Article
Is an IUD a good contraceptive choice for a never sexually active teen?
- Author:
- Ronald T. Burkman, MD
Yes, but some insertions may be required to be performed outside of the office setting. Authors of this...
Article
Are women seeking short-acting contraception satisfied with LARC after giving it a try?
- Author:
- Ronald T. Burkman, MD
Yes—and their chances of continuing contraception at 2 years are greater and their chances of unintended pregnancy at 2 years are less than their...
Article

Contraceptive considerations for women with headache and migraine
- Author:
- Ronald T. Burkman, MD
What are the benefits and risks of using hormonal contraceptives in women with headache and migraine?
Video

Webcast: Emergency contraception: How to choose the right one for your patient
- Author:
- Ronald T. Burkman, MD
Article
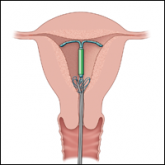
Overcoming LARC complications: 7 case challenges
- Author:
- David R. Kattan, MD, MPH
- Ronald T. Burkman, MD
The strings to your patient’s intrauterine device (IUD) are “missing.” Clinical experience and ACOG direction guide the management plans for this...
Video

Webcast: Contraceptive considerations for women with headache and migraine
- Author:
- Ronald T. Burkman, MD
With 43% of reproductive-aged women in the US reporting migraine headache and roughly the same percentage also using hormonal contraception, Dr....
Video

Webcast: Hormonal contraception and risk of venous thromboembolism
- Author:
- Ronald T. Burkman, MD
Which hormonal contraceptives increase the risk of venous thromboembolism (VTE)? Are there differences by specific preparations? What groups of...
Video

Webcast: Oral contraceptives and breast cancer: What’s the risk?
- Author:
- Ronald T. Burkman, MD
Does the use of oral contraceptives, particularly the presence of estrogen and progesterone, increase the risk of breast cancer? And what about a...
Video
Webcast: Providing LARC methods of contraception to adolescents
- Author:
- Ronald T. Burkman, MD
News

With no budge in more than 20 years, are US unintended pregnancy rates finally on the decline?
- Author:
- Ronald T. Burkman, MD
Yes. In 2008, the rate of unintended pregnancy was 54 per 1,000 among women and girls aged 15 to 44 years. In 2011, this rate dropped by 18%, to...
Video
Shoulder dystocia: Taking the fear out of management
- Author:
- John T. Repke, MD
- Ronald T. Burkman, MD
What are the risk factors for shoulder dystocia, as well as ways to prevent, better manage, and improve communication between clinicians when it...
Video

Webcast: Factors that contribute to overall contraceptive efficacy and risks
- Author:
- Ronald T. Burkman, MD
In this webcast Dr. Burkman compares perfect and typical use failure rates of the 2 most popular forms of contraception, OCs and condoms, with...
Video

Webcast: Obesity and contraceptive efficacy and risks
- Author:
- Ronald T. Burkman, MD
What you should know before counseling your obese patients on choosing a contraceptive
Video

Webcast: How to use the CDC's online tools to manage complex cases in contraception
- Author:
- Ronald T. Burkman, MD
Mastering these resources for contraception and condition compatibility could go a long way during busy days of patient care
News
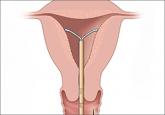
Your teenage patient and contraception: Think “long-acting” first
- Author:
- David R. Kattan, MD, MPH
- Ronald T. Burkman, MD
Although use of long-acting reversible contraception is increasing slowly in the United States, there is plenty of room for improvement,...
