User login
Patients with challenging behaviors: Communication strategies
From time to time, all physicians encounter patients whose behavior evokes negative emotions. In 1978, in an article titled “Taking care of the hateful patient,”1 Groves detailed 4 types of patients—“dependent clingers, entitled demanders, manipulative help-rejecters, and self-destructive deniers”1—that even the most seasoned physicians dread, and provided suggestions for managing interactions with them. The topic was revisited and updated in 2006 by Strous et al.2
Now, more than 10 years later, the challenge of how to interact with difficult patients is more relevant than ever. A cultural environment in which every patient can become an “expert” via the Internet has added new challenges. Patients who are especially time-consuming and emotionally draining exacerbate the many other pressures physicians face today (eg, increased paperwork, cost-consciousness, shortened appointment times, and the move to electronic medical records), contributing to physician burnout.
This article further updates the topic of managing challenging patients to reflect the current practice climate. We provide a more modern view of challenging patients and provide guidance on handling them. Although it may be tempting to diagnose some of these patients as having a personality disorder, it can often be more helpful to recognize patterns of behavior and have a clear plan for management. We also discuss general coping strategies for avoiding physician burnout.
INTERNET-SEEKING, QUESTIONING
A 45-year-old man carries in an overstuffed briefcase for his first primary care visit. He is a medical editor for a national journal and recently worked on a case study involving a rare cancer. As he edited, he recognized that he had the same symptoms and diagnosed himself with the same disease. He has brought with him a sheaf of articles he found on the Internet detailing clinical trials for experimental treatments. When the doctor begins to ask questions, he says the answers are irrelevant: he explains that he would have gone straight to an oncologist, but his insurance policy requires that he also have a primary care physician. He now expects the doctor to order magnetic resonance imaging, refer him to an oncologist, and support his request for the treatment he has identified as best.
The Internet: A blessing and a curse
Patients now have access to enormous amounts of information of variable accuracy. As in this case, patients may come to an appointment carrying early research studies that the physician has not yet reviewed. Others get their information from patient blogs that frequently offer opinions without evidence. Often, based on an advertisement or Internet reading, a patient requests a particular medication or test that may not be cost-effective or medically justified.
In a survey more than 10 years ago, more than 75% of physicians reported that they had patients who brought in information from online sources.3 Hu et al4 reported that 70% of patients who had online information planned to discuss it with their physicians. This practice is only growing, including in older patients.5
Physicians may feel confused and frustrated by patients who come armed with information. They may infer that patients do not trust them to diagnose correctly or treat optimally. In addition, discussing such information takes time, causing others on the schedule to wait, adding to the stress of coping with over-booked appointments.
Why so overprepared?
Patients who have or fear that they have cancer may be particularly worried that an important treatment will be overlooked.6 Since they feel that their life is hanging in the balance, their search for a definitive cure is understandable.
Internet-seeking, intensely questioning patients clearly want more information about the treatments they are receiving, alternative medical or procedural options, and complementary therapies.7 The response to their desire for more information affects their impression of physician empathy.8
Adapting to a more informed patient
Approaching these patients as an opportunity to educate may result in a more trusting patient and one more likely to be open to physician guidance and more likely to adhere to an advised treatment plan. Triangulation of the 3 actors—the physician, the patient, and the Web—can help patients to make more-informed choices and foster an attitude of partnership with the physician to lead them to optimal healthcare.
In a review of the impact of Internet use on healthcare and the physician-patient relationship, Wald et al9 urged physicians to:
- Adopt a positive attitude toward discussing Internet contributions
- Encourage patients to take an active role in maintaining health
- Acknowledge patient concerns and fears
- Avoid becoming defensive
- Recommend credible Internet sources.
Laing et al10 urged physicians to recognize rather than deny the effects of patients’ online searching for information and support, and not to ignore the potential impact on treatment. Consumers are gaining autonomy and self-efficacy, and Laing et al encouraged healthcare providers to develop ways to incorporate this new reality into the services they provide.10
How Web-based interaction can assist in patient decision-making for colorectal cancer screening is being explored.11 Patients at home can use an online tool to learn about screening choices and would be more knowledgable and comfortable discussing the options with their care provider. The hope is to build in an automatic reminder for the clinician, who would better understand the patient’s preference before the office visit.
One approach to our patient is to say, “I can see how worried you are about having the same type of cancer you read about, and I want to help you. It is clear to me that you know a lot about healthcare, and I appreciate your engagement in your health. How about starting over? Let me ask a few questions so I can get a better perspective on your symptoms?” Many times, this strategy can help patients reframe their view and accept help.
DEMANDING, LITIGATION-THREATENING
A 60-year-old lawyer is admitted to the hospital for evaluation of abdominal pain. His physician recommends placing a nasogastric tube to provide nutrition while the evaluation is completed. His wife, a former nurse practitioner, insists that a nasogastric tube would be too dangerous and demands that he be allowed to eat instead. The couple declares the primary internal medicine physician incompetent, does not want any residents to be involved in his care, and antagonizes the nurses with constant demands. Soon, the entire team avoids the patient’s room.
Why so hostile?
People with demanding behavior often have a hostile and confrontational manner. They may use medical jargon and appear to believe that they know more than their healthcare team. Many demand to know why they have not been offered a particular test, diagnosis, or treatment, especially if they or a family member has a healthcare background. Such patients appear to feel that they are being treated incorrectly and leave us feeling vulnerable, wondering whether the patient might one day come back to haunt us with a lawsuit, especially if the medical outcome is unfavorable.
Understanding the motivation for the behavior can help a physician to empathize with the demanding patient.12 Although it may seem that the demanding patient is trying to intimidate the physician, the goal is usually the same: to find the best possible treatment. Anger and hostility are often motivated by fear and a sense of losing control.
Ironically, this maladaptive coping style may alienate the very people who can help the patient. Hostile behavior evokes defensiveness and resentment in others. A power struggle may ensue: as the patient makes more unreasonable demands and threats, the physician reacts by asserting his or her views in an attempt to maintain control. Or the physician and the rest of the healthcare team may simply avoid the patient as much as possible.
Collaboration can defuse anger
The best strategy is often to steer the encounter away from a power struggle by legitimizing the patient’s feeling of entitlement to the best possible treatment.13 Take a collaborative stance with the patient, with the common goal of finding and implementing the most effective and lowest-risk diagnostic and treatment plan. Empathy and exploration of the patient’s concerns are always in order.
Physicians can try several strategies to improve interactions with demanding patients and caregivers:
Be consistent. All members of the healthcare team, including nurses and specialists, should convey consistent messages regarding diagnostic testing and treatment plans.
Don’t play the game. Demanding patients often complain about being mistreated by other healthcare providers. When confronted with such complaints, acknowledge the patient’s feelings while refraining from blaming or criticizing other members of the healthcare team.
Clarify expectations. Clarifying expectations from the initial patient encounter can prevent conflicts later. Support a patient who must accept a diagnosis of a terminal illness, and then when appropriate, discuss goals moving forward. Collaboration within the framework of reasonable expectations is key.
For our case, the physician could say, “We want to work with you together as a team. We will work hard to address your concerns, but our nurses must have a safe environment in which to help you.” Such a statement highlights shared goals and expression of concern without judgment. The next step is to clarify expectations by describing the hospital routine and how decisions are made.
Offer choices. Offering choices whenever possible can help a demanding patient feel more in control. Rather than dismiss a patient’s ideas, explore the alternatives. While effective patient communication is preferable to repeated referrals to specialists,14 judicious referral can engender trust in the physician’s competence if a diagnosis is not forthcoming.15
A unique challenge in teaching hospitals is the patient who refuses to interact with residents and students. It is best to acknowledge the patient’s concerns and offer alternative options:
- If the patient is worried about lack of completed training, then clarify the residents’ roles and reassure the patient that you communicate with residents and supervisors regarding any clinical decisions
- If possible, offer to see the patient alone or have the resident interact only on an as-needed basis
- Consider transferring the patient to a nonteaching service or to another hospital.
Admit failings. Although not easy, admitting to and apologizing for things that have gone wrong can help to calm a demanding patient and even reduce the likelihood of a lawsuit.16 The physician should not convey defensiveness and instead should acknowledge the limitations of the healthcare system.
Legitimize concerns—to an extent. Legitimizing a demanding patient’s concerns is important, but never be bullied into taking actions that create unnecessary risk. Upsetting a demanding patient is better than ordering tests or providing treatments that are potentially harmful. Good physician-patient communication can go a long way toward preventing adverse outcomes.
CONSTANTLY SEEKING REASSURANCE
A 25-year-old professional presents to a new primary care provider concerned about a mole on her back. She discusses her sun exposure and family history of skin cancer and produces photographs documenting changes in the mole over time. Impressed with this level of detail, the physician takes time to explain his concerns before referring her to a dermatologist. Later that day, she calls to let the doctor know that her procedure has been scheduled and to thank him for his care. A few weeks after the mole is removed, she returns to discuss treatment options for the small remaining scar.
After this appointment, she calls the office repeatedly with a wide array of concerns, including an isolated symptom of fatigue that could indicate cancer and the relative merits of different sunscreens. She also sends the physician frequent e-mail messages through the personal health record system with pictures of inconsequential marks on her skin.
Needing reassurance is normal—to a point
Many patients seek reassurance from their physicians, and this can be done in a healthy and respectful manner. But requests for reassurance may escalate to becoming repeated, insistent, and even aggressive.1 This can elicit reactions from physicians ranging from feeling annoyed and burdened to feeling angry and overwhelmed.17 This can lead to significant stress, which, if not managed well, can lead to excessively control of physician behavior and substandard care.18
Reassurance-seeking behavior can manifest anywhere along the spectrum of health and disease.19 It may be a symptom of health anxiety (ie, an exaggerated fear of illness) or hypochondria (ie, the persistent conviction that one is currently or likely to become ill).20,21
Why so needy?
Attachment theory may help explain neediness. Parental bonding during childhood is associated with mental and physical health and health-related behaviors in adults.22,23 People with insecure-preoccupied attachment styles tend to be overly emotionally dependent on the acceptance of others and may exhibit dependent and care-seeking behaviors with a physician.24
Needy patients are often genuinely grateful for the care and attention from a physician.1 In the beginning, the doctor may appreciate the patient’s validation of care provided, but this positive feeling wanes as calls and requests become incessant. As the physician’s exhaustion increases with each request, the care and well-being of the patient may no longer be the primary focus.1
Set boundaries
Be alert to signs that a patient is crossing the line to an unhealthy need for reassurance. Address medical concerns appropriately, then institute clear guidelines for follow-up, which should be reinforced by the entire care team if necessary.22
The following strategies can be useful for defining boundaries:
- Instruct the patient to come to the office only for scheduled follow-up visits and to call only during office hours or in an emergency
- Be up-front about the time allowed for each appointment and ask the patient to help focus the discussion according to his or her main concerns25
- Consider telling the patient, “You seem really worried about a lot of physical symptoms. I want to reassure you that I find no evidence of a medical illness that would require intervention. I am concerned about your phone calls and e-mails, and I wonder what would be helpful at this point to address your concerns?”
- Consider treating the patient for anxiety.
It is important to remain responsive to all types of patient concerns. Setting boundaries will guide patients to express health concerns in an appropriate manner so that they can be heard and managed.18,19
SELF-INJURY
A 22-year-old woman presents to the emergency department complaining of abdominal pain. After a full workup, the physician clears her medically and orders a few laboratory tests. As the nurse draws blood samples, she notices multiple fresh cuts on the patient’s arm and informs the physician. The patient is questioned and examined again and acknowledges occasional thoughts of self-harm.
Her parents arrive and appear appropriately concerned. They report that she has been “cutting” for 4 years and is regularly seeing a therapist. However, they say that they are not worried for her safety and that she has an appointment with her therapist this week. Based on this, the emergency department physician discharges her.
Two weeks later, the patient returns to the emergency department with continued cutting and apparent cellulitis, prompting medical admission.
Self-injury presents in many ways
Self-injurious behaviors come in many forms other than the easily recognized one presented in this case: eg, a patient with cirrhosis who continues to drink, a patient with severe epilepsy who forgets to take medications and lands in the emergency department every week for status epilepticus, a patient with diabetes who eats a high-sugar diet, a patient with renal insufficiency who ignores water restrictions, or a patient with an organ transplant who misses medications and relapses.
There is an important psychological difference between patients who knowingly continue to challenge their luck and those who do not fully understand the severity of their condition and the consequences of their actions. The patient who simply does not “get it” can sometimes be managed effectively with education and by working with family members to create an environment to facilitate critical healthy behaviors.
Patients who willfully self-inflict injury are asking for help while doing everything to avoid being helped. They typically come to the office or the emergency department with assorted complaints, not divulging the real reason for their visit until the last minute as they are leaving. Then they drop a clue to the real concern, leaving the physician confused and frustrated.
Why deny an obvious problem?
Fear of the stigma of mental illness can be a major barrier to full disclosure of symptoms of psychological distress, and this especially tends to be the case for patients from some ethnic minorities.26
On the other hand, patients with borderline or antisocial personality disorder (and less often, schizotypal or narcissistic personality disorder) frequently use denial as their primary psychological defense. Self-destructive denial is sometimes associated with traumatic memories, feelings of worthlessness, or a desire to reduce self-awareness and rationalize harmful behaviors. Such patients usually need lengthy treatment, and although the likelihood of cure is low, therapy can be helpful.27–29
Lessons from psychiatry
It can be difficult to maintain empathy for patients who intentionally harm themselves. It is helpful to think of these patients as having a terminal illness and to recognize that they are suffering.
Different interventions have been studied for such patients. Dialectical behavior therapy, an approach that teaches patients better coping skills for regulating emotions, can help reduce maladaptive emotional distress and self-destructive behaviors.30–32 Lessons from this approach can be applied by general practitioners:
- Engage the patient and together establish an effective crisis management plan
- With patient permission, involve the family in the treatment plan
- Set clear limits about self-harm: once the patient values interaction with the doctor, he or she will be less likely to break the agreement.
Patients with severe or continuing issues can be referred to appropriate services that offer dialectical behavior therapy or other intensive outpatient programs.
To handle our patient, one might start by saying, “I am sorry to see you back in the ER. We need to treat the cellulitis and get your outpatient behavioral team on board, so we know the plan.” Then, it is critical that the entire team keep to that plan.
HOW TO STAY IN CONTROL AND IMPROVE INTERACTIONS
Patients with challenging behaviors will always be part of medical practice. Physicians should be aware of their reactions and feelings towards a patient (known in psychiatry as countertransference), as they can increase physician stress and interfere with providing optimal care. Finding effective ways to work with difficult patients will avoid these outcomes.
Physicians also feel loss of control
Most physicians are resilient, but they can feel overwhelmed under certain circumstances. According to Scudder and Shanafelt,33 a physician’s sense of well-being is influenced by several factors, including feelings of control in the workplace. It is easy to imagine how one or more difficult patients can create a sense of overwhelming demand and loss of control.
These tips can help maintain a sense of control and improve interactions with patients:
Have a plan for effective communication. Not having a plan for communicating in a difficult situation can contribute to loss of control in a hectic schedule that is already stretched to its limits. Practicing responses with a colleague for especially difficult patients or using a team approach can be helpful. Remaining compassionate while setting boundaries will result in the best outcome for the patient and physician.
Stop to analyze the situation. One of the tenets of cognitive-behavioral therapy is recognizing that negative thoughts can quickly take us down a dangerous path. Feeling angry and resentful without stopping to think and reflect on the causes can lead to the physician feeling victimized (just like many difficult patients feel).
It is important to step back and think, not just feel. While difficult patients present in different ways, all are reacting to losing control of their situation and want support. During a difficult interaction with a patient, pause to consider, “Why is he behaving this way? Is he afraid? Does he feel that no one cares?”
When a patient verbally attacks beyond what is appropriate, recognize that this is probably due less to anything the physician did than to the patient’s internal issues. Identifying the driver of a patient’s behavior makes it easier to control our own emotions.
Practice empathy. Difficult patients usually have something in their background that can help explain their inappropriate behavior, such as a lack of parental support or abuse. Being open to hearing their story facilitates an empathetic connection.
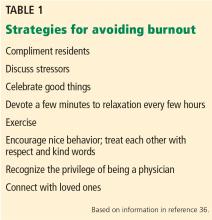
AVOIDING BURNOUT
Discuss problems
Sadly, physicians often neglect to talk with each other and with trainees about issues leading to burnout, thereby missing important opportunities for empathy, objectivity, reflection, and teaching moments.
Lessons can be gleaned from training in psychiatry, a field in which one must learn methods for working effectively in challenging situations. Dozens of scenarios are practiced using videotapes or observation through one-way mirrors. While not everyone has such opportunities, everyone can discuss issues with one another. Regularly scheduled facilitated groups devoted to discussing problems with colleagues can be enormously helpful.
Schedule quiet times
Mindfulness is an excellent way to spend a few minutes out of every 3- to 4-hour block. There are many ways to help facilitate such moments. Residents and students can be provided with a small book, Mindfulness on the Go,37 aimed for the busy person.
Deep, slow breathing can bring rapid relief to intense negative feelings. Not only does it reduce anxiety faster than medication, but it is also free, is easily taught to others, and can be done unobtrusively. A short description of the role of the blood pH in managing the locus ceruleus and vagus nerve’s balance of sympathetic and parasympathetic activity may capture the curiosity of someone who may otherwise be resistant to the exercise.
Increasingly, hospitals are developing mindfulness sessions and offering a variety of skills physicians can put into their toolbox. Lessons from cognitive-behavioral therapy, dialectical behavior therapy, imagery, and muscle relaxation can help physicians in responding to patients. Investing in communication skills training specific to challenging behaviors seen in different specialties better equips physicians with more effective strategies.
- Groves JE. Taking care of the hateful patient. N Engl J Med 1978; 298:883–887.
- Strous RD, Ulman AM, Kotler M. The hateful patient revisited: relevance for 21st century medicine. Eur J Intern Med 2006; 17:387–393.
- Malone M, Mathes L, Dooley J, While AE. Health information seeking and its effect on the doctor-patient digital divide. J Telemed Telecare 2005; 11(suppl1):25–28.
- Hu X, Bell RA, Kravitz RL, Orrange S. The prepared patient: information seeking of online support group members before their medical appointments. J Health Commun 2012; 17:960–978.
- Tse MM, Choi KC, Leung RS. E-health for older people: the use of technology in health promotion. Cyberpsychol Behav 2008; 11:475–479.
- Pereira JL, Koski S, Hanson J, Bruera ED, Mackey JR. Internet usage among women with breast cancer: an exploratory study. Clin Breast Cancer 2000; 1:148–153.
- Brauer JA, El Sehamy A, Metz JN, Mao JJ. Complementary and alternative and supportive care at leading cancer centers: a systematic analysis of websites. J Altern Complement Med 2010; 16:183–186.
- Smith SG, Pandit A, Rush SR, Wolf MS, Simon C. The association between patient activation and accessing online health information: results from a national survey of US adults. Health Expect 2015; 18:3262–3273.
- Wald HS, Dube CE, Anthony DC. Untangling the Web—the impact of Internet use on health care and the physician-patient relationship. Patient Educ Couns 2007; 68:218–224.
- Laing A, Hogg G, Winkelman D. Healthcare and the information revolution: re-configuring the healthcare service encounter. Health Serv Manage Res 2004; 17:188–199.
- Jimbo M, Shultz CG, Nease DE, Fetters MD, Power D, Ruffin MT 4th. Perceived barriers and facilitators of using a Web-based interactive decision aid for colorectal cancer screening in community practice settings: findings from focus groups with primary care clinicians and medical office staff. J Med Internet Res 2013; 15:e286.
- Steinmetz D, Tabenkin H. The ‘difficult patient’ as perceived by family physicians. Fam Pract 2001; 18:495–500.
- Arciniegas DB, Beresford TP. Managing difficult interactions with patients in neurology practices: a practical approach. Neurology 2010; 75(suppl 1):S39–S44.
- Gallagher TH, Lo B, Chesney M, Christensen K. How do physicians respond to patient’s requests for costly, unindicated services? J Gen Intern Med 1997; 12:663–668.
- Breen KJ, Greenberg PB. Difficult physician-patient encounters. Intern Med J 2010; 40:682–688.
- Huntington B, Kuhn N. Communication gaffes: a root cause of malpractice claims. Proc (Bayl Univ Med Cent) 2003; 16:157–161.
- Maunder RG, Panzer A, Viljoen M, Owen J, Human S, Hunter JJ. Physicians’ difficulty with emergency department patients is related to patients’ attachment style. Soc Sci Med 2006; 63:552–562.
- Thompson D, Ciechanowski PS. Attaching a new understanding to the patient-physician relationship in family practice. J Am Board Fam Pract 2003; 16:219–226.
- Groves M, Muskin P. Psychological responses to illness. In: Levenson JL, ed. The American Psychiatric Publishing Textbook of Psychosomatic Medicine. Arlington, VA: American Psychiatric Publishing, Inc; 2004:68–88.
- Görgen SM, Hiller W, Witthöft M. Health anxiety, cognitive coping, and emotion regulation: a latent variable approach. Int J Behav Med 2014; 21:364–374.
- Strand J, Goulding A, Tidefors I. Attachment styles and symptoms in individuals with psychosis. Nord J Psychiatry 2015; 69:67–72.
- Hooper LM, Tomek S, Newman CR. Using attachment theory in medical settings: implications for primary care physicians. J Ment Health 2012; 21:23–37.
- Bowlby J. Attachment and loss. 1. Attachment. New York, NY: Basic Books; 1969.
- Fuertes JN, Anand P, Haggerty G, Kestenbaum M, Rosenblum GC. The physician-patient working alliance and patient psychological attachment, adherence, outcome expectations, and satisfaction in a sample of rheumatology patients. Behav Med 2015; 41:60–68.
- Frederiksen HB, Kragstrup J, Dehlholm-Lambertsen B. Attachment in the doctor-patient relationship in general practice: a qualitative study. Scand J Prim Health Care 2010; 28:185–190.
- Rastogi P, Khushalani S, Dhawan S, et al. Understanding clinician perception of common presentations in South Asians seeking mental health treatment and determining barriers and facilitators to treatment. Asian J Psychiatr 2014; 7:15–21.
- van der Kolk BA, Perry JC, Herman JL. Childhood origins of self-destructive behavior. Am J Psychiatry 1991; 148:1665–1671.
- Gacono CB, Meloy JR, Berg JL. Object relations, defensive operations, and affective states in narcissistic, borderline, and antisocial personality disorder. J Pers Assess 1992; 59:32–49.
- Perry JC, Presniak MD, Olson TR. Defense mechanisms in schizotypal, borderline, antisocial, and narcissistic personality disorders. Psychiatry 2013; 76:32–52.
- Gibson J, Booth R, Davenport J, Keogh K, Owens T. Dialectical behaviour therapy-informed skills training for deliberate self-harm: a controlled trial with 3-month follow-up data. Behav Res Ther 2014; 60:8–14.
- Fischer S, Peterson C. Dialectical behavior therapy for adolescent binge eating, purging, suicidal behavior, and non-suicidal self-injury: a pilot study. Psychotherapy (Chic). 2015; 52:78–92.
- Booth R, Keogh K, Doyle J, Owens T. Living through distress: a skills training group for reducing deliberate self-harm. Behav Cogn Psychother 2014; 42:156–165.
- Scudder L, Shanafelt TD. Two sides of the physician coin: burnout and well-being. Medscape. Feb 09, 2015. http://nbpsa.org/images/PRP/PhysicianBurnoutMedscape.pdf. Accessed June 2, 2017.
- McAbee JH, Ragel BT, McCartney S, et al. Factors associated with career satisfaction and burnout among US neurosurgeons: results of a nationwide survey. J Neurosurg 2015; 123:161–173.
- Schneider S, Kingsolver K, Rosdahl J. Can physician self-care enhance patient-centered healthcare? Qualitative findings from a physician well-being coaching program. J Fam Med 2015; 2:6.
- Simonds G, Sotile W. Building Resilience in Neurosurgical Residents: A Primer. B Wright Publishing; 2015.
- Bays JC. Mindfulness on the Go: Simple Meditation Practices You Can Do Anywhere. Boulder, CO: Shambhala Publications; 2014.
From time to time, all physicians encounter patients whose behavior evokes negative emotions. In 1978, in an article titled “Taking care of the hateful patient,”1 Groves detailed 4 types of patients—“dependent clingers, entitled demanders, manipulative help-rejecters, and self-destructive deniers”1—that even the most seasoned physicians dread, and provided suggestions for managing interactions with them. The topic was revisited and updated in 2006 by Strous et al.2
Now, more than 10 years later, the challenge of how to interact with difficult patients is more relevant than ever. A cultural environment in which every patient can become an “expert” via the Internet has added new challenges. Patients who are especially time-consuming and emotionally draining exacerbate the many other pressures physicians face today (eg, increased paperwork, cost-consciousness, shortened appointment times, and the move to electronic medical records), contributing to physician burnout.
This article further updates the topic of managing challenging patients to reflect the current practice climate. We provide a more modern view of challenging patients and provide guidance on handling them. Although it may be tempting to diagnose some of these patients as having a personality disorder, it can often be more helpful to recognize patterns of behavior and have a clear plan for management. We also discuss general coping strategies for avoiding physician burnout.
INTERNET-SEEKING, QUESTIONING
A 45-year-old man carries in an overstuffed briefcase for his first primary care visit. He is a medical editor for a national journal and recently worked on a case study involving a rare cancer. As he edited, he recognized that he had the same symptoms and diagnosed himself with the same disease. He has brought with him a sheaf of articles he found on the Internet detailing clinical trials for experimental treatments. When the doctor begins to ask questions, he says the answers are irrelevant: he explains that he would have gone straight to an oncologist, but his insurance policy requires that he also have a primary care physician. He now expects the doctor to order magnetic resonance imaging, refer him to an oncologist, and support his request for the treatment he has identified as best.
The Internet: A blessing and a curse
Patients now have access to enormous amounts of information of variable accuracy. As in this case, patients may come to an appointment carrying early research studies that the physician has not yet reviewed. Others get their information from patient blogs that frequently offer opinions without evidence. Often, based on an advertisement or Internet reading, a patient requests a particular medication or test that may not be cost-effective or medically justified.
In a survey more than 10 years ago, more than 75% of physicians reported that they had patients who brought in information from online sources.3 Hu et al4 reported that 70% of patients who had online information planned to discuss it with their physicians. This practice is only growing, including in older patients.5
Physicians may feel confused and frustrated by patients who come armed with information. They may infer that patients do not trust them to diagnose correctly or treat optimally. In addition, discussing such information takes time, causing others on the schedule to wait, adding to the stress of coping with over-booked appointments.
Why so overprepared?
Patients who have or fear that they have cancer may be particularly worried that an important treatment will be overlooked.6 Since they feel that their life is hanging in the balance, their search for a definitive cure is understandable.
Internet-seeking, intensely questioning patients clearly want more information about the treatments they are receiving, alternative medical or procedural options, and complementary therapies.7 The response to their desire for more information affects their impression of physician empathy.8
Adapting to a more informed patient
Approaching these patients as an opportunity to educate may result in a more trusting patient and one more likely to be open to physician guidance and more likely to adhere to an advised treatment plan. Triangulation of the 3 actors—the physician, the patient, and the Web—can help patients to make more-informed choices and foster an attitude of partnership with the physician to lead them to optimal healthcare.
In a review of the impact of Internet use on healthcare and the physician-patient relationship, Wald et al9 urged physicians to:
- Adopt a positive attitude toward discussing Internet contributions
- Encourage patients to take an active role in maintaining health
- Acknowledge patient concerns and fears
- Avoid becoming defensive
- Recommend credible Internet sources.
Laing et al10 urged physicians to recognize rather than deny the effects of patients’ online searching for information and support, and not to ignore the potential impact on treatment. Consumers are gaining autonomy and self-efficacy, and Laing et al encouraged healthcare providers to develop ways to incorporate this new reality into the services they provide.10
How Web-based interaction can assist in patient decision-making for colorectal cancer screening is being explored.11 Patients at home can use an online tool to learn about screening choices and would be more knowledgable and comfortable discussing the options with their care provider. The hope is to build in an automatic reminder for the clinician, who would better understand the patient’s preference before the office visit.
One approach to our patient is to say, “I can see how worried you are about having the same type of cancer you read about, and I want to help you. It is clear to me that you know a lot about healthcare, and I appreciate your engagement in your health. How about starting over? Let me ask a few questions so I can get a better perspective on your symptoms?” Many times, this strategy can help patients reframe their view and accept help.
DEMANDING, LITIGATION-THREATENING
A 60-year-old lawyer is admitted to the hospital for evaluation of abdominal pain. His physician recommends placing a nasogastric tube to provide nutrition while the evaluation is completed. His wife, a former nurse practitioner, insists that a nasogastric tube would be too dangerous and demands that he be allowed to eat instead. The couple declares the primary internal medicine physician incompetent, does not want any residents to be involved in his care, and antagonizes the nurses with constant demands. Soon, the entire team avoids the patient’s room.
Why so hostile?
People with demanding behavior often have a hostile and confrontational manner. They may use medical jargon and appear to believe that they know more than their healthcare team. Many demand to know why they have not been offered a particular test, diagnosis, or treatment, especially if they or a family member has a healthcare background. Such patients appear to feel that they are being treated incorrectly and leave us feeling vulnerable, wondering whether the patient might one day come back to haunt us with a lawsuit, especially if the medical outcome is unfavorable.
Understanding the motivation for the behavior can help a physician to empathize with the demanding patient.12 Although it may seem that the demanding patient is trying to intimidate the physician, the goal is usually the same: to find the best possible treatment. Anger and hostility are often motivated by fear and a sense of losing control.
Ironically, this maladaptive coping style may alienate the very people who can help the patient. Hostile behavior evokes defensiveness and resentment in others. A power struggle may ensue: as the patient makes more unreasonable demands and threats, the physician reacts by asserting his or her views in an attempt to maintain control. Or the physician and the rest of the healthcare team may simply avoid the patient as much as possible.
Collaboration can defuse anger
The best strategy is often to steer the encounter away from a power struggle by legitimizing the patient’s feeling of entitlement to the best possible treatment.13 Take a collaborative stance with the patient, with the common goal of finding and implementing the most effective and lowest-risk diagnostic and treatment plan. Empathy and exploration of the patient’s concerns are always in order.
Physicians can try several strategies to improve interactions with demanding patients and caregivers:
Be consistent. All members of the healthcare team, including nurses and specialists, should convey consistent messages regarding diagnostic testing and treatment plans.
Don’t play the game. Demanding patients often complain about being mistreated by other healthcare providers. When confronted with such complaints, acknowledge the patient’s feelings while refraining from blaming or criticizing other members of the healthcare team.
Clarify expectations. Clarifying expectations from the initial patient encounter can prevent conflicts later. Support a patient who must accept a diagnosis of a terminal illness, and then when appropriate, discuss goals moving forward. Collaboration within the framework of reasonable expectations is key.
For our case, the physician could say, “We want to work with you together as a team. We will work hard to address your concerns, but our nurses must have a safe environment in which to help you.” Such a statement highlights shared goals and expression of concern without judgment. The next step is to clarify expectations by describing the hospital routine and how decisions are made.
Offer choices. Offering choices whenever possible can help a demanding patient feel more in control. Rather than dismiss a patient’s ideas, explore the alternatives. While effective patient communication is preferable to repeated referrals to specialists,14 judicious referral can engender trust in the physician’s competence if a diagnosis is not forthcoming.15
A unique challenge in teaching hospitals is the patient who refuses to interact with residents and students. It is best to acknowledge the patient’s concerns and offer alternative options:
- If the patient is worried about lack of completed training, then clarify the residents’ roles and reassure the patient that you communicate with residents and supervisors regarding any clinical decisions
- If possible, offer to see the patient alone or have the resident interact only on an as-needed basis
- Consider transferring the patient to a nonteaching service or to another hospital.
Admit failings. Although not easy, admitting to and apologizing for things that have gone wrong can help to calm a demanding patient and even reduce the likelihood of a lawsuit.16 The physician should not convey defensiveness and instead should acknowledge the limitations of the healthcare system.
Legitimize concerns—to an extent. Legitimizing a demanding patient’s concerns is important, but never be bullied into taking actions that create unnecessary risk. Upsetting a demanding patient is better than ordering tests or providing treatments that are potentially harmful. Good physician-patient communication can go a long way toward preventing adverse outcomes.
CONSTANTLY SEEKING REASSURANCE
A 25-year-old professional presents to a new primary care provider concerned about a mole on her back. She discusses her sun exposure and family history of skin cancer and produces photographs documenting changes in the mole over time. Impressed with this level of detail, the physician takes time to explain his concerns before referring her to a dermatologist. Later that day, she calls to let the doctor know that her procedure has been scheduled and to thank him for his care. A few weeks after the mole is removed, she returns to discuss treatment options for the small remaining scar.
After this appointment, she calls the office repeatedly with a wide array of concerns, including an isolated symptom of fatigue that could indicate cancer and the relative merits of different sunscreens. She also sends the physician frequent e-mail messages through the personal health record system with pictures of inconsequential marks on her skin.
Needing reassurance is normal—to a point
Many patients seek reassurance from their physicians, and this can be done in a healthy and respectful manner. But requests for reassurance may escalate to becoming repeated, insistent, and even aggressive.1 This can elicit reactions from physicians ranging from feeling annoyed and burdened to feeling angry and overwhelmed.17 This can lead to significant stress, which, if not managed well, can lead to excessively control of physician behavior and substandard care.18
Reassurance-seeking behavior can manifest anywhere along the spectrum of health and disease.19 It may be a symptom of health anxiety (ie, an exaggerated fear of illness) or hypochondria (ie, the persistent conviction that one is currently or likely to become ill).20,21
Why so needy?
Attachment theory may help explain neediness. Parental bonding during childhood is associated with mental and physical health and health-related behaviors in adults.22,23 People with insecure-preoccupied attachment styles tend to be overly emotionally dependent on the acceptance of others and may exhibit dependent and care-seeking behaviors with a physician.24
Needy patients are often genuinely grateful for the care and attention from a physician.1 In the beginning, the doctor may appreciate the patient’s validation of care provided, but this positive feeling wanes as calls and requests become incessant. As the physician’s exhaustion increases with each request, the care and well-being of the patient may no longer be the primary focus.1
Set boundaries
Be alert to signs that a patient is crossing the line to an unhealthy need for reassurance. Address medical concerns appropriately, then institute clear guidelines for follow-up, which should be reinforced by the entire care team if necessary.22
The following strategies can be useful for defining boundaries:
- Instruct the patient to come to the office only for scheduled follow-up visits and to call only during office hours or in an emergency
- Be up-front about the time allowed for each appointment and ask the patient to help focus the discussion according to his or her main concerns25
- Consider telling the patient, “You seem really worried about a lot of physical symptoms. I want to reassure you that I find no evidence of a medical illness that would require intervention. I am concerned about your phone calls and e-mails, and I wonder what would be helpful at this point to address your concerns?”
- Consider treating the patient for anxiety.
It is important to remain responsive to all types of patient concerns. Setting boundaries will guide patients to express health concerns in an appropriate manner so that they can be heard and managed.18,19
SELF-INJURY
A 22-year-old woman presents to the emergency department complaining of abdominal pain. After a full workup, the physician clears her medically and orders a few laboratory tests. As the nurse draws blood samples, she notices multiple fresh cuts on the patient’s arm and informs the physician. The patient is questioned and examined again and acknowledges occasional thoughts of self-harm.
Her parents arrive and appear appropriately concerned. They report that she has been “cutting” for 4 years and is regularly seeing a therapist. However, they say that they are not worried for her safety and that she has an appointment with her therapist this week. Based on this, the emergency department physician discharges her.
Two weeks later, the patient returns to the emergency department with continued cutting and apparent cellulitis, prompting medical admission.
Self-injury presents in many ways
Self-injurious behaviors come in many forms other than the easily recognized one presented in this case: eg, a patient with cirrhosis who continues to drink, a patient with severe epilepsy who forgets to take medications and lands in the emergency department every week for status epilepticus, a patient with diabetes who eats a high-sugar diet, a patient with renal insufficiency who ignores water restrictions, or a patient with an organ transplant who misses medications and relapses.
There is an important psychological difference between patients who knowingly continue to challenge their luck and those who do not fully understand the severity of their condition and the consequences of their actions. The patient who simply does not “get it” can sometimes be managed effectively with education and by working with family members to create an environment to facilitate critical healthy behaviors.
Patients who willfully self-inflict injury are asking for help while doing everything to avoid being helped. They typically come to the office or the emergency department with assorted complaints, not divulging the real reason for their visit until the last minute as they are leaving. Then they drop a clue to the real concern, leaving the physician confused and frustrated.
Why deny an obvious problem?
Fear of the stigma of mental illness can be a major barrier to full disclosure of symptoms of psychological distress, and this especially tends to be the case for patients from some ethnic minorities.26
On the other hand, patients with borderline or antisocial personality disorder (and less often, schizotypal or narcissistic personality disorder) frequently use denial as their primary psychological defense. Self-destructive denial is sometimes associated with traumatic memories, feelings of worthlessness, or a desire to reduce self-awareness and rationalize harmful behaviors. Such patients usually need lengthy treatment, and although the likelihood of cure is low, therapy can be helpful.27–29
Lessons from psychiatry
It can be difficult to maintain empathy for patients who intentionally harm themselves. It is helpful to think of these patients as having a terminal illness and to recognize that they are suffering.
Different interventions have been studied for such patients. Dialectical behavior therapy, an approach that teaches patients better coping skills for regulating emotions, can help reduce maladaptive emotional distress and self-destructive behaviors.30–32 Lessons from this approach can be applied by general practitioners:
- Engage the patient and together establish an effective crisis management plan
- With patient permission, involve the family in the treatment plan
- Set clear limits about self-harm: once the patient values interaction with the doctor, he or she will be less likely to break the agreement.
Patients with severe or continuing issues can be referred to appropriate services that offer dialectical behavior therapy or other intensive outpatient programs.
To handle our patient, one might start by saying, “I am sorry to see you back in the ER. We need to treat the cellulitis and get your outpatient behavioral team on board, so we know the plan.” Then, it is critical that the entire team keep to that plan.
HOW TO STAY IN CONTROL AND IMPROVE INTERACTIONS
Patients with challenging behaviors will always be part of medical practice. Physicians should be aware of their reactions and feelings towards a patient (known in psychiatry as countertransference), as they can increase physician stress and interfere with providing optimal care. Finding effective ways to work with difficult patients will avoid these outcomes.
Physicians also feel loss of control
Most physicians are resilient, but they can feel overwhelmed under certain circumstances. According to Scudder and Shanafelt,33 a physician’s sense of well-being is influenced by several factors, including feelings of control in the workplace. It is easy to imagine how one or more difficult patients can create a sense of overwhelming demand and loss of control.
These tips can help maintain a sense of control and improve interactions with patients:
Have a plan for effective communication. Not having a plan for communicating in a difficult situation can contribute to loss of control in a hectic schedule that is already stretched to its limits. Practicing responses with a colleague for especially difficult patients or using a team approach can be helpful. Remaining compassionate while setting boundaries will result in the best outcome for the patient and physician.
Stop to analyze the situation. One of the tenets of cognitive-behavioral therapy is recognizing that negative thoughts can quickly take us down a dangerous path. Feeling angry and resentful without stopping to think and reflect on the causes can lead to the physician feeling victimized (just like many difficult patients feel).
It is important to step back and think, not just feel. While difficult patients present in different ways, all are reacting to losing control of their situation and want support. During a difficult interaction with a patient, pause to consider, “Why is he behaving this way? Is he afraid? Does he feel that no one cares?”
When a patient verbally attacks beyond what is appropriate, recognize that this is probably due less to anything the physician did than to the patient’s internal issues. Identifying the driver of a patient’s behavior makes it easier to control our own emotions.
Practice empathy. Difficult patients usually have something in their background that can help explain their inappropriate behavior, such as a lack of parental support or abuse. Being open to hearing their story facilitates an empathetic connection.
AVOIDING BURNOUT
Discuss problems
Sadly, physicians often neglect to talk with each other and with trainees about issues leading to burnout, thereby missing important opportunities for empathy, objectivity, reflection, and teaching moments.
Lessons can be gleaned from training in psychiatry, a field in which one must learn methods for working effectively in challenging situations. Dozens of scenarios are practiced using videotapes or observation through one-way mirrors. While not everyone has such opportunities, everyone can discuss issues with one another. Regularly scheduled facilitated groups devoted to discussing problems with colleagues can be enormously helpful.
Schedule quiet times
Mindfulness is an excellent way to spend a few minutes out of every 3- to 4-hour block. There are many ways to help facilitate such moments. Residents and students can be provided with a small book, Mindfulness on the Go,37 aimed for the busy person.
Deep, slow breathing can bring rapid relief to intense negative feelings. Not only does it reduce anxiety faster than medication, but it is also free, is easily taught to others, and can be done unobtrusively. A short description of the role of the blood pH in managing the locus ceruleus and vagus nerve’s balance of sympathetic and parasympathetic activity may capture the curiosity of someone who may otherwise be resistant to the exercise.
Increasingly, hospitals are developing mindfulness sessions and offering a variety of skills physicians can put into their toolbox. Lessons from cognitive-behavioral therapy, dialectical behavior therapy, imagery, and muscle relaxation can help physicians in responding to patients. Investing in communication skills training specific to challenging behaviors seen in different specialties better equips physicians with more effective strategies.
From time to time, all physicians encounter patients whose behavior evokes negative emotions. In 1978, in an article titled “Taking care of the hateful patient,”1 Groves detailed 4 types of patients—“dependent clingers, entitled demanders, manipulative help-rejecters, and self-destructive deniers”1—that even the most seasoned physicians dread, and provided suggestions for managing interactions with them. The topic was revisited and updated in 2006 by Strous et al.2
Now, more than 10 years later, the challenge of how to interact with difficult patients is more relevant than ever. A cultural environment in which every patient can become an “expert” via the Internet has added new challenges. Patients who are especially time-consuming and emotionally draining exacerbate the many other pressures physicians face today (eg, increased paperwork, cost-consciousness, shortened appointment times, and the move to electronic medical records), contributing to physician burnout.
This article further updates the topic of managing challenging patients to reflect the current practice climate. We provide a more modern view of challenging patients and provide guidance on handling them. Although it may be tempting to diagnose some of these patients as having a personality disorder, it can often be more helpful to recognize patterns of behavior and have a clear plan for management. We also discuss general coping strategies for avoiding physician burnout.
INTERNET-SEEKING, QUESTIONING
A 45-year-old man carries in an overstuffed briefcase for his first primary care visit. He is a medical editor for a national journal and recently worked on a case study involving a rare cancer. As he edited, he recognized that he had the same symptoms and diagnosed himself with the same disease. He has brought with him a sheaf of articles he found on the Internet detailing clinical trials for experimental treatments. When the doctor begins to ask questions, he says the answers are irrelevant: he explains that he would have gone straight to an oncologist, but his insurance policy requires that he also have a primary care physician. He now expects the doctor to order magnetic resonance imaging, refer him to an oncologist, and support his request for the treatment he has identified as best.
The Internet: A blessing and a curse
Patients now have access to enormous amounts of information of variable accuracy. As in this case, patients may come to an appointment carrying early research studies that the physician has not yet reviewed. Others get their information from patient blogs that frequently offer opinions without evidence. Often, based on an advertisement or Internet reading, a patient requests a particular medication or test that may not be cost-effective or medically justified.
In a survey more than 10 years ago, more than 75% of physicians reported that they had patients who brought in information from online sources.3 Hu et al4 reported that 70% of patients who had online information planned to discuss it with their physicians. This practice is only growing, including in older patients.5
Physicians may feel confused and frustrated by patients who come armed with information. They may infer that patients do not trust them to diagnose correctly or treat optimally. In addition, discussing such information takes time, causing others on the schedule to wait, adding to the stress of coping with over-booked appointments.
Why so overprepared?
Patients who have or fear that they have cancer may be particularly worried that an important treatment will be overlooked.6 Since they feel that their life is hanging in the balance, their search for a definitive cure is understandable.
Internet-seeking, intensely questioning patients clearly want more information about the treatments they are receiving, alternative medical or procedural options, and complementary therapies.7 The response to their desire for more information affects their impression of physician empathy.8
Adapting to a more informed patient
Approaching these patients as an opportunity to educate may result in a more trusting patient and one more likely to be open to physician guidance and more likely to adhere to an advised treatment plan. Triangulation of the 3 actors—the physician, the patient, and the Web—can help patients to make more-informed choices and foster an attitude of partnership with the physician to lead them to optimal healthcare.
In a review of the impact of Internet use on healthcare and the physician-patient relationship, Wald et al9 urged physicians to:
- Adopt a positive attitude toward discussing Internet contributions
- Encourage patients to take an active role in maintaining health
- Acknowledge patient concerns and fears
- Avoid becoming defensive
- Recommend credible Internet sources.
Laing et al10 urged physicians to recognize rather than deny the effects of patients’ online searching for information and support, and not to ignore the potential impact on treatment. Consumers are gaining autonomy and self-efficacy, and Laing et al encouraged healthcare providers to develop ways to incorporate this new reality into the services they provide.10
How Web-based interaction can assist in patient decision-making for colorectal cancer screening is being explored.11 Patients at home can use an online tool to learn about screening choices and would be more knowledgable and comfortable discussing the options with their care provider. The hope is to build in an automatic reminder for the clinician, who would better understand the patient’s preference before the office visit.
One approach to our patient is to say, “I can see how worried you are about having the same type of cancer you read about, and I want to help you. It is clear to me that you know a lot about healthcare, and I appreciate your engagement in your health. How about starting over? Let me ask a few questions so I can get a better perspective on your symptoms?” Many times, this strategy can help patients reframe their view and accept help.
DEMANDING, LITIGATION-THREATENING
A 60-year-old lawyer is admitted to the hospital for evaluation of abdominal pain. His physician recommends placing a nasogastric tube to provide nutrition while the evaluation is completed. His wife, a former nurse practitioner, insists that a nasogastric tube would be too dangerous and demands that he be allowed to eat instead. The couple declares the primary internal medicine physician incompetent, does not want any residents to be involved in his care, and antagonizes the nurses with constant demands. Soon, the entire team avoids the patient’s room.
Why so hostile?
People with demanding behavior often have a hostile and confrontational manner. They may use medical jargon and appear to believe that they know more than their healthcare team. Many demand to know why they have not been offered a particular test, diagnosis, or treatment, especially if they or a family member has a healthcare background. Such patients appear to feel that they are being treated incorrectly and leave us feeling vulnerable, wondering whether the patient might one day come back to haunt us with a lawsuit, especially if the medical outcome is unfavorable.
Understanding the motivation for the behavior can help a physician to empathize with the demanding patient.12 Although it may seem that the demanding patient is trying to intimidate the physician, the goal is usually the same: to find the best possible treatment. Anger and hostility are often motivated by fear and a sense of losing control.
Ironically, this maladaptive coping style may alienate the very people who can help the patient. Hostile behavior evokes defensiveness and resentment in others. A power struggle may ensue: as the patient makes more unreasonable demands and threats, the physician reacts by asserting his or her views in an attempt to maintain control. Or the physician and the rest of the healthcare team may simply avoid the patient as much as possible.
Collaboration can defuse anger
The best strategy is often to steer the encounter away from a power struggle by legitimizing the patient’s feeling of entitlement to the best possible treatment.13 Take a collaborative stance with the patient, with the common goal of finding and implementing the most effective and lowest-risk diagnostic and treatment plan. Empathy and exploration of the patient’s concerns are always in order.
Physicians can try several strategies to improve interactions with demanding patients and caregivers:
Be consistent. All members of the healthcare team, including nurses and specialists, should convey consistent messages regarding diagnostic testing and treatment plans.
Don’t play the game. Demanding patients often complain about being mistreated by other healthcare providers. When confronted with such complaints, acknowledge the patient’s feelings while refraining from blaming or criticizing other members of the healthcare team.
Clarify expectations. Clarifying expectations from the initial patient encounter can prevent conflicts later. Support a patient who must accept a diagnosis of a terminal illness, and then when appropriate, discuss goals moving forward. Collaboration within the framework of reasonable expectations is key.
For our case, the physician could say, “We want to work with you together as a team. We will work hard to address your concerns, but our nurses must have a safe environment in which to help you.” Such a statement highlights shared goals and expression of concern without judgment. The next step is to clarify expectations by describing the hospital routine and how decisions are made.
Offer choices. Offering choices whenever possible can help a demanding patient feel more in control. Rather than dismiss a patient’s ideas, explore the alternatives. While effective patient communication is preferable to repeated referrals to specialists,14 judicious referral can engender trust in the physician’s competence if a diagnosis is not forthcoming.15
A unique challenge in teaching hospitals is the patient who refuses to interact with residents and students. It is best to acknowledge the patient’s concerns and offer alternative options:
- If the patient is worried about lack of completed training, then clarify the residents’ roles and reassure the patient that you communicate with residents and supervisors regarding any clinical decisions
- If possible, offer to see the patient alone or have the resident interact only on an as-needed basis
- Consider transferring the patient to a nonteaching service or to another hospital.
Admit failings. Although not easy, admitting to and apologizing for things that have gone wrong can help to calm a demanding patient and even reduce the likelihood of a lawsuit.16 The physician should not convey defensiveness and instead should acknowledge the limitations of the healthcare system.
Legitimize concerns—to an extent. Legitimizing a demanding patient’s concerns is important, but never be bullied into taking actions that create unnecessary risk. Upsetting a demanding patient is better than ordering tests or providing treatments that are potentially harmful. Good physician-patient communication can go a long way toward preventing adverse outcomes.
CONSTANTLY SEEKING REASSURANCE
A 25-year-old professional presents to a new primary care provider concerned about a mole on her back. She discusses her sun exposure and family history of skin cancer and produces photographs documenting changes in the mole over time. Impressed with this level of detail, the physician takes time to explain his concerns before referring her to a dermatologist. Later that day, she calls to let the doctor know that her procedure has been scheduled and to thank him for his care. A few weeks after the mole is removed, she returns to discuss treatment options for the small remaining scar.
After this appointment, she calls the office repeatedly with a wide array of concerns, including an isolated symptom of fatigue that could indicate cancer and the relative merits of different sunscreens. She also sends the physician frequent e-mail messages through the personal health record system with pictures of inconsequential marks on her skin.
Needing reassurance is normal—to a point
Many patients seek reassurance from their physicians, and this can be done in a healthy and respectful manner. But requests for reassurance may escalate to becoming repeated, insistent, and even aggressive.1 This can elicit reactions from physicians ranging from feeling annoyed and burdened to feeling angry and overwhelmed.17 This can lead to significant stress, which, if not managed well, can lead to excessively control of physician behavior and substandard care.18
Reassurance-seeking behavior can manifest anywhere along the spectrum of health and disease.19 It may be a symptom of health anxiety (ie, an exaggerated fear of illness) or hypochondria (ie, the persistent conviction that one is currently or likely to become ill).20,21
Why so needy?
Attachment theory may help explain neediness. Parental bonding during childhood is associated with mental and physical health and health-related behaviors in adults.22,23 People with insecure-preoccupied attachment styles tend to be overly emotionally dependent on the acceptance of others and may exhibit dependent and care-seeking behaviors with a physician.24
Needy patients are often genuinely grateful for the care and attention from a physician.1 In the beginning, the doctor may appreciate the patient’s validation of care provided, but this positive feeling wanes as calls and requests become incessant. As the physician’s exhaustion increases with each request, the care and well-being of the patient may no longer be the primary focus.1
Set boundaries
Be alert to signs that a patient is crossing the line to an unhealthy need for reassurance. Address medical concerns appropriately, then institute clear guidelines for follow-up, which should be reinforced by the entire care team if necessary.22
The following strategies can be useful for defining boundaries:
- Instruct the patient to come to the office only for scheduled follow-up visits and to call only during office hours or in an emergency
- Be up-front about the time allowed for each appointment and ask the patient to help focus the discussion according to his or her main concerns25
- Consider telling the patient, “You seem really worried about a lot of physical symptoms. I want to reassure you that I find no evidence of a medical illness that would require intervention. I am concerned about your phone calls and e-mails, and I wonder what would be helpful at this point to address your concerns?”
- Consider treating the patient for anxiety.
It is important to remain responsive to all types of patient concerns. Setting boundaries will guide patients to express health concerns in an appropriate manner so that they can be heard and managed.18,19
SELF-INJURY
A 22-year-old woman presents to the emergency department complaining of abdominal pain. After a full workup, the physician clears her medically and orders a few laboratory tests. As the nurse draws blood samples, she notices multiple fresh cuts on the patient’s arm and informs the physician. The patient is questioned and examined again and acknowledges occasional thoughts of self-harm.
Her parents arrive and appear appropriately concerned. They report that she has been “cutting” for 4 years and is regularly seeing a therapist. However, they say that they are not worried for her safety and that she has an appointment with her therapist this week. Based on this, the emergency department physician discharges her.
Two weeks later, the patient returns to the emergency department with continued cutting and apparent cellulitis, prompting medical admission.
Self-injury presents in many ways
Self-injurious behaviors come in many forms other than the easily recognized one presented in this case: eg, a patient with cirrhosis who continues to drink, a patient with severe epilepsy who forgets to take medications and lands in the emergency department every week for status epilepticus, a patient with diabetes who eats a high-sugar diet, a patient with renal insufficiency who ignores water restrictions, or a patient with an organ transplant who misses medications and relapses.
There is an important psychological difference between patients who knowingly continue to challenge their luck and those who do not fully understand the severity of their condition and the consequences of their actions. The patient who simply does not “get it” can sometimes be managed effectively with education and by working with family members to create an environment to facilitate critical healthy behaviors.
Patients who willfully self-inflict injury are asking for help while doing everything to avoid being helped. They typically come to the office or the emergency department with assorted complaints, not divulging the real reason for their visit until the last minute as they are leaving. Then they drop a clue to the real concern, leaving the physician confused and frustrated.
Why deny an obvious problem?
Fear of the stigma of mental illness can be a major barrier to full disclosure of symptoms of psychological distress, and this especially tends to be the case for patients from some ethnic minorities.26
On the other hand, patients with borderline or antisocial personality disorder (and less often, schizotypal or narcissistic personality disorder) frequently use denial as their primary psychological defense. Self-destructive denial is sometimes associated with traumatic memories, feelings of worthlessness, or a desire to reduce self-awareness and rationalize harmful behaviors. Such patients usually need lengthy treatment, and although the likelihood of cure is low, therapy can be helpful.27–29
Lessons from psychiatry
It can be difficult to maintain empathy for patients who intentionally harm themselves. It is helpful to think of these patients as having a terminal illness and to recognize that they are suffering.
Different interventions have been studied for such patients. Dialectical behavior therapy, an approach that teaches patients better coping skills for regulating emotions, can help reduce maladaptive emotional distress and self-destructive behaviors.30–32 Lessons from this approach can be applied by general practitioners:
- Engage the patient and together establish an effective crisis management plan
- With patient permission, involve the family in the treatment plan
- Set clear limits about self-harm: once the patient values interaction with the doctor, he or she will be less likely to break the agreement.
Patients with severe or continuing issues can be referred to appropriate services that offer dialectical behavior therapy or other intensive outpatient programs.
To handle our patient, one might start by saying, “I am sorry to see you back in the ER. We need to treat the cellulitis and get your outpatient behavioral team on board, so we know the plan.” Then, it is critical that the entire team keep to that plan.
HOW TO STAY IN CONTROL AND IMPROVE INTERACTIONS
Patients with challenging behaviors will always be part of medical practice. Physicians should be aware of their reactions and feelings towards a patient (known in psychiatry as countertransference), as they can increase physician stress and interfere with providing optimal care. Finding effective ways to work with difficult patients will avoid these outcomes.
Physicians also feel loss of control
Most physicians are resilient, but they can feel overwhelmed under certain circumstances. According to Scudder and Shanafelt,33 a physician’s sense of well-being is influenced by several factors, including feelings of control in the workplace. It is easy to imagine how one or more difficult patients can create a sense of overwhelming demand and loss of control.
These tips can help maintain a sense of control and improve interactions with patients:
Have a plan for effective communication. Not having a plan for communicating in a difficult situation can contribute to loss of control in a hectic schedule that is already stretched to its limits. Practicing responses with a colleague for especially difficult patients or using a team approach can be helpful. Remaining compassionate while setting boundaries will result in the best outcome for the patient and physician.
Stop to analyze the situation. One of the tenets of cognitive-behavioral therapy is recognizing that negative thoughts can quickly take us down a dangerous path. Feeling angry and resentful without stopping to think and reflect on the causes can lead to the physician feeling victimized (just like many difficult patients feel).
It is important to step back and think, not just feel. While difficult patients present in different ways, all are reacting to losing control of their situation and want support. During a difficult interaction with a patient, pause to consider, “Why is he behaving this way? Is he afraid? Does he feel that no one cares?”
When a patient verbally attacks beyond what is appropriate, recognize that this is probably due less to anything the physician did than to the patient’s internal issues. Identifying the driver of a patient’s behavior makes it easier to control our own emotions.
Practice empathy. Difficult patients usually have something in their background that can help explain their inappropriate behavior, such as a lack of parental support or abuse. Being open to hearing their story facilitates an empathetic connection.
AVOIDING BURNOUT
Discuss problems
Sadly, physicians often neglect to talk with each other and with trainees about issues leading to burnout, thereby missing important opportunities for empathy, objectivity, reflection, and teaching moments.
Lessons can be gleaned from training in psychiatry, a field in which one must learn methods for working effectively in challenging situations. Dozens of scenarios are practiced using videotapes or observation through one-way mirrors. While not everyone has such opportunities, everyone can discuss issues with one another. Regularly scheduled facilitated groups devoted to discussing problems with colleagues can be enormously helpful.
Schedule quiet times
Mindfulness is an excellent way to spend a few minutes out of every 3- to 4-hour block. There are many ways to help facilitate such moments. Residents and students can be provided with a small book, Mindfulness on the Go,37 aimed for the busy person.
Deep, slow breathing can bring rapid relief to intense negative feelings. Not only does it reduce anxiety faster than medication, but it is also free, is easily taught to others, and can be done unobtrusively. A short description of the role of the blood pH in managing the locus ceruleus and vagus nerve’s balance of sympathetic and parasympathetic activity may capture the curiosity of someone who may otherwise be resistant to the exercise.
Increasingly, hospitals are developing mindfulness sessions and offering a variety of skills physicians can put into their toolbox. Lessons from cognitive-behavioral therapy, dialectical behavior therapy, imagery, and muscle relaxation can help physicians in responding to patients. Investing in communication skills training specific to challenging behaviors seen in different specialties better equips physicians with more effective strategies.
- Groves JE. Taking care of the hateful patient. N Engl J Med 1978; 298:883–887.
- Strous RD, Ulman AM, Kotler M. The hateful patient revisited: relevance for 21st century medicine. Eur J Intern Med 2006; 17:387–393.
- Malone M, Mathes L, Dooley J, While AE. Health information seeking and its effect on the doctor-patient digital divide. J Telemed Telecare 2005; 11(suppl1):25–28.
- Hu X, Bell RA, Kravitz RL, Orrange S. The prepared patient: information seeking of online support group members before their medical appointments. J Health Commun 2012; 17:960–978.
- Tse MM, Choi KC, Leung RS. E-health for older people: the use of technology in health promotion. Cyberpsychol Behav 2008; 11:475–479.
- Pereira JL, Koski S, Hanson J, Bruera ED, Mackey JR. Internet usage among women with breast cancer: an exploratory study. Clin Breast Cancer 2000; 1:148–153.
- Brauer JA, El Sehamy A, Metz JN, Mao JJ. Complementary and alternative and supportive care at leading cancer centers: a systematic analysis of websites. J Altern Complement Med 2010; 16:183–186.
- Smith SG, Pandit A, Rush SR, Wolf MS, Simon C. The association between patient activation and accessing online health information: results from a national survey of US adults. Health Expect 2015; 18:3262–3273.
- Wald HS, Dube CE, Anthony DC. Untangling the Web—the impact of Internet use on health care and the physician-patient relationship. Patient Educ Couns 2007; 68:218–224.
- Laing A, Hogg G, Winkelman D. Healthcare and the information revolution: re-configuring the healthcare service encounter. Health Serv Manage Res 2004; 17:188–199.
- Jimbo M, Shultz CG, Nease DE, Fetters MD, Power D, Ruffin MT 4th. Perceived barriers and facilitators of using a Web-based interactive decision aid for colorectal cancer screening in community practice settings: findings from focus groups with primary care clinicians and medical office staff. J Med Internet Res 2013; 15:e286.
- Steinmetz D, Tabenkin H. The ‘difficult patient’ as perceived by family physicians. Fam Pract 2001; 18:495–500.
- Arciniegas DB, Beresford TP. Managing difficult interactions with patients in neurology practices: a practical approach. Neurology 2010; 75(suppl 1):S39–S44.
- Gallagher TH, Lo B, Chesney M, Christensen K. How do physicians respond to patient’s requests for costly, unindicated services? J Gen Intern Med 1997; 12:663–668.
- Breen KJ, Greenberg PB. Difficult physician-patient encounters. Intern Med J 2010; 40:682–688.
- Huntington B, Kuhn N. Communication gaffes: a root cause of malpractice claims. Proc (Bayl Univ Med Cent) 2003; 16:157–161.
- Maunder RG, Panzer A, Viljoen M, Owen J, Human S, Hunter JJ. Physicians’ difficulty with emergency department patients is related to patients’ attachment style. Soc Sci Med 2006; 63:552–562.
- Thompson D, Ciechanowski PS. Attaching a new understanding to the patient-physician relationship in family practice. J Am Board Fam Pract 2003; 16:219–226.
- Groves M, Muskin P. Psychological responses to illness. In: Levenson JL, ed. The American Psychiatric Publishing Textbook of Psychosomatic Medicine. Arlington, VA: American Psychiatric Publishing, Inc; 2004:68–88.
- Görgen SM, Hiller W, Witthöft M. Health anxiety, cognitive coping, and emotion regulation: a latent variable approach. Int J Behav Med 2014; 21:364–374.
- Strand J, Goulding A, Tidefors I. Attachment styles and symptoms in individuals with psychosis. Nord J Psychiatry 2015; 69:67–72.
- Hooper LM, Tomek S, Newman CR. Using attachment theory in medical settings: implications for primary care physicians. J Ment Health 2012; 21:23–37.
- Bowlby J. Attachment and loss. 1. Attachment. New York, NY: Basic Books; 1969.
- Fuertes JN, Anand P, Haggerty G, Kestenbaum M, Rosenblum GC. The physician-patient working alliance and patient psychological attachment, adherence, outcome expectations, and satisfaction in a sample of rheumatology patients. Behav Med 2015; 41:60–68.
- Frederiksen HB, Kragstrup J, Dehlholm-Lambertsen B. Attachment in the doctor-patient relationship in general practice: a qualitative study. Scand J Prim Health Care 2010; 28:185–190.
- Rastogi P, Khushalani S, Dhawan S, et al. Understanding clinician perception of common presentations in South Asians seeking mental health treatment and determining barriers and facilitators to treatment. Asian J Psychiatr 2014; 7:15–21.
- van der Kolk BA, Perry JC, Herman JL. Childhood origins of self-destructive behavior. Am J Psychiatry 1991; 148:1665–1671.
- Gacono CB, Meloy JR, Berg JL. Object relations, defensive operations, and affective states in narcissistic, borderline, and antisocial personality disorder. J Pers Assess 1992; 59:32–49.
- Perry JC, Presniak MD, Olson TR. Defense mechanisms in schizotypal, borderline, antisocial, and narcissistic personality disorders. Psychiatry 2013; 76:32–52.
- Gibson J, Booth R, Davenport J, Keogh K, Owens T. Dialectical behaviour therapy-informed skills training for deliberate self-harm: a controlled trial with 3-month follow-up data. Behav Res Ther 2014; 60:8–14.
- Fischer S, Peterson C. Dialectical behavior therapy for adolescent binge eating, purging, suicidal behavior, and non-suicidal self-injury: a pilot study. Psychotherapy (Chic). 2015; 52:78–92.
- Booth R, Keogh K, Doyle J, Owens T. Living through distress: a skills training group for reducing deliberate self-harm. Behav Cogn Psychother 2014; 42:156–165.
- Scudder L, Shanafelt TD. Two sides of the physician coin: burnout and well-being. Medscape. Feb 09, 2015. http://nbpsa.org/images/PRP/PhysicianBurnoutMedscape.pdf. Accessed June 2, 2017.
- McAbee JH, Ragel BT, McCartney S, et al. Factors associated with career satisfaction and burnout among US neurosurgeons: results of a nationwide survey. J Neurosurg 2015; 123:161–173.
- Schneider S, Kingsolver K, Rosdahl J. Can physician self-care enhance patient-centered healthcare? Qualitative findings from a physician well-being coaching program. J Fam Med 2015; 2:6.
- Simonds G, Sotile W. Building Resilience in Neurosurgical Residents: A Primer. B Wright Publishing; 2015.
- Bays JC. Mindfulness on the Go: Simple Meditation Practices You Can Do Anywhere. Boulder, CO: Shambhala Publications; 2014.
- Groves JE. Taking care of the hateful patient. N Engl J Med 1978; 298:883–887.
- Strous RD, Ulman AM, Kotler M. The hateful patient revisited: relevance for 21st century medicine. Eur J Intern Med 2006; 17:387–393.
- Malone M, Mathes L, Dooley J, While AE. Health information seeking and its effect on the doctor-patient digital divide. J Telemed Telecare 2005; 11(suppl1):25–28.
- Hu X, Bell RA, Kravitz RL, Orrange S. The prepared patient: information seeking of online support group members before their medical appointments. J Health Commun 2012; 17:960–978.
- Tse MM, Choi KC, Leung RS. E-health for older people: the use of technology in health promotion. Cyberpsychol Behav 2008; 11:475–479.
- Pereira JL, Koski S, Hanson J, Bruera ED, Mackey JR. Internet usage among women with breast cancer: an exploratory study. Clin Breast Cancer 2000; 1:148–153.
- Brauer JA, El Sehamy A, Metz JN, Mao JJ. Complementary and alternative and supportive care at leading cancer centers: a systematic analysis of websites. J Altern Complement Med 2010; 16:183–186.
- Smith SG, Pandit A, Rush SR, Wolf MS, Simon C. The association between patient activation and accessing online health information: results from a national survey of US adults. Health Expect 2015; 18:3262–3273.
- Wald HS, Dube CE, Anthony DC. Untangling the Web—the impact of Internet use on health care and the physician-patient relationship. Patient Educ Couns 2007; 68:218–224.
- Laing A, Hogg G, Winkelman D. Healthcare and the information revolution: re-configuring the healthcare service encounter. Health Serv Manage Res 2004; 17:188–199.
- Jimbo M, Shultz CG, Nease DE, Fetters MD, Power D, Ruffin MT 4th. Perceived barriers and facilitators of using a Web-based interactive decision aid for colorectal cancer screening in community practice settings: findings from focus groups with primary care clinicians and medical office staff. J Med Internet Res 2013; 15:e286.
- Steinmetz D, Tabenkin H. The ‘difficult patient’ as perceived by family physicians. Fam Pract 2001; 18:495–500.
- Arciniegas DB, Beresford TP. Managing difficult interactions with patients in neurology practices: a practical approach. Neurology 2010; 75(suppl 1):S39–S44.
- Gallagher TH, Lo B, Chesney M, Christensen K. How do physicians respond to patient’s requests for costly, unindicated services? J Gen Intern Med 1997; 12:663–668.
- Breen KJ, Greenberg PB. Difficult physician-patient encounters. Intern Med J 2010; 40:682–688.
- Huntington B, Kuhn N. Communication gaffes: a root cause of malpractice claims. Proc (Bayl Univ Med Cent) 2003; 16:157–161.
- Maunder RG, Panzer A, Viljoen M, Owen J, Human S, Hunter JJ. Physicians’ difficulty with emergency department patients is related to patients’ attachment style. Soc Sci Med 2006; 63:552–562.
- Thompson D, Ciechanowski PS. Attaching a new understanding to the patient-physician relationship in family practice. J Am Board Fam Pract 2003; 16:219–226.
- Groves M, Muskin P. Psychological responses to illness. In: Levenson JL, ed. The American Psychiatric Publishing Textbook of Psychosomatic Medicine. Arlington, VA: American Psychiatric Publishing, Inc; 2004:68–88.
- Görgen SM, Hiller W, Witthöft M. Health anxiety, cognitive coping, and emotion regulation: a latent variable approach. Int J Behav Med 2014; 21:364–374.
- Strand J, Goulding A, Tidefors I. Attachment styles and symptoms in individuals with psychosis. Nord J Psychiatry 2015; 69:67–72.
- Hooper LM, Tomek S, Newman CR. Using attachment theory in medical settings: implications for primary care physicians. J Ment Health 2012; 21:23–37.
- Bowlby J. Attachment and loss. 1. Attachment. New York, NY: Basic Books; 1969.
- Fuertes JN, Anand P, Haggerty G, Kestenbaum M, Rosenblum GC. The physician-patient working alliance and patient psychological attachment, adherence, outcome expectations, and satisfaction in a sample of rheumatology patients. Behav Med 2015; 41:60–68.
- Frederiksen HB, Kragstrup J, Dehlholm-Lambertsen B. Attachment in the doctor-patient relationship in general practice: a qualitative study. Scand J Prim Health Care 2010; 28:185–190.
- Rastogi P, Khushalani S, Dhawan S, et al. Understanding clinician perception of common presentations in South Asians seeking mental health treatment and determining barriers and facilitators to treatment. Asian J Psychiatr 2014; 7:15–21.
- van der Kolk BA, Perry JC, Herman JL. Childhood origins of self-destructive behavior. Am J Psychiatry 1991; 148:1665–1671.
- Gacono CB, Meloy JR, Berg JL. Object relations, defensive operations, and affective states in narcissistic, borderline, and antisocial personality disorder. J Pers Assess 1992; 59:32–49.
- Perry JC, Presniak MD, Olson TR. Defense mechanisms in schizotypal, borderline, antisocial, and narcissistic personality disorders. Psychiatry 2013; 76:32–52.
- Gibson J, Booth R, Davenport J, Keogh K, Owens T. Dialectical behaviour therapy-informed skills training for deliberate self-harm: a controlled trial with 3-month follow-up data. Behav Res Ther 2014; 60:8–14.
- Fischer S, Peterson C. Dialectical behavior therapy for adolescent binge eating, purging, suicidal behavior, and non-suicidal self-injury: a pilot study. Psychotherapy (Chic). 2015; 52:78–92.
- Booth R, Keogh K, Doyle J, Owens T. Living through distress: a skills training group for reducing deliberate self-harm. Behav Cogn Psychother 2014; 42:156–165.
- Scudder L, Shanafelt TD. Two sides of the physician coin: burnout and well-being. Medscape. Feb 09, 2015. http://nbpsa.org/images/PRP/PhysicianBurnoutMedscape.pdf. Accessed June 2, 2017.
- McAbee JH, Ragel BT, McCartney S, et al. Factors associated with career satisfaction and burnout among US neurosurgeons: results of a nationwide survey. J Neurosurg 2015; 123:161–173.
- Schneider S, Kingsolver K, Rosdahl J. Can physician self-care enhance patient-centered healthcare? Qualitative findings from a physician well-being coaching program. J Fam Med 2015; 2:6.
- Simonds G, Sotile W. Building Resilience in Neurosurgical Residents: A Primer. B Wright Publishing; 2015.
- Bays JC. Mindfulness on the Go: Simple Meditation Practices You Can Do Anywhere. Boulder, CO: Shambhala Publications; 2014.
KEY POINTS
- Patients who intensely question everything need validation of their need for information and a collaborative approach based on sound medical evidence.
- Patients whose behavior is hostile and demanding need limits placed on aggressive behavior and assurance that the healthcare team is working in their best interests.
- Patients who seek reassurance to the point of overuse of the doctor’s time need to have boundaries set.
- Many patients who injure themselves and deny the problem have a personality disorder. They need empathy and a clear plan for care, often involving behavioral therapy.
- Physicians should plan effective communication strategies for difficult patients, discuss issues with colleagues, and use relaxation methods to help avoid burnout.
Is an adult with Asperger syndrome sitting in your waiting room?
In 1944, Hans Asperger described a subset of children who exhibited “a lack of empathy, little ability to form friendships, one-sided conversation, intense absorption in a special interest, and clumsy movements.”1
In recent years, Asperger syndrome has become increasingly recognized in the medical community and by the general public. It has been popularized in the media in John Elder Robison’s bestselling book, Look Me in the Eye; with the television character Sheldon Cooper in The Big Bang Theory; and in the 2009 film, Adam, a romantic comedy with the title character accurately portraying a young man with Asperger syndrome.
In this article, we discuss the causes and characteristics of Asperger syndrome, with special focus on adults: how it presents, how to treat it, and how to enhance the delivery of care.
PREVALENCE SEEMS TO BE INCREASING
One in 88 children is diagnosed with an autism spectrum disorder, and the rates of Asperger syndrome and other autism spectrum disorders appear to be increasing.2 Whether this increase is the result of more thorough assessment and identification or of environmental changes is hotly debated.3 The rise began before the proposed changes to the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-V) to combine autism, Asperger syndrome, and pervasive developmental disorder not otherwise specified to simplify diagnosis.4 Asperger syndrome affects males three to four times more often than females.5 For most patients, the effects persist throughout life.
BEHAVIORAL IMPAIRMENTS CHARACTERIZE THE SYNDROME
Poor social skills are a hallmark
People with Asperger syndrome struggle with social interaction and face challenges in forming and maintaining relationships. They tend to have less eye contact (often the first indicator), smiling, animated speech, and physical communication such as hand gestures. They tend not to solicit another’s attention to something they themselves find interesting. They often lack social and emotional reciprocity and have difficulty understanding another person’s thoughts or feelings,6 and they have marked difficulty reading social cues. Some adults may appear rigid, selfish, or narrow-minded.
Sometimes behavior is in the normal range but is out of context for a particular situation.7 For example, a preprofessional student with Asperger syndrome might walk into a psychiatric evaluation to assess fitness for duty and take a seat cross-legged on the floor and have a snack. Poor grooming inappropriate for the occasion may also be observed, such as showing up for a formal photo with unkempt hair and in a stained shirt that is half tucked in.
Many adults with autism spectrum disorders are oblivious to their social reputation.8 They are often unaware that their behavior is out of place and only learn that it is not normal when they are told. Others recognize that they have trouble empathizing with or understanding the perspectives of others, but they are at a loss as to how to improve. The syndrome has a tremendous impact on broader aspects of life, such as employment, functional independence, relationships, and social networks.
Other odd behaviors are common
Repetitive behaviors. Many patients with Asperger syndrome have repetitive behaviors, which can manifest as repeating phrases or expressions, attempting to imitate others, and rocking. They tend to follow routines, do not enjoy spontaneity, and are more inflexible and uncomfortable when their planned regimen is altered.
Gait or balance issues may be observed on physical examination.9 Uncoordinated motion and clumsiness are common,10 and some patients may have a bouncy, stilted gait or may walk on their toes, although the latter is more common in children than adults. Many patients have illegible handwriting.11
Fixations. Many Asperger patients have unusual and intense obsessions with subjects like numbers, dates, or aerodynamics of planes. Children with such fascinations are described as “little professors” or as having “geek syndrome.”12 Certain obsessions often continue into adulthood, although one area of interest may fade and another may take over. Such “expertise” in adults may gain them respect, even though they may seem very odd in other ways.
Lack of boundaries. Patients with Asperger syndrome tend to have poor spatial awareness and to be unaware of physical boundaries, standing too close for others’ comfort or unusually far away. Lack of boundaries may extend beyond the physical, as patients may inappropriately help themselves to food or use an item belonging to another without invitation, being unaware that the behavior may be intrusive or inappropriate.
BEHAVIORAL ASSESSMENTS HELP MAKE DIAGNOSIS
Asperger syndrome is most often diagnosed in early childhood, although it may remain undiagnosed into adulthood. Coexisting depression, attention deficit hyperactivity disorder, or anxiety disorders are also often present.
Establishing the diagnosis is aided by information from family members and others who interact with the patient, from the observations of trained professionals, and from self-reported data. However, self-reported assessments are not always reliable, because the syndrome can affect insight.
The most common assessment tool for autism spectrum disorders is the Autism Diagnostic Interview-Revised (ADI-R),13 a battery of tests given in a structured interview to identify and quantify symptoms, determine where a patient falls on the autism spectrum,14 and point toward interventions. The ADI-R also organizes critical developmental history to evaluate if something else is present, such as prodromal schizophrenia. Although the ADI-R can be very useful in the diagnostic process, it is based on parental reporting, which is neither always available nor fully reliable.
A specific diagnostic tool for adults is the Adult Asperger Assessment.15 Patients are asked to complete two screening questionnaires that gauge cognitive function and gather information about thinking, processing, and behavior.
Table 1 lists the criteria for Asperger syndrome from the DSM Fourth Edition, Text Revision (DSM-IV-TR).16 Asperger syndrome differs from general autism in that it is not associated with language delay. In addition, patients with Asperger syndrome usually have average or above-average IQ scores.17 Still, determining whether a patient has Asperger syndrome or high-functioning autism is sometimes challenging.6
In DSM-V, Asperger syndrome will be subsumed under autism spectrum disorder
In 2013, the DSM-V will replace the DSMIV-TR and will combine autism, Asperger syndrome, and pervasive developmental disorder not otherwise classified into a single diagnosis: autism spectrum disorder. The new system uses two instead of the previous three clusters of core symptoms, centered on “social reciprocity and communication” in one arm and “restricted interests and repetitive behavior” in the other.18 There will be less emphasis on play and imagination than in the past. Some authors suggest adding sensory criteria, particularly reduced pain and increased hearing sensitivity.19
The proposed system is sensitive and specific for autism spectrum disorders, allows early diagnosis, and indicates degree of severity.20 It is hoped that the new system, which accounts for the range and severity of symptoms, should help physicians refer patients to the correct level of treatment.
On the other hand, it may be difficult to think of the three disorders as a single diagnosis. Asperger syndrome manifests in distinct ways, and clear behavioral criteria for diagnosis can be invaluable in helping people with the syndrome. Also, the public may continue to refer to it as Asperger syndrome, and parents and patients may feel uncomfortable having it considered to be the same diagnosis as autism.
BEHAVIORAL THERAPY CAN HELP ACHIEVE INDEPENDENCE
Although there is no cure for Asperger syndrome, various interventions can dramatically improve quality of life and independence. The health care team may include a primary care physician, psychologist, psychiatrist, neurologist, and speech therapist.
Behavioral therapies can help patients with Asperger syndrome learn skills to reduce their symptoms. Occupational and physical therapy can improve dexterity, fluidity, and coordination. Desensitization training may help patients adapt to uncomfortable sights, sounds, or smells that may arise. This can be critical in a job situation. For example, while an average person exposed to a foul odor in public is likely to react tactfully, a person with Asperger syndrome may scream loudly, make inappropriate comments, or run from the room. Social training, especially targeted to the workplace, can provide strategies for promoting typical behaviors and be key to maximizing functional independence.
Speech therapists can teach patients how to sound more relaxed and help them master the natural give-and-take of conversational exchange. Psychotherapy can provide a safe place to work on anxiety, express emotions, and manage restricted interests or repeated behaviors. Group therapy or social training can be a venue for learning improved interactions.
Living independently can be very challenging, and patients with Asperger syndrome may need functional independence training to help with a variety of skills, from handling finances to organizing the home.
Improving quality of life includes determining the best learning environments from childhood into college years and beyond.21–23 Socialization can be enhanced with additional social support at home or on campus, through family interactions and collaborative learning, and by teaching empathy.24 Vocational training can be extremely useful.
DRUG THERAPY MAY HAVE A ROLE
Medications are not usually prescribed unless depression or anxiety is also present, but they may also help manage irritability, anger, stereotypical mannerisms, and disturbing movements. Fluoxetine (Prozac) helps reduce repetitive behaviors in adults with Asperger syndrome. Propranolol (Inderal), a well-known antihypertensive, is also used for performance anxiety and improves word fluency, understanding of verbal communication, and verbal problem-solving in patients with an autism spectrum disorder.25
Giving oxytocin (Pitocin) intranasally in a spray formulation is currently being tested to enhance social skills. Patients with an autism spectrum disorder were more able to perceive emotions of others and to respond more appropriately.26 Oxytocin has long been associated with bonding and is believed to enhance mothering skills. It is naturally present in both sexes, but levels are higher in women, which may in part explain the lower rate of autism spectrum disorders in females.27
HEALTH CARE REQUIRES SPECIAL CONSIDERATIONS
Medical care for patients with Asperger syndrome is enhanced by understanding the patient’s experience. Adults, in particular, may have learned to suppress symptoms of Asperger syndrome to better function in society but still experience stress in situations in which others would not. Patients with Asperger syndrome may struggle with social interactions during medical examinations or procedures, and clinicians may find interaction with the patient challenging.
It is important for health care providers to be calm and patient and to understand that anxiety may prevent people with Asperger syndrome from making eye contact. The clinician should confirm that a patient is engaged but should avoid seeming pushy or invasive.
When anxious, patients may employ strange gestures that they find soothing, such as flapping the hands, rocking, or cracking the knuckles. It is usually easier to allow them to continue unless the activity hinders the examination or treatment.
Patients are likely to respond better to direct requests than to subtle questions: eg, “Open your mouth, please” instead of “Could you open your mouth?” Using clear, specific language and avoiding metaphors, irony, and nonverbal communication are best. It is important to explicitly ask for everything needed, as patients may not volunteer information and may have trouble articulating what they are thinking or feeling. While educating patients about their health needs, physicians may need to reiterate guidance several times or approach the same topic from different angles in order for the patient to accept a concern.
All actions, especially touching the patient, should be explained clearly beforehand. If possible, the doctor should demonstrate using visuals or on his or her own body if appropriate. For invasive procedures, anesthetizing the local area is recommended.
People with Asperger syndrome often rely heavily on a regular routine to maintain a sense of organization. By interrupting this routine, a doctor’s visit can induce anxiety. Waiting also increases anxiety, so scheduling patients with Asperger syndrome either first or last in the day may help.
Hypersensitivity poses challenges
Many people with Asperger syndrome have abnormal sensitivity to stimuli, with differences in pain sensation and hearing perhaps most prominent. Loud noises, such as beeping equipment, whirring fans, or buzzing lights may be distressful and should be reduced if possible. Patients may also be strongly affected by bright lights or scents such as perfumes.
Patients may also have an altered sense of taste, with consequences that go beyond simple “picky eating.” Patients should be asked about unusual eating patterns, diets, or food aversions. People with autism spectrum disorders often do not consume adequate vitamin C because of an aversion to fruits and vegetables. Vitamin deficiency may have originated in infancy but may not be identified or treated until adulthood.28
The sense of touch may be intensified, causing patients to be extremely ticklish; they may actually prefer to be touched more firmly. When it is necessary to make physical contact with patients, it will make the process easier if the physician determines their comfort level and finds ways to help them endure the experience with the least amount of discomfort.
Some patients with impaired sensory expression may have a high tolerance for extreme temperatures and pain, leading to delay in seeking aid.29 Patients may downgrade pain levels, masking the severity of an illness or injury.
Transition from pediatric to adult care
Pediatrics is often a warm environment in which children develop a trusting relationship with their care providers. The transition to adult care can be daunting for patients with Asperger syndrome and their families, and many postpone the change for as long as possible.
Although time-consuming, a collaborative effort between the pediatric and adult care teams can dramatically smooth the transition. It can help to have a familiar person from the pediatric team, such as a nurse, be present at the initial interaction with the new adult care team. Both teams should be familiar with the other’s clinical practices and be aware of the patient’s stressors and ways to ameliorate them.30
THE SEARCH FOR A CAUSE CONTINUES
Numerous studies are attempting to understand the anatomic and physiologic causes of autism spectrum disorders, and to find effective treatments and improve the quality of life.
Prenatal factors implicated
Several recent studies have focused on environmental factors during pregnancy as risk factors for autism spectrum disorder. Selective serotonin reuptake inhibitors were found to increase the risk,31 but the severity of the mother’s depressive illness must be considered before counseling against using these drugs. Older maternal or paternal age was also found to increase the risk of an autism spectrum disorder.32 Recent research indicates that older fathers are in particular more likely to have children with disorders such as autism because of an increase in random mutations associated with advanced age.33
Maternal illness during pregnancy is also associated. Preliminary studies found an increased risk of autism if the mother had had a prenatal viral infection.34 A more recent study found that untreated fever during pregnancy rather than a specific viral infection is more strongly linked.35
Maternal antibodies have been implicated as well. One review found that psoriasis is the only maternal autoimmune condition significantly associated with the development of an autism spectrum disorder.36 Elevated levels of antibodies against the fetal brain have been found in mothers with autistic children.37 One study found that autistic children and their siblings have elevated antibrain antibodies in distinct brain regions, including the caudate nucleus, putamen, prefrontal cortex, cerebellum, and cingulate gyrus (why the siblings are spared from having the disorder is unclear).38 Some have questioned whether a child’s own immune system might even be involved.39
Functional magnetic resonance imaging reveals multiple differences
Functional magnetic resonance imaging (fMRI) has been used to investigate impaired social interaction, specific deficits of facial perception and recognition, sensory processing, working memory, and “theory of mind.” Hypoactivation, hyperactivation, and decreased functional connectivity have been observed depending on the mental processes evaluated.40
When undergoing facial perception tasks, subjects with autism spectrum disorders exhibit hypoactivation in the lateral aspect of the middle region of the fusiform gyrus, responsible for face identification. But they have significant activation of the limbic system, specifically the amygdala, during facial recognition. Hypoactivity in the fusiform gyrus is observed when trying to identify faces or read facial expressions.41,42 This cluster of findings helps explain misinterpretations, misidentification, and heightened affect.
A hallmark characteristic of autism is the difficulty patients have in determining intentions and interpreting others’ behavior, thoughts, or emotions. Studies of people with autism spectrum disorders show that areas often responsible for “sensitivity to others” are hypoactive.43 There is also diminished activation in the medial cingulate cortex, normally activated when these people are asked to think about themselves and who they are.44
The resting state in the brains of people with autism spectrum disorders is abnormally activated.45 They are often particularly good at attention to detail but challenged in integrating information needed for general executive functioning. Impaired sensory processing makes it difficult for them to simultaneously interpret multiple sources of sensory input.46
Perhaps some of the most exciting fMRI news comes from infant studies. Radical and axial diffusivity and fractional anisotropy techniques demonstrate differences in the brains of infants 6 to 24 months old, before symptoms of autism spectrum disorders are observed. It is hoped that early intervention could come into play before the syndrome develops fully.47
The synthesis of input of social and emotional cues is sometimes referred to in the literature as “theory of mind.” It is impaired in Asperger syndrome,48 as manifested by a lack of empathy and by challenges in perceiving others’ thoughts and feelings. The basis of impairment may be related to abnormalities in the amygdala.49 Normal awareness involves the integration of multiple neural networks in the anterior paracingulate cortex, the superior temporal sulci, and the temporal poles bilaterally, but different regions appear to be used in patients with Asperger syndrome.50 A small series of five case studies using positron emission tomography indicated that the left prefrontal cortex was the primary location for theory of mind in Asperger syndrome.51
Epilepsy, gastrointestinal problems, and sleep disturbances are associated
About 25% of people with autism spectrum disorders have epilepsy vs 2% to 3% in the general population. Asperger syndrome is associated with a much lower but still elevated risk of 4% to 6%.47,52
Gastrointestinal complaints, most often constipation or chronic diarrhea, are much more common in children with autism spectrum disorders than in the general population. Preliminary data showed that children with an autism spectrum disorder have a 42% rate of gastrointestinal problems vs 12% in unaffected siblings. There is also a correlation between the severity of gastrointestinal problems and severity of autistic symptoms.53
Research is ongoing to determine the prevalence of insomnia or interrupted sleep in those with autism spectrum disorders.54–56 Changes in sleep architecture can explain nighttime activity.
NONTRADITIONAL CONSIDERATIONS
Dietary treatment: Mixed findings
A popular hypothesis is that adherence to a gluten-free or casein-free diet can reduce symptoms of autism spectrum disorders. Preliminary reports identified several cases of children showing improvement.57 However, this has not been replicated, and more studies refute benefits of these diets.58
Essential nutritional needs should be met with any diet, whether it is designed to reduce symptoms or not. Patients with autism spectrum disorders may have strong food aversions, and dietary supplements of vitamins and minerals may be required.
Vaccines do not cause autism
Despite popular concern, recent research indicates that vaccines do not cause autism. Thimerosal, a mercury-based preservative used in childhood vaccines, was at one time implicated as a risk factor for autism spectrum disorders. The US Centers for Disease Control and Prevention (CDC) issued a precaution against using thimerosal-containing vaccines while testing was done to determine the effects on neuropsychological development.59 The CDC study as well as newer studies did not demonstrate that exposure to mercury causes these neuropsychological concerns, but researchers have continued to study the subject.60–62 The original study implicating thimerosal was disproven as scientifically unsound and fraught with conflict of interest and legal concerns. It has since been retracted, and its findings have been completely discredited.63
Other areas of research
Current research is exploring the higher prevalence of autism spectrum disorders in particular families.64–66 Autism and autism spectrum disorders may be caused by hundreds of simultaneous gene alterations or may develop as a result of reduced gene expression in two areas of the cerebral cortex where higher-order processing occurs, in the frontal and temporal lobes.67
Although genetic theories of autism predominate, a 2011 project suggests that environment is also important. A study of twins found that genetics accounted for 40% or less of cases of autism spectrum disorder, with at least 55% of cases being attributable to environmental factors.68
- Frith U, editor. Autism and Asperger Syndrome. New York: Cambridge University Press, 1991:37–92.
- Autism and Developmental Disabilities Monitoring Network Surveillance Year 2008 Principal Investigators. Prevalence of autism spectrum disorders—Autism and Developmental Disabilities Monitoring Network, 14 sites, United States, 2008. MMWR Surveill Summ 2012; 61( 3):1–19.
- Rutter M. Incidence of autism spectrum disorders: changes over time and their meaning. Acta Paediatr 2005; 94:2–15.
- Happé F. Criteria, categories, and continua: autism and related disorders in DSM-5. J Am Acad Child Adolesc Psychiatry 2011; 50:540–542.
- National Institute of Neurological Disorders and Stroke. Asperger syndrome fact sheet. http://www.ninds.nih.gov/disorders/asperger/detail_asperger.htm. Accessed October 11, 2012.
- Toth K, King BH. Asperger’s syndrome: diagnosis and treatment. Am J Psychiatry 2008; 165:958–963.
- Vermeulen P. Autism: from mind blindness to context blindness. Asperger’s Digest November/December 2011. http://autismdigest.com/autism-from-mind-blindness-to-context-blindness/. Accessed October 11, 2012.
- Izuma K, Matsumoto K, Camerer CF, Adolphs R. Insensitivity to social reputation in autism. Proc Natl Acad Sci U S A. 2011; 108:17302–17307.
- Weimer AK, Schatz AM, Lincoln A, Ballantyne AO, Trauner DA. “Motor” impairment in Asperger’s syndrome: evidence for a deficit in proprioception. J Dev Behav Pediatr 2001; 22:92–101.
- Siaperas P, Ring HA, McAllister CJ, et al. Atypical movement performance and sensory integration in Asperger’s syndrome. J Autism Dev Disord 2012; 42:718–725.
- Kushki A, Chau T, Anagnostou E. Handwriting difficulties in children with autism spectrum disorders: a scoping review. J Autism Dev Disord 2011; 41:1706–1716.
- Nash JM, Bonesteel A. The geek syndrome. Time Magazine U.S. 2002. http://www.time.com/time/magazine/article/0,9171,1002365-1,00.html. Accessed October 11, 2012.
- Le Couteur A, Rutter M, Lord C, et al. Autism diagnostic interview: a standardized investigatorbased instrument. J Autism Dev Disord 1989; 19:363–387.
- Rutter M, Le Couteur A, Lord C. Autism Diagnostic Interview-Revised WPS Edition Manual. Los Angeles, CA. Western Psychological Services; 2003.
- Baron-Cohen S, Wheelwright S, Robinson J, Woodbury-Smith M. The Adult Asperger’s Assessment (AAA): a diagnostic method. J Autism Developmental Disord 2005; 35:807–819.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders Text Revision DSM IV–TR 4th Ed. 2000; Washington, DC: American Psychiatric Association; 2000:80–84.
- Centers for Disease Control. Asperger syndrome fact sheet. http://www.cdc.gov/ncbddd/actearly/pdf/parents_pdfs/Asperger_Syndrome.pdf. Accessed October 11, 2012.
- Peckham C. The current state in autism—still tough to treat but encouraging progress. An expert interview with Fred R. Volkmar, MD. Medscape Pediatrics 2010. http://www.medscape.com/viewarticle/720802?src=mp&spon=17. Accessed October 31, 2012.
- Muscari ME. How should I evaluate an adult for possible Asperger’s syndrome? Medscape News Today 2006.
- Hollander E. Can we treat core symptoms of autism spectrum disorders in adults? December 21, 2011; 1( 18). http://www.medscape.com/viewarticle/531750. Accessed October 1, 2012.
- Müller E, Schuler A, Yates GB. Social challenges and supports from the perspective of individuals with Asperger’s syndrome and other autism spectrum disabilities. Autism 2008; 12:173–190.
- Helman T, Berger O. Parents of children with Asperger’s syndrome or with learning disabilities: family environment and social support. Res Dev Disabil 2008; 29;289–300.
- Taylor CM. Campus commons. When pigs fly: a new perspective on learning. About Campus 2011; 16:30–32.
- Cheng Y, Chiang H, Ye J, Cheng L. Enhancing empathy instruction using a collaborative virtual learning environment for children with autistic spectrum conditions. Comput Edu 2010; 55:1449–1458.
- Beversdorf DQ, Saklayen S, Higgins KF, Bodner KE, Kanne SM, Christ SE. Effect of propranolol on word fluency in autism. Cogn Behav Neurol 2011; 24:11–17.
- Kuehn BM. Scientists probe oxytocin therapy for social deficits in autism, schizophrenia. JAMA 2011; 305:659–661.
- Pfaff DW, Rapin I, Goldman S. Male dominance in autism: neuroendocrine influences on arousal and social anxiety. Autism Res 2011; 4:163–176.
- Brauser D. Children with autism routinely exhibit feeding difficulties in infancy. Medscape Medical News 2010. http://www.medscape.org/viewarticle/726060. Accessed October 31, 2012.
- Baron MG, Groden J, Groden G, Lipsitt L. Stress and coping in autism. New York: Oxford University Press; 2006:355.
- Camfield P, Camfield C. Transition to adult care for children with chronic neurological disorders. Ann Neurol 2001; 69:437–444.
- Croen LA, Grether JK, Yoshida CK, Odouli R, Hendrick V. Antidepressant use during pregnancy and childhood autism spectrum disorders. Arch Gen Psychiatry 2011; 68:1104–1112.
- Croen LA, Najjar DV, Fireman B, Grether JK. Maternal and paternal age and risk of autism spectrum disorders. Arch Pediatr Adolesc Med 2007; 161:334–340.
- Kong A, Frigge ML, Masson G, et al. Rate of de novo mutations and the importance of father’s age to disease risk. Nature 2012; 488:471–475.
- Atlandóttir HO, Thorsen P, Østergaard L, et al. Maternal infection requiring hospitalization during pregnancy and autism spectrum disorders. J Autism Dev Disord 2010; 40:1423–1430.
- Zerbo O, Iosif A-M, Walker C, Ozonoff S, Hansen RL, Hertz-Picciotto I. Is maternal influenza or fever during pregnancy associated with autism or developmental delays? Results from the CHARGE (CHildhood Autism Risks from Genetics and Environment) study. J Autism Dev Disord 2012; 10.1007/s10803-012-1540-x.
- Crown LA, Grether JK, Yoshida CK, Odouli R, Van de Water J. Maternal autoimmune diseases, asthma and allergies, and childhood autism spectrum disorders: a case-control study. Arch Pediatr Adolesc Med 2005; 159:151–157.
- Singer HS, Morris CM, Gause CD, Gillin PK, Crawford S, Zimmerman AW. Antibodies against fetal brain in sera of mothers with autistic children. J Neruoimmunol 2008; 194:165–172.
- Singer HS, Morris CM, Williams PN, Yoon DY, Hong JJ, Zimmerman AW. Antibrain antibodies in children with autism and their unaffected siblings. J Neuroimmunol 2006; 178:149–155.
- Ashwood P, Van de Water J. Is autism an autoimmune disease? Autoimmunity Rev 2004; 3:557–562.
- South M, Diehl JJ. Functional magnetic resonance imaging. In:Hollander E, Kolevzon A, Coyle J, editors. Textbook of Autism Spectrum Disorders. Washington, DC: American Psychiatric Publishing; 2011:409–414.
- Shultz RT, Gauthier I, Klin A, et al. Abnormal ventral temporal cortical activity during face discrimination among individuals with autism and Asperger syndrome. Arch Gen Psychiatry 2000; 57:331–340.
- Wang AT, Dapretto M, Hariri AR, et al. Neural correlates of facial affect processing in children and adolescents with autism spectrum disorder. J Am Acad Child Adolesc Psychiatry 2004; 43:481–490.
- Mason RA, Williams DL, Kana RK, et al. Theory of mind disruption and recruitment of the right hemisphere during narrative comprehension in autism. Neuropsychologia 2008; 46:269–280.
- Chiu PH, Kayali MA, Kishida KT, et al. Self responses along cingulate cortex reveal quantitative neural phenotype for high-functioning autism. Neuron 2008; 57:463–437.
- Kennedy DP, Redcay E, Courchesne E. Failing to deactivate: resting functional abnormalities in autism. Proc Natl Acad Sci U S A 2006; 103:8275–8280.
- Bölte S, Hubl D, Dierks T, et al. An fMRI-study of locally oriented perception in autism: altered early visual processing of the block design test. J Neural Transm 2008; 115:545–552.
- Maski KP, Jeste SS, Spencer SJ. Common neurological co-morbidities in autism spectrum disorders. Curr Opin Pediatr 2011; 23:609–615.
- Kleinman J, Marciano P, Ault RL. Advanced theory of mind in high functioning adults with autism. J Autism Dev Disord 2011; 31:29–36.
- Fine C, Lumsden J, Blair RJ. Dissociation between ‘theory of mind and executive functions in a patient with early left amygdala damage. Brain 2001; 124:287–298.
- Gallagher HL, Frith CD. Functional imaging of ‘theory of mind.’ Trends Cogn Sci 2003; 7:77–83.
- Happé F, Ehlers S, Pletcher P, et al. ‘Theory of mind’ in the brain. Evidence from a PET scan study of Asperger’s syndrome. Neuroreport 1996; 8:197–207.
- Kugimiya S. Clinical features and possible correlations between autism and epilepsy. Neurology Asia 2010; 15(suppl 1):44–45.
- Wang LW, Tancredi DJ, Thomas DW. The prevalence of gastrointestinal problems in children across the United States with autism spectrum disorders from families with multiple affected members. J Dev Behav Pediatr 2011; 32:351–360.
- Bruni O, Ferri R, Vittori E, et al. Sleep architecture and NREM alterations in children and adolescents with Asperger syndrome. Sleep 2007; 30:1577–1585.
- Richdale AL, Schreck KA. Sleep problems in autism spectrum disorders: prevalence, nature, & possible biopsychosocial aetiologies. Sleep Med Rev 2009; 13:403–411.
- Paavonen EJ, Vehkalahti K, Vanhala R, von Wendt L, Nieminen-von Wendt T, Aronen ET. Sleep in children with Asperger’s syndrome. J Autism Dev Disord 2007; 38:41–51.
- Elder JH, Shankar M, Shuster J, Theriaque D, Burns S, Sherrill L. The gluten-free, casein-free diet in autism: results of a preliminary double blind clinical trial. J Autism Dev Disord 2006; 36:413–420.
- Keller DM. Diet free of gluten and casein has no effect on autism symptoms. Medscape News May 24, 2010. http://www.medscape.com/viewarticle/722283.
- Centers for Disease Control and Prevention (CDC). Recommendations regarding the use of vaccines that contain thimerosal as a preservative. MMWR Morb Mortal Wkly Rep 1999; 48:996–998.
- Thompson WW, Price C, Goodson B, et al; Vaccine Safety Datalink Team. Early thimerosal exposure and neuropsychological outcomes at 7 to 10 years. N Engl J Med 2007; 357:1281–1292.
- Price CS, Thompson WW, Goodson B, et al. Prenatal and infant exposure to thimerosal from vaccines and immunoglobulins and risk of autism. Pediatrics 2010; 126:656–664.
- Centers for Disease Control and Prevention (CDC). CDC study on “Prenatal and infant exposure to thimerosal from vaccines and immunoglobulins and risk of autism.” www.cdc.gov/vaccinesafety/Concerns/Thimerosal/QA_Pediatrics-thimerosal-autism.html. Accessed November 5, 2012.
- Deer B. How the case against the MMR vaccine was fixed. BMJ 2011; 342:c5347.
- Losh M, Sullivan PF, Trembath D, Piven J. Current developments in the genetics of autism: from phenome to genome. J Neuropathol Exp Neurol 2008; 67:829–837.
- Curran S, Bolton P. Genetics of autism. In:Kim Y-K, editor. Handbook of Behavior Genetics, Part IV. New York, NY: Springer; 2009:397–410.
- State MW. The genetics of child psychiatric disorders: focus on autism and Tourette syndrome. Neuron 2010; 68:254–269.
- Voineagu I, Wang X, Johnston P, et al. Transcriptomic analysis of autistic brain reveals convergent molecular pathology. Nature 2011; 474:380–384.
- Hallmayer J, Cleveland S, Torres A, et al. Genetic heritability and shared environmental factors among twin pairs with autism. Arch Gen Psychiatry 2011; 68:1095–1102.
In 1944, Hans Asperger described a subset of children who exhibited “a lack of empathy, little ability to form friendships, one-sided conversation, intense absorption in a special interest, and clumsy movements.”1
In recent years, Asperger syndrome has become increasingly recognized in the medical community and by the general public. It has been popularized in the media in John Elder Robison’s bestselling book, Look Me in the Eye; with the television character Sheldon Cooper in The Big Bang Theory; and in the 2009 film, Adam, a romantic comedy with the title character accurately portraying a young man with Asperger syndrome.
In this article, we discuss the causes and characteristics of Asperger syndrome, with special focus on adults: how it presents, how to treat it, and how to enhance the delivery of care.
PREVALENCE SEEMS TO BE INCREASING
One in 88 children is diagnosed with an autism spectrum disorder, and the rates of Asperger syndrome and other autism spectrum disorders appear to be increasing.2 Whether this increase is the result of more thorough assessment and identification or of environmental changes is hotly debated.3 The rise began before the proposed changes to the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-V) to combine autism, Asperger syndrome, and pervasive developmental disorder not otherwise specified to simplify diagnosis.4 Asperger syndrome affects males three to four times more often than females.5 For most patients, the effects persist throughout life.
BEHAVIORAL IMPAIRMENTS CHARACTERIZE THE SYNDROME
Poor social skills are a hallmark
People with Asperger syndrome struggle with social interaction and face challenges in forming and maintaining relationships. They tend to have less eye contact (often the first indicator), smiling, animated speech, and physical communication such as hand gestures. They tend not to solicit another’s attention to something they themselves find interesting. They often lack social and emotional reciprocity and have difficulty understanding another person’s thoughts or feelings,6 and they have marked difficulty reading social cues. Some adults may appear rigid, selfish, or narrow-minded.
Sometimes behavior is in the normal range but is out of context for a particular situation.7 For example, a preprofessional student with Asperger syndrome might walk into a psychiatric evaluation to assess fitness for duty and take a seat cross-legged on the floor and have a snack. Poor grooming inappropriate for the occasion may also be observed, such as showing up for a formal photo with unkempt hair and in a stained shirt that is half tucked in.
Many adults with autism spectrum disorders are oblivious to their social reputation.8 They are often unaware that their behavior is out of place and only learn that it is not normal when they are told. Others recognize that they have trouble empathizing with or understanding the perspectives of others, but they are at a loss as to how to improve. The syndrome has a tremendous impact on broader aspects of life, such as employment, functional independence, relationships, and social networks.
Other odd behaviors are common
Repetitive behaviors. Many patients with Asperger syndrome have repetitive behaviors, which can manifest as repeating phrases or expressions, attempting to imitate others, and rocking. They tend to follow routines, do not enjoy spontaneity, and are more inflexible and uncomfortable when their planned regimen is altered.
Gait or balance issues may be observed on physical examination.9 Uncoordinated motion and clumsiness are common,10 and some patients may have a bouncy, stilted gait or may walk on their toes, although the latter is more common in children than adults. Many patients have illegible handwriting.11
Fixations. Many Asperger patients have unusual and intense obsessions with subjects like numbers, dates, or aerodynamics of planes. Children with such fascinations are described as “little professors” or as having “geek syndrome.”12 Certain obsessions often continue into adulthood, although one area of interest may fade and another may take over. Such “expertise” in adults may gain them respect, even though they may seem very odd in other ways.
Lack of boundaries. Patients with Asperger syndrome tend to have poor spatial awareness and to be unaware of physical boundaries, standing too close for others’ comfort or unusually far away. Lack of boundaries may extend beyond the physical, as patients may inappropriately help themselves to food or use an item belonging to another without invitation, being unaware that the behavior may be intrusive or inappropriate.
BEHAVIORAL ASSESSMENTS HELP MAKE DIAGNOSIS
Asperger syndrome is most often diagnosed in early childhood, although it may remain undiagnosed into adulthood. Coexisting depression, attention deficit hyperactivity disorder, or anxiety disorders are also often present.
Establishing the diagnosis is aided by information from family members and others who interact with the patient, from the observations of trained professionals, and from self-reported data. However, self-reported assessments are not always reliable, because the syndrome can affect insight.
The most common assessment tool for autism spectrum disorders is the Autism Diagnostic Interview-Revised (ADI-R),13 a battery of tests given in a structured interview to identify and quantify symptoms, determine where a patient falls on the autism spectrum,14 and point toward interventions. The ADI-R also organizes critical developmental history to evaluate if something else is present, such as prodromal schizophrenia. Although the ADI-R can be very useful in the diagnostic process, it is based on parental reporting, which is neither always available nor fully reliable.
A specific diagnostic tool for adults is the Adult Asperger Assessment.15 Patients are asked to complete two screening questionnaires that gauge cognitive function and gather information about thinking, processing, and behavior.
Table 1 lists the criteria for Asperger syndrome from the DSM Fourth Edition, Text Revision (DSM-IV-TR).16 Asperger syndrome differs from general autism in that it is not associated with language delay. In addition, patients with Asperger syndrome usually have average or above-average IQ scores.17 Still, determining whether a patient has Asperger syndrome or high-functioning autism is sometimes challenging.6
In DSM-V, Asperger syndrome will be subsumed under autism spectrum disorder
In 2013, the DSM-V will replace the DSMIV-TR and will combine autism, Asperger syndrome, and pervasive developmental disorder not otherwise classified into a single diagnosis: autism spectrum disorder. The new system uses two instead of the previous three clusters of core symptoms, centered on “social reciprocity and communication” in one arm and “restricted interests and repetitive behavior” in the other.18 There will be less emphasis on play and imagination than in the past. Some authors suggest adding sensory criteria, particularly reduced pain and increased hearing sensitivity.19
The proposed system is sensitive and specific for autism spectrum disorders, allows early diagnosis, and indicates degree of severity.20 It is hoped that the new system, which accounts for the range and severity of symptoms, should help physicians refer patients to the correct level of treatment.
On the other hand, it may be difficult to think of the three disorders as a single diagnosis. Asperger syndrome manifests in distinct ways, and clear behavioral criteria for diagnosis can be invaluable in helping people with the syndrome. Also, the public may continue to refer to it as Asperger syndrome, and parents and patients may feel uncomfortable having it considered to be the same diagnosis as autism.
BEHAVIORAL THERAPY CAN HELP ACHIEVE INDEPENDENCE
Although there is no cure for Asperger syndrome, various interventions can dramatically improve quality of life and independence. The health care team may include a primary care physician, psychologist, psychiatrist, neurologist, and speech therapist.
Behavioral therapies can help patients with Asperger syndrome learn skills to reduce their symptoms. Occupational and physical therapy can improve dexterity, fluidity, and coordination. Desensitization training may help patients adapt to uncomfortable sights, sounds, or smells that may arise. This can be critical in a job situation. For example, while an average person exposed to a foul odor in public is likely to react tactfully, a person with Asperger syndrome may scream loudly, make inappropriate comments, or run from the room. Social training, especially targeted to the workplace, can provide strategies for promoting typical behaviors and be key to maximizing functional independence.
Speech therapists can teach patients how to sound more relaxed and help them master the natural give-and-take of conversational exchange. Psychotherapy can provide a safe place to work on anxiety, express emotions, and manage restricted interests or repeated behaviors. Group therapy or social training can be a venue for learning improved interactions.
Living independently can be very challenging, and patients with Asperger syndrome may need functional independence training to help with a variety of skills, from handling finances to organizing the home.
Improving quality of life includes determining the best learning environments from childhood into college years and beyond.21–23 Socialization can be enhanced with additional social support at home or on campus, through family interactions and collaborative learning, and by teaching empathy.24 Vocational training can be extremely useful.
DRUG THERAPY MAY HAVE A ROLE
Medications are not usually prescribed unless depression or anxiety is also present, but they may also help manage irritability, anger, stereotypical mannerisms, and disturbing movements. Fluoxetine (Prozac) helps reduce repetitive behaviors in adults with Asperger syndrome. Propranolol (Inderal), a well-known antihypertensive, is also used for performance anxiety and improves word fluency, understanding of verbal communication, and verbal problem-solving in patients with an autism spectrum disorder.25
Giving oxytocin (Pitocin) intranasally in a spray formulation is currently being tested to enhance social skills. Patients with an autism spectrum disorder were more able to perceive emotions of others and to respond more appropriately.26 Oxytocin has long been associated with bonding and is believed to enhance mothering skills. It is naturally present in both sexes, but levels are higher in women, which may in part explain the lower rate of autism spectrum disorders in females.27
HEALTH CARE REQUIRES SPECIAL CONSIDERATIONS
Medical care for patients with Asperger syndrome is enhanced by understanding the patient’s experience. Adults, in particular, may have learned to suppress symptoms of Asperger syndrome to better function in society but still experience stress in situations in which others would not. Patients with Asperger syndrome may struggle with social interactions during medical examinations or procedures, and clinicians may find interaction with the patient challenging.
It is important for health care providers to be calm and patient and to understand that anxiety may prevent people with Asperger syndrome from making eye contact. The clinician should confirm that a patient is engaged but should avoid seeming pushy or invasive.
When anxious, patients may employ strange gestures that they find soothing, such as flapping the hands, rocking, or cracking the knuckles. It is usually easier to allow them to continue unless the activity hinders the examination or treatment.
Patients are likely to respond better to direct requests than to subtle questions: eg, “Open your mouth, please” instead of “Could you open your mouth?” Using clear, specific language and avoiding metaphors, irony, and nonverbal communication are best. It is important to explicitly ask for everything needed, as patients may not volunteer information and may have trouble articulating what they are thinking or feeling. While educating patients about their health needs, physicians may need to reiterate guidance several times or approach the same topic from different angles in order for the patient to accept a concern.
All actions, especially touching the patient, should be explained clearly beforehand. If possible, the doctor should demonstrate using visuals or on his or her own body if appropriate. For invasive procedures, anesthetizing the local area is recommended.
People with Asperger syndrome often rely heavily on a regular routine to maintain a sense of organization. By interrupting this routine, a doctor’s visit can induce anxiety. Waiting also increases anxiety, so scheduling patients with Asperger syndrome either first or last in the day may help.
Hypersensitivity poses challenges
Many people with Asperger syndrome have abnormal sensitivity to stimuli, with differences in pain sensation and hearing perhaps most prominent. Loud noises, such as beeping equipment, whirring fans, or buzzing lights may be distressful and should be reduced if possible. Patients may also be strongly affected by bright lights or scents such as perfumes.
Patients may also have an altered sense of taste, with consequences that go beyond simple “picky eating.” Patients should be asked about unusual eating patterns, diets, or food aversions. People with autism spectrum disorders often do not consume adequate vitamin C because of an aversion to fruits and vegetables. Vitamin deficiency may have originated in infancy but may not be identified or treated until adulthood.28
The sense of touch may be intensified, causing patients to be extremely ticklish; they may actually prefer to be touched more firmly. When it is necessary to make physical contact with patients, it will make the process easier if the physician determines their comfort level and finds ways to help them endure the experience with the least amount of discomfort.
Some patients with impaired sensory expression may have a high tolerance for extreme temperatures and pain, leading to delay in seeking aid.29 Patients may downgrade pain levels, masking the severity of an illness or injury.
Transition from pediatric to adult care
Pediatrics is often a warm environment in which children develop a trusting relationship with their care providers. The transition to adult care can be daunting for patients with Asperger syndrome and their families, and many postpone the change for as long as possible.
Although time-consuming, a collaborative effort between the pediatric and adult care teams can dramatically smooth the transition. It can help to have a familiar person from the pediatric team, such as a nurse, be present at the initial interaction with the new adult care team. Both teams should be familiar with the other’s clinical practices and be aware of the patient’s stressors and ways to ameliorate them.30
THE SEARCH FOR A CAUSE CONTINUES
Numerous studies are attempting to understand the anatomic and physiologic causes of autism spectrum disorders, and to find effective treatments and improve the quality of life.
Prenatal factors implicated
Several recent studies have focused on environmental factors during pregnancy as risk factors for autism spectrum disorder. Selective serotonin reuptake inhibitors were found to increase the risk,31 but the severity of the mother’s depressive illness must be considered before counseling against using these drugs. Older maternal or paternal age was also found to increase the risk of an autism spectrum disorder.32 Recent research indicates that older fathers are in particular more likely to have children with disorders such as autism because of an increase in random mutations associated with advanced age.33
Maternal illness during pregnancy is also associated. Preliminary studies found an increased risk of autism if the mother had had a prenatal viral infection.34 A more recent study found that untreated fever during pregnancy rather than a specific viral infection is more strongly linked.35
Maternal antibodies have been implicated as well. One review found that psoriasis is the only maternal autoimmune condition significantly associated with the development of an autism spectrum disorder.36 Elevated levels of antibodies against the fetal brain have been found in mothers with autistic children.37 One study found that autistic children and their siblings have elevated antibrain antibodies in distinct brain regions, including the caudate nucleus, putamen, prefrontal cortex, cerebellum, and cingulate gyrus (why the siblings are spared from having the disorder is unclear).38 Some have questioned whether a child’s own immune system might even be involved.39
Functional magnetic resonance imaging reveals multiple differences
Functional magnetic resonance imaging (fMRI) has been used to investigate impaired social interaction, specific deficits of facial perception and recognition, sensory processing, working memory, and “theory of mind.” Hypoactivation, hyperactivation, and decreased functional connectivity have been observed depending on the mental processes evaluated.40
When undergoing facial perception tasks, subjects with autism spectrum disorders exhibit hypoactivation in the lateral aspect of the middle region of the fusiform gyrus, responsible for face identification. But they have significant activation of the limbic system, specifically the amygdala, during facial recognition. Hypoactivity in the fusiform gyrus is observed when trying to identify faces or read facial expressions.41,42 This cluster of findings helps explain misinterpretations, misidentification, and heightened affect.
A hallmark characteristic of autism is the difficulty patients have in determining intentions and interpreting others’ behavior, thoughts, or emotions. Studies of people with autism spectrum disorders show that areas often responsible for “sensitivity to others” are hypoactive.43 There is also diminished activation in the medial cingulate cortex, normally activated when these people are asked to think about themselves and who they are.44
The resting state in the brains of people with autism spectrum disorders is abnormally activated.45 They are often particularly good at attention to detail but challenged in integrating information needed for general executive functioning. Impaired sensory processing makes it difficult for them to simultaneously interpret multiple sources of sensory input.46
Perhaps some of the most exciting fMRI news comes from infant studies. Radical and axial diffusivity and fractional anisotropy techniques demonstrate differences in the brains of infants 6 to 24 months old, before symptoms of autism spectrum disorders are observed. It is hoped that early intervention could come into play before the syndrome develops fully.47
The synthesis of input of social and emotional cues is sometimes referred to in the literature as “theory of mind.” It is impaired in Asperger syndrome,48 as manifested by a lack of empathy and by challenges in perceiving others’ thoughts and feelings. The basis of impairment may be related to abnormalities in the amygdala.49 Normal awareness involves the integration of multiple neural networks in the anterior paracingulate cortex, the superior temporal sulci, and the temporal poles bilaterally, but different regions appear to be used in patients with Asperger syndrome.50 A small series of five case studies using positron emission tomography indicated that the left prefrontal cortex was the primary location for theory of mind in Asperger syndrome.51
Epilepsy, gastrointestinal problems, and sleep disturbances are associated
About 25% of people with autism spectrum disorders have epilepsy vs 2% to 3% in the general population. Asperger syndrome is associated with a much lower but still elevated risk of 4% to 6%.47,52
Gastrointestinal complaints, most often constipation or chronic diarrhea, are much more common in children with autism spectrum disorders than in the general population. Preliminary data showed that children with an autism spectrum disorder have a 42% rate of gastrointestinal problems vs 12% in unaffected siblings. There is also a correlation between the severity of gastrointestinal problems and severity of autistic symptoms.53
Research is ongoing to determine the prevalence of insomnia or interrupted sleep in those with autism spectrum disorders.54–56 Changes in sleep architecture can explain nighttime activity.
NONTRADITIONAL CONSIDERATIONS
Dietary treatment: Mixed findings
A popular hypothesis is that adherence to a gluten-free or casein-free diet can reduce symptoms of autism spectrum disorders. Preliminary reports identified several cases of children showing improvement.57 However, this has not been replicated, and more studies refute benefits of these diets.58
Essential nutritional needs should be met with any diet, whether it is designed to reduce symptoms or not. Patients with autism spectrum disorders may have strong food aversions, and dietary supplements of vitamins and minerals may be required.
Vaccines do not cause autism
Despite popular concern, recent research indicates that vaccines do not cause autism. Thimerosal, a mercury-based preservative used in childhood vaccines, was at one time implicated as a risk factor for autism spectrum disorders. The US Centers for Disease Control and Prevention (CDC) issued a precaution against using thimerosal-containing vaccines while testing was done to determine the effects on neuropsychological development.59 The CDC study as well as newer studies did not demonstrate that exposure to mercury causes these neuropsychological concerns, but researchers have continued to study the subject.60–62 The original study implicating thimerosal was disproven as scientifically unsound and fraught with conflict of interest and legal concerns. It has since been retracted, and its findings have been completely discredited.63
Other areas of research
Current research is exploring the higher prevalence of autism spectrum disorders in particular families.64–66 Autism and autism spectrum disorders may be caused by hundreds of simultaneous gene alterations or may develop as a result of reduced gene expression in two areas of the cerebral cortex where higher-order processing occurs, in the frontal and temporal lobes.67
Although genetic theories of autism predominate, a 2011 project suggests that environment is also important. A study of twins found that genetics accounted for 40% or less of cases of autism spectrum disorder, with at least 55% of cases being attributable to environmental factors.68
In 1944, Hans Asperger described a subset of children who exhibited “a lack of empathy, little ability to form friendships, one-sided conversation, intense absorption in a special interest, and clumsy movements.”1
In recent years, Asperger syndrome has become increasingly recognized in the medical community and by the general public. It has been popularized in the media in John Elder Robison’s bestselling book, Look Me in the Eye; with the television character Sheldon Cooper in The Big Bang Theory; and in the 2009 film, Adam, a romantic comedy with the title character accurately portraying a young man with Asperger syndrome.
In this article, we discuss the causes and characteristics of Asperger syndrome, with special focus on adults: how it presents, how to treat it, and how to enhance the delivery of care.
PREVALENCE SEEMS TO BE INCREASING
One in 88 children is diagnosed with an autism spectrum disorder, and the rates of Asperger syndrome and other autism spectrum disorders appear to be increasing.2 Whether this increase is the result of more thorough assessment and identification or of environmental changes is hotly debated.3 The rise began before the proposed changes to the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-V) to combine autism, Asperger syndrome, and pervasive developmental disorder not otherwise specified to simplify diagnosis.4 Asperger syndrome affects males three to four times more often than females.5 For most patients, the effects persist throughout life.
BEHAVIORAL IMPAIRMENTS CHARACTERIZE THE SYNDROME
Poor social skills are a hallmark
People with Asperger syndrome struggle with social interaction and face challenges in forming and maintaining relationships. They tend to have less eye contact (often the first indicator), smiling, animated speech, and physical communication such as hand gestures. They tend not to solicit another’s attention to something they themselves find interesting. They often lack social and emotional reciprocity and have difficulty understanding another person’s thoughts or feelings,6 and they have marked difficulty reading social cues. Some adults may appear rigid, selfish, or narrow-minded.
Sometimes behavior is in the normal range but is out of context for a particular situation.7 For example, a preprofessional student with Asperger syndrome might walk into a psychiatric evaluation to assess fitness for duty and take a seat cross-legged on the floor and have a snack. Poor grooming inappropriate for the occasion may also be observed, such as showing up for a formal photo with unkempt hair and in a stained shirt that is half tucked in.
Many adults with autism spectrum disorders are oblivious to their social reputation.8 They are often unaware that their behavior is out of place and only learn that it is not normal when they are told. Others recognize that they have trouble empathizing with or understanding the perspectives of others, but they are at a loss as to how to improve. The syndrome has a tremendous impact on broader aspects of life, such as employment, functional independence, relationships, and social networks.
Other odd behaviors are common
Repetitive behaviors. Many patients with Asperger syndrome have repetitive behaviors, which can manifest as repeating phrases or expressions, attempting to imitate others, and rocking. They tend to follow routines, do not enjoy spontaneity, and are more inflexible and uncomfortable when their planned regimen is altered.
Gait or balance issues may be observed on physical examination.9 Uncoordinated motion and clumsiness are common,10 and some patients may have a bouncy, stilted gait or may walk on their toes, although the latter is more common in children than adults. Many patients have illegible handwriting.11
Fixations. Many Asperger patients have unusual and intense obsessions with subjects like numbers, dates, or aerodynamics of planes. Children with such fascinations are described as “little professors” or as having “geek syndrome.”12 Certain obsessions often continue into adulthood, although one area of interest may fade and another may take over. Such “expertise” in adults may gain them respect, even though they may seem very odd in other ways.
Lack of boundaries. Patients with Asperger syndrome tend to have poor spatial awareness and to be unaware of physical boundaries, standing too close for others’ comfort or unusually far away. Lack of boundaries may extend beyond the physical, as patients may inappropriately help themselves to food or use an item belonging to another without invitation, being unaware that the behavior may be intrusive or inappropriate.
BEHAVIORAL ASSESSMENTS HELP MAKE DIAGNOSIS
Asperger syndrome is most often diagnosed in early childhood, although it may remain undiagnosed into adulthood. Coexisting depression, attention deficit hyperactivity disorder, or anxiety disorders are also often present.
Establishing the diagnosis is aided by information from family members and others who interact with the patient, from the observations of trained professionals, and from self-reported data. However, self-reported assessments are not always reliable, because the syndrome can affect insight.
The most common assessment tool for autism spectrum disorders is the Autism Diagnostic Interview-Revised (ADI-R),13 a battery of tests given in a structured interview to identify and quantify symptoms, determine where a patient falls on the autism spectrum,14 and point toward interventions. The ADI-R also organizes critical developmental history to evaluate if something else is present, such as prodromal schizophrenia. Although the ADI-R can be very useful in the diagnostic process, it is based on parental reporting, which is neither always available nor fully reliable.
A specific diagnostic tool for adults is the Adult Asperger Assessment.15 Patients are asked to complete two screening questionnaires that gauge cognitive function and gather information about thinking, processing, and behavior.
Table 1 lists the criteria for Asperger syndrome from the DSM Fourth Edition, Text Revision (DSM-IV-TR).16 Asperger syndrome differs from general autism in that it is not associated with language delay. In addition, patients with Asperger syndrome usually have average or above-average IQ scores.17 Still, determining whether a patient has Asperger syndrome or high-functioning autism is sometimes challenging.6
In DSM-V, Asperger syndrome will be subsumed under autism spectrum disorder
In 2013, the DSM-V will replace the DSMIV-TR and will combine autism, Asperger syndrome, and pervasive developmental disorder not otherwise classified into a single diagnosis: autism spectrum disorder. The new system uses two instead of the previous three clusters of core symptoms, centered on “social reciprocity and communication” in one arm and “restricted interests and repetitive behavior” in the other.18 There will be less emphasis on play and imagination than in the past. Some authors suggest adding sensory criteria, particularly reduced pain and increased hearing sensitivity.19
The proposed system is sensitive and specific for autism spectrum disorders, allows early diagnosis, and indicates degree of severity.20 It is hoped that the new system, which accounts for the range and severity of symptoms, should help physicians refer patients to the correct level of treatment.
On the other hand, it may be difficult to think of the three disorders as a single diagnosis. Asperger syndrome manifests in distinct ways, and clear behavioral criteria for diagnosis can be invaluable in helping people with the syndrome. Also, the public may continue to refer to it as Asperger syndrome, and parents and patients may feel uncomfortable having it considered to be the same diagnosis as autism.
BEHAVIORAL THERAPY CAN HELP ACHIEVE INDEPENDENCE
Although there is no cure for Asperger syndrome, various interventions can dramatically improve quality of life and independence. The health care team may include a primary care physician, psychologist, psychiatrist, neurologist, and speech therapist.
Behavioral therapies can help patients with Asperger syndrome learn skills to reduce their symptoms. Occupational and physical therapy can improve dexterity, fluidity, and coordination. Desensitization training may help patients adapt to uncomfortable sights, sounds, or smells that may arise. This can be critical in a job situation. For example, while an average person exposed to a foul odor in public is likely to react tactfully, a person with Asperger syndrome may scream loudly, make inappropriate comments, or run from the room. Social training, especially targeted to the workplace, can provide strategies for promoting typical behaviors and be key to maximizing functional independence.
Speech therapists can teach patients how to sound more relaxed and help them master the natural give-and-take of conversational exchange. Psychotherapy can provide a safe place to work on anxiety, express emotions, and manage restricted interests or repeated behaviors. Group therapy or social training can be a venue for learning improved interactions.
Living independently can be very challenging, and patients with Asperger syndrome may need functional independence training to help with a variety of skills, from handling finances to organizing the home.
Improving quality of life includes determining the best learning environments from childhood into college years and beyond.21–23 Socialization can be enhanced with additional social support at home or on campus, through family interactions and collaborative learning, and by teaching empathy.24 Vocational training can be extremely useful.
DRUG THERAPY MAY HAVE A ROLE
Medications are not usually prescribed unless depression or anxiety is also present, but they may also help manage irritability, anger, stereotypical mannerisms, and disturbing movements. Fluoxetine (Prozac) helps reduce repetitive behaviors in adults with Asperger syndrome. Propranolol (Inderal), a well-known antihypertensive, is also used for performance anxiety and improves word fluency, understanding of verbal communication, and verbal problem-solving in patients with an autism spectrum disorder.25
Giving oxytocin (Pitocin) intranasally in a spray formulation is currently being tested to enhance social skills. Patients with an autism spectrum disorder were more able to perceive emotions of others and to respond more appropriately.26 Oxytocin has long been associated with bonding and is believed to enhance mothering skills. It is naturally present in both sexes, but levels are higher in women, which may in part explain the lower rate of autism spectrum disorders in females.27
HEALTH CARE REQUIRES SPECIAL CONSIDERATIONS
Medical care for patients with Asperger syndrome is enhanced by understanding the patient’s experience. Adults, in particular, may have learned to suppress symptoms of Asperger syndrome to better function in society but still experience stress in situations in which others would not. Patients with Asperger syndrome may struggle with social interactions during medical examinations or procedures, and clinicians may find interaction with the patient challenging.
It is important for health care providers to be calm and patient and to understand that anxiety may prevent people with Asperger syndrome from making eye contact. The clinician should confirm that a patient is engaged but should avoid seeming pushy or invasive.
When anxious, patients may employ strange gestures that they find soothing, such as flapping the hands, rocking, or cracking the knuckles. It is usually easier to allow them to continue unless the activity hinders the examination or treatment.
Patients are likely to respond better to direct requests than to subtle questions: eg, “Open your mouth, please” instead of “Could you open your mouth?” Using clear, specific language and avoiding metaphors, irony, and nonverbal communication are best. It is important to explicitly ask for everything needed, as patients may not volunteer information and may have trouble articulating what they are thinking or feeling. While educating patients about their health needs, physicians may need to reiterate guidance several times or approach the same topic from different angles in order for the patient to accept a concern.
All actions, especially touching the patient, should be explained clearly beforehand. If possible, the doctor should demonstrate using visuals or on his or her own body if appropriate. For invasive procedures, anesthetizing the local area is recommended.
People with Asperger syndrome often rely heavily on a regular routine to maintain a sense of organization. By interrupting this routine, a doctor’s visit can induce anxiety. Waiting also increases anxiety, so scheduling patients with Asperger syndrome either first or last in the day may help.
Hypersensitivity poses challenges
Many people with Asperger syndrome have abnormal sensitivity to stimuli, with differences in pain sensation and hearing perhaps most prominent. Loud noises, such as beeping equipment, whirring fans, or buzzing lights may be distressful and should be reduced if possible. Patients may also be strongly affected by bright lights or scents such as perfumes.
Patients may also have an altered sense of taste, with consequences that go beyond simple “picky eating.” Patients should be asked about unusual eating patterns, diets, or food aversions. People with autism spectrum disorders often do not consume adequate vitamin C because of an aversion to fruits and vegetables. Vitamin deficiency may have originated in infancy but may not be identified or treated until adulthood.28
The sense of touch may be intensified, causing patients to be extremely ticklish; they may actually prefer to be touched more firmly. When it is necessary to make physical contact with patients, it will make the process easier if the physician determines their comfort level and finds ways to help them endure the experience with the least amount of discomfort.
Some patients with impaired sensory expression may have a high tolerance for extreme temperatures and pain, leading to delay in seeking aid.29 Patients may downgrade pain levels, masking the severity of an illness or injury.
Transition from pediatric to adult care
Pediatrics is often a warm environment in which children develop a trusting relationship with their care providers. The transition to adult care can be daunting for patients with Asperger syndrome and their families, and many postpone the change for as long as possible.
Although time-consuming, a collaborative effort between the pediatric and adult care teams can dramatically smooth the transition. It can help to have a familiar person from the pediatric team, such as a nurse, be present at the initial interaction with the new adult care team. Both teams should be familiar with the other’s clinical practices and be aware of the patient’s stressors and ways to ameliorate them.30
THE SEARCH FOR A CAUSE CONTINUES
Numerous studies are attempting to understand the anatomic and physiologic causes of autism spectrum disorders, and to find effective treatments and improve the quality of life.
Prenatal factors implicated
Several recent studies have focused on environmental factors during pregnancy as risk factors for autism spectrum disorder. Selective serotonin reuptake inhibitors were found to increase the risk,31 but the severity of the mother’s depressive illness must be considered before counseling against using these drugs. Older maternal or paternal age was also found to increase the risk of an autism spectrum disorder.32 Recent research indicates that older fathers are in particular more likely to have children with disorders such as autism because of an increase in random mutations associated with advanced age.33
Maternal illness during pregnancy is also associated. Preliminary studies found an increased risk of autism if the mother had had a prenatal viral infection.34 A more recent study found that untreated fever during pregnancy rather than a specific viral infection is more strongly linked.35
Maternal antibodies have been implicated as well. One review found that psoriasis is the only maternal autoimmune condition significantly associated with the development of an autism spectrum disorder.36 Elevated levels of antibodies against the fetal brain have been found in mothers with autistic children.37 One study found that autistic children and their siblings have elevated antibrain antibodies in distinct brain regions, including the caudate nucleus, putamen, prefrontal cortex, cerebellum, and cingulate gyrus (why the siblings are spared from having the disorder is unclear).38 Some have questioned whether a child’s own immune system might even be involved.39
Functional magnetic resonance imaging reveals multiple differences
Functional magnetic resonance imaging (fMRI) has been used to investigate impaired social interaction, specific deficits of facial perception and recognition, sensory processing, working memory, and “theory of mind.” Hypoactivation, hyperactivation, and decreased functional connectivity have been observed depending on the mental processes evaluated.40
When undergoing facial perception tasks, subjects with autism spectrum disorders exhibit hypoactivation in the lateral aspect of the middle region of the fusiform gyrus, responsible for face identification. But they have significant activation of the limbic system, specifically the amygdala, during facial recognition. Hypoactivity in the fusiform gyrus is observed when trying to identify faces or read facial expressions.41,42 This cluster of findings helps explain misinterpretations, misidentification, and heightened affect.
A hallmark characteristic of autism is the difficulty patients have in determining intentions and interpreting others’ behavior, thoughts, or emotions. Studies of people with autism spectrum disorders show that areas often responsible for “sensitivity to others” are hypoactive.43 There is also diminished activation in the medial cingulate cortex, normally activated when these people are asked to think about themselves and who they are.44
The resting state in the brains of people with autism spectrum disorders is abnormally activated.45 They are often particularly good at attention to detail but challenged in integrating information needed for general executive functioning. Impaired sensory processing makes it difficult for them to simultaneously interpret multiple sources of sensory input.46
Perhaps some of the most exciting fMRI news comes from infant studies. Radical and axial diffusivity and fractional anisotropy techniques demonstrate differences in the brains of infants 6 to 24 months old, before symptoms of autism spectrum disorders are observed. It is hoped that early intervention could come into play before the syndrome develops fully.47
The synthesis of input of social and emotional cues is sometimes referred to in the literature as “theory of mind.” It is impaired in Asperger syndrome,48 as manifested by a lack of empathy and by challenges in perceiving others’ thoughts and feelings. The basis of impairment may be related to abnormalities in the amygdala.49 Normal awareness involves the integration of multiple neural networks in the anterior paracingulate cortex, the superior temporal sulci, and the temporal poles bilaterally, but different regions appear to be used in patients with Asperger syndrome.50 A small series of five case studies using positron emission tomography indicated that the left prefrontal cortex was the primary location for theory of mind in Asperger syndrome.51
Epilepsy, gastrointestinal problems, and sleep disturbances are associated
About 25% of people with autism spectrum disorders have epilepsy vs 2% to 3% in the general population. Asperger syndrome is associated with a much lower but still elevated risk of 4% to 6%.47,52
Gastrointestinal complaints, most often constipation or chronic diarrhea, are much more common in children with autism spectrum disorders than in the general population. Preliminary data showed that children with an autism spectrum disorder have a 42% rate of gastrointestinal problems vs 12% in unaffected siblings. There is also a correlation between the severity of gastrointestinal problems and severity of autistic symptoms.53
Research is ongoing to determine the prevalence of insomnia or interrupted sleep in those with autism spectrum disorders.54–56 Changes in sleep architecture can explain nighttime activity.
NONTRADITIONAL CONSIDERATIONS
Dietary treatment: Mixed findings
A popular hypothesis is that adherence to a gluten-free or casein-free diet can reduce symptoms of autism spectrum disorders. Preliminary reports identified several cases of children showing improvement.57 However, this has not been replicated, and more studies refute benefits of these diets.58
Essential nutritional needs should be met with any diet, whether it is designed to reduce symptoms or not. Patients with autism spectrum disorders may have strong food aversions, and dietary supplements of vitamins and minerals may be required.
Vaccines do not cause autism
Despite popular concern, recent research indicates that vaccines do not cause autism. Thimerosal, a mercury-based preservative used in childhood vaccines, was at one time implicated as a risk factor for autism spectrum disorders. The US Centers for Disease Control and Prevention (CDC) issued a precaution against using thimerosal-containing vaccines while testing was done to determine the effects on neuropsychological development.59 The CDC study as well as newer studies did not demonstrate that exposure to mercury causes these neuropsychological concerns, but researchers have continued to study the subject.60–62 The original study implicating thimerosal was disproven as scientifically unsound and fraught with conflict of interest and legal concerns. It has since been retracted, and its findings have been completely discredited.63
Other areas of research
Current research is exploring the higher prevalence of autism spectrum disorders in particular families.64–66 Autism and autism spectrum disorders may be caused by hundreds of simultaneous gene alterations or may develop as a result of reduced gene expression in two areas of the cerebral cortex where higher-order processing occurs, in the frontal and temporal lobes.67
Although genetic theories of autism predominate, a 2011 project suggests that environment is also important. A study of twins found that genetics accounted for 40% or less of cases of autism spectrum disorder, with at least 55% of cases being attributable to environmental factors.68
- Frith U, editor. Autism and Asperger Syndrome. New York: Cambridge University Press, 1991:37–92.
- Autism and Developmental Disabilities Monitoring Network Surveillance Year 2008 Principal Investigators. Prevalence of autism spectrum disorders—Autism and Developmental Disabilities Monitoring Network, 14 sites, United States, 2008. MMWR Surveill Summ 2012; 61( 3):1–19.
- Rutter M. Incidence of autism spectrum disorders: changes over time and their meaning. Acta Paediatr 2005; 94:2–15.
- Happé F. Criteria, categories, and continua: autism and related disorders in DSM-5. J Am Acad Child Adolesc Psychiatry 2011; 50:540–542.
- National Institute of Neurological Disorders and Stroke. Asperger syndrome fact sheet. http://www.ninds.nih.gov/disorders/asperger/detail_asperger.htm. Accessed October 11, 2012.
- Toth K, King BH. Asperger’s syndrome: diagnosis and treatment. Am J Psychiatry 2008; 165:958–963.
- Vermeulen P. Autism: from mind blindness to context blindness. Asperger’s Digest November/December 2011. http://autismdigest.com/autism-from-mind-blindness-to-context-blindness/. Accessed October 11, 2012.
- Izuma K, Matsumoto K, Camerer CF, Adolphs R. Insensitivity to social reputation in autism. Proc Natl Acad Sci U S A. 2011; 108:17302–17307.
- Weimer AK, Schatz AM, Lincoln A, Ballantyne AO, Trauner DA. “Motor” impairment in Asperger’s syndrome: evidence for a deficit in proprioception. J Dev Behav Pediatr 2001; 22:92–101.
- Siaperas P, Ring HA, McAllister CJ, et al. Atypical movement performance and sensory integration in Asperger’s syndrome. J Autism Dev Disord 2012; 42:718–725.
- Kushki A, Chau T, Anagnostou E. Handwriting difficulties in children with autism spectrum disorders: a scoping review. J Autism Dev Disord 2011; 41:1706–1716.
- Nash JM, Bonesteel A. The geek syndrome. Time Magazine U.S. 2002. http://www.time.com/time/magazine/article/0,9171,1002365-1,00.html. Accessed October 11, 2012.
- Le Couteur A, Rutter M, Lord C, et al. Autism diagnostic interview: a standardized investigatorbased instrument. J Autism Dev Disord 1989; 19:363–387.
- Rutter M, Le Couteur A, Lord C. Autism Diagnostic Interview-Revised WPS Edition Manual. Los Angeles, CA. Western Psychological Services; 2003.
- Baron-Cohen S, Wheelwright S, Robinson J, Woodbury-Smith M. The Adult Asperger’s Assessment (AAA): a diagnostic method. J Autism Developmental Disord 2005; 35:807–819.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders Text Revision DSM IV–TR 4th Ed. 2000; Washington, DC: American Psychiatric Association; 2000:80–84.
- Centers for Disease Control. Asperger syndrome fact sheet. http://www.cdc.gov/ncbddd/actearly/pdf/parents_pdfs/Asperger_Syndrome.pdf. Accessed October 11, 2012.
- Peckham C. The current state in autism—still tough to treat but encouraging progress. An expert interview with Fred R. Volkmar, MD. Medscape Pediatrics 2010. http://www.medscape.com/viewarticle/720802?src=mp&spon=17. Accessed October 31, 2012.
- Muscari ME. How should I evaluate an adult for possible Asperger’s syndrome? Medscape News Today 2006.
- Hollander E. Can we treat core symptoms of autism spectrum disorders in adults? December 21, 2011; 1( 18). http://www.medscape.com/viewarticle/531750. Accessed October 1, 2012.
- Müller E, Schuler A, Yates GB. Social challenges and supports from the perspective of individuals with Asperger’s syndrome and other autism spectrum disabilities. Autism 2008; 12:173–190.
- Helman T, Berger O. Parents of children with Asperger’s syndrome or with learning disabilities: family environment and social support. Res Dev Disabil 2008; 29;289–300.
- Taylor CM. Campus commons. When pigs fly: a new perspective on learning. About Campus 2011; 16:30–32.
- Cheng Y, Chiang H, Ye J, Cheng L. Enhancing empathy instruction using a collaborative virtual learning environment for children with autistic spectrum conditions. Comput Edu 2010; 55:1449–1458.
- Beversdorf DQ, Saklayen S, Higgins KF, Bodner KE, Kanne SM, Christ SE. Effect of propranolol on word fluency in autism. Cogn Behav Neurol 2011; 24:11–17.
- Kuehn BM. Scientists probe oxytocin therapy for social deficits in autism, schizophrenia. JAMA 2011; 305:659–661.
- Pfaff DW, Rapin I, Goldman S. Male dominance in autism: neuroendocrine influences on arousal and social anxiety. Autism Res 2011; 4:163–176.
- Brauser D. Children with autism routinely exhibit feeding difficulties in infancy. Medscape Medical News 2010. http://www.medscape.org/viewarticle/726060. Accessed October 31, 2012.
- Baron MG, Groden J, Groden G, Lipsitt L. Stress and coping in autism. New York: Oxford University Press; 2006:355.
- Camfield P, Camfield C. Transition to adult care for children with chronic neurological disorders. Ann Neurol 2001; 69:437–444.
- Croen LA, Grether JK, Yoshida CK, Odouli R, Hendrick V. Antidepressant use during pregnancy and childhood autism spectrum disorders. Arch Gen Psychiatry 2011; 68:1104–1112.
- Croen LA, Najjar DV, Fireman B, Grether JK. Maternal and paternal age and risk of autism spectrum disorders. Arch Pediatr Adolesc Med 2007; 161:334–340.
- Kong A, Frigge ML, Masson G, et al. Rate of de novo mutations and the importance of father’s age to disease risk. Nature 2012; 488:471–475.
- Atlandóttir HO, Thorsen P, Østergaard L, et al. Maternal infection requiring hospitalization during pregnancy and autism spectrum disorders. J Autism Dev Disord 2010; 40:1423–1430.
- Zerbo O, Iosif A-M, Walker C, Ozonoff S, Hansen RL, Hertz-Picciotto I. Is maternal influenza or fever during pregnancy associated with autism or developmental delays? Results from the CHARGE (CHildhood Autism Risks from Genetics and Environment) study. J Autism Dev Disord 2012; 10.1007/s10803-012-1540-x.
- Crown LA, Grether JK, Yoshida CK, Odouli R, Van de Water J. Maternal autoimmune diseases, asthma and allergies, and childhood autism spectrum disorders: a case-control study. Arch Pediatr Adolesc Med 2005; 159:151–157.
- Singer HS, Morris CM, Gause CD, Gillin PK, Crawford S, Zimmerman AW. Antibodies against fetal brain in sera of mothers with autistic children. J Neruoimmunol 2008; 194:165–172.
- Singer HS, Morris CM, Williams PN, Yoon DY, Hong JJ, Zimmerman AW. Antibrain antibodies in children with autism and their unaffected siblings. J Neuroimmunol 2006; 178:149–155.
- Ashwood P, Van de Water J. Is autism an autoimmune disease? Autoimmunity Rev 2004; 3:557–562.
- South M, Diehl JJ. Functional magnetic resonance imaging. In:Hollander E, Kolevzon A, Coyle J, editors. Textbook of Autism Spectrum Disorders. Washington, DC: American Psychiatric Publishing; 2011:409–414.
- Shultz RT, Gauthier I, Klin A, et al. Abnormal ventral temporal cortical activity during face discrimination among individuals with autism and Asperger syndrome. Arch Gen Psychiatry 2000; 57:331–340.
- Wang AT, Dapretto M, Hariri AR, et al. Neural correlates of facial affect processing in children and adolescents with autism spectrum disorder. J Am Acad Child Adolesc Psychiatry 2004; 43:481–490.
- Mason RA, Williams DL, Kana RK, et al. Theory of mind disruption and recruitment of the right hemisphere during narrative comprehension in autism. Neuropsychologia 2008; 46:269–280.
- Chiu PH, Kayali MA, Kishida KT, et al. Self responses along cingulate cortex reveal quantitative neural phenotype for high-functioning autism. Neuron 2008; 57:463–437.
- Kennedy DP, Redcay E, Courchesne E. Failing to deactivate: resting functional abnormalities in autism. Proc Natl Acad Sci U S A 2006; 103:8275–8280.
- Bölte S, Hubl D, Dierks T, et al. An fMRI-study of locally oriented perception in autism: altered early visual processing of the block design test. J Neural Transm 2008; 115:545–552.
- Maski KP, Jeste SS, Spencer SJ. Common neurological co-morbidities in autism spectrum disorders. Curr Opin Pediatr 2011; 23:609–615.
- Kleinman J, Marciano P, Ault RL. Advanced theory of mind in high functioning adults with autism. J Autism Dev Disord 2011; 31:29–36.
- Fine C, Lumsden J, Blair RJ. Dissociation between ‘theory of mind and executive functions in a patient with early left amygdala damage. Brain 2001; 124:287–298.
- Gallagher HL, Frith CD. Functional imaging of ‘theory of mind.’ Trends Cogn Sci 2003; 7:77–83.
- Happé F, Ehlers S, Pletcher P, et al. ‘Theory of mind’ in the brain. Evidence from a PET scan study of Asperger’s syndrome. Neuroreport 1996; 8:197–207.
- Kugimiya S. Clinical features and possible correlations between autism and epilepsy. Neurology Asia 2010; 15(suppl 1):44–45.
- Wang LW, Tancredi DJ, Thomas DW. The prevalence of gastrointestinal problems in children across the United States with autism spectrum disorders from families with multiple affected members. J Dev Behav Pediatr 2011; 32:351–360.
- Bruni O, Ferri R, Vittori E, et al. Sleep architecture and NREM alterations in children and adolescents with Asperger syndrome. Sleep 2007; 30:1577–1585.
- Richdale AL, Schreck KA. Sleep problems in autism spectrum disorders: prevalence, nature, & possible biopsychosocial aetiologies. Sleep Med Rev 2009; 13:403–411.
- Paavonen EJ, Vehkalahti K, Vanhala R, von Wendt L, Nieminen-von Wendt T, Aronen ET. Sleep in children with Asperger’s syndrome. J Autism Dev Disord 2007; 38:41–51.
- Elder JH, Shankar M, Shuster J, Theriaque D, Burns S, Sherrill L. The gluten-free, casein-free diet in autism: results of a preliminary double blind clinical trial. J Autism Dev Disord 2006; 36:413–420.
- Keller DM. Diet free of gluten and casein has no effect on autism symptoms. Medscape News May 24, 2010. http://www.medscape.com/viewarticle/722283.
- Centers for Disease Control and Prevention (CDC). Recommendations regarding the use of vaccines that contain thimerosal as a preservative. MMWR Morb Mortal Wkly Rep 1999; 48:996–998.
- Thompson WW, Price C, Goodson B, et al; Vaccine Safety Datalink Team. Early thimerosal exposure and neuropsychological outcomes at 7 to 10 years. N Engl J Med 2007; 357:1281–1292.
- Price CS, Thompson WW, Goodson B, et al. Prenatal and infant exposure to thimerosal from vaccines and immunoglobulins and risk of autism. Pediatrics 2010; 126:656–664.
- Centers for Disease Control and Prevention (CDC). CDC study on “Prenatal and infant exposure to thimerosal from vaccines and immunoglobulins and risk of autism.” www.cdc.gov/vaccinesafety/Concerns/Thimerosal/QA_Pediatrics-thimerosal-autism.html. Accessed November 5, 2012.
- Deer B. How the case against the MMR vaccine was fixed. BMJ 2011; 342:c5347.
- Losh M, Sullivan PF, Trembath D, Piven J. Current developments in the genetics of autism: from phenome to genome. J Neuropathol Exp Neurol 2008; 67:829–837.
- Curran S, Bolton P. Genetics of autism. In:Kim Y-K, editor. Handbook of Behavior Genetics, Part IV. New York, NY: Springer; 2009:397–410.
- State MW. The genetics of child psychiatric disorders: focus on autism and Tourette syndrome. Neuron 2010; 68:254–269.
- Voineagu I, Wang X, Johnston P, et al. Transcriptomic analysis of autistic brain reveals convergent molecular pathology. Nature 2011; 474:380–384.
- Hallmayer J, Cleveland S, Torres A, et al. Genetic heritability and shared environmental factors among twin pairs with autism. Arch Gen Psychiatry 2011; 68:1095–1102.
- Frith U, editor. Autism and Asperger Syndrome. New York: Cambridge University Press, 1991:37–92.
- Autism and Developmental Disabilities Monitoring Network Surveillance Year 2008 Principal Investigators. Prevalence of autism spectrum disorders—Autism and Developmental Disabilities Monitoring Network, 14 sites, United States, 2008. MMWR Surveill Summ 2012; 61( 3):1–19.
- Rutter M. Incidence of autism spectrum disorders: changes over time and their meaning. Acta Paediatr 2005; 94:2–15.
- Happé F. Criteria, categories, and continua: autism and related disorders in DSM-5. J Am Acad Child Adolesc Psychiatry 2011; 50:540–542.
- National Institute of Neurological Disorders and Stroke. Asperger syndrome fact sheet. http://www.ninds.nih.gov/disorders/asperger/detail_asperger.htm. Accessed October 11, 2012.
- Toth K, King BH. Asperger’s syndrome: diagnosis and treatment. Am J Psychiatry 2008; 165:958–963.
- Vermeulen P. Autism: from mind blindness to context blindness. Asperger’s Digest November/December 2011. http://autismdigest.com/autism-from-mind-blindness-to-context-blindness/. Accessed October 11, 2012.
- Izuma K, Matsumoto K, Camerer CF, Adolphs R. Insensitivity to social reputation in autism. Proc Natl Acad Sci U S A. 2011; 108:17302–17307.
- Weimer AK, Schatz AM, Lincoln A, Ballantyne AO, Trauner DA. “Motor” impairment in Asperger’s syndrome: evidence for a deficit in proprioception. J Dev Behav Pediatr 2001; 22:92–101.
- Siaperas P, Ring HA, McAllister CJ, et al. Atypical movement performance and sensory integration in Asperger’s syndrome. J Autism Dev Disord 2012; 42:718–725.
- Kushki A, Chau T, Anagnostou E. Handwriting difficulties in children with autism spectrum disorders: a scoping review. J Autism Dev Disord 2011; 41:1706–1716.
- Nash JM, Bonesteel A. The geek syndrome. Time Magazine U.S. 2002. http://www.time.com/time/magazine/article/0,9171,1002365-1,00.html. Accessed October 11, 2012.
- Le Couteur A, Rutter M, Lord C, et al. Autism diagnostic interview: a standardized investigatorbased instrument. J Autism Dev Disord 1989; 19:363–387.
- Rutter M, Le Couteur A, Lord C. Autism Diagnostic Interview-Revised WPS Edition Manual. Los Angeles, CA. Western Psychological Services; 2003.
- Baron-Cohen S, Wheelwright S, Robinson J, Woodbury-Smith M. The Adult Asperger’s Assessment (AAA): a diagnostic method. J Autism Developmental Disord 2005; 35:807–819.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders Text Revision DSM IV–TR 4th Ed. 2000; Washington, DC: American Psychiatric Association; 2000:80–84.
- Centers for Disease Control. Asperger syndrome fact sheet. http://www.cdc.gov/ncbddd/actearly/pdf/parents_pdfs/Asperger_Syndrome.pdf. Accessed October 11, 2012.
- Peckham C. The current state in autism—still tough to treat but encouraging progress. An expert interview with Fred R. Volkmar, MD. Medscape Pediatrics 2010. http://www.medscape.com/viewarticle/720802?src=mp&spon=17. Accessed October 31, 2012.
- Muscari ME. How should I evaluate an adult for possible Asperger’s syndrome? Medscape News Today 2006.
- Hollander E. Can we treat core symptoms of autism spectrum disorders in adults? December 21, 2011; 1( 18). http://www.medscape.com/viewarticle/531750. Accessed October 1, 2012.
- Müller E, Schuler A, Yates GB. Social challenges and supports from the perspective of individuals with Asperger’s syndrome and other autism spectrum disabilities. Autism 2008; 12:173–190.
- Helman T, Berger O. Parents of children with Asperger’s syndrome or with learning disabilities: family environment and social support. Res Dev Disabil 2008; 29;289–300.
- Taylor CM. Campus commons. When pigs fly: a new perspective on learning. About Campus 2011; 16:30–32.
- Cheng Y, Chiang H, Ye J, Cheng L. Enhancing empathy instruction using a collaborative virtual learning environment for children with autistic spectrum conditions. Comput Edu 2010; 55:1449–1458.
- Beversdorf DQ, Saklayen S, Higgins KF, Bodner KE, Kanne SM, Christ SE. Effect of propranolol on word fluency in autism. Cogn Behav Neurol 2011; 24:11–17.
- Kuehn BM. Scientists probe oxytocin therapy for social deficits in autism, schizophrenia. JAMA 2011; 305:659–661.
- Pfaff DW, Rapin I, Goldman S. Male dominance in autism: neuroendocrine influences on arousal and social anxiety. Autism Res 2011; 4:163–176.
- Brauser D. Children with autism routinely exhibit feeding difficulties in infancy. Medscape Medical News 2010. http://www.medscape.org/viewarticle/726060. Accessed October 31, 2012.
- Baron MG, Groden J, Groden G, Lipsitt L. Stress and coping in autism. New York: Oxford University Press; 2006:355.
- Camfield P, Camfield C. Transition to adult care for children with chronic neurological disorders. Ann Neurol 2001; 69:437–444.
- Croen LA, Grether JK, Yoshida CK, Odouli R, Hendrick V. Antidepressant use during pregnancy and childhood autism spectrum disorders. Arch Gen Psychiatry 2011; 68:1104–1112.
- Croen LA, Najjar DV, Fireman B, Grether JK. Maternal and paternal age and risk of autism spectrum disorders. Arch Pediatr Adolesc Med 2007; 161:334–340.
- Kong A, Frigge ML, Masson G, et al. Rate of de novo mutations and the importance of father’s age to disease risk. Nature 2012; 488:471–475.
- Atlandóttir HO, Thorsen P, Østergaard L, et al. Maternal infection requiring hospitalization during pregnancy and autism spectrum disorders. J Autism Dev Disord 2010; 40:1423–1430.
- Zerbo O, Iosif A-M, Walker C, Ozonoff S, Hansen RL, Hertz-Picciotto I. Is maternal influenza or fever during pregnancy associated with autism or developmental delays? Results from the CHARGE (CHildhood Autism Risks from Genetics and Environment) study. J Autism Dev Disord 2012; 10.1007/s10803-012-1540-x.
- Crown LA, Grether JK, Yoshida CK, Odouli R, Van de Water J. Maternal autoimmune diseases, asthma and allergies, and childhood autism spectrum disorders: a case-control study. Arch Pediatr Adolesc Med 2005; 159:151–157.
- Singer HS, Morris CM, Gause CD, Gillin PK, Crawford S, Zimmerman AW. Antibodies against fetal brain in sera of mothers with autistic children. J Neruoimmunol 2008; 194:165–172.
- Singer HS, Morris CM, Williams PN, Yoon DY, Hong JJ, Zimmerman AW. Antibrain antibodies in children with autism and their unaffected siblings. J Neuroimmunol 2006; 178:149–155.
- Ashwood P, Van de Water J. Is autism an autoimmune disease? Autoimmunity Rev 2004; 3:557–562.
- South M, Diehl JJ. Functional magnetic resonance imaging. In:Hollander E, Kolevzon A, Coyle J, editors. Textbook of Autism Spectrum Disorders. Washington, DC: American Psychiatric Publishing; 2011:409–414.
- Shultz RT, Gauthier I, Klin A, et al. Abnormal ventral temporal cortical activity during face discrimination among individuals with autism and Asperger syndrome. Arch Gen Psychiatry 2000; 57:331–340.
- Wang AT, Dapretto M, Hariri AR, et al. Neural correlates of facial affect processing in children and adolescents with autism spectrum disorder. J Am Acad Child Adolesc Psychiatry 2004; 43:481–490.
- Mason RA, Williams DL, Kana RK, et al. Theory of mind disruption and recruitment of the right hemisphere during narrative comprehension in autism. Neuropsychologia 2008; 46:269–280.
- Chiu PH, Kayali MA, Kishida KT, et al. Self responses along cingulate cortex reveal quantitative neural phenotype for high-functioning autism. Neuron 2008; 57:463–437.
- Kennedy DP, Redcay E, Courchesne E. Failing to deactivate: resting functional abnormalities in autism. Proc Natl Acad Sci U S A 2006; 103:8275–8280.
- Bölte S, Hubl D, Dierks T, et al. An fMRI-study of locally oriented perception in autism: altered early visual processing of the block design test. J Neural Transm 2008; 115:545–552.
- Maski KP, Jeste SS, Spencer SJ. Common neurological co-morbidities in autism spectrum disorders. Curr Opin Pediatr 2011; 23:609–615.
- Kleinman J, Marciano P, Ault RL. Advanced theory of mind in high functioning adults with autism. J Autism Dev Disord 2011; 31:29–36.
- Fine C, Lumsden J, Blair RJ. Dissociation between ‘theory of mind and executive functions in a patient with early left amygdala damage. Brain 2001; 124:287–298.
- Gallagher HL, Frith CD. Functional imaging of ‘theory of mind.’ Trends Cogn Sci 2003; 7:77–83.
- Happé F, Ehlers S, Pletcher P, et al. ‘Theory of mind’ in the brain. Evidence from a PET scan study of Asperger’s syndrome. Neuroreport 1996; 8:197–207.
- Kugimiya S. Clinical features and possible correlations between autism and epilepsy. Neurology Asia 2010; 15(suppl 1):44–45.
- Wang LW, Tancredi DJ, Thomas DW. The prevalence of gastrointestinal problems in children across the United States with autism spectrum disorders from families with multiple affected members. J Dev Behav Pediatr 2011; 32:351–360.
- Bruni O, Ferri R, Vittori E, et al. Sleep architecture and NREM alterations in children and adolescents with Asperger syndrome. Sleep 2007; 30:1577–1585.
- Richdale AL, Schreck KA. Sleep problems in autism spectrum disorders: prevalence, nature, & possible biopsychosocial aetiologies. Sleep Med Rev 2009; 13:403–411.
- Paavonen EJ, Vehkalahti K, Vanhala R, von Wendt L, Nieminen-von Wendt T, Aronen ET. Sleep in children with Asperger’s syndrome. J Autism Dev Disord 2007; 38:41–51.
- Elder JH, Shankar M, Shuster J, Theriaque D, Burns S, Sherrill L. The gluten-free, casein-free diet in autism: results of a preliminary double blind clinical trial. J Autism Dev Disord 2006; 36:413–420.
- Keller DM. Diet free of gluten and casein has no effect on autism symptoms. Medscape News May 24, 2010. http://www.medscape.com/viewarticle/722283.
- Centers for Disease Control and Prevention (CDC). Recommendations regarding the use of vaccines that contain thimerosal as a preservative. MMWR Morb Mortal Wkly Rep 1999; 48:996–998.
- Thompson WW, Price C, Goodson B, et al; Vaccine Safety Datalink Team. Early thimerosal exposure and neuropsychological outcomes at 7 to 10 years. N Engl J Med 2007; 357:1281–1292.
- Price CS, Thompson WW, Goodson B, et al. Prenatal and infant exposure to thimerosal from vaccines and immunoglobulins and risk of autism. Pediatrics 2010; 126:656–664.
- Centers for Disease Control and Prevention (CDC). CDC study on “Prenatal and infant exposure to thimerosal from vaccines and immunoglobulins and risk of autism.” www.cdc.gov/vaccinesafety/Concerns/Thimerosal/QA_Pediatrics-thimerosal-autism.html. Accessed November 5, 2012.
- Deer B. How the case against the MMR vaccine was fixed. BMJ 2011; 342:c5347.
- Losh M, Sullivan PF, Trembath D, Piven J. Current developments in the genetics of autism: from phenome to genome. J Neuropathol Exp Neurol 2008; 67:829–837.
- Curran S, Bolton P. Genetics of autism. In:Kim Y-K, editor. Handbook of Behavior Genetics, Part IV. New York, NY: Springer; 2009:397–410.
- State MW. The genetics of child psychiatric disorders: focus on autism and Tourette syndrome. Neuron 2010; 68:254–269.
- Voineagu I, Wang X, Johnston P, et al. Transcriptomic analysis of autistic brain reveals convergent molecular pathology. Nature 2011; 474:380–384.
- Hallmayer J, Cleveland S, Torres A, et al. Genetic heritability and shared environmental factors among twin pairs with autism. Arch Gen Psychiatry 2011; 68:1095–1102.
KEY POINTS
- Indicators of Asperger syndrome include lack of eye contact, inappropriate comments, odd posture, high anxiety, and intensely focused interests.
- Asperger syndrome is evident in childhood, but it also presents undiagnosed in adulthood.
- Physicians should be aware of patients’ social differences and increased sensitivities in order to improve health care delivery.
- Episodic cognitive behavioral therapy addressing interpersonal skills can dramatically improve quality of life and independence.
- Proposed diagnostic changes scheduled to take effect in 2013 involve including Asperger syndrome as an autism spectrum disorder.
Depression and heart disease: What do we know, and where are we headed?
Depression is a risk factor for heart disease, and in patients with heart disease, it is a risk factor for complications and death. Unfortunately, in the trials performed to date, treating depression in cardiac patients did not lead to lower rates of recurrent cardiovascular events or death. Nevertheless, we recommend that clinicians systematically screen for it in their heart patients, in view of the benefits of antidepressant therapy.
In this article we review key epidemiologic and psychosocial studies, the mechanistic links between depression and heart disease, and recent intervention trials. We also offer practical management advice and address the continued need for guidelines and risk stratification in the treatment of depressed cardiac patients.
After we submitted our review article, the American Heart Association (AHA)1 released a consensus document recommending that health care providers screen for and treat depression in patients with coronary heart disease. We will discuss the same screening tests that have been recommended by the AHA.
DEPRESSION AND HEART DISEASE: COMMON AND LINKED
Depression and heart disease are very common and often coexist: the prevalence of depression in various heart conditions ranges from 15% to 20%.1–3 According to data from the World Health Organization, by the year 2020 depression will be the second-leading cause of disability in developed countries (after heart disease).4
The World Health Survey5 showed that depression worsens health more than angina, arthritis, asthma, or diabetes. Furthermore, patients with severe mental illness have a higher risk of dying from heart disease and stroke.6
SOME HEART DISEASE RISK FACTORS ARE PSYCHOSOCIAL
In the 1980s, the “type A” personality (ambitious, aggressive, hostile, and competitive, with a chronic sense of urgency) was linked to heart disease.7 Later studies differed as to whether the entire set of features is valid as a collective risk factor for progressive heart disease,8 but hostility remains a validated risk factor and a focus of behavior modification.9,10
Other psychosocial risk factors have been implicated,11,12 one of which is social isolation.9,13 Another is the “type D” personality, which includes a tendency to experience negative emotions across time and situations coupled with social inhibition and which is believed to be more valid than the type A personality as a risk factor for cardiac disease.14,15
The INTERHEART study16 gathered data about attributable risk in the development of myocardial infarction (MI) in 52 countries in a case-control fashion. Psychosocial factors including stress, low generalized locus of control (ie, the perceived inability to control one’s life), and depression accounted for 32.5% of the attributable risk for an MI.17 This would mean that they account for slightly less attributable risk than that of lifetime smoking but more than that of hypertension and obesity.
Job stress increases the risk of initial coronary heart disease18 and also the risk of recurrent cardiac events after a first MI.19 Even though numerous psychosocial risk factors have been associated with coronary heart disease, including anxiety,20,21 depression is perhaps the best studied.
PROSPECTIVE STUDIES OF DEPRESSION AND HEART DISEASE
To examine the impact of depression in coronary heart disease, prospective studies have been done in healthy people and in patients with established cardiovascular disease who develop depression.22
In healthy people, depression increases the risk of coronary disease
The 1996 Epidemiologic Catchment Area study23 found that people with major depression had a risk of MI four times higher than the norm, and people with 2 weeks of sadness or dysphoria had a risk two times higher.
A subsequent meta-analysis of 11 studies,24 which included 36,000 patients, found that the overall relative risk of developing heart disease in depressed but healthy people was 1.64.
A meta-analysis by Van der Kooy et al25 of 28 epidemiologic studies with nearly 80,000 patients showed depression to be an independent risk factor for cardiovascular disease.
Wulsin and Singal26 performed a systematic review to see if depression increases the risk of coronary disease. In 10 studies with a follow-up of more than 4 years, the relative risk in people with depression was 1.64, which was less than that in active smokers (2.5) but more than that in passive smokers (1.25).
Depression can also exacerbate the classic risk factors for coronary disease, such as smoking, diabetes, obesity, and physical inactivity. 27
A 2007 study from Sweden28 prospectively followed patients who were hospitalized for depression. The odds ratio of developing an acute MI was 2.9, and the risk persisted for decades after the initial hospitalization.
A prospective United Kingdom cohort study of people initially free of heart disease revealed major depression to be associated with a higher rate of death from ischemic heart disease.29 Specifically, patients who had depression currently or in the past 12 months had a 2.7 times higher risk of dying than those who had never had depression or who had had it more than 12 months previously.
In existing heart disease, depression predicts recurrent events, death
Carney et el30 found that patients with major depressive disorder had a higher incidence of new cardiac events in the 12 months after undergoing cardiac catheterization than those without major depressive disorder.
Frasure-Smith et al,31 in a landmark study, showed that patients who were depressed at 1 week after an MI were three to four times more likely to die in the next 6 months than nondepressed post-MI patients. Even after 18 months, depression remained an independent risk factor for cardiac-related death.32
In longer studies (with up to 19.4 years of follow-up), depression was associated with higher rates of death from cardiac and all causes in patients with coronary artery disease.33 Lespérance et al34 found that in MI patients, the higher the Beck Depression Inventory score at the time of hospital admission, the higher the 5-year death rate.
Using meta-analysis, Barth et al35 found the risk of dying in the first 2 years after initial assessment to be twice as high in depressed cardiac patients as in nondepressed cardiac patients (odds ratio 2.24).
Van Melle et al36 reviewed 22 studies and found that in the 2 years after an MI, depressed patients had a 2 to 2.5 times higher risk of dying of a cardiac or any other cause than did nondepressed patients.
Depression also predicts higher morbidity and mortality rates in patients undergoing coronary artery bypass grafting,37,38 patients with congestive heart failure,39 and heart transplant recipients.40
MEDICAL ILLNESS CAN PREDISPOSE TO DEPRESSION, AND VICE VERSA
Medical illnesses can predispose a patient to develop depression. Specifically, compared with healthy people, cardiac patients appear to be at greater risk of developing depression for many years after the initial medical diagnosis is made.41
Katon et al42 reviewed 31 studies involving 16,922 patients, that assessed the impact of depression and anxiety in chronic medical illnesses such as heart disease, diabetes, pulmonary disease, and arthritis. After the severity of the medical disorder was controlled for, patients with depression and anxiety reported a higher number of medical symptoms.
DEPRESSION WORSENS QUALITY OF LIFE AND ADHERENCE TO TREATMENT
Depressed patients perceive their health status and quality of life negatively. In the Heart and Soul study,43 depressive symptoms and low exercise capacity—but not low ejection fraction or ischemia—were significantly associated with perceived deterioration of health in patients with coronary artery disease.
After an MI, patients who take their cardiac drugs properly have a better chance of survival.44,45 Clinical depression can worsen compliance with cardiac medication regimens,46 and reducing depression increases medication adherence overall.47 Not surprisingly, depressed patients also adhere less well to other recommendations,48 including modifying the diet, exercising, stopping smoking, and attending cardiac rehabilitation programs. 49
PLAUSIBLE MECHANISMS LINK DEPRESSION AND HEART DISEASE
Traditional cardiac risk factors such as smoking, high cholesterol, hypertension, diabetes, and obesity tend to cluster in depressed patients. 50 Other mechanisms linking depression and heart disease are reviewed below.51,52
Autonomic imbalance
Excessive sympathetic stimulation or diminished vagal stimulation or both are associated with higher rates of morbidity and death.53
Lack of variability in the heart rate reflects a sympathetic-vagal imbalance and is a risk factor for ventricular arrhythmias and sudden cardiac death in patients with cardiovascular disease.54 Carney et al55 reported that patients with coronary artery disease and depression had significantly less heart rate variability than nondepressed cardiac patients. Similarly, after an MI, depressed patients had significantly less heart rate variability than nondepressed patients,56 implying that low heart rate variability may mediate the adverse effect of depression on survival after an MI.57
In the Heart and Soul study, Gehi et al58 found no distinct relationship between heart rate variability and depression. However, in the same study, de Jong et al59 did find specific somatic symptoms of depression to be associated with lower heart rate variability, although cognitive symptoms were not.
Platelet activation, endothelial dysfunction
Depressed patients have been found to have exaggerated platelet reactivity.60 Plasma levels of platelet factor IV and beta-thromboglobulin, markers of platelet activation, are higher in depressed patients with ischemic heart disease than in nondepressed patients with ischemic heart disease and in control patients.61 This activation of platelets can lead to vascular damage and thrombosis.
In a subset study of the Sertraline Anti-Depressant Heart Attack Randomized Trial (SADHART), depressed MI patients were treated with sertraline (Zoloft), a selective serotonin reuptake inhibitor (SSRI), and had substantially less platelet and endothelial biomarker release.62
Depressed cardiac patients also have impaired flow-mediated dilation of the brachial artery, a sign of endothelial dysfunction.63 Although a recent study did not find coronary endothelial dysfunction in depressed patients who did not have cardiac disease, these patients had more clustering of other cardiac risk factors.64
Hypothalamic-pituitary-adrenocortical and sympathetic adrenal medullary activation
High cortisol levels can accelerate the development of hypertension and atherosclerosis and result in endothelial vascular injury. Sympathoadrenal activation in turn can lead to higher levels of catecholamines, predisposing to vasoconstriction, a rapid heart rate, and platelet activation. Depressed patients have more activation of the hypothalamic-pituitary-adrenocortical and sympathetic adrenal medullary systems,51,65 yet another plausible mechanism for worse clinical outcomes in depressed cardiac patients.
Sudden emotional stress can cause transient left ventricular dysfunction, even in people without coronary disease, an effect that may be mediated by elevated plasma catecholamine levels.66
Inflammatory cytokines
Inflammatory cytokines play a key role in the development of atherosclerosis.67 C-reactive protein, an acute-phase reactant produced in hepatocytes, can be induced by cytokines such as interleukin 6. Damage to endothelial tissues leads to the release of inflammatory cytokines, including interleukin 1, interleukin 6, and tumor tumor necrosis factor alpha.
Depressed patients have higher levels of these inflammatory markers.68,69 A prospective study reported direct correlations between depression scores and C-reactive protein levels in post-MI patients.70 The Heart and Soul study, however, did not confirm that coronary patients have more inflammation if they have depression,71 indicating that the relationship is complex and is perhaps more evident in specific types of depression.72
Anticholinergic inflammatory pathway
Tracey73 proposed a theory that vagal tone inhibits the release of inflammatory cytokines. This has important implications for treatment, as exercise, biofeedback, and meditation can stimulate the vagus nerve and therefore have beneficial anti-inflammatory effects.74
Polymorphism in the serotonin transport promoter region gene
Research is focusing on the serotonin transport promoter region gene (5-HTTLPR).75 The gene exists in two forms, a long one and a less-effective short one that appears to predispose to depression.76
Nakatani et al77 showed that MI patients were more likely to become depressed and to have subsequent cardiac events if one or both of their alleles of this gene were short. Otte et al,78 using Heart and Soul study data, found that patients with a short allele had a higher likelihood of depression, higher perceived levels of stress, and higher urinary norepinephrine secretion. However, the long allele genotype may be associated with a higher risk of developing an MI.79
Our knowledge of the genetic interplay of depression and cardiovascular disease is still in its infancy, and further studies are needed to clarify these findings.
IN TRIALS, LESS DEPRESSION BUT NO EFFECT ON DEATHS, RECURRENT MI
Major behavioral and drug trials conducted in the last 15 years have focused on how to best treat depression in cardiac patients.80–85
The Montreal Heart Attack Readjustment Trial (MHART)81 used telephone calls and home nursing visits to explore and monitor psychological distress for up to 1 year after an MI. The overall trial did not show these interventions to have any impact on survival compared with usual care. In fact, in women receiving the telephone intervention, there was a trend toward higher rates of cardiac and all-cause death, which was quite unexpected. Uncovering stresses and problems without resolving them, rather than encouraging patients to place these on the “back burner,” may partially explain these results.
SADHART82 studied the safety of sertraline in depressed post-MI patients. No major differences in cardiac function were noted between the sertraline and placebo groups, showing that sertraline was safe for these patients. The sertraline group had fewer cardiovascular events, but the difference was not statistically significant.
The Enhancing Recovery in Coronary Heart Disease (ENRICHD) study83 was primarily designed to see whether a psychosocial intervention would decrease deaths in depressed cardiac patients. Much to the chagrin of behavioral medicine, the group undergoing cognitive behavioral therapy did not have a higher rate of event-free survival, although the intervention had a favorable impact on depression and social support.
The Myocardial Infarction Depression Intervention Trial (MIND-IT)84 looked at whether the antidepressant mirtazapine (Remeron) would improve long-term depression and cardiovascular outcomes in depressed post-MI patients. In 18 months of follow-up, neither objective was obtained.
The Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial85 tested the efficacy of the SSRI citalopram (Celexa) and interpersonal therapy in a short-term intervention. Here, the antidepressant was superior to placebo in the primary outcome of treating depression, but interpersonal therapy had no advantage over “clinical management,” ie, a shorter, 20-minute supportive intervention.
Common threads in these studies.
- In ENRICHD and MIND-IT, patients whose depression did not respond to treatment were at higher risk of cardiac events during follow-up.86–88
- In SADHART and CREATE, which used drug treatment, the antidepressant response was more robust in patients with a history of depression before their heart attacks, suggesting that a patient with recurrent depression at the time of a cardiac event should receive medication for it.85,89
CLINICAL RECOMMENDATIONS
Use a depression screening tool
Ziegelstein et al90 recently studied the ability of clinical personnel to detect depression in hospitalized MI patients. If a screening tool was not used, the results were abysmal, indicating the need to use formal screening for symptoms of depression in acute MI patients.
Many self-rating scales are available, among which are the Beck Depression Inventory (BDI) and the Hospital Anxiety and Depression Scale (HADS). Others are:
The PHQ-2 consists of the two first questions of the PHQ-9, which deal with mood and lack of pleasure. A cut-off score of 3 or higher has a sensitivity of 83% and a specificity of 92%,96 fulfilling the need for a quick and reliable depression screening tool. The clinician can also ask for a yes-or-no answer to the two questions of the PHQ-2 (Table 1). A yes to either of the two questions is up to 90% sensitive and 75% specific.92,97
When to suspect depression in cardiac patients
Which type of psychotherapy is best?
The negative results of psychosocial interventions (phone calls and home visits from a nurse) in MHART and of cognitive behavioral therapy in ENRICHD raise questions about which type of psychotherapy is best for depression in heart disease. CREATE found that 50-minute weekly sessions of interpersonal psychotherapy were no more beneficial than clinical management, ie, 20-minute weekly sessions that focused on compliance with treatment and education about depression and overall management. Perhaps a type of therapy akin to “clinical management” in this study or the brief behavior-based and targeted therapy used in the Improving Mood Promoting Access to Collaborative Care Treatment (IMPACT) trials of depression in primary care99 could be designed specifically to treat depression in cardiac disease. However, it is also quite possible that treatments that focus on uncovering stresses or problems may not be timely for these patients.
Which therapy is best for women is another area of consideration. In MHART, even after 5 years of follow-up,100 women who received the psychosocial support intervention did marginally worse. In the ENRICHD study, women did not experience a benefit from cognitive behavioral therapy. Further studies must address sex differences in response to different therapies.
SSRIs seem to be better than other antidepressants for cardiac patients
Before SSRIs were available, tricyclic antidepressants were the mainstays. Subsequent analysis showed the tricyclics to have an unfavorable risk-benefit profile in cardiac patients,101 and since other types of antidepressants are available, tricyclics should be avoided altogether in cardiac patients.102
Whether the SSRIs actually decrease one’s risk of death in heart disease is still an issue of debate, but there are encouraging signs. In SADHART, the rate of death and recurrent nonfatal MI was 20% lower in the patients randomized to receive sertraline, although the difference was not statistically significant.82 In ENRICHD, patients who did not respond to cognitive behavioral treatment or had severe depression could receive sertraline or other antidepressant drugs on a nonrandomized basis, and those who did had a 42% lower incidence of death or recurrent MI.103
The SADHART and CREATE trials provide convincing evidence of the cardiac safety and antidepressant efficacy of two SSRIs (sertraline and citalopram) in depressed cardiac patients. Mirtazapine, studied in MIND-IT, was not effective in treating depression in cardiac patients, although it had a better adverse effect and safety profile than tricyclic antidepressants. 104
Clinical observations indicate that SSRIs are associated with less risk of MI than non-SSRI drugs.105,106 During hospitalization for acute coronary syndromes, patients on SSRIs had lower rates of recurrent ischemia and heart failure but higher bleeding rates than patients not taking SSRIs.107 In a retrospective study of patients undergoing coronary artery bypass grafting, those on an SSRI before surgery had higher rates of death and rehospitalization.108 Being on antidepressant medication could be interpreted as a surrogate marker of having more severe depression before surgery; this issue clearly requires further study.
Given current observations and recent data from interventional trials coupled with the safe drug-interaction profile of sertraline and citalopram, these two SSRIs are recommended for treating depression in cardiac patients. If the patient is also receiving an anticoagulant, one should monitor for bleeding, as all SSRIs are associated with a prolonged bleeding time. Monitoring for rare cases of hyponatremia and bradycardia should also be part of early follow-up.
Do cardiac drugs have psychiatric effects?
Some concerns have arisen about cardiovascular drugs causing or aggravating psychiatric conditions.
Statins were once suspected of causing clinical depression or even suicide. However, subsequent studies have not substantiated this.109,110 In fact, long-term statin use has been associated with improved psychological wellbeing. 111 Whether the favorable psychological profile is due to an improved lifestyle, a direct noncholesterol effect, or an immunomodulatory effect has yet to be determined.
Beta-blockers have been suspected of increasing depression and fatigue. Robust metaanalyses have shown no increased risk of depressive symptoms but a small increased risk of fatigue and sexual dysfunction.112 Observational trials in the first year post-MI have shown no differences between beta-blocker users and nonusers in depressive symptoms or depressive disorders.113
Statins and beta-blockers offer both immense cardiac benefit and low risk, and both may be prescribed with confidence in depressed cardiac patients.
Refer patients for cardiac rehabilitation
The American Association of Cardiovascular and Pulmonary Rehabilitation strongly recommends screening cardiac patients for depression and referring them to cardiac rehabilitation programs.114 Typical programs run 12 weeks, affording an opportunity to further listen to and assess the patient and to promote general wellness via nutrition, stress management, and exercise.
These interventions by themselves can favorably affect depression. Blumenthal and colleagues,115 in the Standard Medical Intervention and Long-Term Exercise (SMILE) study, found that exercise was as effective as drug treatment in reducing depression. In addition, stress management as a psychosocial treatment in cardiac rehabilitation can reduce death rates in cardiac patients.116
Unfortunately, many patients who are eligible for cardiac rehabilitation programs do not avail themselves of them.117
Our algorithm
FUTURE DIRECTIONS FOR RESEARCH
Can we predict the course of depression?
We need to identify better which patients will have a spontaneous remission of their depressive symptoms after a cardiac event, which patients will linger with depression, and which patients will best respond to treatment. Risk stratification, using the psychiatric history, symptoms and severity of depression, and genetic predisposition118 might allow improved targeted therapies.
Does depression cause cardiac disease?
The link between depression and heart disease can be seen as merely an association. In the interventional trials performed to date, we have not yet seen a reduction in cardiac deaths when depression was treated, challenging any assumption of a causal relationship between depression and heart disease. The debate about association vs cause is germane to behavioral medicine,119 and the better we understand the mechanistic pathways, the better we can advise patients and treat depression comorbid with heart disease.
Behavioral medicine is currently measuring the aspects of depression associated with cardiac disease, including the spectrum of somatic (body) and affective (mood) symptoms120 and specific areas such as sympathetic arousal and early morning insomnia.121 If we can determine the depression subtype that carries a worse cardiac prognosis, we may untangle the biobehavioral links that bidirectionally bridge clinical depression and cardiac disease.
Another area of interest, emotional vitality (a positive state associated with interest, enthusiasm, excitement, and energy for living) has been shown to protect against coronary heart disease122 and holds much promise.
In the plenary lecture of the Academy of Psychosomatic Medicine in 2006, Frasure-Smith spoke of the “pleiotropism” of our antidepressant interventions on the various risk factors in depressed cardiac patients.123 We need behavioral medicine studies that elucidate these mechanisms, guiding more precise treatments as well as novel therapies. Omega-3 fatty acids, which benefit heart disease and clinical depression,124 will be used in a randomized controlled trial by Lespérance and colleagues.125 We await the results of this exciting research.
Will treating depression help in other types of heart disease?
The SADHART-CHF trial is examining whether 12 weeks of sertraline therapy is better than placebo in preventing death and improving cardiac outcomes in patients with chronic heart failure and comorbid major depressive disorder. It was to be completed in the fall of 2008. The results and experience of this study will help in designing future interventional trials to reduce the risk of depression in cardiovascular diseases.
We also await the results of a National Heart, Lung, and Blood Institute (NHLBI) trial, “Bypassing the Blues,” which is studying the treatment of depression after cardiac bypass surgery. This study should provide further insights into management of the depressed cardiac patient. Further prognostic studies in cardiac patients are also needed using the PHQ-9 and its shorter version, PHQ-2.
Current and future guidelines
For years our European colleagues have been ahead of us in recognizing depression screening and stress management as key to cardiac disease-prevention strategies.126 The NHLBI nicely outlined recommendations on the assessment and treatment of depression in cardiovascular patients.127 The just-published AHA Science Advisory should further encourage clinicians to screen and treat depression in the patient population.1 As our knowledge grows, we look forward to future evidence-based guidelines for depressed cardiac patients.
- Lichtman JH, Bigger JT, Blumenthal JA, et al. Depression and coronary heart disease. Recommendations for screening, referral, and treatment. Circulation 2008; 118:1768–1775.
- Jiang W, Glassman A, Krishnan R, O’Connor CM, Califf RM. Depression and ischemic heart disease: what have we learned so far and what must we do in the future? Am Heart J 2005; 150:54–78.
- Freedland KE, Rich MW, Skala JA, Carney RM, Davila-Roman VG, Jaffe AS. Prevalence of depression in hospitalized patients with congestive heart failure. Psychosom Med 2003; 65:119–128.
- Murray CJ, Lopez AD, Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet 1997; 349:1436–1442.
- Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet 2007; 370:851–858.
- Osborn DP, Levy G, Nazareth I, Petersen I, Islam A, King MB. Relative risk of cardiovascular and cancer mortality in people with severe mental illness from the United Kingdom’s general practice research database. Arch Gen Psychiatry 2007; 64:242–249.
- Friedman M, Thoresen CE, Gill JJ, et al. Alteration of type A behavior and its effect on cardiac recurrences in post myocardial infarction patients: summary results of the recurrent coronary prevention project. Am Heart J 1986; 112:653–665.
- Ragland DR, Brand RJ. Type A behavior and mortality from coronary heart disease. N Engl J Med 1988; 318:65–69.
- Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation 1999; 99:2192–2217.
- Iribarren C, Sidney S, Bild DE, et al. Association of hostility with coronary artery calcification in young adults: the CARDIA study. Coronary Artery Risk Development in Young Adults. JAMA 2000; 283:2546–2551.
- Williams RB, Barefoot JC, Schneiderman N. Psychosocial risk factors for cardiovascular disease: more than one culprit at work. JAMA 2003; 290:2190–2192.
- Rozanski A, Blumenthal JA, Davidson KW, Saab PG, Kubzansky L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: the emerging field of behavioral cardiology. J Am Coll Cardiol 2005; 45:637–651.
- Hemingway H, Marmot M. Evidence based cardiology: psychosocial factors in the aetiology and prognosis of coronary heart disease: systematic review of prospective cohort studies. BMJ 1999; 318:1460–1467.
- Denollet J. DS14: Standard assessment of negative affectivity, social inhibition, and type D personality. Psychosom Med 2005; 67:89–97.
- Steptoe A, Molloy GJ. Personality and heart disease. Heart 2007; 93:783–784.
- Yusuf S, Hawken S, Ôunpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004; 364:937–952.
- Rosengren A, Hawken S, Ounpuu S, et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case-control study. Lancet 2004; 364:953–962.
- Kuper H, Marmot M. Job strain, job demands, decision latitude, and risk of coronary heart disease within the Whitehall II study. J Epidemiol Community Health 2003; 57:147–153.
- Aboa-Eboule C, Brisson C, Maunsell E, et al. Job strain and risk of acute recurrent coronary heart disease events. JAMA 2007; 298:1652–1660.
- Frasure-Smith N, Lespérance F. Depression and anxiety as predictors of 2-year cardiac events in patients with stable coronary artery disease. Arch Gen Psychiatry 2008; 65:62–71.
- Shen B-J, Avivi YE, Todaro JF, et al. Anxiety characteristics independently and prospectively predict myocardial infarction in men. J Am Coll Cardiol 2008; 51:113–119.
- Carney RM, Freedland KE. Depression, mortality, and medical morbidity in patients with coronary heart disease. Biol Psychiatry 2003; 54:241–247.
- Pratt LA, Ford DE, Crum RM, Armenian HK, Gallo JJ, Eaton WW. Depression, psychotropic medication, and risk of myocardial infarction: prospective data from the Baltimore ECA follow-up. Circulation 1996; 94:3123–3129.
- Rugulies R. Depression as a predictor for coronary heart disease. A review and meta-analysis. Am J Prev Med 2002; 23:51–61.
- Van der Kooy K, van Hout H, Marwijk H, Marten H, Stehouwer C, Beekman A. Depression and the risk for cardiovascular diseases: systematic review and meta analysis. Int J Geriatr Psychiatry 2007; 22:613–626.
- Wulsin LR, Singal BM. Do depressive symptoms increase the risk for the onset of coronary disease? A systematic quantitative review. Psychosom Med 2003; 65:201–210.
- Wulsin LR. Is depression a major risk factor for coronary disease? A systematic review of the epidemiologic evidence. Harv Rev Psychiatry 2004; 12:79–93.
- Janszky I, Ahlbom A, Hallqvist J, Ahnve S. Hospitalization for depression is associated with an increased risk for myocardial infarction not explained by lifestyle, lipids, coagulation, and inflammation: The SHEEP Study. Biol Psychiatry 2007; 62:25–32.
- Surtees PG, Wainwright NWJ, Luben RN, Wareham NJ, Bingham SA, Khaw K-T. Depression and ischemic heart disease mortality: evidence from the EPIC-Norfolk United Kingdom Prospective Cohort Study. Am J Psychiatry 2008; 165:515–523.
- Carney RM, Rich MW, Freedland KE, et al. Major depressive disorder predicts cardiac events in patients with coronary artery disease. Psychosom Med 1988; 50:627–633.
- Frasure-Smith N, Lespérance F, Talajic M. Depression following myocardial infarction. Impact on 6-month survival. JAMA 1993; 270:1819–1825.
- Frasure-Smith N, Lespérance F, Talajic M. Depression and 18-month prognosis after myocardial infarction. Circulation 1995; 91:999–1005.
- Barefoot JC, Helms MJ, Mark DB, et al. Depression and long-term mortality risk in patients with coronary artery disease. Am J Cardiol 1996; 78:613–617.
- Lespérance F, Frasure-Smith N, Talajic M, Bourassa MG. Five-year risk of cardiac mortality in relation to initial severity and one-year changes in depression symptoms after myocardial infarction. Circulation 2002; 105:1049–1053.
- Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med 2004; 66:802–813.
- van Melle JP, de Jonge P, Spijkerman TA, et al. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis. Psychosom Med 2004; 66:814–822.
- Blumenthal JA, Lett HS, Babyak MA, et al. Depression as a risk factor for mortality after coronary artery bypass surgery. Lancet 2003; 362:604–609.
- Sullivan MD, LaCroix AZ, Spertus JA, Hecht J, Russo J. Depression predicts revascularization procedures for 5 years after coronary angiography. Psychosom Med 2003; 65:229–236.
- Jiang W, Alexander J, Christopher E, et al. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med 2001; 161:1849–1856.
- Zipfel S, Schneider A, Wild B, et al. Effect of depressive symptoms on survival after heart transplantation. Psychosom Med 2002; 64:740–747.
- Polsky D, Doshi JA, Marcus S, et al. Long-term risk for depressive symptoms after a medical diagnosis. Arch Intern Med 2005; 165:1260–1266.
- Katon W, Lin EHB, Kroenke K. The association of depression and anxiety with medical symptom burden in patients with chronic medical illness. Gen Hosp Psychiatry 2007; 29:147–155.
- Ruo B, Rumsfeld JS, Hlatky MA, Liu H, Browner WS, Whooley MA. Depressive symptoms and health-related quality of life: the Heart and Soul Study. JAMA 2003; 290:215–221.
- Rasmussen JN, Chong A, Alter DA. Relationship between adherence to evidence-based pharmacotherapy and long-term mortality after acute myocardial infarction. JAMA 2007; 297:177–186.
- Gehi AK, Ali S, Na B, Whooley MA. Self-reported medication adherence and cardiovascular events in patients with stable coronary heart disease: the Heart and Soul Study. Arch Intern Med 2007; 167:1798–1803.
- Gehi A, Haas D, Pipkin S, Whooley MA. Depression and medication adherence in outpatients with coronary heart disease: findings from the Heart and Soul Study. Arch Intern Med 2005; 165:2508–2513.
- Rieckmann N, Gerin W, Kronish IM, et al. Course of depressive symptoms and medication adherence after acute coronary syndromes: an electronic medication monitoring study. J Am Coll Cardiol 2006; 48:2218–2222.
- Ziegelstein RC, Fauerbach JA, Stevens SS, Romanelli J, Richter DP, Bush DE. Patients with depression are less likely to follow recommendations to reduce cardiac risk during recovery from a myocardial infarction. Arch Intern Med 2000; 160:1818–1823.
- Kronish IM, Rieckmann N, Halm EA, et al. Persistent depression affects adherence to secondary prevention behaviors after acute coronary syndromes. J Gen Intern Med 2006; 21:1178–1183.
- Joynt KE, Whellan DJ, O’Connor CM. Depression and cardiovascular disease: mechanisms of interaction. Biol Psychiatry 2003; 54:248–261.
- Musselman DL, Evans DL, Nemeroff CB. The relationship of depression to cardiovascular disease: epidemiology, biology, and treatment. Arch Gen Psychiatry 1998; 55:580–592.
- Lespérance F, Frasure-Smith N. Depression and heart disease. Cleve Clin J Med 2007; 74(suppl 1):S63–S66.
- Curtis BM. Autonomic tone as a cardiovascular risk factor: the dangers of chronic fight or flight. Mayo Clin Proc 2002; 77:45–54.
- Topol EJ. Textbook of Cardiovascular Medicine, 2nd ed. Philadelphia: Lippincott Williams & Williams 2002.
- Carney RM, Saunders RD, Freedland KE, Stein P, Rich MW, Jaffe AS. Association of depression with reduced heart rate variability in coronary artery disease. Am J Cardiol 1995; 76:562–564.
- Carney RM, Blumenthal JA, Stein PK, et al. Depression, heart rate variability, and acute myocardial infarction. Circulation 2001; 104:2024–2028.
- Carney RM, Blumenthal JA, Freedland KE, et al. Low heart rate variability and the effect of depression on post-myocardial infarction mortality. Arch Intern Med 2005; 165:1486–1491.
- Gehi A, Mangano D, Pipkin S, Browner WS, Whooley MA. Depression and heart rate variability in patients with stable coronary heart disease: findings from the Heart and Soul Study. Arch Gen Psychiatry 2005; 62:661–666.
- de Jonge P, Mangano D, Whooley MA. Differential association of cognitive and somatic depressive symptoms with heart rate variability in patients with stable coronary heart disease: findings from the Heart and Soul Study. Psychosom Med 2007; 69:735–739.
- Musselman DL, Tomer A, Manatunga AK, et al. Exaggerated platelet reactivity in major depression. Am J Psychiatry 1996; 153:1313–1317.
- Laghrissi-Thode F, Wagner WR, Pollock BG, Johnson PC, Finkel MS. Elevated platelet factor 4 and beta-thromboglobulin plasma levels in depressed patients with ischemic heart disease. Biol Psychiatry 1997; 42:290–295.
- Serebruany VL, Glassman AH, Malinin AI, et al. Platelet/endothelial biomarkers in depressed patients treated with the selective serotonin reuptake inhibitor sertraline after acute coronary events: the Sertraline AntiDepressant Heart Attack Randomized Trial (SADHART) Platelet Substudy. Circulation 2003; 108:939–944.
- Sherwood A, Hinderliter AL, Watkins LL, Waugh RA, Blumenthal JA. Impaired endothelial function in coronary heart disease patients with depressive symptomatology. J Am Coll Cardiol 2005; 46:656–659.
- Yang EH, Lerman S, Lennon RJ, Simari RD, Lerman LO, Lerman A. Relation of depression to coronary endothelial function. Am J Cardiol 2007; 99:1134–1136.
- Otte C, Neylan TC, Pipkin SS, Browner WS, Whooley MA. Depressive symptoms and 24-hour urinary norepinephrine excretion levels in patients with coronary disease: findings from the Heart and Soul Study. Am J Psychiatry 2005; 162:2139–2145.
- Wittstein IS, Thiemann DR, Lima JAC, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med 2005; 352:539–548.
- Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med 2005; 352:1685–1695.
- Miller GE, Stetler CA, Carney RM, Freedland KE, Banks WA. Clinical depression and inflammatory risk markers for coronary heart disease. Am J Cardiol 2002; 90:1279–1283.
- Empana JP, Sykes DH, Luc G, et al. Contributions of depressive mood and circulating inflammatory markers to coronary heart disease in healthy European men: the Prospective Epidemiological Study of Myocardial Infarction (PRIME). Circulation 2005; 111:2299–2305.
- Frasure-Smith N, Lespérance F, Irwin MR, Sauvé C, Lespérance J, Théroux P. Depression, C-reactive protein and two-year major adverse cardiac events in men after acute coronary syndromes. Biol Psychiatry 2007; 62:302–308.
- Whooley MA, Caska CM, Hendrickson BE, Rourke MA, Ho J, Ali S. Depression and inflammation in patients with coronary heart disease: findings from the Heart and Soul Study. Biol Psychiatry 2007; 62:314–320.
- Glassman AH, Miller GE. Where there is depression, there is inflammation…sometimes! Biol Psychiatry 2007; 62:280–281.
- Tracey KJ. Physiology and immunology of the cholinergic antiinflammatory pathway. J Clin Invest 2007; 117:289–296.
- Tracey KJ. The inflammatory reflex. Nature 2002; 420:853–859.
- McCaffery JM, Frasure-Smith N, Dubé M-P, et al. Common genetic vulnerability to depressive symptoms and coronary artery disease: a review and development of candidate genes related to inflammation and serotonin. Psychosom Med 2006; 68:187–200.
- Caspi A, Sugden K, Moffitt TE, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science 2003; 301:386–389.
- Nakatani D, Sato H, Sakata Y, et al. Influence of serotonin transporter gene polymorphism on depressive symptoms and new cardiac events after acute myocardial infarction. Am Heart J 2005; 150:652–658.
- Otte C, McCaffery J, Ali S, Whooley MA. Association of a serotonin transporter polymorphism (5-HTTLPR) with depression, perceived stress, and norepinephrine in patients with coronary disease: the Heart and Soul Study. Am J Psychiatry 2007; 164:1379–1384.
- Fumeron F, Betoulle D, Nicaud V, et al. Serotonin transporter gene polymorphism and myocardial infarction: Etude Cas-Témoins de l’Infarctus du Myocarde (ECTIM). Circulation 2002; 105:2943–2945.
- Rivelli S, Jiang W. Depression and ischemic heart disease: what have we learned from clinical trials? Curr Opin Cardiol 2007; 22:286–291.
- Frasure-Smith N, Lespérance F, Prince RH, et al. Randomised trial of home-based psychosocial nursing intervention for patients recovering from myocardial infarction. Lancet 1997; 350:473–479.
- Glassman AH, O’Connor CM, Califf RM, et al. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA 2002; 288:701–709.
- Writing Committee for the EI. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) randomized trial. JAMA 2003; 289:3106–3116.
- van Melle JP, de Jonge P, Honig A, et al. Effects of antidepressant treatment following myocardial infarction. Br J Psychiatry 2007; 190:460–466.
- Lespérance F, Frasure-Smith N, Koszycki D, et al. Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease: the Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial. JAMA 2007; 297:367–379.
- Carney RM, Blumenthal JA, Freedland KE, et al. Depression and late mortality after myocardial infarction in the Enhancing Recovery in Coronary Heart Disease (ENRICHD) Study. Psychosom Med 2004; 66:466–474.
- de Jonge P, Honig A, van Melle JP, et al. Nonresponse to treatment for depression following myocardial infarction: association with subsequent cardiac events. Am J Psychiatry 2007; 164:1371–1378.
- Carney RM, Freedland KE. Depression and coronary heart disease: more pieces of the puzzle. Am J Psychiatry 2007; 164:1307–1309.
- Glassman AH, Bigger JT, Gaffney M, Shapiro PA, Swenson JR. Onset of major depression associated with acute coronary syndromes: relationship of onset, major depressive disorder history, and episode severity to sertraline benefit. Arch Gen Psychiatry 2006; 63:283–288.
- Ziegelstein RC, Kim SY, Kao D, et al. Can doctors and nurses recognize depression in patients hospitalized with an acute myocardial infarction in the absence of formal screening? Psychosom Med 2005; 67:393–397.
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9. Validity of a brief depression severity measure. J Gen Intern Med 2001; 16:606–613.
- Löwe B, Unutzer J, Callahan CM, Perkins AJ, Kroenke K. Monitoring depression treatment outcomes with the Patient Health Questionnaire-9. Med Care 2004; 42:1194–1201.
- Parashar S, Rumsfeld JS, Spertus JA, et al. Time course of depression and outcome of myocardial infarction. Arch Intern Med 2006; 166:2035–2043.
- Amin AA, Jones AMH, Nugent K, Rumsfeld JS, Spertus JA. The prevalence of unrecognized depression in patients with acute coronary syndrome. Am Heart J 2006; 152:928–934.
- McManus D, Pipkin SS, Whooley MA. Screening for depression in patients with coronary heart disease (data from the Heart and Soul Study). Am J Cardiol 2005; 96:1076–1081.
- Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care 2003; 41:1284–1292.
- Spitzer RL, Williams JB, Kroenke K, et al. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA 1994; 272:1749–1756.
- Lespérance F, Frasure-Smith N. Depression in patients with cardiac disease. J Psychosom Res 2000; 48:379–391.
- Hunkeler EM, Katon W, Tang L, et al. Long term outcomes from the IMPACT randomised trial for depressed elderly patients in primary care. BMJ 2006; 332:259–263.
- Frasure-Smith N, Lespérance F, Gravel G, Masson A, Juneau M, Bourassa MG. Long-term survival differences among low-anxious, high-anxious and repressive copers enrolled in the Montreal Heart Attack Readjustment Trial. Psychosom Med 2002; 64:571–579.
- Glassman AH, Roose SP, Bigger JT. The safety of tricyclic antidepressants in cardiac patients: risk-benefit reconsidered. JAMA 1993; 269:2673–2675.
- Cohen HW, Gibson G, Alderman MH. Excess risk of myocardial infarction in patients treated with antidepressant medications: association with use of tricyclic agents. Am J Med 2000; 108:2–8.
- Taylor CB, Youngblood ME, Catellier D, et al. Effects of antidepressant medication on morbidity and mortality in depressed patients after myocardial infarction. Arch Gen Psychiatry 2005; 62:792–798.
- Montgomery SA. Safety of mirtazapine: a review. Int Clin Psychopharmacol 1995; 10(suppl 4):37–45.
- Sauer WH, Berlin JA, Kimmel SE. Selective serotonin reuptake inhibitors and myocardial infarction. Circulation 2001; 104:1894–1898.
- Sauer WH, Berlin JA, Kimmel SE. Effect of antidepressants and their relative affinity for the serotonin transporter on the risk of myocardial infarction. Circulation 2003; 108:32–36.
- Ziegelstein RC, Meuchel J, Kim TJ, et al. Selective serotonin reuptake inhibitor use by patients with acute coronary syndromes. Am J Med 2007; 120:525–530.
- Xiong GL, Jiang W, Clare R, et al. Prognosis of patients taking selective serotonin reuptake inhibitors before coronary artery bypass grafting. Am J Cardiol 2006; 98:42–47.
- Yang C-C, Jick SS, Jick H. Lipid-lowering drugs and the risk of depression and suicidal behavior. Arch Intern Med 2003; 163:1926–1932.
- Callreus T, Agerskov Andersen U, Hallas J, Andersen M. Cardiovascular drugs and the risk of suicide: a nested case-control study. Eur J Clin Pharmacol 2007; 63:591–596.
- Young-Xu Y, Chan KA, Liao JK, Ravid S, Blatt CM. Long-term statin use and psychological well-being. J Am Coll Cardiol 2003; 42:690–697.
- Ko DT, Hebert PR, Coffey CS, Sedrakyan A, Curtis JP, Krumholz HM. Beta-blocker therapy and symptoms of depression, fatigue, and sexual dysfunction. JAMA 2002; 288:351–357.
- van Melle JP, Verbeek D, van den Berg MP, Ormel J, van der Line MR, de Jonge P. Beta-blockers and depression after myocardial infarction. J Am Coll Cardiol 2006; 48:2209–2214.
- Thomas RJ, King M, Lui K, et al. AACVPR/ACC/AHA 2007 performance measures on cardiac rehabilitation for referral to and delivery of cardiac rehabilitation/secondary prevention services. J Am Coll Cardiol 2007; 50:1400–1433.
- Blumenthal JA, Babyak MA, Doraiswamy PM, et al. Exercise and pharmacotherapy in the treatment of major depressive disorder. Psychosom Med 2007; 69:587–596.
- Linden W, Phillips MJ, Leclerc J. Psychological treatment of cardiac patients: a meta-analysis. Eur Heart J 2007; 28:2972–2984.
- Centers for Disease Control and Prevention. Receipt of outpatient cardiac rehabilitation among heart attack survivors—United States, 2005. JAMA 2008; 299:1534–1536.
- Williams RB. Treating depression after myocardial infarction: can selecting patients on the basis of genetic susceptibility improve psychiatric and medical outcomes? Am Heart J 2005; 150:617–619.
- Schneiderman N, Williams RB. The great debate editorial, revisited. Psychosom Med 2006; 68:636–638.
- de Jonge P, Ormel J, van den Brink RHS, et al. Symptom dimensions of depression following myocardial infarction and their relationship with somatic health status and cardiovascular prognosis. Am J Psychiatry 2006; 163:138–144.
- Fraguas R, Iosifescu DV, Alpert J, et al. Major depressive disorder and comorbid cardiac disease: is there a depressive subtype with greater cardiovascular morbidity? Results from the STAR*D Study. Psychosomatics 2007; 48:418–425.
- Kubzansky LD, Thurston RC. Emotional vitality and incident coronary heart disease: benefits of healthy psychological functioning. Arch Gen Psychiatry 2007; 64:1393–1401.
- Frasure-Smith N. Reflections on depression as a cardiac risk factor Academy of Psychosomatic Medicine, 53rd Annual Meeting, Tucson, Arizona, 2006.
- Frasure-Smith N, Lespérance F. Major depression is associated with lower omega-3 fatty acid levels in patients with recent acute coronary syndromes. Biol Psychiatry 2004; 55:891–896.
- Lespérance F. Annual Research Award Lecture Academy of Psychosomatic Medicine, Amelia Island, Florida, 2007.
- Graham I, Atar D, Borch-Johnsen K, et al. European guidelines on cardiovascular disease prevention in clinical practice: executive summary. Eur Heart J 2007; 28:2375–2414.
- Davidson KW, Kupfer DJ, Bigger JT, et al. Assessment and treatment of depression in patients with cardiovascular disease: National Heart, Lung, and Blood Institute Working Group Report. Psychosom Med 2006; 68:645–650.
Depression is a risk factor for heart disease, and in patients with heart disease, it is a risk factor for complications and death. Unfortunately, in the trials performed to date, treating depression in cardiac patients did not lead to lower rates of recurrent cardiovascular events or death. Nevertheless, we recommend that clinicians systematically screen for it in their heart patients, in view of the benefits of antidepressant therapy.
In this article we review key epidemiologic and psychosocial studies, the mechanistic links between depression and heart disease, and recent intervention trials. We also offer practical management advice and address the continued need for guidelines and risk stratification in the treatment of depressed cardiac patients.
After we submitted our review article, the American Heart Association (AHA)1 released a consensus document recommending that health care providers screen for and treat depression in patients with coronary heart disease. We will discuss the same screening tests that have been recommended by the AHA.
DEPRESSION AND HEART DISEASE: COMMON AND LINKED
Depression and heart disease are very common and often coexist: the prevalence of depression in various heart conditions ranges from 15% to 20%.1–3 According to data from the World Health Organization, by the year 2020 depression will be the second-leading cause of disability in developed countries (after heart disease).4
The World Health Survey5 showed that depression worsens health more than angina, arthritis, asthma, or diabetes. Furthermore, patients with severe mental illness have a higher risk of dying from heart disease and stroke.6
SOME HEART DISEASE RISK FACTORS ARE PSYCHOSOCIAL
In the 1980s, the “type A” personality (ambitious, aggressive, hostile, and competitive, with a chronic sense of urgency) was linked to heart disease.7 Later studies differed as to whether the entire set of features is valid as a collective risk factor for progressive heart disease,8 but hostility remains a validated risk factor and a focus of behavior modification.9,10
Other psychosocial risk factors have been implicated,11,12 one of which is social isolation.9,13 Another is the “type D” personality, which includes a tendency to experience negative emotions across time and situations coupled with social inhibition and which is believed to be more valid than the type A personality as a risk factor for cardiac disease.14,15
The INTERHEART study16 gathered data about attributable risk in the development of myocardial infarction (MI) in 52 countries in a case-control fashion. Psychosocial factors including stress, low generalized locus of control (ie, the perceived inability to control one’s life), and depression accounted for 32.5% of the attributable risk for an MI.17 This would mean that they account for slightly less attributable risk than that of lifetime smoking but more than that of hypertension and obesity.
Job stress increases the risk of initial coronary heart disease18 and also the risk of recurrent cardiac events after a first MI.19 Even though numerous psychosocial risk factors have been associated with coronary heart disease, including anxiety,20,21 depression is perhaps the best studied.
PROSPECTIVE STUDIES OF DEPRESSION AND HEART DISEASE
To examine the impact of depression in coronary heart disease, prospective studies have been done in healthy people and in patients with established cardiovascular disease who develop depression.22
In healthy people, depression increases the risk of coronary disease
The 1996 Epidemiologic Catchment Area study23 found that people with major depression had a risk of MI four times higher than the norm, and people with 2 weeks of sadness or dysphoria had a risk two times higher.
A subsequent meta-analysis of 11 studies,24 which included 36,000 patients, found that the overall relative risk of developing heart disease in depressed but healthy people was 1.64.
A meta-analysis by Van der Kooy et al25 of 28 epidemiologic studies with nearly 80,000 patients showed depression to be an independent risk factor for cardiovascular disease.
Wulsin and Singal26 performed a systematic review to see if depression increases the risk of coronary disease. In 10 studies with a follow-up of more than 4 years, the relative risk in people with depression was 1.64, which was less than that in active smokers (2.5) but more than that in passive smokers (1.25).
Depression can also exacerbate the classic risk factors for coronary disease, such as smoking, diabetes, obesity, and physical inactivity. 27
A 2007 study from Sweden28 prospectively followed patients who were hospitalized for depression. The odds ratio of developing an acute MI was 2.9, and the risk persisted for decades after the initial hospitalization.
A prospective United Kingdom cohort study of people initially free of heart disease revealed major depression to be associated with a higher rate of death from ischemic heart disease.29 Specifically, patients who had depression currently or in the past 12 months had a 2.7 times higher risk of dying than those who had never had depression or who had had it more than 12 months previously.
In existing heart disease, depression predicts recurrent events, death
Carney et el30 found that patients with major depressive disorder had a higher incidence of new cardiac events in the 12 months after undergoing cardiac catheterization than those without major depressive disorder.
Frasure-Smith et al,31 in a landmark study, showed that patients who were depressed at 1 week after an MI were three to four times more likely to die in the next 6 months than nondepressed post-MI patients. Even after 18 months, depression remained an independent risk factor for cardiac-related death.32
In longer studies (with up to 19.4 years of follow-up), depression was associated with higher rates of death from cardiac and all causes in patients with coronary artery disease.33 Lespérance et al34 found that in MI patients, the higher the Beck Depression Inventory score at the time of hospital admission, the higher the 5-year death rate.
Using meta-analysis, Barth et al35 found the risk of dying in the first 2 years after initial assessment to be twice as high in depressed cardiac patients as in nondepressed cardiac patients (odds ratio 2.24).
Van Melle et al36 reviewed 22 studies and found that in the 2 years after an MI, depressed patients had a 2 to 2.5 times higher risk of dying of a cardiac or any other cause than did nondepressed patients.
Depression also predicts higher morbidity and mortality rates in patients undergoing coronary artery bypass grafting,37,38 patients with congestive heart failure,39 and heart transplant recipients.40
MEDICAL ILLNESS CAN PREDISPOSE TO DEPRESSION, AND VICE VERSA
Medical illnesses can predispose a patient to develop depression. Specifically, compared with healthy people, cardiac patients appear to be at greater risk of developing depression for many years after the initial medical diagnosis is made.41
Katon et al42 reviewed 31 studies involving 16,922 patients, that assessed the impact of depression and anxiety in chronic medical illnesses such as heart disease, diabetes, pulmonary disease, and arthritis. After the severity of the medical disorder was controlled for, patients with depression and anxiety reported a higher number of medical symptoms.
DEPRESSION WORSENS QUALITY OF LIFE AND ADHERENCE TO TREATMENT
Depressed patients perceive their health status and quality of life negatively. In the Heart and Soul study,43 depressive symptoms and low exercise capacity—but not low ejection fraction or ischemia—were significantly associated with perceived deterioration of health in patients with coronary artery disease.
After an MI, patients who take their cardiac drugs properly have a better chance of survival.44,45 Clinical depression can worsen compliance with cardiac medication regimens,46 and reducing depression increases medication adherence overall.47 Not surprisingly, depressed patients also adhere less well to other recommendations,48 including modifying the diet, exercising, stopping smoking, and attending cardiac rehabilitation programs. 49
PLAUSIBLE MECHANISMS LINK DEPRESSION AND HEART DISEASE
Traditional cardiac risk factors such as smoking, high cholesterol, hypertension, diabetes, and obesity tend to cluster in depressed patients. 50 Other mechanisms linking depression and heart disease are reviewed below.51,52
Autonomic imbalance
Excessive sympathetic stimulation or diminished vagal stimulation or both are associated with higher rates of morbidity and death.53
Lack of variability in the heart rate reflects a sympathetic-vagal imbalance and is a risk factor for ventricular arrhythmias and sudden cardiac death in patients with cardiovascular disease.54 Carney et al55 reported that patients with coronary artery disease and depression had significantly less heart rate variability than nondepressed cardiac patients. Similarly, after an MI, depressed patients had significantly less heart rate variability than nondepressed patients,56 implying that low heart rate variability may mediate the adverse effect of depression on survival after an MI.57
In the Heart and Soul study, Gehi et al58 found no distinct relationship between heart rate variability and depression. However, in the same study, de Jong et al59 did find specific somatic symptoms of depression to be associated with lower heart rate variability, although cognitive symptoms were not.
Platelet activation, endothelial dysfunction
Depressed patients have been found to have exaggerated platelet reactivity.60 Plasma levels of platelet factor IV and beta-thromboglobulin, markers of platelet activation, are higher in depressed patients with ischemic heart disease than in nondepressed patients with ischemic heart disease and in control patients.61 This activation of platelets can lead to vascular damage and thrombosis.
In a subset study of the Sertraline Anti-Depressant Heart Attack Randomized Trial (SADHART), depressed MI patients were treated with sertraline (Zoloft), a selective serotonin reuptake inhibitor (SSRI), and had substantially less platelet and endothelial biomarker release.62
Depressed cardiac patients also have impaired flow-mediated dilation of the brachial artery, a sign of endothelial dysfunction.63 Although a recent study did not find coronary endothelial dysfunction in depressed patients who did not have cardiac disease, these patients had more clustering of other cardiac risk factors.64
Hypothalamic-pituitary-adrenocortical and sympathetic adrenal medullary activation
High cortisol levels can accelerate the development of hypertension and atherosclerosis and result in endothelial vascular injury. Sympathoadrenal activation in turn can lead to higher levels of catecholamines, predisposing to vasoconstriction, a rapid heart rate, and platelet activation. Depressed patients have more activation of the hypothalamic-pituitary-adrenocortical and sympathetic adrenal medullary systems,51,65 yet another plausible mechanism for worse clinical outcomes in depressed cardiac patients.
Sudden emotional stress can cause transient left ventricular dysfunction, even in people without coronary disease, an effect that may be mediated by elevated plasma catecholamine levels.66
Inflammatory cytokines
Inflammatory cytokines play a key role in the development of atherosclerosis.67 C-reactive protein, an acute-phase reactant produced in hepatocytes, can be induced by cytokines such as interleukin 6. Damage to endothelial tissues leads to the release of inflammatory cytokines, including interleukin 1, interleukin 6, and tumor tumor necrosis factor alpha.
Depressed patients have higher levels of these inflammatory markers.68,69 A prospective study reported direct correlations between depression scores and C-reactive protein levels in post-MI patients.70 The Heart and Soul study, however, did not confirm that coronary patients have more inflammation if they have depression,71 indicating that the relationship is complex and is perhaps more evident in specific types of depression.72
Anticholinergic inflammatory pathway
Tracey73 proposed a theory that vagal tone inhibits the release of inflammatory cytokines. This has important implications for treatment, as exercise, biofeedback, and meditation can stimulate the vagus nerve and therefore have beneficial anti-inflammatory effects.74
Polymorphism in the serotonin transport promoter region gene
Research is focusing on the serotonin transport promoter region gene (5-HTTLPR).75 The gene exists in two forms, a long one and a less-effective short one that appears to predispose to depression.76
Nakatani et al77 showed that MI patients were more likely to become depressed and to have subsequent cardiac events if one or both of their alleles of this gene were short. Otte et al,78 using Heart and Soul study data, found that patients with a short allele had a higher likelihood of depression, higher perceived levels of stress, and higher urinary norepinephrine secretion. However, the long allele genotype may be associated with a higher risk of developing an MI.79
Our knowledge of the genetic interplay of depression and cardiovascular disease is still in its infancy, and further studies are needed to clarify these findings.
IN TRIALS, LESS DEPRESSION BUT NO EFFECT ON DEATHS, RECURRENT MI
Major behavioral and drug trials conducted in the last 15 years have focused on how to best treat depression in cardiac patients.80–85
The Montreal Heart Attack Readjustment Trial (MHART)81 used telephone calls and home nursing visits to explore and monitor psychological distress for up to 1 year after an MI. The overall trial did not show these interventions to have any impact on survival compared with usual care. In fact, in women receiving the telephone intervention, there was a trend toward higher rates of cardiac and all-cause death, which was quite unexpected. Uncovering stresses and problems without resolving them, rather than encouraging patients to place these on the “back burner,” may partially explain these results.
SADHART82 studied the safety of sertraline in depressed post-MI patients. No major differences in cardiac function were noted between the sertraline and placebo groups, showing that sertraline was safe for these patients. The sertraline group had fewer cardiovascular events, but the difference was not statistically significant.
The Enhancing Recovery in Coronary Heart Disease (ENRICHD) study83 was primarily designed to see whether a psychosocial intervention would decrease deaths in depressed cardiac patients. Much to the chagrin of behavioral medicine, the group undergoing cognitive behavioral therapy did not have a higher rate of event-free survival, although the intervention had a favorable impact on depression and social support.
The Myocardial Infarction Depression Intervention Trial (MIND-IT)84 looked at whether the antidepressant mirtazapine (Remeron) would improve long-term depression and cardiovascular outcomes in depressed post-MI patients. In 18 months of follow-up, neither objective was obtained.
The Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial85 tested the efficacy of the SSRI citalopram (Celexa) and interpersonal therapy in a short-term intervention. Here, the antidepressant was superior to placebo in the primary outcome of treating depression, but interpersonal therapy had no advantage over “clinical management,” ie, a shorter, 20-minute supportive intervention.
Common threads in these studies.
- In ENRICHD and MIND-IT, patients whose depression did not respond to treatment were at higher risk of cardiac events during follow-up.86–88
- In SADHART and CREATE, which used drug treatment, the antidepressant response was more robust in patients with a history of depression before their heart attacks, suggesting that a patient with recurrent depression at the time of a cardiac event should receive medication for it.85,89
CLINICAL RECOMMENDATIONS
Use a depression screening tool
Ziegelstein et al90 recently studied the ability of clinical personnel to detect depression in hospitalized MI patients. If a screening tool was not used, the results were abysmal, indicating the need to use formal screening for symptoms of depression in acute MI patients.
Many self-rating scales are available, among which are the Beck Depression Inventory (BDI) and the Hospital Anxiety and Depression Scale (HADS). Others are:
The PHQ-2 consists of the two first questions of the PHQ-9, which deal with mood and lack of pleasure. A cut-off score of 3 or higher has a sensitivity of 83% and a specificity of 92%,96 fulfilling the need for a quick and reliable depression screening tool. The clinician can also ask for a yes-or-no answer to the two questions of the PHQ-2 (Table 1). A yes to either of the two questions is up to 90% sensitive and 75% specific.92,97
When to suspect depression in cardiac patients
Which type of psychotherapy is best?
The negative results of psychosocial interventions (phone calls and home visits from a nurse) in MHART and of cognitive behavioral therapy in ENRICHD raise questions about which type of psychotherapy is best for depression in heart disease. CREATE found that 50-minute weekly sessions of interpersonal psychotherapy were no more beneficial than clinical management, ie, 20-minute weekly sessions that focused on compliance with treatment and education about depression and overall management. Perhaps a type of therapy akin to “clinical management” in this study or the brief behavior-based and targeted therapy used in the Improving Mood Promoting Access to Collaborative Care Treatment (IMPACT) trials of depression in primary care99 could be designed specifically to treat depression in cardiac disease. However, it is also quite possible that treatments that focus on uncovering stresses or problems may not be timely for these patients.
Which therapy is best for women is another area of consideration. In MHART, even after 5 years of follow-up,100 women who received the psychosocial support intervention did marginally worse. In the ENRICHD study, women did not experience a benefit from cognitive behavioral therapy. Further studies must address sex differences in response to different therapies.
SSRIs seem to be better than other antidepressants for cardiac patients
Before SSRIs were available, tricyclic antidepressants were the mainstays. Subsequent analysis showed the tricyclics to have an unfavorable risk-benefit profile in cardiac patients,101 and since other types of antidepressants are available, tricyclics should be avoided altogether in cardiac patients.102
Whether the SSRIs actually decrease one’s risk of death in heart disease is still an issue of debate, but there are encouraging signs. In SADHART, the rate of death and recurrent nonfatal MI was 20% lower in the patients randomized to receive sertraline, although the difference was not statistically significant.82 In ENRICHD, patients who did not respond to cognitive behavioral treatment or had severe depression could receive sertraline or other antidepressant drugs on a nonrandomized basis, and those who did had a 42% lower incidence of death or recurrent MI.103
The SADHART and CREATE trials provide convincing evidence of the cardiac safety and antidepressant efficacy of two SSRIs (sertraline and citalopram) in depressed cardiac patients. Mirtazapine, studied in MIND-IT, was not effective in treating depression in cardiac patients, although it had a better adverse effect and safety profile than tricyclic antidepressants. 104
Clinical observations indicate that SSRIs are associated with less risk of MI than non-SSRI drugs.105,106 During hospitalization for acute coronary syndromes, patients on SSRIs had lower rates of recurrent ischemia and heart failure but higher bleeding rates than patients not taking SSRIs.107 In a retrospective study of patients undergoing coronary artery bypass grafting, those on an SSRI before surgery had higher rates of death and rehospitalization.108 Being on antidepressant medication could be interpreted as a surrogate marker of having more severe depression before surgery; this issue clearly requires further study.
Given current observations and recent data from interventional trials coupled with the safe drug-interaction profile of sertraline and citalopram, these two SSRIs are recommended for treating depression in cardiac patients. If the patient is also receiving an anticoagulant, one should monitor for bleeding, as all SSRIs are associated with a prolonged bleeding time. Monitoring for rare cases of hyponatremia and bradycardia should also be part of early follow-up.
Do cardiac drugs have psychiatric effects?
Some concerns have arisen about cardiovascular drugs causing or aggravating psychiatric conditions.
Statins were once suspected of causing clinical depression or even suicide. However, subsequent studies have not substantiated this.109,110 In fact, long-term statin use has been associated with improved psychological wellbeing. 111 Whether the favorable psychological profile is due to an improved lifestyle, a direct noncholesterol effect, or an immunomodulatory effect has yet to be determined.
Beta-blockers have been suspected of increasing depression and fatigue. Robust metaanalyses have shown no increased risk of depressive symptoms but a small increased risk of fatigue and sexual dysfunction.112 Observational trials in the first year post-MI have shown no differences between beta-blocker users and nonusers in depressive symptoms or depressive disorders.113
Statins and beta-blockers offer both immense cardiac benefit and low risk, and both may be prescribed with confidence in depressed cardiac patients.
Refer patients for cardiac rehabilitation
The American Association of Cardiovascular and Pulmonary Rehabilitation strongly recommends screening cardiac patients for depression and referring them to cardiac rehabilitation programs.114 Typical programs run 12 weeks, affording an opportunity to further listen to and assess the patient and to promote general wellness via nutrition, stress management, and exercise.
These interventions by themselves can favorably affect depression. Blumenthal and colleagues,115 in the Standard Medical Intervention and Long-Term Exercise (SMILE) study, found that exercise was as effective as drug treatment in reducing depression. In addition, stress management as a psychosocial treatment in cardiac rehabilitation can reduce death rates in cardiac patients.116
Unfortunately, many patients who are eligible for cardiac rehabilitation programs do not avail themselves of them.117
Our algorithm
FUTURE DIRECTIONS FOR RESEARCH
Can we predict the course of depression?
We need to identify better which patients will have a spontaneous remission of their depressive symptoms after a cardiac event, which patients will linger with depression, and which patients will best respond to treatment. Risk stratification, using the psychiatric history, symptoms and severity of depression, and genetic predisposition118 might allow improved targeted therapies.
Does depression cause cardiac disease?
The link between depression and heart disease can be seen as merely an association. In the interventional trials performed to date, we have not yet seen a reduction in cardiac deaths when depression was treated, challenging any assumption of a causal relationship between depression and heart disease. The debate about association vs cause is germane to behavioral medicine,119 and the better we understand the mechanistic pathways, the better we can advise patients and treat depression comorbid with heart disease.
Behavioral medicine is currently measuring the aspects of depression associated with cardiac disease, including the spectrum of somatic (body) and affective (mood) symptoms120 and specific areas such as sympathetic arousal and early morning insomnia.121 If we can determine the depression subtype that carries a worse cardiac prognosis, we may untangle the biobehavioral links that bidirectionally bridge clinical depression and cardiac disease.
Another area of interest, emotional vitality (a positive state associated with interest, enthusiasm, excitement, and energy for living) has been shown to protect against coronary heart disease122 and holds much promise.
In the plenary lecture of the Academy of Psychosomatic Medicine in 2006, Frasure-Smith spoke of the “pleiotropism” of our antidepressant interventions on the various risk factors in depressed cardiac patients.123 We need behavioral medicine studies that elucidate these mechanisms, guiding more precise treatments as well as novel therapies. Omega-3 fatty acids, which benefit heart disease and clinical depression,124 will be used in a randomized controlled trial by Lespérance and colleagues.125 We await the results of this exciting research.
Will treating depression help in other types of heart disease?
The SADHART-CHF trial is examining whether 12 weeks of sertraline therapy is better than placebo in preventing death and improving cardiac outcomes in patients with chronic heart failure and comorbid major depressive disorder. It was to be completed in the fall of 2008. The results and experience of this study will help in designing future interventional trials to reduce the risk of depression in cardiovascular diseases.
We also await the results of a National Heart, Lung, and Blood Institute (NHLBI) trial, “Bypassing the Blues,” which is studying the treatment of depression after cardiac bypass surgery. This study should provide further insights into management of the depressed cardiac patient. Further prognostic studies in cardiac patients are also needed using the PHQ-9 and its shorter version, PHQ-2.
Current and future guidelines
For years our European colleagues have been ahead of us in recognizing depression screening and stress management as key to cardiac disease-prevention strategies.126 The NHLBI nicely outlined recommendations on the assessment and treatment of depression in cardiovascular patients.127 The just-published AHA Science Advisory should further encourage clinicians to screen and treat depression in the patient population.1 As our knowledge grows, we look forward to future evidence-based guidelines for depressed cardiac patients.
Depression is a risk factor for heart disease, and in patients with heart disease, it is a risk factor for complications and death. Unfortunately, in the trials performed to date, treating depression in cardiac patients did not lead to lower rates of recurrent cardiovascular events or death. Nevertheless, we recommend that clinicians systematically screen for it in their heart patients, in view of the benefits of antidepressant therapy.
In this article we review key epidemiologic and psychosocial studies, the mechanistic links between depression and heart disease, and recent intervention trials. We also offer practical management advice and address the continued need for guidelines and risk stratification in the treatment of depressed cardiac patients.
After we submitted our review article, the American Heart Association (AHA)1 released a consensus document recommending that health care providers screen for and treat depression in patients with coronary heart disease. We will discuss the same screening tests that have been recommended by the AHA.
DEPRESSION AND HEART DISEASE: COMMON AND LINKED
Depression and heart disease are very common and often coexist: the prevalence of depression in various heart conditions ranges from 15% to 20%.1–3 According to data from the World Health Organization, by the year 2020 depression will be the second-leading cause of disability in developed countries (after heart disease).4
The World Health Survey5 showed that depression worsens health more than angina, arthritis, asthma, or diabetes. Furthermore, patients with severe mental illness have a higher risk of dying from heart disease and stroke.6
SOME HEART DISEASE RISK FACTORS ARE PSYCHOSOCIAL
In the 1980s, the “type A” personality (ambitious, aggressive, hostile, and competitive, with a chronic sense of urgency) was linked to heart disease.7 Later studies differed as to whether the entire set of features is valid as a collective risk factor for progressive heart disease,8 but hostility remains a validated risk factor and a focus of behavior modification.9,10
Other psychosocial risk factors have been implicated,11,12 one of which is social isolation.9,13 Another is the “type D” personality, which includes a tendency to experience negative emotions across time and situations coupled with social inhibition and which is believed to be more valid than the type A personality as a risk factor for cardiac disease.14,15
The INTERHEART study16 gathered data about attributable risk in the development of myocardial infarction (MI) in 52 countries in a case-control fashion. Psychosocial factors including stress, low generalized locus of control (ie, the perceived inability to control one’s life), and depression accounted for 32.5% of the attributable risk for an MI.17 This would mean that they account for slightly less attributable risk than that of lifetime smoking but more than that of hypertension and obesity.
Job stress increases the risk of initial coronary heart disease18 and also the risk of recurrent cardiac events after a first MI.19 Even though numerous psychosocial risk factors have been associated with coronary heart disease, including anxiety,20,21 depression is perhaps the best studied.
PROSPECTIVE STUDIES OF DEPRESSION AND HEART DISEASE
To examine the impact of depression in coronary heart disease, prospective studies have been done in healthy people and in patients with established cardiovascular disease who develop depression.22
In healthy people, depression increases the risk of coronary disease
The 1996 Epidemiologic Catchment Area study23 found that people with major depression had a risk of MI four times higher than the norm, and people with 2 weeks of sadness or dysphoria had a risk two times higher.
A subsequent meta-analysis of 11 studies,24 which included 36,000 patients, found that the overall relative risk of developing heart disease in depressed but healthy people was 1.64.
A meta-analysis by Van der Kooy et al25 of 28 epidemiologic studies with nearly 80,000 patients showed depression to be an independent risk factor for cardiovascular disease.
Wulsin and Singal26 performed a systematic review to see if depression increases the risk of coronary disease. In 10 studies with a follow-up of more than 4 years, the relative risk in people with depression was 1.64, which was less than that in active smokers (2.5) but more than that in passive smokers (1.25).
Depression can also exacerbate the classic risk factors for coronary disease, such as smoking, diabetes, obesity, and physical inactivity. 27
A 2007 study from Sweden28 prospectively followed patients who were hospitalized for depression. The odds ratio of developing an acute MI was 2.9, and the risk persisted for decades after the initial hospitalization.
A prospective United Kingdom cohort study of people initially free of heart disease revealed major depression to be associated with a higher rate of death from ischemic heart disease.29 Specifically, patients who had depression currently or in the past 12 months had a 2.7 times higher risk of dying than those who had never had depression or who had had it more than 12 months previously.
In existing heart disease, depression predicts recurrent events, death
Carney et el30 found that patients with major depressive disorder had a higher incidence of new cardiac events in the 12 months after undergoing cardiac catheterization than those without major depressive disorder.
Frasure-Smith et al,31 in a landmark study, showed that patients who were depressed at 1 week after an MI were three to four times more likely to die in the next 6 months than nondepressed post-MI patients. Even after 18 months, depression remained an independent risk factor for cardiac-related death.32
In longer studies (with up to 19.4 years of follow-up), depression was associated with higher rates of death from cardiac and all causes in patients with coronary artery disease.33 Lespérance et al34 found that in MI patients, the higher the Beck Depression Inventory score at the time of hospital admission, the higher the 5-year death rate.
Using meta-analysis, Barth et al35 found the risk of dying in the first 2 years after initial assessment to be twice as high in depressed cardiac patients as in nondepressed cardiac patients (odds ratio 2.24).
Van Melle et al36 reviewed 22 studies and found that in the 2 years after an MI, depressed patients had a 2 to 2.5 times higher risk of dying of a cardiac or any other cause than did nondepressed patients.
Depression also predicts higher morbidity and mortality rates in patients undergoing coronary artery bypass grafting,37,38 patients with congestive heart failure,39 and heart transplant recipients.40
MEDICAL ILLNESS CAN PREDISPOSE TO DEPRESSION, AND VICE VERSA
Medical illnesses can predispose a patient to develop depression. Specifically, compared with healthy people, cardiac patients appear to be at greater risk of developing depression for many years after the initial medical diagnosis is made.41
Katon et al42 reviewed 31 studies involving 16,922 patients, that assessed the impact of depression and anxiety in chronic medical illnesses such as heart disease, diabetes, pulmonary disease, and arthritis. After the severity of the medical disorder was controlled for, patients with depression and anxiety reported a higher number of medical symptoms.
DEPRESSION WORSENS QUALITY OF LIFE AND ADHERENCE TO TREATMENT
Depressed patients perceive their health status and quality of life negatively. In the Heart and Soul study,43 depressive symptoms and low exercise capacity—but not low ejection fraction or ischemia—were significantly associated with perceived deterioration of health in patients with coronary artery disease.
After an MI, patients who take their cardiac drugs properly have a better chance of survival.44,45 Clinical depression can worsen compliance with cardiac medication regimens,46 and reducing depression increases medication adherence overall.47 Not surprisingly, depressed patients also adhere less well to other recommendations,48 including modifying the diet, exercising, stopping smoking, and attending cardiac rehabilitation programs. 49
PLAUSIBLE MECHANISMS LINK DEPRESSION AND HEART DISEASE
Traditional cardiac risk factors such as smoking, high cholesterol, hypertension, diabetes, and obesity tend to cluster in depressed patients. 50 Other mechanisms linking depression and heart disease are reviewed below.51,52
Autonomic imbalance
Excessive sympathetic stimulation or diminished vagal stimulation or both are associated with higher rates of morbidity and death.53
Lack of variability in the heart rate reflects a sympathetic-vagal imbalance and is a risk factor for ventricular arrhythmias and sudden cardiac death in patients with cardiovascular disease.54 Carney et al55 reported that patients with coronary artery disease and depression had significantly less heart rate variability than nondepressed cardiac patients. Similarly, after an MI, depressed patients had significantly less heart rate variability than nondepressed patients,56 implying that low heart rate variability may mediate the adverse effect of depression on survival after an MI.57
In the Heart and Soul study, Gehi et al58 found no distinct relationship between heart rate variability and depression. However, in the same study, de Jong et al59 did find specific somatic symptoms of depression to be associated with lower heart rate variability, although cognitive symptoms were not.
Platelet activation, endothelial dysfunction
Depressed patients have been found to have exaggerated platelet reactivity.60 Plasma levels of platelet factor IV and beta-thromboglobulin, markers of platelet activation, are higher in depressed patients with ischemic heart disease than in nondepressed patients with ischemic heart disease and in control patients.61 This activation of platelets can lead to vascular damage and thrombosis.
In a subset study of the Sertraline Anti-Depressant Heart Attack Randomized Trial (SADHART), depressed MI patients were treated with sertraline (Zoloft), a selective serotonin reuptake inhibitor (SSRI), and had substantially less platelet and endothelial biomarker release.62
Depressed cardiac patients also have impaired flow-mediated dilation of the brachial artery, a sign of endothelial dysfunction.63 Although a recent study did not find coronary endothelial dysfunction in depressed patients who did not have cardiac disease, these patients had more clustering of other cardiac risk factors.64
Hypothalamic-pituitary-adrenocortical and sympathetic adrenal medullary activation
High cortisol levels can accelerate the development of hypertension and atherosclerosis and result in endothelial vascular injury. Sympathoadrenal activation in turn can lead to higher levels of catecholamines, predisposing to vasoconstriction, a rapid heart rate, and platelet activation. Depressed patients have more activation of the hypothalamic-pituitary-adrenocortical and sympathetic adrenal medullary systems,51,65 yet another plausible mechanism for worse clinical outcomes in depressed cardiac patients.
Sudden emotional stress can cause transient left ventricular dysfunction, even in people without coronary disease, an effect that may be mediated by elevated plasma catecholamine levels.66
Inflammatory cytokines
Inflammatory cytokines play a key role in the development of atherosclerosis.67 C-reactive protein, an acute-phase reactant produced in hepatocytes, can be induced by cytokines such as interleukin 6. Damage to endothelial tissues leads to the release of inflammatory cytokines, including interleukin 1, interleukin 6, and tumor tumor necrosis factor alpha.
Depressed patients have higher levels of these inflammatory markers.68,69 A prospective study reported direct correlations between depression scores and C-reactive protein levels in post-MI patients.70 The Heart and Soul study, however, did not confirm that coronary patients have more inflammation if they have depression,71 indicating that the relationship is complex and is perhaps more evident in specific types of depression.72
Anticholinergic inflammatory pathway
Tracey73 proposed a theory that vagal tone inhibits the release of inflammatory cytokines. This has important implications for treatment, as exercise, biofeedback, and meditation can stimulate the vagus nerve and therefore have beneficial anti-inflammatory effects.74
Polymorphism in the serotonin transport promoter region gene
Research is focusing on the serotonin transport promoter region gene (5-HTTLPR).75 The gene exists in two forms, a long one and a less-effective short one that appears to predispose to depression.76
Nakatani et al77 showed that MI patients were more likely to become depressed and to have subsequent cardiac events if one or both of their alleles of this gene were short. Otte et al,78 using Heart and Soul study data, found that patients with a short allele had a higher likelihood of depression, higher perceived levels of stress, and higher urinary norepinephrine secretion. However, the long allele genotype may be associated with a higher risk of developing an MI.79
Our knowledge of the genetic interplay of depression and cardiovascular disease is still in its infancy, and further studies are needed to clarify these findings.
IN TRIALS, LESS DEPRESSION BUT NO EFFECT ON DEATHS, RECURRENT MI
Major behavioral and drug trials conducted in the last 15 years have focused on how to best treat depression in cardiac patients.80–85
The Montreal Heart Attack Readjustment Trial (MHART)81 used telephone calls and home nursing visits to explore and monitor psychological distress for up to 1 year after an MI. The overall trial did not show these interventions to have any impact on survival compared with usual care. In fact, in women receiving the telephone intervention, there was a trend toward higher rates of cardiac and all-cause death, which was quite unexpected. Uncovering stresses and problems without resolving them, rather than encouraging patients to place these on the “back burner,” may partially explain these results.
SADHART82 studied the safety of sertraline in depressed post-MI patients. No major differences in cardiac function were noted between the sertraline and placebo groups, showing that sertraline was safe for these patients. The sertraline group had fewer cardiovascular events, but the difference was not statistically significant.
The Enhancing Recovery in Coronary Heart Disease (ENRICHD) study83 was primarily designed to see whether a psychosocial intervention would decrease deaths in depressed cardiac patients. Much to the chagrin of behavioral medicine, the group undergoing cognitive behavioral therapy did not have a higher rate of event-free survival, although the intervention had a favorable impact on depression and social support.
The Myocardial Infarction Depression Intervention Trial (MIND-IT)84 looked at whether the antidepressant mirtazapine (Remeron) would improve long-term depression and cardiovascular outcomes in depressed post-MI patients. In 18 months of follow-up, neither objective was obtained.
The Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial85 tested the efficacy of the SSRI citalopram (Celexa) and interpersonal therapy in a short-term intervention. Here, the antidepressant was superior to placebo in the primary outcome of treating depression, but interpersonal therapy had no advantage over “clinical management,” ie, a shorter, 20-minute supportive intervention.
Common threads in these studies.
- In ENRICHD and MIND-IT, patients whose depression did not respond to treatment were at higher risk of cardiac events during follow-up.86–88
- In SADHART and CREATE, which used drug treatment, the antidepressant response was more robust in patients with a history of depression before their heart attacks, suggesting that a patient with recurrent depression at the time of a cardiac event should receive medication for it.85,89
CLINICAL RECOMMENDATIONS
Use a depression screening tool
Ziegelstein et al90 recently studied the ability of clinical personnel to detect depression in hospitalized MI patients. If a screening tool was not used, the results were abysmal, indicating the need to use formal screening for symptoms of depression in acute MI patients.
Many self-rating scales are available, among which are the Beck Depression Inventory (BDI) and the Hospital Anxiety and Depression Scale (HADS). Others are:
The PHQ-2 consists of the two first questions of the PHQ-9, which deal with mood and lack of pleasure. A cut-off score of 3 or higher has a sensitivity of 83% and a specificity of 92%,96 fulfilling the need for a quick and reliable depression screening tool. The clinician can also ask for a yes-or-no answer to the two questions of the PHQ-2 (Table 1). A yes to either of the two questions is up to 90% sensitive and 75% specific.92,97
When to suspect depression in cardiac patients
Which type of psychotherapy is best?
The negative results of psychosocial interventions (phone calls and home visits from a nurse) in MHART and of cognitive behavioral therapy in ENRICHD raise questions about which type of psychotherapy is best for depression in heart disease. CREATE found that 50-minute weekly sessions of interpersonal psychotherapy were no more beneficial than clinical management, ie, 20-minute weekly sessions that focused on compliance with treatment and education about depression and overall management. Perhaps a type of therapy akin to “clinical management” in this study or the brief behavior-based and targeted therapy used in the Improving Mood Promoting Access to Collaborative Care Treatment (IMPACT) trials of depression in primary care99 could be designed specifically to treat depression in cardiac disease. However, it is also quite possible that treatments that focus on uncovering stresses or problems may not be timely for these patients.
Which therapy is best for women is another area of consideration. In MHART, even after 5 years of follow-up,100 women who received the psychosocial support intervention did marginally worse. In the ENRICHD study, women did not experience a benefit from cognitive behavioral therapy. Further studies must address sex differences in response to different therapies.
SSRIs seem to be better than other antidepressants for cardiac patients
Before SSRIs were available, tricyclic antidepressants were the mainstays. Subsequent analysis showed the tricyclics to have an unfavorable risk-benefit profile in cardiac patients,101 and since other types of antidepressants are available, tricyclics should be avoided altogether in cardiac patients.102
Whether the SSRIs actually decrease one’s risk of death in heart disease is still an issue of debate, but there are encouraging signs. In SADHART, the rate of death and recurrent nonfatal MI was 20% lower in the patients randomized to receive sertraline, although the difference was not statistically significant.82 In ENRICHD, patients who did not respond to cognitive behavioral treatment or had severe depression could receive sertraline or other antidepressant drugs on a nonrandomized basis, and those who did had a 42% lower incidence of death or recurrent MI.103
The SADHART and CREATE trials provide convincing evidence of the cardiac safety and antidepressant efficacy of two SSRIs (sertraline and citalopram) in depressed cardiac patients. Mirtazapine, studied in MIND-IT, was not effective in treating depression in cardiac patients, although it had a better adverse effect and safety profile than tricyclic antidepressants. 104
Clinical observations indicate that SSRIs are associated with less risk of MI than non-SSRI drugs.105,106 During hospitalization for acute coronary syndromes, patients on SSRIs had lower rates of recurrent ischemia and heart failure but higher bleeding rates than patients not taking SSRIs.107 In a retrospective study of patients undergoing coronary artery bypass grafting, those on an SSRI before surgery had higher rates of death and rehospitalization.108 Being on antidepressant medication could be interpreted as a surrogate marker of having more severe depression before surgery; this issue clearly requires further study.
Given current observations and recent data from interventional trials coupled with the safe drug-interaction profile of sertraline and citalopram, these two SSRIs are recommended for treating depression in cardiac patients. If the patient is also receiving an anticoagulant, one should monitor for bleeding, as all SSRIs are associated with a prolonged bleeding time. Monitoring for rare cases of hyponatremia and bradycardia should also be part of early follow-up.
Do cardiac drugs have psychiatric effects?
Some concerns have arisen about cardiovascular drugs causing or aggravating psychiatric conditions.
Statins were once suspected of causing clinical depression or even suicide. However, subsequent studies have not substantiated this.109,110 In fact, long-term statin use has been associated with improved psychological wellbeing. 111 Whether the favorable psychological profile is due to an improved lifestyle, a direct noncholesterol effect, or an immunomodulatory effect has yet to be determined.
Beta-blockers have been suspected of increasing depression and fatigue. Robust metaanalyses have shown no increased risk of depressive symptoms but a small increased risk of fatigue and sexual dysfunction.112 Observational trials in the first year post-MI have shown no differences between beta-blocker users and nonusers in depressive symptoms or depressive disorders.113
Statins and beta-blockers offer both immense cardiac benefit and low risk, and both may be prescribed with confidence in depressed cardiac patients.
Refer patients for cardiac rehabilitation
The American Association of Cardiovascular and Pulmonary Rehabilitation strongly recommends screening cardiac patients for depression and referring them to cardiac rehabilitation programs.114 Typical programs run 12 weeks, affording an opportunity to further listen to and assess the patient and to promote general wellness via nutrition, stress management, and exercise.
These interventions by themselves can favorably affect depression. Blumenthal and colleagues,115 in the Standard Medical Intervention and Long-Term Exercise (SMILE) study, found that exercise was as effective as drug treatment in reducing depression. In addition, stress management as a psychosocial treatment in cardiac rehabilitation can reduce death rates in cardiac patients.116
Unfortunately, many patients who are eligible for cardiac rehabilitation programs do not avail themselves of them.117
Our algorithm
FUTURE DIRECTIONS FOR RESEARCH
Can we predict the course of depression?
We need to identify better which patients will have a spontaneous remission of their depressive symptoms after a cardiac event, which patients will linger with depression, and which patients will best respond to treatment. Risk stratification, using the psychiatric history, symptoms and severity of depression, and genetic predisposition118 might allow improved targeted therapies.
Does depression cause cardiac disease?
The link between depression and heart disease can be seen as merely an association. In the interventional trials performed to date, we have not yet seen a reduction in cardiac deaths when depression was treated, challenging any assumption of a causal relationship between depression and heart disease. The debate about association vs cause is germane to behavioral medicine,119 and the better we understand the mechanistic pathways, the better we can advise patients and treat depression comorbid with heart disease.
Behavioral medicine is currently measuring the aspects of depression associated with cardiac disease, including the spectrum of somatic (body) and affective (mood) symptoms120 and specific areas such as sympathetic arousal and early morning insomnia.121 If we can determine the depression subtype that carries a worse cardiac prognosis, we may untangle the biobehavioral links that bidirectionally bridge clinical depression and cardiac disease.
Another area of interest, emotional vitality (a positive state associated with interest, enthusiasm, excitement, and energy for living) has been shown to protect against coronary heart disease122 and holds much promise.
In the plenary lecture of the Academy of Psychosomatic Medicine in 2006, Frasure-Smith spoke of the “pleiotropism” of our antidepressant interventions on the various risk factors in depressed cardiac patients.123 We need behavioral medicine studies that elucidate these mechanisms, guiding more precise treatments as well as novel therapies. Omega-3 fatty acids, which benefit heart disease and clinical depression,124 will be used in a randomized controlled trial by Lespérance and colleagues.125 We await the results of this exciting research.
Will treating depression help in other types of heart disease?
The SADHART-CHF trial is examining whether 12 weeks of sertraline therapy is better than placebo in preventing death and improving cardiac outcomes in patients with chronic heart failure and comorbid major depressive disorder. It was to be completed in the fall of 2008. The results and experience of this study will help in designing future interventional trials to reduce the risk of depression in cardiovascular diseases.
We also await the results of a National Heart, Lung, and Blood Institute (NHLBI) trial, “Bypassing the Blues,” which is studying the treatment of depression after cardiac bypass surgery. This study should provide further insights into management of the depressed cardiac patient. Further prognostic studies in cardiac patients are also needed using the PHQ-9 and its shorter version, PHQ-2.
Current and future guidelines
For years our European colleagues have been ahead of us in recognizing depression screening and stress management as key to cardiac disease-prevention strategies.126 The NHLBI nicely outlined recommendations on the assessment and treatment of depression in cardiovascular patients.127 The just-published AHA Science Advisory should further encourage clinicians to screen and treat depression in the patient population.1 As our knowledge grows, we look forward to future evidence-based guidelines for depressed cardiac patients.
- Lichtman JH, Bigger JT, Blumenthal JA, et al. Depression and coronary heart disease. Recommendations for screening, referral, and treatment. Circulation 2008; 118:1768–1775.
- Jiang W, Glassman A, Krishnan R, O’Connor CM, Califf RM. Depression and ischemic heart disease: what have we learned so far and what must we do in the future? Am Heart J 2005; 150:54–78.
- Freedland KE, Rich MW, Skala JA, Carney RM, Davila-Roman VG, Jaffe AS. Prevalence of depression in hospitalized patients with congestive heart failure. Psychosom Med 2003; 65:119–128.
- Murray CJ, Lopez AD, Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet 1997; 349:1436–1442.
- Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet 2007; 370:851–858.
- Osborn DP, Levy G, Nazareth I, Petersen I, Islam A, King MB. Relative risk of cardiovascular and cancer mortality in people with severe mental illness from the United Kingdom’s general practice research database. Arch Gen Psychiatry 2007; 64:242–249.
- Friedman M, Thoresen CE, Gill JJ, et al. Alteration of type A behavior and its effect on cardiac recurrences in post myocardial infarction patients: summary results of the recurrent coronary prevention project. Am Heart J 1986; 112:653–665.
- Ragland DR, Brand RJ. Type A behavior and mortality from coronary heart disease. N Engl J Med 1988; 318:65–69.
- Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation 1999; 99:2192–2217.
- Iribarren C, Sidney S, Bild DE, et al. Association of hostility with coronary artery calcification in young adults: the CARDIA study. Coronary Artery Risk Development in Young Adults. JAMA 2000; 283:2546–2551.
- Williams RB, Barefoot JC, Schneiderman N. Psychosocial risk factors for cardiovascular disease: more than one culprit at work. JAMA 2003; 290:2190–2192.
- Rozanski A, Blumenthal JA, Davidson KW, Saab PG, Kubzansky L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: the emerging field of behavioral cardiology. J Am Coll Cardiol 2005; 45:637–651.
- Hemingway H, Marmot M. Evidence based cardiology: psychosocial factors in the aetiology and prognosis of coronary heart disease: systematic review of prospective cohort studies. BMJ 1999; 318:1460–1467.
- Denollet J. DS14: Standard assessment of negative affectivity, social inhibition, and type D personality. Psychosom Med 2005; 67:89–97.
- Steptoe A, Molloy GJ. Personality and heart disease. Heart 2007; 93:783–784.
- Yusuf S, Hawken S, Ôunpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004; 364:937–952.
- Rosengren A, Hawken S, Ounpuu S, et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case-control study. Lancet 2004; 364:953–962.
- Kuper H, Marmot M. Job strain, job demands, decision latitude, and risk of coronary heart disease within the Whitehall II study. J Epidemiol Community Health 2003; 57:147–153.
- Aboa-Eboule C, Brisson C, Maunsell E, et al. Job strain and risk of acute recurrent coronary heart disease events. JAMA 2007; 298:1652–1660.
- Frasure-Smith N, Lespérance F. Depression and anxiety as predictors of 2-year cardiac events in patients with stable coronary artery disease. Arch Gen Psychiatry 2008; 65:62–71.
- Shen B-J, Avivi YE, Todaro JF, et al. Anxiety characteristics independently and prospectively predict myocardial infarction in men. J Am Coll Cardiol 2008; 51:113–119.
- Carney RM, Freedland KE. Depression, mortality, and medical morbidity in patients with coronary heart disease. Biol Psychiatry 2003; 54:241–247.
- Pratt LA, Ford DE, Crum RM, Armenian HK, Gallo JJ, Eaton WW. Depression, psychotropic medication, and risk of myocardial infarction: prospective data from the Baltimore ECA follow-up. Circulation 1996; 94:3123–3129.
- Rugulies R. Depression as a predictor for coronary heart disease. A review and meta-analysis. Am J Prev Med 2002; 23:51–61.
- Van der Kooy K, van Hout H, Marwijk H, Marten H, Stehouwer C, Beekman A. Depression and the risk for cardiovascular diseases: systematic review and meta analysis. Int J Geriatr Psychiatry 2007; 22:613–626.
- Wulsin LR, Singal BM. Do depressive symptoms increase the risk for the onset of coronary disease? A systematic quantitative review. Psychosom Med 2003; 65:201–210.
- Wulsin LR. Is depression a major risk factor for coronary disease? A systematic review of the epidemiologic evidence. Harv Rev Psychiatry 2004; 12:79–93.
- Janszky I, Ahlbom A, Hallqvist J, Ahnve S. Hospitalization for depression is associated with an increased risk for myocardial infarction not explained by lifestyle, lipids, coagulation, and inflammation: The SHEEP Study. Biol Psychiatry 2007; 62:25–32.
- Surtees PG, Wainwright NWJ, Luben RN, Wareham NJ, Bingham SA, Khaw K-T. Depression and ischemic heart disease mortality: evidence from the EPIC-Norfolk United Kingdom Prospective Cohort Study. Am J Psychiatry 2008; 165:515–523.
- Carney RM, Rich MW, Freedland KE, et al. Major depressive disorder predicts cardiac events in patients with coronary artery disease. Psychosom Med 1988; 50:627–633.
- Frasure-Smith N, Lespérance F, Talajic M. Depression following myocardial infarction. Impact on 6-month survival. JAMA 1993; 270:1819–1825.
- Frasure-Smith N, Lespérance F, Talajic M. Depression and 18-month prognosis after myocardial infarction. Circulation 1995; 91:999–1005.
- Barefoot JC, Helms MJ, Mark DB, et al. Depression and long-term mortality risk in patients with coronary artery disease. Am J Cardiol 1996; 78:613–617.
- Lespérance F, Frasure-Smith N, Talajic M, Bourassa MG. Five-year risk of cardiac mortality in relation to initial severity and one-year changes in depression symptoms after myocardial infarction. Circulation 2002; 105:1049–1053.
- Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med 2004; 66:802–813.
- van Melle JP, de Jonge P, Spijkerman TA, et al. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis. Psychosom Med 2004; 66:814–822.
- Blumenthal JA, Lett HS, Babyak MA, et al. Depression as a risk factor for mortality after coronary artery bypass surgery. Lancet 2003; 362:604–609.
- Sullivan MD, LaCroix AZ, Spertus JA, Hecht J, Russo J. Depression predicts revascularization procedures for 5 years after coronary angiography. Psychosom Med 2003; 65:229–236.
- Jiang W, Alexander J, Christopher E, et al. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med 2001; 161:1849–1856.
- Zipfel S, Schneider A, Wild B, et al. Effect of depressive symptoms on survival after heart transplantation. Psychosom Med 2002; 64:740–747.
- Polsky D, Doshi JA, Marcus S, et al. Long-term risk for depressive symptoms after a medical diagnosis. Arch Intern Med 2005; 165:1260–1266.
- Katon W, Lin EHB, Kroenke K. The association of depression and anxiety with medical symptom burden in patients with chronic medical illness. Gen Hosp Psychiatry 2007; 29:147–155.
- Ruo B, Rumsfeld JS, Hlatky MA, Liu H, Browner WS, Whooley MA. Depressive symptoms and health-related quality of life: the Heart and Soul Study. JAMA 2003; 290:215–221.
- Rasmussen JN, Chong A, Alter DA. Relationship between adherence to evidence-based pharmacotherapy and long-term mortality after acute myocardial infarction. JAMA 2007; 297:177–186.
- Gehi AK, Ali S, Na B, Whooley MA. Self-reported medication adherence and cardiovascular events in patients with stable coronary heart disease: the Heart and Soul Study. Arch Intern Med 2007; 167:1798–1803.
- Gehi A, Haas D, Pipkin S, Whooley MA. Depression and medication adherence in outpatients with coronary heart disease: findings from the Heart and Soul Study. Arch Intern Med 2005; 165:2508–2513.
- Rieckmann N, Gerin W, Kronish IM, et al. Course of depressive symptoms and medication adherence after acute coronary syndromes: an electronic medication monitoring study. J Am Coll Cardiol 2006; 48:2218–2222.
- Ziegelstein RC, Fauerbach JA, Stevens SS, Romanelli J, Richter DP, Bush DE. Patients with depression are less likely to follow recommendations to reduce cardiac risk during recovery from a myocardial infarction. Arch Intern Med 2000; 160:1818–1823.
- Kronish IM, Rieckmann N, Halm EA, et al. Persistent depression affects adherence to secondary prevention behaviors after acute coronary syndromes. J Gen Intern Med 2006; 21:1178–1183.
- Joynt KE, Whellan DJ, O’Connor CM. Depression and cardiovascular disease: mechanisms of interaction. Biol Psychiatry 2003; 54:248–261.
- Musselman DL, Evans DL, Nemeroff CB. The relationship of depression to cardiovascular disease: epidemiology, biology, and treatment. Arch Gen Psychiatry 1998; 55:580–592.
- Lespérance F, Frasure-Smith N. Depression and heart disease. Cleve Clin J Med 2007; 74(suppl 1):S63–S66.
- Curtis BM. Autonomic tone as a cardiovascular risk factor: the dangers of chronic fight or flight. Mayo Clin Proc 2002; 77:45–54.
- Topol EJ. Textbook of Cardiovascular Medicine, 2nd ed. Philadelphia: Lippincott Williams & Williams 2002.
- Carney RM, Saunders RD, Freedland KE, Stein P, Rich MW, Jaffe AS. Association of depression with reduced heart rate variability in coronary artery disease. Am J Cardiol 1995; 76:562–564.
- Carney RM, Blumenthal JA, Stein PK, et al. Depression, heart rate variability, and acute myocardial infarction. Circulation 2001; 104:2024–2028.
- Carney RM, Blumenthal JA, Freedland KE, et al. Low heart rate variability and the effect of depression on post-myocardial infarction mortality. Arch Intern Med 2005; 165:1486–1491.
- Gehi A, Mangano D, Pipkin S, Browner WS, Whooley MA. Depression and heart rate variability in patients with stable coronary heart disease: findings from the Heart and Soul Study. Arch Gen Psychiatry 2005; 62:661–666.
- de Jonge P, Mangano D, Whooley MA. Differential association of cognitive and somatic depressive symptoms with heart rate variability in patients with stable coronary heart disease: findings from the Heart and Soul Study. Psychosom Med 2007; 69:735–739.
- Musselman DL, Tomer A, Manatunga AK, et al. Exaggerated platelet reactivity in major depression. Am J Psychiatry 1996; 153:1313–1317.
- Laghrissi-Thode F, Wagner WR, Pollock BG, Johnson PC, Finkel MS. Elevated platelet factor 4 and beta-thromboglobulin plasma levels in depressed patients with ischemic heart disease. Biol Psychiatry 1997; 42:290–295.
- Serebruany VL, Glassman AH, Malinin AI, et al. Platelet/endothelial biomarkers in depressed patients treated with the selective serotonin reuptake inhibitor sertraline after acute coronary events: the Sertraline AntiDepressant Heart Attack Randomized Trial (SADHART) Platelet Substudy. Circulation 2003; 108:939–944.
- Sherwood A, Hinderliter AL, Watkins LL, Waugh RA, Blumenthal JA. Impaired endothelial function in coronary heart disease patients with depressive symptomatology. J Am Coll Cardiol 2005; 46:656–659.
- Yang EH, Lerman S, Lennon RJ, Simari RD, Lerman LO, Lerman A. Relation of depression to coronary endothelial function. Am J Cardiol 2007; 99:1134–1136.
- Otte C, Neylan TC, Pipkin SS, Browner WS, Whooley MA. Depressive symptoms and 24-hour urinary norepinephrine excretion levels in patients with coronary disease: findings from the Heart and Soul Study. Am J Psychiatry 2005; 162:2139–2145.
- Wittstein IS, Thiemann DR, Lima JAC, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med 2005; 352:539–548.
- Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med 2005; 352:1685–1695.
- Miller GE, Stetler CA, Carney RM, Freedland KE, Banks WA. Clinical depression and inflammatory risk markers for coronary heart disease. Am J Cardiol 2002; 90:1279–1283.
- Empana JP, Sykes DH, Luc G, et al. Contributions of depressive mood and circulating inflammatory markers to coronary heart disease in healthy European men: the Prospective Epidemiological Study of Myocardial Infarction (PRIME). Circulation 2005; 111:2299–2305.
- Frasure-Smith N, Lespérance F, Irwin MR, Sauvé C, Lespérance J, Théroux P. Depression, C-reactive protein and two-year major adverse cardiac events in men after acute coronary syndromes. Biol Psychiatry 2007; 62:302–308.
- Whooley MA, Caska CM, Hendrickson BE, Rourke MA, Ho J, Ali S. Depression and inflammation in patients with coronary heart disease: findings from the Heart and Soul Study. Biol Psychiatry 2007; 62:314–320.
- Glassman AH, Miller GE. Where there is depression, there is inflammation…sometimes! Biol Psychiatry 2007; 62:280–281.
- Tracey KJ. Physiology and immunology of the cholinergic antiinflammatory pathway. J Clin Invest 2007; 117:289–296.
- Tracey KJ. The inflammatory reflex. Nature 2002; 420:853–859.
- McCaffery JM, Frasure-Smith N, Dubé M-P, et al. Common genetic vulnerability to depressive symptoms and coronary artery disease: a review and development of candidate genes related to inflammation and serotonin. Psychosom Med 2006; 68:187–200.
- Caspi A, Sugden K, Moffitt TE, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science 2003; 301:386–389.
- Nakatani D, Sato H, Sakata Y, et al. Influence of serotonin transporter gene polymorphism on depressive symptoms and new cardiac events after acute myocardial infarction. Am Heart J 2005; 150:652–658.
- Otte C, McCaffery J, Ali S, Whooley MA. Association of a serotonin transporter polymorphism (5-HTTLPR) with depression, perceived stress, and norepinephrine in patients with coronary disease: the Heart and Soul Study. Am J Psychiatry 2007; 164:1379–1384.
- Fumeron F, Betoulle D, Nicaud V, et al. Serotonin transporter gene polymorphism and myocardial infarction: Etude Cas-Témoins de l’Infarctus du Myocarde (ECTIM). Circulation 2002; 105:2943–2945.
- Rivelli S, Jiang W. Depression and ischemic heart disease: what have we learned from clinical trials? Curr Opin Cardiol 2007; 22:286–291.
- Frasure-Smith N, Lespérance F, Prince RH, et al. Randomised trial of home-based psychosocial nursing intervention for patients recovering from myocardial infarction. Lancet 1997; 350:473–479.
- Glassman AH, O’Connor CM, Califf RM, et al. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA 2002; 288:701–709.
- Writing Committee for the EI. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) randomized trial. JAMA 2003; 289:3106–3116.
- van Melle JP, de Jonge P, Honig A, et al. Effects of antidepressant treatment following myocardial infarction. Br J Psychiatry 2007; 190:460–466.
- Lespérance F, Frasure-Smith N, Koszycki D, et al. Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease: the Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial. JAMA 2007; 297:367–379.
- Carney RM, Blumenthal JA, Freedland KE, et al. Depression and late mortality after myocardial infarction in the Enhancing Recovery in Coronary Heart Disease (ENRICHD) Study. Psychosom Med 2004; 66:466–474.
- de Jonge P, Honig A, van Melle JP, et al. Nonresponse to treatment for depression following myocardial infarction: association with subsequent cardiac events. Am J Psychiatry 2007; 164:1371–1378.
- Carney RM, Freedland KE. Depression and coronary heart disease: more pieces of the puzzle. Am J Psychiatry 2007; 164:1307–1309.
- Glassman AH, Bigger JT, Gaffney M, Shapiro PA, Swenson JR. Onset of major depression associated with acute coronary syndromes: relationship of onset, major depressive disorder history, and episode severity to sertraline benefit. Arch Gen Psychiatry 2006; 63:283–288.
- Ziegelstein RC, Kim SY, Kao D, et al. Can doctors and nurses recognize depression in patients hospitalized with an acute myocardial infarction in the absence of formal screening? Psychosom Med 2005; 67:393–397.
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9. Validity of a brief depression severity measure. J Gen Intern Med 2001; 16:606–613.
- Löwe B, Unutzer J, Callahan CM, Perkins AJ, Kroenke K. Monitoring depression treatment outcomes with the Patient Health Questionnaire-9. Med Care 2004; 42:1194–1201.
- Parashar S, Rumsfeld JS, Spertus JA, et al. Time course of depression and outcome of myocardial infarction. Arch Intern Med 2006; 166:2035–2043.
- Amin AA, Jones AMH, Nugent K, Rumsfeld JS, Spertus JA. The prevalence of unrecognized depression in patients with acute coronary syndrome. Am Heart J 2006; 152:928–934.
- McManus D, Pipkin SS, Whooley MA. Screening for depression in patients with coronary heart disease (data from the Heart and Soul Study). Am J Cardiol 2005; 96:1076–1081.
- Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care 2003; 41:1284–1292.
- Spitzer RL, Williams JB, Kroenke K, et al. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA 1994; 272:1749–1756.
- Lespérance F, Frasure-Smith N. Depression in patients with cardiac disease. J Psychosom Res 2000; 48:379–391.
- Hunkeler EM, Katon W, Tang L, et al. Long term outcomes from the IMPACT randomised trial for depressed elderly patients in primary care. BMJ 2006; 332:259–263.
- Frasure-Smith N, Lespérance F, Gravel G, Masson A, Juneau M, Bourassa MG. Long-term survival differences among low-anxious, high-anxious and repressive copers enrolled in the Montreal Heart Attack Readjustment Trial. Psychosom Med 2002; 64:571–579.
- Glassman AH, Roose SP, Bigger JT. The safety of tricyclic antidepressants in cardiac patients: risk-benefit reconsidered. JAMA 1993; 269:2673–2675.
- Cohen HW, Gibson G, Alderman MH. Excess risk of myocardial infarction in patients treated with antidepressant medications: association with use of tricyclic agents. Am J Med 2000; 108:2–8.
- Taylor CB, Youngblood ME, Catellier D, et al. Effects of antidepressant medication on morbidity and mortality in depressed patients after myocardial infarction. Arch Gen Psychiatry 2005; 62:792–798.
- Montgomery SA. Safety of mirtazapine: a review. Int Clin Psychopharmacol 1995; 10(suppl 4):37–45.
- Sauer WH, Berlin JA, Kimmel SE. Selective serotonin reuptake inhibitors and myocardial infarction. Circulation 2001; 104:1894–1898.
- Sauer WH, Berlin JA, Kimmel SE. Effect of antidepressants and their relative affinity for the serotonin transporter on the risk of myocardial infarction. Circulation 2003; 108:32–36.
- Ziegelstein RC, Meuchel J, Kim TJ, et al. Selective serotonin reuptake inhibitor use by patients with acute coronary syndromes. Am J Med 2007; 120:525–530.
- Xiong GL, Jiang W, Clare R, et al. Prognosis of patients taking selective serotonin reuptake inhibitors before coronary artery bypass grafting. Am J Cardiol 2006; 98:42–47.
- Yang C-C, Jick SS, Jick H. Lipid-lowering drugs and the risk of depression and suicidal behavior. Arch Intern Med 2003; 163:1926–1932.
- Callreus T, Agerskov Andersen U, Hallas J, Andersen M. Cardiovascular drugs and the risk of suicide: a nested case-control study. Eur J Clin Pharmacol 2007; 63:591–596.
- Young-Xu Y, Chan KA, Liao JK, Ravid S, Blatt CM. Long-term statin use and psychological well-being. J Am Coll Cardiol 2003; 42:690–697.
- Ko DT, Hebert PR, Coffey CS, Sedrakyan A, Curtis JP, Krumholz HM. Beta-blocker therapy and symptoms of depression, fatigue, and sexual dysfunction. JAMA 2002; 288:351–357.
- van Melle JP, Verbeek D, van den Berg MP, Ormel J, van der Line MR, de Jonge P. Beta-blockers and depression after myocardial infarction. J Am Coll Cardiol 2006; 48:2209–2214.
- Thomas RJ, King M, Lui K, et al. AACVPR/ACC/AHA 2007 performance measures on cardiac rehabilitation for referral to and delivery of cardiac rehabilitation/secondary prevention services. J Am Coll Cardiol 2007; 50:1400–1433.
- Blumenthal JA, Babyak MA, Doraiswamy PM, et al. Exercise and pharmacotherapy in the treatment of major depressive disorder. Psychosom Med 2007; 69:587–596.
- Linden W, Phillips MJ, Leclerc J. Psychological treatment of cardiac patients: a meta-analysis. Eur Heart J 2007; 28:2972–2984.
- Centers for Disease Control and Prevention. Receipt of outpatient cardiac rehabilitation among heart attack survivors—United States, 2005. JAMA 2008; 299:1534–1536.
- Williams RB. Treating depression after myocardial infarction: can selecting patients on the basis of genetic susceptibility improve psychiatric and medical outcomes? Am Heart J 2005; 150:617–619.
- Schneiderman N, Williams RB. The great debate editorial, revisited. Psychosom Med 2006; 68:636–638.
- de Jonge P, Ormel J, van den Brink RHS, et al. Symptom dimensions of depression following myocardial infarction and their relationship with somatic health status and cardiovascular prognosis. Am J Psychiatry 2006; 163:138–144.
- Fraguas R, Iosifescu DV, Alpert J, et al. Major depressive disorder and comorbid cardiac disease: is there a depressive subtype with greater cardiovascular morbidity? Results from the STAR*D Study. Psychosomatics 2007; 48:418–425.
- Kubzansky LD, Thurston RC. Emotional vitality and incident coronary heart disease: benefits of healthy psychological functioning. Arch Gen Psychiatry 2007; 64:1393–1401.
- Frasure-Smith N. Reflections on depression as a cardiac risk factor Academy of Psychosomatic Medicine, 53rd Annual Meeting, Tucson, Arizona, 2006.
- Frasure-Smith N, Lespérance F. Major depression is associated with lower omega-3 fatty acid levels in patients with recent acute coronary syndromes. Biol Psychiatry 2004; 55:891–896.
- Lespérance F. Annual Research Award Lecture Academy of Psychosomatic Medicine, Amelia Island, Florida, 2007.
- Graham I, Atar D, Borch-Johnsen K, et al. European guidelines on cardiovascular disease prevention in clinical practice: executive summary. Eur Heart J 2007; 28:2375–2414.
- Davidson KW, Kupfer DJ, Bigger JT, et al. Assessment and treatment of depression in patients with cardiovascular disease: National Heart, Lung, and Blood Institute Working Group Report. Psychosom Med 2006; 68:645–650.
- Lichtman JH, Bigger JT, Blumenthal JA, et al. Depression and coronary heart disease. Recommendations for screening, referral, and treatment. Circulation 2008; 118:1768–1775.
- Jiang W, Glassman A, Krishnan R, O’Connor CM, Califf RM. Depression and ischemic heart disease: what have we learned so far and what must we do in the future? Am Heart J 2005; 150:54–78.
- Freedland KE, Rich MW, Skala JA, Carney RM, Davila-Roman VG, Jaffe AS. Prevalence of depression in hospitalized patients with congestive heart failure. Psychosom Med 2003; 65:119–128.
- Murray CJ, Lopez AD, Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet 1997; 349:1436–1442.
- Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet 2007; 370:851–858.
- Osborn DP, Levy G, Nazareth I, Petersen I, Islam A, King MB. Relative risk of cardiovascular and cancer mortality in people with severe mental illness from the United Kingdom’s general practice research database. Arch Gen Psychiatry 2007; 64:242–249.
- Friedman M, Thoresen CE, Gill JJ, et al. Alteration of type A behavior and its effect on cardiac recurrences in post myocardial infarction patients: summary results of the recurrent coronary prevention project. Am Heart J 1986; 112:653–665.
- Ragland DR, Brand RJ. Type A behavior and mortality from coronary heart disease. N Engl J Med 1988; 318:65–69.
- Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation 1999; 99:2192–2217.
- Iribarren C, Sidney S, Bild DE, et al. Association of hostility with coronary artery calcification in young adults: the CARDIA study. Coronary Artery Risk Development in Young Adults. JAMA 2000; 283:2546–2551.
- Williams RB, Barefoot JC, Schneiderman N. Psychosocial risk factors for cardiovascular disease: more than one culprit at work. JAMA 2003; 290:2190–2192.
- Rozanski A, Blumenthal JA, Davidson KW, Saab PG, Kubzansky L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: the emerging field of behavioral cardiology. J Am Coll Cardiol 2005; 45:637–651.
- Hemingway H, Marmot M. Evidence based cardiology: psychosocial factors in the aetiology and prognosis of coronary heart disease: systematic review of prospective cohort studies. BMJ 1999; 318:1460–1467.
- Denollet J. DS14: Standard assessment of negative affectivity, social inhibition, and type D personality. Psychosom Med 2005; 67:89–97.
- Steptoe A, Molloy GJ. Personality and heart disease. Heart 2007; 93:783–784.
- Yusuf S, Hawken S, Ôunpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004; 364:937–952.
- Rosengren A, Hawken S, Ounpuu S, et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case-control study. Lancet 2004; 364:953–962.
- Kuper H, Marmot M. Job strain, job demands, decision latitude, and risk of coronary heart disease within the Whitehall II study. J Epidemiol Community Health 2003; 57:147–153.
- Aboa-Eboule C, Brisson C, Maunsell E, et al. Job strain and risk of acute recurrent coronary heart disease events. JAMA 2007; 298:1652–1660.
- Frasure-Smith N, Lespérance F. Depression and anxiety as predictors of 2-year cardiac events in patients with stable coronary artery disease. Arch Gen Psychiatry 2008; 65:62–71.
- Shen B-J, Avivi YE, Todaro JF, et al. Anxiety characteristics independently and prospectively predict myocardial infarction in men. J Am Coll Cardiol 2008; 51:113–119.
- Carney RM, Freedland KE. Depression, mortality, and medical morbidity in patients with coronary heart disease. Biol Psychiatry 2003; 54:241–247.
- Pratt LA, Ford DE, Crum RM, Armenian HK, Gallo JJ, Eaton WW. Depression, psychotropic medication, and risk of myocardial infarction: prospective data from the Baltimore ECA follow-up. Circulation 1996; 94:3123–3129.
- Rugulies R. Depression as a predictor for coronary heart disease. A review and meta-analysis. Am J Prev Med 2002; 23:51–61.
- Van der Kooy K, van Hout H, Marwijk H, Marten H, Stehouwer C, Beekman A. Depression and the risk for cardiovascular diseases: systematic review and meta analysis. Int J Geriatr Psychiatry 2007; 22:613–626.
- Wulsin LR, Singal BM. Do depressive symptoms increase the risk for the onset of coronary disease? A systematic quantitative review. Psychosom Med 2003; 65:201–210.
- Wulsin LR. Is depression a major risk factor for coronary disease? A systematic review of the epidemiologic evidence. Harv Rev Psychiatry 2004; 12:79–93.
- Janszky I, Ahlbom A, Hallqvist J, Ahnve S. Hospitalization for depression is associated with an increased risk for myocardial infarction not explained by lifestyle, lipids, coagulation, and inflammation: The SHEEP Study. Biol Psychiatry 2007; 62:25–32.
- Surtees PG, Wainwright NWJ, Luben RN, Wareham NJ, Bingham SA, Khaw K-T. Depression and ischemic heart disease mortality: evidence from the EPIC-Norfolk United Kingdom Prospective Cohort Study. Am J Psychiatry 2008; 165:515–523.
- Carney RM, Rich MW, Freedland KE, et al. Major depressive disorder predicts cardiac events in patients with coronary artery disease. Psychosom Med 1988; 50:627–633.
- Frasure-Smith N, Lespérance F, Talajic M. Depression following myocardial infarction. Impact on 6-month survival. JAMA 1993; 270:1819–1825.
- Frasure-Smith N, Lespérance F, Talajic M. Depression and 18-month prognosis after myocardial infarction. Circulation 1995; 91:999–1005.
- Barefoot JC, Helms MJ, Mark DB, et al. Depression and long-term mortality risk in patients with coronary artery disease. Am J Cardiol 1996; 78:613–617.
- Lespérance F, Frasure-Smith N, Talajic M, Bourassa MG. Five-year risk of cardiac mortality in relation to initial severity and one-year changes in depression symptoms after myocardial infarction. Circulation 2002; 105:1049–1053.
- Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med 2004; 66:802–813.
- van Melle JP, de Jonge P, Spijkerman TA, et al. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis. Psychosom Med 2004; 66:814–822.
- Blumenthal JA, Lett HS, Babyak MA, et al. Depression as a risk factor for mortality after coronary artery bypass surgery. Lancet 2003; 362:604–609.
- Sullivan MD, LaCroix AZ, Spertus JA, Hecht J, Russo J. Depression predicts revascularization procedures for 5 years after coronary angiography. Psychosom Med 2003; 65:229–236.
- Jiang W, Alexander J, Christopher E, et al. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med 2001; 161:1849–1856.
- Zipfel S, Schneider A, Wild B, et al. Effect of depressive symptoms on survival after heart transplantation. Psychosom Med 2002; 64:740–747.
- Polsky D, Doshi JA, Marcus S, et al. Long-term risk for depressive symptoms after a medical diagnosis. Arch Intern Med 2005; 165:1260–1266.
- Katon W, Lin EHB, Kroenke K. The association of depression and anxiety with medical symptom burden in patients with chronic medical illness. Gen Hosp Psychiatry 2007; 29:147–155.
- Ruo B, Rumsfeld JS, Hlatky MA, Liu H, Browner WS, Whooley MA. Depressive symptoms and health-related quality of life: the Heart and Soul Study. JAMA 2003; 290:215–221.
- Rasmussen JN, Chong A, Alter DA. Relationship between adherence to evidence-based pharmacotherapy and long-term mortality after acute myocardial infarction. JAMA 2007; 297:177–186.
- Gehi AK, Ali S, Na B, Whooley MA. Self-reported medication adherence and cardiovascular events in patients with stable coronary heart disease: the Heart and Soul Study. Arch Intern Med 2007; 167:1798–1803.
- Gehi A, Haas D, Pipkin S, Whooley MA. Depression and medication adherence in outpatients with coronary heart disease: findings from the Heart and Soul Study. Arch Intern Med 2005; 165:2508–2513.
- Rieckmann N, Gerin W, Kronish IM, et al. Course of depressive symptoms and medication adherence after acute coronary syndromes: an electronic medication monitoring study. J Am Coll Cardiol 2006; 48:2218–2222.
- Ziegelstein RC, Fauerbach JA, Stevens SS, Romanelli J, Richter DP, Bush DE. Patients with depression are less likely to follow recommendations to reduce cardiac risk during recovery from a myocardial infarction. Arch Intern Med 2000; 160:1818–1823.
- Kronish IM, Rieckmann N, Halm EA, et al. Persistent depression affects adherence to secondary prevention behaviors after acute coronary syndromes. J Gen Intern Med 2006; 21:1178–1183.
- Joynt KE, Whellan DJ, O’Connor CM. Depression and cardiovascular disease: mechanisms of interaction. Biol Psychiatry 2003; 54:248–261.
- Musselman DL, Evans DL, Nemeroff CB. The relationship of depression to cardiovascular disease: epidemiology, biology, and treatment. Arch Gen Psychiatry 1998; 55:580–592.
- Lespérance F, Frasure-Smith N. Depression and heart disease. Cleve Clin J Med 2007; 74(suppl 1):S63–S66.
- Curtis BM. Autonomic tone as a cardiovascular risk factor: the dangers of chronic fight or flight. Mayo Clin Proc 2002; 77:45–54.
- Topol EJ. Textbook of Cardiovascular Medicine, 2nd ed. Philadelphia: Lippincott Williams & Williams 2002.
- Carney RM, Saunders RD, Freedland KE, Stein P, Rich MW, Jaffe AS. Association of depression with reduced heart rate variability in coronary artery disease. Am J Cardiol 1995; 76:562–564.
- Carney RM, Blumenthal JA, Stein PK, et al. Depression, heart rate variability, and acute myocardial infarction. Circulation 2001; 104:2024–2028.
- Carney RM, Blumenthal JA, Freedland KE, et al. Low heart rate variability and the effect of depression on post-myocardial infarction mortality. Arch Intern Med 2005; 165:1486–1491.
- Gehi A, Mangano D, Pipkin S, Browner WS, Whooley MA. Depression and heart rate variability in patients with stable coronary heart disease: findings from the Heart and Soul Study. Arch Gen Psychiatry 2005; 62:661–666.
- de Jonge P, Mangano D, Whooley MA. Differential association of cognitive and somatic depressive symptoms with heart rate variability in patients with stable coronary heart disease: findings from the Heart and Soul Study. Psychosom Med 2007; 69:735–739.
- Musselman DL, Tomer A, Manatunga AK, et al. Exaggerated platelet reactivity in major depression. Am J Psychiatry 1996; 153:1313–1317.
- Laghrissi-Thode F, Wagner WR, Pollock BG, Johnson PC, Finkel MS. Elevated platelet factor 4 and beta-thromboglobulin plasma levels in depressed patients with ischemic heart disease. Biol Psychiatry 1997; 42:290–295.
- Serebruany VL, Glassman AH, Malinin AI, et al. Platelet/endothelial biomarkers in depressed patients treated with the selective serotonin reuptake inhibitor sertraline after acute coronary events: the Sertraline AntiDepressant Heart Attack Randomized Trial (SADHART) Platelet Substudy. Circulation 2003; 108:939–944.
- Sherwood A, Hinderliter AL, Watkins LL, Waugh RA, Blumenthal JA. Impaired endothelial function in coronary heart disease patients with depressive symptomatology. J Am Coll Cardiol 2005; 46:656–659.
- Yang EH, Lerman S, Lennon RJ, Simari RD, Lerman LO, Lerman A. Relation of depression to coronary endothelial function. Am J Cardiol 2007; 99:1134–1136.
- Otte C, Neylan TC, Pipkin SS, Browner WS, Whooley MA. Depressive symptoms and 24-hour urinary norepinephrine excretion levels in patients with coronary disease: findings from the Heart and Soul Study. Am J Psychiatry 2005; 162:2139–2145.
- Wittstein IS, Thiemann DR, Lima JAC, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med 2005; 352:539–548.
- Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med 2005; 352:1685–1695.
- Miller GE, Stetler CA, Carney RM, Freedland KE, Banks WA. Clinical depression and inflammatory risk markers for coronary heart disease. Am J Cardiol 2002; 90:1279–1283.
- Empana JP, Sykes DH, Luc G, et al. Contributions of depressive mood and circulating inflammatory markers to coronary heart disease in healthy European men: the Prospective Epidemiological Study of Myocardial Infarction (PRIME). Circulation 2005; 111:2299–2305.
- Frasure-Smith N, Lespérance F, Irwin MR, Sauvé C, Lespérance J, Théroux P. Depression, C-reactive protein and two-year major adverse cardiac events in men after acute coronary syndromes. Biol Psychiatry 2007; 62:302–308.
- Whooley MA, Caska CM, Hendrickson BE, Rourke MA, Ho J, Ali S. Depression and inflammation in patients with coronary heart disease: findings from the Heart and Soul Study. Biol Psychiatry 2007; 62:314–320.
- Glassman AH, Miller GE. Where there is depression, there is inflammation…sometimes! Biol Psychiatry 2007; 62:280–281.
- Tracey KJ. Physiology and immunology of the cholinergic antiinflammatory pathway. J Clin Invest 2007; 117:289–296.
- Tracey KJ. The inflammatory reflex. Nature 2002; 420:853–859.
- McCaffery JM, Frasure-Smith N, Dubé M-P, et al. Common genetic vulnerability to depressive symptoms and coronary artery disease: a review and development of candidate genes related to inflammation and serotonin. Psychosom Med 2006; 68:187–200.
- Caspi A, Sugden K, Moffitt TE, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science 2003; 301:386–389.
- Nakatani D, Sato H, Sakata Y, et al. Influence of serotonin transporter gene polymorphism on depressive symptoms and new cardiac events after acute myocardial infarction. Am Heart J 2005; 150:652–658.
- Otte C, McCaffery J, Ali S, Whooley MA. Association of a serotonin transporter polymorphism (5-HTTLPR) with depression, perceived stress, and norepinephrine in patients with coronary disease: the Heart and Soul Study. Am J Psychiatry 2007; 164:1379–1384.
- Fumeron F, Betoulle D, Nicaud V, et al. Serotonin transporter gene polymorphism and myocardial infarction: Etude Cas-Témoins de l’Infarctus du Myocarde (ECTIM). Circulation 2002; 105:2943–2945.
- Rivelli S, Jiang W. Depression and ischemic heart disease: what have we learned from clinical trials? Curr Opin Cardiol 2007; 22:286–291.
- Frasure-Smith N, Lespérance F, Prince RH, et al. Randomised trial of home-based psychosocial nursing intervention for patients recovering from myocardial infarction. Lancet 1997; 350:473–479.
- Glassman AH, O’Connor CM, Califf RM, et al. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA 2002; 288:701–709.
- Writing Committee for the EI. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) randomized trial. JAMA 2003; 289:3106–3116.
- van Melle JP, de Jonge P, Honig A, et al. Effects of antidepressant treatment following myocardial infarction. Br J Psychiatry 2007; 190:460–466.
- Lespérance F, Frasure-Smith N, Koszycki D, et al. Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease: the Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial. JAMA 2007; 297:367–379.
- Carney RM, Blumenthal JA, Freedland KE, et al. Depression and late mortality after myocardial infarction in the Enhancing Recovery in Coronary Heart Disease (ENRICHD) Study. Psychosom Med 2004; 66:466–474.
- de Jonge P, Honig A, van Melle JP, et al. Nonresponse to treatment for depression following myocardial infarction: association with subsequent cardiac events. Am J Psychiatry 2007; 164:1371–1378.
- Carney RM, Freedland KE. Depression and coronary heart disease: more pieces of the puzzle. Am J Psychiatry 2007; 164:1307–1309.
- Glassman AH, Bigger JT, Gaffney M, Shapiro PA, Swenson JR. Onset of major depression associated with acute coronary syndromes: relationship of onset, major depressive disorder history, and episode severity to sertraline benefit. Arch Gen Psychiatry 2006; 63:283–288.
- Ziegelstein RC, Kim SY, Kao D, et al. Can doctors and nurses recognize depression in patients hospitalized with an acute myocardial infarction in the absence of formal screening? Psychosom Med 2005; 67:393–397.
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9. Validity of a brief depression severity measure. J Gen Intern Med 2001; 16:606–613.
- Löwe B, Unutzer J, Callahan CM, Perkins AJ, Kroenke K. Monitoring depression treatment outcomes with the Patient Health Questionnaire-9. Med Care 2004; 42:1194–1201.
- Parashar S, Rumsfeld JS, Spertus JA, et al. Time course of depression and outcome of myocardial infarction. Arch Intern Med 2006; 166:2035–2043.
- Amin AA, Jones AMH, Nugent K, Rumsfeld JS, Spertus JA. The prevalence of unrecognized depression in patients with acute coronary syndrome. Am Heart J 2006; 152:928–934.
- McManus D, Pipkin SS, Whooley MA. Screening for depression in patients with coronary heart disease (data from the Heart and Soul Study). Am J Cardiol 2005; 96:1076–1081.
- Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care 2003; 41:1284–1292.
- Spitzer RL, Williams JB, Kroenke K, et al. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA 1994; 272:1749–1756.
- Lespérance F, Frasure-Smith N. Depression in patients with cardiac disease. J Psychosom Res 2000; 48:379–391.
- Hunkeler EM, Katon W, Tang L, et al. Long term outcomes from the IMPACT randomised trial for depressed elderly patients in primary care. BMJ 2006; 332:259–263.
- Frasure-Smith N, Lespérance F, Gravel G, Masson A, Juneau M, Bourassa MG. Long-term survival differences among low-anxious, high-anxious and repressive copers enrolled in the Montreal Heart Attack Readjustment Trial. Psychosom Med 2002; 64:571–579.
- Glassman AH, Roose SP, Bigger JT. The safety of tricyclic antidepressants in cardiac patients: risk-benefit reconsidered. JAMA 1993; 269:2673–2675.
- Cohen HW, Gibson G, Alderman MH. Excess risk of myocardial infarction in patients treated with antidepressant medications: association with use of tricyclic agents. Am J Med 2000; 108:2–8.
- Taylor CB, Youngblood ME, Catellier D, et al. Effects of antidepressant medication on morbidity and mortality in depressed patients after myocardial infarction. Arch Gen Psychiatry 2005; 62:792–798.
- Montgomery SA. Safety of mirtazapine: a review. Int Clin Psychopharmacol 1995; 10(suppl 4):37–45.
- Sauer WH, Berlin JA, Kimmel SE. Selective serotonin reuptake inhibitors and myocardial infarction. Circulation 2001; 104:1894–1898.
- Sauer WH, Berlin JA, Kimmel SE. Effect of antidepressants and their relative affinity for the serotonin transporter on the risk of myocardial infarction. Circulation 2003; 108:32–36.
- Ziegelstein RC, Meuchel J, Kim TJ, et al. Selective serotonin reuptake inhibitor use by patients with acute coronary syndromes. Am J Med 2007; 120:525–530.
- Xiong GL, Jiang W, Clare R, et al. Prognosis of patients taking selective serotonin reuptake inhibitors before coronary artery bypass grafting. Am J Cardiol 2006; 98:42–47.
- Yang C-C, Jick SS, Jick H. Lipid-lowering drugs and the risk of depression and suicidal behavior. Arch Intern Med 2003; 163:1926–1932.
- Callreus T, Agerskov Andersen U, Hallas J, Andersen M. Cardiovascular drugs and the risk of suicide: a nested case-control study. Eur J Clin Pharmacol 2007; 63:591–596.
- Young-Xu Y, Chan KA, Liao JK, Ravid S, Blatt CM. Long-term statin use and psychological well-being. J Am Coll Cardiol 2003; 42:690–697.
- Ko DT, Hebert PR, Coffey CS, Sedrakyan A, Curtis JP, Krumholz HM. Beta-blocker therapy and symptoms of depression, fatigue, and sexual dysfunction. JAMA 2002; 288:351–357.
- van Melle JP, Verbeek D, van den Berg MP, Ormel J, van der Line MR, de Jonge P. Beta-blockers and depression after myocardial infarction. J Am Coll Cardiol 2006; 48:2209–2214.
- Thomas RJ, King M, Lui K, et al. AACVPR/ACC/AHA 2007 performance measures on cardiac rehabilitation for referral to and delivery of cardiac rehabilitation/secondary prevention services. J Am Coll Cardiol 2007; 50:1400–1433.
- Blumenthal JA, Babyak MA, Doraiswamy PM, et al. Exercise and pharmacotherapy in the treatment of major depressive disorder. Psychosom Med 2007; 69:587–596.
- Linden W, Phillips MJ, Leclerc J. Psychological treatment of cardiac patients: a meta-analysis. Eur Heart J 2007; 28:2972–2984.
- Centers for Disease Control and Prevention. Receipt of outpatient cardiac rehabilitation among heart attack survivors—United States, 2005. JAMA 2008; 299:1534–1536.
- Williams RB. Treating depression after myocardial infarction: can selecting patients on the basis of genetic susceptibility improve psychiatric and medical outcomes? Am Heart J 2005; 150:617–619.
- Schneiderman N, Williams RB. The great debate editorial, revisited. Psychosom Med 2006; 68:636–638.
- de Jonge P, Ormel J, van den Brink RHS, et al. Symptom dimensions of depression following myocardial infarction and their relationship with somatic health status and cardiovascular prognosis. Am J Psychiatry 2006; 163:138–144.
- Fraguas R, Iosifescu DV, Alpert J, et al. Major depressive disorder and comorbid cardiac disease: is there a depressive subtype with greater cardiovascular morbidity? Results from the STAR*D Study. Psychosomatics 2007; 48:418–425.
- Kubzansky LD, Thurston RC. Emotional vitality and incident coronary heart disease: benefits of healthy psychological functioning. Arch Gen Psychiatry 2007; 64:1393–1401.
- Frasure-Smith N. Reflections on depression as a cardiac risk factor Academy of Psychosomatic Medicine, 53rd Annual Meeting, Tucson, Arizona, 2006.
- Frasure-Smith N, Lespérance F. Major depression is associated with lower omega-3 fatty acid levels in patients with recent acute coronary syndromes. Biol Psychiatry 2004; 55:891–896.
- Lespérance F. Annual Research Award Lecture Academy of Psychosomatic Medicine, Amelia Island, Florida, 2007.
- Graham I, Atar D, Borch-Johnsen K, et al. European guidelines on cardiovascular disease prevention in clinical practice: executive summary. Eur Heart J 2007; 28:2375–2414.
- Davidson KW, Kupfer DJ, Bigger JT, et al. Assessment and treatment of depression in patients with cardiovascular disease: National Heart, Lung, and Blood Institute Working Group Report. Psychosom Med 2006; 68:645–650.
KEY POINTS
- Depression is a risk factor for new cardiac disease and has a detrimental impact in established cardiac disease.
- Numerous mechanistic pathways have been implicated.
- In clinical trials, drug therapy and psychotherapy have not clearly decreased the rate of cardiac death in depressed cardiac patients, but they did improve depression, adherence to drug therapy, and quality of life.
- Clinicians should routinely screen for depression in cardiac patients and should not hesitate to treat it.
- Eligible patients should routinely be referred to cardiac rehabilitation programs.