User login
Verbal Communication at Discharge
Hospital discharge can be hazardous because discontinuity and fragmentation of care increase risks to the patient. Inadequate communication has been identified as a major etiology for errors and adverse events occurring shortly after discharge.1, 2 Another potential result of a failed hospital discharge is patient dissatisfaction. Increased patient involvement in care improves health outcomes, and may improve patient satisfaction.3 To engage patients in their care, healthcare providers must collaborate with patients to coordinate care across settings.
In this study, we sought to determine what patients and their caregivers view as essential elements of a safe and high‐quality discharge process. We developed a survey with a broad range of questions related to the hospital discharge process (see Supporting Information, Appendix A, in the online version of this article). The survey included several questions derived from Project BOOST (Better Outcomes for Older adults through Safe Transitions) discharge care plans.4
METHODS
Study Design
We surveyed patients on the second day of admission to the internal medicine wards at the University of Washington Medical Center (a 450‐bed tertiary care teaching hospital) and Harborview Medical Center (a 412‐bed county teaching hospital) from June 1, 2010 to August 1, 2010. All patients 18 years old who were admitted during weekdays were considered for participation. Any potential participant unable to manually fill out the survey was offered the opportunity to use a proxy to help complete the survey. A proxy was any adult support person who was present in the room at the time the patient was approached with the opportunity to participate. Patients were excluded only if they (or their proxies) could not read English. The second day of hospitalization was chosen for several reasons: 1) to attempt to assess patients at a similar point in their hospital stay; 2) to avoid the day of discharge, as this may have introduced confounders such as patients who were actively engaged in the discharge process; and 3) to avoid the day of admission to increase the likelihood that patients would be medically stable at the time of the survey.
The Survey
The study protocol was reviewed and approved by the University of Washington Committee for the Protection of Human Subjects. All subjects gave verbal informed consent. The survey consisted of 3 sections: demographics, questions gauging the importance of various key points in the discharge process to patients, and open‐ended questions. Responses to questions used a Likert scale. Responses to open‐ended questions were handwritten on the paper survey.
Statistical Analysis
The quantitative data were classified categorically and analyzed using Fisher's exact test. Three investigators (M.S., S.E.M., M.B.J.) individually reviewed and coded all written patient or proxy comments using grounded theory methodology.5 Discrepant coding was identified and reconciled. The reconciled coded comments were aggregated into themes.
RESULTS
Demographics
We screened 240 patients or proxies and 200 completed the survey; 10.4% were ineligible due to language barrier, and 6.3% refused. Ninety‐two percent of patients completed the surveys. A majority were male (62.5%), 1859 years old (80%); spoke English as their first language (66%); were community‐dwelling prior to hospitalization (59%); were followed by a primary care provider (PCP) (53%), and many had at least a 4‐year‐college education (45%). One hundred eighty‐five surveys (92.5%) were completed by patients, and 15 (7.5%) were completed by proxies. Ninety surveys were completed at the county teaching hospital, and 110 surveys were completed at the tertiary teaching hospital. See Table 1 for detailed demographic information.
| Patient age, n (%) | |
| 1859 yr | 160 (80) |
| 6069 yr | 30 (15) |
| 7079 yr | 5 (2.5) |
| 80 and older | 5 (2.5) |
| Patient gender, n (%) | |
| Male | 125 (62.5) |
| Female | 75 (37.5) |
| Patient schooling, n (%) | |
| Less than high school | 20 (10) |
| High school | 50 (25) |
| Two‐year college | 40 (20) |
| Four‐year college | 70 (35) |
| Graduate education | 20 (10) |
| English is patient's first language, n (%) | |
| Yes | 132 (66) |
| No | 68 (34) |
| Patient has a primary care doctor, n (%) | |
| Yes | 106 (53) |
| No | 94 (47) |
| Patient's residence before hospitalization, n (%) | |
| Home without home health | 64 (32) |
| Home with home health | 54 (27) |
| Skilled nursing facility | 52 (26) |
| Shelter | 30 (15) |
Survey Results
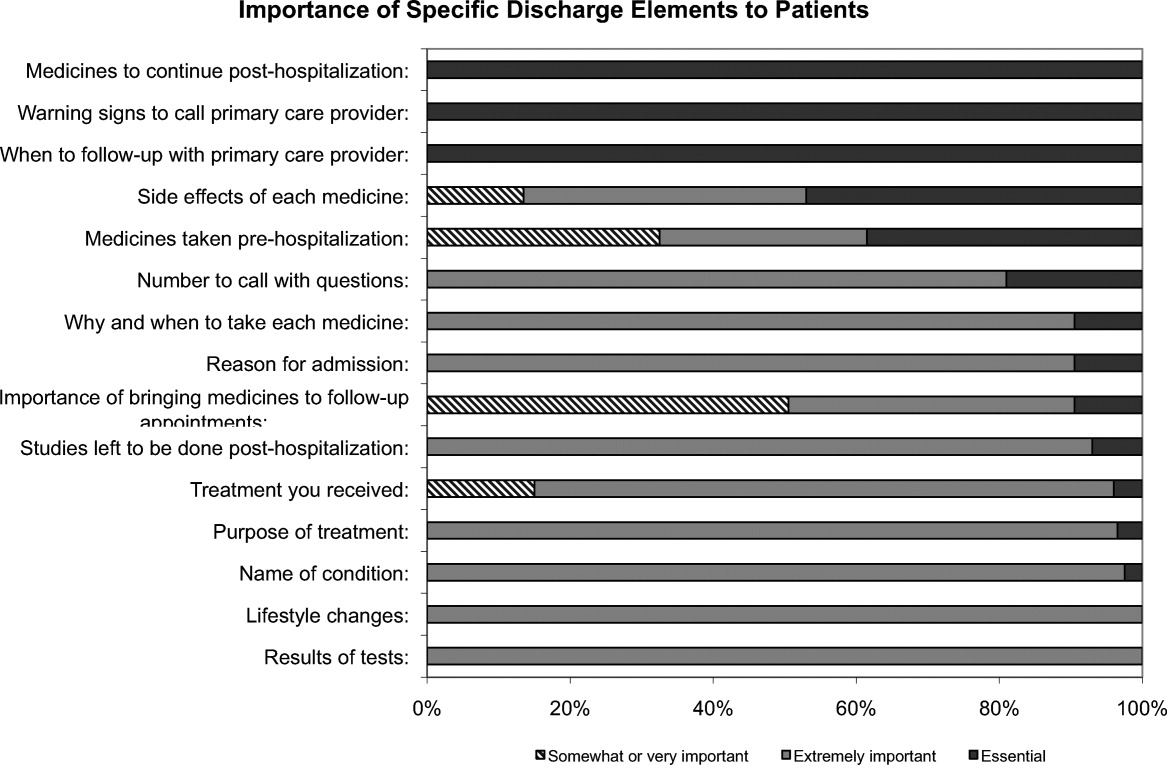
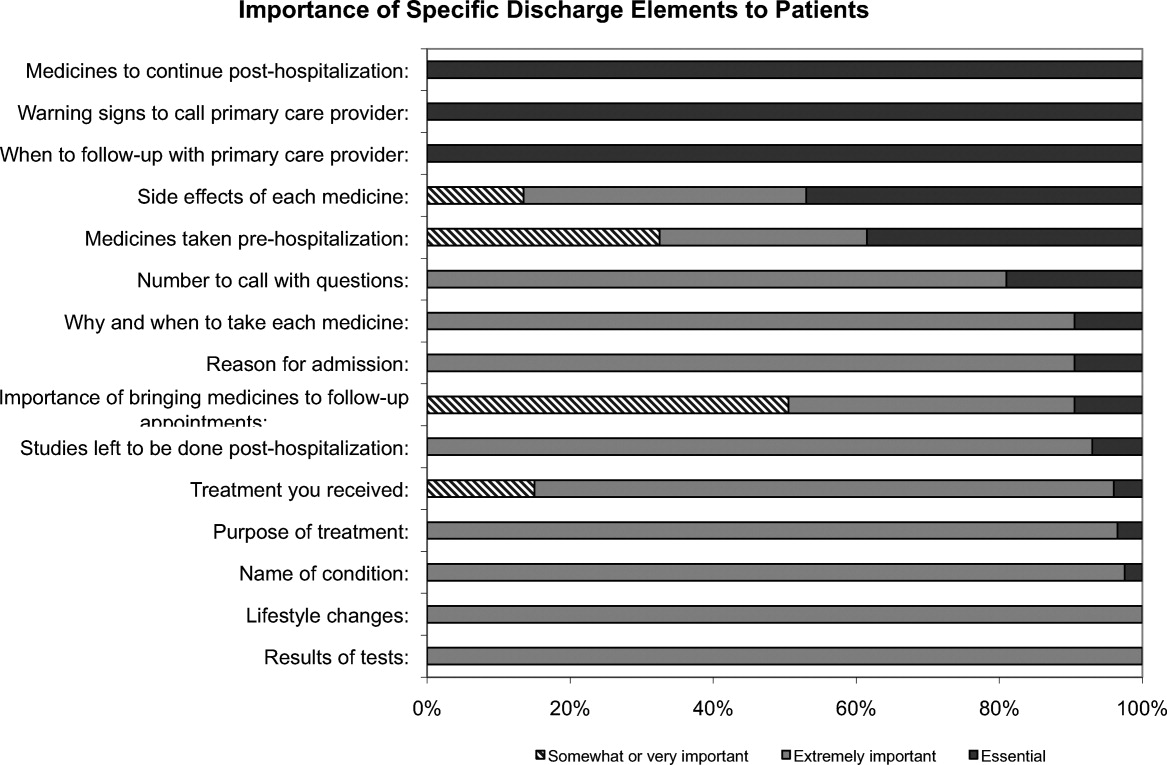
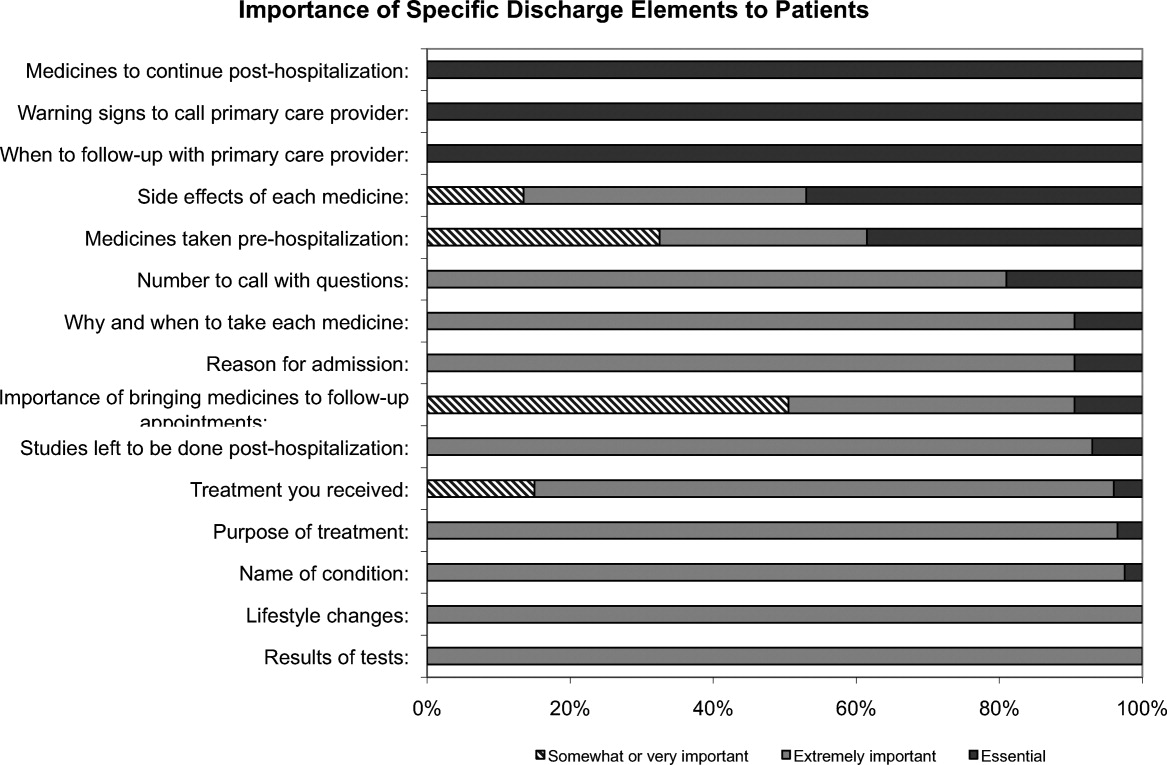
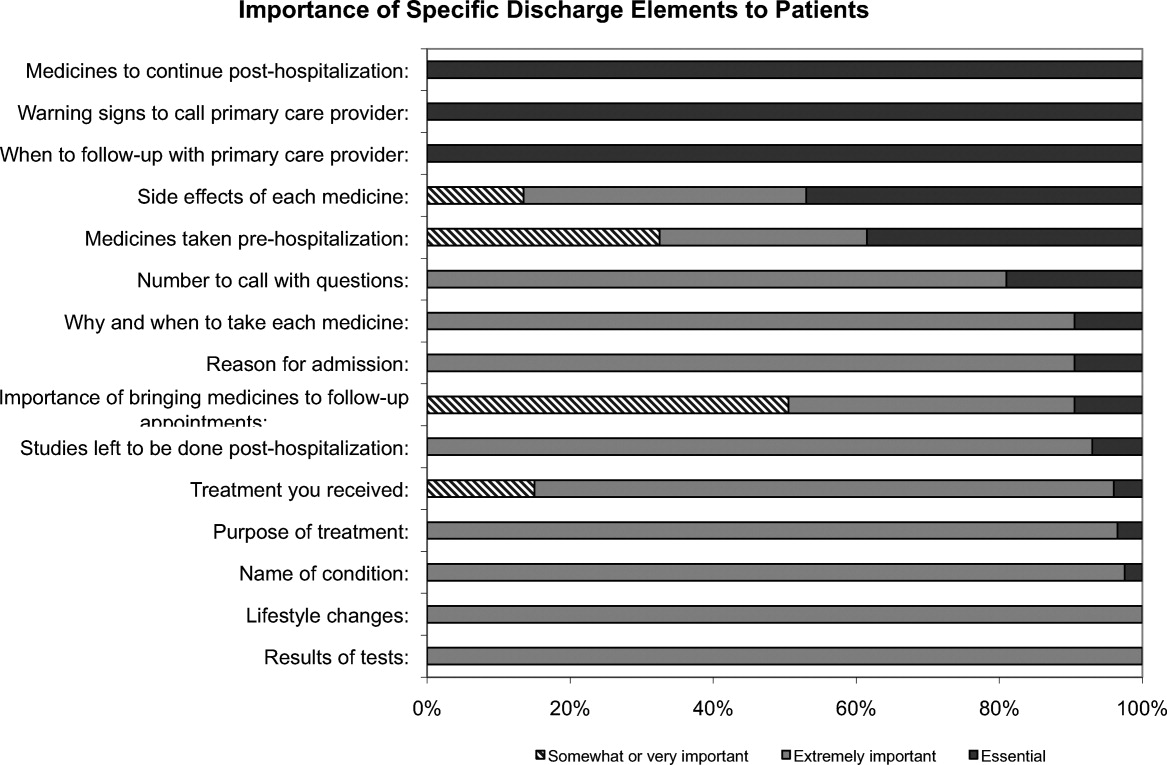
One hundred percent of patients rated the following items as essential (highest category on Likert Scale): when you need to follow‐up with primary care doctor, warning signs to call primary care doctor, and medicines to continue post‐hospitalization (Figure 1). Patients rated the following items as less important (these items were not unanimously rated as extremely important or essential): treatment you received, medicines you took pre‐hospitalization, importance of bringing all your medicines to follow‐up appointments, and given the side effect of each medication. One hundred percent of patients wanted a lot of explanation (highest category on Likert Scale) about my condition and my test results. Only 39% of patients wanted a lot of explanation about discharge medications. Sixty‐one percent wanted somewhat of an explanation about discharge medications. When asked to choose the most important piece of information, 67.5% of patients chose lifestyle changes. See Figure 1 for the relative importance of the items.
The majority of patients surveyed, 173 (86.5%), wanted verbal discharge instructions with or without written discharge instructions, with only 10.5% requesting only written discharge instructions (P < 0.0001). The majority of patients, 168 (84%), wanted resources to read about their medical condition, with 97 (57%) requesting brochures and 62 (36.9%) requesting Web sites. One hundred percent of patients thought that personal communication between the inpatient provider and the primary care doctor was extremely important or essential.
We identified 4 major themes in our qualitative review of the patients' and proxies' comments: verbal communication, frustration, opacity of system, and too many physicians. Participant quotes related to the 4 major themes are presented in Table 2. Many participants expressed a desire for verbal, rather than written, communication at the time of discharge with their healthcare team; patients particularly requested time for verbal communication with their physician. In the frustration theme, many patients and caregivers expressed frustration that the healthcare team was not carefully listening to them. In the theme of too many physicians, many patients expressed feeling overwhelmed by the number of different doctors involved in their care; particularly at discharge, patients did not know to whom to direct questions. Finally, as part of the opacity of system theme, patient comments included concerns regarding how information will be passed to outside doctors, and that the system of communication is not clear.
| Verbal communication |
| Can we just stop and talk? Everybody is rushing in and out. |
| I just want my doctor to stop by before I go home and tell me what the plan is. |
| Sometimes I feel like no one is talking to me. All they do is give me paperwork. |
| I want my doctors to sit down with me before I leave the hospital and tell me exactly what I need to do so that I don't come back. |
| I don't want papers, I want people. I want to talk to someone and not read my problems from a sheet of paper. |
| Frustration |
| I wonder sometimes if anyone is listening to me I seem to be part of a very elaborate organization that has its own rules and regulations and will not alter its ways. |
| Why do I have to keep retelling my story? It gets tiring. I wish my story could just be told once. |
| Too many physicians |
| I saw lots of doctors during my time here, but I didn't see them again when I was leaving. |
| I see so many doctors I have no idea who is in charge and who I should direct my questions to. |
| I feel overwhelmed by the number of doctors I see every time I come into the hospital. |
| I want my main doctor to talk to me. I get so confused when I hear from more than one doctor. |
| I miss the days when my primary doctor came in to check on me. He knew exactly what I needed. Now, I meet new people every time I go into the hospital. |
| Opacity of system |
| I wonder if all my doctors talk to each other. Sometimes, it seems like they don't. |
| Who keeps track of all this information? Is there someone who will pass on what happened to me here to the outside world? |
DISCUSSION
Discharge is a period of transition from hospital to home that involves a transfer in responsibility from the inpatient care team to the patient and/or caregivers and primary care physician. Ineffective communication, planning, and coordination of care can undermine patient satisfaction, increase adverse events, and contribute to more frequent hospital readmissions.
The patients we surveyed uniformly placed high value on verbal (more than written) communication about discharge care plans. Protected time during the discharge process for hospital staff to provide verbal recommendations to patients, especially about when they should return for follow‐up, warning signs to contact PCP sooner, and medications to continue after discharge, may improve patient satisfaction.
In open‐ended comments, several subjects suggested that physicians should sit down in the patient's room and provide verbal discharge instructions. Although it is well recognized that verbal communication alone has limitations and that providing patients with written instructions remains crucial, verbal reinforcement may highlight the most important instructions.
Interestingly, subjects valued information about lifestyle changes over detailed information about their medications. This may suggest that hospitalized patients are particularly receptive to information about lifestyle changes such as smoking cessation or importance of compliance with medical appointments.
Lastly, patients we surveyed value personal communication between inpatient and outpatient providers. It is plausible that this would improve transitions of care, and previous studies have suggested that direct communication between inpatient and outpatient providers occurs infrequently, with only 20% of primary care providers in 1 study reporting that they are always notified when their patient is being discharged from a hospitalist service.6
The themes that emerged from our open‐ended questions also highlight the importance of direct verbal communication with patients and careful coordination of care with outside physicians. Because patients may be unlikely to fully remember verbal instructions at discharge, providers may consider providing patients and family members with patient‐centered written materials to take home in order to reinforce important self‐care instructions. The patient comments further suggest that patients may be more satisfied, and that discharges may be smoother, if 1 or 2 physicians were always identified to the patients and their caregivers as the leaders of the care team throughout the hospital course and discharge process.
Our study had several limitations. We only surveyed patients on general medicine services, so our findings might not apply to other populations. We did not enroll participants on weekends and holidays; it is possible that this led to some bias in the enrollment of subjects. We also only surveyed patients and/or proxies who could speak and read English, and this was a fairly highly educated population, with almost half having completed 4 years of college. Finally, we relied on participant self‐report for demographic information because we did not have access to the electronic medical record. This study was conducted at 2 large academic medical centers that include resident physicians in the daily care of patients; thus, these results may not be generalizable to other settings.
Effective verbal communication between physicians, outpatient providers, patients, and their caregivers about discharge care plans might improve patients' understanding of their hospitalizations, increase their satisfaction with care, and reduce readmissions. In addition, physicians should recognize that patients value advice about lifestyle interventions that might improve their health, as part of the discharge care plan. Intervention studies are necessary to test these hypotheses in large, diverse populations.
Acknowledgements
Disclosure: Nothing to report.
- ,,,.Medical errors related to discontinuity of care from an inpatient to an outpatient setting.J Gen Intern Med.2003;18(8):646–651.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297(8):831–841.
- ,,.Expanding patient involvement in care. Effects on patient outcomes.Ann Intern Med.1985;102(4):520–528.
- Society of Hospital Medicine. Project BOOST, Better Outcomes for Older adults through Safe Transitions. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Home1998.
- ,,,.Primary care physician attitudes regarding communication with hospitalists.Am J Med.2001;111(9B):15S–20S.
Hospital discharge can be hazardous because discontinuity and fragmentation of care increase risks to the patient. Inadequate communication has been identified as a major etiology for errors and adverse events occurring shortly after discharge.1, 2 Another potential result of a failed hospital discharge is patient dissatisfaction. Increased patient involvement in care improves health outcomes, and may improve patient satisfaction.3 To engage patients in their care, healthcare providers must collaborate with patients to coordinate care across settings.
In this study, we sought to determine what patients and their caregivers view as essential elements of a safe and high‐quality discharge process. We developed a survey with a broad range of questions related to the hospital discharge process (see Supporting Information, Appendix A, in the online version of this article). The survey included several questions derived from Project BOOST (Better Outcomes for Older adults through Safe Transitions) discharge care plans.4
METHODS
Study Design
We surveyed patients on the second day of admission to the internal medicine wards at the University of Washington Medical Center (a 450‐bed tertiary care teaching hospital) and Harborview Medical Center (a 412‐bed county teaching hospital) from June 1, 2010 to August 1, 2010. All patients 18 years old who were admitted during weekdays were considered for participation. Any potential participant unable to manually fill out the survey was offered the opportunity to use a proxy to help complete the survey. A proxy was any adult support person who was present in the room at the time the patient was approached with the opportunity to participate. Patients were excluded only if they (or their proxies) could not read English. The second day of hospitalization was chosen for several reasons: 1) to attempt to assess patients at a similar point in their hospital stay; 2) to avoid the day of discharge, as this may have introduced confounders such as patients who were actively engaged in the discharge process; and 3) to avoid the day of admission to increase the likelihood that patients would be medically stable at the time of the survey.
The Survey
The study protocol was reviewed and approved by the University of Washington Committee for the Protection of Human Subjects. All subjects gave verbal informed consent. The survey consisted of 3 sections: demographics, questions gauging the importance of various key points in the discharge process to patients, and open‐ended questions. Responses to questions used a Likert scale. Responses to open‐ended questions were handwritten on the paper survey.
Statistical Analysis
The quantitative data were classified categorically and analyzed using Fisher's exact test. Three investigators (M.S., S.E.M., M.B.J.) individually reviewed and coded all written patient or proxy comments using grounded theory methodology.5 Discrepant coding was identified and reconciled. The reconciled coded comments were aggregated into themes.
RESULTS
Demographics
We screened 240 patients or proxies and 200 completed the survey; 10.4% were ineligible due to language barrier, and 6.3% refused. Ninety‐two percent of patients completed the surveys. A majority were male (62.5%), 1859 years old (80%); spoke English as their first language (66%); were community‐dwelling prior to hospitalization (59%); were followed by a primary care provider (PCP) (53%), and many had at least a 4‐year‐college education (45%). One hundred eighty‐five surveys (92.5%) were completed by patients, and 15 (7.5%) were completed by proxies. Ninety surveys were completed at the county teaching hospital, and 110 surveys were completed at the tertiary teaching hospital. See Table 1 for detailed demographic information.
| Patient age, n (%) | |
| 1859 yr | 160 (80) |
| 6069 yr | 30 (15) |
| 7079 yr | 5 (2.5) |
| 80 and older | 5 (2.5) |
| Patient gender, n (%) | |
| Male | 125 (62.5) |
| Female | 75 (37.5) |
| Patient schooling, n (%) | |
| Less than high school | 20 (10) |
| High school | 50 (25) |
| Two‐year college | 40 (20) |
| Four‐year college | 70 (35) |
| Graduate education | 20 (10) |
| English is patient's first language, n (%) | |
| Yes | 132 (66) |
| No | 68 (34) |
| Patient has a primary care doctor, n (%) | |
| Yes | 106 (53) |
| No | 94 (47) |
| Patient's residence before hospitalization, n (%) | |
| Home without home health | 64 (32) |
| Home with home health | 54 (27) |
| Skilled nursing facility | 52 (26) |
| Shelter | 30 (15) |
Survey Results
One hundred percent of patients rated the following items as essential (highest category on Likert Scale): when you need to follow‐up with primary care doctor, warning signs to call primary care doctor, and medicines to continue post‐hospitalization (Figure 1). Patients rated the following items as less important (these items were not unanimously rated as extremely important or essential): treatment you received, medicines you took pre‐hospitalization, importance of bringing all your medicines to follow‐up appointments, and given the side effect of each medication. One hundred percent of patients wanted a lot of explanation (highest category on Likert Scale) about my condition and my test results. Only 39% of patients wanted a lot of explanation about discharge medications. Sixty‐one percent wanted somewhat of an explanation about discharge medications. When asked to choose the most important piece of information, 67.5% of patients chose lifestyle changes. See Figure 1 for the relative importance of the items.
The majority of patients surveyed, 173 (86.5%), wanted verbal discharge instructions with or without written discharge instructions, with only 10.5% requesting only written discharge instructions (P < 0.0001). The majority of patients, 168 (84%), wanted resources to read about their medical condition, with 97 (57%) requesting brochures and 62 (36.9%) requesting Web sites. One hundred percent of patients thought that personal communication between the inpatient provider and the primary care doctor was extremely important or essential.
We identified 4 major themes in our qualitative review of the patients' and proxies' comments: verbal communication, frustration, opacity of system, and too many physicians. Participant quotes related to the 4 major themes are presented in Table 2. Many participants expressed a desire for verbal, rather than written, communication at the time of discharge with their healthcare team; patients particularly requested time for verbal communication with their physician. In the frustration theme, many patients and caregivers expressed frustration that the healthcare team was not carefully listening to them. In the theme of too many physicians, many patients expressed feeling overwhelmed by the number of different doctors involved in their care; particularly at discharge, patients did not know to whom to direct questions. Finally, as part of the opacity of system theme, patient comments included concerns regarding how information will be passed to outside doctors, and that the system of communication is not clear.
| Verbal communication |
| Can we just stop and talk? Everybody is rushing in and out. |
| I just want my doctor to stop by before I go home and tell me what the plan is. |
| Sometimes I feel like no one is talking to me. All they do is give me paperwork. |
| I want my doctors to sit down with me before I leave the hospital and tell me exactly what I need to do so that I don't come back. |
| I don't want papers, I want people. I want to talk to someone and not read my problems from a sheet of paper. |
| Frustration |
| I wonder sometimes if anyone is listening to me I seem to be part of a very elaborate organization that has its own rules and regulations and will not alter its ways. |
| Why do I have to keep retelling my story? It gets tiring. I wish my story could just be told once. |
| Too many physicians |
| I saw lots of doctors during my time here, but I didn't see them again when I was leaving. |
| I see so many doctors I have no idea who is in charge and who I should direct my questions to. |
| I feel overwhelmed by the number of doctors I see every time I come into the hospital. |
| I want my main doctor to talk to me. I get so confused when I hear from more than one doctor. |
| I miss the days when my primary doctor came in to check on me. He knew exactly what I needed. Now, I meet new people every time I go into the hospital. |
| Opacity of system |
| I wonder if all my doctors talk to each other. Sometimes, it seems like they don't. |
| Who keeps track of all this information? Is there someone who will pass on what happened to me here to the outside world? |
DISCUSSION
Discharge is a period of transition from hospital to home that involves a transfer in responsibility from the inpatient care team to the patient and/or caregivers and primary care physician. Ineffective communication, planning, and coordination of care can undermine patient satisfaction, increase adverse events, and contribute to more frequent hospital readmissions.
The patients we surveyed uniformly placed high value on verbal (more than written) communication about discharge care plans. Protected time during the discharge process for hospital staff to provide verbal recommendations to patients, especially about when they should return for follow‐up, warning signs to contact PCP sooner, and medications to continue after discharge, may improve patient satisfaction.
In open‐ended comments, several subjects suggested that physicians should sit down in the patient's room and provide verbal discharge instructions. Although it is well recognized that verbal communication alone has limitations and that providing patients with written instructions remains crucial, verbal reinforcement may highlight the most important instructions.
Interestingly, subjects valued information about lifestyle changes over detailed information about their medications. This may suggest that hospitalized patients are particularly receptive to information about lifestyle changes such as smoking cessation or importance of compliance with medical appointments.
Lastly, patients we surveyed value personal communication between inpatient and outpatient providers. It is plausible that this would improve transitions of care, and previous studies have suggested that direct communication between inpatient and outpatient providers occurs infrequently, with only 20% of primary care providers in 1 study reporting that they are always notified when their patient is being discharged from a hospitalist service.6
The themes that emerged from our open‐ended questions also highlight the importance of direct verbal communication with patients and careful coordination of care with outside physicians. Because patients may be unlikely to fully remember verbal instructions at discharge, providers may consider providing patients and family members with patient‐centered written materials to take home in order to reinforce important self‐care instructions. The patient comments further suggest that patients may be more satisfied, and that discharges may be smoother, if 1 or 2 physicians were always identified to the patients and their caregivers as the leaders of the care team throughout the hospital course and discharge process.
Our study had several limitations. We only surveyed patients on general medicine services, so our findings might not apply to other populations. We did not enroll participants on weekends and holidays; it is possible that this led to some bias in the enrollment of subjects. We also only surveyed patients and/or proxies who could speak and read English, and this was a fairly highly educated population, with almost half having completed 4 years of college. Finally, we relied on participant self‐report for demographic information because we did not have access to the electronic medical record. This study was conducted at 2 large academic medical centers that include resident physicians in the daily care of patients; thus, these results may not be generalizable to other settings.
Effective verbal communication between physicians, outpatient providers, patients, and their caregivers about discharge care plans might improve patients' understanding of their hospitalizations, increase their satisfaction with care, and reduce readmissions. In addition, physicians should recognize that patients value advice about lifestyle interventions that might improve their health, as part of the discharge care plan. Intervention studies are necessary to test these hypotheses in large, diverse populations.
Acknowledgements
Disclosure: Nothing to report.
Hospital discharge can be hazardous because discontinuity and fragmentation of care increase risks to the patient. Inadequate communication has been identified as a major etiology for errors and adverse events occurring shortly after discharge.1, 2 Another potential result of a failed hospital discharge is patient dissatisfaction. Increased patient involvement in care improves health outcomes, and may improve patient satisfaction.3 To engage patients in their care, healthcare providers must collaborate with patients to coordinate care across settings.
In this study, we sought to determine what patients and their caregivers view as essential elements of a safe and high‐quality discharge process. We developed a survey with a broad range of questions related to the hospital discharge process (see Supporting Information, Appendix A, in the online version of this article). The survey included several questions derived from Project BOOST (Better Outcomes for Older adults through Safe Transitions) discharge care plans.4
METHODS
Study Design
We surveyed patients on the second day of admission to the internal medicine wards at the University of Washington Medical Center (a 450‐bed tertiary care teaching hospital) and Harborview Medical Center (a 412‐bed county teaching hospital) from June 1, 2010 to August 1, 2010. All patients 18 years old who were admitted during weekdays were considered for participation. Any potential participant unable to manually fill out the survey was offered the opportunity to use a proxy to help complete the survey. A proxy was any adult support person who was present in the room at the time the patient was approached with the opportunity to participate. Patients were excluded only if they (or their proxies) could not read English. The second day of hospitalization was chosen for several reasons: 1) to attempt to assess patients at a similar point in their hospital stay; 2) to avoid the day of discharge, as this may have introduced confounders such as patients who were actively engaged in the discharge process; and 3) to avoid the day of admission to increase the likelihood that patients would be medically stable at the time of the survey.
The Survey
The study protocol was reviewed and approved by the University of Washington Committee for the Protection of Human Subjects. All subjects gave verbal informed consent. The survey consisted of 3 sections: demographics, questions gauging the importance of various key points in the discharge process to patients, and open‐ended questions. Responses to questions used a Likert scale. Responses to open‐ended questions were handwritten on the paper survey.
Statistical Analysis
The quantitative data were classified categorically and analyzed using Fisher's exact test. Three investigators (M.S., S.E.M., M.B.J.) individually reviewed and coded all written patient or proxy comments using grounded theory methodology.5 Discrepant coding was identified and reconciled. The reconciled coded comments were aggregated into themes.
RESULTS
Demographics
We screened 240 patients or proxies and 200 completed the survey; 10.4% were ineligible due to language barrier, and 6.3% refused. Ninety‐two percent of patients completed the surveys. A majority were male (62.5%), 1859 years old (80%); spoke English as their first language (66%); were community‐dwelling prior to hospitalization (59%); were followed by a primary care provider (PCP) (53%), and many had at least a 4‐year‐college education (45%). One hundred eighty‐five surveys (92.5%) were completed by patients, and 15 (7.5%) were completed by proxies. Ninety surveys were completed at the county teaching hospital, and 110 surveys were completed at the tertiary teaching hospital. See Table 1 for detailed demographic information.
| Patient age, n (%) | |
| 1859 yr | 160 (80) |
| 6069 yr | 30 (15) |
| 7079 yr | 5 (2.5) |
| 80 and older | 5 (2.5) |
| Patient gender, n (%) | |
| Male | 125 (62.5) |
| Female | 75 (37.5) |
| Patient schooling, n (%) | |
| Less than high school | 20 (10) |
| High school | 50 (25) |
| Two‐year college | 40 (20) |
| Four‐year college | 70 (35) |
| Graduate education | 20 (10) |
| English is patient's first language, n (%) | |
| Yes | 132 (66) |
| No | 68 (34) |
| Patient has a primary care doctor, n (%) | |
| Yes | 106 (53) |
| No | 94 (47) |
| Patient's residence before hospitalization, n (%) | |
| Home without home health | 64 (32) |
| Home with home health | 54 (27) |
| Skilled nursing facility | 52 (26) |
| Shelter | 30 (15) |
Survey Results
One hundred percent of patients rated the following items as essential (highest category on Likert Scale): when you need to follow‐up with primary care doctor, warning signs to call primary care doctor, and medicines to continue post‐hospitalization (Figure 1). Patients rated the following items as less important (these items were not unanimously rated as extremely important or essential): treatment you received, medicines you took pre‐hospitalization, importance of bringing all your medicines to follow‐up appointments, and given the side effect of each medication. One hundred percent of patients wanted a lot of explanation (highest category on Likert Scale) about my condition and my test results. Only 39% of patients wanted a lot of explanation about discharge medications. Sixty‐one percent wanted somewhat of an explanation about discharge medications. When asked to choose the most important piece of information, 67.5% of patients chose lifestyle changes. See Figure 1 for the relative importance of the items.
The majority of patients surveyed, 173 (86.5%), wanted verbal discharge instructions with or without written discharge instructions, with only 10.5% requesting only written discharge instructions (P < 0.0001). The majority of patients, 168 (84%), wanted resources to read about their medical condition, with 97 (57%) requesting brochures and 62 (36.9%) requesting Web sites. One hundred percent of patients thought that personal communication between the inpatient provider and the primary care doctor was extremely important or essential.
We identified 4 major themes in our qualitative review of the patients' and proxies' comments: verbal communication, frustration, opacity of system, and too many physicians. Participant quotes related to the 4 major themes are presented in Table 2. Many participants expressed a desire for verbal, rather than written, communication at the time of discharge with their healthcare team; patients particularly requested time for verbal communication with their physician. In the frustration theme, many patients and caregivers expressed frustration that the healthcare team was not carefully listening to them. In the theme of too many physicians, many patients expressed feeling overwhelmed by the number of different doctors involved in their care; particularly at discharge, patients did not know to whom to direct questions. Finally, as part of the opacity of system theme, patient comments included concerns regarding how information will be passed to outside doctors, and that the system of communication is not clear.
| Verbal communication |
| Can we just stop and talk? Everybody is rushing in and out. |
| I just want my doctor to stop by before I go home and tell me what the plan is. |
| Sometimes I feel like no one is talking to me. All they do is give me paperwork. |
| I want my doctors to sit down with me before I leave the hospital and tell me exactly what I need to do so that I don't come back. |
| I don't want papers, I want people. I want to talk to someone and not read my problems from a sheet of paper. |
| Frustration |
| I wonder sometimes if anyone is listening to me I seem to be part of a very elaborate organization that has its own rules and regulations and will not alter its ways. |
| Why do I have to keep retelling my story? It gets tiring. I wish my story could just be told once. |
| Too many physicians |
| I saw lots of doctors during my time here, but I didn't see them again when I was leaving. |
| I see so many doctors I have no idea who is in charge and who I should direct my questions to. |
| I feel overwhelmed by the number of doctors I see every time I come into the hospital. |
| I want my main doctor to talk to me. I get so confused when I hear from more than one doctor. |
| I miss the days when my primary doctor came in to check on me. He knew exactly what I needed. Now, I meet new people every time I go into the hospital. |
| Opacity of system |
| I wonder if all my doctors talk to each other. Sometimes, it seems like they don't. |
| Who keeps track of all this information? Is there someone who will pass on what happened to me here to the outside world? |
DISCUSSION
Discharge is a period of transition from hospital to home that involves a transfer in responsibility from the inpatient care team to the patient and/or caregivers and primary care physician. Ineffective communication, planning, and coordination of care can undermine patient satisfaction, increase adverse events, and contribute to more frequent hospital readmissions.
The patients we surveyed uniformly placed high value on verbal (more than written) communication about discharge care plans. Protected time during the discharge process for hospital staff to provide verbal recommendations to patients, especially about when they should return for follow‐up, warning signs to contact PCP sooner, and medications to continue after discharge, may improve patient satisfaction.
In open‐ended comments, several subjects suggested that physicians should sit down in the patient's room and provide verbal discharge instructions. Although it is well recognized that verbal communication alone has limitations and that providing patients with written instructions remains crucial, verbal reinforcement may highlight the most important instructions.
Interestingly, subjects valued information about lifestyle changes over detailed information about their medications. This may suggest that hospitalized patients are particularly receptive to information about lifestyle changes such as smoking cessation or importance of compliance with medical appointments.
Lastly, patients we surveyed value personal communication between inpatient and outpatient providers. It is plausible that this would improve transitions of care, and previous studies have suggested that direct communication between inpatient and outpatient providers occurs infrequently, with only 20% of primary care providers in 1 study reporting that they are always notified when their patient is being discharged from a hospitalist service.6
The themes that emerged from our open‐ended questions also highlight the importance of direct verbal communication with patients and careful coordination of care with outside physicians. Because patients may be unlikely to fully remember verbal instructions at discharge, providers may consider providing patients and family members with patient‐centered written materials to take home in order to reinforce important self‐care instructions. The patient comments further suggest that patients may be more satisfied, and that discharges may be smoother, if 1 or 2 physicians were always identified to the patients and their caregivers as the leaders of the care team throughout the hospital course and discharge process.
Our study had several limitations. We only surveyed patients on general medicine services, so our findings might not apply to other populations. We did not enroll participants on weekends and holidays; it is possible that this led to some bias in the enrollment of subjects. We also only surveyed patients and/or proxies who could speak and read English, and this was a fairly highly educated population, with almost half having completed 4 years of college. Finally, we relied on participant self‐report for demographic information because we did not have access to the electronic medical record. This study was conducted at 2 large academic medical centers that include resident physicians in the daily care of patients; thus, these results may not be generalizable to other settings.
Effective verbal communication between physicians, outpatient providers, patients, and their caregivers about discharge care plans might improve patients' understanding of their hospitalizations, increase their satisfaction with care, and reduce readmissions. In addition, physicians should recognize that patients value advice about lifestyle interventions that might improve their health, as part of the discharge care plan. Intervention studies are necessary to test these hypotheses in large, diverse populations.
Acknowledgements
Disclosure: Nothing to report.
- ,,,.Medical errors related to discontinuity of care from an inpatient to an outpatient setting.J Gen Intern Med.2003;18(8):646–651.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297(8):831–841.
- ,,.Expanding patient involvement in care. Effects on patient outcomes.Ann Intern Med.1985;102(4):520–528.
- Society of Hospital Medicine. Project BOOST, Better Outcomes for Older adults through Safe Transitions. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Home1998.
- ,,,.Primary care physician attitudes regarding communication with hospitalists.Am J Med.2001;111(9B):15S–20S.
- ,,,.Medical errors related to discontinuity of care from an inpatient to an outpatient setting.J Gen Intern Med.2003;18(8):646–651.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297(8):831–841.
- ,,.Expanding patient involvement in care. Effects on patient outcomes.Ann Intern Med.1985;102(4):520–528.
- Society of Hospital Medicine. Project BOOST, Better Outcomes for Older adults through Safe Transitions. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Home1998.
- ,,,.Primary care physician attitudes regarding communication with hospitalists.Am J Med.2001;111(9B):15S–20S.
Continuing Medical Education Program in
If you wish to receive credit for this activity, please refer to the website: www.wileyblackwellcme.com.
Accreditation and Designation Statement
Blackwell Futura Media Services designates this journal‐based CME activity for a maximum of 1 AMA PRA Category 1 Credit.. Physicians should only claim credit commensurate with the extent of their participation in the activity.
Blackwell Futura Media Services is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
Educational Objectives
The objectives need to be changed. Please remove the existing ones, and include these two:
-
Identify complications elderly patients are at risk for during hospitalization.
-
Suggest evidence‐based strategies to prevent and treat common causes of hospitalization‐related complications in geriatric patients.
This manuscript underwent peer review in line with the standards of editorial integrity and publication ethics maintained by Journal of Hospital Medicine. The peer reviewers have no relevant financial relationships. The peer review process for Journal of Hospital Medicine is single‐blinded. As such, the identities of the reviewers are not disclosed in line with the standard accepted practices of medical journal peer review.
Conflicts of interest have been identified and resolved in accordance with Blackwell Futura Media Services's Policy on Activity Disclosure and Conflict of Interest. The primary resolution method used was peer review and review by a non‐conflicted expert.
Instructions on Receiving Credit
For information on applicability and acceptance of CME credit for this activity, please consult your professional licensing board.
This activity is designed to be completed within an hour; physicians should claim only those credits that reflect the time actually spent in the activity. To successfully earn credit, participants must complete the activity during the valid credit period, which is up to two years from initial publication.
Follow these steps to earn credit:
-
Log on to www.wileyblackwellcme.com
-
Read the target audience, learning objectives, and author disclosures.
-
Read the article in print or online format.
-
Reflect on the article.
-
Access the CME Exam, and choose the best answer to each question.
-
Complete the required evaluation component of the activity.
This activity will be available for CME credit for twelve months following its publication date. At that time, it will be reviewed and potentially updated and extended for an additional twelve months.
If you wish to receive credit for this activity, please refer to the website: www.wileyblackwellcme.com.
Accreditation and Designation Statement
Blackwell Futura Media Services designates this journal‐based CME activity for a maximum of 1 AMA PRA Category 1 Credit.. Physicians should only claim credit commensurate with the extent of their participation in the activity.
Blackwell Futura Media Services is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
Educational Objectives
The objectives need to be changed. Please remove the existing ones, and include these two:
-
Identify complications elderly patients are at risk for during hospitalization.
-
Suggest evidence‐based strategies to prevent and treat common causes of hospitalization‐related complications in geriatric patients.
This manuscript underwent peer review in line with the standards of editorial integrity and publication ethics maintained by Journal of Hospital Medicine. The peer reviewers have no relevant financial relationships. The peer review process for Journal of Hospital Medicine is single‐blinded. As such, the identities of the reviewers are not disclosed in line with the standard accepted practices of medical journal peer review.
Conflicts of interest have been identified and resolved in accordance with Blackwell Futura Media Services's Policy on Activity Disclosure and Conflict of Interest. The primary resolution method used was peer review and review by a non‐conflicted expert.
Instructions on Receiving Credit
For information on applicability and acceptance of CME credit for this activity, please consult your professional licensing board.
This activity is designed to be completed within an hour; physicians should claim only those credits that reflect the time actually spent in the activity. To successfully earn credit, participants must complete the activity during the valid credit period, which is up to two years from initial publication.
Follow these steps to earn credit:
-
Log on to www.wileyblackwellcme.com
-
Read the target audience, learning objectives, and author disclosures.
-
Read the article in print or online format.
-
Reflect on the article.
-
Access the CME Exam, and choose the best answer to each question.
-
Complete the required evaluation component of the activity.
This activity will be available for CME credit for twelve months following its publication date. At that time, it will be reviewed and potentially updated and extended for an additional twelve months.
If you wish to receive credit for this activity, please refer to the website: www.wileyblackwellcme.com.
Accreditation and Designation Statement
Blackwell Futura Media Services designates this journal‐based CME activity for a maximum of 1 AMA PRA Category 1 Credit.. Physicians should only claim credit commensurate with the extent of their participation in the activity.
Blackwell Futura Media Services is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
Educational Objectives
The objectives need to be changed. Please remove the existing ones, and include these two:
-
Identify complications elderly patients are at risk for during hospitalization.
-
Suggest evidence‐based strategies to prevent and treat common causes of hospitalization‐related complications in geriatric patients.
This manuscript underwent peer review in line with the standards of editorial integrity and publication ethics maintained by Journal of Hospital Medicine. The peer reviewers have no relevant financial relationships. The peer review process for Journal of Hospital Medicine is single‐blinded. As such, the identities of the reviewers are not disclosed in line with the standard accepted practices of medical journal peer review.
Conflicts of interest have been identified and resolved in accordance with Blackwell Futura Media Services's Policy on Activity Disclosure and Conflict of Interest. The primary resolution method used was peer review and review by a non‐conflicted expert.
Instructions on Receiving Credit
For information on applicability and acceptance of CME credit for this activity, please consult your professional licensing board.
This activity is designed to be completed within an hour; physicians should claim only those credits that reflect the time actually spent in the activity. To successfully earn credit, participants must complete the activity during the valid credit period, which is up to two years from initial publication.
Follow these steps to earn credit:
-
Log on to www.wileyblackwellcme.com
-
Read the target audience, learning objectives, and author disclosures.
-
Read the article in print or online format.
-
Reflect on the article.
-
Access the CME Exam, and choose the best answer to each question.
-
Complete the required evaluation component of the activity.
This activity will be available for CME credit for twelve months following its publication date. At that time, it will be reviewed and potentially updated and extended for an additional twelve months.
Ten Things About Elderly Patients
Recent studies of the growth of the hospitalist movement have confirmed that hospitalists are taking care of an increasing percentage of hospitalized older adults.1, 2 Unfortunately, few hospitalist groups have specific programs or protocols to address the special needs of older patients.3, 4 We were inspired by a top 10 article written by nephrologists for primary care physicians to compile 10 evidence‐based pearls that may be helpful to hospitalists caring for older persons.5
1. Many Health Conditions in Older Patients are Multifactorial and Require a Multifactorial Approach to Care
A geriatric syndrome is a multifactorial condition occurring primarily in frail elderly which is usually due to multiple contributing factors and results from an interaction between patient‐specific impairments and situation‐specific stressors.68 Geriatric syndromes cannot be treated easily with a single intervention; the approach must target each modifiable risk factor. Table 1 illustrates for an example of how this approach differs from the traditional medical approach in the case of falls, a common geriatric syndrome. Hospitalists commonly encounter the geriatric syndromes that either lead to hospitalization, such as falls or dementia, or that can complicate a hospitalization for another condition, such as delirium, falls, or urinary incontinence. Two geriatric syndromes in particular, delirium and falls, are associated with increased length of stay, increased healthcare costs, and substantial morbidity.9, 10 Multifactorial interventions such as the Hospital Elder Life Project (HELP) have been shown to prevent delirium and falls.1114 Studies of the HELP intervention demonstrated benefits on outcomes that are important to hospitalists, including shortened length of stay.10, 15 While implementing these interventions is not possible at every institution, it may be possible to implement some aspects in a targeted fashion (for example, early physical therapy and mobilization to decrease risk of delirium and falls) or to work with hospital administration to implement the larger interventions.
| Traditional Medical Approach (Diagnosis and Treatment) | Geriatric Approach (Risk Factor Assessment and Reduction) | |
|---|---|---|
| ||
| Search for cause of falls | Search for cause of falls | |
| (eg, syncope workup including echocardiogram, neurologic workup including imaging) | Assess for risk factors and target interventions reduce or eliminate risk factors identified, eg: | |
| Risk factor | Intervention | |
| Leg weakness | Strength training | |
| Falls when transferring | Training in use of assistive device for transfers | |
| Inadequate lighting at home | Home safety evaluation by physical therapist and installation of lights at home | |
2. Screening Elderly Patients for the Presence of Common Geriatric Syndromes can Improve Care
Comprehensive geriatric assessment, a process of multifactorial health evaluation of the older patient, is an important part of geriatric medicine and has been shown to reduce functional decline.16 While comprehensive geriatric assessment may not be practical in the acute care setting, some basic principles and tools of geriatric assessment, namely screening for geriatric syndromes, can be helpful. Here is one efficient, evidence‐based approach to screening hospitalized elderly patients for cognitive impairment and falls, and then using the results of screening to improve care:
Brief cognitive assessment using the Mini‐Cog screening tool
Even with cognitive screening, it can sometimes be difficult to distinguish between dementia and delirium in an acutely ill person. However, knowing who is cognitively impaired on admission tells us who is likely to develop delirium and may need to be discharged to a supervised location, such as a nursing facility.17, 18 The Mini‐Cog (shown in Table 2) is our preferred tool for cognitive screening, because it takes only 24 minutes to administer, has a sensitivity of 76% and specificity of 89% [similar to the Mini‐Mental State Examination (MMSE)], and has been validated in a multiethnic, multilingual sample with low literacy.19, 20 The Mini‐Cog has not been studied extensively in the inpatient setting, but one study did find that abnormal Mini‐Cog scores correlated with the development of delirium among hospitalized elderly patients.21 Other tools appropriate for brief cognitive screening of hospitalized patients include the MMSE, which is widely known but limited by copyright for clinical use and longer time needed for administration, and the Short Portable Mental Status Questionnaire (SPMSQ), which is entirely verbal and does not require that the patient write or draw.22, 23 A new tool, the Sweet 16, which is also entirely verbal and takes about 2 minutes to administer, shows promise but has not been validated in the inpatient setting.24
|
| The Mini‐Cog combines an uncued three‐item recall test with a clock‐drawing test (CDT) that serves as the recall distractor. The Mini‐Cog can be administered in about three minutes, requires no special equipment, and is less influenced by level of education or language differences. |
| Administration |
| 1. Make sure you have the patient's attention. Then instruct the patient to listen carefully to, repeat back to you, and remember (now and later) three unrelated words. You may present the same words up to 3 times if necessary. |
| 2. Instruct the patient to draw the face of a clock, either on a blank sheet of paper, or on a sheet with the clock circle already drawn on the page. After the patient puts the numbers on the clock face, ask him or her to draw the hands to read a specific time (11:10 or 8:20 are most commonly used; however, other times that require use of both halves of the clock face may be effective). These instructions can be repeated, but no additional instructions should be given. If the patient cannot complete the CDT in three minutes or less, move on to the next step. |
| 3. Ask the patient to repeat the three previously presented words. |
| Scoring |
| Give 1 point for each recalled word after the CDT distractor. Score 03 for recall. |
| Give 2 points for a normal CDT, and 0 points for an abnormal CDT. The CDT is considered normal if all numbers are depicted, once each, in the correct sequence and position around the circle, and the hands readably display the requested time. Do not count equal hand length as an error. Add the recall and CDT scores together to get the Mini‐Cog score: |
| 02 positive screen for dementia. |
| 35 negative screen for dementia. |
Fall screen: Have you fallen in the past year? with more detailed inquiry for frequent fallers
An elderly patient with a history of falls is at high risk for falling while in the hospital. Interventions that target multiple risk factors appear to be effective in reducing risk and rate of falling.25 Some aspects of these multifactorial interventions include environmental modifications such as low beds, high‐impact floor mats, restraint removal, bedside posters and patient education materials, and exercise.13, 26 Medication review and reductions in medications that contribute to falls (psychoactive medications, diuretics, blood pressure agents) can also reduce fall risk.13, 14 Many experts recommend checking a 25‐hydroxy vitamin D level for patients who come into the hospital for treatment of a fall‐related injury, starting or continuing vitamin D and calcium supplementation for those with normal vitamin D levels, and starting aggressive vitamin D replacement with 50,000 units of oral ergocalciferol weekly for those with a level below 20 ng/mL. Vitamin D appears to play an important role in neuromuscular function as well as bone density.27 Meta‐analyses have demonstrated that vitamin D supplementation of 7001,000 IU daily may reduce the risk of falls in the elderly by about 20%, that the effect is achieved in the short term (on the order of 25 months), and that the benefit persists for up to 36 months.28, 29
3. Elderly Patients are at Risk for Functional Decline During Hospitalization and Measures Can Be Taken to Prevent This
A cascade to dependency has been described in which the effects of usual aging (eg, fragile skin) and hospitalization (eg, immobilization) interact with each other, often producing complications (eg, pressure ulcers) that can lead to the loss of the ability to live independently.30 Functional decline during hospitalization is common and is associated with poor prognosis. In one study of elderly patients with new Activities of Daily Living (ADL) disability at discharge, over 40% were dead by 12 months after discharge, and only 30% had returned to baseline function.31, 32 Functional status may affect discharge planning, especially if the patient is not able to return safely to his or her previous living environment. Elderly patients are very vulnerable to new ADL dependency and loss of ambulatory ability as a result of a hospitalization.33, 34 The initial evaluation of an elderly patient should always include an inquiry into the patient's functional abilities, including whether the patient requires assistance to perform self‐care (ADL) activities or instrumental activities of daily living (IADLs), and who is available to help at home. We remember ADLs as those activities we learn as a young child (bathing, dressing, feeding, toileting, transfers) and IADLs as activities we learn when we leave our parents' home to live independently (shopping, cooking, laundry, housekeeping, managing money, using public transportation). Patients in assisted living facilities and adult family homes receive varying degrees of help with ADLs and IADLs, and no particular level of assistance can be assumed; assisted living residents may be at higher risk of functional decline during hospitalization than community‐dwelling persons.35
Acute Care of Elderly (ACE) units have been shown to reduce functional disability and discharge to long‐term care settings, with length of stay and hospital charges similar to that of usual care.36 Most hospitals do not have ACE units, but implementing some components of the intervention, such as early physical and occupational therapy, early discharge planning, early mobility, and adequate nutrition may reduce functional disability. A Cochrane review found a small decrease in length of stay of about a day among elderly patients who participated in a structured exercise program, which could be extrapolated to support the usefulness of increased mobility and early physical therapy.37
4. Delirium is a Common but Serious Condition Among Hospitalized Elderly Patients and in Some Cases Can Be Prevented
The incidence of delirium appears to be as high as 60% in hospitalized elderly patients with multiple risk factors for this condition.38, 39 Delirium predicts longer hospital stay, increases likelihood of discharge to a skilled nursing facility, and is a marker for significant morbidity and mortality.4042 Cognitive screening, as discussed above, can help determine who is at risk for delirium, and the Confusion Assessment Method (CAM) is becoming more widely used as a bedside screening tool for detecting delirium.43 Other important risk factors for delirium in addition to preexisting cognitive impairment include age over 65, prior delirium, polypharmacy, functional dependence, and sensory impairment.44 A landmark randomized controlled trial by Sharon Inouye et al. showed that delirium can often be prevented in high‐risk patients by ensuring frequent reorientation, maintenance of the patient's usual sleep‐wake cycle, early mobilization, adequate nutrition and hydration, and regular use of sensory aids such as glasses and hearing aids.11
When delirium does occur despite preventive efforts, it should trigger a thorough investigation for an underlying cause. Common contributing factors to delirium in hospitalized patients include infections such as urinary tract infections or hospital‐acquired pneumonia, pain, electrolyte abnormalities, cardiac ischemia, medication side effects, and urinary retention or constipation. Any psychoactive or anticholinergic medication can contribute to, or exacerbate, delirium; common culprits include diphenhydramine, benzodiazepines, and muscle relaxants.44 Although one or more treatable underlying causes should always be sought, many cases of delirium in the hospital are multifactorial.
If pharmacologic treatment for delirium is necessary, low‐dose haloperidol is the first‐line agent, starting with 0.25 mg intravenously or 0.5 mg by mouth, nightly to twice a day. A recent systematic review supported the use of haloperidol as a first‐line agent in the acute setting; second‐generation antipsychotics are an alternative, but studies have shown no benefits of these agents over haloperidol in terms of safety or efficacy.45 Physical restraints should be avoided in delirious patients, as they may actually worsen delirium and have not been proven to reduce falls or secondary injury.46
5. Treating Nondementia Illnesses in Hospitalized Elders With Dementia Requires Consideration of the Patient's Limited Life Expectancy and Cognitive Deficits
Elderly patients with dementia are frequently hospitalized for medical illness and pose special challenges to the hospitalist. Patients with dementia may not be able to accurately report symptoms and side effects of therapy, and may lack decisional capacity. The clinician should also carefully consider the benefits and burdens of a proposed therapy or diagnostic test, taking into account the patient's cognitive deficits and limited life expectancy.47 The median postdiagnosis life expectancy of a patient with Alzheimer disease is about 4 years for men and about 6 years for women, with a range from about 2 to 9 years, according to population‐based studies of incident Alzheimer dementia.48, 49 In a patient with early or mild dementia, the hospitalist may first need to establish whether the patient does indeed have dementia. It is also important to question family about how the patient is managing at home so that appropriate discharge plans can be made.
Any intervention such as surgery or intubation in a patient with dementia should be considered carefully in the context of the patient's dementia, keeping in mind the remaining life expectancy, increased risk for delirium after surgery, and potential difficulty with adherence to postoperative precautions or participation in rehabilitation. Invasive procedures such as mechanical ventilation or central line placement may not be indicated in patients with advanced dementia. In one prospective cohort study, patients with advanced dementia admitted to the hospital for hip fractures or pneumonia had much higher mortality than those without dementia, despite having equal rates of procedures such as mechanical ventilation and central line placement.50
A common scenario in a patient with advanced dementia is the patient presenting with decreased intake and dysphagia; family and/or caregivers inquire about enteral tube feeding and/or long‐term intravenous hydration. This situation requires a thoughtfully presented, informative discussion with the family about artificial feeding in advanced dementia. There is no evidence that artificial feeding improves outcomes, and a recent Cochrane systematic review found insufficient evidence to suggest that enteral tube feeding is beneficial in patients with dementia.5153 Instead, dementia patients at the end of their lives benefit from a palliative approach, which would include hand‐feeding for comfort if the patient indicates hunger.54
6. Frail Elderly Patients are at High Risk for Iatrogenic Complications During Hospitalization
Frail elders are at increased risk for iatrogenic complications, including surgical‐ and procedure‐related events, adverse drug events, nosocomial infections, pressure ulcers, and falls.5557 In the Harvard Medical Practice Study, a retrospective study of adverse events in 30,000 patients, those age 65 and over accounted for 27% of the hospitalized population but 43% of the adverse events. In this study, four types of adverse events occurred at least twice as often in older patients: fractures, falls, nontechnical postoperative complications, and adverse events related to noninvasive treatments.58 The risk of hospital‐acquired infection also rises dramatically with age; risk is ten times higher in patients over 70 than those aged 49 and under, with urinary tract infections and surgical site infections the most common.59 The oldest, most seriously ill and most functionally impaired elderly patients are at particularly high risk of cascade iatrogenesis, where one medical intervention triggers a series of adverse events.60 Frail elderly patients are at greater risk for adverse events during hospitalization, and careful consideration of the need for all diagnostic tests and procedures may reduce risks. Table 3 lists the iatrogenic complications that disproportionately affect the elderly.
7. Pain Should Be Aggressively Identified and Appropriately Treated
Adequate treatment of pain in the elderly can improve functional status, mobility, and mood. Clinicians are understandably wary of prescribing opioids in the elderly, but undertreatment of pain is also common and in hospitalized patients can lead to delirium, delays in rehabilitation, and higher healthcare costs.44, 61 Acetaminophen is generally safe and is recommended as first‐line therapy in most cases of pain. Nonsteroidal antiinflammatory drugs (NSAIDS) should be used with caution, as the risk of gastrointestinal toxicity increases with age; long‐acting agents such as toradol should be avoided.62 A study of adverse drug reactions causing hospitalization in elderly individuals implicated NSAIDs in 23.5% of cases.63 If a patient has severe pain that limits functional capacity but does not respond to acetaminophen, it is reasonable to consider low‐dose opioids. The 2009 American Geriatrics Society guidelines recommend that opioids be used for severe pain, especially when it limits functional capacity. Opioids should be given orally when possible and started at low doses (for example, 2.5 to 5 milligrams of oxycodone offered every 4 hours as needed). Either oxycodone or morphine can be used as a first‐line, short‐acting opioid, but morphine should be used cautiously in patients with renal insufficiency, as toxic metabolites are renally cleared. Methadone should be used very cautiously and ideally by clinicians experienced in its use because of its long and variable half‐life. Serotonin‐norepinephrine reuptake inhibitors such as duloxetine, and anticonvulsants such as gabapentin, can be helpful adjuncts for neuropathic pain; tricyclics should generally be avoided, because the elderly are particularly sensitive to the anticholinergic side effects (ie, sedation, orthostatic hypotension, urinary retention, constipation) of these agents.61 Nortriptyline, which has the least anticholinergic properties of this medication class, may be the best option if a tricyclic is desired.
8. Hospitalization Can Be an Opportunity for a Thorough Review and Reduction of Outpatient Medications in Collaboration With the Patient's Primary Care Provider
Adverse drug reactions (ADRs) are potentially life‐threatening for all patients, but elderly individuals are disproportionately affected. It is estimated that 30% of hospital admissions of older patients are due to drug‐related toxicity.64 The Beers criteria provide expert consensus on drugs that should either be avoided or used cautiously in the elderly; we have highlighted some of the drugs on the Beers list that are relevant to the hospitalist in Table 4. Notable inclusions on the most recent Beers list include nitrofurantoin, ferrous sulfate at dosages greater than 325 mg per day, doxazosin, and fluoxetine.65 Anticholinergics (such as oxybutynin) and cholinesterase inhibitors (such as donepezil) should not be used together, because the interaction makes them ineffective.
| Falls and fractures58 |
| Nosocomial infections59 |
| Delirium44 |
| Surgical and postoperative complications58 |
| Adverse drug events56 |
| Pressure sores56 |
| Medication | Rationale |
|---|---|
| |
| Benzodiazepines | Can contribute to delirium and falls. |
| Muscle relaxants | Anticholinergic side effects; sedating; can contribute to delirium. |
| Diphenhydramine | Very sedating; can contribute to delirium; do not use as a sleep aid, and use lowest possible dose when treating allergic reactions. |
| Nitrofurantoin | Can cause renal impairment. |
| Ketorolac | Can lead to gastrointestinal bleeds and renal impairment. |
| Ferrous sulfate in doses >325 mg/day | Can cause severe constipation; higher doses not well absorbed. |
| Digoxin in doses of >0.125 mg/day | Decreased renal clearance can increase risk of toxicity (higher doses acceptable for atrial arrythmias). |
| Amiodarone | Multiple toxicities; lack of proven efficacy in older adults. |
| Fluoxetine | Long half‐life; can cause agitation and sleep disturbance. |
| Meperidine | Can cause seizures and contribute to delirium. |
| Doxazosin | Can cause hypotension and contribute to falls. |
Many ADRs are caused by medications that are not on the Beers list but have narrow therapeutic windows, especially warfarin and insulin; digoxin, which is on the Beers list, is another common culprit in ADRs leading to emergency room visits.66 Medications that are clearly causing ADRs should be discontinued, with the knowledge and input of the primary care provider, and with written documentation on the discharge summary and clear instructions to the patient. Even when a hospital admission is not a result of an ADR, it may provide an opportunity to review the patient's medication list, clarify that the patient is taking medications as directed by their primary care provider, and determine if the list contains medications where risks now outweigh benefits, in which case those medications should be discontinued. Studies have shown that elimination of medications that are associated with falls reduces the risk of future falls.67 Adjustments to patient's medications should be made in close collaboration with the primary care provider and with a clinical pharmacist, if available.
9. Discharge Planning for an Elderly Patient Should Start Early, Be Comprehensive, and Involve the Patient and Caregivers
A successful discharge plan for an elderly patient must start early, take functional status into account, and perhaps most importantly, the planning process should involve the patient and family, if appropriate. One study of patients over 70 discharged from an urban, academic public hospital found that only 10% recalled receiving written discharge instructions, and only 53% who were prescribed a new medication actually had that medication at home.68 Growing evidence suggests that older patients have poorer functional health literacy regarding medications.69 Care transitions are an active area of research, and multiple studies have shown lower rates of rehospitalization with comprehensive transitional care programs involving transition coaches or advance practice nurses providing home visits and follow‐up telephone calls.70, 71 More research is needed in this area to develop simple, cost‐effective care transitions programs. In the meantime, hospitalists can actively involve a multidisciplinary team (pharmacists and social workers, for example) early in the hospitalization, provide more patient‐friendly discharge materials such as those available as part of the Society of Hospital Medicine's BOOST, and place targeted follow‐up phone calls after discharge.52, 7274 Ensuring that a frail elderly patient's primary care provider is aware of the hospitalization may be particularly important in avoiding postdischarge problems.75
10. Elderly Patients are Often Very Clear About Their Preferences for Treatment. Discussing This on Admission Can Help Clarify the Goals of the Hospitalization
The risks and benefits of any intervention being considered should be presented and discussed with the patient in the context of the likelihood of the intervention restoring an acceptable quality of life to the patient. Many common chronic conditions in the elderly such as Parkinson disease, congestive heart failure, and dementia are progressive and life‐limiting. Qualitative studies confirm that elderly patients want to know the likelihood that a proposed intervention will help them return to their previous level of functioning or a level that is acceptable to them.76, 77 In one prospective cohort study, older age was found to correlate with a higher rate of withholding ventilatory support, dialysis, and surgery.78 However, a more recent study has suggested that patient preferences are more dynamic, and that older patients will make decisions based on current health status rather than core values.76 While families should be involved in the process of clarification of goals of care, the patients' own values should be elicited whenever possible, with bedside assessment of decision‐making capacity to ensure that patients are allowed to speak for themselves if they possess decisional capacity for the decision at hand.79
Hospitalists should have a special approach to the elderly patient which takes into account the elder's increased vulnerability to iatrogenic complications and acute functional decline, the presence of geriatric syndromes, and individual preferences. Early assessment of an elderly patient's cognitive and physical functioning, level of pain, fall risk, and preferences for care are necessary for optimal inpatient care and may result in preserved function and a decrease in adverse events.
- , , , .Growth in the care of older patients by hospitalists in the United States.N Engl J Med.2009;360(11):1102–1112.
- , , , , , .Continuity of outpatient and inpatient care by primary care physicians for hospitalized older adults.JAMA.2009;301(16):1671–1680.
- , , .Is there a geriatrician in the house? Geriatric care approaches in hospitalist programs.J Hosp Med.2006;1(1):29–35.
- .Care of hospitalized older patients: opportunities for hospital‐based physicians.J Hosp Med.2006;1(1):42–47.
- , .The top 10 things nephrologists wish every primary care physician knew.Mayo Clin Proc.2009;84(2):180–186.
- .What is a geriatric syndrome anyway?J Am Geriatr Soc.2003;51(4):574–576.
- , , , .Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept.J Am Geriatr Soc.2007;55(5):780–791.
- , , .Some considerations regarding geriatric syndromes.Ann Intern Med.2001;135(12):1095.
- , , , et al.Impact and recognition of cognitive impairment among hospitalized elders.J Hosp Med.2010;5(2):69–75.
- , , , , , .A longitudinal analysis of total 3‐year healthcare costs for older adults who experience a fall requiring medical care.J Am Geriatr Soc.2010;58(5):853–860.
- , , , et al.A multicomponent intervention to prevent delirium in hospitalized older patients.N Engl J Med.1999;340(9):669–676.
- , , , .Shared risk factors for falls, incontinence, and functional dependence. Unifying the approach to geriatric syndromes.JAMA.1995;273(17):1348–1353.
- , , , et al.Strategies to prevent falls and fractures in hospitals and care homes and effect of cognitive impairment: systematic review and meta‐analyses.BMJ.2007;334(7584):82.
- , , , et al.Interventions for preventing falls in acute‐ and chronic‐care hospitals: a systematic review and meta‐analysis.J Am Geriatr Soc.2008;56(1):29–36.
- , , , et al.Postoperative delirium in the elderly: risk factors and outcomes.Ann Surg.2009;249(1):173–178.
- , , , et al.A controlled trial of inpatient and outpatient geriatric evaluation and management.N Engl J Med.2002;346(12):905–912.
- , , , et al.Risk factors for preoperative and postoperative delirium in elderly patients with hip fracture.J Am Geriatr Soc.2009;57(8):1354‐1361.
- , , , , , .Risk factors for delirium in intensive care patients: a prospective cohort study.Crit Care.2009;13(3):R77.
- , , , .The Mini‐Cog as a screen for dementia: validation in a population‐based sample.J Am Geriatr Soc.2003;51(10):1451–1454.
- , , , , .Improving identification of cognitive impairment in primary care.Int J Geriatr Psychiatry.2006;21(4):349–355.
- , , , et al.Simple cognitive testing (Mini‐Cog) predicts inhospital delirium in the elderly.J Am Geriatr Soc.2007;55(2):314–316.
- , , , .Short Portable Mental Status Questionnaire as a screening test for dementia and delirium among the elderly.J Am Geriatr Soc.1987;35(5):412–416.
- , , .“Mini‐mental state.” A practical method for grading the cognitive state of patients for the clinician.J Psychiatr Res.1975;12(3):189–198.
- , , , et al.Development and validation of a brief cognitive assessment tool: the Sweet 16.Arch Intern Med.2010. [Epub ahead of Print].
- , , , et al.Interventions for preventing falls in older people in nursing care facilities and hospitals.Cochrane Database Syst Rev.2010;(1):CD005465.
- , , , et al.Fall prevention in acute care hospitals: a randomized trial.JAMA.2010;304(17):1912–1918.
- , , , et al.Vitamin D supplementation improves neuromuscular function in older people who fall.Age Ageing.2004;33(6):589–595.
- , , , et al.Effect of vitamin D on falls: a meta‐analysis.JAMA.2004;291(16):1999–2006.
- , et al.Fall prevention with supplemental and active forms of vitamin D: a meta‐analysis of randomised controlled trials.BMJ.2009;339:b3692.
- .Hazards of hospitalization of the elderly.Ann Intern Med.1993;118(3):219–223.
- , , , .Hospitalization, restricted activity, and the development of disability among older persons.JAMA.2004;292(17):2115–2124.
- , , , et al.Recovery of activities of daily living in older adults after hospitalization for acute medical illness.J Am Geriatr Soc.2008;56(12):2171–2179.
- , , , et al.Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age.J Am Geriatr Soc.2003;51(4):451–458.
- , , .New walking dependence associated with hospitalization for acute medical illness: incidence and significance.J Gerontol A Biol Sci Med Sci.1998;53(4):M307–M312.
- , , , .Hazards of hospitalization: residence prior to admission predicts outcomes.Gerontologist.2008;48(4):537–541.
- , , , , , et al.A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients.N Engl J Med.1995;332(20):1338–1344.
- , .Exercise for acutely hospitalised older medical inpatients.Cochrane Database Syst Rev.2007;(1):CD005955.
- , , .Occurrence and outcome of delirium in medical in‐patients: a systematic literature review.Age Ageing.2006;35(4):350–364.
- , , .A prospective study of delirium in hospitalized elderly.JAMA.1990;263(8):1097–1101.
- , , , , .Delirium predicts 12‐month mortality.Arch Intern Med.2002;162(4):457–463.
- , , , , .The course of delirium in older medical inpatients: a prospective study.J Gen Intern Med.2003;18(9):696–704.
- , , , .Does delirium increase hospital stay?J Am Geriatr Soc.2003;51(11):1539–1546.
- , , , .The Confusion Assessment Method: a systematic review of current usage.J Am Geriatr Soc.2008;56(5):823–830.
- .Delirium in older persons.N Engl J Med.2006;354(11):1157–1165.
- , , , et al.Pharmacological management of delirium in hospitalized adults—a systematic evidence review.J Gen Intern Med.2009;24(7):848‐853.
- , , .Safety and efficacy of physical restraints for the elderly. Review of the evidence.Can Fam Physician.1996;42:2402–2409.
- , , .Treating nondementia illnesses in patients with dementia.JAMA.2000;283(24):3230–3235.
- , , , , , .Survival in Alzheimer disease: a multiethnic, population‐based study of incident cases.Neurology.2008;71(19):1489–1495.
- , , , et al.Survival after initial diagnosis of Alzheimer disease.Ann Intern Med.2004;140(7):501–509.
- , .Mortality from pneumonia and hip fractures in patients with advanced dementia.JAMA.2000;284(19):2447–2448.
- .Rethinking the role of tube feeding in patients with advanced dementia.N Engl J Med.2000;342(3):206–210.
- Society of Hospital Medicine. BOOSTing Care Transitions Resource Room. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_CareTransitions/CT_Home.cfm. Accessed January 25,2011.
- , , .Enteral tube feeding for older people with advanced dementia.Cochrane Database Syst Rev.2009;(2):CD007209.
- .A 93‐year‐old man with advanced dementia and eating problems.JAMA.2007;298(21):2527–2536.
- , , .Patient safety in geriatrics: a call for action.J Gerontol A Biol Sci Med Sci.2003;58(9):M813–M819.
- , , .Preventable medical injuries in older patients.Arch Intern Med.2000;160(18):2717–2728.
- , , , et al.Iatrogenic complications in high‐risk, elderly patients.Arch Intern Med.1992;152(10):2074–2080.
- , , , et al.The nature of adverse events in hospitalized patients. Results of the Harvard Medical Practice Study II.N Engl J Med.1991.
- , , , , et al.Nosocomial infections: decade‐specific risk.Infect Control.1983;4(3):145–147.
- , , , , , .A quality‐of‐care analysis of cascade iatrogenesis in frail elderly hospital patients.QRB Qual Rev Bull.1993;19(6):199‐2.
- American Geriatrics Society Panel on the Pharmacological Management of Persistent Pain in Older Persons.Pharmacological management of persistent pain in older persons.J Am Geriatr Soc.2009;57(8):1331–1346.
- , , , , .The rate of NSAID‐induced endoscopic ulcers increases linearly but not exponentially with age: a pooled analysis of 12 randomised trials.Ann Rheum Dis.2007;66(3):417–418.
- , , , et al.Prevalence, clinical features and avoidability of adverse drug reactions as cause of admission to a geriatric unit: a prospective study of 1756 patients.Drug Saf.2008;31(6):545–556.
- , , , et al.Adverse drug events in high risk older outpatients.J Am Geriatr Soc.1997;45(8):945–948.
- , , , , , .Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts.Arch Intern Med.2003;163(22):2716–2724.
- , , , .Medication use leading to emergency department visits for adverse drug events in older adults.Ann Intern Med.2007;147(11):755–765.
- , .The patient who falls: “It's always a trade‐off.”JAMA.2010;303(3):258–266.
- , , .Hospital discharge information and older patients: do they get what they need?J Hosp Med.2007;2(5):291–296.
- , , .Functional health literacy and understanding of medications at discharge.Mayo Clin Proc.2008;83(5):554–548.
- , , , .The care transitions intervention: results of a randomized controlled trial.Arch Intern Med.2006;166(17):1822–1828.
- , , , , , .Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial.J Am Geriatr Soc.2004;52(5):675–684.
- , , , .The impact of follow‐up telephone calls to patients after hospitalization.Am J Med.2001;111(9B):26S‐30S.
- , , , et al.A quality improvement intervention to facilitate the transition of older adults from three hospitals back to their homes.J Am GeriatrSoc.2009;57(9):1540–1546.
- , , , et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Intern Med.2009;150(3):178–187.
- , , , et al.Problems after discharge and understanding of communication with their primary care physicians among hospitalized seniors: a mixed methods study.J Hosp Med.2010;5(7):385–391.
- , .What matters to seriously ill older persons making end‐of‐life treatment decisions? A qualitative study.J Palliat Med.2003;6(2):237–244.
- , , .End‐of‐life decision making: a qualitative study of elderly individuals.J Gen Intern Med.2000;15(9):620–625.
- , , , et al.Patient age and decisions to withhold life‐sustaining treatments from seriously ill, hospitalized adults. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment.Ann Intern Med.1999;130(2):116–125.
- .Clinical practice. Assessment of patients' competence to consent to treatment.N Engl J Med.2007;357(18):1834–1840.
- , , , , .The Mini‐Cog: a cognitive “vital signs” measure for dementia screening in multi‐lingual elderly.Int J Geriatr Psychiatry.2000;15(11):1021–1027.
Recent studies of the growth of the hospitalist movement have confirmed that hospitalists are taking care of an increasing percentage of hospitalized older adults.1, 2 Unfortunately, few hospitalist groups have specific programs or protocols to address the special needs of older patients.3, 4 We were inspired by a top 10 article written by nephrologists for primary care physicians to compile 10 evidence‐based pearls that may be helpful to hospitalists caring for older persons.5
1. Many Health Conditions in Older Patients are Multifactorial and Require a Multifactorial Approach to Care
A geriatric syndrome is a multifactorial condition occurring primarily in frail elderly which is usually due to multiple contributing factors and results from an interaction between patient‐specific impairments and situation‐specific stressors.68 Geriatric syndromes cannot be treated easily with a single intervention; the approach must target each modifiable risk factor. Table 1 illustrates for an example of how this approach differs from the traditional medical approach in the case of falls, a common geriatric syndrome. Hospitalists commonly encounter the geriatric syndromes that either lead to hospitalization, such as falls or dementia, or that can complicate a hospitalization for another condition, such as delirium, falls, or urinary incontinence. Two geriatric syndromes in particular, delirium and falls, are associated with increased length of stay, increased healthcare costs, and substantial morbidity.9, 10 Multifactorial interventions such as the Hospital Elder Life Project (HELP) have been shown to prevent delirium and falls.1114 Studies of the HELP intervention demonstrated benefits on outcomes that are important to hospitalists, including shortened length of stay.10, 15 While implementing these interventions is not possible at every institution, it may be possible to implement some aspects in a targeted fashion (for example, early physical therapy and mobilization to decrease risk of delirium and falls) or to work with hospital administration to implement the larger interventions.
| Traditional Medical Approach (Diagnosis and Treatment) | Geriatric Approach (Risk Factor Assessment and Reduction) | |
|---|---|---|
| ||
| Search for cause of falls | Search for cause of falls | |
| (eg, syncope workup including echocardiogram, neurologic workup including imaging) | Assess for risk factors and target interventions reduce or eliminate risk factors identified, eg: | |
| Risk factor | Intervention | |
| Leg weakness | Strength training | |
| Falls when transferring | Training in use of assistive device for transfers | |
| Inadequate lighting at home | Home safety evaluation by physical therapist and installation of lights at home | |
2. Screening Elderly Patients for the Presence of Common Geriatric Syndromes can Improve Care
Comprehensive geriatric assessment, a process of multifactorial health evaluation of the older patient, is an important part of geriatric medicine and has been shown to reduce functional decline.16 While comprehensive geriatric assessment may not be practical in the acute care setting, some basic principles and tools of geriatric assessment, namely screening for geriatric syndromes, can be helpful. Here is one efficient, evidence‐based approach to screening hospitalized elderly patients for cognitive impairment and falls, and then using the results of screening to improve care:
Brief cognitive assessment using the Mini‐Cog screening tool
Even with cognitive screening, it can sometimes be difficult to distinguish between dementia and delirium in an acutely ill person. However, knowing who is cognitively impaired on admission tells us who is likely to develop delirium and may need to be discharged to a supervised location, such as a nursing facility.17, 18 The Mini‐Cog (shown in Table 2) is our preferred tool for cognitive screening, because it takes only 24 minutes to administer, has a sensitivity of 76% and specificity of 89% [similar to the Mini‐Mental State Examination (MMSE)], and has been validated in a multiethnic, multilingual sample with low literacy.19, 20 The Mini‐Cog has not been studied extensively in the inpatient setting, but one study did find that abnormal Mini‐Cog scores correlated with the development of delirium among hospitalized elderly patients.21 Other tools appropriate for brief cognitive screening of hospitalized patients include the MMSE, which is widely known but limited by copyright for clinical use and longer time needed for administration, and the Short Portable Mental Status Questionnaire (SPMSQ), which is entirely verbal and does not require that the patient write or draw.22, 23 A new tool, the Sweet 16, which is also entirely verbal and takes about 2 minutes to administer, shows promise but has not been validated in the inpatient setting.24
|
| The Mini‐Cog combines an uncued three‐item recall test with a clock‐drawing test (CDT) that serves as the recall distractor. The Mini‐Cog can be administered in about three minutes, requires no special equipment, and is less influenced by level of education or language differences. |
| Administration |
| 1. Make sure you have the patient's attention. Then instruct the patient to listen carefully to, repeat back to you, and remember (now and later) three unrelated words. You may present the same words up to 3 times if necessary. |
| 2. Instruct the patient to draw the face of a clock, either on a blank sheet of paper, or on a sheet with the clock circle already drawn on the page. After the patient puts the numbers on the clock face, ask him or her to draw the hands to read a specific time (11:10 or 8:20 are most commonly used; however, other times that require use of both halves of the clock face may be effective). These instructions can be repeated, but no additional instructions should be given. If the patient cannot complete the CDT in three minutes or less, move on to the next step. |
| 3. Ask the patient to repeat the three previously presented words. |
| Scoring |
| Give 1 point for each recalled word after the CDT distractor. Score 03 for recall. |
| Give 2 points for a normal CDT, and 0 points for an abnormal CDT. The CDT is considered normal if all numbers are depicted, once each, in the correct sequence and position around the circle, and the hands readably display the requested time. Do not count equal hand length as an error. Add the recall and CDT scores together to get the Mini‐Cog score: |
| 02 positive screen for dementia. |
| 35 negative screen for dementia. |
Fall screen: Have you fallen in the past year? with more detailed inquiry for frequent fallers
An elderly patient with a history of falls is at high risk for falling while in the hospital. Interventions that target multiple risk factors appear to be effective in reducing risk and rate of falling.25 Some aspects of these multifactorial interventions include environmental modifications such as low beds, high‐impact floor mats, restraint removal, bedside posters and patient education materials, and exercise.13, 26 Medication review and reductions in medications that contribute to falls (psychoactive medications, diuretics, blood pressure agents) can also reduce fall risk.13, 14 Many experts recommend checking a 25‐hydroxy vitamin D level for patients who come into the hospital for treatment of a fall‐related injury, starting or continuing vitamin D and calcium supplementation for those with normal vitamin D levels, and starting aggressive vitamin D replacement with 50,000 units of oral ergocalciferol weekly for those with a level below 20 ng/mL. Vitamin D appears to play an important role in neuromuscular function as well as bone density.27 Meta‐analyses have demonstrated that vitamin D supplementation of 7001,000 IU daily may reduce the risk of falls in the elderly by about 20%, that the effect is achieved in the short term (on the order of 25 months), and that the benefit persists for up to 36 months.28, 29
3. Elderly Patients are at Risk for Functional Decline During Hospitalization and Measures Can Be Taken to Prevent This
A cascade to dependency has been described in which the effects of usual aging (eg, fragile skin) and hospitalization (eg, immobilization) interact with each other, often producing complications (eg, pressure ulcers) that can lead to the loss of the ability to live independently.30 Functional decline during hospitalization is common and is associated with poor prognosis. In one study of elderly patients with new Activities of Daily Living (ADL) disability at discharge, over 40% were dead by 12 months after discharge, and only 30% had returned to baseline function.31, 32 Functional status may affect discharge planning, especially if the patient is not able to return safely to his or her previous living environment. Elderly patients are very vulnerable to new ADL dependency and loss of ambulatory ability as a result of a hospitalization.33, 34 The initial evaluation of an elderly patient should always include an inquiry into the patient's functional abilities, including whether the patient requires assistance to perform self‐care (ADL) activities or instrumental activities of daily living (IADLs), and who is available to help at home. We remember ADLs as those activities we learn as a young child (bathing, dressing, feeding, toileting, transfers) and IADLs as activities we learn when we leave our parents' home to live independently (shopping, cooking, laundry, housekeeping, managing money, using public transportation). Patients in assisted living facilities and adult family homes receive varying degrees of help with ADLs and IADLs, and no particular level of assistance can be assumed; assisted living residents may be at higher risk of functional decline during hospitalization than community‐dwelling persons.35
Acute Care of Elderly (ACE) units have been shown to reduce functional disability and discharge to long‐term care settings, with length of stay and hospital charges similar to that of usual care.36 Most hospitals do not have ACE units, but implementing some components of the intervention, such as early physical and occupational therapy, early discharge planning, early mobility, and adequate nutrition may reduce functional disability. A Cochrane review found a small decrease in length of stay of about a day among elderly patients who participated in a structured exercise program, which could be extrapolated to support the usefulness of increased mobility and early physical therapy.37
4. Delirium is a Common but Serious Condition Among Hospitalized Elderly Patients and in Some Cases Can Be Prevented
The incidence of delirium appears to be as high as 60% in hospitalized elderly patients with multiple risk factors for this condition.38, 39 Delirium predicts longer hospital stay, increases likelihood of discharge to a skilled nursing facility, and is a marker for significant morbidity and mortality.4042 Cognitive screening, as discussed above, can help determine who is at risk for delirium, and the Confusion Assessment Method (CAM) is becoming more widely used as a bedside screening tool for detecting delirium.43 Other important risk factors for delirium in addition to preexisting cognitive impairment include age over 65, prior delirium, polypharmacy, functional dependence, and sensory impairment.44 A landmark randomized controlled trial by Sharon Inouye et al. showed that delirium can often be prevented in high‐risk patients by ensuring frequent reorientation, maintenance of the patient's usual sleep‐wake cycle, early mobilization, adequate nutrition and hydration, and regular use of sensory aids such as glasses and hearing aids.11
When delirium does occur despite preventive efforts, it should trigger a thorough investigation for an underlying cause. Common contributing factors to delirium in hospitalized patients include infections such as urinary tract infections or hospital‐acquired pneumonia, pain, electrolyte abnormalities, cardiac ischemia, medication side effects, and urinary retention or constipation. Any psychoactive or anticholinergic medication can contribute to, or exacerbate, delirium; common culprits include diphenhydramine, benzodiazepines, and muscle relaxants.44 Although one or more treatable underlying causes should always be sought, many cases of delirium in the hospital are multifactorial.
If pharmacologic treatment for delirium is necessary, low‐dose haloperidol is the first‐line agent, starting with 0.25 mg intravenously or 0.5 mg by mouth, nightly to twice a day. A recent systematic review supported the use of haloperidol as a first‐line agent in the acute setting; second‐generation antipsychotics are an alternative, but studies have shown no benefits of these agents over haloperidol in terms of safety or efficacy.45 Physical restraints should be avoided in delirious patients, as they may actually worsen delirium and have not been proven to reduce falls or secondary injury.46
5. Treating Nondementia Illnesses in Hospitalized Elders With Dementia Requires Consideration of the Patient's Limited Life Expectancy and Cognitive Deficits
Elderly patients with dementia are frequently hospitalized for medical illness and pose special challenges to the hospitalist. Patients with dementia may not be able to accurately report symptoms and side effects of therapy, and may lack decisional capacity. The clinician should also carefully consider the benefits and burdens of a proposed therapy or diagnostic test, taking into account the patient's cognitive deficits and limited life expectancy.47 The median postdiagnosis life expectancy of a patient with Alzheimer disease is about 4 years for men and about 6 years for women, with a range from about 2 to 9 years, according to population‐based studies of incident Alzheimer dementia.48, 49 In a patient with early or mild dementia, the hospitalist may first need to establish whether the patient does indeed have dementia. It is also important to question family about how the patient is managing at home so that appropriate discharge plans can be made.
Any intervention such as surgery or intubation in a patient with dementia should be considered carefully in the context of the patient's dementia, keeping in mind the remaining life expectancy, increased risk for delirium after surgery, and potential difficulty with adherence to postoperative precautions or participation in rehabilitation. Invasive procedures such as mechanical ventilation or central line placement may not be indicated in patients with advanced dementia. In one prospective cohort study, patients with advanced dementia admitted to the hospital for hip fractures or pneumonia had much higher mortality than those without dementia, despite having equal rates of procedures such as mechanical ventilation and central line placement.50
A common scenario in a patient with advanced dementia is the patient presenting with decreased intake and dysphagia; family and/or caregivers inquire about enteral tube feeding and/or long‐term intravenous hydration. This situation requires a thoughtfully presented, informative discussion with the family about artificial feeding in advanced dementia. There is no evidence that artificial feeding improves outcomes, and a recent Cochrane systematic review found insufficient evidence to suggest that enteral tube feeding is beneficial in patients with dementia.5153 Instead, dementia patients at the end of their lives benefit from a palliative approach, which would include hand‐feeding for comfort if the patient indicates hunger.54
6. Frail Elderly Patients are at High Risk for Iatrogenic Complications During Hospitalization
Frail elders are at increased risk for iatrogenic complications, including surgical‐ and procedure‐related events, adverse drug events, nosocomial infections, pressure ulcers, and falls.5557 In the Harvard Medical Practice Study, a retrospective study of adverse events in 30,000 patients, those age 65 and over accounted for 27% of the hospitalized population but 43% of the adverse events. In this study, four types of adverse events occurred at least twice as often in older patients: fractures, falls, nontechnical postoperative complications, and adverse events related to noninvasive treatments.58 The risk of hospital‐acquired infection also rises dramatically with age; risk is ten times higher in patients over 70 than those aged 49 and under, with urinary tract infections and surgical site infections the most common.59 The oldest, most seriously ill and most functionally impaired elderly patients are at particularly high risk of cascade iatrogenesis, where one medical intervention triggers a series of adverse events.60 Frail elderly patients are at greater risk for adverse events during hospitalization, and careful consideration of the need for all diagnostic tests and procedures may reduce risks. Table 3 lists the iatrogenic complications that disproportionately affect the elderly.
7. Pain Should Be Aggressively Identified and Appropriately Treated
Adequate treatment of pain in the elderly can improve functional status, mobility, and mood. Clinicians are understandably wary of prescribing opioids in the elderly, but undertreatment of pain is also common and in hospitalized patients can lead to delirium, delays in rehabilitation, and higher healthcare costs.44, 61 Acetaminophen is generally safe and is recommended as first‐line therapy in most cases of pain. Nonsteroidal antiinflammatory drugs (NSAIDS) should be used with caution, as the risk of gastrointestinal toxicity increases with age; long‐acting agents such as toradol should be avoided.62 A study of adverse drug reactions causing hospitalization in elderly individuals implicated NSAIDs in 23.5% of cases.63 If a patient has severe pain that limits functional capacity but does not respond to acetaminophen, it is reasonable to consider low‐dose opioids. The 2009 American Geriatrics Society guidelines recommend that opioids be used for severe pain, especially when it limits functional capacity. Opioids should be given orally when possible and started at low doses (for example, 2.5 to 5 milligrams of oxycodone offered every 4 hours as needed). Either oxycodone or morphine can be used as a first‐line, short‐acting opioid, but morphine should be used cautiously in patients with renal insufficiency, as toxic metabolites are renally cleared. Methadone should be used very cautiously and ideally by clinicians experienced in its use because of its long and variable half‐life. Serotonin‐norepinephrine reuptake inhibitors such as duloxetine, and anticonvulsants such as gabapentin, can be helpful adjuncts for neuropathic pain; tricyclics should generally be avoided, because the elderly are particularly sensitive to the anticholinergic side effects (ie, sedation, orthostatic hypotension, urinary retention, constipation) of these agents.61 Nortriptyline, which has the least anticholinergic properties of this medication class, may be the best option if a tricyclic is desired.
8. Hospitalization Can Be an Opportunity for a Thorough Review and Reduction of Outpatient Medications in Collaboration With the Patient's Primary Care Provider
Adverse drug reactions (ADRs) are potentially life‐threatening for all patients, but elderly individuals are disproportionately affected. It is estimated that 30% of hospital admissions of older patients are due to drug‐related toxicity.64 The Beers criteria provide expert consensus on drugs that should either be avoided or used cautiously in the elderly; we have highlighted some of the drugs on the Beers list that are relevant to the hospitalist in Table 4. Notable inclusions on the most recent Beers list include nitrofurantoin, ferrous sulfate at dosages greater than 325 mg per day, doxazosin, and fluoxetine.65 Anticholinergics (such as oxybutynin) and cholinesterase inhibitors (such as donepezil) should not be used together, because the interaction makes them ineffective.
| Falls and fractures58 |
| Nosocomial infections59 |
| Delirium44 |
| Surgical and postoperative complications58 |
| Adverse drug events56 |
| Pressure sores56 |
| Medication | Rationale |
|---|---|
| |
| Benzodiazepines | Can contribute to delirium and falls. |
| Muscle relaxants | Anticholinergic side effects; sedating; can contribute to delirium. |
| Diphenhydramine | Very sedating; can contribute to delirium; do not use as a sleep aid, and use lowest possible dose when treating allergic reactions. |
| Nitrofurantoin | Can cause renal impairment. |
| Ketorolac | Can lead to gastrointestinal bleeds and renal impairment. |
| Ferrous sulfate in doses >325 mg/day | Can cause severe constipation; higher doses not well absorbed. |
| Digoxin in doses of >0.125 mg/day | Decreased renal clearance can increase risk of toxicity (higher doses acceptable for atrial arrythmias). |
| Amiodarone | Multiple toxicities; lack of proven efficacy in older adults. |
| Fluoxetine | Long half‐life; can cause agitation and sleep disturbance. |
| Meperidine | Can cause seizures and contribute to delirium. |
| Doxazosin | Can cause hypotension and contribute to falls. |
Many ADRs are caused by medications that are not on the Beers list but have narrow therapeutic windows, especially warfarin and insulin; digoxin, which is on the Beers list, is another common culprit in ADRs leading to emergency room visits.66 Medications that are clearly causing ADRs should be discontinued, with the knowledge and input of the primary care provider, and with written documentation on the discharge summary and clear instructions to the patient. Even when a hospital admission is not a result of an ADR, it may provide an opportunity to review the patient's medication list, clarify that the patient is taking medications as directed by their primary care provider, and determine if the list contains medications where risks now outweigh benefits, in which case those medications should be discontinued. Studies have shown that elimination of medications that are associated with falls reduces the risk of future falls.67 Adjustments to patient's medications should be made in close collaboration with the primary care provider and with a clinical pharmacist, if available.
9. Discharge Planning for an Elderly Patient Should Start Early, Be Comprehensive, and Involve the Patient and Caregivers
A successful discharge plan for an elderly patient must start early, take functional status into account, and perhaps most importantly, the planning process should involve the patient and family, if appropriate. One study of patients over 70 discharged from an urban, academic public hospital found that only 10% recalled receiving written discharge instructions, and only 53% who were prescribed a new medication actually had that medication at home.68 Growing evidence suggests that older patients have poorer functional health literacy regarding medications.69 Care transitions are an active area of research, and multiple studies have shown lower rates of rehospitalization with comprehensive transitional care programs involving transition coaches or advance practice nurses providing home visits and follow‐up telephone calls.70, 71 More research is needed in this area to develop simple, cost‐effective care transitions programs. In the meantime, hospitalists can actively involve a multidisciplinary team (pharmacists and social workers, for example) early in the hospitalization, provide more patient‐friendly discharge materials such as those available as part of the Society of Hospital Medicine's BOOST, and place targeted follow‐up phone calls after discharge.52, 7274 Ensuring that a frail elderly patient's primary care provider is aware of the hospitalization may be particularly important in avoiding postdischarge problems.75
10. Elderly Patients are Often Very Clear About Their Preferences for Treatment. Discussing This on Admission Can Help Clarify the Goals of the Hospitalization
The risks and benefits of any intervention being considered should be presented and discussed with the patient in the context of the likelihood of the intervention restoring an acceptable quality of life to the patient. Many common chronic conditions in the elderly such as Parkinson disease, congestive heart failure, and dementia are progressive and life‐limiting. Qualitative studies confirm that elderly patients want to know the likelihood that a proposed intervention will help them return to their previous level of functioning or a level that is acceptable to them.76, 77 In one prospective cohort study, older age was found to correlate with a higher rate of withholding ventilatory support, dialysis, and surgery.78 However, a more recent study has suggested that patient preferences are more dynamic, and that older patients will make decisions based on current health status rather than core values.76 While families should be involved in the process of clarification of goals of care, the patients' own values should be elicited whenever possible, with bedside assessment of decision‐making capacity to ensure that patients are allowed to speak for themselves if they possess decisional capacity for the decision at hand.79
Hospitalists should have a special approach to the elderly patient which takes into account the elder's increased vulnerability to iatrogenic complications and acute functional decline, the presence of geriatric syndromes, and individual preferences. Early assessment of an elderly patient's cognitive and physical functioning, level of pain, fall risk, and preferences for care are necessary for optimal inpatient care and may result in preserved function and a decrease in adverse events.
Recent studies of the growth of the hospitalist movement have confirmed that hospitalists are taking care of an increasing percentage of hospitalized older adults.1, 2 Unfortunately, few hospitalist groups have specific programs or protocols to address the special needs of older patients.3, 4 We were inspired by a top 10 article written by nephrologists for primary care physicians to compile 10 evidence‐based pearls that may be helpful to hospitalists caring for older persons.5
1. Many Health Conditions in Older Patients are Multifactorial and Require a Multifactorial Approach to Care
A geriatric syndrome is a multifactorial condition occurring primarily in frail elderly which is usually due to multiple contributing factors and results from an interaction between patient‐specific impairments and situation‐specific stressors.68 Geriatric syndromes cannot be treated easily with a single intervention; the approach must target each modifiable risk factor. Table 1 illustrates for an example of how this approach differs from the traditional medical approach in the case of falls, a common geriatric syndrome. Hospitalists commonly encounter the geriatric syndromes that either lead to hospitalization, such as falls or dementia, or that can complicate a hospitalization for another condition, such as delirium, falls, or urinary incontinence. Two geriatric syndromes in particular, delirium and falls, are associated with increased length of stay, increased healthcare costs, and substantial morbidity.9, 10 Multifactorial interventions such as the Hospital Elder Life Project (HELP) have been shown to prevent delirium and falls.1114 Studies of the HELP intervention demonstrated benefits on outcomes that are important to hospitalists, including shortened length of stay.10, 15 While implementing these interventions is not possible at every institution, it may be possible to implement some aspects in a targeted fashion (for example, early physical therapy and mobilization to decrease risk of delirium and falls) or to work with hospital administration to implement the larger interventions.
| Traditional Medical Approach (Diagnosis and Treatment) | Geriatric Approach (Risk Factor Assessment and Reduction) | |
|---|---|---|
| ||
| Search for cause of falls | Search for cause of falls | |
| (eg, syncope workup including echocardiogram, neurologic workup including imaging) | Assess for risk factors and target interventions reduce or eliminate risk factors identified, eg: | |
| Risk factor | Intervention | |
| Leg weakness | Strength training | |
| Falls when transferring | Training in use of assistive device for transfers | |
| Inadequate lighting at home | Home safety evaluation by physical therapist and installation of lights at home | |
2. Screening Elderly Patients for the Presence of Common Geriatric Syndromes can Improve Care
Comprehensive geriatric assessment, a process of multifactorial health evaluation of the older patient, is an important part of geriatric medicine and has been shown to reduce functional decline.16 While comprehensive geriatric assessment may not be practical in the acute care setting, some basic principles and tools of geriatric assessment, namely screening for geriatric syndromes, can be helpful. Here is one efficient, evidence‐based approach to screening hospitalized elderly patients for cognitive impairment and falls, and then using the results of screening to improve care:
Brief cognitive assessment using the Mini‐Cog screening tool
Even with cognitive screening, it can sometimes be difficult to distinguish between dementia and delirium in an acutely ill person. However, knowing who is cognitively impaired on admission tells us who is likely to develop delirium and may need to be discharged to a supervised location, such as a nursing facility.17, 18 The Mini‐Cog (shown in Table 2) is our preferred tool for cognitive screening, because it takes only 24 minutes to administer, has a sensitivity of 76% and specificity of 89% [similar to the Mini‐Mental State Examination (MMSE)], and has been validated in a multiethnic, multilingual sample with low literacy.19, 20 The Mini‐Cog has not been studied extensively in the inpatient setting, but one study did find that abnormal Mini‐Cog scores correlated with the development of delirium among hospitalized elderly patients.21 Other tools appropriate for brief cognitive screening of hospitalized patients include the MMSE, which is widely known but limited by copyright for clinical use and longer time needed for administration, and the Short Portable Mental Status Questionnaire (SPMSQ), which is entirely verbal and does not require that the patient write or draw.22, 23 A new tool, the Sweet 16, which is also entirely verbal and takes about 2 minutes to administer, shows promise but has not been validated in the inpatient setting.24
|
| The Mini‐Cog combines an uncued three‐item recall test with a clock‐drawing test (CDT) that serves as the recall distractor. The Mini‐Cog can be administered in about three minutes, requires no special equipment, and is less influenced by level of education or language differences. |
| Administration |
| 1. Make sure you have the patient's attention. Then instruct the patient to listen carefully to, repeat back to you, and remember (now and later) three unrelated words. You may present the same words up to 3 times if necessary. |
| 2. Instruct the patient to draw the face of a clock, either on a blank sheet of paper, or on a sheet with the clock circle already drawn on the page. After the patient puts the numbers on the clock face, ask him or her to draw the hands to read a specific time (11:10 or 8:20 are most commonly used; however, other times that require use of both halves of the clock face may be effective). These instructions can be repeated, but no additional instructions should be given. If the patient cannot complete the CDT in three minutes or less, move on to the next step. |
| 3. Ask the patient to repeat the three previously presented words. |
| Scoring |
| Give 1 point for each recalled word after the CDT distractor. Score 03 for recall. |
| Give 2 points for a normal CDT, and 0 points for an abnormal CDT. The CDT is considered normal if all numbers are depicted, once each, in the correct sequence and position around the circle, and the hands readably display the requested time. Do not count equal hand length as an error. Add the recall and CDT scores together to get the Mini‐Cog score: |
| 02 positive screen for dementia. |
| 35 negative screen for dementia. |
Fall screen: Have you fallen in the past year? with more detailed inquiry for frequent fallers
An elderly patient with a history of falls is at high risk for falling while in the hospital. Interventions that target multiple risk factors appear to be effective in reducing risk and rate of falling.25 Some aspects of these multifactorial interventions include environmental modifications such as low beds, high‐impact floor mats, restraint removal, bedside posters and patient education materials, and exercise.13, 26 Medication review and reductions in medications that contribute to falls (psychoactive medications, diuretics, blood pressure agents) can also reduce fall risk.13, 14 Many experts recommend checking a 25‐hydroxy vitamin D level for patients who come into the hospital for treatment of a fall‐related injury, starting or continuing vitamin D and calcium supplementation for those with normal vitamin D levels, and starting aggressive vitamin D replacement with 50,000 units of oral ergocalciferol weekly for those with a level below 20 ng/mL. Vitamin D appears to play an important role in neuromuscular function as well as bone density.27 Meta‐analyses have demonstrated that vitamin D supplementation of 7001,000 IU daily may reduce the risk of falls in the elderly by about 20%, that the effect is achieved in the short term (on the order of 25 months), and that the benefit persists for up to 36 months.28, 29
3. Elderly Patients are at Risk for Functional Decline During Hospitalization and Measures Can Be Taken to Prevent This
A cascade to dependency has been described in which the effects of usual aging (eg, fragile skin) and hospitalization (eg, immobilization) interact with each other, often producing complications (eg, pressure ulcers) that can lead to the loss of the ability to live independently.30 Functional decline during hospitalization is common and is associated with poor prognosis. In one study of elderly patients with new Activities of Daily Living (ADL) disability at discharge, over 40% were dead by 12 months after discharge, and only 30% had returned to baseline function.31, 32 Functional status may affect discharge planning, especially if the patient is not able to return safely to his or her previous living environment. Elderly patients are very vulnerable to new ADL dependency and loss of ambulatory ability as a result of a hospitalization.33, 34 The initial evaluation of an elderly patient should always include an inquiry into the patient's functional abilities, including whether the patient requires assistance to perform self‐care (ADL) activities or instrumental activities of daily living (IADLs), and who is available to help at home. We remember ADLs as those activities we learn as a young child (bathing, dressing, feeding, toileting, transfers) and IADLs as activities we learn when we leave our parents' home to live independently (shopping, cooking, laundry, housekeeping, managing money, using public transportation). Patients in assisted living facilities and adult family homes receive varying degrees of help with ADLs and IADLs, and no particular level of assistance can be assumed; assisted living residents may be at higher risk of functional decline during hospitalization than community‐dwelling persons.35
Acute Care of Elderly (ACE) units have been shown to reduce functional disability and discharge to long‐term care settings, with length of stay and hospital charges similar to that of usual care.36 Most hospitals do not have ACE units, but implementing some components of the intervention, such as early physical and occupational therapy, early discharge planning, early mobility, and adequate nutrition may reduce functional disability. A Cochrane review found a small decrease in length of stay of about a day among elderly patients who participated in a structured exercise program, which could be extrapolated to support the usefulness of increased mobility and early physical therapy.37
4. Delirium is a Common but Serious Condition Among Hospitalized Elderly Patients and in Some Cases Can Be Prevented
The incidence of delirium appears to be as high as 60% in hospitalized elderly patients with multiple risk factors for this condition.38, 39 Delirium predicts longer hospital stay, increases likelihood of discharge to a skilled nursing facility, and is a marker for significant morbidity and mortality.4042 Cognitive screening, as discussed above, can help determine who is at risk for delirium, and the Confusion Assessment Method (CAM) is becoming more widely used as a bedside screening tool for detecting delirium.43 Other important risk factors for delirium in addition to preexisting cognitive impairment include age over 65, prior delirium, polypharmacy, functional dependence, and sensory impairment.44 A landmark randomized controlled trial by Sharon Inouye et al. showed that delirium can often be prevented in high‐risk patients by ensuring frequent reorientation, maintenance of the patient's usual sleep‐wake cycle, early mobilization, adequate nutrition and hydration, and regular use of sensory aids such as glasses and hearing aids.11
When delirium does occur despite preventive efforts, it should trigger a thorough investigation for an underlying cause. Common contributing factors to delirium in hospitalized patients include infections such as urinary tract infections or hospital‐acquired pneumonia, pain, electrolyte abnormalities, cardiac ischemia, medication side effects, and urinary retention or constipation. Any psychoactive or anticholinergic medication can contribute to, or exacerbate, delirium; common culprits include diphenhydramine, benzodiazepines, and muscle relaxants.44 Although one or more treatable underlying causes should always be sought, many cases of delirium in the hospital are multifactorial.
If pharmacologic treatment for delirium is necessary, low‐dose haloperidol is the first‐line agent, starting with 0.25 mg intravenously or 0.5 mg by mouth, nightly to twice a day. A recent systematic review supported the use of haloperidol as a first‐line agent in the acute setting; second‐generation antipsychotics are an alternative, but studies have shown no benefits of these agents over haloperidol in terms of safety or efficacy.45 Physical restraints should be avoided in delirious patients, as they may actually worsen delirium and have not been proven to reduce falls or secondary injury.46
5. Treating Nondementia Illnesses in Hospitalized Elders With Dementia Requires Consideration of the Patient's Limited Life Expectancy and Cognitive Deficits
Elderly patients with dementia are frequently hospitalized for medical illness and pose special challenges to the hospitalist. Patients with dementia may not be able to accurately report symptoms and side effects of therapy, and may lack decisional capacity. The clinician should also carefully consider the benefits and burdens of a proposed therapy or diagnostic test, taking into account the patient's cognitive deficits and limited life expectancy.47 The median postdiagnosis life expectancy of a patient with Alzheimer disease is about 4 years for men and about 6 years for women, with a range from about 2 to 9 years, according to population‐based studies of incident Alzheimer dementia.48, 49 In a patient with early or mild dementia, the hospitalist may first need to establish whether the patient does indeed have dementia. It is also important to question family about how the patient is managing at home so that appropriate discharge plans can be made.
Any intervention such as surgery or intubation in a patient with dementia should be considered carefully in the context of the patient's dementia, keeping in mind the remaining life expectancy, increased risk for delirium after surgery, and potential difficulty with adherence to postoperative precautions or participation in rehabilitation. Invasive procedures such as mechanical ventilation or central line placement may not be indicated in patients with advanced dementia. In one prospective cohort study, patients with advanced dementia admitted to the hospital for hip fractures or pneumonia had much higher mortality than those without dementia, despite having equal rates of procedures such as mechanical ventilation and central line placement.50
A common scenario in a patient with advanced dementia is the patient presenting with decreased intake and dysphagia; family and/or caregivers inquire about enteral tube feeding and/or long‐term intravenous hydration. This situation requires a thoughtfully presented, informative discussion with the family about artificial feeding in advanced dementia. There is no evidence that artificial feeding improves outcomes, and a recent Cochrane systematic review found insufficient evidence to suggest that enteral tube feeding is beneficial in patients with dementia.5153 Instead, dementia patients at the end of their lives benefit from a palliative approach, which would include hand‐feeding for comfort if the patient indicates hunger.54
6. Frail Elderly Patients are at High Risk for Iatrogenic Complications During Hospitalization
Frail elders are at increased risk for iatrogenic complications, including surgical‐ and procedure‐related events, adverse drug events, nosocomial infections, pressure ulcers, and falls.5557 In the Harvard Medical Practice Study, a retrospective study of adverse events in 30,000 patients, those age 65 and over accounted for 27% of the hospitalized population but 43% of the adverse events. In this study, four types of adverse events occurred at least twice as often in older patients: fractures, falls, nontechnical postoperative complications, and adverse events related to noninvasive treatments.58 The risk of hospital‐acquired infection also rises dramatically with age; risk is ten times higher in patients over 70 than those aged 49 and under, with urinary tract infections and surgical site infections the most common.59 The oldest, most seriously ill and most functionally impaired elderly patients are at particularly high risk of cascade iatrogenesis, where one medical intervention triggers a series of adverse events.60 Frail elderly patients are at greater risk for adverse events during hospitalization, and careful consideration of the need for all diagnostic tests and procedures may reduce risks. Table 3 lists the iatrogenic complications that disproportionately affect the elderly.
7. Pain Should Be Aggressively Identified and Appropriately Treated
Adequate treatment of pain in the elderly can improve functional status, mobility, and mood. Clinicians are understandably wary of prescribing opioids in the elderly, but undertreatment of pain is also common and in hospitalized patients can lead to delirium, delays in rehabilitation, and higher healthcare costs.44, 61 Acetaminophen is generally safe and is recommended as first‐line therapy in most cases of pain. Nonsteroidal antiinflammatory drugs (NSAIDS) should be used with caution, as the risk of gastrointestinal toxicity increases with age; long‐acting agents such as toradol should be avoided.62 A study of adverse drug reactions causing hospitalization in elderly individuals implicated NSAIDs in 23.5% of cases.63 If a patient has severe pain that limits functional capacity but does not respond to acetaminophen, it is reasonable to consider low‐dose opioids. The 2009 American Geriatrics Society guidelines recommend that opioids be used for severe pain, especially when it limits functional capacity. Opioids should be given orally when possible and started at low doses (for example, 2.5 to 5 milligrams of oxycodone offered every 4 hours as needed). Either oxycodone or morphine can be used as a first‐line, short‐acting opioid, but morphine should be used cautiously in patients with renal insufficiency, as toxic metabolites are renally cleared. Methadone should be used very cautiously and ideally by clinicians experienced in its use because of its long and variable half‐life. Serotonin‐norepinephrine reuptake inhibitors such as duloxetine, and anticonvulsants such as gabapentin, can be helpful adjuncts for neuropathic pain; tricyclics should generally be avoided, because the elderly are particularly sensitive to the anticholinergic side effects (ie, sedation, orthostatic hypotension, urinary retention, constipation) of these agents.61 Nortriptyline, which has the least anticholinergic properties of this medication class, may be the best option if a tricyclic is desired.
8. Hospitalization Can Be an Opportunity for a Thorough Review and Reduction of Outpatient Medications in Collaboration With the Patient's Primary Care Provider
Adverse drug reactions (ADRs) are potentially life‐threatening for all patients, but elderly individuals are disproportionately affected. It is estimated that 30% of hospital admissions of older patients are due to drug‐related toxicity.64 The Beers criteria provide expert consensus on drugs that should either be avoided or used cautiously in the elderly; we have highlighted some of the drugs on the Beers list that are relevant to the hospitalist in Table 4. Notable inclusions on the most recent Beers list include nitrofurantoin, ferrous sulfate at dosages greater than 325 mg per day, doxazosin, and fluoxetine.65 Anticholinergics (such as oxybutynin) and cholinesterase inhibitors (such as donepezil) should not be used together, because the interaction makes them ineffective.
| Falls and fractures58 |
| Nosocomial infections59 |
| Delirium44 |
| Surgical and postoperative complications58 |
| Adverse drug events56 |
| Pressure sores56 |
| Medication | Rationale |
|---|---|
| |
| Benzodiazepines | Can contribute to delirium and falls. |
| Muscle relaxants | Anticholinergic side effects; sedating; can contribute to delirium. |
| Diphenhydramine | Very sedating; can contribute to delirium; do not use as a sleep aid, and use lowest possible dose when treating allergic reactions. |
| Nitrofurantoin | Can cause renal impairment. |
| Ketorolac | Can lead to gastrointestinal bleeds and renal impairment. |
| Ferrous sulfate in doses >325 mg/day | Can cause severe constipation; higher doses not well absorbed. |
| Digoxin in doses of >0.125 mg/day | Decreased renal clearance can increase risk of toxicity (higher doses acceptable for atrial arrythmias). |
| Amiodarone | Multiple toxicities; lack of proven efficacy in older adults. |
| Fluoxetine | Long half‐life; can cause agitation and sleep disturbance. |
| Meperidine | Can cause seizures and contribute to delirium. |
| Doxazosin | Can cause hypotension and contribute to falls. |
Many ADRs are caused by medications that are not on the Beers list but have narrow therapeutic windows, especially warfarin and insulin; digoxin, which is on the Beers list, is another common culprit in ADRs leading to emergency room visits.66 Medications that are clearly causing ADRs should be discontinued, with the knowledge and input of the primary care provider, and with written documentation on the discharge summary and clear instructions to the patient. Even when a hospital admission is not a result of an ADR, it may provide an opportunity to review the patient's medication list, clarify that the patient is taking medications as directed by their primary care provider, and determine if the list contains medications where risks now outweigh benefits, in which case those medications should be discontinued. Studies have shown that elimination of medications that are associated with falls reduces the risk of future falls.67 Adjustments to patient's medications should be made in close collaboration with the primary care provider and with a clinical pharmacist, if available.
9. Discharge Planning for an Elderly Patient Should Start Early, Be Comprehensive, and Involve the Patient and Caregivers
A successful discharge plan for an elderly patient must start early, take functional status into account, and perhaps most importantly, the planning process should involve the patient and family, if appropriate. One study of patients over 70 discharged from an urban, academic public hospital found that only 10% recalled receiving written discharge instructions, and only 53% who were prescribed a new medication actually had that medication at home.68 Growing evidence suggests that older patients have poorer functional health literacy regarding medications.69 Care transitions are an active area of research, and multiple studies have shown lower rates of rehospitalization with comprehensive transitional care programs involving transition coaches or advance practice nurses providing home visits and follow‐up telephone calls.70, 71 More research is needed in this area to develop simple, cost‐effective care transitions programs. In the meantime, hospitalists can actively involve a multidisciplinary team (pharmacists and social workers, for example) early in the hospitalization, provide more patient‐friendly discharge materials such as those available as part of the Society of Hospital Medicine's BOOST, and place targeted follow‐up phone calls after discharge.52, 7274 Ensuring that a frail elderly patient's primary care provider is aware of the hospitalization may be particularly important in avoiding postdischarge problems.75
10. Elderly Patients are Often Very Clear About Their Preferences for Treatment. Discussing This on Admission Can Help Clarify the Goals of the Hospitalization
The risks and benefits of any intervention being considered should be presented and discussed with the patient in the context of the likelihood of the intervention restoring an acceptable quality of life to the patient. Many common chronic conditions in the elderly such as Parkinson disease, congestive heart failure, and dementia are progressive and life‐limiting. Qualitative studies confirm that elderly patients want to know the likelihood that a proposed intervention will help them return to their previous level of functioning or a level that is acceptable to them.76, 77 In one prospective cohort study, older age was found to correlate with a higher rate of withholding ventilatory support, dialysis, and surgery.78 However, a more recent study has suggested that patient preferences are more dynamic, and that older patients will make decisions based on current health status rather than core values.76 While families should be involved in the process of clarification of goals of care, the patients' own values should be elicited whenever possible, with bedside assessment of decision‐making capacity to ensure that patients are allowed to speak for themselves if they possess decisional capacity for the decision at hand.79
Hospitalists should have a special approach to the elderly patient which takes into account the elder's increased vulnerability to iatrogenic complications and acute functional decline, the presence of geriatric syndromes, and individual preferences. Early assessment of an elderly patient's cognitive and physical functioning, level of pain, fall risk, and preferences for care are necessary for optimal inpatient care and may result in preserved function and a decrease in adverse events.
- , , , .Growth in the care of older patients by hospitalists in the United States.N Engl J Med.2009;360(11):1102–1112.
- , , , , , .Continuity of outpatient and inpatient care by primary care physicians for hospitalized older adults.JAMA.2009;301(16):1671–1680.
- , , .Is there a geriatrician in the house? Geriatric care approaches in hospitalist programs.J Hosp Med.2006;1(1):29–35.
- .Care of hospitalized older patients: opportunities for hospital‐based physicians.J Hosp Med.2006;1(1):42–47.
- , .The top 10 things nephrologists wish every primary care physician knew.Mayo Clin Proc.2009;84(2):180–186.
- .What is a geriatric syndrome anyway?J Am Geriatr Soc.2003;51(4):574–576.
- , , , .Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept.J Am Geriatr Soc.2007;55(5):780–791.
- , , .Some considerations regarding geriatric syndromes.Ann Intern Med.2001;135(12):1095.
- , , , et al.Impact and recognition of cognitive impairment among hospitalized elders.J Hosp Med.2010;5(2):69–75.
- , , , , , .A longitudinal analysis of total 3‐year healthcare costs for older adults who experience a fall requiring medical care.J Am Geriatr Soc.2010;58(5):853–860.
- , , , et al.A multicomponent intervention to prevent delirium in hospitalized older patients.N Engl J Med.1999;340(9):669–676.
- , , , .Shared risk factors for falls, incontinence, and functional dependence. Unifying the approach to geriatric syndromes.JAMA.1995;273(17):1348–1353.
- , , , et al.Strategies to prevent falls and fractures in hospitals and care homes and effect of cognitive impairment: systematic review and meta‐analyses.BMJ.2007;334(7584):82.
- , , , et al.Interventions for preventing falls in acute‐ and chronic‐care hospitals: a systematic review and meta‐analysis.J Am Geriatr Soc.2008;56(1):29–36.
- , , , et al.Postoperative delirium in the elderly: risk factors and outcomes.Ann Surg.2009;249(1):173–178.
- , , , et al.A controlled trial of inpatient and outpatient geriatric evaluation and management.N Engl J Med.2002;346(12):905–912.
- , , , et al.Risk factors for preoperative and postoperative delirium in elderly patients with hip fracture.J Am Geriatr Soc.2009;57(8):1354‐1361.
- , , , , , .Risk factors for delirium in intensive care patients: a prospective cohort study.Crit Care.2009;13(3):R77.
- , , , .The Mini‐Cog as a screen for dementia: validation in a population‐based sample.J Am Geriatr Soc.2003;51(10):1451–1454.
- , , , , .Improving identification of cognitive impairment in primary care.Int J Geriatr Psychiatry.2006;21(4):349–355.
- , , , et al.Simple cognitive testing (Mini‐Cog) predicts inhospital delirium in the elderly.J Am Geriatr Soc.2007;55(2):314–316.
- , , , .Short Portable Mental Status Questionnaire as a screening test for dementia and delirium among the elderly.J Am Geriatr Soc.1987;35(5):412–416.
- , , .“Mini‐mental state.” A practical method for grading the cognitive state of patients for the clinician.J Psychiatr Res.1975;12(3):189–198.
- , , , et al.Development and validation of a brief cognitive assessment tool: the Sweet 16.Arch Intern Med.2010. [Epub ahead of Print].
- , , , et al.Interventions for preventing falls in older people in nursing care facilities and hospitals.Cochrane Database Syst Rev.2010;(1):CD005465.
- , , , et al.Fall prevention in acute care hospitals: a randomized trial.JAMA.2010;304(17):1912–1918.
- , , , et al.Vitamin D supplementation improves neuromuscular function in older people who fall.Age Ageing.2004;33(6):589–595.
- , , , et al.Effect of vitamin D on falls: a meta‐analysis.JAMA.2004;291(16):1999–2006.
- , et al.Fall prevention with supplemental and active forms of vitamin D: a meta‐analysis of randomised controlled trials.BMJ.2009;339:b3692.
- .Hazards of hospitalization of the elderly.Ann Intern Med.1993;118(3):219–223.
- , , , .Hospitalization, restricted activity, and the development of disability among older persons.JAMA.2004;292(17):2115–2124.
- , , , et al.Recovery of activities of daily living in older adults after hospitalization for acute medical illness.J Am Geriatr Soc.2008;56(12):2171–2179.
- , , , et al.Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age.J Am Geriatr Soc.2003;51(4):451–458.
- , , .New walking dependence associated with hospitalization for acute medical illness: incidence and significance.J Gerontol A Biol Sci Med Sci.1998;53(4):M307–M312.
- , , , .Hazards of hospitalization: residence prior to admission predicts outcomes.Gerontologist.2008;48(4):537–541.
- , , , , , et al.A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients.N Engl J Med.1995;332(20):1338–1344.
- , .Exercise for acutely hospitalised older medical inpatients.Cochrane Database Syst Rev.2007;(1):CD005955.
- , , .Occurrence and outcome of delirium in medical in‐patients: a systematic literature review.Age Ageing.2006;35(4):350–364.
- , , .A prospective study of delirium in hospitalized elderly.JAMA.1990;263(8):1097–1101.
- , , , , .Delirium predicts 12‐month mortality.Arch Intern Med.2002;162(4):457–463.
- , , , , .The course of delirium in older medical inpatients: a prospective study.J Gen Intern Med.2003;18(9):696–704.
- , , , .Does delirium increase hospital stay?J Am Geriatr Soc.2003;51(11):1539–1546.
- , , , .The Confusion Assessment Method: a systematic review of current usage.J Am Geriatr Soc.2008;56(5):823–830.
- .Delirium in older persons.N Engl J Med.2006;354(11):1157–1165.
- , , , et al.Pharmacological management of delirium in hospitalized adults—a systematic evidence review.J Gen Intern Med.2009;24(7):848‐853.
- , , .Safety and efficacy of physical restraints for the elderly. Review of the evidence.Can Fam Physician.1996;42:2402–2409.
- , , .Treating nondementia illnesses in patients with dementia.JAMA.2000;283(24):3230–3235.
- , , , , , .Survival in Alzheimer disease: a multiethnic, population‐based study of incident cases.Neurology.2008;71(19):1489–1495.
- , , , et al.Survival after initial diagnosis of Alzheimer disease.Ann Intern Med.2004;140(7):501–509.
- , .Mortality from pneumonia and hip fractures in patients with advanced dementia.JAMA.2000;284(19):2447–2448.
- .Rethinking the role of tube feeding in patients with advanced dementia.N Engl J Med.2000;342(3):206–210.
- Society of Hospital Medicine. BOOSTing Care Transitions Resource Room. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_CareTransitions/CT_Home.cfm. Accessed January 25,2011.
- , , .Enteral tube feeding for older people with advanced dementia.Cochrane Database Syst Rev.2009;(2):CD007209.
- .A 93‐year‐old man with advanced dementia and eating problems.JAMA.2007;298(21):2527–2536.
- , , .Patient safety in geriatrics: a call for action.J Gerontol A Biol Sci Med Sci.2003;58(9):M813–M819.
- , , .Preventable medical injuries in older patients.Arch Intern Med.2000;160(18):2717–2728.
- , , , et al.Iatrogenic complications in high‐risk, elderly patients.Arch Intern Med.1992;152(10):2074–2080.
- , , , et al.The nature of adverse events in hospitalized patients. Results of the Harvard Medical Practice Study II.N Engl J Med.1991.
- , , , , et al.Nosocomial infections: decade‐specific risk.Infect Control.1983;4(3):145–147.
- , , , , , .A quality‐of‐care analysis of cascade iatrogenesis in frail elderly hospital patients.QRB Qual Rev Bull.1993;19(6):199‐2.
- American Geriatrics Society Panel on the Pharmacological Management of Persistent Pain in Older Persons.Pharmacological management of persistent pain in older persons.J Am Geriatr Soc.2009;57(8):1331–1346.
- , , , , .The rate of NSAID‐induced endoscopic ulcers increases linearly but not exponentially with age: a pooled analysis of 12 randomised trials.Ann Rheum Dis.2007;66(3):417–418.
- , , , et al.Prevalence, clinical features and avoidability of adverse drug reactions as cause of admission to a geriatric unit: a prospective study of 1756 patients.Drug Saf.2008;31(6):545–556.
- , , , et al.Adverse drug events in high risk older outpatients.J Am Geriatr Soc.1997;45(8):945–948.
- , , , , , .Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts.Arch Intern Med.2003;163(22):2716–2724.
- , , , .Medication use leading to emergency department visits for adverse drug events in older adults.Ann Intern Med.2007;147(11):755–765.
- , .The patient who falls: “It's always a trade‐off.”JAMA.2010;303(3):258–266.
- , , .Hospital discharge information and older patients: do they get what they need?J Hosp Med.2007;2(5):291–296.
- , , .Functional health literacy and understanding of medications at discharge.Mayo Clin Proc.2008;83(5):554–548.
- , , , .The care transitions intervention: results of a randomized controlled trial.Arch Intern Med.2006;166(17):1822–1828.
- , , , , , .Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial.J Am Geriatr Soc.2004;52(5):675–684.
- , , , .The impact of follow‐up telephone calls to patients after hospitalization.Am J Med.2001;111(9B):26S‐30S.
- , , , et al.A quality improvement intervention to facilitate the transition of older adults from three hospitals back to their homes.J Am GeriatrSoc.2009;57(9):1540–1546.
- , , , et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Intern Med.2009;150(3):178–187.
- , , , et al.Problems after discharge and understanding of communication with their primary care physicians among hospitalized seniors: a mixed methods study.J Hosp Med.2010;5(7):385–391.
- , .What matters to seriously ill older persons making end‐of‐life treatment decisions? A qualitative study.J Palliat Med.2003;6(2):237–244.
- , , .End‐of‐life decision making: a qualitative study of elderly individuals.J Gen Intern Med.2000;15(9):620–625.
- , , , et al.Patient age and decisions to withhold life‐sustaining treatments from seriously ill, hospitalized adults. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment.Ann Intern Med.1999;130(2):116–125.
- .Clinical practice. Assessment of patients' competence to consent to treatment.N Engl J Med.2007;357(18):1834–1840.
- , , , , .The Mini‐Cog: a cognitive “vital signs” measure for dementia screening in multi‐lingual elderly.Int J Geriatr Psychiatry.2000;15(11):1021–1027.
- , , , .Growth in the care of older patients by hospitalists in the United States.N Engl J Med.2009;360(11):1102–1112.
- , , , , , .Continuity of outpatient and inpatient care by primary care physicians for hospitalized older adults.JAMA.2009;301(16):1671–1680.
- , , .Is there a geriatrician in the house? Geriatric care approaches in hospitalist programs.J Hosp Med.2006;1(1):29–35.
- .Care of hospitalized older patients: opportunities for hospital‐based physicians.J Hosp Med.2006;1(1):42–47.
- , .The top 10 things nephrologists wish every primary care physician knew.Mayo Clin Proc.2009;84(2):180–186.
- .What is a geriatric syndrome anyway?J Am Geriatr Soc.2003;51(4):574–576.
- , , , .Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept.J Am Geriatr Soc.2007;55(5):780–791.
- , , .Some considerations regarding geriatric syndromes.Ann Intern Med.2001;135(12):1095.
- , , , et al.Impact and recognition of cognitive impairment among hospitalized elders.J Hosp Med.2010;5(2):69–75.
- , , , , , .A longitudinal analysis of total 3‐year healthcare costs for older adults who experience a fall requiring medical care.J Am Geriatr Soc.2010;58(5):853–860.
- , , , et al.A multicomponent intervention to prevent delirium in hospitalized older patients.N Engl J Med.1999;340(9):669–676.
- , , , .Shared risk factors for falls, incontinence, and functional dependence. Unifying the approach to geriatric syndromes.JAMA.1995;273(17):1348–1353.
- , , , et al.Strategies to prevent falls and fractures in hospitals and care homes and effect of cognitive impairment: systematic review and meta‐analyses.BMJ.2007;334(7584):82.
- , , , et al.Interventions for preventing falls in acute‐ and chronic‐care hospitals: a systematic review and meta‐analysis.J Am Geriatr Soc.2008;56(1):29–36.
- , , , et al.Postoperative delirium in the elderly: risk factors and outcomes.Ann Surg.2009;249(1):173–178.
- , , , et al.A controlled trial of inpatient and outpatient geriatric evaluation and management.N Engl J Med.2002;346(12):905–912.
- , , , et al.Risk factors for preoperative and postoperative delirium in elderly patients with hip fracture.J Am Geriatr Soc.2009;57(8):1354‐1361.
- , , , , , .Risk factors for delirium in intensive care patients: a prospective cohort study.Crit Care.2009;13(3):R77.
- , , , .The Mini‐Cog as a screen for dementia: validation in a population‐based sample.J Am Geriatr Soc.2003;51(10):1451–1454.
- , , , , .Improving identification of cognitive impairment in primary care.Int J Geriatr Psychiatry.2006;21(4):349–355.
- , , , et al.Simple cognitive testing (Mini‐Cog) predicts inhospital delirium in the elderly.J Am Geriatr Soc.2007;55(2):314–316.
- , , , .Short Portable Mental Status Questionnaire as a screening test for dementia and delirium among the elderly.J Am Geriatr Soc.1987;35(5):412–416.
- , , .“Mini‐mental state.” A practical method for grading the cognitive state of patients for the clinician.J Psychiatr Res.1975;12(3):189–198.
- , , , et al.Development and validation of a brief cognitive assessment tool: the Sweet 16.Arch Intern Med.2010. [Epub ahead of Print].
- , , , et al.Interventions for preventing falls in older people in nursing care facilities and hospitals.Cochrane Database Syst Rev.2010;(1):CD005465.
- , , , et al.Fall prevention in acute care hospitals: a randomized trial.JAMA.2010;304(17):1912–1918.
- , , , et al.Vitamin D supplementation improves neuromuscular function in older people who fall.Age Ageing.2004;33(6):589–595.
- , , , et al.Effect of vitamin D on falls: a meta‐analysis.JAMA.2004;291(16):1999–2006.
- , et al.Fall prevention with supplemental and active forms of vitamin D: a meta‐analysis of randomised controlled trials.BMJ.2009;339:b3692.
- .Hazards of hospitalization of the elderly.Ann Intern Med.1993;118(3):219–223.
- , , , .Hospitalization, restricted activity, and the development of disability among older persons.JAMA.2004;292(17):2115–2124.
- , , , et al.Recovery of activities of daily living in older adults after hospitalization for acute medical illness.J Am Geriatr Soc.2008;56(12):2171–2179.
- , , , et al.Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age.J Am Geriatr Soc.2003;51(4):451–458.
- , , .New walking dependence associated with hospitalization for acute medical illness: incidence and significance.J Gerontol A Biol Sci Med Sci.1998;53(4):M307–M312.
- , , , .Hazards of hospitalization: residence prior to admission predicts outcomes.Gerontologist.2008;48(4):537–541.
- , , , , , et al.A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients.N Engl J Med.1995;332(20):1338–1344.
- , .Exercise for acutely hospitalised older medical inpatients.Cochrane Database Syst Rev.2007;(1):CD005955.
- , , .Occurrence and outcome of delirium in medical in‐patients: a systematic literature review.Age Ageing.2006;35(4):350–364.
- , , .A prospective study of delirium in hospitalized elderly.JAMA.1990;263(8):1097–1101.
- , , , , .Delirium predicts 12‐month mortality.Arch Intern Med.2002;162(4):457–463.
- , , , , .The course of delirium in older medical inpatients: a prospective study.J Gen Intern Med.2003;18(9):696–704.
- , , , .Does delirium increase hospital stay?J Am Geriatr Soc.2003;51(11):1539–1546.
- , , , .The Confusion Assessment Method: a systematic review of current usage.J Am Geriatr Soc.2008;56(5):823–830.
- .Delirium in older persons.N Engl J Med.2006;354(11):1157–1165.
- , , , et al.Pharmacological management of delirium in hospitalized adults—a systematic evidence review.J Gen Intern Med.2009;24(7):848‐853.
- , , .Safety and efficacy of physical restraints for the elderly. Review of the evidence.Can Fam Physician.1996;42:2402–2409.
- , , .Treating nondementia illnesses in patients with dementia.JAMA.2000;283(24):3230–3235.
- , , , , , .Survival in Alzheimer disease: a multiethnic, population‐based study of incident cases.Neurology.2008;71(19):1489–1495.
- , , , et al.Survival after initial diagnosis of Alzheimer disease.Ann Intern Med.2004;140(7):501–509.
- , .Mortality from pneumonia and hip fractures in patients with advanced dementia.JAMA.2000;284(19):2447–2448.
- .Rethinking the role of tube feeding in patients with advanced dementia.N Engl J Med.2000;342(3):206–210.
- Society of Hospital Medicine. BOOSTing Care Transitions Resource Room. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_CareTransitions/CT_Home.cfm. Accessed January 25,2011.
- , , .Enteral tube feeding for older people with advanced dementia.Cochrane Database Syst Rev.2009;(2):CD007209.
- .A 93‐year‐old man with advanced dementia and eating problems.JAMA.2007;298(21):2527–2536.
- , , .Patient safety in geriatrics: a call for action.J Gerontol A Biol Sci Med Sci.2003;58(9):M813–M819.
- , , .Preventable medical injuries in older patients.Arch Intern Med.2000;160(18):2717–2728.
- , , , et al.Iatrogenic complications in high‐risk, elderly patients.Arch Intern Med.1992;152(10):2074–2080.
- , , , et al.The nature of adverse events in hospitalized patients. Results of the Harvard Medical Practice Study II.N Engl J Med.1991.
- , , , , et al.Nosocomial infections: decade‐specific risk.Infect Control.1983;4(3):145–147.
- , , , , , .A quality‐of‐care analysis of cascade iatrogenesis in frail elderly hospital patients.QRB Qual Rev Bull.1993;19(6):199‐2.
- American Geriatrics Society Panel on the Pharmacological Management of Persistent Pain in Older Persons.Pharmacological management of persistent pain in older persons.J Am Geriatr Soc.2009;57(8):1331–1346.
- , , , , .The rate of NSAID‐induced endoscopic ulcers increases linearly but not exponentially with age: a pooled analysis of 12 randomised trials.Ann Rheum Dis.2007;66(3):417–418.
- , , , et al.Prevalence, clinical features and avoidability of adverse drug reactions as cause of admission to a geriatric unit: a prospective study of 1756 patients.Drug Saf.2008;31(6):545–556.
- , , , et al.Adverse drug events in high risk older outpatients.J Am Geriatr Soc.1997;45(8):945–948.
- , , , , , .Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts.Arch Intern Med.2003;163(22):2716–2724.
- , , , .Medication use leading to emergency department visits for adverse drug events in older adults.Ann Intern Med.2007;147(11):755–765.
- , .The patient who falls: “It's always a trade‐off.”JAMA.2010;303(3):258–266.
- , , .Hospital discharge information and older patients: do they get what they need?J Hosp Med.2007;2(5):291–296.
- , , .Functional health literacy and understanding of medications at discharge.Mayo Clin Proc.2008;83(5):554–548.
- , , , .The care transitions intervention: results of a randomized controlled trial.Arch Intern Med.2006;166(17):1822–1828.
- , , , , , .Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial.J Am Geriatr Soc.2004;52(5):675–684.
- , , , .The impact of follow‐up telephone calls to patients after hospitalization.Am J Med.2001;111(9B):26S‐30S.
- , , , et al.A quality improvement intervention to facilitate the transition of older adults from three hospitals back to their homes.J Am GeriatrSoc.2009;57(9):1540–1546.
- , , , et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Intern Med.2009;150(3):178–187.
- , , , et al.Problems after discharge and understanding of communication with their primary care physicians among hospitalized seniors: a mixed methods study.J Hosp Med.2010;5(7):385–391.
- , .What matters to seriously ill older persons making end‐of‐life treatment decisions? A qualitative study.J Palliat Med.2003;6(2):237–244.
- , , .End‐of‐life decision making: a qualitative study of elderly individuals.J Gen Intern Med.2000;15(9):620–625.
- , , , et al.Patient age and decisions to withhold life‐sustaining treatments from seriously ill, hospitalized adults. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment.Ann Intern Med.1999;130(2):116–125.
- .Clinical practice. Assessment of patients' competence to consent to treatment.N Engl J Med.2007;357(18):1834–1840.
- , , , , .The Mini‐Cog: a cognitive “vital signs” measure for dementia screening in multi‐lingual elderly.Int J Geriatr Psychiatry.2000;15(11):1021–1027.