduces adverse effects
- Comorbidities contribute to potentially avoidable hospital readmissions
- Resident handoff bundle reduces medical errors and adverse events, improves handoff quality
- Uncomplicated skin infections in the ambulatory setting commonly involve avoidable antibiotic exposure
- Warfarin initiation in atrial fibrillation associated with increased short-term risk of stroke
- Multifaceted discharge interventions reduce rates of pediatric readmission and post-hospital ED utilization
- Sepsis diagnoses are common, but many septic patients in ED do not receive antibiotics
- New oral anticoagulants safe, effective for atrial fibrillation treatment
Healthcare-Associated Infections Continue to Impact the U.S. Healthcare System Financially
Clinical question: What is the estimated cost of healthcare-associated infections (HAI) to the U.S. healthcare system?
Background: In spite of education efforts, HAIs occur frequently and contribute to high healthcare costs in the U.S. This study sought to estimate the costs of HAIs to the U.S. system using statistical analyses of published data.
Study design: Simulations of published data.
Setting: Published studies on five major HAIs.
Synopsis: Monte Carlo simulations based upon published point estimates were used to estimate per-case cost and confidence intervals, with extrapolation to total costs to the U.S. healthcare system. Overall, five major HAIs occur approximately 440,000 times annually and cost the healthcare system an estimated $9.78 billion (range $8.28 to $11.5 billion) in 2009.
Surgical site infections (36.0%) were the most common of the studied HAIs, with increased per-case cost of $20,785, equating to an estimated $3.30 billion annually (33.7% of total HAI costs). Clostridium difficile infection accounted for 30.3% of HAI but only 15.4% of costs ($1.51 billion). Central line-associated bloodstream infections were most costly per case ($45,814), with total costs of $1.85 billion (18.9% of costs). Ventilator-associated pneumonia accounted for $3.09 billion, or 31.7% of total costs. Catheter-associated urinary tract infection only represented 0.3% of total costs, or $27.9 million annually.
The authors suggest that changes in payment reform likely will drive hospitals to further invest in HAI reduction efforts.
Bottom line: HAIs remain frequent and expensive complications of hospitalization, in spite of improvement efforts to date.
Citation: Zimlichman E, Henderson D, Tamir O, et al. Health care-associated infections: a meta-analysis of costs and financial impact on the US health care system. JAMA Intern Med. 2013;173(22):2039-2046.
No Mortality Benefit with Treatment of Single Peripheral Pulmonary Emboli
Clinical question: Does treatment of single peripheral pulmonary emboli impact mortality and rates of post-discharge venous thromboembolism (VTE)?
Background: With the increase in CT pulmonary angiography (CTPA) use the past decade, there has been an increased rate of detection of peripheral filling defects. When confronted with a single peripheral filling defect (SPFD), clinicians face the dilemma of whether treatment is necessary, given the risks associated with anticoagulation.
Study design: Retrospective cohort.
Setting: Community teaching hospital in Norwalk, Conn.
Synopsis: A total of 4,906 CTPAs were screened, revealing 153 scans with an SPFD. Primary analysis included 134 patients 18 years or older. Of these patients, 61 (45.5%) received treatment with anticoagulation (n=51) or IVC filter alone (n=10).
This study revealed no difference in adjusted 90-day mortality between treated and untreated groups. No statistically significant difference was found in the rate of post-discharge VTE within 90 days.
Characteristics associated with treatment for SPFD were patient immobility, previous VTE, and radiology labeling the filling defect as a pulmonary embolus. It is important to note that none of the patients who had a normal second imaging study (e.g. V/Q scan or ultrasound) were treated; therefore, the use of secondary studies could mitigate some of the uncertainty around SPFD management, though this is not recommended in current diagnostic algorithms. Because this is a single-center study with a modest sample size, the comparability of findings to other centers might be limited. Larger studies are needed to help clarify these findings.
Bottom line: Treatment of SPFD was not associated with a difference in mortality or post-discharge VTE within 90 days.
Citation: Green O, Lempel J, Kolodziej A, et al. Treatment of single peripheral pulmonary emboli: patient outcomes and factors associated with decision to treat. J Hosp Med. 2014;9(1):42-47.
Modified IV Acetylcysteine Infusion Reduces Adverse Effects
Clinical question: Does a shorter regimen of IV acetylcysteine reduce adverse effects compared to the standard regimen?
Background: Acetaminophen poisoning is common, and recommended treatment is IV acetylcysteine; however, the standard regimen has many adverse effects, including vomiting and anaphylactoid reactions. Although studies have outlined these side effects, no published trials have compared their frequency to that of a shorter protocol.
Study design: Double-blinded, randomized controlled trial.
Setting: Three acute care hospitals in the United Kingdom.
Synopsis: Of 3,311 patients who presented with acetaminophen overdose, 222 underwent randomization to the standard (duration 20-25 hours) or modified (12 hours) acetylcysteine regimen, with or without pre-treatment with IV ondansetron 4 mg. The primary outcome of vomiting, retching, or need for rescue antiemetic treatment within two hours of acetylcysteine initiation was significantly less frequent in patients who received the shorter regimen, compared to those allocated to the standard regimen.
Specifically, the adjusted odds ratio was 0.26 with the modified regimen (97.5% CI, 0.13-0.52; P<0.0001). The primary outcome was significantly less in patients pre-treated with ondansetron compared to placebo (OR 0.41, 97.5% CI 0.2-0.8; P=0.003). Anaphylactic reactions were significantly reduced with the shorter protocol; no significant difference in hepatotoxicity was noted.
It is reasonable to infer that the shorter acetylcysteine regimen substantially reduces the frequency of vomiting and serious anaphylactoid reactions when compared with the standard schedule; however, hospitalists should note that this study was not powered to assess for non-inferiority of the shorter regimen with regard to prevention of acetaminophen’s hepatotoxic effects. Further studies are needed to confirm the efficacy and safety of the modified regimen before widespread adoption into clinical practice.
Bottom line: A shorter acetylcysteine regimen is associated with decreased occurrence of vomiting and anaphylactoid reactions compared to the standard protocol for treating acetaminophen toxicity. Additional research is needed to assess non-inferiority of this modified regimen for prevention of hepatotoxic effects.
Citation: Bateman DN, Dear JW, Thanacoody HK, et al. Reduction of adverse effects from intravenous acetylcysteine treatment for paracetamol poisoning: a randomized controlled trial. Lancet. 2014;383(9918):697-704.
Comorbidities Contribute to Potentially Avoidable Hospital Readmissions
Clinical question: What is the role of comorbidities in 30-day potentially avoidable readmissions?
Background: Higher comorbidity burden has been associated with 30-day readmissions. This study evaluated the role of comorbidities in the 30-day rate of potentially avoidable readmissions from a tertiary-care medical center.
Study design: Retrospective cohort.
Setting: Tertiary-care teaching hospital and affiliated network.
Synopsis: Investigators tested the hypothesis that comorbidities significantly contribute to 30-day, potentially avoidable readmissions in a cohort of consecutively discharged medical patients at an academic medical center over a 12-month period. Out of a total of 10,731 discharges, there were 2,398 readmissions to hospitals in the same health system. Of those 2,398 readmissions, 858 (35.8%) were judged potentially avoidable using a validated algorithm. Frequently, the reason for readmission was not related to the index discharge diagnosis but to a complication of known comorbidities.
The authors identified the top five diagnoses for readmission as infection, neoplasm, heart failure, gastrointestinal disorder, and liver disorder. Among those patients who had a readmission diagnosis different from the index-case discharge diagnosis, the comorbidities of neoplastic disease, heart failure, and chronic kidney disease significantly contributed to readmission as compared to those without similar comorbidities.
Bottom line: The reason for readmission often is not related to the index hospitalization diagnosis but, rather, to comorbidities present at the index episode of care; thus, attention to management of comorbidities in the post-discharge period is important in circumventing potentially avoidable readmissions.
Citation: Donzé J, Lipsitz S, Bates DW, Schnipper JL. Causes and patterns of readmissions in patients with common comorbidities: retrospective cohort study. BMJ. 2013;347:F7171.
Resident Handoff Bundle Reduces Medical Errors and Adverse Events, Improves Handoff Quality
Clinical question: In a pediatric inpatient setting, is the use of a handoff program associated with improved patient safety measures and handoff quality?
Background: Sentinel events related to errors in communication are a significant patient safety dilemma and an impetus for ongoing efforts to improve handoffs in postgraduate medical education. Various strategies to be incorporated into the handoff process have been suggested in the literature, but research is limited with regard to the relationship between handoffs and patient safety.
Study design: Prospective, pre-post study.
Setting: Academic, pediatric hospital in an urban setting.
Synopsis: Overall, 1,255 patient admissions (642 pre-/613 post-handoff intervention) were evaluated on two inpatient units during the periods of July 2009-September 2009 (pre-intervention) and November 2009-January 2010 (post-intervention). The intervention was a handoff “bundle” consisting of a standardized communication and handoff training session, a verbal mnemonic to standardize handoffs, and a new unified resident-intern handoff structure in a private, quiet setting. A computerized handoff tool was also added in one unit. Primary outcomes were a comparison of the rate of medical errors per 100 admissions and rates of preventable adverse events before and after the intervention.
Implementation of the bundle resulted in a significant decrease in medical errors (18.3 from 33.8 per 100 admissions, P<0.001) and preventable adverse events (1.5 from 3.3 per 100 admissions, P=0.04). Secondary outcomes included reductions in omissions of key data in the written handoff (even greater in the group using the computerized tool) and increased percentage of time spent in direct patient care, with no change in handoff duration. Additionally, handoffs were more likely to occur in a quiet, private location.
Limitations included the potential for confounding in a pre-post intervention design, the difficulty in ascertaining the value of the individual components of the bundle, and the potential lack of generalizability.
Bottom line: In a pediatric hospital setting, a multifaceted handoff bundle is associated with improved handoff quality and reductions in medical errors and preventable adverse events.
Citation: Starmer AJ, Sectish TC, Simon DW, et al. Rates of medical errors and preventable adverse events among hospitalized children following implementation of a resident handoff bundle. JAMA. 2013;310(21):2262-2270.
Uncomplicated Skin Infections in Ambulatory Setting Commonly Involve Avoidable Antibiotic Exposure
Clinical question: What are the current prescribing practices for antibiotics used to treat skin and soft tissue infections in the outpatient setting?
Background: Uncomplicated skin and soft tissue infections are among the most frequent indications for outpatient antibiotic use. Because antibiotic use is associated with bacterial resistance and adverse events, understanding antibiotic prescribing practices is necessary to minimize these types of complications.
Study design: Retrospective cohort.
Setting: Ambulatory care setting in the Denver Health System.
Synopsis: Data from 364 adults and children who presented to an ambulatory setting with a primary diagnosis of skin and soft tissue infection were analyzed using a stepwise multivariate logistic regression in order to determine factors associated with avoidable antibiotic exposure. Among cellulitis cases, 61% of patients were prescribed antibiotics to treat methicillin-resistant Staphylococcus aureus. Avoidable antibiotic exposure occurred in 46% of cases, including use of antibiotics with broad Gram-negative activity (4%), combination therapy (12%), and treatment for ≥10 days (42%). Use of short-course, single-antibiotic treatment approaches consistent with national guidelines would have reduced prescribed antibiotic days by 19%, to 55%.
Bottom line: Avoidable antibiotic exposure frequently occurs in the treatment of uncomplicated skin infections; using short-course, single-antibiotic treatment strategies could significantly reduce total antibiotic use.
Citation: Hurley HJ, Knepper BC, Price CS, Mehler PS, Burman WJ, Jenkins TC. Avoidable antibiotic exposure for uncomplicated skin and soft tissue infections in the ambulatory care setting. Am J Med. 2013;126(12):1099-1106.
Warfarin Initiation in Atrial Fibrillation Associated with Increased Short-Term Risk of Stroke
Clinical question: Is the initiation of warfarin associated with an increased risk of ischemic stroke in patients with atrial fibrillation (Afib)?
Background: Two Afib trials of oral factor Xa inhibitors showed an increased risk of stroke when patients were transitioned to open label warfarin at the end of the study. Warfarin can, theoretically, lead to a transient hypercoagulable state upon treatment initiation, so further study is indicated to determine if the initiation of warfarin is associated with increased stroke risk among Afib patients.
Study design: Population-based, nested case-control.
Setting: UK Clinical Practice Research Datalink.
Synopsis: A cohort of 70,766 patients with newly diagnosed Afib was identified from a large primary care database. Conditional logistic regression was used to estimate adjusted rate ratios (RR) of stroke associated with warfarin monotherapy, classified according to time since initiation of treatment when compared to patients not on antithrombotic therapy.
Warfarin was associated with a 71% increased risk of stroke in the first 30 days of use (RR 1.71, 95% CI 1.39-2.12). Risk was highest in the first week of warfarin treatment, which is consistent with the known transient pro-coagulant effect of warfarin. Decreased risks were observed with warfarin initiation >30 days before the ischemic event (31-90 days: RR 0.50, 95% CI 0.34-0.75; >90 days: RR 0.55, 95% CI 0.50-0.61).
Limitations included the extraction of data from a database, which could lead to misclassification of diagnosis or therapy, and the observational nature of the study.
Bottom line: There may be an increased risk of ischemic stroke during the first 30 days of treatment with warfarin in patients with Afib.
Citation: Azoulay L, Dell-Aniello S, Simon T, Renoux C, Suissa S. Initiation of warfarin in patients with atrial fibrillation: early effects on ischaemic strokes [published online ahead of print December 18, 2013]. Eur Heart J.
Multifaceted Discharge Interventions Reduce Rates of Pediatric Readmission and Post-Hospital ED Utilization
Clinical question: Do interventions at discharge reduce the rate of readmissions and post-hospitalization ED visits among pediatric patients?
Background: Readmissions are a high-priority quality measure in both the adult and pediatric settings. Although a broadening body of literature is evaluating the impact of interventions on readmissions in adult populations, the literature does not contain a similar breadth of assessments of interventions in the pediatric setting.
Study design: Systematic review.
Setting: English-language articles studying pediatric inpatient discharge interventions.
Synopsis: A total of 1,296 unique articles were identified from PubMed and the Cumulative Index to Nursing and Allied Health Literature. Additional articles were identified on review of references, yielding 14 articles that met inclusion criteria. Included studies evaluated the effect of pediatric discharge interventions on the primary outcomes of hospital readmission or post-hospitalization ED visits. Interventions focused on three main patient populations: asthma, cancer, and prematurity.
Six studies demonstrated statistically significant reductions in readmissions and/or ED visits, while two studies actually demonstrated an increase in post-discharge utilization. All successful interventions began in the inpatient setting and were multifaceted, with four of six studies including an educational component and a post-discharge follow-up component.
While all of the studies evaluated sought to enhance the transitional care from the inpatient to outpatient setting, only the interventions that included one responsible party (individual or team) with expertise in the medical condition providing oversight and support were successful in reducing the specified outcomes. A significant limitation was that many of the studies identified were not sufficiently powered to detect either outcome of interest.
Bottom line: A multifaceted intervention involving educational and post-discharge follow-up components with an experienced individual or team supporting the transition is associated with a reduction in hospital readmissions and post-discharge ED utilization.
Citation: Auger KA, Kenyon CC, Feudtner C, Davis MM. Pediatric hospital discharge interventions to reduce subsequent utilization: a systematic review [published online ahead of print December 20, 2013]. J Hosp Med.
Sepsis Diagnoses Are Common in ED, but Many Septic Patients in the ED Do Not Receive Antibiotics
Clinical question: Has the frequency of sepsis rates, along with administration of antibiotics in U.S. emergency departments (EDs), changed over time?
Background: Prior studies reviewing discharge data from hospitals suggest an increase of sepsis over time; however, little epidemiological research has evaluated the diagnosis of sepsis and antibiotic use in ED settings.
Study design: Retrospective, four-stage probability sample.
Setting: National Hospital Ambulatory Medical Care Survey (NHAMCS).
Synopsis: The NHAMCS includes a sample of all U.S. ED visits, except federal, military, and VA hospitals. According to NHAMCS data, an estimated 1.3 billion visits by adults to U.S. EDs occurred from 1994-2009, or approximately 81 million visits per year. Explicit sepsis was defined by the presence of the following, with ICD-9 codes: septicemia (038), sepsis (995.91), severe sepsis (995.92), or septic shock (785.52). Implicit sepsis was defined as a code indicating infection plus a code indicting organ dysfunction.
In U.S. EDs, explicit sepsis did not become more prevalent from 1994-2009; however, implicitly diagnosed sepsis increased by 7% every two years. There were 260,000 explicit sepsis-related ED visits per year, or 1.23 visits per 1,000 U.S. population. In-hospital mortality was 17% and 9% for the explicit and implicit diagnosis groups, respectively. On review of the explicit sepsis group, only 61% of the patients were found to have received antibiotics in the ED. The rate did increase over the time studied, from 52% in 1994-1997 to 69% in 2006-2009.
The study was limited by the retrospective analysis of data not designed to track sepsis or antibiotic use.
Bottom Line: Explicitly recognized sepsis remained stable in the ED setting from 1994-2009, and early antibiotic use has improved during this time, but there is still much opportunity for improvement.
Citation: Filbin MR, Arias SA, Camargo CA Jr, Barche A, Pallin DJ. Sepsis visits and antibiotic utilization in the U.S. emergency departments. Crit Care Med. 2014;42(3):528-535.
New Oral Anticoagulants Safe and Effective for Atrial Fibrillation Treatment
Clinical question: Is there a difference in efficacy and safety among new oral anticoagulants compared to warfarin in subgroups of patients with atrial fibrillation (Afib)?
Background: Studies of new oral anticoagulants have demonstrated that these agents are at least as safe and effective as warfarin for prevention of stroke and systemic embolism in Afib. This study was designed to look at available phase 3 randomized trials, with the goal of subgroup analysis for both efficacy and bleeding risks.
Study design: Meta-analysis.
Setting: Phase 3 randomized controlled trials of patients with Afib.
Synopsis: The analysis included four trials of Afib patients randomized to receive warfarin or a novel oral anticoagulant (NOAC), including dabigatran, rivaroxaban, apixaban, and edoxaban. In total, 42,411 patients received an NOAC and 29,272 patients received warfarin. Separate analyses were performed for high-dose and low-dose NOACs.
The high-dose NOAC demonstrated a 19% reduction in stroke and systemic embolic events as compared to warfarin, largely due to the reduction of hemorrhagic strokes by the NOAC. The low-dose NOAC showed similar efficacy to warfarin for reduction of stroke and systemic embolic events, with an increase noted in the subset of ischemic stroke in low-dose NOAC. Both doses of NOAC demonstrated a significant reduction in all-cause mortality. NOAC showed a non-significant reduction in bleeding compared to warfarin; however, subset analysis demonstrated an increase in gastrointestinal bleeding with high-dose NOAC and a significant reduction in intracranial hemorrhage with low-dose NOAC.
A notable limitation of the study is that it only included clinical trials in the analysis.
Bottom line: In relation to stroke, systemic embolic events, and all-cause mortality, new oral anticoagulants showed a favorable efficacy and safety profile as compared to warfarin in Afib patients.
Citation: Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383(9921):955-962.
In the Literature: Research You Need to Know
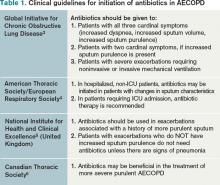
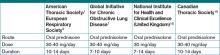
Clinical question: What are the changes in the updated Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines?
Background: Chronic obstructive pulmonary disease (COPD) remains a leading cause of death in the U.S. and worldwide. The GOLD guidelines are an international consensus report on COPD diagnosis, management, and prevention, first released in 2001. The 2011 revision to the guidelines was recently published and outlines substantial changes based on updated literature and expert opinion.
Study design: Guidelines based on studies with varying designs.
Setting: Expert panel review of multiple studies from different settings.
Synopsis: While the diagnosis of COPD remains based on a post-bronchodilator fixed ratio of FEV1/FVC <0.70, there is more emphasis on global clinical assessment in the new guidelines. The updated approach describes classifying COPD severity based on risk/symptom frequency using established symptom assessment and the frequency of acute exacerbations of COPD. Instead of five “stages” based on FEV1 measures alone, there are now four "grades" of A through D (A: low risk/fewer symptoms; B: low risk/more symptoms; C: high risk/fewer symptoms; D: high risk/more symptoms) to more easily guide treatment options.
Treatment strategies are also updated, focusing not only on reduction of current symptoms, but also risk of future events. Pharmacologic treatment recommendations include using bronchodilator monotherapy in Group A patients, favoring long-acting over short-acting bronchodilators in Group B patients, prescribing inhaled corticosteroids only in combination with long-acting bronchodilators in Groups C and D patients, and considering newer agents such as phosphodiesterase-4 inhibitors in Group D patients.
Non-pharmacologic interventions include ongoing smoking cessation strategies, exercise promotion, treatment of comorbidities, and even public health strategies in pollution control.
Bottom line: The GOLD guidelines have undergone major revisions that provide a more practical approach to classification of COPD based on symptom severity and risk assessment in order to direct providers in evidence-based treatment that addresses both short-term and long-term impact of the disease.
Citation: Global Initiative for Chronic Obstructive Lung Disease. Global strategy for diagnosis, management, and prevention of COPD. Global Initiative for Chronic Obstructive Lung Disease website. Accessed Oct. 29, 2012.
For more physician reviews of recent HM-relevant literature, visit our website.
Clinical question: What are the changes in the updated Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines?
Background: Chronic obstructive pulmonary disease (COPD) remains a leading cause of death in the U.S. and worldwide. The GOLD guidelines are an international consensus report on COPD diagnosis, management, and prevention, first released in 2001. The 2011 revision to the guidelines was recently published and outlines substantial changes based on updated literature and expert opinion.
Study design: Guidelines based on studies with varying designs.
Setting: Expert panel review of multiple studies from different settings.
Synopsis: While the diagnosis of COPD remains based on a post-bronchodilator fixed ratio of FEV1/FVC <0.70, there is more emphasis on global clinical assessment in the new guidelines. The updated approach describes classifying COPD severity based on risk/symptom frequency using established symptom assessment and the frequency of acute exacerbations of COPD. Instead of five “stages” based on FEV1 measures alone, there are now four "grades" of A through D (A: low risk/fewer symptoms; B: low risk/more symptoms; C: high risk/fewer symptoms; D: high risk/more symptoms) to more easily guide treatment options.
Treatment strategies are also updated, focusing not only on reduction of current symptoms, but also risk of future events. Pharmacologic treatment recommendations include using bronchodilator monotherapy in Group A patients, favoring long-acting over short-acting bronchodilators in Group B patients, prescribing inhaled corticosteroids only in combination with long-acting bronchodilators in Groups C and D patients, and considering newer agents such as phosphodiesterase-4 inhibitors in Group D patients.
Non-pharmacologic interventions include ongoing smoking cessation strategies, exercise promotion, treatment of comorbidities, and even public health strategies in pollution control.
Bottom line: The GOLD guidelines have undergone major revisions that provide a more practical approach to classification of COPD based on symptom severity and risk assessment in order to direct providers in evidence-based treatment that addresses both short-term and long-term impact of the disease.
Citation: Global Initiative for Chronic Obstructive Lung Disease. Global strategy for diagnosis, management, and prevention of COPD. Global Initiative for Chronic Obstructive Lung Disease website. Accessed Oct. 29, 2012.
For more physician reviews of recent HM-relevant literature, visit our website.
Clinical question: What are the changes in the updated Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines?
Background: Chronic obstructive pulmonary disease (COPD) remains a leading cause of death in the U.S. and worldwide. The GOLD guidelines are an international consensus report on COPD diagnosis, management, and prevention, first released in 2001. The 2011 revision to the guidelines was recently published and outlines substantial changes based on updated literature and expert opinion.
Study design: Guidelines based on studies with varying designs.
Setting: Expert panel review of multiple studies from different settings.
Synopsis: While the diagnosis of COPD remains based on a post-bronchodilator fixed ratio of FEV1/FVC <0.70, there is more emphasis on global clinical assessment in the new guidelines. The updated approach describes classifying COPD severity based on risk/symptom frequency using established symptom assessment and the frequency of acute exacerbations of COPD. Instead of five “stages” based on FEV1 measures alone, there are now four "grades" of A through D (A: low risk/fewer symptoms; B: low risk/more symptoms; C: high risk/fewer symptoms; D: high risk/more symptoms) to more easily guide treatment options.
Treatment strategies are also updated, focusing not only on reduction of current symptoms, but also risk of future events. Pharmacologic treatment recommendations include using bronchodilator monotherapy in Group A patients, favoring long-acting over short-acting bronchodilators in Group B patients, prescribing inhaled corticosteroids only in combination with long-acting bronchodilators in Groups C and D patients, and considering newer agents such as phosphodiesterase-4 inhibitors in Group D patients.
Non-pharmacologic interventions include ongoing smoking cessation strategies, exercise promotion, treatment of comorbidities, and even public health strategies in pollution control.
Bottom line: The GOLD guidelines have undergone major revisions that provide a more practical approach to classification of COPD based on symptom severity and risk assessment in order to direct providers in evidence-based treatment that addresses both short-term and long-term impact of the disease.
Citation: Global Initiative for Chronic Obstructive Lung Disease. Global strategy for diagnosis, management, and prevention of COPD. Global Initiative for Chronic Obstructive Lung Disease website. Accessed Oct. 29, 2012.
For more physician reviews of recent HM-relevant literature, visit our website.
ITL: Physician Reviews of HM-Relevant Research
In This Edition
Literature At A Glance
A guide to this month’s studies
- Interventions that improve discharge handovers reviewed
- Duration of in-hospital cardiac resuscitation and survival rates
- Early sepsis intervention strategies to decrease mortality risk
- Hypoglycemia linked to increased mortality in critically ill
- Increased bleeding risk for cardiac patients
- Hospital-run vs. anesthesiologist-run preoperative clinics
- Postoperative delirium and cognitive impairment in cardiac patients
- Benefits of resuming anticoagulants after GI bleeding
- Preoperative hyponatremia and risk of perioperative mortality
Systematic Review Highlights Several Interventions That Improve Discharge Handovers
Clinical question: Do interventions to improve patient handovers at discharge have positive effects on patient care?
Background: The transition from hospital to primary care is often suboptimal and has been associated with unfavorable outcomes, including hospital readmission, increased healthcare utilization, and adverse drug events post-discharge. This review sought to characterize different types of interventions aimed at improving discharge handovers and to evaluate their effects.
Study design: Systematic review of randomized controlled trials.
Setting: Studies published from January 1990 to March 2011.
Synopsis: Review of published databases identified 36 randomized controlled studies on interventions to improve discharge handovers. Studies were blindly evaluated by two reviewers on quality, interventions, and outcomes. There was significant heterogeneity in interventions and outcomes; thus, statistical analysis was not possible. Most studies evaluated multicomponent interventions and had more than one outcome measure.
Of the 36 studies reviewed, 25 reported statistically significant improvements in outcomes, including reduced hospital utilization and improved continuity of care. Effective interventions included medication reconciliation; structured discharge information (facilitated by electronic resources); multidisciplinary discharge planning; shared involvement in arranging care between inpatient and outpatient physicians; and Web-based access to discharge information by the outpatient provider.
The complexity of the interventions and the heterogeneity of reported results did not allow for firm conclusions to be drawn regarding which specific interventions had the strongest effects.
Bottom line: Interventions that target the quality and safety of handovers between hospital and outpatient providers at discharge can significantly reduce hospital utilization and improve continuity of care.
Citation: Hesselink G, Schoonhoven L, Barach P, et al. Improving patient handovers from hospital to primary care: a systematic review. Ann Intern Med. 2012;157:417-428.
Longer Duration of In-Hospital Cardiac Resuscitation Associated with Increased Survival
Clinical question: Are prolonged cardiac resuscitation efforts associated with improved outcomes?
Background: There is little evidence or guidelines on how long to maintain resuscitative efforts during in-hospital cardiac arrest, leading to variation in practice. This study characterized patterns of resuscitation duration and relationship to the return of spontaneous circulation and survival to discharge.
Study design: Retrospective observational study.
Setting: Four hundred thirty-five U.S. hospitals reporting data to the American Heart Association’s Get With The Guidelines: Resuscitation registry.
Synopsis: Using duration of resuscitation in nonsurvivors as a surrogate for the tendency of a facility to perform prolonged efforts, hospitals were divided into quartiles. Overall, of 64,339 patients in the registry, 31,198 (48.5%) had return of circulation and 9,912 (15.4%) survived to discharge. Resuscitative efforts in nonsurvivors ranged from a median of 16 to 25 minutes between the lowest and highest quartiles.
There was a stepwise increase in the likelihood for patients to have return of spontaneous circulation and to survive to discharge between each quartile. Specifically, comparing shortest to longest, there was a significant adjusted odds ratio of 1.12 for both the return of circulation (P<0.0001) and survival to discharge (P=0.021). The survival benefit was most apparent for those with pulseless electrical activity or asystole as initial rhythms, as compared to ventricular tachycardia or fibrillation.
Limitations included the study’s observational design, which meant causality could not be determined. Additionally, the study did not account for the quality of resuscitative efforts (e.g. depth of chest compressions, adherence with guidelines), which might have influenced outcomes. Importantly, the study looked at survival to discharge, but it did not evaluate long-term survival or functional status post-discharge, which might better reflect the success of resuscitation.
Bottom line: Prolonged resuscitative efforts were observed to be associated with increased likelihood of return of spontaneous circulation and survival to discharge; this data might provide clinical guidance in determining when to stop resuscitation efforts.
Citation: Goldberger ZD, Chan PS, Berg RA, et al. Duration of resuscitation efforts and survival after in-hospital cardiac arrest: an observational study. Lancet. 2012;380:1473-1481.
Early Sepsis Intervention Strategies Decrease Mortality, Length of Stay, and Cost
Clinical question: For patients with sepsis or septic shock, what is the impact of a real-time comprehensive continuous quality-improvement (QI) initiative on in-hospital mortality, morbidity, and healthcare resource utilization in community and tertiary-care hospitals in the U.S.?
Background: Multiple single-center trials have demonstrated that early sepsis intervention strategies (early goal-directed therapy, resuscitation bundles) improve in-hospital mortality. Little is known about the effectiveness of incorporating these strategies into a real-time continuous QI initiative and implementing interventions across multiple sites simultaneously.
Study design: Pre-post at some sites and concurrent implementation design at other sites.
Setting: Five community and six-tertiary care U.S. hospitals.
Synopsis: The GENeralized Early Sepsis Intervention Strategies (GENESIS) project was a CQI initiative that combined several QI concepts with validated early sepsis interventions known as resuscitation bundles (RB). Continuous QI was implemented on patients with severe sepsis or septic shock in both before and after designs (eight hospitals), and in concurrent designs (three hospitals). The control group was comprised of historical controls treated before GENESIS and patients with incomplete implementation of RB, totaling 1,554 patients. The treatment group included patients treated after GENESIS and those with complete RB compliance, totaling 4,801 patients.
Compared with the control group, patients in the treatment group had a 33% decreased risk of in-hospital mortality (RR 0.67, 95% CI 0.63-0.72), an absolute decrease in hospital length of stay (LOS) by 5.1 days (20.7 days vs. 15.6 days, P<0.001) and a $47,923 reduction in total hospital charges (P<0.001). Limitations included the study design (not a prospective randomized trial), and the possibility of other concurrent unmeasured quality initiatives taking place at the study sites, which might have contributed to improved outcomes.
Bottom line: Early sepsis intervention strategies in the form of a comprehensive continuous QI initiative can decrease mortality, hospital LOS, and cost in both tertiary-care and community hospitals.
Citation: Cannon CM, Holthaus CV, Zubrow MT, et al. The GENESIS project (GENeralized Early Sepsis Intervention Strategies): a multicenter quality improvement collaborative. J Intensive Care Med. 2012; Aug 17. doi:10.1177/0885066612453025.
Hypoglycemia Associated with Increased Mortality in the Critically Ill
Clinical question: Is hypoglycemia associated with mortality in critically ill patients?
Background: Initial studies suggested that intensive glucose control reduces mortality in surgical ICU patients and reduces morbidity in medical ICU patients, but further studies have not supported these findings. Recent literature shows conflicting results on the effects of intense glucose control in critically ill patients.
Study design: Post-hoc analysis of the NICE-SUGAR study database.
Setting: ICUs in 42 hospitals in Australia, New Zealand, and Canada.
Synopsis: The NICE-SUGAR study was a multicenter trial that randomized 6,104 ICU patients to intensive (glucose 80 to 108 mg/dL) or conventional glucose control (≤180 mg/dL). Patients were followed for 90 days or until death, with death being the primary end point. Severe hypoglycemia (<40 mg/dL) was recorded in 6.8% of patients in the intensive glucose control group versus 0.5% in the conventional group. The study showed that intensive glucose control was associated with increased mortality among adult ICU patients.
Using the NICE-SUGAR database, the authors conducted a Cox regression analysis to examine the associations between hypoglycemia and death. A total of 2,714 patients had moderate hypoglycemia (glucose 41 to 70 mg/dL), and 223 patients had severe hypoglycemia. The hazard ratio for mortality was 1.41 (95% CI 1.21-1.62, P<0.001) for patients with moderate hypoglycemia and 2.10 (95% CI 1.59-2.77, P<0.001) for severe hypoglycemia, compared to patients without hypoglycemia.
These findings show a strong association between mortality and hypoglycemia but do not prove causality. Hospitalists caring for ICU patients must be aware that hypoglycemia is associated with mortality and focus on avoiding hypoglycemia. The American Diabetes Association currently recommends a target blood glucose level of 140 to 180 mg/dL for most critically ill patients.
Bottom line: Hypoglycemia (glucose <70 mg/dL) is associated with increased risk of mortality in ICU patients.
Citation: Finfer S, Chittock DR, Su SY, et al. Hypoglycemia and risk of death in critically ill patients. New Engl J Med. 2012;367(12):1108-1118.
Increased Bleeding Risk for Cardiac Patients on Multiple Antithrombotic Drugs
Clinical question: Is there an increased risk of bleeding in atrial fibrillation patients treated with multiple antithrombotic agents following acute myocardial infarction (MI) or percutaneous coronary intervention (PCI)?
Background: Current treatment for atrial fibrillation patients with MI or PCI includes vitamin K antagonist (VKA) therapy to prevent stroke and antiplatelet agents to prevent further coronary events. There are inconsistent findings on the safety and efficacy of combined therapy with VKA, aspirin, and clopidogrel, specifically with regard to bleeding risk.
Study design: Retrospective cohort study.
Setting: Nationwide registry in Denmark.
Synopsis: Using the National Patient Registry in Denmark, 11,480 patients with atrial fibrillation who were admitted for MI or PCI were identified. Patients were grouped by medication regimen, including monotherapy (aspirin, clopidogrel, or VKA), dual therapy (dual antiplatelet or VKA+antiplatelet), or triple therapy (VKA+aspirin+clopidogrel). The primary outcome was nonfatal or fatal bleeding within one year.
Patients receiving triple therapy had the highest rate of bleeding, with a crude incidence of 14.2 events per 100 person-years. Patients treated with VKA+aspirin+clopidogel were significantly more likely than those on VKA+antiplatelet (HR 1.47, 95% CI 1.04-2.08) or dual antiplatelet (HR 2.20, 95% CI 1.58-3.08) treatment to have a bleeding event within 90 days, and similar trends were seen at 90 to 360 days. There was no significant difference in thromboembolic events among patients on VKA+aspirin+clopidogrel versus VKA+antiplatelet therapy.
Only bleeding events that required hospitalization were recorded, which might underestimate the bleeding risks of these regimens. Additionally, INR levels were not determined, which could impact both bleeding and thromboembolic outcomes.
However, this study does suggest that there are significant bleeding risks among patients treated with triple therapy. Hospitalists should weigh the risks of thromboembolic events with bleeding risks in patients with atrial fibrillation and MI/PCI, and only prescribe VKA+aspirin+clopidogrel with these risks in mind.
Bottom line: Immediate and continued bleeding risk is increased in patients with atrial fibrillation admitted with PCI or MI who are placed on triple antithrombotic therapy with VKA+aspirin+clopidogrel.
Citation: Lamberts M, Olesen JB, Ruwald MH, et al. Bleeding after initiation of multiple antithrombotic drugs, including triple therapy, in atrial fibrillation patients following myocardial infarction and coronary intervention. Circulation. 2012;126:1185-1193.
Hospitalist-Run Preoperative Clinic Improves Outcomes in Complex Surgical Patients
Clinical question: Do hospitalist-run preoperative clinics improve outcomes for medically complex patients undergoing noncardiac surgery compared to traditional anesthesiologist-run preoperative clinics?
Background: Studies of perioperative medical consultation have shown inconsistent effects on quality of care, but preoperative medical consultation has only been evaluated in the immediate preoperative period (one day prior to surgery or less). Little is known about the impact of involving hospitalists earlier in the preoperative period.
Study design: Retrospective, pre-post study.
Setting: Veterans Affairs Greater Los Angeles Healthcare System (VAGLAHS).
Synopsis: In July 2004, the VAGLAHS Preoperative Clinic transitioned from being anesthesiologist-run to hospitalist-run. Mid-level providers were trained on preoperative medical assessment, and patients were only evaluated by anesthesia staff on the day of surgery, after they had been deemed medically acceptable for surgery. All patients seen in the clinic from July 2003 to July 2005 were included in the study. Period A included patients evaluated when anesthesia staff supervised the clinic. Period B included patients evaluated during the first year of the hospitalist-run system.
There were 1,101 patients with inpatient surgeries in Period A, and 1,126 patients in Period B. Mean length of stay (LOS) decreased to 5.28 days during the hospitalist-run model from 9.87 days during the anesthesiologist-run model. LOS reductions were most notable in patients with ASA scores of 3 or higher; LOS reductions were not seen in an internal control of surgical patients who were not evaluated in the preoperative clinic. Inpatient mortality was also reduced in Period B compared with Period A, to 4 cases (0.36%) from 14 cases (1.27%) (P=0.0158). Specific processes that led to improved outcomes for patients in Period B could not be identified. The VA study setting might limit the generalizability of the results.
Bottom line: A hospitalist-run preoperative clinic was associated with decreased LOS and inpatient mortality compared with a traditional anesthesiologist-run clinic.
Citation: Vazirani S, Lankarani-Fard A, Lian LJ, Stelzner M, Asch SM. Preoperative processes and outcomes after implementation of a hospitalist-run preoperative clinic. J Hosp Med. 2012 Sep 7. doi:10.1002/jhm.1968.
Delirium after Cardiac Surgery Associated with Prolonged Cognitive Impairment
Clinical question: Is postoperative delirium associated with decreased cognitive function in the first year after cardiac surgery?
Background: In general populations, delirium has been associated with long-term decline in cognitive ability. Delirium and cognitive dysfunction are both common following cardiac surgery, but the effects of postoperative delirium on the trajectory of cognitive function over time is unclear.
Study design: Prospective cohort study.
Setting: Two academic medical centers and a Veterans Administration hospital.
Synopsis: Two hundred twenty-five patients aged 60 or older who were scheduled to undergo coronary artery bypass grafting or valve replacement surgery were included. Patients underwent preoperative assessment cognitive function with the use of the Mini-Mental State Examination (MMSE). Starting on postoperative Day 2, patients underwent daily assessment for delirium. After discharge, cognitive function was reassessed at months one, six, and 12.
Postoperative delirium occurred in 103 patients (46%). Patients with delirium were older, had higher comorbidity scores, and had lower MMSE scores at baseline. Among the overall study population, adjusted MMSE scores dropped 4.6 points from baseline to postoperative Day 2, then were observed to increase by approximately one point per day during postoperative days 3 to 5 with minimal change thereafter. Patients with delirium had greater decrease in cognitive function in the immediate postoperative period compared to patients without delirium (7.7 points vs. 2.1, P<0.001).
Patients without delirium returned to their baseline cognitive ability by one month postoperatively, while patients who had delirium were still making gains up to six months post-operatively, never returning to baseline level of function by one year. Unmeasured confounders and uncertain sensitivity of the MMSE to detect mild cognitive impairment might limit these findings.
Bottom line: Cognitive function decreases in the immediate postoperative period following cardiac surgery. Compared to patients without delirium, patients with delirium experience more dramatic and prolonged cognitive impairment postoperatively, without returning to their preoperative level of cognitive function at one year.
Citation: Saczynski JS, Marcantonio ER, Quach L, et al. Cognitive trajectories after postoperative delirium. New Engl J Med. 2012;367:30-39.
Benefits of Resuming Anticoagulation after GI Bleed Outweigh Risks for Most Patients
Clinical question: In warfarin-treated patients who have experienced gastrointestinal (GI) bleeding, what are the patterns of restarting warfarin therapy and the incidence of thrombosis, recurrent GI bleed, and death in the 90 days following index bleed?
Background: In warfarin-treated patients who experience GI bleeding, warfarin is often temporarily held or permanently discontinued, placing patients at increased risk for developing thromboembolism. Little is known about the risks, benefits, and timing of restarting warfarin in this patient population.
Study design: Retrospective cohort study.
Setting: Kaiser Permanente Colorado.
Synopsis: Using clinical and administrative databases, 442 patients who presented with GI bleeding while receiving warfarin therapy were identified. Patients were grouped by whether they resumed warfarin (n=260, including 41 patients in whom anticoagulation was never interrupted), or did not resume warfarin therapy (n=182) in the 90 days following index GI bleed. Patients with prosthetic heart valves or GI bleeding localized to the rectum/anus were more commonly restarted on warfarin, whereas older patients and those in whom the source of bleeding was not identified were less likely to be restarted on warfarin therapy.
Restarting warfarin therapy after index GI bleed was associated with lower risk of thrombosis (HR 0.05, 95% CI 0.01-0.58) and death from any cause (HR 0.31, 95% CI 0.15-0.62), and it was not associated with a significant increase in risk for recurrent GI bleed (HR 1.32, 95% CI 0.50-3.57).
The authors concluded that for many patients who experience a warfarin-associated GI bleed, the benefits of restarting warfarin therapy outweigh the risks. No conclusions were made regarding the optimal timing of resuming therapy. Limitations included the use of administrative data and inability to determine the potential influence of aspirin use on outcomes.
Bottom line: Resuming warfarin in the 90 days following a warfarin-associated GI bleed is associated with decreased risk of thrombosis and death without increased risk for recurrent GI bleed.
Citation: Witt DM, Delate T, Garcia DA, et al. Risk of thromboembolism, recurrent hemorrhage, and death after warfarin therapy interruption for gastrointestinal tract bleeding. Arch Intern Med. 2012 Sep 12. doi:10.1001/archinternmed.2012.4261.
Preoperative Hyponatremia Associated with Increased Risk for Perioperative Complications and Mortality
Clinical question: Is preoperative hyponatremia an indicator of perioperative morbidity and mortality?
Background: Hyponatremia is a common diagnosis in the hospital setting and is associated with adverse outcomes, even in mild cases. However, it is unclear if this association exists in surgical patients when detected preoperatively.
Study design: Retrospective cohort study.
Setting: Academic and community hospitals participating in the American College of Surgeons National Surgical Quality Improvement Program (NSQIP).
Synopsis: A total of 75,423 adult patients with hyponatremia (sodium <135 mEq/L) who were undergoing major surgery were compared to 888,840 patients with normal preoperative sodium levels over a six-year period. The primary outcome was 30-day mortality. Secondary outcomes included postoperative major coronary events, stroke, wound infection, pneumonia, and length of stay (LOS).
Compared to patients with normal sodium levels, those with preoperative hyponatremia had higher rates of perioperative mortality (5.2% vs. 1.3%; adjusted odds ratio 1.44, 95% CI 1.38-1.50), with increased risk that correlated with increasing severity of hyponatremia. Association with postoperative mortality was particularly strong among hyponatremic patients with ASA scores of 1 or 2 and those undergoing nonemergency surgery.
Patients with preoperative hyponatremia were also found to have increased risk for all postoperative complications evaluated, with the exception of stroke. Limitations included the potential for unmeasured confounders and not being able to account for the role of medications used perioperatively. Research is needed to determine whether correcting preoperative hyponatremia lessens the risk of mortality and other postoperative complications.
Bottom line: Among patients undergoing major surgery, preoperative hyponatremia is a predictor of postoperative 30-day mortality and morbidity.
Citation: Leung AA, McAlister FA, Rogers SO, et al. Preoperative hyponatremia and perioperative complications. Arch Intern Med. 2012;172:1-8.
In This Edition
Literature At A Glance
A guide to this month’s studies
- Interventions that improve discharge handovers reviewed
- Duration of in-hospital cardiac resuscitation and survival rates
- Early sepsis intervention strategies to decrease mortality risk
- Hypoglycemia linked to increased mortality in critically ill
- Increased bleeding risk for cardiac patients
- Hospital-run vs. anesthesiologist-run preoperative clinics
- Postoperative delirium and cognitive impairment in cardiac patients
- Benefits of resuming anticoagulants after GI bleeding
- Preoperative hyponatremia and risk of perioperative mortality
Systematic Review Highlights Several Interventions That Improve Discharge Handovers
Clinical question: Do interventions to improve patient handovers at discharge have positive effects on patient care?
Background: The transition from hospital to primary care is often suboptimal and has been associated with unfavorable outcomes, including hospital readmission, increased healthcare utilization, and adverse drug events post-discharge. This review sought to characterize different types of interventions aimed at improving discharge handovers and to evaluate their effects.
Study design: Systematic review of randomized controlled trials.
Setting: Studies published from January 1990 to March 2011.
Synopsis: Review of published databases identified 36 randomized controlled studies on interventions to improve discharge handovers. Studies were blindly evaluated by two reviewers on quality, interventions, and outcomes. There was significant heterogeneity in interventions and outcomes; thus, statistical analysis was not possible. Most studies evaluated multicomponent interventions and had more than one outcome measure.
Of the 36 studies reviewed, 25 reported statistically significant improvements in outcomes, including reduced hospital utilization and improved continuity of care. Effective interventions included medication reconciliation; structured discharge information (facilitated by electronic resources); multidisciplinary discharge planning; shared involvement in arranging care between inpatient and outpatient physicians; and Web-based access to discharge information by the outpatient provider.
The complexity of the interventions and the heterogeneity of reported results did not allow for firm conclusions to be drawn regarding which specific interventions had the strongest effects.
Bottom line: Interventions that target the quality and safety of handovers between hospital and outpatient providers at discharge can significantly reduce hospital utilization and improve continuity of care.
Citation: Hesselink G, Schoonhoven L, Barach P, et al. Improving patient handovers from hospital to primary care: a systematic review. Ann Intern Med. 2012;157:417-428.
Longer Duration of In-Hospital Cardiac Resuscitation Associated with Increased Survival
Clinical question: Are prolonged cardiac resuscitation efforts associated with improved outcomes?
Background: There is little evidence or guidelines on how long to maintain resuscitative efforts during in-hospital cardiac arrest, leading to variation in practice. This study characterized patterns of resuscitation duration and relationship to the return of spontaneous circulation and survival to discharge.
Study design: Retrospective observational study.
Setting: Four hundred thirty-five U.S. hospitals reporting data to the American Heart Association’s Get With The Guidelines: Resuscitation registry.
Synopsis: Using duration of resuscitation in nonsurvivors as a surrogate for the tendency of a facility to perform prolonged efforts, hospitals were divided into quartiles. Overall, of 64,339 patients in the registry, 31,198 (48.5%) had return of circulation and 9,912 (15.4%) survived to discharge. Resuscitative efforts in nonsurvivors ranged from a median of 16 to 25 minutes between the lowest and highest quartiles.
There was a stepwise increase in the likelihood for patients to have return of spontaneous circulation and to survive to discharge between each quartile. Specifically, comparing shortest to longest, there was a significant adjusted odds ratio of 1.12 for both the return of circulation (P<0.0001) and survival to discharge (P=0.021). The survival benefit was most apparent for those with pulseless electrical activity or asystole as initial rhythms, as compared to ventricular tachycardia or fibrillation.
Limitations included the study’s observational design, which meant causality could not be determined. Additionally, the study did not account for the quality of resuscitative efforts (e.g. depth of chest compressions, adherence with guidelines), which might have influenced outcomes. Importantly, the study looked at survival to discharge, but it did not evaluate long-term survival or functional status post-discharge, which might better reflect the success of resuscitation.
Bottom line: Prolonged resuscitative efforts were observed to be associated with increased likelihood of return of spontaneous circulation and survival to discharge; this data might provide clinical guidance in determining when to stop resuscitation efforts.
Citation: Goldberger ZD, Chan PS, Berg RA, et al. Duration of resuscitation efforts and survival after in-hospital cardiac arrest: an observational study. Lancet. 2012;380:1473-1481.
Early Sepsis Intervention Strategies Decrease Mortality, Length of Stay, and Cost
Clinical question: For patients with sepsis or septic shock, what is the impact of a real-time comprehensive continuous quality-improvement (QI) initiative on in-hospital mortality, morbidity, and healthcare resource utilization in community and tertiary-care hospitals in the U.S.?
Background: Multiple single-center trials have demonstrated that early sepsis intervention strategies (early goal-directed therapy, resuscitation bundles) improve in-hospital mortality. Little is known about the effectiveness of incorporating these strategies into a real-time continuous QI initiative and implementing interventions across multiple sites simultaneously.
Study design: Pre-post at some sites and concurrent implementation design at other sites.
Setting: Five community and six-tertiary care U.S. hospitals.
Synopsis: The GENeralized Early Sepsis Intervention Strategies (GENESIS) project was a CQI initiative that combined several QI concepts with validated early sepsis interventions known as resuscitation bundles (RB). Continuous QI was implemented on patients with severe sepsis or septic shock in both before and after designs (eight hospitals), and in concurrent designs (three hospitals). The control group was comprised of historical controls treated before GENESIS and patients with incomplete implementation of RB, totaling 1,554 patients. The treatment group included patients treated after GENESIS and those with complete RB compliance, totaling 4,801 patients.
Compared with the control group, patients in the treatment group had a 33% decreased risk of in-hospital mortality (RR 0.67, 95% CI 0.63-0.72), an absolute decrease in hospital length of stay (LOS) by 5.1 days (20.7 days vs. 15.6 days, P<0.001) and a $47,923 reduction in total hospital charges (P<0.001). Limitations included the study design (not a prospective randomized trial), and the possibility of other concurrent unmeasured quality initiatives taking place at the study sites, which might have contributed to improved outcomes.
Bottom line: Early sepsis intervention strategies in the form of a comprehensive continuous QI initiative can decrease mortality, hospital LOS, and cost in both tertiary-care and community hospitals.
Citation: Cannon CM, Holthaus CV, Zubrow MT, et al. The GENESIS project (GENeralized Early Sepsis Intervention Strategies): a multicenter quality improvement collaborative. J Intensive Care Med. 2012; Aug 17. doi:10.1177/0885066612453025.
Hypoglycemia Associated with Increased Mortality in the Critically Ill
Clinical question: Is hypoglycemia associated with mortality in critically ill patients?
Background: Initial studies suggested that intensive glucose control reduces mortality in surgical ICU patients and reduces morbidity in medical ICU patients, but further studies have not supported these findings. Recent literature shows conflicting results on the effects of intense glucose control in critically ill patients.
Study design: Post-hoc analysis of the NICE-SUGAR study database.
Setting: ICUs in 42 hospitals in Australia, New Zealand, and Canada.
Synopsis: The NICE-SUGAR study was a multicenter trial that randomized 6,104 ICU patients to intensive (glucose 80 to 108 mg/dL) or conventional glucose control (≤180 mg/dL). Patients were followed for 90 days or until death, with death being the primary end point. Severe hypoglycemia (<40 mg/dL) was recorded in 6.8% of patients in the intensive glucose control group versus 0.5% in the conventional group. The study showed that intensive glucose control was associated with increased mortality among adult ICU patients.
Using the NICE-SUGAR database, the authors conducted a Cox regression analysis to examine the associations between hypoglycemia and death. A total of 2,714 patients had moderate hypoglycemia (glucose 41 to 70 mg/dL), and 223 patients had severe hypoglycemia. The hazard ratio for mortality was 1.41 (95% CI 1.21-1.62, P<0.001) for patients with moderate hypoglycemia and 2.10 (95% CI 1.59-2.77, P<0.001) for severe hypoglycemia, compared to patients without hypoglycemia.
These findings show a strong association between mortality and hypoglycemia but do not prove causality. Hospitalists caring for ICU patients must be aware that hypoglycemia is associated with mortality and focus on avoiding hypoglycemia. The American Diabetes Association currently recommends a target blood glucose level of 140 to 180 mg/dL for most critically ill patients.
Bottom line: Hypoglycemia (glucose <70 mg/dL) is associated with increased risk of mortality in ICU patients.
Citation: Finfer S, Chittock DR, Su SY, et al. Hypoglycemia and risk of death in critically ill patients. New Engl J Med. 2012;367(12):1108-1118.
Increased Bleeding Risk for Cardiac Patients on Multiple Antithrombotic Drugs
Clinical question: Is there an increased risk of bleeding in atrial fibrillation patients treated with multiple antithrombotic agents following acute myocardial infarction (MI) or percutaneous coronary intervention (PCI)?
Background: Current treatment for atrial fibrillation patients with MI or PCI includes vitamin K antagonist (VKA) therapy to prevent stroke and antiplatelet agents to prevent further coronary events. There are inconsistent findings on the safety and efficacy of combined therapy with VKA, aspirin, and clopidogrel, specifically with regard to bleeding risk.
Study design: Retrospective cohort study.
Setting: Nationwide registry in Denmark.
Synopsis: Using the National Patient Registry in Denmark, 11,480 patients with atrial fibrillation who were admitted for MI or PCI were identified. Patients were grouped by medication regimen, including monotherapy (aspirin, clopidogrel, or VKA), dual therapy (dual antiplatelet or VKA+antiplatelet), or triple therapy (VKA+aspirin+clopidogrel). The primary outcome was nonfatal or fatal bleeding within one year.
Patients receiving triple therapy had the highest rate of bleeding, with a crude incidence of 14.2 events per 100 person-years. Patients treated with VKA+aspirin+clopidogel were significantly more likely than those on VKA+antiplatelet (HR 1.47, 95% CI 1.04-2.08) or dual antiplatelet (HR 2.20, 95% CI 1.58-3.08) treatment to have a bleeding event within 90 days, and similar trends were seen at 90 to 360 days. There was no significant difference in thromboembolic events among patients on VKA+aspirin+clopidogrel versus VKA+antiplatelet therapy.
Only bleeding events that required hospitalization were recorded, which might underestimate the bleeding risks of these regimens. Additionally, INR levels were not determined, which could impact both bleeding and thromboembolic outcomes.
However, this study does suggest that there are significant bleeding risks among patients treated with triple therapy. Hospitalists should weigh the risks of thromboembolic events with bleeding risks in patients with atrial fibrillation and MI/PCI, and only prescribe VKA+aspirin+clopidogrel with these risks in mind.
Bottom line: Immediate and continued bleeding risk is increased in patients with atrial fibrillation admitted with PCI or MI who are placed on triple antithrombotic therapy with VKA+aspirin+clopidogrel.
Citation: Lamberts M, Olesen JB, Ruwald MH, et al. Bleeding after initiation of multiple antithrombotic drugs, including triple therapy, in atrial fibrillation patients following myocardial infarction and coronary intervention. Circulation. 2012;126:1185-1193.
Hospitalist-Run Preoperative Clinic Improves Outcomes in Complex Surgical Patients
Clinical question: Do hospitalist-run preoperative clinics improve outcomes for medically complex patients undergoing noncardiac surgery compared to traditional anesthesiologist-run preoperative clinics?
Background: Studies of perioperative medical consultation have shown inconsistent effects on quality of care, but preoperative medical consultation has only been evaluated in the immediate preoperative period (one day prior to surgery or less). Little is known about the impact of involving hospitalists earlier in the preoperative period.
Study design: Retrospective, pre-post study.
Setting: Veterans Affairs Greater Los Angeles Healthcare System (VAGLAHS).
Synopsis: In July 2004, the VAGLAHS Preoperative Clinic transitioned from being anesthesiologist-run to hospitalist-run. Mid-level providers were trained on preoperative medical assessment, and patients were only evaluated by anesthesia staff on the day of surgery, after they had been deemed medically acceptable for surgery. All patients seen in the clinic from July 2003 to July 2005 were included in the study. Period A included patients evaluated when anesthesia staff supervised the clinic. Period B included patients evaluated during the first year of the hospitalist-run system.
There were 1,101 patients with inpatient surgeries in Period A, and 1,126 patients in Period B. Mean length of stay (LOS) decreased to 5.28 days during the hospitalist-run model from 9.87 days during the anesthesiologist-run model. LOS reductions were most notable in patients with ASA scores of 3 or higher; LOS reductions were not seen in an internal control of surgical patients who were not evaluated in the preoperative clinic. Inpatient mortality was also reduced in Period B compared with Period A, to 4 cases (0.36%) from 14 cases (1.27%) (P=0.0158). Specific processes that led to improved outcomes for patients in Period B could not be identified. The VA study setting might limit the generalizability of the results.
Bottom line: A hospitalist-run preoperative clinic was associated with decreased LOS and inpatient mortality compared with a traditional anesthesiologist-run clinic.
Citation: Vazirani S, Lankarani-Fard A, Lian LJ, Stelzner M, Asch SM. Preoperative processes and outcomes after implementation of a hospitalist-run preoperative clinic. J Hosp Med. 2012 Sep 7. doi:10.1002/jhm.1968.
Delirium after Cardiac Surgery Associated with Prolonged Cognitive Impairment
Clinical question: Is postoperative delirium associated with decreased cognitive function in the first year after cardiac surgery?
Background: In general populations, delirium has been associated with long-term decline in cognitive ability. Delirium and cognitive dysfunction are both common following cardiac surgery, but the effects of postoperative delirium on the trajectory of cognitive function over time is unclear.
Study design: Prospective cohort study.
Setting: Two academic medical centers and a Veterans Administration hospital.
Synopsis: Two hundred twenty-five patients aged 60 or older who were scheduled to undergo coronary artery bypass grafting or valve replacement surgery were included. Patients underwent preoperative assessment cognitive function with the use of the Mini-Mental State Examination (MMSE). Starting on postoperative Day 2, patients underwent daily assessment for delirium. After discharge, cognitive function was reassessed at months one, six, and 12.
Postoperative delirium occurred in 103 patients (46%). Patients with delirium were older, had higher comorbidity scores, and had lower MMSE scores at baseline. Among the overall study population, adjusted MMSE scores dropped 4.6 points from baseline to postoperative Day 2, then were observed to increase by approximately one point per day during postoperative days 3 to 5 with minimal change thereafter. Patients with delirium had greater decrease in cognitive function in the immediate postoperative period compared to patients without delirium (7.7 points vs. 2.1, P<0.001).
Patients without delirium returned to their baseline cognitive ability by one month postoperatively, while patients who had delirium were still making gains up to six months post-operatively, never returning to baseline level of function by one year. Unmeasured confounders and uncertain sensitivity of the MMSE to detect mild cognitive impairment might limit these findings.
Bottom line: Cognitive function decreases in the immediate postoperative period following cardiac surgery. Compared to patients without delirium, patients with delirium experience more dramatic and prolonged cognitive impairment postoperatively, without returning to their preoperative level of cognitive function at one year.
Citation: Saczynski JS, Marcantonio ER, Quach L, et al. Cognitive trajectories after postoperative delirium. New Engl J Med. 2012;367:30-39.
Benefits of Resuming Anticoagulation after GI Bleed Outweigh Risks for Most Patients
Clinical question: In warfarin-treated patients who have experienced gastrointestinal (GI) bleeding, what are the patterns of restarting warfarin therapy and the incidence of thrombosis, recurrent GI bleed, and death in the 90 days following index bleed?
Background: In warfarin-treated patients who experience GI bleeding, warfarin is often temporarily held or permanently discontinued, placing patients at increased risk for developing thromboembolism. Little is known about the risks, benefits, and timing of restarting warfarin in this patient population.
Study design: Retrospective cohort study.
Setting: Kaiser Permanente Colorado.
Synopsis: Using clinical and administrative databases, 442 patients who presented with GI bleeding while receiving warfarin therapy were identified. Patients were grouped by whether they resumed warfarin (n=260, including 41 patients in whom anticoagulation was never interrupted), or did not resume warfarin therapy (n=182) in the 90 days following index GI bleed. Patients with prosthetic heart valves or GI bleeding localized to the rectum/anus were more commonly restarted on warfarin, whereas older patients and those in whom the source of bleeding was not identified were less likely to be restarted on warfarin therapy.
Restarting warfarin therapy after index GI bleed was associated with lower risk of thrombosis (HR 0.05, 95% CI 0.01-0.58) and death from any cause (HR 0.31, 95% CI 0.15-0.62), and it was not associated with a significant increase in risk for recurrent GI bleed (HR 1.32, 95% CI 0.50-3.57).
The authors concluded that for many patients who experience a warfarin-associated GI bleed, the benefits of restarting warfarin therapy outweigh the risks. No conclusions were made regarding the optimal timing of resuming therapy. Limitations included the use of administrative data and inability to determine the potential influence of aspirin use on outcomes.
Bottom line: Resuming warfarin in the 90 days following a warfarin-associated GI bleed is associated with decreased risk of thrombosis and death without increased risk for recurrent GI bleed.
Citation: Witt DM, Delate T, Garcia DA, et al. Risk of thromboembolism, recurrent hemorrhage, and death after warfarin therapy interruption for gastrointestinal tract bleeding. Arch Intern Med. 2012 Sep 12. doi:10.1001/archinternmed.2012.4261.
Preoperative Hyponatremia Associated with Increased Risk for Perioperative Complications and Mortality
Clinical question: Is preoperative hyponatremia an indicator of perioperative morbidity and mortality?
Background: Hyponatremia is a common diagnosis in the hospital setting and is associated with adverse outcomes, even in mild cases. However, it is unclear if this association exists in surgical patients when detected preoperatively.
Study design: Retrospective cohort study.
Setting: Academic and community hospitals participating in the American College of Surgeons National Surgical Quality Improvement Program (NSQIP).
Synopsis: A total of 75,423 adult patients with hyponatremia (sodium <135 mEq/L) who were undergoing major surgery were compared to 888,840 patients with normal preoperative sodium levels over a six-year period. The primary outcome was 30-day mortality. Secondary outcomes included postoperative major coronary events, stroke, wound infection, pneumonia, and length of stay (LOS).
Compared to patients with normal sodium levels, those with preoperative hyponatremia had higher rates of perioperative mortality (5.2% vs. 1.3%; adjusted odds ratio 1.44, 95% CI 1.38-1.50), with increased risk that correlated with increasing severity of hyponatremia. Association with postoperative mortality was particularly strong among hyponatremic patients with ASA scores of 1 or 2 and those undergoing nonemergency surgery.
Patients with preoperative hyponatremia were also found to have increased risk for all postoperative complications evaluated, with the exception of stroke. Limitations included the potential for unmeasured confounders and not being able to account for the role of medications used perioperatively. Research is needed to determine whether correcting preoperative hyponatremia lessens the risk of mortality and other postoperative complications.
Bottom line: Among patients undergoing major surgery, preoperative hyponatremia is a predictor of postoperative 30-day mortality and morbidity.
Citation: Leung AA, McAlister FA, Rogers SO, et al. Preoperative hyponatremia and perioperative complications. Arch Intern Med. 2012;172:1-8.
In This Edition
Literature At A Glance
A guide to this month’s studies
- Interventions that improve discharge handovers reviewed
- Duration of in-hospital cardiac resuscitation and survival rates
- Early sepsis intervention strategies to decrease mortality risk
- Hypoglycemia linked to increased mortality in critically ill
- Increased bleeding risk for cardiac patients
- Hospital-run vs. anesthesiologist-run preoperative clinics
- Postoperative delirium and cognitive impairment in cardiac patients
- Benefits of resuming anticoagulants after GI bleeding
- Preoperative hyponatremia and risk of perioperative mortality
Systematic Review Highlights Several Interventions That Improve Discharge Handovers
Clinical question: Do interventions to improve patient handovers at discharge have positive effects on patient care?
Background: The transition from hospital to primary care is often suboptimal and has been associated with unfavorable outcomes, including hospital readmission, increased healthcare utilization, and adverse drug events post-discharge. This review sought to characterize different types of interventions aimed at improving discharge handovers and to evaluate their effects.
Study design: Systematic review of randomized controlled trials.
Setting: Studies published from January 1990 to March 2011.
Synopsis: Review of published databases identified 36 randomized controlled studies on interventions to improve discharge handovers. Studies were blindly evaluated by two reviewers on quality, interventions, and outcomes. There was significant heterogeneity in interventions and outcomes; thus, statistical analysis was not possible. Most studies evaluated multicomponent interventions and had more than one outcome measure.
Of the 36 studies reviewed, 25 reported statistically significant improvements in outcomes, including reduced hospital utilization and improved continuity of care. Effective interventions included medication reconciliation; structured discharge information (facilitated by electronic resources); multidisciplinary discharge planning; shared involvement in arranging care between inpatient and outpatient physicians; and Web-based access to discharge information by the outpatient provider.
The complexity of the interventions and the heterogeneity of reported results did not allow for firm conclusions to be drawn regarding which specific interventions had the strongest effects.
Bottom line: Interventions that target the quality and safety of handovers between hospital and outpatient providers at discharge can significantly reduce hospital utilization and improve continuity of care.
Citation: Hesselink G, Schoonhoven L, Barach P, et al. Improving patient handovers from hospital to primary care: a systematic review. Ann Intern Med. 2012;157:417-428.
Longer Duration of In-Hospital Cardiac Resuscitation Associated with Increased Survival
Clinical question: Are prolonged cardiac resuscitation efforts associated with improved outcomes?
Background: There is little evidence or guidelines on how long to maintain resuscitative efforts during in-hospital cardiac arrest, leading to variation in practice. This study characterized patterns of resuscitation duration and relationship to the return of spontaneous circulation and survival to discharge.
Study design: Retrospective observational study.
Setting: Four hundred thirty-five U.S. hospitals reporting data to the American Heart Association’s Get With The Guidelines: Resuscitation registry.
Synopsis: Using duration of resuscitation in nonsurvivors as a surrogate for the tendency of a facility to perform prolonged efforts, hospitals were divided into quartiles. Overall, of 64,339 patients in the registry, 31,198 (48.5%) had return of circulation and 9,912 (15.4%) survived to discharge. Resuscitative efforts in nonsurvivors ranged from a median of 16 to 25 minutes between the lowest and highest quartiles.
There was a stepwise increase in the likelihood for patients to have return of spontaneous circulation and to survive to discharge between each quartile. Specifically, comparing shortest to longest, there was a significant adjusted odds ratio of 1.12 for both the return of circulation (P<0.0001) and survival to discharge (P=0.021). The survival benefit was most apparent for those with pulseless electrical activity or asystole as initial rhythms, as compared to ventricular tachycardia or fibrillation.
Limitations included the study’s observational design, which meant causality could not be determined. Additionally, the study did not account for the quality of resuscitative efforts (e.g. depth of chest compressions, adherence with guidelines), which might have influenced outcomes. Importantly, the study looked at survival to discharge, but it did not evaluate long-term survival or functional status post-discharge, which might better reflect the success of resuscitation.
Bottom line: Prolonged resuscitative efforts were observed to be associated with increased likelihood of return of spontaneous circulation and survival to discharge; this data might provide clinical guidance in determining when to stop resuscitation efforts.
Citation: Goldberger ZD, Chan PS, Berg RA, et al. Duration of resuscitation efforts and survival after in-hospital cardiac arrest: an observational study. Lancet. 2012;380:1473-1481.
Early Sepsis Intervention Strategies Decrease Mortality, Length of Stay, and Cost
Clinical question: For patients with sepsis or septic shock, what is the impact of a real-time comprehensive continuous quality-improvement (QI) initiative on in-hospital mortality, morbidity, and healthcare resource utilization in community and tertiary-care hospitals in the U.S.?
Background: Multiple single-center trials have demonstrated that early sepsis intervention strategies (early goal-directed therapy, resuscitation bundles) improve in-hospital mortality. Little is known about the effectiveness of incorporating these strategies into a real-time continuous QI initiative and implementing interventions across multiple sites simultaneously.
Study design: Pre-post at some sites and concurrent implementation design at other sites.
Setting: Five community and six-tertiary care U.S. hospitals.
Synopsis: The GENeralized Early Sepsis Intervention Strategies (GENESIS) project was a CQI initiative that combined several QI concepts with validated early sepsis interventions known as resuscitation bundles (RB). Continuous QI was implemented on patients with severe sepsis or septic shock in both before and after designs (eight hospitals), and in concurrent designs (three hospitals). The control group was comprised of historical controls treated before GENESIS and patients with incomplete implementation of RB, totaling 1,554 patients. The treatment group included patients treated after GENESIS and those with complete RB compliance, totaling 4,801 patients.
Compared with the control group, patients in the treatment group had a 33% decreased risk of in-hospital mortality (RR 0.67, 95% CI 0.63-0.72), an absolute decrease in hospital length of stay (LOS) by 5.1 days (20.7 days vs. 15.6 days, P<0.001) and a $47,923 reduction in total hospital charges (P<0.001). Limitations included the study design (not a prospective randomized trial), and the possibility of other concurrent unmeasured quality initiatives taking place at the study sites, which might have contributed to improved outcomes.
Bottom line: Early sepsis intervention strategies in the form of a comprehensive continuous QI initiative can decrease mortality, hospital LOS, and cost in both tertiary-care and community hospitals.
Citation: Cannon CM, Holthaus CV, Zubrow MT, et al. The GENESIS project (GENeralized Early Sepsis Intervention Strategies): a multicenter quality improvement collaborative. J Intensive Care Med. 2012; Aug 17. doi:10.1177/0885066612453025.
Hypoglycemia Associated with Increased Mortality in the Critically Ill
Clinical question: Is hypoglycemia associated with mortality in critically ill patients?
Background: Initial studies suggested that intensive glucose control reduces mortality in surgical ICU patients and reduces morbidity in medical ICU patients, but further studies have not supported these findings. Recent literature shows conflicting results on the effects of intense glucose control in critically ill patients.
Study design: Post-hoc analysis of the NICE-SUGAR study database.
Setting: ICUs in 42 hospitals in Australia, New Zealand, and Canada.
Synopsis: The NICE-SUGAR study was a multicenter trial that randomized 6,104 ICU patients to intensive (glucose 80 to 108 mg/dL) or conventional glucose control (≤180 mg/dL). Patients were followed for 90 days or until death, with death being the primary end point. Severe hypoglycemia (<40 mg/dL) was recorded in 6.8% of patients in the intensive glucose control group versus 0.5% in the conventional group. The study showed that intensive glucose control was associated with increased mortality among adult ICU patients.
Using the NICE-SUGAR database, the authors conducted a Cox regression analysis to examine the associations between hypoglycemia and death. A total of 2,714 patients had moderate hypoglycemia (glucose 41 to 70 mg/dL), and 223 patients had severe hypoglycemia. The hazard ratio for mortality was 1.41 (95% CI 1.21-1.62, P<0.001) for patients with moderate hypoglycemia and 2.10 (95% CI 1.59-2.77, P<0.001) for severe hypoglycemia, compared to patients without hypoglycemia.
These findings show a strong association between mortality and hypoglycemia but do not prove causality. Hospitalists caring for ICU patients must be aware that hypoglycemia is associated with mortality and focus on avoiding hypoglycemia. The American Diabetes Association currently recommends a target blood glucose level of 140 to 180 mg/dL for most critically ill patients.
Bottom line: Hypoglycemia (glucose <70 mg/dL) is associated with increased risk of mortality in ICU patients.
Citation: Finfer S, Chittock DR, Su SY, et al. Hypoglycemia and risk of death in critically ill patients. New Engl J Med. 2012;367(12):1108-1118.
Increased Bleeding Risk for Cardiac Patients on Multiple Antithrombotic Drugs
Clinical question: Is there an increased risk of bleeding in atrial fibrillation patients treated with multiple antithrombotic agents following acute myocardial infarction (MI) or percutaneous coronary intervention (PCI)?
Background: Current treatment for atrial fibrillation patients with MI or PCI includes vitamin K antagonist (VKA) therapy to prevent stroke and antiplatelet agents to prevent further coronary events. There are inconsistent findings on the safety and efficacy of combined therapy with VKA, aspirin, and clopidogrel, specifically with regard to bleeding risk.
Study design: Retrospective cohort study.
Setting: Nationwide registry in Denmark.
Synopsis: Using the National Patient Registry in Denmark, 11,480 patients with atrial fibrillation who were admitted for MI or PCI were identified. Patients were grouped by medication regimen, including monotherapy (aspirin, clopidogrel, or VKA), dual therapy (dual antiplatelet or VKA+antiplatelet), or triple therapy (VKA+aspirin+clopidogrel). The primary outcome was nonfatal or fatal bleeding within one year.
Patients receiving triple therapy had the highest rate of bleeding, with a crude incidence of 14.2 events per 100 person-years. Patients treated with VKA+aspirin+clopidogel were significantly more likely than those on VKA+antiplatelet (HR 1.47, 95% CI 1.04-2.08) or dual antiplatelet (HR 2.20, 95% CI 1.58-3.08) treatment to have a bleeding event within 90 days, and similar trends were seen at 90 to 360 days. There was no significant difference in thromboembolic events among patients on VKA+aspirin+clopidogrel versus VKA+antiplatelet therapy.
Only bleeding events that required hospitalization were recorded, which might underestimate the bleeding risks of these regimens. Additionally, INR levels were not determined, which could impact both bleeding and thromboembolic outcomes.
However, this study does suggest that there are significant bleeding risks among patients treated with triple therapy. Hospitalists should weigh the risks of thromboembolic events with bleeding risks in patients with atrial fibrillation and MI/PCI, and only prescribe VKA+aspirin+clopidogrel with these risks in mind.
Bottom line: Immediate and continued bleeding risk is increased in patients with atrial fibrillation admitted with PCI or MI who are placed on triple antithrombotic therapy with VKA+aspirin+clopidogrel.
Citation: Lamberts M, Olesen JB, Ruwald MH, et al. Bleeding after initiation of multiple antithrombotic drugs, including triple therapy, in atrial fibrillation patients following myocardial infarction and coronary intervention. Circulation. 2012;126:1185-1193.
Hospitalist-Run Preoperative Clinic Improves Outcomes in Complex Surgical Patients
Clinical question: Do hospitalist-run preoperative clinics improve outcomes for medically complex patients undergoing noncardiac surgery compared to traditional anesthesiologist-run preoperative clinics?
Background: Studies of perioperative medical consultation have shown inconsistent effects on quality of care, but preoperative medical consultation has only been evaluated in the immediate preoperative period (one day prior to surgery or less). Little is known about the impact of involving hospitalists earlier in the preoperative period.
Study design: Retrospective, pre-post study.
Setting: Veterans Affairs Greater Los Angeles Healthcare System (VAGLAHS).
Synopsis: In July 2004, the VAGLAHS Preoperative Clinic transitioned from being anesthesiologist-run to hospitalist-run. Mid-level providers were trained on preoperative medical assessment, and patients were only evaluated by anesthesia staff on the day of surgery, after they had been deemed medically acceptable for surgery. All patients seen in the clinic from July 2003 to July 2005 were included in the study. Period A included patients evaluated when anesthesia staff supervised the clinic. Period B included patients evaluated during the first year of the hospitalist-run system.
There were 1,101 patients with inpatient surgeries in Period A, and 1,126 patients in Period B. Mean length of stay (LOS) decreased to 5.28 days during the hospitalist-run model from 9.87 days during the anesthesiologist-run model. LOS reductions were most notable in patients with ASA scores of 3 or higher; LOS reductions were not seen in an internal control of surgical patients who were not evaluated in the preoperative clinic. Inpatient mortality was also reduced in Period B compared with Period A, to 4 cases (0.36%) from 14 cases (1.27%) (P=0.0158). Specific processes that led to improved outcomes for patients in Period B could not be identified. The VA study setting might limit the generalizability of the results.
Bottom line: A hospitalist-run preoperative clinic was associated with decreased LOS and inpatient mortality compared with a traditional anesthesiologist-run clinic.
Citation: Vazirani S, Lankarani-Fard A, Lian LJ, Stelzner M, Asch SM. Preoperative processes and outcomes after implementation of a hospitalist-run preoperative clinic. J Hosp Med. 2012 Sep 7. doi:10.1002/jhm.1968.
Delirium after Cardiac Surgery Associated with Prolonged Cognitive Impairment
Clinical question: Is postoperative delirium associated with decreased cognitive function in the first year after cardiac surgery?
Background: In general populations, delirium has been associated with long-term decline in cognitive ability. Delirium and cognitive dysfunction are both common following cardiac surgery, but the effects of postoperative delirium on the trajectory of cognitive function over time is unclear.
Study design: Prospective cohort study.
Setting: Two academic medical centers and a Veterans Administration hospital.
Synopsis: Two hundred twenty-five patients aged 60 or older who were scheduled to undergo coronary artery bypass grafting or valve replacement surgery were included. Patients underwent preoperative assessment cognitive function with the use of the Mini-Mental State Examination (MMSE). Starting on postoperative Day 2, patients underwent daily assessment for delirium. After discharge, cognitive function was reassessed at months one, six, and 12.
Postoperative delirium occurred in 103 patients (46%). Patients with delirium were older, had higher comorbidity scores, and had lower MMSE scores at baseline. Among the overall study population, adjusted MMSE scores dropped 4.6 points from baseline to postoperative Day 2, then were observed to increase by approximately one point per day during postoperative days 3 to 5 with minimal change thereafter. Patients with delirium had greater decrease in cognitive function in the immediate postoperative period compared to patients without delirium (7.7 points vs. 2.1, P<0.001).
Patients without delirium returned to their baseline cognitive ability by one month postoperatively, while patients who had delirium were still making gains up to six months post-operatively, never returning to baseline level of function by one year. Unmeasured confounders and uncertain sensitivity of the MMSE to detect mild cognitive impairment might limit these findings.
Bottom line: Cognitive function decreases in the immediate postoperative period following cardiac surgery. Compared to patients without delirium, patients with delirium experience more dramatic and prolonged cognitive impairment postoperatively, without returning to their preoperative level of cognitive function at one year.
Citation: Saczynski JS, Marcantonio ER, Quach L, et al. Cognitive trajectories after postoperative delirium. New Engl J Med. 2012;367:30-39.
Benefits of Resuming Anticoagulation after GI Bleed Outweigh Risks for Most Patients
Clinical question: In warfarin-treated patients who have experienced gastrointestinal (GI) bleeding, what are the patterns of restarting warfarin therapy and the incidence of thrombosis, recurrent GI bleed, and death in the 90 days following index bleed?
Background: In warfarin-treated patients who experience GI bleeding, warfarin is often temporarily held or permanently discontinued, placing patients at increased risk for developing thromboembolism. Little is known about the risks, benefits, and timing of restarting warfarin in this patient population.
Study design: Retrospective cohort study.
Setting: Kaiser Permanente Colorado.
Synopsis: Using clinical and administrative databases, 442 patients who presented with GI bleeding while receiving warfarin therapy were identified. Patients were grouped by whether they resumed warfarin (n=260, including 41 patients in whom anticoagulation was never interrupted), or did not resume warfarin therapy (n=182) in the 90 days following index GI bleed. Patients with prosthetic heart valves or GI bleeding localized to the rectum/anus were more commonly restarted on warfarin, whereas older patients and those in whom the source of bleeding was not identified were less likely to be restarted on warfarin therapy.
Restarting warfarin therapy after index GI bleed was associated with lower risk of thrombosis (HR 0.05, 95% CI 0.01-0.58) and death from any cause (HR 0.31, 95% CI 0.15-0.62), and it was not associated with a significant increase in risk for recurrent GI bleed (HR 1.32, 95% CI 0.50-3.57).
The authors concluded that for many patients who experience a warfarin-associated GI bleed, the benefits of restarting warfarin therapy outweigh the risks. No conclusions were made regarding the optimal timing of resuming therapy. Limitations included the use of administrative data and inability to determine the potential influence of aspirin use on outcomes.
Bottom line: Resuming warfarin in the 90 days following a warfarin-associated GI bleed is associated with decreased risk of thrombosis and death without increased risk for recurrent GI bleed.
Citation: Witt DM, Delate T, Garcia DA, et al. Risk of thromboembolism, recurrent hemorrhage, and death after warfarin therapy interruption for gastrointestinal tract bleeding. Arch Intern Med. 2012 Sep 12. doi:10.1001/archinternmed.2012.4261.
Preoperative Hyponatremia Associated with Increased Risk for Perioperative Complications and Mortality
Clinical question: Is preoperative hyponatremia an indicator of perioperative morbidity and mortality?
Background: Hyponatremia is a common diagnosis in the hospital setting and is associated with adverse outcomes, even in mild cases. However, it is unclear if this association exists in surgical patients when detected preoperatively.
Study design: Retrospective cohort study.
Setting: Academic and community hospitals participating in the American College of Surgeons National Surgical Quality Improvement Program (NSQIP).
Synopsis: A total of 75,423 adult patients with hyponatremia (sodium <135 mEq/L) who were undergoing major surgery were compared to 888,840 patients with normal preoperative sodium levels over a six-year period. The primary outcome was 30-day mortality. Secondary outcomes included postoperative major coronary events, stroke, wound infection, pneumonia, and length of stay (LOS).
Compared to patients with normal sodium levels, those with preoperative hyponatremia had higher rates of perioperative mortality (5.2% vs. 1.3%; adjusted odds ratio 1.44, 95% CI 1.38-1.50), with increased risk that correlated with increasing severity of hyponatremia. Association with postoperative mortality was particularly strong among hyponatremic patients with ASA scores of 1 or 2 and those undergoing nonemergency surgery.
Patients with preoperative hyponatremia were also found to have increased risk for all postoperative complications evaluated, with the exception of stroke. Limitations included the potential for unmeasured confounders and not being able to account for the role of medications used perioperatively. Research is needed to determine whether correcting preoperative hyponatremia lessens the risk of mortality and other postoperative complications.
Bottom line: Among patients undergoing major surgery, preoperative hyponatremia is a predictor of postoperative 30-day mortality and morbidity.
Citation: Leung AA, McAlister FA, Rogers SO, et al. Preoperative hyponatremia and perioperative complications. Arch Intern Med. 2012;172:1-8.
In the Literature: Research You Need to Know
Clinical question: What is the relationship between well-being and demographic factors, educational debt, and medical knowledge in internal-medicine residents?
Background: Physician distress during training is common and can negatively impact patient care. There has never been a study of internal-medicine residents nationally that examined the patterns of distress across demographic factors or the association of these factors with medical knowledge.
Study design: Cross-sectional study.
Setting: U.S. internal-medicine residency programs.
Synopsis: Of the 21,208 U.S. internal-medicine residents who completed the 2008 in-training examination, 77.3% had both survey and demographic data available for analysis. Nearly 15% of these 16,394 residents rated quality of life “as bad as it can be” or “somewhat bad,” and 32.9% felt somewhat or very dissatisfied with work-life balance.
Overall burnout, high levels of weekly emotional exhaustion, and weekly depersonalization were reported by 51.5%, 45.8%, and 28.9% of residents, respectively. Symptoms of emotional exhaustion decreased as training increased, while depersonalization increased after the first postgraduate year. Residents reporting quality of life “as bad as it can be,” emotional exhaustion, or debt greater than $200,000 had mean exam scores 2.7, 4.2, and 5 points, respectively, lower than others surveyed.
Although unlikely given the study design, nonresponse bias could affect these results. Not all demographic variables or domains of well-being were studied, and self-reported educational debt could have been misclassified. Nonetheless, findings suggest that distress remains among residents despite the changes made to duty-hour regulations in 2003.
Bottom line: Suboptimal quality of life and burnout were common among internal-medicine residents nationally; symptoms of burnout were associated with higher debt and lower exam scores.
Citation: West CP, Shanafelt TD, Kolars JC. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA. 2011;306:952-960.
Visit our website for more physician reviews of HM-related research.
Clinical question: What is the relationship between well-being and demographic factors, educational debt, and medical knowledge in internal-medicine residents?
Background: Physician distress during training is common and can negatively impact patient care. There has never been a study of internal-medicine residents nationally that examined the patterns of distress across demographic factors or the association of these factors with medical knowledge.
Study design: Cross-sectional study.
Setting: U.S. internal-medicine residency programs.
Synopsis: Of the 21,208 U.S. internal-medicine residents who completed the 2008 in-training examination, 77.3% had both survey and demographic data available for analysis. Nearly 15% of these 16,394 residents rated quality of life “as bad as it can be” or “somewhat bad,” and 32.9% felt somewhat or very dissatisfied with work-life balance.
Overall burnout, high levels of weekly emotional exhaustion, and weekly depersonalization were reported by 51.5%, 45.8%, and 28.9% of residents, respectively. Symptoms of emotional exhaustion decreased as training increased, while depersonalization increased after the first postgraduate year. Residents reporting quality of life “as bad as it can be,” emotional exhaustion, or debt greater than $200,000 had mean exam scores 2.7, 4.2, and 5 points, respectively, lower than others surveyed.
Although unlikely given the study design, nonresponse bias could affect these results. Not all demographic variables or domains of well-being were studied, and self-reported educational debt could have been misclassified. Nonetheless, findings suggest that distress remains among residents despite the changes made to duty-hour regulations in 2003.
Bottom line: Suboptimal quality of life and burnout were common among internal-medicine residents nationally; symptoms of burnout were associated with higher debt and lower exam scores.
Citation: West CP, Shanafelt TD, Kolars JC. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA. 2011;306:952-960.
Visit our website for more physician reviews of HM-related research.
Clinical question: What is the relationship between well-being and demographic factors, educational debt, and medical knowledge in internal-medicine residents?
Background: Physician distress during training is common and can negatively impact patient care. There has never been a study of internal-medicine residents nationally that examined the patterns of distress across demographic factors or the association of these factors with medical knowledge.
Study design: Cross-sectional study.
Setting: U.S. internal-medicine residency programs.
Synopsis: Of the 21,208 U.S. internal-medicine residents who completed the 2008 in-training examination, 77.3% had both survey and demographic data available for analysis. Nearly 15% of these 16,394 residents rated quality of life “as bad as it can be” or “somewhat bad,” and 32.9% felt somewhat or very dissatisfied with work-life balance.
Overall burnout, high levels of weekly emotional exhaustion, and weekly depersonalization were reported by 51.5%, 45.8%, and 28.9% of residents, respectively. Symptoms of emotional exhaustion decreased as training increased, while depersonalization increased after the first postgraduate year. Residents reporting quality of life “as bad as it can be,” emotional exhaustion, or debt greater than $200,000 had mean exam scores 2.7, 4.2, and 5 points, respectively, lower than others surveyed.
Although unlikely given the study design, nonresponse bias could affect these results. Not all demographic variables or domains of well-being were studied, and self-reported educational debt could have been misclassified. Nonetheless, findings suggest that distress remains among residents despite the changes made to duty-hour regulations in 2003.
Bottom line: Suboptimal quality of life and burnout were common among internal-medicine residents nationally; symptoms of burnout were associated with higher debt and lower exam scores.
Citation: West CP, Shanafelt TD, Kolars JC. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA. 2011;306:952-960.
Visit our website for more physician reviews of HM-related research.
What Is the Appropriate Use of Antibiotics In Acute Exacerbations of COPD?
Case
A 58-year-old male smoker with moderate chronic obstructive pulmonary disease (COPD) (FEV1 56% predicted) is admitted with an acute exacerbation of COPD for the second time this year. He presented to the ED with increased productive cough and shortness of breath, similar to prior exacerbations. He denies fevers, myalgias, or upper-respiratory symptoms. Physical exam is notable for bilateral inspiratory and expiratory wheezing. His sputum is purulent. He is given continuous nebulizer therapy and one dose of oral prednisone, but his dyspnea and wheezing persist. Chest X-ray does not reveal an infiltrate.
Should this patient be treated with antibiotics and, if so, what regimen is most appropriate?
Overview
Acute exacerbations of COPD (AECOPD) present a major health burden, accounting for more than 2.4% of all hospital admissions and causing significant morbidity, mortality, and costs.1 During 2006 and 2007, COPD mortality in the United States topped 39 deaths per 100,000 people, and more recently, hospital costs related to COPD were expected to exceed $13 billion annually.2 Patients with AECOPD also experience decreased quality of life and faster decline in pulmonary function, further highlighting the need for timely and appropriate treatment.1
Several guidelines have proposed treatment strategies now considered standard of care in AECOPD management.3,4,5,6 These include the use of corticosteroids, bronchodilator agents, and, in select cases, antibiotics. While there is well-established evidence for the use of steroids and bronchodilators in AECOPD, the debate continues over the appropriate use of antibiotics in the treatment of acute exacerbations. There are multiple potential factors leading to AECOPD, including viruses, bacteria, and common pollutants; as such, antibiotic treatment may not be indicated for all patients presenting with exacerbations. Further, the risks of antibiotic treatment—including adverse drug events, selection for drug-resistant bacteria, and associated costs—are not insignificant.
However, bacterial infections do play a role in approximately 50% of patients with AECOPD and, for this population, use of antibiotics may confer important benefits.7
Interestingly, a retrospective cohort study of 84,621 patients admitted for AECOPD demonstrated that 85% of patients received antibiotics at some point during hospitalization.8
Support for Antibiotics
Several randomized trials have compared clinical outcomes in patients with AECOPD who have received antibiotics versus those who received placebos. Most of these had small sample sizes and studied only ββ-lactam and tetracycline antibiotics in an outpatient setting; there are limited data involving inpatients and newer drugs. Nevertheless, antibiotic treatment has been associated with decreased risk of adverse outcomes in AECOPD.
One meta-analysis demonstrated that antibiotics reduced treatment failures by 66% and in-hospital mortality by 78% in the subset of trials involving hospitalized patients.8 Similarly, analysis of a large retrospective cohort of patients hospitalized for AECOPD found a significantly lower risk of treatment failure in antibiotic-treated versus untreated patients.9 Specifically, treated patients had lower rates of in-hospital mortality and readmission for AECOPD and a lower likelihood of requiring subsequent mechanical ventilation during the index hospitalization.
Data also suggest that antibiotic treatment during exacerbations might favorably impact subsequent exacerbations.10 A retrospective study of 18,928 Dutch patients with AECOPD compared outcomes among patients who had received antibiotics (most frequently doxycycline or a penicillin) as part of their therapy to those who did not. The authors demonstrated that the median time to the next exacerbation was significantly longer in the patients receiving antibiotics.10 Further, both mortality and overall risk of developing a subsequent exacerbation were significantly decreased in the antibiotic group, with median follow-up of approximately two years.
Indications for Antibiotics
Clinical symptoms. A landmark study by Anthonisen and colleagues set forth three clinical criteria that have formed the basis for treating AECOPD with antibiotics in subsequent studies and in clinical practice.11 Often referred to as the “cardinal symptoms” of AECOPD, these include increased dyspnea, sputum volume, and sputum purulence. In this study, 173 outpatients with COPD were randomized to a 10-day course of antibiotics or placebo at onset of an exacerbation and followed clinically. The authors found that antibiotic-treated patients were significantly more likely than the placebo group to achieve treatment success, defined as resolution of all exacerbated symptoms within 21 days (68.1% vs. 55.0%, P<0.01).
Importantly, treated patients were also significantly less likely to experience clinical deterioration after 72 hours (9.9% vs. 18.9%, P<0.05). Patients with Type I exacerbations, characterized by all three cardinal symptoms, were most likely to benefit from antibiotic therapy, followed by patients with Type II exacerbations, in whom only two of the symptoms were present. Subsequent studies have suggested that sputum purulence correlates well with the presence of acute bacterial infection and therefore may be a reliable clinical indicator of patients who are likely to benefit from antibiotic therapy.12
Laboratory data. While sputum purulence is associated with bacterial infection, sputum culture is less reliable, as pathogenic bacteria are commonly isolated from patients with both AECOPD and stable COPD. In fact, the prevalence of bacterial colonization in moderate to severe COPD might be as high as 50%.13 Therefore, a positive bacterial sputum culture, in the absence of purulence or other signs of infection, is not recommended as the sole basis for which to prescribe antibiotics.
Serum biomarkers, most notably C-reactive protein (CRP) and procalcitonin, have been studied as a newer approach to identify patients who might benefit from antibiotic therapy for AECOPD. Studies have demonstrated increased CRP levels during AECOPD, particularly in patients with purulent sputum and positive bacterial sputum cultures.12 Procalcitonin is preferentially elevated in bacterial infections.
One randomized, placebo-controlled trial in hospitalized patients with AECOPD demonstrated a significant reduction in antibiotic usage based on low procalcitonin levels, without negatively impacting clinical success rate, hospital mortality, subsequent antibiotic needs, or time to next exacerbation.14 However, due to inconsistent evidence, use of these markers to guide antibiotic administration in AECOPD has not yet been definitively established.14,15 Additionally, these laboratory results are often not available at the point of care, potentially limiting their utility in the decision to initiate antibiotics.
Severity of illness. Severity of illness is an important factor in the decision to treat AECOPD with antibiotics. Patients with advanced, underlying airway obstruction, as measured by FEV1, are more likely to have a bacterial cause of AECOPD.16 Additionally, baseline clinical characteristics including advanced age and comorbid conditions, particularly cardiovascular disease and diabetes, increase the risk of severe exacerbations.17
One meta-analysis of placebo-controlled trials found that patients with severe exacerbations were likely to benefit from antibiotic therapy, while patients with mild or moderate exacerbations had no reduction in treatment failure or mortality rates.18 Patients presenting with acute respiratory failure necessitating intensive care and/or ventilator support (noninvasive or invasive) have also been shown to benefit from antibiotics.19
Current clinical guidelines vary slightly in their recommendations regarding when to give antibiotics in AECOPD (see Table 1). However, existing evidence favors antibiotic treatment for those patients presenting with two or three cardinal symptoms, specifically those with increased sputum purulence, and those with severe disease (i.e. pre-existing advanced airflow obstruction and/or exacerbations requiring mechanical ventilation). Conversely, studies have shown that many patients, particularly those with milder exacerbations, experience resolution of symptoms without antibiotic treatment.11,18
Antibiotic Choice in AECOPD
Risk stratification. In patients likely to benefit from antibiotic therapy, an understanding of the relationship between severity of COPD, host risk factors for poor outcomes, and microbiology is paramount to guide clinical decision-making. Historically, such bacteria as Haemophilus influenzae, Streptococcus pneumoniae, and Moraxella catarrhalis have been implicated in the pathogenesis of AECOPD.3,7 In patients with simple exacerbations, antibiotics that target these pathogens should be used (see Table 2).
However, patients with more severe underlying airway obstruction (i.e. FEV1<50%) and risk factors for poor outcomes, specifically recent hospitalization (≥2 days during the previous 90 days), frequent antibiotics (>3 courses during the previous year), and severe exacerbations are more likely to be infected with resistant strains or gram-negative organisms.3,7 Pseudomonas aeruginosa, in particular, is of increasing concern in this population. In patients with complicated exacerbations, more broad-coverage, empiric antibiotics should be initiated (see Table 2).
With this in mind, patients meeting criteria for treatment must first be stratified according to the severity of COPD and risk factors for poor outcomes before a decision regarding a specific antibiotic is reached. Figure 1 outlines a recommended approach for antibiotic administration in AECOPD. The optimal choice of antibiotics must consider cost-effectiveness, local patterns of antibiotic resistance, tissue penetration, patient adherence, and risk of such adverse drug events as diarrhea.
Comparative effectiveness. Current treatment guidelines do not favor the use of any particular antibiotic in simple AECOPD.3,4,5,6 However, as selective pressure has led to in vitro resistance to antibiotics traditionally considered first-line (e.g. doxycycline, trimethoprim/sulfamethoxazole, amoxicillin), the use of second-line antibiotics (e.g. fluoroquinolones, macrolides, cephalosporins, β-lactam/ β-lactamase inhibitors) has increased. Consequently, several studies have compared the effectiveness of different antimicrobial regimens.
One meta-analysis found that second-line antibiotics, when compared with first-line agents, provided greater clinical improvement to patients with AECOPD, without significant differences in mortality, microbiologic eradication, or incidence of adverse drug events.20 Among the subgroup of trials enrolling hospitalized patients, the clinical effectiveness of second-line agents remained significantly greater than that of first-line agents.
Another meta-analysis compared trials that studied only macrolides, quinolones, and amoxicillin-clavulanate and found no difference in terms of short-term clinical effectiveness; however, there was weak evidence to suggest that quinolones were associated with better microbiological success and fewer recurrences of AECOPD.21 Fluoroquinolones are preferred in complicated cases of AECOPD in which there is a greater risk for enterobacteriaceae and Pseudomonas species.3,7
Antibiotic Duration
The duration of antibiotic therapy in AECOPD has been studied extensively, with randomized controlled trials consistently demonstrating no additional benefit to courses extending beyond five days. One meta-analysis of 21 studies found similar clinical and microbiologic cure rates among patients randomized to antibiotic treatment for ≤5 days versus >5 days.22 A subgroup analysis of the trials evaluating different durations of the same antibiotic also demonstrated no difference in clinical effectiveness, and this finding was confirmed in a separate meta-analysis.22,23
Advantages to shorter antibiotic courses include improved compliance and decreased rates of resistance. The usual duration of antibiotic therapy is three to seven days, depending upon the response to therapy.3
Back to the Case
As the patient has no significant comorbidities or risk factors, and meets criteria for a simple Anthonisen Type I exacerbation (increased dyspnea, sputum, and sputum purulence), antibiotic therapy with trimethoprim/sulfamethoxazole is initiated on admission, in addition to the previously started steroid and bronchodilator treatments. The patient’s clinical status improves, and he is discharged on hospital Day 3 with a prescription to complete a five-day course of antibiotics.
Bottom Line
Antibiotic therapy is effective in select AECOPD patients, with maximal benefits obtained when the decision to treat is based on careful consideration of characteristic clinical symptoms and severity of illness. Choice and duration of antibiotics should follow likely bacterial causes and current guidelines.
Dr. Cunningham is an assistant professor of internal medicine and academic hospitalist in the section of hospital medicine at Vanderbilt University School of Medicine in Nashville, Tenn. Dr. LaBrin is assistant professor of internal medicine and pediatrics and an academic hospitalist at Vanderbilt. Dr. Markley is a clinical instructor and academic hospitalist at Vanderbilt.
References
- Donaldson GC, Wedzicha JA. COPD exacerbations: 1. Epidemiology. Thorax. 2006;61:164-168.
- National Heart, Lung, and Blood Institute. 2009 NHLBI Morbidity and Mortality Chartbook. National Heart, Lung, and Blood Institute website. Available at: http://www.nhlbi.nih.gov/resources/docs/cht-book.htm Accessed Oct. 10, 2011.
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease. Global Initiative for Chronic Obstructive Lung Disease (GOLD) website. Available at: www.goldcopd.org/guidelines-resources.html Accessed Oct. 10, 2011.
- Celli BR, MacNee W, Agusti A, et al. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Resp J. 2004;23:932-946.
- National Clinical Guideline Centre. Chronic obstructive pulmonary disease: management of chronic obstructive pulmonary disease in adults in primary and secondary care. National Institute for Health and Clinical Excellence website. Available at: http://guidance.nice.org.uk/CG101/Guidance/pdf/English. Accessed Oct. 10, 2011.
- O’Donnell DE, Aaron S, Bourbeau J, et al. Canadian Thoracic Society recommendations for management of chronic obstructive pulmonary disease—2007 update. Can Respir J. 2007;14(Suppl B):5B-32B.
- Sethi S, Murphy TF. Infection in the pathogenesis and course of chronic obstructive pulmonary disease. N Engl J Med. 2008;359:2355-2565.
- Quon BS, Qi Gan W, Sin DD. Contemporary management of acute exacerbations of COPD: a systematic review and metaanalysis. Chest. 2008;133:756-766.
- Rothberg MB, Pekow PS, Lahti M, Brody O, Skiest DJ, Lindenauer PK. Antibiotic therapy and treatment failure in patients hospitalized for acute exacerbations of chronic obstructive pulmonary disease. JAMA. 2010;303:2035-2042.
- Roede BM, Bresser P, Bindels PJE, et al. Antibiotic treatment is associated with reduced risk of subsequent exacerbation in obstructive lung disease: a historical population based cohort study. Thorax. 2008;63:968-973.
- Anthonisen NR, Manfreda J, Warren CP, Hershfield ES, Harding GKM, Nelson NA. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med. 1987;106:196-204.
- Stockley RA, O’Brien C, Pye A, Hill SL. Relationship of sputum color to nature and outpatient management of acute exacerbations of COPD. Chest. 2000;117:1638-1645.
- Rosell A, Monso E, Soler N, et al. Microbiologic determinants of exacerbation in chronic obstructive pulmonary disease. Arch Intern Med. 2005; 165:891-897.
- Stolz D, Christ-Crain M, Bingisser R, et al. Antibiotic treatment of exacerbations of COPD: a randomized, controlled trial comparing procalcitonin-guidance with standard therapy. Chest. 2007;131:9-19.
- Daniels JMA, Schoorl M, Snijders D, et al. Procalcitonin vs C-reactive protein as predictive markers of response to antibiotic therapy in acute exacerbations of COPD. Chest. 2010;138:1108-1015.
- Miravitlles M, Espinosa C, Fernandez-Laso E, Martos JA, Maldonado JA, Gallego M. Relationship between bacterial flora in sputum and functional impairment in patients with acute exacerbations of COPD. Chest. 1999;116:40-46.
- Patil SP, Krishnan JA, Lechtzin N, Diette GB. In-hospital mortality following acute exacerbations of chronic obstructive pulmonary disease. Arch Intern Med. 2003;163:1180-1186.
- Puhan MA, Vollenweider D, Latshang T, Steurer J, Steurer-Stey C. Exacerbations of chronic obstructive lung disease: when are antibiotics indicated? A systematic review. Resp Res. 2007;8:30-40.
- Nouira S, Marghli S, Belghith M, Besbes L, Elatrous S, Abroug F. Once daily ofloxacin in chronic obstructive pulmonary disease exacerbation requiring mechanical ventilation: a randomized placebo-controlled trial. Lancet. 2001;358:2020-2025.
- Dimopoulos G, Siempos II, Korbila IP, Manta KG, Falagas ME. Comparison of first-line with second-line antibiotics for acute exacerbations of chronic bronchitis: a metaanalysis of randomized controlled trials. Chest. 2007;132:447-455.
- Siempos II, Dimopoulos G, Korbila IP, Manta KG, Falagas ME. Macrolides, quinolones and amoxicillin/clavulanate for chronic bronchitis: a meta-analysis. Eur Resp J. 2007;29:1127-1137.
- El-Moussaoui, Roede BM, Speelman P, Bresser P, Prins JM, Bossuyt PMM. Short-course antibiotic treatment in acute exacerbations of chronic bronchitis and COPD: a meta-analysis of double-blind studies. Thorax. 2008;63:415-422.
- Falagas ME, Avgeri SG, Matthaiou DK, Dimopoulos G, Siempos II. Short- versus long-duration antimicrobial treatment for exacerbations of chronic bronchitis: a meta-analysis. J Antimicrob Chemother. 2008;62:442-450.
Case
A 58-year-old male smoker with moderate chronic obstructive pulmonary disease (COPD) (FEV1 56% predicted) is admitted with an acute exacerbation of COPD for the second time this year. He presented to the ED with increased productive cough and shortness of breath, similar to prior exacerbations. He denies fevers, myalgias, or upper-respiratory symptoms. Physical exam is notable for bilateral inspiratory and expiratory wheezing. His sputum is purulent. He is given continuous nebulizer therapy and one dose of oral prednisone, but his dyspnea and wheezing persist. Chest X-ray does not reveal an infiltrate.
Should this patient be treated with antibiotics and, if so, what regimen is most appropriate?
Overview
Acute exacerbations of COPD (AECOPD) present a major health burden, accounting for more than 2.4% of all hospital admissions and causing significant morbidity, mortality, and costs.1 During 2006 and 2007, COPD mortality in the United States topped 39 deaths per 100,000 people, and more recently, hospital costs related to COPD were expected to exceed $13 billion annually.2 Patients with AECOPD also experience decreased quality of life and faster decline in pulmonary function, further highlighting the need for timely and appropriate treatment.1
Several guidelines have proposed treatment strategies now considered standard of care in AECOPD management.3,4,5,6 These include the use of corticosteroids, bronchodilator agents, and, in select cases, antibiotics. While there is well-established evidence for the use of steroids and bronchodilators in AECOPD, the debate continues over the appropriate use of antibiotics in the treatment of acute exacerbations. There are multiple potential factors leading to AECOPD, including viruses, bacteria, and common pollutants; as such, antibiotic treatment may not be indicated for all patients presenting with exacerbations. Further, the risks of antibiotic treatment—including adverse drug events, selection for drug-resistant bacteria, and associated costs—are not insignificant.
However, bacterial infections do play a role in approximately 50% of patients with AECOPD and, for this population, use of antibiotics may confer important benefits.7
Interestingly, a retrospective cohort study of 84,621 patients admitted for AECOPD demonstrated that 85% of patients received antibiotics at some point during hospitalization.8
Support for Antibiotics
Several randomized trials have compared clinical outcomes in patients with AECOPD who have received antibiotics versus those who received placebos. Most of these had small sample sizes and studied only ββ-lactam and tetracycline antibiotics in an outpatient setting; there are limited data involving inpatients and newer drugs. Nevertheless, antibiotic treatment has been associated with decreased risk of adverse outcomes in AECOPD.
One meta-analysis demonstrated that antibiotics reduced treatment failures by 66% and in-hospital mortality by 78% in the subset of trials involving hospitalized patients.8 Similarly, analysis of a large retrospective cohort of patients hospitalized for AECOPD found a significantly lower risk of treatment failure in antibiotic-treated versus untreated patients.9 Specifically, treated patients had lower rates of in-hospital mortality and readmission for AECOPD and a lower likelihood of requiring subsequent mechanical ventilation during the index hospitalization.
Data also suggest that antibiotic treatment during exacerbations might favorably impact subsequent exacerbations.10 A retrospective study of 18,928 Dutch patients with AECOPD compared outcomes among patients who had received antibiotics (most frequently doxycycline or a penicillin) as part of their therapy to those who did not. The authors demonstrated that the median time to the next exacerbation was significantly longer in the patients receiving antibiotics.10 Further, both mortality and overall risk of developing a subsequent exacerbation were significantly decreased in the antibiotic group, with median follow-up of approximately two years.
Indications for Antibiotics
Clinical symptoms. A landmark study by Anthonisen and colleagues set forth three clinical criteria that have formed the basis for treating AECOPD with antibiotics in subsequent studies and in clinical practice.11 Often referred to as the “cardinal symptoms” of AECOPD, these include increased dyspnea, sputum volume, and sputum purulence. In this study, 173 outpatients with COPD were randomized to a 10-day course of antibiotics or placebo at onset of an exacerbation and followed clinically. The authors found that antibiotic-treated patients were significantly more likely than the placebo group to achieve treatment success, defined as resolution of all exacerbated symptoms within 21 days (68.1% vs. 55.0%, P<0.01).
Importantly, treated patients were also significantly less likely to experience clinical deterioration after 72 hours (9.9% vs. 18.9%, P<0.05). Patients with Type I exacerbations, characterized by all three cardinal symptoms, were most likely to benefit from antibiotic therapy, followed by patients with Type II exacerbations, in whom only two of the symptoms were present. Subsequent studies have suggested that sputum purulence correlates well with the presence of acute bacterial infection and therefore may be a reliable clinical indicator of patients who are likely to benefit from antibiotic therapy.12
Laboratory data. While sputum purulence is associated with bacterial infection, sputum culture is less reliable, as pathogenic bacteria are commonly isolated from patients with both AECOPD and stable COPD. In fact, the prevalence of bacterial colonization in moderate to severe COPD might be as high as 50%.13 Therefore, a positive bacterial sputum culture, in the absence of purulence or other signs of infection, is not recommended as the sole basis for which to prescribe antibiotics.
Serum biomarkers, most notably C-reactive protein (CRP) and procalcitonin, have been studied as a newer approach to identify patients who might benefit from antibiotic therapy for AECOPD. Studies have demonstrated increased CRP levels during AECOPD, particularly in patients with purulent sputum and positive bacterial sputum cultures.12 Procalcitonin is preferentially elevated in bacterial infections.
One randomized, placebo-controlled trial in hospitalized patients with AECOPD demonstrated a significant reduction in antibiotic usage based on low procalcitonin levels, without negatively impacting clinical success rate, hospital mortality, subsequent antibiotic needs, or time to next exacerbation.14 However, due to inconsistent evidence, use of these markers to guide antibiotic administration in AECOPD has not yet been definitively established.14,15 Additionally, these laboratory results are often not available at the point of care, potentially limiting their utility in the decision to initiate antibiotics.
Severity of illness. Severity of illness is an important factor in the decision to treat AECOPD with antibiotics. Patients with advanced, underlying airway obstruction, as measured by FEV1, are more likely to have a bacterial cause of AECOPD.16 Additionally, baseline clinical characteristics including advanced age and comorbid conditions, particularly cardiovascular disease and diabetes, increase the risk of severe exacerbations.17
One meta-analysis of placebo-controlled trials found that patients with severe exacerbations were likely to benefit from antibiotic therapy, while patients with mild or moderate exacerbations had no reduction in treatment failure or mortality rates.18 Patients presenting with acute respiratory failure necessitating intensive care and/or ventilator support (noninvasive or invasive) have also been shown to benefit from antibiotics.19
Current clinical guidelines vary slightly in their recommendations regarding when to give antibiotics in AECOPD (see Table 1). However, existing evidence favors antibiotic treatment for those patients presenting with two or three cardinal symptoms, specifically those with increased sputum purulence, and those with severe disease (i.e. pre-existing advanced airflow obstruction and/or exacerbations requiring mechanical ventilation). Conversely, studies have shown that many patients, particularly those with milder exacerbations, experience resolution of symptoms without antibiotic treatment.11,18
Antibiotic Choice in AECOPD
Risk stratification. In patients likely to benefit from antibiotic therapy, an understanding of the relationship between severity of COPD, host risk factors for poor outcomes, and microbiology is paramount to guide clinical decision-making. Historically, such bacteria as Haemophilus influenzae, Streptococcus pneumoniae, and Moraxella catarrhalis have been implicated in the pathogenesis of AECOPD.3,7 In patients with simple exacerbations, antibiotics that target these pathogens should be used (see Table 2).
However, patients with more severe underlying airway obstruction (i.e. FEV1<50%) and risk factors for poor outcomes, specifically recent hospitalization (≥2 days during the previous 90 days), frequent antibiotics (>3 courses during the previous year), and severe exacerbations are more likely to be infected with resistant strains or gram-negative organisms.3,7 Pseudomonas aeruginosa, in particular, is of increasing concern in this population. In patients with complicated exacerbations, more broad-coverage, empiric antibiotics should be initiated (see Table 2).
With this in mind, patients meeting criteria for treatment must first be stratified according to the severity of COPD and risk factors for poor outcomes before a decision regarding a specific antibiotic is reached. Figure 1 outlines a recommended approach for antibiotic administration in AECOPD. The optimal choice of antibiotics must consider cost-effectiveness, local patterns of antibiotic resistance, tissue penetration, patient adherence, and risk of such adverse drug events as diarrhea.
Comparative effectiveness. Current treatment guidelines do not favor the use of any particular antibiotic in simple AECOPD.3,4,5,6 However, as selective pressure has led to in vitro resistance to antibiotics traditionally considered first-line (e.g. doxycycline, trimethoprim/sulfamethoxazole, amoxicillin), the use of second-line antibiotics (e.g. fluoroquinolones, macrolides, cephalosporins, β-lactam/ β-lactamase inhibitors) has increased. Consequently, several studies have compared the effectiveness of different antimicrobial regimens.
One meta-analysis found that second-line antibiotics, when compared with first-line agents, provided greater clinical improvement to patients with AECOPD, without significant differences in mortality, microbiologic eradication, or incidence of adverse drug events.20 Among the subgroup of trials enrolling hospitalized patients, the clinical effectiveness of second-line agents remained significantly greater than that of first-line agents.
Another meta-analysis compared trials that studied only macrolides, quinolones, and amoxicillin-clavulanate and found no difference in terms of short-term clinical effectiveness; however, there was weak evidence to suggest that quinolones were associated with better microbiological success and fewer recurrences of AECOPD.21 Fluoroquinolones are preferred in complicated cases of AECOPD in which there is a greater risk for enterobacteriaceae and Pseudomonas species.3,7
Antibiotic Duration
The duration of antibiotic therapy in AECOPD has been studied extensively, with randomized controlled trials consistently demonstrating no additional benefit to courses extending beyond five days. One meta-analysis of 21 studies found similar clinical and microbiologic cure rates among patients randomized to antibiotic treatment for ≤5 days versus >5 days.22 A subgroup analysis of the trials evaluating different durations of the same antibiotic also demonstrated no difference in clinical effectiveness, and this finding was confirmed in a separate meta-analysis.22,23
Advantages to shorter antibiotic courses include improved compliance and decreased rates of resistance. The usual duration of antibiotic therapy is three to seven days, depending upon the response to therapy.3
Back to the Case
As the patient has no significant comorbidities or risk factors, and meets criteria for a simple Anthonisen Type I exacerbation (increased dyspnea, sputum, and sputum purulence), antibiotic therapy with trimethoprim/sulfamethoxazole is initiated on admission, in addition to the previously started steroid and bronchodilator treatments. The patient’s clinical status improves, and he is discharged on hospital Day 3 with a prescription to complete a five-day course of antibiotics.
Bottom Line
Antibiotic therapy is effective in select AECOPD patients, with maximal benefits obtained when the decision to treat is based on careful consideration of characteristic clinical symptoms and severity of illness. Choice and duration of antibiotics should follow likely bacterial causes and current guidelines.
Dr. Cunningham is an assistant professor of internal medicine and academic hospitalist in the section of hospital medicine at Vanderbilt University School of Medicine in Nashville, Tenn. Dr. LaBrin is assistant professor of internal medicine and pediatrics and an academic hospitalist at Vanderbilt. Dr. Markley is a clinical instructor and academic hospitalist at Vanderbilt.
References
- Donaldson GC, Wedzicha JA. COPD exacerbations: 1. Epidemiology. Thorax. 2006;61:164-168.
- National Heart, Lung, and Blood Institute. 2009 NHLBI Morbidity and Mortality Chartbook. National Heart, Lung, and Blood Institute website. Available at: http://www.nhlbi.nih.gov/resources/docs/cht-book.htm Accessed Oct. 10, 2011.
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease. Global Initiative for Chronic Obstructive Lung Disease (GOLD) website. Available at: www.goldcopd.org/guidelines-resources.html Accessed Oct. 10, 2011.
- Celli BR, MacNee W, Agusti A, et al. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Resp J. 2004;23:932-946.
- National Clinical Guideline Centre. Chronic obstructive pulmonary disease: management of chronic obstructive pulmonary disease in adults in primary and secondary care. National Institute for Health and Clinical Excellence website. Available at: http://guidance.nice.org.uk/CG101/Guidance/pdf/English. Accessed Oct. 10, 2011.
- O’Donnell DE, Aaron S, Bourbeau J, et al. Canadian Thoracic Society recommendations for management of chronic obstructive pulmonary disease—2007 update. Can Respir J. 2007;14(Suppl B):5B-32B.
- Sethi S, Murphy TF. Infection in the pathogenesis and course of chronic obstructive pulmonary disease. N Engl J Med. 2008;359:2355-2565.
- Quon BS, Qi Gan W, Sin DD. Contemporary management of acute exacerbations of COPD: a systematic review and metaanalysis. Chest. 2008;133:756-766.
- Rothberg MB, Pekow PS, Lahti M, Brody O, Skiest DJ, Lindenauer PK. Antibiotic therapy and treatment failure in patients hospitalized for acute exacerbations of chronic obstructive pulmonary disease. JAMA. 2010;303:2035-2042.
- Roede BM, Bresser P, Bindels PJE, et al. Antibiotic treatment is associated with reduced risk of subsequent exacerbation in obstructive lung disease: a historical population based cohort study. Thorax. 2008;63:968-973.
- Anthonisen NR, Manfreda J, Warren CP, Hershfield ES, Harding GKM, Nelson NA. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med. 1987;106:196-204.
- Stockley RA, O’Brien C, Pye A, Hill SL. Relationship of sputum color to nature and outpatient management of acute exacerbations of COPD. Chest. 2000;117:1638-1645.
- Rosell A, Monso E, Soler N, et al. Microbiologic determinants of exacerbation in chronic obstructive pulmonary disease. Arch Intern Med. 2005; 165:891-897.
- Stolz D, Christ-Crain M, Bingisser R, et al. Antibiotic treatment of exacerbations of COPD: a randomized, controlled trial comparing procalcitonin-guidance with standard therapy. Chest. 2007;131:9-19.
- Daniels JMA, Schoorl M, Snijders D, et al. Procalcitonin vs C-reactive protein as predictive markers of response to antibiotic therapy in acute exacerbations of COPD. Chest. 2010;138:1108-1015.
- Miravitlles M, Espinosa C, Fernandez-Laso E, Martos JA, Maldonado JA, Gallego M. Relationship between bacterial flora in sputum and functional impairment in patients with acute exacerbations of COPD. Chest. 1999;116:40-46.
- Patil SP, Krishnan JA, Lechtzin N, Diette GB. In-hospital mortality following acute exacerbations of chronic obstructive pulmonary disease. Arch Intern Med. 2003;163:1180-1186.
- Puhan MA, Vollenweider D, Latshang T, Steurer J, Steurer-Stey C. Exacerbations of chronic obstructive lung disease: when are antibiotics indicated? A systematic review. Resp Res. 2007;8:30-40.
- Nouira S, Marghli S, Belghith M, Besbes L, Elatrous S, Abroug F. Once daily ofloxacin in chronic obstructive pulmonary disease exacerbation requiring mechanical ventilation: a randomized placebo-controlled trial. Lancet. 2001;358:2020-2025.
- Dimopoulos G, Siempos II, Korbila IP, Manta KG, Falagas ME. Comparison of first-line with second-line antibiotics for acute exacerbations of chronic bronchitis: a metaanalysis of randomized controlled trials. Chest. 2007;132:447-455.
- Siempos II, Dimopoulos G, Korbila IP, Manta KG, Falagas ME. Macrolides, quinolones and amoxicillin/clavulanate for chronic bronchitis: a meta-analysis. Eur Resp J. 2007;29:1127-1137.
- El-Moussaoui, Roede BM, Speelman P, Bresser P, Prins JM, Bossuyt PMM. Short-course antibiotic treatment in acute exacerbations of chronic bronchitis and COPD: a meta-analysis of double-blind studies. Thorax. 2008;63:415-422.
- Falagas ME, Avgeri SG, Matthaiou DK, Dimopoulos G, Siempos II. Short- versus long-duration antimicrobial treatment for exacerbations of chronic bronchitis: a meta-analysis. J Antimicrob Chemother. 2008;62:442-450.
Case
A 58-year-old male smoker with moderate chronic obstructive pulmonary disease (COPD) (FEV1 56% predicted) is admitted with an acute exacerbation of COPD for the second time this year. He presented to the ED with increased productive cough and shortness of breath, similar to prior exacerbations. He denies fevers, myalgias, or upper-respiratory symptoms. Physical exam is notable for bilateral inspiratory and expiratory wheezing. His sputum is purulent. He is given continuous nebulizer therapy and one dose of oral prednisone, but his dyspnea and wheezing persist. Chest X-ray does not reveal an infiltrate.
Should this patient be treated with antibiotics and, if so, what regimen is most appropriate?
Overview
Acute exacerbations of COPD (AECOPD) present a major health burden, accounting for more than 2.4% of all hospital admissions and causing significant morbidity, mortality, and costs.1 During 2006 and 2007, COPD mortality in the United States topped 39 deaths per 100,000 people, and more recently, hospital costs related to COPD were expected to exceed $13 billion annually.2 Patients with AECOPD also experience decreased quality of life and faster decline in pulmonary function, further highlighting the need for timely and appropriate treatment.1
Several guidelines have proposed treatment strategies now considered standard of care in AECOPD management.3,4,5,6 These include the use of corticosteroids, bronchodilator agents, and, in select cases, antibiotics. While there is well-established evidence for the use of steroids and bronchodilators in AECOPD, the debate continues over the appropriate use of antibiotics in the treatment of acute exacerbations. There are multiple potential factors leading to AECOPD, including viruses, bacteria, and common pollutants; as such, antibiotic treatment may not be indicated for all patients presenting with exacerbations. Further, the risks of antibiotic treatment—including adverse drug events, selection for drug-resistant bacteria, and associated costs—are not insignificant.
However, bacterial infections do play a role in approximately 50% of patients with AECOPD and, for this population, use of antibiotics may confer important benefits.7
Interestingly, a retrospective cohort study of 84,621 patients admitted for AECOPD demonstrated that 85% of patients received antibiotics at some point during hospitalization.8
Support for Antibiotics
Several randomized trials have compared clinical outcomes in patients with AECOPD who have received antibiotics versus those who received placebos. Most of these had small sample sizes and studied only ββ-lactam and tetracycline antibiotics in an outpatient setting; there are limited data involving inpatients and newer drugs. Nevertheless, antibiotic treatment has been associated with decreased risk of adverse outcomes in AECOPD.
One meta-analysis demonstrated that antibiotics reduced treatment failures by 66% and in-hospital mortality by 78% in the subset of trials involving hospitalized patients.8 Similarly, analysis of a large retrospective cohort of patients hospitalized for AECOPD found a significantly lower risk of treatment failure in antibiotic-treated versus untreated patients.9 Specifically, treated patients had lower rates of in-hospital mortality and readmission for AECOPD and a lower likelihood of requiring subsequent mechanical ventilation during the index hospitalization.
Data also suggest that antibiotic treatment during exacerbations might favorably impact subsequent exacerbations.10 A retrospective study of 18,928 Dutch patients with AECOPD compared outcomes among patients who had received antibiotics (most frequently doxycycline or a penicillin) as part of their therapy to those who did not. The authors demonstrated that the median time to the next exacerbation was significantly longer in the patients receiving antibiotics.10 Further, both mortality and overall risk of developing a subsequent exacerbation were significantly decreased in the antibiotic group, with median follow-up of approximately two years.
Indications for Antibiotics
Clinical symptoms. A landmark study by Anthonisen and colleagues set forth three clinical criteria that have formed the basis for treating AECOPD with antibiotics in subsequent studies and in clinical practice.11 Often referred to as the “cardinal symptoms” of AECOPD, these include increased dyspnea, sputum volume, and sputum purulence. In this study, 173 outpatients with COPD were randomized to a 10-day course of antibiotics or placebo at onset of an exacerbation and followed clinically. The authors found that antibiotic-treated patients were significantly more likely than the placebo group to achieve treatment success, defined as resolution of all exacerbated symptoms within 21 days (68.1% vs. 55.0%, P<0.01).
Importantly, treated patients were also significantly less likely to experience clinical deterioration after 72 hours (9.9% vs. 18.9%, P<0.05). Patients with Type I exacerbations, characterized by all three cardinal symptoms, were most likely to benefit from antibiotic therapy, followed by patients with Type II exacerbations, in whom only two of the symptoms were present. Subsequent studies have suggested that sputum purulence correlates well with the presence of acute bacterial infection and therefore may be a reliable clinical indicator of patients who are likely to benefit from antibiotic therapy.12
Laboratory data. While sputum purulence is associated with bacterial infection, sputum culture is less reliable, as pathogenic bacteria are commonly isolated from patients with both AECOPD and stable COPD. In fact, the prevalence of bacterial colonization in moderate to severe COPD might be as high as 50%.13 Therefore, a positive bacterial sputum culture, in the absence of purulence or other signs of infection, is not recommended as the sole basis for which to prescribe antibiotics.
Serum biomarkers, most notably C-reactive protein (CRP) and procalcitonin, have been studied as a newer approach to identify patients who might benefit from antibiotic therapy for AECOPD. Studies have demonstrated increased CRP levels during AECOPD, particularly in patients with purulent sputum and positive bacterial sputum cultures.12 Procalcitonin is preferentially elevated in bacterial infections.
One randomized, placebo-controlled trial in hospitalized patients with AECOPD demonstrated a significant reduction in antibiotic usage based on low procalcitonin levels, without negatively impacting clinical success rate, hospital mortality, subsequent antibiotic needs, or time to next exacerbation.14 However, due to inconsistent evidence, use of these markers to guide antibiotic administration in AECOPD has not yet been definitively established.14,15 Additionally, these laboratory results are often not available at the point of care, potentially limiting their utility in the decision to initiate antibiotics.
Severity of illness. Severity of illness is an important factor in the decision to treat AECOPD with antibiotics. Patients with advanced, underlying airway obstruction, as measured by FEV1, are more likely to have a bacterial cause of AECOPD.16 Additionally, baseline clinical characteristics including advanced age and comorbid conditions, particularly cardiovascular disease and diabetes, increase the risk of severe exacerbations.17
One meta-analysis of placebo-controlled trials found that patients with severe exacerbations were likely to benefit from antibiotic therapy, while patients with mild or moderate exacerbations had no reduction in treatment failure or mortality rates.18 Patients presenting with acute respiratory failure necessitating intensive care and/or ventilator support (noninvasive or invasive) have also been shown to benefit from antibiotics.19
Current clinical guidelines vary slightly in their recommendations regarding when to give antibiotics in AECOPD (see Table 1). However, existing evidence favors antibiotic treatment for those patients presenting with two or three cardinal symptoms, specifically those with increased sputum purulence, and those with severe disease (i.e. pre-existing advanced airflow obstruction and/or exacerbations requiring mechanical ventilation). Conversely, studies have shown that many patients, particularly those with milder exacerbations, experience resolution of symptoms without antibiotic treatment.11,18
Antibiotic Choice in AECOPD
Risk stratification. In patients likely to benefit from antibiotic therapy, an understanding of the relationship between severity of COPD, host risk factors for poor outcomes, and microbiology is paramount to guide clinical decision-making. Historically, such bacteria as Haemophilus influenzae, Streptococcus pneumoniae, and Moraxella catarrhalis have been implicated in the pathogenesis of AECOPD.3,7 In patients with simple exacerbations, antibiotics that target these pathogens should be used (see Table 2).
However, patients with more severe underlying airway obstruction (i.e. FEV1<50%) and risk factors for poor outcomes, specifically recent hospitalization (≥2 days during the previous 90 days), frequent antibiotics (>3 courses during the previous year), and severe exacerbations are more likely to be infected with resistant strains or gram-negative organisms.3,7 Pseudomonas aeruginosa, in particular, is of increasing concern in this population. In patients with complicated exacerbations, more broad-coverage, empiric antibiotics should be initiated (see Table 2).
With this in mind, patients meeting criteria for treatment must first be stratified according to the severity of COPD and risk factors for poor outcomes before a decision regarding a specific antibiotic is reached. Figure 1 outlines a recommended approach for antibiotic administration in AECOPD. The optimal choice of antibiotics must consider cost-effectiveness, local patterns of antibiotic resistance, tissue penetration, patient adherence, and risk of such adverse drug events as diarrhea.
Comparative effectiveness. Current treatment guidelines do not favor the use of any particular antibiotic in simple AECOPD.3,4,5,6 However, as selective pressure has led to in vitro resistance to antibiotics traditionally considered first-line (e.g. doxycycline, trimethoprim/sulfamethoxazole, amoxicillin), the use of second-line antibiotics (e.g. fluoroquinolones, macrolides, cephalosporins, β-lactam/ β-lactamase inhibitors) has increased. Consequently, several studies have compared the effectiveness of different antimicrobial regimens.
One meta-analysis found that second-line antibiotics, when compared with first-line agents, provided greater clinical improvement to patients with AECOPD, without significant differences in mortality, microbiologic eradication, or incidence of adverse drug events.20 Among the subgroup of trials enrolling hospitalized patients, the clinical effectiveness of second-line agents remained significantly greater than that of first-line agents.
Another meta-analysis compared trials that studied only macrolides, quinolones, and amoxicillin-clavulanate and found no difference in terms of short-term clinical effectiveness; however, there was weak evidence to suggest that quinolones were associated with better microbiological success and fewer recurrences of AECOPD.21 Fluoroquinolones are preferred in complicated cases of AECOPD in which there is a greater risk for enterobacteriaceae and Pseudomonas species.3,7
Antibiotic Duration
The duration of antibiotic therapy in AECOPD has been studied extensively, with randomized controlled trials consistently demonstrating no additional benefit to courses extending beyond five days. One meta-analysis of 21 studies found similar clinical and microbiologic cure rates among patients randomized to antibiotic treatment for ≤5 days versus >5 days.22 A subgroup analysis of the trials evaluating different durations of the same antibiotic also demonstrated no difference in clinical effectiveness, and this finding was confirmed in a separate meta-analysis.22,23
Advantages to shorter antibiotic courses include improved compliance and decreased rates of resistance. The usual duration of antibiotic therapy is three to seven days, depending upon the response to therapy.3
Back to the Case
As the patient has no significant comorbidities or risk factors, and meets criteria for a simple Anthonisen Type I exacerbation (increased dyspnea, sputum, and sputum purulence), antibiotic therapy with trimethoprim/sulfamethoxazole is initiated on admission, in addition to the previously started steroid and bronchodilator treatments. The patient’s clinical status improves, and he is discharged on hospital Day 3 with a prescription to complete a five-day course of antibiotics.
Bottom Line
Antibiotic therapy is effective in select AECOPD patients, with maximal benefits obtained when the decision to treat is based on careful consideration of characteristic clinical symptoms and severity of illness. Choice and duration of antibiotics should follow likely bacterial causes and current guidelines.
Dr. Cunningham is an assistant professor of internal medicine and academic hospitalist in the section of hospital medicine at Vanderbilt University School of Medicine in Nashville, Tenn. Dr. LaBrin is assistant professor of internal medicine and pediatrics and an academic hospitalist at Vanderbilt. Dr. Markley is a clinical instructor and academic hospitalist at Vanderbilt.
References
- Donaldson GC, Wedzicha JA. COPD exacerbations: 1. Epidemiology. Thorax. 2006;61:164-168.
- National Heart, Lung, and Blood Institute. 2009 NHLBI Morbidity and Mortality Chartbook. National Heart, Lung, and Blood Institute website. Available at: http://www.nhlbi.nih.gov/resources/docs/cht-book.htm Accessed Oct. 10, 2011.
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease. Global Initiative for Chronic Obstructive Lung Disease (GOLD) website. Available at: www.goldcopd.org/guidelines-resources.html Accessed Oct. 10, 2011.
- Celli BR, MacNee W, Agusti A, et al. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Resp J. 2004;23:932-946.
- National Clinical Guideline Centre. Chronic obstructive pulmonary disease: management of chronic obstructive pulmonary disease in adults in primary and secondary care. National Institute for Health and Clinical Excellence website. Available at: http://guidance.nice.org.uk/CG101/Guidance/pdf/English. Accessed Oct. 10, 2011.
- O’Donnell DE, Aaron S, Bourbeau J, et al. Canadian Thoracic Society recommendations for management of chronic obstructive pulmonary disease—2007 update. Can Respir J. 2007;14(Suppl B):5B-32B.
- Sethi S, Murphy TF. Infection in the pathogenesis and course of chronic obstructive pulmonary disease. N Engl J Med. 2008;359:2355-2565.
- Quon BS, Qi Gan W, Sin DD. Contemporary management of acute exacerbations of COPD: a systematic review and metaanalysis. Chest. 2008;133:756-766.
- Rothberg MB, Pekow PS, Lahti M, Brody O, Skiest DJ, Lindenauer PK. Antibiotic therapy and treatment failure in patients hospitalized for acute exacerbations of chronic obstructive pulmonary disease. JAMA. 2010;303:2035-2042.
- Roede BM, Bresser P, Bindels PJE, et al. Antibiotic treatment is associated with reduced risk of subsequent exacerbation in obstructive lung disease: a historical population based cohort study. Thorax. 2008;63:968-973.
- Anthonisen NR, Manfreda J, Warren CP, Hershfield ES, Harding GKM, Nelson NA. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med. 1987;106:196-204.
- Stockley RA, O’Brien C, Pye A, Hill SL. Relationship of sputum color to nature and outpatient management of acute exacerbations of COPD. Chest. 2000;117:1638-1645.
- Rosell A, Monso E, Soler N, et al. Microbiologic determinants of exacerbation in chronic obstructive pulmonary disease. Arch Intern Med. 2005; 165:891-897.
- Stolz D, Christ-Crain M, Bingisser R, et al. Antibiotic treatment of exacerbations of COPD: a randomized, controlled trial comparing procalcitonin-guidance with standard therapy. Chest. 2007;131:9-19.
- Daniels JMA, Schoorl M, Snijders D, et al. Procalcitonin vs C-reactive protein as predictive markers of response to antibiotic therapy in acute exacerbations of COPD. Chest. 2010;138:1108-1015.
- Miravitlles M, Espinosa C, Fernandez-Laso E, Martos JA, Maldonado JA, Gallego M. Relationship between bacterial flora in sputum and functional impairment in patients with acute exacerbations of COPD. Chest. 1999;116:40-46.
- Patil SP, Krishnan JA, Lechtzin N, Diette GB. In-hospital mortality following acute exacerbations of chronic obstructive pulmonary disease. Arch Intern Med. 2003;163:1180-1186.
- Puhan MA, Vollenweider D, Latshang T, Steurer J, Steurer-Stey C. Exacerbations of chronic obstructive lung disease: when are antibiotics indicated? A systematic review. Resp Res. 2007;8:30-40.
- Nouira S, Marghli S, Belghith M, Besbes L, Elatrous S, Abroug F. Once daily ofloxacin in chronic obstructive pulmonary disease exacerbation requiring mechanical ventilation: a randomized placebo-controlled trial. Lancet. 2001;358:2020-2025.
- Dimopoulos G, Siempos II, Korbila IP, Manta KG, Falagas ME. Comparison of first-line with second-line antibiotics for acute exacerbations of chronic bronchitis: a metaanalysis of randomized controlled trials. Chest. 2007;132:447-455.
- Siempos II, Dimopoulos G, Korbila IP, Manta KG, Falagas ME. Macrolides, quinolones and amoxicillin/clavulanate for chronic bronchitis: a meta-analysis. Eur Resp J. 2007;29:1127-1137.
- El-Moussaoui, Roede BM, Speelman P, Bresser P, Prins JM, Bossuyt PMM. Short-course antibiotic treatment in acute exacerbations of chronic bronchitis and COPD: a meta-analysis of double-blind studies. Thorax. 2008;63:415-422.
- Falagas ME, Avgeri SG, Matthaiou DK, Dimopoulos G, Siempos II. Short- versus long-duration antimicrobial treatment for exacerbations of chronic bronchitis: a meta-analysis. J Antimicrob Chemother. 2008;62:442-450.
In the Literature: Research You Need to Know
Clinical question: To what extent does diagnostic phlebotomy contribute to hospital-acquired anemia (HAA) during acute myocardial infarction (AMI)?
Background: During AMI, hospital-acquired HAA is associated with higher mortality and poorer health status. Moderate to severe HAA (nadir hemoglobin level <11 g/dL) has been shown to be prognostically important. The contribution of diagnostic phlebotomy blood loss on HAA is unknown and is a potentially modifiable factor.
Study design: Retrospective observational cohort study.
Setting: Fifty-seven U.S. hospitals.
Synopsis: Using Cerner Corp.'s Health Facts database, information was collected on 17,676 patients with AMI. Moderate to severe HAA developed in 3,551 (20%) patients who were not anemic upon admission. The diagnostic blood loss was estimated by assuming minimal blood volume per adult tube required to perform the lab work obtained. The mean phlebotomy volume was higher in patients with HAA compared with patients without HAA (173.8 mL vs. 83.5 mL; P<0.001). There was significant variation of diagnostic blood loss between hospitals. The risk of HAA increased by 18% (RR 1.18; 95% CI, 1.13-1.22) for every 50 mL of diagnostic blood loss.
Patients with HAA were noted to have greater disease severity and comorbidities. No causal inference can be made given the observational nature of the study. Randomized trials are needed to evaluate if strategies to reduce diagnostic blood loss can reduce HAA and improve clinical outcomes for patients with AMI.
Bottom line: Diagnostic blood loss is associated with development of hospital-acquired anemia in patients with acute myocardial infarction.
Citation: Salisbury AC, Reid KJ, Alexander KP, et al. Diagnostic blood loss from phlebotomy and hospital-acquired anemia during acute myocardial infarction. Arch Intern Med. 2011;171:1646-1653.
For more physician reviews of HM-relevant research, visit our website.
Clinical question: To what extent does diagnostic phlebotomy contribute to hospital-acquired anemia (HAA) during acute myocardial infarction (AMI)?
Background: During AMI, hospital-acquired HAA is associated with higher mortality and poorer health status. Moderate to severe HAA (nadir hemoglobin level <11 g/dL) has been shown to be prognostically important. The contribution of diagnostic phlebotomy blood loss on HAA is unknown and is a potentially modifiable factor.
Study design: Retrospective observational cohort study.
Setting: Fifty-seven U.S. hospitals.
Synopsis: Using Cerner Corp.'s Health Facts database, information was collected on 17,676 patients with AMI. Moderate to severe HAA developed in 3,551 (20%) patients who were not anemic upon admission. The diagnostic blood loss was estimated by assuming minimal blood volume per adult tube required to perform the lab work obtained. The mean phlebotomy volume was higher in patients with HAA compared with patients without HAA (173.8 mL vs. 83.5 mL; P<0.001). There was significant variation of diagnostic blood loss between hospitals. The risk of HAA increased by 18% (RR 1.18; 95% CI, 1.13-1.22) for every 50 mL of diagnostic blood loss.
Patients with HAA were noted to have greater disease severity and comorbidities. No causal inference can be made given the observational nature of the study. Randomized trials are needed to evaluate if strategies to reduce diagnostic blood loss can reduce HAA and improve clinical outcomes for patients with AMI.
Bottom line: Diagnostic blood loss is associated with development of hospital-acquired anemia in patients with acute myocardial infarction.
Citation: Salisbury AC, Reid KJ, Alexander KP, et al. Diagnostic blood loss from phlebotomy and hospital-acquired anemia during acute myocardial infarction. Arch Intern Med. 2011;171:1646-1653.
For more physician reviews of HM-relevant research, visit our website.
Clinical question: To what extent does diagnostic phlebotomy contribute to hospital-acquired anemia (HAA) during acute myocardial infarction (AMI)?
Background: During AMI, hospital-acquired HAA is associated with higher mortality and poorer health status. Moderate to severe HAA (nadir hemoglobin level <11 g/dL) has been shown to be prognostically important. The contribution of diagnostic phlebotomy blood loss on HAA is unknown and is a potentially modifiable factor.
Study design: Retrospective observational cohort study.
Setting: Fifty-seven U.S. hospitals.
Synopsis: Using Cerner Corp.'s Health Facts database, information was collected on 17,676 patients with AMI. Moderate to severe HAA developed in 3,551 (20%) patients who were not anemic upon admission. The diagnostic blood loss was estimated by assuming minimal blood volume per adult tube required to perform the lab work obtained. The mean phlebotomy volume was higher in patients with HAA compared with patients without HAA (173.8 mL vs. 83.5 mL; P<0.001). There was significant variation of diagnostic blood loss between hospitals. The risk of HAA increased by 18% (RR 1.18; 95% CI, 1.13-1.22) for every 50 mL of diagnostic blood loss.
Patients with HAA were noted to have greater disease severity and comorbidities. No causal inference can be made given the observational nature of the study. Randomized trials are needed to evaluate if strategies to reduce diagnostic blood loss can reduce HAA and improve clinical outcomes for patients with AMI.
Bottom line: Diagnostic blood loss is associated with development of hospital-acquired anemia in patients with acute myocardial infarction.
Citation: Salisbury AC, Reid KJ, Alexander KP, et al. Diagnostic blood loss from phlebotomy and hospital-acquired anemia during acute myocardial infarction. Arch Intern Med. 2011;171:1646-1653.
For more physician reviews of HM-relevant research, visit our website.
In the Literature: Research You Need to Know
Clinical question: What is the association between time to clinical stability (TCS) and post-discharge death or readmission in patients hospitalized with community-acquired pneumonia (CAP)?
Background: In patients with CAP, inflammatory response during hospitalization might be associated with adverse outcomes after discharge. Studies have not evaluated if time to clinical stability, a reflection of inflammatory response, can be used to identify patients at high risk of adverse outcomes after discharge.
Study design: Retrospective cohort study.
Setting: Veterans Hospital, Louisville, Ky.
Synopsis: Of 464 hospitalized patients with CAP, those with TCS >3 days had a higher rate of readmission or death within 30 days after discharge compared with those who had a TCS =3 days (26% versus 15%; OR 1.98; 95% CI, 1.19-3.3; P=0.008). Longer TCS during hospitalization was associated with a significantly increased risk of adverse outcomes (adjusted OR 1.06, 1.54, 2.40, 10.53 if TCS was reached at days 2, 3, 4, 5 versus Day 1, respectively). The authors proposed that patients with delays in reaching clinical stability should receive a special discharge management approach to decrease the risk of morbidity and mortality after discharge; this may include close observation, home visits, and a follow-up clinic appointment within 10 days.
As a retrospective cohort study, unaccounted-for confounders might exist between TCS and adverse outcomes. The small sample size precluded development of a fully predictive model. Additionally, the population studied was elderly men in a single hospital, which might limit generalizability.
Bottom line: Hospitalized patients with community-acquired pneumonia whose time to clinical stability was greater than three days had a higher risk of readmission or death within 30 days after discharge.
Citation: Aliberti S, Peyrani P, Filardo G, et al. Association between time to clinical stability and outcomes after discharge in hospitalized patients with community-acquired pneumonia. Chest. 2011;140:482-488.
For more physician reviews of HM-relevant research, visit our website.
Clinical question: What is the association between time to clinical stability (TCS) and post-discharge death or readmission in patients hospitalized with community-acquired pneumonia (CAP)?
Background: In patients with CAP, inflammatory response during hospitalization might be associated with adverse outcomes after discharge. Studies have not evaluated if time to clinical stability, a reflection of inflammatory response, can be used to identify patients at high risk of adverse outcomes after discharge.
Study design: Retrospective cohort study.
Setting: Veterans Hospital, Louisville, Ky.
Synopsis: Of 464 hospitalized patients with CAP, those with TCS >3 days had a higher rate of readmission or death within 30 days after discharge compared with those who had a TCS =3 days (26% versus 15%; OR 1.98; 95% CI, 1.19-3.3; P=0.008). Longer TCS during hospitalization was associated with a significantly increased risk of adverse outcomes (adjusted OR 1.06, 1.54, 2.40, 10.53 if TCS was reached at days 2, 3, 4, 5 versus Day 1, respectively). The authors proposed that patients with delays in reaching clinical stability should receive a special discharge management approach to decrease the risk of morbidity and mortality after discharge; this may include close observation, home visits, and a follow-up clinic appointment within 10 days.
As a retrospective cohort study, unaccounted-for confounders might exist between TCS and adverse outcomes. The small sample size precluded development of a fully predictive model. Additionally, the population studied was elderly men in a single hospital, which might limit generalizability.
Bottom line: Hospitalized patients with community-acquired pneumonia whose time to clinical stability was greater than three days had a higher risk of readmission or death within 30 days after discharge.
Citation: Aliberti S, Peyrani P, Filardo G, et al. Association between time to clinical stability and outcomes after discharge in hospitalized patients with community-acquired pneumonia. Chest. 2011;140:482-488.
For more physician reviews of HM-relevant research, visit our website.
Clinical question: What is the association between time to clinical stability (TCS) and post-discharge death or readmission in patients hospitalized with community-acquired pneumonia (CAP)?
Background: In patients with CAP, inflammatory response during hospitalization might be associated with adverse outcomes after discharge. Studies have not evaluated if time to clinical stability, a reflection of inflammatory response, can be used to identify patients at high risk of adverse outcomes after discharge.
Study design: Retrospective cohort study.
Setting: Veterans Hospital, Louisville, Ky.
Synopsis: Of 464 hospitalized patients with CAP, those with TCS >3 days had a higher rate of readmission or death within 30 days after discharge compared with those who had a TCS =3 days (26% versus 15%; OR 1.98; 95% CI, 1.19-3.3; P=0.008). Longer TCS during hospitalization was associated with a significantly increased risk of adverse outcomes (adjusted OR 1.06, 1.54, 2.40, 10.53 if TCS was reached at days 2, 3, 4, 5 versus Day 1, respectively). The authors proposed that patients with delays in reaching clinical stability should receive a special discharge management approach to decrease the risk of morbidity and mortality after discharge; this may include close observation, home visits, and a follow-up clinic appointment within 10 days.
As a retrospective cohort study, unaccounted-for confounders might exist between TCS and adverse outcomes. The small sample size precluded development of a fully predictive model. Additionally, the population studied was elderly men in a single hospital, which might limit generalizability.
Bottom line: Hospitalized patients with community-acquired pneumonia whose time to clinical stability was greater than three days had a higher risk of readmission or death within 30 days after discharge.
Citation: Aliberti S, Peyrani P, Filardo G, et al. Association between time to clinical stability and outcomes after discharge in hospitalized patients with community-acquired pneumonia. Chest. 2011;140:482-488.
For more physician reviews of HM-relevant research, visit our website.
In the Literature: The latest research you need to know
In This Edition
Literature At A Glance
A guide to this month’s studies
- Procalcitonin to guide antimicrobial use in ICU patients
- Platelet reactivity and event rates after PCI
- Conservative treatment of necrotizing pancreatitis
- Use of MRI to diagnose Takotsubo cardiomyopathy
- Rates of inadvertent medication discontinuation after hospitalization
- Role of history and physical exam in diagnosing medical illness
- Red-cell distribution width and rates of mortality
Procalcitonin-Guided Therapy Decreases Antimicrobial Duration in ICU Patients
Clinical question: Can utilization of serum procalcitonin (PCT) levels safely reduce antimicrobial exposure in ICU patients?
Background: Serum PCT levels are elevated in bacterial infections and sepsis and have been used in some settings to guide antimicrobial therapy. Randomized controlled trials have demonstrated reduction of antibiotic use with PCT measurement. This systematic review assessed the safety and effectiveness of PCT measurements in reducing antimicrobial exposure in ICU patients.
Study design: Systematic review.
Setting: Adult medical and surgical ICUs.
Synopsis: A search of MEDLINE and EMBASE yielded 1,018 publications related to PCT, critically ill patients, and antimicrobial therapy. Six randomized controlled trials involving 1,476 patients were reviewed. The duration of antimicrobial use was significantly decreased in all five studies that evaluated treatment duration. The remaining study only assessed the impact of PCT on initiation of antimicrobial therapy and did not demonstrate decreased antimicrobial exposure. Compared with the control group, patients randomized to PCT-guided therapy had relative reductions in duration of first antibiotic course by 21%, down to 38%, and decreases in days of antimicrobial therapy per 1,000 ICU patient days by 20%, down to 23%. PCT intervention also was associated with a 23% to 37% increase in days alive without antimicrobial therapy during the first 28 days. The length of ICU stay was significantly decreased in two studies but was not significantly different in the other studies. There were no significant differences in rates of mortality, infection relapse, or days free of mechanical ventilation.
Bottom line: PCT guidance reduced antimicrobial exposure of ICU patients without increasing rates of mortality or infection relapse.
Citation: Agarwal R, Schwartz DN. Procalcitonin to guide duration of antimicrobial therapy in intensive care units: a systematic review. Clin Infect Dis. 2011;53:379-387.
High Residual Platelet Reactivity Increases Risk of Cardiovascular Events among Patients with Acute Coronary Syndromes Undergoing PCI
Clinical question: Is high residual platelet reactivity (HRPR) in patients receiving clopidogrel associated with increased risk of ischemic events after percutaneous coronary intervention (PCI)?
Background: Studies have demonstrated an increased risk of cardiovascular events associated with HRPR in patients receiving clopidogrel while undergoing PCI. However, these studies have used a variety of platelet function tests, and thresholds for positive tests have not been established. In addition, these studies have enrolled heterogeneous populations with short-term follow-up and few have included patients with acute coronary syndromes (ACSs).
Study design: Prospective cohort study.
Setting: Cardiology service of a referral center in Italy.
Synopsis: This study included 1,789 consecutive patients with ACS undergoing PCI. Patients were given 325 mg aspirin and a 600-mg loading dose of clopidogrel on admission, followed by a daily maintenance dose of aspirin 325 mg and clopidogrel 75 mg for at least six months. Platelet reactivity was measured using adenosine diphosphate (ADP) testing, and those with HRPR (≥70% platelet aggregation) were given increased dosing of clopidogrel or switched to ticlopidine using ADP test guidance. At two-year follow-up, patients with HRPR experienced an increased composite endpoint of cardiac death, myocardial infarction, urgent coronary revascularization, and stroke with a combined event rate of 14.6% in patients with HRPR and 8.7% in patients with low residual platelet reactivity (95% CI, 1.6%-11.1%; P=0.003). Stent thrombosis was also higher in HRPR patients (absolute risk increase 3.2%; 95% CI, 0.4%-6.7%; P=0.01).
This study is nonrandomized, and residual unmeasured confounding cannot be excluded. In addition, use of non-antiplatelet drugs and adherence to recommended drugs might have influenced outcomes.
Bottom line: HRPR is associated with increased risk of ischemic events in patients with ACS receiving antiplatelet agents after PCI.
Citation: Parodi G, Marcucci R, Valenti R, et al. High residual platelet reactivity after clopidogrel loading and long-term cardiovascular events among patients with acute coronary syndromes undergoing PCI. JAMA. 2011;306:1215-1223.
Conservative Treatment of Necrotizing Pancreatitis Is Associated with Improved Outcomes
Clinical question: What are the outcomes of conservative and interventional management of necrotizing pancreatitis?
Background: Open necrosectomy was historically the treatment of choice for necrotizing pancreatitis, but, currently, pancreatic necrosis is only managed invasively when complicated by infection. Other changes in management over time have included a shift in the timing of intervention and the use of minimally invasive techniques. Existing studies do not reflect these changes in practice patterns and have been limited by small sample sizes or the exclusion of important subgroups of patients.
Study design: Prospective cohort study.
Setting: Twenty-one Dutch hospitals.
Synopsis: This study included 639 patients with acute necrotizing pancreatitis confirmed by imaging. Overall mortality was 15%. Conservative treatment was performed in 62% of the patients with a mortality of 7%; however, patients with organ failure (pulmonary, circulatory, and/or renal) who received conservative therapy had a mortality rate of 37%. Intervention (percutaneous drainage, video-assisted retroperitoneal debridement, endoscopic transluminal necrosectomy, laparotomy) in patients with suspected or confirmed infected pancreatic necrosis was performed on 38% of the patients with associated mortality of 27%. Interventions performed within the first 14 days of hospitalization resulted in a 56% mortality rate, whereas interventions performed after Day 29 resulted in a 15% mortality rate (P<0.001). Patients with organ failure experienced significantly greater mortality compared with patients with no organ failure (35% vs. 2%; P<0.001). Primary percutaneous drainage was associated with fewer complications than was primary necrosectomy (42% vs. 64%; P=0.003).
This study was nonrandomized, and final decisions regarding management were left to the treating physician. Notably, while there was no significant difference in APACHE II scores between the conservative and intervention groups, intervention patients had more severe pancreatic disease and scored higher on other measures of disease severity.
Bottom line: Patients with necrotizing pancreatitis can frequently be managed conservatively, though the presence of organ failure and parenchymal necrosis confer poorer prognosis. When intervention is indicated, postponing intervention and utilizing minimally invasive techniques decrease morbidity and mortality.
Citation: Van Santvoort HC, Bakker OJ, Bollen TL, et al. A conservative and minimally invasive approach to necrotizing pancreatitis improves outcome. Gastroenterology. 2011;141:1254-1263.
Cardiac MRI Complements Clinical Findings in Diagnosis of Stress Cardiomyopathy
Clinical question: What are the clinical features and cardiovascular MRI findings in patients with stress (Takotsubo) cardiomyopathy?
Background: Stress cardiomyopathy (SC) is characterized by acute and profound reversible left ventricular dysfunction that is thought to result from increased sympathetic activity related to emotional and/or physical stress. Prior studies evaluating the clinical features of SC were limited by small sample sizes and single-center enrollment, and cardiac MRI use in SC has not been well studied.
Study design: Prospective cohort study.
Setting: Seven North American and European tertiary-care centers.
Synopsis: This study enrolled 256 patients who met diagnostic criteria for SC according to Mayo criteria. Postmenopausal women were most commonly affected; only 11% of participants were men and 8% were women younger than 50 years old. An identifiable stressor was found in 71% of the patients. Clinical presentation was notable for symptoms of acute coronary syndrome (ACS) in 88% of patients, abnormal electrocardiogram in 87%, and elevated troponin T in 90%. Coronary angiography was normal in three-fourths of patients, and no patients had features of acute plaque rupture. Typical apical ballooning was seen on left ventriculography in 82% of patients.
Cardiac MRI findings included severe left ventricular dysfunction in a noncoronary distribution, myocardial edema in areas of regional wall abnormalities, absence of high signal areas in late gadolinium enhancement (e.g., absence of necrosis/fibrosis), and increased early gadolinium uptake (i.e. early inflammation). Repeat cardiac MRI four weeks after initial diagnosis showed near or complete resolution of imaging findings.
Bottom line: Stress cardiomyopathy typically presents like ACS, usually affects postmenopausal women, is often preceded by a stressful event, and is characterized by cardiac MRI findings of regional wall motion abnormalities, reversible myocardial injury, and the absence of fibrosis. Cardiac MRI may be valuable in diagnosing SC in patients who present without the classic clinical features.
Citation: Eitel I, von Knobelsdorff-Brenkenhoff F, Bernhardt P, et al. Clinical characteristics and cardiovascular magnetic resonance findings in stress (Takotsubo) cardiomyopathy. JAMA. 2011;306:277-286.
Increased Risk of Potentially Inadvertent Medication Discontinuation Following Acute-Care Hospitalization
Clinical question: Are medications for chronic diseases inadvertently discontinued after acute-care hospitalization, and is this risk increased in patients who had an ICU stay?
Background: Transitions of care are associated with medical errors. Two such transitions are a shift from the ICU to floor setting and from the inpatient to outpatient setting. Medications for chronic diseases might be held during hospitalization for a variety of reasons, and medication errors may occur if these drugs are not restarted when the acute problem resolves or the patient is discharged from the hospital.
Study design: Population-based cohort study.
Setting: Ontario, Canada.
Synopsis: Using four separate databases, administrative records were reviewed for 396,380 patients aged >65 years who were continuous users of at least one of five evidence-based medication groups for common chronic diseases. Medications included statins, antiplatelet/anticoagulant agents, levothyroxine, respiratory inhalers, and gastric acid suppressants. The primary outcome was potentially unintentional medication discontinuation (measured by failure to renew the prescription at 90 days) for hospitalized versus nonhospitalized patients. All medication groups had statistically significant adjusted odds ratios ranging from 1.18 (95% CI, 1.14-1.23) for discontinuation of levothyroxine to 1.86 (95% CI, 1.77-1.97) for discontinuation of antiplatelet/anticoagulant medications. Treatment in an ICU further increased this risk compared with nonhospitalized patients, and increased the risk for medication discontinuation in four of the five medication groups when compared with patients hospitalized without ICU treatment.
Important study limitations include the lack of appropriate clinical details to classify medication discontinuation as unintentional and the inability of administrative data to prove causality. This study highlights the importance of medication reconciliation and calls attention to inadvertent medication discontinuation during care transitions (see “Reconciliation Act,”).
Bottom line: Patients discharged from the hospital, particularly after ICU treatment, have a higher risk of discontinuation of long-term medications for chronic medical problems when compared with nonhospitalized patients.
Citation: Bell CM, Brener SS, Gunraj N, et al. Association of ICU or hospital admission with unintentional discontinuation of medications for chronic diseases. JAMA. 2011;306:840-847.
Clinical Exam Remains Valuable in the Diagnosis of Patients Admitted to a Medicine Service
Clinical question: Is a clinical exam useful in the diagnosis of newly admitted patients to a general medicine service?
Background: The clinical exam, which comprises the history and physical examination, has long been described as essential to the diagnosis of illness. However, the literature supporting this claim is limited to the ambulatory setting. There has not been evaluation of the clinical exam as a diagnostic tool in the hospital setting, where more advanced testing is readily available.
Study design: Retrospective chart review.
Setting: Urban academic medical center.
Synopsis: The study included 442 adult patients consecutively admitted from the emergency department to the general medicine service who were separately assessed by one senior resident (SR) and one experienced hospital physician (HP) not involved with the case. The SR and HP each made an initial diagnosis and documented the most helpful component(s) in arriving at that diagnosis. Outcomes included comparison of the SR and HP’s admission diagnosis with the discharge diagnosis, and the diagnostic value of the various components of the clinical exam and initial studies.
Compared with the discharge diagnosis, the SR’s initial diagnosis was correct in 80.1% of cases, while the HP was correct in 84.4%. The patient’s history was the most important element in the initial assessment, independently influencing approximately 20% of the correct diagnoses for both physicians. Approximately 60% of correct diagnoses were established using the history and/or physical, and more than 90% were made using a combination of history, physical exam, and/or basic tests (admission labs, electrocardiogram, chest X-ray).
The generalizability of these results is limited by the retrospective, single-center study design, involvement of only one resident physician, and the lack of information regarding number of experienced clinicians and types of diagnoses.
Bottom line: Among patients admitted to a general medicine service, the most powerful tool in obtaining an accurate diagnosis was the combination of a patient’s history and a physical exam.
Citation: Paley L, Zornitzki T, Cohen J, et al. Utility of clinical examination in the diagnosis of emergency department patients admitted to the department of medicine of an academic hospital. Arch Intern Med. 2011;171:1394-1396.
RDW Predicts All-Cause Mortality and Bloodstream Infection in ICU Patients
Clinical question: Among patients admitted to the ICU, is red blood cell distribution width (RDW) a reliable indicator of mortality?
Background: The RDW is an inexpensive test that is commonly included in routine laboratory studies. It has been associated with multiple disease processes and found to be a strong predictor of mortality in the general adult population. However, there has been limited study of the association between RDW and outcomes in critically ill patients.
Study design: Observational cohort study.
Setting: Urban tertiary-care academic medical center.
Synopsis: Data from 51,413 adult patients who received critical care between 1997 and 2007 were obtained from a computerized registry and evaluated for the primary outcome of 30-day mortality after critical-care initiation. Secondary outcomes included 90-day, 365-day, and in-hospital mortality, as well as bloodstream infection. Logistic regression examined both primary and secondary outcomes in association with pre-established RDW quintiles. After multivariable adjustment, RDW was found to be associated with mortality at 30, 90, and 365 days, in addition to in-hospital mortality. The highest RDW quintile (RDW >15.8%) had an adjusted OR of 2.61 (95% CI, 2.37-2.86; P<0.001) for the primary outcome, with similar risk for secondary outcomes of mortality. A subgroup of 18,525 patients with blood culture data was analyzed and an adjusted OR of 1.44 was found in the highest RDW quintile for the secondary outcome of bloodstream infection.
Bottom line: Red blood cell distribution width is a strong independent predictor of all-cause mortality and bloodstream infection in patients receiving intensive care.
Citation: Bazick HS, Chang D, Mahadevappa K, Gibbons FK, Christopher KB. Red cell distribution width and all-cause mortality in critically ill patients. Crit Care Med. 2011;39:1913-1921.
In This Edition
Literature At A Glance
A guide to this month’s studies
- Procalcitonin to guide antimicrobial use in ICU patients
- Platelet reactivity and event rates after PCI
- Conservative treatment of necrotizing pancreatitis
- Use of MRI to diagnose Takotsubo cardiomyopathy
- Rates of inadvertent medication discontinuation after hospitalization
- Role of history and physical exam in diagnosing medical illness
- Red-cell distribution width and rates of mortality
Procalcitonin-Guided Therapy Decreases Antimicrobial Duration in ICU Patients
Clinical question: Can utilization of serum procalcitonin (PCT) levels safely reduce antimicrobial exposure in ICU patients?
Background: Serum PCT levels are elevated in bacterial infections and sepsis and have been used in some settings to guide antimicrobial therapy. Randomized controlled trials have demonstrated reduction of antibiotic use with PCT measurement. This systematic review assessed the safety and effectiveness of PCT measurements in reducing antimicrobial exposure in ICU patients.
Study design: Systematic review.
Setting: Adult medical and surgical ICUs.
Synopsis: A search of MEDLINE and EMBASE yielded 1,018 publications related to PCT, critically ill patients, and antimicrobial therapy. Six randomized controlled trials involving 1,476 patients were reviewed. The duration of antimicrobial use was significantly decreased in all five studies that evaluated treatment duration. The remaining study only assessed the impact of PCT on initiation of antimicrobial therapy and did not demonstrate decreased antimicrobial exposure. Compared with the control group, patients randomized to PCT-guided therapy had relative reductions in duration of first antibiotic course by 21%, down to 38%, and decreases in days of antimicrobial therapy per 1,000 ICU patient days by 20%, down to 23%. PCT intervention also was associated with a 23% to 37% increase in days alive without antimicrobial therapy during the first 28 days. The length of ICU stay was significantly decreased in two studies but was not significantly different in the other studies. There were no significant differences in rates of mortality, infection relapse, or days free of mechanical ventilation.
Bottom line: PCT guidance reduced antimicrobial exposure of ICU patients without increasing rates of mortality or infection relapse.
Citation: Agarwal R, Schwartz DN. Procalcitonin to guide duration of antimicrobial therapy in intensive care units: a systematic review. Clin Infect Dis. 2011;53:379-387.
High Residual Platelet Reactivity Increases Risk of Cardiovascular Events among Patients with Acute Coronary Syndromes Undergoing PCI
Clinical question: Is high residual platelet reactivity (HRPR) in patients receiving clopidogrel associated with increased risk of ischemic events after percutaneous coronary intervention (PCI)?
Background: Studies have demonstrated an increased risk of cardiovascular events associated with HRPR in patients receiving clopidogrel while undergoing PCI. However, these studies have used a variety of platelet function tests, and thresholds for positive tests have not been established. In addition, these studies have enrolled heterogeneous populations with short-term follow-up and few have included patients with acute coronary syndromes (ACSs).
Study design: Prospective cohort study.
Setting: Cardiology service of a referral center in Italy.
Synopsis: This study included 1,789 consecutive patients with ACS undergoing PCI. Patients were given 325 mg aspirin and a 600-mg loading dose of clopidogrel on admission, followed by a daily maintenance dose of aspirin 325 mg and clopidogrel 75 mg for at least six months. Platelet reactivity was measured using adenosine diphosphate (ADP) testing, and those with HRPR (≥70% platelet aggregation) were given increased dosing of clopidogrel or switched to ticlopidine using ADP test guidance. At two-year follow-up, patients with HRPR experienced an increased composite endpoint of cardiac death, myocardial infarction, urgent coronary revascularization, and stroke with a combined event rate of 14.6% in patients with HRPR and 8.7% in patients with low residual platelet reactivity (95% CI, 1.6%-11.1%; P=0.003). Stent thrombosis was also higher in HRPR patients (absolute risk increase 3.2%; 95% CI, 0.4%-6.7%; P=0.01).
This study is nonrandomized, and residual unmeasured confounding cannot be excluded. In addition, use of non-antiplatelet drugs and adherence to recommended drugs might have influenced outcomes.
Bottom line: HRPR is associated with increased risk of ischemic events in patients with ACS receiving antiplatelet agents after PCI.
Citation: Parodi G, Marcucci R, Valenti R, et al. High residual platelet reactivity after clopidogrel loading and long-term cardiovascular events among patients with acute coronary syndromes undergoing PCI. JAMA. 2011;306:1215-1223.
Conservative Treatment of Necrotizing Pancreatitis Is Associated with Improved Outcomes
Clinical question: What are the outcomes of conservative and interventional management of necrotizing pancreatitis?
Background: Open necrosectomy was historically the treatment of choice for necrotizing pancreatitis, but, currently, pancreatic necrosis is only managed invasively when complicated by infection. Other changes in management over time have included a shift in the timing of intervention and the use of minimally invasive techniques. Existing studies do not reflect these changes in practice patterns and have been limited by small sample sizes or the exclusion of important subgroups of patients.
Study design: Prospective cohort study.
Setting: Twenty-one Dutch hospitals.
Synopsis: This study included 639 patients with acute necrotizing pancreatitis confirmed by imaging. Overall mortality was 15%. Conservative treatment was performed in 62% of the patients with a mortality of 7%; however, patients with organ failure (pulmonary, circulatory, and/or renal) who received conservative therapy had a mortality rate of 37%. Intervention (percutaneous drainage, video-assisted retroperitoneal debridement, endoscopic transluminal necrosectomy, laparotomy) in patients with suspected or confirmed infected pancreatic necrosis was performed on 38% of the patients with associated mortality of 27%. Interventions performed within the first 14 days of hospitalization resulted in a 56% mortality rate, whereas interventions performed after Day 29 resulted in a 15% mortality rate (P<0.001). Patients with organ failure experienced significantly greater mortality compared with patients with no organ failure (35% vs. 2%; P<0.001). Primary percutaneous drainage was associated with fewer complications than was primary necrosectomy (42% vs. 64%; P=0.003).
This study was nonrandomized, and final decisions regarding management were left to the treating physician. Notably, while there was no significant difference in APACHE II scores between the conservative and intervention groups, intervention patients had more severe pancreatic disease and scored higher on other measures of disease severity.
Bottom line: Patients with necrotizing pancreatitis can frequently be managed conservatively, though the presence of organ failure and parenchymal necrosis confer poorer prognosis. When intervention is indicated, postponing intervention and utilizing minimally invasive techniques decrease morbidity and mortality.
Citation: Van Santvoort HC, Bakker OJ, Bollen TL, et al. A conservative and minimally invasive approach to necrotizing pancreatitis improves outcome. Gastroenterology. 2011;141:1254-1263.
Cardiac MRI Complements Clinical Findings in Diagnosis of Stress Cardiomyopathy
Clinical question: What are the clinical features and cardiovascular MRI findings in patients with stress (Takotsubo) cardiomyopathy?
Background: Stress cardiomyopathy (SC) is characterized by acute and profound reversible left ventricular dysfunction that is thought to result from increased sympathetic activity related to emotional and/or physical stress. Prior studies evaluating the clinical features of SC were limited by small sample sizes and single-center enrollment, and cardiac MRI use in SC has not been well studied.
Study design: Prospective cohort study.
Setting: Seven North American and European tertiary-care centers.
Synopsis: This study enrolled 256 patients who met diagnostic criteria for SC according to Mayo criteria. Postmenopausal women were most commonly affected; only 11% of participants were men and 8% were women younger than 50 years old. An identifiable stressor was found in 71% of the patients. Clinical presentation was notable for symptoms of acute coronary syndrome (ACS) in 88% of patients, abnormal electrocardiogram in 87%, and elevated troponin T in 90%. Coronary angiography was normal in three-fourths of patients, and no patients had features of acute plaque rupture. Typical apical ballooning was seen on left ventriculography in 82% of patients.
Cardiac MRI findings included severe left ventricular dysfunction in a noncoronary distribution, myocardial edema in areas of regional wall abnormalities, absence of high signal areas in late gadolinium enhancement (e.g., absence of necrosis/fibrosis), and increased early gadolinium uptake (i.e. early inflammation). Repeat cardiac MRI four weeks after initial diagnosis showed near or complete resolution of imaging findings.
Bottom line: Stress cardiomyopathy typically presents like ACS, usually affects postmenopausal women, is often preceded by a stressful event, and is characterized by cardiac MRI findings of regional wall motion abnormalities, reversible myocardial injury, and the absence of fibrosis. Cardiac MRI may be valuable in diagnosing SC in patients who present without the classic clinical features.
Citation: Eitel I, von Knobelsdorff-Brenkenhoff F, Bernhardt P, et al. Clinical characteristics and cardiovascular magnetic resonance findings in stress (Takotsubo) cardiomyopathy. JAMA. 2011;306:277-286.
Increased Risk of Potentially Inadvertent Medication Discontinuation Following Acute-Care Hospitalization
Clinical question: Are medications for chronic diseases inadvertently discontinued after acute-care hospitalization, and is this risk increased in patients who had an ICU stay?
Background: Transitions of care are associated with medical errors. Two such transitions are a shift from the ICU to floor setting and from the inpatient to outpatient setting. Medications for chronic diseases might be held during hospitalization for a variety of reasons, and medication errors may occur if these drugs are not restarted when the acute problem resolves or the patient is discharged from the hospital.
Study design: Population-based cohort study.
Setting: Ontario, Canada.
Synopsis: Using four separate databases, administrative records were reviewed for 396,380 patients aged >65 years who were continuous users of at least one of five evidence-based medication groups for common chronic diseases. Medications included statins, antiplatelet/anticoagulant agents, levothyroxine, respiratory inhalers, and gastric acid suppressants. The primary outcome was potentially unintentional medication discontinuation (measured by failure to renew the prescription at 90 days) for hospitalized versus nonhospitalized patients. All medication groups had statistically significant adjusted odds ratios ranging from 1.18 (95% CI, 1.14-1.23) for discontinuation of levothyroxine to 1.86 (95% CI, 1.77-1.97) for discontinuation of antiplatelet/anticoagulant medications. Treatment in an ICU further increased this risk compared with nonhospitalized patients, and increased the risk for medication discontinuation in four of the five medication groups when compared with patients hospitalized without ICU treatment.
Important study limitations include the lack of appropriate clinical details to classify medication discontinuation as unintentional and the inability of administrative data to prove causality. This study highlights the importance of medication reconciliation and calls attention to inadvertent medication discontinuation during care transitions (see “Reconciliation Act,”).
Bottom line: Patients discharged from the hospital, particularly after ICU treatment, have a higher risk of discontinuation of long-term medications for chronic medical problems when compared with nonhospitalized patients.
Citation: Bell CM, Brener SS, Gunraj N, et al. Association of ICU or hospital admission with unintentional discontinuation of medications for chronic diseases. JAMA. 2011;306:840-847.
Clinical Exam Remains Valuable in the Diagnosis of Patients Admitted to a Medicine Service
Clinical question: Is a clinical exam useful in the diagnosis of newly admitted patients to a general medicine service?
Background: The clinical exam, which comprises the history and physical examination, has long been described as essential to the diagnosis of illness. However, the literature supporting this claim is limited to the ambulatory setting. There has not been evaluation of the clinical exam as a diagnostic tool in the hospital setting, where more advanced testing is readily available.
Study design: Retrospective chart review.
Setting: Urban academic medical center.
Synopsis: The study included 442 adult patients consecutively admitted from the emergency department to the general medicine service who were separately assessed by one senior resident (SR) and one experienced hospital physician (HP) not involved with the case. The SR and HP each made an initial diagnosis and documented the most helpful component(s) in arriving at that diagnosis. Outcomes included comparison of the SR and HP’s admission diagnosis with the discharge diagnosis, and the diagnostic value of the various components of the clinical exam and initial studies.
Compared with the discharge diagnosis, the SR’s initial diagnosis was correct in 80.1% of cases, while the HP was correct in 84.4%. The patient’s history was the most important element in the initial assessment, independently influencing approximately 20% of the correct diagnoses for both physicians. Approximately 60% of correct diagnoses were established using the history and/or physical, and more than 90% were made using a combination of history, physical exam, and/or basic tests (admission labs, electrocardiogram, chest X-ray).
The generalizability of these results is limited by the retrospective, single-center study design, involvement of only one resident physician, and the lack of information regarding number of experienced clinicians and types of diagnoses.
Bottom line: Among patients admitted to a general medicine service, the most powerful tool in obtaining an accurate diagnosis was the combination of a patient’s history and a physical exam.
Citation: Paley L, Zornitzki T, Cohen J, et al. Utility of clinical examination in the diagnosis of emergency department patients admitted to the department of medicine of an academic hospital. Arch Intern Med. 2011;171:1394-1396.
RDW Predicts All-Cause Mortality and Bloodstream Infection in ICU Patients
Clinical question: Among patients admitted to the ICU, is red blood cell distribution width (RDW) a reliable indicator of mortality?
Background: The RDW is an inexpensive test that is commonly included in routine laboratory studies. It has been associated with multiple disease processes and found to be a strong predictor of mortality in the general adult population. However, there has been limited study of the association between RDW and outcomes in critically ill patients.
Study design: Observational cohort study.
Setting: Urban tertiary-care academic medical center.
Synopsis: Data from 51,413 adult patients who received critical care between 1997 and 2007 were obtained from a computerized registry and evaluated for the primary outcome of 30-day mortality after critical-care initiation. Secondary outcomes included 90-day, 365-day, and in-hospital mortality, as well as bloodstream infection. Logistic regression examined both primary and secondary outcomes in association with pre-established RDW quintiles. After multivariable adjustment, RDW was found to be associated with mortality at 30, 90, and 365 days, in addition to in-hospital mortality. The highest RDW quintile (RDW >15.8%) had an adjusted OR of 2.61 (95% CI, 2.37-2.86; P<0.001) for the primary outcome, with similar risk for secondary outcomes of mortality. A subgroup of 18,525 patients with blood culture data was analyzed and an adjusted OR of 1.44 was found in the highest RDW quintile for the secondary outcome of bloodstream infection.
Bottom line: Red blood cell distribution width is a strong independent predictor of all-cause mortality and bloodstream infection in patients receiving intensive care.
Citation: Bazick HS, Chang D, Mahadevappa K, Gibbons FK, Christopher KB. Red cell distribution width and all-cause mortality in critically ill patients. Crit Care Med. 2011;39:1913-1921.
In This Edition
Literature At A Glance
A guide to this month’s studies
- Procalcitonin to guide antimicrobial use in ICU patients
- Platelet reactivity and event rates after PCI
- Conservative treatment of necrotizing pancreatitis
- Use of MRI to diagnose Takotsubo cardiomyopathy
- Rates of inadvertent medication discontinuation after hospitalization
- Role of history and physical exam in diagnosing medical illness
- Red-cell distribution width and rates of mortality
Procalcitonin-Guided Therapy Decreases Antimicrobial Duration in ICU Patients
Clinical question: Can utilization of serum procalcitonin (PCT) levels safely reduce antimicrobial exposure in ICU patients?
Background: Serum PCT levels are elevated in bacterial infections and sepsis and have been used in some settings to guide antimicrobial therapy. Randomized controlled trials have demonstrated reduction of antibiotic use with PCT measurement. This systematic review assessed the safety and effectiveness of PCT measurements in reducing antimicrobial exposure in ICU patients.
Study design: Systematic review.
Setting: Adult medical and surgical ICUs.
Synopsis: A search of MEDLINE and EMBASE yielded 1,018 publications related to PCT, critically ill patients, and antimicrobial therapy. Six randomized controlled trials involving 1,476 patients were reviewed. The duration of antimicrobial use was significantly decreased in all five studies that evaluated treatment duration. The remaining study only assessed the impact of PCT on initiation of antimicrobial therapy and did not demonstrate decreased antimicrobial exposure. Compared with the control group, patients randomized to PCT-guided therapy had relative reductions in duration of first antibiotic course by 21%, down to 38%, and decreases in days of antimicrobial therapy per 1,000 ICU patient days by 20%, down to 23%. PCT intervention also was associated with a 23% to 37% increase in days alive without antimicrobial therapy during the first 28 days. The length of ICU stay was significantly decreased in two studies but was not significantly different in the other studies. There were no significant differences in rates of mortality, infection relapse, or days free of mechanical ventilation.
Bottom line: PCT guidance reduced antimicrobial exposure of ICU patients without increasing rates of mortality or infection relapse.
Citation: Agarwal R, Schwartz DN. Procalcitonin to guide duration of antimicrobial therapy in intensive care units: a systematic review. Clin Infect Dis. 2011;53:379-387.
High Residual Platelet Reactivity Increases Risk of Cardiovascular Events among Patients with Acute Coronary Syndromes Undergoing PCI
Clinical question: Is high residual platelet reactivity (HRPR) in patients receiving clopidogrel associated with increased risk of ischemic events after percutaneous coronary intervention (PCI)?
Background: Studies have demonstrated an increased risk of cardiovascular events associated with HRPR in patients receiving clopidogrel while undergoing PCI. However, these studies have used a variety of platelet function tests, and thresholds for positive tests have not been established. In addition, these studies have enrolled heterogeneous populations with short-term follow-up and few have included patients with acute coronary syndromes (ACSs).
Study design: Prospective cohort study.
Setting: Cardiology service of a referral center in Italy.
Synopsis: This study included 1,789 consecutive patients with ACS undergoing PCI. Patients were given 325 mg aspirin and a 600-mg loading dose of clopidogrel on admission, followed by a daily maintenance dose of aspirin 325 mg and clopidogrel 75 mg for at least six months. Platelet reactivity was measured using adenosine diphosphate (ADP) testing, and those with HRPR (≥70% platelet aggregation) were given increased dosing of clopidogrel or switched to ticlopidine using ADP test guidance. At two-year follow-up, patients with HRPR experienced an increased composite endpoint of cardiac death, myocardial infarction, urgent coronary revascularization, and stroke with a combined event rate of 14.6% in patients with HRPR and 8.7% in patients with low residual platelet reactivity (95% CI, 1.6%-11.1%; P=0.003). Stent thrombosis was also higher in HRPR patients (absolute risk increase 3.2%; 95% CI, 0.4%-6.7%; P=0.01).
This study is nonrandomized, and residual unmeasured confounding cannot be excluded. In addition, use of non-antiplatelet drugs and adherence to recommended drugs might have influenced outcomes.
Bottom line: HRPR is associated with increased risk of ischemic events in patients with ACS receiving antiplatelet agents after PCI.
Citation: Parodi G, Marcucci R, Valenti R, et al. High residual platelet reactivity after clopidogrel loading and long-term cardiovascular events among patients with acute coronary syndromes undergoing PCI. JAMA. 2011;306:1215-1223.
Conservative Treatment of Necrotizing Pancreatitis Is Associated with Improved Outcomes
Clinical question: What are the outcomes of conservative and interventional management of necrotizing pancreatitis?
Background: Open necrosectomy was historically the treatment of choice for necrotizing pancreatitis, but, currently, pancreatic necrosis is only managed invasively when complicated by infection. Other changes in management over time have included a shift in the timing of intervention and the use of minimally invasive techniques. Existing studies do not reflect these changes in practice patterns and have been limited by small sample sizes or the exclusion of important subgroups of patients.
Study design: Prospective cohort study.
Setting: Twenty-one Dutch hospitals.
Synopsis: This study included 639 patients with acute necrotizing pancreatitis confirmed by imaging. Overall mortality was 15%. Conservative treatment was performed in 62% of the patients with a mortality of 7%; however, patients with organ failure (pulmonary, circulatory, and/or renal) who received conservative therapy had a mortality rate of 37%. Intervention (percutaneous drainage, video-assisted retroperitoneal debridement, endoscopic transluminal necrosectomy, laparotomy) in patients with suspected or confirmed infected pancreatic necrosis was performed on 38% of the patients with associated mortality of 27%. Interventions performed within the first 14 days of hospitalization resulted in a 56% mortality rate, whereas interventions performed after Day 29 resulted in a 15% mortality rate (P<0.001). Patients with organ failure experienced significantly greater mortality compared with patients with no organ failure (35% vs. 2%; P<0.001). Primary percutaneous drainage was associated with fewer complications than was primary necrosectomy (42% vs. 64%; P=0.003).
This study was nonrandomized, and final decisions regarding management were left to the treating physician. Notably, while there was no significant difference in APACHE II scores between the conservative and intervention groups, intervention patients had more severe pancreatic disease and scored higher on other measures of disease severity.
Bottom line: Patients with necrotizing pancreatitis can frequently be managed conservatively, though the presence of organ failure and parenchymal necrosis confer poorer prognosis. When intervention is indicated, postponing intervention and utilizing minimally invasive techniques decrease morbidity and mortality.
Citation: Van Santvoort HC, Bakker OJ, Bollen TL, et al. A conservative and minimally invasive approach to necrotizing pancreatitis improves outcome. Gastroenterology. 2011;141:1254-1263.
Cardiac MRI Complements Clinical Findings in Diagnosis of Stress Cardiomyopathy
Clinical question: What are the clinical features and cardiovascular MRI findings in patients with stress (Takotsubo) cardiomyopathy?
Background: Stress cardiomyopathy (SC) is characterized by acute and profound reversible left ventricular dysfunction that is thought to result from increased sympathetic activity related to emotional and/or physical stress. Prior studies evaluating the clinical features of SC were limited by small sample sizes and single-center enrollment, and cardiac MRI use in SC has not been well studied.
Study design: Prospective cohort study.
Setting: Seven North American and European tertiary-care centers.
Synopsis: This study enrolled 256 patients who met diagnostic criteria for SC according to Mayo criteria. Postmenopausal women were most commonly affected; only 11% of participants were men and 8% were women younger than 50 years old. An identifiable stressor was found in 71% of the patients. Clinical presentation was notable for symptoms of acute coronary syndrome (ACS) in 88% of patients, abnormal electrocardiogram in 87%, and elevated troponin T in 90%. Coronary angiography was normal in three-fourths of patients, and no patients had features of acute plaque rupture. Typical apical ballooning was seen on left ventriculography in 82% of patients.
Cardiac MRI findings included severe left ventricular dysfunction in a noncoronary distribution, myocardial edema in areas of regional wall abnormalities, absence of high signal areas in late gadolinium enhancement (e.g., absence of necrosis/fibrosis), and increased early gadolinium uptake (i.e. early inflammation). Repeat cardiac MRI four weeks after initial diagnosis showed near or complete resolution of imaging findings.
Bottom line: Stress cardiomyopathy typically presents like ACS, usually affects postmenopausal women, is often preceded by a stressful event, and is characterized by cardiac MRI findings of regional wall motion abnormalities, reversible myocardial injury, and the absence of fibrosis. Cardiac MRI may be valuable in diagnosing SC in patients who present without the classic clinical features.
Citation: Eitel I, von Knobelsdorff-Brenkenhoff F, Bernhardt P, et al. Clinical characteristics and cardiovascular magnetic resonance findings in stress (Takotsubo) cardiomyopathy. JAMA. 2011;306:277-286.
Increased Risk of Potentially Inadvertent Medication Discontinuation Following Acute-Care Hospitalization
Clinical question: Are medications for chronic diseases inadvertently discontinued after acute-care hospitalization, and is this risk increased in patients who had an ICU stay?
Background: Transitions of care are associated with medical errors. Two such transitions are a shift from the ICU to floor setting and from the inpatient to outpatient setting. Medications for chronic diseases might be held during hospitalization for a variety of reasons, and medication errors may occur if these drugs are not restarted when the acute problem resolves or the patient is discharged from the hospital.
Study design: Population-based cohort study.
Setting: Ontario, Canada.
Synopsis: Using four separate databases, administrative records were reviewed for 396,380 patients aged >65 years who were continuous users of at least one of five evidence-based medication groups for common chronic diseases. Medications included statins, antiplatelet/anticoagulant agents, levothyroxine, respiratory inhalers, and gastric acid suppressants. The primary outcome was potentially unintentional medication discontinuation (measured by failure to renew the prescription at 90 days) for hospitalized versus nonhospitalized patients. All medication groups had statistically significant adjusted odds ratios ranging from 1.18 (95% CI, 1.14-1.23) for discontinuation of levothyroxine to 1.86 (95% CI, 1.77-1.97) for discontinuation of antiplatelet/anticoagulant medications. Treatment in an ICU further increased this risk compared with nonhospitalized patients, and increased the risk for medication discontinuation in four of the five medication groups when compared with patients hospitalized without ICU treatment.
Important study limitations include the lack of appropriate clinical details to classify medication discontinuation as unintentional and the inability of administrative data to prove causality. This study highlights the importance of medication reconciliation and calls attention to inadvertent medication discontinuation during care transitions (see “Reconciliation Act,”).
Bottom line: Patients discharged from the hospital, particularly after ICU treatment, have a higher risk of discontinuation of long-term medications for chronic medical problems when compared with nonhospitalized patients.
Citation: Bell CM, Brener SS, Gunraj N, et al. Association of ICU or hospital admission with unintentional discontinuation of medications for chronic diseases. JAMA. 2011;306:840-847.
Clinical Exam Remains Valuable in the Diagnosis of Patients Admitted to a Medicine Service
Clinical question: Is a clinical exam useful in the diagnosis of newly admitted patients to a general medicine service?
Background: The clinical exam, which comprises the history and physical examination, has long been described as essential to the diagnosis of illness. However, the literature supporting this claim is limited to the ambulatory setting. There has not been evaluation of the clinical exam as a diagnostic tool in the hospital setting, where more advanced testing is readily available.
Study design: Retrospective chart review.
Setting: Urban academic medical center.
Synopsis: The study included 442 adult patients consecutively admitted from the emergency department to the general medicine service who were separately assessed by one senior resident (SR) and one experienced hospital physician (HP) not involved with the case. The SR and HP each made an initial diagnosis and documented the most helpful component(s) in arriving at that diagnosis. Outcomes included comparison of the SR and HP’s admission diagnosis with the discharge diagnosis, and the diagnostic value of the various components of the clinical exam and initial studies.
Compared with the discharge diagnosis, the SR’s initial diagnosis was correct in 80.1% of cases, while the HP was correct in 84.4%. The patient’s history was the most important element in the initial assessment, independently influencing approximately 20% of the correct diagnoses for both physicians. Approximately 60% of correct diagnoses were established using the history and/or physical, and more than 90% were made using a combination of history, physical exam, and/or basic tests (admission labs, electrocardiogram, chest X-ray).
The generalizability of these results is limited by the retrospective, single-center study design, involvement of only one resident physician, and the lack of information regarding number of experienced clinicians and types of diagnoses.
Bottom line: Among patients admitted to a general medicine service, the most powerful tool in obtaining an accurate diagnosis was the combination of a patient’s history and a physical exam.
Citation: Paley L, Zornitzki T, Cohen J, et al. Utility of clinical examination in the diagnosis of emergency department patients admitted to the department of medicine of an academic hospital. Arch Intern Med. 2011;171:1394-1396.
RDW Predicts All-Cause Mortality and Bloodstream Infection in ICU Patients
Clinical question: Among patients admitted to the ICU, is red blood cell distribution width (RDW) a reliable indicator of mortality?
Background: The RDW is an inexpensive test that is commonly included in routine laboratory studies. It has been associated with multiple disease processes and found to be a strong predictor of mortality in the general adult population. However, there has been limited study of the association between RDW and outcomes in critically ill patients.
Study design: Observational cohort study.
Setting: Urban tertiary-care academic medical center.
Synopsis: Data from 51,413 adult patients who received critical care between 1997 and 2007 were obtained from a computerized registry and evaluated for the primary outcome of 30-day mortality after critical-care initiation. Secondary outcomes included 90-day, 365-day, and in-hospital mortality, as well as bloodstream infection. Logistic regression examined both primary and secondary outcomes in association with pre-established RDW quintiles. After multivariable adjustment, RDW was found to be associated with mortality at 30, 90, and 365 days, in addition to in-hospital mortality. The highest RDW quintile (RDW >15.8%) had an adjusted OR of 2.61 (95% CI, 2.37-2.86; P<0.001) for the primary outcome, with similar risk for secondary outcomes of mortality. A subgroup of 18,525 patients with blood culture data was analyzed and an adjusted OR of 1.44 was found in the highest RDW quintile for the secondary outcome of bloodstream infection.
Bottom line: Red blood cell distribution width is a strong independent predictor of all-cause mortality and bloodstream infection in patients receiving intensive care.
Citation: Bazick HS, Chang D, Mahadevappa K, Gibbons FK, Christopher KB. Red cell distribution width and all-cause mortality in critically ill patients. Crit Care Med. 2011;39:1913-1921.
What Corticosteroid is Most Appropriate for treating Acute Exacerbations of CoPD?
Case
A 66-year-old Caucasian female with moderate chronic obstructive pulmonary disease (COPD) (FEV1 55% predicted), obesity, hypertension, and Type 2 diabetes mellitus on insulin therapy presents to the ED with four days of increased cough productive of yellow sputum and progressive shortness of breath. Her physical exam is notable for an oxygen saturation of 87% on room air, along with diffuse expiratory wheezing with use of accessory muscles; her chest X-ray is unchanged from previous. The patient is given oxygen, nebulized bronchodilators, and one dose of IV methylprednisolone. Her symptoms do not improve significantly, and she is admitted for further management. What regimen of corticosteroids is most appropriate to treat her acute exacerbation of COPD?
Overview
COPD is the fourth-leading cause of death in the United States and continues to increase in prevalence.1 Acute exacerbations of COPD (AECOPD) contribute significantly to this high mortality rate, which approaches 40% at one year in those patients requiring mechanical support.1 An exacerbation of COPD has been defined as an acute change in a patient’s baseline dyspnea, cough, and/or sputum beyond day-to-day variability sufficient to warrant a change in therapy.2 Exacerbations commonly occur in COPD patients and often necessitate hospital admission. In fact, COPD consistently is one of the 10 most common reasons for hospitalization, with billions of dollars in associated healthcare costs.3
The goals for inpatient management of AECOPD are to provide acute symptom relief and to minimize the potential for subsequent exacerbations. These are accomplished via a multifaceted approach, including the use of bronchodilators, antibiotics, supplemental oxygen, noninvasive positive pressure ventilation in certain circumstances, and systemic corticosteroids.
The administration of systemic steroids in AECOPD has been prevalent for several decades, with initial studies showing positive effects on lung function, specifically FEV1.4 Studies have demonstrated the benefit of steroids in prolonging the time to subsequent exacerbation, reducing the rate of treatment failure, and reducing length of stay (LOS).5 Corticosteroids have since become an essential component of the standard of care in AECOPD management.
Despite consensus that systemic steroids should be used in COPD exacerbations, a great deal of controversy still surrounds the optimal steroid regimen.6 Steroid use is not without risk, as steroids can lead to adverse outcomes in medically complex hospitalized patients (see Table 1, below). Current guidelines provide limited guidance as to the optimal route of administration, dosing regimen, or length of therapy; clinical practice varies widely.
Review of the Data
Administration route: intravenous (IV) vs. oral. The use of steroids in AECOPD began with such IV formulations as methylprednisolone, and this became the typical method of treating hospitalized patients. This practice was validated in a multicenter Veterans Affairs trial, which demonstrated decreased risk of treatment failure (defined as all-cause mortality, need for intubation, readmission for COPD, or intensification of pharmacologic therapy) for patients randomized to receive an IV-to-oral steroid regimen compared with those randomized to placebo.5 Patients receiving steroids also had shorter LOS and improvements in FEV1 after the first day of treatment. Subsequent randomized controlled trials in patients with AECOPD demonstrated the benefit of oral regimens compared with placebo with regard to FEV1, LOS, and risk of treatment failure.6,7,8
Similarities in the bioavailability of oral and IV steroids have been known for a long time.9 Comparisons in efficacy initially were completed in the management of acute asthma exacerbations, with increasing evidence, including a meta-analysis, demonstrating no difference in improvement in pulmonary function and in preventing relapse of exacerbations for oral compared with IV steroids.10 However, only recently have oral and IV steroids been compared in the treatment of AECOPD. De Jong et al randomized more than 200 patients hospitalized for AECOPD to 60 mg of either IV or oral prednisolone for five days, followed by a week of an oral taper.11 There were no significant differences in treatment failure between the IV and oral groups (62% vs. 56%, respectively, at 90 days; one-sided lower bound of the 95% confidence interval [CI], −5.8%).
A large observational study by Lindenauer et al, including nearly 80,000 AECOPD patients admitted at more than 400 hospitals, added further support to the idea that oral and IV steroids were comparable in efficacy.12 In this study, multivariate analysis found no difference in treatment failure between oral and IV groups (odds ratio [OR] 0.93; 95% CI, 0.84-1.02). The authors also found, however, that current clinical practice still overwhelmingly favors intravenous steroids, with 92% of study patients initially being administered IV steroids.12
Based on the evidence from de Jong and Lindenauer, it appears that there is no significant benefit to the use of IV over oral steroids. Additionally, there is evidence for oral administration being associated with beneficial effects on cost and hospital LOS.12 Oral steroids, therefore, are the preferred route of administration to treat a hospitalized patient with AECOPD, unless the patient is unable to tolerate oral medications. Current guidelines support the practice of giving oral steroids as first-line treatment for AECOPD (see Table 2, above).
High dose vs. low dose. Another important clinical issue concerns the dosing of steroids. The randomized trials examining the use of corticosteroids in AECOPD vary widely in the dosages studied. Further, the majority of these trials have compared steroids to placebo, rather than comparing different dosage regimens. The agents studied have included prednisone, prednisolone, methylprednisolone, and hydrocortisone, or combinations thereof. In order to compare regimens of these different drugs, steroid doses often are converted into prednisone equivalents (see Table 3, below). Though no guidelines define “high dose” and “low dose,” some studies have designated doses of >80 mg prednisone equivalents daily as high-dose and prednisone equivalents of ≤80 mg daily as low-dose.13,14
Starting doses of systemic corticosteroids in the treatment of AECOPD in clinical studies range from prednisone equivalents of 30 mg daily to 625 mg on the first day of treatment.5,8 No randomized studies of high- versus low-dose steroid regimens have been conducted. One retrospective chart review of 145 AECOPD admissions evaluated outcomes among patients who were given higher (mean daily dose >80 mg prednisone equivalent) and lower (mean daily dose of ≤80 mg prednisone) doses.14 The authors found that patients who received higher doses of steroids had significantly longer LOS compared with those who received lower doses, especially among the subset of patients who were admitted to the floor rather than the ICU, though this analysis did not adjust for severity of illness. In this study, the most striking finding noted by the authors was the wide variability in the steroid doses prescribed for the inpatient treatment of AECOPD.
More recently, the study by Lindenauer et al examined outcomes between patients treated with high-dose IV steroids (equivalent of 120 mg-800 mg of prednisone on the first or second day of treatment) compared to low-dose oral steroids (prednisone equivalents of 20 mg-80 mg per day).12 The authors found no differences between the two groups regarding the rate of treatment failure, defined by initiation of mechanical ventilation after the second hospital day, in-hospital mortality, or readmission for COPD within 30 days of discharge. After multivariate adjustment, including the propensity for oral treatment, the low-dose oral therapy group was found to have lower risk of treatment failure, shorter LOS, and lower total hospital cost.
Despite the heterogeneity of the published data and the lack of randomized trials, the existing evidence suggests that low-dose prednisone (or equivalent) is similar in efficacy to higher doses and generally is associated with shorter hospital stays. Recognizing these benefits, guidelines do favor initiating treatment with low-dose steroids in patients admitted with AECOPD. The most recent publications from the American Thoracic Society/European Respiratory Society Task Force (ATS/ERS), the Global Initiative for Chronic Obstructive Lung Disease (GOLD), the National Clinical Guidelines Centre in the United Kingdom, and the Canadian Thoracic Society all recommend equivalent dosing of prednisone in patients admitted with AECOPD who are able to tolerate oral intake (see Table 2).1,2,15,16
Duration. As with the dosing of systemic corticosteroids in AECOPD, the optimal duration of treatment is not well-established. National and international consensus panels vary in their recommendations, as outlined in Table 2. This may be related to the variability in length of treatment found in the literature.
Treatment durations ranging from one day to eight weeks have been studied in inpatients with AECOPD. The landmark randomized controlled trial by Niewoehner and colleagues compared two-week and eight-week courses of systemic corticosteroids and found no difference in the rates of treatment failure, which included death, need for mechanical ventilation, readmission for COPD, and intensification of pharmacologic therapy.5 Based on these results, many experts have concluded that there is no benefit to steroid courses lasting beyond two weeks.
Although improvements in outcomes have been demonstrated with corticosteroid regimens as short as three days compared with placebo, most of the randomized controlled trials have included courses of seven to 14 days.4 Given the risks of adverse events (e.g. hyperglycemia) that are associated with systemic administration of steroids, the shortest effective duration should be considered.
In both clinical practice and clinical studies, steroid regimens often include a taper. A study by Vondracek and Hemstreet found that 79% of hospital discharges for AECOPD included a tapered corticosteroid regimen.14 From a physiologic standpoint, durations of corticosteroid treatment approximately three weeks or less, regardless of dosage, should not lead to adrenal suppression.17 There also is no evidence to suggest that abrupt discontinuation of steroids leads to clinical worsening of disease, and complicated steroid tapers are a potential source of medication errors after hospital discharge.18 Furthermore, the clinical guidelines do not address the tapering of corticosteroids. Therefore, there is a lack of evidence advocating for or against the use of tapered steroid regimens in AECOPD.
Back to the Case
In addition to standard treatment modalities for AECOPD, our patient was administered oral prednisone 40 mg daily. She experienced steroid-induced hyperglycemia, which was corrected with adjustment of her insulin regimen. The patient’s pulmonary symptoms improved within 72 hours, and she was discharged home on hospital day four to complete a seven-day steroid course. At hospital discharge, she was administered influenza and pneumococcal vaccinations, and she was instructed to resume her usual insulin dosing once she finished her prednisone course.
Overview
In the management of AECOPD, there remains a lack of consensus in defining the ideal steroid regimen. Based on current literature, the use of low-dose oral corticosteroids, such as prednisone 40 mg daily, for a seven- to 14-day course is recommended. TH
Dr. Cunningham is an assistant professor of internal medicine and academic hospitalist in the section of hospital medicine at Vanderbilt University School of Medicine in Nashville, Tenn. Dr. LaBrin is an assistant professor of internal medicine and pediatrics and academic hospitalist at Vanderbilt University School of Medicine.
References
- From the Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2010. Global Initiative for Chronic Obstructive Lung Disease website. Available at: www.goldcopd.org/GuidelineItem.asp?intId=989. Accessed Feb. 21, 2011.
- Celli BR, MacNee W, ATS/ERS Task Force. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004;23:932-946.
- Morbidity and mortality: 2009 chart book on cardiovascular, lung, and blood diseases. National Institutes of Health’s National Heart, Lung, and Blood Institute website. Available at: www.nhlbi.nih.gov/resources/docs/2009_ChartBook.pdf. Accessed Feb. 24, 2011.
- Albert RK, Martin TR, Lewis SW. Controlled trial of methylprednisolone in patients with chronic bronchitis and acute respiratory insufficiency. Ann Intern Med. 1980;92(6):753-758.
- Niewoehner DE, Erbland ML, Deupree RH, et al. Effect of systemic glucocorticoids on exacerbations of chronic obstructive pulmonary disease. Department of Veterans Affairs Cooperative Study Group. N Engl J Med. 1999;340(25):1941-1947.
- Thompson WH, Nielson C, Carvalho P, Charan NB, Crowley JJ. Controlled trial of oral prednisone in outpatients with acute COPD exacerbation. Am J Respir Crit Care Med. 1996;154:407-412.
- Seemungal TA, Donaldson GC, Bhowmik A, Jeffries DJ, Wedzicha JA. Time course and recovery of exacerbations in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2000;161:1608-1613.
- Davies L, Angus RM, Calverley PM. Oral corticosteroids in patients admitted to hospital with exacerbations of chronic obstructive pulmonary disease: a prospective randomised controlled trial. Lancet. 1999;354(9177):456-460.
- Al-Habet S, Rogers HJ. Pharmacokinetics of intravenous and oral prednisolone. Br J Clin Pharmacol. 1980;10(5):503-508.
- Rowe BH, Keller JL, Oxman AD. Effectiveness of steroid therapy in acute exacerbations of asthma: a meta-analysis. Am J Emerg Med. 1992;10:301-310.
- De Jong YP, Uil SM, Grotjohan HP, Postma DS, Kerstjens HA, van den Berg JW. Oral or IV prednisolone in the treatment of COPD exacerbations: A randomized, controlled, double-blind study. Chest. 2007;132(6):1741-1747.
- Lindenauer PK, Pekow PS, Lahti MC, Lee Y, Benjamin EM, Rothberg MB. Association of corticosteroid dose and route of administration with risk of treatment failure in acute exacerbation of chronic obstructive pulmonary disease. JAMA. 2010;303(23):2359-2367.
- Manser R, Reid D, Abramsom MJ. Corticosteroids for acute severe asthma in hospitalized patients. Cochrane Database Syst Rev. 2000;(2):CD001740.
- Vondracek SF, Hemstreet BA. Retrospective evaluation of systemic corticosteroids for the management of acute exacerbations of chronic obstructive pulmonary disease. Am J Health Syst Pharm. 2006;63:645-652.
- Chronic obstructive pulmonary disease: management of chronic obstructive pulmonary disease in adults in primary and secondary care. National Institute for Health and Clinical Excellence website. Available at: guidance.nice.org.uk/CG101/Guidance/pdf/English. Accessed Feb. 21, 2011.
- O’Donnell DE, Aaron S, Bourbeau J, et al. Canadian Thoracic Society recommendations for management of chronic obstructive pulmonary disease—2007 update. Can Respir J. 2007;14 Suppl B:5B-32B.
- Webb J, Clark TJ. Recovery of plasma corticotrophin and cortisol levels after three-week course of prednisolone. Thorax. 1981;36:22-24.
- O’Driscoll BR, Kalra S, Wilson M, Pickering CA, Carroll KB, Woodcock AA. Double-blind trial of steroid tapering in acute asthma. Lancet. 1993; 341:324-7.
Case
A 66-year-old Caucasian female with moderate chronic obstructive pulmonary disease (COPD) (FEV1 55% predicted), obesity, hypertension, and Type 2 diabetes mellitus on insulin therapy presents to the ED with four days of increased cough productive of yellow sputum and progressive shortness of breath. Her physical exam is notable for an oxygen saturation of 87% on room air, along with diffuse expiratory wheezing with use of accessory muscles; her chest X-ray is unchanged from previous. The patient is given oxygen, nebulized bronchodilators, and one dose of IV methylprednisolone. Her symptoms do not improve significantly, and she is admitted for further management. What regimen of corticosteroids is most appropriate to treat her acute exacerbation of COPD?
Overview
COPD is the fourth-leading cause of death in the United States and continues to increase in prevalence.1 Acute exacerbations of COPD (AECOPD) contribute significantly to this high mortality rate, which approaches 40% at one year in those patients requiring mechanical support.1 An exacerbation of COPD has been defined as an acute change in a patient’s baseline dyspnea, cough, and/or sputum beyond day-to-day variability sufficient to warrant a change in therapy.2 Exacerbations commonly occur in COPD patients and often necessitate hospital admission. In fact, COPD consistently is one of the 10 most common reasons for hospitalization, with billions of dollars in associated healthcare costs.3
The goals for inpatient management of AECOPD are to provide acute symptom relief and to minimize the potential for subsequent exacerbations. These are accomplished via a multifaceted approach, including the use of bronchodilators, antibiotics, supplemental oxygen, noninvasive positive pressure ventilation in certain circumstances, and systemic corticosteroids.
The administration of systemic steroids in AECOPD has been prevalent for several decades, with initial studies showing positive effects on lung function, specifically FEV1.4 Studies have demonstrated the benefit of steroids in prolonging the time to subsequent exacerbation, reducing the rate of treatment failure, and reducing length of stay (LOS).5 Corticosteroids have since become an essential component of the standard of care in AECOPD management.
Despite consensus that systemic steroids should be used in COPD exacerbations, a great deal of controversy still surrounds the optimal steroid regimen.6 Steroid use is not without risk, as steroids can lead to adverse outcomes in medically complex hospitalized patients (see Table 1, below). Current guidelines provide limited guidance as to the optimal route of administration, dosing regimen, or length of therapy; clinical practice varies widely.
Review of the Data
Administration route: intravenous (IV) vs. oral. The use of steroids in AECOPD began with such IV formulations as methylprednisolone, and this became the typical method of treating hospitalized patients. This practice was validated in a multicenter Veterans Affairs trial, which demonstrated decreased risk of treatment failure (defined as all-cause mortality, need for intubation, readmission for COPD, or intensification of pharmacologic therapy) for patients randomized to receive an IV-to-oral steroid regimen compared with those randomized to placebo.5 Patients receiving steroids also had shorter LOS and improvements in FEV1 after the first day of treatment. Subsequent randomized controlled trials in patients with AECOPD demonstrated the benefit of oral regimens compared with placebo with regard to FEV1, LOS, and risk of treatment failure.6,7,8
Similarities in the bioavailability of oral and IV steroids have been known for a long time.9 Comparisons in efficacy initially were completed in the management of acute asthma exacerbations, with increasing evidence, including a meta-analysis, demonstrating no difference in improvement in pulmonary function and in preventing relapse of exacerbations for oral compared with IV steroids.10 However, only recently have oral and IV steroids been compared in the treatment of AECOPD. De Jong et al randomized more than 200 patients hospitalized for AECOPD to 60 mg of either IV or oral prednisolone for five days, followed by a week of an oral taper.11 There were no significant differences in treatment failure between the IV and oral groups (62% vs. 56%, respectively, at 90 days; one-sided lower bound of the 95% confidence interval [CI], −5.8%).
A large observational study by Lindenauer et al, including nearly 80,000 AECOPD patients admitted at more than 400 hospitals, added further support to the idea that oral and IV steroids were comparable in efficacy.12 In this study, multivariate analysis found no difference in treatment failure between oral and IV groups (odds ratio [OR] 0.93; 95% CI, 0.84-1.02). The authors also found, however, that current clinical practice still overwhelmingly favors intravenous steroids, with 92% of study patients initially being administered IV steroids.12
Based on the evidence from de Jong and Lindenauer, it appears that there is no significant benefit to the use of IV over oral steroids. Additionally, there is evidence for oral administration being associated with beneficial effects on cost and hospital LOS.12 Oral steroids, therefore, are the preferred route of administration to treat a hospitalized patient with AECOPD, unless the patient is unable to tolerate oral medications. Current guidelines support the practice of giving oral steroids as first-line treatment for AECOPD (see Table 2, above).
High dose vs. low dose. Another important clinical issue concerns the dosing of steroids. The randomized trials examining the use of corticosteroids in AECOPD vary widely in the dosages studied. Further, the majority of these trials have compared steroids to placebo, rather than comparing different dosage regimens. The agents studied have included prednisone, prednisolone, methylprednisolone, and hydrocortisone, or combinations thereof. In order to compare regimens of these different drugs, steroid doses often are converted into prednisone equivalents (see Table 3, below). Though no guidelines define “high dose” and “low dose,” some studies have designated doses of >80 mg prednisone equivalents daily as high-dose and prednisone equivalents of ≤80 mg daily as low-dose.13,14
Starting doses of systemic corticosteroids in the treatment of AECOPD in clinical studies range from prednisone equivalents of 30 mg daily to 625 mg on the first day of treatment.5,8 No randomized studies of high- versus low-dose steroid regimens have been conducted. One retrospective chart review of 145 AECOPD admissions evaluated outcomes among patients who were given higher (mean daily dose >80 mg prednisone equivalent) and lower (mean daily dose of ≤80 mg prednisone) doses.14 The authors found that patients who received higher doses of steroids had significantly longer LOS compared with those who received lower doses, especially among the subset of patients who were admitted to the floor rather than the ICU, though this analysis did not adjust for severity of illness. In this study, the most striking finding noted by the authors was the wide variability in the steroid doses prescribed for the inpatient treatment of AECOPD.
More recently, the study by Lindenauer et al examined outcomes between patients treated with high-dose IV steroids (equivalent of 120 mg-800 mg of prednisone on the first or second day of treatment) compared to low-dose oral steroids (prednisone equivalents of 20 mg-80 mg per day).12 The authors found no differences between the two groups regarding the rate of treatment failure, defined by initiation of mechanical ventilation after the second hospital day, in-hospital mortality, or readmission for COPD within 30 days of discharge. After multivariate adjustment, including the propensity for oral treatment, the low-dose oral therapy group was found to have lower risk of treatment failure, shorter LOS, and lower total hospital cost.
Despite the heterogeneity of the published data and the lack of randomized trials, the existing evidence suggests that low-dose prednisone (or equivalent) is similar in efficacy to higher doses and generally is associated with shorter hospital stays. Recognizing these benefits, guidelines do favor initiating treatment with low-dose steroids in patients admitted with AECOPD. The most recent publications from the American Thoracic Society/European Respiratory Society Task Force (ATS/ERS), the Global Initiative for Chronic Obstructive Lung Disease (GOLD), the National Clinical Guidelines Centre in the United Kingdom, and the Canadian Thoracic Society all recommend equivalent dosing of prednisone in patients admitted with AECOPD who are able to tolerate oral intake (see Table 2).1,2,15,16
Duration. As with the dosing of systemic corticosteroids in AECOPD, the optimal duration of treatment is not well-established. National and international consensus panels vary in their recommendations, as outlined in Table 2. This may be related to the variability in length of treatment found in the literature.
Treatment durations ranging from one day to eight weeks have been studied in inpatients with AECOPD. The landmark randomized controlled trial by Niewoehner and colleagues compared two-week and eight-week courses of systemic corticosteroids and found no difference in the rates of treatment failure, which included death, need for mechanical ventilation, readmission for COPD, and intensification of pharmacologic therapy.5 Based on these results, many experts have concluded that there is no benefit to steroid courses lasting beyond two weeks.
Although improvements in outcomes have been demonstrated with corticosteroid regimens as short as three days compared with placebo, most of the randomized controlled trials have included courses of seven to 14 days.4 Given the risks of adverse events (e.g. hyperglycemia) that are associated with systemic administration of steroids, the shortest effective duration should be considered.
In both clinical practice and clinical studies, steroid regimens often include a taper. A study by Vondracek and Hemstreet found that 79% of hospital discharges for AECOPD included a tapered corticosteroid regimen.14 From a physiologic standpoint, durations of corticosteroid treatment approximately three weeks or less, regardless of dosage, should not lead to adrenal suppression.17 There also is no evidence to suggest that abrupt discontinuation of steroids leads to clinical worsening of disease, and complicated steroid tapers are a potential source of medication errors after hospital discharge.18 Furthermore, the clinical guidelines do not address the tapering of corticosteroids. Therefore, there is a lack of evidence advocating for or against the use of tapered steroid regimens in AECOPD.
Back to the Case
In addition to standard treatment modalities for AECOPD, our patient was administered oral prednisone 40 mg daily. She experienced steroid-induced hyperglycemia, which was corrected with adjustment of her insulin regimen. The patient’s pulmonary symptoms improved within 72 hours, and she was discharged home on hospital day four to complete a seven-day steroid course. At hospital discharge, she was administered influenza and pneumococcal vaccinations, and she was instructed to resume her usual insulin dosing once she finished her prednisone course.
Overview
In the management of AECOPD, there remains a lack of consensus in defining the ideal steroid regimen. Based on current literature, the use of low-dose oral corticosteroids, such as prednisone 40 mg daily, for a seven- to 14-day course is recommended. TH
Dr. Cunningham is an assistant professor of internal medicine and academic hospitalist in the section of hospital medicine at Vanderbilt University School of Medicine in Nashville, Tenn. Dr. LaBrin is an assistant professor of internal medicine and pediatrics and academic hospitalist at Vanderbilt University School of Medicine.
References
- From the Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2010. Global Initiative for Chronic Obstructive Lung Disease website. Available at: www.goldcopd.org/GuidelineItem.asp?intId=989. Accessed Feb. 21, 2011.
- Celli BR, MacNee W, ATS/ERS Task Force. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004;23:932-946.
- Morbidity and mortality: 2009 chart book on cardiovascular, lung, and blood diseases. National Institutes of Health’s National Heart, Lung, and Blood Institute website. Available at: www.nhlbi.nih.gov/resources/docs/2009_ChartBook.pdf. Accessed Feb. 24, 2011.
- Albert RK, Martin TR, Lewis SW. Controlled trial of methylprednisolone in patients with chronic bronchitis and acute respiratory insufficiency. Ann Intern Med. 1980;92(6):753-758.
- Niewoehner DE, Erbland ML, Deupree RH, et al. Effect of systemic glucocorticoids on exacerbations of chronic obstructive pulmonary disease. Department of Veterans Affairs Cooperative Study Group. N Engl J Med. 1999;340(25):1941-1947.
- Thompson WH, Nielson C, Carvalho P, Charan NB, Crowley JJ. Controlled trial of oral prednisone in outpatients with acute COPD exacerbation. Am J Respir Crit Care Med. 1996;154:407-412.
- Seemungal TA, Donaldson GC, Bhowmik A, Jeffries DJ, Wedzicha JA. Time course and recovery of exacerbations in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2000;161:1608-1613.
- Davies L, Angus RM, Calverley PM. Oral corticosteroids in patients admitted to hospital with exacerbations of chronic obstructive pulmonary disease: a prospective randomised controlled trial. Lancet. 1999;354(9177):456-460.
- Al-Habet S, Rogers HJ. Pharmacokinetics of intravenous and oral prednisolone. Br J Clin Pharmacol. 1980;10(5):503-508.
- Rowe BH, Keller JL, Oxman AD. Effectiveness of steroid therapy in acute exacerbations of asthma: a meta-analysis. Am J Emerg Med. 1992;10:301-310.
- De Jong YP, Uil SM, Grotjohan HP, Postma DS, Kerstjens HA, van den Berg JW. Oral or IV prednisolone in the treatment of COPD exacerbations: A randomized, controlled, double-blind study. Chest. 2007;132(6):1741-1747.
- Lindenauer PK, Pekow PS, Lahti MC, Lee Y, Benjamin EM, Rothberg MB. Association of corticosteroid dose and route of administration with risk of treatment failure in acute exacerbation of chronic obstructive pulmonary disease. JAMA. 2010;303(23):2359-2367.
- Manser R, Reid D, Abramsom MJ. Corticosteroids for acute severe asthma in hospitalized patients. Cochrane Database Syst Rev. 2000;(2):CD001740.
- Vondracek SF, Hemstreet BA. Retrospective evaluation of systemic corticosteroids for the management of acute exacerbations of chronic obstructive pulmonary disease. Am J Health Syst Pharm. 2006;63:645-652.
- Chronic obstructive pulmonary disease: management of chronic obstructive pulmonary disease in adults in primary and secondary care. National Institute for Health and Clinical Excellence website. Available at: guidance.nice.org.uk/CG101/Guidance/pdf/English. Accessed Feb. 21, 2011.
- O’Donnell DE, Aaron S, Bourbeau J, et al. Canadian Thoracic Society recommendations for management of chronic obstructive pulmonary disease—2007 update. Can Respir J. 2007;14 Suppl B:5B-32B.
- Webb J, Clark TJ. Recovery of plasma corticotrophin and cortisol levels after three-week course of prednisolone. Thorax. 1981;36:22-24.
- O’Driscoll BR, Kalra S, Wilson M, Pickering CA, Carroll KB, Woodcock AA. Double-blind trial of steroid tapering in acute asthma. Lancet. 1993; 341:324-7.
Case
A 66-year-old Caucasian female with moderate chronic obstructive pulmonary disease (COPD) (FEV1 55% predicted), obesity, hypertension, and Type 2 diabetes mellitus on insulin therapy presents to the ED with four days of increased cough productive of yellow sputum and progressive shortness of breath. Her physical exam is notable for an oxygen saturation of 87% on room air, along with diffuse expiratory wheezing with use of accessory muscles; her chest X-ray is unchanged from previous. The patient is given oxygen, nebulized bronchodilators, and one dose of IV methylprednisolone. Her symptoms do not improve significantly, and she is admitted for further management. What regimen of corticosteroids is most appropriate to treat her acute exacerbation of COPD?
Overview
COPD is the fourth-leading cause of death in the United States and continues to increase in prevalence.1 Acute exacerbations of COPD (AECOPD) contribute significantly to this high mortality rate, which approaches 40% at one year in those patients requiring mechanical support.1 An exacerbation of COPD has been defined as an acute change in a patient’s baseline dyspnea, cough, and/or sputum beyond day-to-day variability sufficient to warrant a change in therapy.2 Exacerbations commonly occur in COPD patients and often necessitate hospital admission. In fact, COPD consistently is one of the 10 most common reasons for hospitalization, with billions of dollars in associated healthcare costs.3
The goals for inpatient management of AECOPD are to provide acute symptom relief and to minimize the potential for subsequent exacerbations. These are accomplished via a multifaceted approach, including the use of bronchodilators, antibiotics, supplemental oxygen, noninvasive positive pressure ventilation in certain circumstances, and systemic corticosteroids.
The administration of systemic steroids in AECOPD has been prevalent for several decades, with initial studies showing positive effects on lung function, specifically FEV1.4 Studies have demonstrated the benefit of steroids in prolonging the time to subsequent exacerbation, reducing the rate of treatment failure, and reducing length of stay (LOS).5 Corticosteroids have since become an essential component of the standard of care in AECOPD management.
Despite consensus that systemic steroids should be used in COPD exacerbations, a great deal of controversy still surrounds the optimal steroid regimen.6 Steroid use is not without risk, as steroids can lead to adverse outcomes in medically complex hospitalized patients (see Table 1, below). Current guidelines provide limited guidance as to the optimal route of administration, dosing regimen, or length of therapy; clinical practice varies widely.
Review of the Data
Administration route: intravenous (IV) vs. oral. The use of steroids in AECOPD began with such IV formulations as methylprednisolone, and this became the typical method of treating hospitalized patients. This practice was validated in a multicenter Veterans Affairs trial, which demonstrated decreased risk of treatment failure (defined as all-cause mortality, need for intubation, readmission for COPD, or intensification of pharmacologic therapy) for patients randomized to receive an IV-to-oral steroid regimen compared with those randomized to placebo.5 Patients receiving steroids also had shorter LOS and improvements in FEV1 after the first day of treatment. Subsequent randomized controlled trials in patients with AECOPD demonstrated the benefit of oral regimens compared with placebo with regard to FEV1, LOS, and risk of treatment failure.6,7,8
Similarities in the bioavailability of oral and IV steroids have been known for a long time.9 Comparisons in efficacy initially were completed in the management of acute asthma exacerbations, with increasing evidence, including a meta-analysis, demonstrating no difference in improvement in pulmonary function and in preventing relapse of exacerbations for oral compared with IV steroids.10 However, only recently have oral and IV steroids been compared in the treatment of AECOPD. De Jong et al randomized more than 200 patients hospitalized for AECOPD to 60 mg of either IV or oral prednisolone for five days, followed by a week of an oral taper.11 There were no significant differences in treatment failure between the IV and oral groups (62% vs. 56%, respectively, at 90 days; one-sided lower bound of the 95% confidence interval [CI], −5.8%).
A large observational study by Lindenauer et al, including nearly 80,000 AECOPD patients admitted at more than 400 hospitals, added further support to the idea that oral and IV steroids were comparable in efficacy.12 In this study, multivariate analysis found no difference in treatment failure between oral and IV groups (odds ratio [OR] 0.93; 95% CI, 0.84-1.02). The authors also found, however, that current clinical practice still overwhelmingly favors intravenous steroids, with 92% of study patients initially being administered IV steroids.12
Based on the evidence from de Jong and Lindenauer, it appears that there is no significant benefit to the use of IV over oral steroids. Additionally, there is evidence for oral administration being associated with beneficial effects on cost and hospital LOS.12 Oral steroids, therefore, are the preferred route of administration to treat a hospitalized patient with AECOPD, unless the patient is unable to tolerate oral medications. Current guidelines support the practice of giving oral steroids as first-line treatment for AECOPD (see Table 2, above).
High dose vs. low dose. Another important clinical issue concerns the dosing of steroids. The randomized trials examining the use of corticosteroids in AECOPD vary widely in the dosages studied. Further, the majority of these trials have compared steroids to placebo, rather than comparing different dosage regimens. The agents studied have included prednisone, prednisolone, methylprednisolone, and hydrocortisone, or combinations thereof. In order to compare regimens of these different drugs, steroid doses often are converted into prednisone equivalents (see Table 3, below). Though no guidelines define “high dose” and “low dose,” some studies have designated doses of >80 mg prednisone equivalents daily as high-dose and prednisone equivalents of ≤80 mg daily as low-dose.13,14
Starting doses of systemic corticosteroids in the treatment of AECOPD in clinical studies range from prednisone equivalents of 30 mg daily to 625 mg on the first day of treatment.5,8 No randomized studies of high- versus low-dose steroid regimens have been conducted. One retrospective chart review of 145 AECOPD admissions evaluated outcomes among patients who were given higher (mean daily dose >80 mg prednisone equivalent) and lower (mean daily dose of ≤80 mg prednisone) doses.14 The authors found that patients who received higher doses of steroids had significantly longer LOS compared with those who received lower doses, especially among the subset of patients who were admitted to the floor rather than the ICU, though this analysis did not adjust for severity of illness. In this study, the most striking finding noted by the authors was the wide variability in the steroid doses prescribed for the inpatient treatment of AECOPD.
More recently, the study by Lindenauer et al examined outcomes between patients treated with high-dose IV steroids (equivalent of 120 mg-800 mg of prednisone on the first or second day of treatment) compared to low-dose oral steroids (prednisone equivalents of 20 mg-80 mg per day).12 The authors found no differences between the two groups regarding the rate of treatment failure, defined by initiation of mechanical ventilation after the second hospital day, in-hospital mortality, or readmission for COPD within 30 days of discharge. After multivariate adjustment, including the propensity for oral treatment, the low-dose oral therapy group was found to have lower risk of treatment failure, shorter LOS, and lower total hospital cost.
Despite the heterogeneity of the published data and the lack of randomized trials, the existing evidence suggests that low-dose prednisone (or equivalent) is similar in efficacy to higher doses and generally is associated with shorter hospital stays. Recognizing these benefits, guidelines do favor initiating treatment with low-dose steroids in patients admitted with AECOPD. The most recent publications from the American Thoracic Society/European Respiratory Society Task Force (ATS/ERS), the Global Initiative for Chronic Obstructive Lung Disease (GOLD), the National Clinical Guidelines Centre in the United Kingdom, and the Canadian Thoracic Society all recommend equivalent dosing of prednisone in patients admitted with AECOPD who are able to tolerate oral intake (see Table 2).1,2,15,16
Duration. As with the dosing of systemic corticosteroids in AECOPD, the optimal duration of treatment is not well-established. National and international consensus panels vary in their recommendations, as outlined in Table 2. This may be related to the variability in length of treatment found in the literature.
Treatment durations ranging from one day to eight weeks have been studied in inpatients with AECOPD. The landmark randomized controlled trial by Niewoehner and colleagues compared two-week and eight-week courses of systemic corticosteroids and found no difference in the rates of treatment failure, which included death, need for mechanical ventilation, readmission for COPD, and intensification of pharmacologic therapy.5 Based on these results, many experts have concluded that there is no benefit to steroid courses lasting beyond two weeks.
Although improvements in outcomes have been demonstrated with corticosteroid regimens as short as three days compared with placebo, most of the randomized controlled trials have included courses of seven to 14 days.4 Given the risks of adverse events (e.g. hyperglycemia) that are associated with systemic administration of steroids, the shortest effective duration should be considered.
In both clinical practice and clinical studies, steroid regimens often include a taper. A study by Vondracek and Hemstreet found that 79% of hospital discharges for AECOPD included a tapered corticosteroid regimen.14 From a physiologic standpoint, durations of corticosteroid treatment approximately three weeks or less, regardless of dosage, should not lead to adrenal suppression.17 There also is no evidence to suggest that abrupt discontinuation of steroids leads to clinical worsening of disease, and complicated steroid tapers are a potential source of medication errors after hospital discharge.18 Furthermore, the clinical guidelines do not address the tapering of corticosteroids. Therefore, there is a lack of evidence advocating for or against the use of tapered steroid regimens in AECOPD.
Back to the Case
In addition to standard treatment modalities for AECOPD, our patient was administered oral prednisone 40 mg daily. She experienced steroid-induced hyperglycemia, which was corrected with adjustment of her insulin regimen. The patient’s pulmonary symptoms improved within 72 hours, and she was discharged home on hospital day four to complete a seven-day steroid course. At hospital discharge, she was administered influenza and pneumococcal vaccinations, and she was instructed to resume her usual insulin dosing once she finished her prednisone course.
Overview
In the management of AECOPD, there remains a lack of consensus in defining the ideal steroid regimen. Based on current literature, the use of low-dose oral corticosteroids, such as prednisone 40 mg daily, for a seven- to 14-day course is recommended. TH
Dr. Cunningham is an assistant professor of internal medicine and academic hospitalist in the section of hospital medicine at Vanderbilt University School of Medicine in Nashville, Tenn. Dr. LaBrin is an assistant professor of internal medicine and pediatrics and academic hospitalist at Vanderbilt University School of Medicine.
References
- From the Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2010. Global Initiative for Chronic Obstructive Lung Disease website. Available at: www.goldcopd.org/GuidelineItem.asp?intId=989. Accessed Feb. 21, 2011.
- Celli BR, MacNee W, ATS/ERS Task Force. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004;23:932-946.
- Morbidity and mortality: 2009 chart book on cardiovascular, lung, and blood diseases. National Institutes of Health’s National Heart, Lung, and Blood Institute website. Available at: www.nhlbi.nih.gov/resources/docs/2009_ChartBook.pdf. Accessed Feb. 24, 2011.
- Albert RK, Martin TR, Lewis SW. Controlled trial of methylprednisolone in patients with chronic bronchitis and acute respiratory insufficiency. Ann Intern Med. 1980;92(6):753-758.
- Niewoehner DE, Erbland ML, Deupree RH, et al. Effect of systemic glucocorticoids on exacerbations of chronic obstructive pulmonary disease. Department of Veterans Affairs Cooperative Study Group. N Engl J Med. 1999;340(25):1941-1947.
- Thompson WH, Nielson C, Carvalho P, Charan NB, Crowley JJ. Controlled trial of oral prednisone in outpatients with acute COPD exacerbation. Am J Respir Crit Care Med. 1996;154:407-412.
- Seemungal TA, Donaldson GC, Bhowmik A, Jeffries DJ, Wedzicha JA. Time course and recovery of exacerbations in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2000;161:1608-1613.
- Davies L, Angus RM, Calverley PM. Oral corticosteroids in patients admitted to hospital with exacerbations of chronic obstructive pulmonary disease: a prospective randomised controlled trial. Lancet. 1999;354(9177):456-460.
- Al-Habet S, Rogers HJ. Pharmacokinetics of intravenous and oral prednisolone. Br J Clin Pharmacol. 1980;10(5):503-508.
- Rowe BH, Keller JL, Oxman AD. Effectiveness of steroid therapy in acute exacerbations of asthma: a meta-analysis. Am J Emerg Med. 1992;10:301-310.
- De Jong YP, Uil SM, Grotjohan HP, Postma DS, Kerstjens HA, van den Berg JW. Oral or IV prednisolone in the treatment of COPD exacerbations: A randomized, controlled, double-blind study. Chest. 2007;132(6):1741-1747.
- Lindenauer PK, Pekow PS, Lahti MC, Lee Y, Benjamin EM, Rothberg MB. Association of corticosteroid dose and route of administration with risk of treatment failure in acute exacerbation of chronic obstructive pulmonary disease. JAMA. 2010;303(23):2359-2367.
- Manser R, Reid D, Abramsom MJ. Corticosteroids for acute severe asthma in hospitalized patients. Cochrane Database Syst Rev. 2000;(2):CD001740.
- Vondracek SF, Hemstreet BA. Retrospective evaluation of systemic corticosteroids for the management of acute exacerbations of chronic obstructive pulmonary disease. Am J Health Syst Pharm. 2006;63:645-652.
- Chronic obstructive pulmonary disease: management of chronic obstructive pulmonary disease in adults in primary and secondary care. National Institute for Health and Clinical Excellence website. Available at: guidance.nice.org.uk/CG101/Guidance/pdf/English. Accessed Feb. 21, 2011.
- O’Donnell DE, Aaron S, Bourbeau J, et al. Canadian Thoracic Society recommendations for management of chronic obstructive pulmonary disease—2007 update. Can Respir J. 2007;14 Suppl B:5B-32B.
- Webb J, Clark TJ. Recovery of plasma corticotrophin and cortisol levels after three-week course of prednisolone. Thorax. 1981;36:22-24.
- O’Driscoll BR, Kalra S, Wilson M, Pickering CA, Carroll KB, Woodcock AA. Double-blind trial of steroid tapering in acute asthma. Lancet. 1993; 341:324-7.
In the Literature: HM-Related Research You Need to Know
In This Edition
Literature at a Glance
A guide to this month’s studies
- Continuous insulin infusion in non-ICU patients
- How hospitalists spend their day
- Outcomes of patients leaving against medical advice
- Prediction rule for readmission
- Effects of high- vs. low-dose PPIs for peptic ulcer
- Hospital utilization by generalists before hospitalists
- Effect of hospitalist fragmentation on length of stay
- Medication errors at admissions in older patients
Continuous Insulin Infusion Provides Effective Glycemic Control in Non-ICU Patients
Clinical question: Is continuous insulin infusion (CII) a safe and effective option in the management of hyperglycemia in non-ICU patients?
Background: Hyperglycemia has been associated with worse outcomes in hospitalized patients. Prior research has demonstrated the benefit of CII in managing hyperglycemia in the ICU setting. However, outcomes have not been evaluated in the general medical (non-ICU) setting, where hyperglycemia is often inadequately addressed.
Study design: Retrospective chart review.
Setting: Urban tertiary-care medical center.
Synopsis: Charts of 200 adult patients treated with CII in non-ICU areas were reviewed with the primary outcomes including mean daily blood glucose (BG) levels and number of hyper- and hypoglycemic events occurring on CII. Mean BG dropped from 323 mg/dL to 182 mg/dL by day one, with a BG≤of 150 achieved in 67% of patients by day two of therapy. Twenty-two percent of patients suffered a hypoglycemic event (BG<60), reportedly similar to prior studies of insulin use in ICU and non-ICU settings. Eighty-two percent of patients received some form of nutritional support while on CII. In multivariate analyses, receiving oral nutrition (either a solid or liquid diet) was the only factor associated with increased risk of hyperglycemia and hypoglycemia.
This study was limited by its retrospective analysis in a single center. No comparison was made with basal-bolus or sliding-scale insulin therapy regarding efficacy or safety.
Bottom line: Non-ICU patients with hyperglycemia who received CII were able to achieve effective glycemic control within 48 hours of initiation, with rates of hypoglycemia comparable to those observed in ICU settings.
Citation: Smiley D, Rhee M, Peng L, et al. Safety and efficacy of continuous insulin infusion in noncritical care settings. J Hosp Med. 2010;5(4):212-217.
Hospitalists Spend More Time on Indirect, Rather Than Direct, Patient Care
Clinical question: What are the components of the daily workflow of hospitalists working on a non-housestaff service?
Background: The use of hospitalists is associated with increased efficiency in the hospital setting. However, it is not known how this efficiency is achieved. Prior literature has attempted to address this question, but with increasing demands and patient census, the representativeness of existing data is unclear.
Study design: Observational time-motion study.
Setting: Urban tertiary-care academic medical center.
Synopsis: Twenty-four hospitalists were directly observed for two weekday shifts. An electronic collection tool was developed using initial data on hospitalist activities and piloted prior to formal study data collection. Direct patient care was defined as involving face-to-face interaction between hospitalist and patient, while indirect patient care involved activities relevant to patient care but not performed in the patient’s presence.
Approximately 500 hours of observation were collected. Direct patient care comprised only a mean of 17.4% of the hospitalists’ daily workflow, while more was spent on indirect care, mainly electronic health record (EHR) documentation (mean 34.1%) and communication activities (mean 25.9%). Multitasking occurred 16% of the time, typically during communication or “critical documentation activities” (e.g. writing prescriptions). As patient volume increased, less time was spent in communication, and documentation was deferred to after hours.
These results were consistent with prior observational studies but were limited to a single center and might not represent the workflow of hospitalists in other settings, such as community hospitals, or nocturnists.
Bottom line: Hospitalists on non-housestaff services spend most of their time on indirect patient care and, with increasing patient census, communication is sacrificed. Multitasking is common during periods of communication and critical documentation.
Citation: Tipping MD, Forth VE, O’Leary KJ, et al. Where did the day go?—a time-motion study of hospitalists. J Hosp Med. 2010;5(6):323-328.
Patients Who Leave Against Medical Advice Have Higher Readmission, Mortality Rates
Clinical question: What are the 30-day hospital readmission and mortality rates for Veterans Administration (VA) patients discharged against medical advice (AMA) compared with those appropriately discharged from the hospital?
Background: Patients discharged AMA might be at increased risk of experiencing worse outcomes. Small studies have demonstrated that patients with asthma and acute myocardial infarction (MI) discharged AMA have increased risk of readmission and death. However, it is unclear whether these risks are generalizable to a wider medical population.
Study design: Five-year retrospective cohort study.
Setting: One hundred twenty-nine VA acute-care hospitals.
Synopsis: Of the nearly 2 million patients admitted to the VA from 2004 to 2008, 1.7% were discharged AMA. Patients discharged AMA generally were younger, had lower incomes, and were more likely to be black. Furthermore, patients discharged AMA had statistically significant higher rates of 30-day readmission (17.7% vs. 11%, P<0.001) and higher 30-day mortality rates (0.75% vs. 0.61%, P=0.001) compared with those who had been appropriately discharged. In hazard models, discharge AMA was a significant predictor of 30-day readmission and conferred a nonstatistically significant increase in 30-day mortality.
Because all patients were seen in VA facilities, the results might not be generalizable to other acute-care settings. Although VA patients differ from the general medical population, the characteristics of patients discharged AMA are similar to those in previously published studies. The study utilized administrative data, which are very reliable but limited by little information on clinical factors that could contribute to AMA discharges.
Bottom line: Patients discharged AMA are at increased risk of worse post-hospitalization outcomes, including hospital readmission and death.
Citation: Glasgow JM, Vaughn-Sarrazin M, Kaboli PJ. Leaving against medical advice (AMA): risk of 30-day mortality and hospital readmission. J Gen Intern Med. 2010;25(9): 926-929.
Simple Model Predicts Hospital Readmission
Clinical question: Which patient-level factors can be used in a simple model to predict hospital readmission of medicine patients?
Background: Hospital readmissions are common and costly. Previously published readmission prediction models have had limited utility because they focused on a specific condition, setting, or population, or were too cumbersome for practical use.
Study design: Prospective observational cohort study.
Setting: Six academic medical centers.
Synopsis: Data from nearly 11,000 general medicine patients were included in the analysis. Overall, almost 18% of patients were readmitted within 30 days of discharge.
In the prediction model derived and validated from the data, seven factors were significant predictors of readmission within 30 days of discharge: insurance status, marital status, having a regular healthcare provider, Charlson comorbidity index, SF 12 physical component score, one or more admissions within the last year, and current length of stay greater than two days. Points assigned from each significant predictor were used to create a risk score. The 5% of patients with risk scores of 25 and higher had 30-day readmission rates of approximately 30%, compared to readmission rates of approximately 16% in patients with scores of less than 25.
These results might not be generalizable to small, rural, nonacademic settings. Planned admissions could not be excluded from the data, and readmissions to nonstudy hospitals could not be ascertained. Despite these limitations, this model is easier to use than prior models and relevant to a broad population of patients.
Bottom line: A simple prediction model using patient-level factors can be used to identify patients at higher risk of readmission within 30 days of discharge to home.
Citation: Hasan O, Meltzer DO, Shaykevich SA, et al. Hospital readmission in general medicine patients: a prediction model. J Gen Intern Med. 2010;25(3):211-219.
No Difference in Outcomes Between High- and Non-High-Dose Proton Pump Inhibitors in Bleeding Peptic Ulcers
Clinical question: Do high-dose proton pump inhibitors (PPIs) decrease the rate of rebleeding, surgical intervention, or mortality in patients with bleeding peptic ulcers who have undergone endoscopic treatment?
Background: Previous studies have demonstrated superiority of both high- and low-dose PPIs to H2 receptor antagonists and placebo in reducing rebleeding rates in patients with peptic ulcers. However, no clear evidence is available to suggest that high-dose PPIs are more effective than non-high-dose PPIs for treatment of bleeding peptic ulcers.
Study design: Systematic review and meta-analysis.
Setting: Multicenter and single-site studies conducted in several countries.
Synopsis: Studies were included if they were randomized controlled trials, compared high- versus non-high-dose PPIs, evaluated endoscopically confirmed bleeding ulcers, gave PPIs after endoscopy, and documented outcomes regarding rates of rebleeding, surgical intervention, or mortality. High-dose PPIs were defined as equivalent to omeprazole 80 mg intravenous bolus followed by continuous intravenous infusion at 8 mg/hr for 72 hours.
Seven studies met inclusion criteria. The pooled odds ratios for rebleeding, surgical intervention, and mortality were 1.30 (95% CI, 0.88-1.91), 1.49 (95% CI, 0.66-3.37), and 0.89 (95% CI, 0.37-2.13), respectively, for high-dose versus non-high-dose PPIs. The authors concluded that high-dose PPIs were not superior to non-high-dose PPIs in reducing the rates of these adverse outcomes after endoscopic treatment of bleeding ulcers. Considering the cost of high-dose PPIs, further studies are indicated to help guide PPI dosing for patients with peptic ulcers.
Major limitations of this study were the small number of studies (1,157 patients in total) and their heterogeneity, and the lack of intention-to-treat analysis. The studies also included a high Asian predominance, and it has been shown that Asian populations have an enhanced PPI effect.
Bottom line: High-dose PPIs did not demonstrate reduced rates of ulcer rebleeding, surgical intervention, or mortality compared with non-high-dose PPIs in this meta-analysis, which included a small number of studies and patients.
Citation: Wang CH, Ma MH, Chou HC, et al. High-dose vs. non-high-dose proton pump inhibitors after endoscopic treatment in patients with bleeding peptic ulcer: a systematic review and meta-analysis of randomized controlled trials. Arch Intern Med. 2010;170(9):751-758.
Hospital Utilization by Practicing Generalists Declined before the Emergence of Hospitalists
Clinical question: What has been the pattern of hospital utilization by generalists before and after the emergence of hospitalists?
Background: It has been proposed that the emergence of hospitalists has “crowded out” generalist physicians from the U.S. hospital setting. This study evaluated the trends of inpatient practice by generalists both before and after the emergence of hospitalists.
Study design: Retrospective analysis of national databases.
Setting: U.S. data from 1980 to 2005.
Synopsis: Utilizing the National Hospital Discharge Survey and the American Medical Association’s Physician Characteristics and Distribution in the U.S., information was extracted to evaluate the average number of annual inpatient encounters relative to generalist workforce from 1980 to 2005. Total inpatient encounters for each year were calculated by multiplying the total number of hospital admissions by the average hospital length of stay. The emergence of hospitalists was defined as beginning in 1994.
Total inpatient encounters by generalists declined by 35% in the pre-hospitalist era but remained essentially unchanged in the hospitalist era. During the pre-hospitalist period, the number of generalists doubled, to more than 200,000 from approximately 100,000, while the number of hospital discharges remained relatively stable and the length of stay declined by a third. The decrease in average inpatient encounters in the pre-hospitalist era is thought to have been secondary to decreased length of stay and increased workforce.
Bottom line: Hospital utilization relative to generalist physician workforce was decreasing prior to the emergence of hospitalists mainly due to decreased length of hospital stay and increased numbers of physicians.
Citation: Meltzer DO, Chung JW. U.S. trends in hospitalization and generalist physician workforce and the emergence of hospitalists. J Gen Intern Med. 2010;25(5):453-459.
Fragmentation of Hospitalist Care Is Associated with Increased Length of Stay
Clinical question: Does fragmentation of care (FOC) by hospitalists affect length of stay (LOS)?
Background: Previous investigations have explored the impact of FOC provided by residency programs on LOS and quality of care. Results of these studies have been mixed. However, there have been no prior studies on the impact of the fragmentation of hospitalist care on LOS.
Study design: Concurrent control study.
Setting: Hospitalist practices all over the country managed by IPC: The Hospitalist Company.
Synopsis: Investigators looked at 10,977 patients admitted with diagnoses of pneumonia or heart failure. The primary endpoint was LOS. The independent variable of interest was a measure of FOC. The FOC was calculated as a quantitative index, by determining the percentage of hospitalist care delivered by a physician other than the primary hospitalist.
Multivariable analyses revealed a statistically significant increase in LOS of 0.39 days for each 10% increase in fragmentation level for pneumonia admissions. Similarly, for patients with heart failure, there was a significant increase in LOS of 0.30 days for each 10% increase in fragmentation level.
The study is a concurrent control study, so conclusions cannot be drawn about causality. Additionally, there are likely unmeasured differences between every hospital and hospitalist practice, which could further confound the relationships between hospitalist care and LOS.
Bottom line: Fragmentation of care provided by hospitalists is associated with an increased LOS in patients hospitalized for pneumonia or heart failure.
Citation: Epstein K, Juarez E, Epstein A, Loya K, Singer A. The impact of fragmentation of hospitalist care on length of stay. J Hosp Med. 2010;5(6):335-338.
Admission Medication Errors Are Common and Most Harmful in Older Patients Taking Many Medications
Clinical question: What are the risk factors and potential harm associated with medication errors at hospital admission?
Background: Obtaining a medication history from a hospitalized patient is an error-prone process. Several variables can affect the completeness and quality of medication histories, but existing data are limited regarding patient or medication risk factors associated with medication errors at admission.
Study design: Prospective cohort study.
Setting: Academic hospital in Chicago.
Synopsis: Pharmacist and admitting physician medication histories were compared with admission medication orders to identify any unexplained discrepancies. Discrepancies resulting in order changes were defined as medication errors.
Of the 651 adult medical inpatients studied, 234 (35.9%) had medication order errors identified at admission. Errors originated in the medication histories for 85% of these patients. The most frequent type of error was an omission (48.9%). An age of 65 or older (odds ratio [OR]=2.17, 95% confidence interval [CI], 1.09-4.30) and increased number of medications (OR=1.21, 95% CI, 1.14-1.29) were the only risk factors identified by multivariate analysis to be independently associated with increased risk of medication order errors potentially causing harm or requiring monitoring or intervention. Presenting a medication list upon admission was a significant protective factor (OR=0.35, 95% CI, 0.19-0.63).
Though this is the largest study to date evaluating admission medication errors in hospitalized medical patients, it remains limited by its single hospital site. Because the authors were unable to interview patients who were too ill or unwilling to participate and had no caregiver present, they might have underestimated the number of admission errors. Further, the harm assessment was based on potential and not actual harm.
Bottom line: Admission medication order errors are frequent, most commonly originate in the medication histories, and have increased potential to cause adverse outcomes in older patients and those taking higher numbers of medications.
Citation: Gleason KM, McDaniel MR, Feinglass J, et al. Results of the Medications At Transitions and Clinical Handoffs (MATCH) study: an analysis of medication reconciliation errors and risk factors at hospital admission. J Gen Intern Med. 2010;25(5):441-447.
In This Edition
Literature at a Glance
A guide to this month’s studies
- Continuous insulin infusion in non-ICU patients
- How hospitalists spend their day
- Outcomes of patients leaving against medical advice
- Prediction rule for readmission
- Effects of high- vs. low-dose PPIs for peptic ulcer
- Hospital utilization by generalists before hospitalists
- Effect of hospitalist fragmentation on length of stay
- Medication errors at admissions in older patients
Continuous Insulin Infusion Provides Effective Glycemic Control in Non-ICU Patients
Clinical question: Is continuous insulin infusion (CII) a safe and effective option in the management of hyperglycemia in non-ICU patients?
Background: Hyperglycemia has been associated with worse outcomes in hospitalized patients. Prior research has demonstrated the benefit of CII in managing hyperglycemia in the ICU setting. However, outcomes have not been evaluated in the general medical (non-ICU) setting, where hyperglycemia is often inadequately addressed.
Study design: Retrospective chart review.
Setting: Urban tertiary-care medical center.
Synopsis: Charts of 200 adult patients treated with CII in non-ICU areas were reviewed with the primary outcomes including mean daily blood glucose (BG) levels and number of hyper- and hypoglycemic events occurring on CII. Mean BG dropped from 323 mg/dL to 182 mg/dL by day one, with a BG≤of 150 achieved in 67% of patients by day two of therapy. Twenty-two percent of patients suffered a hypoglycemic event (BG<60), reportedly similar to prior studies of insulin use in ICU and non-ICU settings. Eighty-two percent of patients received some form of nutritional support while on CII. In multivariate analyses, receiving oral nutrition (either a solid or liquid diet) was the only factor associated with increased risk of hyperglycemia and hypoglycemia.
This study was limited by its retrospective analysis in a single center. No comparison was made with basal-bolus or sliding-scale insulin therapy regarding efficacy or safety.
Bottom line: Non-ICU patients with hyperglycemia who received CII were able to achieve effective glycemic control within 48 hours of initiation, with rates of hypoglycemia comparable to those observed in ICU settings.
Citation: Smiley D, Rhee M, Peng L, et al. Safety and efficacy of continuous insulin infusion in noncritical care settings. J Hosp Med. 2010;5(4):212-217.
Hospitalists Spend More Time on Indirect, Rather Than Direct, Patient Care
Clinical question: What are the components of the daily workflow of hospitalists working on a non-housestaff service?
Background: The use of hospitalists is associated with increased efficiency in the hospital setting. However, it is not known how this efficiency is achieved. Prior literature has attempted to address this question, but with increasing demands and patient census, the representativeness of existing data is unclear.
Study design: Observational time-motion study.
Setting: Urban tertiary-care academic medical center.
Synopsis: Twenty-four hospitalists were directly observed for two weekday shifts. An electronic collection tool was developed using initial data on hospitalist activities and piloted prior to formal study data collection. Direct patient care was defined as involving face-to-face interaction between hospitalist and patient, while indirect patient care involved activities relevant to patient care but not performed in the patient’s presence.
Approximately 500 hours of observation were collected. Direct patient care comprised only a mean of 17.4% of the hospitalists’ daily workflow, while more was spent on indirect care, mainly electronic health record (EHR) documentation (mean 34.1%) and communication activities (mean 25.9%). Multitasking occurred 16% of the time, typically during communication or “critical documentation activities” (e.g. writing prescriptions). As patient volume increased, less time was spent in communication, and documentation was deferred to after hours.
These results were consistent with prior observational studies but were limited to a single center and might not represent the workflow of hospitalists in other settings, such as community hospitals, or nocturnists.
Bottom line: Hospitalists on non-housestaff services spend most of their time on indirect patient care and, with increasing patient census, communication is sacrificed. Multitasking is common during periods of communication and critical documentation.
Citation: Tipping MD, Forth VE, O’Leary KJ, et al. Where did the day go?—a time-motion study of hospitalists. J Hosp Med. 2010;5(6):323-328.
Patients Who Leave Against Medical Advice Have Higher Readmission, Mortality Rates
Clinical question: What are the 30-day hospital readmission and mortality rates for Veterans Administration (VA) patients discharged against medical advice (AMA) compared with those appropriately discharged from the hospital?
Background: Patients discharged AMA might be at increased risk of experiencing worse outcomes. Small studies have demonstrated that patients with asthma and acute myocardial infarction (MI) discharged AMA have increased risk of readmission and death. However, it is unclear whether these risks are generalizable to a wider medical population.
Study design: Five-year retrospective cohort study.
Setting: One hundred twenty-nine VA acute-care hospitals.
Synopsis: Of the nearly 2 million patients admitted to the VA from 2004 to 2008, 1.7% were discharged AMA. Patients discharged AMA generally were younger, had lower incomes, and were more likely to be black. Furthermore, patients discharged AMA had statistically significant higher rates of 30-day readmission (17.7% vs. 11%, P<0.001) and higher 30-day mortality rates (0.75% vs. 0.61%, P=0.001) compared with those who had been appropriately discharged. In hazard models, discharge AMA was a significant predictor of 30-day readmission and conferred a nonstatistically significant increase in 30-day mortality.
Because all patients were seen in VA facilities, the results might not be generalizable to other acute-care settings. Although VA patients differ from the general medical population, the characteristics of patients discharged AMA are similar to those in previously published studies. The study utilized administrative data, which are very reliable but limited by little information on clinical factors that could contribute to AMA discharges.
Bottom line: Patients discharged AMA are at increased risk of worse post-hospitalization outcomes, including hospital readmission and death.
Citation: Glasgow JM, Vaughn-Sarrazin M, Kaboli PJ. Leaving against medical advice (AMA): risk of 30-day mortality and hospital readmission. J Gen Intern Med. 2010;25(9): 926-929.
Simple Model Predicts Hospital Readmission
Clinical question: Which patient-level factors can be used in a simple model to predict hospital readmission of medicine patients?
Background: Hospital readmissions are common and costly. Previously published readmission prediction models have had limited utility because they focused on a specific condition, setting, or population, or were too cumbersome for practical use.
Study design: Prospective observational cohort study.
Setting: Six academic medical centers.
Synopsis: Data from nearly 11,000 general medicine patients were included in the analysis. Overall, almost 18% of patients were readmitted within 30 days of discharge.
In the prediction model derived and validated from the data, seven factors were significant predictors of readmission within 30 days of discharge: insurance status, marital status, having a regular healthcare provider, Charlson comorbidity index, SF 12 physical component score, one or more admissions within the last year, and current length of stay greater than two days. Points assigned from each significant predictor were used to create a risk score. The 5% of patients with risk scores of 25 and higher had 30-day readmission rates of approximately 30%, compared to readmission rates of approximately 16% in patients with scores of less than 25.
These results might not be generalizable to small, rural, nonacademic settings. Planned admissions could not be excluded from the data, and readmissions to nonstudy hospitals could not be ascertained. Despite these limitations, this model is easier to use than prior models and relevant to a broad population of patients.
Bottom line: A simple prediction model using patient-level factors can be used to identify patients at higher risk of readmission within 30 days of discharge to home.
Citation: Hasan O, Meltzer DO, Shaykevich SA, et al. Hospital readmission in general medicine patients: a prediction model. J Gen Intern Med. 2010;25(3):211-219.
No Difference in Outcomes Between High- and Non-High-Dose Proton Pump Inhibitors in Bleeding Peptic Ulcers
Clinical question: Do high-dose proton pump inhibitors (PPIs) decrease the rate of rebleeding, surgical intervention, or mortality in patients with bleeding peptic ulcers who have undergone endoscopic treatment?
Background: Previous studies have demonstrated superiority of both high- and low-dose PPIs to H2 receptor antagonists and placebo in reducing rebleeding rates in patients with peptic ulcers. However, no clear evidence is available to suggest that high-dose PPIs are more effective than non-high-dose PPIs for treatment of bleeding peptic ulcers.
Study design: Systematic review and meta-analysis.
Setting: Multicenter and single-site studies conducted in several countries.
Synopsis: Studies were included if they were randomized controlled trials, compared high- versus non-high-dose PPIs, evaluated endoscopically confirmed bleeding ulcers, gave PPIs after endoscopy, and documented outcomes regarding rates of rebleeding, surgical intervention, or mortality. High-dose PPIs were defined as equivalent to omeprazole 80 mg intravenous bolus followed by continuous intravenous infusion at 8 mg/hr for 72 hours.
Seven studies met inclusion criteria. The pooled odds ratios for rebleeding, surgical intervention, and mortality were 1.30 (95% CI, 0.88-1.91), 1.49 (95% CI, 0.66-3.37), and 0.89 (95% CI, 0.37-2.13), respectively, for high-dose versus non-high-dose PPIs. The authors concluded that high-dose PPIs were not superior to non-high-dose PPIs in reducing the rates of these adverse outcomes after endoscopic treatment of bleeding ulcers. Considering the cost of high-dose PPIs, further studies are indicated to help guide PPI dosing for patients with peptic ulcers.
Major limitations of this study were the small number of studies (1,157 patients in total) and their heterogeneity, and the lack of intention-to-treat analysis. The studies also included a high Asian predominance, and it has been shown that Asian populations have an enhanced PPI effect.
Bottom line: High-dose PPIs did not demonstrate reduced rates of ulcer rebleeding, surgical intervention, or mortality compared with non-high-dose PPIs in this meta-analysis, which included a small number of studies and patients.
Citation: Wang CH, Ma MH, Chou HC, et al. High-dose vs. non-high-dose proton pump inhibitors after endoscopic treatment in patients with bleeding peptic ulcer: a systematic review and meta-analysis of randomized controlled trials. Arch Intern Med. 2010;170(9):751-758.
Hospital Utilization by Practicing Generalists Declined before the Emergence of Hospitalists
Clinical question: What has been the pattern of hospital utilization by generalists before and after the emergence of hospitalists?
Background: It has been proposed that the emergence of hospitalists has “crowded out” generalist physicians from the U.S. hospital setting. This study evaluated the trends of inpatient practice by generalists both before and after the emergence of hospitalists.
Study design: Retrospective analysis of national databases.
Setting: U.S. data from 1980 to 2005.
Synopsis: Utilizing the National Hospital Discharge Survey and the American Medical Association’s Physician Characteristics and Distribution in the U.S., information was extracted to evaluate the average number of annual inpatient encounters relative to generalist workforce from 1980 to 2005. Total inpatient encounters for each year were calculated by multiplying the total number of hospital admissions by the average hospital length of stay. The emergence of hospitalists was defined as beginning in 1994.
Total inpatient encounters by generalists declined by 35% in the pre-hospitalist era but remained essentially unchanged in the hospitalist era. During the pre-hospitalist period, the number of generalists doubled, to more than 200,000 from approximately 100,000, while the number of hospital discharges remained relatively stable and the length of stay declined by a third. The decrease in average inpatient encounters in the pre-hospitalist era is thought to have been secondary to decreased length of stay and increased workforce.
Bottom line: Hospital utilization relative to generalist physician workforce was decreasing prior to the emergence of hospitalists mainly due to decreased length of hospital stay and increased numbers of physicians.
Citation: Meltzer DO, Chung JW. U.S. trends in hospitalization and generalist physician workforce and the emergence of hospitalists. J Gen Intern Med. 2010;25(5):453-459.
Fragmentation of Hospitalist Care Is Associated with Increased Length of Stay
Clinical question: Does fragmentation of care (FOC) by hospitalists affect length of stay (LOS)?
Background: Previous investigations have explored the impact of FOC provided by residency programs on LOS and quality of care. Results of these studies have been mixed. However, there have been no prior studies on the impact of the fragmentation of hospitalist care on LOS.
Study design: Concurrent control study.
Setting: Hospitalist practices all over the country managed by IPC: The Hospitalist Company.
Synopsis: Investigators looked at 10,977 patients admitted with diagnoses of pneumonia or heart failure. The primary endpoint was LOS. The independent variable of interest was a measure of FOC. The FOC was calculated as a quantitative index, by determining the percentage of hospitalist care delivered by a physician other than the primary hospitalist.
Multivariable analyses revealed a statistically significant increase in LOS of 0.39 days for each 10% increase in fragmentation level for pneumonia admissions. Similarly, for patients with heart failure, there was a significant increase in LOS of 0.30 days for each 10% increase in fragmentation level.
The study is a concurrent control study, so conclusions cannot be drawn about causality. Additionally, there are likely unmeasured differences between every hospital and hospitalist practice, which could further confound the relationships between hospitalist care and LOS.
Bottom line: Fragmentation of care provided by hospitalists is associated with an increased LOS in patients hospitalized for pneumonia or heart failure.
Citation: Epstein K, Juarez E, Epstein A, Loya K, Singer A. The impact of fragmentation of hospitalist care on length of stay. J Hosp Med. 2010;5(6):335-338.
Admission Medication Errors Are Common and Most Harmful in Older Patients Taking Many Medications
Clinical question: What are the risk factors and potential harm associated with medication errors at hospital admission?
Background: Obtaining a medication history from a hospitalized patient is an error-prone process. Several variables can affect the completeness and quality of medication histories, but existing data are limited regarding patient or medication risk factors associated with medication errors at admission.
Study design: Prospective cohort study.
Setting: Academic hospital in Chicago.
Synopsis: Pharmacist and admitting physician medication histories were compared with admission medication orders to identify any unexplained discrepancies. Discrepancies resulting in order changes were defined as medication errors.
Of the 651 adult medical inpatients studied, 234 (35.9%) had medication order errors identified at admission. Errors originated in the medication histories for 85% of these patients. The most frequent type of error was an omission (48.9%). An age of 65 or older (odds ratio [OR]=2.17, 95% confidence interval [CI], 1.09-4.30) and increased number of medications (OR=1.21, 95% CI, 1.14-1.29) were the only risk factors identified by multivariate analysis to be independently associated with increased risk of medication order errors potentially causing harm or requiring monitoring or intervention. Presenting a medication list upon admission was a significant protective factor (OR=0.35, 95% CI, 0.19-0.63).
Though this is the largest study to date evaluating admission medication errors in hospitalized medical patients, it remains limited by its single hospital site. Because the authors were unable to interview patients who were too ill or unwilling to participate and had no caregiver present, they might have underestimated the number of admission errors. Further, the harm assessment was based on potential and not actual harm.
Bottom line: Admission medication order errors are frequent, most commonly originate in the medication histories, and have increased potential to cause adverse outcomes in older patients and those taking higher numbers of medications.
Citation: Gleason KM, McDaniel MR, Feinglass J, et al. Results of the Medications At Transitions and Clinical Handoffs (MATCH) study: an analysis of medication reconciliation errors and risk factors at hospital admission. J Gen Intern Med. 2010;25(5):441-447.
In This Edition
Literature at a Glance
A guide to this month’s studies
- Continuous insulin infusion in non-ICU patients
- How hospitalists spend their day
- Outcomes of patients leaving against medical advice
- Prediction rule for readmission
- Effects of high- vs. low-dose PPIs for peptic ulcer
- Hospital utilization by generalists before hospitalists
- Effect of hospitalist fragmentation on length of stay
- Medication errors at admissions in older patients
Continuous Insulin Infusion Provides Effective Glycemic Control in Non-ICU Patients
Clinical question: Is continuous insulin infusion (CII) a safe and effective option in the management of hyperglycemia in non-ICU patients?
Background: Hyperglycemia has been associated with worse outcomes in hospitalized patients. Prior research has demonstrated the benefit of CII in managing hyperglycemia in the ICU setting. However, outcomes have not been evaluated in the general medical (non-ICU) setting, where hyperglycemia is often inadequately addressed.
Study design: Retrospective chart review.
Setting: Urban tertiary-care medical center.
Synopsis: Charts of 200 adult patients treated with CII in non-ICU areas were reviewed with the primary outcomes including mean daily blood glucose (BG) levels and number of hyper- and hypoglycemic events occurring on CII. Mean BG dropped from 323 mg/dL to 182 mg/dL by day one, with a BG≤of 150 achieved in 67% of patients by day two of therapy. Twenty-two percent of patients suffered a hypoglycemic event (BG<60), reportedly similar to prior studies of insulin use in ICU and non-ICU settings. Eighty-two percent of patients received some form of nutritional support while on CII. In multivariate analyses, receiving oral nutrition (either a solid or liquid diet) was the only factor associated with increased risk of hyperglycemia and hypoglycemia.
This study was limited by its retrospective analysis in a single center. No comparison was made with basal-bolus or sliding-scale insulin therapy regarding efficacy or safety.
Bottom line: Non-ICU patients with hyperglycemia who received CII were able to achieve effective glycemic control within 48 hours of initiation, with rates of hypoglycemia comparable to those observed in ICU settings.
Citation: Smiley D, Rhee M, Peng L, et al. Safety and efficacy of continuous insulin infusion in noncritical care settings. J Hosp Med. 2010;5(4):212-217.
Hospitalists Spend More Time on Indirect, Rather Than Direct, Patient Care
Clinical question: What are the components of the daily workflow of hospitalists working on a non-housestaff service?
Background: The use of hospitalists is associated with increased efficiency in the hospital setting. However, it is not known how this efficiency is achieved. Prior literature has attempted to address this question, but with increasing demands and patient census, the representativeness of existing data is unclear.
Study design: Observational time-motion study.
Setting: Urban tertiary-care academic medical center.
Synopsis: Twenty-four hospitalists were directly observed for two weekday shifts. An electronic collection tool was developed using initial data on hospitalist activities and piloted prior to formal study data collection. Direct patient care was defined as involving face-to-face interaction between hospitalist and patient, while indirect patient care involved activities relevant to patient care but not performed in the patient’s presence.
Approximately 500 hours of observation were collected. Direct patient care comprised only a mean of 17.4% of the hospitalists’ daily workflow, while more was spent on indirect care, mainly electronic health record (EHR) documentation (mean 34.1%) and communication activities (mean 25.9%). Multitasking occurred 16% of the time, typically during communication or “critical documentation activities” (e.g. writing prescriptions). As patient volume increased, less time was spent in communication, and documentation was deferred to after hours.
These results were consistent with prior observational studies but were limited to a single center and might not represent the workflow of hospitalists in other settings, such as community hospitals, or nocturnists.
Bottom line: Hospitalists on non-housestaff services spend most of their time on indirect patient care and, with increasing patient census, communication is sacrificed. Multitasking is common during periods of communication and critical documentation.
Citation: Tipping MD, Forth VE, O’Leary KJ, et al. Where did the day go?—a time-motion study of hospitalists. J Hosp Med. 2010;5(6):323-328.
Patients Who Leave Against Medical Advice Have Higher Readmission, Mortality Rates
Clinical question: What are the 30-day hospital readmission and mortality rates for Veterans Administration (VA) patients discharged against medical advice (AMA) compared with those appropriately discharged from the hospital?
Background: Patients discharged AMA might be at increased risk of experiencing worse outcomes. Small studies have demonstrated that patients with asthma and acute myocardial infarction (MI) discharged AMA have increased risk of readmission and death. However, it is unclear whether these risks are generalizable to a wider medical population.
Study design: Five-year retrospective cohort study.
Setting: One hundred twenty-nine VA acute-care hospitals.
Synopsis: Of the nearly 2 million patients admitted to the VA from 2004 to 2008, 1.7% were discharged AMA. Patients discharged AMA generally were younger, had lower incomes, and were more likely to be black. Furthermore, patients discharged AMA had statistically significant higher rates of 30-day readmission (17.7% vs. 11%, P<0.001) and higher 30-day mortality rates (0.75% vs. 0.61%, P=0.001) compared with those who had been appropriately discharged. In hazard models, discharge AMA was a significant predictor of 30-day readmission and conferred a nonstatistically significant increase in 30-day mortality.
Because all patients were seen in VA facilities, the results might not be generalizable to other acute-care settings. Although VA patients differ from the general medical population, the characteristics of patients discharged AMA are similar to those in previously published studies. The study utilized administrative data, which are very reliable but limited by little information on clinical factors that could contribute to AMA discharges.
Bottom line: Patients discharged AMA are at increased risk of worse post-hospitalization outcomes, including hospital readmission and death.
Citation: Glasgow JM, Vaughn-Sarrazin M, Kaboli PJ. Leaving against medical advice (AMA): risk of 30-day mortality and hospital readmission. J Gen Intern Med. 2010;25(9): 926-929.
Simple Model Predicts Hospital Readmission
Clinical question: Which patient-level factors can be used in a simple model to predict hospital readmission of medicine patients?
Background: Hospital readmissions are common and costly. Previously published readmission prediction models have had limited utility because they focused on a specific condition, setting, or population, or were too cumbersome for practical use.
Study design: Prospective observational cohort study.
Setting: Six academic medical centers.
Synopsis: Data from nearly 11,000 general medicine patients were included in the analysis. Overall, almost 18% of patients were readmitted within 30 days of discharge.
In the prediction model derived and validated from the data, seven factors were significant predictors of readmission within 30 days of discharge: insurance status, marital status, having a regular healthcare provider, Charlson comorbidity index, SF 12 physical component score, one or more admissions within the last year, and current length of stay greater than two days. Points assigned from each significant predictor were used to create a risk score. The 5% of patients with risk scores of 25 and higher had 30-day readmission rates of approximately 30%, compared to readmission rates of approximately 16% in patients with scores of less than 25.
These results might not be generalizable to small, rural, nonacademic settings. Planned admissions could not be excluded from the data, and readmissions to nonstudy hospitals could not be ascertained. Despite these limitations, this model is easier to use than prior models and relevant to a broad population of patients.
Bottom line: A simple prediction model using patient-level factors can be used to identify patients at higher risk of readmission within 30 days of discharge to home.
Citation: Hasan O, Meltzer DO, Shaykevich SA, et al. Hospital readmission in general medicine patients: a prediction model. J Gen Intern Med. 2010;25(3):211-219.
No Difference in Outcomes Between High- and Non-High-Dose Proton Pump Inhibitors in Bleeding Peptic Ulcers
Clinical question: Do high-dose proton pump inhibitors (PPIs) decrease the rate of rebleeding, surgical intervention, or mortality in patients with bleeding peptic ulcers who have undergone endoscopic treatment?
Background: Previous studies have demonstrated superiority of both high- and low-dose PPIs to H2 receptor antagonists and placebo in reducing rebleeding rates in patients with peptic ulcers. However, no clear evidence is available to suggest that high-dose PPIs are more effective than non-high-dose PPIs for treatment of bleeding peptic ulcers.
Study design: Systematic review and meta-analysis.
Setting: Multicenter and single-site studies conducted in several countries.
Synopsis: Studies were included if they were randomized controlled trials, compared high- versus non-high-dose PPIs, evaluated endoscopically confirmed bleeding ulcers, gave PPIs after endoscopy, and documented outcomes regarding rates of rebleeding, surgical intervention, or mortality. High-dose PPIs were defined as equivalent to omeprazole 80 mg intravenous bolus followed by continuous intravenous infusion at 8 mg/hr for 72 hours.
Seven studies met inclusion criteria. The pooled odds ratios for rebleeding, surgical intervention, and mortality were 1.30 (95% CI, 0.88-1.91), 1.49 (95% CI, 0.66-3.37), and 0.89 (95% CI, 0.37-2.13), respectively, for high-dose versus non-high-dose PPIs. The authors concluded that high-dose PPIs were not superior to non-high-dose PPIs in reducing the rates of these adverse outcomes after endoscopic treatment of bleeding ulcers. Considering the cost of high-dose PPIs, further studies are indicated to help guide PPI dosing for patients with peptic ulcers.
Major limitations of this study were the small number of studies (1,157 patients in total) and their heterogeneity, and the lack of intention-to-treat analysis. The studies also included a high Asian predominance, and it has been shown that Asian populations have an enhanced PPI effect.
Bottom line: High-dose PPIs did not demonstrate reduced rates of ulcer rebleeding, surgical intervention, or mortality compared with non-high-dose PPIs in this meta-analysis, which included a small number of studies and patients.
Citation: Wang CH, Ma MH, Chou HC, et al. High-dose vs. non-high-dose proton pump inhibitors after endoscopic treatment in patients with bleeding peptic ulcer: a systematic review and meta-analysis of randomized controlled trials. Arch Intern Med. 2010;170(9):751-758.
Hospital Utilization by Practicing Generalists Declined before the Emergence of Hospitalists
Clinical question: What has been the pattern of hospital utilization by generalists before and after the emergence of hospitalists?
Background: It has been proposed that the emergence of hospitalists has “crowded out” generalist physicians from the U.S. hospital setting. This study evaluated the trends of inpatient practice by generalists both before and after the emergence of hospitalists.
Study design: Retrospective analysis of national databases.
Setting: U.S. data from 1980 to 2005.
Synopsis: Utilizing the National Hospital Discharge Survey and the American Medical Association’s Physician Characteristics and Distribution in the U.S., information was extracted to evaluate the average number of annual inpatient encounters relative to generalist workforce from 1980 to 2005. Total inpatient encounters for each year were calculated by multiplying the total number of hospital admissions by the average hospital length of stay. The emergence of hospitalists was defined as beginning in 1994.
Total inpatient encounters by generalists declined by 35% in the pre-hospitalist era but remained essentially unchanged in the hospitalist era. During the pre-hospitalist period, the number of generalists doubled, to more than 200,000 from approximately 100,000, while the number of hospital discharges remained relatively stable and the length of stay declined by a third. The decrease in average inpatient encounters in the pre-hospitalist era is thought to have been secondary to decreased length of stay and increased workforce.
Bottom line: Hospital utilization relative to generalist physician workforce was decreasing prior to the emergence of hospitalists mainly due to decreased length of hospital stay and increased numbers of physicians.
Citation: Meltzer DO, Chung JW. U.S. trends in hospitalization and generalist physician workforce and the emergence of hospitalists. J Gen Intern Med. 2010;25(5):453-459.
Fragmentation of Hospitalist Care Is Associated with Increased Length of Stay
Clinical question: Does fragmentation of care (FOC) by hospitalists affect length of stay (LOS)?
Background: Previous investigations have explored the impact of FOC provided by residency programs on LOS and quality of care. Results of these studies have been mixed. However, there have been no prior studies on the impact of the fragmentation of hospitalist care on LOS.
Study design: Concurrent control study.
Setting: Hospitalist practices all over the country managed by IPC: The Hospitalist Company.
Synopsis: Investigators looked at 10,977 patients admitted with diagnoses of pneumonia or heart failure. The primary endpoint was LOS. The independent variable of interest was a measure of FOC. The FOC was calculated as a quantitative index, by determining the percentage of hospitalist care delivered by a physician other than the primary hospitalist.
Multivariable analyses revealed a statistically significant increase in LOS of 0.39 days for each 10% increase in fragmentation level for pneumonia admissions. Similarly, for patients with heart failure, there was a significant increase in LOS of 0.30 days for each 10% increase in fragmentation level.
The study is a concurrent control study, so conclusions cannot be drawn about causality. Additionally, there are likely unmeasured differences between every hospital and hospitalist practice, which could further confound the relationships between hospitalist care and LOS.
Bottom line: Fragmentation of care provided by hospitalists is associated with an increased LOS in patients hospitalized for pneumonia or heart failure.
Citation: Epstein K, Juarez E, Epstein A, Loya K, Singer A. The impact of fragmentation of hospitalist care on length of stay. J Hosp Med. 2010;5(6):335-338.
Admission Medication Errors Are Common and Most Harmful in Older Patients Taking Many Medications
Clinical question: What are the risk factors and potential harm associated with medication errors at hospital admission?
Background: Obtaining a medication history from a hospitalized patient is an error-prone process. Several variables can affect the completeness and quality of medication histories, but existing data are limited regarding patient or medication risk factors associated with medication errors at admission.
Study design: Prospective cohort study.
Setting: Academic hospital in Chicago.
Synopsis: Pharmacist and admitting physician medication histories were compared with admission medication orders to identify any unexplained discrepancies. Discrepancies resulting in order changes were defined as medication errors.
Of the 651 adult medical inpatients studied, 234 (35.9%) had medication order errors identified at admission. Errors originated in the medication histories for 85% of these patients. The most frequent type of error was an omission (48.9%). An age of 65 or older (odds ratio [OR]=2.17, 95% confidence interval [CI], 1.09-4.30) and increased number of medications (OR=1.21, 95% CI, 1.14-1.29) were the only risk factors identified by multivariate analysis to be independently associated with increased risk of medication order errors potentially causing harm or requiring monitoring or intervention. Presenting a medication list upon admission was a significant protective factor (OR=0.35, 95% CI, 0.19-0.63).
Though this is the largest study to date evaluating admission medication errors in hospitalized medical patients, it remains limited by its single hospital site. Because the authors were unable to interview patients who were too ill or unwilling to participate and had no caregiver present, they might have underestimated the number of admission errors. Further, the harm assessment was based on potential and not actual harm.
Bottom line: Admission medication order errors are frequent, most commonly originate in the medication histories, and have increased potential to cause adverse outcomes in older patients and those taking higher numbers of medications.
Citation: Gleason KM, McDaniel MR, Feinglass J, et al. Results of the Medications At Transitions and Clinical Handoffs (MATCH) study: an analysis of medication reconciliation errors and risk factors at hospital admission. J Gen Intern Med. 2010;25(5):441-447.