User login
Mechanism proposed for microvascular thrombosis in thrombotic thrombocytopenic purpura
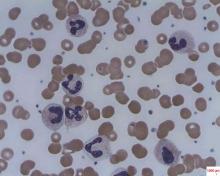
In patients with acquired autoimmune thrombotic thrombocytopenic purpura, elevated plasma levels of human neutrophil proteins 1-3 inhibit proteolytic cleavage of von Willebrand factor by ADAMTS13, Vikram G. Pillai, PhD, of the University of Alabama at Birmingham, and colleagues reported.
The finding may explain how inflammation triggers microvascular thrombosis in these patients and potentially others with immune thrombotic disorders, according to the researchers (Blood 2016;128:110-9).
They performed enzyme-linked immunosorbent assays and found markedly increased levels of plasma human neutrophil proteins (HNPs) 1-3 in most of the patients with acquired autoimmune thrombotic thrombocytopenic purpura (TTP). The median levels in the 19 patients were 170 ng/mL, compared with 23 ng/mL in 18 healthy controls, a statistically significant difference (P less than .0001).
Liquid chromatography plus tandem mass spectrometry similarly confirmed statistically significant increases in HNP1, HNP2, and HNP3 in patient samples (P less than .001).
Measures of HNPs 1-3 by both methods correlated well, and the researchers concluded that HNPs 1-3 likely inhibit ADAMTS13 activity by binding to the central A2 domain of von Willebrand factor and physically blocking ADAMTS13 binding.
The researchers had no relevant financial disclosures.
On Twitter @maryjodales
In patients with acquired autoimmune thrombotic thrombocytopenic purpura, elevated plasma levels of human neutrophil proteins 1-3 inhibit proteolytic cleavage of von Willebrand factor by ADAMTS13, Vikram G. Pillai, PhD, of the University of Alabama at Birmingham, and colleagues reported.
The finding may explain how inflammation triggers microvascular thrombosis in these patients and potentially others with immune thrombotic disorders, according to the researchers (Blood 2016;128:110-9).
They performed enzyme-linked immunosorbent assays and found markedly increased levels of plasma human neutrophil proteins (HNPs) 1-3 in most of the patients with acquired autoimmune thrombotic thrombocytopenic purpura (TTP). The median levels in the 19 patients were 170 ng/mL, compared with 23 ng/mL in 18 healthy controls, a statistically significant difference (P less than .0001).
Liquid chromatography plus tandem mass spectrometry similarly confirmed statistically significant increases in HNP1, HNP2, and HNP3 in patient samples (P less than .001).
Measures of HNPs 1-3 by both methods correlated well, and the researchers concluded that HNPs 1-3 likely inhibit ADAMTS13 activity by binding to the central A2 domain of von Willebrand factor and physically blocking ADAMTS13 binding.
The researchers had no relevant financial disclosures.
On Twitter @maryjodales
In patients with acquired autoimmune thrombotic thrombocytopenic purpura, elevated plasma levels of human neutrophil proteins 1-3 inhibit proteolytic cleavage of von Willebrand factor by ADAMTS13, Vikram G. Pillai, PhD, of the University of Alabama at Birmingham, and colleagues reported.
The finding may explain how inflammation triggers microvascular thrombosis in these patients and potentially others with immune thrombotic disorders, according to the researchers (Blood 2016;128:110-9).
They performed enzyme-linked immunosorbent assays and found markedly increased levels of plasma human neutrophil proteins (HNPs) 1-3 in most of the patients with acquired autoimmune thrombotic thrombocytopenic purpura (TTP). The median levels in the 19 patients were 170 ng/mL, compared with 23 ng/mL in 18 healthy controls, a statistically significant difference (P less than .0001).
Liquid chromatography plus tandem mass spectrometry similarly confirmed statistically significant increases in HNP1, HNP2, and HNP3 in patient samples (P less than .001).
Measures of HNPs 1-3 by both methods correlated well, and the researchers concluded that HNPs 1-3 likely inhibit ADAMTS13 activity by binding to the central A2 domain of von Willebrand factor and physically blocking ADAMTS13 binding.
The researchers had no relevant financial disclosures.
On Twitter @maryjodales
FROM BLOOD
Key clinical point: In patients with acquired autoimmune thrombotic thrombocytopenic purpura, elevated plasma levels of human neutrophil proteins 1-3 inhibit proteolytic cleavage of von Willebrand factor by ADAMTS13.
Major finding: The median levels of plasma human neutrophil proteins 1-3 in patients with acquired autoimmune TTP were 170 ng/mL, compared with 23 ng/mL in healthy controls, a statistically significant difference (P less than .0001).
Data source: Studies in 19 patients with TTP and 18 control subjects.
Disclosures: The researchers had no relevant financial disclosures.
Dematin key to erythrocyte membrane stability in mice
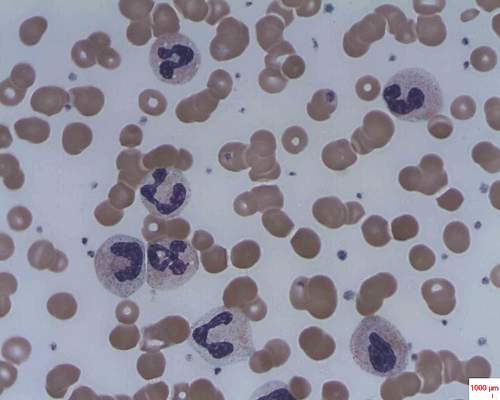
Dematin is newly recognized as a protein that is crucial to red blood cell (RBC) membrane integrity, and dematin’s absence in mice resulted in severe abnormalities of erythrocyte shape, membrane stability, and hemolytic anemia, Yunzhe Lu of Tufts University, Boston, and her colleagues reported in the journal Blood.
The finding indicates that dematin is the major determinant of membrane stability within the junctional protein complex.
The researchers defined the role of dematin by designing a mouse model that lacked the protein. Affected mice developed severe anemia and had abnormally shaped erythrocytes with unstable membranes.
They examined the mechanism behind erythrocyte membrane instability in the mice by using membrane protein analysis, domain mapping, electron microscopy, and dynamic deformability measurements. Although many membrane and cytoskeletal proteins remained at their normal levels, spectrin, adducin, and actin were greatly reduced in these erythrocytes. The findings indicate that dematin plays a critical role in maintaining the fundamental properties of the erythrocyte’s membrane cytoskeleton complex, the researchers wrote (Blood 2016;128:93-103).
On Twitter @maryjodales
Can these findings in the erythrocytes of genetically altered mice be extrapolated to humans?
While similar, membrane composition differs in mouse and human erythrocytes. The junctional complex contains Rh polypeptides in mice but does not in humans. Glucose transporter 1 (Glut1), which associates with dematin and the adducins in humans, is not expressed in the mature erythrocytes of mice. The authors propose a model in which adducin stabilized by dematin provides linkage to the plasma membrane via band 3; however, the relatively mild phenotype seen in the alpha adducin knockout mouse argues for additional linkages, likely via dematin.
It will be important to determine the role of dematin and the effect of its deficiency in junctional complex assembly, in regulation of membrane deformability and stability in human erythrocytes, and in the context of its identified association with Glut1. Given the importance of phosphorylation in regulation of dematin-binding function and interactions, and in light of the gross disruptive effects of dematin absence reported in the study by Ms. Lu and her colleagues, investigation of the role of dematin modification in junctional protein complex assembly, enucleation and cytoskeletal remodeling, and response to malaria invasion of the red blood cell will all represent important areas of future research.
Timothy J. Satchwell, PhD, and Ashley M. Toye, PhD, of the University of Bristol, England, made their comments in an accompanying editorial (Blood. 2016;128:11-12).
Can these findings in the erythrocytes of genetically altered mice be extrapolated to humans?
While similar, membrane composition differs in mouse and human erythrocytes. The junctional complex contains Rh polypeptides in mice but does not in humans. Glucose transporter 1 (Glut1), which associates with dematin and the adducins in humans, is not expressed in the mature erythrocytes of mice. The authors propose a model in which adducin stabilized by dematin provides linkage to the plasma membrane via band 3; however, the relatively mild phenotype seen in the alpha adducin knockout mouse argues for additional linkages, likely via dematin.
It will be important to determine the role of dematin and the effect of its deficiency in junctional complex assembly, in regulation of membrane deformability and stability in human erythrocytes, and in the context of its identified association with Glut1. Given the importance of phosphorylation in regulation of dematin-binding function and interactions, and in light of the gross disruptive effects of dematin absence reported in the study by Ms. Lu and her colleagues, investigation of the role of dematin modification in junctional protein complex assembly, enucleation and cytoskeletal remodeling, and response to malaria invasion of the red blood cell will all represent important areas of future research.
Timothy J. Satchwell, PhD, and Ashley M. Toye, PhD, of the University of Bristol, England, made their comments in an accompanying editorial (Blood. 2016;128:11-12).
Can these findings in the erythrocytes of genetically altered mice be extrapolated to humans?
While similar, membrane composition differs in mouse and human erythrocytes. The junctional complex contains Rh polypeptides in mice but does not in humans. Glucose transporter 1 (Glut1), which associates with dematin and the adducins in humans, is not expressed in the mature erythrocytes of mice. The authors propose a model in which adducin stabilized by dematin provides linkage to the plasma membrane via band 3; however, the relatively mild phenotype seen in the alpha adducin knockout mouse argues for additional linkages, likely via dematin.
It will be important to determine the role of dematin and the effect of its deficiency in junctional complex assembly, in regulation of membrane deformability and stability in human erythrocytes, and in the context of its identified association with Glut1. Given the importance of phosphorylation in regulation of dematin-binding function and interactions, and in light of the gross disruptive effects of dematin absence reported in the study by Ms. Lu and her colleagues, investigation of the role of dematin modification in junctional protein complex assembly, enucleation and cytoskeletal remodeling, and response to malaria invasion of the red blood cell will all represent important areas of future research.
Timothy J. Satchwell, PhD, and Ashley M. Toye, PhD, of the University of Bristol, England, made their comments in an accompanying editorial (Blood. 2016;128:11-12).
Dematin is newly recognized as a protein that is crucial to red blood cell (RBC) membrane integrity, and dematin’s absence in mice resulted in severe abnormalities of erythrocyte shape, membrane stability, and hemolytic anemia, Yunzhe Lu of Tufts University, Boston, and her colleagues reported in the journal Blood.
The finding indicates that dematin is the major determinant of membrane stability within the junctional protein complex.
The researchers defined the role of dematin by designing a mouse model that lacked the protein. Affected mice developed severe anemia and had abnormally shaped erythrocytes with unstable membranes.
They examined the mechanism behind erythrocyte membrane instability in the mice by using membrane protein analysis, domain mapping, electron microscopy, and dynamic deformability measurements. Although many membrane and cytoskeletal proteins remained at their normal levels, spectrin, adducin, and actin were greatly reduced in these erythrocytes. The findings indicate that dematin plays a critical role in maintaining the fundamental properties of the erythrocyte’s membrane cytoskeleton complex, the researchers wrote (Blood 2016;128:93-103).
On Twitter @maryjodales
Dematin is newly recognized as a protein that is crucial to red blood cell (RBC) membrane integrity, and dematin’s absence in mice resulted in severe abnormalities of erythrocyte shape, membrane stability, and hemolytic anemia, Yunzhe Lu of Tufts University, Boston, and her colleagues reported in the journal Blood.
The finding indicates that dematin is the major determinant of membrane stability within the junctional protein complex.
The researchers defined the role of dematin by designing a mouse model that lacked the protein. Affected mice developed severe anemia and had abnormally shaped erythrocytes with unstable membranes.
They examined the mechanism behind erythrocyte membrane instability in the mice by using membrane protein analysis, domain mapping, electron microscopy, and dynamic deformability measurements. Although many membrane and cytoskeletal proteins remained at their normal levels, spectrin, adducin, and actin were greatly reduced in these erythrocytes. The findings indicate that dematin plays a critical role in maintaining the fundamental properties of the erythrocyte’s membrane cytoskeleton complex, the researchers wrote (Blood 2016;128:93-103).
On Twitter @maryjodales
FROM BLOOD
Key clinical point: Dematin is newly recognized as a protein crucial to the integrity of red blood cell membranes.
Major finding: Dematin’s absence in mice resulted in severe abnormalities of erythrocyte shape, membrane stability, and hemolytic anemia.
Data source: Studies in a newly created mouse model designed to lack dematin.
Disclosures: The researchers had no relevant financial disclosures.
Adding obinutuzumab to bendamustine boosts progression-free survival in rituximab-refractory indolent non-Hodgkin lymphoma
Obinutuzumab and bendamustine followed by obinutuzumab maintenance therapy was superior to bendamustine monotherapy based on progression-free survival in rituximab-refractory patients with indolent non-Hodgkin lymphoma, based on a study published online in the Lancet Oncology.
After a median follow-up of 22 months in the obinutuzumab plus bendamustine group and 20 months in the bendamustine monotherapy group, progression-free survival was significantly longer with obinutuzumab plus bendamustine (median not reached; 95% confidence interval, 22.5 months – not estimable) than with bendamustine monotherapy (14.9 months, range, 12.8-16.6; hazard ratio, 0.55; 95% CI 0.40-0.74; P = .0001). About two-thirds of the nearly 400 patients in both study arms had grade 3-5 adverse events.
The anti-CD20 monoclonal antibody obinutuzumab is an option when patients with indolent non-Hodgkin lymphoma relapse or don’t achieve adequate disease control with rituximab-based treatment, wrote Laurie H. Sehn, MD, of the British Columbia Cancer Agency and the University of British Columbia, Vancouver, and her colleagues.
In an open-label, randomized, phase III study called GADOLIN, patients with CD20-positive indolent non-Hodgkin lymphoma were stratified by indolent non-Hodgkin lymphoma subtype, rituximab-refractory type, number of previous therapies, and geographic region.
For the study, 194 patients were assigned to obinutuzumab plus bendamustine and 202 to bendamustine monotherapy. Trial participants received six 28-day cycles with either obinutuzumab plus bendamustine (obinutuzumab 1,000 mg on days 1, 8, and 15, cycle 1; and on day 1, cycles 2-6) plus bendamustine (90 mg/m2 per day on days 1 and 2, cycles 1-6) or bendamustine monotherapy (120 mg/m2 per day on days 1 and 2 of all cycles). Patients in the obinutuzumab plus bendamustine group whose disease did not progress received obinutuzumab maintenance therapy of 1,000 mg once every 2 months for up to 2 years.
Grade 3-5 adverse events occurred in 68% of 194 patients in the obinutuzumab plus bendamustine group and in 62% of 198 patients in the bendamustine monotherapy group. Grade 3 or worse neutropenia affected 33% of the obinutuzumab plus bendamustine group and 26% of the bendamustine monotherapy group. Other grade 3 or worse events included thrombocytopenia in 11% and 16%, anemia in 8% and 10%, and infusion-related reactions in 11% and 6%. Serious adverse events occurred in 38% in the obinutuzumab plus bendamustine group and in 33% in the bendamustine monotherapy group. Adverse events resulted in death in 6% of patients in each group.
The study was funded by Hoffmann-La Roche. Genentech, the maker of obinutuzumab (Gazyva) in the United States, is a wholly owned member of the Roche Group. Dr. Sehn receives honoraria and is a consultant or advisor to Genentech as well as several other drug companies.
On Twitter @maryjodales
Obinutuzumab and bendamustine followed by obinutuzumab maintenance therapy was superior to bendamustine monotherapy based on progression-free survival in rituximab-refractory patients with indolent non-Hodgkin lymphoma, based on a study published online in the Lancet Oncology.
After a median follow-up of 22 months in the obinutuzumab plus bendamustine group and 20 months in the bendamustine monotherapy group, progression-free survival was significantly longer with obinutuzumab plus bendamustine (median not reached; 95% confidence interval, 22.5 months – not estimable) than with bendamustine monotherapy (14.9 months, range, 12.8-16.6; hazard ratio, 0.55; 95% CI 0.40-0.74; P = .0001). About two-thirds of the nearly 400 patients in both study arms had grade 3-5 adverse events.
The anti-CD20 monoclonal antibody obinutuzumab is an option when patients with indolent non-Hodgkin lymphoma relapse or don’t achieve adequate disease control with rituximab-based treatment, wrote Laurie H. Sehn, MD, of the British Columbia Cancer Agency and the University of British Columbia, Vancouver, and her colleagues.
In an open-label, randomized, phase III study called GADOLIN, patients with CD20-positive indolent non-Hodgkin lymphoma were stratified by indolent non-Hodgkin lymphoma subtype, rituximab-refractory type, number of previous therapies, and geographic region.
For the study, 194 patients were assigned to obinutuzumab plus bendamustine and 202 to bendamustine monotherapy. Trial participants received six 28-day cycles with either obinutuzumab plus bendamustine (obinutuzumab 1,000 mg on days 1, 8, and 15, cycle 1; and on day 1, cycles 2-6) plus bendamustine (90 mg/m2 per day on days 1 and 2, cycles 1-6) or bendamustine monotherapy (120 mg/m2 per day on days 1 and 2 of all cycles). Patients in the obinutuzumab plus bendamustine group whose disease did not progress received obinutuzumab maintenance therapy of 1,000 mg once every 2 months for up to 2 years.
Grade 3-5 adverse events occurred in 68% of 194 patients in the obinutuzumab plus bendamustine group and in 62% of 198 patients in the bendamustine monotherapy group. Grade 3 or worse neutropenia affected 33% of the obinutuzumab plus bendamustine group and 26% of the bendamustine monotherapy group. Other grade 3 or worse events included thrombocytopenia in 11% and 16%, anemia in 8% and 10%, and infusion-related reactions in 11% and 6%. Serious adverse events occurred in 38% in the obinutuzumab plus bendamustine group and in 33% in the bendamustine monotherapy group. Adverse events resulted in death in 6% of patients in each group.
The study was funded by Hoffmann-La Roche. Genentech, the maker of obinutuzumab (Gazyva) in the United States, is a wholly owned member of the Roche Group. Dr. Sehn receives honoraria and is a consultant or advisor to Genentech as well as several other drug companies.
On Twitter @maryjodales
Obinutuzumab and bendamustine followed by obinutuzumab maintenance therapy was superior to bendamustine monotherapy based on progression-free survival in rituximab-refractory patients with indolent non-Hodgkin lymphoma, based on a study published online in the Lancet Oncology.
After a median follow-up of 22 months in the obinutuzumab plus bendamustine group and 20 months in the bendamustine monotherapy group, progression-free survival was significantly longer with obinutuzumab plus bendamustine (median not reached; 95% confidence interval, 22.5 months – not estimable) than with bendamustine monotherapy (14.9 months, range, 12.8-16.6; hazard ratio, 0.55; 95% CI 0.40-0.74; P = .0001). About two-thirds of the nearly 400 patients in both study arms had grade 3-5 adverse events.
The anti-CD20 monoclonal antibody obinutuzumab is an option when patients with indolent non-Hodgkin lymphoma relapse or don’t achieve adequate disease control with rituximab-based treatment, wrote Laurie H. Sehn, MD, of the British Columbia Cancer Agency and the University of British Columbia, Vancouver, and her colleagues.
In an open-label, randomized, phase III study called GADOLIN, patients with CD20-positive indolent non-Hodgkin lymphoma were stratified by indolent non-Hodgkin lymphoma subtype, rituximab-refractory type, number of previous therapies, and geographic region.
For the study, 194 patients were assigned to obinutuzumab plus bendamustine and 202 to bendamustine monotherapy. Trial participants received six 28-day cycles with either obinutuzumab plus bendamustine (obinutuzumab 1,000 mg on days 1, 8, and 15, cycle 1; and on day 1, cycles 2-6) plus bendamustine (90 mg/m2 per day on days 1 and 2, cycles 1-6) or bendamustine monotherapy (120 mg/m2 per day on days 1 and 2 of all cycles). Patients in the obinutuzumab plus bendamustine group whose disease did not progress received obinutuzumab maintenance therapy of 1,000 mg once every 2 months for up to 2 years.
Grade 3-5 adverse events occurred in 68% of 194 patients in the obinutuzumab plus bendamustine group and in 62% of 198 patients in the bendamustine monotherapy group. Grade 3 or worse neutropenia affected 33% of the obinutuzumab plus bendamustine group and 26% of the bendamustine monotherapy group. Other grade 3 or worse events included thrombocytopenia in 11% and 16%, anemia in 8% and 10%, and infusion-related reactions in 11% and 6%. Serious adverse events occurred in 38% in the obinutuzumab plus bendamustine group and in 33% in the bendamustine monotherapy group. Adverse events resulted in death in 6% of patients in each group.
The study was funded by Hoffmann-La Roche. Genentech, the maker of obinutuzumab (Gazyva) in the United States, is a wholly owned member of the Roche Group. Dr. Sehn receives honoraria and is a consultant or advisor to Genentech as well as several other drug companies.
On Twitter @maryjodales
FROM THE LANCET ONCOLOGY
Key clinical point: Obinutuzumab is an option when patients with indolent non-Hodgkin lymphoma relapse or don’t achieve adequate disease control with rituximab-based treatment.
Major finding: Progression-free survival was significantly longer with obinutuzumab plus bendamustine (median not reached; 95% CI, 22.5 months – not estimable) than with bendamustine monotherapy (14.9 months, range,12.8-16.6 months; hazard ratio, 0.55; 95% CI, 0.40-0.74; P = ·0001).
Data source: An open-label, randomized, phase III study of 396 patients.
Disclosures: The study was funded by Hoffmann-La Roche. Genentech, the maker of obinutuzumab (Gazyva) in the United States, is a wholly owned member of the Roche Group. Dr. Sehn receives honoraria and is a consultant or adviser to Genentech as well as several other drug companies.
Acalabrutinib shows efficacy as monotherapy in untreated CLL
CHICAGO – Acalabrutinib, which has shown efficacy in relapsed chronic lymphocytic leukemia, has now shown efficacy as a monotherapy for patients with previously untreated CLL, based on results from an ongoing phase I-II study presented as a poster at the annual meeting of the American Society of Clinical Oncology.
In a 74-patient study, best overall response rate was 96%, and median time to response was 2 months. CLL has not progressed in any of the patients, and none have experienced Richter’s transformation, Dr. John C. Byrd, the D. Warren Brown Chair of Leukemia Research at The Ohio State University, Columbus, and his colleagues reported. Based on its favorable safety profile and durable response rates, a phase III trialof acalabrutinib therapy has been initiated (NCT02475681).
Oral acalabrutinib was given at doses of 100 mg twice daily to 37 patients or 200 mg daily to 37 other patients. About half of the patients had bulky lymph nodes of at least 5 cm and 38 of 67 patients had an unmutated IGHV gene. Median time on the study was 11 months.
All patients had rapid declines in lymphadenopathy. Both dose schedules were associated with clinical activity, with Bruton’s tyrosine kinase occupancy highest at 98% with twice-daily dosing and 93% with once-daily dosing. Treatment-related lymphocytosis occurred in 39 of 74 patients and resolved in 38 of the 39. In general, lymphocytosis peaked at a median of 1 week and resolved by a median of 7 weeks.
Acalabrutinib was well tolerated with 72 of 74 patients continuing on the drug. Most adverse events were grade 2 or less, and included headache (42%), diarrhea (35%), arthralgia (22%), contusion (18%), nausea (18%) and increased weight (18%). Grade 3-4 adverse events that occurred in at least two patients included syncope (two patients) and hypertension (two patients). There was one grade 3 upper GI bleed from a gastric ulcer and aspirin use, and one grade 5 case of pneumonia. No atrial fibrillation was reported.
Dr. Byrd receives research funding from Acerta Pharma, the maker of acalabrutinib, as well as from Genentech and Pharmacyclics.
On Twitter @maryjodales
CHICAGO – Acalabrutinib, which has shown efficacy in relapsed chronic lymphocytic leukemia, has now shown efficacy as a monotherapy for patients with previously untreated CLL, based on results from an ongoing phase I-II study presented as a poster at the annual meeting of the American Society of Clinical Oncology.
In a 74-patient study, best overall response rate was 96%, and median time to response was 2 months. CLL has not progressed in any of the patients, and none have experienced Richter’s transformation, Dr. John C. Byrd, the D. Warren Brown Chair of Leukemia Research at The Ohio State University, Columbus, and his colleagues reported. Based on its favorable safety profile and durable response rates, a phase III trialof acalabrutinib therapy has been initiated (NCT02475681).
Oral acalabrutinib was given at doses of 100 mg twice daily to 37 patients or 200 mg daily to 37 other patients. About half of the patients had bulky lymph nodes of at least 5 cm and 38 of 67 patients had an unmutated IGHV gene. Median time on the study was 11 months.
All patients had rapid declines in lymphadenopathy. Both dose schedules were associated with clinical activity, with Bruton’s tyrosine kinase occupancy highest at 98% with twice-daily dosing and 93% with once-daily dosing. Treatment-related lymphocytosis occurred in 39 of 74 patients and resolved in 38 of the 39. In general, lymphocytosis peaked at a median of 1 week and resolved by a median of 7 weeks.
Acalabrutinib was well tolerated with 72 of 74 patients continuing on the drug. Most adverse events were grade 2 or less, and included headache (42%), diarrhea (35%), arthralgia (22%), contusion (18%), nausea (18%) and increased weight (18%). Grade 3-4 adverse events that occurred in at least two patients included syncope (two patients) and hypertension (two patients). There was one grade 3 upper GI bleed from a gastric ulcer and aspirin use, and one grade 5 case of pneumonia. No atrial fibrillation was reported.
Dr. Byrd receives research funding from Acerta Pharma, the maker of acalabrutinib, as well as from Genentech and Pharmacyclics.
On Twitter @maryjodales
CHICAGO – Acalabrutinib, which has shown efficacy in relapsed chronic lymphocytic leukemia, has now shown efficacy as a monotherapy for patients with previously untreated CLL, based on results from an ongoing phase I-II study presented as a poster at the annual meeting of the American Society of Clinical Oncology.
In a 74-patient study, best overall response rate was 96%, and median time to response was 2 months. CLL has not progressed in any of the patients, and none have experienced Richter’s transformation, Dr. John C. Byrd, the D. Warren Brown Chair of Leukemia Research at The Ohio State University, Columbus, and his colleagues reported. Based on its favorable safety profile and durable response rates, a phase III trialof acalabrutinib therapy has been initiated (NCT02475681).
Oral acalabrutinib was given at doses of 100 mg twice daily to 37 patients or 200 mg daily to 37 other patients. About half of the patients had bulky lymph nodes of at least 5 cm and 38 of 67 patients had an unmutated IGHV gene. Median time on the study was 11 months.
All patients had rapid declines in lymphadenopathy. Both dose schedules were associated with clinical activity, with Bruton’s tyrosine kinase occupancy highest at 98% with twice-daily dosing and 93% with once-daily dosing. Treatment-related lymphocytosis occurred in 39 of 74 patients and resolved in 38 of the 39. In general, lymphocytosis peaked at a median of 1 week and resolved by a median of 7 weeks.
Acalabrutinib was well tolerated with 72 of 74 patients continuing on the drug. Most adverse events were grade 2 or less, and included headache (42%), diarrhea (35%), arthralgia (22%), contusion (18%), nausea (18%) and increased weight (18%). Grade 3-4 adverse events that occurred in at least two patients included syncope (two patients) and hypertension (two patients). There was one grade 3 upper GI bleed from a gastric ulcer and aspirin use, and one grade 5 case of pneumonia. No atrial fibrillation was reported.
Dr. Byrd receives research funding from Acerta Pharma, the maker of acalabrutinib, as well as from Genentech and Pharmacyclics.
On Twitter @maryjodales
FROM 2016 ASCO ANNUAL MEETING
Key clinical point: Acalabrutinib, which has shown efficacy in relapsed CLL, has now shown efficacy as a monotherapy for patients with previously untreated CLL.
Major finding: In a 74-patient study, best overall response rate was 96%, and median time to response was 2 months.
Data source: An ongoing phase I-II study.
Disclosures: Dr. Byrd receives research funding from Acerta Pharma, the maker of acalabrutinib, as well as from Genentech and Pharmacyclics.
Ibrutinib at below standard dose may achieve good survival in CLL
Ibrutinib given at doses lower than the standard dose of 420 mg/day was associated with comparable overall survival and progression-free survival as the standard dose in patients with chronic lymphocytic leukemia (CLL), based on the results of a multicenter, retrospective study submitted as a poster at the annual meeting of the American Society of Clinical Oncology.
The initial findings indicate patients who experience toxicity on the 420 mg/day dosage can still do well on a slightly lower dose of ibrutinib, reported Colleen Timlin, Pharm.D., of the Hospital of the University of Pennsylvania, Philadelphia, and her associates.
At a median follow-up of 13.5 months, the median progression-free survival was 37.4 months in the standard dose group and the median progression-free survival had not been reached in the reduced-dose group. The median overall survival had not been reached in either group. The hazard ratio in the reduced-dose group was 1.2 for progression-free survival and 0.6 for overall survival; neither difference was statistically significant. Best overall response rate was 85% in the standard-dose group and 84% in the reduced-dose group.
The study included 197 patients, 37 of whom were shifted to reduced doses of ibrutinib within 3 months of initiating therapy at the recommended 420 mg/day dosage. For reduced-dose patients, the median ibrutinib dose was 4.3 mg/kg per day. The most common reasons for reducing the ibrutinib dose were gastrointestinal toxicity, bleeding, rash, cardiotoxicity, and renal insufficiency, the researchers said.
Most of the patients treated with doses less than 420 mg/day still maintained a dose of greater than 2.5 mg/kg per day, which assured adequate Bruton’s tyrosine kinase occupancy. The 420 mg/day dosage noted in the labeling was established, based on achievement of greater than 90% Bruton’s tyrosine kinase occupancy. Fewer patients achieve greater than 90% occupancy at lower doses, but lower doses may not translate into inferior outcomes.
Weight-based dosing should be considered in future studies and pharmacoeconomic analyses. Comparative analyses of toxicity profiles stratified by ibrutinib dose are underway, according to Dr. Timlin and her colleagues.
Dr. Timlin had no relevant disclosures. Several of her colleagues had multiple financial disclosures.
On Twitter @maryjodales
Ibrutinib given at doses lower than the standard dose of 420 mg/day was associated with comparable overall survival and progression-free survival as the standard dose in patients with chronic lymphocytic leukemia (CLL), based on the results of a multicenter, retrospective study submitted as a poster at the annual meeting of the American Society of Clinical Oncology.
The initial findings indicate patients who experience toxicity on the 420 mg/day dosage can still do well on a slightly lower dose of ibrutinib, reported Colleen Timlin, Pharm.D., of the Hospital of the University of Pennsylvania, Philadelphia, and her associates.
At a median follow-up of 13.5 months, the median progression-free survival was 37.4 months in the standard dose group and the median progression-free survival had not been reached in the reduced-dose group. The median overall survival had not been reached in either group. The hazard ratio in the reduced-dose group was 1.2 for progression-free survival and 0.6 for overall survival; neither difference was statistically significant. Best overall response rate was 85% in the standard-dose group and 84% in the reduced-dose group.
The study included 197 patients, 37 of whom were shifted to reduced doses of ibrutinib within 3 months of initiating therapy at the recommended 420 mg/day dosage. For reduced-dose patients, the median ibrutinib dose was 4.3 mg/kg per day. The most common reasons for reducing the ibrutinib dose were gastrointestinal toxicity, bleeding, rash, cardiotoxicity, and renal insufficiency, the researchers said.
Most of the patients treated with doses less than 420 mg/day still maintained a dose of greater than 2.5 mg/kg per day, which assured adequate Bruton’s tyrosine kinase occupancy. The 420 mg/day dosage noted in the labeling was established, based on achievement of greater than 90% Bruton’s tyrosine kinase occupancy. Fewer patients achieve greater than 90% occupancy at lower doses, but lower doses may not translate into inferior outcomes.
Weight-based dosing should be considered in future studies and pharmacoeconomic analyses. Comparative analyses of toxicity profiles stratified by ibrutinib dose are underway, according to Dr. Timlin and her colleagues.
Dr. Timlin had no relevant disclosures. Several of her colleagues had multiple financial disclosures.
On Twitter @maryjodales
Ibrutinib given at doses lower than the standard dose of 420 mg/day was associated with comparable overall survival and progression-free survival as the standard dose in patients with chronic lymphocytic leukemia (CLL), based on the results of a multicenter, retrospective study submitted as a poster at the annual meeting of the American Society of Clinical Oncology.
The initial findings indicate patients who experience toxicity on the 420 mg/day dosage can still do well on a slightly lower dose of ibrutinib, reported Colleen Timlin, Pharm.D., of the Hospital of the University of Pennsylvania, Philadelphia, and her associates.
At a median follow-up of 13.5 months, the median progression-free survival was 37.4 months in the standard dose group and the median progression-free survival had not been reached in the reduced-dose group. The median overall survival had not been reached in either group. The hazard ratio in the reduced-dose group was 1.2 for progression-free survival and 0.6 for overall survival; neither difference was statistically significant. Best overall response rate was 85% in the standard-dose group and 84% in the reduced-dose group.
The study included 197 patients, 37 of whom were shifted to reduced doses of ibrutinib within 3 months of initiating therapy at the recommended 420 mg/day dosage. For reduced-dose patients, the median ibrutinib dose was 4.3 mg/kg per day. The most common reasons for reducing the ibrutinib dose were gastrointestinal toxicity, bleeding, rash, cardiotoxicity, and renal insufficiency, the researchers said.
Most of the patients treated with doses less than 420 mg/day still maintained a dose of greater than 2.5 mg/kg per day, which assured adequate Bruton’s tyrosine kinase occupancy. The 420 mg/day dosage noted in the labeling was established, based on achievement of greater than 90% Bruton’s tyrosine kinase occupancy. Fewer patients achieve greater than 90% occupancy at lower doses, but lower doses may not translate into inferior outcomes.
Weight-based dosing should be considered in future studies and pharmacoeconomic analyses. Comparative analyses of toxicity profiles stratified by ibrutinib dose are underway, according to Dr. Timlin and her colleagues.
Dr. Timlin had no relevant disclosures. Several of her colleagues had multiple financial disclosures.
On Twitter @maryjodales
Key clinical point: Ibrutinib given at doses lower than the standard dose of 420 mg/day may achieve comparable overall survival and progression-free survival.
Major finding: At a median follow-up of 13.5 months, the median progression-free survival was 37.4 months in the standard dose group, and the median progression-free survival had not been reached in the reduced-dose group.
Data source: A multicenter, retrospective study of 197 patients.
Disclosures: Dr. Timlin had no relevant disclosures. Several of her colleagues had multiple financial disclosures.
Mogamulizumab achieves objective responses in relapsed/refractory adult T-cell leukemia-lymphoma
CHICAGO – The anti-CCR4 monoclonal antibody mogamulizumab was superior to other investigator-selected therapies for the treatment of patients with relapsed/refractory adult T-cell leukemia-lymphoma (ATL), based on results from 71 patients in a prospective, multicenter, randomized study reported at the annual meeting of the American Society of Clinical Oncology.
Commonly used cytotoxic regimens provided limited therapeutic benefit for these patients, but mogamulizumab resulted in an objective response rate that supports its therapeutic potential in this setting, reported Dr. Adrienne Alise Phillips of New York Presbyterian/Weill Cornell Medical College, New York.
A malignancy of T-cells infected with HTLV-1, ATL has a poor prognosis with a median overall survival of less than 3 months in patients with relapsed/refractory disease. CCR4 is expressed in over 90% of ATL patients, and mogamulizumab is approved in Japan for ATL as well as for peripheral T-cell lymphoma and cutaneous T-cell lymphoma.
The 71 patients in the study were from the United States, the European Union and Latin America. The study is the largest randomized clinical trial of relapsed/refractory adult T-cell leukemia-lymphoma thus far conducted. The patients were randomized in 2:1 fashion 47:24 patients) to mogamulizumab, 1.0 mg/kg, given weekly for the first 4-week cycle and then biweekly, or to one of three investigator choice regimens [gemcitabine and oxaliplatin, DHAP (dexamethasone, high-dose cytarabine, and cisplatin), or pralatrexate]. Patients who were in the investigator-choice arm and whose disease progressed were permitted to cross over to mogamulizumab.
The primary endpoint was objective response rate based on modified Tsukasaki criteria and assessed by the treating investigator and in blinded fashion by independent review.
The objective response rate in the mogamulizumab-treated group was 23.4% (11 of 47) by independent review and 34% (16 of 47) by the treating investigator. In the investigator choice group, the overall response rate was 2 of 24 by independent review and 0 of 24 by the treating investigator.
The confirmed objective response rate after 1 month in the mogamulizumab-treated group was 10.6% by independent review and 14.9% by the treating investigator; there were no confirmed responses in the investigator-choice arm. Of 18 patients who crossed over to mogamulizumab, 3 responded. The median duration of response for mogamulizumab was 5 months; one patient had a complete response that lasted over 9 months and the survival data are not yet mature.
Mogamulizumab had few drug-related adverse events, primarily infusion reactions (46.8%), rash/drug eruption (25.5%) and infections (14.9%).
Dr. Phillips disclosed ties to Celgene, Genentech, and Takeda, as well as research funding from Kyowa Hakko Kirin, the sponsor of the study.
On Twitter @maryjodales
 |
| Mary Jo Dales/Frontline Medical News Dr. Sonali M. Smith |
Mogamulizumab was superior to investigator’s choice therapy in the largest prospective randomized trial of this very rare disease. Approximately one-third of patients responded, while the response to investigator’s choice therapies was zero. The potential impact of mogamulizumab on T-cell regulation is intriguing. Could it have applications in other T-cell non-Hodgkin’s lymphomas and cutaneous T-cell lymphomas?
Dr. Sonali M. Smith is with the University of Chicago and was the invited discussant of the study.
 |
| Mary Jo Dales/Frontline Medical News Dr. Sonali M. Smith |
Mogamulizumab was superior to investigator’s choice therapy in the largest prospective randomized trial of this very rare disease. Approximately one-third of patients responded, while the response to investigator’s choice therapies was zero. The potential impact of mogamulizumab on T-cell regulation is intriguing. Could it have applications in other T-cell non-Hodgkin’s lymphomas and cutaneous T-cell lymphomas?
Dr. Sonali M. Smith is with the University of Chicago and was the invited discussant of the study.
 |
| Mary Jo Dales/Frontline Medical News Dr. Sonali M. Smith |
Mogamulizumab was superior to investigator’s choice therapy in the largest prospective randomized trial of this very rare disease. Approximately one-third of patients responded, while the response to investigator’s choice therapies was zero. The potential impact of mogamulizumab on T-cell regulation is intriguing. Could it have applications in other T-cell non-Hodgkin’s lymphomas and cutaneous T-cell lymphomas?
Dr. Sonali M. Smith is with the University of Chicago and was the invited discussant of the study.
CHICAGO – The anti-CCR4 monoclonal antibody mogamulizumab was superior to other investigator-selected therapies for the treatment of patients with relapsed/refractory adult T-cell leukemia-lymphoma (ATL), based on results from 71 patients in a prospective, multicenter, randomized study reported at the annual meeting of the American Society of Clinical Oncology.
Commonly used cytotoxic regimens provided limited therapeutic benefit for these patients, but mogamulizumab resulted in an objective response rate that supports its therapeutic potential in this setting, reported Dr. Adrienne Alise Phillips of New York Presbyterian/Weill Cornell Medical College, New York.
A malignancy of T-cells infected with HTLV-1, ATL has a poor prognosis with a median overall survival of less than 3 months in patients with relapsed/refractory disease. CCR4 is expressed in over 90% of ATL patients, and mogamulizumab is approved in Japan for ATL as well as for peripheral T-cell lymphoma and cutaneous T-cell lymphoma.
The 71 patients in the study were from the United States, the European Union and Latin America. The study is the largest randomized clinical trial of relapsed/refractory adult T-cell leukemia-lymphoma thus far conducted. The patients were randomized in 2:1 fashion 47:24 patients) to mogamulizumab, 1.0 mg/kg, given weekly for the first 4-week cycle and then biweekly, or to one of three investigator choice regimens [gemcitabine and oxaliplatin, DHAP (dexamethasone, high-dose cytarabine, and cisplatin), or pralatrexate]. Patients who were in the investigator-choice arm and whose disease progressed were permitted to cross over to mogamulizumab.
The primary endpoint was objective response rate based on modified Tsukasaki criteria and assessed by the treating investigator and in blinded fashion by independent review.
The objective response rate in the mogamulizumab-treated group was 23.4% (11 of 47) by independent review and 34% (16 of 47) by the treating investigator. In the investigator choice group, the overall response rate was 2 of 24 by independent review and 0 of 24 by the treating investigator.
The confirmed objective response rate after 1 month in the mogamulizumab-treated group was 10.6% by independent review and 14.9% by the treating investigator; there were no confirmed responses in the investigator-choice arm. Of 18 patients who crossed over to mogamulizumab, 3 responded. The median duration of response for mogamulizumab was 5 months; one patient had a complete response that lasted over 9 months and the survival data are not yet mature.
Mogamulizumab had few drug-related adverse events, primarily infusion reactions (46.8%), rash/drug eruption (25.5%) and infections (14.9%).
Dr. Phillips disclosed ties to Celgene, Genentech, and Takeda, as well as research funding from Kyowa Hakko Kirin, the sponsor of the study.
On Twitter @maryjodales
CHICAGO – The anti-CCR4 monoclonal antibody mogamulizumab was superior to other investigator-selected therapies for the treatment of patients with relapsed/refractory adult T-cell leukemia-lymphoma (ATL), based on results from 71 patients in a prospective, multicenter, randomized study reported at the annual meeting of the American Society of Clinical Oncology.
Commonly used cytotoxic regimens provided limited therapeutic benefit for these patients, but mogamulizumab resulted in an objective response rate that supports its therapeutic potential in this setting, reported Dr. Adrienne Alise Phillips of New York Presbyterian/Weill Cornell Medical College, New York.
A malignancy of T-cells infected with HTLV-1, ATL has a poor prognosis with a median overall survival of less than 3 months in patients with relapsed/refractory disease. CCR4 is expressed in over 90% of ATL patients, and mogamulizumab is approved in Japan for ATL as well as for peripheral T-cell lymphoma and cutaneous T-cell lymphoma.
The 71 patients in the study were from the United States, the European Union and Latin America. The study is the largest randomized clinical trial of relapsed/refractory adult T-cell leukemia-lymphoma thus far conducted. The patients were randomized in 2:1 fashion 47:24 patients) to mogamulizumab, 1.0 mg/kg, given weekly for the first 4-week cycle and then biweekly, or to one of three investigator choice regimens [gemcitabine and oxaliplatin, DHAP (dexamethasone, high-dose cytarabine, and cisplatin), or pralatrexate]. Patients who were in the investigator-choice arm and whose disease progressed were permitted to cross over to mogamulizumab.
The primary endpoint was objective response rate based on modified Tsukasaki criteria and assessed by the treating investigator and in blinded fashion by independent review.
The objective response rate in the mogamulizumab-treated group was 23.4% (11 of 47) by independent review and 34% (16 of 47) by the treating investigator. In the investigator choice group, the overall response rate was 2 of 24 by independent review and 0 of 24 by the treating investigator.
The confirmed objective response rate after 1 month in the mogamulizumab-treated group was 10.6% by independent review and 14.9% by the treating investigator; there were no confirmed responses in the investigator-choice arm. Of 18 patients who crossed over to mogamulizumab, 3 responded. The median duration of response for mogamulizumab was 5 months; one patient had a complete response that lasted over 9 months and the survival data are not yet mature.
Mogamulizumab had few drug-related adverse events, primarily infusion reactions (46.8%), rash/drug eruption (25.5%) and infections (14.9%).
Dr. Phillips disclosed ties to Celgene, Genentech, and Takeda, as well as research funding from Kyowa Hakko Kirin, the sponsor of the study.
On Twitter @maryjodales
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: The anti-CCR4 monoclonal antibody mogamulizumab was superior to other investigator-selected therapies for the treatment of patients with relapsed/refractory adult T-cell leukemia-lymphoma.
Major finding: The confirmed objective response rate after 1 month in the mogamulizumab-treated group was 10.6% by independent review and 14.9% by the treating investigator; there were no confirmed responses in the investigator-choice arm.
Data source: Prospective, multicenter, randomized study of 71 patients from the United States, the European Union, and Latin America.
Disclosures: Dr. Phillips disclosed ties to Celgene, Genentech, and Takeda, as well as research funding from Kyowa Hakko Kirin, the sponsor of the study.
Alemtuzumab plus CHOP didn’t boost survival in elderly patients with peripheral T-cell lymphomas
CHICAGO – Adding the monoclonal anti-CD52 antibody alemtuzumab to CHOP (A-CHOP) increased response rates in elderly patients with peripheral T-cell lymphomas but did not improve their survival, based on the final results from 116 patients treated in the international ACT-2 phase III trial.
Complete responses were seen in 43% of 58 patients given CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone) and in 60% of 58 patients given A-CHOP in the trial. However, trial participants did not significantly differ in event-free survival and progression-free survival at 3 years.
Further, overall survival at 3 years was 38% for the patients given A-CHOP and 56% for the patients given CHOP. The poorer overall survival was mainly the result of treatment-related toxicity, Dr. Lorenz H. Trümper reported at the annual meeting of the American Society of Clinical Oncology.
The estimated 3-year disease-free survival is 25% for elderly patients with peripheral T-cell lymphomas. Previous phase II trials had indicated that alemtuzumab was active in primary and relapsed T-cell lymphoma, prompting the study of adjuvant alemtuzumab in combination with dose-dense CHOP-14 in patients with previously untreated peripheral T-cell lymphoma, he said.
Although the treatment protocol demanded stringent monitoring for cytomegalovirus and Epstein-Barr virus and anti-infective prophylaxis, there were more grade 3 or higher infections in the A-CHOP group (40%) than the CHOP group (21%). The higher infection rates were attributed to higher rates of grade 3/4 hematotoxicity in patients given A-CHOP. Grade 4 leukocytopenia was seen in 70% with A-CHOP and 54% with CHOP; grade 3/4 thrombocytopenia was seen in 19% given A-CHOP and 13% given CHOP, according to Dr. Trümper of the University of Göttingen, Germany.
For the study, 116 patients from 52 centers were randomized to receive either six cycles of CHOP or A-CHOP given at 14-day intervals with granulocyte-colony stimulating factor (G-CSF) support. Initially, patients received a total of 360 mg of alemtuzumab (90 mg given at each of the first four cycles of CHOP). After patient 39 was enrolled, the dose was reduced to 120 mg (30 mg given at each of the first four cycles of CHOP). Median patient age was 69 years, and 58% of the trial participants were men.
Treatment was completed as planned in 79% of the CHOP patients and in 57% of the A-CHOP patients.
The study was sponsored by the University of Göttingen. Dr. Trümper is a consultant or adviser to Hexal and Janssen-Ortho, and receives research funding from Genzyme, the maker of alemtuzumab (Lemtrada), as well as other drug companies.
On Twitter @maryjodales
CHICAGO – Adding the monoclonal anti-CD52 antibody alemtuzumab to CHOP (A-CHOP) increased response rates in elderly patients with peripheral T-cell lymphomas but did not improve their survival, based on the final results from 116 patients treated in the international ACT-2 phase III trial.
Complete responses were seen in 43% of 58 patients given CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone) and in 60% of 58 patients given A-CHOP in the trial. However, trial participants did not significantly differ in event-free survival and progression-free survival at 3 years.
Further, overall survival at 3 years was 38% for the patients given A-CHOP and 56% for the patients given CHOP. The poorer overall survival was mainly the result of treatment-related toxicity, Dr. Lorenz H. Trümper reported at the annual meeting of the American Society of Clinical Oncology.
The estimated 3-year disease-free survival is 25% for elderly patients with peripheral T-cell lymphomas. Previous phase II trials had indicated that alemtuzumab was active in primary and relapsed T-cell lymphoma, prompting the study of adjuvant alemtuzumab in combination with dose-dense CHOP-14 in patients with previously untreated peripheral T-cell lymphoma, he said.
Although the treatment protocol demanded stringent monitoring for cytomegalovirus and Epstein-Barr virus and anti-infective prophylaxis, there were more grade 3 or higher infections in the A-CHOP group (40%) than the CHOP group (21%). The higher infection rates were attributed to higher rates of grade 3/4 hematotoxicity in patients given A-CHOP. Grade 4 leukocytopenia was seen in 70% with A-CHOP and 54% with CHOP; grade 3/4 thrombocytopenia was seen in 19% given A-CHOP and 13% given CHOP, according to Dr. Trümper of the University of Göttingen, Germany.
For the study, 116 patients from 52 centers were randomized to receive either six cycles of CHOP or A-CHOP given at 14-day intervals with granulocyte-colony stimulating factor (G-CSF) support. Initially, patients received a total of 360 mg of alemtuzumab (90 mg given at each of the first four cycles of CHOP). After patient 39 was enrolled, the dose was reduced to 120 mg (30 mg given at each of the first four cycles of CHOP). Median patient age was 69 years, and 58% of the trial participants were men.
Treatment was completed as planned in 79% of the CHOP patients and in 57% of the A-CHOP patients.
The study was sponsored by the University of Göttingen. Dr. Trümper is a consultant or adviser to Hexal and Janssen-Ortho, and receives research funding from Genzyme, the maker of alemtuzumab (Lemtrada), as well as other drug companies.
On Twitter @maryjodales
CHICAGO – Adding the monoclonal anti-CD52 antibody alemtuzumab to CHOP (A-CHOP) increased response rates in elderly patients with peripheral T-cell lymphomas but did not improve their survival, based on the final results from 116 patients treated in the international ACT-2 phase III trial.
Complete responses were seen in 43% of 58 patients given CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone) and in 60% of 58 patients given A-CHOP in the trial. However, trial participants did not significantly differ in event-free survival and progression-free survival at 3 years.
Further, overall survival at 3 years was 38% for the patients given A-CHOP and 56% for the patients given CHOP. The poorer overall survival was mainly the result of treatment-related toxicity, Dr. Lorenz H. Trümper reported at the annual meeting of the American Society of Clinical Oncology.
The estimated 3-year disease-free survival is 25% for elderly patients with peripheral T-cell lymphomas. Previous phase II trials had indicated that alemtuzumab was active in primary and relapsed T-cell lymphoma, prompting the study of adjuvant alemtuzumab in combination with dose-dense CHOP-14 in patients with previously untreated peripheral T-cell lymphoma, he said.
Although the treatment protocol demanded stringent monitoring for cytomegalovirus and Epstein-Barr virus and anti-infective prophylaxis, there were more grade 3 or higher infections in the A-CHOP group (40%) than the CHOP group (21%). The higher infection rates were attributed to higher rates of grade 3/4 hematotoxicity in patients given A-CHOP. Grade 4 leukocytopenia was seen in 70% with A-CHOP and 54% with CHOP; grade 3/4 thrombocytopenia was seen in 19% given A-CHOP and 13% given CHOP, according to Dr. Trümper of the University of Göttingen, Germany.
For the study, 116 patients from 52 centers were randomized to receive either six cycles of CHOP or A-CHOP given at 14-day intervals with granulocyte-colony stimulating factor (G-CSF) support. Initially, patients received a total of 360 mg of alemtuzumab (90 mg given at each of the first four cycles of CHOP). After patient 39 was enrolled, the dose was reduced to 120 mg (30 mg given at each of the first four cycles of CHOP). Median patient age was 69 years, and 58% of the trial participants were men.
Treatment was completed as planned in 79% of the CHOP patients and in 57% of the A-CHOP patients.
The study was sponsored by the University of Göttingen. Dr. Trümper is a consultant or adviser to Hexal and Janssen-Ortho, and receives research funding from Genzyme, the maker of alemtuzumab (Lemtrada), as well as other drug companies.
On Twitter @maryjodales
AT ASCO 16
Key clinical point: Adding the monoclonal anti-CD52 antibody alemtuzumab to CHOP (A-CHOP) increased response rates in elderly patients with peripheral T-cell lymphomas but did not improve their survival.
Major finding: Overall survival at 3 years was 38% for the patients given A-CHOP and 56% for the patients given CHOP.
Data source: Results from 116 patients treated in the international ACT-2 phase III trial.
Disclosures: The study was sponsored by the University of Göttingen, Germany. Dr. Trümper is a consultant or adviser to Hexal and Janssen-Ortho, and receives research funding from Genzyme, the maker of alemtuzumab, as well as other drug companies.
Antibodies cut factor VIII half-life in patients with hemophilia A
Non-neutralizing, factor VIII–specific IgG antibodies can contribute significantly to reductions in factor VIII half-life in patients with hemophilia A, according to a study published online in Blood.
Screening for factor VIII–specific IgG may aid in tailoring factor VIII prophylactic regimens for hemophilia A patients, said Christoph J. Hofbauer, Ph.D., of the biopharmaceutical company Baxalta in Vienna, and his associates at the Medical University of Vienna.
The researchers examined the effect of factor VIII–specific IgG antibodies on factor VIII half-life in 42 adult patients with hemophilia A without inhibitors. Patients ranged in age from 18-61 years, and 37 of them had severe disease. Of the cohort, 31 received recombinant factor VIII concentrates and 11 received plasma-derived factor VIII concentrates (Blood. 2016 May 23 [Epub ahead of print])
In the initial antibody screen, 15 patients tested positive for factor VIII–binding IgG with titers of at least 1:20. Factor VIII–specific antibodies were found at titers of at least 1:40 in 9 of the 15 subjects. Most had low- to moderate-affinity IgG1 and IgG3 antibodies. One patient with high-affinity IgG4 antibodies went on to develop low titers of factor VIII inhibitors.
Patients with factor VIII–specific antibodies had a shorter factor VIII half-life (median 7.8 hours) than did patients without antibodies (median 10.4 hours).
Dr. Hofbauer is employed by Baxalta, which makes a variety of antihemophilic factors.
On Twitter @maryjodales
Non-neutralizing, factor VIII–specific IgG antibodies can contribute significantly to reductions in factor VIII half-life in patients with hemophilia A, according to a study published online in Blood.
Screening for factor VIII–specific IgG may aid in tailoring factor VIII prophylactic regimens for hemophilia A patients, said Christoph J. Hofbauer, Ph.D., of the biopharmaceutical company Baxalta in Vienna, and his associates at the Medical University of Vienna.
The researchers examined the effect of factor VIII–specific IgG antibodies on factor VIII half-life in 42 adult patients with hemophilia A without inhibitors. Patients ranged in age from 18-61 years, and 37 of them had severe disease. Of the cohort, 31 received recombinant factor VIII concentrates and 11 received plasma-derived factor VIII concentrates (Blood. 2016 May 23 [Epub ahead of print])
In the initial antibody screen, 15 patients tested positive for factor VIII–binding IgG with titers of at least 1:20. Factor VIII–specific antibodies were found at titers of at least 1:40 in 9 of the 15 subjects. Most had low- to moderate-affinity IgG1 and IgG3 antibodies. One patient with high-affinity IgG4 antibodies went on to develop low titers of factor VIII inhibitors.
Patients with factor VIII–specific antibodies had a shorter factor VIII half-life (median 7.8 hours) than did patients without antibodies (median 10.4 hours).
Dr. Hofbauer is employed by Baxalta, which makes a variety of antihemophilic factors.
On Twitter @maryjodales
Non-neutralizing, factor VIII–specific IgG antibodies can contribute significantly to reductions in factor VIII half-life in patients with hemophilia A, according to a study published online in Blood.
Screening for factor VIII–specific IgG may aid in tailoring factor VIII prophylactic regimens for hemophilia A patients, said Christoph J. Hofbauer, Ph.D., of the biopharmaceutical company Baxalta in Vienna, and his associates at the Medical University of Vienna.
The researchers examined the effect of factor VIII–specific IgG antibodies on factor VIII half-life in 42 adult patients with hemophilia A without inhibitors. Patients ranged in age from 18-61 years, and 37 of them had severe disease. Of the cohort, 31 received recombinant factor VIII concentrates and 11 received plasma-derived factor VIII concentrates (Blood. 2016 May 23 [Epub ahead of print])
In the initial antibody screen, 15 patients tested positive for factor VIII–binding IgG with titers of at least 1:20. Factor VIII–specific antibodies were found at titers of at least 1:40 in 9 of the 15 subjects. Most had low- to moderate-affinity IgG1 and IgG3 antibodies. One patient with high-affinity IgG4 antibodies went on to develop low titers of factor VIII inhibitors.
Patients with factor VIII–specific antibodies had a shorter factor VIII half-life (median 7.8 hours) than did patients without antibodies (median 10.4 hours).
Dr. Hofbauer is employed by Baxalta, which makes a variety of antihemophilic factors.
On Twitter @maryjodales
FROM BLOOD
Key clinical point: Non-neutralizing, factor VIII–specific IgG antibodies can contribute significantly to reductions in factor VIII half-life in patients with hemophilia A.
Major finding: Patients with factor VIII–specific antibodies had a shorter factor VIII half-life (median 7.8 hours) than did patients without antibodies (median 10.4 hours).
Data source: 42 adult patients, ranging in age from 18-61 years, with hemophilia A without inhibitors, 37 of whom had severe disease.
Disclosures: Dr. Hofbauer is employed by Baxalta, which makes a variety of antihemophilic factors.
Maintenance rituximab extends progression-free but not overall survival in CLL
CHICAGO – After 2 years of maintenance immunotherapy with rituximab, elderly patients with chronic lymphocytic leukemia had better rates of progression-free survival than did patients in an observation group, based on results of the CLL 2007 SA trial from the French FILO (French Innovative Leukemia Organisation) Group.
The two groups did not significantly differ in overall survival, however, with 92.6% estimated 3-year overall survival in the rituximab group and 87.2% in the observation group. Further, the patients given rituximab had more adverse events, based on data presented by Dr. Caroline Dartigeas of the University Hospital in Tours, France, at the annual meeting of the American Society of Clinical Oncology.
Given the cost and risk for events with rituximab, the findings raise the question of whether there are any meaningful benefits for maintenance rituximab after induction therapy, Dr. Jonathan W. Friedberg of the University of Rochester, N.Y., who was the discussant of the paper, remarked after the presentation. He asked whether there is any evidence that patients feel better if they’re in remission and, thus, their quality of life is improved.
The study included fit, treatment-naive patients aged 65 years and older with B-cell CLL who lacked del17p. Median patient age was 71.3 years, and two-thirds of the patients were men.
Patients received four cycles of induction therapy with fludarabine, cyclophosphamide, and rituximab on a shortened schedule chosen to reduce the risk of cumulative toxicity. At randomization, patients were stratified for immunoglobulin heavy chain variable (IGHV) status (54.8% of patients had unmutated status) and del11q (21.3% of patients had the deletion). Patients who had complete (25.7% of patients) or partial (62.8% of patients) responses were randomly allocated to either maintenance rituximab (202 patients given 500 mg/m2 twice per month for 2 years) or to observation (207 patients). Median follow-up from randomization was 43.6 months.
Median progression-free survival in the rituximab arm was 59.3 months (95% confidence interval, 49.6; not reached), compared with 49 months (95% CI, 40.9-60.5) in the observation group (hazard ratio, 0.597; 95% CI, 0.437-0.814; P = .0011), corresponding to 3-year progression-free survival of 83% and 64.2% in each arm, respectively.
Estimated overall survival at 3 years was 92.6% with rituximab maintenance and 87.2% in the observation group. Rituximab maintenance significantly improved progression-free survival in patients with and without del11q and in those with unmutated IGHV.
Serious adverse events for hematologic toxicity were seen in 6.9% of rituximab-treated patients and 1.9% of patients in the observation group (P = .027). Serious adverse events for infectious toxicity occurred in 18.8% of rituximab-treated patients and 10.1% of the observation group (P = .036). There were 69 deaths post randomization: 32 in the rituximab-treated group and 37 in the observation group. Secondary cancers, excluding basal cell carcinomas of the skin, occurred in 15.3% of the rituximab arm, including five cases of myelodysplastic syndrome, and in 11.1% of the observation group, including three cases of myelodysplastic syndrome.
Dr. Dartigeas is a consultant to Gilead Sciences and has provided expert testimony for Roche/Genentech. Genentech and Biogen jointly market rituximab (Rituxan).
On Twitter @maryjodales
CHICAGO – After 2 years of maintenance immunotherapy with rituximab, elderly patients with chronic lymphocytic leukemia had better rates of progression-free survival than did patients in an observation group, based on results of the CLL 2007 SA trial from the French FILO (French Innovative Leukemia Organisation) Group.
The two groups did not significantly differ in overall survival, however, with 92.6% estimated 3-year overall survival in the rituximab group and 87.2% in the observation group. Further, the patients given rituximab had more adverse events, based on data presented by Dr. Caroline Dartigeas of the University Hospital in Tours, France, at the annual meeting of the American Society of Clinical Oncology.
Given the cost and risk for events with rituximab, the findings raise the question of whether there are any meaningful benefits for maintenance rituximab after induction therapy, Dr. Jonathan W. Friedberg of the University of Rochester, N.Y., who was the discussant of the paper, remarked after the presentation. He asked whether there is any evidence that patients feel better if they’re in remission and, thus, their quality of life is improved.
The study included fit, treatment-naive patients aged 65 years and older with B-cell CLL who lacked del17p. Median patient age was 71.3 years, and two-thirds of the patients were men.
Patients received four cycles of induction therapy with fludarabine, cyclophosphamide, and rituximab on a shortened schedule chosen to reduce the risk of cumulative toxicity. At randomization, patients were stratified for immunoglobulin heavy chain variable (IGHV) status (54.8% of patients had unmutated status) and del11q (21.3% of patients had the deletion). Patients who had complete (25.7% of patients) or partial (62.8% of patients) responses were randomly allocated to either maintenance rituximab (202 patients given 500 mg/m2 twice per month for 2 years) or to observation (207 patients). Median follow-up from randomization was 43.6 months.
Median progression-free survival in the rituximab arm was 59.3 months (95% confidence interval, 49.6; not reached), compared with 49 months (95% CI, 40.9-60.5) in the observation group (hazard ratio, 0.597; 95% CI, 0.437-0.814; P = .0011), corresponding to 3-year progression-free survival of 83% and 64.2% in each arm, respectively.
Estimated overall survival at 3 years was 92.6% with rituximab maintenance and 87.2% in the observation group. Rituximab maintenance significantly improved progression-free survival in patients with and without del11q and in those with unmutated IGHV.
Serious adverse events for hematologic toxicity were seen in 6.9% of rituximab-treated patients and 1.9% of patients in the observation group (P = .027). Serious adverse events for infectious toxicity occurred in 18.8% of rituximab-treated patients and 10.1% of the observation group (P = .036). There were 69 deaths post randomization: 32 in the rituximab-treated group and 37 in the observation group. Secondary cancers, excluding basal cell carcinomas of the skin, occurred in 15.3% of the rituximab arm, including five cases of myelodysplastic syndrome, and in 11.1% of the observation group, including three cases of myelodysplastic syndrome.
Dr. Dartigeas is a consultant to Gilead Sciences and has provided expert testimony for Roche/Genentech. Genentech and Biogen jointly market rituximab (Rituxan).
On Twitter @maryjodales
CHICAGO – After 2 years of maintenance immunotherapy with rituximab, elderly patients with chronic lymphocytic leukemia had better rates of progression-free survival than did patients in an observation group, based on results of the CLL 2007 SA trial from the French FILO (French Innovative Leukemia Organisation) Group.
The two groups did not significantly differ in overall survival, however, with 92.6% estimated 3-year overall survival in the rituximab group and 87.2% in the observation group. Further, the patients given rituximab had more adverse events, based on data presented by Dr. Caroline Dartigeas of the University Hospital in Tours, France, at the annual meeting of the American Society of Clinical Oncology.
Given the cost and risk for events with rituximab, the findings raise the question of whether there are any meaningful benefits for maintenance rituximab after induction therapy, Dr. Jonathan W. Friedberg of the University of Rochester, N.Y., who was the discussant of the paper, remarked after the presentation. He asked whether there is any evidence that patients feel better if they’re in remission and, thus, their quality of life is improved.
The study included fit, treatment-naive patients aged 65 years and older with B-cell CLL who lacked del17p. Median patient age was 71.3 years, and two-thirds of the patients were men.
Patients received four cycles of induction therapy with fludarabine, cyclophosphamide, and rituximab on a shortened schedule chosen to reduce the risk of cumulative toxicity. At randomization, patients were stratified for immunoglobulin heavy chain variable (IGHV) status (54.8% of patients had unmutated status) and del11q (21.3% of patients had the deletion). Patients who had complete (25.7% of patients) or partial (62.8% of patients) responses were randomly allocated to either maintenance rituximab (202 patients given 500 mg/m2 twice per month for 2 years) or to observation (207 patients). Median follow-up from randomization was 43.6 months.
Median progression-free survival in the rituximab arm was 59.3 months (95% confidence interval, 49.6; not reached), compared with 49 months (95% CI, 40.9-60.5) in the observation group (hazard ratio, 0.597; 95% CI, 0.437-0.814; P = .0011), corresponding to 3-year progression-free survival of 83% and 64.2% in each arm, respectively.
Estimated overall survival at 3 years was 92.6% with rituximab maintenance and 87.2% in the observation group. Rituximab maintenance significantly improved progression-free survival in patients with and without del11q and in those with unmutated IGHV.
Serious adverse events for hematologic toxicity were seen in 6.9% of rituximab-treated patients and 1.9% of patients in the observation group (P = .027). Serious adverse events for infectious toxicity occurred in 18.8% of rituximab-treated patients and 10.1% of the observation group (P = .036). There were 69 deaths post randomization: 32 in the rituximab-treated group and 37 in the observation group. Secondary cancers, excluding basal cell carcinomas of the skin, occurred in 15.3% of the rituximab arm, including five cases of myelodysplastic syndrome, and in 11.1% of the observation group, including three cases of myelodysplastic syndrome.
Dr. Dartigeas is a consultant to Gilead Sciences and has provided expert testimony for Roche/Genentech. Genentech and Biogen jointly market rituximab (Rituxan).
On Twitter @maryjodales
AT 2016 ASCO ANNUAL MEETING
Key clinical point: Progression-free survival, but not overall survival, was improved after 2 years of maintenance immunotherapy with rituximab.
Major finding: Median progression-free survival in the rituximab arm was 59.3 months (95% CI, 49.6; not reached), compared with 49 months (95% CI, 40.9-60.5) in the observation group (HR, 0.597; 95% CI, 0.437-0.814; P = .0011), corresponding to a 3-year progression-free survival of 83% and 64.2% in each arm, respectively.
Data source: Maintenance rituximab (202 patients given 500 mg/m2 twice a month for 2 years) and observation (207 patients) in the CLL 2007 SA trial from the French FILO Group.
Disclosures: Dr. Dartigeas is a consultant to Gilead Sciences and has provided expert testimony for Roche/Genentech. Genentech and Biogen jointly market rituximab (Rituxan).
Brentuximab vedotin boosted PET-negative rate in Hodgkin
CHICAGO – Brentuximab vedotin appears to be safe and effective in eradicating residual disease after induction chemotherapy and may replace radiation for consolidation in patients with limited stage non-bulky Hodgkin lymphoma, Dr. Steven I. Park reported at the annual meeting of the American Society of Clinical Oncology.
After two cycles of ABVD [doxorubicin (Adriamycin), bleomycin, vinblastine, and dacarbazine], 72% of 40 evaluable patients achieved PET-negative disease. After completing brentuximab vedotin therapy, 90% of patients had PET-negative disease. With a median follow-up of 12 months, the estimated 1-year progression-free survival rate is 91%, and the overall survival rate is 96%.
The current standard therapy for limited stage Hodgkin lymphoma is about 4-6 cycles of chemotherapy with or without consolidative radiation therapy. The goal of the study was to reduce the number of cycles of chemotherapy and avoid radiation therapy, which has an unclear overall survival advantage and risks long-term side effects, noted Dr. Park of the University of North Carolina at Chapel Hill, Lineberger Comprehensive Cancer Center.
In this phase II multicenter study, 41 patients with previously untreated limited stage non-bulky Hodgkin lymphoma received ABVD followed by brentuximab vedotin (NCT01578967). Study patients’ median age was 29 years (range 19-67), and 46% presented with unfavorable disease. Over 90% of patients received four or fewer cycles of ABVD, and one patient received radiation due to disease progression.
Grade 3 or higher toxicities associated with brentuximab vedotin included neutropenia in three patients and peripheral neuropathy and rash in one patient each. One patient developed pancreatitis and died due to sepsis and hepatic failure, a rare complication of brentuximab vedotin that cautions regarding its use in patients with hepatic function limitations, Dr. Park said.
According to Seattle Genetics, the maker of brentuximab vedotin, the drug is an anti-CD30 monoclonal antibody attached by a protease-cleavable linker to the cytotoxic agent monomethyl auristatin E, which leads to target cell death when internalized into CD30-expressing tumor cells.
Dr. Park disclosed research funding from Seattle Genetics, the maker of brentuximab vedotin, as well as Teva.
On Twitter @maryjodales
CHICAGO – Brentuximab vedotin appears to be safe and effective in eradicating residual disease after induction chemotherapy and may replace radiation for consolidation in patients with limited stage non-bulky Hodgkin lymphoma, Dr. Steven I. Park reported at the annual meeting of the American Society of Clinical Oncology.
After two cycles of ABVD [doxorubicin (Adriamycin), bleomycin, vinblastine, and dacarbazine], 72% of 40 evaluable patients achieved PET-negative disease. After completing brentuximab vedotin therapy, 90% of patients had PET-negative disease. With a median follow-up of 12 months, the estimated 1-year progression-free survival rate is 91%, and the overall survival rate is 96%.
The current standard therapy for limited stage Hodgkin lymphoma is about 4-6 cycles of chemotherapy with or without consolidative radiation therapy. The goal of the study was to reduce the number of cycles of chemotherapy and avoid radiation therapy, which has an unclear overall survival advantage and risks long-term side effects, noted Dr. Park of the University of North Carolina at Chapel Hill, Lineberger Comprehensive Cancer Center.
In this phase II multicenter study, 41 patients with previously untreated limited stage non-bulky Hodgkin lymphoma received ABVD followed by brentuximab vedotin (NCT01578967). Study patients’ median age was 29 years (range 19-67), and 46% presented with unfavorable disease. Over 90% of patients received four or fewer cycles of ABVD, and one patient received radiation due to disease progression.
Grade 3 or higher toxicities associated with brentuximab vedotin included neutropenia in three patients and peripheral neuropathy and rash in one patient each. One patient developed pancreatitis and died due to sepsis and hepatic failure, a rare complication of brentuximab vedotin that cautions regarding its use in patients with hepatic function limitations, Dr. Park said.
According to Seattle Genetics, the maker of brentuximab vedotin, the drug is an anti-CD30 monoclonal antibody attached by a protease-cleavable linker to the cytotoxic agent monomethyl auristatin E, which leads to target cell death when internalized into CD30-expressing tumor cells.
Dr. Park disclosed research funding from Seattle Genetics, the maker of brentuximab vedotin, as well as Teva.
On Twitter @maryjodales
CHICAGO – Brentuximab vedotin appears to be safe and effective in eradicating residual disease after induction chemotherapy and may replace radiation for consolidation in patients with limited stage non-bulky Hodgkin lymphoma, Dr. Steven I. Park reported at the annual meeting of the American Society of Clinical Oncology.
After two cycles of ABVD [doxorubicin (Adriamycin), bleomycin, vinblastine, and dacarbazine], 72% of 40 evaluable patients achieved PET-negative disease. After completing brentuximab vedotin therapy, 90% of patients had PET-negative disease. With a median follow-up of 12 months, the estimated 1-year progression-free survival rate is 91%, and the overall survival rate is 96%.
The current standard therapy for limited stage Hodgkin lymphoma is about 4-6 cycles of chemotherapy with or without consolidative radiation therapy. The goal of the study was to reduce the number of cycles of chemotherapy and avoid radiation therapy, which has an unclear overall survival advantage and risks long-term side effects, noted Dr. Park of the University of North Carolina at Chapel Hill, Lineberger Comprehensive Cancer Center.
In this phase II multicenter study, 41 patients with previously untreated limited stage non-bulky Hodgkin lymphoma received ABVD followed by brentuximab vedotin (NCT01578967). Study patients’ median age was 29 years (range 19-67), and 46% presented with unfavorable disease. Over 90% of patients received four or fewer cycles of ABVD, and one patient received radiation due to disease progression.
Grade 3 or higher toxicities associated with brentuximab vedotin included neutropenia in three patients and peripheral neuropathy and rash in one patient each. One patient developed pancreatitis and died due to sepsis and hepatic failure, a rare complication of brentuximab vedotin that cautions regarding its use in patients with hepatic function limitations, Dr. Park said.
According to Seattle Genetics, the maker of brentuximab vedotin, the drug is an anti-CD30 monoclonal antibody attached by a protease-cleavable linker to the cytotoxic agent monomethyl auristatin E, which leads to target cell death when internalized into CD30-expressing tumor cells.
Dr. Park disclosed research funding from Seattle Genetics, the maker of brentuximab vedotin, as well as Teva.
On Twitter @maryjodales
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: Brentuximab vedotin appears to eradicate residual disease after induction chemotherapy in a small study of patients with limited stage non-bulky Hodgkin lymphoma.
Major finding: In 40 evaluable patients, 72% were PET-negative after two cycles of ABVD; brentuximab vedotin consolidation boosted PET-negative status to 90% of patients.
Data source: A phase II multicenter study of 41 patients with previously untreated limited stage non-bulky Hodgkin lymphoma.
Disclosures: Dr. Park disclosed research funding from Seattle Genetics, the maker of brentuximab vedotin, as well as Teva.