User login
Karen Appold is a seasoned writer and editor, with more than 20 years of editorial experience and started Write Now Services in 2003. Her scope of work includes writing, editing, and proofreading scholarly peer-reviewed journal content, consumer articles, white papers, and company reports for a variety of medical organizations, businesses, and media. Karen, who holds a BA in English from Penn State University, resides in Lehigh Valley, Pa.
Ready for post-acute care?
The definition of “hospitalist,” according to the SHM website, is a clinician “dedicated to delivering comprehensive medical care to hospitalized patients.” For years, the hospital setting was the specialties’ identifier. But as hospitalists’ scope has expanded, and post-acute care (PAC) in the United States has grown, more hospitalists are extending their roles into this space.
PAC today is more than the traditional nursing home, according to Manoj K. Mathew, MD, SFHM, national medical director of Agilon Health in Los Angeles.
Many of those expanded settings Dr. Mathew describes emerged as a result of the Affordable Care Act. Since its enactment in 2010, the ACA has heightened providers’ focus on the “Triple Aim” of improving the patient experience (including quality and satisfaction), improving the health of populations, and reducing the per capita cost of healthcare.1 Vishal Kuchaculla, MD, New England regional post-acute medical director of Knoxville,Tenn.-based TeamHealth, says new service lines also developed as Medicare clamped down on long-term inpatient hospital stays by giving financial impetus to discharge patients as soon as possible.
“Over the last few years, there’s been a major shift from fee-for-service to risk-based payment models,” Dr. Kuchaculla says. “The government’s financial incentives are driving outcomes to improve performance initiatives.”
“Today, LTACHs can be used as substitutes for short-term acute care,” says Sean R. Muldoon, MD, MPH, FCCP, chief medical officer of Kindred Healthcare in Louisville, Ky., and former chair of SHM’s Post-Acute Care Committee. “This means that a patient can be directly admitted from their home to an LTACH. In fact, many hospice and home-care patients are referred from physicians’ offices without a preceding hospitalization.”

Hospitalists can fill a need

More hospitalists are working in PACs for a number of reasons. Dr. Mathew says PAC facilities and services have “typically lacked the clinical structure and processes to obtain the results that patients and payors expect.
“These deficits needed to be quickly remedied as patients discharged from hospitals have increased acuity and higher disease burdens,” he adds. “Hospitalists were the natural choice to fill roles requiring their expertise and experience.”
Dr. Muldoon considers the expanded scope of practice into PACs an additional layer to hospital medicine’s value proposition to the healthcare system.
“As experts in the management of inpatient populations, it’s natural for hospitalists to expand to other facilities with inpatient-like populations,” he says, noting SNFs are the most popular choice, with IRFs and LTACHs also being common places to work. Few hospitalists work in home care or hospice.
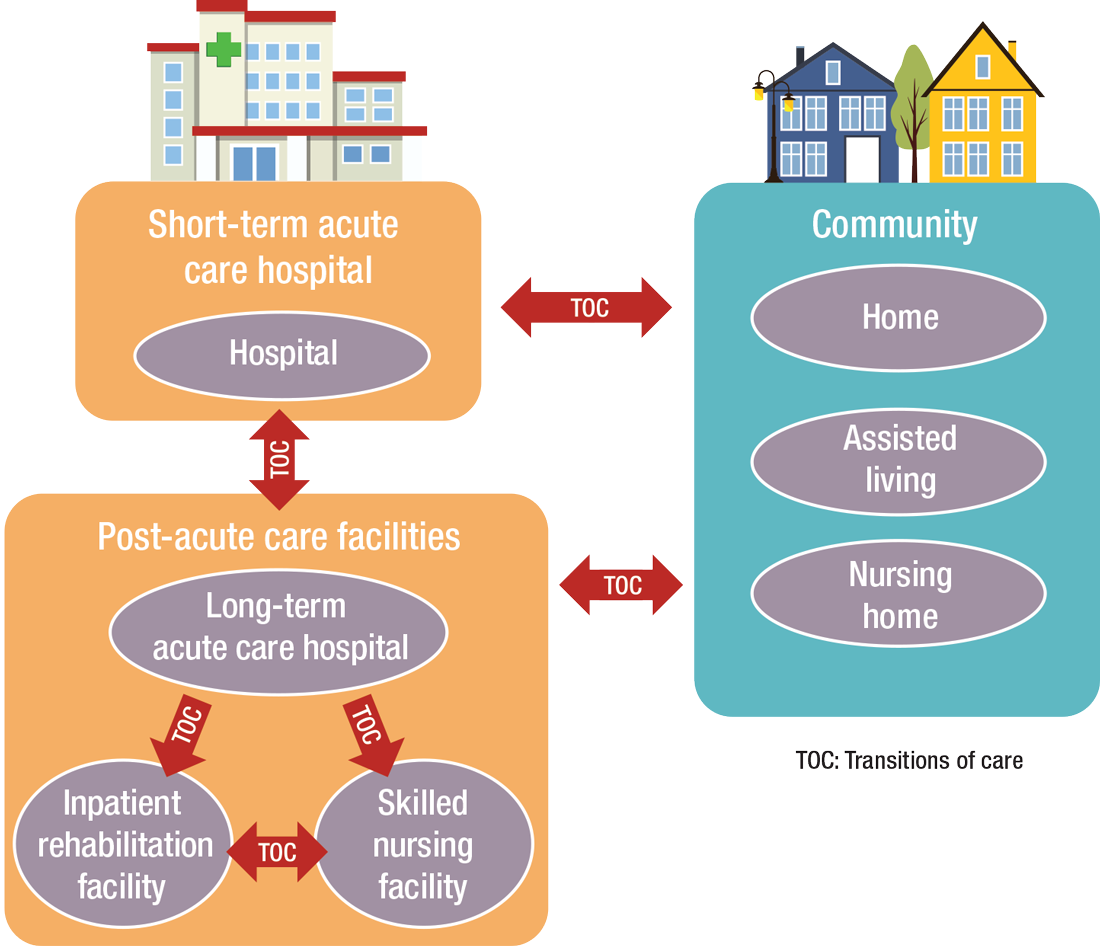
PAC settings are designed to help patients who are transitioning from an inpatient setting back to their home or other setting.
“Many patients go home after a SNF stay, while others will move to a nursing home or other longer-term care setting for the first time,” says Tiffany Radcliff, PhD, a health economist in the department of health policy and management at Texas A&M University School of Public Health in College Station. “With this in mind, hospitalists working in PAC have the opportunity to address each patient’s ongoing care needs and prepare them for their next setting. Hospitalists can manage medication or other care regimen changes that resulted from an inpatient stay, reinforce discharge instructions to the patient and their caregivers, and identify any other issues with continuing care that need to be addressed before discharge to the next care setting.”
Transitioning Care
Even if a hospitalist is not employed at a PAC, it’s important that they know something about them.
“As patients are moved downstream earlier, hospitalists are being asked to help make a judgment regarding when and where an inpatient is transitioned,” Dr. Muldoon says. As organizations move toward becoming fully risk capable, it is necessary to develop referral networks of high-quality PAC providers to achieve the best clinical outcomes, reduce readmissions, and lower costs.2“Therefore, hospitalists should have a working knowledge of the different sites of service as well as some opinion on the suitability of available options in their community,” Dr. Muldoon says. “The hospitalist can also help to educate the hospitalized patient on what to expect at a PAC.”
If a patient is inappropriately prepared for the PAC setting, it could lead to incomplete management of their condition, which ultimately could lead to readmission.
“When hospitalists know how care is provided in a PAC setting, they are better able to ensure a smoother transition of care between settings,” says Tochi Iroku-Malize, MD, MPH, MBA, FAAFP, SFHM, chair of family medicine at Northwell Health in Long Island, N.Y. “This will ultimately prevent unnecessary readmissions.”
Further, the quality metrics that hospitals and thereby hospitalists are judged by no longer end at the hospital’s exit.
“The ownership of acute-care outcomes requires extending the accountability to outside of the institution’s four walls,” Dr. Mathew says. “The inpatient team needs to place great importance on the transition of care and the subsequent quality of that care when the patient is discharged.”
Robert W. Harrington Jr., MD, SFHM, chief medical officer of Plano, Texas–based Reliant Post-Acute Care Solutions and former SHM president, says the health system landscapes are pushing HM beyond the hospitals’ walls.
How PAC settings differ from hospitals
Practicing in PAC has some important nuances that hospitalists from short-term acute care need to get accustomed to, Dr. Muldoon says. Primarily, the diagnostic capabilities are much more limited, as is the presence of high-level staffing. Further, patients are less resilient to medication changes and interventions, so changes need to be done gradually.
“Hospitalists who try to practice acute-care medicine in a PAC setting may become frustrated by the length of time it takes to do a work-up, get a consultation, and respond to a patient’s change of condition,” Dr. Muldoon says. “Nonetheless, hospitalists can overcome this once recognizing this mind shift.”
According to Dr. Harrington, another challenge hospitalists may face is the inability of the hospital’s and PAC facility’s IT platforms to exchange electronic information.
“The major vendors on both sides need to figure out an interoperability strategy,” he says. “Currently, it often takes 1-3 days to receive a new patient’s discharge summary. The summary may consist of a stack of paper that takes significant time to sort through and requires the PAC facility to perform duplicate data entry. It’s a very highly inefficient process that opens up the doors to mistakes and errors of omission and commission that can result in bad patient outcomes.”
Arif Nazir, MD, CMD, FACP, AGSF, chief medical officer of Signature HealthCARE and president of SHC Medical Partners, both in Louisville, Ky., cites additional reasons the lack of seamless communication between a hospital and PAC facility is problematic. “I see physicians order laboratory tests and investigations that were already done in the hospital because they didn’t know they were already performed or never received the results,” he says. “Similarly, I see patients continue to take medications prescribed in the hospital long term even though they were only supposed to take them short term. I’ve also seen patients come to a PAC setting from a hospital without any formal understanding of their rehabilitative period and expectations for recovery.”
What’s ahead?
Looking to the future, Surafel Tsega, MD, clinical instructor at Mount Sinai Hospital in New York, says he thinks there will be a move toward greater collaboration among inpatient and PAC facilities, particularly in the discharge process, given that hospitals have an added incentive to ensure safe transitions because reimbursement from the Centers for Medicare & Medicaid Services is tied to readmissions and there are penalties for readmission. This involves more comprehensive planning regarding “warm handoffs” (e.g., real-time discussions with PAC providers about a patient’s hospital course and plan of care upon discharge), transferring of information, and so forth.
And while it can still be challenging to identify high-risk patients or determine the intensity and duration of their care, Dr. Mathew says risk-stratification tools and care pathways are continually being refined to maximize value with the limited resources available. In addition, with an increased emphasis on employing a team approach to care, there will be better integration of non-medical services to address the social determinants of health, which play significant roles in overall health and healing.
“Working with community-based organizations for this purpose will be a valuable tool for any of the population health–based initiatives,” he says.
Dr. Muldoon says he believes healthcare reform will increasingly view an inpatient admission as something to be avoided.
“If hospitalization can’t be avoided, then it should be shortened as much as possible,” he says. “This will shift inpatient care into LTACHs, SNFs, and IRFs. Hospitalists would be wise to follow patients into those settings as traditional inpatient census is reduced. This will take a few years, so hospitalists should start now in preparing for that downstream transition of individuals who were previously inpatients.”
The cost of care, and other PAC facts and figures
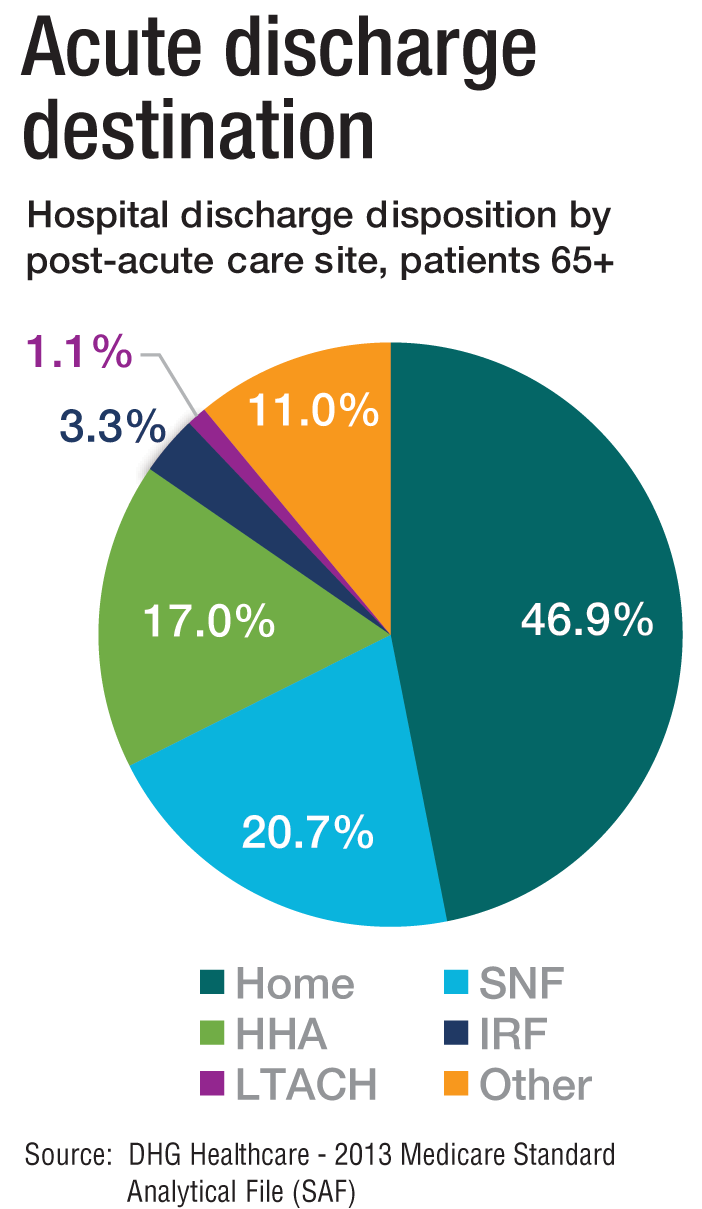
The amount of money that Medicare spends on post-acute care (PAC) has been increasing. In 2012, 12.6% of Medicare beneficiaries used some form of PAC, costing $62 billion.2 That amounts to the Centers for Medicare & Medicaid Services spending close to 25% of Medicare beneficiary expenses on PAC, a 133% increase from 2001 to 2012. Among the different types, $30.4 billion was spent on skilled nursing facilities (SNFs), $18.6 billion on home health, and $13.1 billion on long-term acute care (LTAC) and acute-care rehabilitation.2
It’s also been reported that after short-term acute-care hospitalization, about one in five Medicare beneficiaries requires continued specialized treatment in one of the three typical Medicare PAC settings: inpatient rehabilitation facilities (IRFs), LTAC hospitals, and SNFs.3
What’s more, hospital readmission nearly doubles the cost of an episode, so the financial implications for organizations operating in risk-bearing arrangements are significant. In 2013, 2,213 hospitals were charged $280 million in readmission penalties.2
References
1. The role of post-acute care in new care delivery models. American Hospital Association website. Available at: http://www.aha.org/research/reports/tw/15dec-tw-postacute.pdf. Accessed Nov. 7, 2016.
2. Post-acute care integration: Today and in the future. DHG Healthcare website. Available at: http://www2.dhgllp.com/res_pubs/HCG-Post-Acute-Care-Integration.pdf. Accessed Nov. 7, 2016.
3. Overview: Post-acute care transitions toolkit. Society for Hospital Medicine website. Available at: http://www.hospitalmedicine.org/Web/Quality___Innovation/Implementation_Toolkit/pact/Overview_PACT.aspx?hkey=dea3da3c-8620-46db-a00f-89f07f021958. Accessed Nov. 10, 2016.
The definition of “hospitalist,” according to the SHM website, is a clinician “dedicated to delivering comprehensive medical care to hospitalized patients.” For years, the hospital setting was the specialties’ identifier. But as hospitalists’ scope has expanded, and post-acute care (PAC) in the United States has grown, more hospitalists are extending their roles into this space.
PAC today is more than the traditional nursing home, according to Manoj K. Mathew, MD, SFHM, national medical director of Agilon Health in Los Angeles.
Many of those expanded settings Dr. Mathew describes emerged as a result of the Affordable Care Act. Since its enactment in 2010, the ACA has heightened providers’ focus on the “Triple Aim” of improving the patient experience (including quality and satisfaction), improving the health of populations, and reducing the per capita cost of healthcare.1 Vishal Kuchaculla, MD, New England regional post-acute medical director of Knoxville,Tenn.-based TeamHealth, says new service lines also developed as Medicare clamped down on long-term inpatient hospital stays by giving financial impetus to discharge patients as soon as possible.
“Over the last few years, there’s been a major shift from fee-for-service to risk-based payment models,” Dr. Kuchaculla says. “The government’s financial incentives are driving outcomes to improve performance initiatives.”
“Today, LTACHs can be used as substitutes for short-term acute care,” says Sean R. Muldoon, MD, MPH, FCCP, chief medical officer of Kindred Healthcare in Louisville, Ky., and former chair of SHM’s Post-Acute Care Committee. “This means that a patient can be directly admitted from their home to an LTACH. In fact, many hospice and home-care patients are referred from physicians’ offices without a preceding hospitalization.”

Hospitalists can fill a need

More hospitalists are working in PACs for a number of reasons. Dr. Mathew says PAC facilities and services have “typically lacked the clinical structure and processes to obtain the results that patients and payors expect.
“These deficits needed to be quickly remedied as patients discharged from hospitals have increased acuity and higher disease burdens,” he adds. “Hospitalists were the natural choice to fill roles requiring their expertise and experience.”
Dr. Muldoon considers the expanded scope of practice into PACs an additional layer to hospital medicine’s value proposition to the healthcare system.
“As experts in the management of inpatient populations, it’s natural for hospitalists to expand to other facilities with inpatient-like populations,” he says, noting SNFs are the most popular choice, with IRFs and LTACHs also being common places to work. Few hospitalists work in home care or hospice.
PAC settings are designed to help patients who are transitioning from an inpatient setting back to their home or other setting.
“Many patients go home after a SNF stay, while others will move to a nursing home or other longer-term care setting for the first time,” says Tiffany Radcliff, PhD, a health economist in the department of health policy and management at Texas A&M University School of Public Health in College Station. “With this in mind, hospitalists working in PAC have the opportunity to address each patient’s ongoing care needs and prepare them for their next setting. Hospitalists can manage medication or other care regimen changes that resulted from an inpatient stay, reinforce discharge instructions to the patient and their caregivers, and identify any other issues with continuing care that need to be addressed before discharge to the next care setting.”
Transitioning Care
Even if a hospitalist is not employed at a PAC, it’s important that they know something about them.
“As patients are moved downstream earlier, hospitalists are being asked to help make a judgment regarding when and where an inpatient is transitioned,” Dr. Muldoon says. As organizations move toward becoming fully risk capable, it is necessary to develop referral networks of high-quality PAC providers to achieve the best clinical outcomes, reduce readmissions, and lower costs.2“Therefore, hospitalists should have a working knowledge of the different sites of service as well as some opinion on the suitability of available options in their community,” Dr. Muldoon says. “The hospitalist can also help to educate the hospitalized patient on what to expect at a PAC.”
If a patient is inappropriately prepared for the PAC setting, it could lead to incomplete management of their condition, which ultimately could lead to readmission.
“When hospitalists know how care is provided in a PAC setting, they are better able to ensure a smoother transition of care between settings,” says Tochi Iroku-Malize, MD, MPH, MBA, FAAFP, SFHM, chair of family medicine at Northwell Health in Long Island, N.Y. “This will ultimately prevent unnecessary readmissions.”
Further, the quality metrics that hospitals and thereby hospitalists are judged by no longer end at the hospital’s exit.
“The ownership of acute-care outcomes requires extending the accountability to outside of the institution’s four walls,” Dr. Mathew says. “The inpatient team needs to place great importance on the transition of care and the subsequent quality of that care when the patient is discharged.”
Robert W. Harrington Jr., MD, SFHM, chief medical officer of Plano, Texas–based Reliant Post-Acute Care Solutions and former SHM president, says the health system landscapes are pushing HM beyond the hospitals’ walls.
How PAC settings differ from hospitals
Practicing in PAC has some important nuances that hospitalists from short-term acute care need to get accustomed to, Dr. Muldoon says. Primarily, the diagnostic capabilities are much more limited, as is the presence of high-level staffing. Further, patients are less resilient to medication changes and interventions, so changes need to be done gradually.
“Hospitalists who try to practice acute-care medicine in a PAC setting may become frustrated by the length of time it takes to do a work-up, get a consultation, and respond to a patient’s change of condition,” Dr. Muldoon says. “Nonetheless, hospitalists can overcome this once recognizing this mind shift.”
According to Dr. Harrington, another challenge hospitalists may face is the inability of the hospital’s and PAC facility’s IT platforms to exchange electronic information.
“The major vendors on both sides need to figure out an interoperability strategy,” he says. “Currently, it often takes 1-3 days to receive a new patient’s discharge summary. The summary may consist of a stack of paper that takes significant time to sort through and requires the PAC facility to perform duplicate data entry. It’s a very highly inefficient process that opens up the doors to mistakes and errors of omission and commission that can result in bad patient outcomes.”
Arif Nazir, MD, CMD, FACP, AGSF, chief medical officer of Signature HealthCARE and president of SHC Medical Partners, both in Louisville, Ky., cites additional reasons the lack of seamless communication between a hospital and PAC facility is problematic. “I see physicians order laboratory tests and investigations that were already done in the hospital because they didn’t know they were already performed or never received the results,” he says. “Similarly, I see patients continue to take medications prescribed in the hospital long term even though they were only supposed to take them short term. I’ve also seen patients come to a PAC setting from a hospital without any formal understanding of their rehabilitative period and expectations for recovery.”
What’s ahead?
Looking to the future, Surafel Tsega, MD, clinical instructor at Mount Sinai Hospital in New York, says he thinks there will be a move toward greater collaboration among inpatient and PAC facilities, particularly in the discharge process, given that hospitals have an added incentive to ensure safe transitions because reimbursement from the Centers for Medicare & Medicaid Services is tied to readmissions and there are penalties for readmission. This involves more comprehensive planning regarding “warm handoffs” (e.g., real-time discussions with PAC providers about a patient’s hospital course and plan of care upon discharge), transferring of information, and so forth.
And while it can still be challenging to identify high-risk patients or determine the intensity and duration of their care, Dr. Mathew says risk-stratification tools and care pathways are continually being refined to maximize value with the limited resources available. In addition, with an increased emphasis on employing a team approach to care, there will be better integration of non-medical services to address the social determinants of health, which play significant roles in overall health and healing.
“Working with community-based organizations for this purpose will be a valuable tool for any of the population health–based initiatives,” he says.
Dr. Muldoon says he believes healthcare reform will increasingly view an inpatient admission as something to be avoided.
“If hospitalization can’t be avoided, then it should be shortened as much as possible,” he says. “This will shift inpatient care into LTACHs, SNFs, and IRFs. Hospitalists would be wise to follow patients into those settings as traditional inpatient census is reduced. This will take a few years, so hospitalists should start now in preparing for that downstream transition of individuals who were previously inpatients.”
The cost of care, and other PAC facts and figures
The amount of money that Medicare spends on post-acute care (PAC) has been increasing. In 2012, 12.6% of Medicare beneficiaries used some form of PAC, costing $62 billion.2 That amounts to the Centers for Medicare & Medicaid Services spending close to 25% of Medicare beneficiary expenses on PAC, a 133% increase from 2001 to 2012. Among the different types, $30.4 billion was spent on skilled nursing facilities (SNFs), $18.6 billion on home health, and $13.1 billion on long-term acute care (LTAC) and acute-care rehabilitation.2
It’s also been reported that after short-term acute-care hospitalization, about one in five Medicare beneficiaries requires continued specialized treatment in one of the three typical Medicare PAC settings: inpatient rehabilitation facilities (IRFs), LTAC hospitals, and SNFs.3
What’s more, hospital readmission nearly doubles the cost of an episode, so the financial implications for organizations operating in risk-bearing arrangements are significant. In 2013, 2,213 hospitals were charged $280 million in readmission penalties.2
References
1. The role of post-acute care in new care delivery models. American Hospital Association website. Available at: http://www.aha.org/research/reports/tw/15dec-tw-postacute.pdf. Accessed Nov. 7, 2016.
2. Post-acute care integration: Today and in the future. DHG Healthcare website. Available at: http://www2.dhgllp.com/res_pubs/HCG-Post-Acute-Care-Integration.pdf. Accessed Nov. 7, 2016.
3. Overview: Post-acute care transitions toolkit. Society for Hospital Medicine website. Available at: http://www.hospitalmedicine.org/Web/Quality___Innovation/Implementation_Toolkit/pact/Overview_PACT.aspx?hkey=dea3da3c-8620-46db-a00f-89f07f021958. Accessed Nov. 10, 2016.
The definition of “hospitalist,” according to the SHM website, is a clinician “dedicated to delivering comprehensive medical care to hospitalized patients.” For years, the hospital setting was the specialties’ identifier. But as hospitalists’ scope has expanded, and post-acute care (PAC) in the United States has grown, more hospitalists are extending their roles into this space.
PAC today is more than the traditional nursing home, according to Manoj K. Mathew, MD, SFHM, national medical director of Agilon Health in Los Angeles.
Many of those expanded settings Dr. Mathew describes emerged as a result of the Affordable Care Act. Since its enactment in 2010, the ACA has heightened providers’ focus on the “Triple Aim” of improving the patient experience (including quality and satisfaction), improving the health of populations, and reducing the per capita cost of healthcare.1 Vishal Kuchaculla, MD, New England regional post-acute medical director of Knoxville,Tenn.-based TeamHealth, says new service lines also developed as Medicare clamped down on long-term inpatient hospital stays by giving financial impetus to discharge patients as soon as possible.
“Over the last few years, there’s been a major shift from fee-for-service to risk-based payment models,” Dr. Kuchaculla says. “The government’s financial incentives are driving outcomes to improve performance initiatives.”
“Today, LTACHs can be used as substitutes for short-term acute care,” says Sean R. Muldoon, MD, MPH, FCCP, chief medical officer of Kindred Healthcare in Louisville, Ky., and former chair of SHM’s Post-Acute Care Committee. “This means that a patient can be directly admitted from their home to an LTACH. In fact, many hospice and home-care patients are referred from physicians’ offices without a preceding hospitalization.”

Hospitalists can fill a need

More hospitalists are working in PACs for a number of reasons. Dr. Mathew says PAC facilities and services have “typically lacked the clinical structure and processes to obtain the results that patients and payors expect.
“These deficits needed to be quickly remedied as patients discharged from hospitals have increased acuity and higher disease burdens,” he adds. “Hospitalists were the natural choice to fill roles requiring their expertise and experience.”
Dr. Muldoon considers the expanded scope of practice into PACs an additional layer to hospital medicine’s value proposition to the healthcare system.
“As experts in the management of inpatient populations, it’s natural for hospitalists to expand to other facilities with inpatient-like populations,” he says, noting SNFs are the most popular choice, with IRFs and LTACHs also being common places to work. Few hospitalists work in home care or hospice.
PAC settings are designed to help patients who are transitioning from an inpatient setting back to their home or other setting.
“Many patients go home after a SNF stay, while others will move to a nursing home or other longer-term care setting for the first time,” says Tiffany Radcliff, PhD, a health economist in the department of health policy and management at Texas A&M University School of Public Health in College Station. “With this in mind, hospitalists working in PAC have the opportunity to address each patient’s ongoing care needs and prepare them for their next setting. Hospitalists can manage medication or other care regimen changes that resulted from an inpatient stay, reinforce discharge instructions to the patient and their caregivers, and identify any other issues with continuing care that need to be addressed before discharge to the next care setting.”
Transitioning Care
Even if a hospitalist is not employed at a PAC, it’s important that they know something about them.
“As patients are moved downstream earlier, hospitalists are being asked to help make a judgment regarding when and where an inpatient is transitioned,” Dr. Muldoon says. As organizations move toward becoming fully risk capable, it is necessary to develop referral networks of high-quality PAC providers to achieve the best clinical outcomes, reduce readmissions, and lower costs.2“Therefore, hospitalists should have a working knowledge of the different sites of service as well as some opinion on the suitability of available options in their community,” Dr. Muldoon says. “The hospitalist can also help to educate the hospitalized patient on what to expect at a PAC.”
If a patient is inappropriately prepared for the PAC setting, it could lead to incomplete management of their condition, which ultimately could lead to readmission.
“When hospitalists know how care is provided in a PAC setting, they are better able to ensure a smoother transition of care between settings,” says Tochi Iroku-Malize, MD, MPH, MBA, FAAFP, SFHM, chair of family medicine at Northwell Health in Long Island, N.Y. “This will ultimately prevent unnecessary readmissions.”
Further, the quality metrics that hospitals and thereby hospitalists are judged by no longer end at the hospital’s exit.
“The ownership of acute-care outcomes requires extending the accountability to outside of the institution’s four walls,” Dr. Mathew says. “The inpatient team needs to place great importance on the transition of care and the subsequent quality of that care when the patient is discharged.”
Robert W. Harrington Jr., MD, SFHM, chief medical officer of Plano, Texas–based Reliant Post-Acute Care Solutions and former SHM president, says the health system landscapes are pushing HM beyond the hospitals’ walls.
How PAC settings differ from hospitals
Practicing in PAC has some important nuances that hospitalists from short-term acute care need to get accustomed to, Dr. Muldoon says. Primarily, the diagnostic capabilities are much more limited, as is the presence of high-level staffing. Further, patients are less resilient to medication changes and interventions, so changes need to be done gradually.
“Hospitalists who try to practice acute-care medicine in a PAC setting may become frustrated by the length of time it takes to do a work-up, get a consultation, and respond to a patient’s change of condition,” Dr. Muldoon says. “Nonetheless, hospitalists can overcome this once recognizing this mind shift.”
According to Dr. Harrington, another challenge hospitalists may face is the inability of the hospital’s and PAC facility’s IT platforms to exchange electronic information.
“The major vendors on both sides need to figure out an interoperability strategy,” he says. “Currently, it often takes 1-3 days to receive a new patient’s discharge summary. The summary may consist of a stack of paper that takes significant time to sort through and requires the PAC facility to perform duplicate data entry. It’s a very highly inefficient process that opens up the doors to mistakes and errors of omission and commission that can result in bad patient outcomes.”
Arif Nazir, MD, CMD, FACP, AGSF, chief medical officer of Signature HealthCARE and president of SHC Medical Partners, both in Louisville, Ky., cites additional reasons the lack of seamless communication between a hospital and PAC facility is problematic. “I see physicians order laboratory tests and investigations that were already done in the hospital because they didn’t know they were already performed or never received the results,” he says. “Similarly, I see patients continue to take medications prescribed in the hospital long term even though they were only supposed to take them short term. I’ve also seen patients come to a PAC setting from a hospital without any formal understanding of their rehabilitative period and expectations for recovery.”
What’s ahead?
Looking to the future, Surafel Tsega, MD, clinical instructor at Mount Sinai Hospital in New York, says he thinks there will be a move toward greater collaboration among inpatient and PAC facilities, particularly in the discharge process, given that hospitals have an added incentive to ensure safe transitions because reimbursement from the Centers for Medicare & Medicaid Services is tied to readmissions and there are penalties for readmission. This involves more comprehensive planning regarding “warm handoffs” (e.g., real-time discussions with PAC providers about a patient’s hospital course and plan of care upon discharge), transferring of information, and so forth.
And while it can still be challenging to identify high-risk patients or determine the intensity and duration of their care, Dr. Mathew says risk-stratification tools and care pathways are continually being refined to maximize value with the limited resources available. In addition, with an increased emphasis on employing a team approach to care, there will be better integration of non-medical services to address the social determinants of health, which play significant roles in overall health and healing.
“Working with community-based organizations for this purpose will be a valuable tool for any of the population health–based initiatives,” he says.
Dr. Muldoon says he believes healthcare reform will increasingly view an inpatient admission as something to be avoided.
“If hospitalization can’t be avoided, then it should be shortened as much as possible,” he says. “This will shift inpatient care into LTACHs, SNFs, and IRFs. Hospitalists would be wise to follow patients into those settings as traditional inpatient census is reduced. This will take a few years, so hospitalists should start now in preparing for that downstream transition of individuals who were previously inpatients.”
The cost of care, and other PAC facts and figures
The amount of money that Medicare spends on post-acute care (PAC) has been increasing. In 2012, 12.6% of Medicare beneficiaries used some form of PAC, costing $62 billion.2 That amounts to the Centers for Medicare & Medicaid Services spending close to 25% of Medicare beneficiary expenses on PAC, a 133% increase from 2001 to 2012. Among the different types, $30.4 billion was spent on skilled nursing facilities (SNFs), $18.6 billion on home health, and $13.1 billion on long-term acute care (LTAC) and acute-care rehabilitation.2
It’s also been reported that after short-term acute-care hospitalization, about one in five Medicare beneficiaries requires continued specialized treatment in one of the three typical Medicare PAC settings: inpatient rehabilitation facilities (IRFs), LTAC hospitals, and SNFs.3
What’s more, hospital readmission nearly doubles the cost of an episode, so the financial implications for organizations operating in risk-bearing arrangements are significant. In 2013, 2,213 hospitals were charged $280 million in readmission penalties.2
References
1. The role of post-acute care in new care delivery models. American Hospital Association website. Available at: http://www.aha.org/research/reports/tw/15dec-tw-postacute.pdf. Accessed Nov. 7, 2016.
2. Post-acute care integration: Today and in the future. DHG Healthcare website. Available at: http://www2.dhgllp.com/res_pubs/HCG-Post-Acute-Care-Integration.pdf. Accessed Nov. 7, 2016.
3. Overview: Post-acute care transitions toolkit. Society for Hospital Medicine website. Available at: http://www.hospitalmedicine.org/Web/Quality___Innovation/Implementation_Toolkit/pact/Overview_PACT.aspx?hkey=dea3da3c-8620-46db-a00f-89f07f021958. Accessed Nov. 10, 2016.
Hot-off-the-press insights on heart failure
Hospitalists frequently encounter patients with heart failure – a complex, clinical syndrome, which has high prevalence, mortality, hospitalization rates, and health care costs.
The HM20 Virtual session “Updates in Heart Failure” will provide literature updates for all types of heart failure patient scenarios – patients with acute and chronic heart failure, those who are hospitalized with heart failure, and patients with heart failure with reduced ejection fraction (HFrEF) and heart failure with preserved ejection fraction (HFpEF). The popular session with questions and answers will be held on Aug. 25.
Presenter Dustin Smith, MD, SFHM, associate professor of medicine in the department of medicine at Emory University, Atlanta, and section chief for education in medical specialty at the Atlanta Veterans Affairs Medical Center, will discuss recent trends, diagnostics, therapeutics, and prognostics for heart failure. He’ll also provide a summary of recent changes to clinical practice guidelines.
“The significance of staying knowledgeable and updated regarding this common admission diagnosis cannot be overstated,” Dr. Smith said. Attendees of this clinical update should learn important practices from new evidence in literature, including an unearthed risk grade predictor of acute heart failure mortality, a diagnostic tool for HFpEF in euvolemic patients with unexplained dyspnea, an examination of the potassium “repletion reflex” in patients hospitalized with heart failure, dietary patterns associated with incident heart failure, and therapies efficacious for HFrEF and/or HFpEF.
“The goal of this session is for attendees to incorporate this new information into their clinical practice so they can optimally manage patients with heart failure,” Dr. Smith said.
The session is specifically curated to impact the clinical practice of hospitalists who provide care for patients with heart failure in the acute care setting and beyond. Key impact areas of clinical practice that will be tackled include:
- Augmenting one’s clinical acumen to diagnose HFpEF.
- Calculating mortality risk for patients with acute heart failure.
- Recognizing other predictors of risk for patients hospitalized with heart failure.
- Recommending dietary, medication, and interventional therapies to prevent future heart failure morbidity and mortality.
Dr. Smith will conclude each literature review with a summary of take-home learning points carefully selected to either change, modify, or confirm the current practice and teaching for providers who care for heart failure patients.
Although Dr. Smith has presented the “Updates in Heart Failure” session in various educational arenas in the past, this is a new update. He has gained vast experience and expertise in this area from conducting extensive and in-depth literature reviews on managing heart failure while preparing for presentations on this topic.
In addition, Dr. Smith has contributed to original research manuscripts, book chapters, and board review–style exam questions in cardiology – including heart failure – and evidence-based medicine topics as an author and editor. He has also sought out additional training and completed faculty development programs targeted at improving his knowledge and skill set to teach evidence-based clinical practice.
Dr. Smith had no relevant financial conflicts to disclose.
Updates in Heart Failure
Live Q&A – Tuesday, Aug. 25 1:00 p.m. to 2:00 p.m.
Hospitalists frequently encounter patients with heart failure – a complex, clinical syndrome, which has high prevalence, mortality, hospitalization rates, and health care costs.
The HM20 Virtual session “Updates in Heart Failure” will provide literature updates for all types of heart failure patient scenarios – patients with acute and chronic heart failure, those who are hospitalized with heart failure, and patients with heart failure with reduced ejection fraction (HFrEF) and heart failure with preserved ejection fraction (HFpEF). The popular session with questions and answers will be held on Aug. 25.
Presenter Dustin Smith, MD, SFHM, associate professor of medicine in the department of medicine at Emory University, Atlanta, and section chief for education in medical specialty at the Atlanta Veterans Affairs Medical Center, will discuss recent trends, diagnostics, therapeutics, and prognostics for heart failure. He’ll also provide a summary of recent changes to clinical practice guidelines.
“The significance of staying knowledgeable and updated regarding this common admission diagnosis cannot be overstated,” Dr. Smith said. Attendees of this clinical update should learn important practices from new evidence in literature, including an unearthed risk grade predictor of acute heart failure mortality, a diagnostic tool for HFpEF in euvolemic patients with unexplained dyspnea, an examination of the potassium “repletion reflex” in patients hospitalized with heart failure, dietary patterns associated with incident heart failure, and therapies efficacious for HFrEF and/or HFpEF.
“The goal of this session is for attendees to incorporate this new information into their clinical practice so they can optimally manage patients with heart failure,” Dr. Smith said.
The session is specifically curated to impact the clinical practice of hospitalists who provide care for patients with heart failure in the acute care setting and beyond. Key impact areas of clinical practice that will be tackled include:
- Augmenting one’s clinical acumen to diagnose HFpEF.
- Calculating mortality risk for patients with acute heart failure.
- Recognizing other predictors of risk for patients hospitalized with heart failure.
- Recommending dietary, medication, and interventional therapies to prevent future heart failure morbidity and mortality.
Dr. Smith will conclude each literature review with a summary of take-home learning points carefully selected to either change, modify, or confirm the current practice and teaching for providers who care for heart failure patients.
Although Dr. Smith has presented the “Updates in Heart Failure” session in various educational arenas in the past, this is a new update. He has gained vast experience and expertise in this area from conducting extensive and in-depth literature reviews on managing heart failure while preparing for presentations on this topic.
In addition, Dr. Smith has contributed to original research manuscripts, book chapters, and board review–style exam questions in cardiology – including heart failure – and evidence-based medicine topics as an author and editor. He has also sought out additional training and completed faculty development programs targeted at improving his knowledge and skill set to teach evidence-based clinical practice.
Dr. Smith had no relevant financial conflicts to disclose.
Updates in Heart Failure
Live Q&A – Tuesday, Aug. 25 1:00 p.m. to 2:00 p.m.
Hospitalists frequently encounter patients with heart failure – a complex, clinical syndrome, which has high prevalence, mortality, hospitalization rates, and health care costs.
The HM20 Virtual session “Updates in Heart Failure” will provide literature updates for all types of heart failure patient scenarios – patients with acute and chronic heart failure, those who are hospitalized with heart failure, and patients with heart failure with reduced ejection fraction (HFrEF) and heart failure with preserved ejection fraction (HFpEF). The popular session with questions and answers will be held on Aug. 25.
Presenter Dustin Smith, MD, SFHM, associate professor of medicine in the department of medicine at Emory University, Atlanta, and section chief for education in medical specialty at the Atlanta Veterans Affairs Medical Center, will discuss recent trends, diagnostics, therapeutics, and prognostics for heart failure. He’ll also provide a summary of recent changes to clinical practice guidelines.
“The significance of staying knowledgeable and updated regarding this common admission diagnosis cannot be overstated,” Dr. Smith said. Attendees of this clinical update should learn important practices from new evidence in literature, including an unearthed risk grade predictor of acute heart failure mortality, a diagnostic tool for HFpEF in euvolemic patients with unexplained dyspnea, an examination of the potassium “repletion reflex” in patients hospitalized with heart failure, dietary patterns associated with incident heart failure, and therapies efficacious for HFrEF and/or HFpEF.
“The goal of this session is for attendees to incorporate this new information into their clinical practice so they can optimally manage patients with heart failure,” Dr. Smith said.
The session is specifically curated to impact the clinical practice of hospitalists who provide care for patients with heart failure in the acute care setting and beyond. Key impact areas of clinical practice that will be tackled include:
- Augmenting one’s clinical acumen to diagnose HFpEF.
- Calculating mortality risk for patients with acute heart failure.
- Recognizing other predictors of risk for patients hospitalized with heart failure.
- Recommending dietary, medication, and interventional therapies to prevent future heart failure morbidity and mortality.
Dr. Smith will conclude each literature review with a summary of take-home learning points carefully selected to either change, modify, or confirm the current practice and teaching for providers who care for heart failure patients.
Although Dr. Smith has presented the “Updates in Heart Failure” session in various educational arenas in the past, this is a new update. He has gained vast experience and expertise in this area from conducting extensive and in-depth literature reviews on managing heart failure while preparing for presentations on this topic.
In addition, Dr. Smith has contributed to original research manuscripts, book chapters, and board review–style exam questions in cardiology – including heart failure – and evidence-based medicine topics as an author and editor. He has also sought out additional training and completed faculty development programs targeted at improving his knowledge and skill set to teach evidence-based clinical practice.
Dr. Smith had no relevant financial conflicts to disclose.
Updates in Heart Failure
Live Q&A – Tuesday, Aug. 25 1:00 p.m. to 2:00 p.m.
Keynote speaker urges innovation in the GI field
Endorses AGA’s Center for GI Innovation and Technology as a place to connect with others.
Although the gastroenterology specialty relies heavily on technology, only incremental advances have been made in this space in the last several decades. “While the potential for innovation is huge, we need to overcome structural and conceptual barriers to realize its true potential,” said Pankaj Jay Pasricha, MD, vice chair of the department of medicine at Johns Hopkins University, Baltimore. Dr. Pasricha will discuss what barriers exist and how to overcome them in his keynote presentation at 2019 AGA Tech Summit, sponsored by the AGA Center for GI Innovation and Technology.
Some barriers are risk aversion, reimbursement challenges, and failure to understand true unmet needs. “We need to find practical solutions that are technologically innovative that can get to market,” he said. The general concepts that Dr. Pasricha talks about will be discussed in detail with specific examples during the summit’s sessions.
When looking to bring innovative ideas to market, Dr. Pasricha recommends learning from individuals who have already done this successfully and from those who have tried and failed. One way to do this is to connect with inventors, entrepreneurs, investors, health care providers and institutions, and regulatory and reimbursement stakeholders through the AGA Center for GI Innovation & Technology (CGIT), which he helped found 10 years ago and served as the center's first chair.
The center supports innovation and developing new technology in gastroenterology, hepatology, nutrition, and obesity by guiding medical device and therapeutics innovators through the technology development and adoption process, according to CGIT’s website. It serves as a key resource for industry and physician innovators developing new technology in gastroenterology, and provides guidance to the Food and Drug Administration and other regulatory groups to expedite the device development process.
“CGIT’s purpose is to provide education on how to identify needs, find solutions, and provide roadmaps for connecting ideas and bringing them to the real world,” Dr. Pasricha said. “We need to create disruptive technologies that will address unmet needs at every level from the average gastroenterologist in practice, to advanced endoscopists, and even advanced surgeons who perform gastroenterology procedures.”
CGIT also provides guidance for bringing new technologies into clinical trials through the creation of registries and other means. You can learn more about the center at www.gastro.org/CGIT.
Regarding recent advances in technologies, Dr. Pasricha said there are now better ways to ablate tissue, do tissue anastomosis, prevent reflux, promote weight loss, and resect locally advanced cancer. “Platform” technologies such as new ways to deliver energy, flexible robotics, and artificial intelligence are also beginning to emerge in our specialty.
Dr. Pasricha is quite experienced in bringing new technologies to market. He holds more than 50 patents that have either been issued or are in process by The United States Patent and Trademark Office and has cofounded several companies within both the medtech/endoscopy and biotech gastroenterology spaces.
His contributions to endoscopy include the use of botulinum toxin for gastroenterology disorders, cryotherapy, novel stents, and the POEM procedure. He is currently working with Galvani Bioelectronics to develop a novel neuromodulation therapy for type 2 diabetes, which has become a worldwide scourge.
Dr. Pasricha discloses being a consultant for several pharmaceutical companies.
Endorses AGA’s Center for GI Innovation and Technology as a place to connect with others.
Endorses AGA’s Center for GI Innovation and Technology as a place to connect with others.
Although the gastroenterology specialty relies heavily on technology, only incremental advances have been made in this space in the last several decades. “While the potential for innovation is huge, we need to overcome structural and conceptual barriers to realize its true potential,” said Pankaj Jay Pasricha, MD, vice chair of the department of medicine at Johns Hopkins University, Baltimore. Dr. Pasricha will discuss what barriers exist and how to overcome them in his keynote presentation at 2019 AGA Tech Summit, sponsored by the AGA Center for GI Innovation and Technology.
Some barriers are risk aversion, reimbursement challenges, and failure to understand true unmet needs. “We need to find practical solutions that are technologically innovative that can get to market,” he said. The general concepts that Dr. Pasricha talks about will be discussed in detail with specific examples during the summit’s sessions.
When looking to bring innovative ideas to market, Dr. Pasricha recommends learning from individuals who have already done this successfully and from those who have tried and failed. One way to do this is to connect with inventors, entrepreneurs, investors, health care providers and institutions, and regulatory and reimbursement stakeholders through the AGA Center for GI Innovation & Technology (CGIT), which he helped found 10 years ago and served as the center's first chair.
The center supports innovation and developing new technology in gastroenterology, hepatology, nutrition, and obesity by guiding medical device and therapeutics innovators through the technology development and adoption process, according to CGIT’s website. It serves as a key resource for industry and physician innovators developing new technology in gastroenterology, and provides guidance to the Food and Drug Administration and other regulatory groups to expedite the device development process.
“CGIT’s purpose is to provide education on how to identify needs, find solutions, and provide roadmaps for connecting ideas and bringing them to the real world,” Dr. Pasricha said. “We need to create disruptive technologies that will address unmet needs at every level from the average gastroenterologist in practice, to advanced endoscopists, and even advanced surgeons who perform gastroenterology procedures.”
CGIT also provides guidance for bringing new technologies into clinical trials through the creation of registries and other means. You can learn more about the center at www.gastro.org/CGIT.
Regarding recent advances in technologies, Dr. Pasricha said there are now better ways to ablate tissue, do tissue anastomosis, prevent reflux, promote weight loss, and resect locally advanced cancer. “Platform” technologies such as new ways to deliver energy, flexible robotics, and artificial intelligence are also beginning to emerge in our specialty.
Dr. Pasricha is quite experienced in bringing new technologies to market. He holds more than 50 patents that have either been issued or are in process by The United States Patent and Trademark Office and has cofounded several companies within both the medtech/endoscopy and biotech gastroenterology spaces.
His contributions to endoscopy include the use of botulinum toxin for gastroenterology disorders, cryotherapy, novel stents, and the POEM procedure. He is currently working with Galvani Bioelectronics to develop a novel neuromodulation therapy for type 2 diabetes, which has become a worldwide scourge.
Dr. Pasricha discloses being a consultant for several pharmaceutical companies.
Although the gastroenterology specialty relies heavily on technology, only incremental advances have been made in this space in the last several decades. “While the potential for innovation is huge, we need to overcome structural and conceptual barriers to realize its true potential,” said Pankaj Jay Pasricha, MD, vice chair of the department of medicine at Johns Hopkins University, Baltimore. Dr. Pasricha will discuss what barriers exist and how to overcome them in his keynote presentation at 2019 AGA Tech Summit, sponsored by the AGA Center for GI Innovation and Technology.
Some barriers are risk aversion, reimbursement challenges, and failure to understand true unmet needs. “We need to find practical solutions that are technologically innovative that can get to market,” he said. The general concepts that Dr. Pasricha talks about will be discussed in detail with specific examples during the summit’s sessions.
When looking to bring innovative ideas to market, Dr. Pasricha recommends learning from individuals who have already done this successfully and from those who have tried and failed. One way to do this is to connect with inventors, entrepreneurs, investors, health care providers and institutions, and regulatory and reimbursement stakeholders through the AGA Center for GI Innovation & Technology (CGIT), which he helped found 10 years ago and served as the center's first chair.
The center supports innovation and developing new technology in gastroenterology, hepatology, nutrition, and obesity by guiding medical device and therapeutics innovators through the technology development and adoption process, according to CGIT’s website. It serves as a key resource for industry and physician innovators developing new technology in gastroenterology, and provides guidance to the Food and Drug Administration and other regulatory groups to expedite the device development process.
“CGIT’s purpose is to provide education on how to identify needs, find solutions, and provide roadmaps for connecting ideas and bringing them to the real world,” Dr. Pasricha said. “We need to create disruptive technologies that will address unmet needs at every level from the average gastroenterologist in practice, to advanced endoscopists, and even advanced surgeons who perform gastroenterology procedures.”
CGIT also provides guidance for bringing new technologies into clinical trials through the creation of registries and other means. You can learn more about the center at www.gastro.org/CGIT.
Regarding recent advances in technologies, Dr. Pasricha said there are now better ways to ablate tissue, do tissue anastomosis, prevent reflux, promote weight loss, and resect locally advanced cancer. “Platform” technologies such as new ways to deliver energy, flexible robotics, and artificial intelligence are also beginning to emerge in our specialty.
Dr. Pasricha is quite experienced in bringing new technologies to market. He holds more than 50 patents that have either been issued or are in process by The United States Patent and Trademark Office and has cofounded several companies within both the medtech/endoscopy and biotech gastroenterology spaces.
His contributions to endoscopy include the use of botulinum toxin for gastroenterology disorders, cryotherapy, novel stents, and the POEM procedure. He is currently working with Galvani Bioelectronics to develop a novel neuromodulation therapy for type 2 diabetes, which has become a worldwide scourge.
Dr. Pasricha discloses being a consultant for several pharmaceutical companies.
FROM THE 2019 AGA TECH SUMMIT
Improve palliative care and pain management
Sunday’s pre-course titled “Essentials of Palliative Care and Pain Management for Hospitalists” will focus on how to accurately share a prognosis with patients and their family members, how to discuss care plans with patients, and how to treat severe pain and other symptoms.
“There aren’t enough palliative care physicians for all hospitalized patients with serious illnesses, so it’s vital that hospitalists have the necessary skills and confidence to practice primary palliative care,” said course director Theresa Vettese, MD, who is associate professor in the division of general medicine, department of medicine, Emory University, Atlanta.
“As the U.S. population ages and physicians’ ability to treat medical conditions improves, we will continue to see an increased patient population with serious illness in the hospital setting,” Dr. Vettese said. “Hospitalists will regularly care for these patients and are well positioned to make a major impact on improving their quality of life as well as decreasing their suffering. It’s important that hospitalists have competence in primary palliative care so that they can offer patients and families the greatest compassion and care during difficult times.”
Dr. Vettese said the pre-course’s goals include having participants focus on strategies to become more comfortable and confident in their core communication skills with seriously ill hospitalized patients. Attendees also will gain a better understanding of evidence-based management of pain across a continuum of disease states, from relative health to serious illness and end of life. Speakers will discuss the rational use of opioid analgesics, appropriate use of adjuvant medications for treating pain, and management of complex pain patients. Participants will learn how to assess and provide effective interventions for nonpain symptoms in hospitalized patients with serious illness, including depression/anxiety, nausea/vomiting, dyspnea, pruritus, and fatigue.
Dr. Vettese, whose course codirector is Rab Razzak, MD, assistant professor of medicine and director of outpatient palliative medicine at Johns Hopkins University, Baltimore, said that all hospitalists struggle with difficult cases – whether it’s managing a cancer patient with uncontrolled pain or helping patients align treatment options to their individual values and goals.
“Our hope is that participants will return to their institution and be more comfortable in practicing basic palliative care skills as well as sharing lessons learned with their colleagues,” Dr. Vettese said.
“Developing primary palliative care skills is an outstanding way for hospitalists of all experience levels to broaden their skill set and make a key difference in patients’ lives,” she continued. “Our course will enable participants to provide even better care to their patients.
“Focusing a full day on developing primary palliative care skills is another example of SHM identifying expertise that its members want and need in order to optimally care for patients and educate colleagues and trainees,” Dr. Vettese concluded. Learners of all levels will benefit from the session.
Dr. Vettese had no relevant financial conflicts to disclose.
Essentials of Palliative Care and Pain Management for Hospitalists
Sunday, 8:00 a.m. – 4:30 p.m.
National Harbor 3
Sunday’s pre-course titled “Essentials of Palliative Care and Pain Management for Hospitalists” will focus on how to accurately share a prognosis with patients and their family members, how to discuss care plans with patients, and how to treat severe pain and other symptoms.
“There aren’t enough palliative care physicians for all hospitalized patients with serious illnesses, so it’s vital that hospitalists have the necessary skills and confidence to practice primary palliative care,” said course director Theresa Vettese, MD, who is associate professor in the division of general medicine, department of medicine, Emory University, Atlanta.
“As the U.S. population ages and physicians’ ability to treat medical conditions improves, we will continue to see an increased patient population with serious illness in the hospital setting,” Dr. Vettese said. “Hospitalists will regularly care for these patients and are well positioned to make a major impact on improving their quality of life as well as decreasing their suffering. It’s important that hospitalists have competence in primary palliative care so that they can offer patients and families the greatest compassion and care during difficult times.”
Dr. Vettese said the pre-course’s goals include having participants focus on strategies to become more comfortable and confident in their core communication skills with seriously ill hospitalized patients. Attendees also will gain a better understanding of evidence-based management of pain across a continuum of disease states, from relative health to serious illness and end of life. Speakers will discuss the rational use of opioid analgesics, appropriate use of adjuvant medications for treating pain, and management of complex pain patients. Participants will learn how to assess and provide effective interventions for nonpain symptoms in hospitalized patients with serious illness, including depression/anxiety, nausea/vomiting, dyspnea, pruritus, and fatigue.
Dr. Vettese, whose course codirector is Rab Razzak, MD, assistant professor of medicine and director of outpatient palliative medicine at Johns Hopkins University, Baltimore, said that all hospitalists struggle with difficult cases – whether it’s managing a cancer patient with uncontrolled pain or helping patients align treatment options to their individual values and goals.
“Our hope is that participants will return to their institution and be more comfortable in practicing basic palliative care skills as well as sharing lessons learned with their colleagues,” Dr. Vettese said.
“Developing primary palliative care skills is an outstanding way for hospitalists of all experience levels to broaden their skill set and make a key difference in patients’ lives,” she continued. “Our course will enable participants to provide even better care to their patients.
“Focusing a full day on developing primary palliative care skills is another example of SHM identifying expertise that its members want and need in order to optimally care for patients and educate colleagues and trainees,” Dr. Vettese concluded. Learners of all levels will benefit from the session.
Dr. Vettese had no relevant financial conflicts to disclose.
Essentials of Palliative Care and Pain Management for Hospitalists
Sunday, 8:00 a.m. – 4:30 p.m.
National Harbor 3
Sunday’s pre-course titled “Essentials of Palliative Care and Pain Management for Hospitalists” will focus on how to accurately share a prognosis with patients and their family members, how to discuss care plans with patients, and how to treat severe pain and other symptoms.
“There aren’t enough palliative care physicians for all hospitalized patients with serious illnesses, so it’s vital that hospitalists have the necessary skills and confidence to practice primary palliative care,” said course director Theresa Vettese, MD, who is associate professor in the division of general medicine, department of medicine, Emory University, Atlanta.
“As the U.S. population ages and physicians’ ability to treat medical conditions improves, we will continue to see an increased patient population with serious illness in the hospital setting,” Dr. Vettese said. “Hospitalists will regularly care for these patients and are well positioned to make a major impact on improving their quality of life as well as decreasing their suffering. It’s important that hospitalists have competence in primary palliative care so that they can offer patients and families the greatest compassion and care during difficult times.”
Dr. Vettese said the pre-course’s goals include having participants focus on strategies to become more comfortable and confident in their core communication skills with seriously ill hospitalized patients. Attendees also will gain a better understanding of evidence-based management of pain across a continuum of disease states, from relative health to serious illness and end of life. Speakers will discuss the rational use of opioid analgesics, appropriate use of adjuvant medications for treating pain, and management of complex pain patients. Participants will learn how to assess and provide effective interventions for nonpain symptoms in hospitalized patients with serious illness, including depression/anxiety, nausea/vomiting, dyspnea, pruritus, and fatigue.
Dr. Vettese, whose course codirector is Rab Razzak, MD, assistant professor of medicine and director of outpatient palliative medicine at Johns Hopkins University, Baltimore, said that all hospitalists struggle with difficult cases – whether it’s managing a cancer patient with uncontrolled pain or helping patients align treatment options to their individual values and goals.
“Our hope is that participants will return to their institution and be more comfortable in practicing basic palliative care skills as well as sharing lessons learned with their colleagues,” Dr. Vettese said.
“Developing primary palliative care skills is an outstanding way for hospitalists of all experience levels to broaden their skill set and make a key difference in patients’ lives,” she continued. “Our course will enable participants to provide even better care to their patients.
“Focusing a full day on developing primary palliative care skills is another example of SHM identifying expertise that its members want and need in order to optimally care for patients and educate colleagues and trainees,” Dr. Vettese concluded. Learners of all levels will benefit from the session.
Dr. Vettese had no relevant financial conflicts to disclose.
Essentials of Palliative Care and Pain Management for Hospitalists
Sunday, 8:00 a.m. – 4:30 p.m.
National Harbor 3
Get hands-on with point-of-care ultrasound
Hospitalists and other health care workers will be introduced to the concept of using point-of-care ultrasound to guide bedside diagnostics and clinical decision making at a Sunday pre-course titled “Point-of-Care Ultrasound for the Hospitalist.”
HM19 marks the 10th anniversary of this particular pre-course offering. “It is the SHM annual meeting’s longest-standing pre-course, and it has sold out every year since its inception. Learners always rate it highly,” said course director Nilam J. Soni, MD, MS, associate professor in the department of medicine at the University of Texas, San Antonio. “Faculty members are very experienced and passionate about teaching this innovative technology.”
Dr. Soni said that using portable ultrasound takes clinicians back to the bedside, which is a rarity with new technologies. “It allows clinicians to spend more time with patients, which is fulfilling for the patient and clinician,” he said. “Based on what we’ve seen over the past decade, it can improve hospitalists’ job satisfaction and enjoyment of their clinical work.”
While most medical schools are now introducing point-of-care ultrasound to their medical students, many currently practicing physicians haven’t been trained in using this new technology. This pre-course can help fill that gap.
Although ultrasound technology has existed since the 1940s, large bulky machines weren’t practical for bedside use. Now, ultrasound machines are so small that they can be carried in a coat pocket. “Small machines can be as powerful as some of the larger ones and cost only a few thousand dollars due to increasing market competition,” said Dr. Soni, whose course codirector is Ricardo Franco-Sadud, MD, a hospitalist at Naples (Fla.) Community Hospital. “The availability and portability is driving the uptake of ultrasound.”
In addition to being used at the bedside, ultrasound has other advantages, such as being noninvasive and not emitting radiation like CT scans do.
“It’s time for physicians to have another bedside tool in their black bag,” said Dr. Soni, who notes that the stethoscope is more than 200 years old and human hands and eyes have limitations.
This session will appeal to a mix of attendees. Administrators will gain a better understanding of the multitude of applications of point-of-care ultrasound and how ultrasound can be integrated into their practice. Clinicians will get hands-on experience by practicing a multitude of applications during scanning sessions with live models. Medical educators will glean insight on how to develop training programs and curricula.
“Our goal is to familiarize attendees with using ultrasound for different applications to evaluate common conditions, such as heart failure, pleural effusions, pneumonia, and lower-extremity swelling,” Dr. Soni said.
The pre-course will feature practical and focused lectures combined with hands-on practice sessions. “We’ll start with the basics on how to use ultrasound, then we’ll practicing acquiring images on live models and reviewing normal and abnormal images. We’ll conclude with real patient cases.” Learners will rotate in small groups to different tables where they will practice different skills on varying body parts.
Dr. Soni reports grants from the Department of Veterans Affairs Quality Enhancement Research Initiative Partnered Evaluation Initiative Grant (HX002263-01A1) outside of the submitted work.
Point-of-Care Ultrasound for the Hospitalist
Sunday, 7:30 a.m. – 12:30 p.m. and 1:00 – 6:00 p.m.
Potomac C/1-3
Hospitalists and other health care workers will be introduced to the concept of using point-of-care ultrasound to guide bedside diagnostics and clinical decision making at a Sunday pre-course titled “Point-of-Care Ultrasound for the Hospitalist.”
HM19 marks the 10th anniversary of this particular pre-course offering. “It is the SHM annual meeting’s longest-standing pre-course, and it has sold out every year since its inception. Learners always rate it highly,” said course director Nilam J. Soni, MD, MS, associate professor in the department of medicine at the University of Texas, San Antonio. “Faculty members are very experienced and passionate about teaching this innovative technology.”
Dr. Soni said that using portable ultrasound takes clinicians back to the bedside, which is a rarity with new technologies. “It allows clinicians to spend more time with patients, which is fulfilling for the patient and clinician,” he said. “Based on what we’ve seen over the past decade, it can improve hospitalists’ job satisfaction and enjoyment of their clinical work.”
While most medical schools are now introducing point-of-care ultrasound to their medical students, many currently practicing physicians haven’t been trained in using this new technology. This pre-course can help fill that gap.
Although ultrasound technology has existed since the 1940s, large bulky machines weren’t practical for bedside use. Now, ultrasound machines are so small that they can be carried in a coat pocket. “Small machines can be as powerful as some of the larger ones and cost only a few thousand dollars due to increasing market competition,” said Dr. Soni, whose course codirector is Ricardo Franco-Sadud, MD, a hospitalist at Naples (Fla.) Community Hospital. “The availability and portability is driving the uptake of ultrasound.”
In addition to being used at the bedside, ultrasound has other advantages, such as being noninvasive and not emitting radiation like CT scans do.
“It’s time for physicians to have another bedside tool in their black bag,” said Dr. Soni, who notes that the stethoscope is more than 200 years old and human hands and eyes have limitations.
This session will appeal to a mix of attendees. Administrators will gain a better understanding of the multitude of applications of point-of-care ultrasound and how ultrasound can be integrated into their practice. Clinicians will get hands-on experience by practicing a multitude of applications during scanning sessions with live models. Medical educators will glean insight on how to develop training programs and curricula.
“Our goal is to familiarize attendees with using ultrasound for different applications to evaluate common conditions, such as heart failure, pleural effusions, pneumonia, and lower-extremity swelling,” Dr. Soni said.
The pre-course will feature practical and focused lectures combined with hands-on practice sessions. “We’ll start with the basics on how to use ultrasound, then we’ll practicing acquiring images on live models and reviewing normal and abnormal images. We’ll conclude with real patient cases.” Learners will rotate in small groups to different tables where they will practice different skills on varying body parts.
Dr. Soni reports grants from the Department of Veterans Affairs Quality Enhancement Research Initiative Partnered Evaluation Initiative Grant (HX002263-01A1) outside of the submitted work.
Point-of-Care Ultrasound for the Hospitalist
Sunday, 7:30 a.m. – 12:30 p.m. and 1:00 – 6:00 p.m.
Potomac C/1-3
Hospitalists and other health care workers will be introduced to the concept of using point-of-care ultrasound to guide bedside diagnostics and clinical decision making at a Sunday pre-course titled “Point-of-Care Ultrasound for the Hospitalist.”
HM19 marks the 10th anniversary of this particular pre-course offering. “It is the SHM annual meeting’s longest-standing pre-course, and it has sold out every year since its inception. Learners always rate it highly,” said course director Nilam J. Soni, MD, MS, associate professor in the department of medicine at the University of Texas, San Antonio. “Faculty members are very experienced and passionate about teaching this innovative technology.”
Dr. Soni said that using portable ultrasound takes clinicians back to the bedside, which is a rarity with new technologies. “It allows clinicians to spend more time with patients, which is fulfilling for the patient and clinician,” he said. “Based on what we’ve seen over the past decade, it can improve hospitalists’ job satisfaction and enjoyment of their clinical work.”
While most medical schools are now introducing point-of-care ultrasound to their medical students, many currently practicing physicians haven’t been trained in using this new technology. This pre-course can help fill that gap.
Although ultrasound technology has existed since the 1940s, large bulky machines weren’t practical for bedside use. Now, ultrasound machines are so small that they can be carried in a coat pocket. “Small machines can be as powerful as some of the larger ones and cost only a few thousand dollars due to increasing market competition,” said Dr. Soni, whose course codirector is Ricardo Franco-Sadud, MD, a hospitalist at Naples (Fla.) Community Hospital. “The availability and portability is driving the uptake of ultrasound.”
In addition to being used at the bedside, ultrasound has other advantages, such as being noninvasive and not emitting radiation like CT scans do.
“It’s time for physicians to have another bedside tool in their black bag,” said Dr. Soni, who notes that the stethoscope is more than 200 years old and human hands and eyes have limitations.
This session will appeal to a mix of attendees. Administrators will gain a better understanding of the multitude of applications of point-of-care ultrasound and how ultrasound can be integrated into their practice. Clinicians will get hands-on experience by practicing a multitude of applications during scanning sessions with live models. Medical educators will glean insight on how to develop training programs and curricula.
“Our goal is to familiarize attendees with using ultrasound for different applications to evaluate common conditions, such as heart failure, pleural effusions, pneumonia, and lower-extremity swelling,” Dr. Soni said.
The pre-course will feature practical and focused lectures combined with hands-on practice sessions. “We’ll start with the basics on how to use ultrasound, then we’ll practicing acquiring images on live models and reviewing normal and abnormal images. We’ll conclude with real patient cases.” Learners will rotate in small groups to different tables where they will practice different skills on varying body parts.
Dr. Soni reports grants from the Department of Veterans Affairs Quality Enhancement Research Initiative Partnered Evaluation Initiative Grant (HX002263-01A1) outside of the submitted work.
Point-of-Care Ultrasound for the Hospitalist
Sunday, 7:30 a.m. – 12:30 p.m. and 1:00 – 6:00 p.m.
Potomac C/1-3
SHM names new Masters in Hospital Medicine
This year, the Society of Hospital Medicine will induct two new Masters in Hospital Medicine (MHM), the society’s highest professional honor. After the new honorees receive their designations, there will be only 30 MHMs society-wide, out of a universe of more than 60,000 hospitalists.
“The MHMs are truly the ‘hall of fame’ for hospital medicine and our society,” said Larry Wellikson, MD, MHM, the CEO of SHM.
SHM first introduced the MHM designation in 2010. The honor is reserved for hospitalists who have uniquely distinguished themselves in the specialty through the excellence and significance of their contributions to hospital medicine specifically and health care as a whole. SHM members are nominated for MHM consideration, and the SHM Board of Directors rigorously reviews qualifications and selects each year’s MHM class.
The two hospitalists receiving the MHM designation at HM19 are Brian Harte, MD, MHM, and Samir Shah, MD, MHM.
Brian Harte, MD, MHM
“Dr. Harte was selected as an MHM in honor of his unwavering dedication to hospital medicine and the Society as a stellar clinician and inspiring leader,” Dr. Wellikson said.
Dr. Harte is president of Cleveland Clinic Akron General and the Southern Region and is an associate professor of medicine at Cleveland Clinic Lerner College of Medicine at Case Western Reserve University. He formerly served as president of Cleveland Clinic Hillcrest Hospital and Cleveland Clinic South Pointe Hospital.
Dr. Harte’s contributions to hospital medicine have been numerous, both as an educator and a clinician. “Because of his prowess for improving hospital operations while continuing to uphold the highest standards of clinical care, Dr. Harte advanced quickly, developing and growing the presence of hospital medicine throughout the Cleveland Clinic network,” Dr. Wellikson said.
Regarding the award, Dr. Harte said, “I’m honored to receive this recognition and would like to thank my colleagues at SHM. I will continue to work to advocate for patient care and to challenge physicians to lead improvements in quality and safety.”
Dr. Harte served on the SHM Board of Directors for 6 years, including serving as treasurer and president. He served on a number of committees, including the Annual Conference and Public Policy committees. He has presented at multiple SHM Annual Conferences on leadership, quality and patient safety, and hospital operations.
“SHM is progressive in its thinking,” Dr. Harte said. “The Society’s focus on staying ahead of changes in health care and advocating for patients makes it an organization that will shape health care in the years to come.”
Dr. Harte was also a deputy editor for the Journal of Hospital Medicine – SHM’s flagship, peer-reviewed publication for hospital medicine research – for 9 years, and was instrumental in developing its “Clinical Care Conundrums” series.
Samir S. Shah, MD, MSCE, MHM
Dr. Samir S. Shah was selected as an MHM in honor of his leadership in hospital medicine as a stellar researcher, devoted mentor, and key contributor to the Society.
He is a professor of pediatrics at the University of Cincinnati College of Medicine, as well as director of the division of hospital medicine and chief metrics officer at Cincinnati Children’s Hospital Medical Center, where he holds the James M. Ewell Endowed Chair.
“Dr. Shah is a leading figure in the founding and growing of pediatric hospital medicine, ensuring that research is a central focus of this specialty,” Dr. Wellikson said.
“Much of what I’ve done is foundational – developing leaders and creating networks of mentoring relationships and a culture of sponsorship to help others succeed so that we can advance the field and patient care faster and further together,” Dr. Shah said, commenting on his MHM recognition. “I am honored and humbled. I’m proud to have contributed to the academic development of the field through research, mentorship, and sponsorship. My team and my colleagues have helped me to become a better leader. I view this award as a recognition of their efforts to help me advance pediatric hospital medicine as an academic discipline.”
In January 2019, Dr. Shah assumed the role of Journal of Hospital Medicine editor in chief. He has held other leadership positions with the journal, including associate, deputy, and senior deputy editor, since 2009. He has authored more than 300 peer-reviewed publications and more than 150 book chapters. He is also editor or coeditor of 12 books.
Dr. Shah has also served as the primary research mentor to more than 85 medical students, residents, fellows, junior faculty, and postdoctoral students, and as a career and professional development mentor to countless others. He is the primary research mentor for five current National Institutes of Health or Agency for Healthcare Research and Quality K-series career development award recipients.
Dr. Shah has helped to develop and better leverage data infrastructure to help scale research and link variation in clinical practice to outcomes nationally to determine best clinical practice. For example, he partnered with the Children’s Hospital Association, where he chairs the Pediatric Health Information Research Groups.
“While his individual research accomplishments are exceptional, his more lasting impacts in pediatric hospital medicine are in creating and growing research networks and advancing academic growth of the field,” Dr. Wellikson said.
Dr. Shah received the 2009 Award of Excellence for Research from SHM and has served on both the Awards and Research committees.
This year, the Society of Hospital Medicine will induct two new Masters in Hospital Medicine (MHM), the society’s highest professional honor. After the new honorees receive their designations, there will be only 30 MHMs society-wide, out of a universe of more than 60,000 hospitalists.
“The MHMs are truly the ‘hall of fame’ for hospital medicine and our society,” said Larry Wellikson, MD, MHM, the CEO of SHM.
SHM first introduced the MHM designation in 2010. The honor is reserved for hospitalists who have uniquely distinguished themselves in the specialty through the excellence and significance of their contributions to hospital medicine specifically and health care as a whole. SHM members are nominated for MHM consideration, and the SHM Board of Directors rigorously reviews qualifications and selects each year’s MHM class.
The two hospitalists receiving the MHM designation at HM19 are Brian Harte, MD, MHM, and Samir Shah, MD, MHM.
Brian Harte, MD, MHM
“Dr. Harte was selected as an MHM in honor of his unwavering dedication to hospital medicine and the Society as a stellar clinician and inspiring leader,” Dr. Wellikson said.
Dr. Harte is president of Cleveland Clinic Akron General and the Southern Region and is an associate professor of medicine at Cleveland Clinic Lerner College of Medicine at Case Western Reserve University. He formerly served as president of Cleveland Clinic Hillcrest Hospital and Cleveland Clinic South Pointe Hospital.
Dr. Harte’s contributions to hospital medicine have been numerous, both as an educator and a clinician. “Because of his prowess for improving hospital operations while continuing to uphold the highest standards of clinical care, Dr. Harte advanced quickly, developing and growing the presence of hospital medicine throughout the Cleveland Clinic network,” Dr. Wellikson said.
Regarding the award, Dr. Harte said, “I’m honored to receive this recognition and would like to thank my colleagues at SHM. I will continue to work to advocate for patient care and to challenge physicians to lead improvements in quality and safety.”
Dr. Harte served on the SHM Board of Directors for 6 years, including serving as treasurer and president. He served on a number of committees, including the Annual Conference and Public Policy committees. He has presented at multiple SHM Annual Conferences on leadership, quality and patient safety, and hospital operations.
“SHM is progressive in its thinking,” Dr. Harte said. “The Society’s focus on staying ahead of changes in health care and advocating for patients makes it an organization that will shape health care in the years to come.”
Dr. Harte was also a deputy editor for the Journal of Hospital Medicine – SHM’s flagship, peer-reviewed publication for hospital medicine research – for 9 years, and was instrumental in developing its “Clinical Care Conundrums” series.
Samir S. Shah, MD, MSCE, MHM
Dr. Samir S. Shah was selected as an MHM in honor of his leadership in hospital medicine as a stellar researcher, devoted mentor, and key contributor to the Society.
He is a professor of pediatrics at the University of Cincinnati College of Medicine, as well as director of the division of hospital medicine and chief metrics officer at Cincinnati Children’s Hospital Medical Center, where he holds the James M. Ewell Endowed Chair.
“Dr. Shah is a leading figure in the founding and growing of pediatric hospital medicine, ensuring that research is a central focus of this specialty,” Dr. Wellikson said.
“Much of what I’ve done is foundational – developing leaders and creating networks of mentoring relationships and a culture of sponsorship to help others succeed so that we can advance the field and patient care faster and further together,” Dr. Shah said, commenting on his MHM recognition. “I am honored and humbled. I’m proud to have contributed to the academic development of the field through research, mentorship, and sponsorship. My team and my colleagues have helped me to become a better leader. I view this award as a recognition of their efforts to help me advance pediatric hospital medicine as an academic discipline.”
In January 2019, Dr. Shah assumed the role of Journal of Hospital Medicine editor in chief. He has held other leadership positions with the journal, including associate, deputy, and senior deputy editor, since 2009. He has authored more than 300 peer-reviewed publications and more than 150 book chapters. He is also editor or coeditor of 12 books.
Dr. Shah has also served as the primary research mentor to more than 85 medical students, residents, fellows, junior faculty, and postdoctoral students, and as a career and professional development mentor to countless others. He is the primary research mentor for five current National Institutes of Health or Agency for Healthcare Research and Quality K-series career development award recipients.
Dr. Shah has helped to develop and better leverage data infrastructure to help scale research and link variation in clinical practice to outcomes nationally to determine best clinical practice. For example, he partnered with the Children’s Hospital Association, where he chairs the Pediatric Health Information Research Groups.
“While his individual research accomplishments are exceptional, his more lasting impacts in pediatric hospital medicine are in creating and growing research networks and advancing academic growth of the field,” Dr. Wellikson said.
Dr. Shah received the 2009 Award of Excellence for Research from SHM and has served on both the Awards and Research committees.
This year, the Society of Hospital Medicine will induct two new Masters in Hospital Medicine (MHM), the society’s highest professional honor. After the new honorees receive their designations, there will be only 30 MHMs society-wide, out of a universe of more than 60,000 hospitalists.
“The MHMs are truly the ‘hall of fame’ for hospital medicine and our society,” said Larry Wellikson, MD, MHM, the CEO of SHM.
SHM first introduced the MHM designation in 2010. The honor is reserved for hospitalists who have uniquely distinguished themselves in the specialty through the excellence and significance of their contributions to hospital medicine specifically and health care as a whole. SHM members are nominated for MHM consideration, and the SHM Board of Directors rigorously reviews qualifications and selects each year’s MHM class.
The two hospitalists receiving the MHM designation at HM19 are Brian Harte, MD, MHM, and Samir Shah, MD, MHM.
Brian Harte, MD, MHM
“Dr. Harte was selected as an MHM in honor of his unwavering dedication to hospital medicine and the Society as a stellar clinician and inspiring leader,” Dr. Wellikson said.
Dr. Harte is president of Cleveland Clinic Akron General and the Southern Region and is an associate professor of medicine at Cleveland Clinic Lerner College of Medicine at Case Western Reserve University. He formerly served as president of Cleveland Clinic Hillcrest Hospital and Cleveland Clinic South Pointe Hospital.
Dr. Harte’s contributions to hospital medicine have been numerous, both as an educator and a clinician. “Because of his prowess for improving hospital operations while continuing to uphold the highest standards of clinical care, Dr. Harte advanced quickly, developing and growing the presence of hospital medicine throughout the Cleveland Clinic network,” Dr. Wellikson said.
Regarding the award, Dr. Harte said, “I’m honored to receive this recognition and would like to thank my colleagues at SHM. I will continue to work to advocate for patient care and to challenge physicians to lead improvements in quality and safety.”
Dr. Harte served on the SHM Board of Directors for 6 years, including serving as treasurer and president. He served on a number of committees, including the Annual Conference and Public Policy committees. He has presented at multiple SHM Annual Conferences on leadership, quality and patient safety, and hospital operations.
“SHM is progressive in its thinking,” Dr. Harte said. “The Society’s focus on staying ahead of changes in health care and advocating for patients makes it an organization that will shape health care in the years to come.”
Dr. Harte was also a deputy editor for the Journal of Hospital Medicine – SHM’s flagship, peer-reviewed publication for hospital medicine research – for 9 years, and was instrumental in developing its “Clinical Care Conundrums” series.
Samir S. Shah, MD, MSCE, MHM
Dr. Samir S. Shah was selected as an MHM in honor of his leadership in hospital medicine as a stellar researcher, devoted mentor, and key contributor to the Society.
He is a professor of pediatrics at the University of Cincinnati College of Medicine, as well as director of the division of hospital medicine and chief metrics officer at Cincinnati Children’s Hospital Medical Center, where he holds the James M. Ewell Endowed Chair.
“Dr. Shah is a leading figure in the founding and growing of pediatric hospital medicine, ensuring that research is a central focus of this specialty,” Dr. Wellikson said.
“Much of what I’ve done is foundational – developing leaders and creating networks of mentoring relationships and a culture of sponsorship to help others succeed so that we can advance the field and patient care faster and further together,” Dr. Shah said, commenting on his MHM recognition. “I am honored and humbled. I’m proud to have contributed to the academic development of the field through research, mentorship, and sponsorship. My team and my colleagues have helped me to become a better leader. I view this award as a recognition of their efforts to help me advance pediatric hospital medicine as an academic discipline.”
In January 2019, Dr. Shah assumed the role of Journal of Hospital Medicine editor in chief. He has held other leadership positions with the journal, including associate, deputy, and senior deputy editor, since 2009. He has authored more than 300 peer-reviewed publications and more than 150 book chapters. He is also editor or coeditor of 12 books.
Dr. Shah has also served as the primary research mentor to more than 85 medical students, residents, fellows, junior faculty, and postdoctoral students, and as a career and professional development mentor to countless others. He is the primary research mentor for five current National Institutes of Health or Agency for Healthcare Research and Quality K-series career development award recipients.
Dr. Shah has helped to develop and better leverage data infrastructure to help scale research and link variation in clinical practice to outcomes nationally to determine best clinical practice. For example, he partnered with the Children’s Hospital Association, where he chairs the Pediatric Health Information Research Groups.
“While his individual research accomplishments are exceptional, his more lasting impacts in pediatric hospital medicine are in creating and growing research networks and advancing academic growth of the field,” Dr. Wellikson said.
Dr. Shah received the 2009 Award of Excellence for Research from SHM and has served on both the Awards and Research committees.
Using data to drive quality improvement projects
Measuring and analyzing data is essential for any quality improvement project. Data can validate whether an anecdotal assumption indicates the need for a quality improvement initiative and can help showcase the success of any intervention.
At today’s session, “Using Data to Inform Quality Improvement,” attendees will learn how to develop balanced metrics for quality improvement projects, understand distinctions between quality improvement and traditional research projects, and identify how different measures of the same data can tell vastly different stories.
The session will be divided into three 20-minute sections. Ethan Kuperman, MD, MSc, FHM, clinical assistant professor, University of Iowa Health Care, Iowa City, will begin by discussing how to develop balanced metrics by exploring a venous thromboembolism prophylaxis quality improvement project.
Next, Aparna Kamath, MD, MS, SFHM, assistant professor and academic hospitalist, Duke University Health System, Durham, N.C., will demonstrate the distinction between quality improvement and research by exploring medication reconciliation. “I will also emphasize the need for feasibility and rigor in data gathering and analysis in addition to accuracy when doing a quality improvement project,” she said. “Our workshop will make these tasks less daunting for hospitalists doing quality improvement projects.”
Finally, Justin Glasgow, MD, PhD, inpatient medicine faculty and Value Institute senior clinical scholar, Christiana Care Health System, Newark, Del., will explore how improper data definitions led to differing interpretations while developing and deploying an early warning system. “Attendees will learn how to design a quality improvement project to ensure that they measure interventions in a manner that ensures they have had true success, while not creating any unintended consequences,” Dr. Glasgow said.
“The session is important as it will help attendees develop successful projects that their colleagues will respect and that their bosses will admire,” added Dr. Glasgow. “They will gain confidence to turn their experience into distributable scholarship.”
“Hospitalists at all stages of their careers can benefit from this presentation,” Dr. Kuperman said. “Whether you’re preparing for your first quality improvement project or getting ready for a systemwide redesign, collecting the wrong data or misusing collected data can ruin your results or lead you to the wrong conclusions.”
Each of the three presenters are well versed on the topic and have successfully analyzed data for numerous quality improvement projects and presented these data both in publications and in presentations, including for the Society of Hospital Medicine.
“My best qualification for this talk is the number of times I’ve messed up,” Dr. Kuperman said. “Early in my career, I had several projects in which I spent valuable resources creating an initiative, rolling out the implementation, and then wasn’t able to capture reliable outcomes – ruining the chances for scholarship or renewal.”
Through this presentation, Dr. Kuperman hopes that he can reach other hospitalists and soon-to-be hospitalists and teach them some hard-earned lessons so that they can be more successful from the start.
None of the three presenters have any financial disclosures.
Using Data to Inform Quality Improvement
Wednesday, 8:40-9:40 a.m.
Crystal Ballroom G1/A&B
Measuring and analyzing data is essential for any quality improvement project. Data can validate whether an anecdotal assumption indicates the need for a quality improvement initiative and can help showcase the success of any intervention.
At today’s session, “Using Data to Inform Quality Improvement,” attendees will learn how to develop balanced metrics for quality improvement projects, understand distinctions between quality improvement and traditional research projects, and identify how different measures of the same data can tell vastly different stories.
The session will be divided into three 20-minute sections. Ethan Kuperman, MD, MSc, FHM, clinical assistant professor, University of Iowa Health Care, Iowa City, will begin by discussing how to develop balanced metrics by exploring a venous thromboembolism prophylaxis quality improvement project.
Next, Aparna Kamath, MD, MS, SFHM, assistant professor and academic hospitalist, Duke University Health System, Durham, N.C., will demonstrate the distinction between quality improvement and research by exploring medication reconciliation. “I will also emphasize the need for feasibility and rigor in data gathering and analysis in addition to accuracy when doing a quality improvement project,” she said. “Our workshop will make these tasks less daunting for hospitalists doing quality improvement projects.”
Finally, Justin Glasgow, MD, PhD, inpatient medicine faculty and Value Institute senior clinical scholar, Christiana Care Health System, Newark, Del., will explore how improper data definitions led to differing interpretations while developing and deploying an early warning system. “Attendees will learn how to design a quality improvement project to ensure that they measure interventions in a manner that ensures they have had true success, while not creating any unintended consequences,” Dr. Glasgow said.
“The session is important as it will help attendees develop successful projects that their colleagues will respect and that their bosses will admire,” added Dr. Glasgow. “They will gain confidence to turn their experience into distributable scholarship.”
“Hospitalists at all stages of their careers can benefit from this presentation,” Dr. Kuperman said. “Whether you’re preparing for your first quality improvement project or getting ready for a systemwide redesign, collecting the wrong data or misusing collected data can ruin your results or lead you to the wrong conclusions.”
Each of the three presenters are well versed on the topic and have successfully analyzed data for numerous quality improvement projects and presented these data both in publications and in presentations, including for the Society of Hospital Medicine.
“My best qualification for this talk is the number of times I’ve messed up,” Dr. Kuperman said. “Early in my career, I had several projects in which I spent valuable resources creating an initiative, rolling out the implementation, and then wasn’t able to capture reliable outcomes – ruining the chances for scholarship or renewal.”
Through this presentation, Dr. Kuperman hopes that he can reach other hospitalists and soon-to-be hospitalists and teach them some hard-earned lessons so that they can be more successful from the start.
None of the three presenters have any financial disclosures.
Using Data to Inform Quality Improvement
Wednesday, 8:40-9:40 a.m.
Crystal Ballroom G1/A&B
Measuring and analyzing data is essential for any quality improvement project. Data can validate whether an anecdotal assumption indicates the need for a quality improvement initiative and can help showcase the success of any intervention.
At today’s session, “Using Data to Inform Quality Improvement,” attendees will learn how to develop balanced metrics for quality improvement projects, understand distinctions between quality improvement and traditional research projects, and identify how different measures of the same data can tell vastly different stories.
The session will be divided into three 20-minute sections. Ethan Kuperman, MD, MSc, FHM, clinical assistant professor, University of Iowa Health Care, Iowa City, will begin by discussing how to develop balanced metrics by exploring a venous thromboembolism prophylaxis quality improvement project.
Next, Aparna Kamath, MD, MS, SFHM, assistant professor and academic hospitalist, Duke University Health System, Durham, N.C., will demonstrate the distinction between quality improvement and research by exploring medication reconciliation. “I will also emphasize the need for feasibility and rigor in data gathering and analysis in addition to accuracy when doing a quality improvement project,” she said. “Our workshop will make these tasks less daunting for hospitalists doing quality improvement projects.”
Finally, Justin Glasgow, MD, PhD, inpatient medicine faculty and Value Institute senior clinical scholar, Christiana Care Health System, Newark, Del., will explore how improper data definitions led to differing interpretations while developing and deploying an early warning system. “Attendees will learn how to design a quality improvement project to ensure that they measure interventions in a manner that ensures they have had true success, while not creating any unintended consequences,” Dr. Glasgow said.
“The session is important as it will help attendees develop successful projects that their colleagues will respect and that their bosses will admire,” added Dr. Glasgow. “They will gain confidence to turn their experience into distributable scholarship.”
“Hospitalists at all stages of their careers can benefit from this presentation,” Dr. Kuperman said. “Whether you’re preparing for your first quality improvement project or getting ready for a systemwide redesign, collecting the wrong data or misusing collected data can ruin your results or lead you to the wrong conclusions.”
Each of the three presenters are well versed on the topic and have successfully analyzed data for numerous quality improvement projects and presented these data both in publications and in presentations, including for the Society of Hospital Medicine.
“My best qualification for this talk is the number of times I’ve messed up,” Dr. Kuperman said. “Early in my career, I had several projects in which I spent valuable resources creating an initiative, rolling out the implementation, and then wasn’t able to capture reliable outcomes – ruining the chances for scholarship or renewal.”
Through this presentation, Dr. Kuperman hopes that he can reach other hospitalists and soon-to-be hospitalists and teach them some hard-earned lessons so that they can be more successful from the start.
None of the three presenters have any financial disclosures.
Using Data to Inform Quality Improvement
Wednesday, 8:40-9:40 a.m.
Crystal Ballroom G1/A&B
Learn to employ cultural humility
Many health care providers are guilty of having implicit or unconscious biases against patients, which can negatively affect the care they give. “Once providers come to this realization, they can make a conscious effort to neutralize these biases from manifesting throughout a practice,” said Aziz Ansari, DO, SFHM, associate chief medical officer, Clinical Optimization and Revenue Integrity, and associate professor of medicine, Loyola University Medical Center, Maywood, Ill., who will present today’s session “Winning Hearts and Minds at the Bedside: Battling Unconscious Bias Through Cultural Humility.”
By practicing cultural humility, hospitalists can gain trust from patients and their families, whom they do not know in their everyday practice. This encourages providers to be humble, ascertain what is important to the patient, and learn from every patient encounter.
The session will begin with a case study involving bias, followed by a self-reflection exercise. To determine whether you may be biased against some patient groups, Dr. Ansari recommends taking the online implicit association test at Implicit.harvard.edu.
As a palliative care specialist, Dr. Ansari has repeatedly faced situations in which a lack of cultural humility caused patients or their family member to foster mistrust toward a provider. Consequently, patients and family members may choose aggressive measures that providers might consider futile.
Dr. Ansari also will define what implicit or unconscious biases entail in greater detail. The discussion will then circle back to the original case and reveal how providers can improve their mindset when facing difficult situations by employing a tool called “The 5 Rs of Cultural Humility,” which include reflection, respect, regard, relevance, and resiliency.
Dr. Ansari spearheaded the development of the 5 Rs tool when he chaired the Cultural Humility Workgroup of SHM’s Practice Management Committee. “The goal is to use the tool to attain cultural humility and transform a potentially negative encounter into a gratifying one,” he said.
At a minimum, attendees should take time during the session to reflect on their own thoughts and biases. “This introspection can bring to light practices that providers may have been unaware of and, ultimately, can change their behaviors so every patient and their family feels that they are being seen and heard,” Dr. Ansari said. “In today’s current climate it is more important than ever for providers to self-reflect on their attitudes and perceptions because an increasing number of groups in our diverse society are feeling more marginalized.”
Winning Hearts and Minds at the Bedside: Battling Unconscious Bias Through Cultural Humility
Wednesday, 9:10-9:50 a.m.
Crystal Ballroom G2/C-F
Many health care providers are guilty of having implicit or unconscious biases against patients, which can negatively affect the care they give. “Once providers come to this realization, they can make a conscious effort to neutralize these biases from manifesting throughout a practice,” said Aziz Ansari, DO, SFHM, associate chief medical officer, Clinical Optimization and Revenue Integrity, and associate professor of medicine, Loyola University Medical Center, Maywood, Ill., who will present today’s session “Winning Hearts and Minds at the Bedside: Battling Unconscious Bias Through Cultural Humility.”
By practicing cultural humility, hospitalists can gain trust from patients and their families, whom they do not know in their everyday practice. This encourages providers to be humble, ascertain what is important to the patient, and learn from every patient encounter.
The session will begin with a case study involving bias, followed by a self-reflection exercise. To determine whether you may be biased against some patient groups, Dr. Ansari recommends taking the online implicit association test at Implicit.harvard.edu.
As a palliative care specialist, Dr. Ansari has repeatedly faced situations in which a lack of cultural humility caused patients or their family member to foster mistrust toward a provider. Consequently, patients and family members may choose aggressive measures that providers might consider futile.
Dr. Ansari also will define what implicit or unconscious biases entail in greater detail. The discussion will then circle back to the original case and reveal how providers can improve their mindset when facing difficult situations by employing a tool called “The 5 Rs of Cultural Humility,” which include reflection, respect, regard, relevance, and resiliency.
Dr. Ansari spearheaded the development of the 5 Rs tool when he chaired the Cultural Humility Workgroup of SHM’s Practice Management Committee. “The goal is to use the tool to attain cultural humility and transform a potentially negative encounter into a gratifying one,” he said.
At a minimum, attendees should take time during the session to reflect on their own thoughts and biases. “This introspection can bring to light practices that providers may have been unaware of and, ultimately, can change their behaviors so every patient and their family feels that they are being seen and heard,” Dr. Ansari said. “In today’s current climate it is more important than ever for providers to self-reflect on their attitudes and perceptions because an increasing number of groups in our diverse society are feeling more marginalized.”
Winning Hearts and Minds at the Bedside: Battling Unconscious Bias Through Cultural Humility
Wednesday, 9:10-9:50 a.m.
Crystal Ballroom G2/C-F
Many health care providers are guilty of having implicit or unconscious biases against patients, which can negatively affect the care they give. “Once providers come to this realization, they can make a conscious effort to neutralize these biases from manifesting throughout a practice,” said Aziz Ansari, DO, SFHM, associate chief medical officer, Clinical Optimization and Revenue Integrity, and associate professor of medicine, Loyola University Medical Center, Maywood, Ill., who will present today’s session “Winning Hearts and Minds at the Bedside: Battling Unconscious Bias Through Cultural Humility.”
By practicing cultural humility, hospitalists can gain trust from patients and their families, whom they do not know in their everyday practice. This encourages providers to be humble, ascertain what is important to the patient, and learn from every patient encounter.
The session will begin with a case study involving bias, followed by a self-reflection exercise. To determine whether you may be biased against some patient groups, Dr. Ansari recommends taking the online implicit association test at Implicit.harvard.edu.
As a palliative care specialist, Dr. Ansari has repeatedly faced situations in which a lack of cultural humility caused patients or their family member to foster mistrust toward a provider. Consequently, patients and family members may choose aggressive measures that providers might consider futile.
Dr. Ansari also will define what implicit or unconscious biases entail in greater detail. The discussion will then circle back to the original case and reveal how providers can improve their mindset when facing difficult situations by employing a tool called “The 5 Rs of Cultural Humility,” which include reflection, respect, regard, relevance, and resiliency.
Dr. Ansari spearheaded the development of the 5 Rs tool when he chaired the Cultural Humility Workgroup of SHM’s Practice Management Committee. “The goal is to use the tool to attain cultural humility and transform a potentially negative encounter into a gratifying one,” he said.
At a minimum, attendees should take time during the session to reflect on their own thoughts and biases. “This introspection can bring to light practices that providers may have been unaware of and, ultimately, can change their behaviors so every patient and their family feels that they are being seen and heard,” Dr. Ansari said. “In today’s current climate it is more important than ever for providers to self-reflect on their attitudes and perceptions because an increasing number of groups in our diverse society are feeling more marginalized.”
Winning Hearts and Minds at the Bedside: Battling Unconscious Bias Through Cultural Humility
Wednesday, 9:10-9:50 a.m.
Crystal Ballroom G2/C-F
Aim to achieve ‘zero harm’
“Zero harm” refers to the concept of not having any patients harmed as a result of their interactions with a health care system. For example, no laboratory results are misread or overlooked, no medication errors occur, a patient is not misdiagnosed, and a patient does not fall or get an infection.
As clinicians work to improve quality and safety for patients, some have been able to reach the ideal concept of zero harm.
“But the goal of zero harm should become everyone’s new mantra and, to get there, health care providers need to add new dimensions to their typical quality improvement and patient safety efforts,” said Karyn D. Baum, MD, MSEd, MHA, associate chief medical officer, University of Minnesota, Minneapolis, who will speak during the session “Aiming for Zero Preventable Harm.”
Dr. Baum said the interactive lecture, which she will present with MaryEllen Pfeiffer, DO, SFHM, director of patient safety, WellSpan Health, York, Pa., is designed to review the concept of zero harm. The duo will discuss what this goal entails and explain the skills and concepts that providers need to implement at their sites.
Many of these, which are needed to achieve zero harm, are similar to those already employed in quality improvement efforts, such as employing a plan-do-study-act cycle. To achieve zero harm, however, providers must relentlessly execute all of these efforts. In addition, newer concepts, such as more hospital board involvement in safety, need to be woven into previous concepts for health systems to reach this goal.
“When looking to achieve zero patient harm, look through the lens of operations and care delivery; it will become clear what changes need to be made in order to reach that goal,” Dr. Baum said.
Dr. Baum is a speaker for Boehringer Ingelheim on transitions of care and a consultant for Excelsior HealthCare Group.
Aiming for Zero Preventable Harm
Tues., 2:50-3:50 p.m.
Crystal Ballroom G1/A&B
“Zero harm” refers to the concept of not having any patients harmed as a result of their interactions with a health care system. For example, no laboratory results are misread or overlooked, no medication errors occur, a patient is not misdiagnosed, and a patient does not fall or get an infection.
As clinicians work to improve quality and safety for patients, some have been able to reach the ideal concept of zero harm.
“But the goal of zero harm should become everyone’s new mantra and, to get there, health care providers need to add new dimensions to their typical quality improvement and patient safety efforts,” said Karyn D. Baum, MD, MSEd, MHA, associate chief medical officer, University of Minnesota, Minneapolis, who will speak during the session “Aiming for Zero Preventable Harm.”
Dr. Baum said the interactive lecture, which she will present with MaryEllen Pfeiffer, DO, SFHM, director of patient safety, WellSpan Health, York, Pa., is designed to review the concept of zero harm. The duo will discuss what this goal entails and explain the skills and concepts that providers need to implement at their sites.
Many of these, which are needed to achieve zero harm, are similar to those already employed in quality improvement efforts, such as employing a plan-do-study-act cycle. To achieve zero harm, however, providers must relentlessly execute all of these efforts. In addition, newer concepts, such as more hospital board involvement in safety, need to be woven into previous concepts for health systems to reach this goal.
“When looking to achieve zero patient harm, look through the lens of operations and care delivery; it will become clear what changes need to be made in order to reach that goal,” Dr. Baum said.
Dr. Baum is a speaker for Boehringer Ingelheim on transitions of care and a consultant for Excelsior HealthCare Group.
Aiming for Zero Preventable Harm
Tues., 2:50-3:50 p.m.
Crystal Ballroom G1/A&B
“Zero harm” refers to the concept of not having any patients harmed as a result of their interactions with a health care system. For example, no laboratory results are misread or overlooked, no medication errors occur, a patient is not misdiagnosed, and a patient does not fall or get an infection.
As clinicians work to improve quality and safety for patients, some have been able to reach the ideal concept of zero harm.
“But the goal of zero harm should become everyone’s new mantra and, to get there, health care providers need to add new dimensions to their typical quality improvement and patient safety efforts,” said Karyn D. Baum, MD, MSEd, MHA, associate chief medical officer, University of Minnesota, Minneapolis, who will speak during the session “Aiming for Zero Preventable Harm.”
Dr. Baum said the interactive lecture, which she will present with MaryEllen Pfeiffer, DO, SFHM, director of patient safety, WellSpan Health, York, Pa., is designed to review the concept of zero harm. The duo will discuss what this goal entails and explain the skills and concepts that providers need to implement at their sites.
Many of these, which are needed to achieve zero harm, are similar to those already employed in quality improvement efforts, such as employing a plan-do-study-act cycle. To achieve zero harm, however, providers must relentlessly execute all of these efforts. In addition, newer concepts, such as more hospital board involvement in safety, need to be woven into previous concepts for health systems to reach this goal.
“When looking to achieve zero patient harm, look through the lens of operations and care delivery; it will become clear what changes need to be made in order to reach that goal,” Dr. Baum said.
Dr. Baum is a speaker for Boehringer Ingelheim on transitions of care and a consultant for Excelsior HealthCare Group.
Aiming for Zero Preventable Harm
Tues., 2:50-3:50 p.m.
Crystal Ballroom G1/A&B
Practical changes for improving practice management
An all-day HM18 pre-course – “Hospitalist Practice Management: How to Thrive in a Time of Intense Change” – for hospitalist leaders and practice administrators was all about practicality.
One of the goals of the session was to provide “quick, actionable interventions that attendees can implement right away, as well as alternatives for attendees to consider, which will require some work to employ,” said John Nelson, MD, MHM, a partner at Nelson Flores Hospital Medicine Consultants, La Quinta, Calif., the medical director of the Overlake Medical Center, Bellevue, Wash., and a course codirector and a faculty presenter.
Dr. Nelson pointed out that the hospitalist practice is a unique practice model. “We can’t effectively use the same approaches that other medical specialties use to ensure we have successful practices,” he said.
The pre-course, held Sunday before the official start of HM18, included more commentary and specifics than in past years about how to prosper in the rapidly changing health care landscape and how to reduce the chance of burnout.
Topics addressed included how to find, measure, and demonstrate value; how to incorporate different types of providers and clinical support staffing into a practice to support hospitalists; and how to recruit the right people and build a desirable culture.
The pre-course also covered effective roles for a variety of providers in a hospitalist group, including nurses, scribes, and coordinators, and delineated the benefits of providing telemedicine.
For group leaders and administrators in attendance, the session also shed light on how to interact with individual providers in their group and how to collaborate to build a healthy culture and practice, Ms. Flores said.
The day began with presentations that laid out valuable information and frameworks, including “A Tour of Survey Data: What It Does and Doesn’t Tell You” and “Defining and Measuring Value.” Sessions included six didactic lectures with a question-and-answer period, as well as what Dr. Nelson has dubbed “point/counterpoint” sessions in which faculty members debated particular issues, such as work scheduling models. During the last session, “Learning From Each Other,” participants shared with other attendees their own best practices in the areas covered.
Although there is no single best way to organize a hospitalist’s practice, the course provided lots of information and perspective to help listeners decide what is best for their practice.
“Even though we work in a stressful environment of constant change, hospitalists do have some control over their destiny, and there are things they can do to make hospitalist groups thrive in this challenging environment,” Ms. Flores concluded.
An all-day HM18 pre-course – “Hospitalist Practice Management: How to Thrive in a Time of Intense Change” – for hospitalist leaders and practice administrators was all about practicality.
One of the goals of the session was to provide “quick, actionable interventions that attendees can implement right away, as well as alternatives for attendees to consider, which will require some work to employ,” said John Nelson, MD, MHM, a partner at Nelson Flores Hospital Medicine Consultants, La Quinta, Calif., the medical director of the Overlake Medical Center, Bellevue, Wash., and a course codirector and a faculty presenter.
Dr. Nelson pointed out that the hospitalist practice is a unique practice model. “We can’t effectively use the same approaches that other medical specialties use to ensure we have successful practices,” he said.
The pre-course, held Sunday before the official start of HM18, included more commentary and specifics than in past years about how to prosper in the rapidly changing health care landscape and how to reduce the chance of burnout.
Topics addressed included how to find, measure, and demonstrate value; how to incorporate different types of providers and clinical support staffing into a practice to support hospitalists; and how to recruit the right people and build a desirable culture.
The pre-course also covered effective roles for a variety of providers in a hospitalist group, including nurses, scribes, and coordinators, and delineated the benefits of providing telemedicine.
For group leaders and administrators in attendance, the session also shed light on how to interact with individual providers in their group and how to collaborate to build a healthy culture and practice, Ms. Flores said.
The day began with presentations that laid out valuable information and frameworks, including “A Tour of Survey Data: What It Does and Doesn’t Tell You” and “Defining and Measuring Value.” Sessions included six didactic lectures with a question-and-answer period, as well as what Dr. Nelson has dubbed “point/counterpoint” sessions in which faculty members debated particular issues, such as work scheduling models. During the last session, “Learning From Each Other,” participants shared with other attendees their own best practices in the areas covered.
Although there is no single best way to organize a hospitalist’s practice, the course provided lots of information and perspective to help listeners decide what is best for their practice.
“Even though we work in a stressful environment of constant change, hospitalists do have some control over their destiny, and there are things they can do to make hospitalist groups thrive in this challenging environment,” Ms. Flores concluded.
An all-day HM18 pre-course – “Hospitalist Practice Management: How to Thrive in a Time of Intense Change” – for hospitalist leaders and practice administrators was all about practicality.
One of the goals of the session was to provide “quick, actionable interventions that attendees can implement right away, as well as alternatives for attendees to consider, which will require some work to employ,” said John Nelson, MD, MHM, a partner at Nelson Flores Hospital Medicine Consultants, La Quinta, Calif., the medical director of the Overlake Medical Center, Bellevue, Wash., and a course codirector and a faculty presenter.
Dr. Nelson pointed out that the hospitalist practice is a unique practice model. “We can’t effectively use the same approaches that other medical specialties use to ensure we have successful practices,” he said.
The pre-course, held Sunday before the official start of HM18, included more commentary and specifics than in past years about how to prosper in the rapidly changing health care landscape and how to reduce the chance of burnout.
Topics addressed included how to find, measure, and demonstrate value; how to incorporate different types of providers and clinical support staffing into a practice to support hospitalists; and how to recruit the right people and build a desirable culture.
The pre-course also covered effective roles for a variety of providers in a hospitalist group, including nurses, scribes, and coordinators, and delineated the benefits of providing telemedicine.
For group leaders and administrators in attendance, the session also shed light on how to interact with individual providers in their group and how to collaborate to build a healthy culture and practice, Ms. Flores said.
The day began with presentations that laid out valuable information and frameworks, including “A Tour of Survey Data: What It Does and Doesn’t Tell You” and “Defining and Measuring Value.” Sessions included six didactic lectures with a question-and-answer period, as well as what Dr. Nelson has dubbed “point/counterpoint” sessions in which faculty members debated particular issues, such as work scheduling models. During the last session, “Learning From Each Other,” participants shared with other attendees their own best practices in the areas covered.
Although there is no single best way to organize a hospitalist’s practice, the course provided lots of information and perspective to help listeners decide what is best for their practice.
“Even though we work in a stressful environment of constant change, hospitalists do have some control over their destiny, and there are things they can do to make hospitalist groups thrive in this challenging environment,” Ms. Flores concluded.