User login
VIDEO: Practice changers out of ASH 2017
ATLANTA – There were a lot of new data presented during the annual meeting of the American Society of Hematology. But what findings could actually change the way you practice?
Robert A. Brodsky, MD, director of the division of hematology at Johns Hopkins University in Baltimore and the moderator for the late-breaking abstract session at ASH, highlighted results from two studies.
Data from the MURANO trial showed robust results for a combination of venetoclax and rituximab in patients with relapsed/refractory chronic lymphocytic leukemia (CLL). At a median follow-up of 23.8 months, median progression-free survival -had not been reached in patients randomized to venetoclax/rituximab, while patients who received bendamustine plus rituximab had a median PFS of 17 months.
The based on the data presented, Dr. Brodsky said.
Another “enormously exciting and practice-changing” finding is that direct oral anticoagulants can be used safely in patients with cancer, Dr. Brodsky said in an interview.
In a randomized, open-label study, 12 months of daily treatment with edoxaban was noninferior to standard subcutaneous therapy with dalteparin for treatment of venous thromboembolism in cancer patients.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ATLANTA – There were a lot of new data presented during the annual meeting of the American Society of Hematology. But what findings could actually change the way you practice?
Robert A. Brodsky, MD, director of the division of hematology at Johns Hopkins University in Baltimore and the moderator for the late-breaking abstract session at ASH, highlighted results from two studies.
Data from the MURANO trial showed robust results for a combination of venetoclax and rituximab in patients with relapsed/refractory chronic lymphocytic leukemia (CLL). At a median follow-up of 23.8 months, median progression-free survival -had not been reached in patients randomized to venetoclax/rituximab, while patients who received bendamustine plus rituximab had a median PFS of 17 months.
The based on the data presented, Dr. Brodsky said.
Another “enormously exciting and practice-changing” finding is that direct oral anticoagulants can be used safely in patients with cancer, Dr. Brodsky said in an interview.
In a randomized, open-label study, 12 months of daily treatment with edoxaban was noninferior to standard subcutaneous therapy with dalteparin for treatment of venous thromboembolism in cancer patients.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ATLANTA – There were a lot of new data presented during the annual meeting of the American Society of Hematology. But what findings could actually change the way you practice?
Robert A. Brodsky, MD, director of the division of hematology at Johns Hopkins University in Baltimore and the moderator for the late-breaking abstract session at ASH, highlighted results from two studies.
Data from the MURANO trial showed robust results for a combination of venetoclax and rituximab in patients with relapsed/refractory chronic lymphocytic leukemia (CLL). At a median follow-up of 23.8 months, median progression-free survival -had not been reached in patients randomized to venetoclax/rituximab, while patients who received bendamustine plus rituximab had a median PFS of 17 months.
The based on the data presented, Dr. Brodsky said.
Another “enormously exciting and practice-changing” finding is that direct oral anticoagulants can be used safely in patients with cancer, Dr. Brodsky said in an interview.
In a randomized, open-label study, 12 months of daily treatment with edoxaban was noninferior to standard subcutaneous therapy with dalteparin for treatment of venous thromboembolism in cancer patients.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
REPORTING FROM ASH 2017
CLL drug in limited supply outside U.S.
Ofatumumab (Arzerra), a monoclonal antibody treatment for chronic lymphocytic leukemia, will soon be available outside the United States through compassionate use programs only. The drug will continue to be widely available in the United States.
Novartis announced in January that it would begin limiting the availability of the drug outside of the United States and would work with regulatory authorities to set up compassionate use programs for patients who are currently being treated with the drug. Patients who use these programs will receive the drug for free.
The decision was driven by the surge in CLL drugs that have become available over the last 5 years, according to Novartis.
The decision to pull the drug from international markets will not affect its use in ongoing clinical trials, particularly two phase 3 studies in relapsing multiple sclerosis and indolent non-Hodgkin lymphoma.
Ofatumumab (Arzerra), a monoclonal antibody treatment for chronic lymphocytic leukemia, will soon be available outside the United States through compassionate use programs only. The drug will continue to be widely available in the United States.
Novartis announced in January that it would begin limiting the availability of the drug outside of the United States and would work with regulatory authorities to set up compassionate use programs for patients who are currently being treated with the drug. Patients who use these programs will receive the drug for free.
The decision was driven by the surge in CLL drugs that have become available over the last 5 years, according to Novartis.
The decision to pull the drug from international markets will not affect its use in ongoing clinical trials, particularly two phase 3 studies in relapsing multiple sclerosis and indolent non-Hodgkin lymphoma.
Ofatumumab (Arzerra), a monoclonal antibody treatment for chronic lymphocytic leukemia, will soon be available outside the United States through compassionate use programs only. The drug will continue to be widely available in the United States.
Novartis announced in January that it would begin limiting the availability of the drug outside of the United States and would work with regulatory authorities to set up compassionate use programs for patients who are currently being treated with the drug. Patients who use these programs will receive the drug for free.
The decision was driven by the surge in CLL drugs that have become available over the last 5 years, according to Novartis.
The decision to pull the drug from international markets will not affect its use in ongoing clinical trials, particularly two phase 3 studies in relapsing multiple sclerosis and indolent non-Hodgkin lymphoma.
AUDIO: Immunotherapy’s role in NHL
ATLANTA – The use of immune checkpoint blockade is increasingly becoming standard therapy in Hodgkin lymphoma, but this approach has so far garnered mixed results in non-Hodgkin lymphoma, Stephen Ansell, MD, PhD, said at the annual meeting of the American Society of Hematology.
In an interview, Dr. Ansell, professor of medicine and chair of the lymphoma group at the Mayo Clinic, Rochester, Minn., said responses have been variable with promising results from immune checkpoint inhibitors in primary mediastinal large B-cell lymphoma, some NK/T-cell lymphomas, and primary CNS lymphoma. However, responses have been modest in low-grade lymphoma.
Dr. Ansell, who chaired a session at ASH 2017 on immunotherapy’s expanding role in non-Hodgkin lymphoma, said one of the major challenges of using immune checkpoint blockade in non-Hodgkin lymphoma is the complicated biology. For example, there are a lot of regulatory T cells that actually inhibit the immune response, and many of the T cells that are present within the tumor have an exhausted phenotype and are poorly functioning. Additionally, some of the cytokines that would seem to be stimulating the immune system can, over time, slowly produce T-cell exhaustion.
“Sort of like too much of a good thing ends up being a bad thing,” he said.
These are the issues that are fueling research today, Dr. Ansell said. Going forward he said he expects to see more combination approaches to therapy, such as using an agonistic positive signal plus the blocking of an inhibitory signal with chemotherapy.
Dr. Ansell reported that Mayo Clinic receives clinical trial support from Merck, Bristol-Myers Squibb, Seattle Genetics, Trillium, and Affimed.
ATLANTA – The use of immune checkpoint blockade is increasingly becoming standard therapy in Hodgkin lymphoma, but this approach has so far garnered mixed results in non-Hodgkin lymphoma, Stephen Ansell, MD, PhD, said at the annual meeting of the American Society of Hematology.
In an interview, Dr. Ansell, professor of medicine and chair of the lymphoma group at the Mayo Clinic, Rochester, Minn., said responses have been variable with promising results from immune checkpoint inhibitors in primary mediastinal large B-cell lymphoma, some NK/T-cell lymphomas, and primary CNS lymphoma. However, responses have been modest in low-grade lymphoma.
Dr. Ansell, who chaired a session at ASH 2017 on immunotherapy’s expanding role in non-Hodgkin lymphoma, said one of the major challenges of using immune checkpoint blockade in non-Hodgkin lymphoma is the complicated biology. For example, there are a lot of regulatory T cells that actually inhibit the immune response, and many of the T cells that are present within the tumor have an exhausted phenotype and are poorly functioning. Additionally, some of the cytokines that would seem to be stimulating the immune system can, over time, slowly produce T-cell exhaustion.
“Sort of like too much of a good thing ends up being a bad thing,” he said.
These are the issues that are fueling research today, Dr. Ansell said. Going forward he said he expects to see more combination approaches to therapy, such as using an agonistic positive signal plus the blocking of an inhibitory signal with chemotherapy.
Dr. Ansell reported that Mayo Clinic receives clinical trial support from Merck, Bristol-Myers Squibb, Seattle Genetics, Trillium, and Affimed.
ATLANTA – The use of immune checkpoint blockade is increasingly becoming standard therapy in Hodgkin lymphoma, but this approach has so far garnered mixed results in non-Hodgkin lymphoma, Stephen Ansell, MD, PhD, said at the annual meeting of the American Society of Hematology.
In an interview, Dr. Ansell, professor of medicine and chair of the lymphoma group at the Mayo Clinic, Rochester, Minn., said responses have been variable with promising results from immune checkpoint inhibitors in primary mediastinal large B-cell lymphoma, some NK/T-cell lymphomas, and primary CNS lymphoma. However, responses have been modest in low-grade lymphoma.
Dr. Ansell, who chaired a session at ASH 2017 on immunotherapy’s expanding role in non-Hodgkin lymphoma, said one of the major challenges of using immune checkpoint blockade in non-Hodgkin lymphoma is the complicated biology. For example, there are a lot of regulatory T cells that actually inhibit the immune response, and many of the T cells that are present within the tumor have an exhausted phenotype and are poorly functioning. Additionally, some of the cytokines that would seem to be stimulating the immune system can, over time, slowly produce T-cell exhaustion.
“Sort of like too much of a good thing ends up being a bad thing,” he said.
These are the issues that are fueling research today, Dr. Ansell said. Going forward he said he expects to see more combination approaches to therapy, such as using an agonistic positive signal plus the blocking of an inhibitory signal with chemotherapy.
Dr. Ansell reported that Mayo Clinic receives clinical trial support from Merck, Bristol-Myers Squibb, Seattle Genetics, Trillium, and Affimed.
EXPERT ANALYSIS FROM ASH 2017
FDA expands indication for bosutinib in newly diagnosed CML
Bosutinib is now approved for the treatment of adults with newly diagnosed chronic phase Philadelphia chromosome–positive (Ph+) chronic myelogenous leukemia (CML).
The Food and Drug Administration granted accelerated approval for bosutinib (Bosulif), which is marketed by Pfizer. The approval is based on data from the randomized, multicenter phase 3 BFORE trial of 487 patients with Ph+ newly diagnosed chronic phase CML who received either bosutinib or imatinib 400 mg once daily. Major molecular response at 12 months was 47.2% (95% confidence interval, 40.9-53.4) in the bosutinib arm and 36.9% (95% CI, 30.8-43.0) in the imatinib arm (two-sided P = .0200).
Bosutinib, a kinase inhibitor, was first approved in September 2012 for the treatment of adult patients with chronic, accelerated, or blast phase Ph+ CML with resistance or intolerance to prior therapy.
The recommended dose of bosutinib for newly diagnosed chronic phase Ph+ CML is 400 mg orally once daily with food.
The most common adverse reactions to the drug in newly diagnosed CML patients are diarrhea, nausea, thrombocytopenia, rash, increased alanine aminotransferase, abdominal pain, and increased aspartate aminotransferase.
Bosutinib is now approved for the treatment of adults with newly diagnosed chronic phase Philadelphia chromosome–positive (Ph+) chronic myelogenous leukemia (CML).
The Food and Drug Administration granted accelerated approval for bosutinib (Bosulif), which is marketed by Pfizer. The approval is based on data from the randomized, multicenter phase 3 BFORE trial of 487 patients with Ph+ newly diagnosed chronic phase CML who received either bosutinib or imatinib 400 mg once daily. Major molecular response at 12 months was 47.2% (95% confidence interval, 40.9-53.4) in the bosutinib arm and 36.9% (95% CI, 30.8-43.0) in the imatinib arm (two-sided P = .0200).
Bosutinib, a kinase inhibitor, was first approved in September 2012 for the treatment of adult patients with chronic, accelerated, or blast phase Ph+ CML with resistance or intolerance to prior therapy.
The recommended dose of bosutinib for newly diagnosed chronic phase Ph+ CML is 400 mg orally once daily with food.
The most common adverse reactions to the drug in newly diagnosed CML patients are diarrhea, nausea, thrombocytopenia, rash, increased alanine aminotransferase, abdominal pain, and increased aspartate aminotransferase.
Bosutinib is now approved for the treatment of adults with newly diagnosed chronic phase Philadelphia chromosome–positive (Ph+) chronic myelogenous leukemia (CML).
The Food and Drug Administration granted accelerated approval for bosutinib (Bosulif), which is marketed by Pfizer. The approval is based on data from the randomized, multicenter phase 3 BFORE trial of 487 patients with Ph+ newly diagnosed chronic phase CML who received either bosutinib or imatinib 400 mg once daily. Major molecular response at 12 months was 47.2% (95% confidence interval, 40.9-53.4) in the bosutinib arm and 36.9% (95% CI, 30.8-43.0) in the imatinib arm (two-sided P = .0200).
Bosutinib, a kinase inhibitor, was first approved in September 2012 for the treatment of adult patients with chronic, accelerated, or blast phase Ph+ CML with resistance or intolerance to prior therapy.
The recommended dose of bosutinib for newly diagnosed chronic phase Ph+ CML is 400 mg orally once daily with food.
The most common adverse reactions to the drug in newly diagnosed CML patients are diarrhea, nausea, thrombocytopenia, rash, increased alanine aminotransferase, abdominal pain, and increased aspartate aminotransferase.
Gene therapy regimen for XSCID shows rapid results in newly diagnosed infants
ATLANTA – A new approach to gene therapy produced rapid T cell reconstruction and normal markers of B-cell and natural killer (NK)-cell function in newly diagnosed infants with X-linked Severe Combined Immunodeficiency (XSCID), according to initial results from a phase 1/2 trial.
Researchers used a regimen of safety-modified lentiviral vector plus reduced-exposure busulfan conditioning in seven newly diagnosed infants and found that it was well tolerated in all patients and quickly improved T-cell immunity in five of seven patients.
Initial gene therapy trials used a mouse vector without busulfan conditioning. These trials produced T-cell correction but were unable to restore B-cell function, NK-cell function, or myeloid-cell function. As a result, patients continued to experience viral infections and required monthly, life-long intravenous immunoglobulin infusions, Dr. Mamcarz said.
The phase 1/2 multicenter safety and efficacy study tested the gene therapy regimen for the first time in seven newly diagnosed infants. The regimen involved transducing purified bone marrow CD34+ cells with the lentiviral vector, which was generated by a stable producer cell line and then cryopreserved. The busulfan was given as two single daily doses, which were tailored based on patient age and weight.
In total, seven patients have been treated and all tolerated the low-dose busulfan chemotherapy well. Five patients had normal numbers of previously defective cells (T cells, B cells, and NK cells) and were taken off protective isolation and prophylactic medications. Those infants appear to have functioning immune systems, Dr. Mamcarz said. One infant has stopped monthly intravenous immunoglobulin infusions and has received normal pediatric vaccines, but responses have not yet been tested.
For the two infants who did not show responses, one is early in the trial and there is not yet adequate follow-up data to assess the immune system reconstitution, Dr. Mamcarz said.
The other infant had high levels of maternal T cell engraftment, severe neutropenia, and ongoing cytomegalovirus infection, resulting in delayed and partial T-cell reconstitution. The researchers sought to boost the patient’s immunity through an infusion of corrected cells – without busulfan – at 1 year after receiving the initial therapy. Three months after the second treatment, the infant has normal functioning of T cells and NK cells, but he is not yet engrafting B cells, Dr. Mamcarz said.
Overall, there was no evidence of vector-mediated effects on blood formation, Dr. Mamcarz reported.
The ultimate evaluation of the efficacy of the trial would be to assess vaccine responses in the infants treated with gene therapy, she said.
The study was supported by the Assisi Foundation of Memphis and the California Institute of Regenerative Medicine. Dr. Mamcarz reported having no relevant financial disclosures. Her coauthors reported financial relationships with InsightRX, UpToDate, Invitae, and Homology Medicines.
mschneider@frontlinemedcom.com
SOURCE: Mamcarz E et al. Abstract 523.
ATLANTA – A new approach to gene therapy produced rapid T cell reconstruction and normal markers of B-cell and natural killer (NK)-cell function in newly diagnosed infants with X-linked Severe Combined Immunodeficiency (XSCID), according to initial results from a phase 1/2 trial.
Researchers used a regimen of safety-modified lentiviral vector plus reduced-exposure busulfan conditioning in seven newly diagnosed infants and found that it was well tolerated in all patients and quickly improved T-cell immunity in five of seven patients.
Initial gene therapy trials used a mouse vector without busulfan conditioning. These trials produced T-cell correction but were unable to restore B-cell function, NK-cell function, or myeloid-cell function. As a result, patients continued to experience viral infections and required monthly, life-long intravenous immunoglobulin infusions, Dr. Mamcarz said.
The phase 1/2 multicenter safety and efficacy study tested the gene therapy regimen for the first time in seven newly diagnosed infants. The regimen involved transducing purified bone marrow CD34+ cells with the lentiviral vector, which was generated by a stable producer cell line and then cryopreserved. The busulfan was given as two single daily doses, which were tailored based on patient age and weight.
In total, seven patients have been treated and all tolerated the low-dose busulfan chemotherapy well. Five patients had normal numbers of previously defective cells (T cells, B cells, and NK cells) and were taken off protective isolation and prophylactic medications. Those infants appear to have functioning immune systems, Dr. Mamcarz said. One infant has stopped monthly intravenous immunoglobulin infusions and has received normal pediatric vaccines, but responses have not yet been tested.
For the two infants who did not show responses, one is early in the trial and there is not yet adequate follow-up data to assess the immune system reconstitution, Dr. Mamcarz said.
The other infant had high levels of maternal T cell engraftment, severe neutropenia, and ongoing cytomegalovirus infection, resulting in delayed and partial T-cell reconstitution. The researchers sought to boost the patient’s immunity through an infusion of corrected cells – without busulfan – at 1 year after receiving the initial therapy. Three months after the second treatment, the infant has normal functioning of T cells and NK cells, but he is not yet engrafting B cells, Dr. Mamcarz said.
Overall, there was no evidence of vector-mediated effects on blood formation, Dr. Mamcarz reported.
The ultimate evaluation of the efficacy of the trial would be to assess vaccine responses in the infants treated with gene therapy, she said.
The study was supported by the Assisi Foundation of Memphis and the California Institute of Regenerative Medicine. Dr. Mamcarz reported having no relevant financial disclosures. Her coauthors reported financial relationships with InsightRX, UpToDate, Invitae, and Homology Medicines.
mschneider@frontlinemedcom.com
SOURCE: Mamcarz E et al. Abstract 523.
ATLANTA – A new approach to gene therapy produced rapid T cell reconstruction and normal markers of B-cell and natural killer (NK)-cell function in newly diagnosed infants with X-linked Severe Combined Immunodeficiency (XSCID), according to initial results from a phase 1/2 trial.
Researchers used a regimen of safety-modified lentiviral vector plus reduced-exposure busulfan conditioning in seven newly diagnosed infants and found that it was well tolerated in all patients and quickly improved T-cell immunity in five of seven patients.
Initial gene therapy trials used a mouse vector without busulfan conditioning. These trials produced T-cell correction but were unable to restore B-cell function, NK-cell function, or myeloid-cell function. As a result, patients continued to experience viral infections and required monthly, life-long intravenous immunoglobulin infusions, Dr. Mamcarz said.
The phase 1/2 multicenter safety and efficacy study tested the gene therapy regimen for the first time in seven newly diagnosed infants. The regimen involved transducing purified bone marrow CD34+ cells with the lentiviral vector, which was generated by a stable producer cell line and then cryopreserved. The busulfan was given as two single daily doses, which were tailored based on patient age and weight.
In total, seven patients have been treated and all tolerated the low-dose busulfan chemotherapy well. Five patients had normal numbers of previously defective cells (T cells, B cells, and NK cells) and were taken off protective isolation and prophylactic medications. Those infants appear to have functioning immune systems, Dr. Mamcarz said. One infant has stopped monthly intravenous immunoglobulin infusions and has received normal pediatric vaccines, but responses have not yet been tested.
For the two infants who did not show responses, one is early in the trial and there is not yet adequate follow-up data to assess the immune system reconstitution, Dr. Mamcarz said.
The other infant had high levels of maternal T cell engraftment, severe neutropenia, and ongoing cytomegalovirus infection, resulting in delayed and partial T-cell reconstitution. The researchers sought to boost the patient’s immunity through an infusion of corrected cells – without busulfan – at 1 year after receiving the initial therapy. Three months after the second treatment, the infant has normal functioning of T cells and NK cells, but he is not yet engrafting B cells, Dr. Mamcarz said.
Overall, there was no evidence of vector-mediated effects on blood formation, Dr. Mamcarz reported.
The ultimate evaluation of the efficacy of the trial would be to assess vaccine responses in the infants treated with gene therapy, she said.
The study was supported by the Assisi Foundation of Memphis and the California Institute of Regenerative Medicine. Dr. Mamcarz reported having no relevant financial disclosures. Her coauthors reported financial relationships with InsightRX, UpToDate, Invitae, and Homology Medicines.
mschneider@frontlinemedcom.com
SOURCE: Mamcarz E et al. Abstract 523.
REPORTING FROM ASH 2017
Key clinical point:
Major finding: In total, five of seven infants with XSCID had normal functioning of T cells, B cells, and NK cells.
Study details: A phase 1/2 multicenter study of seven infants with newly diagnosed XSCID.
Disclosures: The study was supported by the Assisi Foundation of Memphis and the California Institute of Regenerative Medicine. Dr. Mamcarz reported having no relevant financial disclosures. Her coauthors reported financial relationships with InsightRX, UpToDate, Invitae, and Homology Medicines.
Source: Mamcarz E et al. Abstract 523.
Anti-BCMA CAR T-cell therapy being fast tracked at FDA
The Food and Drug Administration has granted breakthrough therapy designation to bb2121, a chimeric antigen receptor T-cell (CAR T) therapy that targets b-cell maturation antigen (BCMA) in patients with relapsed/refractory multiple myeloma.
The therapy, being developed jointly by Celgene and bluebird bio, will be given expedited review by the FDA under the program. Meanwhile, European drug officials have granted it Priority Medicines eligibility, which also provides accelerated review.
The decision to fast track the review of bb2121 is based on preliminary data from the ongoing phase I CRB-401 trial. As of May 2017, there was 1-month clinical response data from 18 patients with multiple myeloma who were infused with bb2121. The overall response rate was 89%, but was 100% for patients who had been treated with doses of 150 × 106 CAR+ T cells or higher, according to an abstract from the annual meeting of the American Society of Hematology. Five months of follow-up data on these patients, plus initial data on additional patients, will be presented at ASH 2017 on Dec. 11.
The Food and Drug Administration has granted breakthrough therapy designation to bb2121, a chimeric antigen receptor T-cell (CAR T) therapy that targets b-cell maturation antigen (BCMA) in patients with relapsed/refractory multiple myeloma.
The therapy, being developed jointly by Celgene and bluebird bio, will be given expedited review by the FDA under the program. Meanwhile, European drug officials have granted it Priority Medicines eligibility, which also provides accelerated review.
The decision to fast track the review of bb2121 is based on preliminary data from the ongoing phase I CRB-401 trial. As of May 2017, there was 1-month clinical response data from 18 patients with multiple myeloma who were infused with bb2121. The overall response rate was 89%, but was 100% for patients who had been treated with doses of 150 × 106 CAR+ T cells or higher, according to an abstract from the annual meeting of the American Society of Hematology. Five months of follow-up data on these patients, plus initial data on additional patients, will be presented at ASH 2017 on Dec. 11.
The Food and Drug Administration has granted breakthrough therapy designation to bb2121, a chimeric antigen receptor T-cell (CAR T) therapy that targets b-cell maturation antigen (BCMA) in patients with relapsed/refractory multiple myeloma.
The therapy, being developed jointly by Celgene and bluebird bio, will be given expedited review by the FDA under the program. Meanwhile, European drug officials have granted it Priority Medicines eligibility, which also provides accelerated review.
The decision to fast track the review of bb2121 is based on preliminary data from the ongoing phase I CRB-401 trial. As of May 2017, there was 1-month clinical response data from 18 patients with multiple myeloma who were infused with bb2121. The overall response rate was 89%, but was 100% for patients who had been treated with doses of 150 × 106 CAR+ T cells or higher, according to an abstract from the annual meeting of the American Society of Hematology. Five months of follow-up data on these patients, plus initial data on additional patients, will be presented at ASH 2017 on Dec. 11.
Researchers identify potential gene target for AML drug development
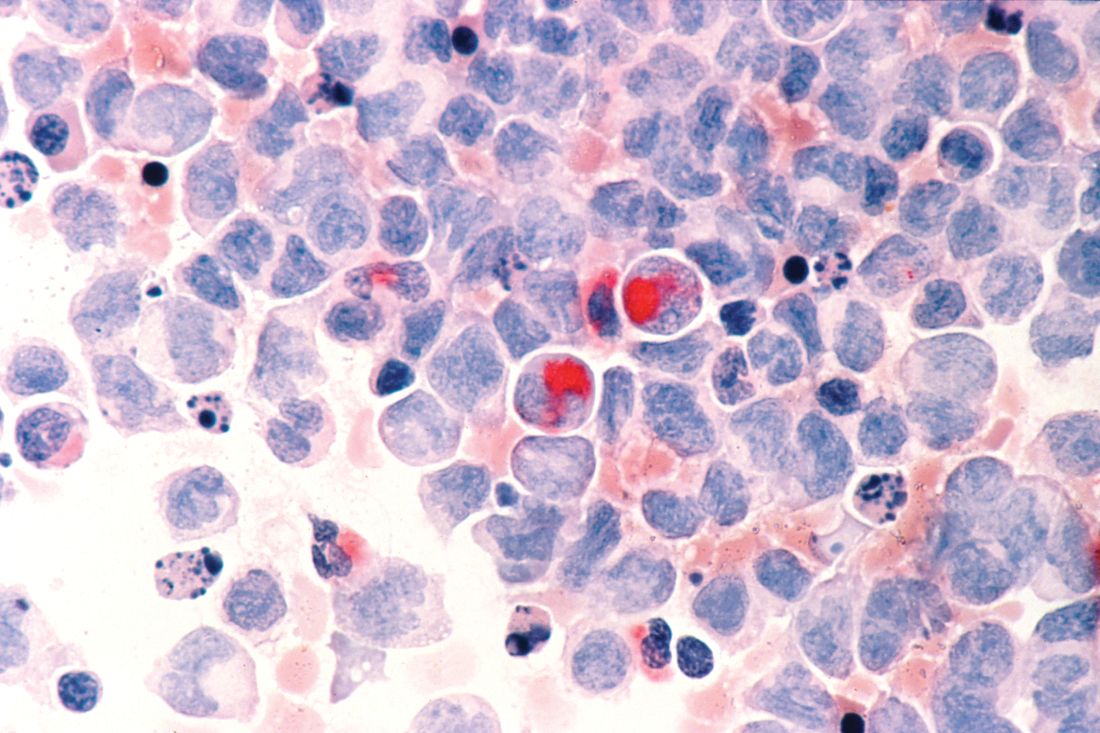
Researchers in the United States and the United Kingdom believe they have found a new gene target that could aid in the development of more effective treatments for acute myeloid leukemia (AML).
Inhibition of the METTL3 gene allowed for the destruction of AML in human and mouse cells without damaging healthy blood cells, the researchers reported in a research letter published Nov. 27 in the journal Nature.
Using mouse cells, the researchers used CRISPR-Cas9 gene editing technology to identify RNA-modifying enzymes that are needed for the survival and proliferation of AML cells. They identified 46 potential candidate genes and further narrowed that to the METTL gene families. They next targeted METTL1, METTL3, METTL14, and METTL16 in 10 human AML cell lines and 10 cell lines from heterogeneous cancer types. METTL3 was shown to have the strongest effect.
Read the full research letter in Nature (doi: 10.1038/nature24678).
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Researchers in the United States and the United Kingdom believe they have found a new gene target that could aid in the development of more effective treatments for acute myeloid leukemia (AML).
Inhibition of the METTL3 gene allowed for the destruction of AML in human and mouse cells without damaging healthy blood cells, the researchers reported in a research letter published Nov. 27 in the journal Nature.
Using mouse cells, the researchers used CRISPR-Cas9 gene editing technology to identify RNA-modifying enzymes that are needed for the survival and proliferation of AML cells. They identified 46 potential candidate genes and further narrowed that to the METTL gene families. They next targeted METTL1, METTL3, METTL14, and METTL16 in 10 human AML cell lines and 10 cell lines from heterogeneous cancer types. METTL3 was shown to have the strongest effect.
Read the full research letter in Nature (doi: 10.1038/nature24678).
mschneider@frontlinemedcom.com
On Twitter @maryellenny
Researchers in the United States and the United Kingdom believe they have found a new gene target that could aid in the development of more effective treatments for acute myeloid leukemia (AML).
Inhibition of the METTL3 gene allowed for the destruction of AML in human and mouse cells without damaging healthy blood cells, the researchers reported in a research letter published Nov. 27 in the journal Nature.
Using mouse cells, the researchers used CRISPR-Cas9 gene editing technology to identify RNA-modifying enzymes that are needed for the survival and proliferation of AML cells. They identified 46 potential candidate genes and further narrowed that to the METTL gene families. They next targeted METTL1, METTL3, METTL14, and METTL16 in 10 human AML cell lines and 10 cell lines from heterogeneous cancer types. METTL3 was shown to have the strongest effect.
Read the full research letter in Nature (doi: 10.1038/nature24678).
mschneider@frontlinemedcom.com
On Twitter @maryellenny
FROM NATURE
Marginal zone lymphoma treatment studies to be presented at ASH
Findings from several studies on marginal zone lymphoma (MZL) will be presented during oral and poster sessions at the annual meeting of the American Society of Hematology, with a focus on evaluating combination treatment approaches.
Some of the MZL treatment–related studies include the assessment of chlorambucil plus rituximab in patients with extranodal marginal zone B-cell lymphoma of mucosa associated lymphoid tissue, the combination of bendamustine with rituximab for first-line treatment of splenic MZL, and the safety and progression-free survival associated with lenalidomide and rituximab in previously untreated patients with MZL.
Other studies consider how to approach refractory disease. One study looks at the use of ibrutinib in patients with relapsed/refractory MZL, and researchers will also present findings from a systematic literature review of the efficacy and safety of various treatments among patients with relapsed/refractory MZL.
Abstract 1506: IELSG-38: A Phase II Study of Chlorambucil in Combination with Rituximab Followed by Maintenance Therapy with Subcutaneous Rituximab in Patients with Extranodal Marginal Zone B-Cell Lymphoma of Mucosa Associated Lymphoid Tissue (MALT) .
Abstract 4062: Bendamustine in Combination with Rituximab as First-Line Treatment of Splenic Marginal Zone Lymphoma (BRISMA). Results of the IELSG-36 Phase II Study.
Abstract 3026: Ibrutinib Therapy in Patients with Relapsed/Refractory Marginal Zone Lymphoma: Analysis by Prior Rituximab Treatment and Baseline Mutations.
Abstract 4040: Safety and Activity of Lenalidomide and Rituximab in Previously Untreated Marginal Zone Lymphoma: Subgroup Analysis and Long-Term Follow-Up of an Open-Label Phase II Trial.
Abstract 2783: Systematic Literature Review of the Clinical Efficacy and Safety of Treatments in the Relapsed/Refractory Setting for Patients with Follicular Lymphoma or Marginal Zone Lymphoma.
Findings from several studies on marginal zone lymphoma (MZL) will be presented during oral and poster sessions at the annual meeting of the American Society of Hematology, with a focus on evaluating combination treatment approaches.
Some of the MZL treatment–related studies include the assessment of chlorambucil plus rituximab in patients with extranodal marginal zone B-cell lymphoma of mucosa associated lymphoid tissue, the combination of bendamustine with rituximab for first-line treatment of splenic MZL, and the safety and progression-free survival associated with lenalidomide and rituximab in previously untreated patients with MZL.
Other studies consider how to approach refractory disease. One study looks at the use of ibrutinib in patients with relapsed/refractory MZL, and researchers will also present findings from a systematic literature review of the efficacy and safety of various treatments among patients with relapsed/refractory MZL.
Abstract 1506: IELSG-38: A Phase II Study of Chlorambucil in Combination with Rituximab Followed by Maintenance Therapy with Subcutaneous Rituximab in Patients with Extranodal Marginal Zone B-Cell Lymphoma of Mucosa Associated Lymphoid Tissue (MALT) .
Abstract 4062: Bendamustine in Combination with Rituximab as First-Line Treatment of Splenic Marginal Zone Lymphoma (BRISMA). Results of the IELSG-36 Phase II Study.
Abstract 3026: Ibrutinib Therapy in Patients with Relapsed/Refractory Marginal Zone Lymphoma: Analysis by Prior Rituximab Treatment and Baseline Mutations.
Abstract 4040: Safety and Activity of Lenalidomide and Rituximab in Previously Untreated Marginal Zone Lymphoma: Subgroup Analysis and Long-Term Follow-Up of an Open-Label Phase II Trial.
Abstract 2783: Systematic Literature Review of the Clinical Efficacy and Safety of Treatments in the Relapsed/Refractory Setting for Patients with Follicular Lymphoma or Marginal Zone Lymphoma.
Findings from several studies on marginal zone lymphoma (MZL) will be presented during oral and poster sessions at the annual meeting of the American Society of Hematology, with a focus on evaluating combination treatment approaches.
Some of the MZL treatment–related studies include the assessment of chlorambucil plus rituximab in patients with extranodal marginal zone B-cell lymphoma of mucosa associated lymphoid tissue, the combination of bendamustine with rituximab for first-line treatment of splenic MZL, and the safety and progression-free survival associated with lenalidomide and rituximab in previously untreated patients with MZL.
Other studies consider how to approach refractory disease. One study looks at the use of ibrutinib in patients with relapsed/refractory MZL, and researchers will also present findings from a systematic literature review of the efficacy and safety of various treatments among patients with relapsed/refractory MZL.
Abstract 1506: IELSG-38: A Phase II Study of Chlorambucil in Combination with Rituximab Followed by Maintenance Therapy with Subcutaneous Rituximab in Patients with Extranodal Marginal Zone B-Cell Lymphoma of Mucosa Associated Lymphoid Tissue (MALT) .
Abstract 4062: Bendamustine in Combination with Rituximab as First-Line Treatment of Splenic Marginal Zone Lymphoma (BRISMA). Results of the IELSG-36 Phase II Study.
Abstract 3026: Ibrutinib Therapy in Patients with Relapsed/Refractory Marginal Zone Lymphoma: Analysis by Prior Rituximab Treatment and Baseline Mutations.
Abstract 4040: Safety and Activity of Lenalidomide and Rituximab in Previously Untreated Marginal Zone Lymphoma: Subgroup Analysis and Long-Term Follow-Up of an Open-Label Phase II Trial.
Abstract 2783: Systematic Literature Review of the Clinical Efficacy and Safety of Treatments in the Relapsed/Refractory Setting for Patients with Follicular Lymphoma or Marginal Zone Lymphoma.
FROM ASH 2017
Mayo experts outline Waldenström macroglobulinemia management
, especially when rapid control is needed for bulky disease, according to treatment guidelines from a multidisciplinary expert panel.
The Mayo Clinic Cancer Center Myeloma, Amyloidosis, and Dysproteinemia and Lymphoma Disease-Oriented Groups, composed of experts who have collectively treated hundreds of patients with Waldenström macroglobulinemia, updated their recommendations for management of the condition in JAMA Oncology. It’s the first update from the group since 2010. The new treatment approaches are based on clinical and observational studies published or presented through December 2015 and consensus recommendations.
The Mayo group said dexamethasone-rituximab-cyclophosphamide can be an alternative treatment for patients with symptomatic Waldenström macroglobulinemia with a low disease burden. But because of an absence of data, the group said rituximab maintenance therapy is not recommended for routine use outside of clinical trials.
Rituximab monotherapy is contraindicated if patients have symptomatic hyperviscosity; without preemptive plasmapheresis, this treatment should be avoided in those with very high serum IgM. They recommended a prompt start of therapeutic plasma exchange for hyperviscosity syndrome, before starting cytoreductive treatment. But rituximab is indicated when patients have symptomatic mild to moderate anemia, symptomatic cryoglobulinemia (in combination with steroids), or hemolytic anemia that does not respond to corticosteroids.
In cases of first or second relapse, autologous stem cell transplantation should be considered in patients with chemosensitive disease who are eligible for transplant, especially when the first remission duration was less than 2 years. Patients with refractory Waldenström macroglobulinemia should not be offered autologous stem cell transplantation.
Read the full set of recommendations in JAMA Oncology (2017 Sep 1;3[9]:1257-65).
mschneider@frontlinemedcom.com
On Twitter @maryellenny
, especially when rapid control is needed for bulky disease, according to treatment guidelines from a multidisciplinary expert panel.
The Mayo Clinic Cancer Center Myeloma, Amyloidosis, and Dysproteinemia and Lymphoma Disease-Oriented Groups, composed of experts who have collectively treated hundreds of patients with Waldenström macroglobulinemia, updated their recommendations for management of the condition in JAMA Oncology. It’s the first update from the group since 2010. The new treatment approaches are based on clinical and observational studies published or presented through December 2015 and consensus recommendations.
The Mayo group said dexamethasone-rituximab-cyclophosphamide can be an alternative treatment for patients with symptomatic Waldenström macroglobulinemia with a low disease burden. But because of an absence of data, the group said rituximab maintenance therapy is not recommended for routine use outside of clinical trials.
Rituximab monotherapy is contraindicated if patients have symptomatic hyperviscosity; without preemptive plasmapheresis, this treatment should be avoided in those with very high serum IgM. They recommended a prompt start of therapeutic plasma exchange for hyperviscosity syndrome, before starting cytoreductive treatment. But rituximab is indicated when patients have symptomatic mild to moderate anemia, symptomatic cryoglobulinemia (in combination with steroids), or hemolytic anemia that does not respond to corticosteroids.
In cases of first or second relapse, autologous stem cell transplantation should be considered in patients with chemosensitive disease who are eligible for transplant, especially when the first remission duration was less than 2 years. Patients with refractory Waldenström macroglobulinemia should not be offered autologous stem cell transplantation.
Read the full set of recommendations in JAMA Oncology (2017 Sep 1;3[9]:1257-65).
mschneider@frontlinemedcom.com
On Twitter @maryellenny
, especially when rapid control is needed for bulky disease, according to treatment guidelines from a multidisciplinary expert panel.
The Mayo Clinic Cancer Center Myeloma, Amyloidosis, and Dysproteinemia and Lymphoma Disease-Oriented Groups, composed of experts who have collectively treated hundreds of patients with Waldenström macroglobulinemia, updated their recommendations for management of the condition in JAMA Oncology. It’s the first update from the group since 2010. The new treatment approaches are based on clinical and observational studies published or presented through December 2015 and consensus recommendations.
The Mayo group said dexamethasone-rituximab-cyclophosphamide can be an alternative treatment for patients with symptomatic Waldenström macroglobulinemia with a low disease burden. But because of an absence of data, the group said rituximab maintenance therapy is not recommended for routine use outside of clinical trials.
Rituximab monotherapy is contraindicated if patients have symptomatic hyperviscosity; without preemptive plasmapheresis, this treatment should be avoided in those with very high serum IgM. They recommended a prompt start of therapeutic plasma exchange for hyperviscosity syndrome, before starting cytoreductive treatment. But rituximab is indicated when patients have symptomatic mild to moderate anemia, symptomatic cryoglobulinemia (in combination with steroids), or hemolytic anemia that does not respond to corticosteroids.
In cases of first or second relapse, autologous stem cell transplantation should be considered in patients with chemosensitive disease who are eligible for transplant, especially when the first remission duration was less than 2 years. Patients with refractory Waldenström macroglobulinemia should not be offered autologous stem cell transplantation.
Read the full set of recommendations in JAMA Oncology (2017 Sep 1;3[9]:1257-65).
mschneider@frontlinemedcom.com
On Twitter @maryellenny
FROM JAMA ONCOLOGY
Generic clofarabine injection hits the market
The generic clofarabine injection for treatment of children with relapsed or refractory acute lymphoblastic leukemia (ALL) is now available on the U.S. market.
The generic version of the drug was approved by the Food and Drug Administration in May 2017 for children up to age 21 years with relapsed or refractory ALL after at least two prior regimens.
The injection, marketed by Mylan N.V., is available in 20 mg/20 mL (1 mg/mL) single-dose vials. It is a generic version of Genzyme’s Clolar.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
The generic clofarabine injection for treatment of children with relapsed or refractory acute lymphoblastic leukemia (ALL) is now available on the U.S. market.
The generic version of the drug was approved by the Food and Drug Administration in May 2017 for children up to age 21 years with relapsed or refractory ALL after at least two prior regimens.
The injection, marketed by Mylan N.V., is available in 20 mg/20 mL (1 mg/mL) single-dose vials. It is a generic version of Genzyme’s Clolar.
mschneider@frontlinemedcom.com
On Twitter @maryellenny
The generic clofarabine injection for treatment of children with relapsed or refractory acute lymphoblastic leukemia (ALL) is now available on the U.S. market.
The generic version of the drug was approved by the Food and Drug Administration in May 2017 for children up to age 21 years with relapsed or refractory ALL after at least two prior regimens.
The injection, marketed by Mylan N.V., is available in 20 mg/20 mL (1 mg/mL) single-dose vials. It is a generic version of Genzyme’s Clolar.
mschneider@frontlinemedcom.com
On Twitter @maryellenny