User login
Provider Expectations and Experiences
Comanagement is common in hospital medicine practice. And yet, there is no consensus about how comanagement is different from traditional consultative practice. At its core, hospitalist comanagement is a practice arrangement wherein hospitalists and other specialists manage complex patients collaboratively. Beyond this, Huddleston et al. distinguish comanagement from traditional consultations in the comanaging hospitalists' prerogative to provide direct medical care in addition to consultative advice.1 Siegal focuses on the shared responsibility and authority among partnering providers in the comanagement model.2 Whinney and Michota see comanagement as patient care referral at the onset of a care episode, in contrast to consultations that are activated to address emergent problems.3 In a recent study that found the growing adoption of medical comanagement in Medicare beneficiaries (as much as 40% of surgical hospitalizations in 2006), comanagement was defined as an intensive form of consultation involving a claim for evaluation and management services on greater than 70% of inpatient days.4
In addition to the intensity, frequency, timing, responsibility, and authority of care, comanagement may be described by participating physicians' roles. With recent attention on multidisciplinary teams and an increasing focus on collaborative care, many of the hierarchical relations among healthcare providers are breaking down.5 Several studies of multidisciplinary teams suggest that more egalitarian, rather than hierarchical, problem‐solving and decision‐making among team members are beneficial to patients.67 However, neither the intended nor natural team structure under comanagement is known. We sought to shed some light on provider interactions by characterizing the expectations and experiences of providers of a comanaged service. The findings yielded an opportunity to generate an evolving, but conceptually supported definition of comanagement.
SETTING
We conducted a survey study of providers participating in a comanaged inpatient hepatology service at the University of Chicago Medical Center, a 572‐bed urban teaching hospital. The service was created in 2006, partly to address staffing problems related to housestaff work hour restrictions and partly to improve the care of candidates and recipients of liver transplantation. Nonsurgical floor patients with liver diseases were managed on the service by two collaborating teams of providers. The hepatology team consisted of an attending physician and a fellow, while the hospitalist team consisted of a hospitalist and one or two nonphysician providers (physician assistant or nurse practitioner). The practice model is characterized as comanagement because of the highly interdependent nature of the team's daily tasks and the norms of intensive communication, through formal joint daily rounds and informal direct exchanges of instructions and updates. Hepatologists were mainly responsible for coordinating admissions, managing issues related to liver dysfunction, communicating with transplant surgeons if necessary, and arranging postdischarge care. Hospitalists were responsible for admitting patients, managing routine (eg, ordering daily labs) and urgent issues (eg, responding to critical lab values) during hospitalizations, coordinating with ancillary and consultative staff, and discharging patients. Occasional meetings between the hepatology and hospital medicine groups were used to clarify assignment of responsibilities. Floor nurses received in‐servicing at the commencement of the service. Additional details about the service are described elsewhere.8
DATA COLLECTION AND ANALYSIS
For the purpose of our analysis, we defined interactions between any member of the hospitalist and hepatologist teams as pertinent to comanagement. The hospitalist nonphysician provider (NPP) and hepatologistfellow relationships are governed by the more traditional hierarchical dynamics based on supervision and authority according to laws and regulations. At the beginning of the study period, each participant completed nine items of a Baseline Survey that addressed respondents' expectations and preferences for the management of an ideally comanaged service. Responses were solicited using a 4‐point Likert‐type scale and were dichotomized such that agree and somewhat agree were grouped, while disagree and somewhat disagree were grouped for data analysis. Items were generated to address the salient issues of comanagement after reviewing the pertinent literature.
Subsequently, participants were asked to complete Repeated Surveys immediately before each change in membership of the comanaged team between April and October 2008. The surveys were hand delivered by one of the authors (K.H.) on the last day of each team's rotation and were often completed immediately. The seven items of the Repeated Survey reprised items from the Baseline Survey that were rephrased to allow respondents to report their direct experiences on specific teams. Because all providers rotated on the service more than once during the study period, the average value for each Likert‐type response across multiple surveys completed by a single provider was calculated before being dichotomized at the midpoint (<2.5, agree; 2.5, disagree). We reported proportions of respondents in agreement with survey item statements.
Comparison statistics across providers were generated using the chi‐square test. Differences in proportions between related items of the Baseline and Repeated Surveys were compared using the two‐sample test of proportions. All analyses were conducted using a statistics application (STATA 10.0, College Station, TX) with alpha equal to, or less than, 0.05 considered significant. The Institutional Review Board of the University of Chicago approved this project.
RESULTS
All 43 providers completed the Baseline Survey. During the study period, 32 of these participants rotated on the service and completed 177 of the 233 Repeated Surveys (79%) administered. The responses describe team interactions on the 47 unique combinations of providers comprising the comanaged teams. Details of the response rates are shown in Table 1.
| Baseline Survey, Completed/ Administered (%) | Repeated Surveys, Completed/ Administered (%) | Respondents Completing Repeated Surveys, n | Repeated Surveys Completed per Respondent, Median (IQR) | |
|---|---|---|---|---|
| ||||
| Hospitalists | 18/18 (100) | 36/43 (84) | 15 | 2 (2, 3) |
| NPPs | 5/5 (100) | 92/97 (95) | 5 | 20 (18, 20) |
| Hepatologists | 6/6 (100) | 26/42 (62) | 6 | 7 (3.75, 8) |
| Fellows | 12/12 (100) | 23/42 (55) | 6 | 7 (5.5, 8.5) |
| Total | 43/43 (100) | 177/223 (79) | 32 | 4.5 (2, 8.25) |
As shown in Table 2A, items 13, more members of the hospitalist team preferred to be informed about every management decision compared to members of the hepatologist team. Conversely, more of members of the hepatologist team than the hospitalist team preferred their comanaging partners to participate in every decision. A statistically similar proportion of respondents in each of the professional roles indicated desire for greater influence in directing management decisions (Table 2B, item 1).
| A. Baseline Survey | Hospitalists, % (n = 18) | NPPs, % (n = 5) | Hepatologists, % (n = 6) | GI Fellows, % (n = 12) | P‐value |
|---|---|---|---|---|---|
| |||||
| 1. I prefer to be informed about every decision. | 83 | 100 | 17 | 42 | <0.01 |
| 2. I prefer to participate in every decision. | 67 | 100 | 33 | 50 | 0.11 |
| 3. I prefer that my comanager participate in every decision. | 22 | 20 | 50 | 75 | 0.02 |
| 4. I prefer to have the final say in every decision. | 50 | 80 | 50 | 33 | 0.38 |
| 5. There should be one physician leader to direct the overall management of the patients' hospital course. | 89* | 100 | 67 | 83 | 0.43 |
| 6. Physician consensus should always be sought in every clinical decision. | 22 | 40 | 50 | 67 | 0.11 |
| 7. I have a clear understanding of my role on the comanagement service. | 61 | 80 | 83 | 75 | 0.66 |
| 8. I have as much a sense of ownership of patients on the comanaged service as on a non‐comanaged service. | 61 | 60 | 83 | 50 | 0.60 |
| 9. Comanagement tends to improve patient care. | 94 | 100* | 83 | 100* | 0.47 |
| B. Repeated Surveys | Hospitalists, % (n = 15) | NPPs, % (n = 5) | Hepatologists, % (n = 6) | GI Fellows, % (n = 6) | P‐value |
| 1. I would have liked greater influence in directing the overall management. | 40 | 60 | 0 | 17 | 0.12 |
| 2. I was responsible for work in clinical areas I was not comfortable managing. | 0 | 0 | 0 | 0 | NA |
| 3. There was one physician leader to direct the overall management of the patients' hospital course. | 60* | 80 | 67 | 83 | 0.70 |
| 4. Physician consensus was always sought in every clinical decision. | 40 | 40 | 50 | 67 | 0.72 |
| 5. I (have/had) a clear understanding of my role on the comanagement service. | 73 | 80 | 100 | 83 | 0.57 |
| 6. I had as much a sense of ownership of patients on the comanaged service as on a non‐comanaged service. | 53 | 80 | 100 | 67 | 0.20 |
| 7. Patients on my service received better care than they would have without comanagement. | 93 | 40* | 67 | 50* | 0.06 |
For the majority of surveyed areas, there was concordance between expectations and experiences of providers on comanagement. Most providers, regardless of professional role, agreed that there should be a single physician leader to direct the overall management (Table 2A, item 5). The majority perceived that a single physician directed the overall management of the patients' hospital course, although fewer hospitalists did so compared with baseline expectations (Table 2B, item 3). Many respondents felt at baseline that physician consensus should govern every management decision, and a similar proportion actually experienced consensus‐seeking on service.
We found that the proportion of providers reporting an understanding of their role increased slightly, though not significantly, from before (Table 2A, item 7) to after rotating on the comanaged service (Table 2B, item 5). Although not statistically significant, there was a trend towards hospitalists and gastrointestinal (GI) fellows reporting a lack of patient ownership, both before and after serving on the comanaged service. Finally, nearly all respondents reported that comanagement should improve care quality, although only the attending hospitalist and hepatologist felt that their experience on the comanaged service actually improved patient care (Table 2B, item 7).
DISCUSSION
In this survey of providers participating on a comanaged medical service, most reported understanding their role in the collaborative arrangement and had an initial perception that comanagement should improve patient care quality. We found that hospitalists preferred and were expected to participate in care globally, while hepatologists themselves preferred and were expected not to focus on every management decision. The prevalence of desire for ultimate authority across the professional roles suggests tensions that exist in this care model around how decisions are made. The majority of providers preferred and experienced a single physician leader under comanagement, but many also experienced consensus‐seeking for every management decision.
From these findings, we conclude that decision‐making processes are not uniform under comanagement and that some role ambiguity is present, but there appears to be a pattern of natural roles. This pattern can be defined by focus (general for hospitalists vs specialty‐specific for hepatologists), rather than by responsibilities for managing particular medical problems. The preference among both generalists and specialists for the broader involvement of hospitalist comanagers suggests an implicit recognition of the need for integrated management to overcome the silo‐effect within the comanagement structure.9 Although details about how such integration was achieved are not available in our data, we found that comanagement may be distinct from traditional consultative practice in that the consultants (hospitalists in this case) manage not only general medical problems, such as diabetes or hypertension, but hospitalizations more generally. From a mission‐based standpoint, comanagement may be seen as a collaborative management of complex patients by two or more clinical experts with distinct knowledge, skills, or focus enacted for the purpose of improving care quality.
The focus of comanagement on improving quality is in line with the founding charge of the hospital medicine specialty to raise hospital care quality.10 In fact, the distinction between comanagement and consultation may be meaningful only if comanagers can work with specialists to implement evidence‐based practice, process improvement, and address quality and cost concerns. But as seen in NPPs and fellows' skepticism of improved quality under comanagement, there is still clearly work to be done to validate this model through measurable improvement in patients' experiences and outcomes. Proving the advantages of comanagement as a platform for practice improvement remains future work.11
Collaborative arrangements create natural tensions related to team function.5 This is seen in the similar proportion of hospitalists and hepatologists indicating desire for final decision‐making authority. Although comanagement evokes assumptions about egalitarian provider interactions involving shared decision‐making and responsibility, it seems to function empirically under hierarchical as well as consensus‐seeking forms of decision‐making. Providers at the top of hierarchical teams typically experience their work as interdependent and collaborative, and report more positive interactions with other care providers.12 Based on the fact that no hepatologists wanted more influence over decision‐making, we assume that hepatologists were the physician leaders for most of the studied comanaged teams. Under situations characterized by high levels of complexity and interdependence, a team governed by a single leader may often be more effective than one governed by shared authority.8 However, even under hierarchical models, a more participatory than supervisory leadership can help avoid alienating partners through a pattern of we decide, you carry it out that is often associated with ineffective leadership styles.1314 In fact, this alienating effect on providers in subordinate roles (ie, NPPs and fellows) may have contributed to the negative perception of the team's function on improving patient care.
This study is limited in the following ways. We did not have 100% participation in the Repeated Surveys. Attitudes and experiences of participants in a single comanagement practice are not representative of all comanaging providers. However, the goal of this studyto collect unique survey data from providers themselves to inform an evolving definition of comanagementis modest enough in scope to not require a generalizable sample. Because this study unearthed differences in expectations and experiences within a single site, they may serve as a lower bound for the extent of differences across and within multiple sites. In addition, comanagement enacted for complex medical patients is not as common as the comanagement of surgical patients. Moreover, comanagement models in academic hospitals may have structural features and priorities not found in community settings. Whether or not these disparate models share enough in common to be categorized under a single rubric is a valid question.
Although the teamwork structure and provider roles within comanagement vary, the practice arrangement's preoccupation with quality can be seen as its defining feature. Limited evidence, to date,1, 1519 and the rapid proliferation of the model, suggest that quality and efficiency advantages can be obtained from an effective implementation of comanagement. As in any team‐based care model, a common understanding of roles and expectations are essential to enhancing teamwork. Our interpretation of the mission of comanagement may further enhance teamwork through an explicit articulation of shared goals.
- ,,, et al.Medical and surgical comanagement after elective hip and knee arthroplasty: A randomized, controlled trial.Ann Intern Med.2004;141(1):28–38.
- .Just because you can, doesn't mean that you should: A call for the rational application of hospitalist comanagement.J Hosp Med.2008;3(5):398–402.
- ,.Surgical comanagement: A natural evolution of hospitalist practice.J Hosp Med.2008;3(5):394–397.
- ,,,,.Comanagement of hospitalized surgical patients by medicine physicians in the United States.Arch Intern Med.2010;170(4):363–368.
- .Structure and meaning in multidisciplinary teamwork.Sociol Health Illn.1998;20(6):848–873.
- ,,,,.Human factors and cardiac surgery: A multicenter study.J Thorac Cardiov Surg.2000;119(4):661–670.
- ,,.The effects of a collaborative model of primary care on the mortality and hospital use of community‐dwelling older adults.J Gerontol A‐Biol.2001;56(2):M106–M112.
- ,,,,,.Effects of provider characteristics on care coordination under comanagement.J Hosp Med.2010;5:508–513.
- ,,.Crossing the Quality Chasm: A New Health System for the Twenty‐First Century.Washington, DC:Institute of Medicine;2001.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335(7):514–517.
- .Internal medicine comanagement of surgical patients: Can we afford to do this?Arch Intern Med.2010;170(22):1965–1966.
- ,,, et al.Operating room teamwork among physicians and nurses: Teamwork in the eye of the beholder.J Am Coll Surg.2006;202(5):746–752.
- .“We decide, you carry it out”: A social network analysis of multidisciplinary longterm care teams.Soc Sci Med.1997;45(9):1411–1421.
- ,,.Patterns of aggressive behavior in experimentally created social climates.J Soc Psychol.1939;10:271–301.
- ,,, et al.Comanagement of surgical patients between neurosurgeons and hospitalists.Arch Intern Med.2010;170(22):2004–2010.
- ,,,,,.Outcomes for older patients with hip fractures: The impact of orthopedic and geriatric medicine cocare.J Orthop Trauma.2006;20(3):172–180.
- ,,, et al.Effects of a hospitalist model on elderly patients with hip fracture.Arch Intern Med.2005;165(7):796–801.
- ,,,.Hip fractures in geriatric patients. Results of an interdisciplinary hospital care program.Clin Orthop Relat Res.1992(274):213–225.
- ,,,.Impact of a comanaged Geriatric Fracture Center on short‐term hip fracture outcomes.Arch Intern Med.2009;169(18):1712–1717.
Comanagement is common in hospital medicine practice. And yet, there is no consensus about how comanagement is different from traditional consultative practice. At its core, hospitalist comanagement is a practice arrangement wherein hospitalists and other specialists manage complex patients collaboratively. Beyond this, Huddleston et al. distinguish comanagement from traditional consultations in the comanaging hospitalists' prerogative to provide direct medical care in addition to consultative advice.1 Siegal focuses on the shared responsibility and authority among partnering providers in the comanagement model.2 Whinney and Michota see comanagement as patient care referral at the onset of a care episode, in contrast to consultations that are activated to address emergent problems.3 In a recent study that found the growing adoption of medical comanagement in Medicare beneficiaries (as much as 40% of surgical hospitalizations in 2006), comanagement was defined as an intensive form of consultation involving a claim for evaluation and management services on greater than 70% of inpatient days.4
In addition to the intensity, frequency, timing, responsibility, and authority of care, comanagement may be described by participating physicians' roles. With recent attention on multidisciplinary teams and an increasing focus on collaborative care, many of the hierarchical relations among healthcare providers are breaking down.5 Several studies of multidisciplinary teams suggest that more egalitarian, rather than hierarchical, problem‐solving and decision‐making among team members are beneficial to patients.67 However, neither the intended nor natural team structure under comanagement is known. We sought to shed some light on provider interactions by characterizing the expectations and experiences of providers of a comanaged service. The findings yielded an opportunity to generate an evolving, but conceptually supported definition of comanagement.
SETTING
We conducted a survey study of providers participating in a comanaged inpatient hepatology service at the University of Chicago Medical Center, a 572‐bed urban teaching hospital. The service was created in 2006, partly to address staffing problems related to housestaff work hour restrictions and partly to improve the care of candidates and recipients of liver transplantation. Nonsurgical floor patients with liver diseases were managed on the service by two collaborating teams of providers. The hepatology team consisted of an attending physician and a fellow, while the hospitalist team consisted of a hospitalist and one or two nonphysician providers (physician assistant or nurse practitioner). The practice model is characterized as comanagement because of the highly interdependent nature of the team's daily tasks and the norms of intensive communication, through formal joint daily rounds and informal direct exchanges of instructions and updates. Hepatologists were mainly responsible for coordinating admissions, managing issues related to liver dysfunction, communicating with transplant surgeons if necessary, and arranging postdischarge care. Hospitalists were responsible for admitting patients, managing routine (eg, ordering daily labs) and urgent issues (eg, responding to critical lab values) during hospitalizations, coordinating with ancillary and consultative staff, and discharging patients. Occasional meetings between the hepatology and hospital medicine groups were used to clarify assignment of responsibilities. Floor nurses received in‐servicing at the commencement of the service. Additional details about the service are described elsewhere.8
DATA COLLECTION AND ANALYSIS
For the purpose of our analysis, we defined interactions between any member of the hospitalist and hepatologist teams as pertinent to comanagement. The hospitalist nonphysician provider (NPP) and hepatologistfellow relationships are governed by the more traditional hierarchical dynamics based on supervision and authority according to laws and regulations. At the beginning of the study period, each participant completed nine items of a Baseline Survey that addressed respondents' expectations and preferences for the management of an ideally comanaged service. Responses were solicited using a 4‐point Likert‐type scale and were dichotomized such that agree and somewhat agree were grouped, while disagree and somewhat disagree were grouped for data analysis. Items were generated to address the salient issues of comanagement after reviewing the pertinent literature.
Subsequently, participants were asked to complete Repeated Surveys immediately before each change in membership of the comanaged team between April and October 2008. The surveys were hand delivered by one of the authors (K.H.) on the last day of each team's rotation and were often completed immediately. The seven items of the Repeated Survey reprised items from the Baseline Survey that were rephrased to allow respondents to report their direct experiences on specific teams. Because all providers rotated on the service more than once during the study period, the average value for each Likert‐type response across multiple surveys completed by a single provider was calculated before being dichotomized at the midpoint (<2.5, agree; 2.5, disagree). We reported proportions of respondents in agreement with survey item statements.
Comparison statistics across providers were generated using the chi‐square test. Differences in proportions between related items of the Baseline and Repeated Surveys were compared using the two‐sample test of proportions. All analyses were conducted using a statistics application (STATA 10.0, College Station, TX) with alpha equal to, or less than, 0.05 considered significant. The Institutional Review Board of the University of Chicago approved this project.
RESULTS
All 43 providers completed the Baseline Survey. During the study period, 32 of these participants rotated on the service and completed 177 of the 233 Repeated Surveys (79%) administered. The responses describe team interactions on the 47 unique combinations of providers comprising the comanaged teams. Details of the response rates are shown in Table 1.
| Baseline Survey, Completed/ Administered (%) | Repeated Surveys, Completed/ Administered (%) | Respondents Completing Repeated Surveys, n | Repeated Surveys Completed per Respondent, Median (IQR) | |
|---|---|---|---|---|
| ||||
| Hospitalists | 18/18 (100) | 36/43 (84) | 15 | 2 (2, 3) |
| NPPs | 5/5 (100) | 92/97 (95) | 5 | 20 (18, 20) |
| Hepatologists | 6/6 (100) | 26/42 (62) | 6 | 7 (3.75, 8) |
| Fellows | 12/12 (100) | 23/42 (55) | 6 | 7 (5.5, 8.5) |
| Total | 43/43 (100) | 177/223 (79) | 32 | 4.5 (2, 8.25) |
As shown in Table 2A, items 13, more members of the hospitalist team preferred to be informed about every management decision compared to members of the hepatologist team. Conversely, more of members of the hepatologist team than the hospitalist team preferred their comanaging partners to participate in every decision. A statistically similar proportion of respondents in each of the professional roles indicated desire for greater influence in directing management decisions (Table 2B, item 1).
| A. Baseline Survey | Hospitalists, % (n = 18) | NPPs, % (n = 5) | Hepatologists, % (n = 6) | GI Fellows, % (n = 12) | P‐value |
|---|---|---|---|---|---|
| |||||
| 1. I prefer to be informed about every decision. | 83 | 100 | 17 | 42 | <0.01 |
| 2. I prefer to participate in every decision. | 67 | 100 | 33 | 50 | 0.11 |
| 3. I prefer that my comanager participate in every decision. | 22 | 20 | 50 | 75 | 0.02 |
| 4. I prefer to have the final say in every decision. | 50 | 80 | 50 | 33 | 0.38 |
| 5. There should be one physician leader to direct the overall management of the patients' hospital course. | 89* | 100 | 67 | 83 | 0.43 |
| 6. Physician consensus should always be sought in every clinical decision. | 22 | 40 | 50 | 67 | 0.11 |
| 7. I have a clear understanding of my role on the comanagement service. | 61 | 80 | 83 | 75 | 0.66 |
| 8. I have as much a sense of ownership of patients on the comanaged service as on a non‐comanaged service. | 61 | 60 | 83 | 50 | 0.60 |
| 9. Comanagement tends to improve patient care. | 94 | 100* | 83 | 100* | 0.47 |
| B. Repeated Surveys | Hospitalists, % (n = 15) | NPPs, % (n = 5) | Hepatologists, % (n = 6) | GI Fellows, % (n = 6) | P‐value |
| 1. I would have liked greater influence in directing the overall management. | 40 | 60 | 0 | 17 | 0.12 |
| 2. I was responsible for work in clinical areas I was not comfortable managing. | 0 | 0 | 0 | 0 | NA |
| 3. There was one physician leader to direct the overall management of the patients' hospital course. | 60* | 80 | 67 | 83 | 0.70 |
| 4. Physician consensus was always sought in every clinical decision. | 40 | 40 | 50 | 67 | 0.72 |
| 5. I (have/had) a clear understanding of my role on the comanagement service. | 73 | 80 | 100 | 83 | 0.57 |
| 6. I had as much a sense of ownership of patients on the comanaged service as on a non‐comanaged service. | 53 | 80 | 100 | 67 | 0.20 |
| 7. Patients on my service received better care than they would have without comanagement. | 93 | 40* | 67 | 50* | 0.06 |
For the majority of surveyed areas, there was concordance between expectations and experiences of providers on comanagement. Most providers, regardless of professional role, agreed that there should be a single physician leader to direct the overall management (Table 2A, item 5). The majority perceived that a single physician directed the overall management of the patients' hospital course, although fewer hospitalists did so compared with baseline expectations (Table 2B, item 3). Many respondents felt at baseline that physician consensus should govern every management decision, and a similar proportion actually experienced consensus‐seeking on service.
We found that the proportion of providers reporting an understanding of their role increased slightly, though not significantly, from before (Table 2A, item 7) to after rotating on the comanaged service (Table 2B, item 5). Although not statistically significant, there was a trend towards hospitalists and gastrointestinal (GI) fellows reporting a lack of patient ownership, both before and after serving on the comanaged service. Finally, nearly all respondents reported that comanagement should improve care quality, although only the attending hospitalist and hepatologist felt that their experience on the comanaged service actually improved patient care (Table 2B, item 7).
DISCUSSION
In this survey of providers participating on a comanaged medical service, most reported understanding their role in the collaborative arrangement and had an initial perception that comanagement should improve patient care quality. We found that hospitalists preferred and were expected to participate in care globally, while hepatologists themselves preferred and were expected not to focus on every management decision. The prevalence of desire for ultimate authority across the professional roles suggests tensions that exist in this care model around how decisions are made. The majority of providers preferred and experienced a single physician leader under comanagement, but many also experienced consensus‐seeking for every management decision.
From these findings, we conclude that decision‐making processes are not uniform under comanagement and that some role ambiguity is present, but there appears to be a pattern of natural roles. This pattern can be defined by focus (general for hospitalists vs specialty‐specific for hepatologists), rather than by responsibilities for managing particular medical problems. The preference among both generalists and specialists for the broader involvement of hospitalist comanagers suggests an implicit recognition of the need for integrated management to overcome the silo‐effect within the comanagement structure.9 Although details about how such integration was achieved are not available in our data, we found that comanagement may be distinct from traditional consultative practice in that the consultants (hospitalists in this case) manage not only general medical problems, such as diabetes or hypertension, but hospitalizations more generally. From a mission‐based standpoint, comanagement may be seen as a collaborative management of complex patients by two or more clinical experts with distinct knowledge, skills, or focus enacted for the purpose of improving care quality.
The focus of comanagement on improving quality is in line with the founding charge of the hospital medicine specialty to raise hospital care quality.10 In fact, the distinction between comanagement and consultation may be meaningful only if comanagers can work with specialists to implement evidence‐based practice, process improvement, and address quality and cost concerns. But as seen in NPPs and fellows' skepticism of improved quality under comanagement, there is still clearly work to be done to validate this model through measurable improvement in patients' experiences and outcomes. Proving the advantages of comanagement as a platform for practice improvement remains future work.11
Collaborative arrangements create natural tensions related to team function.5 This is seen in the similar proportion of hospitalists and hepatologists indicating desire for final decision‐making authority. Although comanagement evokes assumptions about egalitarian provider interactions involving shared decision‐making and responsibility, it seems to function empirically under hierarchical as well as consensus‐seeking forms of decision‐making. Providers at the top of hierarchical teams typically experience their work as interdependent and collaborative, and report more positive interactions with other care providers.12 Based on the fact that no hepatologists wanted more influence over decision‐making, we assume that hepatologists were the physician leaders for most of the studied comanaged teams. Under situations characterized by high levels of complexity and interdependence, a team governed by a single leader may often be more effective than one governed by shared authority.8 However, even under hierarchical models, a more participatory than supervisory leadership can help avoid alienating partners through a pattern of we decide, you carry it out that is often associated with ineffective leadership styles.1314 In fact, this alienating effect on providers in subordinate roles (ie, NPPs and fellows) may have contributed to the negative perception of the team's function on improving patient care.
This study is limited in the following ways. We did not have 100% participation in the Repeated Surveys. Attitudes and experiences of participants in a single comanagement practice are not representative of all comanaging providers. However, the goal of this studyto collect unique survey data from providers themselves to inform an evolving definition of comanagementis modest enough in scope to not require a generalizable sample. Because this study unearthed differences in expectations and experiences within a single site, they may serve as a lower bound for the extent of differences across and within multiple sites. In addition, comanagement enacted for complex medical patients is not as common as the comanagement of surgical patients. Moreover, comanagement models in academic hospitals may have structural features and priorities not found in community settings. Whether or not these disparate models share enough in common to be categorized under a single rubric is a valid question.
Although the teamwork structure and provider roles within comanagement vary, the practice arrangement's preoccupation with quality can be seen as its defining feature. Limited evidence, to date,1, 1519 and the rapid proliferation of the model, suggest that quality and efficiency advantages can be obtained from an effective implementation of comanagement. As in any team‐based care model, a common understanding of roles and expectations are essential to enhancing teamwork. Our interpretation of the mission of comanagement may further enhance teamwork through an explicit articulation of shared goals.
Comanagement is common in hospital medicine practice. And yet, there is no consensus about how comanagement is different from traditional consultative practice. At its core, hospitalist comanagement is a practice arrangement wherein hospitalists and other specialists manage complex patients collaboratively. Beyond this, Huddleston et al. distinguish comanagement from traditional consultations in the comanaging hospitalists' prerogative to provide direct medical care in addition to consultative advice.1 Siegal focuses on the shared responsibility and authority among partnering providers in the comanagement model.2 Whinney and Michota see comanagement as patient care referral at the onset of a care episode, in contrast to consultations that are activated to address emergent problems.3 In a recent study that found the growing adoption of medical comanagement in Medicare beneficiaries (as much as 40% of surgical hospitalizations in 2006), comanagement was defined as an intensive form of consultation involving a claim for evaluation and management services on greater than 70% of inpatient days.4
In addition to the intensity, frequency, timing, responsibility, and authority of care, comanagement may be described by participating physicians' roles. With recent attention on multidisciplinary teams and an increasing focus on collaborative care, many of the hierarchical relations among healthcare providers are breaking down.5 Several studies of multidisciplinary teams suggest that more egalitarian, rather than hierarchical, problem‐solving and decision‐making among team members are beneficial to patients.67 However, neither the intended nor natural team structure under comanagement is known. We sought to shed some light on provider interactions by characterizing the expectations and experiences of providers of a comanaged service. The findings yielded an opportunity to generate an evolving, but conceptually supported definition of comanagement.
SETTING
We conducted a survey study of providers participating in a comanaged inpatient hepatology service at the University of Chicago Medical Center, a 572‐bed urban teaching hospital. The service was created in 2006, partly to address staffing problems related to housestaff work hour restrictions and partly to improve the care of candidates and recipients of liver transplantation. Nonsurgical floor patients with liver diseases were managed on the service by two collaborating teams of providers. The hepatology team consisted of an attending physician and a fellow, while the hospitalist team consisted of a hospitalist and one or two nonphysician providers (physician assistant or nurse practitioner). The practice model is characterized as comanagement because of the highly interdependent nature of the team's daily tasks and the norms of intensive communication, through formal joint daily rounds and informal direct exchanges of instructions and updates. Hepatologists were mainly responsible for coordinating admissions, managing issues related to liver dysfunction, communicating with transplant surgeons if necessary, and arranging postdischarge care. Hospitalists were responsible for admitting patients, managing routine (eg, ordering daily labs) and urgent issues (eg, responding to critical lab values) during hospitalizations, coordinating with ancillary and consultative staff, and discharging patients. Occasional meetings between the hepatology and hospital medicine groups were used to clarify assignment of responsibilities. Floor nurses received in‐servicing at the commencement of the service. Additional details about the service are described elsewhere.8
DATA COLLECTION AND ANALYSIS
For the purpose of our analysis, we defined interactions between any member of the hospitalist and hepatologist teams as pertinent to comanagement. The hospitalist nonphysician provider (NPP) and hepatologistfellow relationships are governed by the more traditional hierarchical dynamics based on supervision and authority according to laws and regulations. At the beginning of the study period, each participant completed nine items of a Baseline Survey that addressed respondents' expectations and preferences for the management of an ideally comanaged service. Responses were solicited using a 4‐point Likert‐type scale and were dichotomized such that agree and somewhat agree were grouped, while disagree and somewhat disagree were grouped for data analysis. Items were generated to address the salient issues of comanagement after reviewing the pertinent literature.
Subsequently, participants were asked to complete Repeated Surveys immediately before each change in membership of the comanaged team between April and October 2008. The surveys were hand delivered by one of the authors (K.H.) on the last day of each team's rotation and were often completed immediately. The seven items of the Repeated Survey reprised items from the Baseline Survey that were rephrased to allow respondents to report their direct experiences on specific teams. Because all providers rotated on the service more than once during the study period, the average value for each Likert‐type response across multiple surveys completed by a single provider was calculated before being dichotomized at the midpoint (<2.5, agree; 2.5, disagree). We reported proportions of respondents in agreement with survey item statements.
Comparison statistics across providers were generated using the chi‐square test. Differences in proportions between related items of the Baseline and Repeated Surveys were compared using the two‐sample test of proportions. All analyses were conducted using a statistics application (STATA 10.0, College Station, TX) with alpha equal to, or less than, 0.05 considered significant. The Institutional Review Board of the University of Chicago approved this project.
RESULTS
All 43 providers completed the Baseline Survey. During the study period, 32 of these participants rotated on the service and completed 177 of the 233 Repeated Surveys (79%) administered. The responses describe team interactions on the 47 unique combinations of providers comprising the comanaged teams. Details of the response rates are shown in Table 1.
| Baseline Survey, Completed/ Administered (%) | Repeated Surveys, Completed/ Administered (%) | Respondents Completing Repeated Surveys, n | Repeated Surveys Completed per Respondent, Median (IQR) | |
|---|---|---|---|---|
| ||||
| Hospitalists | 18/18 (100) | 36/43 (84) | 15 | 2 (2, 3) |
| NPPs | 5/5 (100) | 92/97 (95) | 5 | 20 (18, 20) |
| Hepatologists | 6/6 (100) | 26/42 (62) | 6 | 7 (3.75, 8) |
| Fellows | 12/12 (100) | 23/42 (55) | 6 | 7 (5.5, 8.5) |
| Total | 43/43 (100) | 177/223 (79) | 32 | 4.5 (2, 8.25) |
As shown in Table 2A, items 13, more members of the hospitalist team preferred to be informed about every management decision compared to members of the hepatologist team. Conversely, more of members of the hepatologist team than the hospitalist team preferred their comanaging partners to participate in every decision. A statistically similar proportion of respondents in each of the professional roles indicated desire for greater influence in directing management decisions (Table 2B, item 1).
| A. Baseline Survey | Hospitalists, % (n = 18) | NPPs, % (n = 5) | Hepatologists, % (n = 6) | GI Fellows, % (n = 12) | P‐value |
|---|---|---|---|---|---|
| |||||
| 1. I prefer to be informed about every decision. | 83 | 100 | 17 | 42 | <0.01 |
| 2. I prefer to participate in every decision. | 67 | 100 | 33 | 50 | 0.11 |
| 3. I prefer that my comanager participate in every decision. | 22 | 20 | 50 | 75 | 0.02 |
| 4. I prefer to have the final say in every decision. | 50 | 80 | 50 | 33 | 0.38 |
| 5. There should be one physician leader to direct the overall management of the patients' hospital course. | 89* | 100 | 67 | 83 | 0.43 |
| 6. Physician consensus should always be sought in every clinical decision. | 22 | 40 | 50 | 67 | 0.11 |
| 7. I have a clear understanding of my role on the comanagement service. | 61 | 80 | 83 | 75 | 0.66 |
| 8. I have as much a sense of ownership of patients on the comanaged service as on a non‐comanaged service. | 61 | 60 | 83 | 50 | 0.60 |
| 9. Comanagement tends to improve patient care. | 94 | 100* | 83 | 100* | 0.47 |
| B. Repeated Surveys | Hospitalists, % (n = 15) | NPPs, % (n = 5) | Hepatologists, % (n = 6) | GI Fellows, % (n = 6) | P‐value |
| 1. I would have liked greater influence in directing the overall management. | 40 | 60 | 0 | 17 | 0.12 |
| 2. I was responsible for work in clinical areas I was not comfortable managing. | 0 | 0 | 0 | 0 | NA |
| 3. There was one physician leader to direct the overall management of the patients' hospital course. | 60* | 80 | 67 | 83 | 0.70 |
| 4. Physician consensus was always sought in every clinical decision. | 40 | 40 | 50 | 67 | 0.72 |
| 5. I (have/had) a clear understanding of my role on the comanagement service. | 73 | 80 | 100 | 83 | 0.57 |
| 6. I had as much a sense of ownership of patients on the comanaged service as on a non‐comanaged service. | 53 | 80 | 100 | 67 | 0.20 |
| 7. Patients on my service received better care than they would have without comanagement. | 93 | 40* | 67 | 50* | 0.06 |
For the majority of surveyed areas, there was concordance between expectations and experiences of providers on comanagement. Most providers, regardless of professional role, agreed that there should be a single physician leader to direct the overall management (Table 2A, item 5). The majority perceived that a single physician directed the overall management of the patients' hospital course, although fewer hospitalists did so compared with baseline expectations (Table 2B, item 3). Many respondents felt at baseline that physician consensus should govern every management decision, and a similar proportion actually experienced consensus‐seeking on service.
We found that the proportion of providers reporting an understanding of their role increased slightly, though not significantly, from before (Table 2A, item 7) to after rotating on the comanaged service (Table 2B, item 5). Although not statistically significant, there was a trend towards hospitalists and gastrointestinal (GI) fellows reporting a lack of patient ownership, both before and after serving on the comanaged service. Finally, nearly all respondents reported that comanagement should improve care quality, although only the attending hospitalist and hepatologist felt that their experience on the comanaged service actually improved patient care (Table 2B, item 7).
DISCUSSION
In this survey of providers participating on a comanaged medical service, most reported understanding their role in the collaborative arrangement and had an initial perception that comanagement should improve patient care quality. We found that hospitalists preferred and were expected to participate in care globally, while hepatologists themselves preferred and were expected not to focus on every management decision. The prevalence of desire for ultimate authority across the professional roles suggests tensions that exist in this care model around how decisions are made. The majority of providers preferred and experienced a single physician leader under comanagement, but many also experienced consensus‐seeking for every management decision.
From these findings, we conclude that decision‐making processes are not uniform under comanagement and that some role ambiguity is present, but there appears to be a pattern of natural roles. This pattern can be defined by focus (general for hospitalists vs specialty‐specific for hepatologists), rather than by responsibilities for managing particular medical problems. The preference among both generalists and specialists for the broader involvement of hospitalist comanagers suggests an implicit recognition of the need for integrated management to overcome the silo‐effect within the comanagement structure.9 Although details about how such integration was achieved are not available in our data, we found that comanagement may be distinct from traditional consultative practice in that the consultants (hospitalists in this case) manage not only general medical problems, such as diabetes or hypertension, but hospitalizations more generally. From a mission‐based standpoint, comanagement may be seen as a collaborative management of complex patients by two or more clinical experts with distinct knowledge, skills, or focus enacted for the purpose of improving care quality.
The focus of comanagement on improving quality is in line with the founding charge of the hospital medicine specialty to raise hospital care quality.10 In fact, the distinction between comanagement and consultation may be meaningful only if comanagers can work with specialists to implement evidence‐based practice, process improvement, and address quality and cost concerns. But as seen in NPPs and fellows' skepticism of improved quality under comanagement, there is still clearly work to be done to validate this model through measurable improvement in patients' experiences and outcomes. Proving the advantages of comanagement as a platform for practice improvement remains future work.11
Collaborative arrangements create natural tensions related to team function.5 This is seen in the similar proportion of hospitalists and hepatologists indicating desire for final decision‐making authority. Although comanagement evokes assumptions about egalitarian provider interactions involving shared decision‐making and responsibility, it seems to function empirically under hierarchical as well as consensus‐seeking forms of decision‐making. Providers at the top of hierarchical teams typically experience their work as interdependent and collaborative, and report more positive interactions with other care providers.12 Based on the fact that no hepatologists wanted more influence over decision‐making, we assume that hepatologists were the physician leaders for most of the studied comanaged teams. Under situations characterized by high levels of complexity and interdependence, a team governed by a single leader may often be more effective than one governed by shared authority.8 However, even under hierarchical models, a more participatory than supervisory leadership can help avoid alienating partners through a pattern of we decide, you carry it out that is often associated with ineffective leadership styles.1314 In fact, this alienating effect on providers in subordinate roles (ie, NPPs and fellows) may have contributed to the negative perception of the team's function on improving patient care.
This study is limited in the following ways. We did not have 100% participation in the Repeated Surveys. Attitudes and experiences of participants in a single comanagement practice are not representative of all comanaging providers. However, the goal of this studyto collect unique survey data from providers themselves to inform an evolving definition of comanagementis modest enough in scope to not require a generalizable sample. Because this study unearthed differences in expectations and experiences within a single site, they may serve as a lower bound for the extent of differences across and within multiple sites. In addition, comanagement enacted for complex medical patients is not as common as the comanagement of surgical patients. Moreover, comanagement models in academic hospitals may have structural features and priorities not found in community settings. Whether or not these disparate models share enough in common to be categorized under a single rubric is a valid question.
Although the teamwork structure and provider roles within comanagement vary, the practice arrangement's preoccupation with quality can be seen as its defining feature. Limited evidence, to date,1, 1519 and the rapid proliferation of the model, suggest that quality and efficiency advantages can be obtained from an effective implementation of comanagement. As in any team‐based care model, a common understanding of roles and expectations are essential to enhancing teamwork. Our interpretation of the mission of comanagement may further enhance teamwork through an explicit articulation of shared goals.
- ,,, et al.Medical and surgical comanagement after elective hip and knee arthroplasty: A randomized, controlled trial.Ann Intern Med.2004;141(1):28–38.
- .Just because you can, doesn't mean that you should: A call for the rational application of hospitalist comanagement.J Hosp Med.2008;3(5):398–402.
- ,.Surgical comanagement: A natural evolution of hospitalist practice.J Hosp Med.2008;3(5):394–397.
- ,,,,.Comanagement of hospitalized surgical patients by medicine physicians in the United States.Arch Intern Med.2010;170(4):363–368.
- .Structure and meaning in multidisciplinary teamwork.Sociol Health Illn.1998;20(6):848–873.
- ,,,,.Human factors and cardiac surgery: A multicenter study.J Thorac Cardiov Surg.2000;119(4):661–670.
- ,,.The effects of a collaborative model of primary care on the mortality and hospital use of community‐dwelling older adults.J Gerontol A‐Biol.2001;56(2):M106–M112.
- ,,,,,.Effects of provider characteristics on care coordination under comanagement.J Hosp Med.2010;5:508–513.
- ,,.Crossing the Quality Chasm: A New Health System for the Twenty‐First Century.Washington, DC:Institute of Medicine;2001.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335(7):514–517.
- .Internal medicine comanagement of surgical patients: Can we afford to do this?Arch Intern Med.2010;170(22):1965–1966.
- ,,, et al.Operating room teamwork among physicians and nurses: Teamwork in the eye of the beholder.J Am Coll Surg.2006;202(5):746–752.
- .“We decide, you carry it out”: A social network analysis of multidisciplinary longterm care teams.Soc Sci Med.1997;45(9):1411–1421.
- ,,.Patterns of aggressive behavior in experimentally created social climates.J Soc Psychol.1939;10:271–301.
- ,,, et al.Comanagement of surgical patients between neurosurgeons and hospitalists.Arch Intern Med.2010;170(22):2004–2010.
- ,,,,,.Outcomes for older patients with hip fractures: The impact of orthopedic and geriatric medicine cocare.J Orthop Trauma.2006;20(3):172–180.
- ,,, et al.Effects of a hospitalist model on elderly patients with hip fracture.Arch Intern Med.2005;165(7):796–801.
- ,,,.Hip fractures in geriatric patients. Results of an interdisciplinary hospital care program.Clin Orthop Relat Res.1992(274):213–225.
- ,,,.Impact of a comanaged Geriatric Fracture Center on short‐term hip fracture outcomes.Arch Intern Med.2009;169(18):1712–1717.
- ,,, et al.Medical and surgical comanagement after elective hip and knee arthroplasty: A randomized, controlled trial.Ann Intern Med.2004;141(1):28–38.
- .Just because you can, doesn't mean that you should: A call for the rational application of hospitalist comanagement.J Hosp Med.2008;3(5):398–402.
- ,.Surgical comanagement: A natural evolution of hospitalist practice.J Hosp Med.2008;3(5):394–397.
- ,,,,.Comanagement of hospitalized surgical patients by medicine physicians in the United States.Arch Intern Med.2010;170(4):363–368.
- .Structure and meaning in multidisciplinary teamwork.Sociol Health Illn.1998;20(6):848–873.
- ,,,,.Human factors and cardiac surgery: A multicenter study.J Thorac Cardiov Surg.2000;119(4):661–670.
- ,,.The effects of a collaborative model of primary care on the mortality and hospital use of community‐dwelling older adults.J Gerontol A‐Biol.2001;56(2):M106–M112.
- ,,,,,.Effects of provider characteristics on care coordination under comanagement.J Hosp Med.2010;5:508–513.
- ,,.Crossing the Quality Chasm: A New Health System for the Twenty‐First Century.Washington, DC:Institute of Medicine;2001.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335(7):514–517.
- .Internal medicine comanagement of surgical patients: Can we afford to do this?Arch Intern Med.2010;170(22):1965–1966.
- ,,, et al.Operating room teamwork among physicians and nurses: Teamwork in the eye of the beholder.J Am Coll Surg.2006;202(5):746–752.
- .“We decide, you carry it out”: A social network analysis of multidisciplinary longterm care teams.Soc Sci Med.1997;45(9):1411–1421.
- ,,.Patterns of aggressive behavior in experimentally created social climates.J Soc Psychol.1939;10:271–301.
- ,,, et al.Comanagement of surgical patients between neurosurgeons and hospitalists.Arch Intern Med.2010;170(22):2004–2010.
- ,,,,,.Outcomes for older patients with hip fractures: The impact of orthopedic and geriatric medicine cocare.J Orthop Trauma.2006;20(3):172–180.
- ,,, et al.Effects of a hospitalist model on elderly patients with hip fracture.Arch Intern Med.2005;165(7):796–801.
- ,,,.Hip fractures in geriatric patients. Results of an interdisciplinary hospital care program.Clin Orthop Relat Res.1992(274):213–225.
- ,,,.Impact of a comanaged Geriatric Fracture Center on short‐term hip fracture outcomes.Arch Intern Med.2009;169(18):1712–1717.
Copyright © 2011 Society of Hospital Medicine
Care Coordination Under Comanagement
Technological advances drive medical providers to specialize through the need for proficiency around increasingly focused areas of expertise.1 But the benefits of specialization are attained only by balancing the advantages of increasing expertise and the costs of coordinating care that must be borne as specialization increases.2 Integrating experts into modern medical delivery systems requires attention to the coordinating mechanisms that govern team‐based care.3
Coordination, defined as the management of task interdependencies,4 is a central component and a useful measure of teamwork.5 Several studies demonstrate the patient‐level impact of coordination among providers.69 Gittell et al.8 demonstrated that orthopedic hospitals whose staff had better relational coordination (RC) measures had shorter lengths of stay and better post‐operative pain control for patients undergoing surgery. In medical intensive care units (ICUs), Wheelan et al.9 showed that staff members of units with lower mortality rates perceived their teams as functioning at higher stages of group development and perceived their team members as less dependent and more trusting.
Communication is the cornerstone of effective team coordination.10, 11 As such, practice model interventions that facilitate frequent communication of higher quality are associated with lower error rates10 and better teamwork.11 The use of hospitalists, for example, is shown to capitalize on this advantage by improving coordination through physician availability that facilitates communication and relational interactions among hospital‐based staff.12 While system‐level interventions such as this have received significant attention from experts in organizations, empirical studies that explore the contribution of team member characteristics to overall coordination are lacking.13
Inpatient comanagement services offer a unique model for studying teamwork. While the label is used to describe a variety of arrangements,1416 comanagement broadly describes a practice model wherein providers of various specialties deliver direct care to patients, in contrast to the traditional generalist‐consultant model in which specialists lend expertise.17 Many recent comanagement practices involve hospitalists in partnership with surgeons in the care of patients with concurrent medical and surgical needs,18 but similar arrangements between hospitalists and medical subspecialists are being adopted in some medical centers for the care of complex patients with conditions such as heart failure, cancer, stroke, and solid organ transplantations. Coordination among providers has not been studied in this context.
The goals of this study are: (1) to measure the input of individual providers to the overall coordination of care on a highly interdependent medical comanagement service, (2) to characterize high and low coordinators, and (3) to explore the relationship between coordination and patient outcomes. The main hypothesis is that the quality of team coordination is determined partly by the attributes of its members such that their individual contributions to the coordination of care affect the outcomes of vulnerable hospitalized patients.
Materials and Methods
Setting
The study was conducted at the University of Chicago Medical Center, Chicago, IL, an urban 572‐bed tertiary care hospital. The comanaged multidisciplinary inpatient service serves hospitalized patients with complex medical needs. This study focused on providers and patients from a subset of the comanaged multidisciplinary inpatient service that involved the collaboration of medical hepatologists with hospitalists. A hepatology team, composed of an attending hepatologist and a fellow, comanaged with 2 hospitalist teams, each composed of an attending hospitalist and 1 or 2 nonphysician providers (NPPs). Attending physicians rotated on the service in 1‐week to 3‐week rotations, while fellows rotated in 4‐week stretches. NPPs worked nonuniform 3‐day or 4‐day weeks excluding weekends and holidays. The hepatology team was responsible for arranging admissions, developing a care plan with a specialty focus, coordinating care with transplant surgeons when necessary, and managing post‐discharge care. The hospitalist teams were responsible for admitting patients, managing routine and emergent inpatient issues, coordinating care with ancillary and consultative staff, and discharging patients. Dedicated evening and night hospitalists, who were not part of the comanaging day‐time teams, provided after‐hours care. Outside of these areas, there was no instruction or education about how responsibilities should be shared among providers on the service.
Subjects and Study Design
Baseline Survey of Providers
All hospitalists, NPPs, hepatologists, and fellows scheduled to rotate on the comanaged multidisciplinary inpatient service signed a written consent to participate. In April 2008 a nonanonymous baseline 17‐item paper survey was administered.
Items of the Baseline Survey (supporting information Appendix A) were generated from a consideration of the most salient issues around the management structure of comanagement models from a comprehensive review the literature. Two items addressed the respondents' experience and intent to leave their role. Twelve items addressed their preferences about the provider management structure of an ideally comanaged inpatient service, specifically soliciting their preferences about a single physician leader, consensus seeking, and their preferred degree of information, participation, and decision making under the model. Included in this set of items was a single item assessment of the provider's sense of patient ownership on an ideally comanaged service. The final 3 items addressed the perceived assignment of responsibilities. Each of these items presented a clinical objective followed by up to 7 contingent tasks on whose completion the successful execution of the objective depended. Each respondent was asked to indicate one or more of the 4 provider types that should be responsible for completing each task.
Repeated Survey of Providers
From April to October 2008, providers who rotated on the comanaged liver service were surveyed repeatedly to give information about the actual management structure and coordination within teams, which consisted of combinations of randomly assigned providers. Physicians were surveyed on the day when any 1 of the 3 physician types ended his or her rotation. NPPs were surveyed every Wednesday except on the weeks when none of the physicians had changed since the previous survey. One investigator (KH) hand‐delivered the surveys, usually during the first minutes of the joint daily rounds and collected them immediately upon completion. Surveys that could not be completed immediately were collected on daily rounds on subsequent days within 1 week. The primary reason for nonresponse was lost surveys that were not immediately completed.
The 14‐item Repeated Survey (supporting information Appendix B) consisted of 2 parts. The first 7 items reprised items from the Baseline Survey that addressed management structures, but were rephrased to allow respondents to report their experiences on their immediate rotation. The second part of the Repeated Survey addressed RC, which is described below.
The study protocols, consents, and data collection mechanisms were approved by the institutional review board of the University of Chicago Medical Center. Collection of patient information was designed to comply with the Health Insurance Portability and Accountability Act of 1996.
Patients
Patients were admitted to 1 of the 2 hospitalist teams on the comanaged service on alternating days, which allowed patients to be assigned to providers pseudo‐randomly. Consent to use clinical data was obtained during their stay or by telephone after discharge. If patients were unable to provide consent due to cognitive impairment, consent was sought through designated proxies.19
Main Measurements
Relational Care Coordination
The survey instrument used to measure individual contributions to overall coordination was adapted from the Relational Coordination tool developed by Gittell.20 This instrument was chosen because it has already been validated in various clinical contexts8, 12, 21 and the theoretical assumptions about the independent relational and communication components of coordination are applicable to our context. RC is characterized by the 7 domains of frequent, timely, accurate, and problem‐solving communications; shared goals, shared knowledge, and mutual respect. Respondents rated, on a 5‐point scale (1 = negative, 5 = positive), team members of the other 3 provider types during each rotation on all of the 7 domains. The mean across the domains yielded the RC score. Although the instrument was originally developed to measure the coordination in groups of individuals, the RC for a single provider was calculated by taking the mean of all the RC directed at that individual across team members who worked with him or her during the study period. Because some providers worked more rotations than others, a nonuniform number of observations contributed to the calculation of individual RC (Table 1). For each provider type, individuals were ranked on their RC and categorized in tertiles representing high, middle, and low coordinators.
| Baseline Survey (%) | Repeated Surveys (%) | % Female | Years Experience Median (range) | # RC Evaluations of Each Provider Median (range) | RC Mean (range) | |
|---|---|---|---|---|---|---|
| ||||||
| Hospitalists | 15/15 (100) | 36/43 (84) | 42 | 1 (0‐10) | 6 (3‐21) | 4.71 (4.33‐4.94) |
| NPPs | 5/5 (100) | 92/97 (95) | 100 | 4 (2‐15) | 30 (23‐34) | 4.60 (4.48‐4.71) |
| Hepatologists | 6/6 (100) | 26/42 (62) | 33 | 7 (1‐25) | 16 (5‐51) | 4.37 (4.03‐4.59) |
| GI fellows | 6/6 (100) | 23/42 (55) | 48 | 1 (0‐1) | 19 (8‐37) | 4.28 (3.88‐4.53) |
| Total | 32/32 (100) | 177/223 (79) | 55 | 2 (0‐25) | 12.5 (3‐51) | 4.57 (3.88‐4.94) |
Statistical Analysis
The discriminating ability of the RC for individuals was assessed by comparing the highest and lowest RC of each provider type using the 2‐tailed t‐test. The difference in responses to items from the Baseline and Repeated Surveys by individual RC tertiles was assessed with the Chi‐squared test for categorical data and the 2‐tailed t‐test for comparing means. For each physician type, the frequency of the composite bad outcomes between the highest and lowest RC tertile categories were compared using a 2‐sample Wilcoxon rank‐sum (Mann‐Whitney) test for nonparametric data.
Results
All 32 providers (100%) completed the Baseline Survey and participated in the Repeated Surveys of which 177/224 (79%) were completed. The median number of surveys that contributed to the calculation of individual RC and the mean RC by provider type are summarized in Table 1.
Of the 119 patients managed on the service, the mean age (standard deviation [SD]) was 55 (14) years and 48% were women. Of the 201 hospitalizations, there were 13 floor‐to‐ICU transfers and 5 in‐hospital deaths, however, we excluded from the analysis 1 death of a patient who was admitted under inpatient hospice status.
RC Measures
Individual provider RC ranges were 4.33 to 4.94 (p = 0.05) for hospitalists; 4.48 to 4.71 (p = 0.10) for NP/PAs; 4.03 to 4.59 (p < 0.01) for hepatologists; and 3.88 to 4.52 (p = 0.02) for fellows. The high, middle, and low coordinator categories for each provider type were shown to be durable through time by demonstrating that the coordination ranking of individuals was essentially preserved even when using partial data from each half of the study period. Thus, RC appears to reflect a stable attribute of the provider as opposed to specific circumstances of the rotation. The categories were shown to be durable to the influences of bad outcomes (inpatient deaths and ICU transfers) by demonstrating that the placement of individuals into 1 of the 3 coordination categories were preserved even when data from rotations involving a bad outcome were removed. Nonetheless, in order to address the possibility of bad outcomes negatively affecting perception of coordination, all analysis involving RC used the values that excluded data from these rotations.
Characteristics of Good and Poor Coordinators
Patient Ownership
The single‐item measure of patient ownership in the Baseline Survey reads: I have as much a sense of ownership of my patients on the comanaged service as on a non‐comanaged service. The majority of providers of every type in the high and middle coordinator categories agreed, while providers in the low coordinator category generally disagreed with the statement. The aggregated responses of all the provider types are shown in Table 2.
| Agree | Somewhat Agree | Somewhat Disagree | Disagree | |
|---|---|---|---|---|
| High | 4 | 6 | 0 | 1 |
| Middle | 5 | 4 | 0 | 2 |
| Low | 2 | 0 | 4 | 4 |
| p < 0.01 |
Leadership
Hepatologists are the potential leader of the comanaged team because of their content expertise in liver diseases. Their responses to the 3 items in the Baseline Survey that addressed perceived assignment of responsibilities are shown in Table 3. The high compared to the low coordinator hepatologists delegated the responsibility of completing necessary tasks to more providers, overall, such that an average of 3 providers were redundantly held responsible for the completion of each task by the high coordinators while only 1 provider was held responsible by the low coordinators. Furthermore, the high coordinators delegated the responsibility of completing more tasks to themselves compared to the low coordinators.
| Hepatologists | Mean # of Tasks Delegated Overall, n (SD) | Mean # of Providers Delegated to Each Task, n (SD) | Mean # of Tasks Delegated to Self, n (SD) |
|---|---|---|---|
| |||
| High (n = 2) | 56 (0.0) | 2.9 (0.0) | 11.5 (2.1) |
| Middle (n = 2) | 35 (2.8) | 1.8 (0.2) | 9.5 (3.5) |
| Low (n = 2) | 19 (1.4) | 1.0 (0.1) | 4.5 (2.1) |
| p value(high vs. low) | <0.01 | <0.01 | 0.08 |
According to responses to the management structure items of the Repeated Surveys, more providers of every type indicated that a single physician leader directed the overall management of every patient when a high or middle coordinator hospitalist was on service as opposed to a service with a low coordinator hospitalist (high 76% vs. middle 73% vs. low 58%, P = 0.06). Furthermore, a low coordinator hospitalist on service was more likely to indicate a desire for greater influence in directing the management of patients (desire influence 93% vs. not 7%, P < 0.01). This pattern was also seen with low coordinator NPPs, who more often indicated a desire for greater influence in directing patient management (desire influence 100% vs. not 0%, P < 0.01).
Experience
Age, years in practice, years at the institution, and time spent on the comanaged service were not associated with RC in our small sample of providers.
Outcomes by Provider Coordination
The unit of analysis in this section is the team‐patient encounter, which is the consecutive days during which a unique assortment of physicians managed a patient's hospitalization. NPPs could not be associated with any single team due to their nonuniform work patterns. The 201 hospitalizations in this study were composed of 351 team‐patient encounters. Table 4 displays the unadjusted frequency of inpatient deaths and ICU transfers that occurred during these encounters by RC tertiles. In each of the 3 physician types, composite bad outcomes are most frequent among the lowest coordinators. The pattern is statistically significant for hospitalists.
| Team‐Patient Encounters, n | Mean Length of Encounter, n (days) | ICU Transfer, n (%) | Hospital Death, n (%) | Bad Outcome, n (%) | |
|---|---|---|---|---|---|
| |||||
| Hospitalists | |||||
| High (n = 5) | 92 | 3.1 | 1 (1.1) | 1 (1.1) | 1 (1.1) |
| Middle (n = 5) | 119 | 3.2 | 1 (0.8) | 1 (0.8) | 1 (0.8) |
| Low (n = 5) | 140 | 3.2 | 11 (7.9) | 2 (1.4) | 12 (8.6) |
| p value (high vs. low) | NA | 0.70 | 0.02 | 0.82 | 0.02 |
| Hepatologists | |||||
| High (n = 2) | 99 | 3.2 | (2.0) | 0 (0.0) | 2 (2.0) |
| Middle (n = 2) | 79 | 3.4 | 3 (3.0) | 1 (1.3) | 3 (3.0) |
| Low (n = 2) | 173 | 3.0 | 8 (4.6) | 3 (1.7) | 9 (5.2) |
| p value (high vs. low) | NA | 0.52 | 0.27 | 0.19 | 0.20 |
| GI fellows | |||||
| High (n = 2) | 111 | 3.1 | 2 (1.8) | 0 (0.0) | 2 (1.8) |
| Middle (n = 2) | 67 | 3.3 | 2 (3.0) | 1 (1.5) | 2 (3.0) |
| Low (n = 2) | 173 | 3.2 | 9 (5.2) | 3 (1.7) | 10 (5.8) |
| p value (high vs. low) | NA | 0.74 | 0.15 | 0.16 | 0.10 |
Another interesting observation is the largest number of encounters in the lowest coordination tertile of each physician type. While the reason for this finding is not clear, associations between work‐load and poor coordination evoke issues related to burnout. In order to address the possibility of an artifactually elevated probability of a bad outcome among providers who rotated through the service more often, we calculated the correlation between the number of encounter‐days and the frequency of bad outcomes for the 15 providers who were associated with at last one such event. If these events occurred by chance, we should find a positive correlation between its frequency and the number of encounters. The Pearson's correlation coefficient of 0.38 suggests that bad outcomes do not occur more frequently with providers who work more rotations by chance alone.
Discussion
By adapting Gittell's RC instrument to focus on individual providers, we found that their characteristic attributes such as preference for particular management styles, leadership quality, and patient ownership are associated with their externally perceived contributions to the overall coordination of care. In an unadjusted analysis, we also observed an intriguing trend towards more frequent major hospital complications when the worst coordinators of each physician type were on service.
Existing evidence22, 23 mostly summarized in a recent RAND Health report shows a weak association between clinical teamwork quality and patient mortality. While our data also support this association, it does so with limitations. Most importantly, the small sample size limited our ability to rigorously account for potential confounders that may have contributed to this apparent association. Further studies may better address whether or not bad outcomes are indeed associated with poor coordinators in highly interdependent clinical teams. In addition to confounding, the small sample size of providers makes the analysis vulnerable to type 1 errors. We addressed this issue by intensively surveying providers repeatedly to achieve a high resolution of the coordination and management structure measures from each comanaged team. The potential for omitted variables and reverse causality in that the coordination scores may be negatively influenced by particularly complex patients and bad outcomes remains a valid concern. We addressed this by confirming the stability of provider RC over time and excluding the RC data from rotations with a bad outcome, but the negative perception of an individual tied to past bad outcomes may persist beyond a particular rotation. Survey responses are subject to recall and hindsight biases, which we attempted to minimize by surveying respondents immediately after each team rotation. Finally, all of our findings may be not be generalizable to other comanagement settings. However, the important correlations between coordination and quality have been observed in other contexts.24, 25
In our study, in‐hospital deaths and ICU transfers are treated as consequences of uncoordinated care. This interpretation may be problematic for circumstances when death is inevitable no matter how well coordinated the care, or when transfer to a higher level of care is appropriate. The rationale for grouping the 2 events into 1 composite bad outcome is based on the assumption that both death and the escalation of care can be delayed to an extent, if not wholly prevented, with the coordinated utilization of a modern hospital's resources. The attribution of these events to poor coordinators may indicate the unraveling of coordination that normally must be maintained to help patients overcome decompensating events that are particularly common in the course of patients with severe liver diseases. Due to the exploratory nature of this analysis, additional studies are necessary to fully characterize the relationship between care coordination and care transfers.
An important implication of this study is that the communication skill and ethical disposition of each individual provider is relevant to the coordination that is sought in multi‐provider teams. Training medical professionals to be better team members may have direct impact on the patients they serve. Our finding about patient ownership suggests that commitment to patients in the framework of care is not merely tradition but a characteristic of competent physicians. Moreover, physicians' commitment to patients is a possible factor, not just in achieving patients' satisfaction, but in securing better outcomes. To that end, the teaching of this and other humanistic principles must remain a vital part of medical education at all levels of training.
Several implications about team leadership and hierarchy are apparent from the data. Findings around the perceived assignment of responsibilities show that high coordinator hepatologists acknowledge the advantages of overlapping task boundaries to prevent critical tasks from being missed and risking bad outcomes. High RC hepatologists in our study adopted a more participatory than supervisory role which presumably facilitated better coordination by transmitting organizational goals to other team members. The function of a comanaged team is likely to be enhanced by a fluid assignment of roles to better handle tasks with high uncertainty. Accordingly, comanagement models of care may not be appropriate in settings where tasks are not interdependent.26 Inherent hierarchy appears to be a feature of well coordinated teams. One possible interpretation of our data is that hospitalists who yield the leadership role to the hepatologist are perceived to be better coordinators and that those who insist on exerting more influence in team decisions are perceived to be poor coordinators.
Existing evidence around care coordination predicts that comanagement designs improve provider coordination through stage‐based and site‐based specialization.12 However, the mechanisms that mediate coordination and patient outcomes are not clear. Moreover, the mechanisms of coordinating multi‐disciplinary teams may be specific to each clinical setting. The role of individual provider characteristics on coordination deserves more attention. Similarly, the impact of organizational culture under which favorable provider characteristics thrive is unknown. Finally, a detailed exposition of patient ownership and the role patients play in affecting the coordination of healthcare resources needs further exploration.
- .Technology, specialization, and the allied health professions.J Allied Health.1983;12(3):177–182.
- .Hospitalists and the doctor‐patient relationship.J Legal Stud.2001;30:589–606.
- .From Chaos to Care: The Promise of Team‐Based medicine.Cambridge, MA:Perseus;2002.
- ,,.Determinants of coordination modes within organizations.Am Sociol Rev.1976;41:322–338.
- .Teamwork and patient safety in dynamic domains of healthcare: a review of the literature.Acta Anaesthesiol Scand.2009;53(2):143–151.
- ,,,,.The association between interdisciplinary collaboration and patient outcomes in a medical intensive care unit.Heart Lung.1992;21:18–24.
- ,,, et al.Patterns of coordination and clinical outcomes: a study of surgical services.Health Serv Res.1998;22:1211–1236.
- ,,, et al.Impact of relational coordination on quality of care, postoperative pain and functioning, and length of stay: a nine‐hospital study of surgical patients.Med Care.2000;38(8):807–819.
- ,,.The link between teamwork and patients' outcomes in intensive care units.Am J Crit Care.2003;12(6):527–534.
- ,,.Assessing system failures in operating rooms and intensive care units.Qual Saf health Care.2007;16:45–50.
- ,,, et al.Patient handover from surgery to intensive care: using Formula 1 pit‐stop and aviation models to improve safety and quality.Paediatr Anaesth.2007;17(5):470–478.
- ,,,.Is the doctor in? A relational approach to job design and the coordination of work.Hum Resour Manage.2008;47(4):729–755.
- ,,,.Developing a team performance framework for the intensive care unit.Crit Care Med.2009;37(5):1787–1793.
- ,,, et al.Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized, controlled trial.Ann Intern Med.2004;141(1):28–38.
- ,,.Medical/psychiatric comanagement by nurse practitioners in chronic hepatitis C treatment: a case study.Arch Psychiatr Nurs.2007;21(2):87–90.
- ,.Perioperative medicine for the hospitalized patient.Med Clin North Am.2008;92(2):325–348.
- .The place and training of the general practitioner.Calif Med.1949;70(4):265–268.
- ,.Surgical comanagement: a natural evolution of hospitalist practice.J Hosp Med.2008;3(5):394–397.
- ,,,.Validation of a telephone version of the mini‐mental state examination.J Am Geriatr Soc.1992;40(7):697–702.
- .Organizing work to support relational co‐ordination.Int J of Human Resource Management.2000;11(3):517–539.
- ,,,,.Beyond our walls: impact of patient and provider coordination across the continuum on outcomes for surgical patients.Health Serv Res.2007;42:7–24.
- ,,,,.The effect of multidisciplinary care teams on intensive care unit mortality.Arch Intern Med.2010;170(4):369–376.
- ,,,.Outcome measures for effective teamwork in inpatient care: final report.Santa Monica:RAND Health;2008.
- ,,, et al.The performance of intensive care units: does good management make a difference?Med Care.1994;32(5):508–525.
- ,,,.Observational assessment of surgical teamwork: a feasibility study.World J Surg.2006;30(10):1774–1783.
- .Just because you can, doesn't mean that you should: A call for the rational application of hospitalist comanagement.J Hosp Med.2008;3(5):398–3402.
Technological advances drive medical providers to specialize through the need for proficiency around increasingly focused areas of expertise.1 But the benefits of specialization are attained only by balancing the advantages of increasing expertise and the costs of coordinating care that must be borne as specialization increases.2 Integrating experts into modern medical delivery systems requires attention to the coordinating mechanisms that govern team‐based care.3
Coordination, defined as the management of task interdependencies,4 is a central component and a useful measure of teamwork.5 Several studies demonstrate the patient‐level impact of coordination among providers.69 Gittell et al.8 demonstrated that orthopedic hospitals whose staff had better relational coordination (RC) measures had shorter lengths of stay and better post‐operative pain control for patients undergoing surgery. In medical intensive care units (ICUs), Wheelan et al.9 showed that staff members of units with lower mortality rates perceived their teams as functioning at higher stages of group development and perceived their team members as less dependent and more trusting.
Communication is the cornerstone of effective team coordination.10, 11 As such, practice model interventions that facilitate frequent communication of higher quality are associated with lower error rates10 and better teamwork.11 The use of hospitalists, for example, is shown to capitalize on this advantage by improving coordination through physician availability that facilitates communication and relational interactions among hospital‐based staff.12 While system‐level interventions such as this have received significant attention from experts in organizations, empirical studies that explore the contribution of team member characteristics to overall coordination are lacking.13
Inpatient comanagement services offer a unique model for studying teamwork. While the label is used to describe a variety of arrangements,1416 comanagement broadly describes a practice model wherein providers of various specialties deliver direct care to patients, in contrast to the traditional generalist‐consultant model in which specialists lend expertise.17 Many recent comanagement practices involve hospitalists in partnership with surgeons in the care of patients with concurrent medical and surgical needs,18 but similar arrangements between hospitalists and medical subspecialists are being adopted in some medical centers for the care of complex patients with conditions such as heart failure, cancer, stroke, and solid organ transplantations. Coordination among providers has not been studied in this context.
The goals of this study are: (1) to measure the input of individual providers to the overall coordination of care on a highly interdependent medical comanagement service, (2) to characterize high and low coordinators, and (3) to explore the relationship between coordination and patient outcomes. The main hypothesis is that the quality of team coordination is determined partly by the attributes of its members such that their individual contributions to the coordination of care affect the outcomes of vulnerable hospitalized patients.
Materials and Methods
Setting
The study was conducted at the University of Chicago Medical Center, Chicago, IL, an urban 572‐bed tertiary care hospital. The comanaged multidisciplinary inpatient service serves hospitalized patients with complex medical needs. This study focused on providers and patients from a subset of the comanaged multidisciplinary inpatient service that involved the collaboration of medical hepatologists with hospitalists. A hepatology team, composed of an attending hepatologist and a fellow, comanaged with 2 hospitalist teams, each composed of an attending hospitalist and 1 or 2 nonphysician providers (NPPs). Attending physicians rotated on the service in 1‐week to 3‐week rotations, while fellows rotated in 4‐week stretches. NPPs worked nonuniform 3‐day or 4‐day weeks excluding weekends and holidays. The hepatology team was responsible for arranging admissions, developing a care plan with a specialty focus, coordinating care with transplant surgeons when necessary, and managing post‐discharge care. The hospitalist teams were responsible for admitting patients, managing routine and emergent inpatient issues, coordinating care with ancillary and consultative staff, and discharging patients. Dedicated evening and night hospitalists, who were not part of the comanaging day‐time teams, provided after‐hours care. Outside of these areas, there was no instruction or education about how responsibilities should be shared among providers on the service.
Subjects and Study Design
Baseline Survey of Providers
All hospitalists, NPPs, hepatologists, and fellows scheduled to rotate on the comanaged multidisciplinary inpatient service signed a written consent to participate. In April 2008 a nonanonymous baseline 17‐item paper survey was administered.
Items of the Baseline Survey (supporting information Appendix A) were generated from a consideration of the most salient issues around the management structure of comanagement models from a comprehensive review the literature. Two items addressed the respondents' experience and intent to leave their role. Twelve items addressed their preferences about the provider management structure of an ideally comanaged inpatient service, specifically soliciting their preferences about a single physician leader, consensus seeking, and their preferred degree of information, participation, and decision making under the model. Included in this set of items was a single item assessment of the provider's sense of patient ownership on an ideally comanaged service. The final 3 items addressed the perceived assignment of responsibilities. Each of these items presented a clinical objective followed by up to 7 contingent tasks on whose completion the successful execution of the objective depended. Each respondent was asked to indicate one or more of the 4 provider types that should be responsible for completing each task.
Repeated Survey of Providers
From April to October 2008, providers who rotated on the comanaged liver service were surveyed repeatedly to give information about the actual management structure and coordination within teams, which consisted of combinations of randomly assigned providers. Physicians were surveyed on the day when any 1 of the 3 physician types ended his or her rotation. NPPs were surveyed every Wednesday except on the weeks when none of the physicians had changed since the previous survey. One investigator (KH) hand‐delivered the surveys, usually during the first minutes of the joint daily rounds and collected them immediately upon completion. Surveys that could not be completed immediately were collected on daily rounds on subsequent days within 1 week. The primary reason for nonresponse was lost surveys that were not immediately completed.
The 14‐item Repeated Survey (supporting information Appendix B) consisted of 2 parts. The first 7 items reprised items from the Baseline Survey that addressed management structures, but were rephrased to allow respondents to report their experiences on their immediate rotation. The second part of the Repeated Survey addressed RC, which is described below.
The study protocols, consents, and data collection mechanisms were approved by the institutional review board of the University of Chicago Medical Center. Collection of patient information was designed to comply with the Health Insurance Portability and Accountability Act of 1996.
Patients
Patients were admitted to 1 of the 2 hospitalist teams on the comanaged service on alternating days, which allowed patients to be assigned to providers pseudo‐randomly. Consent to use clinical data was obtained during their stay or by telephone after discharge. If patients were unable to provide consent due to cognitive impairment, consent was sought through designated proxies.19
Main Measurements
Relational Care Coordination
The survey instrument used to measure individual contributions to overall coordination was adapted from the Relational Coordination tool developed by Gittell.20 This instrument was chosen because it has already been validated in various clinical contexts8, 12, 21 and the theoretical assumptions about the independent relational and communication components of coordination are applicable to our context. RC is characterized by the 7 domains of frequent, timely, accurate, and problem‐solving communications; shared goals, shared knowledge, and mutual respect. Respondents rated, on a 5‐point scale (1 = negative, 5 = positive), team members of the other 3 provider types during each rotation on all of the 7 domains. The mean across the domains yielded the RC score. Although the instrument was originally developed to measure the coordination in groups of individuals, the RC for a single provider was calculated by taking the mean of all the RC directed at that individual across team members who worked with him or her during the study period. Because some providers worked more rotations than others, a nonuniform number of observations contributed to the calculation of individual RC (Table 1). For each provider type, individuals were ranked on their RC and categorized in tertiles representing high, middle, and low coordinators.
| Baseline Survey (%) | Repeated Surveys (%) | % Female | Years Experience Median (range) | # RC Evaluations of Each Provider Median (range) | RC Mean (range) | |
|---|---|---|---|---|---|---|
| ||||||
| Hospitalists | 15/15 (100) | 36/43 (84) | 42 | 1 (0‐10) | 6 (3‐21) | 4.71 (4.33‐4.94) |
| NPPs | 5/5 (100) | 92/97 (95) | 100 | 4 (2‐15) | 30 (23‐34) | 4.60 (4.48‐4.71) |
| Hepatologists | 6/6 (100) | 26/42 (62) | 33 | 7 (1‐25) | 16 (5‐51) | 4.37 (4.03‐4.59) |
| GI fellows | 6/6 (100) | 23/42 (55) | 48 | 1 (0‐1) | 19 (8‐37) | 4.28 (3.88‐4.53) |
| Total | 32/32 (100) | 177/223 (79) | 55 | 2 (0‐25) | 12.5 (3‐51) | 4.57 (3.88‐4.94) |
Statistical Analysis
The discriminating ability of the RC for individuals was assessed by comparing the highest and lowest RC of each provider type using the 2‐tailed t‐test. The difference in responses to items from the Baseline and Repeated Surveys by individual RC tertiles was assessed with the Chi‐squared test for categorical data and the 2‐tailed t‐test for comparing means. For each physician type, the frequency of the composite bad outcomes between the highest and lowest RC tertile categories were compared using a 2‐sample Wilcoxon rank‐sum (Mann‐Whitney) test for nonparametric data.
Results
All 32 providers (100%) completed the Baseline Survey and participated in the Repeated Surveys of which 177/224 (79%) were completed. The median number of surveys that contributed to the calculation of individual RC and the mean RC by provider type are summarized in Table 1.
Of the 119 patients managed on the service, the mean age (standard deviation [SD]) was 55 (14) years and 48% were women. Of the 201 hospitalizations, there were 13 floor‐to‐ICU transfers and 5 in‐hospital deaths, however, we excluded from the analysis 1 death of a patient who was admitted under inpatient hospice status.
RC Measures
Individual provider RC ranges were 4.33 to 4.94 (p = 0.05) for hospitalists; 4.48 to 4.71 (p = 0.10) for NP/PAs; 4.03 to 4.59 (p < 0.01) for hepatologists; and 3.88 to 4.52 (p = 0.02) for fellows. The high, middle, and low coordinator categories for each provider type were shown to be durable through time by demonstrating that the coordination ranking of individuals was essentially preserved even when using partial data from each half of the study period. Thus, RC appears to reflect a stable attribute of the provider as opposed to specific circumstances of the rotation. The categories were shown to be durable to the influences of bad outcomes (inpatient deaths and ICU transfers) by demonstrating that the placement of individuals into 1 of the 3 coordination categories were preserved even when data from rotations involving a bad outcome were removed. Nonetheless, in order to address the possibility of bad outcomes negatively affecting perception of coordination, all analysis involving RC used the values that excluded data from these rotations.
Characteristics of Good and Poor Coordinators
Patient Ownership
The single‐item measure of patient ownership in the Baseline Survey reads: I have as much a sense of ownership of my patients on the comanaged service as on a non‐comanaged service. The majority of providers of every type in the high and middle coordinator categories agreed, while providers in the low coordinator category generally disagreed with the statement. The aggregated responses of all the provider types are shown in Table 2.
| Agree | Somewhat Agree | Somewhat Disagree | Disagree | |
|---|---|---|---|---|
| High | 4 | 6 | 0 | 1 |
| Middle | 5 | 4 | 0 | 2 |
| Low | 2 | 0 | 4 | 4 |
| p < 0.01 |
Leadership
Hepatologists are the potential leader of the comanaged team because of their content expertise in liver diseases. Their responses to the 3 items in the Baseline Survey that addressed perceived assignment of responsibilities are shown in Table 3. The high compared to the low coordinator hepatologists delegated the responsibility of completing necessary tasks to more providers, overall, such that an average of 3 providers were redundantly held responsible for the completion of each task by the high coordinators while only 1 provider was held responsible by the low coordinators. Furthermore, the high coordinators delegated the responsibility of completing more tasks to themselves compared to the low coordinators.
| Hepatologists | Mean # of Tasks Delegated Overall, n (SD) | Mean # of Providers Delegated to Each Task, n (SD) | Mean # of Tasks Delegated to Self, n (SD) |
|---|---|---|---|
| |||
| High (n = 2) | 56 (0.0) | 2.9 (0.0) | 11.5 (2.1) |
| Middle (n = 2) | 35 (2.8) | 1.8 (0.2) | 9.5 (3.5) |
| Low (n = 2) | 19 (1.4) | 1.0 (0.1) | 4.5 (2.1) |
| p value(high vs. low) | <0.01 | <0.01 | 0.08 |
According to responses to the management structure items of the Repeated Surveys, more providers of every type indicated that a single physician leader directed the overall management of every patient when a high or middle coordinator hospitalist was on service as opposed to a service with a low coordinator hospitalist (high 76% vs. middle 73% vs. low 58%, P = 0.06). Furthermore, a low coordinator hospitalist on service was more likely to indicate a desire for greater influence in directing the management of patients (desire influence 93% vs. not 7%, P < 0.01). This pattern was also seen with low coordinator NPPs, who more often indicated a desire for greater influence in directing patient management (desire influence 100% vs. not 0%, P < 0.01).
Experience
Age, years in practice, years at the institution, and time spent on the comanaged service were not associated with RC in our small sample of providers.
Outcomes by Provider Coordination
The unit of analysis in this section is the team‐patient encounter, which is the consecutive days during which a unique assortment of physicians managed a patient's hospitalization. NPPs could not be associated with any single team due to their nonuniform work patterns. The 201 hospitalizations in this study were composed of 351 team‐patient encounters. Table 4 displays the unadjusted frequency of inpatient deaths and ICU transfers that occurred during these encounters by RC tertiles. In each of the 3 physician types, composite bad outcomes are most frequent among the lowest coordinators. The pattern is statistically significant for hospitalists.
| Team‐Patient Encounters, n | Mean Length of Encounter, n (days) | ICU Transfer, n (%) | Hospital Death, n (%) | Bad Outcome, n (%) | |
|---|---|---|---|---|---|
| |||||
| Hospitalists | |||||
| High (n = 5) | 92 | 3.1 | 1 (1.1) | 1 (1.1) | 1 (1.1) |
| Middle (n = 5) | 119 | 3.2 | 1 (0.8) | 1 (0.8) | 1 (0.8) |
| Low (n = 5) | 140 | 3.2 | 11 (7.9) | 2 (1.4) | 12 (8.6) |
| p value (high vs. low) | NA | 0.70 | 0.02 | 0.82 | 0.02 |
| Hepatologists | |||||
| High (n = 2) | 99 | 3.2 | (2.0) | 0 (0.0) | 2 (2.0) |
| Middle (n = 2) | 79 | 3.4 | 3 (3.0) | 1 (1.3) | 3 (3.0) |
| Low (n = 2) | 173 | 3.0 | 8 (4.6) | 3 (1.7) | 9 (5.2) |
| p value (high vs. low) | NA | 0.52 | 0.27 | 0.19 | 0.20 |
| GI fellows | |||||
| High (n = 2) | 111 | 3.1 | 2 (1.8) | 0 (0.0) | 2 (1.8) |
| Middle (n = 2) | 67 | 3.3 | 2 (3.0) | 1 (1.5) | 2 (3.0) |
| Low (n = 2) | 173 | 3.2 | 9 (5.2) | 3 (1.7) | 10 (5.8) |
| p value (high vs. low) | NA | 0.74 | 0.15 | 0.16 | 0.10 |
Another interesting observation is the largest number of encounters in the lowest coordination tertile of each physician type. While the reason for this finding is not clear, associations between work‐load and poor coordination evoke issues related to burnout. In order to address the possibility of an artifactually elevated probability of a bad outcome among providers who rotated through the service more often, we calculated the correlation between the number of encounter‐days and the frequency of bad outcomes for the 15 providers who were associated with at last one such event. If these events occurred by chance, we should find a positive correlation between its frequency and the number of encounters. The Pearson's correlation coefficient of 0.38 suggests that bad outcomes do not occur more frequently with providers who work more rotations by chance alone.
Discussion
By adapting Gittell's RC instrument to focus on individual providers, we found that their characteristic attributes such as preference for particular management styles, leadership quality, and patient ownership are associated with their externally perceived contributions to the overall coordination of care. In an unadjusted analysis, we also observed an intriguing trend towards more frequent major hospital complications when the worst coordinators of each physician type were on service.
Existing evidence22, 23 mostly summarized in a recent RAND Health report shows a weak association between clinical teamwork quality and patient mortality. While our data also support this association, it does so with limitations. Most importantly, the small sample size limited our ability to rigorously account for potential confounders that may have contributed to this apparent association. Further studies may better address whether or not bad outcomes are indeed associated with poor coordinators in highly interdependent clinical teams. In addition to confounding, the small sample size of providers makes the analysis vulnerable to type 1 errors. We addressed this issue by intensively surveying providers repeatedly to achieve a high resolution of the coordination and management structure measures from each comanaged team. The potential for omitted variables and reverse causality in that the coordination scores may be negatively influenced by particularly complex patients and bad outcomes remains a valid concern. We addressed this by confirming the stability of provider RC over time and excluding the RC data from rotations with a bad outcome, but the negative perception of an individual tied to past bad outcomes may persist beyond a particular rotation. Survey responses are subject to recall and hindsight biases, which we attempted to minimize by surveying respondents immediately after each team rotation. Finally, all of our findings may be not be generalizable to other comanagement settings. However, the important correlations between coordination and quality have been observed in other contexts.24, 25
In our study, in‐hospital deaths and ICU transfers are treated as consequences of uncoordinated care. This interpretation may be problematic for circumstances when death is inevitable no matter how well coordinated the care, or when transfer to a higher level of care is appropriate. The rationale for grouping the 2 events into 1 composite bad outcome is based on the assumption that both death and the escalation of care can be delayed to an extent, if not wholly prevented, with the coordinated utilization of a modern hospital's resources. The attribution of these events to poor coordinators may indicate the unraveling of coordination that normally must be maintained to help patients overcome decompensating events that are particularly common in the course of patients with severe liver diseases. Due to the exploratory nature of this analysis, additional studies are necessary to fully characterize the relationship between care coordination and care transfers.
An important implication of this study is that the communication skill and ethical disposition of each individual provider is relevant to the coordination that is sought in multi‐provider teams. Training medical professionals to be better team members may have direct impact on the patients they serve. Our finding about patient ownership suggests that commitment to patients in the framework of care is not merely tradition but a characteristic of competent physicians. Moreover, physicians' commitment to patients is a possible factor, not just in achieving patients' satisfaction, but in securing better outcomes. To that end, the teaching of this and other humanistic principles must remain a vital part of medical education at all levels of training.
Several implications about team leadership and hierarchy are apparent from the data. Findings around the perceived assignment of responsibilities show that high coordinator hepatologists acknowledge the advantages of overlapping task boundaries to prevent critical tasks from being missed and risking bad outcomes. High RC hepatologists in our study adopted a more participatory than supervisory role which presumably facilitated better coordination by transmitting organizational goals to other team members. The function of a comanaged team is likely to be enhanced by a fluid assignment of roles to better handle tasks with high uncertainty. Accordingly, comanagement models of care may not be appropriate in settings where tasks are not interdependent.26 Inherent hierarchy appears to be a feature of well coordinated teams. One possible interpretation of our data is that hospitalists who yield the leadership role to the hepatologist are perceived to be better coordinators and that those who insist on exerting more influence in team decisions are perceived to be poor coordinators.
Existing evidence around care coordination predicts that comanagement designs improve provider coordination through stage‐based and site‐based specialization.12 However, the mechanisms that mediate coordination and patient outcomes are not clear. Moreover, the mechanisms of coordinating multi‐disciplinary teams may be specific to each clinical setting. The role of individual provider characteristics on coordination deserves more attention. Similarly, the impact of organizational culture under which favorable provider characteristics thrive is unknown. Finally, a detailed exposition of patient ownership and the role patients play in affecting the coordination of healthcare resources needs further exploration.
Technological advances drive medical providers to specialize through the need for proficiency around increasingly focused areas of expertise.1 But the benefits of specialization are attained only by balancing the advantages of increasing expertise and the costs of coordinating care that must be borne as specialization increases.2 Integrating experts into modern medical delivery systems requires attention to the coordinating mechanisms that govern team‐based care.3
Coordination, defined as the management of task interdependencies,4 is a central component and a useful measure of teamwork.5 Several studies demonstrate the patient‐level impact of coordination among providers.69 Gittell et al.8 demonstrated that orthopedic hospitals whose staff had better relational coordination (RC) measures had shorter lengths of stay and better post‐operative pain control for patients undergoing surgery. In medical intensive care units (ICUs), Wheelan et al.9 showed that staff members of units with lower mortality rates perceived their teams as functioning at higher stages of group development and perceived their team members as less dependent and more trusting.
Communication is the cornerstone of effective team coordination.10, 11 As such, practice model interventions that facilitate frequent communication of higher quality are associated with lower error rates10 and better teamwork.11 The use of hospitalists, for example, is shown to capitalize on this advantage by improving coordination through physician availability that facilitates communication and relational interactions among hospital‐based staff.12 While system‐level interventions such as this have received significant attention from experts in organizations, empirical studies that explore the contribution of team member characteristics to overall coordination are lacking.13
Inpatient comanagement services offer a unique model for studying teamwork. While the label is used to describe a variety of arrangements,1416 comanagement broadly describes a practice model wherein providers of various specialties deliver direct care to patients, in contrast to the traditional generalist‐consultant model in which specialists lend expertise.17 Many recent comanagement practices involve hospitalists in partnership with surgeons in the care of patients with concurrent medical and surgical needs,18 but similar arrangements between hospitalists and medical subspecialists are being adopted in some medical centers for the care of complex patients with conditions such as heart failure, cancer, stroke, and solid organ transplantations. Coordination among providers has not been studied in this context.
The goals of this study are: (1) to measure the input of individual providers to the overall coordination of care on a highly interdependent medical comanagement service, (2) to characterize high and low coordinators, and (3) to explore the relationship between coordination and patient outcomes. The main hypothesis is that the quality of team coordination is determined partly by the attributes of its members such that their individual contributions to the coordination of care affect the outcomes of vulnerable hospitalized patients.
Materials and Methods
Setting
The study was conducted at the University of Chicago Medical Center, Chicago, IL, an urban 572‐bed tertiary care hospital. The comanaged multidisciplinary inpatient service serves hospitalized patients with complex medical needs. This study focused on providers and patients from a subset of the comanaged multidisciplinary inpatient service that involved the collaboration of medical hepatologists with hospitalists. A hepatology team, composed of an attending hepatologist and a fellow, comanaged with 2 hospitalist teams, each composed of an attending hospitalist and 1 or 2 nonphysician providers (NPPs). Attending physicians rotated on the service in 1‐week to 3‐week rotations, while fellows rotated in 4‐week stretches. NPPs worked nonuniform 3‐day or 4‐day weeks excluding weekends and holidays. The hepatology team was responsible for arranging admissions, developing a care plan with a specialty focus, coordinating care with transplant surgeons when necessary, and managing post‐discharge care. The hospitalist teams were responsible for admitting patients, managing routine and emergent inpatient issues, coordinating care with ancillary and consultative staff, and discharging patients. Dedicated evening and night hospitalists, who were not part of the comanaging day‐time teams, provided after‐hours care. Outside of these areas, there was no instruction or education about how responsibilities should be shared among providers on the service.
Subjects and Study Design
Baseline Survey of Providers
All hospitalists, NPPs, hepatologists, and fellows scheduled to rotate on the comanaged multidisciplinary inpatient service signed a written consent to participate. In April 2008 a nonanonymous baseline 17‐item paper survey was administered.
Items of the Baseline Survey (supporting information Appendix A) were generated from a consideration of the most salient issues around the management structure of comanagement models from a comprehensive review the literature. Two items addressed the respondents' experience and intent to leave their role. Twelve items addressed their preferences about the provider management structure of an ideally comanaged inpatient service, specifically soliciting their preferences about a single physician leader, consensus seeking, and their preferred degree of information, participation, and decision making under the model. Included in this set of items was a single item assessment of the provider's sense of patient ownership on an ideally comanaged service. The final 3 items addressed the perceived assignment of responsibilities. Each of these items presented a clinical objective followed by up to 7 contingent tasks on whose completion the successful execution of the objective depended. Each respondent was asked to indicate one or more of the 4 provider types that should be responsible for completing each task.
Repeated Survey of Providers
From April to October 2008, providers who rotated on the comanaged liver service were surveyed repeatedly to give information about the actual management structure and coordination within teams, which consisted of combinations of randomly assigned providers. Physicians were surveyed on the day when any 1 of the 3 physician types ended his or her rotation. NPPs were surveyed every Wednesday except on the weeks when none of the physicians had changed since the previous survey. One investigator (KH) hand‐delivered the surveys, usually during the first minutes of the joint daily rounds and collected them immediately upon completion. Surveys that could not be completed immediately were collected on daily rounds on subsequent days within 1 week. The primary reason for nonresponse was lost surveys that were not immediately completed.
The 14‐item Repeated Survey (supporting information Appendix B) consisted of 2 parts. The first 7 items reprised items from the Baseline Survey that addressed management structures, but were rephrased to allow respondents to report their experiences on their immediate rotation. The second part of the Repeated Survey addressed RC, which is described below.
The study protocols, consents, and data collection mechanisms were approved by the institutional review board of the University of Chicago Medical Center. Collection of patient information was designed to comply with the Health Insurance Portability and Accountability Act of 1996.
Patients
Patients were admitted to 1 of the 2 hospitalist teams on the comanaged service on alternating days, which allowed patients to be assigned to providers pseudo‐randomly. Consent to use clinical data was obtained during their stay or by telephone after discharge. If patients were unable to provide consent due to cognitive impairment, consent was sought through designated proxies.19
Main Measurements
Relational Care Coordination
The survey instrument used to measure individual contributions to overall coordination was adapted from the Relational Coordination tool developed by Gittell.20 This instrument was chosen because it has already been validated in various clinical contexts8, 12, 21 and the theoretical assumptions about the independent relational and communication components of coordination are applicable to our context. RC is characterized by the 7 domains of frequent, timely, accurate, and problem‐solving communications; shared goals, shared knowledge, and mutual respect. Respondents rated, on a 5‐point scale (1 = negative, 5 = positive), team members of the other 3 provider types during each rotation on all of the 7 domains. The mean across the domains yielded the RC score. Although the instrument was originally developed to measure the coordination in groups of individuals, the RC for a single provider was calculated by taking the mean of all the RC directed at that individual across team members who worked with him or her during the study period. Because some providers worked more rotations than others, a nonuniform number of observations contributed to the calculation of individual RC (Table 1). For each provider type, individuals were ranked on their RC and categorized in tertiles representing high, middle, and low coordinators.
| Baseline Survey (%) | Repeated Surveys (%) | % Female | Years Experience Median (range) | # RC Evaluations of Each Provider Median (range) | RC Mean (range) | |
|---|---|---|---|---|---|---|
| ||||||
| Hospitalists | 15/15 (100) | 36/43 (84) | 42 | 1 (0‐10) | 6 (3‐21) | 4.71 (4.33‐4.94) |
| NPPs | 5/5 (100) | 92/97 (95) | 100 | 4 (2‐15) | 30 (23‐34) | 4.60 (4.48‐4.71) |
| Hepatologists | 6/6 (100) | 26/42 (62) | 33 | 7 (1‐25) | 16 (5‐51) | 4.37 (4.03‐4.59) |
| GI fellows | 6/6 (100) | 23/42 (55) | 48 | 1 (0‐1) | 19 (8‐37) | 4.28 (3.88‐4.53) |
| Total | 32/32 (100) | 177/223 (79) | 55 | 2 (0‐25) | 12.5 (3‐51) | 4.57 (3.88‐4.94) |
Statistical Analysis
The discriminating ability of the RC for individuals was assessed by comparing the highest and lowest RC of each provider type using the 2‐tailed t‐test. The difference in responses to items from the Baseline and Repeated Surveys by individual RC tertiles was assessed with the Chi‐squared test for categorical data and the 2‐tailed t‐test for comparing means. For each physician type, the frequency of the composite bad outcomes between the highest and lowest RC tertile categories were compared using a 2‐sample Wilcoxon rank‐sum (Mann‐Whitney) test for nonparametric data.
Results
All 32 providers (100%) completed the Baseline Survey and participated in the Repeated Surveys of which 177/224 (79%) were completed. The median number of surveys that contributed to the calculation of individual RC and the mean RC by provider type are summarized in Table 1.
Of the 119 patients managed on the service, the mean age (standard deviation [SD]) was 55 (14) years and 48% were women. Of the 201 hospitalizations, there were 13 floor‐to‐ICU transfers and 5 in‐hospital deaths, however, we excluded from the analysis 1 death of a patient who was admitted under inpatient hospice status.
RC Measures
Individual provider RC ranges were 4.33 to 4.94 (p = 0.05) for hospitalists; 4.48 to 4.71 (p = 0.10) for NP/PAs; 4.03 to 4.59 (p < 0.01) for hepatologists; and 3.88 to 4.52 (p = 0.02) for fellows. The high, middle, and low coordinator categories for each provider type were shown to be durable through time by demonstrating that the coordination ranking of individuals was essentially preserved even when using partial data from each half of the study period. Thus, RC appears to reflect a stable attribute of the provider as opposed to specific circumstances of the rotation. The categories were shown to be durable to the influences of bad outcomes (inpatient deaths and ICU transfers) by demonstrating that the placement of individuals into 1 of the 3 coordination categories were preserved even when data from rotations involving a bad outcome were removed. Nonetheless, in order to address the possibility of bad outcomes negatively affecting perception of coordination, all analysis involving RC used the values that excluded data from these rotations.
Characteristics of Good and Poor Coordinators
Patient Ownership
The single‐item measure of patient ownership in the Baseline Survey reads: I have as much a sense of ownership of my patients on the comanaged service as on a non‐comanaged service. The majority of providers of every type in the high and middle coordinator categories agreed, while providers in the low coordinator category generally disagreed with the statement. The aggregated responses of all the provider types are shown in Table 2.
| Agree | Somewhat Agree | Somewhat Disagree | Disagree | |
|---|---|---|---|---|
| High | 4 | 6 | 0 | 1 |
| Middle | 5 | 4 | 0 | 2 |
| Low | 2 | 0 | 4 | 4 |
| p < 0.01 |
Leadership
Hepatologists are the potential leader of the comanaged team because of their content expertise in liver diseases. Their responses to the 3 items in the Baseline Survey that addressed perceived assignment of responsibilities are shown in Table 3. The high compared to the low coordinator hepatologists delegated the responsibility of completing necessary tasks to more providers, overall, such that an average of 3 providers were redundantly held responsible for the completion of each task by the high coordinators while only 1 provider was held responsible by the low coordinators. Furthermore, the high coordinators delegated the responsibility of completing more tasks to themselves compared to the low coordinators.
| Hepatologists | Mean # of Tasks Delegated Overall, n (SD) | Mean # of Providers Delegated to Each Task, n (SD) | Mean # of Tasks Delegated to Self, n (SD) |
|---|---|---|---|
| |||
| High (n = 2) | 56 (0.0) | 2.9 (0.0) | 11.5 (2.1) |
| Middle (n = 2) | 35 (2.8) | 1.8 (0.2) | 9.5 (3.5) |
| Low (n = 2) | 19 (1.4) | 1.0 (0.1) | 4.5 (2.1) |
| p value(high vs. low) | <0.01 | <0.01 | 0.08 |
According to responses to the management structure items of the Repeated Surveys, more providers of every type indicated that a single physician leader directed the overall management of every patient when a high or middle coordinator hospitalist was on service as opposed to a service with a low coordinator hospitalist (high 76% vs. middle 73% vs. low 58%, P = 0.06). Furthermore, a low coordinator hospitalist on service was more likely to indicate a desire for greater influence in directing the management of patients (desire influence 93% vs. not 7%, P < 0.01). This pattern was also seen with low coordinator NPPs, who more often indicated a desire for greater influence in directing patient management (desire influence 100% vs. not 0%, P < 0.01).
Experience
Age, years in practice, years at the institution, and time spent on the comanaged service were not associated with RC in our small sample of providers.
Outcomes by Provider Coordination
The unit of analysis in this section is the team‐patient encounter, which is the consecutive days during which a unique assortment of physicians managed a patient's hospitalization. NPPs could not be associated with any single team due to their nonuniform work patterns. The 201 hospitalizations in this study were composed of 351 team‐patient encounters. Table 4 displays the unadjusted frequency of inpatient deaths and ICU transfers that occurred during these encounters by RC tertiles. In each of the 3 physician types, composite bad outcomes are most frequent among the lowest coordinators. The pattern is statistically significant for hospitalists.
| Team‐Patient Encounters, n | Mean Length of Encounter, n (days) | ICU Transfer, n (%) | Hospital Death, n (%) | Bad Outcome, n (%) | |
|---|---|---|---|---|---|
| |||||
| Hospitalists | |||||
| High (n = 5) | 92 | 3.1 | 1 (1.1) | 1 (1.1) | 1 (1.1) |
| Middle (n = 5) | 119 | 3.2 | 1 (0.8) | 1 (0.8) | 1 (0.8) |
| Low (n = 5) | 140 | 3.2 | 11 (7.9) | 2 (1.4) | 12 (8.6) |
| p value (high vs. low) | NA | 0.70 | 0.02 | 0.82 | 0.02 |
| Hepatologists | |||||
| High (n = 2) | 99 | 3.2 | (2.0) | 0 (0.0) | 2 (2.0) |
| Middle (n = 2) | 79 | 3.4 | 3 (3.0) | 1 (1.3) | 3 (3.0) |
| Low (n = 2) | 173 | 3.0 | 8 (4.6) | 3 (1.7) | 9 (5.2) |
| p value (high vs. low) | NA | 0.52 | 0.27 | 0.19 | 0.20 |
| GI fellows | |||||
| High (n = 2) | 111 | 3.1 | 2 (1.8) | 0 (0.0) | 2 (1.8) |
| Middle (n = 2) | 67 | 3.3 | 2 (3.0) | 1 (1.5) | 2 (3.0) |
| Low (n = 2) | 173 | 3.2 | 9 (5.2) | 3 (1.7) | 10 (5.8) |
| p value (high vs. low) | NA | 0.74 | 0.15 | 0.16 | 0.10 |
Another interesting observation is the largest number of encounters in the lowest coordination tertile of each physician type. While the reason for this finding is not clear, associations between work‐load and poor coordination evoke issues related to burnout. In order to address the possibility of an artifactually elevated probability of a bad outcome among providers who rotated through the service more often, we calculated the correlation between the number of encounter‐days and the frequency of bad outcomes for the 15 providers who were associated with at last one such event. If these events occurred by chance, we should find a positive correlation between its frequency and the number of encounters. The Pearson's correlation coefficient of 0.38 suggests that bad outcomes do not occur more frequently with providers who work more rotations by chance alone.
Discussion
By adapting Gittell's RC instrument to focus on individual providers, we found that their characteristic attributes such as preference for particular management styles, leadership quality, and patient ownership are associated with their externally perceived contributions to the overall coordination of care. In an unadjusted analysis, we also observed an intriguing trend towards more frequent major hospital complications when the worst coordinators of each physician type were on service.
Existing evidence22, 23 mostly summarized in a recent RAND Health report shows a weak association between clinical teamwork quality and patient mortality. While our data also support this association, it does so with limitations. Most importantly, the small sample size limited our ability to rigorously account for potential confounders that may have contributed to this apparent association. Further studies may better address whether or not bad outcomes are indeed associated with poor coordinators in highly interdependent clinical teams. In addition to confounding, the small sample size of providers makes the analysis vulnerable to type 1 errors. We addressed this issue by intensively surveying providers repeatedly to achieve a high resolution of the coordination and management structure measures from each comanaged team. The potential for omitted variables and reverse causality in that the coordination scores may be negatively influenced by particularly complex patients and bad outcomes remains a valid concern. We addressed this by confirming the stability of provider RC over time and excluding the RC data from rotations with a bad outcome, but the negative perception of an individual tied to past bad outcomes may persist beyond a particular rotation. Survey responses are subject to recall and hindsight biases, which we attempted to minimize by surveying respondents immediately after each team rotation. Finally, all of our findings may be not be generalizable to other comanagement settings. However, the important correlations between coordination and quality have been observed in other contexts.24, 25
In our study, in‐hospital deaths and ICU transfers are treated as consequences of uncoordinated care. This interpretation may be problematic for circumstances when death is inevitable no matter how well coordinated the care, or when transfer to a higher level of care is appropriate. The rationale for grouping the 2 events into 1 composite bad outcome is based on the assumption that both death and the escalation of care can be delayed to an extent, if not wholly prevented, with the coordinated utilization of a modern hospital's resources. The attribution of these events to poor coordinators may indicate the unraveling of coordination that normally must be maintained to help patients overcome decompensating events that are particularly common in the course of patients with severe liver diseases. Due to the exploratory nature of this analysis, additional studies are necessary to fully characterize the relationship between care coordination and care transfers.
An important implication of this study is that the communication skill and ethical disposition of each individual provider is relevant to the coordination that is sought in multi‐provider teams. Training medical professionals to be better team members may have direct impact on the patients they serve. Our finding about patient ownership suggests that commitment to patients in the framework of care is not merely tradition but a characteristic of competent physicians. Moreover, physicians' commitment to patients is a possible factor, not just in achieving patients' satisfaction, but in securing better outcomes. To that end, the teaching of this and other humanistic principles must remain a vital part of medical education at all levels of training.
Several implications about team leadership and hierarchy are apparent from the data. Findings around the perceived assignment of responsibilities show that high coordinator hepatologists acknowledge the advantages of overlapping task boundaries to prevent critical tasks from being missed and risking bad outcomes. High RC hepatologists in our study adopted a more participatory than supervisory role which presumably facilitated better coordination by transmitting organizational goals to other team members. The function of a comanaged team is likely to be enhanced by a fluid assignment of roles to better handle tasks with high uncertainty. Accordingly, comanagement models of care may not be appropriate in settings where tasks are not interdependent.26 Inherent hierarchy appears to be a feature of well coordinated teams. One possible interpretation of our data is that hospitalists who yield the leadership role to the hepatologist are perceived to be better coordinators and that those who insist on exerting more influence in team decisions are perceived to be poor coordinators.
Existing evidence around care coordination predicts that comanagement designs improve provider coordination through stage‐based and site‐based specialization.12 However, the mechanisms that mediate coordination and patient outcomes are not clear. Moreover, the mechanisms of coordinating multi‐disciplinary teams may be specific to each clinical setting. The role of individual provider characteristics on coordination deserves more attention. Similarly, the impact of organizational culture under which favorable provider characteristics thrive is unknown. Finally, a detailed exposition of patient ownership and the role patients play in affecting the coordination of healthcare resources needs further exploration.
- .Technology, specialization, and the allied health professions.J Allied Health.1983;12(3):177–182.
- .Hospitalists and the doctor‐patient relationship.J Legal Stud.2001;30:589–606.
- .From Chaos to Care: The Promise of Team‐Based medicine.Cambridge, MA:Perseus;2002.
- ,,.Determinants of coordination modes within organizations.Am Sociol Rev.1976;41:322–338.
- .Teamwork and patient safety in dynamic domains of healthcare: a review of the literature.Acta Anaesthesiol Scand.2009;53(2):143–151.
- ,,,,.The association between interdisciplinary collaboration and patient outcomes in a medical intensive care unit.Heart Lung.1992;21:18–24.
- ,,, et al.Patterns of coordination and clinical outcomes: a study of surgical services.Health Serv Res.1998;22:1211–1236.
- ,,, et al.Impact of relational coordination on quality of care, postoperative pain and functioning, and length of stay: a nine‐hospital study of surgical patients.Med Care.2000;38(8):807–819.
- ,,.The link between teamwork and patients' outcomes in intensive care units.Am J Crit Care.2003;12(6):527–534.
- ,,.Assessing system failures in operating rooms and intensive care units.Qual Saf health Care.2007;16:45–50.
- ,,, et al.Patient handover from surgery to intensive care: using Formula 1 pit‐stop and aviation models to improve safety and quality.Paediatr Anaesth.2007;17(5):470–478.
- ,,,.Is the doctor in? A relational approach to job design and the coordination of work.Hum Resour Manage.2008;47(4):729–755.
- ,,,.Developing a team performance framework for the intensive care unit.Crit Care Med.2009;37(5):1787–1793.
- ,,, et al.Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized, controlled trial.Ann Intern Med.2004;141(1):28–38.
- ,,.Medical/psychiatric comanagement by nurse practitioners in chronic hepatitis C treatment: a case study.Arch Psychiatr Nurs.2007;21(2):87–90.
- ,.Perioperative medicine for the hospitalized patient.Med Clin North Am.2008;92(2):325–348.
- .The place and training of the general practitioner.Calif Med.1949;70(4):265–268.
- ,.Surgical comanagement: a natural evolution of hospitalist practice.J Hosp Med.2008;3(5):394–397.
- ,,,.Validation of a telephone version of the mini‐mental state examination.J Am Geriatr Soc.1992;40(7):697–702.
- .Organizing work to support relational co‐ordination.Int J of Human Resource Management.2000;11(3):517–539.
- ,,,,.Beyond our walls: impact of patient and provider coordination across the continuum on outcomes for surgical patients.Health Serv Res.2007;42:7–24.
- ,,,,.The effect of multidisciplinary care teams on intensive care unit mortality.Arch Intern Med.2010;170(4):369–376.
- ,,,.Outcome measures for effective teamwork in inpatient care: final report.Santa Monica:RAND Health;2008.
- ,,, et al.The performance of intensive care units: does good management make a difference?Med Care.1994;32(5):508–525.
- ,,,.Observational assessment of surgical teamwork: a feasibility study.World J Surg.2006;30(10):1774–1783.
- .Just because you can, doesn't mean that you should: A call for the rational application of hospitalist comanagement.J Hosp Med.2008;3(5):398–3402.
- .Technology, specialization, and the allied health professions.J Allied Health.1983;12(3):177–182.
- .Hospitalists and the doctor‐patient relationship.J Legal Stud.2001;30:589–606.
- .From Chaos to Care: The Promise of Team‐Based medicine.Cambridge, MA:Perseus;2002.
- ,,.Determinants of coordination modes within organizations.Am Sociol Rev.1976;41:322–338.
- .Teamwork and patient safety in dynamic domains of healthcare: a review of the literature.Acta Anaesthesiol Scand.2009;53(2):143–151.
- ,,,,.The association between interdisciplinary collaboration and patient outcomes in a medical intensive care unit.Heart Lung.1992;21:18–24.
- ,,, et al.Patterns of coordination and clinical outcomes: a study of surgical services.Health Serv Res.1998;22:1211–1236.
- ,,, et al.Impact of relational coordination on quality of care, postoperative pain and functioning, and length of stay: a nine‐hospital study of surgical patients.Med Care.2000;38(8):807–819.
- ,,.The link between teamwork and patients' outcomes in intensive care units.Am J Crit Care.2003;12(6):527–534.
- ,,.Assessing system failures in operating rooms and intensive care units.Qual Saf health Care.2007;16:45–50.
- ,,, et al.Patient handover from surgery to intensive care: using Formula 1 pit‐stop and aviation models to improve safety and quality.Paediatr Anaesth.2007;17(5):470–478.
- ,,,.Is the doctor in? A relational approach to job design and the coordination of work.Hum Resour Manage.2008;47(4):729–755.
- ,,,.Developing a team performance framework for the intensive care unit.Crit Care Med.2009;37(5):1787–1793.
- ,,, et al.Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized, controlled trial.Ann Intern Med.2004;141(1):28–38.
- ,,.Medical/psychiatric comanagement by nurse practitioners in chronic hepatitis C treatment: a case study.Arch Psychiatr Nurs.2007;21(2):87–90.
- ,.Perioperative medicine for the hospitalized patient.Med Clin North Am.2008;92(2):325–348.
- .The place and training of the general practitioner.Calif Med.1949;70(4):265–268.
- ,.Surgical comanagement: a natural evolution of hospitalist practice.J Hosp Med.2008;3(5):394–397.
- ,,,.Validation of a telephone version of the mini‐mental state examination.J Am Geriatr Soc.1992;40(7):697–702.
- .Organizing work to support relational co‐ordination.Int J of Human Resource Management.2000;11(3):517–539.
- ,,,,.Beyond our walls: impact of patient and provider coordination across the continuum on outcomes for surgical patients.Health Serv Res.2007;42:7–24.
- ,,,,.The effect of multidisciplinary care teams on intensive care unit mortality.Arch Intern Med.2010;170(4):369–376.
- ,,,.Outcome measures for effective teamwork in inpatient care: final report.Santa Monica:RAND Health;2008.
- ,,, et al.The performance of intensive care units: does good management make a difference?Med Care.1994;32(5):508–525.
- ,,,.Observational assessment of surgical teamwork: a feasibility study.World J Surg.2006;30(10):1774–1783.
- .Just because you can, doesn't mean that you should: A call for the rational application of hospitalist comanagement.J Hosp Med.2008;3(5):398–3402.
Copyright © 2010 Society of Hospital Medicine
Nurse Staffing Ratio Trends and Implications
Many studies have reported associations between higher nurse‐to‐patient ratios and decreased mortality and complications. These studies coupled with increasing concern about patient safety, nursing shortages, and nurse burnout have spurred many state legislatures to discuss mandating minimum nurse staffing ratios.15 The California legislature passed law AB394 in 1999, mandating minimum nurse staffing ratios in order to improve patient safety and the nurse work environment. The original implementation date, January 1, 2001, was delayed to allow the California Department of Health Services more time to develop minimum nurse ratios for each unit type.6, 7 California implemented a ratio of at least 1 licensed nurse (RN+LVN) for every 6 patients on general adult medical‐surgical floors on January 1, 2004. This was subsequently increased, on January 1, 2005, to at least 1 licensed nurse for every 5 patients, a ratio that was upheld by the California Supreme Court on March 14, 2005.8
Additional laws regarding nurse staffing are being considered in at least 25 states.9 States have taken 3 main approaches to legislation: mandating nurse staffing ratios for each hospital unit type, requiring hospitals to establish and report nurse staffing plans that typically include ratios, or a combination of mandated ratios and staffing plans.10 This type of legislation would have a major impact on hospitalists, nurses, other health care personnel, hospital administrators, and patients. However, little is known about trends in nurse staffing, how staffing levels vary among hospitals overall, in different markets, and by ownership type and location, and consequently how implementing nurse staffing ratios will affect different types of hospitals, including those that make up the safety net.11
California nurse staffing data are better than many other sources because the state provides nurse staffing hours by unit types in hospitals as opposed to aggregate numbers of nurse hours across an entire hospital or medical center.12 California is also at the forefront of mandated minimum nurse staffing legislation, as it is the only state to have enacted nurse staffing ratio legislation. Examining nurse staffing trends and hospital types currently under mandated or proposed nurse staffing ratios is integral to informing the debate on nurse staffing legislation and its effect on hospitalists. We hypothesized that nurse staffing would increase in California after the legislation was passed in 1999 but that safety‐net hospitals such as those that are urban, government owned, and serving a high percentage of Medicaid and uninsured patients would be more likely to be below minimum ratios.13
MATERIALS AND METHODS
We used hospital financial panel data for 1993 through 2004, the most recent year with complete data, from California's Office of Statewide Health Planning and Development (OSHPD). We included only short‐term acute‐care general hospitals and excluded other hospital types such as long‐term care, children's, and psychiatric hospitals. We investigated staffing of adult general medical‐surgical units and not of other types of units such as intensive care units. The numerator of the staffing variables for each hospital was the combined medical‐surgical productive hours for registered nurses (RNs) and licensed vocational nurses (LVNs), as California allows up to 50% of staffing hours to be LVN hours. Staffing hours of the adult general medical‐surgical units of each hospital are reported on an annual basis. The denominator was total patient days on the acute adult medical‐surgical units of each hospital in a given year. We calculated the number of patients per one nurse by dividing 24 by the nurse hours per patient day (eg, 4.0 nurse hours per patient day is equivalent to a nurse‐to‐patient ratio of 1:6). We did not adjust staffing ratios by the hospital case mix or other factors because the ratio legislation did not take these factors into account.
We further evaluated staffing ratios in 2003 and 2004 based on 5 hospital characteristics: hospital ownership, market competitiveness, teaching status, urban versus rural location, and safety‐net hospitals, using 2 common definitions for the latter. The Institute of Medicine report defines safety‐net providers as those with a substantial share of their patient mix from uninsured and Medicaid populations.13 Safety‐net hospitals have been more specifically defined as short‐term general hospitals whose percentage of Medicaid and uninsured patients is greater than 1 standard deviation above the mean.14 Using this definition, hospitals in California where more than 36% of patients had Medicaid or no insurance in 2004 would be considered safety‐net hospitals. A more comprehensive definition of the hospital safety net that has been used includes urban nonprofit and government hospitals and hospitals with a high percentage of Medicaid/uninsured patients.10, 11, 15 We analyzed nurse staffing ratios using both these definitions. Hospital ownership was designated as for profit, nonprofit, or government owned. Hospital competitiveness was measured using the Hirschman‐Herfindahl Index (HHI), or the sum of squared market shares, a standard approach to defining hospital market competition. Market boundaries were defined as those zip codes from which each hospital draws most of its patients.16 We then dichotomized hospitals into a high‐ or low‐competition category based on the approximate median HHI cut point of 0.34. Teaching status was based on intern/resident‐to‐bed ratio (ie, 0 = nonteaching, 0.010.25 = minor teaching, and >0.25 = major teaching). Location was defined by county location as either urban or nonurban medical service area.
We then analyzed the percentage of hospitals in 2003 and 2004 below the mandated minimum ratios of (1) at least 1 licensed nurse (RN+LVN) per 6 patients effective in 2004, (2) the ratio of 1 (RN+LVN) nurse per 5 patients to be implemented in 2005, (3) the ratio of at least 1 registered nurse (RN only) per 5 patients, and (4) at least 1 nurse (RN+LVN) per 4 patients, as these ratios are under consideration in other states.9, 17 Finally, we examined the trend in nurse staffing ratios from 2003, the pre‐implementation year, to 2004, the post‐implementation year. Data analysis was performed using STATA SE 9.1 (College Station, TX).
RESULTS
Nurse Staffing Trends
The trend in nurse staffing ratios based on licensed nurses (RN + LVN) from 1993 to 2004 is shown in Figure 1, with lines representing the 10th, 25th, 50th (median), and 75th percentiles of hospital nurse staffing ratios. The nurse staffing ratios were essentially flat from 1993 to 1999 without any significant trend. After nurse staffing legislation was passed in 1999, median nurse‐to‐patient ratio rose, with the largest increase from 2003 to the implementation year for staffing ratios, 2004. From 2003 to 2004, the median hospital staffing ratio increased from fewer than 1 nurse per 4 patients to a ratio of more than 1 nurse per 4 patients. The first year that fewer than 25% of hospitals were below the minimum of at least 1 nurse per 5 patients was 2003.
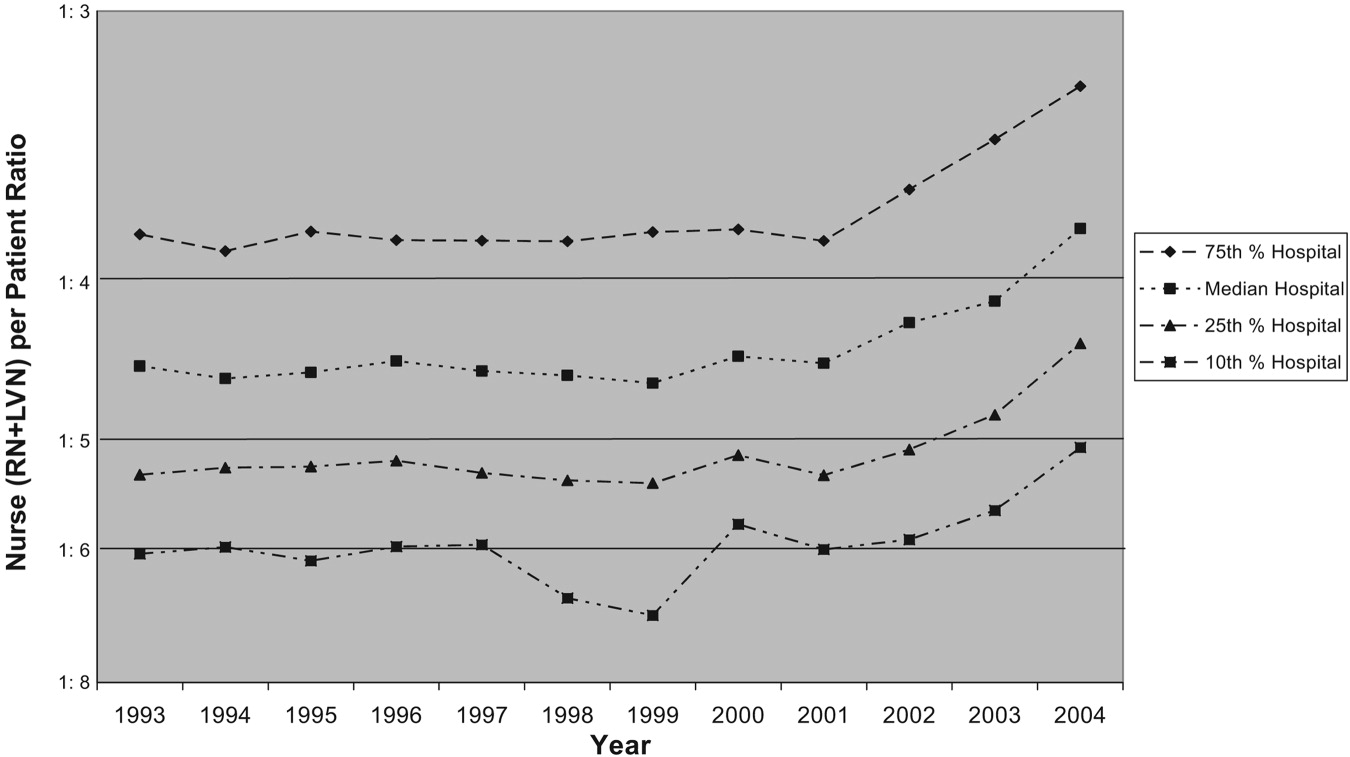
Trends in Nurse Staffing Mix
The legislation in California and the proposed legislation in some other states allow hospitals to meet mandated ratios with both RNs and LVNs or LPNs, that is, with licensed nursing staff. Specifically, California allows up to 50% of nurse staffing ratios to be met by LVN hours. Therefore, we analyzed the overall trend in percentage of nurse staffing hours attributable to LVNs. In 1993, LVNs accounted for 27% of nurse staffing hours. Because of a steady decrease in the proportion of LVNs staffing relative to RNs staffing, LVNs accounted for only 13% of the nurse staffing hours by 2004.
Hospitals Below Implemented and Proposed Ratios
The first column of Table 1 shows the percentage of hospitals of each type in 2003 and 2004 below the mandated ratio of at least 1 licensed nurse (RN+LVN) per 6 patients, which went into effect January 1, 2004. The next column represents the hospitals below the ratio of at least 1 licensed nurse per 5 patients, which was implemented in 2005. The final 2 columns represent ratios that have been considered in other states of at least 1 RN per 5 patients and at least 1 licensed nurse per 4 patients.9, 17 In 2004, only 2.4% of hospitals were below a minimum ratio of at least 1 nurse (RN+LVN) per 6 patients, but 11.4% were below 1:5, 29.5% were below 1 RN per 5 patients, and 40.4% were below at least 1 nurse (RN+LVN) per 4 patients. This demonstrates the substantial increase in the proportion of hospitals that are below minimum ratios as the number of nurses or required training level of nurses is increased.
| <1 Nurse per 6 patients (RN+LVN)* | <1 Nurse per 5 patients (RN+LVN)* | <1 Nurse per 5 patients (RN only)* | <1 Nurse per 4 patients (RN+LVN)* | |||||
|---|---|---|---|---|---|---|---|---|
| 2003 (%) | 2004 (%) | 2003 (%) | 2004 (%) | 2003 (%) | 2004 (%) | 2003 (%) | 2004 (%) | |
| ||||||||
| All hospitals (2003, n = 342; 2004, n = 332) | 5.0% | 2.4% | 19.6% | 11.4% | 39.8 | 29.5% | 53.2% | 40.4% |
| Hospital ownership‖ | ||||||||
| For‐profit (2003, n = 87; 2004, n = 82) | 2.3% | 1.2% | 25.3% | 9.8% | 54.0 | 32.9% | 63.2% | 40.2% |
| Nonprofit (2003, n = 234; 2004, n = 231) | 5.6% | 3.0% | 16.7% | 11.3% | 34.6 | 28.1% | 49.6% | 40.7% |
| Government (2003, n = 21; 2004, n = 19) | 9.5% | 0% | 28.6% | 21.1% | 38.1 | 31.6% | 52.4% | 36.8% |
| More competitive versus less competitive markets‖ | ||||||||
| More competitive (2003, n = 168; 2004, n = 163) | 6.0% | 2.6% | 25.0% | 11.7% | 46.4 | 33.8% | 59.3% | 42.2% |
| Less competitive (2003, n = 174; 2004, n = 169) | 4.0% | 2.2% | 14.4% | 11.2% | 33.3 | 25.8% | 48.3% | 38.8% |
| Teaching status‖ | ||||||||
| No teaching (2003 n = 250; 2004 n = 251) | 5.6% | 2.4% | 20.4% | 12.0% | 42.0% | 30.7% | 56.0% | 41.0% |
| Minor teaching (2003 n = 72; 2004 n = 60) | 2.8% | 3.3% | 18.1% | 10.0% | 36.5% | 28.3% | 48.6% | 41.7% |
| Major teaching (2003 n = 20; 2004 n = 21) | 5.0% | 0% | 15.0% | 9.5% | 20.0% | 19.0% | 35.0% | 28.6% |
| Urban versus nonurban‖ | ||||||||
| Urban (2003 n = 306; 2004 n = 294) | 4.9% | 2.4% | 20.9% | 11.9% | 41.2% | 30.6% | 55.6% | 42.5% |
| Nonurban (2003 n = 36; 2004 n = 38) | 5.6% | 2.6% | 8.3% | 7.9% | 27.8% | 21.1% | 33.3% | 23.7% |
| High versus low Medicaid/uninsured patient population‖ | ||||||||
| High (36%; 2003, n = 65; 2004, n = 60) | 6.2% | 5.0% | 30.8% | 21.7% | 50.8% | 43.3% | 64.6% | 48.7% |
| Low (<36%; 2003, n = 276; 2004, n = 270) | 4.7% | 1.9% | 17.0% | 9.3% | 37.3% | 26.7% | 50.7% | 39.3% |
Nurse Staffing Ratio Changes in First Year of Implementation of Legislation
From 2003 to 2004, there was a decrease in the percentage of hospitals below all the ratios. The absolute decrease was least in the actual mandated ratio in 2004 of at least 1 nurse per 6 patients (5.0% of hospitals below the ratio in 2003 versus 2.4% of hospitals in 2004), and the decrease was greatest in the highest ratio of at least 1 nurse per 4 patients (53.2% versus 40.4%). Although there was a decrease in the percentage of hospitals of all types below the minimum ratios from 2003 to 2004, some hospital types had larger reductions in hospitals below ratios than others. The types of hospitals with the most significant decreases in the percentage below minimum ratios were for‐profit hospitals, hospitals in more competitive markets, nonteaching hospitals, urban hospitals, and non‐safety‐net hospitals with a low percentage of Medicaid/uninsured patients.
Types of Hospitals Below Minimum Ratios
One of the most important considerations is the type of hospital in 2004 below the minimum ratio of at least 1 nurse (RN+LVN) per 5 patients implemented January 1, 2005. The hospital types with the highest percentage of hospitals below the 1:5 ratio were those with a high proportion of Medicaid/uninsured (21.7%), government owned (21.1%), nonteaching (12.0%), urban (11.9%), and in more competitive markets (11.7%). Of note, hospitals with a high proportion of Medicaid/uninsured patients were significantly more likely than hospitals with a low proportion of Medicaid patients to be below minimum ratios. These safety net hospitals also failed to achieve the significant decrease in percentage of hospitals below minimum ratios from 2003 to 2004 that hospitals with a low Medicaid population achieved. There were a total of 38 of 332 hospitals (11.4%) whose ratios were below the minimum of at least 1 nurse (RN+LVN) per 5 patients in 2004 (Table 1). Using the broader definition of hospital safety net, which includes urban nonprofit and government hospitals in addition to those hospitals with a high percentage of Medicaid/uninsured patients, the vast majority of hospitals (84%)32 of 38below the minimum ratio of 1:5 in 2004 were part of the hospital safety net.
DISCUSSION
These data demonstrate that nurse staffing ratios in California were relatively stable from 1993 to 1999. In 1999, law AB 394 with its focus on nurse staffing levels passed, and subsequently, from 1999 to 2004, nurse staffing levels increased significantly, with the largest increase in 2004, the year of implementation. Although multiple factors could account for this trend, a likely cause for the statewide increase in nurse staffing was the anticipation and then implementation of legislation to achieve minimum ratios.
This study had several limitations. The OSHPD data capture nurse staffing on an annual basis, but the California legislation mandated minimum nurse staffing ratios be kept at all times; these data do not capture how often a given hospital was below the minimum ratio on a monthly or shift‐by‐shift basis. These data may overreport nurse staffing hours if they include hours not spent in direct patient care, or they could misrepresent nurse staffing ratios because of poor reporting.
Certain hospitals are more likely to be below mandated ratios. These hospitals are often government owned, in urban areas, and serve a high percentage of Medicaid/uninsured patients. Hospitals with these characteristics are typically considered part of the safety net. These are the hospitals that serve our nation's most vulnerable populations and are likely to struggle disproportionately to meet minimum mandated ratios. As evidence of these precarious finances, 67% of hospitals defined as safety‐net hospitals based on a high percentage of Medicaid/uninsured patients in 2004 had a negative operating margin versus 40% of hospitals not considered to be safety‐net hospitals (P < .001).18 The question remains how hospitals will meet minimum nurse staffing ratios given these tenuous operating margins, as some of the approaches might result in restricted access, reduced services, reduced expenditures on new equipment or technology, or other decisions that might adversely affect quality. These potential tradeoffs will directly affect hospitalists, nurses, and other health care personnel working in hospitals. Because legislation generally does not provide funds or mechanisms to help hospitals meet proposed staffing ratios and there is a national nursing shortage, hospitals may struggle to meet minimum ratios. Cross‐sectional studies have demonstrated a potential link between increased nurse staffing and better patient outcomes,15 but if a financially constrained hospital makes tradeoffs by restricting access to care and services or by diverting funds from other beneficial uses, on balance, mandated nurse staffing ratios may not be beneficial to patients. The potential for unintended but serious negative consequences exists if hospitals in the safety net are mandated to meet minimum nurse staffing ratios without adequate resources.
At all types of hospitals, hospitalists are increasingly becoming responsible for quality improvement programs and outcomes measurement. However, the outcomes of these programs may be strongly influenced by nurse staffing. For example, cross‐sectional studies have demonstrated that increased nurse staffing was associated with decreased mortality, length of stay, failure to rescue from complications, catheter‐associated bloodstream infections, catheter‐associated urinary tract infections, gastrointestinal bleeding, ventilator‐acquired pneumonia, and shock or cardiac arrest.1, 4, 19 These types of quality and patient safety outcomes are likely to be the focus of many hospitalist‐led quality improvement programs and may even be linked to hospitalist compensation. Therefore, hospitals and their hospitalists must take into account the effect that inadequate nurse staffing could have on their patient outcomes while balancing the investment in nurse staffing with other quality improvement investments. An interaction between nurse staffing level and hospitalist staffing may exist, but we are unaware of any published studies investigating this interaction. The nurse burnout documented to be associated with inadequate nurse staffing certainly could affect hospitalists if it increases nurse turnover or inhibits effective communication.1 Additional research is needed to better delineate the effects of nurse staffing, particularly in regard to hospitalists and hospital‐based quality and safety initiatives.
Finally, these data highlight the need for policymakers and hospital administrators to consider whether the aim is to establish a minimal floor or an optimal ratio. California first opted for what many would consider a minimal floor of at least 1 nurse per 6 patients, as only 5% of hospitals were below this ratio in 2003. California then increased the ratio to a 1:5 nurse‐to‐patient ratio, which affected a larger percentage of hospitals, presumably because of a belief that this higher ratio would lead to better outcomes. In addition, some states such as Massachusetts have considered a minimum ratio of 1:4.17 A ratio of 1:4 would require a significant proportion of hospitals to hire more nurses if staffing levels are similar to California. Only a few studies have estimated the cost effectiveness of staffing changes. Based on cross‐sectional data, Needleman et al. estimated that it would cost $8.5 billion nationally to raise all hospitals to the 75th percentile of RN and overall nurse staffing but that this would prevent 70,000 adverse patient outcomes (eg, hospital‐acquired pneumonia). Rothberg et al. estimated that the incremental cost per life saved as a hospital moved from 1 nurse per 8 patients to 1 nurse per 5 patients was $48,100. However, these estimates based on cross‐sectional data fail to inform the debate on optimal nurse staffing ratios. The effect on patient outcomes when hospitals move from 1:6 to 1:5 or 1:4 nurse staffing levels needs to be determined in a longitudinal study. Thus, legislators and hospitals have little to guide them in establishing optimal nurse staffing ratios, and consideration of specific mandated minimum ratios would benefit greatly from comparative information on the cost and quality tradeoffs.
Hospitals, policy makers, health care providers, and researchers are struggling to improve the health care delivered in our hospitals; fortunately, there has been an increased focus on the importance of nurses who deliver medical care on the front lines and are responsible for many aspects of quality. Mandating minimum nurse staffing ratios may seem like an easy fix of the problem; however, we must consider how these ratios can be met, the potential difficulty for hospitals to meet these ratios in the fraying safety net20, and possible unintended negative consequences. Without a mechanism for hospitals to meet ratios, simply mandating a minimum ratio will not necessarily improve care. Hospitalists should be leaders in better understanding the effects of nurse staffing on patient outcomes and quality initiatives in hospitals.
Acknowledgements
We acknowledge the California Office of Statewide Health Planning and Development (OSHPD) for providing the data for this study.
- ,,,,.Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction.JAMA.2002;288:1987–1993.
- ,.Working conditions that support patient safety.J Nurs Care Qual.2005;20:289–292.
- ,,,,.Nurse‐patient ratios: a systematic review on the effects of nurse staffing on patient, nurse employee, and hospital outcomes.J Nurs Adm.2004;34:326–337.
- ,,,,.Nurse‐staffing levels and the quality of care in hospitals.N Engl J Med.2002;346:1715–1722.
- ,,,,.Making health care safer: a critical analysis of patient safety practices.Evid Rep Technol Assess (Summ).2001;43:i–x,1–668.
- Implementation of California's Nurse Staffing Law: History of the Law. Available at: http://www.calhealth.org/public/press/Article%5C113%5CImplementation%20of%20CA%20Nurse%20Ratio%20Law,%20History%20of%20 the%20Law.pdf. Accessed September 5,2007.
- AB 394: California and the Demand for Safe and Effective Nurse to Patient Ratios. Available at: http://www.calnurses.org/research/pdfs/IHSP_AB394_staffing_ratios.pdf. Accessed September 5,2007.
- . Information regarding R‐01‐04E: Licensed Nurse‐to‐Patient Ratio. Available at: http://www.dhs.ca.gov/lnc/pubnotice/NTPR/DADMmemoSupCourtDecision.pdf. Accessed December 3,2006.
- Nationwide State Legislative Agenda: Nurse Staffing Plans and Ratios. Available at: http://www.nursingworld.org/GOVA/state.htm. Accessed April 10,2007.
- Staffing Plans and Ratios. Available at: http://nursingworld.org/MainMenuCategories/ThePracticeofProfessionalNursing/workplace/Workforce/ShortageStaffing/Staffing/staffing12765.aspx. Accessed September 5,2007.
- .California's minimum nurse‐to‐patient ratios: the first few months.J Nurs Adm.2004;34:571–578.
- ,.Addressing measurement error bias in nurse staffing research.Health Serv Res.2006;41:2006–2024.
- Institute of Medicine.America's Health Care Safety Net. Washington, DC;2000.
- ,.Population characteristics of markets of safety‐net and non‐safety‐net hospitals.J Urban Health.1999;76:351–370.
- ,.The evolution of support for safety‐net hospitals.Health Aff (Millwood).1997;16:30–47.
- ,.The effects of hospital competition and the Medicare PPS program on hospital cost behavior in California.J Health Econ.1988;7:301–320.
- Massachusetts Nursing Association. Specific RN‐to‐Patient Ratios. Available at: http://www.massnurses.org/safe_care/ratios.htm. Accessed April 1,2007.
- Office of Statewide Health Planning and Development. Available at: http://www.oshpd.state.ca.us/HQAD/Hospital/financial/hospAF.htm. Accessed May 6,2007.
- ,,, et al.Nurse working conditions and patient safety outcomes.Med Care.2007;45:571–578.
- .By a thread—a fragile, fraying safety net is everybody's problem.Hosp Health Netw.2002;76:32,34–40.
Many studies have reported associations between higher nurse‐to‐patient ratios and decreased mortality and complications. These studies coupled with increasing concern about patient safety, nursing shortages, and nurse burnout have spurred many state legislatures to discuss mandating minimum nurse staffing ratios.15 The California legislature passed law AB394 in 1999, mandating minimum nurse staffing ratios in order to improve patient safety and the nurse work environment. The original implementation date, January 1, 2001, was delayed to allow the California Department of Health Services more time to develop minimum nurse ratios for each unit type.6, 7 California implemented a ratio of at least 1 licensed nurse (RN+LVN) for every 6 patients on general adult medical‐surgical floors on January 1, 2004. This was subsequently increased, on January 1, 2005, to at least 1 licensed nurse for every 5 patients, a ratio that was upheld by the California Supreme Court on March 14, 2005.8
Additional laws regarding nurse staffing are being considered in at least 25 states.9 States have taken 3 main approaches to legislation: mandating nurse staffing ratios for each hospital unit type, requiring hospitals to establish and report nurse staffing plans that typically include ratios, or a combination of mandated ratios and staffing plans.10 This type of legislation would have a major impact on hospitalists, nurses, other health care personnel, hospital administrators, and patients. However, little is known about trends in nurse staffing, how staffing levels vary among hospitals overall, in different markets, and by ownership type and location, and consequently how implementing nurse staffing ratios will affect different types of hospitals, including those that make up the safety net.11
California nurse staffing data are better than many other sources because the state provides nurse staffing hours by unit types in hospitals as opposed to aggregate numbers of nurse hours across an entire hospital or medical center.12 California is also at the forefront of mandated minimum nurse staffing legislation, as it is the only state to have enacted nurse staffing ratio legislation. Examining nurse staffing trends and hospital types currently under mandated or proposed nurse staffing ratios is integral to informing the debate on nurse staffing legislation and its effect on hospitalists. We hypothesized that nurse staffing would increase in California after the legislation was passed in 1999 but that safety‐net hospitals such as those that are urban, government owned, and serving a high percentage of Medicaid and uninsured patients would be more likely to be below minimum ratios.13
MATERIALS AND METHODS
We used hospital financial panel data for 1993 through 2004, the most recent year with complete data, from California's Office of Statewide Health Planning and Development (OSHPD). We included only short‐term acute‐care general hospitals and excluded other hospital types such as long‐term care, children's, and psychiatric hospitals. We investigated staffing of adult general medical‐surgical units and not of other types of units such as intensive care units. The numerator of the staffing variables for each hospital was the combined medical‐surgical productive hours for registered nurses (RNs) and licensed vocational nurses (LVNs), as California allows up to 50% of staffing hours to be LVN hours. Staffing hours of the adult general medical‐surgical units of each hospital are reported on an annual basis. The denominator was total patient days on the acute adult medical‐surgical units of each hospital in a given year. We calculated the number of patients per one nurse by dividing 24 by the nurse hours per patient day (eg, 4.0 nurse hours per patient day is equivalent to a nurse‐to‐patient ratio of 1:6). We did not adjust staffing ratios by the hospital case mix or other factors because the ratio legislation did not take these factors into account.
We further evaluated staffing ratios in 2003 and 2004 based on 5 hospital characteristics: hospital ownership, market competitiveness, teaching status, urban versus rural location, and safety‐net hospitals, using 2 common definitions for the latter. The Institute of Medicine report defines safety‐net providers as those with a substantial share of their patient mix from uninsured and Medicaid populations.13 Safety‐net hospitals have been more specifically defined as short‐term general hospitals whose percentage of Medicaid and uninsured patients is greater than 1 standard deviation above the mean.14 Using this definition, hospitals in California where more than 36% of patients had Medicaid or no insurance in 2004 would be considered safety‐net hospitals. A more comprehensive definition of the hospital safety net that has been used includes urban nonprofit and government hospitals and hospitals with a high percentage of Medicaid/uninsured patients.10, 11, 15 We analyzed nurse staffing ratios using both these definitions. Hospital ownership was designated as for profit, nonprofit, or government owned. Hospital competitiveness was measured using the Hirschman‐Herfindahl Index (HHI), or the sum of squared market shares, a standard approach to defining hospital market competition. Market boundaries were defined as those zip codes from which each hospital draws most of its patients.16 We then dichotomized hospitals into a high‐ or low‐competition category based on the approximate median HHI cut point of 0.34. Teaching status was based on intern/resident‐to‐bed ratio (ie, 0 = nonteaching, 0.010.25 = minor teaching, and >0.25 = major teaching). Location was defined by county location as either urban or nonurban medical service area.
We then analyzed the percentage of hospitals in 2003 and 2004 below the mandated minimum ratios of (1) at least 1 licensed nurse (RN+LVN) per 6 patients effective in 2004, (2) the ratio of 1 (RN+LVN) nurse per 5 patients to be implemented in 2005, (3) the ratio of at least 1 registered nurse (RN only) per 5 patients, and (4) at least 1 nurse (RN+LVN) per 4 patients, as these ratios are under consideration in other states.9, 17 Finally, we examined the trend in nurse staffing ratios from 2003, the pre‐implementation year, to 2004, the post‐implementation year. Data analysis was performed using STATA SE 9.1 (College Station, TX).
RESULTS
Nurse Staffing Trends
The trend in nurse staffing ratios based on licensed nurses (RN + LVN) from 1993 to 2004 is shown in Figure 1, with lines representing the 10th, 25th, 50th (median), and 75th percentiles of hospital nurse staffing ratios. The nurse staffing ratios were essentially flat from 1993 to 1999 without any significant trend. After nurse staffing legislation was passed in 1999, median nurse‐to‐patient ratio rose, with the largest increase from 2003 to the implementation year for staffing ratios, 2004. From 2003 to 2004, the median hospital staffing ratio increased from fewer than 1 nurse per 4 patients to a ratio of more than 1 nurse per 4 patients. The first year that fewer than 25% of hospitals were below the minimum of at least 1 nurse per 5 patients was 2003.
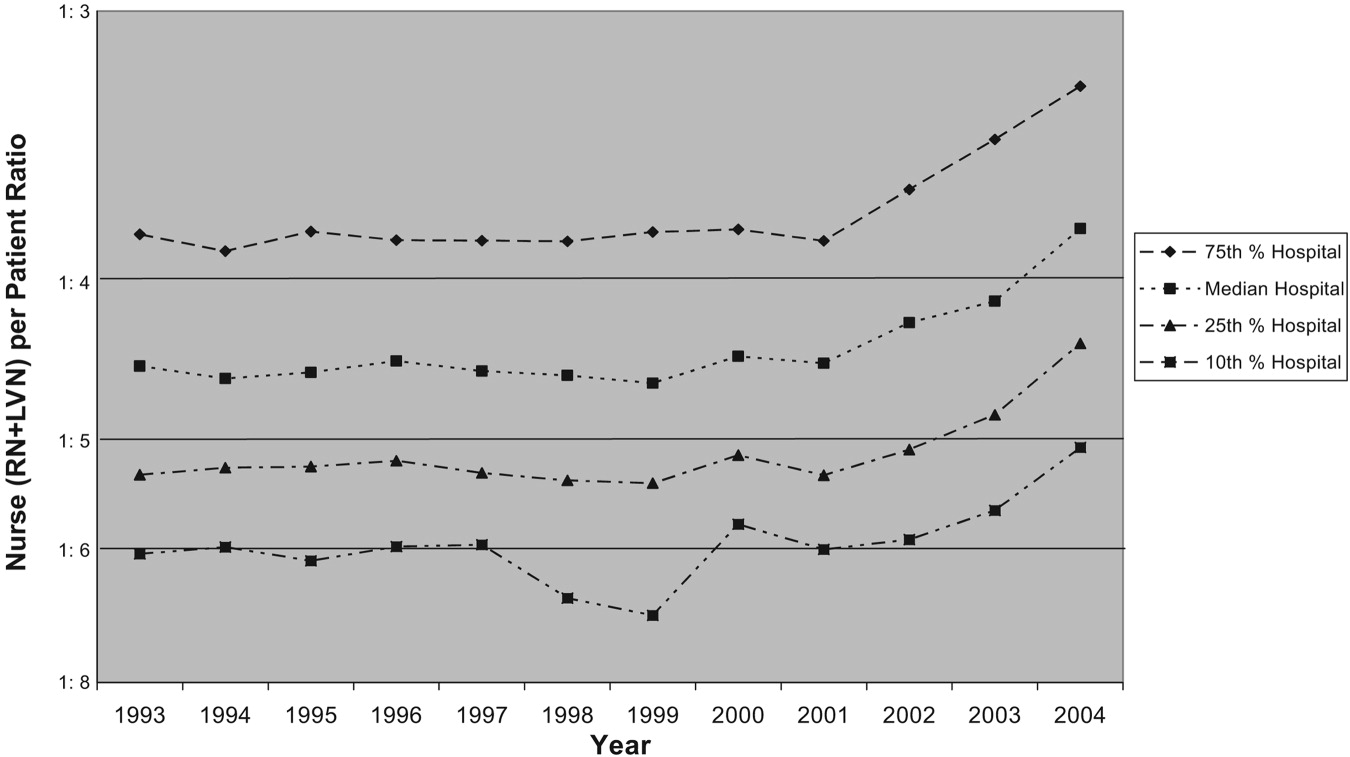
Trends in Nurse Staffing Mix
The legislation in California and the proposed legislation in some other states allow hospitals to meet mandated ratios with both RNs and LVNs or LPNs, that is, with licensed nursing staff. Specifically, California allows up to 50% of nurse staffing ratios to be met by LVN hours. Therefore, we analyzed the overall trend in percentage of nurse staffing hours attributable to LVNs. In 1993, LVNs accounted for 27% of nurse staffing hours. Because of a steady decrease in the proportion of LVNs staffing relative to RNs staffing, LVNs accounted for only 13% of the nurse staffing hours by 2004.
Hospitals Below Implemented and Proposed Ratios
The first column of Table 1 shows the percentage of hospitals of each type in 2003 and 2004 below the mandated ratio of at least 1 licensed nurse (RN+LVN) per 6 patients, which went into effect January 1, 2004. The next column represents the hospitals below the ratio of at least 1 licensed nurse per 5 patients, which was implemented in 2005. The final 2 columns represent ratios that have been considered in other states of at least 1 RN per 5 patients and at least 1 licensed nurse per 4 patients.9, 17 In 2004, only 2.4% of hospitals were below a minimum ratio of at least 1 nurse (RN+LVN) per 6 patients, but 11.4% were below 1:5, 29.5% were below 1 RN per 5 patients, and 40.4% were below at least 1 nurse (RN+LVN) per 4 patients. This demonstrates the substantial increase in the proportion of hospitals that are below minimum ratios as the number of nurses or required training level of nurses is increased.
| <1 Nurse per 6 patients (RN+LVN)* | <1 Nurse per 5 patients (RN+LVN)* | <1 Nurse per 5 patients (RN only)* | <1 Nurse per 4 patients (RN+LVN)* | |||||
|---|---|---|---|---|---|---|---|---|
| 2003 (%) | 2004 (%) | 2003 (%) | 2004 (%) | 2003 (%) | 2004 (%) | 2003 (%) | 2004 (%) | |
| ||||||||
| All hospitals (2003, n = 342; 2004, n = 332) | 5.0% | 2.4% | 19.6% | 11.4% | 39.8 | 29.5% | 53.2% | 40.4% |
| Hospital ownership‖ | ||||||||
| For‐profit (2003, n = 87; 2004, n = 82) | 2.3% | 1.2% | 25.3% | 9.8% | 54.0 | 32.9% | 63.2% | 40.2% |
| Nonprofit (2003, n = 234; 2004, n = 231) | 5.6% | 3.0% | 16.7% | 11.3% | 34.6 | 28.1% | 49.6% | 40.7% |
| Government (2003, n = 21; 2004, n = 19) | 9.5% | 0% | 28.6% | 21.1% | 38.1 | 31.6% | 52.4% | 36.8% |
| More competitive versus less competitive markets‖ | ||||||||
| More competitive (2003, n = 168; 2004, n = 163) | 6.0% | 2.6% | 25.0% | 11.7% | 46.4 | 33.8% | 59.3% | 42.2% |
| Less competitive (2003, n = 174; 2004, n = 169) | 4.0% | 2.2% | 14.4% | 11.2% | 33.3 | 25.8% | 48.3% | 38.8% |
| Teaching status‖ | ||||||||
| No teaching (2003 n = 250; 2004 n = 251) | 5.6% | 2.4% | 20.4% | 12.0% | 42.0% | 30.7% | 56.0% | 41.0% |
| Minor teaching (2003 n = 72; 2004 n = 60) | 2.8% | 3.3% | 18.1% | 10.0% | 36.5% | 28.3% | 48.6% | 41.7% |
| Major teaching (2003 n = 20; 2004 n = 21) | 5.0% | 0% | 15.0% | 9.5% | 20.0% | 19.0% | 35.0% | 28.6% |
| Urban versus nonurban‖ | ||||||||
| Urban (2003 n = 306; 2004 n = 294) | 4.9% | 2.4% | 20.9% | 11.9% | 41.2% | 30.6% | 55.6% | 42.5% |
| Nonurban (2003 n = 36; 2004 n = 38) | 5.6% | 2.6% | 8.3% | 7.9% | 27.8% | 21.1% | 33.3% | 23.7% |
| High versus low Medicaid/uninsured patient population‖ | ||||||||
| High (36%; 2003, n = 65; 2004, n = 60) | 6.2% | 5.0% | 30.8% | 21.7% | 50.8% | 43.3% | 64.6% | 48.7% |
| Low (<36%; 2003, n = 276; 2004, n = 270) | 4.7% | 1.9% | 17.0% | 9.3% | 37.3% | 26.7% | 50.7% | 39.3% |
Nurse Staffing Ratio Changes in First Year of Implementation of Legislation
From 2003 to 2004, there was a decrease in the percentage of hospitals below all the ratios. The absolute decrease was least in the actual mandated ratio in 2004 of at least 1 nurse per 6 patients (5.0% of hospitals below the ratio in 2003 versus 2.4% of hospitals in 2004), and the decrease was greatest in the highest ratio of at least 1 nurse per 4 patients (53.2% versus 40.4%). Although there was a decrease in the percentage of hospitals of all types below the minimum ratios from 2003 to 2004, some hospital types had larger reductions in hospitals below ratios than others. The types of hospitals with the most significant decreases in the percentage below minimum ratios were for‐profit hospitals, hospitals in more competitive markets, nonteaching hospitals, urban hospitals, and non‐safety‐net hospitals with a low percentage of Medicaid/uninsured patients.
Types of Hospitals Below Minimum Ratios
One of the most important considerations is the type of hospital in 2004 below the minimum ratio of at least 1 nurse (RN+LVN) per 5 patients implemented January 1, 2005. The hospital types with the highest percentage of hospitals below the 1:5 ratio were those with a high proportion of Medicaid/uninsured (21.7%), government owned (21.1%), nonteaching (12.0%), urban (11.9%), and in more competitive markets (11.7%). Of note, hospitals with a high proportion of Medicaid/uninsured patients were significantly more likely than hospitals with a low proportion of Medicaid patients to be below minimum ratios. These safety net hospitals also failed to achieve the significant decrease in percentage of hospitals below minimum ratios from 2003 to 2004 that hospitals with a low Medicaid population achieved. There were a total of 38 of 332 hospitals (11.4%) whose ratios were below the minimum of at least 1 nurse (RN+LVN) per 5 patients in 2004 (Table 1). Using the broader definition of hospital safety net, which includes urban nonprofit and government hospitals in addition to those hospitals with a high percentage of Medicaid/uninsured patients, the vast majority of hospitals (84%)32 of 38below the minimum ratio of 1:5 in 2004 were part of the hospital safety net.
DISCUSSION
These data demonstrate that nurse staffing ratios in California were relatively stable from 1993 to 1999. In 1999, law AB 394 with its focus on nurse staffing levels passed, and subsequently, from 1999 to 2004, nurse staffing levels increased significantly, with the largest increase in 2004, the year of implementation. Although multiple factors could account for this trend, a likely cause for the statewide increase in nurse staffing was the anticipation and then implementation of legislation to achieve minimum ratios.
This study had several limitations. The OSHPD data capture nurse staffing on an annual basis, but the California legislation mandated minimum nurse staffing ratios be kept at all times; these data do not capture how often a given hospital was below the minimum ratio on a monthly or shift‐by‐shift basis. These data may overreport nurse staffing hours if they include hours not spent in direct patient care, or they could misrepresent nurse staffing ratios because of poor reporting.
Certain hospitals are more likely to be below mandated ratios. These hospitals are often government owned, in urban areas, and serve a high percentage of Medicaid/uninsured patients. Hospitals with these characteristics are typically considered part of the safety net. These are the hospitals that serve our nation's most vulnerable populations and are likely to struggle disproportionately to meet minimum mandated ratios. As evidence of these precarious finances, 67% of hospitals defined as safety‐net hospitals based on a high percentage of Medicaid/uninsured patients in 2004 had a negative operating margin versus 40% of hospitals not considered to be safety‐net hospitals (P < .001).18 The question remains how hospitals will meet minimum nurse staffing ratios given these tenuous operating margins, as some of the approaches might result in restricted access, reduced services, reduced expenditures on new equipment or technology, or other decisions that might adversely affect quality. These potential tradeoffs will directly affect hospitalists, nurses, and other health care personnel working in hospitals. Because legislation generally does not provide funds or mechanisms to help hospitals meet proposed staffing ratios and there is a national nursing shortage, hospitals may struggle to meet minimum ratios. Cross‐sectional studies have demonstrated a potential link between increased nurse staffing and better patient outcomes,15 but if a financially constrained hospital makes tradeoffs by restricting access to care and services or by diverting funds from other beneficial uses, on balance, mandated nurse staffing ratios may not be beneficial to patients. The potential for unintended but serious negative consequences exists if hospitals in the safety net are mandated to meet minimum nurse staffing ratios without adequate resources.
At all types of hospitals, hospitalists are increasingly becoming responsible for quality improvement programs and outcomes measurement. However, the outcomes of these programs may be strongly influenced by nurse staffing. For example, cross‐sectional studies have demonstrated that increased nurse staffing was associated with decreased mortality, length of stay, failure to rescue from complications, catheter‐associated bloodstream infections, catheter‐associated urinary tract infections, gastrointestinal bleeding, ventilator‐acquired pneumonia, and shock or cardiac arrest.1, 4, 19 These types of quality and patient safety outcomes are likely to be the focus of many hospitalist‐led quality improvement programs and may even be linked to hospitalist compensation. Therefore, hospitals and their hospitalists must take into account the effect that inadequate nurse staffing could have on their patient outcomes while balancing the investment in nurse staffing with other quality improvement investments. An interaction between nurse staffing level and hospitalist staffing may exist, but we are unaware of any published studies investigating this interaction. The nurse burnout documented to be associated with inadequate nurse staffing certainly could affect hospitalists if it increases nurse turnover or inhibits effective communication.1 Additional research is needed to better delineate the effects of nurse staffing, particularly in regard to hospitalists and hospital‐based quality and safety initiatives.
Finally, these data highlight the need for policymakers and hospital administrators to consider whether the aim is to establish a minimal floor or an optimal ratio. California first opted for what many would consider a minimal floor of at least 1 nurse per 6 patients, as only 5% of hospitals were below this ratio in 2003. California then increased the ratio to a 1:5 nurse‐to‐patient ratio, which affected a larger percentage of hospitals, presumably because of a belief that this higher ratio would lead to better outcomes. In addition, some states such as Massachusetts have considered a minimum ratio of 1:4.17 A ratio of 1:4 would require a significant proportion of hospitals to hire more nurses if staffing levels are similar to California. Only a few studies have estimated the cost effectiveness of staffing changes. Based on cross‐sectional data, Needleman et al. estimated that it would cost $8.5 billion nationally to raise all hospitals to the 75th percentile of RN and overall nurse staffing but that this would prevent 70,000 adverse patient outcomes (eg, hospital‐acquired pneumonia). Rothberg et al. estimated that the incremental cost per life saved as a hospital moved from 1 nurse per 8 patients to 1 nurse per 5 patients was $48,100. However, these estimates based on cross‐sectional data fail to inform the debate on optimal nurse staffing ratios. The effect on patient outcomes when hospitals move from 1:6 to 1:5 or 1:4 nurse staffing levels needs to be determined in a longitudinal study. Thus, legislators and hospitals have little to guide them in establishing optimal nurse staffing ratios, and consideration of specific mandated minimum ratios would benefit greatly from comparative information on the cost and quality tradeoffs.
Hospitals, policy makers, health care providers, and researchers are struggling to improve the health care delivered in our hospitals; fortunately, there has been an increased focus on the importance of nurses who deliver medical care on the front lines and are responsible for many aspects of quality. Mandating minimum nurse staffing ratios may seem like an easy fix of the problem; however, we must consider how these ratios can be met, the potential difficulty for hospitals to meet these ratios in the fraying safety net20, and possible unintended negative consequences. Without a mechanism for hospitals to meet ratios, simply mandating a minimum ratio will not necessarily improve care. Hospitalists should be leaders in better understanding the effects of nurse staffing on patient outcomes and quality initiatives in hospitals.
Acknowledgements
We acknowledge the California Office of Statewide Health Planning and Development (OSHPD) for providing the data for this study.
Many studies have reported associations between higher nurse‐to‐patient ratios and decreased mortality and complications. These studies coupled with increasing concern about patient safety, nursing shortages, and nurse burnout have spurred many state legislatures to discuss mandating minimum nurse staffing ratios.15 The California legislature passed law AB394 in 1999, mandating minimum nurse staffing ratios in order to improve patient safety and the nurse work environment. The original implementation date, January 1, 2001, was delayed to allow the California Department of Health Services more time to develop minimum nurse ratios for each unit type.6, 7 California implemented a ratio of at least 1 licensed nurse (RN+LVN) for every 6 patients on general adult medical‐surgical floors on January 1, 2004. This was subsequently increased, on January 1, 2005, to at least 1 licensed nurse for every 5 patients, a ratio that was upheld by the California Supreme Court on March 14, 2005.8
Additional laws regarding nurse staffing are being considered in at least 25 states.9 States have taken 3 main approaches to legislation: mandating nurse staffing ratios for each hospital unit type, requiring hospitals to establish and report nurse staffing plans that typically include ratios, or a combination of mandated ratios and staffing plans.10 This type of legislation would have a major impact on hospitalists, nurses, other health care personnel, hospital administrators, and patients. However, little is known about trends in nurse staffing, how staffing levels vary among hospitals overall, in different markets, and by ownership type and location, and consequently how implementing nurse staffing ratios will affect different types of hospitals, including those that make up the safety net.11
California nurse staffing data are better than many other sources because the state provides nurse staffing hours by unit types in hospitals as opposed to aggregate numbers of nurse hours across an entire hospital or medical center.12 California is also at the forefront of mandated minimum nurse staffing legislation, as it is the only state to have enacted nurse staffing ratio legislation. Examining nurse staffing trends and hospital types currently under mandated or proposed nurse staffing ratios is integral to informing the debate on nurse staffing legislation and its effect on hospitalists. We hypothesized that nurse staffing would increase in California after the legislation was passed in 1999 but that safety‐net hospitals such as those that are urban, government owned, and serving a high percentage of Medicaid and uninsured patients would be more likely to be below minimum ratios.13
MATERIALS AND METHODS
We used hospital financial panel data for 1993 through 2004, the most recent year with complete data, from California's Office of Statewide Health Planning and Development (OSHPD). We included only short‐term acute‐care general hospitals and excluded other hospital types such as long‐term care, children's, and psychiatric hospitals. We investigated staffing of adult general medical‐surgical units and not of other types of units such as intensive care units. The numerator of the staffing variables for each hospital was the combined medical‐surgical productive hours for registered nurses (RNs) and licensed vocational nurses (LVNs), as California allows up to 50% of staffing hours to be LVN hours. Staffing hours of the adult general medical‐surgical units of each hospital are reported on an annual basis. The denominator was total patient days on the acute adult medical‐surgical units of each hospital in a given year. We calculated the number of patients per one nurse by dividing 24 by the nurse hours per patient day (eg, 4.0 nurse hours per patient day is equivalent to a nurse‐to‐patient ratio of 1:6). We did not adjust staffing ratios by the hospital case mix or other factors because the ratio legislation did not take these factors into account.
We further evaluated staffing ratios in 2003 and 2004 based on 5 hospital characteristics: hospital ownership, market competitiveness, teaching status, urban versus rural location, and safety‐net hospitals, using 2 common definitions for the latter. The Institute of Medicine report defines safety‐net providers as those with a substantial share of their patient mix from uninsured and Medicaid populations.13 Safety‐net hospitals have been more specifically defined as short‐term general hospitals whose percentage of Medicaid and uninsured patients is greater than 1 standard deviation above the mean.14 Using this definition, hospitals in California where more than 36% of patients had Medicaid or no insurance in 2004 would be considered safety‐net hospitals. A more comprehensive definition of the hospital safety net that has been used includes urban nonprofit and government hospitals and hospitals with a high percentage of Medicaid/uninsured patients.10, 11, 15 We analyzed nurse staffing ratios using both these definitions. Hospital ownership was designated as for profit, nonprofit, or government owned. Hospital competitiveness was measured using the Hirschman‐Herfindahl Index (HHI), or the sum of squared market shares, a standard approach to defining hospital market competition. Market boundaries were defined as those zip codes from which each hospital draws most of its patients.16 We then dichotomized hospitals into a high‐ or low‐competition category based on the approximate median HHI cut point of 0.34. Teaching status was based on intern/resident‐to‐bed ratio (ie, 0 = nonteaching, 0.010.25 = minor teaching, and >0.25 = major teaching). Location was defined by county location as either urban or nonurban medical service area.
We then analyzed the percentage of hospitals in 2003 and 2004 below the mandated minimum ratios of (1) at least 1 licensed nurse (RN+LVN) per 6 patients effective in 2004, (2) the ratio of 1 (RN+LVN) nurse per 5 patients to be implemented in 2005, (3) the ratio of at least 1 registered nurse (RN only) per 5 patients, and (4) at least 1 nurse (RN+LVN) per 4 patients, as these ratios are under consideration in other states.9, 17 Finally, we examined the trend in nurse staffing ratios from 2003, the pre‐implementation year, to 2004, the post‐implementation year. Data analysis was performed using STATA SE 9.1 (College Station, TX).
RESULTS
Nurse Staffing Trends
The trend in nurse staffing ratios based on licensed nurses (RN + LVN) from 1993 to 2004 is shown in Figure 1, with lines representing the 10th, 25th, 50th (median), and 75th percentiles of hospital nurse staffing ratios. The nurse staffing ratios were essentially flat from 1993 to 1999 without any significant trend. After nurse staffing legislation was passed in 1999, median nurse‐to‐patient ratio rose, with the largest increase from 2003 to the implementation year for staffing ratios, 2004. From 2003 to 2004, the median hospital staffing ratio increased from fewer than 1 nurse per 4 patients to a ratio of more than 1 nurse per 4 patients. The first year that fewer than 25% of hospitals were below the minimum of at least 1 nurse per 5 patients was 2003.
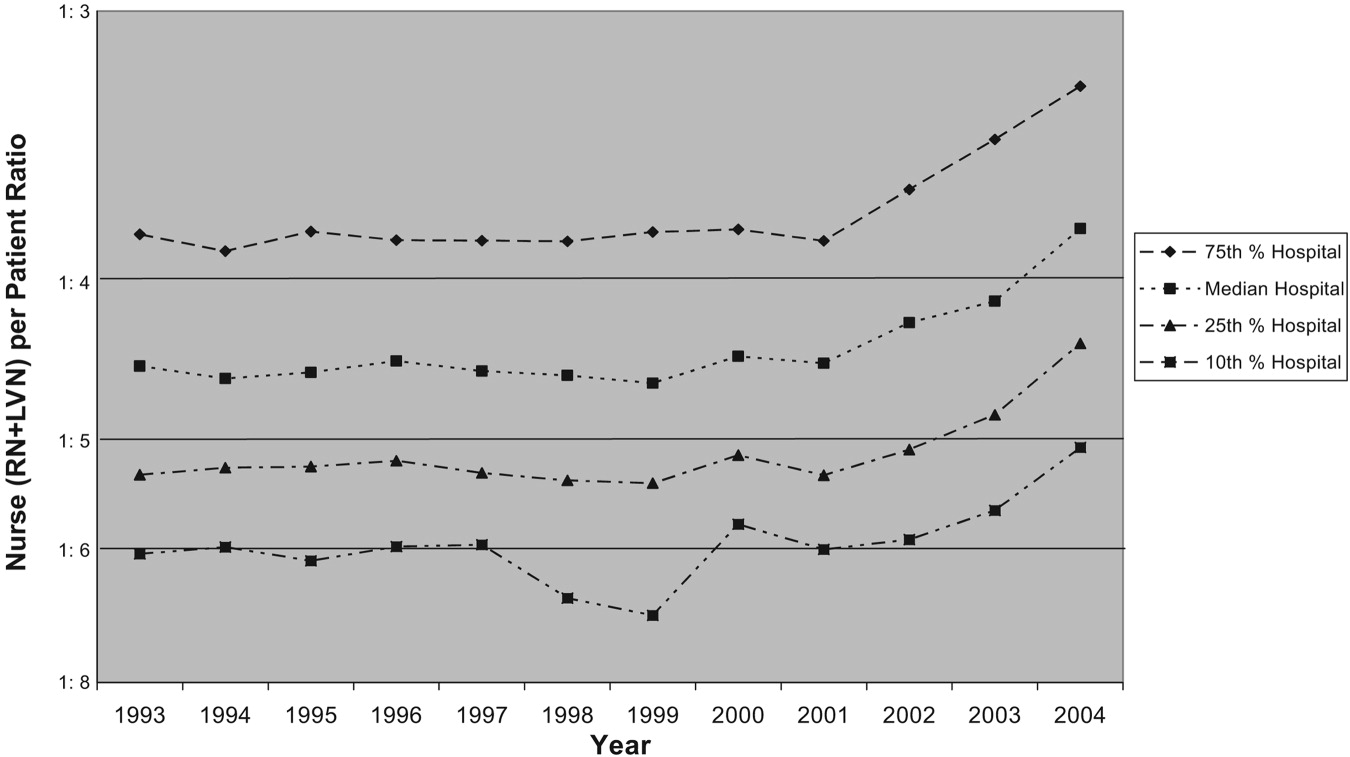
Trends in Nurse Staffing Mix
The legislation in California and the proposed legislation in some other states allow hospitals to meet mandated ratios with both RNs and LVNs or LPNs, that is, with licensed nursing staff. Specifically, California allows up to 50% of nurse staffing ratios to be met by LVN hours. Therefore, we analyzed the overall trend in percentage of nurse staffing hours attributable to LVNs. In 1993, LVNs accounted for 27% of nurse staffing hours. Because of a steady decrease in the proportion of LVNs staffing relative to RNs staffing, LVNs accounted for only 13% of the nurse staffing hours by 2004.
Hospitals Below Implemented and Proposed Ratios
The first column of Table 1 shows the percentage of hospitals of each type in 2003 and 2004 below the mandated ratio of at least 1 licensed nurse (RN+LVN) per 6 patients, which went into effect January 1, 2004. The next column represents the hospitals below the ratio of at least 1 licensed nurse per 5 patients, which was implemented in 2005. The final 2 columns represent ratios that have been considered in other states of at least 1 RN per 5 patients and at least 1 licensed nurse per 4 patients.9, 17 In 2004, only 2.4% of hospitals were below a minimum ratio of at least 1 nurse (RN+LVN) per 6 patients, but 11.4% were below 1:5, 29.5% were below 1 RN per 5 patients, and 40.4% were below at least 1 nurse (RN+LVN) per 4 patients. This demonstrates the substantial increase in the proportion of hospitals that are below minimum ratios as the number of nurses or required training level of nurses is increased.
| <1 Nurse per 6 patients (RN+LVN)* | <1 Nurse per 5 patients (RN+LVN)* | <1 Nurse per 5 patients (RN only)* | <1 Nurse per 4 patients (RN+LVN)* | |||||
|---|---|---|---|---|---|---|---|---|
| 2003 (%) | 2004 (%) | 2003 (%) | 2004 (%) | 2003 (%) | 2004 (%) | 2003 (%) | 2004 (%) | |
| ||||||||
| All hospitals (2003, n = 342; 2004, n = 332) | 5.0% | 2.4% | 19.6% | 11.4% | 39.8 | 29.5% | 53.2% | 40.4% |
| Hospital ownership‖ | ||||||||
| For‐profit (2003, n = 87; 2004, n = 82) | 2.3% | 1.2% | 25.3% | 9.8% | 54.0 | 32.9% | 63.2% | 40.2% |
| Nonprofit (2003, n = 234; 2004, n = 231) | 5.6% | 3.0% | 16.7% | 11.3% | 34.6 | 28.1% | 49.6% | 40.7% |
| Government (2003, n = 21; 2004, n = 19) | 9.5% | 0% | 28.6% | 21.1% | 38.1 | 31.6% | 52.4% | 36.8% |
| More competitive versus less competitive markets‖ | ||||||||
| More competitive (2003, n = 168; 2004, n = 163) | 6.0% | 2.6% | 25.0% | 11.7% | 46.4 | 33.8% | 59.3% | 42.2% |
| Less competitive (2003, n = 174; 2004, n = 169) | 4.0% | 2.2% | 14.4% | 11.2% | 33.3 | 25.8% | 48.3% | 38.8% |
| Teaching status‖ | ||||||||
| No teaching (2003 n = 250; 2004 n = 251) | 5.6% | 2.4% | 20.4% | 12.0% | 42.0% | 30.7% | 56.0% | 41.0% |
| Minor teaching (2003 n = 72; 2004 n = 60) | 2.8% | 3.3% | 18.1% | 10.0% | 36.5% | 28.3% | 48.6% | 41.7% |
| Major teaching (2003 n = 20; 2004 n = 21) | 5.0% | 0% | 15.0% | 9.5% | 20.0% | 19.0% | 35.0% | 28.6% |
| Urban versus nonurban‖ | ||||||||
| Urban (2003 n = 306; 2004 n = 294) | 4.9% | 2.4% | 20.9% | 11.9% | 41.2% | 30.6% | 55.6% | 42.5% |
| Nonurban (2003 n = 36; 2004 n = 38) | 5.6% | 2.6% | 8.3% | 7.9% | 27.8% | 21.1% | 33.3% | 23.7% |
| High versus low Medicaid/uninsured patient population‖ | ||||||||
| High (36%; 2003, n = 65; 2004, n = 60) | 6.2% | 5.0% | 30.8% | 21.7% | 50.8% | 43.3% | 64.6% | 48.7% |
| Low (<36%; 2003, n = 276; 2004, n = 270) | 4.7% | 1.9% | 17.0% | 9.3% | 37.3% | 26.7% | 50.7% | 39.3% |
Nurse Staffing Ratio Changes in First Year of Implementation of Legislation
From 2003 to 2004, there was a decrease in the percentage of hospitals below all the ratios. The absolute decrease was least in the actual mandated ratio in 2004 of at least 1 nurse per 6 patients (5.0% of hospitals below the ratio in 2003 versus 2.4% of hospitals in 2004), and the decrease was greatest in the highest ratio of at least 1 nurse per 4 patients (53.2% versus 40.4%). Although there was a decrease in the percentage of hospitals of all types below the minimum ratios from 2003 to 2004, some hospital types had larger reductions in hospitals below ratios than others. The types of hospitals with the most significant decreases in the percentage below minimum ratios were for‐profit hospitals, hospitals in more competitive markets, nonteaching hospitals, urban hospitals, and non‐safety‐net hospitals with a low percentage of Medicaid/uninsured patients.
Types of Hospitals Below Minimum Ratios
One of the most important considerations is the type of hospital in 2004 below the minimum ratio of at least 1 nurse (RN+LVN) per 5 patients implemented January 1, 2005. The hospital types with the highest percentage of hospitals below the 1:5 ratio were those with a high proportion of Medicaid/uninsured (21.7%), government owned (21.1%), nonteaching (12.0%), urban (11.9%), and in more competitive markets (11.7%). Of note, hospitals with a high proportion of Medicaid/uninsured patients were significantly more likely than hospitals with a low proportion of Medicaid patients to be below minimum ratios. These safety net hospitals also failed to achieve the significant decrease in percentage of hospitals below minimum ratios from 2003 to 2004 that hospitals with a low Medicaid population achieved. There were a total of 38 of 332 hospitals (11.4%) whose ratios were below the minimum of at least 1 nurse (RN+LVN) per 5 patients in 2004 (Table 1). Using the broader definition of hospital safety net, which includes urban nonprofit and government hospitals in addition to those hospitals with a high percentage of Medicaid/uninsured patients, the vast majority of hospitals (84%)32 of 38below the minimum ratio of 1:5 in 2004 were part of the hospital safety net.
DISCUSSION
These data demonstrate that nurse staffing ratios in California were relatively stable from 1993 to 1999. In 1999, law AB 394 with its focus on nurse staffing levels passed, and subsequently, from 1999 to 2004, nurse staffing levels increased significantly, with the largest increase in 2004, the year of implementation. Although multiple factors could account for this trend, a likely cause for the statewide increase in nurse staffing was the anticipation and then implementation of legislation to achieve minimum ratios.
This study had several limitations. The OSHPD data capture nurse staffing on an annual basis, but the California legislation mandated minimum nurse staffing ratios be kept at all times; these data do not capture how often a given hospital was below the minimum ratio on a monthly or shift‐by‐shift basis. These data may overreport nurse staffing hours if they include hours not spent in direct patient care, or they could misrepresent nurse staffing ratios because of poor reporting.
Certain hospitals are more likely to be below mandated ratios. These hospitals are often government owned, in urban areas, and serve a high percentage of Medicaid/uninsured patients. Hospitals with these characteristics are typically considered part of the safety net. These are the hospitals that serve our nation's most vulnerable populations and are likely to struggle disproportionately to meet minimum mandated ratios. As evidence of these precarious finances, 67% of hospitals defined as safety‐net hospitals based on a high percentage of Medicaid/uninsured patients in 2004 had a negative operating margin versus 40% of hospitals not considered to be safety‐net hospitals (P < .001).18 The question remains how hospitals will meet minimum nurse staffing ratios given these tenuous operating margins, as some of the approaches might result in restricted access, reduced services, reduced expenditures on new equipment or technology, or other decisions that might adversely affect quality. These potential tradeoffs will directly affect hospitalists, nurses, and other health care personnel working in hospitals. Because legislation generally does not provide funds or mechanisms to help hospitals meet proposed staffing ratios and there is a national nursing shortage, hospitals may struggle to meet minimum ratios. Cross‐sectional studies have demonstrated a potential link between increased nurse staffing and better patient outcomes,15 but if a financially constrained hospital makes tradeoffs by restricting access to care and services or by diverting funds from other beneficial uses, on balance, mandated nurse staffing ratios may not be beneficial to patients. The potential for unintended but serious negative consequences exists if hospitals in the safety net are mandated to meet minimum nurse staffing ratios without adequate resources.
At all types of hospitals, hospitalists are increasingly becoming responsible for quality improvement programs and outcomes measurement. However, the outcomes of these programs may be strongly influenced by nurse staffing. For example, cross‐sectional studies have demonstrated that increased nurse staffing was associated with decreased mortality, length of stay, failure to rescue from complications, catheter‐associated bloodstream infections, catheter‐associated urinary tract infections, gastrointestinal bleeding, ventilator‐acquired pneumonia, and shock or cardiac arrest.1, 4, 19 These types of quality and patient safety outcomes are likely to be the focus of many hospitalist‐led quality improvement programs and may even be linked to hospitalist compensation. Therefore, hospitals and their hospitalists must take into account the effect that inadequate nurse staffing could have on their patient outcomes while balancing the investment in nurse staffing with other quality improvement investments. An interaction between nurse staffing level and hospitalist staffing may exist, but we are unaware of any published studies investigating this interaction. The nurse burnout documented to be associated with inadequate nurse staffing certainly could affect hospitalists if it increases nurse turnover or inhibits effective communication.1 Additional research is needed to better delineate the effects of nurse staffing, particularly in regard to hospitalists and hospital‐based quality and safety initiatives.
Finally, these data highlight the need for policymakers and hospital administrators to consider whether the aim is to establish a minimal floor or an optimal ratio. California first opted for what many would consider a minimal floor of at least 1 nurse per 6 patients, as only 5% of hospitals were below this ratio in 2003. California then increased the ratio to a 1:5 nurse‐to‐patient ratio, which affected a larger percentage of hospitals, presumably because of a belief that this higher ratio would lead to better outcomes. In addition, some states such as Massachusetts have considered a minimum ratio of 1:4.17 A ratio of 1:4 would require a significant proportion of hospitals to hire more nurses if staffing levels are similar to California. Only a few studies have estimated the cost effectiveness of staffing changes. Based on cross‐sectional data, Needleman et al. estimated that it would cost $8.5 billion nationally to raise all hospitals to the 75th percentile of RN and overall nurse staffing but that this would prevent 70,000 adverse patient outcomes (eg, hospital‐acquired pneumonia). Rothberg et al. estimated that the incremental cost per life saved as a hospital moved from 1 nurse per 8 patients to 1 nurse per 5 patients was $48,100. However, these estimates based on cross‐sectional data fail to inform the debate on optimal nurse staffing ratios. The effect on patient outcomes when hospitals move from 1:6 to 1:5 or 1:4 nurse staffing levels needs to be determined in a longitudinal study. Thus, legislators and hospitals have little to guide them in establishing optimal nurse staffing ratios, and consideration of specific mandated minimum ratios would benefit greatly from comparative information on the cost and quality tradeoffs.
Hospitals, policy makers, health care providers, and researchers are struggling to improve the health care delivered in our hospitals; fortunately, there has been an increased focus on the importance of nurses who deliver medical care on the front lines and are responsible for many aspects of quality. Mandating minimum nurse staffing ratios may seem like an easy fix of the problem; however, we must consider how these ratios can be met, the potential difficulty for hospitals to meet these ratios in the fraying safety net20, and possible unintended negative consequences. Without a mechanism for hospitals to meet ratios, simply mandating a minimum ratio will not necessarily improve care. Hospitalists should be leaders in better understanding the effects of nurse staffing on patient outcomes and quality initiatives in hospitals.
Acknowledgements
We acknowledge the California Office of Statewide Health Planning and Development (OSHPD) for providing the data for this study.
- ,,,,.Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction.JAMA.2002;288:1987–1993.
- ,.Working conditions that support patient safety.J Nurs Care Qual.2005;20:289–292.
- ,,,,.Nurse‐patient ratios: a systematic review on the effects of nurse staffing on patient, nurse employee, and hospital outcomes.J Nurs Adm.2004;34:326–337.
- ,,,,.Nurse‐staffing levels and the quality of care in hospitals.N Engl J Med.2002;346:1715–1722.
- ,,,,.Making health care safer: a critical analysis of patient safety practices.Evid Rep Technol Assess (Summ).2001;43:i–x,1–668.
- Implementation of California's Nurse Staffing Law: History of the Law. Available at: http://www.calhealth.org/public/press/Article%5C113%5CImplementation%20of%20CA%20Nurse%20Ratio%20Law,%20History%20of%20 the%20Law.pdf. Accessed September 5,2007.
- AB 394: California and the Demand for Safe and Effective Nurse to Patient Ratios. Available at: http://www.calnurses.org/research/pdfs/IHSP_AB394_staffing_ratios.pdf. Accessed September 5,2007.
- . Information regarding R‐01‐04E: Licensed Nurse‐to‐Patient Ratio. Available at: http://www.dhs.ca.gov/lnc/pubnotice/NTPR/DADMmemoSupCourtDecision.pdf. Accessed December 3,2006.
- Nationwide State Legislative Agenda: Nurse Staffing Plans and Ratios. Available at: http://www.nursingworld.org/GOVA/state.htm. Accessed April 10,2007.
- Staffing Plans and Ratios. Available at: http://nursingworld.org/MainMenuCategories/ThePracticeofProfessionalNursing/workplace/Workforce/ShortageStaffing/Staffing/staffing12765.aspx. Accessed September 5,2007.
- .California's minimum nurse‐to‐patient ratios: the first few months.J Nurs Adm.2004;34:571–578.
- ,.Addressing measurement error bias in nurse staffing research.Health Serv Res.2006;41:2006–2024.
- Institute of Medicine.America's Health Care Safety Net. Washington, DC;2000.
- ,.Population characteristics of markets of safety‐net and non‐safety‐net hospitals.J Urban Health.1999;76:351–370.
- ,.The evolution of support for safety‐net hospitals.Health Aff (Millwood).1997;16:30–47.
- ,.The effects of hospital competition and the Medicare PPS program on hospital cost behavior in California.J Health Econ.1988;7:301–320.
- Massachusetts Nursing Association. Specific RN‐to‐Patient Ratios. Available at: http://www.massnurses.org/safe_care/ratios.htm. Accessed April 1,2007.
- Office of Statewide Health Planning and Development. Available at: http://www.oshpd.state.ca.us/HQAD/Hospital/financial/hospAF.htm. Accessed May 6,2007.
- ,,, et al.Nurse working conditions and patient safety outcomes.Med Care.2007;45:571–578.
- .By a thread—a fragile, fraying safety net is everybody's problem.Hosp Health Netw.2002;76:32,34–40.
- ,,,,.Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction.JAMA.2002;288:1987–1993.
- ,.Working conditions that support patient safety.J Nurs Care Qual.2005;20:289–292.
- ,,,,.Nurse‐patient ratios: a systematic review on the effects of nurse staffing on patient, nurse employee, and hospital outcomes.J Nurs Adm.2004;34:326–337.
- ,,,,.Nurse‐staffing levels and the quality of care in hospitals.N Engl J Med.2002;346:1715–1722.
- ,,,,.Making health care safer: a critical analysis of patient safety practices.Evid Rep Technol Assess (Summ).2001;43:i–x,1–668.
- Implementation of California's Nurse Staffing Law: History of the Law. Available at: http://www.calhealth.org/public/press/Article%5C113%5CImplementation%20of%20CA%20Nurse%20Ratio%20Law,%20History%20of%20 the%20Law.pdf. Accessed September 5,2007.
- AB 394: California and the Demand for Safe and Effective Nurse to Patient Ratios. Available at: http://www.calnurses.org/research/pdfs/IHSP_AB394_staffing_ratios.pdf. Accessed September 5,2007.
- . Information regarding R‐01‐04E: Licensed Nurse‐to‐Patient Ratio. Available at: http://www.dhs.ca.gov/lnc/pubnotice/NTPR/DADMmemoSupCourtDecision.pdf. Accessed December 3,2006.
- Nationwide State Legislative Agenda: Nurse Staffing Plans and Ratios. Available at: http://www.nursingworld.org/GOVA/state.htm. Accessed April 10,2007.
- Staffing Plans and Ratios. Available at: http://nursingworld.org/MainMenuCategories/ThePracticeofProfessionalNursing/workplace/Workforce/ShortageStaffing/Staffing/staffing12765.aspx. Accessed September 5,2007.
- .California's minimum nurse‐to‐patient ratios: the first few months.J Nurs Adm.2004;34:571–578.
- ,.Addressing measurement error bias in nurse staffing research.Health Serv Res.2006;41:2006–2024.
- Institute of Medicine.America's Health Care Safety Net. Washington, DC;2000.
- ,.Population characteristics of markets of safety‐net and non‐safety‐net hospitals.J Urban Health.1999;76:351–370.
- ,.The evolution of support for safety‐net hospitals.Health Aff (Millwood).1997;16:30–47.
- ,.The effects of hospital competition and the Medicare PPS program on hospital cost behavior in California.J Health Econ.1988;7:301–320.
- Massachusetts Nursing Association. Specific RN‐to‐Patient Ratios. Available at: http://www.massnurses.org/safe_care/ratios.htm. Accessed April 1,2007.
- Office of Statewide Health Planning and Development. Available at: http://www.oshpd.state.ca.us/HQAD/Hospital/financial/hospAF.htm. Accessed May 6,2007.
- ,,, et al.Nurse working conditions and patient safety outcomes.Med Care.2007;45:571–578.
- .By a thread—a fragile, fraying safety net is everybody's problem.Hosp Health Netw.2002;76:32,34–40.
Copyright © 2008 Society of Hospital Medicine