User login
How to screen for and treat teen alcohol use
THE CASE
Paul F* is a 16-year-old White boy who lives with his mother and spends some weekends with his father who has shared custody. He recently presented to the clinic for treatment due to an arrest for disorderly conduct at school. He and a friend were found drinking liquor outside the school building when they were scheduled to be in class. Paul reported that he and his friends often drink at school and at extracurricular functions. He has been using alcohol for the past 2 years, with escalating consumption (5 or more drinks per episode) in the past year. Paul has been drinking most days of the week and has even driven under the influence at times. He said, “I just feel happier when I am drinking.” An accomplished soccer player recruited by colleges, Paul recently was suspended from the team due to his poor grades. His response was, “It’s stupid anyway. What’s the point of playing?”
●
* The patient’s name and some personal details have been changed to protect his identity.
Alcohol is the number 1 substance of abuse for adolescents, used more than tobacco or drugs.1-3 In 2007 and again in 2016, the Surgeon General of the United States issued reports to highlight this important topic,1,2 noting that early and repeated exposure to alcohol during this crucial time of brain development increases the risk for future problems, including addiction.2
Adolescent alcohol use is often underestimated by parents and physicians, including misjudging how much, how often, and how young children are when they begin to drink.1 Boys and girls tend to start drinking at similar ages (13.9 and 14.4 years, respectively),3 but as girls age, they tend to drink more and binge more.4 In 2019, 1 in 4 adolescents reported drinking and more than 4 million reported at least 1 episode of binge drinking in the prior month.4 These numbers have further ramifications: early drinking is associated with alcohol dependence, relapse, use of other substances, risky sexual behaviors, injurious behaviors, suicide, motor vehicle accidents, and dating violence.4-6
Diagnosing alcohol use disorder
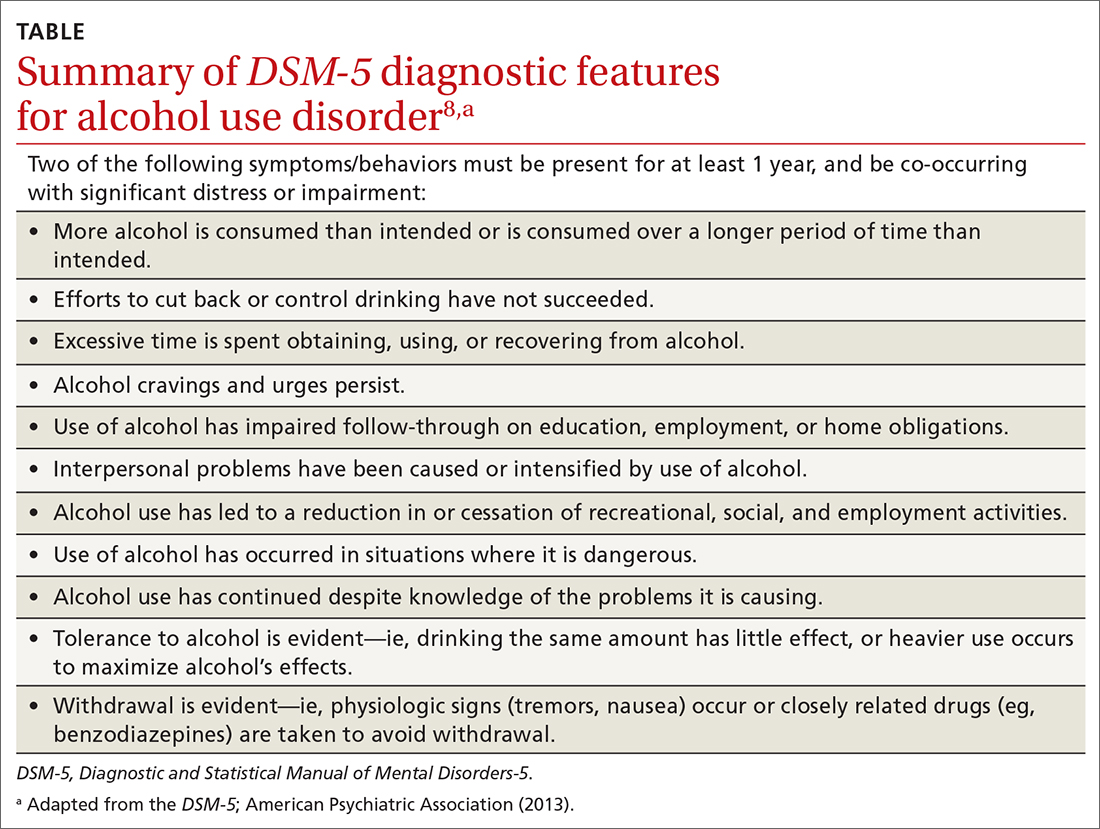
The range of alcohol use includes consumption, bingeing, abuse, and dependence.7,8 Consumption is defined as the drinking of alcoholic beverages. Bingeing is the consumption of more than 5 drinks for men or 4 drinks for women in 2 hours, according to the National Institute on Alcohol Abuse and Alcoholism.7 However, the criterion is slightly different for the Substance Abuse and Mental Health Services Administration, which broadens the timeframe to “on the same occasion.”9 While previously known as separate disorders, alcohol abuse (or misuse) and alcohol dependence are now diagnostically classified together as alcohol use disorders (AUDs), per the Diagnostic and Statistical Manual of Mental Disorders-5 (DSM-5).8 AUD is further stratified as mild, moderate, or severe, depending on the number of criteria that are met by the patient (TABLE).8,10
Alcohol screening
Currently, the US Preventive Services Task Force (USPSTF) does not recommend screening adolescents ages 12 to 17 for AUD, and has instead issued an “I” statement (insufficient evidence).11 While the USPSTF recognizes the potential burdens of adolescent alcohol use, the potential harms of screening include “stigma, anxiety, labeling, discrimination, privacy concerns, and interference with the patient–clinician relationship.”11 The USPSTF also notes that it “did not find any evidence that specifically examined the harms of screening for alcohol use in adolescents.”11
This is at odds with recommendations from the American Academy of Pediatrics (AAP), which in 2011 released a policy statement advocating screening, brief intervention, and referral to treatment for adolescent substance use.12 In the United States, even though 83% of adolescents see a physician at least once each year,12,13 alcohol misuse screening still varies, occurring in the range of 50% to 86% of office visits.12 When screening does occur, it is often based on clinical impression only.12 Studies have shown that when a screening tool is not used, up to two-thirds of substance use disorders may be missed.12-15
Continue to: A full and complete biopsychosocial interview
A full and complete biopsychosocial interview with adolescents is a necessity, and should include queries about alcohol, drugs, and other substances. Acknowledgment of use should trigger further investigation into the substance use areas. Interviews may start with open-ended questions about alcohol use at home or at school before moving to more personalized and detailed questioning and use of screening tools.16
While various screening instruments exist, for the sake of brevity we provide as an example the Screening to Brief Intervention (S2BI) tool. It is an efficient, single-page tool that can help clinicians in their routine care of adolescents to quickly stratify the patient risk of substance use disorder as none/low, moderate, or severe.12 It can be found here: www.mcpap.com/pdf/S2Bi%20Toolkit.pdf (see page 10).
For all patients, but particularly for adolescents, confidentiality is important, and many specialty societies have created language to address this issue.12 Discuss confidentiality with both the adolescent patient and the patient’s caregiver simultaneously, with dialogue that includes: (a) the need to speak with adolescents alone during the office visit, (b) the benefits of confidentiality in the physician–patient relationship, and (c) the need to disclose selected information to keep patients safe.12 Describing the process for required disclosures is essential. Benefits of disclosure include further support for the adolescent patient as well as appropriate parental participation and support for possible referrals.12
Treating AUD
Treatment for AUD should be multifaceted. Screen for comorbid mood disorders, such as generalized anxiety,17,18 social anxiety,18 and depression,19 as well as for insomnia.18 Studies have demonstrated a strong link between insomnia and anxiety, and again between anxiety and AUD.17-19 Finally, screen for adverse childhood events such as trauma, victimization, and abuse.20 Addressing issues discovered in screening allows for more targeted and personalized treatment of AUD.
The National Institute on Drug Abuse categorizes evidence-based treatment into 3 areas: behavioral therapies, family therapies, and medications.21
Continue to: Behavioral therapies
Behavioral therapies can include group therapy, cognitive behavioral therapy (CBT), motivational enhancement therapy, 12-Step facilitation, and contingency management, in which small rewards or incentives are given for participation in treatment to reinforce positive behaviors.21
Family-based therapies, such as brief strategic family therapy, functional family therapy, and multisystem therapy recognize that adolescents exist in systems of families in communities, and that the patient’s success in treatment may be supported by these relationships.21
Some medications may achieve modest benefit for treatment of adolescents with AUD. Naltrexone, acamprosate, and disulfiram have all been used successfully to treat AUD in adults21; some physicians may choose to use these medications “off label” in adolescents. Bupropion has been used successfully in the treatment of nicotine use disorder,21 and a small study in 2005 showed some success with bupropion in treating adolescents with attention-deficit/hyperactivity disorder, comorbid depression, and substance use disorder.22 Naltrexone has also been studied in adolescents with opioid use disorder, although these were not large studies.23
Adolescents with serious, sustained issues with AUD may require more in-depth treatments such as an intensive outpatient program, a partial hospitalization program, or a residential treatment program.15 The least-restrictive environment is preferable.15 Families are generally included as part of the treatment and recovery process in those settings.21 Some patients may require detoxification prior to referral to residential treatment settings; the American Society of Addiction Medicine has published a comprehensive guideline on alcohol withdrawal.24
Paul’s family physician diagnosed his condition as AUD and referred him for CBT with a psychologist, who treated him for both the AUD and an underlying depressive disorder that was later identified. CBT focused on cognitive restructuring of depressive thoughts as well as support for continued abstinence from alcohol. The patient, with family support, declined antidepressant medication.
After 6 months of treatment, Paul and his parents were pleased with his progress. His grades improved to the point that he was permitted to play soccer again, and he was seriously looking at his future college options.
CORRESPONDENCE
Scott A. Fields, PhD, 3200 MacCorkle Avenue Southeast, 5th Floor, Robert C. Byrd Clinical Teaching Center, Department of Family Medicine, Charleston, WV 25304; sfields@hsc.wvu.edu
1. US Department of Health and Human Services. The Surgeon General’s Call to Action to Prevent and Reduce Underage Drinking. Washington, DC; US Department of Health and Human Services, Office of the Surgeon General. 2007.
2. US Department of Health and Human Services. Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health. Washington, DC; US Department of Health and Human Services, Office of the Surgeon General. 2016.
3. Hingson R, White A. New research findings since the 2007 Surgeon General’s Call to Action to Prevent and Reduce Underage Drinking: A review. J Stud Alcohol Drugs Suppl. 2014; 75:158-169.
4. National Institute on Alcohol Abuse and Alcoholism. Underage drinking. National Institute of Health. Accessed December 22, 2021. www.niaaa.nih.gov/publications/brochures-and-fact-sheets/underage-drinking.
5. Hingson R, Zha W, Iannotti R, et al. Physician advice to adolescents about drinking and other health behaviors. Pediatrics. 2013;131:249-257.
6. Schaus JF, Sole ML, McCoy TP, et al. Screening for high-risk drinking in a college student health center: characterizing students based on quantity, frequency, and harms. J Stud Alcohol Drugs Suppl. 2009;16:34-44.
7. National Institute on Alcohol Abuse and Alcoholism. Drinking levels defined. Accessed December 27, 2021. www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking
8. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Arlington, VA; American Psychiatric Association. 2013.
9. Substance Abuse and Mental Health Services Administration. Bringing down binge drinking. Accessed December 27, 2021. www.samhsa.gov/sites/default/files/programs_campaigns/nation_prevention_week/data-binge-drinking.pdf
10. Grant BF, Goldstein RB, Saha TD, et al. Epidemiology of DSM-5 Alcohol Use Disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72:757-766.
11. USPSTF. Screening and behavioral counseling interventions to reduce unhealthy alcohol use in adolescents and adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;320:1899-1909.
12. Levy SJ, Williams JF, Committee on Substance Use and Prevention. Substance use screening, brief intervention, and referral to treatment. Pediatrics. 2016;138:e20161211.
13. MacKay AP, Duran CP. Adolescent Health in the United States. National Center for Health Statistics, Centers for Disease Control and Prevention. 2007.
14. Haller DM, Meynard A, Lefebvre D, et al. Effectiveness of training family physicians to deliver a brief intervention to address excessive substance use among young patients: a cluster randomized controlled trial. CMAJ. 2014;186:E263-E272.
15. Borus J, Parhami I, Levy S. Screening, brief intervention, and referral to treatment. Child Adolesc Psychiatric Clin N Am. 2016;25:579-601.
16. Knight J, Roberts T, Gabrielli J, et al. Adolescent alcohol and substance use and abuse. Performing preventive services: A bright futures handbook. Accessed December 22, 2021. American Academy of Pediatrics. https://ocfcpacourts.us/wp-content/uploads/2020/06/Adolescent_Alcohol_and_Substance_Abuse_001005.pdf
17. Dyer ML, Heron J, Hickman M, et al. Alcohol use in late adolescence and early adulthood: the role of generalized anxiety disorder and drinking to cope motives. Drug Alcohol Depend. 2019;204:107480.
18. Blumenthal H, Taylor DJ, Cloutier RM, et al. The links between social anxiety disorder, insomnia symptoms, and alcohol use disorders: findings from a large sample of adolescents in the United States. Behav Ther. 2019;50:50-59.
19. Pedrelli P, Shapero B, Archibald A, et al. Alcohol use and depression during adolescence and young adulthood: a summary and interpretation of mixed findings. Curr Addict Rep. 2016;3:91-97.
20. Davis JP, Dworkin ER, Helton J, et al. Extending poly-victimization theory: differential effects of adolescents’ experiences of victimization on substance use disorder diagnoses upon treatment entry. Child Abuse Negl. 2019; 89:165-177.
21. NIDA. Principles of adolescent substance use disorder treatment: a research-based guide. Accessed December 22, 2021. www.drugabuse.gov/publications/principles-adolescent-substance-use-disorder-treatment-research-based-guide
22. Solhkhah R, Wilens TE, Daly J, et al. Bupropion SR for the treatment of substance-abusing outpatient adolescents with attention-deficit/hyperactivity disorder and mood disorders. J Child Adolesc Psychopharmacol. 2005:15:777-786.
23. Camenga DR, Colon-Rivera HA, Muvvala SB. Medications for maintenance treatment of opioid use disorder in adolescents. J Stud Alcohol Drugs. 2019;80:393-402.
24. American Society of Addiction Medicine. The ASAM clinical practice guideline on alcohol withdrawal management. Accessed December 22, 2021. www.asam.org/quality-care/clinical-guidelines/alcohol-withdrawal-management-guideline
THE CASE
Paul F* is a 16-year-old White boy who lives with his mother and spends some weekends with his father who has shared custody. He recently presented to the clinic for treatment due to an arrest for disorderly conduct at school. He and a friend were found drinking liquor outside the school building when they were scheduled to be in class. Paul reported that he and his friends often drink at school and at extracurricular functions. He has been using alcohol for the past 2 years, with escalating consumption (5 or more drinks per episode) in the past year. Paul has been drinking most days of the week and has even driven under the influence at times. He said, “I just feel happier when I am drinking.” An accomplished soccer player recruited by colleges, Paul recently was suspended from the team due to his poor grades. His response was, “It’s stupid anyway. What’s the point of playing?”
●
* The patient’s name and some personal details have been changed to protect his identity.
Alcohol is the number 1 substance of abuse for adolescents, used more than tobacco or drugs.1-3 In 2007 and again in 2016, the Surgeon General of the United States issued reports to highlight this important topic,1,2 noting that early and repeated exposure to alcohol during this crucial time of brain development increases the risk for future problems, including addiction.2
Adolescent alcohol use is often underestimated by parents and physicians, including misjudging how much, how often, and how young children are when they begin to drink.1 Boys and girls tend to start drinking at similar ages (13.9 and 14.4 years, respectively),3 but as girls age, they tend to drink more and binge more.4 In 2019, 1 in 4 adolescents reported drinking and more than 4 million reported at least 1 episode of binge drinking in the prior month.4 These numbers have further ramifications: early drinking is associated with alcohol dependence, relapse, use of other substances, risky sexual behaviors, injurious behaviors, suicide, motor vehicle accidents, and dating violence.4-6
Diagnosing alcohol use disorder
The range of alcohol use includes consumption, bingeing, abuse, and dependence.7,8 Consumption is defined as the drinking of alcoholic beverages. Bingeing is the consumption of more than 5 drinks for men or 4 drinks for women in 2 hours, according to the National Institute on Alcohol Abuse and Alcoholism.7 However, the criterion is slightly different for the Substance Abuse and Mental Health Services Administration, which broadens the timeframe to “on the same occasion.”9 While previously known as separate disorders, alcohol abuse (or misuse) and alcohol dependence are now diagnostically classified together as alcohol use disorders (AUDs), per the Diagnostic and Statistical Manual of Mental Disorders-5 (DSM-5).8 AUD is further stratified as mild, moderate, or severe, depending on the number of criteria that are met by the patient (TABLE).8,10
Alcohol screening
Currently, the US Preventive Services Task Force (USPSTF) does not recommend screening adolescents ages 12 to 17 for AUD, and has instead issued an “I” statement (insufficient evidence).11 While the USPSTF recognizes the potential burdens of adolescent alcohol use, the potential harms of screening include “stigma, anxiety, labeling, discrimination, privacy concerns, and interference with the patient–clinician relationship.”11 The USPSTF also notes that it “did not find any evidence that specifically examined the harms of screening for alcohol use in adolescents.”11
This is at odds with recommendations from the American Academy of Pediatrics (AAP), which in 2011 released a policy statement advocating screening, brief intervention, and referral to treatment for adolescent substance use.12 In the United States, even though 83% of adolescents see a physician at least once each year,12,13 alcohol misuse screening still varies, occurring in the range of 50% to 86% of office visits.12 When screening does occur, it is often based on clinical impression only.12 Studies have shown that when a screening tool is not used, up to two-thirds of substance use disorders may be missed.12-15
Continue to: A full and complete biopsychosocial interview
A full and complete biopsychosocial interview with adolescents is a necessity, and should include queries about alcohol, drugs, and other substances. Acknowledgment of use should trigger further investigation into the substance use areas. Interviews may start with open-ended questions about alcohol use at home or at school before moving to more personalized and detailed questioning and use of screening tools.16
While various screening instruments exist, for the sake of brevity we provide as an example the Screening to Brief Intervention (S2BI) tool. It is an efficient, single-page tool that can help clinicians in their routine care of adolescents to quickly stratify the patient risk of substance use disorder as none/low, moderate, or severe.12 It can be found here: www.mcpap.com/pdf/S2Bi%20Toolkit.pdf (see page 10).
For all patients, but particularly for adolescents, confidentiality is important, and many specialty societies have created language to address this issue.12 Discuss confidentiality with both the adolescent patient and the patient’s caregiver simultaneously, with dialogue that includes: (a) the need to speak with adolescents alone during the office visit, (b) the benefits of confidentiality in the physician–patient relationship, and (c) the need to disclose selected information to keep patients safe.12 Describing the process for required disclosures is essential. Benefits of disclosure include further support for the adolescent patient as well as appropriate parental participation and support for possible referrals.12
Treating AUD
Treatment for AUD should be multifaceted. Screen for comorbid mood disorders, such as generalized anxiety,17,18 social anxiety,18 and depression,19 as well as for insomnia.18 Studies have demonstrated a strong link between insomnia and anxiety, and again between anxiety and AUD.17-19 Finally, screen for adverse childhood events such as trauma, victimization, and abuse.20 Addressing issues discovered in screening allows for more targeted and personalized treatment of AUD.
The National Institute on Drug Abuse categorizes evidence-based treatment into 3 areas: behavioral therapies, family therapies, and medications.21
Continue to: Behavioral therapies
Behavioral therapies can include group therapy, cognitive behavioral therapy (CBT), motivational enhancement therapy, 12-Step facilitation, and contingency management, in which small rewards or incentives are given for participation in treatment to reinforce positive behaviors.21
Family-based therapies, such as brief strategic family therapy, functional family therapy, and multisystem therapy recognize that adolescents exist in systems of families in communities, and that the patient’s success in treatment may be supported by these relationships.21
Some medications may achieve modest benefit for treatment of adolescents with AUD. Naltrexone, acamprosate, and disulfiram have all been used successfully to treat AUD in adults21; some physicians may choose to use these medications “off label” in adolescents. Bupropion has been used successfully in the treatment of nicotine use disorder,21 and a small study in 2005 showed some success with bupropion in treating adolescents with attention-deficit/hyperactivity disorder, comorbid depression, and substance use disorder.22 Naltrexone has also been studied in adolescents with opioid use disorder, although these were not large studies.23
Adolescents with serious, sustained issues with AUD may require more in-depth treatments such as an intensive outpatient program, a partial hospitalization program, or a residential treatment program.15 The least-restrictive environment is preferable.15 Families are generally included as part of the treatment and recovery process in those settings.21 Some patients may require detoxification prior to referral to residential treatment settings; the American Society of Addiction Medicine has published a comprehensive guideline on alcohol withdrawal.24
Paul’s family physician diagnosed his condition as AUD and referred him for CBT with a psychologist, who treated him for both the AUD and an underlying depressive disorder that was later identified. CBT focused on cognitive restructuring of depressive thoughts as well as support for continued abstinence from alcohol. The patient, with family support, declined antidepressant medication.
After 6 months of treatment, Paul and his parents were pleased with his progress. His grades improved to the point that he was permitted to play soccer again, and he was seriously looking at his future college options.
CORRESPONDENCE
Scott A. Fields, PhD, 3200 MacCorkle Avenue Southeast, 5th Floor, Robert C. Byrd Clinical Teaching Center, Department of Family Medicine, Charleston, WV 25304; sfields@hsc.wvu.edu
THE CASE
Paul F* is a 16-year-old White boy who lives with his mother and spends some weekends with his father who has shared custody. He recently presented to the clinic for treatment due to an arrest for disorderly conduct at school. He and a friend were found drinking liquor outside the school building when they were scheduled to be in class. Paul reported that he and his friends often drink at school and at extracurricular functions. He has been using alcohol for the past 2 years, with escalating consumption (5 or more drinks per episode) in the past year. Paul has been drinking most days of the week and has even driven under the influence at times. He said, “I just feel happier when I am drinking.” An accomplished soccer player recruited by colleges, Paul recently was suspended from the team due to his poor grades. His response was, “It’s stupid anyway. What’s the point of playing?”
●
* The patient’s name and some personal details have been changed to protect his identity.
Alcohol is the number 1 substance of abuse for adolescents, used more than tobacco or drugs.1-3 In 2007 and again in 2016, the Surgeon General of the United States issued reports to highlight this important topic,1,2 noting that early and repeated exposure to alcohol during this crucial time of brain development increases the risk for future problems, including addiction.2
Adolescent alcohol use is often underestimated by parents and physicians, including misjudging how much, how often, and how young children are when they begin to drink.1 Boys and girls tend to start drinking at similar ages (13.9 and 14.4 years, respectively),3 but as girls age, they tend to drink more and binge more.4 In 2019, 1 in 4 adolescents reported drinking and more than 4 million reported at least 1 episode of binge drinking in the prior month.4 These numbers have further ramifications: early drinking is associated with alcohol dependence, relapse, use of other substances, risky sexual behaviors, injurious behaviors, suicide, motor vehicle accidents, and dating violence.4-6
Diagnosing alcohol use disorder
The range of alcohol use includes consumption, bingeing, abuse, and dependence.7,8 Consumption is defined as the drinking of alcoholic beverages. Bingeing is the consumption of more than 5 drinks for men or 4 drinks for women in 2 hours, according to the National Institute on Alcohol Abuse and Alcoholism.7 However, the criterion is slightly different for the Substance Abuse and Mental Health Services Administration, which broadens the timeframe to “on the same occasion.”9 While previously known as separate disorders, alcohol abuse (or misuse) and alcohol dependence are now diagnostically classified together as alcohol use disorders (AUDs), per the Diagnostic and Statistical Manual of Mental Disorders-5 (DSM-5).8 AUD is further stratified as mild, moderate, or severe, depending on the number of criteria that are met by the patient (TABLE).8,10
Alcohol screening
Currently, the US Preventive Services Task Force (USPSTF) does not recommend screening adolescents ages 12 to 17 for AUD, and has instead issued an “I” statement (insufficient evidence).11 While the USPSTF recognizes the potential burdens of adolescent alcohol use, the potential harms of screening include “stigma, anxiety, labeling, discrimination, privacy concerns, and interference with the patient–clinician relationship.”11 The USPSTF also notes that it “did not find any evidence that specifically examined the harms of screening for alcohol use in adolescents.”11
This is at odds with recommendations from the American Academy of Pediatrics (AAP), which in 2011 released a policy statement advocating screening, brief intervention, and referral to treatment for adolescent substance use.12 In the United States, even though 83% of adolescents see a physician at least once each year,12,13 alcohol misuse screening still varies, occurring in the range of 50% to 86% of office visits.12 When screening does occur, it is often based on clinical impression only.12 Studies have shown that when a screening tool is not used, up to two-thirds of substance use disorders may be missed.12-15
Continue to: A full and complete biopsychosocial interview
A full and complete biopsychosocial interview with adolescents is a necessity, and should include queries about alcohol, drugs, and other substances. Acknowledgment of use should trigger further investigation into the substance use areas. Interviews may start with open-ended questions about alcohol use at home or at school before moving to more personalized and detailed questioning and use of screening tools.16
While various screening instruments exist, for the sake of brevity we provide as an example the Screening to Brief Intervention (S2BI) tool. It is an efficient, single-page tool that can help clinicians in their routine care of adolescents to quickly stratify the patient risk of substance use disorder as none/low, moderate, or severe.12 It can be found here: www.mcpap.com/pdf/S2Bi%20Toolkit.pdf (see page 10).
For all patients, but particularly for adolescents, confidentiality is important, and many specialty societies have created language to address this issue.12 Discuss confidentiality with both the adolescent patient and the patient’s caregiver simultaneously, with dialogue that includes: (a) the need to speak with adolescents alone during the office visit, (b) the benefits of confidentiality in the physician–patient relationship, and (c) the need to disclose selected information to keep patients safe.12 Describing the process for required disclosures is essential. Benefits of disclosure include further support for the adolescent patient as well as appropriate parental participation and support for possible referrals.12
Treating AUD
Treatment for AUD should be multifaceted. Screen for comorbid mood disorders, such as generalized anxiety,17,18 social anxiety,18 and depression,19 as well as for insomnia.18 Studies have demonstrated a strong link between insomnia and anxiety, and again between anxiety and AUD.17-19 Finally, screen for adverse childhood events such as trauma, victimization, and abuse.20 Addressing issues discovered in screening allows for more targeted and personalized treatment of AUD.
The National Institute on Drug Abuse categorizes evidence-based treatment into 3 areas: behavioral therapies, family therapies, and medications.21
Continue to: Behavioral therapies
Behavioral therapies can include group therapy, cognitive behavioral therapy (CBT), motivational enhancement therapy, 12-Step facilitation, and contingency management, in which small rewards or incentives are given for participation in treatment to reinforce positive behaviors.21
Family-based therapies, such as brief strategic family therapy, functional family therapy, and multisystem therapy recognize that adolescents exist in systems of families in communities, and that the patient’s success in treatment may be supported by these relationships.21
Some medications may achieve modest benefit for treatment of adolescents with AUD. Naltrexone, acamprosate, and disulfiram have all been used successfully to treat AUD in adults21; some physicians may choose to use these medications “off label” in adolescents. Bupropion has been used successfully in the treatment of nicotine use disorder,21 and a small study in 2005 showed some success with bupropion in treating adolescents with attention-deficit/hyperactivity disorder, comorbid depression, and substance use disorder.22 Naltrexone has also been studied in adolescents with opioid use disorder, although these were not large studies.23
Adolescents with serious, sustained issues with AUD may require more in-depth treatments such as an intensive outpatient program, a partial hospitalization program, or a residential treatment program.15 The least-restrictive environment is preferable.15 Families are generally included as part of the treatment and recovery process in those settings.21 Some patients may require detoxification prior to referral to residential treatment settings; the American Society of Addiction Medicine has published a comprehensive guideline on alcohol withdrawal.24
Paul’s family physician diagnosed his condition as AUD and referred him for CBT with a psychologist, who treated him for both the AUD and an underlying depressive disorder that was later identified. CBT focused on cognitive restructuring of depressive thoughts as well as support for continued abstinence from alcohol. The patient, with family support, declined antidepressant medication.
After 6 months of treatment, Paul and his parents were pleased with his progress. His grades improved to the point that he was permitted to play soccer again, and he was seriously looking at his future college options.
CORRESPONDENCE
Scott A. Fields, PhD, 3200 MacCorkle Avenue Southeast, 5th Floor, Robert C. Byrd Clinical Teaching Center, Department of Family Medicine, Charleston, WV 25304; sfields@hsc.wvu.edu
1. US Department of Health and Human Services. The Surgeon General’s Call to Action to Prevent and Reduce Underage Drinking. Washington, DC; US Department of Health and Human Services, Office of the Surgeon General. 2007.
2. US Department of Health and Human Services. Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health. Washington, DC; US Department of Health and Human Services, Office of the Surgeon General. 2016.
3. Hingson R, White A. New research findings since the 2007 Surgeon General’s Call to Action to Prevent and Reduce Underage Drinking: A review. J Stud Alcohol Drugs Suppl. 2014; 75:158-169.
4. National Institute on Alcohol Abuse and Alcoholism. Underage drinking. National Institute of Health. Accessed December 22, 2021. www.niaaa.nih.gov/publications/brochures-and-fact-sheets/underage-drinking.
5. Hingson R, Zha W, Iannotti R, et al. Physician advice to adolescents about drinking and other health behaviors. Pediatrics. 2013;131:249-257.
6. Schaus JF, Sole ML, McCoy TP, et al. Screening for high-risk drinking in a college student health center: characterizing students based on quantity, frequency, and harms. J Stud Alcohol Drugs Suppl. 2009;16:34-44.
7. National Institute on Alcohol Abuse and Alcoholism. Drinking levels defined. Accessed December 27, 2021. www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking
8. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Arlington, VA; American Psychiatric Association. 2013.
9. Substance Abuse and Mental Health Services Administration. Bringing down binge drinking. Accessed December 27, 2021. www.samhsa.gov/sites/default/files/programs_campaigns/nation_prevention_week/data-binge-drinking.pdf
10. Grant BF, Goldstein RB, Saha TD, et al. Epidemiology of DSM-5 Alcohol Use Disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72:757-766.
11. USPSTF. Screening and behavioral counseling interventions to reduce unhealthy alcohol use in adolescents and adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;320:1899-1909.
12. Levy SJ, Williams JF, Committee on Substance Use and Prevention. Substance use screening, brief intervention, and referral to treatment. Pediatrics. 2016;138:e20161211.
13. MacKay AP, Duran CP. Adolescent Health in the United States. National Center for Health Statistics, Centers for Disease Control and Prevention. 2007.
14. Haller DM, Meynard A, Lefebvre D, et al. Effectiveness of training family physicians to deliver a brief intervention to address excessive substance use among young patients: a cluster randomized controlled trial. CMAJ. 2014;186:E263-E272.
15. Borus J, Parhami I, Levy S. Screening, brief intervention, and referral to treatment. Child Adolesc Psychiatric Clin N Am. 2016;25:579-601.
16. Knight J, Roberts T, Gabrielli J, et al. Adolescent alcohol and substance use and abuse. Performing preventive services: A bright futures handbook. Accessed December 22, 2021. American Academy of Pediatrics. https://ocfcpacourts.us/wp-content/uploads/2020/06/Adolescent_Alcohol_and_Substance_Abuse_001005.pdf
17. Dyer ML, Heron J, Hickman M, et al. Alcohol use in late adolescence and early adulthood: the role of generalized anxiety disorder and drinking to cope motives. Drug Alcohol Depend. 2019;204:107480.
18. Blumenthal H, Taylor DJ, Cloutier RM, et al. The links between social anxiety disorder, insomnia symptoms, and alcohol use disorders: findings from a large sample of adolescents in the United States. Behav Ther. 2019;50:50-59.
19. Pedrelli P, Shapero B, Archibald A, et al. Alcohol use and depression during adolescence and young adulthood: a summary and interpretation of mixed findings. Curr Addict Rep. 2016;3:91-97.
20. Davis JP, Dworkin ER, Helton J, et al. Extending poly-victimization theory: differential effects of adolescents’ experiences of victimization on substance use disorder diagnoses upon treatment entry. Child Abuse Negl. 2019; 89:165-177.
21. NIDA. Principles of adolescent substance use disorder treatment: a research-based guide. Accessed December 22, 2021. www.drugabuse.gov/publications/principles-adolescent-substance-use-disorder-treatment-research-based-guide
22. Solhkhah R, Wilens TE, Daly J, et al. Bupropion SR for the treatment of substance-abusing outpatient adolescents with attention-deficit/hyperactivity disorder and mood disorders. J Child Adolesc Psychopharmacol. 2005:15:777-786.
23. Camenga DR, Colon-Rivera HA, Muvvala SB. Medications for maintenance treatment of opioid use disorder in adolescents. J Stud Alcohol Drugs. 2019;80:393-402.
24. American Society of Addiction Medicine. The ASAM clinical practice guideline on alcohol withdrawal management. Accessed December 22, 2021. www.asam.org/quality-care/clinical-guidelines/alcohol-withdrawal-management-guideline
1. US Department of Health and Human Services. The Surgeon General’s Call to Action to Prevent and Reduce Underage Drinking. Washington, DC; US Department of Health and Human Services, Office of the Surgeon General. 2007.
2. US Department of Health and Human Services. Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health. Washington, DC; US Department of Health and Human Services, Office of the Surgeon General. 2016.
3. Hingson R, White A. New research findings since the 2007 Surgeon General’s Call to Action to Prevent and Reduce Underage Drinking: A review. J Stud Alcohol Drugs Suppl. 2014; 75:158-169.
4. National Institute on Alcohol Abuse and Alcoholism. Underage drinking. National Institute of Health. Accessed December 22, 2021. www.niaaa.nih.gov/publications/brochures-and-fact-sheets/underage-drinking.
5. Hingson R, Zha W, Iannotti R, et al. Physician advice to adolescents about drinking and other health behaviors. Pediatrics. 2013;131:249-257.
6. Schaus JF, Sole ML, McCoy TP, et al. Screening for high-risk drinking in a college student health center: characterizing students based on quantity, frequency, and harms. J Stud Alcohol Drugs Suppl. 2009;16:34-44.
7. National Institute on Alcohol Abuse and Alcoholism. Drinking levels defined. Accessed December 27, 2021. www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking
8. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Arlington, VA; American Psychiatric Association. 2013.
9. Substance Abuse and Mental Health Services Administration. Bringing down binge drinking. Accessed December 27, 2021. www.samhsa.gov/sites/default/files/programs_campaigns/nation_prevention_week/data-binge-drinking.pdf
10. Grant BF, Goldstein RB, Saha TD, et al. Epidemiology of DSM-5 Alcohol Use Disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72:757-766.
11. USPSTF. Screening and behavioral counseling interventions to reduce unhealthy alcohol use in adolescents and adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;320:1899-1909.
12. Levy SJ, Williams JF, Committee on Substance Use and Prevention. Substance use screening, brief intervention, and referral to treatment. Pediatrics. 2016;138:e20161211.
13. MacKay AP, Duran CP. Adolescent Health in the United States. National Center for Health Statistics, Centers for Disease Control and Prevention. 2007.
14. Haller DM, Meynard A, Lefebvre D, et al. Effectiveness of training family physicians to deliver a brief intervention to address excessive substance use among young patients: a cluster randomized controlled trial. CMAJ. 2014;186:E263-E272.
15. Borus J, Parhami I, Levy S. Screening, brief intervention, and referral to treatment. Child Adolesc Psychiatric Clin N Am. 2016;25:579-601.
16. Knight J, Roberts T, Gabrielli J, et al. Adolescent alcohol and substance use and abuse. Performing preventive services: A bright futures handbook. Accessed December 22, 2021. American Academy of Pediatrics. https://ocfcpacourts.us/wp-content/uploads/2020/06/Adolescent_Alcohol_and_Substance_Abuse_001005.pdf
17. Dyer ML, Heron J, Hickman M, et al. Alcohol use in late adolescence and early adulthood: the role of generalized anxiety disorder and drinking to cope motives. Drug Alcohol Depend. 2019;204:107480.
18. Blumenthal H, Taylor DJ, Cloutier RM, et al. The links between social anxiety disorder, insomnia symptoms, and alcohol use disorders: findings from a large sample of adolescents in the United States. Behav Ther. 2019;50:50-59.
19. Pedrelli P, Shapero B, Archibald A, et al. Alcohol use and depression during adolescence and young adulthood: a summary and interpretation of mixed findings. Curr Addict Rep. 2016;3:91-97.
20. Davis JP, Dworkin ER, Helton J, et al. Extending poly-victimization theory: differential effects of adolescents’ experiences of victimization on substance use disorder diagnoses upon treatment entry. Child Abuse Negl. 2019; 89:165-177.
21. NIDA. Principles of adolescent substance use disorder treatment: a research-based guide. Accessed December 22, 2021. www.drugabuse.gov/publications/principles-adolescent-substance-use-disorder-treatment-research-based-guide
22. Solhkhah R, Wilens TE, Daly J, et al. Bupropion SR for the treatment of substance-abusing outpatient adolescents with attention-deficit/hyperactivity disorder and mood disorders. J Child Adolesc Psychopharmacol. 2005:15:777-786.
23. Camenga DR, Colon-Rivera HA, Muvvala SB. Medications for maintenance treatment of opioid use disorder in adolescents. J Stud Alcohol Drugs. 2019;80:393-402.
24. American Society of Addiction Medicine. The ASAM clinical practice guideline on alcohol withdrawal management. Accessed December 22, 2021. www.asam.org/quality-care/clinical-guidelines/alcohol-withdrawal-management-guideline
A practical guide to the management of phobias
THE CASE
Joe S* is a 25-year-old white man who lives with his mother and has a 5-year history of worsening hypertension. He recently presented to the clinic with heart palpitations, shortness of breath, abdominal distress, and dizziness. He said that it was difficult for him to leave his home due to the intense fear he experiences. He said that these symptoms did not occur at home, nor when he visited specific “safe” locations, such as his girlfriend’s apartment. He reported that his fear had increased over the previous 2 years, and that he had progressively limited the distance he traveled from home. He also reported difficulty being in crowds and said, “The idea of going to the movies is torture.”
●
*The patient’s name has been changed to protect his identity.
The most prevalent psychiatric maladies in primary care are anxiety and mood disorders.1,2 Anxiety disorders are patterns of maladaptive behaviors in conjunction with or response to excessive fear or anxiety.3 The most prevalent anxiety disorder in the United States is specific phobia, the fear of a particular object or situation, with a 12-month prevalence rate of 12.1%.2
Other phobias diagnosed separately in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), include social phobia and agoraphobia, which are, respectively, the fear of being negatively evaluated in social situations and the fear of being trapped in public/open spaces. Social phobia and agoraphobia have diagnostic criteria nearly identical to those of simple phobias regarding the fear response, with the primary differences being the specific phobic situations or stimuli.
Unfortunately, these phobias are likely to be undiagnosed and untreated in primary care partly because patients may not seek treatment.4-6 The ease of avoiding some phobic situations contributes to a lack of treatment seeking.5 Furthermore, commonly used brief measures for psychiatric conditions generally identify depression and anxiety but not phobias. However, family physicians do have resources not only to diagnose these disorders, but also to work with patients to ameliorate them. Collaboration with behavioral health providers is key, as patients with phobias generally benefit from cognitive behavioral therapy (CBT), while those with comorbid psychiatric conditions may benefit from a combination of CBT and medication.
Phobic response vs adaptive fear and anxiety
The terms anxiety and fear often overlap when used to describe a negative emotional state of arousal. However, fear is a response to an actual (or perceived) imminent threat, whereas anxiety is the response to a perceived future threat.3 Fear, although unpleasant, serves an adaptive function in responding to immediate danger.7 Anxiety, in turn, may represent an adaptive function for future activities associated with fear. For example, a cave dweller having seen a bear enter a cave in the past (fear-evoking stimulus) may experience anxiety when exploring a different cave (anxiety that a bear may be present). In this situation, the cave dweller’s fear and anxiety responses are important for survival.
Continue to: With phobias...
With phobias, the fear and anxiety responses become maladaptive.3 Specifically, they involve inaccurate beliefs about a specific type of stimulus that could be an object (snake), environment (ocean), or situation (crowded room). Accompanying the maladaptive thoughts are correspondingly exaggerated emotions, physiologic effects, and behavioral responses in alignment with one another.8 The development of this response and the etiology of phobias is complex and is still being debated.7,9,10 Research points to 4 primary pathways: direct psychological conditioning, modeling (watching others), instruction/information, and nonassociative (innate) acquisition.7,10 While the first 3 pathways involve learned responses, the last results from biological predispositions.
DIAGNOSING PHOBIAS: WHAT TO ZERO IN ON
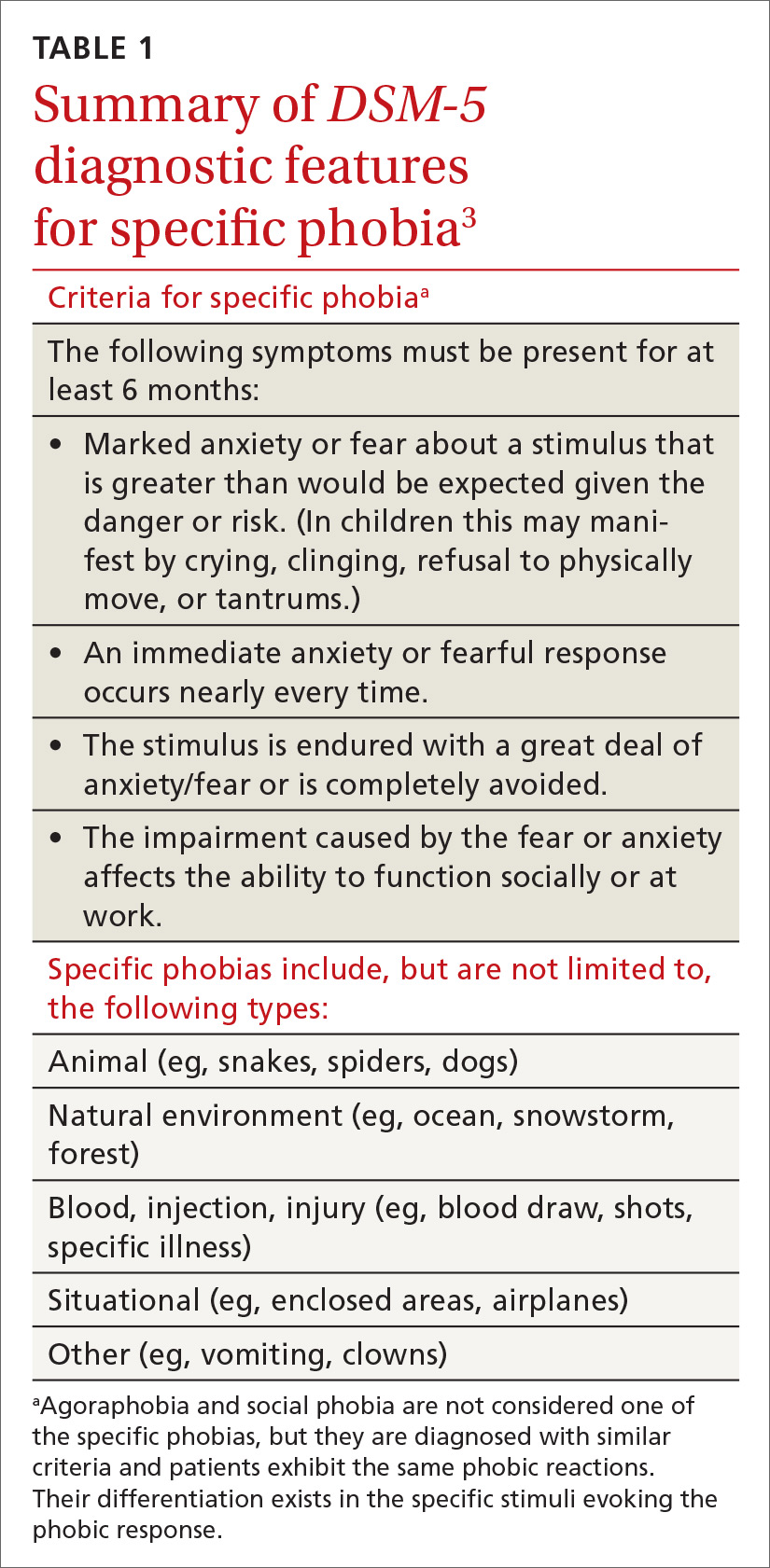
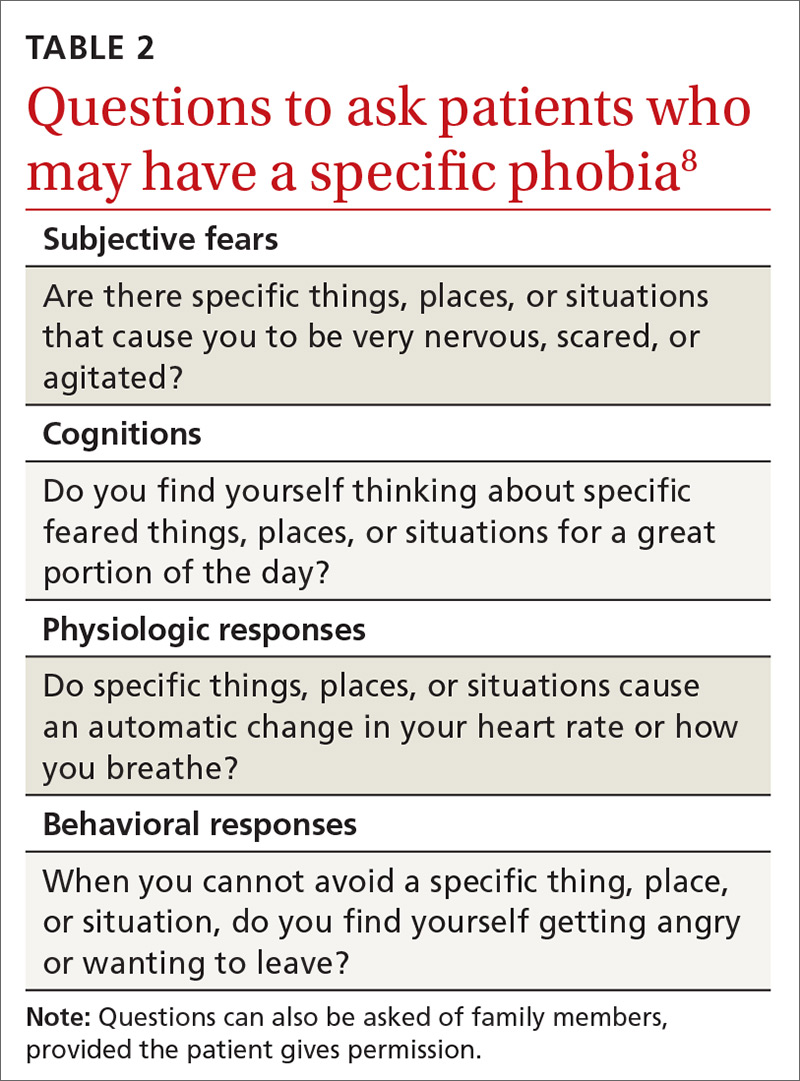
DSM-5 provides diagnostic criteria for specific phobia, agoraphobia, and social phobia, with each diagnosis requiring that symptoms be present for at least 6 months (TABLE 1).3 Diagnosis of phobias should include evaluation of 4 components of a patient’s functioning: subjective fears, cognitions, physiologic responses, and behaviors.8
- Subjective fears: the patient’s described level of distress/agitation to a specific stimulus.
- Cognitions: the patient’s thoughts/beliefs regarding the stimulus.
- Physiologic responses: changes in heart rate, respiration, blood pressure, and other sympathetic nervous system responses with exposure to stimuli.
- Behavioral responses: the most common response is avoidance, with displays of anger, irritability, or apprehension when avoidance of the stimulus is impossible.
Evaluating these 4 components can be accomplished with structured interviews, behavioral observations, or collateral reports from family members or the patient’s peers.8 Thorough questioning and evaluation (TABLE 28) can enable accurate differentiation between phobias unique to specific stimuli and other DSM-5 disorders that might cause similar symptoms. For example, a patient diagnosed with post-traumatic stress disorder (PTSD) might have a fear response even when triggering stimuli are not present. Identification of a clear, life-threatening incident could help with a differential between phobias and PTSD. However, a patient could be diagnosed with both disorders, as the 2 conditions are not mutually exclusive.
The physiologic and behavioral response symptoms of phobia can also mimic purely medical conditions. Hypertension or tachycardia observed during a medical visit could be due to the fear associated with agoraphobia or with a medically related specific phobia. Blood pressure elevated during testing at the medical appointment could be normal with at-home monitoring by the patient. Thus, blood pressure and heart rate screenings performed at home instead of in public places may help to rule out whether potentially elevated numbers are related to a fear response. Fear and avoidance-like symptoms can also be due to substance abuse, and appropriate drug screening can provide information for an accurate diagnosis.
HOW BEST TO TREAT PHOBIAS
Although research demonstrates that a variety of psychotherapeutic and pharmacologic treatments are efficacious for phobias, in some instances the true utility of an intervention to meaningfully improve a patient’s life is questionable. The issue is that the research evaluating treatment often evaluates only one component of a phobic response (eg,
Continue to: Psychotherapeutic interventions...
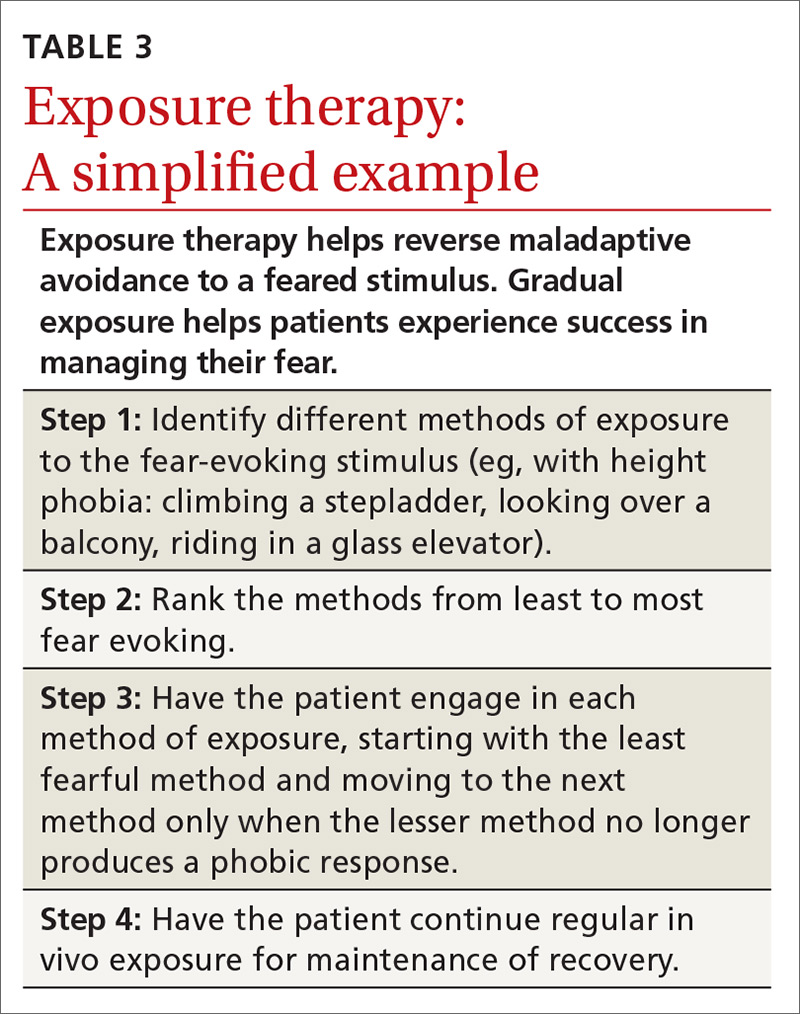
Psychotherapeutic interventions for phobias have shown substantial benefit. CBT is helpful, with the most efficacious technique being exposure therapy.5,6,8,11,12 CBT can begin during the initial primary care visit with the family physician educating the patient about phobias and available treatments.
With exposure therapy, patients are introduced to the source of anxiety over time, whereby they learn to manage the distress
Pharmacologic interventions—specifically selective serotonin reuptake inhibitors (SSRIs) and selective serotonin norepinephrine reuptake inhibitors (SNRIs)—have been effective in treating social phobia and agoraphobia.6 However, treatment of specific phobias via pharmacologic interventions is not supported due to limited efficacy and few studies for SSRIs and SNRIs.5,6
Benzodiazepines, although effective in alleviating some phobic symptoms, are not recommended per current guidelines due to adverse effects and potential exacerbation of the phobic response once discontinued.5,6 This poor result with benzodiazepines may be due to the absence of simultaneous emotional exposure to the feared stimuli. Unfortunately, little research has been done on the long-term effects of pharmacologic intervention once the treatment has been discontinued.11 So, for medication, the question of how long treatment effect lasts after discontinuation remains unanswered.
THE CASE
Mr. S’s family physician diagnosed his condition as agoraphobia with panic attacks. He was prescribed sertraline for his panic attacks and referred for CBT with a psychologist. CBT focused on cognitive restructuring as well as gradual exposure where he would travel with increasing distances to various locations. After 10 months of treatment, Mr. S was able to overcome the agoraphobia and took an “awesome” vacation. He also reported a significant decrease in panic symptoms.
CORRESPONDENCE
Scott A. Fields, PhD, 3200 MacCorkle Avenue Southeast, 5th Floor, Robert C. Byrd Clinical Teaching Center, Department of Family Medicine, Charleston, WV 25304; sfields@hsc.wvu.edu.
1. Simon G, Ormel J, VonKorff M, et al. Health care costs associated with depressive and anxiety disorders in primary care. Am J Psychiatry. 1995; 152:352-357.
2. Kessler RC, Petukhova M, Sampson NA, et al. Twelve‐month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Methods Psychiatr Res. 2012; 21:169-184.
3. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth edition (DSM-5). Arlington, VA: American Psychiatric Association; 2013:189-233.
4. Bandelow B, Michaelis S. Epidemiology of anxiety disorders in the 21st century. Dialogues Clin Neurosci. 2015; 17:327-335.
5. Choy Y, Fyer AJ, Lipsitz JD. Treatment of specific phobia in adults. Clin Psychol Rev. 2007; 27:266-286.
6. Bandelow B, Michaelis S, Wedekind D. Treatment of anxiety disorders. Dialogues Clin Neurosci. 2017; 19:93-107.
7. Poulton R, Menzies RG. Non-associative fear acquisition: a review of the evidence from retrospective and longitudinal research. Behav Res Ther. 2002; 40:127-149.
8. Davis III TE, Ollendick TH. Empirically supported treatments for specific phobia in children: Do efficacious treatments address the components of a phobic response? Clin Psychol Sci Pract. 2005; 12:144-160.
9. Field AP. Is conditioning a useful framework for understanding the development and treatment of phobias? Clin Psychol Rev. 2006; 26:857-875.
10. King NJ, Eleonora G, Ollendick TH. Etiology of childhood phobias: current status of Rachman’s three pathways theory. Behav Res Ther. 1998; 36:297-309.
11. Fedoroff IC, Taylor S. Psychological and pharmacological treatments of social phobia: a meta-analysis. J Clin Psychopharmacol. 2001; 21:311-324.
12. Wolitzky-Taylor KB, Horowitz JD, Powers MB, et al. Psychological approaches in the treatment of specific phobias: a meta-analysis. Clin Psychol Rev. 2008; 28:1021-1037.
13. Zlomke K, Davis III TE. One-session treatment of specific phobias: a detailed description and review of treatment efficacy. Behav Ther. 2008; 39:207-223.
THE CASE
Joe S* is a 25-year-old white man who lives with his mother and has a 5-year history of worsening hypertension. He recently presented to the clinic with heart palpitations, shortness of breath, abdominal distress, and dizziness. He said that it was difficult for him to leave his home due to the intense fear he experiences. He said that these symptoms did not occur at home, nor when he visited specific “safe” locations, such as his girlfriend’s apartment. He reported that his fear had increased over the previous 2 years, and that he had progressively limited the distance he traveled from home. He also reported difficulty being in crowds and said, “The idea of going to the movies is torture.”
●
*The patient’s name has been changed to protect his identity.
The most prevalent psychiatric maladies in primary care are anxiety and mood disorders.1,2 Anxiety disorders are patterns of maladaptive behaviors in conjunction with or response to excessive fear or anxiety.3 The most prevalent anxiety disorder in the United States is specific phobia, the fear of a particular object or situation, with a 12-month prevalence rate of 12.1%.2
Other phobias diagnosed separately in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), include social phobia and agoraphobia, which are, respectively, the fear of being negatively evaluated in social situations and the fear of being trapped in public/open spaces. Social phobia and agoraphobia have diagnostic criteria nearly identical to those of simple phobias regarding the fear response, with the primary differences being the specific phobic situations or stimuli.
Unfortunately, these phobias are likely to be undiagnosed and untreated in primary care partly because patients may not seek treatment.4-6 The ease of avoiding some phobic situations contributes to a lack of treatment seeking.5 Furthermore, commonly used brief measures for psychiatric conditions generally identify depression and anxiety but not phobias. However, family physicians do have resources not only to diagnose these disorders, but also to work with patients to ameliorate them. Collaboration with behavioral health providers is key, as patients with phobias generally benefit from cognitive behavioral therapy (CBT), while those with comorbid psychiatric conditions may benefit from a combination of CBT and medication.
Phobic response vs adaptive fear and anxiety
The terms anxiety and fear often overlap when used to describe a negative emotional state of arousal. However, fear is a response to an actual (or perceived) imminent threat, whereas anxiety is the response to a perceived future threat.3 Fear, although unpleasant, serves an adaptive function in responding to immediate danger.7 Anxiety, in turn, may represent an adaptive function for future activities associated with fear. For example, a cave dweller having seen a bear enter a cave in the past (fear-evoking stimulus) may experience anxiety when exploring a different cave (anxiety that a bear may be present). In this situation, the cave dweller’s fear and anxiety responses are important for survival.
Continue to: With phobias...
With phobias, the fear and anxiety responses become maladaptive.3 Specifically, they involve inaccurate beliefs about a specific type of stimulus that could be an object (snake), environment (ocean), or situation (crowded room). Accompanying the maladaptive thoughts are correspondingly exaggerated emotions, physiologic effects, and behavioral responses in alignment with one another.8 The development of this response and the etiology of phobias is complex and is still being debated.7,9,10 Research points to 4 primary pathways: direct psychological conditioning, modeling (watching others), instruction/information, and nonassociative (innate) acquisition.7,10 While the first 3 pathways involve learned responses, the last results from biological predispositions.
DIAGNOSING PHOBIAS: WHAT TO ZERO IN ON
DSM-5 provides diagnostic criteria for specific phobia, agoraphobia, and social phobia, with each diagnosis requiring that symptoms be present for at least 6 months (TABLE 1).3 Diagnosis of phobias should include evaluation of 4 components of a patient’s functioning: subjective fears, cognitions, physiologic responses, and behaviors.8
- Subjective fears: the patient’s described level of distress/agitation to a specific stimulus.
- Cognitions: the patient’s thoughts/beliefs regarding the stimulus.
- Physiologic responses: changes in heart rate, respiration, blood pressure, and other sympathetic nervous system responses with exposure to stimuli.
- Behavioral responses: the most common response is avoidance, with displays of anger, irritability, or apprehension when avoidance of the stimulus is impossible.
Evaluating these 4 components can be accomplished with structured interviews, behavioral observations, or collateral reports from family members or the patient’s peers.8 Thorough questioning and evaluation (TABLE 28) can enable accurate differentiation between phobias unique to specific stimuli and other DSM-5 disorders that might cause similar symptoms. For example, a patient diagnosed with post-traumatic stress disorder (PTSD) might have a fear response even when triggering stimuli are not present. Identification of a clear, life-threatening incident could help with a differential between phobias and PTSD. However, a patient could be diagnosed with both disorders, as the 2 conditions are not mutually exclusive.
The physiologic and behavioral response symptoms of phobia can also mimic purely medical conditions. Hypertension or tachycardia observed during a medical visit could be due to the fear associated with agoraphobia or with a medically related specific phobia. Blood pressure elevated during testing at the medical appointment could be normal with at-home monitoring by the patient. Thus, blood pressure and heart rate screenings performed at home instead of in public places may help to rule out whether potentially elevated numbers are related to a fear response. Fear and avoidance-like symptoms can also be due to substance abuse, and appropriate drug screening can provide information for an accurate diagnosis.
HOW BEST TO TREAT PHOBIAS
Although research demonstrates that a variety of psychotherapeutic and pharmacologic treatments are efficacious for phobias, in some instances the true utility of an intervention to meaningfully improve a patient’s life is questionable. The issue is that the research evaluating treatment often evaluates only one component of a phobic response (eg,
Continue to: Psychotherapeutic interventions...
Psychotherapeutic interventions for phobias have shown substantial benefit. CBT is helpful, with the most efficacious technique being exposure therapy.5,6,8,11,12 CBT can begin during the initial primary care visit with the family physician educating the patient about phobias and available treatments.
With exposure therapy, patients are introduced to the source of anxiety over time, whereby they learn to manage the distress
Pharmacologic interventions—specifically selective serotonin reuptake inhibitors (SSRIs) and selective serotonin norepinephrine reuptake inhibitors (SNRIs)—have been effective in treating social phobia and agoraphobia.6 However, treatment of specific phobias via pharmacologic interventions is not supported due to limited efficacy and few studies for SSRIs and SNRIs.5,6
Benzodiazepines, although effective in alleviating some phobic symptoms, are not recommended per current guidelines due to adverse effects and potential exacerbation of the phobic response once discontinued.5,6 This poor result with benzodiazepines may be due to the absence of simultaneous emotional exposure to the feared stimuli. Unfortunately, little research has been done on the long-term effects of pharmacologic intervention once the treatment has been discontinued.11 So, for medication, the question of how long treatment effect lasts after discontinuation remains unanswered.
THE CASE
Mr. S’s family physician diagnosed his condition as agoraphobia with panic attacks. He was prescribed sertraline for his panic attacks and referred for CBT with a psychologist. CBT focused on cognitive restructuring as well as gradual exposure where he would travel with increasing distances to various locations. After 10 months of treatment, Mr. S was able to overcome the agoraphobia and took an “awesome” vacation. He also reported a significant decrease in panic symptoms.
CORRESPONDENCE
Scott A. Fields, PhD, 3200 MacCorkle Avenue Southeast, 5th Floor, Robert C. Byrd Clinical Teaching Center, Department of Family Medicine, Charleston, WV 25304; sfields@hsc.wvu.edu.
THE CASE
Joe S* is a 25-year-old white man who lives with his mother and has a 5-year history of worsening hypertension. He recently presented to the clinic with heart palpitations, shortness of breath, abdominal distress, and dizziness. He said that it was difficult for him to leave his home due to the intense fear he experiences. He said that these symptoms did not occur at home, nor when he visited specific “safe” locations, such as his girlfriend’s apartment. He reported that his fear had increased over the previous 2 years, and that he had progressively limited the distance he traveled from home. He also reported difficulty being in crowds and said, “The idea of going to the movies is torture.”
●
*The patient’s name has been changed to protect his identity.
The most prevalent psychiatric maladies in primary care are anxiety and mood disorders.1,2 Anxiety disorders are patterns of maladaptive behaviors in conjunction with or response to excessive fear or anxiety.3 The most prevalent anxiety disorder in the United States is specific phobia, the fear of a particular object or situation, with a 12-month prevalence rate of 12.1%.2
Other phobias diagnosed separately in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), include social phobia and agoraphobia, which are, respectively, the fear of being negatively evaluated in social situations and the fear of being trapped in public/open spaces. Social phobia and agoraphobia have diagnostic criteria nearly identical to those of simple phobias regarding the fear response, with the primary differences being the specific phobic situations or stimuli.
Unfortunately, these phobias are likely to be undiagnosed and untreated in primary care partly because patients may not seek treatment.4-6 The ease of avoiding some phobic situations contributes to a lack of treatment seeking.5 Furthermore, commonly used brief measures for psychiatric conditions generally identify depression and anxiety but not phobias. However, family physicians do have resources not only to diagnose these disorders, but also to work with patients to ameliorate them. Collaboration with behavioral health providers is key, as patients with phobias generally benefit from cognitive behavioral therapy (CBT), while those with comorbid psychiatric conditions may benefit from a combination of CBT and medication.
Phobic response vs adaptive fear and anxiety
The terms anxiety and fear often overlap when used to describe a negative emotional state of arousal. However, fear is a response to an actual (or perceived) imminent threat, whereas anxiety is the response to a perceived future threat.3 Fear, although unpleasant, serves an adaptive function in responding to immediate danger.7 Anxiety, in turn, may represent an adaptive function for future activities associated with fear. For example, a cave dweller having seen a bear enter a cave in the past (fear-evoking stimulus) may experience anxiety when exploring a different cave (anxiety that a bear may be present). In this situation, the cave dweller’s fear and anxiety responses are important for survival.
Continue to: With phobias...
With phobias, the fear and anxiety responses become maladaptive.3 Specifically, they involve inaccurate beliefs about a specific type of stimulus that could be an object (snake), environment (ocean), or situation (crowded room). Accompanying the maladaptive thoughts are correspondingly exaggerated emotions, physiologic effects, and behavioral responses in alignment with one another.8 The development of this response and the etiology of phobias is complex and is still being debated.7,9,10 Research points to 4 primary pathways: direct psychological conditioning, modeling (watching others), instruction/information, and nonassociative (innate) acquisition.7,10 While the first 3 pathways involve learned responses, the last results from biological predispositions.
DIAGNOSING PHOBIAS: WHAT TO ZERO IN ON
DSM-5 provides diagnostic criteria for specific phobia, agoraphobia, and social phobia, with each diagnosis requiring that symptoms be present for at least 6 months (TABLE 1).3 Diagnosis of phobias should include evaluation of 4 components of a patient’s functioning: subjective fears, cognitions, physiologic responses, and behaviors.8
- Subjective fears: the patient’s described level of distress/agitation to a specific stimulus.
- Cognitions: the patient’s thoughts/beliefs regarding the stimulus.
- Physiologic responses: changes in heart rate, respiration, blood pressure, and other sympathetic nervous system responses with exposure to stimuli.
- Behavioral responses: the most common response is avoidance, with displays of anger, irritability, or apprehension when avoidance of the stimulus is impossible.
Evaluating these 4 components can be accomplished with structured interviews, behavioral observations, or collateral reports from family members or the patient’s peers.8 Thorough questioning and evaluation (TABLE 28) can enable accurate differentiation between phobias unique to specific stimuli and other DSM-5 disorders that might cause similar symptoms. For example, a patient diagnosed with post-traumatic stress disorder (PTSD) might have a fear response even when triggering stimuli are not present. Identification of a clear, life-threatening incident could help with a differential between phobias and PTSD. However, a patient could be diagnosed with both disorders, as the 2 conditions are not mutually exclusive.
The physiologic and behavioral response symptoms of phobia can also mimic purely medical conditions. Hypertension or tachycardia observed during a medical visit could be due to the fear associated with agoraphobia or with a medically related specific phobia. Blood pressure elevated during testing at the medical appointment could be normal with at-home monitoring by the patient. Thus, blood pressure and heart rate screenings performed at home instead of in public places may help to rule out whether potentially elevated numbers are related to a fear response. Fear and avoidance-like symptoms can also be due to substance abuse, and appropriate drug screening can provide information for an accurate diagnosis.
HOW BEST TO TREAT PHOBIAS
Although research demonstrates that a variety of psychotherapeutic and pharmacologic treatments are efficacious for phobias, in some instances the true utility of an intervention to meaningfully improve a patient’s life is questionable. The issue is that the research evaluating treatment often evaluates only one component of a phobic response (eg,
Continue to: Psychotherapeutic interventions...
Psychotherapeutic interventions for phobias have shown substantial benefit. CBT is helpful, with the most efficacious technique being exposure therapy.5,6,8,11,12 CBT can begin during the initial primary care visit with the family physician educating the patient about phobias and available treatments.
With exposure therapy, patients are introduced to the source of anxiety over time, whereby they learn to manage the distress
Pharmacologic interventions—specifically selective serotonin reuptake inhibitors (SSRIs) and selective serotonin norepinephrine reuptake inhibitors (SNRIs)—have been effective in treating social phobia and agoraphobia.6 However, treatment of specific phobias via pharmacologic interventions is not supported due to limited efficacy and few studies for SSRIs and SNRIs.5,6
Benzodiazepines, although effective in alleviating some phobic symptoms, are not recommended per current guidelines due to adverse effects and potential exacerbation of the phobic response once discontinued.5,6 This poor result with benzodiazepines may be due to the absence of simultaneous emotional exposure to the feared stimuli. Unfortunately, little research has been done on the long-term effects of pharmacologic intervention once the treatment has been discontinued.11 So, for medication, the question of how long treatment effect lasts after discontinuation remains unanswered.
THE CASE
Mr. S’s family physician diagnosed his condition as agoraphobia with panic attacks. He was prescribed sertraline for his panic attacks and referred for CBT with a psychologist. CBT focused on cognitive restructuring as well as gradual exposure where he would travel with increasing distances to various locations. After 10 months of treatment, Mr. S was able to overcome the agoraphobia and took an “awesome” vacation. He also reported a significant decrease in panic symptoms.
CORRESPONDENCE
Scott A. Fields, PhD, 3200 MacCorkle Avenue Southeast, 5th Floor, Robert C. Byrd Clinical Teaching Center, Department of Family Medicine, Charleston, WV 25304; sfields@hsc.wvu.edu.
1. Simon G, Ormel J, VonKorff M, et al. Health care costs associated with depressive and anxiety disorders in primary care. Am J Psychiatry. 1995; 152:352-357.
2. Kessler RC, Petukhova M, Sampson NA, et al. Twelve‐month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Methods Psychiatr Res. 2012; 21:169-184.
3. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth edition (DSM-5). Arlington, VA: American Psychiatric Association; 2013:189-233.
4. Bandelow B, Michaelis S. Epidemiology of anxiety disorders in the 21st century. Dialogues Clin Neurosci. 2015; 17:327-335.
5. Choy Y, Fyer AJ, Lipsitz JD. Treatment of specific phobia in adults. Clin Psychol Rev. 2007; 27:266-286.
6. Bandelow B, Michaelis S, Wedekind D. Treatment of anxiety disorders. Dialogues Clin Neurosci. 2017; 19:93-107.
7. Poulton R, Menzies RG. Non-associative fear acquisition: a review of the evidence from retrospective and longitudinal research. Behav Res Ther. 2002; 40:127-149.
8. Davis III TE, Ollendick TH. Empirically supported treatments for specific phobia in children: Do efficacious treatments address the components of a phobic response? Clin Psychol Sci Pract. 2005; 12:144-160.
9. Field AP. Is conditioning a useful framework for understanding the development and treatment of phobias? Clin Psychol Rev. 2006; 26:857-875.
10. King NJ, Eleonora G, Ollendick TH. Etiology of childhood phobias: current status of Rachman’s three pathways theory. Behav Res Ther. 1998; 36:297-309.
11. Fedoroff IC, Taylor S. Psychological and pharmacological treatments of social phobia: a meta-analysis. J Clin Psychopharmacol. 2001; 21:311-324.
12. Wolitzky-Taylor KB, Horowitz JD, Powers MB, et al. Psychological approaches in the treatment of specific phobias: a meta-analysis. Clin Psychol Rev. 2008; 28:1021-1037.
13. Zlomke K, Davis III TE. One-session treatment of specific phobias: a detailed description and review of treatment efficacy. Behav Ther. 2008; 39:207-223.
1. Simon G, Ormel J, VonKorff M, et al. Health care costs associated with depressive and anxiety disorders in primary care. Am J Psychiatry. 1995; 152:352-357.
2. Kessler RC, Petukhova M, Sampson NA, et al. Twelve‐month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Methods Psychiatr Res. 2012; 21:169-184.
3. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth edition (DSM-5). Arlington, VA: American Psychiatric Association; 2013:189-233.
4. Bandelow B, Michaelis S. Epidemiology of anxiety disorders in the 21st century. Dialogues Clin Neurosci. 2015; 17:327-335.
5. Choy Y, Fyer AJ, Lipsitz JD. Treatment of specific phobia in adults. Clin Psychol Rev. 2007; 27:266-286.
6. Bandelow B, Michaelis S, Wedekind D. Treatment of anxiety disorders. Dialogues Clin Neurosci. 2017; 19:93-107.
7. Poulton R, Menzies RG. Non-associative fear acquisition: a review of the evidence from retrospective and longitudinal research. Behav Res Ther. 2002; 40:127-149.
8. Davis III TE, Ollendick TH. Empirically supported treatments for specific phobia in children: Do efficacious treatments address the components of a phobic response? Clin Psychol Sci Pract. 2005; 12:144-160.
9. Field AP. Is conditioning a useful framework for understanding the development and treatment of phobias? Clin Psychol Rev. 2006; 26:857-875.
10. King NJ, Eleonora G, Ollendick TH. Etiology of childhood phobias: current status of Rachman’s three pathways theory. Behav Res Ther. 1998; 36:297-309.
11. Fedoroff IC, Taylor S. Psychological and pharmacological treatments of social phobia: a meta-analysis. J Clin Psychopharmacol. 2001; 21:311-324.
12. Wolitzky-Taylor KB, Horowitz JD, Powers MB, et al. Psychological approaches in the treatment of specific phobias: a meta-analysis. Clin Psychol Rev. 2008; 28:1021-1037.
13. Zlomke K, Davis III TE. One-session treatment of specific phobias: a detailed description and review of treatment efficacy. Behav Ther. 2008; 39:207-223.
How to treat complicated grief
THE CASE
Al* is a 48-year-old patient whose wife, Vera, died of complications from chronic illness 14 months ago. Al thinks about Vera constantly and says he still has difficulty accepting that she is gone. He does not leave the house much anymore and continues to set a place for her at the kitchen table on special occasions. He says, “Some nights in bed, I swear I can hear her in the living room.”
How would you proceed with this patient?
* The names of the patient and his spouse have been changed to protect their identities.
After the loss of a loved one, grief is a natural response to the separation and stress that go along with the death. Most people, after suffering a loss, experience distress that varies in intensity and gradually decreases over time. Thus, the grieving individual does not act as they would normally if they were not bereaved. However, gains are generally made month by month, and most people adjust to the grief and adapt their lives after some time dealing with the absence of the loved one.1
There’s grief, and then there’s complicated grief
For about 2% to 4% of the population who have experienced a significant loss, complicated grief is an issue.2 As its hallmark, complicated grief exceeds the typical amount of time (6-12 months) that people need to recover from a loss. Prevalence has been estimated at 10% to 20% among grieving individuals for whom the death being grieved was that of a romantic partner or child.2 At increased risk for this disorder are women older than 60 years, patients diagnosed with depression or substance abuse, individuals under financial strain, and those who have experienced a violent or sudden loss.3
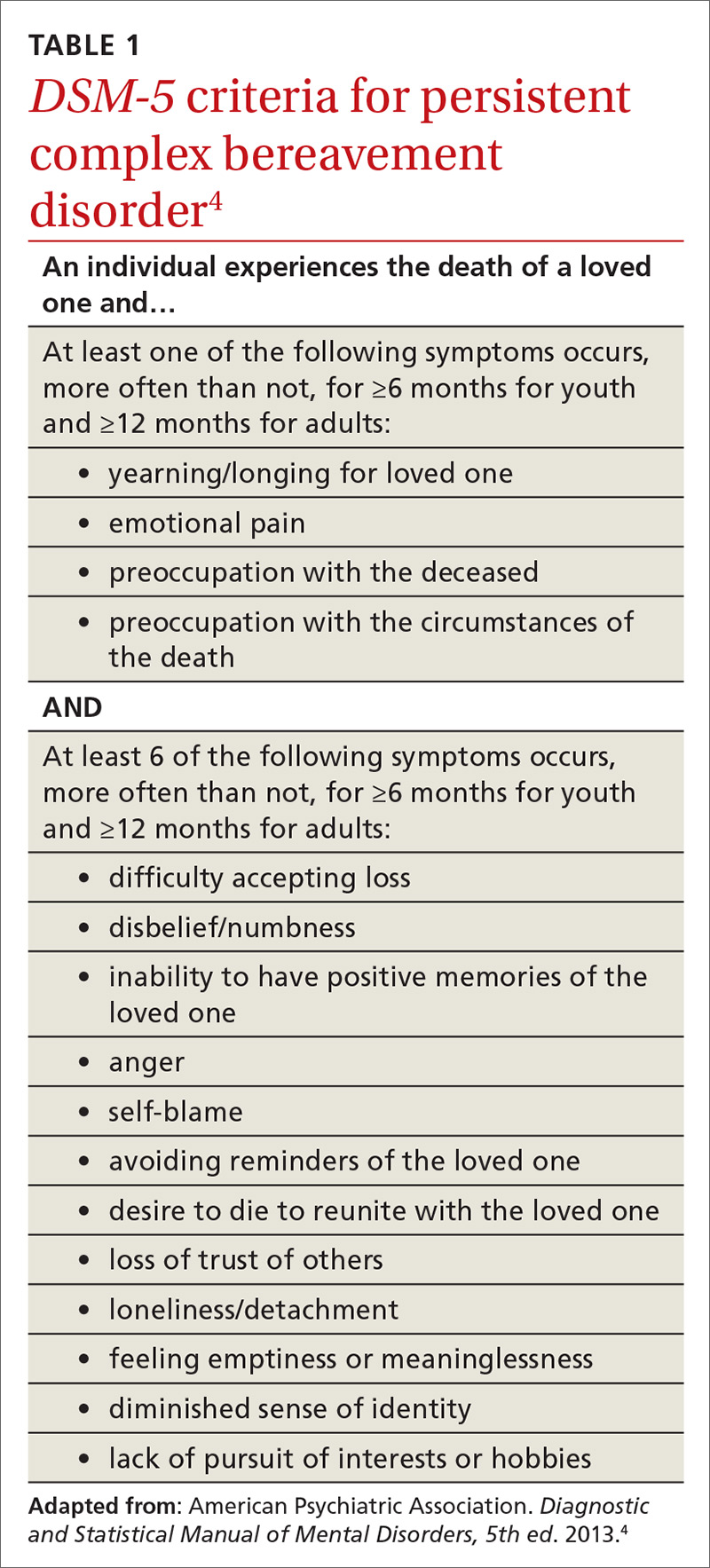
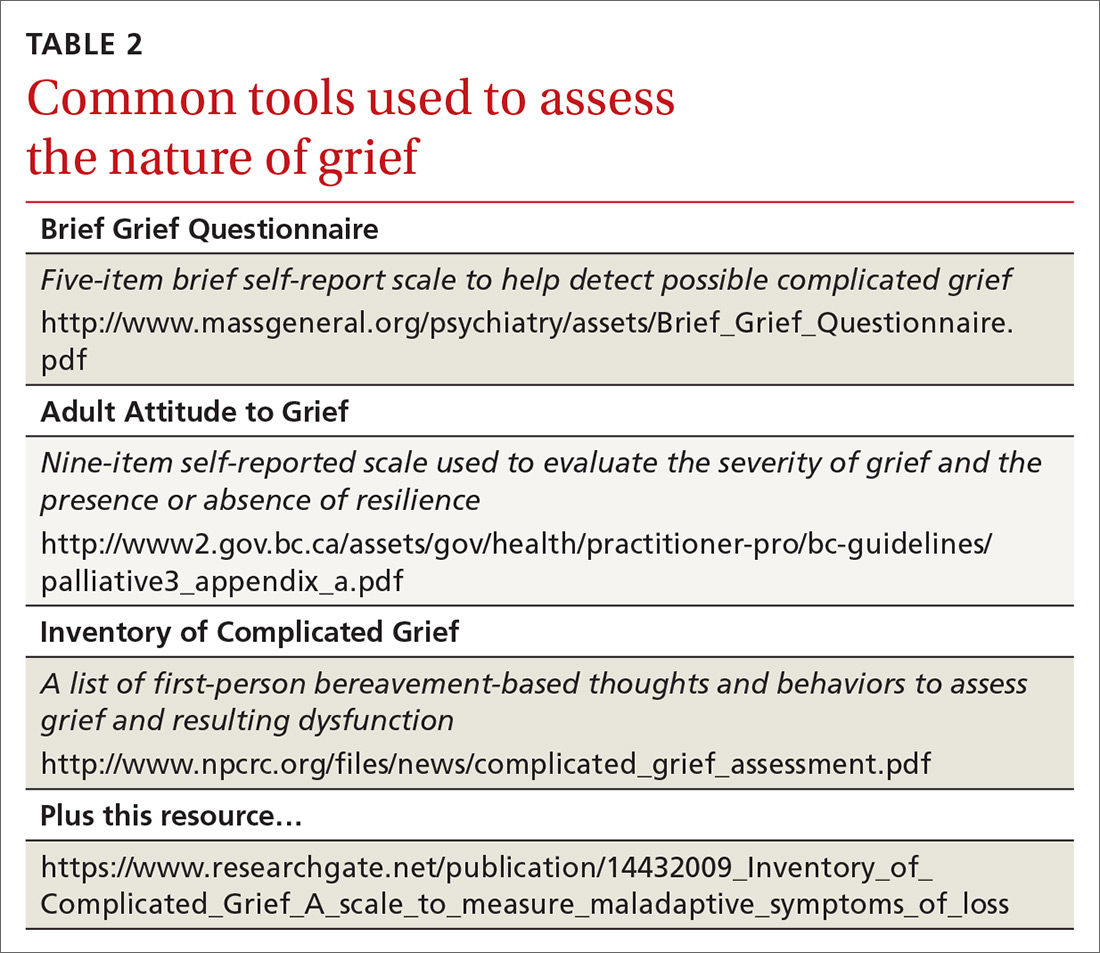
The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) has conceptualized complicated grief with the name, persistent complex bereavement disorder (PCBD).4 While the guidelines for the definition are still in progress, several specified symptoms must have been present for at least 6 months to a year or more (TABLE 14). For instance, the patient has been ruminating about the death, has been unable to accept the death, or has felt shocked or numb. They may also experience anger, have difficulty trusting others, and be preoccupied with the deceased (eg, sense they can hear their lost loved one, feel the loved one’s pain for them). Symptoms of PCBD may also include experiencing vivid reminders of the loss and avoiding situations that bring up thoughts about the death.4 (Of note: A grief diagnosis in ICD-10 is captured by the code F43.21; however, there is no specific code for complicated grief or PCBD.)
PCBD is a “condition for further study” in DSM-5; it was omitted from DSM-IV only after much debate. One reason for its omission was concern that clinicians might “pathologize” grief more than it needs to be.5 Grief is regarded as a natural process that might be stymied by a formal diagnosis leading to medical treatment.
Shifting the grief diagnosis paradigm
One new development is that recently bereaved patients can be diagnosed with depression if they meet the criteria for that diagnosis. In the past, someone who met criteria for major depression would be excluded from that diagnosis if the depression ensued from grief. DSM-5 no longer makes that distinction.4 Given this diagnostic shift, one might wonder about the difference between PCBD and depression, particularly if the patient is a grieving individual with a current diagnosis of depression.5
Continue to: Differences between PCBD and major depression
Differences between PCBD and major depression. While antidepressant medication is helpful for patients with moderate-to-severe depression, it has thus far been less helpful for those solely experiencing complicated grief.6 The same holds true for traditional psychotherapy. While family physicians can confidently refer people to psychotherapy for depression, it is not as efficacious as focused therapy designed for those with PCBD.6
Other differences between PCBD and major depression involve the constructs of guilt and yearning. Depressed patients typically feel guilty about a number of things, while those with complicated grief have specific death-focused guilt.7 Depressed people generally do not yearn, while those with grief yearn for their loved one. Finally, and most concerning to clinicians, some patients with PCBD have suicidal thoughts.8 While such thoughts in depression are often linked to hopelessness, suicidal thoughts for grieving individuals are generally driven by a desire to be reunited with the deceased loved one.
While these differences may help in making treatment decisions, there can be overlap between depression and complicated grief. As with many mental health diagnoses, major depression and PCBD are not mutually exclusive.4
The role of hospice. Another factor sometimes associated with complicated grief is any hindrance to the survivor’s ability to communicate or say goodbye to the loved one at the end of life.9 This may be avoided if the loved one is in hospice care and is not subjected to procedures that impair communication (ie, ventilator use, sedation). Medicare requires that certified hospice programs offer bereavement services for 1 year following patient death.10 Some hospice providers even offer bereavement services to those not enrolled in hospice. However, evidence indicates that only about 30% of bereaved caregivers take advantage of hospice bereavement services.11 Family physicians may help patients during this process by providing an early referral to hospice services and recommending bereavement counseling. Referral to hospice care can also facilitate discussions that the patient may need to have with the physician or others regarding spirituality. Hospital chaplains can also be referred or get involved with patients and family upon request.
Assessment focal points and tools
As is the case with most mental health concerns, primary care is at the forefront of early assessment. Evaluation of grief is an ongoing process and is multifactorial. One focus is the intensity of the grief. Is the patient reacting to the loss in a way that is disproportionately severe when compared with others who grieve? Another factor is the time elapsed since the loss. If the loss was more than 6 months ago, the patient should have made some progress. Assess grieving patients at around 6 months post-loss to determine how they are handling grief. As mentioned, DSM-5 has criteria for PCBD that providers can use in determining a patient’s grief status. Also needed are assessments for the other DSM-5 issues often associated with loss: depression and post-traumatic stress disorder.
Continue to: While no clinical measure is perfect...
While no clinical measure is perfect, there are tools that can help in assessing patients for the possibility of complicated grief (TABLE 2). Also keep in mind that no measure can make a diagnosis of PCBD, as it is a clinical judgment, not a score on a scale. Furthermore, there is no measure that can accurately predict future complicated grief.6 In most busy practices, the Brief Grief Questionnaire (http://www.massgeneral.org/psychiatry/assets/Brief_Grief_Questionnaire.pdf ) would be the easiest tool to administer, but a case could be made for any of the measures.
Treatment
The literature base emphasizes that PCBD treatment requires a different focus than that applied to uncomplicated grief. And while most people with major depression will respond to medication and psychotherapy, there are provisos to keep in mind when depression is associated with complicated grief.
Complicated grief treatment (CGT) has been studied extensively.6 This treatment combines some of the tenets of evidence-based PTSD treatments, interpersonal therapy for grief, and cognitive behavioral therapy. CGT is generally an individual treatment, although group therapy using some of its tenets can also be effective. According to complicated grief researchers, tasks to accomplish in CGT include establishing a “new normal” following the loss, promoting self-regulation in the grieving, building social connections, and setting aspirational goals for the future.6 Other goals are to revisit the world, tell stories of the past, and relive old memories in a more positive light. Common suggestions in CGT that run parallel to conventional thoughts on dealing with grief include increasing time outside the home, getting more involved interpersonally, and increasing mindfulness-based practices.
A second-line evidence-based treatment for PCBD is the use of selective serotonin-reuptake inhibitors (SSRIs).6 Some studies have found benefit from SSRI treatment, although the findings are preliminary and modest.12 One observational study examined patients who had recently experienced loss and were receiving CGT with or without medication. Researchers found that CGT with medication (citalopram) led to a 61% positive response rate while CGT alone led to a 41% response rate.13 Thus, findings revealed some benefit to combining an antidepressant with CGT, indicating that SSRIs may be helpful as an adjunct treatment.
THE CASE
Al was treated for complicated grief by his family physician and a psychologist for approximately a year. He responded well to an SSRI and received psychotherapy that focused on the tenets of CGT. Prior to his last psychotherapy visit, he reported leaving the house regularly to dine at restaurants and meet up with co-workers after hours. He said, “I still miss Vera quite a bit, but I know that I feel better.”
CORRESPONDENCE
Scott A. Fields, PhD, 3200 MacCorkle Avenue Southeast, 5th Floor, Robert C. Byrd Clinical Teaching Center, Department of Family Medicine, Charleston, WV 25304; sfields@hsc.wvu.edu
1. Cozza SJ, Fisher JE, Mauro C, et al. Performance of DSM-5 persistent complex bereavement disorder criteria in a community sample of bereaved military family members. Am J Psychiatry. 2016;173:919-929.
2. Kersting A, Brähler E, Glaesmer H, et al. Prevalence of complicated grief in a representative population-based sample. J Affect Disord. 2011;131:339-343.
3. Fujisawa D, Miyashita M, Nakajima S, et al. Prevalence and determinants of complicated grief in general population. J Affect Disord. 2010;127:352-358.
4. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: APA Press; 2013.
5. Shear MK, Simon N, Wall M, et al. Complicated grief and related issues for DSM-5. Depress Anxiety. 2011;28:103-117.
6. Shear MK. Clinical Practice. Complicated grief. N Engl J Med. 2015;372:153-160.
7. Wolfelt AD. Counseling Skills for Companioning the Mourner: The Fundamentals of Effective Grief Counseling. Fort Collins, CO: Companion Press; 2016.
8. Szanto K, Shear MK, Houck PR, et al. Indirect self-destructive behavior and overt suicidality in patients with complicated grief. J Clin Psychiatry. 2006;67:233-239.
9. Otani H, Yoshida S, Morita T, et al. Meaningful communication before death, but not present at the time of death itself, is associated with better outcomes on measures of depression and complicated grief among bereaved family members of cancer patients. J Pain Symptom Manage. 2017;54:273-279.
10. CMS. Medicare benefit policy manual: coverage of hospice services under hospital insurance. www.cms.gov/Regulations-and-guidance/Guidance/Manuals/downloads/bp102c09.pdf. Accessed February 25, 2018.
11. Cherlin E, Barry LC, Prigerson H, et al. Bereavement services for family caregivers: how often used, why, and why not. J Palliat Med. 2007;10:148–158.
12. Bui E, Nidal-Vicens M, Simon NM. Pharmacologic approaches to the treatment of complicated grief: rationale and a brief review of the literature. Dialogues Clin Neurosci. 2012;14:149-157.
13. Shear MK, Reynolds CF 3rd, Simon NM, et al. Optimizing treatment of complicated grief: a randomized clinical trial. JAMA Psychiatry. 2016;73:685-694.
THE CASE
Al* is a 48-year-old patient whose wife, Vera, died of complications from chronic illness 14 months ago. Al thinks about Vera constantly and says he still has difficulty accepting that she is gone. He does not leave the house much anymore and continues to set a place for her at the kitchen table on special occasions. He says, “Some nights in bed, I swear I can hear her in the living room.”
How would you proceed with this patient?
* The names of the patient and his spouse have been changed to protect their identities.
After the loss of a loved one, grief is a natural response to the separation and stress that go along with the death. Most people, after suffering a loss, experience distress that varies in intensity and gradually decreases over time. Thus, the grieving individual does not act as they would normally if they were not bereaved. However, gains are generally made month by month, and most people adjust to the grief and adapt their lives after some time dealing with the absence of the loved one.1
There’s grief, and then there’s complicated grief
For about 2% to 4% of the population who have experienced a significant loss, complicated grief is an issue.2 As its hallmark, complicated grief exceeds the typical amount of time (6-12 months) that people need to recover from a loss. Prevalence has been estimated at 10% to 20% among grieving individuals for whom the death being grieved was that of a romantic partner or child.2 At increased risk for this disorder are women older than 60 years, patients diagnosed with depression or substance abuse, individuals under financial strain, and those who have experienced a violent or sudden loss.3
The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) has conceptualized complicated grief with the name, persistent complex bereavement disorder (PCBD).4 While the guidelines for the definition are still in progress, several specified symptoms must have been present for at least 6 months to a year or more (TABLE 14). For instance, the patient has been ruminating about the death, has been unable to accept the death, or has felt shocked or numb. They may also experience anger, have difficulty trusting others, and be preoccupied with the deceased (eg, sense they can hear their lost loved one, feel the loved one’s pain for them). Symptoms of PCBD may also include experiencing vivid reminders of the loss and avoiding situations that bring up thoughts about the death.4 (Of note: A grief diagnosis in ICD-10 is captured by the code F43.21; however, there is no specific code for complicated grief or PCBD.)
PCBD is a “condition for further study” in DSM-5; it was omitted from DSM-IV only after much debate. One reason for its omission was concern that clinicians might “pathologize” grief more than it needs to be.5 Grief is regarded as a natural process that might be stymied by a formal diagnosis leading to medical treatment.
Shifting the grief diagnosis paradigm
One new development is that recently bereaved patients can be diagnosed with depression if they meet the criteria for that diagnosis. In the past, someone who met criteria for major depression would be excluded from that diagnosis if the depression ensued from grief. DSM-5 no longer makes that distinction.4 Given this diagnostic shift, one might wonder about the difference between PCBD and depression, particularly if the patient is a grieving individual with a current diagnosis of depression.5
Continue to: Differences between PCBD and major depression
Differences between PCBD and major depression. While antidepressant medication is helpful for patients with moderate-to-severe depression, it has thus far been less helpful for those solely experiencing complicated grief.6 The same holds true for traditional psychotherapy. While family physicians can confidently refer people to psychotherapy for depression, it is not as efficacious as focused therapy designed for those with PCBD.6
Other differences between PCBD and major depression involve the constructs of guilt and yearning. Depressed patients typically feel guilty about a number of things, while those with complicated grief have specific death-focused guilt.7 Depressed people generally do not yearn, while those with grief yearn for their loved one. Finally, and most concerning to clinicians, some patients with PCBD have suicidal thoughts.8 While such thoughts in depression are often linked to hopelessness, suicidal thoughts for grieving individuals are generally driven by a desire to be reunited with the deceased loved one.
While these differences may help in making treatment decisions, there can be overlap between depression and complicated grief. As with many mental health diagnoses, major depression and PCBD are not mutually exclusive.4
The role of hospice. Another factor sometimes associated with complicated grief is any hindrance to the survivor’s ability to communicate or say goodbye to the loved one at the end of life.9 This may be avoided if the loved one is in hospice care and is not subjected to procedures that impair communication (ie, ventilator use, sedation). Medicare requires that certified hospice programs offer bereavement services for 1 year following patient death.10 Some hospice providers even offer bereavement services to those not enrolled in hospice. However, evidence indicates that only about 30% of bereaved caregivers take advantage of hospice bereavement services.11 Family physicians may help patients during this process by providing an early referral to hospice services and recommending bereavement counseling. Referral to hospice care can also facilitate discussions that the patient may need to have with the physician or others regarding spirituality. Hospital chaplains can also be referred or get involved with patients and family upon request.
Assessment focal points and tools
As is the case with most mental health concerns, primary care is at the forefront of early assessment. Evaluation of grief is an ongoing process and is multifactorial. One focus is the intensity of the grief. Is the patient reacting to the loss in a way that is disproportionately severe when compared with others who grieve? Another factor is the time elapsed since the loss. If the loss was more than 6 months ago, the patient should have made some progress. Assess grieving patients at around 6 months post-loss to determine how they are handling grief. As mentioned, DSM-5 has criteria for PCBD that providers can use in determining a patient’s grief status. Also needed are assessments for the other DSM-5 issues often associated with loss: depression and post-traumatic stress disorder.
Continue to: While no clinical measure is perfect...
While no clinical measure is perfect, there are tools that can help in assessing patients for the possibility of complicated grief (TABLE 2). Also keep in mind that no measure can make a diagnosis of PCBD, as it is a clinical judgment, not a score on a scale. Furthermore, there is no measure that can accurately predict future complicated grief.6 In most busy practices, the Brief Grief Questionnaire (http://www.massgeneral.org/psychiatry/assets/Brief_Grief_Questionnaire.pdf ) would be the easiest tool to administer, but a case could be made for any of the measures.
Treatment
The literature base emphasizes that PCBD treatment requires a different focus than that applied to uncomplicated grief. And while most people with major depression will respond to medication and psychotherapy, there are provisos to keep in mind when depression is associated with complicated grief.
Complicated grief treatment (CGT) has been studied extensively.6 This treatment combines some of the tenets of evidence-based PTSD treatments, interpersonal therapy for grief, and cognitive behavioral therapy. CGT is generally an individual treatment, although group therapy using some of its tenets can also be effective. According to complicated grief researchers, tasks to accomplish in CGT include establishing a “new normal” following the loss, promoting self-regulation in the grieving, building social connections, and setting aspirational goals for the future.6 Other goals are to revisit the world, tell stories of the past, and relive old memories in a more positive light. Common suggestions in CGT that run parallel to conventional thoughts on dealing with grief include increasing time outside the home, getting more involved interpersonally, and increasing mindfulness-based practices.
A second-line evidence-based treatment for PCBD is the use of selective serotonin-reuptake inhibitors (SSRIs).6 Some studies have found benefit from SSRI treatment, although the findings are preliminary and modest.12 One observational study examined patients who had recently experienced loss and were receiving CGT with or without medication. Researchers found that CGT with medication (citalopram) led to a 61% positive response rate while CGT alone led to a 41% response rate.13 Thus, findings revealed some benefit to combining an antidepressant with CGT, indicating that SSRIs may be helpful as an adjunct treatment.
THE CASE
Al was treated for complicated grief by his family physician and a psychologist for approximately a year. He responded well to an SSRI and received psychotherapy that focused on the tenets of CGT. Prior to his last psychotherapy visit, he reported leaving the house regularly to dine at restaurants and meet up with co-workers after hours. He said, “I still miss Vera quite a bit, but I know that I feel better.”
CORRESPONDENCE
Scott A. Fields, PhD, 3200 MacCorkle Avenue Southeast, 5th Floor, Robert C. Byrd Clinical Teaching Center, Department of Family Medicine, Charleston, WV 25304; sfields@hsc.wvu.edu
THE CASE
Al* is a 48-year-old patient whose wife, Vera, died of complications from chronic illness 14 months ago. Al thinks about Vera constantly and says he still has difficulty accepting that she is gone. He does not leave the house much anymore and continues to set a place for her at the kitchen table on special occasions. He says, “Some nights in bed, I swear I can hear her in the living room.”
How would you proceed with this patient?
* The names of the patient and his spouse have been changed to protect their identities.
After the loss of a loved one, grief is a natural response to the separation and stress that go along with the death. Most people, after suffering a loss, experience distress that varies in intensity and gradually decreases over time. Thus, the grieving individual does not act as they would normally if they were not bereaved. However, gains are generally made month by month, and most people adjust to the grief and adapt their lives after some time dealing with the absence of the loved one.1
There’s grief, and then there’s complicated grief
For about 2% to 4% of the population who have experienced a significant loss, complicated grief is an issue.2 As its hallmark, complicated grief exceeds the typical amount of time (6-12 months) that people need to recover from a loss. Prevalence has been estimated at 10% to 20% among grieving individuals for whom the death being grieved was that of a romantic partner or child.2 At increased risk for this disorder are women older than 60 years, patients diagnosed with depression or substance abuse, individuals under financial strain, and those who have experienced a violent or sudden loss.3
The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) has conceptualized complicated grief with the name, persistent complex bereavement disorder (PCBD).4 While the guidelines for the definition are still in progress, several specified symptoms must have been present for at least 6 months to a year or more (TABLE 14). For instance, the patient has been ruminating about the death, has been unable to accept the death, or has felt shocked or numb. They may also experience anger, have difficulty trusting others, and be preoccupied with the deceased (eg, sense they can hear their lost loved one, feel the loved one’s pain for them). Symptoms of PCBD may also include experiencing vivid reminders of the loss and avoiding situations that bring up thoughts about the death.4 (Of note: A grief diagnosis in ICD-10 is captured by the code F43.21; however, there is no specific code for complicated grief or PCBD.)
PCBD is a “condition for further study” in DSM-5; it was omitted from DSM-IV only after much debate. One reason for its omission was concern that clinicians might “pathologize” grief more than it needs to be.5 Grief is regarded as a natural process that might be stymied by a formal diagnosis leading to medical treatment.
Shifting the grief diagnosis paradigm
One new development is that recently bereaved patients can be diagnosed with depression if they meet the criteria for that diagnosis. In the past, someone who met criteria for major depression would be excluded from that diagnosis if the depression ensued from grief. DSM-5 no longer makes that distinction.4 Given this diagnostic shift, one might wonder about the difference between PCBD and depression, particularly if the patient is a grieving individual with a current diagnosis of depression.5
Continue to: Differences between PCBD and major depression
Differences between PCBD and major depression. While antidepressant medication is helpful for patients with moderate-to-severe depression, it has thus far been less helpful for those solely experiencing complicated grief.6 The same holds true for traditional psychotherapy. While family physicians can confidently refer people to psychotherapy for depression, it is not as efficacious as focused therapy designed for those with PCBD.6
Other differences between PCBD and major depression involve the constructs of guilt and yearning. Depressed patients typically feel guilty about a number of things, while those with complicated grief have specific death-focused guilt.7 Depressed people generally do not yearn, while those with grief yearn for their loved one. Finally, and most concerning to clinicians, some patients with PCBD have suicidal thoughts.8 While such thoughts in depression are often linked to hopelessness, suicidal thoughts for grieving individuals are generally driven by a desire to be reunited with the deceased loved one.
While these differences may help in making treatment decisions, there can be overlap between depression and complicated grief. As with many mental health diagnoses, major depression and PCBD are not mutually exclusive.4
The role of hospice. Another factor sometimes associated with complicated grief is any hindrance to the survivor’s ability to communicate or say goodbye to the loved one at the end of life.9 This may be avoided if the loved one is in hospice care and is not subjected to procedures that impair communication (ie, ventilator use, sedation). Medicare requires that certified hospice programs offer bereavement services for 1 year following patient death.10 Some hospice providers even offer bereavement services to those not enrolled in hospice. However, evidence indicates that only about 30% of bereaved caregivers take advantage of hospice bereavement services.11 Family physicians may help patients during this process by providing an early referral to hospice services and recommending bereavement counseling. Referral to hospice care can also facilitate discussions that the patient may need to have with the physician or others regarding spirituality. Hospital chaplains can also be referred or get involved with patients and family upon request.
Assessment focal points and tools
As is the case with most mental health concerns, primary care is at the forefront of early assessment. Evaluation of grief is an ongoing process and is multifactorial. One focus is the intensity of the grief. Is the patient reacting to the loss in a way that is disproportionately severe when compared with others who grieve? Another factor is the time elapsed since the loss. If the loss was more than 6 months ago, the patient should have made some progress. Assess grieving patients at around 6 months post-loss to determine how they are handling grief. As mentioned, DSM-5 has criteria for PCBD that providers can use in determining a patient’s grief status. Also needed are assessments for the other DSM-5 issues often associated with loss: depression and post-traumatic stress disorder.
Continue to: While no clinical measure is perfect...
While no clinical measure is perfect, there are tools that can help in assessing patients for the possibility of complicated grief (TABLE 2). Also keep in mind that no measure can make a diagnosis of PCBD, as it is a clinical judgment, not a score on a scale. Furthermore, there is no measure that can accurately predict future complicated grief.6 In most busy practices, the Brief Grief Questionnaire (http://www.massgeneral.org/psychiatry/assets/Brief_Grief_Questionnaire.pdf ) would be the easiest tool to administer, but a case could be made for any of the measures.
Treatment
The literature base emphasizes that PCBD treatment requires a different focus than that applied to uncomplicated grief. And while most people with major depression will respond to medication and psychotherapy, there are provisos to keep in mind when depression is associated with complicated grief.
Complicated grief treatment (CGT) has been studied extensively.6 This treatment combines some of the tenets of evidence-based PTSD treatments, interpersonal therapy for grief, and cognitive behavioral therapy. CGT is generally an individual treatment, although group therapy using some of its tenets can also be effective. According to complicated grief researchers, tasks to accomplish in CGT include establishing a “new normal” following the loss, promoting self-regulation in the grieving, building social connections, and setting aspirational goals for the future.6 Other goals are to revisit the world, tell stories of the past, and relive old memories in a more positive light. Common suggestions in CGT that run parallel to conventional thoughts on dealing with grief include increasing time outside the home, getting more involved interpersonally, and increasing mindfulness-based practices.
A second-line evidence-based treatment for PCBD is the use of selective serotonin-reuptake inhibitors (SSRIs).6 Some studies have found benefit from SSRI treatment, although the findings are preliminary and modest.12 One observational study examined patients who had recently experienced loss and were receiving CGT with or without medication. Researchers found that CGT with medication (citalopram) led to a 61% positive response rate while CGT alone led to a 41% response rate.13 Thus, findings revealed some benefit to combining an antidepressant with CGT, indicating that SSRIs may be helpful as an adjunct treatment.
THE CASE
Al was treated for complicated grief by his family physician and a psychologist for approximately a year. He responded well to an SSRI and received psychotherapy that focused on the tenets of CGT. Prior to his last psychotherapy visit, he reported leaving the house regularly to dine at restaurants and meet up with co-workers after hours. He said, “I still miss Vera quite a bit, but I know that I feel better.”
CORRESPONDENCE
Scott A. Fields, PhD, 3200 MacCorkle Avenue Southeast, 5th Floor, Robert C. Byrd Clinical Teaching Center, Department of Family Medicine, Charleston, WV 25304; sfields@hsc.wvu.edu
1. Cozza SJ, Fisher JE, Mauro C, et al. Performance of DSM-5 persistent complex bereavement disorder criteria in a community sample of bereaved military family members. Am J Psychiatry. 2016;173:919-929.
2. Kersting A, Brähler E, Glaesmer H, et al. Prevalence of complicated grief in a representative population-based sample. J Affect Disord. 2011;131:339-343.
3. Fujisawa D, Miyashita M, Nakajima S, et al. Prevalence and determinants of complicated grief in general population. J Affect Disord. 2010;127:352-358.
4. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: APA Press; 2013.
5. Shear MK, Simon N, Wall M, et al. Complicated grief and related issues for DSM-5. Depress Anxiety. 2011;28:103-117.
6. Shear MK. Clinical Practice. Complicated grief. N Engl J Med. 2015;372:153-160.
7. Wolfelt AD. Counseling Skills for Companioning the Mourner: The Fundamentals of Effective Grief Counseling. Fort Collins, CO: Companion Press; 2016.
8. Szanto K, Shear MK, Houck PR, et al. Indirect self-destructive behavior and overt suicidality in patients with complicated grief. J Clin Psychiatry. 2006;67:233-239.
9. Otani H, Yoshida S, Morita T, et al. Meaningful communication before death, but not present at the time of death itself, is associated with better outcomes on measures of depression and complicated grief among bereaved family members of cancer patients. J Pain Symptom Manage. 2017;54:273-279.
10. CMS. Medicare benefit policy manual: coverage of hospice services under hospital insurance. www.cms.gov/Regulations-and-guidance/Guidance/Manuals/downloads/bp102c09.pdf. Accessed February 25, 2018.
11. Cherlin E, Barry LC, Prigerson H, et al. Bereavement services for family caregivers: how often used, why, and why not. J Palliat Med. 2007;10:148–158.
12. Bui E, Nidal-Vicens M, Simon NM. Pharmacologic approaches to the treatment of complicated grief: rationale and a brief review of the literature. Dialogues Clin Neurosci. 2012;14:149-157.
13. Shear MK, Reynolds CF 3rd, Simon NM, et al. Optimizing treatment of complicated grief: a randomized clinical trial. JAMA Psychiatry. 2016;73:685-694.
1. Cozza SJ, Fisher JE, Mauro C, et al. Performance of DSM-5 persistent complex bereavement disorder criteria in a community sample of bereaved military family members. Am J Psychiatry. 2016;173:919-929.
2. Kersting A, Brähler E, Glaesmer H, et al. Prevalence of complicated grief in a representative population-based sample. J Affect Disord. 2011;131:339-343.
3. Fujisawa D, Miyashita M, Nakajima S, et al. Prevalence and determinants of complicated grief in general population. J Affect Disord. 2010;127:352-358.
4. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: APA Press; 2013.
5. Shear MK, Simon N, Wall M, et al. Complicated grief and related issues for DSM-5. Depress Anxiety. 2011;28:103-117.
6. Shear MK. Clinical Practice. Complicated grief. N Engl J Med. 2015;372:153-160.
7. Wolfelt AD. Counseling Skills for Companioning the Mourner: The Fundamentals of Effective Grief Counseling. Fort Collins, CO: Companion Press; 2016.
8. Szanto K, Shear MK, Houck PR, et al. Indirect self-destructive behavior and overt suicidality in patients with complicated grief. J Clin Psychiatry. 2006;67:233-239.
9. Otani H, Yoshida S, Morita T, et al. Meaningful communication before death, but not present at the time of death itself, is associated with better outcomes on measures of depression and complicated grief among bereaved family members of cancer patients. J Pain Symptom Manage. 2017;54:273-279.
10. CMS. Medicare benefit policy manual: coverage of hospice services under hospital insurance. www.cms.gov/Regulations-and-guidance/Guidance/Manuals/downloads/bp102c09.pdf. Accessed February 25, 2018.
11. Cherlin E, Barry LC, Prigerson H, et al. Bereavement services for family caregivers: how often used, why, and why not. J Palliat Med. 2007;10:148–158.
12. Bui E, Nidal-Vicens M, Simon NM. Pharmacologic approaches to the treatment of complicated grief: rationale and a brief review of the literature. Dialogues Clin Neurosci. 2012;14:149-157.
13. Shear MK, Reynolds CF 3rd, Simon NM, et al. Optimizing treatment of complicated grief: a randomized clinical trial. JAMA Psychiatry. 2016;73:685-694.
Adult ADHD: Addressing a unique set of challenges
Attention-deficit/hyperactivity disorder (ADHD) in adults brings with it unique challenges, not the least of which are arriving at a proper diagnosis and ensuring that any psychostimulant drugs that you prescribe are not misused. A number of conditions such as anxiety, bipolar disorder, and substance abuse can mimic some of the symptoms of ADHD, and diagnostic criteria for the condition in adults changed with the latest edition of the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5).
Furthermore, for many of the estimated 4.4% of adults who have ADHD,1 psychostimulants provide necessary and effective treatment, but misuse and diversion of these agents are real concerns. In fact, recent research reveals that these issues are more common than previously thought.2 Data suggest that the prevalence of misuse and diversion of ADHD medication is 5% to 10% among high school students and 5% to 35% among college students.2,3
This is not meant to indicate that adults diagnosed with ADHD should go untreated. In fact, adults with ADHD often struggle in their professional and family lives because they do not receive the treatment they need.
Rather, family physicians should take certain steps, first to diagnose ADHD correctly, and then to ascertain and maintain correct use of psychostimulants and other treatments among their adult patient populations. Read on for several practical strategies.
Criteria for adult Dx differ from those in children
ADHD, a common behavioral disorder that often, but not always, begins in childhood, is characterized by deficits in paying attention, difficulty controlling impulses, and marked hyperactivity. Diagnosis of ADHD is based on the DSM-5 criteria and supplemented with historical data and clinical observations.4 Using self-report measures may also aid in the diagnosis, and psychological testing may be required for some individuals when the clinical presentation is unclear.
With the DSM-5 changes (TABLE 14), the diagnosis of ADHD in adults (people ≥18 years) requires fewer symptoms than the diagnosis of ADHD in children; just 5 symptoms from either of the 2 categories of diagnostic criteria are sufficient now, whereas 6 symptoms were required previously and still are required to make the diagnosis in young people. People may present with the inattentive profile (5 or more symptoms of inattention), the hyperactive-impulsive profile (5 or more hyperactive-impulsive symptoms), or a combination of the 2 (5 or more symptoms of inattention plus 5 or more symptoms of hyperactivity-impulsivity for a total of 10 or more symptoms). While children are more likely to present with the combined type of ADHD, adults of any age are more likely to present with the inattentive type.4
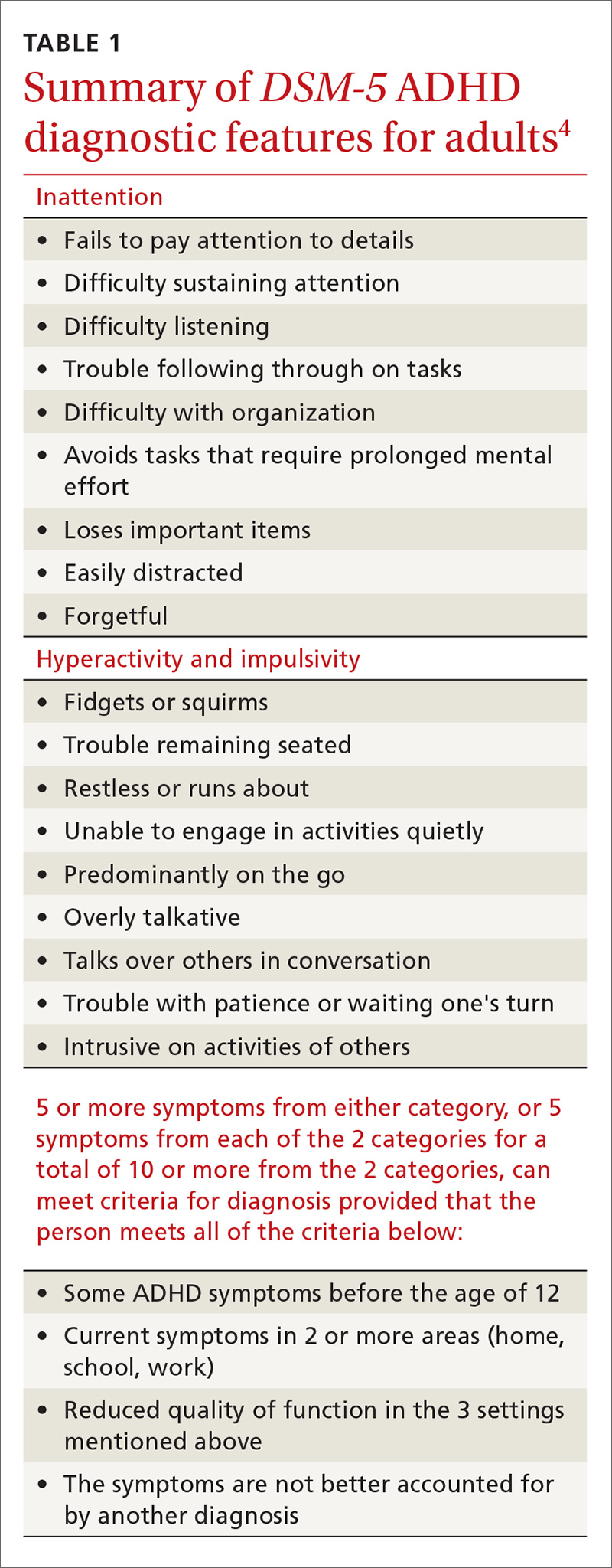
In addition, patients must meet the diagnostic criteria for ADHD for at least 6 months, have had some of the symptoms prior to age 12, and the symptoms must cause significant impairment in 2 or more environments (eg, home, work, school). When the diagnosis is unclear, it is important to obtain collateral information from the family, school, or workplace. The requirement regarding symptomatology before age 12 indicates the need for a review of the patient’s educational history. Research reveals that many adults with ADHD struggled in school and were considered “underachievers” as students.5
Common complaints and characteristics. Previous studies have shown the following to be common complaints and characteristics of adult patients diagnosed with ADHD:5
- difficulty meeting time limits
- vocational struggles, such as frequent job changes or nonpromotion at work
- anger issues
- addiction
- relationship/social strain
- comprehension problems, and
- a family history of ADHD.
Common correlates include low socioeconomic status, driving violations, frequent injuries, legal problems, alcohol and/or tobacco use, and self-reported maladjustment.5 People treated for ADHD have a comorbid DSM diagnosis 81% of the time with the most likely diagnoses being substance abuse, depression, and anxiety.6
Adult-onset ADHD? Even though the DSM-5 criteria for an ADHD diagnosis in adulthood require that some ADHD symptoms were manifest prior to age 12, recent longitudinal research on ADHD in Brazil and the United Kingdom reveals that a large portion of people who meet the criteria for ADHD in adulthood did not meet the criteria as children. The researchers in these studies proposed that there may be a form of ADHD that manifests later in life, a so-called “adult-onset ADHD.”7 While this information is something for clinicians to consider, further research is needed to justify a paradigm shift in how ADHD is diagnosed.
Self-rating measures can offer clarification. Whether or not history-gathering leaves the diagnosis murky, self-rating measures can be valuable in rounding out the clinical picture and alerting clinicians to any inconsistencies in symptoms.8 Four common ADHD self-rating measures are provided in TABLE 2. As one example, the Adult ADHD Self-Report Scale (ASRS) Symptom Checklist is a valuable ADHD screening tool that is free of charge and takes only 5 to 10 minutes.8 Other self-report measures require a similar amount of time, but are not available on a complimentary basis.
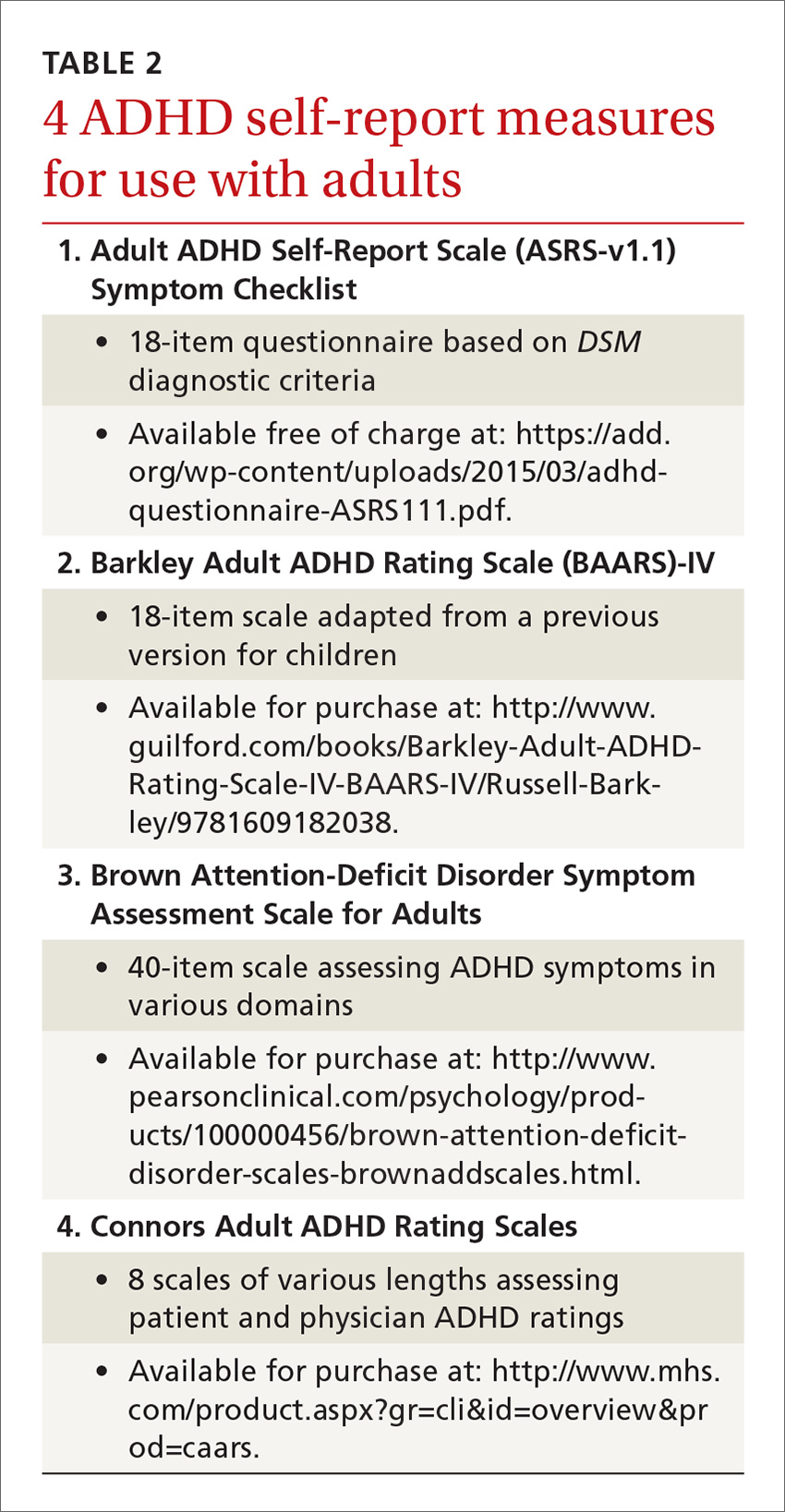
Psychological testing. Some adults who seem to have symptoms of ADHD may require a referral for psychological testing. These may be patients who present with complicated cases or whose histories and/or findings do not consistently indicate an ADHD diagnosis. In such cases, psychological testing can fill in the holes and provide a more complete picture of the patient’s neurocognitive abilities and deficits.9,10
Psychostimulant treatment: Opt for longer-acting agents
The standard treatment for ADHD is a psychostimulant. One controlled trial, for example, of a mixed amphetamine salts compound (Adderall) found that the compound effectively treated ADHD symptoms (hyperactivity, impulsivity, inattention) in adults and was well tolerated.11 While far fewer studies have been performed in adult vs youth populations, those that have been conducted in adults indicate that psychostimulants are largely safe and efficacious. In fact, the study mentioned above found that 70% of patients with ADHD ages 18 and older reported improvement of symptoms while on a short-acting psychostimulant, as compared to 7% who reported improvement on placebo.11
Similarly, a meta-analysis of 1991 participants in 11 studies found significant improvement in patients who received medication vs placebo, with stimulant medications demonstrating greater efficacy than non-stimulant treatments for ADHD.12 In general, psychostimulant treatment for adults is similar to that for children; the only difference is that adults tend to be more forthcoming with information regarding how the treatment is working and what adjustments might be needed.
Longer-acting stimulants (ie, extended release) tend to be preferred by patients to short-acting ones because they typically provide adequate control of symptoms over a longer period of time and thus may be taken less frequently.13 Also, the potential for abuse of psychostimulant medication tends to be lower with the longer-acting, extended-release formulations.14 A shorter acting formulation may be preferred if a patient has a specific window of time when their ADHD symptoms impact them. For example, a patient may request a short-acting form of medication for afternoons if he or she has to attend many business meetings at that time of day. A relatively new category is the intermediate-acting psychostimulants. For more on specific psychostimulants, see Table 3.15
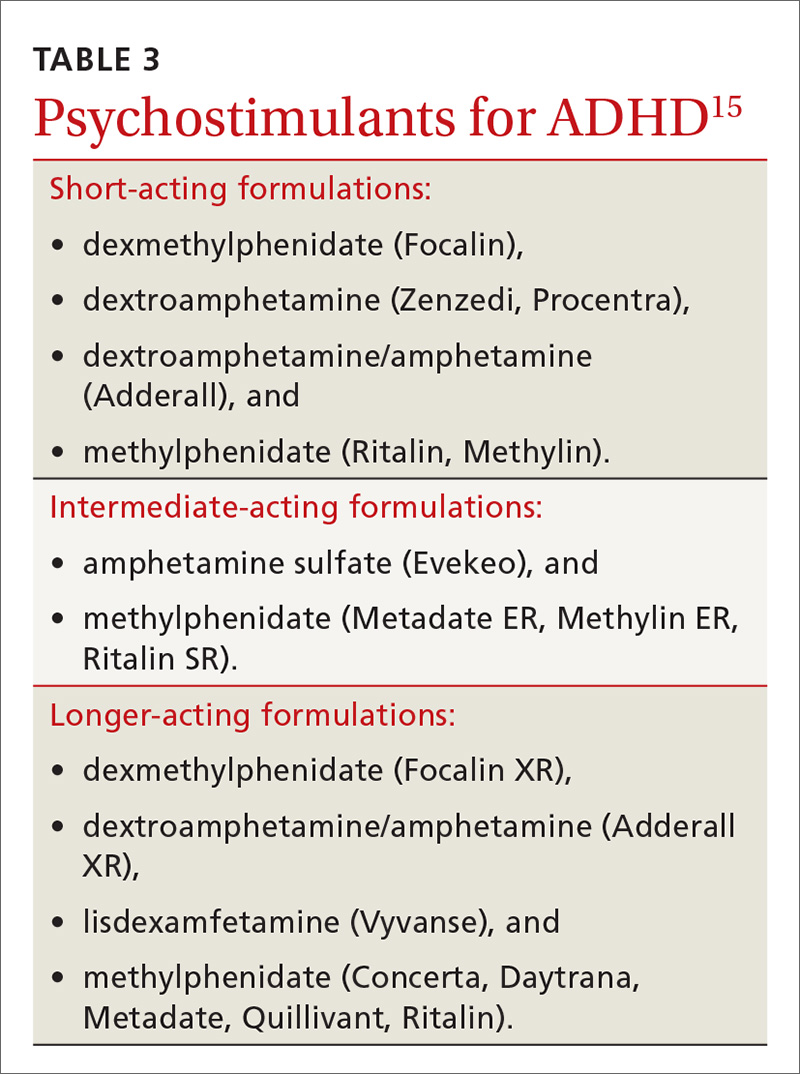
Adverse effects lead many to discontinue treatment
Regardless of the length of action of the psychostimulant, studies show that about 30% of adults (and, incidentally, 10% to 30% of children) discontinue treatment due to uncontrolled/unwanted symptoms or adverse effects.16 These include decreased appetite, headache, insomnia, abdominal pain, and irritable mood.17 If you are prescribing a psychostimulant for an adult with ADHD, it is important to tell the patient that if the effects become intolerable, adjustments can be made, such as tweaking dosages, switching to a different medication, or adding an adjunctive therapy such as cognitive behavioral therapy. Keep in mind, too, that if a medication is to be discontinued, tapering is suggested for most psychostimulants; patients should take a lower (eg, half) dose for about a week prior to complete discontinuation. People who have difficulties with a number of treatments for ADHD should be reevaluated in a year to see if circumstances have changed.5
Combatting misuse and diversion
Perhaps the most controversial issues surrounding the treatment of adults with ADHD are abuse and diversion of psychostimulants. Abuse generally refers to misuse of the drug by the person prescribed the agent, whereas diversion refers to use of the drug by people for whom the drug was not intended—with or without the prescribee’s knowledge.3 Although rare, chronic abuse of psychostimulants can lead to serious problems such as aggression, suicidal thoughts/behaviors, psychosis, and mania.5
While earlier studies tended to downplay the likelihood of diversion, recent research indicates that physicians should not underestimate the possibility. In fact, a previous article in this journal about student athletes with ADHD (http://bit.ly/2k1a6TL) indicated that psychostimulants have “great potential for misuse” and that recently there has been “a surge in nonprescription stimulant use among adolescents and young adults.”17 The authors of the article concluded, however, that while physicians should be aware of the potential for misuse, fear should not preclude treatment.17
A national multi-cohort study of 4572 US high school seniors who had used psychostimulants either medically or nonmedically indicated that while one in 6 high school seniors had been exposed to psychostimulants, about half were appropriately exposed through prescription use, while the other half was not. The researchers also reported that current nonmedical users of psychostimulants and those with a history of nonmedical use had a greater risk of substance use and abuse when compared to medical users of psychostimulants.18
Young men are at higher risk for diversion. In a nationwide survey of a sample of adults ages 18 to 49 years who had a prescription for psychostimulant medication in the past month, 17% admitted diverting their medication.
In another study, 483 students ages 17 to 19 years were followed for one year and interviewed frequently regarding their use of medications.20 The researchers reported that the lifetime prevalence of diversion of any medication in those students was around 36%. They also found that of those who diverted medication, 62% diverted ADHD medications at least once. These were most commonly diverted by sharing (34%) and selling (9%) the psychostimulants. Interview analysis revealed that those students who diverted were more likely to have used illicit drugs and to have had conduct problems. The authors advised “vigilance regarding…stimulant medications for young adults.”
Psychostimulant prescriptions do not cause substance abuse. Nevertheless, a salient point in the literature is that there is no causal relationship between psychostimulant prescriptions that are properly prescribed for people who have ADHD and substance abuse. One study that followed young people with ADHD for 8 years into adulthood revealed that psychostimulant treatment did not make adolescents or young adults any more or less likely to abuse drugs.21 The study also found that alcohol use was common in young adults whether they were diagnosed with ADHD or not. Nonetheless, family physicians should urge those taking psychostimulants to refrain from alcohol use or at least to drink in moderation.
The bottom line is that adults diagnosed with ADHD carry about the same risk of substance abuse as the general population if they are effectively treated for their presenting attention problems.22 If they are taking a psychostimulant, however, they have access to a controlled substance, unlike most of their cohorts. So it's important to teach patients with ADHD that for safety and legal reasons, they should not share or sell their stimulant medication to anyone.
Minimize the risk for abuse, diversion using these strategies
As with any drug regimen, it is important to monitor the patient’s response to treatment and minimize adverse effects and outcomes. When the drug is a psychostimulant for adults diagnosed with ADHD, it’s also important to minimize the risk for abuse and diversion. The following steps can help:
- Obtain a signed controlled substance agreement.23 This agreement between the physician and the patient usually outlines such specifics as frequency of office visits, circumstances surrounding medication refills, urine drug monitoring, and pill counts. (For more on the specifics of a controlled substance agreement, see "Key points of a controlled substance agreement.")
- Schedule frequent follow-up appointments with open communication about abuse and diversion.20,23 The age-old adage, “Start low, go slow,” applies to stimulant medications for ADHD. Medication dosage may vary and necessitate titration depending on the person’s weight and tolerance. At the onset of treatment, frequent office visits allow the physician to gauge treatment response and the patient’s commitment to therapy.
- Review your state’s prescription drug monitoring program.24 It is imperative that providers check their state’s medical board rules for prescribing controlled medications to ensure practice compliance. As diversion rates of controlled medications have risen in this country, most states have established monitoring systems through their pharmacy boards.24 Although the names of the programs vary, these prescription drug monitoring programs provide information on any medication prescribed. This allows the prescribing physician to ensure patient compliance and ascertain that no other controlled medications are being prescribed that could interfere with treatment. (For more information about state prescription drug monitoring programs, see https://www.deadiversion.usdoj.gov/faq/rx_monitor.htm.)
- Perform random urine drug screenings (UDS).20,23 An important strategy for ensuring adherence to the treatment plan and the controlled substance contract is UDS. Explain to patients that this is a way of making sure they are taking the medication exactly as prescribed. If the UDS indicates that the patient has not been taking the medication, then the provider should intervene by either restricting or discontinuing the controlled substance to prevent or counteract potential diversion. Similarly, if a higher dose is requested by a patient, the provider can closely monitor the situation to determine whether the additional drug is actually being taken and whether the dose is optimal. (See JFP’s October 2016 “3 in 3” video on urine drug testing at: http://bit.ly/2iDnfgD.)
- Employ a team-based, multimodal approach.25 A referral to a mental health professional and multimodal treatment are often recommended in the literature as best practices.25 Behavioral therapies are a cornerstone of treatment in adults with ADHD and often serve as important adjuncts to pharmacotherapy. Also, a referral provides a second professional opinion about the patient’s motivations, adherence, and response to treatment.
Trained cognitive behavioral therapists (eg, psychologists, counselors) can be helpful with treatment for ADHD.23 Therapists can be useful in setting goals for the patient regarding adherence, organization, impulse control, and social skills training. Therapists may wish to involve the family in treatment, depending on the nature of the patient’s presenting issues.
SIDEBAR
Key points of a controlled substance agreementThe primary purpose of a controlled substance agreement is to provide clarity for the provider and the patient regarding the use of controlled medications. The document is meant to prevent potential problems and confusion down the road. There are generally 3 parts:
- a doctor/patient agreement
- information about medications
- patient consent to utilize controlled substances that the provider believes would be beneficial.
Patients are typically told of the potential value of controlled medications in helping them and are warned about the potential for problems should the medications be used in ways other than intended. While wording may differ, patients are generally asked to agree to variations of the following 10 guidelines:
- I will talk with my doctor before using more than the prescribed amount of the medicine or discontinuing its use.
- I will tell my doctor if new medications are prescribed by another provider.
- I will tell the doctor if I become pregnant, so that any necessary medication adjustments can be made.
- If I abuse this drug, I understand that the doctor may need to stop treatment.
- I will uphold the visit schedule to the office/clinic according to guidelines for controlled substances (eg, every 90 days).
- I will refrain from using illicit drugs including marijuana and excessive quantities of alcohol.
- I will refrain from sharing, trading, or selling controlled substances.
- I will submit to regular urine drug screens as requested by the doctor.
- I understand that a failed drug screen may mean discontinuation of treatment.
- I will be forthright and honest about how the treatment is going, adverse effects, and how I am taking the medication.
Adapted from: https://www.drugabuse.gov/sites/default/files/files/SamplePatientAgreementForms.pdf.
Don’t tempt fate. As with any controlled medication, safe storage of psychostimulants is paramount. Patients should be urged to keep their medication in a locked box or cupboard that is accessible to only the adult for whom the drug is prescribed. Prior research cautions that open access to controlled substances can lead to larger issues with abuse and diversion, particularly when adolescents are in the home.26
Consider atomoxetine. Research has also demonstrated that the non-stimulant medication atomoxetine has some benefit in the treatment of ADHD.12 Unlike psychostimulants that act on the neurotransmitter dopamine, atomoxetine acts on the neurotransmitter norepinephrine. This different mechanism of action results in a lower potential for abuse and diversion.
CORRESPONDENCE
Scott A. Fields, PhD, 3200 MacCorkle Avenue Southeast, 5th Floor, Robert C. Byrd Clinical Teaching Center, Department of Family Medicine, Charleston, WV 25304; sfields@hsc.wvu.edu.
1. Kessler RC, Adler LA, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163:716-723.
2. Clemow DB, Walker DJ. The potential for misuse and abuse of medications in ADHD: a review. Postgrad Med. 2014;126:64-81.
3. Novak SP, Kroutil LA, Williams RL, et al. The nonmedical use of prescription ADHD medications: results from a national internet panel. Subst Abuse Treat Prev Policy. 2007;2:32.
4. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: American Psychiatric Association Press; 2013.
5. Kolar D, Keller A, Golfinopoulos M, et al. Treatment of adults with attention-deficit/hyperactivity disorder. Neuropsychiatr Dis Treat. 2008;4:389-403.
6. McGough JJ, Smalley SL, McCracken JT, et al. Psychiatric comorbidity in adult attention deficit hyperactivity disorder: findings from multiplex families. Am J Psychiatry. 2005;162:1621-1627.
7. Faraone SV, Biederman J. Can attention-deficit/hyperactivity disorder onset occur in adulthood? JAMA Psychiatry.
8. van de Glind G, van den Brink W, Koeter MWJ, et al. Validity of the Adult ADHD Self-Report Scale (ASRS) as a screener for adult ADHD in treatment seeking substance use disorder patients. Drug Alcohol Depend. 2013;132:587-596.
9. Gualtieri CT, Johnson LG. ADHD: Is objective diagnosis possible? Psychiatry. 2005;2:44-53.
10. Perrin AE, Jotwani VM. Addressing the unique issues of student athletes with ADHD. J Fam Pract. 2014;63:E1-E9.
11. Spencer T, Biederman J, Wilens T, et al. Efficacy of mixed amphetamine salts compound in adults with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 2001;58:775-782.
12. Mészáros A, Czobor P, Bálint S, et al. Pharmacotherapy of adult attention deficit hyperactivity disorder (ADHD): a meta-analysis. Int J Neuropsychopharmacol. 2009;12:1137-1147.
13. Weiss M, Shingler T, Capone NM. Medication satisfaction among adults with ADHD: long term results from the Quality of Life, Effectiveness, Safety and Tolerability (Qu.S.T) study. New Orleans: Program and Abstracts of the 19th US Psychiatric and Mental Health Congress, Abstract 120, 2006.
14. Lopez FA, Leroux JR.
15. Felt BT, Biermann B, Christner JG, et al. Diagnosis and management of ADHD in children. Am Fam Physician. 2014;90:456-464.
16. Spencer T, Biederman J, Wilens T. Nonstimulant treatment of adult attention-deficit/hyperactivity disorder. Psychiatr Clin North Am. 2004;27:373-383.
17. Withrow LM, Hash PA, Holten KB. Managing ADHD in children: are you doing enough? J Fam Pract. 2011;60:E1-E3.
18. McCabe SE, West BT. Medical and nonmedical use of prescription stimulants: results from a national multicohort study. J Am Acad Child Adolesc Psychiatry. 2013;52:1272-1280.
19. Aldridge AP, Kroutil LA, Cowell AJ, et al. Medication costs to private insurers of diversion of medications for attention-deficit hyperactivity disorder. Pharmacoeconomics. 2011;29:621-635.
20. Garnier LM, Arria AM, Caldeira KM, et al. Sharing and selling of prescription medications in a college student sample. J Clin Psychiatry. 2010;71:262-269.
21. Molina BSG, Hinshaw SP, Arnold LE, et al. Adolescent substance use in the Multimodal Treatment Study of Attention-Deficit/Hyperactivity Disorder (ADHD) (MTA) as a function of childhood ADHD, random assignment to childhood treatments, and subsequent medication. J Am Acad Child Adolesc Psychiatry. 2013;52:250-263.
22. Brahmbhatt K, Hilty DM, Hah M, et al. Diagnosis and treatment of attention deficit hyperactivity disorder during adolescence in the primary care setting: a concise review. J Adolesc Health. 2016;59:135-143.
23. Post RE, Kurlansik SL. Diagnosis and management of attention-deficit/hyperactivity disorder in adults. Am Fam Physician. 2012;85:890-896.
24. Cepeda MS, Fife D, Berwaerts J, et al. Doctor shopping for medications used in the treatment of attention deficit hyperactivity disorder: shoppers often pay in cash and cross state lines. Am J Drug Alcohol Abuse. 2015;41:226-229.
25. Safren SA, Sprich S, Mimiaga MJ, et al. Cognitive behavioral therapy vs relaxation with educational support for medication-treated adults with ADHD and persistent symptoms: a randomized controlled trial. JAMA. 2010;304:875-880.
26. Ross-Durow PL, McCabe SE, Boyd CJ. Adolescents’ access to their own prescription medication in the home. J Adolesc Health. 2013;53:260-264.
Attention-deficit/hyperactivity disorder (ADHD) in adults brings with it unique challenges, not the least of which are arriving at a proper diagnosis and ensuring that any psychostimulant drugs that you prescribe are not misused. A number of conditions such as anxiety, bipolar disorder, and substance abuse can mimic some of the symptoms of ADHD, and diagnostic criteria for the condition in adults changed with the latest edition of the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5).
Furthermore, for many of the estimated 4.4% of adults who have ADHD,1 psychostimulants provide necessary and effective treatment, but misuse and diversion of these agents are real concerns. In fact, recent research reveals that these issues are more common than previously thought.2 Data suggest that the prevalence of misuse and diversion of ADHD medication is 5% to 10% among high school students and 5% to 35% among college students.2,3
This is not meant to indicate that adults diagnosed with ADHD should go untreated. In fact, adults with ADHD often struggle in their professional and family lives because they do not receive the treatment they need.
Rather, family physicians should take certain steps, first to diagnose ADHD correctly, and then to ascertain and maintain correct use of psychostimulants and other treatments among their adult patient populations. Read on for several practical strategies.
Criteria for adult Dx differ from those in children
ADHD, a common behavioral disorder that often, but not always, begins in childhood, is characterized by deficits in paying attention, difficulty controlling impulses, and marked hyperactivity. Diagnosis of ADHD is based on the DSM-5 criteria and supplemented with historical data and clinical observations.4 Using self-report measures may also aid in the diagnosis, and psychological testing may be required for some individuals when the clinical presentation is unclear.
With the DSM-5 changes (TABLE 14), the diagnosis of ADHD in adults (people ≥18 years) requires fewer symptoms than the diagnosis of ADHD in children; just 5 symptoms from either of the 2 categories of diagnostic criteria are sufficient now, whereas 6 symptoms were required previously and still are required to make the diagnosis in young people. People may present with the inattentive profile (5 or more symptoms of inattention), the hyperactive-impulsive profile (5 or more hyperactive-impulsive symptoms), or a combination of the 2 (5 or more symptoms of inattention plus 5 or more symptoms of hyperactivity-impulsivity for a total of 10 or more symptoms). While children are more likely to present with the combined type of ADHD, adults of any age are more likely to present with the inattentive type.4
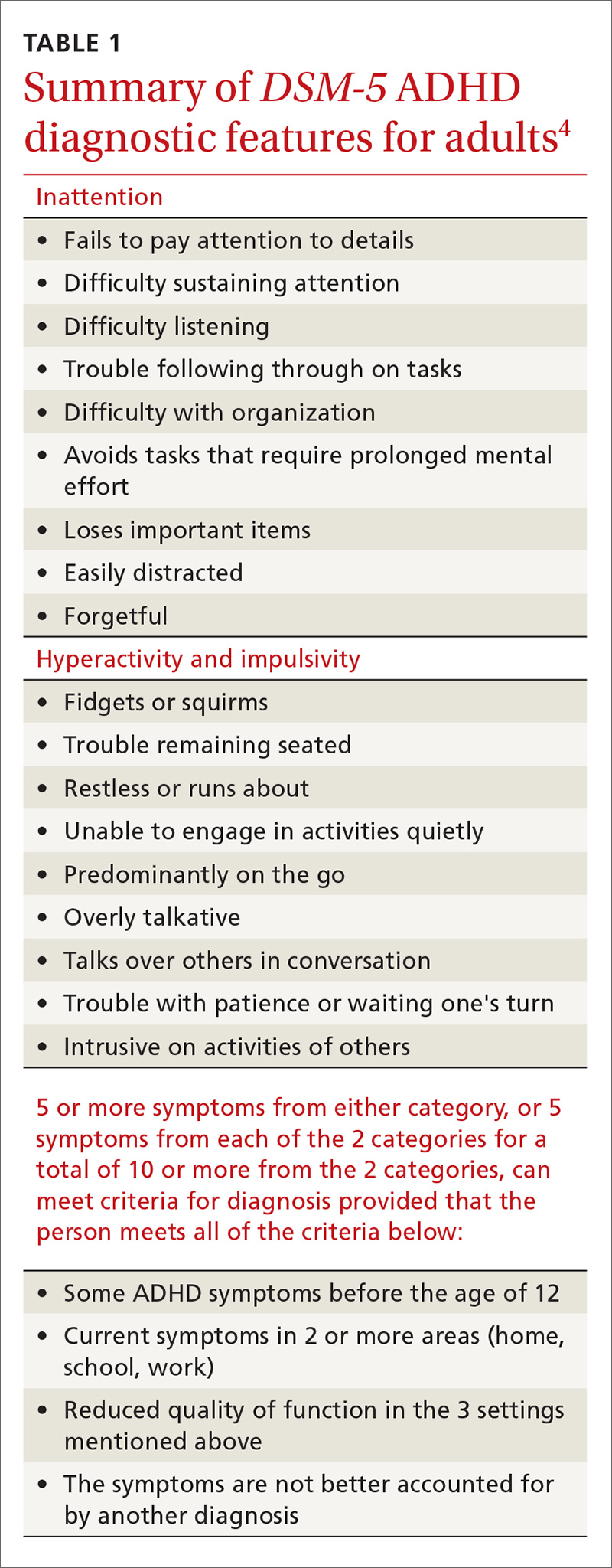
In addition, patients must meet the diagnostic criteria for ADHD for at least 6 months, have had some of the symptoms prior to age 12, and the symptoms must cause significant impairment in 2 or more environments (eg, home, work, school). When the diagnosis is unclear, it is important to obtain collateral information from the family, school, or workplace. The requirement regarding symptomatology before age 12 indicates the need for a review of the patient’s educational history. Research reveals that many adults with ADHD struggled in school and were considered “underachievers” as students.5
Common complaints and characteristics. Previous studies have shown the following to be common complaints and characteristics of adult patients diagnosed with ADHD:5
- difficulty meeting time limits
- vocational struggles, such as frequent job changes or nonpromotion at work
- anger issues
- addiction
- relationship/social strain
- comprehension problems, and
- a family history of ADHD.
Common correlates include low socioeconomic status, driving violations, frequent injuries, legal problems, alcohol and/or tobacco use, and self-reported maladjustment.5 People treated for ADHD have a comorbid DSM diagnosis 81% of the time with the most likely diagnoses being substance abuse, depression, and anxiety.6
Adult-onset ADHD? Even though the DSM-5 criteria for an ADHD diagnosis in adulthood require that some ADHD symptoms were manifest prior to age 12, recent longitudinal research on ADHD in Brazil and the United Kingdom reveals that a large portion of people who meet the criteria for ADHD in adulthood did not meet the criteria as children. The researchers in these studies proposed that there may be a form of ADHD that manifests later in life, a so-called “adult-onset ADHD.”7 While this information is something for clinicians to consider, further research is needed to justify a paradigm shift in how ADHD is diagnosed.
Self-rating measures can offer clarification. Whether or not history-gathering leaves the diagnosis murky, self-rating measures can be valuable in rounding out the clinical picture and alerting clinicians to any inconsistencies in symptoms.8 Four common ADHD self-rating measures are provided in TABLE 2. As one example, the Adult ADHD Self-Report Scale (ASRS) Symptom Checklist is a valuable ADHD screening tool that is free of charge and takes only 5 to 10 minutes.8 Other self-report measures require a similar amount of time, but are not available on a complimentary basis.
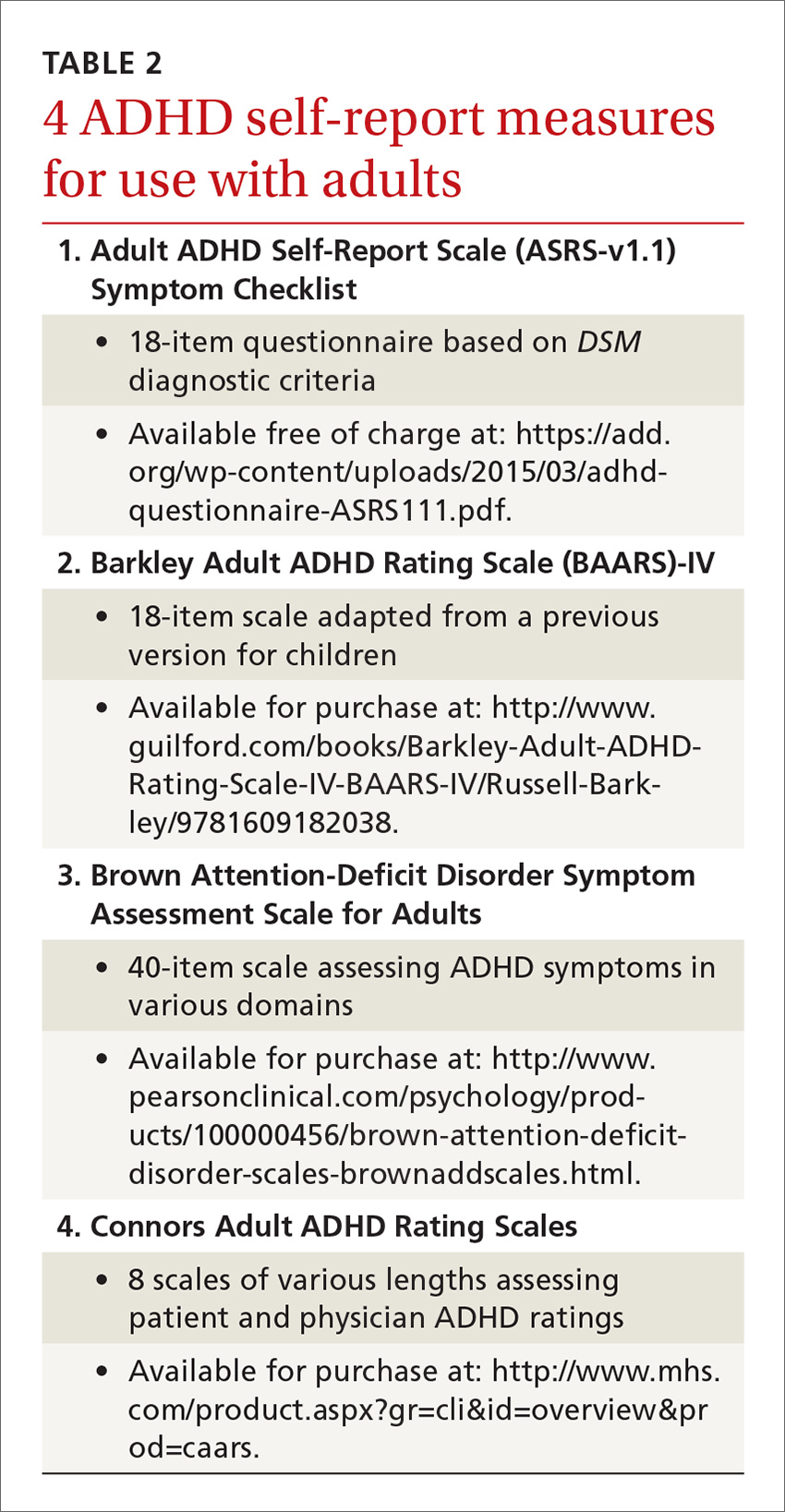
Psychological testing. Some adults who seem to have symptoms of ADHD may require a referral for psychological testing. These may be patients who present with complicated cases or whose histories and/or findings do not consistently indicate an ADHD diagnosis. In such cases, psychological testing can fill in the holes and provide a more complete picture of the patient’s neurocognitive abilities and deficits.9,10
Psychostimulant treatment: Opt for longer-acting agents
The standard treatment for ADHD is a psychostimulant. One controlled trial, for example, of a mixed amphetamine salts compound (Adderall) found that the compound effectively treated ADHD symptoms (hyperactivity, impulsivity, inattention) in adults and was well tolerated.11 While far fewer studies have been performed in adult vs youth populations, those that have been conducted in adults indicate that psychostimulants are largely safe and efficacious. In fact, the study mentioned above found that 70% of patients with ADHD ages 18 and older reported improvement of symptoms while on a short-acting psychostimulant, as compared to 7% who reported improvement on placebo.11
Similarly, a meta-analysis of 1991 participants in 11 studies found significant improvement in patients who received medication vs placebo, with stimulant medications demonstrating greater efficacy than non-stimulant treatments for ADHD.12 In general, psychostimulant treatment for adults is similar to that for children; the only difference is that adults tend to be more forthcoming with information regarding how the treatment is working and what adjustments might be needed.
Longer-acting stimulants (ie, extended release) tend to be preferred by patients to short-acting ones because they typically provide adequate control of symptoms over a longer period of time and thus may be taken less frequently.13 Also, the potential for abuse of psychostimulant medication tends to be lower with the longer-acting, extended-release formulations.14 A shorter acting formulation may be preferred if a patient has a specific window of time when their ADHD symptoms impact them. For example, a patient may request a short-acting form of medication for afternoons if he or she has to attend many business meetings at that time of day. A relatively new category is the intermediate-acting psychostimulants. For more on specific psychostimulants, see Table 3.15
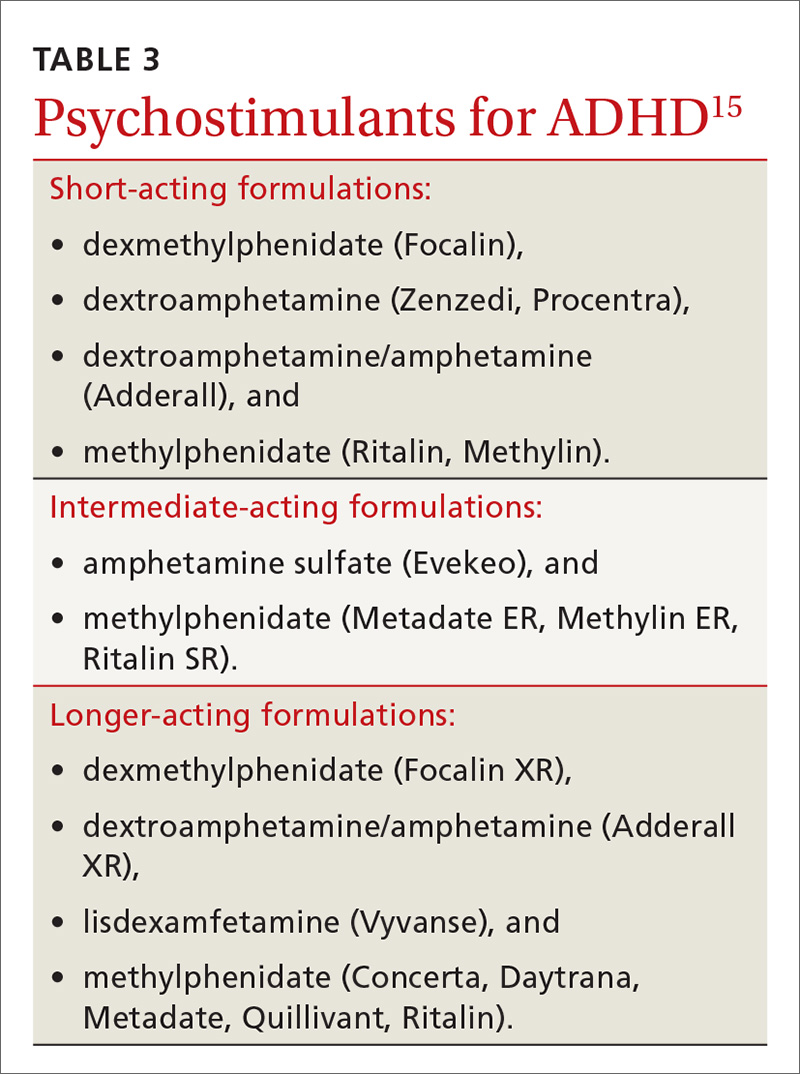
Adverse effects lead many to discontinue treatment
Regardless of the length of action of the psychostimulant, studies show that about 30% of adults (and, incidentally, 10% to 30% of children) discontinue treatment due to uncontrolled/unwanted symptoms or adverse effects.16 These include decreased appetite, headache, insomnia, abdominal pain, and irritable mood.17 If you are prescribing a psychostimulant for an adult with ADHD, it is important to tell the patient that if the effects become intolerable, adjustments can be made, such as tweaking dosages, switching to a different medication, or adding an adjunctive therapy such as cognitive behavioral therapy. Keep in mind, too, that if a medication is to be discontinued, tapering is suggested for most psychostimulants; patients should take a lower (eg, half) dose for about a week prior to complete discontinuation. People who have difficulties with a number of treatments for ADHD should be reevaluated in a year to see if circumstances have changed.5
Combatting misuse and diversion
Perhaps the most controversial issues surrounding the treatment of adults with ADHD are abuse and diversion of psychostimulants. Abuse generally refers to misuse of the drug by the person prescribed the agent, whereas diversion refers to use of the drug by people for whom the drug was not intended—with or without the prescribee’s knowledge.3 Although rare, chronic abuse of psychostimulants can lead to serious problems such as aggression, suicidal thoughts/behaviors, psychosis, and mania.5
While earlier studies tended to downplay the likelihood of diversion, recent research indicates that physicians should not underestimate the possibility. In fact, a previous article in this journal about student athletes with ADHD (http://bit.ly/2k1a6TL) indicated that psychostimulants have “great potential for misuse” and that recently there has been “a surge in nonprescription stimulant use among adolescents and young adults.”17 The authors of the article concluded, however, that while physicians should be aware of the potential for misuse, fear should not preclude treatment.17
A national multi-cohort study of 4572 US high school seniors who had used psychostimulants either medically or nonmedically indicated that while one in 6 high school seniors had been exposed to psychostimulants, about half were appropriately exposed through prescription use, while the other half was not. The researchers also reported that current nonmedical users of psychostimulants and those with a history of nonmedical use had a greater risk of substance use and abuse when compared to medical users of psychostimulants.18
Young men are at higher risk for diversion. In a nationwide survey of a sample of adults ages 18 to 49 years who had a prescription for psychostimulant medication in the past month, 17% admitted diverting their medication.
In another study, 483 students ages 17 to 19 years were followed for one year and interviewed frequently regarding their use of medications.20 The researchers reported that the lifetime prevalence of diversion of any medication in those students was around 36%. They also found that of those who diverted medication, 62% diverted ADHD medications at least once. These were most commonly diverted by sharing (34%) and selling (9%) the psychostimulants. Interview analysis revealed that those students who diverted were more likely to have used illicit drugs and to have had conduct problems. The authors advised “vigilance regarding…stimulant medications for young adults.”
Psychostimulant prescriptions do not cause substance abuse. Nevertheless, a salient point in the literature is that there is no causal relationship between psychostimulant prescriptions that are properly prescribed for people who have ADHD and substance abuse. One study that followed young people with ADHD for 8 years into adulthood revealed that psychostimulant treatment did not make adolescents or young adults any more or less likely to abuse drugs.21 The study also found that alcohol use was common in young adults whether they were diagnosed with ADHD or not. Nonetheless, family physicians should urge those taking psychostimulants to refrain from alcohol use or at least to drink in moderation.
The bottom line is that adults diagnosed with ADHD carry about the same risk of substance abuse as the general population if they are effectively treated for their presenting attention problems.22 If they are taking a psychostimulant, however, they have access to a controlled substance, unlike most of their cohorts. So it's important to teach patients with ADHD that for safety and legal reasons, they should not share or sell their stimulant medication to anyone.
Minimize the risk for abuse, diversion using these strategies
As with any drug regimen, it is important to monitor the patient’s response to treatment and minimize adverse effects and outcomes. When the drug is a psychostimulant for adults diagnosed with ADHD, it’s also important to minimize the risk for abuse and diversion. The following steps can help:
- Obtain a signed controlled substance agreement.23 This agreement between the physician and the patient usually outlines such specifics as frequency of office visits, circumstances surrounding medication refills, urine drug monitoring, and pill counts. (For more on the specifics of a controlled substance agreement, see "Key points of a controlled substance agreement.")
- Schedule frequent follow-up appointments with open communication about abuse and diversion.20,23 The age-old adage, “Start low, go slow,” applies to stimulant medications for ADHD. Medication dosage may vary and necessitate titration depending on the person’s weight and tolerance. At the onset of treatment, frequent office visits allow the physician to gauge treatment response and the patient’s commitment to therapy.
- Review your state’s prescription drug monitoring program.24 It is imperative that providers check their state’s medical board rules for prescribing controlled medications to ensure practice compliance. As diversion rates of controlled medications have risen in this country, most states have established monitoring systems through their pharmacy boards.24 Although the names of the programs vary, these prescription drug monitoring programs provide information on any medication prescribed. This allows the prescribing physician to ensure patient compliance and ascertain that no other controlled medications are being prescribed that could interfere with treatment. (For more information about state prescription drug monitoring programs, see https://www.deadiversion.usdoj.gov/faq/rx_monitor.htm.)
- Perform random urine drug screenings (UDS).20,23 An important strategy for ensuring adherence to the treatment plan and the controlled substance contract is UDS. Explain to patients that this is a way of making sure they are taking the medication exactly as prescribed. If the UDS indicates that the patient has not been taking the medication, then the provider should intervene by either restricting or discontinuing the controlled substance to prevent or counteract potential diversion. Similarly, if a higher dose is requested by a patient, the provider can closely monitor the situation to determine whether the additional drug is actually being taken and whether the dose is optimal. (See JFP’s October 2016 “3 in 3” video on urine drug testing at: http://bit.ly/2iDnfgD.)
- Employ a team-based, multimodal approach.25 A referral to a mental health professional and multimodal treatment are often recommended in the literature as best practices.25 Behavioral therapies are a cornerstone of treatment in adults with ADHD and often serve as important adjuncts to pharmacotherapy. Also, a referral provides a second professional opinion about the patient’s motivations, adherence, and response to treatment.
Trained cognitive behavioral therapists (eg, psychologists, counselors) can be helpful with treatment for ADHD.23 Therapists can be useful in setting goals for the patient regarding adherence, organization, impulse control, and social skills training. Therapists may wish to involve the family in treatment, depending on the nature of the patient’s presenting issues.
SIDEBAR
Key points of a controlled substance agreementThe primary purpose of a controlled substance agreement is to provide clarity for the provider and the patient regarding the use of controlled medications. The document is meant to prevent potential problems and confusion down the road. There are generally 3 parts:
- a doctor/patient agreement
- information about medications
- patient consent to utilize controlled substances that the provider believes would be beneficial.
Patients are typically told of the potential value of controlled medications in helping them and are warned about the potential for problems should the medications be used in ways other than intended. While wording may differ, patients are generally asked to agree to variations of the following 10 guidelines:
- I will talk with my doctor before using more than the prescribed amount of the medicine or discontinuing its use.
- I will tell my doctor if new medications are prescribed by another provider.
- I will tell the doctor if I become pregnant, so that any necessary medication adjustments can be made.
- If I abuse this drug, I understand that the doctor may need to stop treatment.
- I will uphold the visit schedule to the office/clinic according to guidelines for controlled substances (eg, every 90 days).
- I will refrain from using illicit drugs including marijuana and excessive quantities of alcohol.
- I will refrain from sharing, trading, or selling controlled substances.
- I will submit to regular urine drug screens as requested by the doctor.
- I understand that a failed drug screen may mean discontinuation of treatment.
- I will be forthright and honest about how the treatment is going, adverse effects, and how I am taking the medication.
Adapted from: https://www.drugabuse.gov/sites/default/files/files/SamplePatientAgreementForms.pdf.
Don’t tempt fate. As with any controlled medication, safe storage of psychostimulants is paramount. Patients should be urged to keep their medication in a locked box or cupboard that is accessible to only the adult for whom the drug is prescribed. Prior research cautions that open access to controlled substances can lead to larger issues with abuse and diversion, particularly when adolescents are in the home.26
Consider atomoxetine. Research has also demonstrated that the non-stimulant medication atomoxetine has some benefit in the treatment of ADHD.12 Unlike psychostimulants that act on the neurotransmitter dopamine, atomoxetine acts on the neurotransmitter norepinephrine. This different mechanism of action results in a lower potential for abuse and diversion.
CORRESPONDENCE
Scott A. Fields, PhD, 3200 MacCorkle Avenue Southeast, 5th Floor, Robert C. Byrd Clinical Teaching Center, Department of Family Medicine, Charleston, WV 25304; sfields@hsc.wvu.edu.
Attention-deficit/hyperactivity disorder (ADHD) in adults brings with it unique challenges, not the least of which are arriving at a proper diagnosis and ensuring that any psychostimulant drugs that you prescribe are not misused. A number of conditions such as anxiety, bipolar disorder, and substance abuse can mimic some of the symptoms of ADHD, and diagnostic criteria for the condition in adults changed with the latest edition of the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5).
Furthermore, for many of the estimated 4.4% of adults who have ADHD,1 psychostimulants provide necessary and effective treatment, but misuse and diversion of these agents are real concerns. In fact, recent research reveals that these issues are more common than previously thought.2 Data suggest that the prevalence of misuse and diversion of ADHD medication is 5% to 10% among high school students and 5% to 35% among college students.2,3
This is not meant to indicate that adults diagnosed with ADHD should go untreated. In fact, adults with ADHD often struggle in their professional and family lives because they do not receive the treatment they need.
Rather, family physicians should take certain steps, first to diagnose ADHD correctly, and then to ascertain and maintain correct use of psychostimulants and other treatments among their adult patient populations. Read on for several practical strategies.
Criteria for adult Dx differ from those in children
ADHD, a common behavioral disorder that often, but not always, begins in childhood, is characterized by deficits in paying attention, difficulty controlling impulses, and marked hyperactivity. Diagnosis of ADHD is based on the DSM-5 criteria and supplemented with historical data and clinical observations.4 Using self-report measures may also aid in the diagnosis, and psychological testing may be required for some individuals when the clinical presentation is unclear.
With the DSM-5 changes (TABLE 14), the diagnosis of ADHD in adults (people ≥18 years) requires fewer symptoms than the diagnosis of ADHD in children; just 5 symptoms from either of the 2 categories of diagnostic criteria are sufficient now, whereas 6 symptoms were required previously and still are required to make the diagnosis in young people. People may present with the inattentive profile (5 or more symptoms of inattention), the hyperactive-impulsive profile (5 or more hyperactive-impulsive symptoms), or a combination of the 2 (5 or more symptoms of inattention plus 5 or more symptoms of hyperactivity-impulsivity for a total of 10 or more symptoms). While children are more likely to present with the combined type of ADHD, adults of any age are more likely to present with the inattentive type.4
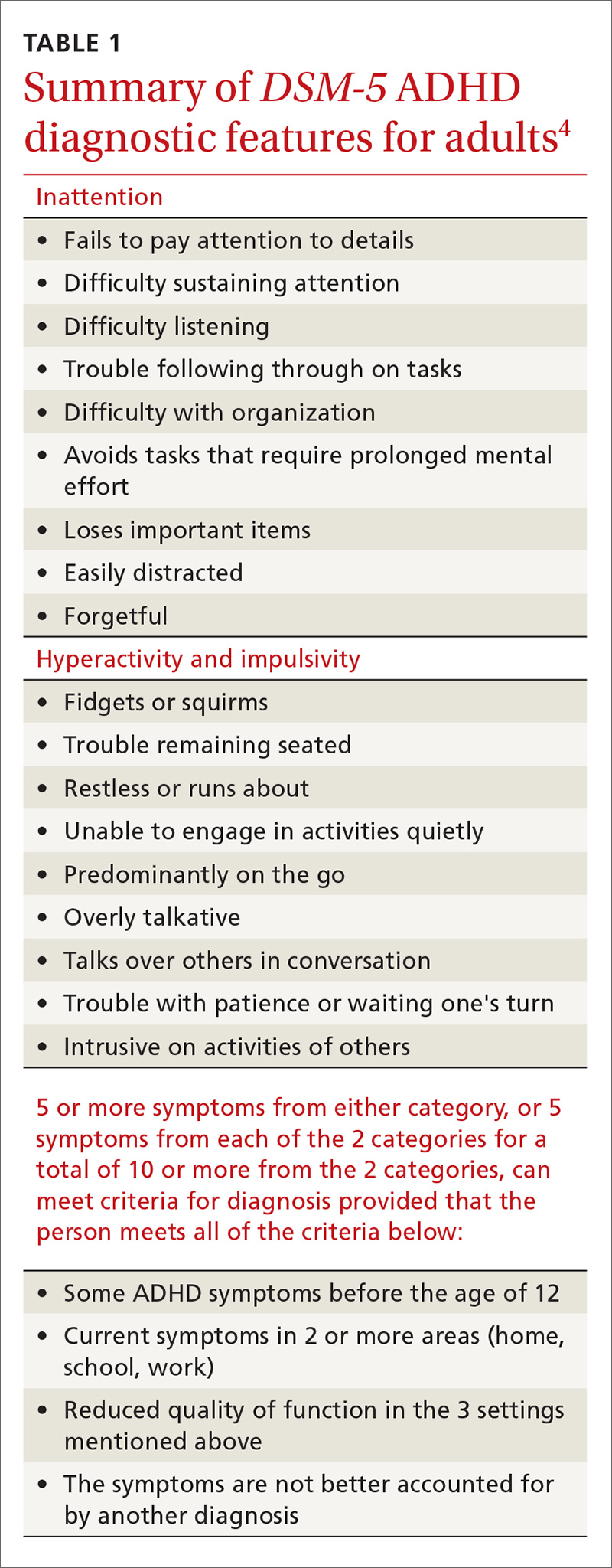
In addition, patients must meet the diagnostic criteria for ADHD for at least 6 months, have had some of the symptoms prior to age 12, and the symptoms must cause significant impairment in 2 or more environments (eg, home, work, school). When the diagnosis is unclear, it is important to obtain collateral information from the family, school, or workplace. The requirement regarding symptomatology before age 12 indicates the need for a review of the patient’s educational history. Research reveals that many adults with ADHD struggled in school and were considered “underachievers” as students.5
Common complaints and characteristics. Previous studies have shown the following to be common complaints and characteristics of adult patients diagnosed with ADHD:5
- difficulty meeting time limits
- vocational struggles, such as frequent job changes or nonpromotion at work
- anger issues
- addiction
- relationship/social strain
- comprehension problems, and
- a family history of ADHD.
Common correlates include low socioeconomic status, driving violations, frequent injuries, legal problems, alcohol and/or tobacco use, and self-reported maladjustment.5 People treated for ADHD have a comorbid DSM diagnosis 81% of the time with the most likely diagnoses being substance abuse, depression, and anxiety.6
Adult-onset ADHD? Even though the DSM-5 criteria for an ADHD diagnosis in adulthood require that some ADHD symptoms were manifest prior to age 12, recent longitudinal research on ADHD in Brazil and the United Kingdom reveals that a large portion of people who meet the criteria for ADHD in adulthood did not meet the criteria as children. The researchers in these studies proposed that there may be a form of ADHD that manifests later in life, a so-called “adult-onset ADHD.”7 While this information is something for clinicians to consider, further research is needed to justify a paradigm shift in how ADHD is diagnosed.
Self-rating measures can offer clarification. Whether or not history-gathering leaves the diagnosis murky, self-rating measures can be valuable in rounding out the clinical picture and alerting clinicians to any inconsistencies in symptoms.8 Four common ADHD self-rating measures are provided in TABLE 2. As one example, the Adult ADHD Self-Report Scale (ASRS) Symptom Checklist is a valuable ADHD screening tool that is free of charge and takes only 5 to 10 minutes.8 Other self-report measures require a similar amount of time, but are not available on a complimentary basis.
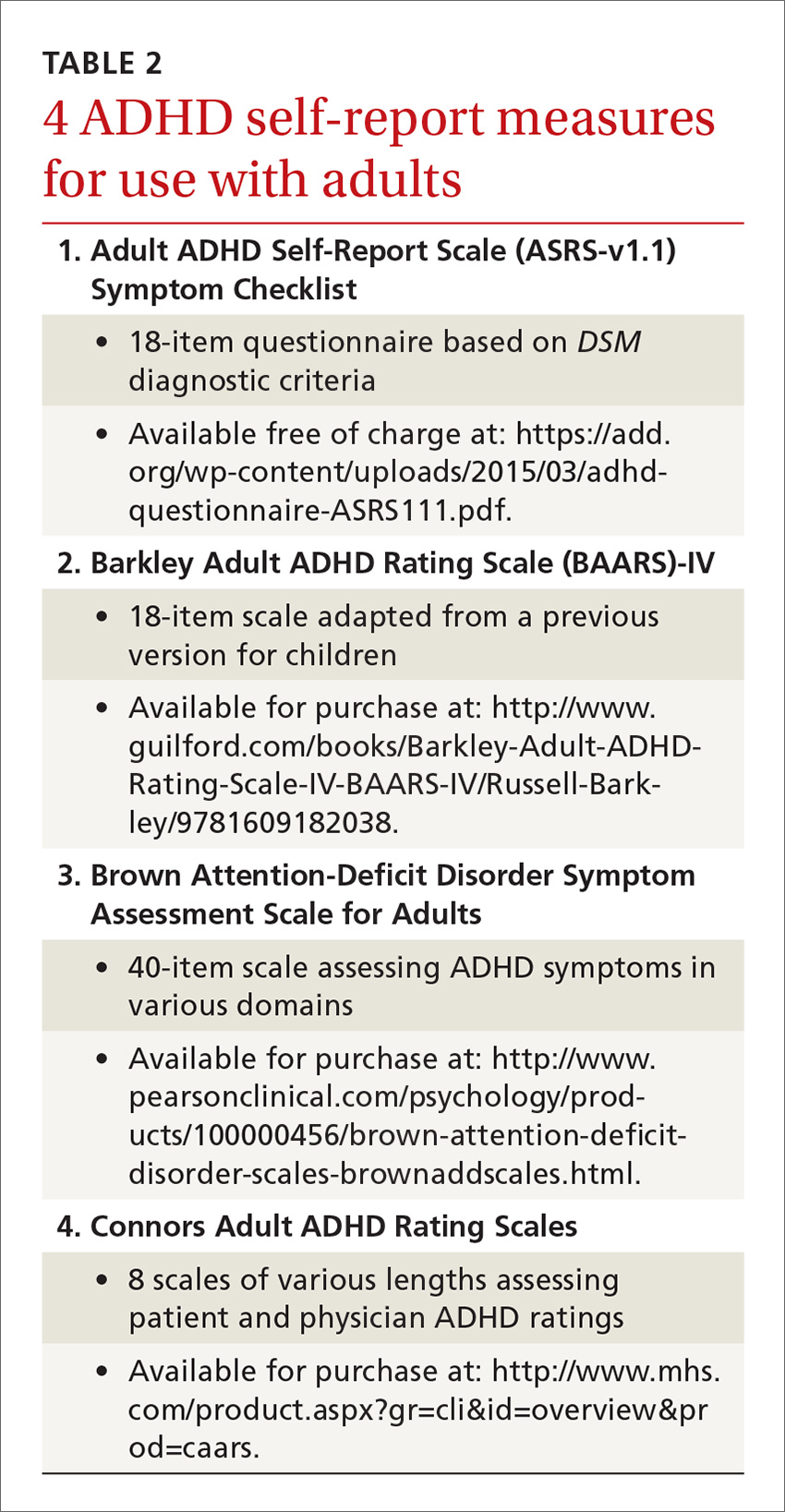
Psychological testing. Some adults who seem to have symptoms of ADHD may require a referral for psychological testing. These may be patients who present with complicated cases or whose histories and/or findings do not consistently indicate an ADHD diagnosis. In such cases, psychological testing can fill in the holes and provide a more complete picture of the patient’s neurocognitive abilities and deficits.9,10
Psychostimulant treatment: Opt for longer-acting agents
The standard treatment for ADHD is a psychostimulant. One controlled trial, for example, of a mixed amphetamine salts compound (Adderall) found that the compound effectively treated ADHD symptoms (hyperactivity, impulsivity, inattention) in adults and was well tolerated.11 While far fewer studies have been performed in adult vs youth populations, those that have been conducted in adults indicate that psychostimulants are largely safe and efficacious. In fact, the study mentioned above found that 70% of patients with ADHD ages 18 and older reported improvement of symptoms while on a short-acting psychostimulant, as compared to 7% who reported improvement on placebo.11
Similarly, a meta-analysis of 1991 participants in 11 studies found significant improvement in patients who received medication vs placebo, with stimulant medications demonstrating greater efficacy than non-stimulant treatments for ADHD.12 In general, psychostimulant treatment for adults is similar to that for children; the only difference is that adults tend to be more forthcoming with information regarding how the treatment is working and what adjustments might be needed.
Longer-acting stimulants (ie, extended release) tend to be preferred by patients to short-acting ones because they typically provide adequate control of symptoms over a longer period of time and thus may be taken less frequently.13 Also, the potential for abuse of psychostimulant medication tends to be lower with the longer-acting, extended-release formulations.14 A shorter acting formulation may be preferred if a patient has a specific window of time when their ADHD symptoms impact them. For example, a patient may request a short-acting form of medication for afternoons if he or she has to attend many business meetings at that time of day. A relatively new category is the intermediate-acting psychostimulants. For more on specific psychostimulants, see Table 3.15
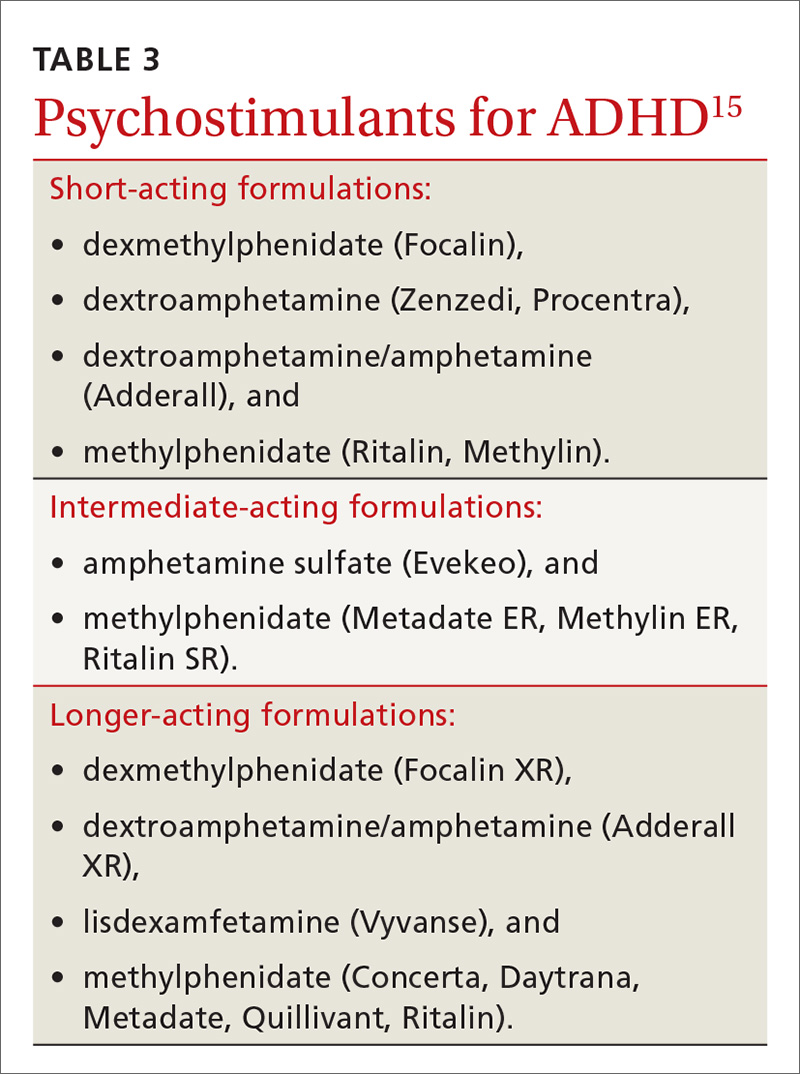
Adverse effects lead many to discontinue treatment
Regardless of the length of action of the psychostimulant, studies show that about 30% of adults (and, incidentally, 10% to 30% of children) discontinue treatment due to uncontrolled/unwanted symptoms or adverse effects.16 These include decreased appetite, headache, insomnia, abdominal pain, and irritable mood.17 If you are prescribing a psychostimulant for an adult with ADHD, it is important to tell the patient that if the effects become intolerable, adjustments can be made, such as tweaking dosages, switching to a different medication, or adding an adjunctive therapy such as cognitive behavioral therapy. Keep in mind, too, that if a medication is to be discontinued, tapering is suggested for most psychostimulants; patients should take a lower (eg, half) dose for about a week prior to complete discontinuation. People who have difficulties with a number of treatments for ADHD should be reevaluated in a year to see if circumstances have changed.5
Combatting misuse and diversion
Perhaps the most controversial issues surrounding the treatment of adults with ADHD are abuse and diversion of psychostimulants. Abuse generally refers to misuse of the drug by the person prescribed the agent, whereas diversion refers to use of the drug by people for whom the drug was not intended—with or without the prescribee’s knowledge.3 Although rare, chronic abuse of psychostimulants can lead to serious problems such as aggression, suicidal thoughts/behaviors, psychosis, and mania.5
While earlier studies tended to downplay the likelihood of diversion, recent research indicates that physicians should not underestimate the possibility. In fact, a previous article in this journal about student athletes with ADHD (http://bit.ly/2k1a6TL) indicated that psychostimulants have “great potential for misuse” and that recently there has been “a surge in nonprescription stimulant use among adolescents and young adults.”17 The authors of the article concluded, however, that while physicians should be aware of the potential for misuse, fear should not preclude treatment.17
A national multi-cohort study of 4572 US high school seniors who had used psychostimulants either medically or nonmedically indicated that while one in 6 high school seniors had been exposed to psychostimulants, about half were appropriately exposed through prescription use, while the other half was not. The researchers also reported that current nonmedical users of psychostimulants and those with a history of nonmedical use had a greater risk of substance use and abuse when compared to medical users of psychostimulants.18
Young men are at higher risk for diversion. In a nationwide survey of a sample of adults ages 18 to 49 years who had a prescription for psychostimulant medication in the past month, 17% admitted diverting their medication.
In another study, 483 students ages 17 to 19 years were followed for one year and interviewed frequently regarding their use of medications.20 The researchers reported that the lifetime prevalence of diversion of any medication in those students was around 36%. They also found that of those who diverted medication, 62% diverted ADHD medications at least once. These were most commonly diverted by sharing (34%) and selling (9%) the psychostimulants. Interview analysis revealed that those students who diverted were more likely to have used illicit drugs and to have had conduct problems. The authors advised “vigilance regarding…stimulant medications for young adults.”
Psychostimulant prescriptions do not cause substance abuse. Nevertheless, a salient point in the literature is that there is no causal relationship between psychostimulant prescriptions that are properly prescribed for people who have ADHD and substance abuse. One study that followed young people with ADHD for 8 years into adulthood revealed that psychostimulant treatment did not make adolescents or young adults any more or less likely to abuse drugs.21 The study also found that alcohol use was common in young adults whether they were diagnosed with ADHD or not. Nonetheless, family physicians should urge those taking psychostimulants to refrain from alcohol use or at least to drink in moderation.
The bottom line is that adults diagnosed with ADHD carry about the same risk of substance abuse as the general population if they are effectively treated for their presenting attention problems.22 If they are taking a psychostimulant, however, they have access to a controlled substance, unlike most of their cohorts. So it's important to teach patients with ADHD that for safety and legal reasons, they should not share or sell their stimulant medication to anyone.
Minimize the risk for abuse, diversion using these strategies
As with any drug regimen, it is important to monitor the patient’s response to treatment and minimize adverse effects and outcomes. When the drug is a psychostimulant for adults diagnosed with ADHD, it’s also important to minimize the risk for abuse and diversion. The following steps can help:
- Obtain a signed controlled substance agreement.23 This agreement between the physician and the patient usually outlines such specifics as frequency of office visits, circumstances surrounding medication refills, urine drug monitoring, and pill counts. (For more on the specifics of a controlled substance agreement, see "Key points of a controlled substance agreement.")
- Schedule frequent follow-up appointments with open communication about abuse and diversion.20,23 The age-old adage, “Start low, go slow,” applies to stimulant medications for ADHD. Medication dosage may vary and necessitate titration depending on the person’s weight and tolerance. At the onset of treatment, frequent office visits allow the physician to gauge treatment response and the patient’s commitment to therapy.
- Review your state’s prescription drug monitoring program.24 It is imperative that providers check their state’s medical board rules for prescribing controlled medications to ensure practice compliance. As diversion rates of controlled medications have risen in this country, most states have established monitoring systems through their pharmacy boards.24 Although the names of the programs vary, these prescription drug monitoring programs provide information on any medication prescribed. This allows the prescribing physician to ensure patient compliance and ascertain that no other controlled medications are being prescribed that could interfere with treatment. (For more information about state prescription drug monitoring programs, see https://www.deadiversion.usdoj.gov/faq/rx_monitor.htm.)
- Perform random urine drug screenings (UDS).20,23 An important strategy for ensuring adherence to the treatment plan and the controlled substance contract is UDS. Explain to patients that this is a way of making sure they are taking the medication exactly as prescribed. If the UDS indicates that the patient has not been taking the medication, then the provider should intervene by either restricting or discontinuing the controlled substance to prevent or counteract potential diversion. Similarly, if a higher dose is requested by a patient, the provider can closely monitor the situation to determine whether the additional drug is actually being taken and whether the dose is optimal. (See JFP’s October 2016 “3 in 3” video on urine drug testing at: http://bit.ly/2iDnfgD.)
- Employ a team-based, multimodal approach.25 A referral to a mental health professional and multimodal treatment are often recommended in the literature as best practices.25 Behavioral therapies are a cornerstone of treatment in adults with ADHD and often serve as important adjuncts to pharmacotherapy. Also, a referral provides a second professional opinion about the patient’s motivations, adherence, and response to treatment.
Trained cognitive behavioral therapists (eg, psychologists, counselors) can be helpful with treatment for ADHD.23 Therapists can be useful in setting goals for the patient regarding adherence, organization, impulse control, and social skills training. Therapists may wish to involve the family in treatment, depending on the nature of the patient’s presenting issues.
SIDEBAR
Key points of a controlled substance agreementThe primary purpose of a controlled substance agreement is to provide clarity for the provider and the patient regarding the use of controlled medications. The document is meant to prevent potential problems and confusion down the road. There are generally 3 parts:
- a doctor/patient agreement
- information about medications
- patient consent to utilize controlled substances that the provider believes would be beneficial.
Patients are typically told of the potential value of controlled medications in helping them and are warned about the potential for problems should the medications be used in ways other than intended. While wording may differ, patients are generally asked to agree to variations of the following 10 guidelines:
- I will talk with my doctor before using more than the prescribed amount of the medicine or discontinuing its use.
- I will tell my doctor if new medications are prescribed by another provider.
- I will tell the doctor if I become pregnant, so that any necessary medication adjustments can be made.
- If I abuse this drug, I understand that the doctor may need to stop treatment.
- I will uphold the visit schedule to the office/clinic according to guidelines for controlled substances (eg, every 90 days).
- I will refrain from using illicit drugs including marijuana and excessive quantities of alcohol.
- I will refrain from sharing, trading, or selling controlled substances.
- I will submit to regular urine drug screens as requested by the doctor.
- I understand that a failed drug screen may mean discontinuation of treatment.
- I will be forthright and honest about how the treatment is going, adverse effects, and how I am taking the medication.
Adapted from: https://www.drugabuse.gov/sites/default/files/files/SamplePatientAgreementForms.pdf.
Don’t tempt fate. As with any controlled medication, safe storage of psychostimulants is paramount. Patients should be urged to keep their medication in a locked box or cupboard that is accessible to only the adult for whom the drug is prescribed. Prior research cautions that open access to controlled substances can lead to larger issues with abuse and diversion, particularly when adolescents are in the home.26
Consider atomoxetine. Research has also demonstrated that the non-stimulant medication atomoxetine has some benefit in the treatment of ADHD.12 Unlike psychostimulants that act on the neurotransmitter dopamine, atomoxetine acts on the neurotransmitter norepinephrine. This different mechanism of action results in a lower potential for abuse and diversion.
CORRESPONDENCE
Scott A. Fields, PhD, 3200 MacCorkle Avenue Southeast, 5th Floor, Robert C. Byrd Clinical Teaching Center, Department of Family Medicine, Charleston, WV 25304; sfields@hsc.wvu.edu.
1. Kessler RC, Adler LA, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163:716-723.
2. Clemow DB, Walker DJ. The potential for misuse and abuse of medications in ADHD: a review. Postgrad Med. 2014;126:64-81.
3. Novak SP, Kroutil LA, Williams RL, et al. The nonmedical use of prescription ADHD medications: results from a national internet panel. Subst Abuse Treat Prev Policy. 2007;2:32.
4. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: American Psychiatric Association Press; 2013.
5. Kolar D, Keller A, Golfinopoulos M, et al. Treatment of adults with attention-deficit/hyperactivity disorder. Neuropsychiatr Dis Treat. 2008;4:389-403.
6. McGough JJ, Smalley SL, McCracken JT, et al. Psychiatric comorbidity in adult attention deficit hyperactivity disorder: findings from multiplex families. Am J Psychiatry. 2005;162:1621-1627.
7. Faraone SV, Biederman J. Can attention-deficit/hyperactivity disorder onset occur in adulthood? JAMA Psychiatry.
8. van de Glind G, van den Brink W, Koeter MWJ, et al. Validity of the Adult ADHD Self-Report Scale (ASRS) as a screener for adult ADHD in treatment seeking substance use disorder patients. Drug Alcohol Depend. 2013;132:587-596.
9. Gualtieri CT, Johnson LG. ADHD: Is objective diagnosis possible? Psychiatry. 2005;2:44-53.
10. Perrin AE, Jotwani VM. Addressing the unique issues of student athletes with ADHD. J Fam Pract. 2014;63:E1-E9.
11. Spencer T, Biederman J, Wilens T, et al. Efficacy of mixed amphetamine salts compound in adults with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 2001;58:775-782.
12. Mészáros A, Czobor P, Bálint S, et al. Pharmacotherapy of adult attention deficit hyperactivity disorder (ADHD): a meta-analysis. Int J Neuropsychopharmacol. 2009;12:1137-1147.
13. Weiss M, Shingler T, Capone NM. Medication satisfaction among adults with ADHD: long term results from the Quality of Life, Effectiveness, Safety and Tolerability (Qu.S.T) study. New Orleans: Program and Abstracts of the 19th US Psychiatric and Mental Health Congress, Abstract 120, 2006.
14. Lopez FA, Leroux JR.
15. Felt BT, Biermann B, Christner JG, et al. Diagnosis and management of ADHD in children. Am Fam Physician. 2014;90:456-464.
16. Spencer T, Biederman J, Wilens T. Nonstimulant treatment of adult attention-deficit/hyperactivity disorder. Psychiatr Clin North Am. 2004;27:373-383.
17. Withrow LM, Hash PA, Holten KB. Managing ADHD in children: are you doing enough? J Fam Pract. 2011;60:E1-E3.
18. McCabe SE, West BT. Medical and nonmedical use of prescription stimulants: results from a national multicohort study. J Am Acad Child Adolesc Psychiatry. 2013;52:1272-1280.
19. Aldridge AP, Kroutil LA, Cowell AJ, et al. Medication costs to private insurers of diversion of medications for attention-deficit hyperactivity disorder. Pharmacoeconomics. 2011;29:621-635.
20. Garnier LM, Arria AM, Caldeira KM, et al. Sharing and selling of prescription medications in a college student sample. J Clin Psychiatry. 2010;71:262-269.
21. Molina BSG, Hinshaw SP, Arnold LE, et al. Adolescent substance use in the Multimodal Treatment Study of Attention-Deficit/Hyperactivity Disorder (ADHD) (MTA) as a function of childhood ADHD, random assignment to childhood treatments, and subsequent medication. J Am Acad Child Adolesc Psychiatry. 2013;52:250-263.
22. Brahmbhatt K, Hilty DM, Hah M, et al. Diagnosis and treatment of attention deficit hyperactivity disorder during adolescence in the primary care setting: a concise review. J Adolesc Health. 2016;59:135-143.
23. Post RE, Kurlansik SL. Diagnosis and management of attention-deficit/hyperactivity disorder in adults. Am Fam Physician. 2012;85:890-896.
24. Cepeda MS, Fife D, Berwaerts J, et al. Doctor shopping for medications used in the treatment of attention deficit hyperactivity disorder: shoppers often pay in cash and cross state lines. Am J Drug Alcohol Abuse. 2015;41:226-229.
25. Safren SA, Sprich S, Mimiaga MJ, et al. Cognitive behavioral therapy vs relaxation with educational support for medication-treated adults with ADHD and persistent symptoms: a randomized controlled trial. JAMA. 2010;304:875-880.
26. Ross-Durow PL, McCabe SE, Boyd CJ. Adolescents’ access to their own prescription medication in the home. J Adolesc Health. 2013;53:260-264.
1. Kessler RC, Adler LA, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163:716-723.
2. Clemow DB, Walker DJ. The potential for misuse and abuse of medications in ADHD: a review. Postgrad Med. 2014;126:64-81.
3. Novak SP, Kroutil LA, Williams RL, et al. The nonmedical use of prescription ADHD medications: results from a national internet panel. Subst Abuse Treat Prev Policy. 2007;2:32.
4. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: American Psychiatric Association Press; 2013.
5. Kolar D, Keller A, Golfinopoulos M, et al. Treatment of adults with attention-deficit/hyperactivity disorder. Neuropsychiatr Dis Treat. 2008;4:389-403.
6. McGough JJ, Smalley SL, McCracken JT, et al. Psychiatric comorbidity in adult attention deficit hyperactivity disorder: findings from multiplex families. Am J Psychiatry. 2005;162:1621-1627.
7. Faraone SV, Biederman J. Can attention-deficit/hyperactivity disorder onset occur in adulthood? JAMA Psychiatry.
8. van de Glind G, van den Brink W, Koeter MWJ, et al. Validity of the Adult ADHD Self-Report Scale (ASRS) as a screener for adult ADHD in treatment seeking substance use disorder patients. Drug Alcohol Depend. 2013;132:587-596.
9. Gualtieri CT, Johnson LG. ADHD: Is objective diagnosis possible? Psychiatry. 2005;2:44-53.
10. Perrin AE, Jotwani VM. Addressing the unique issues of student athletes with ADHD. J Fam Pract. 2014;63:E1-E9.
11. Spencer T, Biederman J, Wilens T, et al. Efficacy of mixed amphetamine salts compound in adults with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 2001;58:775-782.
12. Mészáros A, Czobor P, Bálint S, et al. Pharmacotherapy of adult attention deficit hyperactivity disorder (ADHD): a meta-analysis. Int J Neuropsychopharmacol. 2009;12:1137-1147.
13. Weiss M, Shingler T, Capone NM. Medication satisfaction among adults with ADHD: long term results from the Quality of Life, Effectiveness, Safety and Tolerability (Qu.S.T) study. New Orleans: Program and Abstracts of the 19th US Psychiatric and Mental Health Congress, Abstract 120, 2006.
14. Lopez FA, Leroux JR.
15. Felt BT, Biermann B, Christner JG, et al. Diagnosis and management of ADHD in children. Am Fam Physician. 2014;90:456-464.
16. Spencer T, Biederman J, Wilens T. Nonstimulant treatment of adult attention-deficit/hyperactivity disorder. Psychiatr Clin North Am. 2004;27:373-383.
17. Withrow LM, Hash PA, Holten KB. Managing ADHD in children: are you doing enough? J Fam Pract. 2011;60:E1-E3.
18. McCabe SE, West BT. Medical and nonmedical use of prescription stimulants: results from a national multicohort study. J Am Acad Child Adolesc Psychiatry. 2013;52:1272-1280.
19. Aldridge AP, Kroutil LA, Cowell AJ, et al. Medication costs to private insurers of diversion of medications for attention-deficit hyperactivity disorder. Pharmacoeconomics. 2011;29:621-635.
20. Garnier LM, Arria AM, Caldeira KM, et al. Sharing and selling of prescription medications in a college student sample. J Clin Psychiatry. 2010;71:262-269.
21. Molina BSG, Hinshaw SP, Arnold LE, et al. Adolescent substance use in the Multimodal Treatment Study of Attention-Deficit/Hyperactivity Disorder (ADHD) (MTA) as a function of childhood ADHD, random assignment to childhood treatments, and subsequent medication. J Am Acad Child Adolesc Psychiatry. 2013;52:250-263.
22. Brahmbhatt K, Hilty DM, Hah M, et al. Diagnosis and treatment of attention deficit hyperactivity disorder during adolescence in the primary care setting: a concise review. J Adolesc Health. 2016;59:135-143.
23. Post RE, Kurlansik SL. Diagnosis and management of attention-deficit/hyperactivity disorder in adults. Am Fam Physician. 2012;85:890-896.
24. Cepeda MS, Fife D, Berwaerts J, et al. Doctor shopping for medications used in the treatment of attention deficit hyperactivity disorder: shoppers often pay in cash and cross state lines. Am J Drug Alcohol Abuse. 2015;41:226-229.
25. Safren SA, Sprich S, Mimiaga MJ, et al. Cognitive behavioral therapy vs relaxation with educational support for medication-treated adults with ADHD and persistent symptoms: a randomized controlled trial. JAMA. 2010;304:875-880.
26. Ross-Durow PL, McCabe SE, Boyd CJ. Adolescents’ access to their own prescription medication in the home. J Adolesc Health. 2013;53:260-264.
PRACTICE RECOMMENDATIONS
› Be sure to take steps, which include utilization of a self-report measure—to correctly diagnose attention-deficit/hyperactivity disorder (ADHD) in adult patients before beginning treatment.
› Consider prescribing stimulant medications, such as the short-acting dextroamphetamine/amphetamine or the long-acting lisdexamfetamine, for adults with ADHD.
› Don't underestimate the problems of misuse and diversion among patients taking psychostimulant medications, particularly among younger men.
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series