User login
Outcomes after 2011 Residency Reform
The Accreditation Council for Graduate Medical Education (ACGME) Common Program Requirements implemented in July 2011 increased supervision requirements and limited continuous work hours for first‐year residents.[1] Similar to the 2003 mandates, these requirements were introduced to improve patient safety and education at academic medical centers.[2] Work‐hour reforms have been associated with decreased resident burnout and improved sleep.[3, 4, 5] However, national observational studies and systematic reviews of the impact of the 2003 reforms on patient safety and quality of care have been varied in terms of outcome.[6, 7, 8, 9, 10] Small studies of the 2011 recommendations have shown increased sleep duration and decreased burnout, but also an increased number of handoffs and increased resident concerns about making a serious medical error.[11, 12, 13, 14] Although national surveys of residents and program directors have not indicated improvements in education or quality of life, 1 observational study did show improvement in clinical exposure and conference attendance.[15, 16, 17, 18] The impact of the 2011 reforms on patient safety remains unclear.[19, 20]
The objective of this study was to evaluate the association between implementation of the 2011 residency work‐hour mandates and patient safety outcomes at a large academic medical center.
METHODS
Study Design
This observational study used a quasi‐experimental difference‐in‐differences approach to evaluate whether residency work‐hour changes were associated with patient safety outcomes among general medicine inpatients. We compared safety outcomes among adult patients discharged from resident general medical services (referred to as resident) to safety outcomes among patients discharged by the hospitalist general medical service (referred to as hospitalist) before and after the 2011 residency work‐hour reforms at a large academic medical center. Differences in outcomes for the resident group were compared to differences observed in the hospitalist group, with adjustment for relevant demographic and case mix factors.[21] We used the hospitalist service as a control group, because ACGME changes applied only to resident services. The strength of this design is that it controls for secular trends that are correlated with patient safety, impacting both residents and hospitalists similarly.[9]
Approval for this study and a Health Insurance Portability and Accountability Act waiver were granted by the Johns Hopkins University School of Medicine institutional review board. We retrospectively examined administrative data on all patient discharges from the general medicine services at Johns Hopkins Hospital between July 1, 2008 and June 30, 2012 that were identified as pertaining to resident or hospitalist services.
Patient Allocation and Physician Scheduling
Patient admission to the resident or hospitalist service was decided by a number of factors. To maintain continuity of care, patients were preferentially admitted to the same service as for prior admissions. New patients were admitted to a service based on bed availability, nurse staffing, patient gender, isolation precautions, and cardiac monitor availability.
The inpatient resident services were staffed prior to July 2011 using a traditional 30‐hour overnight call system. Following July 2011, the inpatient resident services were staffed using a modified overnight call system, in which interns took overnight calls from 8 pm until 12 pm the following day, once every 5 nights with supervision by upper‐level residents. These interns rotated through daytime admitting and coverage roles on the intervening days. The hospitalist service was organized into a 3‐physician rotation of day shift, evening shift, and overnight shift.
Data and Outcomes
Twenty‐nine percent of patients in the sample were admitted more than once during the study period, and patients were generally admitted to the same resident team during each admission. Patients with multiple admissions were counted multiple times in the model. We categorized admissions as prereform (July 1, 2008June 30, 2011) and postreform (July 1, 2011June 30, 2012). Outcomes evaluated included hospital length of stay, 30‐day readmission, intensive care unit stay (ICU) stay, inpatient mortality, and number of Maryland Hospital Acquired Conditions (MHACs). ICU stay pertained to any ICU admission including initial admission and transfer from the inpatient floor. MHACs are a set of inpatient performance indicators derived from a list of 64 inpatient Potentially Preventable Complications developed by 3M Health Information Systems.[22] MHACs are used by the Maryland Health Services Cost Review Commission to link hospital payment to performance for costly, preventable, and clinically relevant complications. MHACs were coded in our analysis as a dichotomous variable. Independent variables included patient age at admission, race, gender, and case mix index. Case mix index (CMI) is a numeric score that measures resource utilization for a specific patient population. CMI is a weighted value assigned to patients based on resource utilization and All Patient Refined Diagnostic Related Group and was included as an indicator of patient illness severity and risk of mortality.[23] Data were obtained from administrative records from the case mix research team at Johns Hopkins Medicine.
To account for transitional differences that may have coincided with the opening of a new hospital wing in late April 2012, we conducted a sensitivity analysis, in which we excluded from analysis any visits that took place in May 2012 to June 2012.
Data Analysis
Based on historical studies, we calculated that a sample size of at least 3600 discharges would allow us to detect a difference of 5% between the pre‐ and postreform period assuming baseline 20% occurrence of dichotomous outcomes (=0.05; =0.2; r=4).[21]
The primary unit of analysis was the hospital discharge. Similar to Horwitz et al., we analyzed data using a difference‐in‐differences estimation strategy.[21] We used multivariable linear regression for length of stay measured as a continuous variable, and multivariable logistic regression for inpatient mortality, 30‐day readmission, MHACs coded as a dichotomous variable, and ICU stay coded as a dichotomous variable.[9] The difference‐in‐differences estimation was used to determine whether the postreform period relative to prereform period was associated with differences in outcomes comparing resident and hospitalist services. In the regression models, the independent variables of interest included an indicator variable for whether a patient was treated on a resident service, an indicator variable for whether a patient was discharged in the postreform period, and the interaction of these 2 variables (resident*postreform). The interaction term can be interpreted as a differential change over time comparing resident and hospitalist services. In all models, we adjusted for patient age, gender, race, and case mix index.
To determine whether prereform trends were similar among the resident and hospitalist services, we performed a test of controls as described by Volpp and colleagues.[6] Interaction terms for resident service and prereform years 2010 and 2011 were added to the model. A Wald test was then used to test for improved model fit, which would indicate differential trends among resident and hospitalist services during the prereform period. Where such trends were found, postreform results were compared only to 2011 rather than the 2009 to 2011 prereform period.[6]
To account for correlation within patients who had multiple discharges, we used a clustering approach and estimated robust variances.[24] From the regression model results, we calculated predicted probabilities adjusted for relevant covariates and prepost differences, and used linear probability models to estimate percentage‐point differences in outcomes, comparing residents and hospitalists in the pre‐ and postreform periods.[25] All analyses were performed using Stata/IC version 11 (StataCorp, College Station, TX).
RESULTS
In the 3 years before the 2011 residency work‐hour reforms were implemented (prereform), there were a total of 15,688 discharges for 8983 patients to the resident services and 4622 discharges for 3649 patients to the hospitalist services. In the year following implementation of residency work‐hour changes (postreform), there were 5253 discharges for 3805 patients to the resident services and 1767 discharges for 1454 patients to the hospitalist service. Table 1 shows the characteristics of patients discharged from the resident and hospitalist services in the pre‐ and postreform periods. Patients discharged from the resident services were more likely to be older, male, African American, and have a higher CMI.
| Resident Services | Hospitalist Service | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 2009 | 2010 | 2011 | 2012 | 2009 | 2010 | 2011 | 2012 | P Valuea | |
| |||||||||
| Discharges, n | 5345 | 5299 | 5044 | 5253 | 1366 | 1492 | 1764 | 1767 | |
| Unique patients, n | 3082 | 2968 | 2933 | 3805 | 1106 | 1180 | 1363 | 1454 | |
| Age, y, mean (SD) | 55.1 (17.7) | 55.7 (17.4) | 56.4 (17.9) | 56.7 (17.1) | 55.9 (17.9) | 56.2 (18.4) | 55.5 (18.8) | 54 (18.7) | 0.02 |
| Sex male, n (%) | 1503 (48.8) | 1397 (47.1) | 1432 (48.8) | 1837 (48.3) | 520 (47) | 550 (46.6) | 613 (45) | 654 (45) | <0.01 |
| Race | |||||||||
| African American, n (%) | 2072 (67.2) | 1922 (64.8) | 1820 (62.1) | 2507 (65.9) | 500 (45.2) | 592 (50.2) | 652 (47.8) | 747 (51.4) | <0.01 |
| White, n (%) | 897 (29.1) | 892 (30.1) | 957 (32.6) | 1118 (29.4) | 534 (48.3) | 527 (44.7) | 621 (45.6) | 619 (42.6) | |
| Asian, n (%) | 19 (.6%) | 35 (1.2) | 28 (1) | 32 (.8) | 11 (1) | 7 (.6) | 25 (1.8) | 12 (.8) | |
| Other, n (%) | 94 (3.1) | 119 (4) | 128 (4.4) | 148 (3.9) | 61 (5.5) | 54 (4.6) | 65 (4.8) | 76 (5.2) | |
| Case mix index, mean (SD) | 1.2 (1) | 1.1 (0.9) | 1.1 (0.9) | 1.1 (1.2) | 1.2 (1) | 1.1 (1) | 1.1 (1) | 1 (0.7) | <0.01 |
Differences in Outcomes Among Resident and Hospitalist Services Pre‐ and Postreform
Table 2 shows unadjusted results. Patients discharged from the resident services in the postreform period as compared to the prereform period had a higher likelihood of an ICU stay (5.9% vs 4.5%, P<0.01), and lower likelihood of 30‐day readmission (17.1% vs 20.1%, P<0.01). Patients discharged from the hospitalist service in the postreform period as compared to the prereform period had a significantly shorter mean length of stay (4.51 vs 4.88 days, P=0.03)
| Resident Services | Hospitalist Service | |||||
|---|---|---|---|---|---|---|
| Outcome | Prereforma | Postreform | P Value | Prereforma | Postreform | P Value |
| ||||||
| Length of stay (mean) | 4.55 (5.39) | 4.50 (5.47) | 0.61 | 4.88 (5.36) | 4.51 (4.64) | 0.03 |
| Any ICU stay (%) | 225 (4.5%) | 310 (5.9%) | <0.01 | 82 (4.7%) | 83 (4.7%) | 0.95 |
| Any MHACs (%) | 560 (3.6%) | 180 (3.4%) | 0.62 | 210 (4.5%) | 64 (3.6%) | 0.09 |
| Readmit in 30 days (%) | 3155 (20.1%) | 900 (17.1%) | <0.01 | 852 (18.4%) | 296 (16.8%) | 0.11 |
| Inpatient mortality (%) | 71 (0.5%) | 28 (0.5%) | 0.48 | 18 (0.4%) | 7 (0.4%) | 0.97 |
Table 3 presents the results of regression analyses examining correlates of patient safety outcomes, adjusted for age, gender, race, and CMI. As the test of controls indicated differential prereform trends for ICU admission and length of stay, the prereform period was limited to 2011 for these outcomes. After adjustment for covariates, the probability of an ICU stay remained greater, and the 30‐day readmission rate was lower among patients discharged from resident services in the postreform period than the prereform period. Among patients discharged from the hospitalist services, there were no significant differences in length of stay, readmissions, ICU admissions, MHACs, or inpatient mortality comparing the pre‐ and postreform periods.
| Resident Services | Hospitalist Service | Difference in Differences | |||||
|---|---|---|---|---|---|---|---|
| Outcome | Prereforma | Postreform | Difference | Prereform | Postreform | Difference | (ResidentHospitalist) |
| |||||||
| ICU stay | 4.5% (4.0% to 5.1%) | 5.7% (5.1% to 6.3%) | 1.4% (0.5% to 2.2%) | 4.4% (3.5% to 5.3%) | 5.3% (4.3% to 6.3%) | 1.1% (0.2 to 2.4%) | 0.3% (1.1% to 1.8%) |
| Inpatient mortality | 0.5% (0.4% to 0.6%) | 0.5% (0.3% to 0.7%) | 0 (0.2% to 0.2%) | 0.3% (0.2% to 0.6%) | 0.5% (0.1% to 0.8%) | 0.1% (0.3% to 0.5%) | 0.1% (0.5% to 0.3%) |
| MHACs | 3.6% (3.3% to 3.9%) | 3.3% (2.9% to 3.7%) | 0.4% (0.9 to 0.2%) | 4.5% (3.9% to 5.1%) | 4.1% (3.2% to 5.1%) | 0.3% (1.4% to 0.7%) | 0.2% (1.0% to 1.3%) |
| Readmit 30 days | 20.1% (19.1% to 21.1%) | 17.2% (15.9% to 18.5%) | 2.8% (4.3% to 1.3%) | 18.4% (16.5% to 20.2%) | 16.6% (14.7% to 18.5%) | 1.7% (4.1% to 0.8%) | 1.8% (0.2% to 3.7%) |
| Length of stay | 4.6 (4.4 to 4.7) | 4.4 (4.3 to 4.6) | 0.1 (0.3 to 0.1) | 4.9 (4.6 to 5.1) | 4.7 (4.5 to 5.0) | 0.1 (0.4 to 0.2) | 0.01 (0.37 to 0.34) |
Differences in Outcomes Comparing Resident and Hospitalist Services Pre‐ and Postreform
Comparing pre‐ and postreform periods in the resident and hospitalist services, there were no significant differences in ICU admission, length of stay, MHACs, 30‐day readmissions, or inpatient mortality. In the sensitivity analysis, in which we excluded all discharges in May 2012 to June 2012, results were not significantly different for any of the outcomes examined.
DISCUSSION
Using difference‐in‐differences estimation, we evaluated whether the implementation of the 2011 residency work‐hour mandate was associated with differences in patient safety outcomes including length of stay, 30‐day readmission, inpatient mortality, MHACs, and ICU admissions comparing resident and hospitalist services at a large academic medical center. Adjusting for patient age, race, gender, and clinical complexity, we found no significant changes in any of the patient safety outcomes indicators in the postreform period comparing resident to hospitalist services.
Our quasiexperimental study design allowed us to gauge differences in patient safety outcomes, while reducing bias due to unmeasured confounders that might impact patient safety indicators.[9] We were able to examine all discharges from the resident and hospitalist general medicine services during the academic years 2009 to 2012, while adjusting for age, race, gender, and clinical complexity. Though ICU admission was higher and readmission rates were lower on the resident services post‐2011, we did not observe a significant difference in ICU admission or 30‐day readmission rates in the postreform period comparing patients discharged from the resident and hospitalist services and all patients in the prereform period.
Our neutral findings differ from some other single‐institution evaluations of reduced resident work hours, several of which have shown improved quality of life, education, and patient safety indicators.[18, 21, 26, 27, 28] It is unclear why improvements in patient safety were not identified in the current study. The 2011 reforms were more broad‐based than some of the preliminary studies of reduced work hours, and therefore additional variables may be at play. For instance, challenges related to decreased work hours, including the increased number of handoffs in care and work compression, may require specific interventions to produce sustained improvements in patient safety.[3, 14, 29, 30]
Improving patient safety requires more than changing resident work hours. Blum et al. recommended enhanced funding to increase supervision, decrease resident caseload, and incentivize achievement of quality indicators to achieve the goal of improved patient safety within work‐hour reform.[31] Schumacher et al. proposed a focus on supervision, professionalism, safe transitions of care, and optimizing workloads as a means to improve patient safety and education within the new residency training paradigm.[29]
Limitations of this study include limited follow‐up time after implementation of the work‐hour reforms. It may take more time to optimize systems of care to see benefits in patient safety indicators. This was a single‐institution study of a limited number of outcomes in a single department, which limits generalizability and may reflect local experience rather than broader trends. The call schedule on the resident service in this study differs from programs that have adopted night float schedules. [27] This may have had an effect on patient care outcomes.[32] In an attempt to conduct a timely study of inpatient safety indicators following the 2011 changes, our study was not powered to detect small changes in low‐frequency outcomes such as mortality; longer‐term studies at multiple institutions will be needed to answer these key questions. We limited the prereform period where our test of controls indicated differential prereform trends, which reduced power.
As this was an observational study rather than an experiment, there may have been both measured and unmeasured differences in patient characteristics and comorbidity between the intervention and control group. For example, CMI was lower on the hospitalist service than the resident services. Demographics varied somewhat between services; male and African American patients were more likely to be discharged from resident services than hospitalist services for unknown reasons. Although we adjusted for demographics and CMI in our model, there may be residual confounding. Limitations in data collection did not allow us to separate patients initially admitted to the ICU from patients transferred to the ICU from the inpatient floors. We attempted to overcome this limitation through use of a difference‐in‐differences model to account for secular trends, but factors other than residency work hours may have impacted the resident and hospitalist services differentially. For example, hospital quality‐improvement programs or provider‐level factors may have differentially impacted the resident versus hospitalist services during the study period.
Work‐hour limitations for residents were established to improve residency education and patient safety. As noted by the Institute of Medicine, improving patient safety will require significant investment by program directors, hospitals, and the public to keep resident caseloads manageable, ensure adequate supervision of first‐year residents, train residents on safe handoffs in care, and conduct ongoing evaluations of patient safety and any unintended consequences of the regulations.[33] In the first year after implementation of the 2011 work‐hour reforms, we found no change in ICU admission, inpatient mortality, 30‐day readmission rates, length of stay, or MHACs compared with patients treated by hospitalists. Studies of the long‐term impact of residency work‐hour reform are necessary to determine whether changes in work hours have been associated with improvement in resident education and patient safety.
Disclosure: Nothing to report.
- Accreditation Council for Graduate Medical Education. Common program requirements effective: July 1, 2011. Available at: http://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramResources/Common_Program_Requirements_07012011[1].pdf. Accessed February 10, 2014.
- , , . The new recommendations on duty hours from the ACGME Task Force. N Engl J Med. 2010;363:e3.
- , , , , . Interns' compliance with Accreditation Council for Graduate Medical Education work‐hour limits. JAMA. 2006;296(9):1063–1070.
- , , , , , . Effects of work hour reduction on residents' lives: a systematic review. JAMA. 2005;294(9):1088–1100.
- , , , et al. Effects of the ACGME duty hour limits on sleep, work hours, and safety. Pediatrics. 2008;122(2):250–258.
- , , . Teaching hospital five‐year mortality trends in the wake of duty hour reforms. J Gen Intern Med. 2013;28(8):1048–1055.
- , , , . Duty hour limits and patient care and resident outcomes: can high‐quality studies offer insight into complex relationships? Ann Rev Med. 2013;64:467–483.
- , , . Patient safety, resident education and resident well‐being following implementation of the 2003 ACGME duty hour rules. J Gen Intern Med. 2011;26(8):907–919.
- , , , et al. Mortality among hospitalized Medicare beneficiaries in the first 2 years following ACGME resident duty hour reform. JAMA. 2007;298(9):975–983.
- , , , et al. Effects of resident duty hour reform on surgical and procedural patient safety indicators among hospitalized Veterans Health Administration and Medicare patients. Med Care. 2009;47(7):723–731.
- , , , et al. Pilot trial of IOM duty hour recommendations in neurology residency programs. Neurology. 2011;77(9):883–887.
- , , , et al. Effect of 16‐hour duty periods of patient care and resident education. Mayo Clin Proc. 2011;86:192–196.
- , , , et al. Effects of the 2011 duty hour reforms on interns and their patients: a prospective longitudinal cohort study. JAMA Intern Med. 2013;173(8):657–662.
- , , , et al. Effect of the 2011 vs 2003 duty hour regulation—compliant models on sleep duration, trainee education, and continuity of patient care among internal medicine house staff. JAMA Intern Med. 2013;173(8):649–655.
- , , . Residents' response to duty‐hour regulations—a follow‐up national survey. N Engl J Med. 2012;366:e35.
- , , , . Surgical residents' perceptions of 2011 Accreditation Council for Graduate Medical Education duty hour regulations. JAMA Surg. 2013;148(5):427–433.
- , , . The 2011 duty hour requirements—a survey of residency program directors. N Engl J Med. 2013;368:694–697.
- , , , et al. The effect of reducing maximum shift lengths to 16 hours on internal medicine interns' educational opportunities. Acad Med. 2013;88(4):512–518.
- , . Residency work‐hours reform. A cost analysis including preventable adverse events. J Gen Intern Med. 2005;20(10):873–878.
- , , , , . Cost implications of reduced work hours and workloads for resident physicians. N Engl J Med. 2009;360:2202–2215.
- , , , . Changes in outcomes for internal medicine inpatients after work‐hour regulations. Ann Intern Med. 2007;147:97–103.
- .Maryland Health Services Cost Review Commission. Complications: Maryland Hospital Acquired Conditions. Available at: http://www.hscrc.state.md.us/init_qi_MHAC.cfm. Accessed May 23, 2013.
- , , , et al. What are APR‐DRGs? An introduction to severity of illness and risk of mortality adjustment methodology. 3M Health Information Systems. Available at: http://solutions.3m.com/3MContentRetrievalAPI/BlobServlet?locale=it_IT44(4):1049–1060.
- , , , , . Impact of the 2008 US Preventive Services Task Force Recommendation to discontinue prostate cancer screening among male Medicare beneficiaries. Arch Intern Med. 2012;172(20):1601–1603.
- , , , et al. Effect of reducing interns' work hour on serious medical errors in intensive care units. N Engl J Med. 2004;351(18):1838–1848.
- , , . Effects of reducing or eliminating resident work shifts over 16 hours: a systematic review. Sleep. 2010;33(8):1043–1053.
- , , , et al. Impact of duty hours restrictions on quality of care and clinical outcomes. Am J Med. 2007;120(11):968–974.
- , , , , , . Beyond counting hours: the importance of supervision, professionalism, transitions in care, and workload in residency training. Acad Med. 2012;87(7):883–888.
- , , , , , . One possible future for resident hours: interns' perspective on a one‐month trial of the Institute of Medicine recommended duty hour limits. J Grad Med Educ. 2009;1(2):185–187.
- , , , , . Implementing the 2009 Institute of Medicine recommendations on resident physician work hours, supervision, and safety. Nature Sci Sleep. 2001;3:47–85.
- , . Night float teaching and learning: perceptions of residents and faculty. J Grad Med Educ. 2010;2(2):236–241.
- Institute of Medicine. Resident duty hours: enhancing sleep, supervision, and safety. Report brief. Washington, DC: National Academies; 2008. Available at: http://www.iom.edu/∼/media/Files/Report Files/2008/Resident‐Duty‐Hours/residency hours revised for web.pdf. Accessed May 23, 2013.
The Accreditation Council for Graduate Medical Education (ACGME) Common Program Requirements implemented in July 2011 increased supervision requirements and limited continuous work hours for first‐year residents.[1] Similar to the 2003 mandates, these requirements were introduced to improve patient safety and education at academic medical centers.[2] Work‐hour reforms have been associated with decreased resident burnout and improved sleep.[3, 4, 5] However, national observational studies and systematic reviews of the impact of the 2003 reforms on patient safety and quality of care have been varied in terms of outcome.[6, 7, 8, 9, 10] Small studies of the 2011 recommendations have shown increased sleep duration and decreased burnout, but also an increased number of handoffs and increased resident concerns about making a serious medical error.[11, 12, 13, 14] Although national surveys of residents and program directors have not indicated improvements in education or quality of life, 1 observational study did show improvement in clinical exposure and conference attendance.[15, 16, 17, 18] The impact of the 2011 reforms on patient safety remains unclear.[19, 20]
The objective of this study was to evaluate the association between implementation of the 2011 residency work‐hour mandates and patient safety outcomes at a large academic medical center.
METHODS
Study Design
This observational study used a quasi‐experimental difference‐in‐differences approach to evaluate whether residency work‐hour changes were associated with patient safety outcomes among general medicine inpatients. We compared safety outcomes among adult patients discharged from resident general medical services (referred to as resident) to safety outcomes among patients discharged by the hospitalist general medical service (referred to as hospitalist) before and after the 2011 residency work‐hour reforms at a large academic medical center. Differences in outcomes for the resident group were compared to differences observed in the hospitalist group, with adjustment for relevant demographic and case mix factors.[21] We used the hospitalist service as a control group, because ACGME changes applied only to resident services. The strength of this design is that it controls for secular trends that are correlated with patient safety, impacting both residents and hospitalists similarly.[9]
Approval for this study and a Health Insurance Portability and Accountability Act waiver were granted by the Johns Hopkins University School of Medicine institutional review board. We retrospectively examined administrative data on all patient discharges from the general medicine services at Johns Hopkins Hospital between July 1, 2008 and June 30, 2012 that were identified as pertaining to resident or hospitalist services.
Patient Allocation and Physician Scheduling
Patient admission to the resident or hospitalist service was decided by a number of factors. To maintain continuity of care, patients were preferentially admitted to the same service as for prior admissions. New patients were admitted to a service based on bed availability, nurse staffing, patient gender, isolation precautions, and cardiac monitor availability.
The inpatient resident services were staffed prior to July 2011 using a traditional 30‐hour overnight call system. Following July 2011, the inpatient resident services were staffed using a modified overnight call system, in which interns took overnight calls from 8 pm until 12 pm the following day, once every 5 nights with supervision by upper‐level residents. These interns rotated through daytime admitting and coverage roles on the intervening days. The hospitalist service was organized into a 3‐physician rotation of day shift, evening shift, and overnight shift.
Data and Outcomes
Twenty‐nine percent of patients in the sample were admitted more than once during the study period, and patients were generally admitted to the same resident team during each admission. Patients with multiple admissions were counted multiple times in the model. We categorized admissions as prereform (July 1, 2008June 30, 2011) and postreform (July 1, 2011June 30, 2012). Outcomes evaluated included hospital length of stay, 30‐day readmission, intensive care unit stay (ICU) stay, inpatient mortality, and number of Maryland Hospital Acquired Conditions (MHACs). ICU stay pertained to any ICU admission including initial admission and transfer from the inpatient floor. MHACs are a set of inpatient performance indicators derived from a list of 64 inpatient Potentially Preventable Complications developed by 3M Health Information Systems.[22] MHACs are used by the Maryland Health Services Cost Review Commission to link hospital payment to performance for costly, preventable, and clinically relevant complications. MHACs were coded in our analysis as a dichotomous variable. Independent variables included patient age at admission, race, gender, and case mix index. Case mix index (CMI) is a numeric score that measures resource utilization for a specific patient population. CMI is a weighted value assigned to patients based on resource utilization and All Patient Refined Diagnostic Related Group and was included as an indicator of patient illness severity and risk of mortality.[23] Data were obtained from administrative records from the case mix research team at Johns Hopkins Medicine.
To account for transitional differences that may have coincided with the opening of a new hospital wing in late April 2012, we conducted a sensitivity analysis, in which we excluded from analysis any visits that took place in May 2012 to June 2012.
Data Analysis
Based on historical studies, we calculated that a sample size of at least 3600 discharges would allow us to detect a difference of 5% between the pre‐ and postreform period assuming baseline 20% occurrence of dichotomous outcomes (=0.05; =0.2; r=4).[21]
The primary unit of analysis was the hospital discharge. Similar to Horwitz et al., we analyzed data using a difference‐in‐differences estimation strategy.[21] We used multivariable linear regression for length of stay measured as a continuous variable, and multivariable logistic regression for inpatient mortality, 30‐day readmission, MHACs coded as a dichotomous variable, and ICU stay coded as a dichotomous variable.[9] The difference‐in‐differences estimation was used to determine whether the postreform period relative to prereform period was associated with differences in outcomes comparing resident and hospitalist services. In the regression models, the independent variables of interest included an indicator variable for whether a patient was treated on a resident service, an indicator variable for whether a patient was discharged in the postreform period, and the interaction of these 2 variables (resident*postreform). The interaction term can be interpreted as a differential change over time comparing resident and hospitalist services. In all models, we adjusted for patient age, gender, race, and case mix index.
To determine whether prereform trends were similar among the resident and hospitalist services, we performed a test of controls as described by Volpp and colleagues.[6] Interaction terms for resident service and prereform years 2010 and 2011 were added to the model. A Wald test was then used to test for improved model fit, which would indicate differential trends among resident and hospitalist services during the prereform period. Where such trends were found, postreform results were compared only to 2011 rather than the 2009 to 2011 prereform period.[6]
To account for correlation within patients who had multiple discharges, we used a clustering approach and estimated robust variances.[24] From the regression model results, we calculated predicted probabilities adjusted for relevant covariates and prepost differences, and used linear probability models to estimate percentage‐point differences in outcomes, comparing residents and hospitalists in the pre‐ and postreform periods.[25] All analyses were performed using Stata/IC version 11 (StataCorp, College Station, TX).
RESULTS
In the 3 years before the 2011 residency work‐hour reforms were implemented (prereform), there were a total of 15,688 discharges for 8983 patients to the resident services and 4622 discharges for 3649 patients to the hospitalist services. In the year following implementation of residency work‐hour changes (postreform), there were 5253 discharges for 3805 patients to the resident services and 1767 discharges for 1454 patients to the hospitalist service. Table 1 shows the characteristics of patients discharged from the resident and hospitalist services in the pre‐ and postreform periods. Patients discharged from the resident services were more likely to be older, male, African American, and have a higher CMI.
| Resident Services | Hospitalist Service | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 2009 | 2010 | 2011 | 2012 | 2009 | 2010 | 2011 | 2012 | P Valuea | |
| |||||||||
| Discharges, n | 5345 | 5299 | 5044 | 5253 | 1366 | 1492 | 1764 | 1767 | |
| Unique patients, n | 3082 | 2968 | 2933 | 3805 | 1106 | 1180 | 1363 | 1454 | |
| Age, y, mean (SD) | 55.1 (17.7) | 55.7 (17.4) | 56.4 (17.9) | 56.7 (17.1) | 55.9 (17.9) | 56.2 (18.4) | 55.5 (18.8) | 54 (18.7) | 0.02 |
| Sex male, n (%) | 1503 (48.8) | 1397 (47.1) | 1432 (48.8) | 1837 (48.3) | 520 (47) | 550 (46.6) | 613 (45) | 654 (45) | <0.01 |
| Race | |||||||||
| African American, n (%) | 2072 (67.2) | 1922 (64.8) | 1820 (62.1) | 2507 (65.9) | 500 (45.2) | 592 (50.2) | 652 (47.8) | 747 (51.4) | <0.01 |
| White, n (%) | 897 (29.1) | 892 (30.1) | 957 (32.6) | 1118 (29.4) | 534 (48.3) | 527 (44.7) | 621 (45.6) | 619 (42.6) | |
| Asian, n (%) | 19 (.6%) | 35 (1.2) | 28 (1) | 32 (.8) | 11 (1) | 7 (.6) | 25 (1.8) | 12 (.8) | |
| Other, n (%) | 94 (3.1) | 119 (4) | 128 (4.4) | 148 (3.9) | 61 (5.5) | 54 (4.6) | 65 (4.8) | 76 (5.2) | |
| Case mix index, mean (SD) | 1.2 (1) | 1.1 (0.9) | 1.1 (0.9) | 1.1 (1.2) | 1.2 (1) | 1.1 (1) | 1.1 (1) | 1 (0.7) | <0.01 |
Differences in Outcomes Among Resident and Hospitalist Services Pre‐ and Postreform
Table 2 shows unadjusted results. Patients discharged from the resident services in the postreform period as compared to the prereform period had a higher likelihood of an ICU stay (5.9% vs 4.5%, P<0.01), and lower likelihood of 30‐day readmission (17.1% vs 20.1%, P<0.01). Patients discharged from the hospitalist service in the postreform period as compared to the prereform period had a significantly shorter mean length of stay (4.51 vs 4.88 days, P=0.03)
| Resident Services | Hospitalist Service | |||||
|---|---|---|---|---|---|---|
| Outcome | Prereforma | Postreform | P Value | Prereforma | Postreform | P Value |
| ||||||
| Length of stay (mean) | 4.55 (5.39) | 4.50 (5.47) | 0.61 | 4.88 (5.36) | 4.51 (4.64) | 0.03 |
| Any ICU stay (%) | 225 (4.5%) | 310 (5.9%) | <0.01 | 82 (4.7%) | 83 (4.7%) | 0.95 |
| Any MHACs (%) | 560 (3.6%) | 180 (3.4%) | 0.62 | 210 (4.5%) | 64 (3.6%) | 0.09 |
| Readmit in 30 days (%) | 3155 (20.1%) | 900 (17.1%) | <0.01 | 852 (18.4%) | 296 (16.8%) | 0.11 |
| Inpatient mortality (%) | 71 (0.5%) | 28 (0.5%) | 0.48 | 18 (0.4%) | 7 (0.4%) | 0.97 |
Table 3 presents the results of regression analyses examining correlates of patient safety outcomes, adjusted for age, gender, race, and CMI. As the test of controls indicated differential prereform trends for ICU admission and length of stay, the prereform period was limited to 2011 for these outcomes. After adjustment for covariates, the probability of an ICU stay remained greater, and the 30‐day readmission rate was lower among patients discharged from resident services in the postreform period than the prereform period. Among patients discharged from the hospitalist services, there were no significant differences in length of stay, readmissions, ICU admissions, MHACs, or inpatient mortality comparing the pre‐ and postreform periods.
| Resident Services | Hospitalist Service | Difference in Differences | |||||
|---|---|---|---|---|---|---|---|
| Outcome | Prereforma | Postreform | Difference | Prereform | Postreform | Difference | (ResidentHospitalist) |
| |||||||
| ICU stay | 4.5% (4.0% to 5.1%) | 5.7% (5.1% to 6.3%) | 1.4% (0.5% to 2.2%) | 4.4% (3.5% to 5.3%) | 5.3% (4.3% to 6.3%) | 1.1% (0.2 to 2.4%) | 0.3% (1.1% to 1.8%) |
| Inpatient mortality | 0.5% (0.4% to 0.6%) | 0.5% (0.3% to 0.7%) | 0 (0.2% to 0.2%) | 0.3% (0.2% to 0.6%) | 0.5% (0.1% to 0.8%) | 0.1% (0.3% to 0.5%) | 0.1% (0.5% to 0.3%) |
| MHACs | 3.6% (3.3% to 3.9%) | 3.3% (2.9% to 3.7%) | 0.4% (0.9 to 0.2%) | 4.5% (3.9% to 5.1%) | 4.1% (3.2% to 5.1%) | 0.3% (1.4% to 0.7%) | 0.2% (1.0% to 1.3%) |
| Readmit 30 days | 20.1% (19.1% to 21.1%) | 17.2% (15.9% to 18.5%) | 2.8% (4.3% to 1.3%) | 18.4% (16.5% to 20.2%) | 16.6% (14.7% to 18.5%) | 1.7% (4.1% to 0.8%) | 1.8% (0.2% to 3.7%) |
| Length of stay | 4.6 (4.4 to 4.7) | 4.4 (4.3 to 4.6) | 0.1 (0.3 to 0.1) | 4.9 (4.6 to 5.1) | 4.7 (4.5 to 5.0) | 0.1 (0.4 to 0.2) | 0.01 (0.37 to 0.34) |
Differences in Outcomes Comparing Resident and Hospitalist Services Pre‐ and Postreform
Comparing pre‐ and postreform periods in the resident and hospitalist services, there were no significant differences in ICU admission, length of stay, MHACs, 30‐day readmissions, or inpatient mortality. In the sensitivity analysis, in which we excluded all discharges in May 2012 to June 2012, results were not significantly different for any of the outcomes examined.
DISCUSSION
Using difference‐in‐differences estimation, we evaluated whether the implementation of the 2011 residency work‐hour mandate was associated with differences in patient safety outcomes including length of stay, 30‐day readmission, inpatient mortality, MHACs, and ICU admissions comparing resident and hospitalist services at a large academic medical center. Adjusting for patient age, race, gender, and clinical complexity, we found no significant changes in any of the patient safety outcomes indicators in the postreform period comparing resident to hospitalist services.
Our quasiexperimental study design allowed us to gauge differences in patient safety outcomes, while reducing bias due to unmeasured confounders that might impact patient safety indicators.[9] We were able to examine all discharges from the resident and hospitalist general medicine services during the academic years 2009 to 2012, while adjusting for age, race, gender, and clinical complexity. Though ICU admission was higher and readmission rates were lower on the resident services post‐2011, we did not observe a significant difference in ICU admission or 30‐day readmission rates in the postreform period comparing patients discharged from the resident and hospitalist services and all patients in the prereform period.
Our neutral findings differ from some other single‐institution evaluations of reduced resident work hours, several of which have shown improved quality of life, education, and patient safety indicators.[18, 21, 26, 27, 28] It is unclear why improvements in patient safety were not identified in the current study. The 2011 reforms were more broad‐based than some of the preliminary studies of reduced work hours, and therefore additional variables may be at play. For instance, challenges related to decreased work hours, including the increased number of handoffs in care and work compression, may require specific interventions to produce sustained improvements in patient safety.[3, 14, 29, 30]
Improving patient safety requires more than changing resident work hours. Blum et al. recommended enhanced funding to increase supervision, decrease resident caseload, and incentivize achievement of quality indicators to achieve the goal of improved patient safety within work‐hour reform.[31] Schumacher et al. proposed a focus on supervision, professionalism, safe transitions of care, and optimizing workloads as a means to improve patient safety and education within the new residency training paradigm.[29]
Limitations of this study include limited follow‐up time after implementation of the work‐hour reforms. It may take more time to optimize systems of care to see benefits in patient safety indicators. This was a single‐institution study of a limited number of outcomes in a single department, which limits generalizability and may reflect local experience rather than broader trends. The call schedule on the resident service in this study differs from programs that have adopted night float schedules. [27] This may have had an effect on patient care outcomes.[32] In an attempt to conduct a timely study of inpatient safety indicators following the 2011 changes, our study was not powered to detect small changes in low‐frequency outcomes such as mortality; longer‐term studies at multiple institutions will be needed to answer these key questions. We limited the prereform period where our test of controls indicated differential prereform trends, which reduced power.
As this was an observational study rather than an experiment, there may have been both measured and unmeasured differences in patient characteristics and comorbidity between the intervention and control group. For example, CMI was lower on the hospitalist service than the resident services. Demographics varied somewhat between services; male and African American patients were more likely to be discharged from resident services than hospitalist services for unknown reasons. Although we adjusted for demographics and CMI in our model, there may be residual confounding. Limitations in data collection did not allow us to separate patients initially admitted to the ICU from patients transferred to the ICU from the inpatient floors. We attempted to overcome this limitation through use of a difference‐in‐differences model to account for secular trends, but factors other than residency work hours may have impacted the resident and hospitalist services differentially. For example, hospital quality‐improvement programs or provider‐level factors may have differentially impacted the resident versus hospitalist services during the study period.
Work‐hour limitations for residents were established to improve residency education and patient safety. As noted by the Institute of Medicine, improving patient safety will require significant investment by program directors, hospitals, and the public to keep resident caseloads manageable, ensure adequate supervision of first‐year residents, train residents on safe handoffs in care, and conduct ongoing evaluations of patient safety and any unintended consequences of the regulations.[33] In the first year after implementation of the 2011 work‐hour reforms, we found no change in ICU admission, inpatient mortality, 30‐day readmission rates, length of stay, or MHACs compared with patients treated by hospitalists. Studies of the long‐term impact of residency work‐hour reform are necessary to determine whether changes in work hours have been associated with improvement in resident education and patient safety.
Disclosure: Nothing to report.
The Accreditation Council for Graduate Medical Education (ACGME) Common Program Requirements implemented in July 2011 increased supervision requirements and limited continuous work hours for first‐year residents.[1] Similar to the 2003 mandates, these requirements were introduced to improve patient safety and education at academic medical centers.[2] Work‐hour reforms have been associated with decreased resident burnout and improved sleep.[3, 4, 5] However, national observational studies and systematic reviews of the impact of the 2003 reforms on patient safety and quality of care have been varied in terms of outcome.[6, 7, 8, 9, 10] Small studies of the 2011 recommendations have shown increased sleep duration and decreased burnout, but also an increased number of handoffs and increased resident concerns about making a serious medical error.[11, 12, 13, 14] Although national surveys of residents and program directors have not indicated improvements in education or quality of life, 1 observational study did show improvement in clinical exposure and conference attendance.[15, 16, 17, 18] The impact of the 2011 reforms on patient safety remains unclear.[19, 20]
The objective of this study was to evaluate the association between implementation of the 2011 residency work‐hour mandates and patient safety outcomes at a large academic medical center.
METHODS
Study Design
This observational study used a quasi‐experimental difference‐in‐differences approach to evaluate whether residency work‐hour changes were associated with patient safety outcomes among general medicine inpatients. We compared safety outcomes among adult patients discharged from resident general medical services (referred to as resident) to safety outcomes among patients discharged by the hospitalist general medical service (referred to as hospitalist) before and after the 2011 residency work‐hour reforms at a large academic medical center. Differences in outcomes for the resident group were compared to differences observed in the hospitalist group, with adjustment for relevant demographic and case mix factors.[21] We used the hospitalist service as a control group, because ACGME changes applied only to resident services. The strength of this design is that it controls for secular trends that are correlated with patient safety, impacting both residents and hospitalists similarly.[9]
Approval for this study and a Health Insurance Portability and Accountability Act waiver were granted by the Johns Hopkins University School of Medicine institutional review board. We retrospectively examined administrative data on all patient discharges from the general medicine services at Johns Hopkins Hospital between July 1, 2008 and June 30, 2012 that were identified as pertaining to resident or hospitalist services.
Patient Allocation and Physician Scheduling
Patient admission to the resident or hospitalist service was decided by a number of factors. To maintain continuity of care, patients were preferentially admitted to the same service as for prior admissions. New patients were admitted to a service based on bed availability, nurse staffing, patient gender, isolation precautions, and cardiac monitor availability.
The inpatient resident services were staffed prior to July 2011 using a traditional 30‐hour overnight call system. Following July 2011, the inpatient resident services were staffed using a modified overnight call system, in which interns took overnight calls from 8 pm until 12 pm the following day, once every 5 nights with supervision by upper‐level residents. These interns rotated through daytime admitting and coverage roles on the intervening days. The hospitalist service was organized into a 3‐physician rotation of day shift, evening shift, and overnight shift.
Data and Outcomes
Twenty‐nine percent of patients in the sample were admitted more than once during the study period, and patients were generally admitted to the same resident team during each admission. Patients with multiple admissions were counted multiple times in the model. We categorized admissions as prereform (July 1, 2008June 30, 2011) and postreform (July 1, 2011June 30, 2012). Outcomes evaluated included hospital length of stay, 30‐day readmission, intensive care unit stay (ICU) stay, inpatient mortality, and number of Maryland Hospital Acquired Conditions (MHACs). ICU stay pertained to any ICU admission including initial admission and transfer from the inpatient floor. MHACs are a set of inpatient performance indicators derived from a list of 64 inpatient Potentially Preventable Complications developed by 3M Health Information Systems.[22] MHACs are used by the Maryland Health Services Cost Review Commission to link hospital payment to performance for costly, preventable, and clinically relevant complications. MHACs were coded in our analysis as a dichotomous variable. Independent variables included patient age at admission, race, gender, and case mix index. Case mix index (CMI) is a numeric score that measures resource utilization for a specific patient population. CMI is a weighted value assigned to patients based on resource utilization and All Patient Refined Diagnostic Related Group and was included as an indicator of patient illness severity and risk of mortality.[23] Data were obtained from administrative records from the case mix research team at Johns Hopkins Medicine.
To account for transitional differences that may have coincided with the opening of a new hospital wing in late April 2012, we conducted a sensitivity analysis, in which we excluded from analysis any visits that took place in May 2012 to June 2012.
Data Analysis
Based on historical studies, we calculated that a sample size of at least 3600 discharges would allow us to detect a difference of 5% between the pre‐ and postreform period assuming baseline 20% occurrence of dichotomous outcomes (=0.05; =0.2; r=4).[21]
The primary unit of analysis was the hospital discharge. Similar to Horwitz et al., we analyzed data using a difference‐in‐differences estimation strategy.[21] We used multivariable linear regression for length of stay measured as a continuous variable, and multivariable logistic regression for inpatient mortality, 30‐day readmission, MHACs coded as a dichotomous variable, and ICU stay coded as a dichotomous variable.[9] The difference‐in‐differences estimation was used to determine whether the postreform period relative to prereform period was associated with differences in outcomes comparing resident and hospitalist services. In the regression models, the independent variables of interest included an indicator variable for whether a patient was treated on a resident service, an indicator variable for whether a patient was discharged in the postreform period, and the interaction of these 2 variables (resident*postreform). The interaction term can be interpreted as a differential change over time comparing resident and hospitalist services. In all models, we adjusted for patient age, gender, race, and case mix index.
To determine whether prereform trends were similar among the resident and hospitalist services, we performed a test of controls as described by Volpp and colleagues.[6] Interaction terms for resident service and prereform years 2010 and 2011 were added to the model. A Wald test was then used to test for improved model fit, which would indicate differential trends among resident and hospitalist services during the prereform period. Where such trends were found, postreform results were compared only to 2011 rather than the 2009 to 2011 prereform period.[6]
To account for correlation within patients who had multiple discharges, we used a clustering approach and estimated robust variances.[24] From the regression model results, we calculated predicted probabilities adjusted for relevant covariates and prepost differences, and used linear probability models to estimate percentage‐point differences in outcomes, comparing residents and hospitalists in the pre‐ and postreform periods.[25] All analyses were performed using Stata/IC version 11 (StataCorp, College Station, TX).
RESULTS
In the 3 years before the 2011 residency work‐hour reforms were implemented (prereform), there were a total of 15,688 discharges for 8983 patients to the resident services and 4622 discharges for 3649 patients to the hospitalist services. In the year following implementation of residency work‐hour changes (postreform), there were 5253 discharges for 3805 patients to the resident services and 1767 discharges for 1454 patients to the hospitalist service. Table 1 shows the characteristics of patients discharged from the resident and hospitalist services in the pre‐ and postreform periods. Patients discharged from the resident services were more likely to be older, male, African American, and have a higher CMI.
| Resident Services | Hospitalist Service | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 2009 | 2010 | 2011 | 2012 | 2009 | 2010 | 2011 | 2012 | P Valuea | |
| |||||||||
| Discharges, n | 5345 | 5299 | 5044 | 5253 | 1366 | 1492 | 1764 | 1767 | |
| Unique patients, n | 3082 | 2968 | 2933 | 3805 | 1106 | 1180 | 1363 | 1454 | |
| Age, y, mean (SD) | 55.1 (17.7) | 55.7 (17.4) | 56.4 (17.9) | 56.7 (17.1) | 55.9 (17.9) | 56.2 (18.4) | 55.5 (18.8) | 54 (18.7) | 0.02 |
| Sex male, n (%) | 1503 (48.8) | 1397 (47.1) | 1432 (48.8) | 1837 (48.3) | 520 (47) | 550 (46.6) | 613 (45) | 654 (45) | <0.01 |
| Race | |||||||||
| African American, n (%) | 2072 (67.2) | 1922 (64.8) | 1820 (62.1) | 2507 (65.9) | 500 (45.2) | 592 (50.2) | 652 (47.8) | 747 (51.4) | <0.01 |
| White, n (%) | 897 (29.1) | 892 (30.1) | 957 (32.6) | 1118 (29.4) | 534 (48.3) | 527 (44.7) | 621 (45.6) | 619 (42.6) | |
| Asian, n (%) | 19 (.6%) | 35 (1.2) | 28 (1) | 32 (.8) | 11 (1) | 7 (.6) | 25 (1.8) | 12 (.8) | |
| Other, n (%) | 94 (3.1) | 119 (4) | 128 (4.4) | 148 (3.9) | 61 (5.5) | 54 (4.6) | 65 (4.8) | 76 (5.2) | |
| Case mix index, mean (SD) | 1.2 (1) | 1.1 (0.9) | 1.1 (0.9) | 1.1 (1.2) | 1.2 (1) | 1.1 (1) | 1.1 (1) | 1 (0.7) | <0.01 |
Differences in Outcomes Among Resident and Hospitalist Services Pre‐ and Postreform
Table 2 shows unadjusted results. Patients discharged from the resident services in the postreform period as compared to the prereform period had a higher likelihood of an ICU stay (5.9% vs 4.5%, P<0.01), and lower likelihood of 30‐day readmission (17.1% vs 20.1%, P<0.01). Patients discharged from the hospitalist service in the postreform period as compared to the prereform period had a significantly shorter mean length of stay (4.51 vs 4.88 days, P=0.03)
| Resident Services | Hospitalist Service | |||||
|---|---|---|---|---|---|---|
| Outcome | Prereforma | Postreform | P Value | Prereforma | Postreform | P Value |
| ||||||
| Length of stay (mean) | 4.55 (5.39) | 4.50 (5.47) | 0.61 | 4.88 (5.36) | 4.51 (4.64) | 0.03 |
| Any ICU stay (%) | 225 (4.5%) | 310 (5.9%) | <0.01 | 82 (4.7%) | 83 (4.7%) | 0.95 |
| Any MHACs (%) | 560 (3.6%) | 180 (3.4%) | 0.62 | 210 (4.5%) | 64 (3.6%) | 0.09 |
| Readmit in 30 days (%) | 3155 (20.1%) | 900 (17.1%) | <0.01 | 852 (18.4%) | 296 (16.8%) | 0.11 |
| Inpatient mortality (%) | 71 (0.5%) | 28 (0.5%) | 0.48 | 18 (0.4%) | 7 (0.4%) | 0.97 |
Table 3 presents the results of regression analyses examining correlates of patient safety outcomes, adjusted for age, gender, race, and CMI. As the test of controls indicated differential prereform trends for ICU admission and length of stay, the prereform period was limited to 2011 for these outcomes. After adjustment for covariates, the probability of an ICU stay remained greater, and the 30‐day readmission rate was lower among patients discharged from resident services in the postreform period than the prereform period. Among patients discharged from the hospitalist services, there were no significant differences in length of stay, readmissions, ICU admissions, MHACs, or inpatient mortality comparing the pre‐ and postreform periods.
| Resident Services | Hospitalist Service | Difference in Differences | |||||
|---|---|---|---|---|---|---|---|
| Outcome | Prereforma | Postreform | Difference | Prereform | Postreform | Difference | (ResidentHospitalist) |
| |||||||
| ICU stay | 4.5% (4.0% to 5.1%) | 5.7% (5.1% to 6.3%) | 1.4% (0.5% to 2.2%) | 4.4% (3.5% to 5.3%) | 5.3% (4.3% to 6.3%) | 1.1% (0.2 to 2.4%) | 0.3% (1.1% to 1.8%) |
| Inpatient mortality | 0.5% (0.4% to 0.6%) | 0.5% (0.3% to 0.7%) | 0 (0.2% to 0.2%) | 0.3% (0.2% to 0.6%) | 0.5% (0.1% to 0.8%) | 0.1% (0.3% to 0.5%) | 0.1% (0.5% to 0.3%) |
| MHACs | 3.6% (3.3% to 3.9%) | 3.3% (2.9% to 3.7%) | 0.4% (0.9 to 0.2%) | 4.5% (3.9% to 5.1%) | 4.1% (3.2% to 5.1%) | 0.3% (1.4% to 0.7%) | 0.2% (1.0% to 1.3%) |
| Readmit 30 days | 20.1% (19.1% to 21.1%) | 17.2% (15.9% to 18.5%) | 2.8% (4.3% to 1.3%) | 18.4% (16.5% to 20.2%) | 16.6% (14.7% to 18.5%) | 1.7% (4.1% to 0.8%) | 1.8% (0.2% to 3.7%) |
| Length of stay | 4.6 (4.4 to 4.7) | 4.4 (4.3 to 4.6) | 0.1 (0.3 to 0.1) | 4.9 (4.6 to 5.1) | 4.7 (4.5 to 5.0) | 0.1 (0.4 to 0.2) | 0.01 (0.37 to 0.34) |
Differences in Outcomes Comparing Resident and Hospitalist Services Pre‐ and Postreform
Comparing pre‐ and postreform periods in the resident and hospitalist services, there were no significant differences in ICU admission, length of stay, MHACs, 30‐day readmissions, or inpatient mortality. In the sensitivity analysis, in which we excluded all discharges in May 2012 to June 2012, results were not significantly different for any of the outcomes examined.
DISCUSSION
Using difference‐in‐differences estimation, we evaluated whether the implementation of the 2011 residency work‐hour mandate was associated with differences in patient safety outcomes including length of stay, 30‐day readmission, inpatient mortality, MHACs, and ICU admissions comparing resident and hospitalist services at a large academic medical center. Adjusting for patient age, race, gender, and clinical complexity, we found no significant changes in any of the patient safety outcomes indicators in the postreform period comparing resident to hospitalist services.
Our quasiexperimental study design allowed us to gauge differences in patient safety outcomes, while reducing bias due to unmeasured confounders that might impact patient safety indicators.[9] We were able to examine all discharges from the resident and hospitalist general medicine services during the academic years 2009 to 2012, while adjusting for age, race, gender, and clinical complexity. Though ICU admission was higher and readmission rates were lower on the resident services post‐2011, we did not observe a significant difference in ICU admission or 30‐day readmission rates in the postreform period comparing patients discharged from the resident and hospitalist services and all patients in the prereform period.
Our neutral findings differ from some other single‐institution evaluations of reduced resident work hours, several of which have shown improved quality of life, education, and patient safety indicators.[18, 21, 26, 27, 28] It is unclear why improvements in patient safety were not identified in the current study. The 2011 reforms were more broad‐based than some of the preliminary studies of reduced work hours, and therefore additional variables may be at play. For instance, challenges related to decreased work hours, including the increased number of handoffs in care and work compression, may require specific interventions to produce sustained improvements in patient safety.[3, 14, 29, 30]
Improving patient safety requires more than changing resident work hours. Blum et al. recommended enhanced funding to increase supervision, decrease resident caseload, and incentivize achievement of quality indicators to achieve the goal of improved patient safety within work‐hour reform.[31] Schumacher et al. proposed a focus on supervision, professionalism, safe transitions of care, and optimizing workloads as a means to improve patient safety and education within the new residency training paradigm.[29]
Limitations of this study include limited follow‐up time after implementation of the work‐hour reforms. It may take more time to optimize systems of care to see benefits in patient safety indicators. This was a single‐institution study of a limited number of outcomes in a single department, which limits generalizability and may reflect local experience rather than broader trends. The call schedule on the resident service in this study differs from programs that have adopted night float schedules. [27] This may have had an effect on patient care outcomes.[32] In an attempt to conduct a timely study of inpatient safety indicators following the 2011 changes, our study was not powered to detect small changes in low‐frequency outcomes such as mortality; longer‐term studies at multiple institutions will be needed to answer these key questions. We limited the prereform period where our test of controls indicated differential prereform trends, which reduced power.
As this was an observational study rather than an experiment, there may have been both measured and unmeasured differences in patient characteristics and comorbidity between the intervention and control group. For example, CMI was lower on the hospitalist service than the resident services. Demographics varied somewhat between services; male and African American patients were more likely to be discharged from resident services than hospitalist services for unknown reasons. Although we adjusted for demographics and CMI in our model, there may be residual confounding. Limitations in data collection did not allow us to separate patients initially admitted to the ICU from patients transferred to the ICU from the inpatient floors. We attempted to overcome this limitation through use of a difference‐in‐differences model to account for secular trends, but factors other than residency work hours may have impacted the resident and hospitalist services differentially. For example, hospital quality‐improvement programs or provider‐level factors may have differentially impacted the resident versus hospitalist services during the study period.
Work‐hour limitations for residents were established to improve residency education and patient safety. As noted by the Institute of Medicine, improving patient safety will require significant investment by program directors, hospitals, and the public to keep resident caseloads manageable, ensure adequate supervision of first‐year residents, train residents on safe handoffs in care, and conduct ongoing evaluations of patient safety and any unintended consequences of the regulations.[33] In the first year after implementation of the 2011 work‐hour reforms, we found no change in ICU admission, inpatient mortality, 30‐day readmission rates, length of stay, or MHACs compared with patients treated by hospitalists. Studies of the long‐term impact of residency work‐hour reform are necessary to determine whether changes in work hours have been associated with improvement in resident education and patient safety.
Disclosure: Nothing to report.
- Accreditation Council for Graduate Medical Education. Common program requirements effective: July 1, 2011. Available at: http://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramResources/Common_Program_Requirements_07012011[1].pdf. Accessed February 10, 2014.
- , , . The new recommendations on duty hours from the ACGME Task Force. N Engl J Med. 2010;363:e3.
- , , , , . Interns' compliance with Accreditation Council for Graduate Medical Education work‐hour limits. JAMA. 2006;296(9):1063–1070.
- , , , , , . Effects of work hour reduction on residents' lives: a systematic review. JAMA. 2005;294(9):1088–1100.
- , , , et al. Effects of the ACGME duty hour limits on sleep, work hours, and safety. Pediatrics. 2008;122(2):250–258.
- , , . Teaching hospital five‐year mortality trends in the wake of duty hour reforms. J Gen Intern Med. 2013;28(8):1048–1055.
- , , , . Duty hour limits and patient care and resident outcomes: can high‐quality studies offer insight into complex relationships? Ann Rev Med. 2013;64:467–483.
- , , . Patient safety, resident education and resident well‐being following implementation of the 2003 ACGME duty hour rules. J Gen Intern Med. 2011;26(8):907–919.
- , , , et al. Mortality among hospitalized Medicare beneficiaries in the first 2 years following ACGME resident duty hour reform. JAMA. 2007;298(9):975–983.
- , , , et al. Effects of resident duty hour reform on surgical and procedural patient safety indicators among hospitalized Veterans Health Administration and Medicare patients. Med Care. 2009;47(7):723–731.
- , , , et al. Pilot trial of IOM duty hour recommendations in neurology residency programs. Neurology. 2011;77(9):883–887.
- , , , et al. Effect of 16‐hour duty periods of patient care and resident education. Mayo Clin Proc. 2011;86:192–196.
- , , , et al. Effects of the 2011 duty hour reforms on interns and their patients: a prospective longitudinal cohort study. JAMA Intern Med. 2013;173(8):657–662.
- , , , et al. Effect of the 2011 vs 2003 duty hour regulation—compliant models on sleep duration, trainee education, and continuity of patient care among internal medicine house staff. JAMA Intern Med. 2013;173(8):649–655.
- , , . Residents' response to duty‐hour regulations—a follow‐up national survey. N Engl J Med. 2012;366:e35.
- , , , . Surgical residents' perceptions of 2011 Accreditation Council for Graduate Medical Education duty hour regulations. JAMA Surg. 2013;148(5):427–433.
- , , . The 2011 duty hour requirements—a survey of residency program directors. N Engl J Med. 2013;368:694–697.
- , , , et al. The effect of reducing maximum shift lengths to 16 hours on internal medicine interns' educational opportunities. Acad Med. 2013;88(4):512–518.
- , . Residency work‐hours reform. A cost analysis including preventable adverse events. J Gen Intern Med. 2005;20(10):873–878.
- , , , , . Cost implications of reduced work hours and workloads for resident physicians. N Engl J Med. 2009;360:2202–2215.
- , , , . Changes in outcomes for internal medicine inpatients after work‐hour regulations. Ann Intern Med. 2007;147:97–103.
- .Maryland Health Services Cost Review Commission. Complications: Maryland Hospital Acquired Conditions. Available at: http://www.hscrc.state.md.us/init_qi_MHAC.cfm. Accessed May 23, 2013.
- , , , et al. What are APR‐DRGs? An introduction to severity of illness and risk of mortality adjustment methodology. 3M Health Information Systems. Available at: http://solutions.3m.com/3MContentRetrievalAPI/BlobServlet?locale=it_IT44(4):1049–1060.
- , , , , . Impact of the 2008 US Preventive Services Task Force Recommendation to discontinue prostate cancer screening among male Medicare beneficiaries. Arch Intern Med. 2012;172(20):1601–1603.
- , , , et al. Effect of reducing interns' work hour on serious medical errors in intensive care units. N Engl J Med. 2004;351(18):1838–1848.
- , , . Effects of reducing or eliminating resident work shifts over 16 hours: a systematic review. Sleep. 2010;33(8):1043–1053.
- , , , et al. Impact of duty hours restrictions on quality of care and clinical outcomes. Am J Med. 2007;120(11):968–974.
- , , , , , . Beyond counting hours: the importance of supervision, professionalism, transitions in care, and workload in residency training. Acad Med. 2012;87(7):883–888.
- , , , , , . One possible future for resident hours: interns' perspective on a one‐month trial of the Institute of Medicine recommended duty hour limits. J Grad Med Educ. 2009;1(2):185–187.
- , , , , . Implementing the 2009 Institute of Medicine recommendations on resident physician work hours, supervision, and safety. Nature Sci Sleep. 2001;3:47–85.
- , . Night float teaching and learning: perceptions of residents and faculty. J Grad Med Educ. 2010;2(2):236–241.
- Institute of Medicine. Resident duty hours: enhancing sleep, supervision, and safety. Report brief. Washington, DC: National Academies; 2008. Available at: http://www.iom.edu/∼/media/Files/Report Files/2008/Resident‐Duty‐Hours/residency hours revised for web.pdf. Accessed May 23, 2013.
- Accreditation Council for Graduate Medical Education. Common program requirements effective: July 1, 2011. Available at: http://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramResources/Common_Program_Requirements_07012011[1].pdf. Accessed February 10, 2014.
- , , . The new recommendations on duty hours from the ACGME Task Force. N Engl J Med. 2010;363:e3.
- , , , , . Interns' compliance with Accreditation Council for Graduate Medical Education work‐hour limits. JAMA. 2006;296(9):1063–1070.
- , , , , , . Effects of work hour reduction on residents' lives: a systematic review. JAMA. 2005;294(9):1088–1100.
- , , , et al. Effects of the ACGME duty hour limits on sleep, work hours, and safety. Pediatrics. 2008;122(2):250–258.
- , , . Teaching hospital five‐year mortality trends in the wake of duty hour reforms. J Gen Intern Med. 2013;28(8):1048–1055.
- , , , . Duty hour limits and patient care and resident outcomes: can high‐quality studies offer insight into complex relationships? Ann Rev Med. 2013;64:467–483.
- , , . Patient safety, resident education and resident well‐being following implementation of the 2003 ACGME duty hour rules. J Gen Intern Med. 2011;26(8):907–919.
- , , , et al. Mortality among hospitalized Medicare beneficiaries in the first 2 years following ACGME resident duty hour reform. JAMA. 2007;298(9):975–983.
- , , , et al. Effects of resident duty hour reform on surgical and procedural patient safety indicators among hospitalized Veterans Health Administration and Medicare patients. Med Care. 2009;47(7):723–731.
- , , , et al. Pilot trial of IOM duty hour recommendations in neurology residency programs. Neurology. 2011;77(9):883–887.
- , , , et al. Effect of 16‐hour duty periods of patient care and resident education. Mayo Clin Proc. 2011;86:192–196.
- , , , et al. Effects of the 2011 duty hour reforms on interns and their patients: a prospective longitudinal cohort study. JAMA Intern Med. 2013;173(8):657–662.
- , , , et al. Effect of the 2011 vs 2003 duty hour regulation—compliant models on sleep duration, trainee education, and continuity of patient care among internal medicine house staff. JAMA Intern Med. 2013;173(8):649–655.
- , , . Residents' response to duty‐hour regulations—a follow‐up national survey. N Engl J Med. 2012;366:e35.
- , , , . Surgical residents' perceptions of 2011 Accreditation Council for Graduate Medical Education duty hour regulations. JAMA Surg. 2013;148(5):427–433.
- , , . The 2011 duty hour requirements—a survey of residency program directors. N Engl J Med. 2013;368:694–697.
- , , , et al. The effect of reducing maximum shift lengths to 16 hours on internal medicine interns' educational opportunities. Acad Med. 2013;88(4):512–518.
- , . Residency work‐hours reform. A cost analysis including preventable adverse events. J Gen Intern Med. 2005;20(10):873–878.
- , , , , . Cost implications of reduced work hours and workloads for resident physicians. N Engl J Med. 2009;360:2202–2215.
- , , , . Changes in outcomes for internal medicine inpatients after work‐hour regulations. Ann Intern Med. 2007;147:97–103.
- .Maryland Health Services Cost Review Commission. Complications: Maryland Hospital Acquired Conditions. Available at: http://www.hscrc.state.md.us/init_qi_MHAC.cfm. Accessed May 23, 2013.
- , , , et al. What are APR‐DRGs? An introduction to severity of illness and risk of mortality adjustment methodology. 3M Health Information Systems. Available at: http://solutions.3m.com/3MContentRetrievalAPI/BlobServlet?locale=it_IT44(4):1049–1060.
- , , , , . Impact of the 2008 US Preventive Services Task Force Recommendation to discontinue prostate cancer screening among male Medicare beneficiaries. Arch Intern Med. 2012;172(20):1601–1603.
- , , , et al. Effect of reducing interns' work hour on serious medical errors in intensive care units. N Engl J Med. 2004;351(18):1838–1848.
- , , . Effects of reducing or eliminating resident work shifts over 16 hours: a systematic review. Sleep. 2010;33(8):1043–1053.
- , , , et al. Impact of duty hours restrictions on quality of care and clinical outcomes. Am J Med. 2007;120(11):968–974.
- , , , , , . Beyond counting hours: the importance of supervision, professionalism, transitions in care, and workload in residency training. Acad Med. 2012;87(7):883–888.
- , , , , , . One possible future for resident hours: interns' perspective on a one‐month trial of the Institute of Medicine recommended duty hour limits. J Grad Med Educ. 2009;1(2):185–187.
- , , , , . Implementing the 2009 Institute of Medicine recommendations on resident physician work hours, supervision, and safety. Nature Sci Sleep. 2001;3:47–85.
- , . Night float teaching and learning: perceptions of residents and faculty. J Grad Med Educ. 2010;2(2):236–241.
- Institute of Medicine. Resident duty hours: enhancing sleep, supervision, and safety. Report brief. Washington, DC: National Academies; 2008. Available at: http://www.iom.edu/∼/media/Files/Report Files/2008/Resident‐Duty‐Hours/residency hours revised for web.pdf. Accessed May 23, 2013.
© 2014 Society of Hospital Medicine
Etiquette‐Based Medicine Among Interns
Patient‐centered communication may impact several aspects of the patientdoctor relationship including patient disclosure of illness‐related information, patient satisfaction, anxiety, and compliance with medical recommendations.[1, 2, 3, 4] Etiquette‐based medicine, a term coined by Kahn, involves simple patient‐centered communication strategies that convey professionalism and respect to patients.[5] Studies have confirmed that patients prefer physicians who practice etiquette‐based medicine behaviors, including sitting down and introducing one's self.[6, 7, 8, 9] Performance of etiquette‐based medicine is associated with higher Press Ganey patient satisfaction scores. However, these easy‐to‐practice behaviors may not be modeled commonly in the inpatient setting.[10] We sought to understand whether etiquette‐based communication behaviors are practiced by trainees on inpatient medicine rotations.
METHODS
Design
This was a prospective study incorporating direct observation of intern interactions with patients during January 2012 at 2 internal medicine residency programs in Baltimore Maryland, Johns Hopkins Hospital (JHH) and the University of Maryland Medical Center (UMMC). We then surveyed participants from JHH in June 2012 to assess perceptions of their practice of etiquette‐based communication.
Participants and Setting
We observed a convenience sample of 29 internal medicine interns from the 2 institutions. We sought to observe interns over an equal number of hours at both sites and to sample shifts in proportion to the amount of time interns spend on each of these shifts. All interns who were asked to participate in the study agreed and comprised a total of 27% of the 108 interns in the 2 programs. The institutional review board at Johns Hopkins School of Medicine approved the study; the University of Maryland institutional review board deemed it not human subjects research. All observed interns provided informed consent to be observed during 1 to 4 inpatient shifts.
Observers
Twenty‐two undergraduate university students served as the observers for the study and were trained to collect data with the iPod Touch (Apple, Cupertino, CA) without interrupting patient care. We then tested the observers to ensure 85% concordance rate with the researchers in mock observation. Four hours of quality assurance were completed at both institutions during the study. Congruence between observer and research team member was >85% for each hour of observation.
Observation
Observers recorded intern activities on the iPod Touch spreadsheet application. The application allowed for real‐time data entry and direct export of results. The primary dependent variables for this study were 5 behaviors that were assessed each time an intern went into a patient's room. The 5 observed behaviors included (1) introducing one's self, (2) introducing one's role on the medical team, (3) touching the patient, (4) sitting down, and (5) asking the patient at least 1 open‐ended question. These behaviors were chosen for observation because they are central to Kahn's framework of etiquette‐based medicine, applicable to each inpatient encounter, and readily observed by trained nonmedical observers. These behaviors are defined in Table 1. Use of open‐ended questions was observed as a more general form of Kahn's recommendation to ask how the patient is feeling. Interns were not aware of which behaviors were being evaluated.
| Behavior | Definition |
|---|---|
| Introduced self | Providing a name |
| Introduced role | Uses term doctor, resident, intern, or medical team |
| Sat down | Sitting on the bed, in a chair, or crouching if no chair was available during at least part of the encounter |
| Touched the patient | Any form of physical contact that occurred at least once during the encounter including shaking a patient's hand, touching a patient on the shoulder, or performing any part of the physical exam |
| Asked open‐ended question | Asked the patient any question that required more than a yes/no answer |
Each time an observed intern entered a patient room, the observer recorded whether or not each of the 5 behaviors was performed, coded as a dichotomous variable. Although data collection was anonymous, observers recorded the team, hospital site, gender of the intern, and whether the intern was admitting new patients during the shift.
Survey
Following the observational portion of the study, participants at JHH completed a cross‐sectional, anonymous survey that asked them to estimate how frequently they currently performed each of the behaviors observed in this study. Response options included the following categories: <20%, 20% to 40%, 40% to 60%, 60% to 80%, or 80% to 100%.
Data Analysis
We determined the percent of patient visits during which each behavior was performed. Data were analyzed using Student t and [2] tests evaluating differences by hospital, intern gender, type of shift, and time of day. To account for correlation within subjects and observers, we performed multilevel logistic regression analysis adjusted for clustering at the intern and observer levels. For the survey analysis, the mean of the response category was used as the basis for comparison. All quantitative analyses were performed in Excel 2010 (Microsoft Corp., Redmond, WA) and Stata/IC version 11 (StataCorp, College Station, TX).
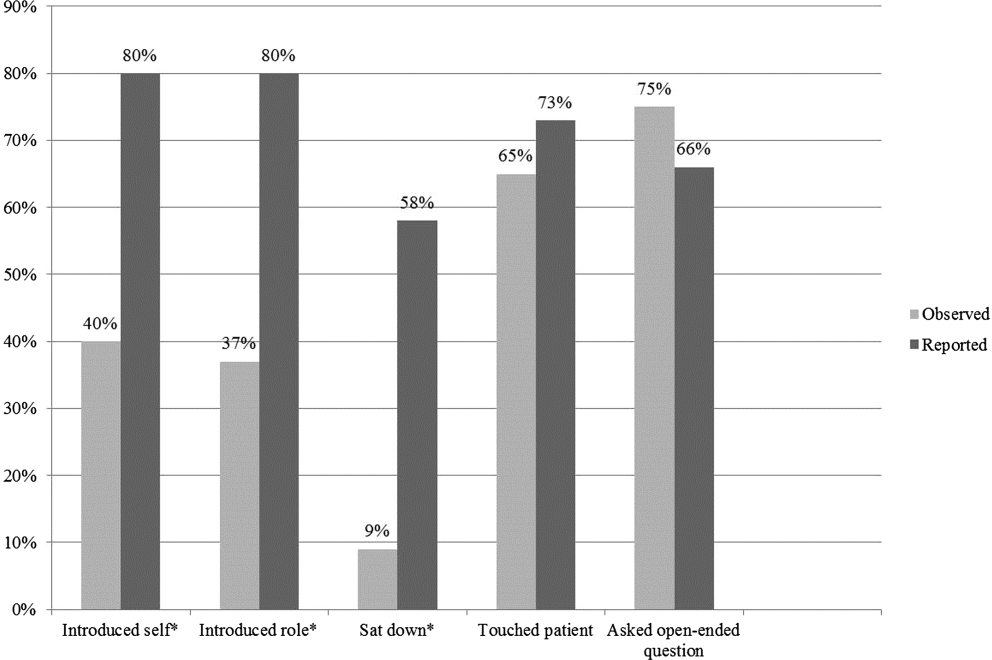
RESULTS
A total of 732 inpatient encounters were observed during 118 intern shifts. Interns were observed for a mean of 25 patient encounters each (range, 361; standard deviation [SD] 17). Overall, interns introduced themselves 40% of the time and stated their role 37% of the time (Table 2). Interns touched patients on 65% of visits, sat down with patients during 9% of visits, and asked open‐ended questions on 75% of visits. Interns performed all 5 of the behaviors during 4% of the total encounters. The percentage of the 5 behaviors performed by each intern during all observed visits ranged from 24% to 100%, with a mean of 51% (SD 17%) per intern.
| Total Encounters, N (%) | Introduced Self (%) | Introduced Role (%) | Touched Patient (%) | Sat Down (%) | Open‐Ended Question (%) | |
|---|---|---|---|---|---|---|
| ||||||
| Overall | 732 | 40 | 37 | 65 | 9 | 75 |
| JHH | 373 (51) | 35ab | 29ab | 62a | 10 | 70a |
| UMMC | 359 (49) | 45 | 44 | 69 | 8 | 81 |
| Male | 284 (39) | 39 | 35 | 64 | 9 | 74 |
| Female | 448 (61) | 41 | 38 | 67 | 10 | 76 |
| Day shift | 551 (75) | 37a | 34a | 65 | 9 | 77 |
| Night shift | 181 (25) | 48 | 45 | 67 | 12 | 71 |
| Admitting shift | 377 (52) | 46a | 42a | 63 | 10 | 75 |
| Nonadmitting shift | 355 (48) | 34 | 30 | 69 | 9 | 76 |
During night shifts as compared to day shifts, interns were more likely to introduce themselves (48% vs 37%, P=0.01) and their role (45% vs 34%, P<0.01). During shifts in which they admitted patients as compared to coverage shifts, interns were more likely to introduce themselves (46% vs 34%, P<0.01) and their role (42% vs 30%, P<0.01). Interns at UMMC as compared to JHH interns were more likely to introduce themselves (45% vs 35%, P<0.01) and describe their role to patients (44% vs 29%, P<0.01). Interns at UMMC were also more likely to ask open‐ended questions (81% vs 70%, P<0.01) and to touch patients (69% vs 62%, P=0.04). Performance of these behaviors did not vary significantly by gender, time of day, or shift. After adjustment for clustering at the observer and intern levels, differences by institution persisted in the rate of introducing oneself and one's role.
We performed a sensitivity analysis examining the first patient encounters of the day, and found that interns were somewhat more likely to introduce themselves (50% vs 40%, P=0.03) but were not significantly more likely to introduce their role, sit down, ask open‐ended questions, or touch the patient.
Nine of the 10 interns at JHH who participated in the study completed the survey (response rate=90%). Interns estimated introducing themselves and their role and sitting with patients significantly more frequently than was observed (80% vs 40%, P<0.01; 80% vs 37%, P<0.01; and 58% vs 9%, P<0.01, respectively) (Figure 1).
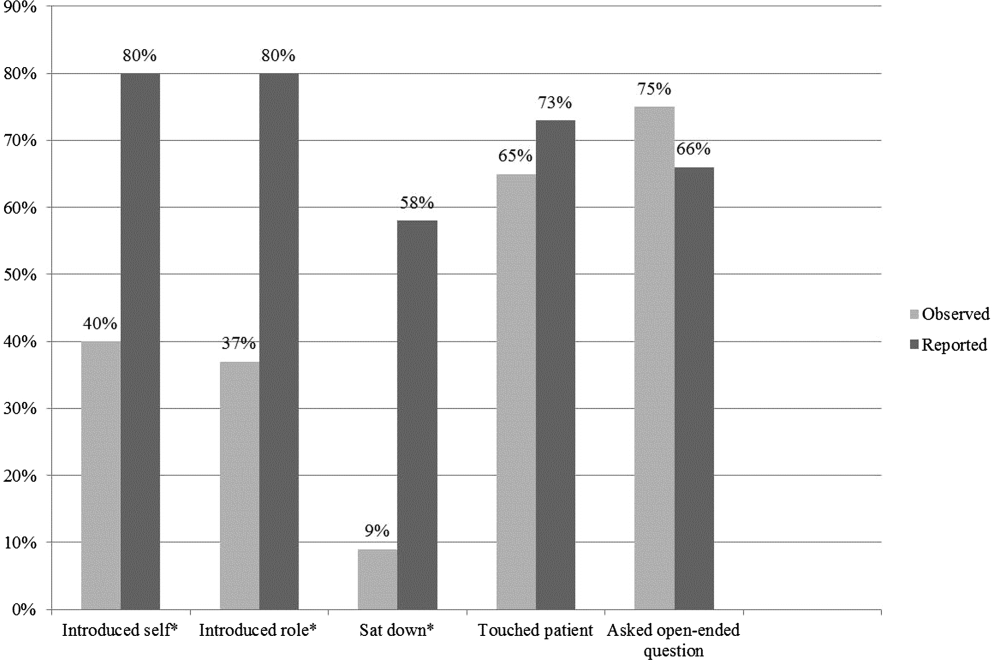
DISCUSSION
The interns we observed in 2 urban academic internal medicine residency programs did not routinely practice etiquette‐based communication. Interns surveyed tended to overestimate their performance of these behaviors. These behaviors are simple to perform and are each associated with improved patient experiences of hospital care. Tackett et al. recently demonstrated that interns are not alone. Hospitalist physicians do not universally practice etiquette‐based medicine, even though these behaviors correlate with patient satisfaction scores.[10]
Introducing oneself to patients may improve patient satisfaction and acceptance of trainee involvement in care.[6] However, only 10% of hospitalized patients in 1 study correctly identified a physician on their inpatient team, demonstrating the need for introductions during each and every inpatient encounter.[11] The interns we observed introduced themselves to patients in only 40% of encounters. During admitting shifts, when the first encounter with a patient likely took place, interns introduced themselves during 46% of encounters.
A comforting touch has been shown to reduce anxiety levels among patients and improve compliance with treatment regimens, but the interns did not touch patients in one‐third of visits, including during admitting shifts. Sixty‐six percent of patients consider a physician's touch comforting, and 58% believe it to be healing.[8]
A randomized trial found that most patients preferred a sitting physician, and believed that practitioners who sat were more compassionate and spent more time with them.[9] Unfortunately, interns sat down with patients in fewer than 10% of encounters.
We do not know why interns do not engage in these simple behaviors, but it is not surprising given that their role models, including hospitalist physicians, do not practice them universally.[10] Personality differences, medical school experiences, and hospital factors such as patient volume and complexity may explain variability in performance.
Importantly, we know that habits learned in residency tend to be retained when physicians enter independent practice.[12] If we want attending physicians to practice etiquette‐based communication, then it must be role modeled, taught, and evaluated during residency by clinical educators and hospitalist physicians. The gap between intern perceptions and actual practice of these behaviors provides a window of opportunity for education and feedback in bedside communication. Attending physicians rate communication skills as 1 of the top values they seek to pass on to house officers.[13] Curricula on communication skills improve physician attitudes and beliefs about the importance of good communication as well as long‐term performance of communication skills.[14]
Our study had several limitations. First, all 732 patient encounters were assessed, regardless of whether the intern had seen the patient previously. This differed slightly from Kahn's assertion that these behaviors be performed at least on the first encounter with the patient. We believe that the need for common courtesy does not diminish after the first visit, and although certain behaviors may not be indicated on 100% of visits, our sensitivity analysis indicated performance of these behaviors was not likely even on the first visit of the day.
Second, our observations were limited to medicine interns at 2 programs in Baltimore during a single month, limiting generalizability. A convenience sample of interns was chosen for recruitment based on rotation on a general medicine rotation during the study month. We observed interns over the course of several shifts and throughout various positions in the call cycle.
Third, in any observational study, the Hawthorne effect is a potential limitation. We attempted to limit this bias by collecting information anonymously and not indicating to the interns which aspects of the patient encounter were being recorded.
Fourth, we defined the behaviors broadly in an attempt to measure the outcomes conservatively and maximize inter‐rater reliability. For instance, we did not differentiate in data collection between comforting touch and physical examination. Because chairs may not be readily available in all patient rooms, we included sitting on the patient's bed or crouching next to the bed as sitting with the patient. Use of open‐ended questions was observed as a more general form of Kahn's recommendation to ask how the patient is feeling.
Fifth, our poststudy survey was conducted 6 months after the observations were performed, used an ordinal rather than continuous response scale, and was limited to only 1 of the 2 programs and 9 of the 29 participants. Given this small sample size, generalizability of the results is limited. Additionally, intern practice of etiquette‐based communication may have improved between the observations and survey that took place 6 months later.
As hospital admissions are a time of vulnerability for patients, physicians can take a basic etiquette‐based communication approach to comfort patients and help them feel more secure. We found that even though interns believed they were practicing Kahn's recommended etiquette‐based communication, only a minority actually were. Curricula on communication styles or environmental changes, such as providing chairs in patient rooms or photographs identifying members of the medical team, may encourage performance of these behaviors.[15]
Acknowledgments
The authors acknowledge Dr. Lisa Cooper, MD, MPH, and Dr. Mary Catherine Beach, MD, MPH, who provided tremendous help in editing. The authors also thank Kevin Wang, whose assistance with observer hiring, training, and management was essential.
Disclosures: The Osler Center for Clinical Excellence at Johns Hopkins and the Johns Hopkins Hospitalist Scholars Fund provided stipends for our observers as well as transportation and logistical costs of the study. The authors report no conflicts of interest.
- , , . Physician‐patient communication in the primary care office: a systematic review. J Am Board Fam Pract. 2002;15:25–38.
- , . Physicians' nonverbal rapport building and patients' talk about the subjective component of illness. Hum Commun Res. 2001;27:299–311.
- , , , , . Can 40 seconds of compassion reduce patient anxiety? J Clin Oncol. 1999;17:371–379.
- , , , . House staff nonverbal communication skills and patient satisfaction. J Gen Intern Med. 2003;18:170–174.
- . Etiquette‐based medicine. N Engl J Med. 2008;358:1988–1989.
- , , . Patient satisfaction associated with correct identification of physician's photographs. Mayo Clin Proc. 2001;76:604–608.
- . Effective physician‐patient communication and health outcomes: a review. CMAJ. 1995;152:1423–1433.
- , , , . Patients' attitudes to comforting touch in family practice. Can Fam Physician. 2000;46:2411–2416.
- , , , et al. Impact of physician sitting versus standing during inpatient oncology consultations: patients' preference and perception of compassion and duration. A randomized controlled trial. J Pain Symptom Manage. 2005;29:489–497.
- , , , , . Appraising the practice of etiquette‐based medicine in the inpatient setting. J Gen Intern Med. 2013;28(7):908–913.
- , , , , , . Ability of hospitalized patients to identify their in‐hospital physicians. Arch Intern Med. 2009;169:199–201.
- , , . The content of internal medicine residency training and its relevance to the practice of medicine. J Gen Intern Med. 1989;4:304–308.
- , . Which values to attending physicians try to pass on to house officers? Med Educ. 2001;35:941–945.
- , , , , , . Relationship of resident characteristics, attitudes, prior training, and clinical knowledge to communication skills performance. Med Educ. 2006;40:18–25.
- , , , . PHACES (Photographs of academic clinicians and their educational status): a tool to improve delivery of family‐centered care. Acad Pediatr. 2010;10:138–145.
Patient‐centered communication may impact several aspects of the patientdoctor relationship including patient disclosure of illness‐related information, patient satisfaction, anxiety, and compliance with medical recommendations.[1, 2, 3, 4] Etiquette‐based medicine, a term coined by Kahn, involves simple patient‐centered communication strategies that convey professionalism and respect to patients.[5] Studies have confirmed that patients prefer physicians who practice etiquette‐based medicine behaviors, including sitting down and introducing one's self.[6, 7, 8, 9] Performance of etiquette‐based medicine is associated with higher Press Ganey patient satisfaction scores. However, these easy‐to‐practice behaviors may not be modeled commonly in the inpatient setting.[10] We sought to understand whether etiquette‐based communication behaviors are practiced by trainees on inpatient medicine rotations.
METHODS
Design
This was a prospective study incorporating direct observation of intern interactions with patients during January 2012 at 2 internal medicine residency programs in Baltimore Maryland, Johns Hopkins Hospital (JHH) and the University of Maryland Medical Center (UMMC). We then surveyed participants from JHH in June 2012 to assess perceptions of their practice of etiquette‐based communication.
Participants and Setting
We observed a convenience sample of 29 internal medicine interns from the 2 institutions. We sought to observe interns over an equal number of hours at both sites and to sample shifts in proportion to the amount of time interns spend on each of these shifts. All interns who were asked to participate in the study agreed and comprised a total of 27% of the 108 interns in the 2 programs. The institutional review board at Johns Hopkins School of Medicine approved the study; the University of Maryland institutional review board deemed it not human subjects research. All observed interns provided informed consent to be observed during 1 to 4 inpatient shifts.
Observers
Twenty‐two undergraduate university students served as the observers for the study and were trained to collect data with the iPod Touch (Apple, Cupertino, CA) without interrupting patient care. We then tested the observers to ensure 85% concordance rate with the researchers in mock observation. Four hours of quality assurance were completed at both institutions during the study. Congruence between observer and research team member was >85% for each hour of observation.
Observation
Observers recorded intern activities on the iPod Touch spreadsheet application. The application allowed for real‐time data entry and direct export of results. The primary dependent variables for this study were 5 behaviors that were assessed each time an intern went into a patient's room. The 5 observed behaviors included (1) introducing one's self, (2) introducing one's role on the medical team, (3) touching the patient, (4) sitting down, and (5) asking the patient at least 1 open‐ended question. These behaviors were chosen for observation because they are central to Kahn's framework of etiquette‐based medicine, applicable to each inpatient encounter, and readily observed by trained nonmedical observers. These behaviors are defined in Table 1. Use of open‐ended questions was observed as a more general form of Kahn's recommendation to ask how the patient is feeling. Interns were not aware of which behaviors were being evaluated.
| Behavior | Definition |
|---|---|
| Introduced self | Providing a name |
| Introduced role | Uses term doctor, resident, intern, or medical team |
| Sat down | Sitting on the bed, in a chair, or crouching if no chair was available during at least part of the encounter |
| Touched the patient | Any form of physical contact that occurred at least once during the encounter including shaking a patient's hand, touching a patient on the shoulder, or performing any part of the physical exam |
| Asked open‐ended question | Asked the patient any question that required more than a yes/no answer |
Each time an observed intern entered a patient room, the observer recorded whether or not each of the 5 behaviors was performed, coded as a dichotomous variable. Although data collection was anonymous, observers recorded the team, hospital site, gender of the intern, and whether the intern was admitting new patients during the shift.
Survey
Following the observational portion of the study, participants at JHH completed a cross‐sectional, anonymous survey that asked them to estimate how frequently they currently performed each of the behaviors observed in this study. Response options included the following categories: <20%, 20% to 40%, 40% to 60%, 60% to 80%, or 80% to 100%.
Data Analysis
We determined the percent of patient visits during which each behavior was performed. Data were analyzed using Student t and [2] tests evaluating differences by hospital, intern gender, type of shift, and time of day. To account for correlation within subjects and observers, we performed multilevel logistic regression analysis adjusted for clustering at the intern and observer levels. For the survey analysis, the mean of the response category was used as the basis for comparison. All quantitative analyses were performed in Excel 2010 (Microsoft Corp., Redmond, WA) and Stata/IC version 11 (StataCorp, College Station, TX).
RESULTS
A total of 732 inpatient encounters were observed during 118 intern shifts. Interns were observed for a mean of 25 patient encounters each (range, 361; standard deviation [SD] 17). Overall, interns introduced themselves 40% of the time and stated their role 37% of the time (Table 2). Interns touched patients on 65% of visits, sat down with patients during 9% of visits, and asked open‐ended questions on 75% of visits. Interns performed all 5 of the behaviors during 4% of the total encounters. The percentage of the 5 behaviors performed by each intern during all observed visits ranged from 24% to 100%, with a mean of 51% (SD 17%) per intern.
| Total Encounters, N (%) | Introduced Self (%) | Introduced Role (%) | Touched Patient (%) | Sat Down (%) | Open‐Ended Question (%) | |
|---|---|---|---|---|---|---|
| ||||||
| Overall | 732 | 40 | 37 | 65 | 9 | 75 |
| JHH | 373 (51) | 35ab | 29ab | 62a | 10 | 70a |
| UMMC | 359 (49) | 45 | 44 | 69 | 8 | 81 |
| Male | 284 (39) | 39 | 35 | 64 | 9 | 74 |
| Female | 448 (61) | 41 | 38 | 67 | 10 | 76 |
| Day shift | 551 (75) | 37a | 34a | 65 | 9 | 77 |
| Night shift | 181 (25) | 48 | 45 | 67 | 12 | 71 |
| Admitting shift | 377 (52) | 46a | 42a | 63 | 10 | 75 |
| Nonadmitting shift | 355 (48) | 34 | 30 | 69 | 9 | 76 |
During night shifts as compared to day shifts, interns were more likely to introduce themselves (48% vs 37%, P=0.01) and their role (45% vs 34%, P<0.01). During shifts in which they admitted patients as compared to coverage shifts, interns were more likely to introduce themselves (46% vs 34%, P<0.01) and their role (42% vs 30%, P<0.01). Interns at UMMC as compared to JHH interns were more likely to introduce themselves (45% vs 35%, P<0.01) and describe their role to patients (44% vs 29%, P<0.01). Interns at UMMC were also more likely to ask open‐ended questions (81% vs 70%, P<0.01) and to touch patients (69% vs 62%, P=0.04). Performance of these behaviors did not vary significantly by gender, time of day, or shift. After adjustment for clustering at the observer and intern levels, differences by institution persisted in the rate of introducing oneself and one's role.
We performed a sensitivity analysis examining the first patient encounters of the day, and found that interns were somewhat more likely to introduce themselves (50% vs 40%, P=0.03) but were not significantly more likely to introduce their role, sit down, ask open‐ended questions, or touch the patient.
Nine of the 10 interns at JHH who participated in the study completed the survey (response rate=90%). Interns estimated introducing themselves and their role and sitting with patients significantly more frequently than was observed (80% vs 40%, P<0.01; 80% vs 37%, P<0.01; and 58% vs 9%, P<0.01, respectively) (Figure 1).
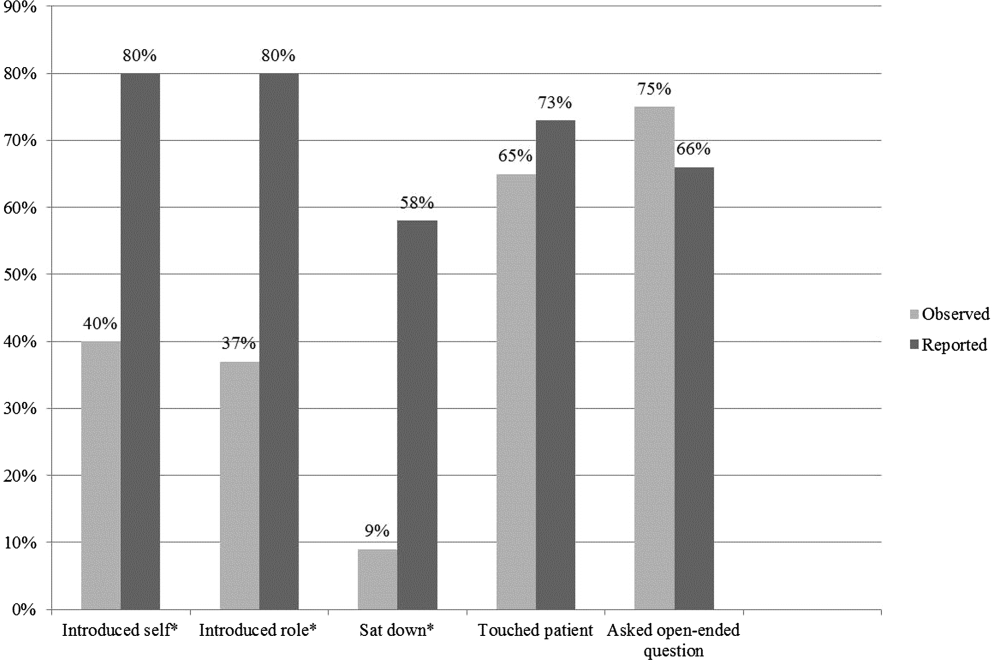
DISCUSSION
The interns we observed in 2 urban academic internal medicine residency programs did not routinely practice etiquette‐based communication. Interns surveyed tended to overestimate their performance of these behaviors. These behaviors are simple to perform and are each associated with improved patient experiences of hospital care. Tackett et al. recently demonstrated that interns are not alone. Hospitalist physicians do not universally practice etiquette‐based medicine, even though these behaviors correlate with patient satisfaction scores.[10]
Introducing oneself to patients may improve patient satisfaction and acceptance of trainee involvement in care.[6] However, only 10% of hospitalized patients in 1 study correctly identified a physician on their inpatient team, demonstrating the need for introductions during each and every inpatient encounter.[11] The interns we observed introduced themselves to patients in only 40% of encounters. During admitting shifts, when the first encounter with a patient likely took place, interns introduced themselves during 46% of encounters.
A comforting touch has been shown to reduce anxiety levels among patients and improve compliance with treatment regimens, but the interns did not touch patients in one‐third of visits, including during admitting shifts. Sixty‐six percent of patients consider a physician's touch comforting, and 58% believe it to be healing.[8]
A randomized trial found that most patients preferred a sitting physician, and believed that practitioners who sat were more compassionate and spent more time with them.[9] Unfortunately, interns sat down with patients in fewer than 10% of encounters.
We do not know why interns do not engage in these simple behaviors, but it is not surprising given that their role models, including hospitalist physicians, do not practice them universally.[10] Personality differences, medical school experiences, and hospital factors such as patient volume and complexity may explain variability in performance.
Importantly, we know that habits learned in residency tend to be retained when physicians enter independent practice.[12] If we want attending physicians to practice etiquette‐based communication, then it must be role modeled, taught, and evaluated during residency by clinical educators and hospitalist physicians. The gap between intern perceptions and actual practice of these behaviors provides a window of opportunity for education and feedback in bedside communication. Attending physicians rate communication skills as 1 of the top values they seek to pass on to house officers.[13] Curricula on communication skills improve physician attitudes and beliefs about the importance of good communication as well as long‐term performance of communication skills.[14]
Our study had several limitations. First, all 732 patient encounters were assessed, regardless of whether the intern had seen the patient previously. This differed slightly from Kahn's assertion that these behaviors be performed at least on the first encounter with the patient. We believe that the need for common courtesy does not diminish after the first visit, and although certain behaviors may not be indicated on 100% of visits, our sensitivity analysis indicated performance of these behaviors was not likely even on the first visit of the day.
Second, our observations were limited to medicine interns at 2 programs in Baltimore during a single month, limiting generalizability. A convenience sample of interns was chosen for recruitment based on rotation on a general medicine rotation during the study month. We observed interns over the course of several shifts and throughout various positions in the call cycle.
Third, in any observational study, the Hawthorne effect is a potential limitation. We attempted to limit this bias by collecting information anonymously and not indicating to the interns which aspects of the patient encounter were being recorded.
Fourth, we defined the behaviors broadly in an attempt to measure the outcomes conservatively and maximize inter‐rater reliability. For instance, we did not differentiate in data collection between comforting touch and physical examination. Because chairs may not be readily available in all patient rooms, we included sitting on the patient's bed or crouching next to the bed as sitting with the patient. Use of open‐ended questions was observed as a more general form of Kahn's recommendation to ask how the patient is feeling.
Fifth, our poststudy survey was conducted 6 months after the observations were performed, used an ordinal rather than continuous response scale, and was limited to only 1 of the 2 programs and 9 of the 29 participants. Given this small sample size, generalizability of the results is limited. Additionally, intern practice of etiquette‐based communication may have improved between the observations and survey that took place 6 months later.
As hospital admissions are a time of vulnerability for patients, physicians can take a basic etiquette‐based communication approach to comfort patients and help them feel more secure. We found that even though interns believed they were practicing Kahn's recommended etiquette‐based communication, only a minority actually were. Curricula on communication styles or environmental changes, such as providing chairs in patient rooms or photographs identifying members of the medical team, may encourage performance of these behaviors.[15]
Acknowledgments
The authors acknowledge Dr. Lisa Cooper, MD, MPH, and Dr. Mary Catherine Beach, MD, MPH, who provided tremendous help in editing. The authors also thank Kevin Wang, whose assistance with observer hiring, training, and management was essential.
Disclosures: The Osler Center for Clinical Excellence at Johns Hopkins and the Johns Hopkins Hospitalist Scholars Fund provided stipends for our observers as well as transportation and logistical costs of the study. The authors report no conflicts of interest.
Patient‐centered communication may impact several aspects of the patientdoctor relationship including patient disclosure of illness‐related information, patient satisfaction, anxiety, and compliance with medical recommendations.[1, 2, 3, 4] Etiquette‐based medicine, a term coined by Kahn, involves simple patient‐centered communication strategies that convey professionalism and respect to patients.[5] Studies have confirmed that patients prefer physicians who practice etiquette‐based medicine behaviors, including sitting down and introducing one's self.[6, 7, 8, 9] Performance of etiquette‐based medicine is associated with higher Press Ganey patient satisfaction scores. However, these easy‐to‐practice behaviors may not be modeled commonly in the inpatient setting.[10] We sought to understand whether etiquette‐based communication behaviors are practiced by trainees on inpatient medicine rotations.
METHODS
Design
This was a prospective study incorporating direct observation of intern interactions with patients during January 2012 at 2 internal medicine residency programs in Baltimore Maryland, Johns Hopkins Hospital (JHH) and the University of Maryland Medical Center (UMMC). We then surveyed participants from JHH in June 2012 to assess perceptions of their practice of etiquette‐based communication.
Participants and Setting
We observed a convenience sample of 29 internal medicine interns from the 2 institutions. We sought to observe interns over an equal number of hours at both sites and to sample shifts in proportion to the amount of time interns spend on each of these shifts. All interns who were asked to participate in the study agreed and comprised a total of 27% of the 108 interns in the 2 programs. The institutional review board at Johns Hopkins School of Medicine approved the study; the University of Maryland institutional review board deemed it not human subjects research. All observed interns provided informed consent to be observed during 1 to 4 inpatient shifts.
Observers
Twenty‐two undergraduate university students served as the observers for the study and were trained to collect data with the iPod Touch (Apple, Cupertino, CA) without interrupting patient care. We then tested the observers to ensure 85% concordance rate with the researchers in mock observation. Four hours of quality assurance were completed at both institutions during the study. Congruence between observer and research team member was >85% for each hour of observation.
Observation
Observers recorded intern activities on the iPod Touch spreadsheet application. The application allowed for real‐time data entry and direct export of results. The primary dependent variables for this study were 5 behaviors that were assessed each time an intern went into a patient's room. The 5 observed behaviors included (1) introducing one's self, (2) introducing one's role on the medical team, (3) touching the patient, (4) sitting down, and (5) asking the patient at least 1 open‐ended question. These behaviors were chosen for observation because they are central to Kahn's framework of etiquette‐based medicine, applicable to each inpatient encounter, and readily observed by trained nonmedical observers. These behaviors are defined in Table 1. Use of open‐ended questions was observed as a more general form of Kahn's recommendation to ask how the patient is feeling. Interns were not aware of which behaviors were being evaluated.
| Behavior | Definition |
|---|---|
| Introduced self | Providing a name |
| Introduced role | Uses term doctor, resident, intern, or medical team |
| Sat down | Sitting on the bed, in a chair, or crouching if no chair was available during at least part of the encounter |
| Touched the patient | Any form of physical contact that occurred at least once during the encounter including shaking a patient's hand, touching a patient on the shoulder, or performing any part of the physical exam |
| Asked open‐ended question | Asked the patient any question that required more than a yes/no answer |
Each time an observed intern entered a patient room, the observer recorded whether or not each of the 5 behaviors was performed, coded as a dichotomous variable. Although data collection was anonymous, observers recorded the team, hospital site, gender of the intern, and whether the intern was admitting new patients during the shift.
Survey
Following the observational portion of the study, participants at JHH completed a cross‐sectional, anonymous survey that asked them to estimate how frequently they currently performed each of the behaviors observed in this study. Response options included the following categories: <20%, 20% to 40%, 40% to 60%, 60% to 80%, or 80% to 100%.
Data Analysis
We determined the percent of patient visits during which each behavior was performed. Data were analyzed using Student t and [2] tests evaluating differences by hospital, intern gender, type of shift, and time of day. To account for correlation within subjects and observers, we performed multilevel logistic regression analysis adjusted for clustering at the intern and observer levels. For the survey analysis, the mean of the response category was used as the basis for comparison. All quantitative analyses were performed in Excel 2010 (Microsoft Corp., Redmond, WA) and Stata/IC version 11 (StataCorp, College Station, TX).
RESULTS
A total of 732 inpatient encounters were observed during 118 intern shifts. Interns were observed for a mean of 25 patient encounters each (range, 361; standard deviation [SD] 17). Overall, interns introduced themselves 40% of the time and stated their role 37% of the time (Table 2). Interns touched patients on 65% of visits, sat down with patients during 9% of visits, and asked open‐ended questions on 75% of visits. Interns performed all 5 of the behaviors during 4% of the total encounters. The percentage of the 5 behaviors performed by each intern during all observed visits ranged from 24% to 100%, with a mean of 51% (SD 17%) per intern.
| Total Encounters, N (%) | Introduced Self (%) | Introduced Role (%) | Touched Patient (%) | Sat Down (%) | Open‐Ended Question (%) | |
|---|---|---|---|---|---|---|
| ||||||
| Overall | 732 | 40 | 37 | 65 | 9 | 75 |
| JHH | 373 (51) | 35ab | 29ab | 62a | 10 | 70a |
| UMMC | 359 (49) | 45 | 44 | 69 | 8 | 81 |
| Male | 284 (39) | 39 | 35 | 64 | 9 | 74 |
| Female | 448 (61) | 41 | 38 | 67 | 10 | 76 |
| Day shift | 551 (75) | 37a | 34a | 65 | 9 | 77 |
| Night shift | 181 (25) | 48 | 45 | 67 | 12 | 71 |
| Admitting shift | 377 (52) | 46a | 42a | 63 | 10 | 75 |
| Nonadmitting shift | 355 (48) | 34 | 30 | 69 | 9 | 76 |
During night shifts as compared to day shifts, interns were more likely to introduce themselves (48% vs 37%, P=0.01) and their role (45% vs 34%, P<0.01). During shifts in which they admitted patients as compared to coverage shifts, interns were more likely to introduce themselves (46% vs 34%, P<0.01) and their role (42% vs 30%, P<0.01). Interns at UMMC as compared to JHH interns were more likely to introduce themselves (45% vs 35%, P<0.01) and describe their role to patients (44% vs 29%, P<0.01). Interns at UMMC were also more likely to ask open‐ended questions (81% vs 70%, P<0.01) and to touch patients (69% vs 62%, P=0.04). Performance of these behaviors did not vary significantly by gender, time of day, or shift. After adjustment for clustering at the observer and intern levels, differences by institution persisted in the rate of introducing oneself and one's role.
We performed a sensitivity analysis examining the first patient encounters of the day, and found that interns were somewhat more likely to introduce themselves (50% vs 40%, P=0.03) but were not significantly more likely to introduce their role, sit down, ask open‐ended questions, or touch the patient.
Nine of the 10 interns at JHH who participated in the study completed the survey (response rate=90%). Interns estimated introducing themselves and their role and sitting with patients significantly more frequently than was observed (80% vs 40%, P<0.01; 80% vs 37%, P<0.01; and 58% vs 9%, P<0.01, respectively) (Figure 1).
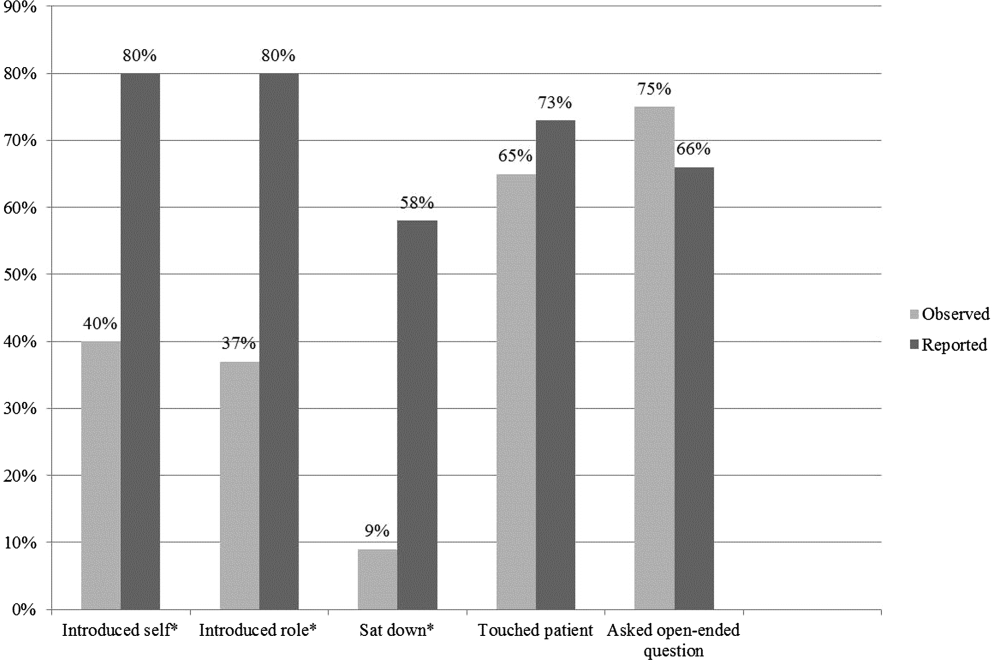
DISCUSSION
The interns we observed in 2 urban academic internal medicine residency programs did not routinely practice etiquette‐based communication. Interns surveyed tended to overestimate their performance of these behaviors. These behaviors are simple to perform and are each associated with improved patient experiences of hospital care. Tackett et al. recently demonstrated that interns are not alone. Hospitalist physicians do not universally practice etiquette‐based medicine, even though these behaviors correlate with patient satisfaction scores.[10]
Introducing oneself to patients may improve patient satisfaction and acceptance of trainee involvement in care.[6] However, only 10% of hospitalized patients in 1 study correctly identified a physician on their inpatient team, demonstrating the need for introductions during each and every inpatient encounter.[11] The interns we observed introduced themselves to patients in only 40% of encounters. During admitting shifts, when the first encounter with a patient likely took place, interns introduced themselves during 46% of encounters.
A comforting touch has been shown to reduce anxiety levels among patients and improve compliance with treatment regimens, but the interns did not touch patients in one‐third of visits, including during admitting shifts. Sixty‐six percent of patients consider a physician's touch comforting, and 58% believe it to be healing.[8]
A randomized trial found that most patients preferred a sitting physician, and believed that practitioners who sat were more compassionate and spent more time with them.[9] Unfortunately, interns sat down with patients in fewer than 10% of encounters.
We do not know why interns do not engage in these simple behaviors, but it is not surprising given that their role models, including hospitalist physicians, do not practice them universally.[10] Personality differences, medical school experiences, and hospital factors such as patient volume and complexity may explain variability in performance.
Importantly, we know that habits learned in residency tend to be retained when physicians enter independent practice.[12] If we want attending physicians to practice etiquette‐based communication, then it must be role modeled, taught, and evaluated during residency by clinical educators and hospitalist physicians. The gap between intern perceptions and actual practice of these behaviors provides a window of opportunity for education and feedback in bedside communication. Attending physicians rate communication skills as 1 of the top values they seek to pass on to house officers.[13] Curricula on communication skills improve physician attitudes and beliefs about the importance of good communication as well as long‐term performance of communication skills.[14]
Our study had several limitations. First, all 732 patient encounters were assessed, regardless of whether the intern had seen the patient previously. This differed slightly from Kahn's assertion that these behaviors be performed at least on the first encounter with the patient. We believe that the need for common courtesy does not diminish after the first visit, and although certain behaviors may not be indicated on 100% of visits, our sensitivity analysis indicated performance of these behaviors was not likely even on the first visit of the day.
Second, our observations were limited to medicine interns at 2 programs in Baltimore during a single month, limiting generalizability. A convenience sample of interns was chosen for recruitment based on rotation on a general medicine rotation during the study month. We observed interns over the course of several shifts and throughout various positions in the call cycle.
Third, in any observational study, the Hawthorne effect is a potential limitation. We attempted to limit this bias by collecting information anonymously and not indicating to the interns which aspects of the patient encounter were being recorded.
Fourth, we defined the behaviors broadly in an attempt to measure the outcomes conservatively and maximize inter‐rater reliability. For instance, we did not differentiate in data collection between comforting touch and physical examination. Because chairs may not be readily available in all patient rooms, we included sitting on the patient's bed or crouching next to the bed as sitting with the patient. Use of open‐ended questions was observed as a more general form of Kahn's recommendation to ask how the patient is feeling.
Fifth, our poststudy survey was conducted 6 months after the observations were performed, used an ordinal rather than continuous response scale, and was limited to only 1 of the 2 programs and 9 of the 29 participants. Given this small sample size, generalizability of the results is limited. Additionally, intern practice of etiquette‐based communication may have improved between the observations and survey that took place 6 months later.
As hospital admissions are a time of vulnerability for patients, physicians can take a basic etiquette‐based communication approach to comfort patients and help them feel more secure. We found that even though interns believed they were practicing Kahn's recommended etiquette‐based communication, only a minority actually were. Curricula on communication styles or environmental changes, such as providing chairs in patient rooms or photographs identifying members of the medical team, may encourage performance of these behaviors.[15]
Acknowledgments
The authors acknowledge Dr. Lisa Cooper, MD, MPH, and Dr. Mary Catherine Beach, MD, MPH, who provided tremendous help in editing. The authors also thank Kevin Wang, whose assistance with observer hiring, training, and management was essential.
Disclosures: The Osler Center for Clinical Excellence at Johns Hopkins and the Johns Hopkins Hospitalist Scholars Fund provided stipends for our observers as well as transportation and logistical costs of the study. The authors report no conflicts of interest.
- , , . Physician‐patient communication in the primary care office: a systematic review. J Am Board Fam Pract. 2002;15:25–38.
- , . Physicians' nonverbal rapport building and patients' talk about the subjective component of illness. Hum Commun Res. 2001;27:299–311.
- , , , , . Can 40 seconds of compassion reduce patient anxiety? J Clin Oncol. 1999;17:371–379.
- , , , . House staff nonverbal communication skills and patient satisfaction. J Gen Intern Med. 2003;18:170–174.
- . Etiquette‐based medicine. N Engl J Med. 2008;358:1988–1989.
- , , . Patient satisfaction associated with correct identification of physician's photographs. Mayo Clin Proc. 2001;76:604–608.
- . Effective physician‐patient communication and health outcomes: a review. CMAJ. 1995;152:1423–1433.
- , , , . Patients' attitudes to comforting touch in family practice. Can Fam Physician. 2000;46:2411–2416.
- , , , et al. Impact of physician sitting versus standing during inpatient oncology consultations: patients' preference and perception of compassion and duration. A randomized controlled trial. J Pain Symptom Manage. 2005;29:489–497.
- , , , , . Appraising the practice of etiquette‐based medicine in the inpatient setting. J Gen Intern Med. 2013;28(7):908–913.
- , , , , , . Ability of hospitalized patients to identify their in‐hospital physicians. Arch Intern Med. 2009;169:199–201.
- , , . The content of internal medicine residency training and its relevance to the practice of medicine. J Gen Intern Med. 1989;4:304–308.
- , . Which values to attending physicians try to pass on to house officers? Med Educ. 2001;35:941–945.
- , , , , , . Relationship of resident characteristics, attitudes, prior training, and clinical knowledge to communication skills performance. Med Educ. 2006;40:18–25.
- , , , . PHACES (Photographs of academic clinicians and their educational status): a tool to improve delivery of family‐centered care. Acad Pediatr. 2010;10:138–145.
- , , . Physician‐patient communication in the primary care office: a systematic review. J Am Board Fam Pract. 2002;15:25–38.
- , . Physicians' nonverbal rapport building and patients' talk about the subjective component of illness. Hum Commun Res. 2001;27:299–311.
- , , , , . Can 40 seconds of compassion reduce patient anxiety? J Clin Oncol. 1999;17:371–379.
- , , , . House staff nonverbal communication skills and patient satisfaction. J Gen Intern Med. 2003;18:170–174.
- . Etiquette‐based medicine. N Engl J Med. 2008;358:1988–1989.
- , , . Patient satisfaction associated with correct identification of physician's photographs. Mayo Clin Proc. 2001;76:604–608.
- . Effective physician‐patient communication and health outcomes: a review. CMAJ. 1995;152:1423–1433.
- , , , . Patients' attitudes to comforting touch in family practice. Can Fam Physician. 2000;46:2411–2416.
- , , , et al. Impact of physician sitting versus standing during inpatient oncology consultations: patients' preference and perception of compassion and duration. A randomized controlled trial. J Pain Symptom Manage. 2005;29:489–497.
- , , , , . Appraising the practice of etiquette‐based medicine in the inpatient setting. J Gen Intern Med. 2013;28(7):908–913.
- , , , , , . Ability of hospitalized patients to identify their in‐hospital physicians. Arch Intern Med. 2009;169:199–201.
- , , . The content of internal medicine residency training and its relevance to the practice of medicine. J Gen Intern Med. 1989;4:304–308.
- , . Which values to attending physicians try to pass on to house officers? Med Educ. 2001;35:941–945.
- , , , , , . Relationship of resident characteristics, attitudes, prior training, and clinical knowledge to communication skills performance. Med Educ. 2006;40:18–25.
- , , , . PHACES (Photographs of academic clinicians and their educational status): a tool to improve delivery of family‐centered care. Acad Pediatr. 2010;10:138–145.