User login
Geriatric Train‐The‐Trainer Program
Nearly half of the hospital beds in the United States are occupied by the elderly,1 whose numbers are increasing.2 The odds of a hospitalized Medicare patient being cared for by a hospitalist are increasing by nearly 30% per year.3 Hospitalists require competence in geriatrics to serve their patients and to teach trainees. Train‐the‐Trainer (TTT) programs both educate health care providers and provide educational materials, information, and skills for teaching others.4 This model has been successfully used in geriatrics to impact knowledge, attitudes, and self‐efficacy among health care workers.46
A prominent example of a geriatrics TTT program is the University of Chicago Curriculum for the Hospitalized Aging Medical Patient (CHAMP),7 which requires 48 hours of instruction over 12 sessions. To create a less time‐intensive learning format for busy hospitalists, the University of Chicago developed Mini‐CHAMP, a streamlined 2‐day workshop with web‐based components for hospitalist clinicians, but not necessarily hospitalist educators.7
We created The Donald W. Reynolds Program for Advancing Geriatrics Education (PAGE) at the University of California, San Francisco (UCSF), in light of the time intensity of CHAMP, to integrate geriatric TTT sessions within preexisting hospitalist faculty meetings. This model is consistent with current practices in faculty development.8 This paper describes the evaluation of the PAGE Model, which sought answers to 3 research questions: (1) Does PAGE increase faculty confidence in teaching geriatrics?, (2) Does PAGE increase the frequency of hospitalist teaching geriatrics topics?, and (3) Does PAGE increase residents' practice of geriatrics skills?
Methods
The PAGE Model
The PAGE Model comprises 10 hour‐long monthly seminars held at UCSF from January through December 2008 to teach specific geriatrics principles and clinical skills relevant to providing competent care to a hospitalized older adult. The aims of the PAGE are to:
Give hospitalist physicians knowledge and skills to teach geriatric topics to trainees in a time‐limited environment
Provide exportable teaching modules on geriatric topics for inpatient teaching
Increase teaching about geriatrics received by internal medicine residents
Increase resident use of 15 specific geriatric skills
Create a collaborative environment between the Geriatrics and Hospital Medicine Divisions at UCSF
The PAGE Development Group, which included 2 hospitalists, 2 geriatricians, and an analyst funded by the Donald W. Reynolds Foundation, reviewed American Geriatrics Society core competencies,9 national guidelines and mandates,10, 11 and existing published geriatric curricula.7, 1214 In late 2007, an email‐based needs assessment listing 38 possible topics, drawn from the resources above, was emailed to the 31 hospitalists at UCSF. Each hospitalist identified, in no particular order, 5 topics considered most useful to improve his/her geriatric teaching skills, with write‐in space for additional topic suggestions. The needs assessment also queried what format of teaching tools would be most useful and efficient, such as PowerPoint slides or pocket cards, and interest in session coteaching.
The topics most commonly selected by the respondents (n = 14, response rate 45%) included: home/community resources (64%), delirium/dementia (57%), minimizing medication problems (50%), using prognostic indices to make decisions (43%), and general approach to older inpatients (43%). The Development Group identified less popular topics (falls, pressure ulcers, indwelling catheters/emncontinence) that were gaining significant national attention.15 Finally, a topic suggested by many hospitalists, pain management, was added. Each topic session was mapped to 1 or more of the 15 geriatrics skills in the CHAMP model7 for residents to acquire. The requested and selected topics were then modified to create distinct sessions grouped around a theme, shown in Table 1. For example home and community resources was addressed in the session on Framework on Transitions in Care.
| Topics | Geriatric Skills Addressed for Hospitalized Older Patients |
|---|---|
| |
| 1. Approach to the vulnerable older patient; assessing function; goals of care | Conduct functional status assessmentMobilize early to prevent deconditioning |
| 2. Minimizing medication problems | Reduce polypharmacy and use of high risk/low benefit drugs |
| 3. Framework for transitions in care (including home and community resources) | Develop a safe and appropriate discharge plan, involving communication with other team members, family members and primary care physicians |
| 4. Using prognostics to guide treatment decisions | Give bad news |
| Document advance directives and DNR orders | |
| Discuss hospice care | |
| 5. Falls & immobility | Identify risk factors of hospital falls, including conventional and unconventional types of restraints |
| 6. Delirium | Assess risk and prevent delirium |
| 7. Dementia & depression | Conduct cognitive assessmentScreen for depression |
| Routinely assess pain at bedside in persons with dementia | |
| 8. Pain assessment in the elderly | Routinely assess pain at bedside in persons with dementia |
| Manage pain using the WHO 3‐step ladder and opiate conversion table and manage side effects of opiates | |
| 9. Foley catheters and incontinence | Determine appropriateness for urinary catheter use, discontinuing when inappropriate |
| 10. Pressure ulcers and wound care | Routinely perform a complete skin exam |
Most respondents (86%) wanted teaching materials in a format suitable for attending rounds; 64% preferred teaching cases, 29% PowerPoint presentations, and 29% quality improvement resources. The Development Group, with approval of the Chief of Hospital Medicine, planned 10, 1‐hour monthly sessions during weekly hospitalist meetings to optimize participation. Nine hospitalists agreed to lead sessions with geriatricians; 1 session was co‐led by a hospitalist and urologist.
The Development Group encouraged session leaders to create case‐based PowerPoint teaching modules that could be used during attending rounds, highlighting teaching triggers or teachable moments that modify or reinforce skills.1618 A Development Group hospitalist/geriatrician team cotaught the first session, which modeled the structure and style recommended. A teaching team typically met at least once to define goals and outline their teaching hour; most met repeatedly to refine their presentations. An example of a 1 PAGE session can be found online.19
Evaluation
Evaluation involved data from hospitalist faculty trainees, hospitalist and geriatrician session leaders, and internal medicine residents. The institutional review board approved this study. Self‐report rating scales were used for data collection, which were reviewed by experts in medical education at UCSF and piloted on nonparticipant faculty, or had been previously used by the CHAMP study.7
Hospitalist Trainees' Program Perceptions and Self‐Efficacy
Hospitalist trainees (n = 36) completed paper questionnaires after each session to assess perceived likelihood to use the teaching tools that were presented (1: not at all likely, 5: highly likely), whether they would recommend the program to colleagues (1: do not recommend, 5: highly recommend), and the utility of the PAGE program (Was this experience useful? and Prior to the sessions, did you think it would be useful? 1: definitely not, 5: definitely yes). Change in trainees' perceived self‐efficacy20 to teach geriatrics skills was assessed at the end of the PAGE program, using a posttest and retrospective pretest format with a 12‐items (1: low, 5: high) that was used in the CHAMP study.7 This format was used to avoid response shift bias, or the program‐produced change in a participant's understanding of the construct being measured.21
Faculty Session Leaders' Program Perceptions
After PAGE completion, all faculty session leaders (n = 15) completed an online questionnaire assessing teaching satisfaction (Likert‐type 5‐point scales), experience with coteaching, and years of faculty teaching experience.
Medical Residents
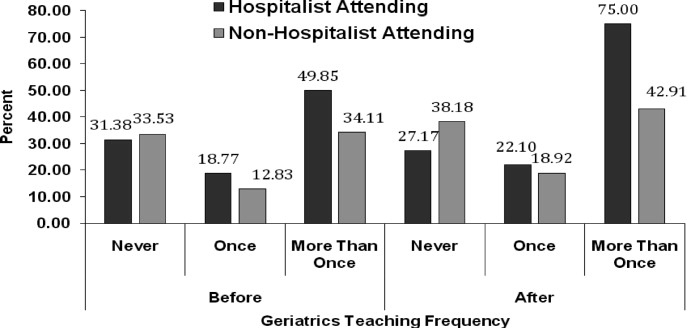
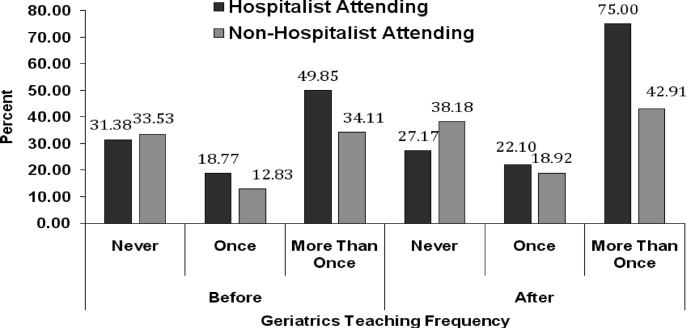
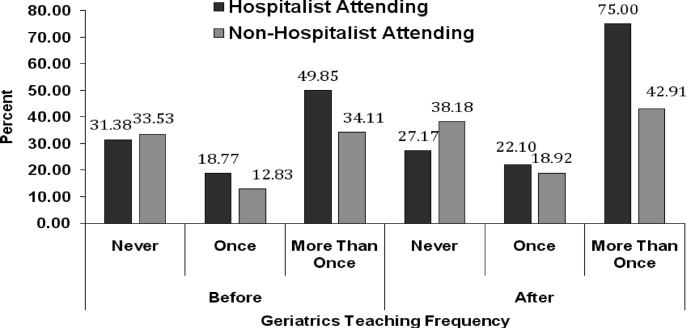
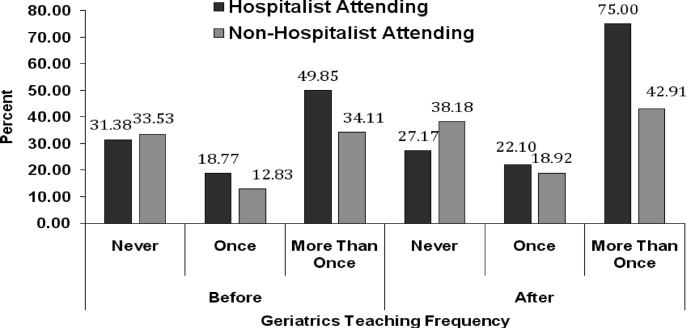
To assess change in hospitalists' teaching about geriatrics and residents' practice of geriatric clinical skills, residents (n = 56; post‐graduate year (PGY)1 = 29, PGY2 = 27) who would not complete residency before the end of PAGE received an online questionnaire, modified from the CHAMP study,7 prior to and after the completion of PAGE. Respondents received monetary gift cards as incentives. Residents gave separate ratings for their inpatient teaching attendings who were hospitalists (80% of inpatient ward attendings) and nonhospitalists (20%, mostly generalists) regarding frequency over the past year of being taught each of 15 geriatric clinical skills. A 3‐point scale was used: (1) never, (2) once, and (3) more than once. Residents also reported the frequency of practicing those skills themselves, using a questionnaire from the CHAMP study,7 with a scale of (1) never to (5) always.
Analysis
Descriptive statistics were computed for all measures. Scale means were constructed from all individual items for the retrospective pretest and posttest measures. Wilcoxon matched‐pairs signed ranks‐tests were used to compare teaching differences between hospitalist and other attendings. For the unmatched pre‐post data on frequency of teaching, Wilcoxon‐Mann‐Whitney tests were used to determine significant differences in instruction, conducting separate tests for hospitalists and nonhospitalist attendings. Effect size22 was calculated using Cohen's d23 to determine the magnitude of increase in self‐efficacy to teach geriatrics; an effect size exceeding 0.8 is considered large. Statistics were performed using PASW Statistics 17.0 (SPSS Inc., Chicago, IL, USA).
Results
The hospitalist group grew from 31 to 36 members in June of 2008. On average, 14 hospitalists (M = 14.40, standard deviation [SD] = 2.41, range 1119) attended each session, with all hospitalists (n = 36) attending 1 session (M = 3.83, SD = 2.35, range 19). At each session, an average of 72% completed a post‐session evaluation form. Overall, faculty were likely to use the PAGE teaching tools (M = 4.61, SD = 0.53) and would recommend PAGE to other hospitalists (M = 4.63, SD = 0.51).
Thirteen hospitalist trainees of 36 (36%) completed a post‐PAGE online questionnaire. Respondents taught on faculty for an average of 5 years (mean (M) = 5.08, SD = 3.52). Faculty perceived self‐efficacy at teaching residents about geriatrics improved significantly with a large effect size (pretest M = 3.05, SD = .60; posttest M = 3.96, SD = .36, d = 1.52; P < 0.001). Session attendance was positively correlated with the increase in geriatrics teaching self‐efficacy (r = .62, P < 0.05), while teaching experience was not (r = 0.05, P = 0.88). Hospitalist trainees found the PAGE model more useful after participating (M = 4.62, SD = 0.65), than they had expected (M = 3.92, SD = 0.76; P < 0.05).
All session leaders (n = 15) completed the questionnaire after PAGE (9 hospitalists, 5 geriatricians, 1 urologist). Two‐thirds had 5 years on faculty; eight had no prior experience as a faculty development trainer. Over 80% indicated that they found their coteaching experience, enjoyable, useful and collaborative. Only 1 participant did not commit to interdisciplinary teaching again. Most hospitalist session leaders reported that coteaching with a geriatrician enhanced their knowledge; they were more likely to consult a geriatrician regarding patients. All but 2 session leaders felt that the model fostered a collaborative environment between their 2 divisions.
Of the 56 residents, 41% (16 PGY1, 7 PGY2) completed a pretest; 43% (15 PGY1, 9 PGY2) completed a posttest. Residents reported receiving inpatient teaching on geriatrics skills significantly more frequently from hospitalists vs. nonhospitalist attendings both before PAGE (hospitalists M = 2.18, SD = 0.37; nonhospitalists M = 2.00, SD = 0.53, P < 0.05), and after (hospitalists M = 2.39, SD = 0.46; nonhospitalists M = 2.05, SD = 0.57, P < 0.05; see Fig. 1). Although hospitalists taught more frequently about geriatrics than nonhospitalists before PAGE, our findings suggest that they increased their teaching by a greater magnitude than nonhospitalists (P < 0.01, P > 0.05, respectively). Residents reported increased geriatric skill practice after PAGE with a medium effect size (pretest M = 2.92, SD = 0.55, posttest M = 3.28, SD = 0.66, P = 0.052, d = 0.66). There was greater mean reported practice for all skills with the exception of hospice care, which already was being performed between often and very often before PAGE. The largest increases in skill practice were (descending order, most increased first): assessing polypharmacy, performing skin exams, prognostication, performing functional assessments and examining Foley catheter use.
Discussion
Our aging population and a shortage of geriatricians necessitates new, feasible models for geriatric training. Similar to the CHAMP model,7 PAGE had a favorable impact on faculty perceived behavioral change; after the PAGE sessions, faculty reported significantly greater self‐efficacy of teaching geriatrics. However, this study also examined the impact of the PAGE Model on 2 groups not previously reported in the literature: faculty session leaders and medicine residents.
To our knowledge, this is the first study about a hospitalist TTT program codeveloped with nonhospitalists aimed at teaching geriatrics skills to residents, though smaller scale programs for medical students exist.24 We believe codevelopment was important in our model for many reasons. First, using hospitalist peers and local geriatricians likely increased trust in the educational curricula and allowed for strong communication channels between instructors.25, 26 Second, coteaching allowed for hospitalist mentorship. Hospitalists acknowledged their coleaders as mentors and several hospitalists subsequently engaged in new geriatric projects. Third, coteaching was felt to enhance patient care and increase geriatrician consultations. Coteaching may have applicability to other hospitalist faculty development such as intensive care and palliative care, and hospitalist programs may benefit from creating faculty development programs internally with their colleagues, rather than using online resources.
Another important finding of this study is that training hospitalists to teach about geriatrics seems to result in an increase in both the geriatric teaching that residents receive and residents' practice of geriatric skills. This outcome has not been previously demonstrated with geriatric TTT activities.27 This trickle‐down effect to residents likely results from both the increased teaching efficacy of hospitalists after the PAGE Model and the exportable nature of the teaching tools.
Several continuing medical education best practices were used which we believe contributed to the success of PAGE. First, we conducted a needs assessment, which improves knowledge outcomes.28, 29 Second, sessions included cases, lectures, and discussions. Use of multiple educational techniques yields greater knowledge and behavioral change as compared to a single method, such as lecture alone.24, 25, 30, 31 Finally, sessions were sequenced over a year, rather than clustered in short, intensive activity. Sequenced, or learn‐work‐learn opportunities allow education to be translated to practice and reinforced.8, 27, 30, 32
We believe that the PAGE Model is transportable to other hospitalist programs due to its cost and flexible nature. In economically‐lean times, hospitalist divisions can create a program similar to the PAGE Model essentially at no cost, except for donated faculty preparation time. In contrast, CHAMP was expensive, costing nearly $72,000 for 12 faculty to participate in the 48‐hour curriculum,7, 33 and volunteering physicians were compensated for their time. Though Mini‐CHAMP is a streamlined 2‐day workshop that offers free online lectures and slide sets, there may be some benefit to producing a faculty development program internally, as we stated above, and PAGE included additional topics (urinary catheters and decubitus ulcers/wound care) not covered in mini‐CHAMP.
There were several limitations to this study. First, some outcomes of the PAGE Model were assessed by retrospective self‐report, which may allow for recall bias. Although self‐report may or may not correlate with actual behavior,34 faculty and resident perspectives of their teaching and learning experiences are themselves important. Furthermore, a retrospective presurvey allows for content of an educational program or intervention to be explained prior to a survey, so that participants first assess their new level of understanding or skill on the post test, then reflectively assess the level of understanding or skill they had prior to the workshop. This avoids response shift bias and can improve internal validity.21, 35
Second, the small numbers of session leaders, hospitalist trainees, and residents restricted statistical power to detect small effects. The fact that we found significant improvements enhances the likelihood that the differences observed were not due to chance.
Third, the low response rates from the hospitalist trainee post‐intervention questionnaire and the residents' questionnaires may affect the validity of our results. For the resident survey, the subjects were not matched, and we cannot state that an individual's geriatric skill practice changed due to PAGE, though the results suggest the residency program as a whole improved the frequency of geriatric skill practice.
Finally, the residents were required to report the frequency of teaching on and practice of geriatric skills practice over the prior year and accuracy of recall may be an issue. However, frequencies were queried both pre and post intervention and favorable change was noted. Furthermore, because the high end of the 3‐point teaching scale was limited to more than once, the true amount of teaching may have been underestimated if more than once actually represented high frequencies.
Future studies are needed to replicate these findings at other institutions to confirm generalizability. It would be beneficial to measure patient outcomes to determine whether increased teaching and skill practice benefits patients using measures such as reduction in catheter related urinary tract infections, falls, and inadequate pain management. Further investigations of cotaught faculty development programs between hospitalists and other specialists help emphasize why internally created TTT programs are of greater value than online resources.
Conclusions
This time‐sensitive adaptation of a hospitalist geriatric TTT program was successfully implemented at an academic medical center and suggests improved hospitalist faculty self‐efficacy at teaching geriatric skills, increased frequency of inpatient geriatric teaching by hospitalists and increased resident geriatric skill practice. Confidence to care for geriatric patients and a strong skill set to assess risks and manage them appropriately will equip hospitalists and trainees to provide care that reduces geriatric patients' in‐hospital morbidity and costs of care. As hospitalists increasingly care for older adults, the need for time‐efficient methods of teaching geriatrics will continue to grow. The PAGE Model, and other new models of geriatric training for hospitalists, demonstrates that we are beginning to address this urgent need.
Acknowledgements
The authors thank Joan Abrams, MA, MPA, and Patricia O'Sullivan, EdD, whose work was key to the success of this program and this manuscript. They also thank the Donald W. Reynolds Foundation for support of this project.
- ,.2005 National Hospital Discharge Survey.Adv Data.2007;385:1–19.
- ,,,. In:U.S. Census Bureau, Current Population Reports, 65+ in the United States: 2005,Washington, D.C.:U.S. Government Printing Office;2005:23–209.
- ,,,.Growth in the care of older patients by hospitalists in the United States.N Engl J Med.2009;360(11):1102–1112.
- ,,,.Providing dementia outreach education to rural communities: lessons learned from a train‐the‐trainer program.J Appl Gerontol.2002;21:294–313.
- .Gerontologizing health care: a train‐the‐trainer program for nurses.Gerontol Geriatr Educ.1999;19:47–56.
- ,,.A statewide model detection and prevention program for geriatric alcoholism and alcohol abuse: increased knowledge among service providers.Community Ment Health J.2000;36:137–148.
- ,,, et al.The curriculum for the hospitalized aging medical patient program: a collaborative faculty development program for hospitalists, general internists, and geriatricians.J Hosp Med.2008;3(5):384–393.
- Reframing professional development through understanding authentic professional learning.Rev Educ Res.2009;79:702–739.
- The Education Committee Writing Group of the American Geriatrics Society.Core competencies for the care of older patients: recommendations of the American Geriatrics Society.Acad Med.2000;75:252–255.
- ,,, et al.American Geriatrics Society Task Force on the future of geriatric medicine.J Am Geriatr Soc.2005;53 (6 Suppl):S245–S256.
- Nadzam, Deborah. Preventing patient falls. Joint Commission Resources. Available at: http://www.jcrinc.com/Preventing‐Patient‐Falls. Accessed April2010.
- ,.Curricular recommendations for resident training in nursing home care. A collaborative effort of the Society of General Internal Medicine Task Force on Geriatric Medicine, the Society of Teachers of Family Medicine Geriatrics Task Force, the American Medical Directors Association, and the American Geriatrics Society Education Committee.J Am Geriatr Soc.1994;42:1200–1201.
- ,,,,.Curriculum recommendations for resident training in geriatrics interdisciplinary team care.J Am Geriatr Soc.1999;47:1145–1148.
- ,.ACGME requirements for geriatrics medicine curricula in medical specialties: Progress made and progress needed.Acad Med.2005;80:279–285.
- CMS Office of Public Affairs. CMS Improves Patient Safety for Medicare and Medicaid by Addressing Never Events, August 04, 2008. Available at: http://www.cms.gov/apps/media/press/factsheet.asp?Counter=322434(5):337–343.
- ,.The changing paradigm for continuing medical education: impact of information on the teachable moment.Bull Med Libr Assoc.1990;78(2):173–179.
- ,.Creating the teachable moment.J Nurs Educ.1998;37(6):278–280.
- Society of Hospital Medicine, BOOSTing Care Transitions Resource Room. Mazotti L, Johnston CB. Faculty development: Teaching triggers for transitional care. “A train‐the‐trainer model.” Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_CareTransitions/PDFs/Mazotti_UCSF_Transitions.PPT. Accessed April2010.
- .Self‐efficacy: The Exercise of Control.New York:W.H. Freeman and Company;1997.
- .Internal invalidity in pretest‐posttest self‐report evaluations and a re‐evaluation of retrospective pretests.Applied Psychological Measurement.1979;3:1–23.
- ,.A visitor's guide to effect sizes.Adv Health Sci Educ Theory Pract.2004;9:241–249.
- .Statistical Power Analyses for the Behavioral Sciences.2nd ed.Hillsdale, NJ:Lawrence Erlbaum Associates;1988.
- ,,,.Hazards of hospitalization: Hospitalists and geriatricians educating medical students about delirium and falls in geriatric patients.Gerontol Geriatr Educ.2008;28(4):94–104.
- ,,, et al.Continuing medical education, continuing professional development, and knowledge translation: Improving care of older patients by practicing physicians.J Am Geriatr Soc.2006:54(10):1610–1618.
- ,,, et al.Practicing physician education in geriatrics: Lessons learned from a train‐the‐trainer model.J Am Geriatr Soc.2007:55(8):1281–1286.
- ,.CHAMP trains champions: hospitalist‐educators develop new ways to teach care for older patients.J Hosp Med.2008;3(5):357–360.
- ,,,,,.Impact of formal continuing medical education: Do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes?JAMA.1999;282(9):867–874.
- ,.Association for the Study of Medical Education Booklet: The effectiveness of continuing professional development.Edinburgh, Scotland:Association for the Study of Medical Education;2000.
- ,,, et al.Effectiveness of continuing medical education.Evid Rep Technol Assess (Full Rep).2007;149:1–69.
- ,,, et al.Continuing education meetings and workshops: effects on professional practice and health care outcomes.Cochrane Database Syst Rev.2009;(2):CD003030.
- ,.Continuing medical education and the physician as learner: guide to the evidence.JAMA.2002;288(9):1057–1060.
- .Care of hospitalized older patients: opportunities for hospital‐based physicians.J Hosp Med.2006;1:42–47.
- ,.What we say and what we do: self‐reported teaching behavior versus performances in written simulations among medical school faculty.Acad Med.1992;67(8):522–527.
- ,.The retrospective pretest and the role of pretest information in evaluation studies.Psychol Rep.1992;70:699–704.
Nearly half of the hospital beds in the United States are occupied by the elderly,1 whose numbers are increasing.2 The odds of a hospitalized Medicare patient being cared for by a hospitalist are increasing by nearly 30% per year.3 Hospitalists require competence in geriatrics to serve their patients and to teach trainees. Train‐the‐Trainer (TTT) programs both educate health care providers and provide educational materials, information, and skills for teaching others.4 This model has been successfully used in geriatrics to impact knowledge, attitudes, and self‐efficacy among health care workers.46
A prominent example of a geriatrics TTT program is the University of Chicago Curriculum for the Hospitalized Aging Medical Patient (CHAMP),7 which requires 48 hours of instruction over 12 sessions. To create a less time‐intensive learning format for busy hospitalists, the University of Chicago developed Mini‐CHAMP, a streamlined 2‐day workshop with web‐based components for hospitalist clinicians, but not necessarily hospitalist educators.7
We created The Donald W. Reynolds Program for Advancing Geriatrics Education (PAGE) at the University of California, San Francisco (UCSF), in light of the time intensity of CHAMP, to integrate geriatric TTT sessions within preexisting hospitalist faculty meetings. This model is consistent with current practices in faculty development.8 This paper describes the evaluation of the PAGE Model, which sought answers to 3 research questions: (1) Does PAGE increase faculty confidence in teaching geriatrics?, (2) Does PAGE increase the frequency of hospitalist teaching geriatrics topics?, and (3) Does PAGE increase residents' practice of geriatrics skills?
Methods
The PAGE Model
The PAGE Model comprises 10 hour‐long monthly seminars held at UCSF from January through December 2008 to teach specific geriatrics principles and clinical skills relevant to providing competent care to a hospitalized older adult. The aims of the PAGE are to:
Give hospitalist physicians knowledge and skills to teach geriatric topics to trainees in a time‐limited environment
Provide exportable teaching modules on geriatric topics for inpatient teaching
Increase teaching about geriatrics received by internal medicine residents
Increase resident use of 15 specific geriatric skills
Create a collaborative environment between the Geriatrics and Hospital Medicine Divisions at UCSF
The PAGE Development Group, which included 2 hospitalists, 2 geriatricians, and an analyst funded by the Donald W. Reynolds Foundation, reviewed American Geriatrics Society core competencies,9 national guidelines and mandates,10, 11 and existing published geriatric curricula.7, 1214 In late 2007, an email‐based needs assessment listing 38 possible topics, drawn from the resources above, was emailed to the 31 hospitalists at UCSF. Each hospitalist identified, in no particular order, 5 topics considered most useful to improve his/her geriatric teaching skills, with write‐in space for additional topic suggestions. The needs assessment also queried what format of teaching tools would be most useful and efficient, such as PowerPoint slides or pocket cards, and interest in session coteaching.
The topics most commonly selected by the respondents (n = 14, response rate 45%) included: home/community resources (64%), delirium/dementia (57%), minimizing medication problems (50%), using prognostic indices to make decisions (43%), and general approach to older inpatients (43%). The Development Group identified less popular topics (falls, pressure ulcers, indwelling catheters/emncontinence) that were gaining significant national attention.15 Finally, a topic suggested by many hospitalists, pain management, was added. Each topic session was mapped to 1 or more of the 15 geriatrics skills in the CHAMP model7 for residents to acquire. The requested and selected topics were then modified to create distinct sessions grouped around a theme, shown in Table 1. For example home and community resources was addressed in the session on Framework on Transitions in Care.
| Topics | Geriatric Skills Addressed for Hospitalized Older Patients |
|---|---|
| |
| 1. Approach to the vulnerable older patient; assessing function; goals of care | Conduct functional status assessmentMobilize early to prevent deconditioning |
| 2. Minimizing medication problems | Reduce polypharmacy and use of high risk/low benefit drugs |
| 3. Framework for transitions in care (including home and community resources) | Develop a safe and appropriate discharge plan, involving communication with other team members, family members and primary care physicians |
| 4. Using prognostics to guide treatment decisions | Give bad news |
| Document advance directives and DNR orders | |
| Discuss hospice care | |
| 5. Falls & immobility | Identify risk factors of hospital falls, including conventional and unconventional types of restraints |
| 6. Delirium | Assess risk and prevent delirium |
| 7. Dementia & depression | Conduct cognitive assessmentScreen for depression |
| Routinely assess pain at bedside in persons with dementia | |
| 8. Pain assessment in the elderly | Routinely assess pain at bedside in persons with dementia |
| Manage pain using the WHO 3‐step ladder and opiate conversion table and manage side effects of opiates | |
| 9. Foley catheters and incontinence | Determine appropriateness for urinary catheter use, discontinuing when inappropriate |
| 10. Pressure ulcers and wound care | Routinely perform a complete skin exam |
Most respondents (86%) wanted teaching materials in a format suitable for attending rounds; 64% preferred teaching cases, 29% PowerPoint presentations, and 29% quality improvement resources. The Development Group, with approval of the Chief of Hospital Medicine, planned 10, 1‐hour monthly sessions during weekly hospitalist meetings to optimize participation. Nine hospitalists agreed to lead sessions with geriatricians; 1 session was co‐led by a hospitalist and urologist.
The Development Group encouraged session leaders to create case‐based PowerPoint teaching modules that could be used during attending rounds, highlighting teaching triggers or teachable moments that modify or reinforce skills.1618 A Development Group hospitalist/geriatrician team cotaught the first session, which modeled the structure and style recommended. A teaching team typically met at least once to define goals and outline their teaching hour; most met repeatedly to refine their presentations. An example of a 1 PAGE session can be found online.19
Evaluation
Evaluation involved data from hospitalist faculty trainees, hospitalist and geriatrician session leaders, and internal medicine residents. The institutional review board approved this study. Self‐report rating scales were used for data collection, which were reviewed by experts in medical education at UCSF and piloted on nonparticipant faculty, or had been previously used by the CHAMP study.7
Hospitalist Trainees' Program Perceptions and Self‐Efficacy
Hospitalist trainees (n = 36) completed paper questionnaires after each session to assess perceived likelihood to use the teaching tools that were presented (1: not at all likely, 5: highly likely), whether they would recommend the program to colleagues (1: do not recommend, 5: highly recommend), and the utility of the PAGE program (Was this experience useful? and Prior to the sessions, did you think it would be useful? 1: definitely not, 5: definitely yes). Change in trainees' perceived self‐efficacy20 to teach geriatrics skills was assessed at the end of the PAGE program, using a posttest and retrospective pretest format with a 12‐items (1: low, 5: high) that was used in the CHAMP study.7 This format was used to avoid response shift bias, or the program‐produced change in a participant's understanding of the construct being measured.21
Faculty Session Leaders' Program Perceptions
After PAGE completion, all faculty session leaders (n = 15) completed an online questionnaire assessing teaching satisfaction (Likert‐type 5‐point scales), experience with coteaching, and years of faculty teaching experience.
Medical Residents
To assess change in hospitalists' teaching about geriatrics and residents' practice of geriatric clinical skills, residents (n = 56; post‐graduate year (PGY)1 = 29, PGY2 = 27) who would not complete residency before the end of PAGE received an online questionnaire, modified from the CHAMP study,7 prior to and after the completion of PAGE. Respondents received monetary gift cards as incentives. Residents gave separate ratings for their inpatient teaching attendings who were hospitalists (80% of inpatient ward attendings) and nonhospitalists (20%, mostly generalists) regarding frequency over the past year of being taught each of 15 geriatric clinical skills. A 3‐point scale was used: (1) never, (2) once, and (3) more than once. Residents also reported the frequency of practicing those skills themselves, using a questionnaire from the CHAMP study,7 with a scale of (1) never to (5) always.
Analysis
Descriptive statistics were computed for all measures. Scale means were constructed from all individual items for the retrospective pretest and posttest measures. Wilcoxon matched‐pairs signed ranks‐tests were used to compare teaching differences between hospitalist and other attendings. For the unmatched pre‐post data on frequency of teaching, Wilcoxon‐Mann‐Whitney tests were used to determine significant differences in instruction, conducting separate tests for hospitalists and nonhospitalist attendings. Effect size22 was calculated using Cohen's d23 to determine the magnitude of increase in self‐efficacy to teach geriatrics; an effect size exceeding 0.8 is considered large. Statistics were performed using PASW Statistics 17.0 (SPSS Inc., Chicago, IL, USA).
Results
The hospitalist group grew from 31 to 36 members in June of 2008. On average, 14 hospitalists (M = 14.40, standard deviation [SD] = 2.41, range 1119) attended each session, with all hospitalists (n = 36) attending 1 session (M = 3.83, SD = 2.35, range 19). At each session, an average of 72% completed a post‐session evaluation form. Overall, faculty were likely to use the PAGE teaching tools (M = 4.61, SD = 0.53) and would recommend PAGE to other hospitalists (M = 4.63, SD = 0.51).
Thirteen hospitalist trainees of 36 (36%) completed a post‐PAGE online questionnaire. Respondents taught on faculty for an average of 5 years (mean (M) = 5.08, SD = 3.52). Faculty perceived self‐efficacy at teaching residents about geriatrics improved significantly with a large effect size (pretest M = 3.05, SD = .60; posttest M = 3.96, SD = .36, d = 1.52; P < 0.001). Session attendance was positively correlated with the increase in geriatrics teaching self‐efficacy (r = .62, P < 0.05), while teaching experience was not (r = 0.05, P = 0.88). Hospitalist trainees found the PAGE model more useful after participating (M = 4.62, SD = 0.65), than they had expected (M = 3.92, SD = 0.76; P < 0.05).
All session leaders (n = 15) completed the questionnaire after PAGE (9 hospitalists, 5 geriatricians, 1 urologist). Two‐thirds had 5 years on faculty; eight had no prior experience as a faculty development trainer. Over 80% indicated that they found their coteaching experience, enjoyable, useful and collaborative. Only 1 participant did not commit to interdisciplinary teaching again. Most hospitalist session leaders reported that coteaching with a geriatrician enhanced their knowledge; they were more likely to consult a geriatrician regarding patients. All but 2 session leaders felt that the model fostered a collaborative environment between their 2 divisions.
Of the 56 residents, 41% (16 PGY1, 7 PGY2) completed a pretest; 43% (15 PGY1, 9 PGY2) completed a posttest. Residents reported receiving inpatient teaching on geriatrics skills significantly more frequently from hospitalists vs. nonhospitalist attendings both before PAGE (hospitalists M = 2.18, SD = 0.37; nonhospitalists M = 2.00, SD = 0.53, P < 0.05), and after (hospitalists M = 2.39, SD = 0.46; nonhospitalists M = 2.05, SD = 0.57, P < 0.05; see Fig. 1). Although hospitalists taught more frequently about geriatrics than nonhospitalists before PAGE, our findings suggest that they increased their teaching by a greater magnitude than nonhospitalists (P < 0.01, P > 0.05, respectively). Residents reported increased geriatric skill practice after PAGE with a medium effect size (pretest M = 2.92, SD = 0.55, posttest M = 3.28, SD = 0.66, P = 0.052, d = 0.66). There was greater mean reported practice for all skills with the exception of hospice care, which already was being performed between often and very often before PAGE. The largest increases in skill practice were (descending order, most increased first): assessing polypharmacy, performing skin exams, prognostication, performing functional assessments and examining Foley catheter use.
Discussion
Our aging population and a shortage of geriatricians necessitates new, feasible models for geriatric training. Similar to the CHAMP model,7 PAGE had a favorable impact on faculty perceived behavioral change; after the PAGE sessions, faculty reported significantly greater self‐efficacy of teaching geriatrics. However, this study also examined the impact of the PAGE Model on 2 groups not previously reported in the literature: faculty session leaders and medicine residents.
To our knowledge, this is the first study about a hospitalist TTT program codeveloped with nonhospitalists aimed at teaching geriatrics skills to residents, though smaller scale programs for medical students exist.24 We believe codevelopment was important in our model for many reasons. First, using hospitalist peers and local geriatricians likely increased trust in the educational curricula and allowed for strong communication channels between instructors.25, 26 Second, coteaching allowed for hospitalist mentorship. Hospitalists acknowledged their coleaders as mentors and several hospitalists subsequently engaged in new geriatric projects. Third, coteaching was felt to enhance patient care and increase geriatrician consultations. Coteaching may have applicability to other hospitalist faculty development such as intensive care and palliative care, and hospitalist programs may benefit from creating faculty development programs internally with their colleagues, rather than using online resources.
Another important finding of this study is that training hospitalists to teach about geriatrics seems to result in an increase in both the geriatric teaching that residents receive and residents' practice of geriatric skills. This outcome has not been previously demonstrated with geriatric TTT activities.27 This trickle‐down effect to residents likely results from both the increased teaching efficacy of hospitalists after the PAGE Model and the exportable nature of the teaching tools.
Several continuing medical education best practices were used which we believe contributed to the success of PAGE. First, we conducted a needs assessment, which improves knowledge outcomes.28, 29 Second, sessions included cases, lectures, and discussions. Use of multiple educational techniques yields greater knowledge and behavioral change as compared to a single method, such as lecture alone.24, 25, 30, 31 Finally, sessions were sequenced over a year, rather than clustered in short, intensive activity. Sequenced, or learn‐work‐learn opportunities allow education to be translated to practice and reinforced.8, 27, 30, 32
We believe that the PAGE Model is transportable to other hospitalist programs due to its cost and flexible nature. In economically‐lean times, hospitalist divisions can create a program similar to the PAGE Model essentially at no cost, except for donated faculty preparation time. In contrast, CHAMP was expensive, costing nearly $72,000 for 12 faculty to participate in the 48‐hour curriculum,7, 33 and volunteering physicians were compensated for their time. Though Mini‐CHAMP is a streamlined 2‐day workshop that offers free online lectures and slide sets, there may be some benefit to producing a faculty development program internally, as we stated above, and PAGE included additional topics (urinary catheters and decubitus ulcers/wound care) not covered in mini‐CHAMP.
There were several limitations to this study. First, some outcomes of the PAGE Model were assessed by retrospective self‐report, which may allow for recall bias. Although self‐report may or may not correlate with actual behavior,34 faculty and resident perspectives of their teaching and learning experiences are themselves important. Furthermore, a retrospective presurvey allows for content of an educational program or intervention to be explained prior to a survey, so that participants first assess their new level of understanding or skill on the post test, then reflectively assess the level of understanding or skill they had prior to the workshop. This avoids response shift bias and can improve internal validity.21, 35
Second, the small numbers of session leaders, hospitalist trainees, and residents restricted statistical power to detect small effects. The fact that we found significant improvements enhances the likelihood that the differences observed were not due to chance.
Third, the low response rates from the hospitalist trainee post‐intervention questionnaire and the residents' questionnaires may affect the validity of our results. For the resident survey, the subjects were not matched, and we cannot state that an individual's geriatric skill practice changed due to PAGE, though the results suggest the residency program as a whole improved the frequency of geriatric skill practice.
Finally, the residents were required to report the frequency of teaching on and practice of geriatric skills practice over the prior year and accuracy of recall may be an issue. However, frequencies were queried both pre and post intervention and favorable change was noted. Furthermore, because the high end of the 3‐point teaching scale was limited to more than once, the true amount of teaching may have been underestimated if more than once actually represented high frequencies.
Future studies are needed to replicate these findings at other institutions to confirm generalizability. It would be beneficial to measure patient outcomes to determine whether increased teaching and skill practice benefits patients using measures such as reduction in catheter related urinary tract infections, falls, and inadequate pain management. Further investigations of cotaught faculty development programs between hospitalists and other specialists help emphasize why internally created TTT programs are of greater value than online resources.
Conclusions
This time‐sensitive adaptation of a hospitalist geriatric TTT program was successfully implemented at an academic medical center and suggests improved hospitalist faculty self‐efficacy at teaching geriatric skills, increased frequency of inpatient geriatric teaching by hospitalists and increased resident geriatric skill practice. Confidence to care for geriatric patients and a strong skill set to assess risks and manage them appropriately will equip hospitalists and trainees to provide care that reduces geriatric patients' in‐hospital morbidity and costs of care. As hospitalists increasingly care for older adults, the need for time‐efficient methods of teaching geriatrics will continue to grow. The PAGE Model, and other new models of geriatric training for hospitalists, demonstrates that we are beginning to address this urgent need.
Acknowledgements
The authors thank Joan Abrams, MA, MPA, and Patricia O'Sullivan, EdD, whose work was key to the success of this program and this manuscript. They also thank the Donald W. Reynolds Foundation for support of this project.
Nearly half of the hospital beds in the United States are occupied by the elderly,1 whose numbers are increasing.2 The odds of a hospitalized Medicare patient being cared for by a hospitalist are increasing by nearly 30% per year.3 Hospitalists require competence in geriatrics to serve their patients and to teach trainees. Train‐the‐Trainer (TTT) programs both educate health care providers and provide educational materials, information, and skills for teaching others.4 This model has been successfully used in geriatrics to impact knowledge, attitudes, and self‐efficacy among health care workers.46
A prominent example of a geriatrics TTT program is the University of Chicago Curriculum for the Hospitalized Aging Medical Patient (CHAMP),7 which requires 48 hours of instruction over 12 sessions. To create a less time‐intensive learning format for busy hospitalists, the University of Chicago developed Mini‐CHAMP, a streamlined 2‐day workshop with web‐based components for hospitalist clinicians, but not necessarily hospitalist educators.7
We created The Donald W. Reynolds Program for Advancing Geriatrics Education (PAGE) at the University of California, San Francisco (UCSF), in light of the time intensity of CHAMP, to integrate geriatric TTT sessions within preexisting hospitalist faculty meetings. This model is consistent with current practices in faculty development.8 This paper describes the evaluation of the PAGE Model, which sought answers to 3 research questions: (1) Does PAGE increase faculty confidence in teaching geriatrics?, (2) Does PAGE increase the frequency of hospitalist teaching geriatrics topics?, and (3) Does PAGE increase residents' practice of geriatrics skills?
Methods
The PAGE Model
The PAGE Model comprises 10 hour‐long monthly seminars held at UCSF from January through December 2008 to teach specific geriatrics principles and clinical skills relevant to providing competent care to a hospitalized older adult. The aims of the PAGE are to:
Give hospitalist physicians knowledge and skills to teach geriatric topics to trainees in a time‐limited environment
Provide exportable teaching modules on geriatric topics for inpatient teaching
Increase teaching about geriatrics received by internal medicine residents
Increase resident use of 15 specific geriatric skills
Create a collaborative environment between the Geriatrics and Hospital Medicine Divisions at UCSF
The PAGE Development Group, which included 2 hospitalists, 2 geriatricians, and an analyst funded by the Donald W. Reynolds Foundation, reviewed American Geriatrics Society core competencies,9 national guidelines and mandates,10, 11 and existing published geriatric curricula.7, 1214 In late 2007, an email‐based needs assessment listing 38 possible topics, drawn from the resources above, was emailed to the 31 hospitalists at UCSF. Each hospitalist identified, in no particular order, 5 topics considered most useful to improve his/her geriatric teaching skills, with write‐in space for additional topic suggestions. The needs assessment also queried what format of teaching tools would be most useful and efficient, such as PowerPoint slides or pocket cards, and interest in session coteaching.
The topics most commonly selected by the respondents (n = 14, response rate 45%) included: home/community resources (64%), delirium/dementia (57%), minimizing medication problems (50%), using prognostic indices to make decisions (43%), and general approach to older inpatients (43%). The Development Group identified less popular topics (falls, pressure ulcers, indwelling catheters/emncontinence) that were gaining significant national attention.15 Finally, a topic suggested by many hospitalists, pain management, was added. Each topic session was mapped to 1 or more of the 15 geriatrics skills in the CHAMP model7 for residents to acquire. The requested and selected topics were then modified to create distinct sessions grouped around a theme, shown in Table 1. For example home and community resources was addressed in the session on Framework on Transitions in Care.
| Topics | Geriatric Skills Addressed for Hospitalized Older Patients |
|---|---|
| |
| 1. Approach to the vulnerable older patient; assessing function; goals of care | Conduct functional status assessmentMobilize early to prevent deconditioning |
| 2. Minimizing medication problems | Reduce polypharmacy and use of high risk/low benefit drugs |
| 3. Framework for transitions in care (including home and community resources) | Develop a safe and appropriate discharge plan, involving communication with other team members, family members and primary care physicians |
| 4. Using prognostics to guide treatment decisions | Give bad news |
| Document advance directives and DNR orders | |
| Discuss hospice care | |
| 5. Falls & immobility | Identify risk factors of hospital falls, including conventional and unconventional types of restraints |
| 6. Delirium | Assess risk and prevent delirium |
| 7. Dementia & depression | Conduct cognitive assessmentScreen for depression |
| Routinely assess pain at bedside in persons with dementia | |
| 8. Pain assessment in the elderly | Routinely assess pain at bedside in persons with dementia |
| Manage pain using the WHO 3‐step ladder and opiate conversion table and manage side effects of opiates | |
| 9. Foley catheters and incontinence | Determine appropriateness for urinary catheter use, discontinuing when inappropriate |
| 10. Pressure ulcers and wound care | Routinely perform a complete skin exam |
Most respondents (86%) wanted teaching materials in a format suitable for attending rounds; 64% preferred teaching cases, 29% PowerPoint presentations, and 29% quality improvement resources. The Development Group, with approval of the Chief of Hospital Medicine, planned 10, 1‐hour monthly sessions during weekly hospitalist meetings to optimize participation. Nine hospitalists agreed to lead sessions with geriatricians; 1 session was co‐led by a hospitalist and urologist.
The Development Group encouraged session leaders to create case‐based PowerPoint teaching modules that could be used during attending rounds, highlighting teaching triggers or teachable moments that modify or reinforce skills.1618 A Development Group hospitalist/geriatrician team cotaught the first session, which modeled the structure and style recommended. A teaching team typically met at least once to define goals and outline their teaching hour; most met repeatedly to refine their presentations. An example of a 1 PAGE session can be found online.19
Evaluation
Evaluation involved data from hospitalist faculty trainees, hospitalist and geriatrician session leaders, and internal medicine residents. The institutional review board approved this study. Self‐report rating scales were used for data collection, which were reviewed by experts in medical education at UCSF and piloted on nonparticipant faculty, or had been previously used by the CHAMP study.7
Hospitalist Trainees' Program Perceptions and Self‐Efficacy
Hospitalist trainees (n = 36) completed paper questionnaires after each session to assess perceived likelihood to use the teaching tools that were presented (1: not at all likely, 5: highly likely), whether they would recommend the program to colleagues (1: do not recommend, 5: highly recommend), and the utility of the PAGE program (Was this experience useful? and Prior to the sessions, did you think it would be useful? 1: definitely not, 5: definitely yes). Change in trainees' perceived self‐efficacy20 to teach geriatrics skills was assessed at the end of the PAGE program, using a posttest and retrospective pretest format with a 12‐items (1: low, 5: high) that was used in the CHAMP study.7 This format was used to avoid response shift bias, or the program‐produced change in a participant's understanding of the construct being measured.21
Faculty Session Leaders' Program Perceptions
After PAGE completion, all faculty session leaders (n = 15) completed an online questionnaire assessing teaching satisfaction (Likert‐type 5‐point scales), experience with coteaching, and years of faculty teaching experience.
Medical Residents
To assess change in hospitalists' teaching about geriatrics and residents' practice of geriatric clinical skills, residents (n = 56; post‐graduate year (PGY)1 = 29, PGY2 = 27) who would not complete residency before the end of PAGE received an online questionnaire, modified from the CHAMP study,7 prior to and after the completion of PAGE. Respondents received monetary gift cards as incentives. Residents gave separate ratings for their inpatient teaching attendings who were hospitalists (80% of inpatient ward attendings) and nonhospitalists (20%, mostly generalists) regarding frequency over the past year of being taught each of 15 geriatric clinical skills. A 3‐point scale was used: (1) never, (2) once, and (3) more than once. Residents also reported the frequency of practicing those skills themselves, using a questionnaire from the CHAMP study,7 with a scale of (1) never to (5) always.
Analysis
Descriptive statistics were computed for all measures. Scale means were constructed from all individual items for the retrospective pretest and posttest measures. Wilcoxon matched‐pairs signed ranks‐tests were used to compare teaching differences between hospitalist and other attendings. For the unmatched pre‐post data on frequency of teaching, Wilcoxon‐Mann‐Whitney tests were used to determine significant differences in instruction, conducting separate tests for hospitalists and nonhospitalist attendings. Effect size22 was calculated using Cohen's d23 to determine the magnitude of increase in self‐efficacy to teach geriatrics; an effect size exceeding 0.8 is considered large. Statistics were performed using PASW Statistics 17.0 (SPSS Inc., Chicago, IL, USA).
Results
The hospitalist group grew from 31 to 36 members in June of 2008. On average, 14 hospitalists (M = 14.40, standard deviation [SD] = 2.41, range 1119) attended each session, with all hospitalists (n = 36) attending 1 session (M = 3.83, SD = 2.35, range 19). At each session, an average of 72% completed a post‐session evaluation form. Overall, faculty were likely to use the PAGE teaching tools (M = 4.61, SD = 0.53) and would recommend PAGE to other hospitalists (M = 4.63, SD = 0.51).
Thirteen hospitalist trainees of 36 (36%) completed a post‐PAGE online questionnaire. Respondents taught on faculty for an average of 5 years (mean (M) = 5.08, SD = 3.52). Faculty perceived self‐efficacy at teaching residents about geriatrics improved significantly with a large effect size (pretest M = 3.05, SD = .60; posttest M = 3.96, SD = .36, d = 1.52; P < 0.001). Session attendance was positively correlated with the increase in geriatrics teaching self‐efficacy (r = .62, P < 0.05), while teaching experience was not (r = 0.05, P = 0.88). Hospitalist trainees found the PAGE model more useful after participating (M = 4.62, SD = 0.65), than they had expected (M = 3.92, SD = 0.76; P < 0.05).
All session leaders (n = 15) completed the questionnaire after PAGE (9 hospitalists, 5 geriatricians, 1 urologist). Two‐thirds had 5 years on faculty; eight had no prior experience as a faculty development trainer. Over 80% indicated that they found their coteaching experience, enjoyable, useful and collaborative. Only 1 participant did not commit to interdisciplinary teaching again. Most hospitalist session leaders reported that coteaching with a geriatrician enhanced their knowledge; they were more likely to consult a geriatrician regarding patients. All but 2 session leaders felt that the model fostered a collaborative environment between their 2 divisions.
Of the 56 residents, 41% (16 PGY1, 7 PGY2) completed a pretest; 43% (15 PGY1, 9 PGY2) completed a posttest. Residents reported receiving inpatient teaching on geriatrics skills significantly more frequently from hospitalists vs. nonhospitalist attendings both before PAGE (hospitalists M = 2.18, SD = 0.37; nonhospitalists M = 2.00, SD = 0.53, P < 0.05), and after (hospitalists M = 2.39, SD = 0.46; nonhospitalists M = 2.05, SD = 0.57, P < 0.05; see Fig. 1). Although hospitalists taught more frequently about geriatrics than nonhospitalists before PAGE, our findings suggest that they increased their teaching by a greater magnitude than nonhospitalists (P < 0.01, P > 0.05, respectively). Residents reported increased geriatric skill practice after PAGE with a medium effect size (pretest M = 2.92, SD = 0.55, posttest M = 3.28, SD = 0.66, P = 0.052, d = 0.66). There was greater mean reported practice for all skills with the exception of hospice care, which already was being performed between often and very often before PAGE. The largest increases in skill practice were (descending order, most increased first): assessing polypharmacy, performing skin exams, prognostication, performing functional assessments and examining Foley catheter use.
Discussion
Our aging population and a shortage of geriatricians necessitates new, feasible models for geriatric training. Similar to the CHAMP model,7 PAGE had a favorable impact on faculty perceived behavioral change; after the PAGE sessions, faculty reported significantly greater self‐efficacy of teaching geriatrics. However, this study also examined the impact of the PAGE Model on 2 groups not previously reported in the literature: faculty session leaders and medicine residents.
To our knowledge, this is the first study about a hospitalist TTT program codeveloped with nonhospitalists aimed at teaching geriatrics skills to residents, though smaller scale programs for medical students exist.24 We believe codevelopment was important in our model for many reasons. First, using hospitalist peers and local geriatricians likely increased trust in the educational curricula and allowed for strong communication channels between instructors.25, 26 Second, coteaching allowed for hospitalist mentorship. Hospitalists acknowledged their coleaders as mentors and several hospitalists subsequently engaged in new geriatric projects. Third, coteaching was felt to enhance patient care and increase geriatrician consultations. Coteaching may have applicability to other hospitalist faculty development such as intensive care and palliative care, and hospitalist programs may benefit from creating faculty development programs internally with their colleagues, rather than using online resources.
Another important finding of this study is that training hospitalists to teach about geriatrics seems to result in an increase in both the geriatric teaching that residents receive and residents' practice of geriatric skills. This outcome has not been previously demonstrated with geriatric TTT activities.27 This trickle‐down effect to residents likely results from both the increased teaching efficacy of hospitalists after the PAGE Model and the exportable nature of the teaching tools.
Several continuing medical education best practices were used which we believe contributed to the success of PAGE. First, we conducted a needs assessment, which improves knowledge outcomes.28, 29 Second, sessions included cases, lectures, and discussions. Use of multiple educational techniques yields greater knowledge and behavioral change as compared to a single method, such as lecture alone.24, 25, 30, 31 Finally, sessions were sequenced over a year, rather than clustered in short, intensive activity. Sequenced, or learn‐work‐learn opportunities allow education to be translated to practice and reinforced.8, 27, 30, 32
We believe that the PAGE Model is transportable to other hospitalist programs due to its cost and flexible nature. In economically‐lean times, hospitalist divisions can create a program similar to the PAGE Model essentially at no cost, except for donated faculty preparation time. In contrast, CHAMP was expensive, costing nearly $72,000 for 12 faculty to participate in the 48‐hour curriculum,7, 33 and volunteering physicians were compensated for their time. Though Mini‐CHAMP is a streamlined 2‐day workshop that offers free online lectures and slide sets, there may be some benefit to producing a faculty development program internally, as we stated above, and PAGE included additional topics (urinary catheters and decubitus ulcers/wound care) not covered in mini‐CHAMP.
There were several limitations to this study. First, some outcomes of the PAGE Model were assessed by retrospective self‐report, which may allow for recall bias. Although self‐report may or may not correlate with actual behavior,34 faculty and resident perspectives of their teaching and learning experiences are themselves important. Furthermore, a retrospective presurvey allows for content of an educational program or intervention to be explained prior to a survey, so that participants first assess their new level of understanding or skill on the post test, then reflectively assess the level of understanding or skill they had prior to the workshop. This avoids response shift bias and can improve internal validity.21, 35
Second, the small numbers of session leaders, hospitalist trainees, and residents restricted statistical power to detect small effects. The fact that we found significant improvements enhances the likelihood that the differences observed were not due to chance.
Third, the low response rates from the hospitalist trainee post‐intervention questionnaire and the residents' questionnaires may affect the validity of our results. For the resident survey, the subjects were not matched, and we cannot state that an individual's geriatric skill practice changed due to PAGE, though the results suggest the residency program as a whole improved the frequency of geriatric skill practice.
Finally, the residents were required to report the frequency of teaching on and practice of geriatric skills practice over the prior year and accuracy of recall may be an issue. However, frequencies were queried both pre and post intervention and favorable change was noted. Furthermore, because the high end of the 3‐point teaching scale was limited to more than once, the true amount of teaching may have been underestimated if more than once actually represented high frequencies.
Future studies are needed to replicate these findings at other institutions to confirm generalizability. It would be beneficial to measure patient outcomes to determine whether increased teaching and skill practice benefits patients using measures such as reduction in catheter related urinary tract infections, falls, and inadequate pain management. Further investigations of cotaught faculty development programs between hospitalists and other specialists help emphasize why internally created TTT programs are of greater value than online resources.
Conclusions
This time‐sensitive adaptation of a hospitalist geriatric TTT program was successfully implemented at an academic medical center and suggests improved hospitalist faculty self‐efficacy at teaching geriatric skills, increased frequency of inpatient geriatric teaching by hospitalists and increased resident geriatric skill practice. Confidence to care for geriatric patients and a strong skill set to assess risks and manage them appropriately will equip hospitalists and trainees to provide care that reduces geriatric patients' in‐hospital morbidity and costs of care. As hospitalists increasingly care for older adults, the need for time‐efficient methods of teaching geriatrics will continue to grow. The PAGE Model, and other new models of geriatric training for hospitalists, demonstrates that we are beginning to address this urgent need.
Acknowledgements
The authors thank Joan Abrams, MA, MPA, and Patricia O'Sullivan, EdD, whose work was key to the success of this program and this manuscript. They also thank the Donald W. Reynolds Foundation for support of this project.
- ,.2005 National Hospital Discharge Survey.Adv Data.2007;385:1–19.
- ,,,. In:U.S. Census Bureau, Current Population Reports, 65+ in the United States: 2005,Washington, D.C.:U.S. Government Printing Office;2005:23–209.
- ,,,.Growth in the care of older patients by hospitalists in the United States.N Engl J Med.2009;360(11):1102–1112.
- ,,,.Providing dementia outreach education to rural communities: lessons learned from a train‐the‐trainer program.J Appl Gerontol.2002;21:294–313.
- .Gerontologizing health care: a train‐the‐trainer program for nurses.Gerontol Geriatr Educ.1999;19:47–56.
- ,,.A statewide model detection and prevention program for geriatric alcoholism and alcohol abuse: increased knowledge among service providers.Community Ment Health J.2000;36:137–148.
- ,,, et al.The curriculum for the hospitalized aging medical patient program: a collaborative faculty development program for hospitalists, general internists, and geriatricians.J Hosp Med.2008;3(5):384–393.
- Reframing professional development through understanding authentic professional learning.Rev Educ Res.2009;79:702–739.
- The Education Committee Writing Group of the American Geriatrics Society.Core competencies for the care of older patients: recommendations of the American Geriatrics Society.Acad Med.2000;75:252–255.
- ,,, et al.American Geriatrics Society Task Force on the future of geriatric medicine.J Am Geriatr Soc.2005;53 (6 Suppl):S245–S256.
- Nadzam, Deborah. Preventing patient falls. Joint Commission Resources. Available at: http://www.jcrinc.com/Preventing‐Patient‐Falls. Accessed April2010.
- ,.Curricular recommendations for resident training in nursing home care. A collaborative effort of the Society of General Internal Medicine Task Force on Geriatric Medicine, the Society of Teachers of Family Medicine Geriatrics Task Force, the American Medical Directors Association, and the American Geriatrics Society Education Committee.J Am Geriatr Soc.1994;42:1200–1201.
- ,,,,.Curriculum recommendations for resident training in geriatrics interdisciplinary team care.J Am Geriatr Soc.1999;47:1145–1148.
- ,.ACGME requirements for geriatrics medicine curricula in medical specialties: Progress made and progress needed.Acad Med.2005;80:279–285.
- CMS Office of Public Affairs. CMS Improves Patient Safety for Medicare and Medicaid by Addressing Never Events, August 04, 2008. Available at: http://www.cms.gov/apps/media/press/factsheet.asp?Counter=322434(5):337–343.
- ,.The changing paradigm for continuing medical education: impact of information on the teachable moment.Bull Med Libr Assoc.1990;78(2):173–179.
- ,.Creating the teachable moment.J Nurs Educ.1998;37(6):278–280.
- Society of Hospital Medicine, BOOSTing Care Transitions Resource Room. Mazotti L, Johnston CB. Faculty development: Teaching triggers for transitional care. “A train‐the‐trainer model.” Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_CareTransitions/PDFs/Mazotti_UCSF_Transitions.PPT. Accessed April2010.
- .Self‐efficacy: The Exercise of Control.New York:W.H. Freeman and Company;1997.
- .Internal invalidity in pretest‐posttest self‐report evaluations and a re‐evaluation of retrospective pretests.Applied Psychological Measurement.1979;3:1–23.
- ,.A visitor's guide to effect sizes.Adv Health Sci Educ Theory Pract.2004;9:241–249.
- .Statistical Power Analyses for the Behavioral Sciences.2nd ed.Hillsdale, NJ:Lawrence Erlbaum Associates;1988.
- ,,,.Hazards of hospitalization: Hospitalists and geriatricians educating medical students about delirium and falls in geriatric patients.Gerontol Geriatr Educ.2008;28(4):94–104.
- ,,, et al.Continuing medical education, continuing professional development, and knowledge translation: Improving care of older patients by practicing physicians.J Am Geriatr Soc.2006:54(10):1610–1618.
- ,,, et al.Practicing physician education in geriatrics: Lessons learned from a train‐the‐trainer model.J Am Geriatr Soc.2007:55(8):1281–1286.
- ,.CHAMP trains champions: hospitalist‐educators develop new ways to teach care for older patients.J Hosp Med.2008;3(5):357–360.
- ,,,,,.Impact of formal continuing medical education: Do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes?JAMA.1999;282(9):867–874.
- ,.Association for the Study of Medical Education Booklet: The effectiveness of continuing professional development.Edinburgh, Scotland:Association for the Study of Medical Education;2000.
- ,,, et al.Effectiveness of continuing medical education.Evid Rep Technol Assess (Full Rep).2007;149:1–69.
- ,,, et al.Continuing education meetings and workshops: effects on professional practice and health care outcomes.Cochrane Database Syst Rev.2009;(2):CD003030.
- ,.Continuing medical education and the physician as learner: guide to the evidence.JAMA.2002;288(9):1057–1060.
- .Care of hospitalized older patients: opportunities for hospital‐based physicians.J Hosp Med.2006;1:42–47.
- ,.What we say and what we do: self‐reported teaching behavior versus performances in written simulations among medical school faculty.Acad Med.1992;67(8):522–527.
- ,.The retrospective pretest and the role of pretest information in evaluation studies.Psychol Rep.1992;70:699–704.
- ,.2005 National Hospital Discharge Survey.Adv Data.2007;385:1–19.
- ,,,. In:U.S. Census Bureau, Current Population Reports, 65+ in the United States: 2005,Washington, D.C.:U.S. Government Printing Office;2005:23–209.
- ,,,.Growth in the care of older patients by hospitalists in the United States.N Engl J Med.2009;360(11):1102–1112.
- ,,,.Providing dementia outreach education to rural communities: lessons learned from a train‐the‐trainer program.J Appl Gerontol.2002;21:294–313.
- .Gerontologizing health care: a train‐the‐trainer program for nurses.Gerontol Geriatr Educ.1999;19:47–56.
- ,,.A statewide model detection and prevention program for geriatric alcoholism and alcohol abuse: increased knowledge among service providers.Community Ment Health J.2000;36:137–148.
- ,,, et al.The curriculum for the hospitalized aging medical patient program: a collaborative faculty development program for hospitalists, general internists, and geriatricians.J Hosp Med.2008;3(5):384–393.
- Reframing professional development through understanding authentic professional learning.Rev Educ Res.2009;79:702–739.
- The Education Committee Writing Group of the American Geriatrics Society.Core competencies for the care of older patients: recommendations of the American Geriatrics Society.Acad Med.2000;75:252–255.
- ,,, et al.American Geriatrics Society Task Force on the future of geriatric medicine.J Am Geriatr Soc.2005;53 (6 Suppl):S245–S256.
- Nadzam, Deborah. Preventing patient falls. Joint Commission Resources. Available at: http://www.jcrinc.com/Preventing‐Patient‐Falls. Accessed April2010.
- ,.Curricular recommendations for resident training in nursing home care. A collaborative effort of the Society of General Internal Medicine Task Force on Geriatric Medicine, the Society of Teachers of Family Medicine Geriatrics Task Force, the American Medical Directors Association, and the American Geriatrics Society Education Committee.J Am Geriatr Soc.1994;42:1200–1201.
- ,,,,.Curriculum recommendations for resident training in geriatrics interdisciplinary team care.J Am Geriatr Soc.1999;47:1145–1148.
- ,.ACGME requirements for geriatrics medicine curricula in medical specialties: Progress made and progress needed.Acad Med.2005;80:279–285.
- CMS Office of Public Affairs. CMS Improves Patient Safety for Medicare and Medicaid by Addressing Never Events, August 04, 2008. Available at: http://www.cms.gov/apps/media/press/factsheet.asp?Counter=322434(5):337–343.
- ,.The changing paradigm for continuing medical education: impact of information on the teachable moment.Bull Med Libr Assoc.1990;78(2):173–179.
- ,.Creating the teachable moment.J Nurs Educ.1998;37(6):278–280.
- Society of Hospital Medicine, BOOSTing Care Transitions Resource Room. Mazotti L, Johnston CB. Faculty development: Teaching triggers for transitional care. “A train‐the‐trainer model.” Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_CareTransitions/PDFs/Mazotti_UCSF_Transitions.PPT. Accessed April2010.
- .Self‐efficacy: The Exercise of Control.New York:W.H. Freeman and Company;1997.
- .Internal invalidity in pretest‐posttest self‐report evaluations and a re‐evaluation of retrospective pretests.Applied Psychological Measurement.1979;3:1–23.
- ,.A visitor's guide to effect sizes.Adv Health Sci Educ Theory Pract.2004;9:241–249.
- .Statistical Power Analyses for the Behavioral Sciences.2nd ed.Hillsdale, NJ:Lawrence Erlbaum Associates;1988.
- ,,,.Hazards of hospitalization: Hospitalists and geriatricians educating medical students about delirium and falls in geriatric patients.Gerontol Geriatr Educ.2008;28(4):94–104.
- ,,, et al.Continuing medical education, continuing professional development, and knowledge translation: Improving care of older patients by practicing physicians.J Am Geriatr Soc.2006:54(10):1610–1618.
- ,,, et al.Practicing physician education in geriatrics: Lessons learned from a train‐the‐trainer model.J Am Geriatr Soc.2007:55(8):1281–1286.
- ,.CHAMP trains champions: hospitalist‐educators develop new ways to teach care for older patients.J Hosp Med.2008;3(5):357–360.
- ,,,,,.Impact of formal continuing medical education: Do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes?JAMA.1999;282(9):867–874.
- ,.Association for the Study of Medical Education Booklet: The effectiveness of continuing professional development.Edinburgh, Scotland:Association for the Study of Medical Education;2000.
- ,,, et al.Effectiveness of continuing medical education.Evid Rep Technol Assess (Full Rep).2007;149:1–69.
- ,,, et al.Continuing education meetings and workshops: effects on professional practice and health care outcomes.Cochrane Database Syst Rev.2009;(2):CD003030.
- ,.Continuing medical education and the physician as learner: guide to the evidence.JAMA.2002;288(9):1057–1060.
- .Care of hospitalized older patients: opportunities for hospital‐based physicians.J Hosp Med.2006;1:42–47.
- ,.What we say and what we do: self‐reported teaching behavior versus performances in written simulations among medical school faculty.Acad Med.1992;67(8):522–527.
- ,.The retrospective pretest and the role of pretest information in evaluation studies.Psychol Rep.1992;70:699–704.
Copyright © 2010 Society of Hospital Medicine
In the Literature
Literature at a Glance
A guide to this month’s studies.
- Carotid stenting is equivalent to endarterectomy in carotid artery stenosis.
- Idiopathic ventricular fibrillation is associated with early repolarization.
- Aggressive LDL and blood pressure management may benefit diabetic patients.
- Treatment of hypertension in patients older than age 80 improves outcomes.
- Length of stay predicts mortality in pulmonary embolism patients.
- Poor symptom control and lack of family support during end-of-life hospital stays.
- Potentially inappropriate medication use in hospitalized elders is common.
- Steroids may not help in pediatric meningitis.
- PCI and CABG may be equivalent in the treatment of left main disease.
Is Stenting or Endarterectomy Best for Carotid Artery Stenosis?
Background: Patients with moderate to severe symptomatic carotid artery stenosis and those with severe asymptomatic carotid stenosis benefit from carotid endarterectomy. Carotid stenting may provide an alternative therapy, but the long-term protection against stroke compared with endarterectomy is unclear.
Study Design: Prospective randomized trial.
Setting: 29 centers in the United States.
Synopsis: This article reports the long-term (three years) follow-up of the SAPPHIRE trial, published in 2004, which compared carotid stenting to endarterectomy in patients at high surgical risk. In that trial, 334 patients randomized to either stenting or endarterectomy had similar outcomes at one year. Patients were followed for three years with death and major cardiovascular events as endpoints.
Rates of stroke at three years were approximately 10% with an overall death rate of approximately 20%. There was no difference between carotid stenting and endarterectomy with regards to death, stroke, or other cardiovascular outcome.
Notably, follow-up was not complete (78%), a specific type of stenting procedure was used, and the patient population was at high risk for surgical complications. Therefore, results may not be applicable in other centers or in other patient populations. Yet, this trial provides follow-up, long-term evidence that carotid stenting may be a viable alternative to endarterectomy in patients with carotid artery stenosis.
Bottom line: Carotid stenting and endarterectomy had similar outcomes at three years in high-risk patients with carotid artery stenosis.
Citation: Gurm HS, Yadav JS, Fayad P, et al. Long-term results of carotid stenting versus endarterectomy in high-risk patients. N Engl J Med. 2008;358:1572-1579.
Is Early Repolarization on EKG Associated with Sudden Cardiac Arrest?
Background: Electrocardiographic early repolarization, defined as elevation of the QRS-ST junction of at least 0.1mV from baseline in the inferior or lateral leads (manifested as slurring or notching), occurs in 1% to 5% of patients. It is considered benign, but experimental studies have suggested it may be arrhythmogenic.
Study Design: Prospective case-control.
Setting: 22 international tertiary care centers.
Synopsis: Case subjects were less than 60 years of age and were resuscitated after ventricular fibrillation (VF) arrest ultimately deemed idiopathic. All had normal echocardiograms, no evidence of coronary artery disease, and no repolarization abnormalities (including Brugada and long-QT). Of 206 patients, 31% had early repolarization on EKG, versus only 5% in controls without heart disease. In case subjects with prior EKGs, early repolarization was proven to be pre-existing.
The mean magnitude of J-point elevation was 2 mm in cases versus 1.2 mm in controls, and in cases this magnitude increased during later episodes of arrhythmia. Electrophysiologic mapping showed that ectopy originated at sites concordant with the location of abnormal repolarization. During five years of follow-up, arrhythmic recurrence was twice as common in cases with early repolarization.
Although long-term observational studies of persons with early repolarization have shown a benign natural course, this study may change our approach to those with syncope or a family history of sudden death.
Bottom line: Early repolarization on EKG is associated with idiopathic ventricular fibrillation.
Citation: Haissaguerre M, Derval N, Sacher F, et al. Sudden cardiac arrest associated with early repolarization. N Engl J Med. 2008;358(19):2016-2023.
Does Aggressive Blood Pressure and LDL Treatment in Diabetics Affect Development of Subclinical Atherosclerosis?
Background: There is evidence to suggest more aggressive treatment of LDL cholesterol in patients with known coronary artery disease is beneficial and more aggressive blood pressure control can improve outcomes in some patient populations. However, it is unclear if patients with diabetes without cardiovascular disease would benefit from more aggressive LDL and systolic blood pressure (SBP) treatment.
Study Design: Randomized, open-label, blinded-to-end point trial.
Setting: Four centers in Oklahoma, Arizona, and South Dakota.
Synopsis: Investigators studied 499 type 2 diabetic American Indian men with no history of cardiovascular disease. Patients were randomized to receive treatment to achieve aggressive (70 mg/dL and 115 mmHg) or standard (100 mg/dL and 130 mmHg) targets for their LDL cholesterol and SBP, respectively.
At three years, the aggressive group showed decreased carotid intima-media thickness (IMT) and decreased left ventricular mass, whereas both IMT and left ventricular volume increased in the standard group. There were no differences in clinical cardiovascular events between the aggressive and standard group and both groups had lower-than-expected clinical events.
This study included no women and was limited to an American Indian population. Of note, there was an increase in adverse events related to blood pressure medications in the aggressive group. It also is unclear how the surrogates of cardiovascular disease or subclinical atherosclerosis relate to significant clinical outcomes.
Bottom line: More aggressive LDL and SBP treatment in diabetics without coronary disease decreased subclinical atherosclerosis but did not impact clinical outcomes.
Citation: Howard B, Roman M, Devereux R, et al. Effect of lower targets for blood pressure and LDL cholesterol on atherosclerosis in diabetes. JAMA. 2008;299(14):1678-1689.
Should We Treat Hypertension in Patients Older Than 80?
Background: There is debate about whether treatment of hypertension in the elderly is beneficial. Numerous studies suggest blood pressure control does less to prevent strokes in patients older than 80 years than for younger patients. Moreover, other evidence shows controlling blood pressure in elderly patients may result in an increase in mortality even if there was a decreased risk of stroke.
Study Design: Randomized, double-blind, placebo-controlled trial.
Setting: 195 centers in 13 countries in Europe, China, Australasia, and North Africa.
Synopsis: This study evaluated 3,845 patients, age 80 or older, with a sustained systolic blood pressure (SBP) of 160 mmHg and randomized them to receive indapamide (sustained release) or placebo. Perindopril, or placebo, was added if necessary to achieve a target blood pressure of 150/80 mmHg. Patients who received the indapamide with or without the perindopril had lower blood pressure, lower rate of stroke, lower rate of heart failure, lower rate of death from a cardiovascular cause, and a 21% reduction in all-cause mortality (all statistically significant). There were very few adverse drug events and fewer adverse events overall in the treatment group.
Of note, exclusion criteria included a history of heart failure requiring anti-hypertensive medication, dementia, need for nursing care, an inability to stand or walk, and a creatinine more than 1.7 mg/dL. As well, the “target” SBP of 150 mmHg (which only half of the treatment group achieved) is still considered hypertensive according to the JNC 7 guidelines.
Bottom line: In some patients older than 80, treatment of hypertension may reduce the incidence of stroke, death from stroke, heart failure, and all-cause mortality.
Citation: Beckett N, Peters R, Fletcher A, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358:1887-1898.
What Is the Optimal Hospital LOS for Patients with PE?
Background: Though there are clear trends toward shorter hospital stays after pulmonary embolism (PE), especially with the introduction of low molecular weight heparin, the optimal timing of discharge and the effect of decreased length of stay (LOS) on post-discharge mortality are unknown. Furthermore, there is no risk stratification strategy used to identify low-risk patients with PE who can safely be discharged early or treated in the outpatient setting.
Study Design: Retrospective cohort study.
Setting: 186 acute care hospitals in Pennsylvania from January 2000 to November 2002.
Synopsis: Using a statewide database of 15,531 patients discharged with pulmonary embolism (PE), the authors sought to identify patient and hospital factors associated with LOS and assess whether LOS was associated with post-discharge mortality.
Findings indicate there is considerable variation in LOS for PE between and within hospitals in Pennsylvania. The median LOS for patients with PE was six days; patients with a LOS of four or fewer days had significantly higher post-discharge mortality than patients hospitalized five to eight days. More than half the patients discharged at four or fewer days were classified as high-risk, with Pulmonary Embolism Severity Index (PESI) scores of III-V (3.1% to 24.5% risk of mortality at 30 days).
Although we cannot infer causation (i.e., early discharge=death), clinicians should be aware of the results and consider severity of illness (using PESI or other criteria) in the discharge decision in patients with PE. Future prognostic models and evidence-based criteria would be helpful to identify patients with PE who can be safely discharged early.
Bottom line: Physicians may inappropriately select patients with PE for early discharge who are at increased risk of complications.
Citation: Aujesky D, Stone RA, Kim S, et al. Length of hospital stay and post-discharge mortality in patients with pulmonary embolism. Arch Intern Med. 2008;168(7):706-712.
Do Patients Have a “Good Death” in the Hospital?
Background: Despite an increasing focus on providing appropriate end-of-life care, the majority of patients in developed countries die in the hospital. The circumstances and quality of care provided at the time of death are poorly described.
Study Design: Cross-sectional survey.
Setting: 613 departments in 200 French hospitals.
Synopsis: For 3,793 in-hospital deaths, the investigators surveyed the bedside nurses about the circumstances and details of the death. Twenty-three percent of the patients were admitted for end-of-life care, 29% had a malignancy, and 50% of patients were identified as terminally ill for three days prior to their death.
A family member or relative was present in only 25% of all deaths; 20% of patients were alone at the time of death. In the last few hours of life, up to 70% of patients had symptoms of respiratory distress, while only 44% received opiate analgesia. Only 35% of nurses were satisfied with the quality of death. Satisfaction increased with presence of family members and having written protocols for care at the end of life.
This large, multicenter study has limitations but provides a concerning snapshot of death in the hospital. Hospitalists should be aggressive about symptom control at the end of life as well as attempt to ensure patients are not alone at the time of death.
Bottom line: Many patients die in the hospital in some degree of respiratory distress and without family or friends at the bedside.
Citation: Ferrand E, Jabre P, Vincent-Genod C, et al. Circumstances of death in hospitalized patients and nurses’ perceptions. Arch Intern Med. 2008;168(8):867-875.
How Common Is Potentially Inappropriate Medication Use in the Hospital?
Background: Use of potentially inappropriate medications (PIM) in the elderly based on the Beers’ List is common in nursing homes, the emergency department (ED), and outpatient settings and is associated with adverse outcomes and hospitalization. Frequency of PIM use the inpatient setting has not been well studied.
Study Design: A retrospective cohort study.
Setting: 384 U.S. hospitals.
Synopsis: In this retrospective cohort study of 493,971 inpatients (older than 65) admitted with medical diagnoses to non-surgeons, PIM prescription was evaluated. Forty nine percent of all patients were prescribed at least one PIM, while 6% were prescribed three or more. In a multivariable model, physician specialty was associated with variation in high severity PIM (HSPIM) prescription. In comparison with internal medicine physicians, cardiologists (odds ratio [OR] 1.32) and pulmonologists (OR 1.10) were more likely to prescribe HSPIMs, while hospitalists (OR 0.90) and geriatricians (OR 0.60) were less likely. In addition, patient age older than 85 was associated with decreased HSPIM prescription (OR 0.59) compared with those younger than 85.
Compared with patients in the Midwest, patients in the South (OR 1.63) and West (OR 1.43) were more likely to prescribe HSPIMs, while those in the Northeast (OR 0.85) were less likely. Hospitals with geriatric services had less PIM use. The study couldn’t account for continuation of chronic medications and did not evaluate adverse outcomes from PIM prescribing.
Bottom line: PIM prescription to hospitalized geriatric patients is common and associated with provider and hospital characteristics.
Citation: Rothberg MB, Pekow PS, Liu F, et al. Potentially inappropriate medication use in hospitalized elders. J Hosp Med. 2008;3:91-102:91-102.
Is There a Benefit to Corticosteroids When Treating Bacterial Meningitis in Children?
Background: The benefit of adjuvant corticosteroids in the treatment of bacterial meningitis in children in the developed world remains unclear; recent expert guidelines reflect this uncertainty.
Study Design: Retrospective cohort study.
Setting: Twenty-seven tertiary care hospitals in the United States.
Synopsis: Researchers examined 2,780 children with a primary diagnosis of bacterial meningitis discharged from 27 tertiary care centers in the U.S. from 2001-2006. Using a propensity analysis (to control for severity of illness), the study compared those who had received adjunctive corticosteroids with those who had not, with mortality and length of study (LOS) as primary outcomes.
The median age was nine months, 8.9% of children received corticosteroids, and the overall mortality rate was 4.2%. Adjuvent corticosteroids did not reduce mortality or LOS. The outcomes were unchanged in subgroup analyses.
Although limited by its retrospective design and lack of other outcome measures (e.g., hearing loss, neurological deficits), this study provides reasonable evidence that corticosteroid use in bacterial meningitis in children may not save lives or shorten LOS. Pediatric hospitalists may not want to routinely give steroids in this setting pending large randomized-controlled trials.
Bottom line: Adjunctive corticosteroids therapy in children with bacterial meningitis may not save lives or reduce LOS.
Citation: Mongelluzzo J, Mohamad Z, Ten Have TR, Shah SS. Corticosteroids and mortality in children with bacterial meningitis. JAMA. 2008;299(17):2048-2055.
Should Unprotected Left Main Disease Be Treated With PCI or CABG?
Background: The current standard of care for the treatment of left main coronary artery disease is coronary-artery bypass grafting (CABG). With the advent of drug-eluting stents, there is growing interest in the use of percutaneous coronary intervention (PCI) to treat left main disease.
Study Design: Prospective observational study.
Setting: Twelve Korean cardiac centers.
Synopsis: From 2000 to 2006, patients with left main disease were treated with PCI or CABG at the discretion of the physician. Nearly 1,100 patients in each cohort were compared and evaluated for death and a composite outcome of death, myocardial infarction, or stroke. Propensity-matching was employed to control for confounders.
In the overall cohort matched by propensity score, there was no significant difference in death or the composite outcome between the PCI and CABG groups after three years. Type of stent (bare metal vs. drug-eluting) did not affect the outcome. Rates of target-vessel revascularization were significantly higher in the group that received stents.
The results are limited by the observational nature and the need for propensity analysis and yet provide an intriguing result. The standard of care for treatment of left main disease remains CABG, but clinicians may be more comfortable treating with stents while we await randomized-controlled trials.
Bottom line: In this observational study, PCI and CABG had similar outcomes in patients with left main disease.
Citation: Seung KB, Park D, Kim Y, Lee S. Stents versus coronary-artery bypass grafting for left main coronary artery disease. N Engl J Med. 2008;358:1781-1792.
Literature at a Glance
A guide to this month’s studies.
- Carotid stenting is equivalent to endarterectomy in carotid artery stenosis.
- Idiopathic ventricular fibrillation is associated with early repolarization.
- Aggressive LDL and blood pressure management may benefit diabetic patients.
- Treatment of hypertension in patients older than age 80 improves outcomes.
- Length of stay predicts mortality in pulmonary embolism patients.
- Poor symptom control and lack of family support during end-of-life hospital stays.
- Potentially inappropriate medication use in hospitalized elders is common.
- Steroids may not help in pediatric meningitis.
- PCI and CABG may be equivalent in the treatment of left main disease.
Is Stenting or Endarterectomy Best for Carotid Artery Stenosis?
Background: Patients with moderate to severe symptomatic carotid artery stenosis and those with severe asymptomatic carotid stenosis benefit from carotid endarterectomy. Carotid stenting may provide an alternative therapy, but the long-term protection against stroke compared with endarterectomy is unclear.
Study Design: Prospective randomized trial.
Setting: 29 centers in the United States.
Synopsis: This article reports the long-term (three years) follow-up of the SAPPHIRE trial, published in 2004, which compared carotid stenting to endarterectomy in patients at high surgical risk. In that trial, 334 patients randomized to either stenting or endarterectomy had similar outcomes at one year. Patients were followed for three years with death and major cardiovascular events as endpoints.
Rates of stroke at three years were approximately 10% with an overall death rate of approximately 20%. There was no difference between carotid stenting and endarterectomy with regards to death, stroke, or other cardiovascular outcome.
Notably, follow-up was not complete (78%), a specific type of stenting procedure was used, and the patient population was at high risk for surgical complications. Therefore, results may not be applicable in other centers or in other patient populations. Yet, this trial provides follow-up, long-term evidence that carotid stenting may be a viable alternative to endarterectomy in patients with carotid artery stenosis.
Bottom line: Carotid stenting and endarterectomy had similar outcomes at three years in high-risk patients with carotid artery stenosis.
Citation: Gurm HS, Yadav JS, Fayad P, et al. Long-term results of carotid stenting versus endarterectomy in high-risk patients. N Engl J Med. 2008;358:1572-1579.
Is Early Repolarization on EKG Associated with Sudden Cardiac Arrest?
Background: Electrocardiographic early repolarization, defined as elevation of the QRS-ST junction of at least 0.1mV from baseline in the inferior or lateral leads (manifested as slurring or notching), occurs in 1% to 5% of patients. It is considered benign, but experimental studies have suggested it may be arrhythmogenic.
Study Design: Prospective case-control.
Setting: 22 international tertiary care centers.
Synopsis: Case subjects were less than 60 years of age and were resuscitated after ventricular fibrillation (VF) arrest ultimately deemed idiopathic. All had normal echocardiograms, no evidence of coronary artery disease, and no repolarization abnormalities (including Brugada and long-QT). Of 206 patients, 31% had early repolarization on EKG, versus only 5% in controls without heart disease. In case subjects with prior EKGs, early repolarization was proven to be pre-existing.
The mean magnitude of J-point elevation was 2 mm in cases versus 1.2 mm in controls, and in cases this magnitude increased during later episodes of arrhythmia. Electrophysiologic mapping showed that ectopy originated at sites concordant with the location of abnormal repolarization. During five years of follow-up, arrhythmic recurrence was twice as common in cases with early repolarization.
Although long-term observational studies of persons with early repolarization have shown a benign natural course, this study may change our approach to those with syncope or a family history of sudden death.
Bottom line: Early repolarization on EKG is associated with idiopathic ventricular fibrillation.
Citation: Haissaguerre M, Derval N, Sacher F, et al. Sudden cardiac arrest associated with early repolarization. N Engl J Med. 2008;358(19):2016-2023.
Does Aggressive Blood Pressure and LDL Treatment in Diabetics Affect Development of Subclinical Atherosclerosis?
Background: There is evidence to suggest more aggressive treatment of LDL cholesterol in patients with known coronary artery disease is beneficial and more aggressive blood pressure control can improve outcomes in some patient populations. However, it is unclear if patients with diabetes without cardiovascular disease would benefit from more aggressive LDL and systolic blood pressure (SBP) treatment.
Study Design: Randomized, open-label, blinded-to-end point trial.
Setting: Four centers in Oklahoma, Arizona, and South Dakota.
Synopsis: Investigators studied 499 type 2 diabetic American Indian men with no history of cardiovascular disease. Patients were randomized to receive treatment to achieve aggressive (70 mg/dL and 115 mmHg) or standard (100 mg/dL and 130 mmHg) targets for their LDL cholesterol and SBP, respectively.
At three years, the aggressive group showed decreased carotid intima-media thickness (IMT) and decreased left ventricular mass, whereas both IMT and left ventricular volume increased in the standard group. There were no differences in clinical cardiovascular events between the aggressive and standard group and both groups had lower-than-expected clinical events.
This study included no women and was limited to an American Indian population. Of note, there was an increase in adverse events related to blood pressure medications in the aggressive group. It also is unclear how the surrogates of cardiovascular disease or subclinical atherosclerosis relate to significant clinical outcomes.
Bottom line: More aggressive LDL and SBP treatment in diabetics without coronary disease decreased subclinical atherosclerosis but did not impact clinical outcomes.
Citation: Howard B, Roman M, Devereux R, et al. Effect of lower targets for blood pressure and LDL cholesterol on atherosclerosis in diabetes. JAMA. 2008;299(14):1678-1689.
Should We Treat Hypertension in Patients Older Than 80?
Background: There is debate about whether treatment of hypertension in the elderly is beneficial. Numerous studies suggest blood pressure control does less to prevent strokes in patients older than 80 years than for younger patients. Moreover, other evidence shows controlling blood pressure in elderly patients may result in an increase in mortality even if there was a decreased risk of stroke.
Study Design: Randomized, double-blind, placebo-controlled trial.
Setting: 195 centers in 13 countries in Europe, China, Australasia, and North Africa.
Synopsis: This study evaluated 3,845 patients, age 80 or older, with a sustained systolic blood pressure (SBP) of 160 mmHg and randomized them to receive indapamide (sustained release) or placebo. Perindopril, or placebo, was added if necessary to achieve a target blood pressure of 150/80 mmHg. Patients who received the indapamide with or without the perindopril had lower blood pressure, lower rate of stroke, lower rate of heart failure, lower rate of death from a cardiovascular cause, and a 21% reduction in all-cause mortality (all statistically significant). There were very few adverse drug events and fewer adverse events overall in the treatment group.
Of note, exclusion criteria included a history of heart failure requiring anti-hypertensive medication, dementia, need for nursing care, an inability to stand or walk, and a creatinine more than 1.7 mg/dL. As well, the “target” SBP of 150 mmHg (which only half of the treatment group achieved) is still considered hypertensive according to the JNC 7 guidelines.
Bottom line: In some patients older than 80, treatment of hypertension may reduce the incidence of stroke, death from stroke, heart failure, and all-cause mortality.
Citation: Beckett N, Peters R, Fletcher A, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358:1887-1898.
What Is the Optimal Hospital LOS for Patients with PE?
Background: Though there are clear trends toward shorter hospital stays after pulmonary embolism (PE), especially with the introduction of low molecular weight heparin, the optimal timing of discharge and the effect of decreased length of stay (LOS) on post-discharge mortality are unknown. Furthermore, there is no risk stratification strategy used to identify low-risk patients with PE who can safely be discharged early or treated in the outpatient setting.
Study Design: Retrospective cohort study.
Setting: 186 acute care hospitals in Pennsylvania from January 2000 to November 2002.
Synopsis: Using a statewide database of 15,531 patients discharged with pulmonary embolism (PE), the authors sought to identify patient and hospital factors associated with LOS and assess whether LOS was associated with post-discharge mortality.
Findings indicate there is considerable variation in LOS for PE between and within hospitals in Pennsylvania. The median LOS for patients with PE was six days; patients with a LOS of four or fewer days had significantly higher post-discharge mortality than patients hospitalized five to eight days. More than half the patients discharged at four or fewer days were classified as high-risk, with Pulmonary Embolism Severity Index (PESI) scores of III-V (3.1% to 24.5% risk of mortality at 30 days).
Although we cannot infer causation (i.e., early discharge=death), clinicians should be aware of the results and consider severity of illness (using PESI or other criteria) in the discharge decision in patients with PE. Future prognostic models and evidence-based criteria would be helpful to identify patients with PE who can be safely discharged early.
Bottom line: Physicians may inappropriately select patients with PE for early discharge who are at increased risk of complications.
Citation: Aujesky D, Stone RA, Kim S, et al. Length of hospital stay and post-discharge mortality in patients with pulmonary embolism. Arch Intern Med. 2008;168(7):706-712.
Do Patients Have a “Good Death” in the Hospital?
Background: Despite an increasing focus on providing appropriate end-of-life care, the majority of patients in developed countries die in the hospital. The circumstances and quality of care provided at the time of death are poorly described.
Study Design: Cross-sectional survey.
Setting: 613 departments in 200 French hospitals.
Synopsis: For 3,793 in-hospital deaths, the investigators surveyed the bedside nurses about the circumstances and details of the death. Twenty-three percent of the patients were admitted for end-of-life care, 29% had a malignancy, and 50% of patients were identified as terminally ill for three days prior to their death.
A family member or relative was present in only 25% of all deaths; 20% of patients were alone at the time of death. In the last few hours of life, up to 70% of patients had symptoms of respiratory distress, while only 44% received opiate analgesia. Only 35% of nurses were satisfied with the quality of death. Satisfaction increased with presence of family members and having written protocols for care at the end of life.
This large, multicenter study has limitations but provides a concerning snapshot of death in the hospital. Hospitalists should be aggressive about symptom control at the end of life as well as attempt to ensure patients are not alone at the time of death.
Bottom line: Many patients die in the hospital in some degree of respiratory distress and without family or friends at the bedside.
Citation: Ferrand E, Jabre P, Vincent-Genod C, et al. Circumstances of death in hospitalized patients and nurses’ perceptions. Arch Intern Med. 2008;168(8):867-875.
How Common Is Potentially Inappropriate Medication Use in the Hospital?
Background: Use of potentially inappropriate medications (PIM) in the elderly based on the Beers’ List is common in nursing homes, the emergency department (ED), and outpatient settings and is associated with adverse outcomes and hospitalization. Frequency of PIM use the inpatient setting has not been well studied.
Study Design: A retrospective cohort study.
Setting: 384 U.S. hospitals.
Synopsis: In this retrospective cohort study of 493,971 inpatients (older than 65) admitted with medical diagnoses to non-surgeons, PIM prescription was evaluated. Forty nine percent of all patients were prescribed at least one PIM, while 6% were prescribed three or more. In a multivariable model, physician specialty was associated with variation in high severity PIM (HSPIM) prescription. In comparison with internal medicine physicians, cardiologists (odds ratio [OR] 1.32) and pulmonologists (OR 1.10) were more likely to prescribe HSPIMs, while hospitalists (OR 0.90) and geriatricians (OR 0.60) were less likely. In addition, patient age older than 85 was associated with decreased HSPIM prescription (OR 0.59) compared with those younger than 85.
Compared with patients in the Midwest, patients in the South (OR 1.63) and West (OR 1.43) were more likely to prescribe HSPIMs, while those in the Northeast (OR 0.85) were less likely. Hospitals with geriatric services had less PIM use. The study couldn’t account for continuation of chronic medications and did not evaluate adverse outcomes from PIM prescribing.
Bottom line: PIM prescription to hospitalized geriatric patients is common and associated with provider and hospital characteristics.
Citation: Rothberg MB, Pekow PS, Liu F, et al. Potentially inappropriate medication use in hospitalized elders. J Hosp Med. 2008;3:91-102:91-102.
Is There a Benefit to Corticosteroids When Treating Bacterial Meningitis in Children?
Background: The benefit of adjuvant corticosteroids in the treatment of bacterial meningitis in children in the developed world remains unclear; recent expert guidelines reflect this uncertainty.
Study Design: Retrospective cohort study.
Setting: Twenty-seven tertiary care hospitals in the United States.
Synopsis: Researchers examined 2,780 children with a primary diagnosis of bacterial meningitis discharged from 27 tertiary care centers in the U.S. from 2001-2006. Using a propensity analysis (to control for severity of illness), the study compared those who had received adjunctive corticosteroids with those who had not, with mortality and length of study (LOS) as primary outcomes.
The median age was nine months, 8.9% of children received corticosteroids, and the overall mortality rate was 4.2%. Adjuvent corticosteroids did not reduce mortality or LOS. The outcomes were unchanged in subgroup analyses.
Although limited by its retrospective design and lack of other outcome measures (e.g., hearing loss, neurological deficits), this study provides reasonable evidence that corticosteroid use in bacterial meningitis in children may not save lives or shorten LOS. Pediatric hospitalists may not want to routinely give steroids in this setting pending large randomized-controlled trials.
Bottom line: Adjunctive corticosteroids therapy in children with bacterial meningitis may not save lives or reduce LOS.
Citation: Mongelluzzo J, Mohamad Z, Ten Have TR, Shah SS. Corticosteroids and mortality in children with bacterial meningitis. JAMA. 2008;299(17):2048-2055.
Should Unprotected Left Main Disease Be Treated With PCI or CABG?
Background: The current standard of care for the treatment of left main coronary artery disease is coronary-artery bypass grafting (CABG). With the advent of drug-eluting stents, there is growing interest in the use of percutaneous coronary intervention (PCI) to treat left main disease.
Study Design: Prospective observational study.
Setting: Twelve Korean cardiac centers.
Synopsis: From 2000 to 2006, patients with left main disease were treated with PCI or CABG at the discretion of the physician. Nearly 1,100 patients in each cohort were compared and evaluated for death and a composite outcome of death, myocardial infarction, or stroke. Propensity-matching was employed to control for confounders.
In the overall cohort matched by propensity score, there was no significant difference in death or the composite outcome between the PCI and CABG groups after three years. Type of stent (bare metal vs. drug-eluting) did not affect the outcome. Rates of target-vessel revascularization were significantly higher in the group that received stents.
The results are limited by the observational nature and the need for propensity analysis and yet provide an intriguing result. The standard of care for treatment of left main disease remains CABG, but clinicians may be more comfortable treating with stents while we await randomized-controlled trials.
Bottom line: In this observational study, PCI and CABG had similar outcomes in patients with left main disease.
Citation: Seung KB, Park D, Kim Y, Lee S. Stents versus coronary-artery bypass grafting for left main coronary artery disease. N Engl J Med. 2008;358:1781-1792.
Literature at a Glance
A guide to this month’s studies.
- Carotid stenting is equivalent to endarterectomy in carotid artery stenosis.
- Idiopathic ventricular fibrillation is associated with early repolarization.
- Aggressive LDL and blood pressure management may benefit diabetic patients.
- Treatment of hypertension in patients older than age 80 improves outcomes.
- Length of stay predicts mortality in pulmonary embolism patients.
- Poor symptom control and lack of family support during end-of-life hospital stays.
- Potentially inappropriate medication use in hospitalized elders is common.
- Steroids may not help in pediatric meningitis.
- PCI and CABG may be equivalent in the treatment of left main disease.
Is Stenting or Endarterectomy Best for Carotid Artery Stenosis?
Background: Patients with moderate to severe symptomatic carotid artery stenosis and those with severe asymptomatic carotid stenosis benefit from carotid endarterectomy. Carotid stenting may provide an alternative therapy, but the long-term protection against stroke compared with endarterectomy is unclear.
Study Design: Prospective randomized trial.
Setting: 29 centers in the United States.
Synopsis: This article reports the long-term (three years) follow-up of the SAPPHIRE trial, published in 2004, which compared carotid stenting to endarterectomy in patients at high surgical risk. In that trial, 334 patients randomized to either stenting or endarterectomy had similar outcomes at one year. Patients were followed for three years with death and major cardiovascular events as endpoints.
Rates of stroke at three years were approximately 10% with an overall death rate of approximately 20%. There was no difference between carotid stenting and endarterectomy with regards to death, stroke, or other cardiovascular outcome.
Notably, follow-up was not complete (78%), a specific type of stenting procedure was used, and the patient population was at high risk for surgical complications. Therefore, results may not be applicable in other centers or in other patient populations. Yet, this trial provides follow-up, long-term evidence that carotid stenting may be a viable alternative to endarterectomy in patients with carotid artery stenosis.
Bottom line: Carotid stenting and endarterectomy had similar outcomes at three years in high-risk patients with carotid artery stenosis.
Citation: Gurm HS, Yadav JS, Fayad P, et al. Long-term results of carotid stenting versus endarterectomy in high-risk patients. N Engl J Med. 2008;358:1572-1579.
Is Early Repolarization on EKG Associated with Sudden Cardiac Arrest?
Background: Electrocardiographic early repolarization, defined as elevation of the QRS-ST junction of at least 0.1mV from baseline in the inferior or lateral leads (manifested as slurring or notching), occurs in 1% to 5% of patients. It is considered benign, but experimental studies have suggested it may be arrhythmogenic.
Study Design: Prospective case-control.
Setting: 22 international tertiary care centers.
Synopsis: Case subjects were less than 60 years of age and were resuscitated after ventricular fibrillation (VF) arrest ultimately deemed idiopathic. All had normal echocardiograms, no evidence of coronary artery disease, and no repolarization abnormalities (including Brugada and long-QT). Of 206 patients, 31% had early repolarization on EKG, versus only 5% in controls without heart disease. In case subjects with prior EKGs, early repolarization was proven to be pre-existing.
The mean magnitude of J-point elevation was 2 mm in cases versus 1.2 mm in controls, and in cases this magnitude increased during later episodes of arrhythmia. Electrophysiologic mapping showed that ectopy originated at sites concordant with the location of abnormal repolarization. During five years of follow-up, arrhythmic recurrence was twice as common in cases with early repolarization.
Although long-term observational studies of persons with early repolarization have shown a benign natural course, this study may change our approach to those with syncope or a family history of sudden death.
Bottom line: Early repolarization on EKG is associated with idiopathic ventricular fibrillation.
Citation: Haissaguerre M, Derval N, Sacher F, et al. Sudden cardiac arrest associated with early repolarization. N Engl J Med. 2008;358(19):2016-2023.
Does Aggressive Blood Pressure and LDL Treatment in Diabetics Affect Development of Subclinical Atherosclerosis?
Background: There is evidence to suggest more aggressive treatment of LDL cholesterol in patients with known coronary artery disease is beneficial and more aggressive blood pressure control can improve outcomes in some patient populations. However, it is unclear if patients with diabetes without cardiovascular disease would benefit from more aggressive LDL and systolic blood pressure (SBP) treatment.
Study Design: Randomized, open-label, blinded-to-end point trial.
Setting: Four centers in Oklahoma, Arizona, and South Dakota.
Synopsis: Investigators studied 499 type 2 diabetic American Indian men with no history of cardiovascular disease. Patients were randomized to receive treatment to achieve aggressive (70 mg/dL and 115 mmHg) or standard (100 mg/dL and 130 mmHg) targets for their LDL cholesterol and SBP, respectively.
At three years, the aggressive group showed decreased carotid intima-media thickness (IMT) and decreased left ventricular mass, whereas both IMT and left ventricular volume increased in the standard group. There were no differences in clinical cardiovascular events between the aggressive and standard group and both groups had lower-than-expected clinical events.
This study included no women and was limited to an American Indian population. Of note, there was an increase in adverse events related to blood pressure medications in the aggressive group. It also is unclear how the surrogates of cardiovascular disease or subclinical atherosclerosis relate to significant clinical outcomes.
Bottom line: More aggressive LDL and SBP treatment in diabetics without coronary disease decreased subclinical atherosclerosis but did not impact clinical outcomes.
Citation: Howard B, Roman M, Devereux R, et al. Effect of lower targets for blood pressure and LDL cholesterol on atherosclerosis in diabetes. JAMA. 2008;299(14):1678-1689.
Should We Treat Hypertension in Patients Older Than 80?
Background: There is debate about whether treatment of hypertension in the elderly is beneficial. Numerous studies suggest blood pressure control does less to prevent strokes in patients older than 80 years than for younger patients. Moreover, other evidence shows controlling blood pressure in elderly patients may result in an increase in mortality even if there was a decreased risk of stroke.
Study Design: Randomized, double-blind, placebo-controlled trial.
Setting: 195 centers in 13 countries in Europe, China, Australasia, and North Africa.
Synopsis: This study evaluated 3,845 patients, age 80 or older, with a sustained systolic blood pressure (SBP) of 160 mmHg and randomized them to receive indapamide (sustained release) or placebo. Perindopril, or placebo, was added if necessary to achieve a target blood pressure of 150/80 mmHg. Patients who received the indapamide with or without the perindopril had lower blood pressure, lower rate of stroke, lower rate of heart failure, lower rate of death from a cardiovascular cause, and a 21% reduction in all-cause mortality (all statistically significant). There were very few adverse drug events and fewer adverse events overall in the treatment group.
Of note, exclusion criteria included a history of heart failure requiring anti-hypertensive medication, dementia, need for nursing care, an inability to stand or walk, and a creatinine more than 1.7 mg/dL. As well, the “target” SBP of 150 mmHg (which only half of the treatment group achieved) is still considered hypertensive according to the JNC 7 guidelines.
Bottom line: In some patients older than 80, treatment of hypertension may reduce the incidence of stroke, death from stroke, heart failure, and all-cause mortality.
Citation: Beckett N, Peters R, Fletcher A, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358:1887-1898.
What Is the Optimal Hospital LOS for Patients with PE?
Background: Though there are clear trends toward shorter hospital stays after pulmonary embolism (PE), especially with the introduction of low molecular weight heparin, the optimal timing of discharge and the effect of decreased length of stay (LOS) on post-discharge mortality are unknown. Furthermore, there is no risk stratification strategy used to identify low-risk patients with PE who can safely be discharged early or treated in the outpatient setting.
Study Design: Retrospective cohort study.
Setting: 186 acute care hospitals in Pennsylvania from January 2000 to November 2002.
Synopsis: Using a statewide database of 15,531 patients discharged with pulmonary embolism (PE), the authors sought to identify patient and hospital factors associated with LOS and assess whether LOS was associated with post-discharge mortality.
Findings indicate there is considerable variation in LOS for PE between and within hospitals in Pennsylvania. The median LOS for patients with PE was six days; patients with a LOS of four or fewer days had significantly higher post-discharge mortality than patients hospitalized five to eight days. More than half the patients discharged at four or fewer days were classified as high-risk, with Pulmonary Embolism Severity Index (PESI) scores of III-V (3.1% to 24.5% risk of mortality at 30 days).
Although we cannot infer causation (i.e., early discharge=death), clinicians should be aware of the results and consider severity of illness (using PESI or other criteria) in the discharge decision in patients with PE. Future prognostic models and evidence-based criteria would be helpful to identify patients with PE who can be safely discharged early.
Bottom line: Physicians may inappropriately select patients with PE for early discharge who are at increased risk of complications.
Citation: Aujesky D, Stone RA, Kim S, et al. Length of hospital stay and post-discharge mortality in patients with pulmonary embolism. Arch Intern Med. 2008;168(7):706-712.
Do Patients Have a “Good Death” in the Hospital?
Background: Despite an increasing focus on providing appropriate end-of-life care, the majority of patients in developed countries die in the hospital. The circumstances and quality of care provided at the time of death are poorly described.
Study Design: Cross-sectional survey.
Setting: 613 departments in 200 French hospitals.
Synopsis: For 3,793 in-hospital deaths, the investigators surveyed the bedside nurses about the circumstances and details of the death. Twenty-three percent of the patients were admitted for end-of-life care, 29% had a malignancy, and 50% of patients were identified as terminally ill for three days prior to their death.
A family member or relative was present in only 25% of all deaths; 20% of patients were alone at the time of death. In the last few hours of life, up to 70% of patients had symptoms of respiratory distress, while only 44% received opiate analgesia. Only 35% of nurses were satisfied with the quality of death. Satisfaction increased with presence of family members and having written protocols for care at the end of life.
This large, multicenter study has limitations but provides a concerning snapshot of death in the hospital. Hospitalists should be aggressive about symptom control at the end of life as well as attempt to ensure patients are not alone at the time of death.
Bottom line: Many patients die in the hospital in some degree of respiratory distress and without family or friends at the bedside.
Citation: Ferrand E, Jabre P, Vincent-Genod C, et al. Circumstances of death in hospitalized patients and nurses’ perceptions. Arch Intern Med. 2008;168(8):867-875.
How Common Is Potentially Inappropriate Medication Use in the Hospital?
Background: Use of potentially inappropriate medications (PIM) in the elderly based on the Beers’ List is common in nursing homes, the emergency department (ED), and outpatient settings and is associated with adverse outcomes and hospitalization. Frequency of PIM use the inpatient setting has not been well studied.
Study Design: A retrospective cohort study.
Setting: 384 U.S. hospitals.
Synopsis: In this retrospective cohort study of 493,971 inpatients (older than 65) admitted with medical diagnoses to non-surgeons, PIM prescription was evaluated. Forty nine percent of all patients were prescribed at least one PIM, while 6% were prescribed three or more. In a multivariable model, physician specialty was associated with variation in high severity PIM (HSPIM) prescription. In comparison with internal medicine physicians, cardiologists (odds ratio [OR] 1.32) and pulmonologists (OR 1.10) were more likely to prescribe HSPIMs, while hospitalists (OR 0.90) and geriatricians (OR 0.60) were less likely. In addition, patient age older than 85 was associated with decreased HSPIM prescription (OR 0.59) compared with those younger than 85.
Compared with patients in the Midwest, patients in the South (OR 1.63) and West (OR 1.43) were more likely to prescribe HSPIMs, while those in the Northeast (OR 0.85) were less likely. Hospitals with geriatric services had less PIM use. The study couldn’t account for continuation of chronic medications and did not evaluate adverse outcomes from PIM prescribing.
Bottom line: PIM prescription to hospitalized geriatric patients is common and associated with provider and hospital characteristics.
Citation: Rothberg MB, Pekow PS, Liu F, et al. Potentially inappropriate medication use in hospitalized elders. J Hosp Med. 2008;3:91-102:91-102.
Is There a Benefit to Corticosteroids When Treating Bacterial Meningitis in Children?
Background: The benefit of adjuvant corticosteroids in the treatment of bacterial meningitis in children in the developed world remains unclear; recent expert guidelines reflect this uncertainty.
Study Design: Retrospective cohort study.
Setting: Twenty-seven tertiary care hospitals in the United States.
Synopsis: Researchers examined 2,780 children with a primary diagnosis of bacterial meningitis discharged from 27 tertiary care centers in the U.S. from 2001-2006. Using a propensity analysis (to control for severity of illness), the study compared those who had received adjunctive corticosteroids with those who had not, with mortality and length of study (LOS) as primary outcomes.
The median age was nine months, 8.9% of children received corticosteroids, and the overall mortality rate was 4.2%. Adjuvent corticosteroids did not reduce mortality or LOS. The outcomes were unchanged in subgroup analyses.
Although limited by its retrospective design and lack of other outcome measures (e.g., hearing loss, neurological deficits), this study provides reasonable evidence that corticosteroid use in bacterial meningitis in children may not save lives or shorten LOS. Pediatric hospitalists may not want to routinely give steroids in this setting pending large randomized-controlled trials.
Bottom line: Adjunctive corticosteroids therapy in children with bacterial meningitis may not save lives or reduce LOS.
Citation: Mongelluzzo J, Mohamad Z, Ten Have TR, Shah SS. Corticosteroids and mortality in children with bacterial meningitis. JAMA. 2008;299(17):2048-2055.
Should Unprotected Left Main Disease Be Treated With PCI or CABG?
Background: The current standard of care for the treatment of left main coronary artery disease is coronary-artery bypass grafting (CABG). With the advent of drug-eluting stents, there is growing interest in the use of percutaneous coronary intervention (PCI) to treat left main disease.
Study Design: Prospective observational study.
Setting: Twelve Korean cardiac centers.
Synopsis: From 2000 to 2006, patients with left main disease were treated with PCI or CABG at the discretion of the physician. Nearly 1,100 patients in each cohort were compared and evaluated for death and a composite outcome of death, myocardial infarction, or stroke. Propensity-matching was employed to control for confounders.
In the overall cohort matched by propensity score, there was no significant difference in death or the composite outcome between the PCI and CABG groups after three years. Type of stent (bare metal vs. drug-eluting) did not affect the outcome. Rates of target-vessel revascularization were significantly higher in the group that received stents.
The results are limited by the observational nature and the need for propensity analysis and yet provide an intriguing result. The standard of care for treatment of left main disease remains CABG, but clinicians may be more comfortable treating with stents while we await randomized-controlled trials.
Bottom line: In this observational study, PCI and CABG had similar outcomes in patients with left main disease.
Citation: Seung KB, Park D, Kim Y, Lee S. Stents versus coronary-artery bypass grafting for left main coronary artery disease. N Engl J Med. 2008;358:1781-1792.