User login
Thromboembolism Prophylaxis in Liver Disease
Venous thromboembolism (VTE) is a major cause of morbidity and mortality in hospitalized patients.13 Major efforts are underway to increase appropriate VTE prophylaxis (VTEP)4 and adherence to VTEP guidelines are increasingly used as a quality of care measure. National 2008 VTEP guidelines suggest that all medical patients ill enough to require hospitalization, particularly those requiring admission to the Intensive Care Unit (ICU), have at least a moderate risk of developing VTE and prophylaxis is recommended.4 Hospitalized patients with end‐stage liver disease (ESLD), despite their coagulopathy, are known to be at risk for VTE48 and may be VTEP candidates.
Based on available literature, it is unknown whether pharmacologic VTEP should be utilized in acutely ill, hospitalized patients with ESLD, particularly in those admitted with variceal bleeding. These patients are at high risk for rebleeding, with the highest risk in the first 5 days.9 Early rebleeding, defined as recurrent bleeding within 6 weeks of initial bleed, declined from 47% in the 1980s to 13% by 2000 because of increased early endoscopic intervention and use of medications to prevent rebleeding.911 In multicenter cohort studies, D'Amico and De Franchis12 reported that 13% of patients with variceal bleeding had uncontrolled bleeding, rebleeding, or death within 5 days of admission while Bahmba et al.13 reported a 16% rate of rebleeding within 5 days. We are unaware of prior reports regarding the safety of VTEP in this high‐risk group of patients.
Objective
We sought to describe rebleeding in a series of 22 patients with ESLD admitted with variceal bleeding who received pharmacologic VTEP.
Methods
We identified all patients 18 years and older with upper gastrointestinal bleeding admitted to Harborview Medical Center, a 400‐bed urban county teaching hospital in Seattle, Washington, between January 1, 2003 and December 31, 2005 (Figure 1), just prior to medical center‐wide implementation of a VTEP guideline. Potential cases were identified using administrative data based on 8 discharge diagnoses (Supporting Information Appendix 1) and 10 procedure codes (Supporting Information Appendix 2).14 Inpatient pharmacy data indicating continuous octreotide infusion were used to refine the sample. At our institution, it is a standard of care to initiate octreotide in patients admitted with variceal bleeding. We excluded patients who did not have ESLD (defined as evidence of cirrhosis and associated complications including but not limited to ascites, encephalopathy, variceal bleeding, portal hypertension) documented in their problem list or past medical history and those with no variceal bleeding based on medical record review. We identified cases receiving pharmacologic VTEP, either subcutaneous unfractionated heparin (UFH) or low molecular weight heparin (LMWH), during hospitalization from pharmacy records.
We obtained demographic and clinical data from administrative billing systems, electronic and paper medical records, and inpatient pharmacy databases and verified transfusion data from the Puget Sound Blood Center. We abstracted esophagogastroduodenoscopy (EGD) findings indicating high risk of rebleeding including variceal grade and stigmata of recent bleeding such as red spots or wales.15, 16 Data were abstracted by the first 3 authors (AS, MS, KJ) and reviewed again by 2 authors (AS, KJ) blinded to the others' abstractions.
We calculated Model for ESLD (MELD) scores on admission. These scores correlate with 3 month mortality in ESLD.17 We tabulated 5 factors shown in some studies to predict bleeding including high International Normalized Ratio (INR) (>1.5), low hematocrit (<25%), low platelet count (<100,000 per microliter), active bleeding at EGD, and transfusion of four or more units of red cells within 24 hours of admission.1013
We defined rebleeding as a decrease in hematocrit of greater than 5 percentage points compared with postresuscitation hematocrit, transfusion of additional red cells more than 48 hours after initial resuscitation, repeat unscheduled EGD, or return to the ICU for therapies related to rebleeding.18 The University of Washington Human Subjects Board approved this study.
Results
Of 224 patients initially identified, 36 received pharmacologic VTEP. We excluded 14 who did not have ESLD (n = 1) or did not have a variceal bleed (n = 13). The remaining 22 patients form the sample described in Figure 1.
The median age of patients was 52 years (range 42‐85) and 77% were men (Table 1). Twenty‐one of 22 patients (95%) were initially admitted to the ICU; median length of stay was 8 days (range 4‐30). Median MELD score on admission was 15 (range 825). On EGD, the number of variceal columns ranged from 1 to 4; 17 patients (77%) had at least 3. A total of 15 patients (68%) had stigmata of recent bleeding and 16 (72%) underwent banding (range 16 bands). All patients had at least 1 bleeding risk factor (Table 1) of which the most common factors observed were initial transfusion of 4 or more units of red cells (50%, n = 11), INR > 1.5 (45%, n = 10), and hematocrit < 25% (45%, n = 10).
| Parameter | Range | Median Value/% | Interquartile Range | Mean | Standard Deviation |
|---|---|---|---|---|---|
| |||||
| Age (years) | 4285 | 52 | 4758 | 53 | 9 |
| Sex (men) | 17 | 77% | |||
| MELD scores | 825 | 14.5 | 1120 | 15 | 5 |
| Initial ICU admission | 21 | 95% | |||
| Hospital length of stay (days) | 430 | 8 | 9.9 | 6.7 | |
| Initial INR | 1.12.4 | 1.5 | 1.42.0 | 1.7 | 0.4 |
| Initial hematocrit (%) | 1444 | 26 | 2232 | 27 | 8 |
| Initial platelets (thousand/L) | 43494 | 131 | 83159 | 147 | 98 |
| EGD results | |||||
| Grade 1 | 3 | 14% | |||
| Grade 2 | 6 | 27% | |||
| Grade 3 | 12 | 55% | |||
| Grade 4 | 1 | 5% | |||
| Stigmata of recent bleeding | 15 | 68% | |||
| Number of risk factors for rebleeding* | |||||
| 0 | 0 | 0% | |||
| 1 | 9 | 41% | |||
| 2 | 7 | 32% | |||
| 3 | 5 | 23% | |||
| 4 | 1 | 4% | |||
| Initial transfusion red blood cells | |||||
| None | 2 | 9% | |||
| 13 units | 9 | 41% | |||
| 4+ units | 11 | 50% | |||
| Initial transfusion frozen plasma | |||||
| None | 10 | 45% | |||
| 14 units | 3 | 14% | |||
| 58 units | 6 | 27% | |||
| 9+ units | 4 | 18% | |||
| Initial transfusion platelets | |||||
| None | 13 | 59% | |||
| 14 units | 4 | 18% | |||
| 5+ units | 5 | 23% | |||
A total of 12 patients (55%) received 5000 units of UFH every 8 hours, 8 (36%) received 5000 units UFH every 12 hours, and 2 (9%) received LMWH. VTEP was initiated as early as day of admission and as late as day 19. Median VTEP start date was hospital day 4. Median duration of of VTEP was 5 days.
Only 1 patient (4.5%) rebled after VTEP initiation. The patient received UFH every 8 hours starting on hospital day 6, and rebleeding occurred on day 9. Repeat EGD showed ulcers at banding sites. The patient was restarted on VTEP on hospital day 13 without recurrence of rebleeding. This patient had a MELD score of 24, initial INR >2, hematocrit <25%, had grade 3 varices and stigmata of recent bleeding on EGD, and received 4 units of packed red cells. These values are similar to those of the cohort as a whole (Table 1). This patient also was diagnosed with DVT while receiving VTEP on hospital day 15. This patient's coagulopathy was in the setting of terminal illness; the patient expired on hospital day 25.
One additional patient rebled prior to VTEP initiation on day 3 with repeat EGD showing a bleeding varix. This patient was nevertheless started on VTEP 4 days after rebleeding. Despite use of VTEP, this patient was diagnosed with DVT on hospital day 9 (and may well have had the DVT at the time of VTEP initiation). The patient was transitioned to therapeutic dose heparin which was tolerated without recurrence of rebleeding.
There were no other confirmed cases of DVT in this series. One additional patient underwent angiogram that showed no pulmonary embolism; 2 other patients underwent lower extremity ultrasounds that were negative for DVT.
Discussion
At our medical center, only a few inpatients with ESLD admitted with variceal bleed received VTEP. These patients were seemingly at high risk for bleeding and rebleeding given high MELD scores, variceal bleeding, and presence of at least one clinical factor suggesting bleeding risk, and in several cases 3 or more such factors.13, 18 Despite this, only 1 patient rebled while receiving VTEP. We captured rebleeding rates only during the index hospitalization. We therefore may underestimate early rebleeding rates.1013 Nevertheless, our inpatient data included complete coverage of the earliest period after the index bleeds and the period during which patients were exposed to VTEP, which should be the time of highest rebleeding risk related to VTEP exposure. Interestingly the patient who rebled while on VTEP was also diagnosed with VTE while on VTEP. Two patients (9%) in our sample were diagnosed with VTE.
This case series is limited by its small sample size, retrospective nature, single center observation, and perhaps especially by possible selection bias. We were unable to specifically quantify rebleeding risk. Several authors have identified individual factors associated with rebleeding,1013 these were tabulated for patients in this case series (Table 1) and all patients had at least 1 of these factors. Concurrent infection and hepatic vein pressure gradient have been shown to predict rebleeding;9, 19 we were unable to identify these factors in our data.
There was considerable variability in this case series in timing of VTEP initiation relative to initial bleed. We were unable to characterize provider or patient characteristics that may have influenced the decision to initiate VTEP and timing. The sample size was also too small to comment upon factors associated with choice of UFH versus LMWH and any potential differences in rebleeding risk between the 2. We also did not look at outcomes postindex hospitalization so we can not comment on the extended risk of rebleeding with VTEP after discharge. However, the risk of rebleeding is highest within the first 96 hours13 and all patients in this series were hospitalized at least 4 days. Nonetheless, we captured all patients with ESLD and variceal bleeding exposed to VTEP at a large center over a three‐year period and found rebleeding rates less than what might be expected.
Conclusions
Our observations suggest that some inpatients with ESLD and variceal bleeding may tolerate pharmacologic VTEP. In this small group of patients, VTEP was associated with an unexpectedly low incidence of rebleeding. While this case series does not support broad use of VTEP in this population, the lower‐than‐expected rates of rebleeding suggest that further study of the safety and effectiveness of pharmacologic VTEP in inpatient populations with ESLD may be warranted, particularly given the recommendations of recent national VTE prophylaxis guidelines.4
- ,,, et al.Validation of a model to predict adverse outcomes in patients with pulmonary embolism.Eur Heart J.2006;27(4):476–481.
- .The epidemiology of venous thromboembolism.Circulation.2003;107(23 Suppl 1):I4–I8.
- ,,,,.The prevalence of risk factors for venous thromboembolism among hospital patients.Arch Intern Med.1992;152(8):1660–1664.
- ,,, et al.Prevention of venous thromboembolism: American College of Chest Physicians Evidence‐Based Clinical Practice Guidelines. 8th Edition.Chest.2008;133(6 Suppl):381S–453S.
- ,,, et al.Coagulopathy does not fully protect hospitalized cirrhosis patients from peripheral venous thromboembolism.Am J Gastroenterol.2006;101(7):1524–1528; quiz 680.
- ,,,.Coagulation disorders in liver disease.Semin Liver Dis.2002;22(1):83–96.
- ,,,,.Deep vein thrombosis and pulmonary embolism in cirrhosis patients.Dig Dis Sci.2008;53(11):3012–3017.
- ,,,,,.Risk of venous thromboembolism in patients with liver disease: a nationwide population‐based case‐control study.Am J Gastroenterol.2009;104(1):96–101.
- ,.Non‐invasive diagnosis of cirrhosis and the natural history of its complications.Best Pract Res Clin Gastroenterol.2007;21(1):3–18.
- ,,,et al.Improved patient survival after acute variceal bleeding: a multicenter, cohort study.Am J Gastroenterol.2003;98(3):653–659.
- ,,,,,.Improved survival after variceal bleeding in patients with cirrhosis over the past two decades.Hepatology.2004;40(3):652–659.
- ,.Upper digestive bleeding in cirrhosis. Post‐therapeutic outcome and prognostic indicators.Hepatology.2003;38(3):599–612.
- ,,,,,.Predictors of early re‐bleeding and mortality after acute variceal haemorrhage in patients with cirrhosis.Gut.2008;57(6):814–820.
- ,,,,,.Use of hospital administrative data to assess quality improvement initiatives.J Gen Intern Med.2007;22(Supplement).
- ,.UK guidelines on the management of variceal haemorrhage in cirrhotic patients.Gut.2000,year="2000"2000;46(90003):iii1–15.
- ,,,,,.Prognostic significance of the white nipple sign in variceal bleeding.Gastrointest Endosc.1991;37(1):51–55.
- ,,, et al.A model to predict survival in patients with end‐stage liver disease.Hepatology.2001;33(2):464–470.
- .Evolving consensus in portal hypertension. Report of the Baveno IV consensus workshop on methodology of diagnosis and therapy in portal hypertension.J Hepatol.2005;43(1):167–176.
- ,,, et al.Antibiotic prophylaxis after endoscopic therapy prevents rebleeding in acute variceal hemorrhage: a randomized trial.Hepatology.2004;39(3):746–753.
Venous thromboembolism (VTE) is a major cause of morbidity and mortality in hospitalized patients.13 Major efforts are underway to increase appropriate VTE prophylaxis (VTEP)4 and adherence to VTEP guidelines are increasingly used as a quality of care measure. National 2008 VTEP guidelines suggest that all medical patients ill enough to require hospitalization, particularly those requiring admission to the Intensive Care Unit (ICU), have at least a moderate risk of developing VTE and prophylaxis is recommended.4 Hospitalized patients with end‐stage liver disease (ESLD), despite their coagulopathy, are known to be at risk for VTE48 and may be VTEP candidates.
Based on available literature, it is unknown whether pharmacologic VTEP should be utilized in acutely ill, hospitalized patients with ESLD, particularly in those admitted with variceal bleeding. These patients are at high risk for rebleeding, with the highest risk in the first 5 days.9 Early rebleeding, defined as recurrent bleeding within 6 weeks of initial bleed, declined from 47% in the 1980s to 13% by 2000 because of increased early endoscopic intervention and use of medications to prevent rebleeding.911 In multicenter cohort studies, D'Amico and De Franchis12 reported that 13% of patients with variceal bleeding had uncontrolled bleeding, rebleeding, or death within 5 days of admission while Bahmba et al.13 reported a 16% rate of rebleeding within 5 days. We are unaware of prior reports regarding the safety of VTEP in this high‐risk group of patients.
Objective
We sought to describe rebleeding in a series of 22 patients with ESLD admitted with variceal bleeding who received pharmacologic VTEP.
Methods
We identified all patients 18 years and older with upper gastrointestinal bleeding admitted to Harborview Medical Center, a 400‐bed urban county teaching hospital in Seattle, Washington, between January 1, 2003 and December 31, 2005 (Figure 1), just prior to medical center‐wide implementation of a VTEP guideline. Potential cases were identified using administrative data based on 8 discharge diagnoses (Supporting Information Appendix 1) and 10 procedure codes (Supporting Information Appendix 2).14 Inpatient pharmacy data indicating continuous octreotide infusion were used to refine the sample. At our institution, it is a standard of care to initiate octreotide in patients admitted with variceal bleeding. We excluded patients who did not have ESLD (defined as evidence of cirrhosis and associated complications including but not limited to ascites, encephalopathy, variceal bleeding, portal hypertension) documented in their problem list or past medical history and those with no variceal bleeding based on medical record review. We identified cases receiving pharmacologic VTEP, either subcutaneous unfractionated heparin (UFH) or low molecular weight heparin (LMWH), during hospitalization from pharmacy records.
We obtained demographic and clinical data from administrative billing systems, electronic and paper medical records, and inpatient pharmacy databases and verified transfusion data from the Puget Sound Blood Center. We abstracted esophagogastroduodenoscopy (EGD) findings indicating high risk of rebleeding including variceal grade and stigmata of recent bleeding such as red spots or wales.15, 16 Data were abstracted by the first 3 authors (AS, MS, KJ) and reviewed again by 2 authors (AS, KJ) blinded to the others' abstractions.
We calculated Model for ESLD (MELD) scores on admission. These scores correlate with 3 month mortality in ESLD.17 We tabulated 5 factors shown in some studies to predict bleeding including high International Normalized Ratio (INR) (>1.5), low hematocrit (<25%), low platelet count (<100,000 per microliter), active bleeding at EGD, and transfusion of four or more units of red cells within 24 hours of admission.1013
We defined rebleeding as a decrease in hematocrit of greater than 5 percentage points compared with postresuscitation hematocrit, transfusion of additional red cells more than 48 hours after initial resuscitation, repeat unscheduled EGD, or return to the ICU for therapies related to rebleeding.18 The University of Washington Human Subjects Board approved this study.
Results
Of 224 patients initially identified, 36 received pharmacologic VTEP. We excluded 14 who did not have ESLD (n = 1) or did not have a variceal bleed (n = 13). The remaining 22 patients form the sample described in Figure 1.
The median age of patients was 52 years (range 42‐85) and 77% were men (Table 1). Twenty‐one of 22 patients (95%) were initially admitted to the ICU; median length of stay was 8 days (range 4‐30). Median MELD score on admission was 15 (range 825). On EGD, the number of variceal columns ranged from 1 to 4; 17 patients (77%) had at least 3. A total of 15 patients (68%) had stigmata of recent bleeding and 16 (72%) underwent banding (range 16 bands). All patients had at least 1 bleeding risk factor (Table 1) of which the most common factors observed were initial transfusion of 4 or more units of red cells (50%, n = 11), INR > 1.5 (45%, n = 10), and hematocrit < 25% (45%, n = 10).
| Parameter | Range | Median Value/% | Interquartile Range | Mean | Standard Deviation |
|---|---|---|---|---|---|
| |||||
| Age (years) | 4285 | 52 | 4758 | 53 | 9 |
| Sex (men) | 17 | 77% | |||
| MELD scores | 825 | 14.5 | 1120 | 15 | 5 |
| Initial ICU admission | 21 | 95% | |||
| Hospital length of stay (days) | 430 | 8 | 9.9 | 6.7 | |
| Initial INR | 1.12.4 | 1.5 | 1.42.0 | 1.7 | 0.4 |
| Initial hematocrit (%) | 1444 | 26 | 2232 | 27 | 8 |
| Initial platelets (thousand/L) | 43494 | 131 | 83159 | 147 | 98 |
| EGD results | |||||
| Grade 1 | 3 | 14% | |||
| Grade 2 | 6 | 27% | |||
| Grade 3 | 12 | 55% | |||
| Grade 4 | 1 | 5% | |||
| Stigmata of recent bleeding | 15 | 68% | |||
| Number of risk factors for rebleeding* | |||||
| 0 | 0 | 0% | |||
| 1 | 9 | 41% | |||
| 2 | 7 | 32% | |||
| 3 | 5 | 23% | |||
| 4 | 1 | 4% | |||
| Initial transfusion red blood cells | |||||
| None | 2 | 9% | |||
| 13 units | 9 | 41% | |||
| 4+ units | 11 | 50% | |||
| Initial transfusion frozen plasma | |||||
| None | 10 | 45% | |||
| 14 units | 3 | 14% | |||
| 58 units | 6 | 27% | |||
| 9+ units | 4 | 18% | |||
| Initial transfusion platelets | |||||
| None | 13 | 59% | |||
| 14 units | 4 | 18% | |||
| 5+ units | 5 | 23% | |||
A total of 12 patients (55%) received 5000 units of UFH every 8 hours, 8 (36%) received 5000 units UFH every 12 hours, and 2 (9%) received LMWH. VTEP was initiated as early as day of admission and as late as day 19. Median VTEP start date was hospital day 4. Median duration of of VTEP was 5 days.
Only 1 patient (4.5%) rebled after VTEP initiation. The patient received UFH every 8 hours starting on hospital day 6, and rebleeding occurred on day 9. Repeat EGD showed ulcers at banding sites. The patient was restarted on VTEP on hospital day 13 without recurrence of rebleeding. This patient had a MELD score of 24, initial INR >2, hematocrit <25%, had grade 3 varices and stigmata of recent bleeding on EGD, and received 4 units of packed red cells. These values are similar to those of the cohort as a whole (Table 1). This patient also was diagnosed with DVT while receiving VTEP on hospital day 15. This patient's coagulopathy was in the setting of terminal illness; the patient expired on hospital day 25.
One additional patient rebled prior to VTEP initiation on day 3 with repeat EGD showing a bleeding varix. This patient was nevertheless started on VTEP 4 days after rebleeding. Despite use of VTEP, this patient was diagnosed with DVT on hospital day 9 (and may well have had the DVT at the time of VTEP initiation). The patient was transitioned to therapeutic dose heparin which was tolerated without recurrence of rebleeding.
There were no other confirmed cases of DVT in this series. One additional patient underwent angiogram that showed no pulmonary embolism; 2 other patients underwent lower extremity ultrasounds that were negative for DVT.
Discussion
At our medical center, only a few inpatients with ESLD admitted with variceal bleed received VTEP. These patients were seemingly at high risk for bleeding and rebleeding given high MELD scores, variceal bleeding, and presence of at least one clinical factor suggesting bleeding risk, and in several cases 3 or more such factors.13, 18 Despite this, only 1 patient rebled while receiving VTEP. We captured rebleeding rates only during the index hospitalization. We therefore may underestimate early rebleeding rates.1013 Nevertheless, our inpatient data included complete coverage of the earliest period after the index bleeds and the period during which patients were exposed to VTEP, which should be the time of highest rebleeding risk related to VTEP exposure. Interestingly the patient who rebled while on VTEP was also diagnosed with VTE while on VTEP. Two patients (9%) in our sample were diagnosed with VTE.
This case series is limited by its small sample size, retrospective nature, single center observation, and perhaps especially by possible selection bias. We were unable to specifically quantify rebleeding risk. Several authors have identified individual factors associated with rebleeding,1013 these were tabulated for patients in this case series (Table 1) and all patients had at least 1 of these factors. Concurrent infection and hepatic vein pressure gradient have been shown to predict rebleeding;9, 19 we were unable to identify these factors in our data.
There was considerable variability in this case series in timing of VTEP initiation relative to initial bleed. We were unable to characterize provider or patient characteristics that may have influenced the decision to initiate VTEP and timing. The sample size was also too small to comment upon factors associated with choice of UFH versus LMWH and any potential differences in rebleeding risk between the 2. We also did not look at outcomes postindex hospitalization so we can not comment on the extended risk of rebleeding with VTEP after discharge. However, the risk of rebleeding is highest within the first 96 hours13 and all patients in this series were hospitalized at least 4 days. Nonetheless, we captured all patients with ESLD and variceal bleeding exposed to VTEP at a large center over a three‐year period and found rebleeding rates less than what might be expected.
Conclusions
Our observations suggest that some inpatients with ESLD and variceal bleeding may tolerate pharmacologic VTEP. In this small group of patients, VTEP was associated with an unexpectedly low incidence of rebleeding. While this case series does not support broad use of VTEP in this population, the lower‐than‐expected rates of rebleeding suggest that further study of the safety and effectiveness of pharmacologic VTEP in inpatient populations with ESLD may be warranted, particularly given the recommendations of recent national VTE prophylaxis guidelines.4
Venous thromboembolism (VTE) is a major cause of morbidity and mortality in hospitalized patients.13 Major efforts are underway to increase appropriate VTE prophylaxis (VTEP)4 and adherence to VTEP guidelines are increasingly used as a quality of care measure. National 2008 VTEP guidelines suggest that all medical patients ill enough to require hospitalization, particularly those requiring admission to the Intensive Care Unit (ICU), have at least a moderate risk of developing VTE and prophylaxis is recommended.4 Hospitalized patients with end‐stage liver disease (ESLD), despite their coagulopathy, are known to be at risk for VTE48 and may be VTEP candidates.
Based on available literature, it is unknown whether pharmacologic VTEP should be utilized in acutely ill, hospitalized patients with ESLD, particularly in those admitted with variceal bleeding. These patients are at high risk for rebleeding, with the highest risk in the first 5 days.9 Early rebleeding, defined as recurrent bleeding within 6 weeks of initial bleed, declined from 47% in the 1980s to 13% by 2000 because of increased early endoscopic intervention and use of medications to prevent rebleeding.911 In multicenter cohort studies, D'Amico and De Franchis12 reported that 13% of patients with variceal bleeding had uncontrolled bleeding, rebleeding, or death within 5 days of admission while Bahmba et al.13 reported a 16% rate of rebleeding within 5 days. We are unaware of prior reports regarding the safety of VTEP in this high‐risk group of patients.
Objective
We sought to describe rebleeding in a series of 22 patients with ESLD admitted with variceal bleeding who received pharmacologic VTEP.
Methods
We identified all patients 18 years and older with upper gastrointestinal bleeding admitted to Harborview Medical Center, a 400‐bed urban county teaching hospital in Seattle, Washington, between January 1, 2003 and December 31, 2005 (Figure 1), just prior to medical center‐wide implementation of a VTEP guideline. Potential cases were identified using administrative data based on 8 discharge diagnoses (Supporting Information Appendix 1) and 10 procedure codes (Supporting Information Appendix 2).14 Inpatient pharmacy data indicating continuous octreotide infusion were used to refine the sample. At our institution, it is a standard of care to initiate octreotide in patients admitted with variceal bleeding. We excluded patients who did not have ESLD (defined as evidence of cirrhosis and associated complications including but not limited to ascites, encephalopathy, variceal bleeding, portal hypertension) documented in their problem list or past medical history and those with no variceal bleeding based on medical record review. We identified cases receiving pharmacologic VTEP, either subcutaneous unfractionated heparin (UFH) or low molecular weight heparin (LMWH), during hospitalization from pharmacy records.
We obtained demographic and clinical data from administrative billing systems, electronic and paper medical records, and inpatient pharmacy databases and verified transfusion data from the Puget Sound Blood Center. We abstracted esophagogastroduodenoscopy (EGD) findings indicating high risk of rebleeding including variceal grade and stigmata of recent bleeding such as red spots or wales.15, 16 Data were abstracted by the first 3 authors (AS, MS, KJ) and reviewed again by 2 authors (AS, KJ) blinded to the others' abstractions.
We calculated Model for ESLD (MELD) scores on admission. These scores correlate with 3 month mortality in ESLD.17 We tabulated 5 factors shown in some studies to predict bleeding including high International Normalized Ratio (INR) (>1.5), low hematocrit (<25%), low platelet count (<100,000 per microliter), active bleeding at EGD, and transfusion of four or more units of red cells within 24 hours of admission.1013
We defined rebleeding as a decrease in hematocrit of greater than 5 percentage points compared with postresuscitation hematocrit, transfusion of additional red cells more than 48 hours after initial resuscitation, repeat unscheduled EGD, or return to the ICU for therapies related to rebleeding.18 The University of Washington Human Subjects Board approved this study.
Results
Of 224 patients initially identified, 36 received pharmacologic VTEP. We excluded 14 who did not have ESLD (n = 1) or did not have a variceal bleed (n = 13). The remaining 22 patients form the sample described in Figure 1.
The median age of patients was 52 years (range 42‐85) and 77% were men (Table 1). Twenty‐one of 22 patients (95%) were initially admitted to the ICU; median length of stay was 8 days (range 4‐30). Median MELD score on admission was 15 (range 825). On EGD, the number of variceal columns ranged from 1 to 4; 17 patients (77%) had at least 3. A total of 15 patients (68%) had stigmata of recent bleeding and 16 (72%) underwent banding (range 16 bands). All patients had at least 1 bleeding risk factor (Table 1) of which the most common factors observed were initial transfusion of 4 or more units of red cells (50%, n = 11), INR > 1.5 (45%, n = 10), and hematocrit < 25% (45%, n = 10).
| Parameter | Range | Median Value/% | Interquartile Range | Mean | Standard Deviation |
|---|---|---|---|---|---|
| |||||
| Age (years) | 4285 | 52 | 4758 | 53 | 9 |
| Sex (men) | 17 | 77% | |||
| MELD scores | 825 | 14.5 | 1120 | 15 | 5 |
| Initial ICU admission | 21 | 95% | |||
| Hospital length of stay (days) | 430 | 8 | 9.9 | 6.7 | |
| Initial INR | 1.12.4 | 1.5 | 1.42.0 | 1.7 | 0.4 |
| Initial hematocrit (%) | 1444 | 26 | 2232 | 27 | 8 |
| Initial platelets (thousand/L) | 43494 | 131 | 83159 | 147 | 98 |
| EGD results | |||||
| Grade 1 | 3 | 14% | |||
| Grade 2 | 6 | 27% | |||
| Grade 3 | 12 | 55% | |||
| Grade 4 | 1 | 5% | |||
| Stigmata of recent bleeding | 15 | 68% | |||
| Number of risk factors for rebleeding* | |||||
| 0 | 0 | 0% | |||
| 1 | 9 | 41% | |||
| 2 | 7 | 32% | |||
| 3 | 5 | 23% | |||
| 4 | 1 | 4% | |||
| Initial transfusion red blood cells | |||||
| None | 2 | 9% | |||
| 13 units | 9 | 41% | |||
| 4+ units | 11 | 50% | |||
| Initial transfusion frozen plasma | |||||
| None | 10 | 45% | |||
| 14 units | 3 | 14% | |||
| 58 units | 6 | 27% | |||
| 9+ units | 4 | 18% | |||
| Initial transfusion platelets | |||||
| None | 13 | 59% | |||
| 14 units | 4 | 18% | |||
| 5+ units | 5 | 23% | |||
A total of 12 patients (55%) received 5000 units of UFH every 8 hours, 8 (36%) received 5000 units UFH every 12 hours, and 2 (9%) received LMWH. VTEP was initiated as early as day of admission and as late as day 19. Median VTEP start date was hospital day 4. Median duration of of VTEP was 5 days.
Only 1 patient (4.5%) rebled after VTEP initiation. The patient received UFH every 8 hours starting on hospital day 6, and rebleeding occurred on day 9. Repeat EGD showed ulcers at banding sites. The patient was restarted on VTEP on hospital day 13 without recurrence of rebleeding. This patient had a MELD score of 24, initial INR >2, hematocrit <25%, had grade 3 varices and stigmata of recent bleeding on EGD, and received 4 units of packed red cells. These values are similar to those of the cohort as a whole (Table 1). This patient also was diagnosed with DVT while receiving VTEP on hospital day 15. This patient's coagulopathy was in the setting of terminal illness; the patient expired on hospital day 25.
One additional patient rebled prior to VTEP initiation on day 3 with repeat EGD showing a bleeding varix. This patient was nevertheless started on VTEP 4 days after rebleeding. Despite use of VTEP, this patient was diagnosed with DVT on hospital day 9 (and may well have had the DVT at the time of VTEP initiation). The patient was transitioned to therapeutic dose heparin which was tolerated without recurrence of rebleeding.
There were no other confirmed cases of DVT in this series. One additional patient underwent angiogram that showed no pulmonary embolism; 2 other patients underwent lower extremity ultrasounds that were negative for DVT.
Discussion
At our medical center, only a few inpatients with ESLD admitted with variceal bleed received VTEP. These patients were seemingly at high risk for bleeding and rebleeding given high MELD scores, variceal bleeding, and presence of at least one clinical factor suggesting bleeding risk, and in several cases 3 or more such factors.13, 18 Despite this, only 1 patient rebled while receiving VTEP. We captured rebleeding rates only during the index hospitalization. We therefore may underestimate early rebleeding rates.1013 Nevertheless, our inpatient data included complete coverage of the earliest period after the index bleeds and the period during which patients were exposed to VTEP, which should be the time of highest rebleeding risk related to VTEP exposure. Interestingly the patient who rebled while on VTEP was also diagnosed with VTE while on VTEP. Two patients (9%) in our sample were diagnosed with VTE.
This case series is limited by its small sample size, retrospective nature, single center observation, and perhaps especially by possible selection bias. We were unable to specifically quantify rebleeding risk. Several authors have identified individual factors associated with rebleeding,1013 these were tabulated for patients in this case series (Table 1) and all patients had at least 1 of these factors. Concurrent infection and hepatic vein pressure gradient have been shown to predict rebleeding;9, 19 we were unable to identify these factors in our data.
There was considerable variability in this case series in timing of VTEP initiation relative to initial bleed. We were unable to characterize provider or patient characteristics that may have influenced the decision to initiate VTEP and timing. The sample size was also too small to comment upon factors associated with choice of UFH versus LMWH and any potential differences in rebleeding risk between the 2. We also did not look at outcomes postindex hospitalization so we can not comment on the extended risk of rebleeding with VTEP after discharge. However, the risk of rebleeding is highest within the first 96 hours13 and all patients in this series were hospitalized at least 4 days. Nonetheless, we captured all patients with ESLD and variceal bleeding exposed to VTEP at a large center over a three‐year period and found rebleeding rates less than what might be expected.
Conclusions
Our observations suggest that some inpatients with ESLD and variceal bleeding may tolerate pharmacologic VTEP. In this small group of patients, VTEP was associated with an unexpectedly low incidence of rebleeding. While this case series does not support broad use of VTEP in this population, the lower‐than‐expected rates of rebleeding suggest that further study of the safety and effectiveness of pharmacologic VTEP in inpatient populations with ESLD may be warranted, particularly given the recommendations of recent national VTE prophylaxis guidelines.4
- ,,, et al.Validation of a model to predict adverse outcomes in patients with pulmonary embolism.Eur Heart J.2006;27(4):476–481.
- .The epidemiology of venous thromboembolism.Circulation.2003;107(23 Suppl 1):I4–I8.
- ,,,,.The prevalence of risk factors for venous thromboembolism among hospital patients.Arch Intern Med.1992;152(8):1660–1664.
- ,,, et al.Prevention of venous thromboembolism: American College of Chest Physicians Evidence‐Based Clinical Practice Guidelines. 8th Edition.Chest.2008;133(6 Suppl):381S–453S.
- ,,, et al.Coagulopathy does not fully protect hospitalized cirrhosis patients from peripheral venous thromboembolism.Am J Gastroenterol.2006;101(7):1524–1528; quiz 680.
- ,,,.Coagulation disorders in liver disease.Semin Liver Dis.2002;22(1):83–96.
- ,,,,.Deep vein thrombosis and pulmonary embolism in cirrhosis patients.Dig Dis Sci.2008;53(11):3012–3017.
- ,,,,,.Risk of venous thromboembolism in patients with liver disease: a nationwide population‐based case‐control study.Am J Gastroenterol.2009;104(1):96–101.
- ,.Non‐invasive diagnosis of cirrhosis and the natural history of its complications.Best Pract Res Clin Gastroenterol.2007;21(1):3–18.
- ,,,et al.Improved patient survival after acute variceal bleeding: a multicenter, cohort study.Am J Gastroenterol.2003;98(3):653–659.
- ,,,,,.Improved survival after variceal bleeding in patients with cirrhosis over the past two decades.Hepatology.2004;40(3):652–659.
- ,.Upper digestive bleeding in cirrhosis. Post‐therapeutic outcome and prognostic indicators.Hepatology.2003;38(3):599–612.
- ,,,,,.Predictors of early re‐bleeding and mortality after acute variceal haemorrhage in patients with cirrhosis.Gut.2008;57(6):814–820.
- ,,,,,.Use of hospital administrative data to assess quality improvement initiatives.J Gen Intern Med.2007;22(Supplement).
- ,.UK guidelines on the management of variceal haemorrhage in cirrhotic patients.Gut.2000,year="2000"2000;46(90003):iii1–15.
- ,,,,,.Prognostic significance of the white nipple sign in variceal bleeding.Gastrointest Endosc.1991;37(1):51–55.
- ,,, et al.A model to predict survival in patients with end‐stage liver disease.Hepatology.2001;33(2):464–470.
- .Evolving consensus in portal hypertension. Report of the Baveno IV consensus workshop on methodology of diagnosis and therapy in portal hypertension.J Hepatol.2005;43(1):167–176.
- ,,, et al.Antibiotic prophylaxis after endoscopic therapy prevents rebleeding in acute variceal hemorrhage: a randomized trial.Hepatology.2004;39(3):746–753.
- ,,, et al.Validation of a model to predict adverse outcomes in patients with pulmonary embolism.Eur Heart J.2006;27(4):476–481.
- .The epidemiology of venous thromboembolism.Circulation.2003;107(23 Suppl 1):I4–I8.
- ,,,,.The prevalence of risk factors for venous thromboembolism among hospital patients.Arch Intern Med.1992;152(8):1660–1664.
- ,,, et al.Prevention of venous thromboembolism: American College of Chest Physicians Evidence‐Based Clinical Practice Guidelines. 8th Edition.Chest.2008;133(6 Suppl):381S–453S.
- ,,, et al.Coagulopathy does not fully protect hospitalized cirrhosis patients from peripheral venous thromboembolism.Am J Gastroenterol.2006;101(7):1524–1528; quiz 680.
- ,,,.Coagulation disorders in liver disease.Semin Liver Dis.2002;22(1):83–96.
- ,,,,.Deep vein thrombosis and pulmonary embolism in cirrhosis patients.Dig Dis Sci.2008;53(11):3012–3017.
- ,,,,,.Risk of venous thromboembolism in patients with liver disease: a nationwide population‐based case‐control study.Am J Gastroenterol.2009;104(1):96–101.
- ,.Non‐invasive diagnosis of cirrhosis and the natural history of its complications.Best Pract Res Clin Gastroenterol.2007;21(1):3–18.
- ,,,et al.Improved patient survival after acute variceal bleeding: a multicenter, cohort study.Am J Gastroenterol.2003;98(3):653–659.
- ,,,,,.Improved survival after variceal bleeding in patients with cirrhosis over the past two decades.Hepatology.2004;40(3):652–659.
- ,.Upper digestive bleeding in cirrhosis. Post‐therapeutic outcome and prognostic indicators.Hepatology.2003;38(3):599–612.
- ,,,,,.Predictors of early re‐bleeding and mortality after acute variceal haemorrhage in patients with cirrhosis.Gut.2008;57(6):814–820.
- ,,,,,.Use of hospital administrative data to assess quality improvement initiatives.J Gen Intern Med.2007;22(Supplement).
- ,.UK guidelines on the management of variceal haemorrhage in cirrhotic patients.Gut.2000,year="2000"2000;46(90003):iii1–15.
- ,,,,,.Prognostic significance of the white nipple sign in variceal bleeding.Gastrointest Endosc.1991;37(1):51–55.
- ,,, et al.A model to predict survival in patients with end‐stage liver disease.Hepatology.2001;33(2):464–470.
- .Evolving consensus in portal hypertension. Report of the Baveno IV consensus workshop on methodology of diagnosis and therapy in portal hypertension.J Hepatol.2005;43(1):167–176.
- ,,, et al.Antibiotic prophylaxis after endoscopic therapy prevents rebleeding in acute variceal hemorrhage: a randomized trial.Hepatology.2004;39(3):746–753.
Spontaneous Retroperitoneal Hematoma
A 56‐year‐old male presented to the emergency department with a 2‐week history of increasing abdominal girth, nausea, vomiting, and lower extremity edema. His girlfriend had also noted a yellow tinge to his skin and eyes. His past medical history was significant for bipolar disorder, alcohol‐related seizures, and pneumonia. He had no allergies and denied medications prior to admission. Family history was negative for liver disease and social history was notable for ongoing tobacco use and alcohol dependence. He was afebrile with stable vital signs. Physical examination demonstrated an alert gentleman whose answers to questions required occasional factual correction by his partner. His abdomen was distended and nontender with prominent vasculature and shifting dullness. Lower extremity edema was symmetric and bilateral, rated as 2+. Scattered spider angiomata and a fine bilateral hand tremor without asterixis were also noted. Initial laboratory data demonstrated a white blood cell count of 13,900/L, hematocrit 37%, and platelet count 176,000/L. His sodium was 130 mg/dL, blood urea nitrogen (BUN) 1 mg/dL, and creatinine 0.7 mg/dL. International normalized ratio (INR) was 1.8, aspartate aminotransferase (AST) was 117 U/L, alanine aminotransferase (ALT) 33 U/L, alkaline phosphatase 191 U/L, total bilirubin 9.2 mg/dL, total protein 7.0 g/dL, and albumin 1.9 g/dL. Abdominal ultrasound revealed a diffusely hyperechoic liver with a large amount of ascites.
The patient was admitted with the diagnoses of presumed alcoholic hepatitis and end‐stage liver disease. Model for End‐Stage Liver Disease (MELD) score was 21 and discriminant function 16.8. Paracentesis demonstrated a serum‐ascites albumin gradient of >1.1 and no evidence of spontaneous bacterial peritonitis. Diuresis was initiated. He was placed on unfractionated heparin at a dose of 5000 units every 8 hours for deep venous thrombosis (DVT) prophylaxis. By hospital day 3, the patient's laboratory values had improved, yet his stay was prolonged by alcohol withdrawal requiring benzodiazepines, altered mental status presumed secondary to hepatic encephalopathy, acute renal failure, aspiration pneumonia, and persistent unexplained leukocytosis. He required medical restraints during this time given confusion and propensity to ambulate without assistance, yet sustained no falls or other known trauma in care delivered during this time.
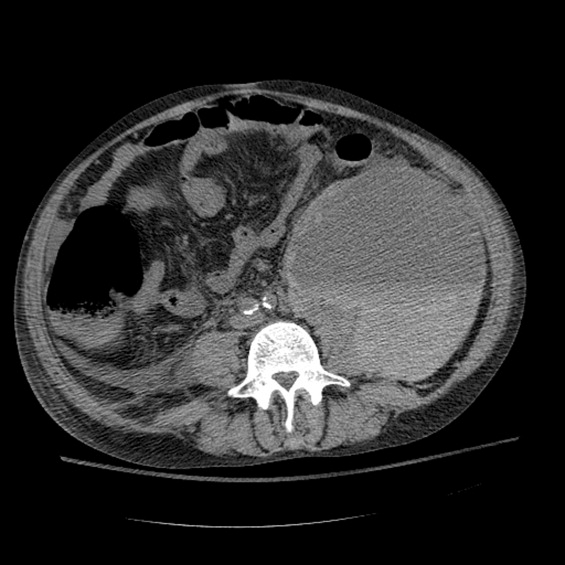
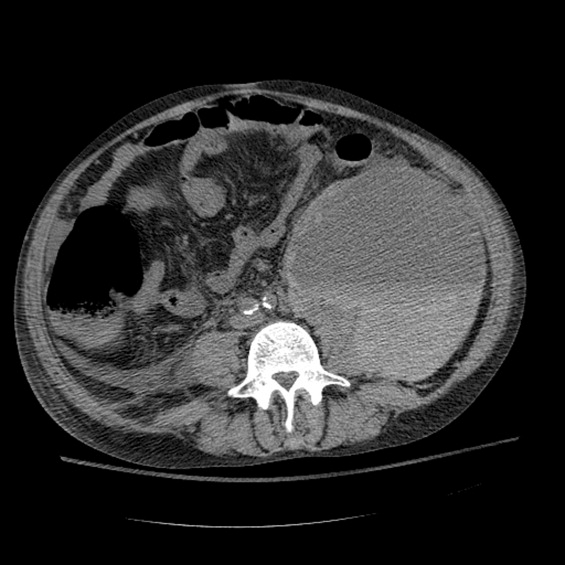
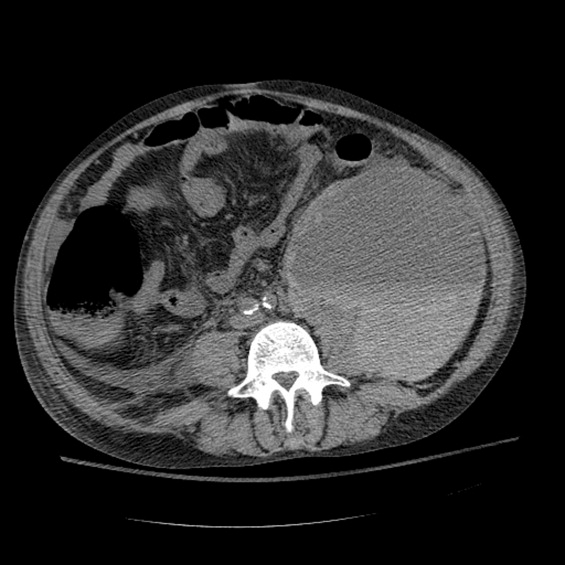
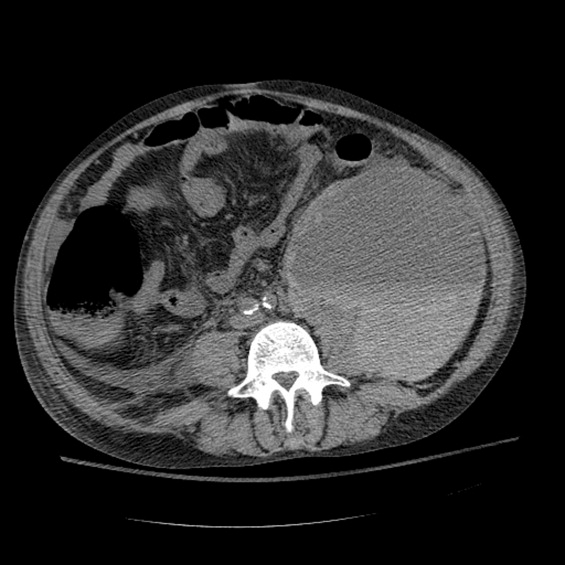
Between days 14 and 17, the patient's hematocrit fell from 36% to 30%; vital signs remained stable. He underwent an uncomplicated, ultrasound‐guided therapeutic paracentesis, which yielded 1.4 L of straw‐colored fluid on the afternoon of day 17; the procedure was attempted only on the right side. On the morning of day 18, the patient's blood pressure dropped to 78/55 mmHg with a pulse of 123 beats per minute; he became pale and unresponsive. Physical examination was notable for somnolence and a tender, warm left flank mass, contralateral to his paracentesis site. No flank or periumbilical ecchymoses were identified. Complete blood count demonstrated a white blood count (WBC) of 22,970/L, hematocrit 16%, and platelet count 104,000/L. INR was 2.0, unchanged from the last check on day 10. Partial thromboplastin time was 41 seconds and fibrinogen was 293 mg/dL (normal 150‐400 mg/dL). Peripheral blood smear was negative for red cell fragments. Blood chemistries revealed a sodium of 134 mg/dL, bicarbonate 20 mEq/L, anion gap 7, BUN 24 mg/dL, and creatinine 1.6 mg/dL (up from 1.0 mg/dL the previous day). His venous lactate level was 4.6 mmol/L and arterial blood gas sampling on room air demonstrated a pH of 7.35, partial pressure of carbon dioxide (pCO2) 29 mmHg, partial pressure of oxygen (pCO2) 54 mmHg, and bicarbonate 15 mEq/L. A femoral introducer was placed for volume resuscitation and the patient was urgently transfused with packed red blood cells (PRBCs) and fresh‐frozen plasma (FFP) to correct his coagulopathy. Computed tomography of the abdomen revealed a large left retroperitoneal hematoma measuring 15 15 22 cm3 (Figure 1). Despite transfusion, his hematocrit continued to fall. Urgent angiography was performed, upon which he was found to have active bleeding from the left L3‐L5 lumbar arteries. These were successfully embolized. He required PRBCs and FFP transfusion only once following this procedure. Given a transient decrease in his urine output, his bladder pressures were followed closely for evidence of abdominal compartment syndrome, which did not develop. He was transferred from the intensive care unit (ICU) to the floor on day 20, where his physical exam and hematocrit remained stable and his delirium slowly cleared. He was ultimately discharged to a skilled nursing facility on day 33.
Discussion
Spontaneous retroperitoneal hematoma is a well‐recognized entity that may present with the classic triad of abdominal or groin pain, palpable abdominal or flank mass, and shock or lower extremity motor or sensory changes due to femoral nerve compression.1 Although classically described as skin findings associated with retroperitoneal hemorrhage, Cullen and Grey‐Turner signs are relatively late findings that may not develop in all patients.
Retroperitoneal hemorrhage is well‐recognized as a result of iatrogenic anticoagulation,1 but has been reported less commonly as a result of coagulopathy related to cirrhosis. Di Bisceglie and Richart2 describe 2 patients with MELD scores of 29 and 25, respectively, who developed spontaneous retroperitoneal and rectus muscle hemorrhage. Both had evidence of associated disseminated intravascular coagulation (DIC) and died. Even less common is spontaneous lumbar artery rupture, occurring rarely in the absence of trauma or instrumentation. One reported bleed developed in the context of systemic anticoagulation for a mechanical valve.3 Halak et al.4 relate a case in which the only known risk factor was chronic renal disease. Hama et al.5 describe a patient with a history of alcoholic liver cirrhosis and INR of 2.3 whose lumbar artery rupture was successfully managed with transcatheter arterial embolization.
It is difficult to ascertain the effect of prophylactic anticoagulation in development of this particular hemorrhage. Retroperitoneal bleeding is a very rare complication of pharmacologic prophylaxis for DVT reported with both low‐molecular weight and unfractionated heparins.6 There may be additive risk of prophylaxis in a cirrhotic patient with baseline elevated INR and thrombocytopenia, particularly in the context of renal failure.
Options in the management of spontaneous retroperitoneal hematoma include transarterial embolization, percutaneous decompression, and open surgery. Nonoperative management of these bleeds when possible may be preferable in cirrhotic patients, as their baseline liver disease renders them higher‐risk candidates for surgery. There are no randomized trials comparing these approaches.1
In summary, we report the case of a 56‐year‐old man with end‐stage liver disease and associated coagulopathy without evidence of DIC who survived to discharge with intravascular management of a spontaneous retroperitoneal hemorrhage from the lumbar arteries. To our knowledge, this is the second reported case of spontaneous retroperitoneal hemorrhage in a cirrhotic in which the lumbar arteries were implicated and the first in which multiple arteries were found to be bleeding simultaneously. Any hospitalized patient who develops abdominal pain, flank pain, or hemodynamic instability in the context of coagulopathy, regardless of cause, warrants evaluation for retroperitoneal bleed. Appropriate early management includes immediate resuscitation, intensive monitoring, urgent imaging, and surgical and interventional radiology consultation in order to prevent a fatal outcome.
- ,,,.Management of spontaneous and iatrogenic retroperitoneal haemorrhage: conservative management, endovascular intervention or open surgery?Int J Clin Pract.2007;62:1604–1613.
- ,.Spontaneous retroperitoneal and rectus muscle hemorrhage as a potentially lethal complication of cirrhosis.Liver Int.2006;26:1291–1293.
- ,,.Spontaneous rupture of a lumbar artery. A rare etiology of retroperitoneal hematoma.Urologe A.2003;42:840–844.
- ,,,,.Spontaneous ruptured lumbar artery in a chronic renal failure patient.Eur J Vasc Endovasc Surg.2001;21:569–571.
- ,,.Spontaneous rupture of the lumbar artery.Intern Med.2004;43:759.
- ,,.The rate of bleeding complications after pharmacologic deep venous thrombosis prophylaxis.Arch Surg.2006;141:790–799.
A 56‐year‐old male presented to the emergency department with a 2‐week history of increasing abdominal girth, nausea, vomiting, and lower extremity edema. His girlfriend had also noted a yellow tinge to his skin and eyes. His past medical history was significant for bipolar disorder, alcohol‐related seizures, and pneumonia. He had no allergies and denied medications prior to admission. Family history was negative for liver disease and social history was notable for ongoing tobacco use and alcohol dependence. He was afebrile with stable vital signs. Physical examination demonstrated an alert gentleman whose answers to questions required occasional factual correction by his partner. His abdomen was distended and nontender with prominent vasculature and shifting dullness. Lower extremity edema was symmetric and bilateral, rated as 2+. Scattered spider angiomata and a fine bilateral hand tremor without asterixis were also noted. Initial laboratory data demonstrated a white blood cell count of 13,900/L, hematocrit 37%, and platelet count 176,000/L. His sodium was 130 mg/dL, blood urea nitrogen (BUN) 1 mg/dL, and creatinine 0.7 mg/dL. International normalized ratio (INR) was 1.8, aspartate aminotransferase (AST) was 117 U/L, alanine aminotransferase (ALT) 33 U/L, alkaline phosphatase 191 U/L, total bilirubin 9.2 mg/dL, total protein 7.0 g/dL, and albumin 1.9 g/dL. Abdominal ultrasound revealed a diffusely hyperechoic liver with a large amount of ascites.
The patient was admitted with the diagnoses of presumed alcoholic hepatitis and end‐stage liver disease. Model for End‐Stage Liver Disease (MELD) score was 21 and discriminant function 16.8. Paracentesis demonstrated a serum‐ascites albumin gradient of >1.1 and no evidence of spontaneous bacterial peritonitis. Diuresis was initiated. He was placed on unfractionated heparin at a dose of 5000 units every 8 hours for deep venous thrombosis (DVT) prophylaxis. By hospital day 3, the patient's laboratory values had improved, yet his stay was prolonged by alcohol withdrawal requiring benzodiazepines, altered mental status presumed secondary to hepatic encephalopathy, acute renal failure, aspiration pneumonia, and persistent unexplained leukocytosis. He required medical restraints during this time given confusion and propensity to ambulate without assistance, yet sustained no falls or other known trauma in care delivered during this time.
Between days 14 and 17, the patient's hematocrit fell from 36% to 30%; vital signs remained stable. He underwent an uncomplicated, ultrasound‐guided therapeutic paracentesis, which yielded 1.4 L of straw‐colored fluid on the afternoon of day 17; the procedure was attempted only on the right side. On the morning of day 18, the patient's blood pressure dropped to 78/55 mmHg with a pulse of 123 beats per minute; he became pale and unresponsive. Physical examination was notable for somnolence and a tender, warm left flank mass, contralateral to his paracentesis site. No flank or periumbilical ecchymoses were identified. Complete blood count demonstrated a white blood count (WBC) of 22,970/L, hematocrit 16%, and platelet count 104,000/L. INR was 2.0, unchanged from the last check on day 10. Partial thromboplastin time was 41 seconds and fibrinogen was 293 mg/dL (normal 150‐400 mg/dL). Peripheral blood smear was negative for red cell fragments. Blood chemistries revealed a sodium of 134 mg/dL, bicarbonate 20 mEq/L, anion gap 7, BUN 24 mg/dL, and creatinine 1.6 mg/dL (up from 1.0 mg/dL the previous day). His venous lactate level was 4.6 mmol/L and arterial blood gas sampling on room air demonstrated a pH of 7.35, partial pressure of carbon dioxide (pCO2) 29 mmHg, partial pressure of oxygen (pCO2) 54 mmHg, and bicarbonate 15 mEq/L. A femoral introducer was placed for volume resuscitation and the patient was urgently transfused with packed red blood cells (PRBCs) and fresh‐frozen plasma (FFP) to correct his coagulopathy. Computed tomography of the abdomen revealed a large left retroperitoneal hematoma measuring 15 15 22 cm3 (Figure 1). Despite transfusion, his hematocrit continued to fall. Urgent angiography was performed, upon which he was found to have active bleeding from the left L3‐L5 lumbar arteries. These were successfully embolized. He required PRBCs and FFP transfusion only once following this procedure. Given a transient decrease in his urine output, his bladder pressures were followed closely for evidence of abdominal compartment syndrome, which did not develop. He was transferred from the intensive care unit (ICU) to the floor on day 20, where his physical exam and hematocrit remained stable and his delirium slowly cleared. He was ultimately discharged to a skilled nursing facility on day 33.
Discussion
Spontaneous retroperitoneal hematoma is a well‐recognized entity that may present with the classic triad of abdominal or groin pain, palpable abdominal or flank mass, and shock or lower extremity motor or sensory changes due to femoral nerve compression.1 Although classically described as skin findings associated with retroperitoneal hemorrhage, Cullen and Grey‐Turner signs are relatively late findings that may not develop in all patients.
Retroperitoneal hemorrhage is well‐recognized as a result of iatrogenic anticoagulation,1 but has been reported less commonly as a result of coagulopathy related to cirrhosis. Di Bisceglie and Richart2 describe 2 patients with MELD scores of 29 and 25, respectively, who developed spontaneous retroperitoneal and rectus muscle hemorrhage. Both had evidence of associated disseminated intravascular coagulation (DIC) and died. Even less common is spontaneous lumbar artery rupture, occurring rarely in the absence of trauma or instrumentation. One reported bleed developed in the context of systemic anticoagulation for a mechanical valve.3 Halak et al.4 relate a case in which the only known risk factor was chronic renal disease. Hama et al.5 describe a patient with a history of alcoholic liver cirrhosis and INR of 2.3 whose lumbar artery rupture was successfully managed with transcatheter arterial embolization.
It is difficult to ascertain the effect of prophylactic anticoagulation in development of this particular hemorrhage. Retroperitoneal bleeding is a very rare complication of pharmacologic prophylaxis for DVT reported with both low‐molecular weight and unfractionated heparins.6 There may be additive risk of prophylaxis in a cirrhotic patient with baseline elevated INR and thrombocytopenia, particularly in the context of renal failure.
Options in the management of spontaneous retroperitoneal hematoma include transarterial embolization, percutaneous decompression, and open surgery. Nonoperative management of these bleeds when possible may be preferable in cirrhotic patients, as their baseline liver disease renders them higher‐risk candidates for surgery. There are no randomized trials comparing these approaches.1
In summary, we report the case of a 56‐year‐old man with end‐stage liver disease and associated coagulopathy without evidence of DIC who survived to discharge with intravascular management of a spontaneous retroperitoneal hemorrhage from the lumbar arteries. To our knowledge, this is the second reported case of spontaneous retroperitoneal hemorrhage in a cirrhotic in which the lumbar arteries were implicated and the first in which multiple arteries were found to be bleeding simultaneously. Any hospitalized patient who develops abdominal pain, flank pain, or hemodynamic instability in the context of coagulopathy, regardless of cause, warrants evaluation for retroperitoneal bleed. Appropriate early management includes immediate resuscitation, intensive monitoring, urgent imaging, and surgical and interventional radiology consultation in order to prevent a fatal outcome.
A 56‐year‐old male presented to the emergency department with a 2‐week history of increasing abdominal girth, nausea, vomiting, and lower extremity edema. His girlfriend had also noted a yellow tinge to his skin and eyes. His past medical history was significant for bipolar disorder, alcohol‐related seizures, and pneumonia. He had no allergies and denied medications prior to admission. Family history was negative for liver disease and social history was notable for ongoing tobacco use and alcohol dependence. He was afebrile with stable vital signs. Physical examination demonstrated an alert gentleman whose answers to questions required occasional factual correction by his partner. His abdomen was distended and nontender with prominent vasculature and shifting dullness. Lower extremity edema was symmetric and bilateral, rated as 2+. Scattered spider angiomata and a fine bilateral hand tremor without asterixis were also noted. Initial laboratory data demonstrated a white blood cell count of 13,900/L, hematocrit 37%, and platelet count 176,000/L. His sodium was 130 mg/dL, blood urea nitrogen (BUN) 1 mg/dL, and creatinine 0.7 mg/dL. International normalized ratio (INR) was 1.8, aspartate aminotransferase (AST) was 117 U/L, alanine aminotransferase (ALT) 33 U/L, alkaline phosphatase 191 U/L, total bilirubin 9.2 mg/dL, total protein 7.0 g/dL, and albumin 1.9 g/dL. Abdominal ultrasound revealed a diffusely hyperechoic liver with a large amount of ascites.
The patient was admitted with the diagnoses of presumed alcoholic hepatitis and end‐stage liver disease. Model for End‐Stage Liver Disease (MELD) score was 21 and discriminant function 16.8. Paracentesis demonstrated a serum‐ascites albumin gradient of >1.1 and no evidence of spontaneous bacterial peritonitis. Diuresis was initiated. He was placed on unfractionated heparin at a dose of 5000 units every 8 hours for deep venous thrombosis (DVT) prophylaxis. By hospital day 3, the patient's laboratory values had improved, yet his stay was prolonged by alcohol withdrawal requiring benzodiazepines, altered mental status presumed secondary to hepatic encephalopathy, acute renal failure, aspiration pneumonia, and persistent unexplained leukocytosis. He required medical restraints during this time given confusion and propensity to ambulate without assistance, yet sustained no falls or other known trauma in care delivered during this time.
Between days 14 and 17, the patient's hematocrit fell from 36% to 30%; vital signs remained stable. He underwent an uncomplicated, ultrasound‐guided therapeutic paracentesis, which yielded 1.4 L of straw‐colored fluid on the afternoon of day 17; the procedure was attempted only on the right side. On the morning of day 18, the patient's blood pressure dropped to 78/55 mmHg with a pulse of 123 beats per minute; he became pale and unresponsive. Physical examination was notable for somnolence and a tender, warm left flank mass, contralateral to his paracentesis site. No flank or periumbilical ecchymoses were identified. Complete blood count demonstrated a white blood count (WBC) of 22,970/L, hematocrit 16%, and platelet count 104,000/L. INR was 2.0, unchanged from the last check on day 10. Partial thromboplastin time was 41 seconds and fibrinogen was 293 mg/dL (normal 150‐400 mg/dL). Peripheral blood smear was negative for red cell fragments. Blood chemistries revealed a sodium of 134 mg/dL, bicarbonate 20 mEq/L, anion gap 7, BUN 24 mg/dL, and creatinine 1.6 mg/dL (up from 1.0 mg/dL the previous day). His venous lactate level was 4.6 mmol/L and arterial blood gas sampling on room air demonstrated a pH of 7.35, partial pressure of carbon dioxide (pCO2) 29 mmHg, partial pressure of oxygen (pCO2) 54 mmHg, and bicarbonate 15 mEq/L. A femoral introducer was placed for volume resuscitation and the patient was urgently transfused with packed red blood cells (PRBCs) and fresh‐frozen plasma (FFP) to correct his coagulopathy. Computed tomography of the abdomen revealed a large left retroperitoneal hematoma measuring 15 15 22 cm3 (Figure 1). Despite transfusion, his hematocrit continued to fall. Urgent angiography was performed, upon which he was found to have active bleeding from the left L3‐L5 lumbar arteries. These were successfully embolized. He required PRBCs and FFP transfusion only once following this procedure. Given a transient decrease in his urine output, his bladder pressures were followed closely for evidence of abdominal compartment syndrome, which did not develop. He was transferred from the intensive care unit (ICU) to the floor on day 20, where his physical exam and hematocrit remained stable and his delirium slowly cleared. He was ultimately discharged to a skilled nursing facility on day 33.
Discussion
Spontaneous retroperitoneal hematoma is a well‐recognized entity that may present with the classic triad of abdominal or groin pain, palpable abdominal or flank mass, and shock or lower extremity motor or sensory changes due to femoral nerve compression.1 Although classically described as skin findings associated with retroperitoneal hemorrhage, Cullen and Grey‐Turner signs are relatively late findings that may not develop in all patients.
Retroperitoneal hemorrhage is well‐recognized as a result of iatrogenic anticoagulation,1 but has been reported less commonly as a result of coagulopathy related to cirrhosis. Di Bisceglie and Richart2 describe 2 patients with MELD scores of 29 and 25, respectively, who developed spontaneous retroperitoneal and rectus muscle hemorrhage. Both had evidence of associated disseminated intravascular coagulation (DIC) and died. Even less common is spontaneous lumbar artery rupture, occurring rarely in the absence of trauma or instrumentation. One reported bleed developed in the context of systemic anticoagulation for a mechanical valve.3 Halak et al.4 relate a case in which the only known risk factor was chronic renal disease. Hama et al.5 describe a patient with a history of alcoholic liver cirrhosis and INR of 2.3 whose lumbar artery rupture was successfully managed with transcatheter arterial embolization.
It is difficult to ascertain the effect of prophylactic anticoagulation in development of this particular hemorrhage. Retroperitoneal bleeding is a very rare complication of pharmacologic prophylaxis for DVT reported with both low‐molecular weight and unfractionated heparins.6 There may be additive risk of prophylaxis in a cirrhotic patient with baseline elevated INR and thrombocytopenia, particularly in the context of renal failure.
Options in the management of spontaneous retroperitoneal hematoma include transarterial embolization, percutaneous decompression, and open surgery. Nonoperative management of these bleeds when possible may be preferable in cirrhotic patients, as their baseline liver disease renders them higher‐risk candidates for surgery. There are no randomized trials comparing these approaches.1
In summary, we report the case of a 56‐year‐old man with end‐stage liver disease and associated coagulopathy without evidence of DIC who survived to discharge with intravascular management of a spontaneous retroperitoneal hemorrhage from the lumbar arteries. To our knowledge, this is the second reported case of spontaneous retroperitoneal hemorrhage in a cirrhotic in which the lumbar arteries were implicated and the first in which multiple arteries were found to be bleeding simultaneously. Any hospitalized patient who develops abdominal pain, flank pain, or hemodynamic instability in the context of coagulopathy, regardless of cause, warrants evaluation for retroperitoneal bleed. Appropriate early management includes immediate resuscitation, intensive monitoring, urgent imaging, and surgical and interventional radiology consultation in order to prevent a fatal outcome.
- ,,,.Management of spontaneous and iatrogenic retroperitoneal haemorrhage: conservative management, endovascular intervention or open surgery?Int J Clin Pract.2007;62:1604–1613.
- ,.Spontaneous retroperitoneal and rectus muscle hemorrhage as a potentially lethal complication of cirrhosis.Liver Int.2006;26:1291–1293.
- ,,.Spontaneous rupture of a lumbar artery. A rare etiology of retroperitoneal hematoma.Urologe A.2003;42:840–844.
- ,,,,.Spontaneous ruptured lumbar artery in a chronic renal failure patient.Eur J Vasc Endovasc Surg.2001;21:569–571.
- ,,.Spontaneous rupture of the lumbar artery.Intern Med.2004;43:759.
- ,,.The rate of bleeding complications after pharmacologic deep venous thrombosis prophylaxis.Arch Surg.2006;141:790–799.
- ,,,.Management of spontaneous and iatrogenic retroperitoneal haemorrhage: conservative management, endovascular intervention or open surgery?Int J Clin Pract.2007;62:1604–1613.
- ,.Spontaneous retroperitoneal and rectus muscle hemorrhage as a potentially lethal complication of cirrhosis.Liver Int.2006;26:1291–1293.
- ,,.Spontaneous rupture of a lumbar artery. A rare etiology of retroperitoneal hematoma.Urologe A.2003;42:840–844.
- ,,,,.Spontaneous ruptured lumbar artery in a chronic renal failure patient.Eur J Vasc Endovasc Surg.2001;21:569–571.
- ,,.Spontaneous rupture of the lumbar artery.Intern Med.2004;43:759.
- ,,.The rate of bleeding complications after pharmacologic deep venous thrombosis prophylaxis.Arch Surg.2006;141:790–799.