User login
Heart Failure in the Emergency Department
Patients with heart failure (HF) present daily to busy EDs. An estimated 6.5 million Americans are living with this diagnosis, and the number is predicted to grow to 8 million by 2023.1 Most HF patients (82.1%) who present to EDs are hospitalized, while a selected minority are either managed in the ED and discharged (11.6%) or managed in observation units (OU) (6.3%).2 The prognosis after HF is initially diagnosed is poor, with a 5-year mortality of 50%,3 and after a single HF hospitalization, 29% will die within 1 year.4
One-third of the total Medicare budget is spent on HF, despite the fact that HF represents only 10.5% of the Medicare population.2 Up to 80% of HF costs are for hospitalizations, which cost an average of $11,840 per inpatient admission.5,6 The high costs are due to an average length of stay (LOS) of 5.2 days7 (Table 1).
Adding to hospital costs is the degree of “reactivism,” with approximately 20% of patients discharged from the ED returning within 2 weeks, of whom nearly 50% will be hospitalized.11 Following HF hospitalization and discharge, the 30-day readmission rate is 26.2%,2 increasing to 36% by 90 days.12 The Centers for Medicare & Medicaid Services (CMS) has incentivized hospitals and providers to reduce admissions, but penalize hospitals that do not. Overall, CMS will reduce payments by up to 3% to hospitals with excess readmissions for select conditions, including HF.13
Causes of Heart Failure
Heart failure represents a final common pathway, which in the United States is most often due to coronary artery disease (CAD). Many types of pathology ultimately result in left ventricular (LV) dysfunction, and much of its rising prevalence is a result of the success we now have in managing historically fatal cardiovascular (CV) conditions. These include hypertension, diabetes mellitus (DM), CAD, and valvular and other CV structural conditions.
Heart failure is caused by either a dilated ventricle with a reduced ejection fraction (HFrEF) and inability to eject volume, or a stiffened ventricle with a preserved EF (HFpEF) that is unable to receive increased venous return. Both conditions acutely decompensate pulmonary congestion. A preserved EF is defined as an EF at or greater than 50%, whereas a reduced EF is at or less than 40%, with the 41% to 49% range considered as borderline preserved EF.3
While there are important differences in the treatment of chronic and subacute HF, driven by the EF, the effect of EF on early decision-making and treatment in the ED is negligible: Although the probability of HFpEF increases with increasing initial ED systolic blood pressure (SBP), clinical presentation and treatment in the ED are initially identical—regardless of the EF.
Noninvasive continuous transcutaneous hemodynamic monitoring is available for ED use, and may provide further insight into the underlying pathophysiology. A study of 127 acute heart failure (AHF) ED patients identified three hemodynamic AHF phenotypes. These include normal cardiac index (CI) and systemic vascular resistance index (SVRI), low CI and SVRI, and low CI and elevated SVRI.14 While it is attractive to suggest therapeutic interventions based on these measurements, outcome data are lacking.
Presentation
The most common ED presentation of patients suffering from AHF is dyspnea secondary to volume overload, or as the result of acute hypertension with relatively less volume overload. However, regardless of the cause of dyspnea, it is not only the most common resulting complaint, but one that requires immediate treatment. Ultimately, 59% of all HF admissions are attributed to volume overload and dyspnea (Figure 1).15
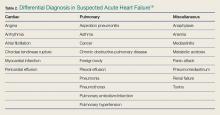
Heart failure can also present in a more protean manner, with cough, fatigue, and edema, as well as more subtle symptoms predominating and resulting in a complicated differential diagnosis (Table 2).16
Because HF is a disease that most significantly affects older patients who frequently have concomitant morbidities (eg, myocardial ischemia, chronic obstructive pulmonary disease [COPD] exacerbation, uncontrolled DM), other less clinically obvious disease presentations may actually be the cause of the AHF exacerbation.
Diagnosis
A focused history and physical examination that is part of all ED evaluations should be expedited whenever there is evidence of hemodynamic instability or respiratory compromise. An early working diagnosis is essential to avoid a delay in appropriate treatment, which is associated with increased mortality.
When HF is likely, the potential etiology and precipitants for decompensation must be considered. This list is long, but medication noncompliance and dietary indiscretion are the most common causes.
Symptoms and Prior History of HF
The classic symptoms for AHF include dyspnea at rest or exertion, and orthopnea, both of which unfortunately have poor sensitivity and specificity for AHF. As an isolated symptom, dyspnea is of marginal diagnostic utility (sensitivity and specificity for an HF diagnosis is 56% and 53%, respectively), and orthopnea is only slightly better (sensitivity and specificity 77% and 50%, respectively). A prior HF diagnosis makes repeat presentations much more likely (sensitivity and specificity 60% and 90%, respectively).17
Physical Examination
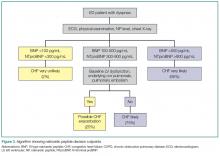
Simple observation and a directed examination can rapidly point to the diagnosis (Figure 2).
Electrocardiography
Because CAD is one of the most common underlying AHF etiologies, an electrocardiogram (ECG) should always be obtained early for a patient presenting with potential AHF. Although the ECG does not usually contribute to ED management, the identification of new ST-segment changes or a malignant arrhythmia will guide critical management decisions.
Imaging Studies
Chest X-ray Imaging. A chest X-ray (CXR) study must be considered early when a patient presents with signs and symptoms suggestive of AHF. Although the classic findings of HF (eg, Kerley B lines [short horizontal lines perpendicular to the pleural surface],18 interstitial congestion, pulmonary effusion) can lag behind the clinical presentation, and also be nondiagnostic in the setting of mild HF, the CXR is an effective aid in identifying other causes of dyspnea such as pneumonia. Ultimately, the utility of the CXR for diagnosis is similar to that of the history and physical examination in that it will be diagnostic when positive but cannot exclude AHF if normal.
Ultrasound. Because it is fast, inexpensive, noninvasive, and readily available in the ED, ultrasound is frequently used to evaluate potential HF patients. Several studies have demonstrated that the presence of B lines in two or more regions is specific for AHF (specificity 75%-100%), although the sensitivity may be limited (40%-91%).19-21 The presence of inferior vena cava (IVC) dilation is also associated with adverse outcomes.22 In 80 patients hospitalized with acute decompensated HF (ADHF), a dilated IVC (≥1.9 cm) at admission was associated with higher 90-day mortality (25.4% vs 3.4%, P = 0.009).23 These findings may be considered in groups: In an evaluation of the combination of LV EF, IVC collapsibility, and B lines for an HF diagnosis, the combination of all three had a poor sensitivity (36%) but an excellent specificity (100%), and any two of the three had a specificity of at least 93%.24
Laboratory Evaluation
Myocardial Strain: BNP/NTproBNP. Natriuretic peptides (NPs) are not AHF-specific, but rather they are synthesized and released by the myocardium in the setting of myocardial pressure or volume stress. They are manufactured as preproBNP, then enzymatically cleaved into the active BNP and the inactive fragment N-terminal proBNP (NTproBNP). The predominant hormonal effects of BNP are vasodilation and natriuresis, as well as antagonism of the hormones associated with sodium retention (aldosterone) and vasoconstriction (endothelin, norepinephrine).
As AHF results in myocardial stress, NP elevation provides diagnostic and prognostic information. Clinical judgment supported by a BNP greater than 100 pg/mL is a better predictor of AHF than clinical judgment alone (accuracy 81% vs 74%, respectively).25 While low levels (BNP <100 pg/mL or NTproBNP <300 pg/mL) reliably exclude the diagnosis of HF (sensitivities >95%), higher levels (BNP >500 pg/mL, NTproBNP >900 pg/mL) are useful as “rule-in” markers, with specificity greater than 95%. The NTproBNP also requires adjustment for patients older than age 75 years, with a higher level (>1,800 pg/mL) to rule-in HF. The NP grey zone (BNP 100-500 pg/mL, NTproBNP 300-900 pg/mL)requires additional testing for accurate diagnoses (Figure 3).25-29
There are several confounders to the interpretation of NP results: NPs are negatively confounded by the presence of obesity, resulting in a lowering of the value as compared to the clinical presentation.Thus, the measured BNP level should be doubled if the patient’s body mass index exceeds 35 kg/m2.30 Secondly, because NP metabolism is partially renal dependent, elevated levels may not reflect AHF in the presence of renal failure. If the estimated glomerular filtration rate is less than 60 mL/min, measured BNP levels should be halved.31
AHF vs Myocardial Ischemia: Troponin Levels. Large registry data using contemporary troponin assays clearly identify the association between elevated troponin levels (>99th percentile in a healthy population) and increased short-term risk. With the US Food and Drug Association (FDA) approval of a high-sensitivity troponin (hs-cTnT) assay, a greater frequency of elevated cardiac troponin T (cTnT) and cardiac troponin I (cTnl) will be identified in AHF patients in the ED.
In one retrospective study of 4,705 AHF patients in the ED, hs-cTnT were elevated in 48.4% of cases (25.3% in cTnI, 37.9% in cTnT, and 82.2% in hs-cTnT). Although 1-year mortality was higher in those with elevated troponin (adjusted heart rate [HR] 1.61; CI 95% 1.38-1.88), elevated troponin was not associated with 30-day revisits to the ED (1.01; 0.87-1.19) and high sensitive elevations less than double the reference value had no impact on outcomes.32 Thus, in terms of management of AHF in the ED, slightly elevated stable serial troponins are more consistent with underlying HF, and should be managed as such. This is not true of rising/falling troponin levels, which should still engender concern for underlying myocardial ischemia and a different management pathway.
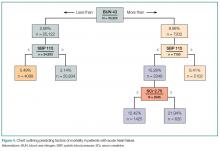
Renal function. Comprised renal function is an important predictor of AHF outcome. Large registry data from hospitalized HF patients demonstrate that a presenting blood urea nitrogen level greater than 43 mg/dL is one of the most important predictors of increased acute mortality,33 and levels below 30 mg/dL identify a cohort likely to be successfully managed in an observation environment.34 Creatinine is a helpful lagging indicator of mortality, with higher levels (>2.75 mg/dL) associated with increased short-term adverse outcomes and decreased therapeutic responsiveness (Figure 4).
For patients presenting with ADHF, a newer test recently approved by the FDA uses the product of the urine markers tissue inhibitor of metalloproteinase-2 and insulin-like growth factor-binding protein 7, to generate a score predictive of acute kidney injury.35 While promising, no studies of ED outcomes are currently available.
Volume Assessment
Objective volume assessment is useful for diagnosis and prognosis in AHF. Bioimpedance vector analysis (BIVA) is a rapid, inexpensive, noninvasive technique that measures total body water by placing a pair of electrodes on the wrist and ipsilateral ankle. The BIVA measurements have strong correlations with the gold standard volume-assessment technique of deuterium dilution (r > 0.99).36 In HF, BIVA can assess volume depletion37 and overload,38 and identifies differences in hydration status between 90-day survivors and non-survivors (P < 0.01).39
Used in combination with BNP, one prospective study of 292 dyspneic patients found that, while BIVA was a strong predictor of AHF (c-statistic 0.93, P = 0.016), the most accurate volume status determination was the combination of both (c-statistic, 0.99; P = 0.005), for which the combined accuracy exceeded either alone.40 Finally, in 166 hospitalized HF patients discharged by BNP and BIVA parameters, vs 149 discharged based on clinical impressions, those assessed with BNP and BIVA had lower 6-month readmissions (23% vs 35%, P = 0.02) and overall cost of care.41
Combination Technologies
Obviously, EPs may consider multiple technologies to arrive at an accurate diagnosis. One prospective evaluation enrolled 236 patients to determine the diagnostic accuracy for AHF in the ED and reported lung ultrasound, CXR, and NTproBNP had a sensitivity of 57.7% and 88.0%, 74.5% and 86.3%, and a specificity of 97.6% and 28.0%. The best overall combination was the CXR with lung ultrasound (sensitivity 84.7%, specificity 77.7%).42
Another prospective study evaluated IVC diameter, bioelectrical impedance analysis (BIA), and NTproBNP in 96 elderly patients. ADHF patients had higher IVC diameters and lower collapsibility index, lower resistance and reactance, and higher NTproBNP levels. While all had high and statistically similar C-statistics (range 0.8 to 0.9) for an ADHF diagnosis, they concluded that IVC ultrasonography and BIA were as useful as NT-proBNP for diagnosing ADHF. 24
Diagnostic Scoring Systems
A scoring system has been proposed to improve diagnosis in the ED. Unfortunately, the value over clinical impression has not been clearly proven, though one randomized, controlled trial did not show statistically significant improvement in diagnostic accuracy when compared to standard care (77% vs 74%, P = 0.77).43
Differential Diagnosis
The differential diagnosis for acute dyspnea is long and potentially arcane. Efforts should focus on excluding non-HF causes of dyspnea, while considering the high risk of alternative etiologies for signs and symptoms. These include asthma, COPD, pneumonia, and pulmonary embolism, which may represent the primary pathologies in a patient with a history of HF, or be the cause of a HF exacerbation. Additional causes of noncardiogenic pulmonary edema should also be considered (eg, acute respiratory distress syndrome, toxins, etc). Acute coronary syndrome and dyspnea may be angina equivalents—one important consideration.
Treatment and Management
Airway Management
Treatment of CH in the ED must always start with an immediate airway evaluation, with the possible need for endotracheal intubation preceding all diagnostic or other management considerations. Intubation is a decision most successfully based on physician clinical assessment, including oxygen (O2) selection rather than waiting for the results of objective measures such as arterial blood gas analysis.
Oxygen
Supplemental O2 should be administered to maintain an O2 saturation above 95%, but obviously is unnecessary in the absence of hypoxia.
Noninvasive Ventilation
Two kinds of noninvasive ventilation (NIV) are available, continuous positive airway pressure and bilevel positive airway pressure ventilation. The physiological differences between these types of NIV have little bearing on ED treatment.
Noninvasive ventilation has not been clearly shown to provide long-term mortality benefit. Large registry data44 report that outcomes are no worse than the alternative of endotracheal intubation, while multiple systematic reviews,45,46meta-analysis,47and Cochrane reviews48,49have established NIV as an acute pulmonary edema intervention that provides reductions in hospital mortality (numbers needed to treat [NNT] 13) and intubation (NNT 8), the prospective randomized C3PO (Congenital Cardiac Catheterization Project on Outcomes) trial50 failed to demonstrate any mortality reduction.
In patients with severe respiratory distress, NIV is a reasonable strategy during the aggressive administration of medical therapy in an attempt to avoid endotracheal intubation. However, NIV is not a stand-alone therapy and though its use may obviate the need for immediate intubation, its implementation should not be considered definitive management.
Correction of Abnormal Vital Signs: Abnormal SBP
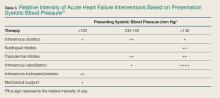
Vital signs are an important determinant of therapy, driving treatment strategies. Interventions for HF are based on the patient’s SBP, in particular correction of symptomatic hypotension and hypertensive HF (Table 3).51
Symptomatic Hypotension. The presence of symptomatic hypotension is an extremely poor prognostic finding in AHF. Inotrope therapy may be considered, but it does not reduce mortality except as a bridge to mechanical interventions (LV assist device or transplant).52-54 Temporary inotropic support is recommended for cardiogenic shock to maintain systemic perfusion and prevent end organ damage.3 The inotropic support includes administration of dopamine, dobutamine, or milrinone, though none have been proven to be superior over the other. The lowest possible dose of the selected inotrope should be used to limit arrhythmogenic effects. Inotropic agents should not be used in the absence of severe systolic dysfunction, or low BP, or impaired perfusion, or evidence of significantly decreased cardiac output.
Hypertensive Heart Failure. Defined as the rapid onset of pulmonary congestion with an SBP greater than 140 mm Hg, and commonly greater than 160 mm Hg, these patients may have profound dyspnea, requiring endotracheal intubation. However, in this situation, aggressive vasodilation is typically rapidly effective. Overall, patients presenting with an elevated SBP have lower rates of in-hospital mortality, 30-day myocardial infarction (MI), death, or rehospitalization, and a greater likelihood of discharge within 24 hours—as long as the elevated SBP is aggressively and rapidly treated.
Pharmacological Therapy
Pharmacological management is the mainstay for treating HF. No other acute therapy (eg, NIV) has demonstrated a morality benefit (See Table 4 for specific dose and administration strategies).55 The time to initiate pharmacological therapy and whether an aggressive approach is indicated must be based on the severity of the clinical symptoms and objective risk stratification measures (eg, NP, troponin levels).
Furosemide. Except for hypertensive HF—in which case BP lowering is the most important goal—diuretics are a mainstay of AHF treatment, and consensus guidelines provide a class I recommendation for their use.3 The DOSE (Diuretic Strategies in Patients with ADHF) trial56 prospectively evaluated diuretics in 308 hospitalized AHF patients and found no outcome differences in administration route (bolus or continuous infusion) or dose (high vs low dose). This study reported trends toward greater improvement with higher furosemide dosing, as well as greater diuresis, but at a cost of transient worsening of renal function.
In general, diuretics should be administered in an intravenous (IV) dose equal to 1 to 2.5 times the patient’s usual daily oral dose. For patients who are diuretic-naïve, a dose of 40 mg IV furosemide or 1 mg IV bumetanide, with subsequent dosing titrated to urine output, is recommended.
Vasodilators. In patients with both AHF and even mildly elevated BP, vasodilators can be extremely effective in achieving symptom improvement. The choice of vasodilator, and how aggressive to increase dosing, depends upon symptom severity. The purpose of vasodilators is to lower BP and therefore, should not be used in the setting of hypotension or signs of hypoperfusion. Flow-limiting, preload-dependent CV states (eg, right ventricular infarction) increase the risk of hypotension, and are relative contraindications to the use of vasodilators. For patients who are severely dyspneic and with critical presentations, the emergency physician (EP) should preclude a detailed history and examination to initiate immediate therapy with short-acting agents that can be terminated rapidly in the case of an adverse event (eg, unexpected hypotension) are preferred.
Nitroglycerin. Nitroglycerin is the vasodilation agent of choice for hypertensive AHF. It is a short-acting, rapid-onset, venous and arterial dilator that decreases BP by preload reduction, and by afterload reduction in higher doses. Nitroglycerin has coronary vasodilatory effects associated with decreased ischemia, but should be avoided in patients taking phosphodiesterase inhibitors.55 Its most common side effect is headache, and hypotension occurs in about 3.5% of patients.57
Commonly given as a continuous infusion at IV doses up to 400 mcg/min, nitroglycerin may be associated with higher costs and longer LOS.58 Some authors suggest that bolus nitroglycerin therapy may be superior: In a retrospective study of 395 patients, an IV bolus of nitroglycerin 0.5 mg was superior to both an infusion, or a combination of bolus and infusion, as demonstrated by lower rates of ICU admission (48% vs 67% and 79%, respectively, P = 0.006) and shorter hospital stays (4.4 vs 6.3 and 7.3 days, respectively, P = 0.01). In all cohorts, adverse event rates were similar for hypotension, troponin elevation, and creatinine increase over 48 hours.59 Nitroprusside. Nitroprusside is a potent arterial and venous dilator that causes rapid decrease in BP and LV-filling pressures. It is usually considered more effective than nitroglycerin, despite a small study showing similar hemodynamic responses.60
Initial dosing of nitroprusside starts at 0.3 µg/kg/min IV, and is increased every 5 minutes to a maximum of 10 mcg/kg/min, based on BP and clinical response. The most common acute complication of nitroprusside infusions is hypotension. Cyanide toxicity may occur with prolonged use, high doses, or in patients with renal failure.55
Nesiritide. Exogenously administered, the B-type NP nesiritide is effective in lowering BP and improving dyspnea in AHF,55 although large prospective studies showed it had little long-term advantage over standard care.61 In a small, randomized, controlled trial, nesiritide reduced 30-day revisit LOS when given in an OU.62 The 22-minute half-life of nesiritide is longer than that of the nitrates, and its side effect is predominately hypotension, which occurs at rates similar to those of other vasodilators.55
Angiotensin Converting Enzyme Inhibitors. Because angiotensin converting enzyme inhibitors (ACEIs) have chronic mortality reduction benefits, their use in the acute setting is theoretically attractive, however, this has been poorly proven in AHF ED patients. In a retrospective review of 103 patients with elevated NTproBNP levels receiving bolus IV enalaprilat within 3 hours of presentation, the mean SBP decreased by 30 mm Hg, with only 2% of patients developing hypotension.63 However, with the longer half-life of ACEIs, if hypotension occurs, the potential for a prolonged BP-lowering effect exists.
Calcium Channel Blockers. Clevidipine and nicardipine are rapidly acting IV calcium channel blockers that lower BP by selective arteriolar vasodilation and increased cardiac output as vascular resistance declines.55 Because these agents have no negative inotropic or chronotropic effects, they may be beneficial in hypertensive AHF. In an open-label trial of 104 hypertensive AHF patients, clevidipine was more effective than standard care for the rapid control of BP and relief of dyspnea.64
Morphine. Large registry analyses have demonstrated potential harm with the routine use of morphine,65 as do recent propensity score matched analyses.66 Until there are studies demonstrating benefit, the use of morphine at present should be reserved for palliative care.
Time to Treatment
Although a randomized controlled trial on the importance of time to treatment of AHF is unlikely to ever be completed, data suggest that, as in the case of MI, delayed AHF therapy is associated with adverse outcomes. In a study of 499 suspected AHF patients transferred by ambulance, patients randomized to immediate therapy vs those whose therapy was not initiated until hospital arrival (mean delay of 36 minutes), had a 251% increase in survival (P < 0.01).67
Furthermore, the delayed administration of vasoactive agents, defined as medication administered to alter hemodynamics (eg, dobutamine, dopamine, nitroglycerin, nesiritide) is also associated with harm,68 and registry studies demonstrate increased death rates (n = 35,700).69 Finally, another registry (n = 14,900) study demonstrated early IV furosemide is associated with decreased mortality.70 This latter finding was also validated in a prospective observational cohort study (mortality 2.3 vs 6.0 in early vs delayed therapy groups, respectively).71
Patient Disposition
One of the unique features of emergency medicine is the need to determine, with very limited information and time, a patient’s very short-term clinical trajectory. Few physicians are required to have greater accuracy with less information or time than do EPs. Several studies report objective data points and risk scores to assist in this task, but none has been universally adopted, reflecting the challenge of applying population data to individuals.
Short-term Prognosis
In 1,638 patients evaluated for 14-day outcomes, an HR lower than 50% maximal HR (MHR), and an SBP greater than 140 mm Hg were associated with the lowest rate of serious adverse events (SAEs) (6%) and hospitalization (38%).72 An MHR over 75% was associated with the highest SAE rate, although SAEs decreased as SBP increased (30%, 24%, and 21% with SBPs < 120 mm Hg, 120-140 mm Hg, and > 140 mm Hg, respectively).72
Risk Scores
In a prospective, observational cohort study of 1,100 ED patients, the Ottawa Heart Failure Risk Scale, combined with NTproBNP values, had a sensitivity of 95.8%—at the cost of increasing the admission rate (from 60.8% to 88%)—for serious adverse events (defined as death within 30 days), admission to a monitored unit, intubation, NIV, MI, or relapse resulting in hospital admission within 14 days.73
Observation Unit
Overall, 44% of in-patient HF admissions are for less than 3 days (Table 1),2 supporting the practice of managing selected patients in shorter clinical-care environments than in inpatient units. Further, ED patients presenting with moderate dyspnea require both a diagnosis and an evaluation of their therapeutic response to determine the need for hospitalization. However, evaluating therapeutic response requires more time than is available in the typical ED. Thus, an ED OU offers the following:
(1) The OU provides the EP with a longer evaluation time, and therefore a more accurate disposition may be effected;
(2) Costs are significantly lower in patients managed in an ED OU; and
(3) Patient satisfaction may be improved, as most patients prefer home management over hospitalization.
All three of these opportunities are supported by a number of studies,74-78 with validated entry and exclusion criteria, treatment algorithms and discharge metrics. Most recently, in a registry of hospitals in Spain registry, patients presenting to hospitals that had OUs had a 2.2-day shorter LOS, lower 30-day ED revisit rate, and similar mortality rates compared to those in institutions without OUs—although these beneficial effects occurred at the cost of an 8.9% higher admission rate.79
Patient Education
Intuitively, it would be expected that patient education would reduce return visits, 30-day hospitalizations, and AHF-related mortality. Unfortunately, it has not been demonstrated that patient education results in a consistent benefit at hospital discharge, or in the outpatient environment.80-85
Although AHF education in the ED has been poorly studied, areas that have shown promise are education occurring before ED management (ie, in the ED waiting area) in underinsured patients,86 and during ED care for patients with poor health care literacy.87 As educational interventions are both inexpensive and unlikely to result in harm, their implementation should be considered.
Conclusion
The spectrum of HF is a common presentation in the ED. Because HF generally appears as dyspnea, in a cohort with multiple comorbidities, the diagnosis can be challenging. This is complicated by the fact that patients with severe presentations may require life-saving interventions long before a clinical evaluation is completed (or even initiated). The skill of the EP, and his or her ability to improve the clinical condition before intubation is required, will determine the patient’s trajectory. Conversely, as a chronic condition, HF may present with moderate symptoms for which a short diuretic “tune-up” in an observation environment may be appropriate.
How these decisions are made will depend upon the local environment, the availability of outpatient resources, and individual patient choices. There are few chronic diseases that are more complex, are seen more often in the ED, or that require more skill and finesse in management.
1. Benjamin EJ, Blaha MJ, Chiuve SE, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation. 2017;135(10):e146-e603.
2. Fitch KV, Engel T, Lauet J. The cost burden of worsening heart failure in the Medicare fee for service population: an actuarial analysis. Milliman Web site. 2017. http://www.milliman.com/insight/2017/The-cost-burden-of-worsening-heart-failure-in-the-Medicare-fee-for-service-population-An-actuarial-analysis/ Published April 3, 2017. Accessed June 1, 2017.
3. Yancy CW, Jessup M, Bozkurt B, et al; American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2013. J Am Coll Cardiol. 2013;62(16):e147-e239. doi:10.1016/j.jacc.2013.05.019.
4. Chen J, Normand SL, Wang Y, Krumholz HM. National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries, 1998-2008. JAMA. 2011;306(15):1669-1678. doi:10.1001/jama.2011.1474.
5. Heidenreich PA, Albert NM, Allen LA, et al; American Heart Association Advocacy Coordinating Committee; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular Radiology and Intervention; Council on Clinical Cardiology; Council on Epidemiology and Prevention; Stroke Council. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6(3):606-619. doi:10.1161/HHF.0b013e318291329a.
6. Dunlay SM, Shah ND, Shi Q, et al. Lifetime costs of medical care after heart failure diagnosis. Circ Cardiovasc Qual Outcomes. 2011;4(1):68-75. doi:10.1161/CIRCOUTCOMES.110.957225.
7. HCUP National Inpatient Sample (NIS); 2014 Agency for Healthcare Research and Quality (AHRQ). HCUPnet Healthcare Cost and Utilization Project. http://bit.ly/2u2ymFA. Published 2014. Accessed July 27, 2017.
8. FY 2017 Final Rule and Correction Notice Tables. CMS 2014 data based on DRGs, Table 5:List of MS-DRGs, Relative Weighting Factors and Geometric and Arithmetic Mean Length of Stay. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/FY2017-IPPS-Final-Rule-Home-Page-Items/FY2017-IPPS-Final-Rule-Tables.html. Published 2017. Accessed August 28, 2017.
9. Hospital Adjusted Expenses per Inpatient Day by Ownership. Kaiser Family Foundation. http://www.kff.org/health-costs/state-indicator/expenses-per-inpatient-day-by-ownership/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. Accessed August 2, 2017
10. Ellison, A. Average cost per inpatient day across 50 states. Becker’s Hospital CFO Report. http://www.beckershospitalreview.com/finance/average-cost-per-inpatient-day-across-50-states-2016.html. Published January 13, 2016. Accessed August 2, 2017
11. Claret PG, Calder LA, Stiell IG, et al. Rates and predictive factors of return to the emergency department following an initial release by the emergency department for acute heart failure. [published online ahead of print April 3, 2017]. CJEM. 1-8. doi:10.1017/cem.2017.14.
12. Yam FK, Lew T, Eraly SA, Lin HW, Hirsch JD, Devor M. Changes in medication regimen complexity and the risk for 90-day hospital readmission and/or emergency department visits in U.S. Veterans with heart failure. Res Social Adm Pharm. 2016;12(5):713-721. doi:10.1016/j.sapharm.2015.10.004.
13. Readmissions Reduction Program. CMS. https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html Updated April 18, 2016. Accessed July 13, 2017.
14. Nowak RM, Reed BP, DiSomma S, et al. Presenting phenotypes of acute heart failure patients in the ED: Identification and implications. Am J Emerg Med. 2017;35(4):536-542. doi:10.1016/j.ajem.2016.12.003.
15. Bennett SJ, Huster GA, Baker SL, et al. Characterization of the precipitants of hospitalization for heart failure decompensation. Am J Crit Care. 1998;7(3):168-174.
16. Kuo DC, Peacock WF. Diagnosing and managing acute heart failure in the emergency department. Clin Exp Emerg Med. 2015;2(3):141-149. eCollection 2015 Sep. doi:10.15441/ceem.15.007.
17. Wang CS, FitzGerald JM, Schulzer M, Mak E, Ayas NT. Does this dyspneic patient in the emergency department have congestive heart failure? JAMA. 2005;294:1944-1956.
18. Koga T, Fujimoto K. Images in clinical medicine. Kerley’s A, B, and C line. N Engl J Med. 2009;360(15):1539. doi:10.1056/NEJMicm0708489.
19. Glöckner E, Christ M, Geier F, et al. Accuracy of point-of-care B-Line lung ultrasound in comparison to NT-ProBNP for screening acute heart failure. Ultrasound Int Open. 2016;2(3):e90-e92. doi:10.1055/s-0042-108343.
20. Bitar Z, Maadarani O, Almerri K. Sonographic chest B-lines anticipate elevated B-type natriuretic peptide level, irrespective of ejection fraction. Ann Intensive Care. 2015;5(1): 56. doi:10.1186/s13613-015-0100-x.
21. Miglioranza MH, Gargani L, Sant’Anna RT, et al. Lung ultrasound for the evaluation of pulmonary congestion in outpatients: a comparison with clinical assessment, natriuretic peptides, and echocardiography. JACC Cardiovasc Imaging. 2013;6(11):1141-1151. doi:10.1016/j.jcmg.2013.08.004.
22. Anderson KL, Jenq KY, Fields JM, Panebianco NL, Dean AJ. Diagnosing heart failure among acutely dyspneic patients with cardiac, inferior vena cava, and lung ultrasonography. Am J Emerg Med. 2013;31(8):1208-1214. doi:10.1016/j.ajem.2013.05.007.
23. Cubo-Romano P, Torres-Macho J, Soni NJ, et al. Admission inferior vena cava measurements are associated with mortality after hospitalization for acute decompensated heart failure. J Hosp Med. 2016;11(11):778-784. doi:10.1002/jhm.2620.
24. Martínez PG, Martínez DM, García JC, Loidi JC. Amino-terminal pro–B-type natriuretic peptide, inferior vena cava ultrasound, and bioelectrical impedance analysis for the diagnosis of acute decompensated CHF. Am J Emerg Med. 2016;34(9): 1817–1822. doi:10.1016/j.ajem.2016.06.043.

25. Maisel AS, Krishnaswamy P, Nowak RM, et al; Breathing Not Properly Multinational Study Investigators. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med. 2002;347(3):161-167.
26. Van Kimmenade RR, Pinto YM, Bayes-Genis A, Lainchbury JG, Richards AM, Januzzi JL Jr. Usefulness of intermediate amino-terminal pro-brain natriuretic peptide concentrations for diagnosis and prognosis of acute heart failure. Am J Cardiol. 2006;98(3):386-390.
27. Moe GW, Howlett J, Januzzi JL, Zowall H; Canadian Multicenter Improved Management of Patients With Congestive Heart Failure (IMPROVE-CHF) Study Investigators. N-terminal pro-B-type natriuretic peptide testing improves the management of patients with suspected acute heart failure: primary results of the Canadian prospective randomized multicenter IMPROVE-CHF study. Circulation. 2007;115(24):3103-3110.
28. Mayo DD, Colletti JE, Kuo DC. Brain natriuretic peptide (BNP) testing in the emergency department. J Emerg Med. 2006;31(2):201-210.
29. Mueller C, Scholer A, Laule-Kilian K, et al. Use of B-type natriuretic peptide in the evaluation and management of acute dyspnea. N Engl J Med. 2004;350(7):647-654.
30. Krauser DG, Lloyd-Jones DM, Chae CU, et al. Effect of body mass index on natriuretic peptide levels in patients with acute congestive heart failure: a ProBNP Investigation of Dyspnea in the Emergency Department (PRIDE) substudy. Am Heart J. 2005;149(4):744-750.
31. McCullough PA, Duc P, Omland T, et al. B-type natriuretic peptide and renal function in the diagnosis of heart failure: an analysis from the Breathing Not Properly Multinational Study. Am J Kidney Dis. 2003;41(3):571-579.
32. Jacob J, Roset A, Miró Ò, et al; ICA-SEMES Research Group. EAHFE - TROPICA2 study. Prognostic value of troponin in patients with acute heart failure treated in Spanish hospital emergency departments. Biomarkers. 2017;22(3-4):337-344. doi:10.1080/1354750X.2016.1265006.
33. Fonarow GC, Adams KF Jr, Abraham WT, et al; ADHERE Scientific Advisory Committee, Study Group, and Investigators. Risk stratification for in-hospital mortality in acutely decompensated heart failure: classification and regression tree analysis. JAMA. 2005;293(5):572-580.
34. Burkhardt J, Peacock WF, Emerman CL. Predictors of emergency department observation unit outcomes. Acad Emerg Med. 2005;12(9):869-874.
35. Schanz M, Shi J, Wasser C, Alscher MD, Kimmel M. Urinary [TIMP-2] × [IGFBP7] for risk prediction of acute kidney injury in decompensated heart failure. Clin Cardiol. 2017;40(7):485-491. doi:10.1002/clc.22683.
36. Kushner RF, Schoeller DA, Fjeld CR, Danford L: Is the impedance index (ht2/R) significant in predicting total body water? Am J Clin Nutr. 1992;56(5): 835-839.
37. Ackland GL, Singh-Ranger D, Fox S, et al. Assessment of preoperative fluid depletion using bioimpedance analysis. Br J Anaesth. 2004;92(1): 134-136.
38. Uszko-Lencer NH, Bothmer F, van Pol PE, Schols AM. Measuring body composition in chronic heart failure: a comparison of methods. Eur J Heart Fail. 2006;8(2): 208-214.
39. Santarelli S, Russo V, Lalle I, et al; GREAT network. Usefulness of combining admission brain natriuretic peptide (BNP) plus hospital discharge bioelectrical impedance vector analysis (BIVA) in predicting 90 days cardiovascular mortality in patients with acute heart failure. Intern Emerg Med. 2017;12(4):445-451. doi:10.1007/s11739-016-1581-9.
40. Parrinello G, Paterna S, Di Pasquale P, et al. The usefulness of bioelectrical impedance analysis in differentiating dyspnea due to decompensated heart failure. J Card Fail. 2008;14(8): 676-686. doi:10.1016/j.cardfail.2008.04.005.
41. Valle R, Aspromonte N, Carbonieri E, et al. Fall in readmission rate for heart failure after implementation of B-type natriuretic peptide testing for discharge decision: a retrospective study. Int J Cardiol. 2008;126(3): 400-406.
42. Sartini S, Frizzi J, Borselli M, et al. Which method is best for an early accurate diagnosis of acute heart failure? Comparison between lung ultrasound, chest X-ray and NT pro-BNP performance: a prospective study. [published online ahead of print July 11, 2016]. Intern Emerg Med. doi:10.1007/s11739-016-1498-3.
43. Steinhart BD, Levy P, Vandenberghe H, et al. A randomized control trial using a validated prediction model for diagnosing acute heart failure in undifferentiated dyspneic emergency department patients-results of the GASP4Ar study. J Card Fail. 2017;23(2):145-152. doi:10.1016/j.cardfail.2016.08.007.
44. Tallman TA, Peacock WF, Emerman CL, et al; ADHERE Registry. Noninvasive ventilation outcomes in 2,430 acute decompensated heart failure patients: an ADHERE registry analysis. Acad EM. 2008;15(4):355–362. doi:10.1111/j.1553-2712.2008.00059.x.
45. Pang D, Keenan SP, Cook DJ, Sibbald WJ. The effect of positive pressure airway support on mortality and the need for intubation in cardiogenic pulmonary edema: a systematic review. Chest. 1998;114(4):1185-1192.
46. Peter JV, Moran JL, Phillips-Hughes J, Graham P, Bersten AD. Effect of non-invasive positive pressure ventilation (NIPPV) on mortality in patients with acute cardiogenic pulmonary oedema: a meta-analysis. Lancet. 2006;367(9517):1155-1163.
47. Weng CL, Zhao YT, Liu QH, et al. Meta-analysis: Noninvasive ventilation in acute cardiogenic pulmonary edema. Ann Intern Med. 2010;152(9):590-600
48. Vital FM, Saconato H, Ladeira MT, et al. Noninvasive positive pressure ventilation (CPAP or bilevel NPPV) for cardiogenic pulmonary edema. Cochrane Database Syst Rev. 2008;(3):CD005351. doi:10.1002/14651858.CD005351.pub2.
49. Vital FM, Ladeira MT, Atallah AN. Non-invasive positive pressure ventilation (CPAP or bilevel NPPV) for cardiogenic pulmonary oedema. Cochrane Database Syst Rev. 2013;(5):CD005351. doi:10.1002/14651858.CD005351.pub3.
50. Gray A, Goodacre S, Seah M, Tilley S. Diuretic, opiate and nitrate use in severe acidotic acute cardiogenic pulmonary oedema: analysis from the 3CPO trial. QJM. 2010;103(8):573-581. doi:10.1093/qjmed/hcq077.
51. Collins SP, Storrow AB, Levy PD, et al. Early management of patients with acute heart failure: state of the art and future directions—a consensus document from the SAEM/HFSA acute heart failure working group. Acad Emerg Med. 2015;22(1):94-112. doi:10.1111/acem.12538.]
52. O’Connor CM, Gattis WA, Uretsky BF, et al. Continuous intravenous dobutamine is associated with an increased risk of death in patients with advanced heart failure: insights from the Flolan International Randomized Survival Trial (FIRST). Am Heart J. 1999;138(1 Pt 1):78-86.
53. Hershberger RE, Nauman D, Walker TL, Dutton D, Burgess D. Care processes and clinical outcomes of continuous outpatient support with inotropes (COSI) in patients with refractory endstage heart failure. J Card Fail. 2003;(9):180-187.
54. Gorodeski EZ, Chu EC, Reese JR, Shishehbor MH, Hsich E, Starling RC. Prognosis on chronic dobutamine or milrinone infusions for stage D heart failure. Circ Heart Fail. 2009;2(4):320-324. doi:10.1161/CIRCHEARTFAILURE.108.839076.
55. Collins SP, Levy PD, Martindale JL, et al. Clinical and research considerations for patients with hypertensive acute heart failure: A consensus statement from the Society for Academic Emergency Medicine and the Heart Failure Society of America Acute Heart Failure Working Group. Acad Emerg Med. 2016;23(8):922-931. doi:10.1111/acem.13025.
56. Felker GM, Lee KL, Bull DA, et al. Diuretic strategies in patients with acute decompensated heart failure. N Engl J Med. 2011; 364(9):797-805. doi:10.1056/NEJMoa1005419.

57. Publication Committee for the VMAC Investigators (Vasodilatation in the Management of Acute CHF). Intravenous nesiritide vs nitroglycerin for treatment of decompensated congestive heart failure: a randomized controlled trial. JAMA. 2002;287(12):1531-1540.
58. Gradman AH, Vekeman F, Eldar-Lissai A, Trahey A, Ong SH, Duh MS. Is addition of vasodilators to loop diuretics of value in the care of hospitalized acute heart failure patients? Real-world evidence from a retrospective analysis of a large United States hospital database. J Card Fail. 2014;20(11):853-863. doi:10.1016/j.cardfail.2014.08.006.
59. Wilson SS, Kwiatkowski GM, Millis SR, Purakal JD, Mahajan AP, Levy PD. Use of nitroglycerin by bolus prevents intensive care unit admission in patients with acute hypertensive heart failure. Am J Emerg Med. 2017;35(1):126-131. doi:10.1016/j.ajem.2016.10.038.
60. Eryonucu B, Guler N, Guntekin U, Tuncer M. Comparison of the effects of nitroglycerin and nitroprusside on transmitral Doppler flow parameters in patients with hypertensive urgency. Ann Pharmacother. 2005;39(6):997–1001.
61. O’Connor CM, Starling RC, Hernandez AF, et al. Effect of nesiritide in patients with acute decompensated heart failure. N Engl J Med. 2011;365(1):32-43. doi:10.1056/NEJMoa1100171.
62. Peacock WF 4th, Holland R, Gyarmathy R, et al. Observation unit treatment of heart failure with nesiritide: results from the proaction trial. J Emerg Med. 2005;29(3):243-252.
63. Ayaz SI, Sharkey CM, Kwiatkowski GM, et al. Intravenous enalaprilat for treatment of acute hypertensive heart failure in the emergency department. Int J Emerg Med. 2016;9(1):28. doi:10.1186/s12245-016-0125-4.
64. Peacock WF 4th, Chandra A, Char D, et al. Clevidipine in acute heart failure: results of the A study of BP control in acute heart failure-a pilot study (PRONTO). Am Heart J. 2014;167(4):529-536. doi:10.1016/j.ahj.2013.12.023.
65. Peacock WF 4th, Hollander JE, Diercks DB, et al. Morphine and outcomes in acute decompensated heart failure: an ADHERE analysis. Emerg Med J. 2008;25(4):205-209. doi:10.1136/emj.2007.050419.
66. Miró Ò, Gil V, Martín-Sánchez FJ, Herrero-Puente P, Jet al; ICA-SEMES Research Group. Morphine use in the ED and outcomes of patients with acute heart failure: a propensity score-matching analysis based on the EAHFE registry. [published ahead of print April 12, 2017] Chest. pii:S0012-3692(17)30707-9. doi:10.1016/j.chest.2017.03.037.
67. Wuerz RC, Meador SA. Effects of prehospital medications on mortality and length of stay in congestive heart failure. Ann Emerg Med. 1992;21(6):669-674.
68. Peacock WF 4th, Fonarow GC, Emerman CL, Mills RM, Wynne J; ADHERE Scientific Advisory Committee and Investigators; Adhere Study Group. Impact of early initiation of intravenous therapy for acute decompensated heart failure on outcomes in ADHERE. Cardiology. 2007; 107(1):44-51. doi:10.1159/000093612.
69. Peacock WF, Emerman C, Costanzo MR, Diercks DB, Lopatin M, Fonarow GC. Early vasoactive drugs improve heart failure outcomes. Congest Heart Fail. 2009;15(6): 256-264. doi:10.1111/j.1751-7133.2009.00112.x.
70. Maisel AS, Peacock WF, McMullin N, et al. Timing of immunoreactive B-type natriuretic peptide levels and treatment delay in acute decompensated heart failure: an ADHERE (Acute Decompensated Heart Failure National Registry) analysis. J Am Coll Cardiol. 2008;52(7):534-540. doi:10.1016/j.jacc.2008.05.010.
71. Matsue Y, Damman K, Voors AA, et al. Time-to-Furosemide Treatment and Mortality in Patients Hospitalized With Acute Heart Failure. J Am Coll Cardiol. 2017 Jun 27;69(25):3042-3051. doi:10.1016/j.jacc.2017.04.042.
72. Claret PG, Stiell IG, Yan JW, et al. Hemodynamic, management, and outcomes of patients admitted to emergency department with heart failure. Scand J Trauma Resusc Emerg Med. 2016;24(1):132.
73. Stiell IG, Perry JJ, Clement CM, et al. Prospective and explicit clinical validation of the Ottawa Heart Failure Risk Scale, with and without use of quantitative NT-proBNP. Acad Emerg Med. 2017;24(3):316-327. doi:10.1111/acem.13141.
74. Pang PS, Jesse R, Collins SP, Maisel A. Patients with acute heart failure in the emergency department: do they all need to be admitted? J Card Fail. 2012;18:900-903. doi:10.1016/j.cardfail.2012.10.014.
75. Peacock WF 4th, Young J, Collins S, Emerman C, Diercks D. Heart failure observation units: optimizing care. Ann Emerg Med. 2006;47(1):22-33.
76. Storrow AB, Collins SP, Lyons MS, Wagoner LE, Gibler WB, Lindsell CJ. Emergency department observation of heart failure: preliminary analysis of safety and cost. Congest Heart Fail. 2005;11(2):68-72.
77. Peacock WF 4th, Remer EE, Aponte J, Moffa DA, Emerman CE, Albert NM. Effective observation unit treatment of decompensated heart failure. Congest Heart Fail. 2002;8(2):68 -73.
78. Peacock WF 4th, Albert NM. Observation unit management of heart failure. Emerg Med Clin North Am. 2001;19(1):209-232.
79. Miró O, Carbajosa V, Peacock WF 4th, et al; ICA-SEMES group. The effect of a short-stay unit on hospital admission and length of stay in acute heart failure: REDUCE-AHF study. Eur J Intern Med. 2017;40:30-36. doi:10.1016/j.ejim.2017.01.015.
80. Ekman I, Andersson B, Ehnfors M, Matejka G, Persson B, Fagerberg B. Feasibility of a nurse-monitored, outpatient-care programme for elderly patients with moderate-to-severe, chronic heart failure. Eur Heart J. 1998;19(8):1254-1260.
81. Riegel B, Carlson B, Kopp Z, LePetri B, Glaser D, Unger A. Effect of a standardized nurse case-management telephone intervention on resource use in patients with chronic heart failure. Arch Intern Med. 2002;162(6):705-712.
82. Laramee AS, Levinsky SK, Sargent J, Ross R, Callas P. Case management in a heterogeneous congestive heart failure population: a randomized controlled trial. Arch Intern Med. 2003;163(7):809-817.
83. Stewart S, Pearson S, Horowitz JD. Effects of a home-based intervention among patients with congestive heart failure discharged from acute hospital care. Arch Intern Med. 1998;158(10):1067-1072.
84. Stewart S, Marley JE, Horowitz JD. Effects of a multidisciplinary, home-based intervention on unplanned readmissions and survival among patients with chronic congestive heart failure: a randomised controlled study. Lancet. 1999;354(9184):1077-1083.
85. Weinberger M, Oddone EZ, Henderson WG; Veterans Affairs Cooperative Study Group. Does increased access to primary care reduce hospital readmissions? Veterans Affairs Cooperative Study Group on primary care and hospital readmission. N Engl J Med. 1996;334(22):1441-1447.
86. Asthana V, Sundararajan M, Karun V, et al. Educational strategy for management of heart failure markedly reduces 90-day emergency department and hospital readmissions in un- and underinsured patients. J Am Coll Cardiol. 2017;69(11Suppl): 780. doi:10.1016/S0735-1097(17)34169-4.
87. Bell SP, Schnipper JL, Goggins K, et al; Pharmacist Intervention for Low Literacy in Cardiovascular Disease (PILL-CVD) Study Group. Effect of pharmacist counseling intervention on health care utilization following hospital discharge: a randomized control trial. J Gen Intern Med. 2016;31(5):470-477. doi:10.1007/s11606-016-3596-3.
Patients with heart failure (HF) present daily to busy EDs. An estimated 6.5 million Americans are living with this diagnosis, and the number is predicted to grow to 8 million by 2023.1 Most HF patients (82.1%) who present to EDs are hospitalized, while a selected minority are either managed in the ED and discharged (11.6%) or managed in observation units (OU) (6.3%).2 The prognosis after HF is initially diagnosed is poor, with a 5-year mortality of 50%,3 and after a single HF hospitalization, 29% will die within 1 year.4
One-third of the total Medicare budget is spent on HF, despite the fact that HF represents only 10.5% of the Medicare population.2 Up to 80% of HF costs are for hospitalizations, which cost an average of $11,840 per inpatient admission.5,6 The high costs are due to an average length of stay (LOS) of 5.2 days7 (Table 1).
Adding to hospital costs is the degree of “reactivism,” with approximately 20% of patients discharged from the ED returning within 2 weeks, of whom nearly 50% will be hospitalized.11 Following HF hospitalization and discharge, the 30-day readmission rate is 26.2%,2 increasing to 36% by 90 days.12 The Centers for Medicare & Medicaid Services (CMS) has incentivized hospitals and providers to reduce admissions, but penalize hospitals that do not. Overall, CMS will reduce payments by up to 3% to hospitals with excess readmissions for select conditions, including HF.13
Causes of Heart Failure
Heart failure represents a final common pathway, which in the United States is most often due to coronary artery disease (CAD). Many types of pathology ultimately result in left ventricular (LV) dysfunction, and much of its rising prevalence is a result of the success we now have in managing historically fatal cardiovascular (CV) conditions. These include hypertension, diabetes mellitus (DM), CAD, and valvular and other CV structural conditions.
Heart failure is caused by either a dilated ventricle with a reduced ejection fraction (HFrEF) and inability to eject volume, or a stiffened ventricle with a preserved EF (HFpEF) that is unable to receive increased venous return. Both conditions acutely decompensate pulmonary congestion. A preserved EF is defined as an EF at or greater than 50%, whereas a reduced EF is at or less than 40%, with the 41% to 49% range considered as borderline preserved EF.3
While there are important differences in the treatment of chronic and subacute HF, driven by the EF, the effect of EF on early decision-making and treatment in the ED is negligible: Although the probability of HFpEF increases with increasing initial ED systolic blood pressure (SBP), clinical presentation and treatment in the ED are initially identical—regardless of the EF.
Noninvasive continuous transcutaneous hemodynamic monitoring is available for ED use, and may provide further insight into the underlying pathophysiology. A study of 127 acute heart failure (AHF) ED patients identified three hemodynamic AHF phenotypes. These include normal cardiac index (CI) and systemic vascular resistance index (SVRI), low CI and SVRI, and low CI and elevated SVRI.14 While it is attractive to suggest therapeutic interventions based on these measurements, outcome data are lacking.
Presentation
The most common ED presentation of patients suffering from AHF is dyspnea secondary to volume overload, or as the result of acute hypertension with relatively less volume overload. However, regardless of the cause of dyspnea, it is not only the most common resulting complaint, but one that requires immediate treatment. Ultimately, 59% of all HF admissions are attributed to volume overload and dyspnea (Figure 1).15
Heart failure can also present in a more protean manner, with cough, fatigue, and edema, as well as more subtle symptoms predominating and resulting in a complicated differential diagnosis (Table 2).16
Because HF is a disease that most significantly affects older patients who frequently have concomitant morbidities (eg, myocardial ischemia, chronic obstructive pulmonary disease [COPD] exacerbation, uncontrolled DM), other less clinically obvious disease presentations may actually be the cause of the AHF exacerbation.
Diagnosis
A focused history and physical examination that is part of all ED evaluations should be expedited whenever there is evidence of hemodynamic instability or respiratory compromise. An early working diagnosis is essential to avoid a delay in appropriate treatment, which is associated with increased mortality.
When HF is likely, the potential etiology and precipitants for decompensation must be considered. This list is long, but medication noncompliance and dietary indiscretion are the most common causes.
Symptoms and Prior History of HF
The classic symptoms for AHF include dyspnea at rest or exertion, and orthopnea, both of which unfortunately have poor sensitivity and specificity for AHF. As an isolated symptom, dyspnea is of marginal diagnostic utility (sensitivity and specificity for an HF diagnosis is 56% and 53%, respectively), and orthopnea is only slightly better (sensitivity and specificity 77% and 50%, respectively). A prior HF diagnosis makes repeat presentations much more likely (sensitivity and specificity 60% and 90%, respectively).17
Physical Examination
Simple observation and a directed examination can rapidly point to the diagnosis (Figure 2).
Electrocardiography
Because CAD is one of the most common underlying AHF etiologies, an electrocardiogram (ECG) should always be obtained early for a patient presenting with potential AHF. Although the ECG does not usually contribute to ED management, the identification of new ST-segment changes or a malignant arrhythmia will guide critical management decisions.
Imaging Studies
Chest X-ray Imaging. A chest X-ray (CXR) study must be considered early when a patient presents with signs and symptoms suggestive of AHF. Although the classic findings of HF (eg, Kerley B lines [short horizontal lines perpendicular to the pleural surface],18 interstitial congestion, pulmonary effusion) can lag behind the clinical presentation, and also be nondiagnostic in the setting of mild HF, the CXR is an effective aid in identifying other causes of dyspnea such as pneumonia. Ultimately, the utility of the CXR for diagnosis is similar to that of the history and physical examination in that it will be diagnostic when positive but cannot exclude AHF if normal.
Ultrasound. Because it is fast, inexpensive, noninvasive, and readily available in the ED, ultrasound is frequently used to evaluate potential HF patients. Several studies have demonstrated that the presence of B lines in two or more regions is specific for AHF (specificity 75%-100%), although the sensitivity may be limited (40%-91%).19-21 The presence of inferior vena cava (IVC) dilation is also associated with adverse outcomes.22 In 80 patients hospitalized with acute decompensated HF (ADHF), a dilated IVC (≥1.9 cm) at admission was associated with higher 90-day mortality (25.4% vs 3.4%, P = 0.009).23 These findings may be considered in groups: In an evaluation of the combination of LV EF, IVC collapsibility, and B lines for an HF diagnosis, the combination of all three had a poor sensitivity (36%) but an excellent specificity (100%), and any two of the three had a specificity of at least 93%.24
Laboratory Evaluation
Myocardial Strain: BNP/NTproBNP. Natriuretic peptides (NPs) are not AHF-specific, but rather they are synthesized and released by the myocardium in the setting of myocardial pressure or volume stress. They are manufactured as preproBNP, then enzymatically cleaved into the active BNP and the inactive fragment N-terminal proBNP (NTproBNP). The predominant hormonal effects of BNP are vasodilation and natriuresis, as well as antagonism of the hormones associated with sodium retention (aldosterone) and vasoconstriction (endothelin, norepinephrine).
As AHF results in myocardial stress, NP elevation provides diagnostic and prognostic information. Clinical judgment supported by a BNP greater than 100 pg/mL is a better predictor of AHF than clinical judgment alone (accuracy 81% vs 74%, respectively).25 While low levels (BNP <100 pg/mL or NTproBNP <300 pg/mL) reliably exclude the diagnosis of HF (sensitivities >95%), higher levels (BNP >500 pg/mL, NTproBNP >900 pg/mL) are useful as “rule-in” markers, with specificity greater than 95%. The NTproBNP also requires adjustment for patients older than age 75 years, with a higher level (>1,800 pg/mL) to rule-in HF. The NP grey zone (BNP 100-500 pg/mL, NTproBNP 300-900 pg/mL)requires additional testing for accurate diagnoses (Figure 3).25-29
There are several confounders to the interpretation of NP results: NPs are negatively confounded by the presence of obesity, resulting in a lowering of the value as compared to the clinical presentation.Thus, the measured BNP level should be doubled if the patient’s body mass index exceeds 35 kg/m2.30 Secondly, because NP metabolism is partially renal dependent, elevated levels may not reflect AHF in the presence of renal failure. If the estimated glomerular filtration rate is less than 60 mL/min, measured BNP levels should be halved.31
AHF vs Myocardial Ischemia: Troponin Levels. Large registry data using contemporary troponin assays clearly identify the association between elevated troponin levels (>99th percentile in a healthy population) and increased short-term risk. With the US Food and Drug Association (FDA) approval of a high-sensitivity troponin (hs-cTnT) assay, a greater frequency of elevated cardiac troponin T (cTnT) and cardiac troponin I (cTnl) will be identified in AHF patients in the ED.
In one retrospective study of 4,705 AHF patients in the ED, hs-cTnT were elevated in 48.4% of cases (25.3% in cTnI, 37.9% in cTnT, and 82.2% in hs-cTnT). Although 1-year mortality was higher in those with elevated troponin (adjusted heart rate [HR] 1.61; CI 95% 1.38-1.88), elevated troponin was not associated with 30-day revisits to the ED (1.01; 0.87-1.19) and high sensitive elevations less than double the reference value had no impact on outcomes.32 Thus, in terms of management of AHF in the ED, slightly elevated stable serial troponins are more consistent with underlying HF, and should be managed as such. This is not true of rising/falling troponin levels, which should still engender concern for underlying myocardial ischemia and a different management pathway.
Renal function. Comprised renal function is an important predictor of AHF outcome. Large registry data from hospitalized HF patients demonstrate that a presenting blood urea nitrogen level greater than 43 mg/dL is one of the most important predictors of increased acute mortality,33 and levels below 30 mg/dL identify a cohort likely to be successfully managed in an observation environment.34 Creatinine is a helpful lagging indicator of mortality, with higher levels (>2.75 mg/dL) associated with increased short-term adverse outcomes and decreased therapeutic responsiveness (Figure 4).
For patients presenting with ADHF, a newer test recently approved by the FDA uses the product of the urine markers tissue inhibitor of metalloproteinase-2 and insulin-like growth factor-binding protein 7, to generate a score predictive of acute kidney injury.35 While promising, no studies of ED outcomes are currently available.
Volume Assessment
Objective volume assessment is useful for diagnosis and prognosis in AHF. Bioimpedance vector analysis (BIVA) is a rapid, inexpensive, noninvasive technique that measures total body water by placing a pair of electrodes on the wrist and ipsilateral ankle. The BIVA measurements have strong correlations with the gold standard volume-assessment technique of deuterium dilution (r > 0.99).36 In HF, BIVA can assess volume depletion37 and overload,38 and identifies differences in hydration status between 90-day survivors and non-survivors (P < 0.01).39
Used in combination with BNP, one prospective study of 292 dyspneic patients found that, while BIVA was a strong predictor of AHF (c-statistic 0.93, P = 0.016), the most accurate volume status determination was the combination of both (c-statistic, 0.99; P = 0.005), for which the combined accuracy exceeded either alone.40 Finally, in 166 hospitalized HF patients discharged by BNP and BIVA parameters, vs 149 discharged based on clinical impressions, those assessed with BNP and BIVA had lower 6-month readmissions (23% vs 35%, P = 0.02) and overall cost of care.41
Combination Technologies
Obviously, EPs may consider multiple technologies to arrive at an accurate diagnosis. One prospective evaluation enrolled 236 patients to determine the diagnostic accuracy for AHF in the ED and reported lung ultrasound, CXR, and NTproBNP had a sensitivity of 57.7% and 88.0%, 74.5% and 86.3%, and a specificity of 97.6% and 28.0%. The best overall combination was the CXR with lung ultrasound (sensitivity 84.7%, specificity 77.7%).42
Another prospective study evaluated IVC diameter, bioelectrical impedance analysis (BIA), and NTproBNP in 96 elderly patients. ADHF patients had higher IVC diameters and lower collapsibility index, lower resistance and reactance, and higher NTproBNP levels. While all had high and statistically similar C-statistics (range 0.8 to 0.9) for an ADHF diagnosis, they concluded that IVC ultrasonography and BIA were as useful as NT-proBNP for diagnosing ADHF. 24
Diagnostic Scoring Systems
A scoring system has been proposed to improve diagnosis in the ED. Unfortunately, the value over clinical impression has not been clearly proven, though one randomized, controlled trial did not show statistically significant improvement in diagnostic accuracy when compared to standard care (77% vs 74%, P = 0.77).43
Differential Diagnosis
The differential diagnosis for acute dyspnea is long and potentially arcane. Efforts should focus on excluding non-HF causes of dyspnea, while considering the high risk of alternative etiologies for signs and symptoms. These include asthma, COPD, pneumonia, and pulmonary embolism, which may represent the primary pathologies in a patient with a history of HF, or be the cause of a HF exacerbation. Additional causes of noncardiogenic pulmonary edema should also be considered (eg, acute respiratory distress syndrome, toxins, etc). Acute coronary syndrome and dyspnea may be angina equivalents—one important consideration.
Treatment and Management
Airway Management
Treatment of CH in the ED must always start with an immediate airway evaluation, with the possible need for endotracheal intubation preceding all diagnostic or other management considerations. Intubation is a decision most successfully based on physician clinical assessment, including oxygen (O2) selection rather than waiting for the results of objective measures such as arterial blood gas analysis.
Oxygen
Supplemental O2 should be administered to maintain an O2 saturation above 95%, but obviously is unnecessary in the absence of hypoxia.
Noninvasive Ventilation
Two kinds of noninvasive ventilation (NIV) are available, continuous positive airway pressure and bilevel positive airway pressure ventilation. The physiological differences between these types of NIV have little bearing on ED treatment.
Noninvasive ventilation has not been clearly shown to provide long-term mortality benefit. Large registry data44 report that outcomes are no worse than the alternative of endotracheal intubation, while multiple systematic reviews,45,46meta-analysis,47and Cochrane reviews48,49have established NIV as an acute pulmonary edema intervention that provides reductions in hospital mortality (numbers needed to treat [NNT] 13) and intubation (NNT 8), the prospective randomized C3PO (Congenital Cardiac Catheterization Project on Outcomes) trial50 failed to demonstrate any mortality reduction.
In patients with severe respiratory distress, NIV is a reasonable strategy during the aggressive administration of medical therapy in an attempt to avoid endotracheal intubation. However, NIV is not a stand-alone therapy and though its use may obviate the need for immediate intubation, its implementation should not be considered definitive management.
Correction of Abnormal Vital Signs: Abnormal SBP
Vital signs are an important determinant of therapy, driving treatment strategies. Interventions for HF are based on the patient’s SBP, in particular correction of symptomatic hypotension and hypertensive HF (Table 3).51
Symptomatic Hypotension. The presence of symptomatic hypotension is an extremely poor prognostic finding in AHF. Inotrope therapy may be considered, but it does not reduce mortality except as a bridge to mechanical interventions (LV assist device or transplant).52-54 Temporary inotropic support is recommended for cardiogenic shock to maintain systemic perfusion and prevent end organ damage.3 The inotropic support includes administration of dopamine, dobutamine, or milrinone, though none have been proven to be superior over the other. The lowest possible dose of the selected inotrope should be used to limit arrhythmogenic effects. Inotropic agents should not be used in the absence of severe systolic dysfunction, or low BP, or impaired perfusion, or evidence of significantly decreased cardiac output.
Hypertensive Heart Failure. Defined as the rapid onset of pulmonary congestion with an SBP greater than 140 mm Hg, and commonly greater than 160 mm Hg, these patients may have profound dyspnea, requiring endotracheal intubation. However, in this situation, aggressive vasodilation is typically rapidly effective. Overall, patients presenting with an elevated SBP have lower rates of in-hospital mortality, 30-day myocardial infarction (MI), death, or rehospitalization, and a greater likelihood of discharge within 24 hours—as long as the elevated SBP is aggressively and rapidly treated.
Pharmacological Therapy
Pharmacological management is the mainstay for treating HF. No other acute therapy (eg, NIV) has demonstrated a morality benefit (See Table 4 for specific dose and administration strategies).55 The time to initiate pharmacological therapy and whether an aggressive approach is indicated must be based on the severity of the clinical symptoms and objective risk stratification measures (eg, NP, troponin levels).
Furosemide. Except for hypertensive HF—in which case BP lowering is the most important goal—diuretics are a mainstay of AHF treatment, and consensus guidelines provide a class I recommendation for their use.3 The DOSE (Diuretic Strategies in Patients with ADHF) trial56 prospectively evaluated diuretics in 308 hospitalized AHF patients and found no outcome differences in administration route (bolus or continuous infusion) or dose (high vs low dose). This study reported trends toward greater improvement with higher furosemide dosing, as well as greater diuresis, but at a cost of transient worsening of renal function.
In general, diuretics should be administered in an intravenous (IV) dose equal to 1 to 2.5 times the patient’s usual daily oral dose. For patients who are diuretic-naïve, a dose of 40 mg IV furosemide or 1 mg IV bumetanide, with subsequent dosing titrated to urine output, is recommended.
Vasodilators. In patients with both AHF and even mildly elevated BP, vasodilators can be extremely effective in achieving symptom improvement. The choice of vasodilator, and how aggressive to increase dosing, depends upon symptom severity. The purpose of vasodilators is to lower BP and therefore, should not be used in the setting of hypotension or signs of hypoperfusion. Flow-limiting, preload-dependent CV states (eg, right ventricular infarction) increase the risk of hypotension, and are relative contraindications to the use of vasodilators. For patients who are severely dyspneic and with critical presentations, the emergency physician (EP) should preclude a detailed history and examination to initiate immediate therapy with short-acting agents that can be terminated rapidly in the case of an adverse event (eg, unexpected hypotension) are preferred.
Nitroglycerin. Nitroglycerin is the vasodilation agent of choice for hypertensive AHF. It is a short-acting, rapid-onset, venous and arterial dilator that decreases BP by preload reduction, and by afterload reduction in higher doses. Nitroglycerin has coronary vasodilatory effects associated with decreased ischemia, but should be avoided in patients taking phosphodiesterase inhibitors.55 Its most common side effect is headache, and hypotension occurs in about 3.5% of patients.57
Commonly given as a continuous infusion at IV doses up to 400 mcg/min, nitroglycerin may be associated with higher costs and longer LOS.58 Some authors suggest that bolus nitroglycerin therapy may be superior: In a retrospective study of 395 patients, an IV bolus of nitroglycerin 0.5 mg was superior to both an infusion, or a combination of bolus and infusion, as demonstrated by lower rates of ICU admission (48% vs 67% and 79%, respectively, P = 0.006) and shorter hospital stays (4.4 vs 6.3 and 7.3 days, respectively, P = 0.01). In all cohorts, adverse event rates were similar for hypotension, troponin elevation, and creatinine increase over 48 hours.59 Nitroprusside. Nitroprusside is a potent arterial and venous dilator that causes rapid decrease in BP and LV-filling pressures. It is usually considered more effective than nitroglycerin, despite a small study showing similar hemodynamic responses.60
Initial dosing of nitroprusside starts at 0.3 µg/kg/min IV, and is increased every 5 minutes to a maximum of 10 mcg/kg/min, based on BP and clinical response. The most common acute complication of nitroprusside infusions is hypotension. Cyanide toxicity may occur with prolonged use, high doses, or in patients with renal failure.55
Nesiritide. Exogenously administered, the B-type NP nesiritide is effective in lowering BP and improving dyspnea in AHF,55 although large prospective studies showed it had little long-term advantage over standard care.61 In a small, randomized, controlled trial, nesiritide reduced 30-day revisit LOS when given in an OU.62 The 22-minute half-life of nesiritide is longer than that of the nitrates, and its side effect is predominately hypotension, which occurs at rates similar to those of other vasodilators.55
Angiotensin Converting Enzyme Inhibitors. Because angiotensin converting enzyme inhibitors (ACEIs) have chronic mortality reduction benefits, their use in the acute setting is theoretically attractive, however, this has been poorly proven in AHF ED patients. In a retrospective review of 103 patients with elevated NTproBNP levels receiving bolus IV enalaprilat within 3 hours of presentation, the mean SBP decreased by 30 mm Hg, with only 2% of patients developing hypotension.63 However, with the longer half-life of ACEIs, if hypotension occurs, the potential for a prolonged BP-lowering effect exists.
Calcium Channel Blockers. Clevidipine and nicardipine are rapidly acting IV calcium channel blockers that lower BP by selective arteriolar vasodilation and increased cardiac output as vascular resistance declines.55 Because these agents have no negative inotropic or chronotropic effects, they may be beneficial in hypertensive AHF. In an open-label trial of 104 hypertensive AHF patients, clevidipine was more effective than standard care for the rapid control of BP and relief of dyspnea.64
Morphine. Large registry analyses have demonstrated potential harm with the routine use of morphine,65 as do recent propensity score matched analyses.66 Until there are studies demonstrating benefit, the use of morphine at present should be reserved for palliative care.
Time to Treatment
Although a randomized controlled trial on the importance of time to treatment of AHF is unlikely to ever be completed, data suggest that, as in the case of MI, delayed AHF therapy is associated with adverse outcomes. In a study of 499 suspected AHF patients transferred by ambulance, patients randomized to immediate therapy vs those whose therapy was not initiated until hospital arrival (mean delay of 36 minutes), had a 251% increase in survival (P < 0.01).67
Furthermore, the delayed administration of vasoactive agents, defined as medication administered to alter hemodynamics (eg, dobutamine, dopamine, nitroglycerin, nesiritide) is also associated with harm,68 and registry studies demonstrate increased death rates (n = 35,700).69 Finally, another registry (n = 14,900) study demonstrated early IV furosemide is associated with decreased mortality.70 This latter finding was also validated in a prospective observational cohort study (mortality 2.3 vs 6.0 in early vs delayed therapy groups, respectively).71
Patient Disposition
One of the unique features of emergency medicine is the need to determine, with very limited information and time, a patient’s very short-term clinical trajectory. Few physicians are required to have greater accuracy with less information or time than do EPs. Several studies report objective data points and risk scores to assist in this task, but none has been universally adopted, reflecting the challenge of applying population data to individuals.
Short-term Prognosis
In 1,638 patients evaluated for 14-day outcomes, an HR lower than 50% maximal HR (MHR), and an SBP greater than 140 mm Hg were associated with the lowest rate of serious adverse events (SAEs) (6%) and hospitalization (38%).72 An MHR over 75% was associated with the highest SAE rate, although SAEs decreased as SBP increased (30%, 24%, and 21% with SBPs < 120 mm Hg, 120-140 mm Hg, and > 140 mm Hg, respectively).72
Risk Scores
In a prospective, observational cohort study of 1,100 ED patients, the Ottawa Heart Failure Risk Scale, combined with NTproBNP values, had a sensitivity of 95.8%—at the cost of increasing the admission rate (from 60.8% to 88%)—for serious adverse events (defined as death within 30 days), admission to a monitored unit, intubation, NIV, MI, or relapse resulting in hospital admission within 14 days.73
Observation Unit
Overall, 44% of in-patient HF admissions are for less than 3 days (Table 1),2 supporting the practice of managing selected patients in shorter clinical-care environments than in inpatient units. Further, ED patients presenting with moderate dyspnea require both a diagnosis and an evaluation of their therapeutic response to determine the need for hospitalization. However, evaluating therapeutic response requires more time than is available in the typical ED. Thus, an ED OU offers the following:
(1) The OU provides the EP with a longer evaluation time, and therefore a more accurate disposition may be effected;
(2) Costs are significantly lower in patients managed in an ED OU; and
(3) Patient satisfaction may be improved, as most patients prefer home management over hospitalization.
All three of these opportunities are supported by a number of studies,74-78 with validated entry and exclusion criteria, treatment algorithms and discharge metrics. Most recently, in a registry of hospitals in Spain registry, patients presenting to hospitals that had OUs had a 2.2-day shorter LOS, lower 30-day ED revisit rate, and similar mortality rates compared to those in institutions without OUs—although these beneficial effects occurred at the cost of an 8.9% higher admission rate.79
Patient Education
Intuitively, it would be expected that patient education would reduce return visits, 30-day hospitalizations, and AHF-related mortality. Unfortunately, it has not been demonstrated that patient education results in a consistent benefit at hospital discharge, or in the outpatient environment.80-85
Although AHF education in the ED has been poorly studied, areas that have shown promise are education occurring before ED management (ie, in the ED waiting area) in underinsured patients,86 and during ED care for patients with poor health care literacy.87 As educational interventions are both inexpensive and unlikely to result in harm, their implementation should be considered.
Conclusion
The spectrum of HF is a common presentation in the ED. Because HF generally appears as dyspnea, in a cohort with multiple comorbidities, the diagnosis can be challenging. This is complicated by the fact that patients with severe presentations may require life-saving interventions long before a clinical evaluation is completed (or even initiated). The skill of the EP, and his or her ability to improve the clinical condition before intubation is required, will determine the patient’s trajectory. Conversely, as a chronic condition, HF may present with moderate symptoms for which a short diuretic “tune-up” in an observation environment may be appropriate.
How these decisions are made will depend upon the local environment, the availability of outpatient resources, and individual patient choices. There are few chronic diseases that are more complex, are seen more often in the ED, or that require more skill and finesse in management.
Patients with heart failure (HF) present daily to busy EDs. An estimated 6.5 million Americans are living with this diagnosis, and the number is predicted to grow to 8 million by 2023.1 Most HF patients (82.1%) who present to EDs are hospitalized, while a selected minority are either managed in the ED and discharged (11.6%) or managed in observation units (OU) (6.3%).2 The prognosis after HF is initially diagnosed is poor, with a 5-year mortality of 50%,3 and after a single HF hospitalization, 29% will die within 1 year.4
One-third of the total Medicare budget is spent on HF, despite the fact that HF represents only 10.5% of the Medicare population.2 Up to 80% of HF costs are for hospitalizations, which cost an average of $11,840 per inpatient admission.5,6 The high costs are due to an average length of stay (LOS) of 5.2 days7 (Table 1).
Adding to hospital costs is the degree of “reactivism,” with approximately 20% of patients discharged from the ED returning within 2 weeks, of whom nearly 50% will be hospitalized.11 Following HF hospitalization and discharge, the 30-day readmission rate is 26.2%,2 increasing to 36% by 90 days.12 The Centers for Medicare & Medicaid Services (CMS) has incentivized hospitals and providers to reduce admissions, but penalize hospitals that do not. Overall, CMS will reduce payments by up to 3% to hospitals with excess readmissions for select conditions, including HF.13
Causes of Heart Failure
Heart failure represents a final common pathway, which in the United States is most often due to coronary artery disease (CAD). Many types of pathology ultimately result in left ventricular (LV) dysfunction, and much of its rising prevalence is a result of the success we now have in managing historically fatal cardiovascular (CV) conditions. These include hypertension, diabetes mellitus (DM), CAD, and valvular and other CV structural conditions.
Heart failure is caused by either a dilated ventricle with a reduced ejection fraction (HFrEF) and inability to eject volume, or a stiffened ventricle with a preserved EF (HFpEF) that is unable to receive increased venous return. Both conditions acutely decompensate pulmonary congestion. A preserved EF is defined as an EF at or greater than 50%, whereas a reduced EF is at or less than 40%, with the 41% to 49% range considered as borderline preserved EF.3
While there are important differences in the treatment of chronic and subacute HF, driven by the EF, the effect of EF on early decision-making and treatment in the ED is negligible: Although the probability of HFpEF increases with increasing initial ED systolic blood pressure (SBP), clinical presentation and treatment in the ED are initially identical—regardless of the EF.
Noninvasive continuous transcutaneous hemodynamic monitoring is available for ED use, and may provide further insight into the underlying pathophysiology. A study of 127 acute heart failure (AHF) ED patients identified three hemodynamic AHF phenotypes. These include normal cardiac index (CI) and systemic vascular resistance index (SVRI), low CI and SVRI, and low CI and elevated SVRI.14 While it is attractive to suggest therapeutic interventions based on these measurements, outcome data are lacking.
Presentation
The most common ED presentation of patients suffering from AHF is dyspnea secondary to volume overload, or as the result of acute hypertension with relatively less volume overload. However, regardless of the cause of dyspnea, it is not only the most common resulting complaint, but one that requires immediate treatment. Ultimately, 59% of all HF admissions are attributed to volume overload and dyspnea (Figure 1).15
Heart failure can also present in a more protean manner, with cough, fatigue, and edema, as well as more subtle symptoms predominating and resulting in a complicated differential diagnosis (Table 2).16
Because HF is a disease that most significantly affects older patients who frequently have concomitant morbidities (eg, myocardial ischemia, chronic obstructive pulmonary disease [COPD] exacerbation, uncontrolled DM), other less clinically obvious disease presentations may actually be the cause of the AHF exacerbation.
Diagnosis
A focused history and physical examination that is part of all ED evaluations should be expedited whenever there is evidence of hemodynamic instability or respiratory compromise. An early working diagnosis is essential to avoid a delay in appropriate treatment, which is associated with increased mortality.
When HF is likely, the potential etiology and precipitants for decompensation must be considered. This list is long, but medication noncompliance and dietary indiscretion are the most common causes.
Symptoms and Prior History of HF
The classic symptoms for AHF include dyspnea at rest or exertion, and orthopnea, both of which unfortunately have poor sensitivity and specificity for AHF. As an isolated symptom, dyspnea is of marginal diagnostic utility (sensitivity and specificity for an HF diagnosis is 56% and 53%, respectively), and orthopnea is only slightly better (sensitivity and specificity 77% and 50%, respectively). A prior HF diagnosis makes repeat presentations much more likely (sensitivity and specificity 60% and 90%, respectively).17
Physical Examination
Simple observation and a directed examination can rapidly point to the diagnosis (Figure 2).
Electrocardiography
Because CAD is one of the most common underlying AHF etiologies, an electrocardiogram (ECG) should always be obtained early for a patient presenting with potential AHF. Although the ECG does not usually contribute to ED management, the identification of new ST-segment changes or a malignant arrhythmia will guide critical management decisions.
Imaging Studies
Chest X-ray Imaging. A chest X-ray (CXR) study must be considered early when a patient presents with signs and symptoms suggestive of AHF. Although the classic findings of HF (eg, Kerley B lines [short horizontal lines perpendicular to the pleural surface],18 interstitial congestion, pulmonary effusion) can lag behind the clinical presentation, and also be nondiagnostic in the setting of mild HF, the CXR is an effective aid in identifying other causes of dyspnea such as pneumonia. Ultimately, the utility of the CXR for diagnosis is similar to that of the history and physical examination in that it will be diagnostic when positive but cannot exclude AHF if normal.
Ultrasound. Because it is fast, inexpensive, noninvasive, and readily available in the ED, ultrasound is frequently used to evaluate potential HF patients. Several studies have demonstrated that the presence of B lines in two or more regions is specific for AHF (specificity 75%-100%), although the sensitivity may be limited (40%-91%).19-21 The presence of inferior vena cava (IVC) dilation is also associated with adverse outcomes.22 In 80 patients hospitalized with acute decompensated HF (ADHF), a dilated IVC (≥1.9 cm) at admission was associated with higher 90-day mortality (25.4% vs 3.4%, P = 0.009).23 These findings may be considered in groups: In an evaluation of the combination of LV EF, IVC collapsibility, and B lines for an HF diagnosis, the combination of all three had a poor sensitivity (36%) but an excellent specificity (100%), and any two of the three had a specificity of at least 93%.24
Laboratory Evaluation
Myocardial Strain: BNP/NTproBNP. Natriuretic peptides (NPs) are not AHF-specific, but rather they are synthesized and released by the myocardium in the setting of myocardial pressure or volume stress. They are manufactured as preproBNP, then enzymatically cleaved into the active BNP and the inactive fragment N-terminal proBNP (NTproBNP). The predominant hormonal effects of BNP are vasodilation and natriuresis, as well as antagonism of the hormones associated with sodium retention (aldosterone) and vasoconstriction (endothelin, norepinephrine).
As AHF results in myocardial stress, NP elevation provides diagnostic and prognostic information. Clinical judgment supported by a BNP greater than 100 pg/mL is a better predictor of AHF than clinical judgment alone (accuracy 81% vs 74%, respectively).25 While low levels (BNP <100 pg/mL or NTproBNP <300 pg/mL) reliably exclude the diagnosis of HF (sensitivities >95%), higher levels (BNP >500 pg/mL, NTproBNP >900 pg/mL) are useful as “rule-in” markers, with specificity greater than 95%. The NTproBNP also requires adjustment for patients older than age 75 years, with a higher level (>1,800 pg/mL) to rule-in HF. The NP grey zone (BNP 100-500 pg/mL, NTproBNP 300-900 pg/mL)requires additional testing for accurate diagnoses (Figure 3).25-29
There are several confounders to the interpretation of NP results: NPs are negatively confounded by the presence of obesity, resulting in a lowering of the value as compared to the clinical presentation.Thus, the measured BNP level should be doubled if the patient’s body mass index exceeds 35 kg/m2.30 Secondly, because NP metabolism is partially renal dependent, elevated levels may not reflect AHF in the presence of renal failure. If the estimated glomerular filtration rate is less than 60 mL/min, measured BNP levels should be halved.31
AHF vs Myocardial Ischemia: Troponin Levels. Large registry data using contemporary troponin assays clearly identify the association between elevated troponin levels (>99th percentile in a healthy population) and increased short-term risk. With the US Food and Drug Association (FDA) approval of a high-sensitivity troponin (hs-cTnT) assay, a greater frequency of elevated cardiac troponin T (cTnT) and cardiac troponin I (cTnl) will be identified in AHF patients in the ED.
In one retrospective study of 4,705 AHF patients in the ED, hs-cTnT were elevated in 48.4% of cases (25.3% in cTnI, 37.9% in cTnT, and 82.2% in hs-cTnT). Although 1-year mortality was higher in those with elevated troponin (adjusted heart rate [HR] 1.61; CI 95% 1.38-1.88), elevated troponin was not associated with 30-day revisits to the ED (1.01; 0.87-1.19) and high sensitive elevations less than double the reference value had no impact on outcomes.32 Thus, in terms of management of AHF in the ED, slightly elevated stable serial troponins are more consistent with underlying HF, and should be managed as such. This is not true of rising/falling troponin levels, which should still engender concern for underlying myocardial ischemia and a different management pathway.
Renal function. Comprised renal function is an important predictor of AHF outcome. Large registry data from hospitalized HF patients demonstrate that a presenting blood urea nitrogen level greater than 43 mg/dL is one of the most important predictors of increased acute mortality,33 and levels below 30 mg/dL identify a cohort likely to be successfully managed in an observation environment.34 Creatinine is a helpful lagging indicator of mortality, with higher levels (>2.75 mg/dL) associated with increased short-term adverse outcomes and decreased therapeutic responsiveness (Figure 4).
For patients presenting with ADHF, a newer test recently approved by the FDA uses the product of the urine markers tissue inhibitor of metalloproteinase-2 and insulin-like growth factor-binding protein 7, to generate a score predictive of acute kidney injury.35 While promising, no studies of ED outcomes are currently available.
Volume Assessment
Objective volume assessment is useful for diagnosis and prognosis in AHF. Bioimpedance vector analysis (BIVA) is a rapid, inexpensive, noninvasive technique that measures total body water by placing a pair of electrodes on the wrist and ipsilateral ankle. The BIVA measurements have strong correlations with the gold standard volume-assessment technique of deuterium dilution (r > 0.99).36 In HF, BIVA can assess volume depletion37 and overload,38 and identifies differences in hydration status between 90-day survivors and non-survivors (P < 0.01).39
Used in combination with BNP, one prospective study of 292 dyspneic patients found that, while BIVA was a strong predictor of AHF (c-statistic 0.93, P = 0.016), the most accurate volume status determination was the combination of both (c-statistic, 0.99; P = 0.005), for which the combined accuracy exceeded either alone.40 Finally, in 166 hospitalized HF patients discharged by BNP and BIVA parameters, vs 149 discharged based on clinical impressions, those assessed with BNP and BIVA had lower 6-month readmissions (23% vs 35%, P = 0.02) and overall cost of care.41
Combination Technologies
Obviously, EPs may consider multiple technologies to arrive at an accurate diagnosis. One prospective evaluation enrolled 236 patients to determine the diagnostic accuracy for AHF in the ED and reported lung ultrasound, CXR, and NTproBNP had a sensitivity of 57.7% and 88.0%, 74.5% and 86.3%, and a specificity of 97.6% and 28.0%. The best overall combination was the CXR with lung ultrasound (sensitivity 84.7%, specificity 77.7%).42
Another prospective study evaluated IVC diameter, bioelectrical impedance analysis (BIA), and NTproBNP in 96 elderly patients. ADHF patients had higher IVC diameters and lower collapsibility index, lower resistance and reactance, and higher NTproBNP levels. While all had high and statistically similar C-statistics (range 0.8 to 0.9) for an ADHF diagnosis, they concluded that IVC ultrasonography and BIA were as useful as NT-proBNP for diagnosing ADHF. 24
Diagnostic Scoring Systems
A scoring system has been proposed to improve diagnosis in the ED. Unfortunately, the value over clinical impression has not been clearly proven, though one randomized, controlled trial did not show statistically significant improvement in diagnostic accuracy when compared to standard care (77% vs 74%, P = 0.77).43
Differential Diagnosis
The differential diagnosis for acute dyspnea is long and potentially arcane. Efforts should focus on excluding non-HF causes of dyspnea, while considering the high risk of alternative etiologies for signs and symptoms. These include asthma, COPD, pneumonia, and pulmonary embolism, which may represent the primary pathologies in a patient with a history of HF, or be the cause of a HF exacerbation. Additional causes of noncardiogenic pulmonary edema should also be considered (eg, acute respiratory distress syndrome, toxins, etc). Acute coronary syndrome and dyspnea may be angina equivalents—one important consideration.
Treatment and Management
Airway Management
Treatment of CH in the ED must always start with an immediate airway evaluation, with the possible need for endotracheal intubation preceding all diagnostic or other management considerations. Intubation is a decision most successfully based on physician clinical assessment, including oxygen (O2) selection rather than waiting for the results of objective measures such as arterial blood gas analysis.
Oxygen
Supplemental O2 should be administered to maintain an O2 saturation above 95%, but obviously is unnecessary in the absence of hypoxia.
Noninvasive Ventilation
Two kinds of noninvasive ventilation (NIV) are available, continuous positive airway pressure and bilevel positive airway pressure ventilation. The physiological differences between these types of NIV have little bearing on ED treatment.
Noninvasive ventilation has not been clearly shown to provide long-term mortality benefit. Large registry data44 report that outcomes are no worse than the alternative of endotracheal intubation, while multiple systematic reviews,45,46meta-analysis,47and Cochrane reviews48,49have established NIV as an acute pulmonary edema intervention that provides reductions in hospital mortality (numbers needed to treat [NNT] 13) and intubation (NNT 8), the prospective randomized C3PO (Congenital Cardiac Catheterization Project on Outcomes) trial50 failed to demonstrate any mortality reduction.
In patients with severe respiratory distress, NIV is a reasonable strategy during the aggressive administration of medical therapy in an attempt to avoid endotracheal intubation. However, NIV is not a stand-alone therapy and though its use may obviate the need for immediate intubation, its implementation should not be considered definitive management.
Correction of Abnormal Vital Signs: Abnormal SBP
Vital signs are an important determinant of therapy, driving treatment strategies. Interventions for HF are based on the patient’s SBP, in particular correction of symptomatic hypotension and hypertensive HF (Table 3).51
Symptomatic Hypotension. The presence of symptomatic hypotension is an extremely poor prognostic finding in AHF. Inotrope therapy may be considered, but it does not reduce mortality except as a bridge to mechanical interventions (LV assist device or transplant).52-54 Temporary inotropic support is recommended for cardiogenic shock to maintain systemic perfusion and prevent end organ damage.3 The inotropic support includes administration of dopamine, dobutamine, or milrinone, though none have been proven to be superior over the other. The lowest possible dose of the selected inotrope should be used to limit arrhythmogenic effects. Inotropic agents should not be used in the absence of severe systolic dysfunction, or low BP, or impaired perfusion, or evidence of significantly decreased cardiac output.
Hypertensive Heart Failure. Defined as the rapid onset of pulmonary congestion with an SBP greater than 140 mm Hg, and commonly greater than 160 mm Hg, these patients may have profound dyspnea, requiring endotracheal intubation. However, in this situation, aggressive vasodilation is typically rapidly effective. Overall, patients presenting with an elevated SBP have lower rates of in-hospital mortality, 30-day myocardial infarction (MI), death, or rehospitalization, and a greater likelihood of discharge within 24 hours—as long as the elevated SBP is aggressively and rapidly treated.
Pharmacological Therapy
Pharmacological management is the mainstay for treating HF. No other acute therapy (eg, NIV) has demonstrated a morality benefit (See Table 4 for specific dose and administration strategies).55 The time to initiate pharmacological therapy and whether an aggressive approach is indicated must be based on the severity of the clinical symptoms and objective risk stratification measures (eg, NP, troponin levels).
Furosemide. Except for hypertensive HF—in which case BP lowering is the most important goal—diuretics are a mainstay of AHF treatment, and consensus guidelines provide a class I recommendation for their use.3 The DOSE (Diuretic Strategies in Patients with ADHF) trial56 prospectively evaluated diuretics in 308 hospitalized AHF patients and found no outcome differences in administration route (bolus or continuous infusion) or dose (high vs low dose). This study reported trends toward greater improvement with higher furosemide dosing, as well as greater diuresis, but at a cost of transient worsening of renal function.
In general, diuretics should be administered in an intravenous (IV) dose equal to 1 to 2.5 times the patient’s usual daily oral dose. For patients who are diuretic-naïve, a dose of 40 mg IV furosemide or 1 mg IV bumetanide, with subsequent dosing titrated to urine output, is recommended.
Vasodilators. In patients with both AHF and even mildly elevated BP, vasodilators can be extremely effective in achieving symptom improvement. The choice of vasodilator, and how aggressive to increase dosing, depends upon symptom severity. The purpose of vasodilators is to lower BP and therefore, should not be used in the setting of hypotension or signs of hypoperfusion. Flow-limiting, preload-dependent CV states (eg, right ventricular infarction) increase the risk of hypotension, and are relative contraindications to the use of vasodilators. For patients who are severely dyspneic and with critical presentations, the emergency physician (EP) should preclude a detailed history and examination to initiate immediate therapy with short-acting agents that can be terminated rapidly in the case of an adverse event (eg, unexpected hypotension) are preferred.
Nitroglycerin. Nitroglycerin is the vasodilation agent of choice for hypertensive AHF. It is a short-acting, rapid-onset, venous and arterial dilator that decreases BP by preload reduction, and by afterload reduction in higher doses. Nitroglycerin has coronary vasodilatory effects associated with decreased ischemia, but should be avoided in patients taking phosphodiesterase inhibitors.55 Its most common side effect is headache, and hypotension occurs in about 3.5% of patients.57
Commonly given as a continuous infusion at IV doses up to 400 mcg/min, nitroglycerin may be associated with higher costs and longer LOS.58 Some authors suggest that bolus nitroglycerin therapy may be superior: In a retrospective study of 395 patients, an IV bolus of nitroglycerin 0.5 mg was superior to both an infusion, or a combination of bolus and infusion, as demonstrated by lower rates of ICU admission (48% vs 67% and 79%, respectively, P = 0.006) and shorter hospital stays (4.4 vs 6.3 and 7.3 days, respectively, P = 0.01). In all cohorts, adverse event rates were similar for hypotension, troponin elevation, and creatinine increase over 48 hours.59 Nitroprusside. Nitroprusside is a potent arterial and venous dilator that causes rapid decrease in BP and LV-filling pressures. It is usually considered more effective than nitroglycerin, despite a small study showing similar hemodynamic responses.60
Initial dosing of nitroprusside starts at 0.3 µg/kg/min IV, and is increased every 5 minutes to a maximum of 10 mcg/kg/min, based on BP and clinical response. The most common acute complication of nitroprusside infusions is hypotension. Cyanide toxicity may occur with prolonged use, high doses, or in patients with renal failure.55
Nesiritide. Exogenously administered, the B-type NP nesiritide is effective in lowering BP and improving dyspnea in AHF,55 although large prospective studies showed it had little long-term advantage over standard care.61 In a small, randomized, controlled trial, nesiritide reduced 30-day revisit LOS when given in an OU.62 The 22-minute half-life of nesiritide is longer than that of the nitrates, and its side effect is predominately hypotension, which occurs at rates similar to those of other vasodilators.55
Angiotensin Converting Enzyme Inhibitors. Because angiotensin converting enzyme inhibitors (ACEIs) have chronic mortality reduction benefits, their use in the acute setting is theoretically attractive, however, this has been poorly proven in AHF ED patients. In a retrospective review of 103 patients with elevated NTproBNP levels receiving bolus IV enalaprilat within 3 hours of presentation, the mean SBP decreased by 30 mm Hg, with only 2% of patients developing hypotension.63 However, with the longer half-life of ACEIs, if hypotension occurs, the potential for a prolonged BP-lowering effect exists.
Calcium Channel Blockers. Clevidipine and nicardipine are rapidly acting IV calcium channel blockers that lower BP by selective arteriolar vasodilation and increased cardiac output as vascular resistance declines.55 Because these agents have no negative inotropic or chronotropic effects, they may be beneficial in hypertensive AHF. In an open-label trial of 104 hypertensive AHF patients, clevidipine was more effective than standard care for the rapid control of BP and relief of dyspnea.64
Morphine. Large registry analyses have demonstrated potential harm with the routine use of morphine,65 as do recent propensity score matched analyses.66 Until there are studies demonstrating benefit, the use of morphine at present should be reserved for palliative care.
Time to Treatment
Although a randomized controlled trial on the importance of time to treatment of AHF is unlikely to ever be completed, data suggest that, as in the case of MI, delayed AHF therapy is associated with adverse outcomes. In a study of 499 suspected AHF patients transferred by ambulance, patients randomized to immediate therapy vs those whose therapy was not initiated until hospital arrival (mean delay of 36 minutes), had a 251% increase in survival (P < 0.01).67
Furthermore, the delayed administration of vasoactive agents, defined as medication administered to alter hemodynamics (eg, dobutamine, dopamine, nitroglycerin, nesiritide) is also associated with harm,68 and registry studies demonstrate increased death rates (n = 35,700).69 Finally, another registry (n = 14,900) study demonstrated early IV furosemide is associated with decreased mortality.70 This latter finding was also validated in a prospective observational cohort study (mortality 2.3 vs 6.0 in early vs delayed therapy groups, respectively).71
Patient Disposition
One of the unique features of emergency medicine is the need to determine, with very limited information and time, a patient’s very short-term clinical trajectory. Few physicians are required to have greater accuracy with less information or time than do EPs. Several studies report objective data points and risk scores to assist in this task, but none has been universally adopted, reflecting the challenge of applying population data to individuals.
Short-term Prognosis
In 1,638 patients evaluated for 14-day outcomes, an HR lower than 50% maximal HR (MHR), and an SBP greater than 140 mm Hg were associated with the lowest rate of serious adverse events (SAEs) (6%) and hospitalization (38%).72 An MHR over 75% was associated with the highest SAE rate, although SAEs decreased as SBP increased (30%, 24%, and 21% with SBPs < 120 mm Hg, 120-140 mm Hg, and > 140 mm Hg, respectively).72
Risk Scores
In a prospective, observational cohort study of 1,100 ED patients, the Ottawa Heart Failure Risk Scale, combined with NTproBNP values, had a sensitivity of 95.8%—at the cost of increasing the admission rate (from 60.8% to 88%)—for serious adverse events (defined as death within 30 days), admission to a monitored unit, intubation, NIV, MI, or relapse resulting in hospital admission within 14 days.73
Observation Unit
Overall, 44% of in-patient HF admissions are for less than 3 days (Table 1),2 supporting the practice of managing selected patients in shorter clinical-care environments than in inpatient units. Further, ED patients presenting with moderate dyspnea require both a diagnosis and an evaluation of their therapeutic response to determine the need for hospitalization. However, evaluating therapeutic response requires more time than is available in the typical ED. Thus, an ED OU offers the following:
(1) The OU provides the EP with a longer evaluation time, and therefore a more accurate disposition may be effected;
(2) Costs are significantly lower in patients managed in an ED OU; and
(3) Patient satisfaction may be improved, as most patients prefer home management over hospitalization.
All three of these opportunities are supported by a number of studies,74-78 with validated entry and exclusion criteria, treatment algorithms and discharge metrics. Most recently, in a registry of hospitals in Spain registry, patients presenting to hospitals that had OUs had a 2.2-day shorter LOS, lower 30-day ED revisit rate, and similar mortality rates compared to those in institutions without OUs—although these beneficial effects occurred at the cost of an 8.9% higher admission rate.79
Patient Education
Intuitively, it would be expected that patient education would reduce return visits, 30-day hospitalizations, and AHF-related mortality. Unfortunately, it has not been demonstrated that patient education results in a consistent benefit at hospital discharge, or in the outpatient environment.80-85
Although AHF education in the ED has been poorly studied, areas that have shown promise are education occurring before ED management (ie, in the ED waiting area) in underinsured patients,86 and during ED care for patients with poor health care literacy.87 As educational interventions are both inexpensive and unlikely to result in harm, their implementation should be considered.
Conclusion
The spectrum of HF is a common presentation in the ED. Because HF generally appears as dyspnea, in a cohort with multiple comorbidities, the diagnosis can be challenging. This is complicated by the fact that patients with severe presentations may require life-saving interventions long before a clinical evaluation is completed (or even initiated). The skill of the EP, and his or her ability to improve the clinical condition before intubation is required, will determine the patient’s trajectory. Conversely, as a chronic condition, HF may present with moderate symptoms for which a short diuretic “tune-up” in an observation environment may be appropriate.
How these decisions are made will depend upon the local environment, the availability of outpatient resources, and individual patient choices. There are few chronic diseases that are more complex, are seen more often in the ED, or that require more skill and finesse in management.
1. Benjamin EJ, Blaha MJ, Chiuve SE, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation. 2017;135(10):e146-e603.
2. Fitch KV, Engel T, Lauet J. The cost burden of worsening heart failure in the Medicare fee for service population: an actuarial analysis. Milliman Web site. 2017. http://www.milliman.com/insight/2017/The-cost-burden-of-worsening-heart-failure-in-the-Medicare-fee-for-service-population-An-actuarial-analysis/ Published April 3, 2017. Accessed June 1, 2017.
3. Yancy CW, Jessup M, Bozkurt B, et al; American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2013. J Am Coll Cardiol. 2013;62(16):e147-e239. doi:10.1016/j.jacc.2013.05.019.
4. Chen J, Normand SL, Wang Y, Krumholz HM. National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries, 1998-2008. JAMA. 2011;306(15):1669-1678. doi:10.1001/jama.2011.1474.
5. Heidenreich PA, Albert NM, Allen LA, et al; American Heart Association Advocacy Coordinating Committee; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular Radiology and Intervention; Council on Clinical Cardiology; Council on Epidemiology and Prevention; Stroke Council. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6(3):606-619. doi:10.1161/HHF.0b013e318291329a.
6. Dunlay SM, Shah ND, Shi Q, et al. Lifetime costs of medical care after heart failure diagnosis. Circ Cardiovasc Qual Outcomes. 2011;4(1):68-75. doi:10.1161/CIRCOUTCOMES.110.957225.
7. HCUP National Inpatient Sample (NIS); 2014 Agency for Healthcare Research and Quality (AHRQ). HCUPnet Healthcare Cost and Utilization Project. http://bit.ly/2u2ymFA. Published 2014. Accessed July 27, 2017.
8. FY 2017 Final Rule and Correction Notice Tables. CMS 2014 data based on DRGs, Table 5:List of MS-DRGs, Relative Weighting Factors and Geometric and Arithmetic Mean Length of Stay. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/FY2017-IPPS-Final-Rule-Home-Page-Items/FY2017-IPPS-Final-Rule-Tables.html. Published 2017. Accessed August 28, 2017.
9. Hospital Adjusted Expenses per Inpatient Day by Ownership. Kaiser Family Foundation. http://www.kff.org/health-costs/state-indicator/expenses-per-inpatient-day-by-ownership/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. Accessed August 2, 2017
10. Ellison, A. Average cost per inpatient day across 50 states. Becker’s Hospital CFO Report. http://www.beckershospitalreview.com/finance/average-cost-per-inpatient-day-across-50-states-2016.html. Published January 13, 2016. Accessed August 2, 2017
11. Claret PG, Calder LA, Stiell IG, et al. Rates and predictive factors of return to the emergency department following an initial release by the emergency department for acute heart failure. [published online ahead of print April 3, 2017]. CJEM. 1-8. doi:10.1017/cem.2017.14.
12. Yam FK, Lew T, Eraly SA, Lin HW, Hirsch JD, Devor M. Changes in medication regimen complexity and the risk for 90-day hospital readmission and/or emergency department visits in U.S. Veterans with heart failure. Res Social Adm Pharm. 2016;12(5):713-721. doi:10.1016/j.sapharm.2015.10.004.
13. Readmissions Reduction Program. CMS. https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html Updated April 18, 2016. Accessed July 13, 2017.
14. Nowak RM, Reed BP, DiSomma S, et al. Presenting phenotypes of acute heart failure patients in the ED: Identification and implications. Am J Emerg Med. 2017;35(4):536-542. doi:10.1016/j.ajem.2016.12.003.
15. Bennett SJ, Huster GA, Baker SL, et al. Characterization of the precipitants of hospitalization for heart failure decompensation. Am J Crit Care. 1998;7(3):168-174.
16. Kuo DC, Peacock WF. Diagnosing and managing acute heart failure in the emergency department. Clin Exp Emerg Med. 2015;2(3):141-149. eCollection 2015 Sep. doi:10.15441/ceem.15.007.
17. Wang CS, FitzGerald JM, Schulzer M, Mak E, Ayas NT. Does this dyspneic patient in the emergency department have congestive heart failure? JAMA. 2005;294:1944-1956.
18. Koga T, Fujimoto K. Images in clinical medicine. Kerley’s A, B, and C line. N Engl J Med. 2009;360(15):1539. doi:10.1056/NEJMicm0708489.
19. Glöckner E, Christ M, Geier F, et al. Accuracy of point-of-care B-Line lung ultrasound in comparison to NT-ProBNP for screening acute heart failure. Ultrasound Int Open. 2016;2(3):e90-e92. doi:10.1055/s-0042-108343.
20. Bitar Z, Maadarani O, Almerri K. Sonographic chest B-lines anticipate elevated B-type natriuretic peptide level, irrespective of ejection fraction. Ann Intensive Care. 2015;5(1): 56. doi:10.1186/s13613-015-0100-x.
21. Miglioranza MH, Gargani L, Sant’Anna RT, et al. Lung ultrasound for the evaluation of pulmonary congestion in outpatients: a comparison with clinical assessment, natriuretic peptides, and echocardiography. JACC Cardiovasc Imaging. 2013;6(11):1141-1151. doi:10.1016/j.jcmg.2013.08.004.
22. Anderson KL, Jenq KY, Fields JM, Panebianco NL, Dean AJ. Diagnosing heart failure among acutely dyspneic patients with cardiac, inferior vena cava, and lung ultrasonography. Am J Emerg Med. 2013;31(8):1208-1214. doi:10.1016/j.ajem.2013.05.007.
23. Cubo-Romano P, Torres-Macho J, Soni NJ, et al. Admission inferior vena cava measurements are associated with mortality after hospitalization for acute decompensated heart failure. J Hosp Med. 2016;11(11):778-784. doi:10.1002/jhm.2620.
24. Martínez PG, Martínez DM, García JC, Loidi JC. Amino-terminal pro–B-type natriuretic peptide, inferior vena cava ultrasound, and bioelectrical impedance analysis for the diagnosis of acute decompensated CHF. Am J Emerg Med. 2016;34(9): 1817–1822. doi:10.1016/j.ajem.2016.06.043.

25. Maisel AS, Krishnaswamy P, Nowak RM, et al; Breathing Not Properly Multinational Study Investigators. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med. 2002;347(3):161-167.
26. Van Kimmenade RR, Pinto YM, Bayes-Genis A, Lainchbury JG, Richards AM, Januzzi JL Jr. Usefulness of intermediate amino-terminal pro-brain natriuretic peptide concentrations for diagnosis and prognosis of acute heart failure. Am J Cardiol. 2006;98(3):386-390.
27. Moe GW, Howlett J, Januzzi JL, Zowall H; Canadian Multicenter Improved Management of Patients With Congestive Heart Failure (IMPROVE-CHF) Study Investigators. N-terminal pro-B-type natriuretic peptide testing improves the management of patients with suspected acute heart failure: primary results of the Canadian prospective randomized multicenter IMPROVE-CHF study. Circulation. 2007;115(24):3103-3110.
28. Mayo DD, Colletti JE, Kuo DC. Brain natriuretic peptide (BNP) testing in the emergency department. J Emerg Med. 2006;31(2):201-210.
29. Mueller C, Scholer A, Laule-Kilian K, et al. Use of B-type natriuretic peptide in the evaluation and management of acute dyspnea. N Engl J Med. 2004;350(7):647-654.
30. Krauser DG, Lloyd-Jones DM, Chae CU, et al. Effect of body mass index on natriuretic peptide levels in patients with acute congestive heart failure: a ProBNP Investigation of Dyspnea in the Emergency Department (PRIDE) substudy. Am Heart J. 2005;149(4):744-750.
31. McCullough PA, Duc P, Omland T, et al. B-type natriuretic peptide and renal function in the diagnosis of heart failure: an analysis from the Breathing Not Properly Multinational Study. Am J Kidney Dis. 2003;41(3):571-579.
32. Jacob J, Roset A, Miró Ò, et al; ICA-SEMES Research Group. EAHFE - TROPICA2 study. Prognostic value of troponin in patients with acute heart failure treated in Spanish hospital emergency departments. Biomarkers. 2017;22(3-4):337-344. doi:10.1080/1354750X.2016.1265006.
33. Fonarow GC, Adams KF Jr, Abraham WT, et al; ADHERE Scientific Advisory Committee, Study Group, and Investigators. Risk stratification for in-hospital mortality in acutely decompensated heart failure: classification and regression tree analysis. JAMA. 2005;293(5):572-580.
34. Burkhardt J, Peacock WF, Emerman CL. Predictors of emergency department observation unit outcomes. Acad Emerg Med. 2005;12(9):869-874.
35. Schanz M, Shi J, Wasser C, Alscher MD, Kimmel M. Urinary [TIMP-2] × [IGFBP7] for risk prediction of acute kidney injury in decompensated heart failure. Clin Cardiol. 2017;40(7):485-491. doi:10.1002/clc.22683.
36. Kushner RF, Schoeller DA, Fjeld CR, Danford L: Is the impedance index (ht2/R) significant in predicting total body water? Am J Clin Nutr. 1992;56(5): 835-839.
37. Ackland GL, Singh-Ranger D, Fox S, et al. Assessment of preoperative fluid depletion using bioimpedance analysis. Br J Anaesth. 2004;92(1): 134-136.
38. Uszko-Lencer NH, Bothmer F, van Pol PE, Schols AM. Measuring body composition in chronic heart failure: a comparison of methods. Eur J Heart Fail. 2006;8(2): 208-214.
39. Santarelli S, Russo V, Lalle I, et al; GREAT network. Usefulness of combining admission brain natriuretic peptide (BNP) plus hospital discharge bioelectrical impedance vector analysis (BIVA) in predicting 90 days cardiovascular mortality in patients with acute heart failure. Intern Emerg Med. 2017;12(4):445-451. doi:10.1007/s11739-016-1581-9.
40. Parrinello G, Paterna S, Di Pasquale P, et al. The usefulness of bioelectrical impedance analysis in differentiating dyspnea due to decompensated heart failure. J Card Fail. 2008;14(8): 676-686. doi:10.1016/j.cardfail.2008.04.005.
41. Valle R, Aspromonte N, Carbonieri E, et al. Fall in readmission rate for heart failure after implementation of B-type natriuretic peptide testing for discharge decision: a retrospective study. Int J Cardiol. 2008;126(3): 400-406.
42. Sartini S, Frizzi J, Borselli M, et al. Which method is best for an early accurate diagnosis of acute heart failure? Comparison between lung ultrasound, chest X-ray and NT pro-BNP performance: a prospective study. [published online ahead of print July 11, 2016]. Intern Emerg Med. doi:10.1007/s11739-016-1498-3.
43. Steinhart BD, Levy P, Vandenberghe H, et al. A randomized control trial using a validated prediction model for diagnosing acute heart failure in undifferentiated dyspneic emergency department patients-results of the GASP4Ar study. J Card Fail. 2017;23(2):145-152. doi:10.1016/j.cardfail.2016.08.007.
44. Tallman TA, Peacock WF, Emerman CL, et al; ADHERE Registry. Noninvasive ventilation outcomes in 2,430 acute decompensated heart failure patients: an ADHERE registry analysis. Acad EM. 2008;15(4):355–362. doi:10.1111/j.1553-2712.2008.00059.x.
45. Pang D, Keenan SP, Cook DJ, Sibbald WJ. The effect of positive pressure airway support on mortality and the need for intubation in cardiogenic pulmonary edema: a systematic review. Chest. 1998;114(4):1185-1192.
46. Peter JV, Moran JL, Phillips-Hughes J, Graham P, Bersten AD. Effect of non-invasive positive pressure ventilation (NIPPV) on mortality in patients with acute cardiogenic pulmonary oedema: a meta-analysis. Lancet. 2006;367(9517):1155-1163.
47. Weng CL, Zhao YT, Liu QH, et al. Meta-analysis: Noninvasive ventilation in acute cardiogenic pulmonary edema. Ann Intern Med. 2010;152(9):590-600
48. Vital FM, Saconato H, Ladeira MT, et al. Noninvasive positive pressure ventilation (CPAP or bilevel NPPV) for cardiogenic pulmonary edema. Cochrane Database Syst Rev. 2008;(3):CD005351. doi:10.1002/14651858.CD005351.pub2.
49. Vital FM, Ladeira MT, Atallah AN. Non-invasive positive pressure ventilation (CPAP or bilevel NPPV) for cardiogenic pulmonary oedema. Cochrane Database Syst Rev. 2013;(5):CD005351. doi:10.1002/14651858.CD005351.pub3.
50. Gray A, Goodacre S, Seah M, Tilley S. Diuretic, opiate and nitrate use in severe acidotic acute cardiogenic pulmonary oedema: analysis from the 3CPO trial. QJM. 2010;103(8):573-581. doi:10.1093/qjmed/hcq077.
51. Collins SP, Storrow AB, Levy PD, et al. Early management of patients with acute heart failure: state of the art and future directions—a consensus document from the SAEM/HFSA acute heart failure working group. Acad Emerg Med. 2015;22(1):94-112. doi:10.1111/acem.12538.]
52. O’Connor CM, Gattis WA, Uretsky BF, et al. Continuous intravenous dobutamine is associated with an increased risk of death in patients with advanced heart failure: insights from the Flolan International Randomized Survival Trial (FIRST). Am Heart J. 1999;138(1 Pt 1):78-86.
53. Hershberger RE, Nauman D, Walker TL, Dutton D, Burgess D. Care processes and clinical outcomes of continuous outpatient support with inotropes (COSI) in patients with refractory endstage heart failure. J Card Fail. 2003;(9):180-187.
54. Gorodeski EZ, Chu EC, Reese JR, Shishehbor MH, Hsich E, Starling RC. Prognosis on chronic dobutamine or milrinone infusions for stage D heart failure. Circ Heart Fail. 2009;2(4):320-324. doi:10.1161/CIRCHEARTFAILURE.108.839076.
55. Collins SP, Levy PD, Martindale JL, et al. Clinical and research considerations for patients with hypertensive acute heart failure: A consensus statement from the Society for Academic Emergency Medicine and the Heart Failure Society of America Acute Heart Failure Working Group. Acad Emerg Med. 2016;23(8):922-931. doi:10.1111/acem.13025.
56. Felker GM, Lee KL, Bull DA, et al. Diuretic strategies in patients with acute decompensated heart failure. N Engl J Med. 2011; 364(9):797-805. doi:10.1056/NEJMoa1005419.

57. Publication Committee for the VMAC Investigators (Vasodilatation in the Management of Acute CHF). Intravenous nesiritide vs nitroglycerin for treatment of decompensated congestive heart failure: a randomized controlled trial. JAMA. 2002;287(12):1531-1540.
58. Gradman AH, Vekeman F, Eldar-Lissai A, Trahey A, Ong SH, Duh MS. Is addition of vasodilators to loop diuretics of value in the care of hospitalized acute heart failure patients? Real-world evidence from a retrospective analysis of a large United States hospital database. J Card Fail. 2014;20(11):853-863. doi:10.1016/j.cardfail.2014.08.006.
59. Wilson SS, Kwiatkowski GM, Millis SR, Purakal JD, Mahajan AP, Levy PD. Use of nitroglycerin by bolus prevents intensive care unit admission in patients with acute hypertensive heart failure. Am J Emerg Med. 2017;35(1):126-131. doi:10.1016/j.ajem.2016.10.038.
60. Eryonucu B, Guler N, Guntekin U, Tuncer M. Comparison of the effects of nitroglycerin and nitroprusside on transmitral Doppler flow parameters in patients with hypertensive urgency. Ann Pharmacother. 2005;39(6):997–1001.
61. O’Connor CM, Starling RC, Hernandez AF, et al. Effect of nesiritide in patients with acute decompensated heart failure. N Engl J Med. 2011;365(1):32-43. doi:10.1056/NEJMoa1100171.
62. Peacock WF 4th, Holland R, Gyarmathy R, et al. Observation unit treatment of heart failure with nesiritide: results from the proaction trial. J Emerg Med. 2005;29(3):243-252.
63. Ayaz SI, Sharkey CM, Kwiatkowski GM, et al. Intravenous enalaprilat for treatment of acute hypertensive heart failure in the emergency department. Int J Emerg Med. 2016;9(1):28. doi:10.1186/s12245-016-0125-4.
64. Peacock WF 4th, Chandra A, Char D, et al. Clevidipine in acute heart failure: results of the A study of BP control in acute heart failure-a pilot study (PRONTO). Am Heart J. 2014;167(4):529-536. doi:10.1016/j.ahj.2013.12.023.
65. Peacock WF 4th, Hollander JE, Diercks DB, et al. Morphine and outcomes in acute decompensated heart failure: an ADHERE analysis. Emerg Med J. 2008;25(4):205-209. doi:10.1136/emj.2007.050419.
66. Miró Ò, Gil V, Martín-Sánchez FJ, Herrero-Puente P, Jet al; ICA-SEMES Research Group. Morphine use in the ED and outcomes of patients with acute heart failure: a propensity score-matching analysis based on the EAHFE registry. [published ahead of print April 12, 2017] Chest. pii:S0012-3692(17)30707-9. doi:10.1016/j.chest.2017.03.037.
67. Wuerz RC, Meador SA. Effects of prehospital medications on mortality and length of stay in congestive heart failure. Ann Emerg Med. 1992;21(6):669-674.
68. Peacock WF 4th, Fonarow GC, Emerman CL, Mills RM, Wynne J; ADHERE Scientific Advisory Committee and Investigators; Adhere Study Group. Impact of early initiation of intravenous therapy for acute decompensated heart failure on outcomes in ADHERE. Cardiology. 2007; 107(1):44-51. doi:10.1159/000093612.
69. Peacock WF, Emerman C, Costanzo MR, Diercks DB, Lopatin M, Fonarow GC. Early vasoactive drugs improve heart failure outcomes. Congest Heart Fail. 2009;15(6): 256-264. doi:10.1111/j.1751-7133.2009.00112.x.
70. Maisel AS, Peacock WF, McMullin N, et al. Timing of immunoreactive B-type natriuretic peptide levels and treatment delay in acute decompensated heart failure: an ADHERE (Acute Decompensated Heart Failure National Registry) analysis. J Am Coll Cardiol. 2008;52(7):534-540. doi:10.1016/j.jacc.2008.05.010.
71. Matsue Y, Damman K, Voors AA, et al. Time-to-Furosemide Treatment and Mortality in Patients Hospitalized With Acute Heart Failure. J Am Coll Cardiol. 2017 Jun 27;69(25):3042-3051. doi:10.1016/j.jacc.2017.04.042.
72. Claret PG, Stiell IG, Yan JW, et al. Hemodynamic, management, and outcomes of patients admitted to emergency department with heart failure. Scand J Trauma Resusc Emerg Med. 2016;24(1):132.
73. Stiell IG, Perry JJ, Clement CM, et al. Prospective and explicit clinical validation of the Ottawa Heart Failure Risk Scale, with and without use of quantitative NT-proBNP. Acad Emerg Med. 2017;24(3):316-327. doi:10.1111/acem.13141.
74. Pang PS, Jesse R, Collins SP, Maisel A. Patients with acute heart failure in the emergency department: do they all need to be admitted? J Card Fail. 2012;18:900-903. doi:10.1016/j.cardfail.2012.10.014.
75. Peacock WF 4th, Young J, Collins S, Emerman C, Diercks D. Heart failure observation units: optimizing care. Ann Emerg Med. 2006;47(1):22-33.
76. Storrow AB, Collins SP, Lyons MS, Wagoner LE, Gibler WB, Lindsell CJ. Emergency department observation of heart failure: preliminary analysis of safety and cost. Congest Heart Fail. 2005;11(2):68-72.
77. Peacock WF 4th, Remer EE, Aponte J, Moffa DA, Emerman CE, Albert NM. Effective observation unit treatment of decompensated heart failure. Congest Heart Fail. 2002;8(2):68 -73.
78. Peacock WF 4th, Albert NM. Observation unit management of heart failure. Emerg Med Clin North Am. 2001;19(1):209-232.
79. Miró O, Carbajosa V, Peacock WF 4th, et al; ICA-SEMES group. The effect of a short-stay unit on hospital admission and length of stay in acute heart failure: REDUCE-AHF study. Eur J Intern Med. 2017;40:30-36. doi:10.1016/j.ejim.2017.01.015.
80. Ekman I, Andersson B, Ehnfors M, Matejka G, Persson B, Fagerberg B. Feasibility of a nurse-monitored, outpatient-care programme for elderly patients with moderate-to-severe, chronic heart failure. Eur Heart J. 1998;19(8):1254-1260.
81. Riegel B, Carlson B, Kopp Z, LePetri B, Glaser D, Unger A. Effect of a standardized nurse case-management telephone intervention on resource use in patients with chronic heart failure. Arch Intern Med. 2002;162(6):705-712.
82. Laramee AS, Levinsky SK, Sargent J, Ross R, Callas P. Case management in a heterogeneous congestive heart failure population: a randomized controlled trial. Arch Intern Med. 2003;163(7):809-817.
83. Stewart S, Pearson S, Horowitz JD. Effects of a home-based intervention among patients with congestive heart failure discharged from acute hospital care. Arch Intern Med. 1998;158(10):1067-1072.
84. Stewart S, Marley JE, Horowitz JD. Effects of a multidisciplinary, home-based intervention on unplanned readmissions and survival among patients with chronic congestive heart failure: a randomised controlled study. Lancet. 1999;354(9184):1077-1083.
85. Weinberger M, Oddone EZ, Henderson WG; Veterans Affairs Cooperative Study Group. Does increased access to primary care reduce hospital readmissions? Veterans Affairs Cooperative Study Group on primary care and hospital readmission. N Engl J Med. 1996;334(22):1441-1447.
86. Asthana V, Sundararajan M, Karun V, et al. Educational strategy for management of heart failure markedly reduces 90-day emergency department and hospital readmissions in un- and underinsured patients. J Am Coll Cardiol. 2017;69(11Suppl): 780. doi:10.1016/S0735-1097(17)34169-4.
87. Bell SP, Schnipper JL, Goggins K, et al; Pharmacist Intervention for Low Literacy in Cardiovascular Disease (PILL-CVD) Study Group. Effect of pharmacist counseling intervention on health care utilization following hospital discharge: a randomized control trial. J Gen Intern Med. 2016;31(5):470-477. doi:10.1007/s11606-016-3596-3.
1. Benjamin EJ, Blaha MJ, Chiuve SE, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation. 2017;135(10):e146-e603.
2. Fitch KV, Engel T, Lauet J. The cost burden of worsening heart failure in the Medicare fee for service population: an actuarial analysis. Milliman Web site. 2017. http://www.milliman.com/insight/2017/The-cost-burden-of-worsening-heart-failure-in-the-Medicare-fee-for-service-population-An-actuarial-analysis/ Published April 3, 2017. Accessed June 1, 2017.
3. Yancy CW, Jessup M, Bozkurt B, et al; American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2013. J Am Coll Cardiol. 2013;62(16):e147-e239. doi:10.1016/j.jacc.2013.05.019.
4. Chen J, Normand SL, Wang Y, Krumholz HM. National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries, 1998-2008. JAMA. 2011;306(15):1669-1678. doi:10.1001/jama.2011.1474.
5. Heidenreich PA, Albert NM, Allen LA, et al; American Heart Association Advocacy Coordinating Committee; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular Radiology and Intervention; Council on Clinical Cardiology; Council on Epidemiology and Prevention; Stroke Council. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6(3):606-619. doi:10.1161/HHF.0b013e318291329a.
6. Dunlay SM, Shah ND, Shi Q, et al. Lifetime costs of medical care after heart failure diagnosis. Circ Cardiovasc Qual Outcomes. 2011;4(1):68-75. doi:10.1161/CIRCOUTCOMES.110.957225.
7. HCUP National Inpatient Sample (NIS); 2014 Agency for Healthcare Research and Quality (AHRQ). HCUPnet Healthcare Cost and Utilization Project. http://bit.ly/2u2ymFA. Published 2014. Accessed July 27, 2017.
8. FY 2017 Final Rule and Correction Notice Tables. CMS 2014 data based on DRGs, Table 5:List of MS-DRGs, Relative Weighting Factors and Geometric and Arithmetic Mean Length of Stay. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/FY2017-IPPS-Final-Rule-Home-Page-Items/FY2017-IPPS-Final-Rule-Tables.html. Published 2017. Accessed August 28, 2017.
9. Hospital Adjusted Expenses per Inpatient Day by Ownership. Kaiser Family Foundation. http://www.kff.org/health-costs/state-indicator/expenses-per-inpatient-day-by-ownership/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. Accessed August 2, 2017
10. Ellison, A. Average cost per inpatient day across 50 states. Becker’s Hospital CFO Report. http://www.beckershospitalreview.com/finance/average-cost-per-inpatient-day-across-50-states-2016.html. Published January 13, 2016. Accessed August 2, 2017
11. Claret PG, Calder LA, Stiell IG, et al. Rates and predictive factors of return to the emergency department following an initial release by the emergency department for acute heart failure. [published online ahead of print April 3, 2017]. CJEM. 1-8. doi:10.1017/cem.2017.14.
12. Yam FK, Lew T, Eraly SA, Lin HW, Hirsch JD, Devor M. Changes in medication regimen complexity and the risk for 90-day hospital readmission and/or emergency department visits in U.S. Veterans with heart failure. Res Social Adm Pharm. 2016;12(5):713-721. doi:10.1016/j.sapharm.2015.10.004.
13. Readmissions Reduction Program. CMS. https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html Updated April 18, 2016. Accessed July 13, 2017.
14. Nowak RM, Reed BP, DiSomma S, et al. Presenting phenotypes of acute heart failure patients in the ED: Identification and implications. Am J Emerg Med. 2017;35(4):536-542. doi:10.1016/j.ajem.2016.12.003.
15. Bennett SJ, Huster GA, Baker SL, et al. Characterization of the precipitants of hospitalization for heart failure decompensation. Am J Crit Care. 1998;7(3):168-174.
16. Kuo DC, Peacock WF. Diagnosing and managing acute heart failure in the emergency department. Clin Exp Emerg Med. 2015;2(3):141-149. eCollection 2015 Sep. doi:10.15441/ceem.15.007.
17. Wang CS, FitzGerald JM, Schulzer M, Mak E, Ayas NT. Does this dyspneic patient in the emergency department have congestive heart failure? JAMA. 2005;294:1944-1956.
18. Koga T, Fujimoto K. Images in clinical medicine. Kerley’s A, B, and C line. N Engl J Med. 2009;360(15):1539. doi:10.1056/NEJMicm0708489.
19. Glöckner E, Christ M, Geier F, et al. Accuracy of point-of-care B-Line lung ultrasound in comparison to NT-ProBNP for screening acute heart failure. Ultrasound Int Open. 2016;2(3):e90-e92. doi:10.1055/s-0042-108343.
20. Bitar Z, Maadarani O, Almerri K. Sonographic chest B-lines anticipate elevated B-type natriuretic peptide level, irrespective of ejection fraction. Ann Intensive Care. 2015;5(1): 56. doi:10.1186/s13613-015-0100-x.
21. Miglioranza MH, Gargani L, Sant’Anna RT, et al. Lung ultrasound for the evaluation of pulmonary congestion in outpatients: a comparison with clinical assessment, natriuretic peptides, and echocardiography. JACC Cardiovasc Imaging. 2013;6(11):1141-1151. doi:10.1016/j.jcmg.2013.08.004.
22. Anderson KL, Jenq KY, Fields JM, Panebianco NL, Dean AJ. Diagnosing heart failure among acutely dyspneic patients with cardiac, inferior vena cava, and lung ultrasonography. Am J Emerg Med. 2013;31(8):1208-1214. doi:10.1016/j.ajem.2013.05.007.
23. Cubo-Romano P, Torres-Macho J, Soni NJ, et al. Admission inferior vena cava measurements are associated with mortality after hospitalization for acute decompensated heart failure. J Hosp Med. 2016;11(11):778-784. doi:10.1002/jhm.2620.
24. Martínez PG, Martínez DM, García JC, Loidi JC. Amino-terminal pro–B-type natriuretic peptide, inferior vena cava ultrasound, and bioelectrical impedance analysis for the diagnosis of acute decompensated CHF. Am J Emerg Med. 2016;34(9): 1817–1822. doi:10.1016/j.ajem.2016.06.043.

25. Maisel AS, Krishnaswamy P, Nowak RM, et al; Breathing Not Properly Multinational Study Investigators. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med. 2002;347(3):161-167.
26. Van Kimmenade RR, Pinto YM, Bayes-Genis A, Lainchbury JG, Richards AM, Januzzi JL Jr. Usefulness of intermediate amino-terminal pro-brain natriuretic peptide concentrations for diagnosis and prognosis of acute heart failure. Am J Cardiol. 2006;98(3):386-390.
27. Moe GW, Howlett J, Januzzi JL, Zowall H; Canadian Multicenter Improved Management of Patients With Congestive Heart Failure (IMPROVE-CHF) Study Investigators. N-terminal pro-B-type natriuretic peptide testing improves the management of patients with suspected acute heart failure: primary results of the Canadian prospective randomized multicenter IMPROVE-CHF study. Circulation. 2007;115(24):3103-3110.
28. Mayo DD, Colletti JE, Kuo DC. Brain natriuretic peptide (BNP) testing in the emergency department. J Emerg Med. 2006;31(2):201-210.
29. Mueller C, Scholer A, Laule-Kilian K, et al. Use of B-type natriuretic peptide in the evaluation and management of acute dyspnea. N Engl J Med. 2004;350(7):647-654.
30. Krauser DG, Lloyd-Jones DM, Chae CU, et al. Effect of body mass index on natriuretic peptide levels in patients with acute congestive heart failure: a ProBNP Investigation of Dyspnea in the Emergency Department (PRIDE) substudy. Am Heart J. 2005;149(4):744-750.
31. McCullough PA, Duc P, Omland T, et al. B-type natriuretic peptide and renal function in the diagnosis of heart failure: an analysis from the Breathing Not Properly Multinational Study. Am J Kidney Dis. 2003;41(3):571-579.
32. Jacob J, Roset A, Miró Ò, et al; ICA-SEMES Research Group. EAHFE - TROPICA2 study. Prognostic value of troponin in patients with acute heart failure treated in Spanish hospital emergency departments. Biomarkers. 2017;22(3-4):337-344. doi:10.1080/1354750X.2016.1265006.
33. Fonarow GC, Adams KF Jr, Abraham WT, et al; ADHERE Scientific Advisory Committee, Study Group, and Investigators. Risk stratification for in-hospital mortality in acutely decompensated heart failure: classification and regression tree analysis. JAMA. 2005;293(5):572-580.
34. Burkhardt J, Peacock WF, Emerman CL. Predictors of emergency department observation unit outcomes. Acad Emerg Med. 2005;12(9):869-874.
35. Schanz M, Shi J, Wasser C, Alscher MD, Kimmel M. Urinary [TIMP-2] × [IGFBP7] for risk prediction of acute kidney injury in decompensated heart failure. Clin Cardiol. 2017;40(7):485-491. doi:10.1002/clc.22683.
36. Kushner RF, Schoeller DA, Fjeld CR, Danford L: Is the impedance index (ht2/R) significant in predicting total body water? Am J Clin Nutr. 1992;56(5): 835-839.
37. Ackland GL, Singh-Ranger D, Fox S, et al. Assessment of preoperative fluid depletion using bioimpedance analysis. Br J Anaesth. 2004;92(1): 134-136.
38. Uszko-Lencer NH, Bothmer F, van Pol PE, Schols AM. Measuring body composition in chronic heart failure: a comparison of methods. Eur J Heart Fail. 2006;8(2): 208-214.
39. Santarelli S, Russo V, Lalle I, et al; GREAT network. Usefulness of combining admission brain natriuretic peptide (BNP) plus hospital discharge bioelectrical impedance vector analysis (BIVA) in predicting 90 days cardiovascular mortality in patients with acute heart failure. Intern Emerg Med. 2017;12(4):445-451. doi:10.1007/s11739-016-1581-9.
40. Parrinello G, Paterna S, Di Pasquale P, et al. The usefulness of bioelectrical impedance analysis in differentiating dyspnea due to decompensated heart failure. J Card Fail. 2008;14(8): 676-686. doi:10.1016/j.cardfail.2008.04.005.
41. Valle R, Aspromonte N, Carbonieri E, et al. Fall in readmission rate for heart failure after implementation of B-type natriuretic peptide testing for discharge decision: a retrospective study. Int J Cardiol. 2008;126(3): 400-406.
42. Sartini S, Frizzi J, Borselli M, et al. Which method is best for an early accurate diagnosis of acute heart failure? Comparison between lung ultrasound, chest X-ray and NT pro-BNP performance: a prospective study. [published online ahead of print July 11, 2016]. Intern Emerg Med. doi:10.1007/s11739-016-1498-3.
43. Steinhart BD, Levy P, Vandenberghe H, et al. A randomized control trial using a validated prediction model for diagnosing acute heart failure in undifferentiated dyspneic emergency department patients-results of the GASP4Ar study. J Card Fail. 2017;23(2):145-152. doi:10.1016/j.cardfail.2016.08.007.
44. Tallman TA, Peacock WF, Emerman CL, et al; ADHERE Registry. Noninvasive ventilation outcomes in 2,430 acute decompensated heart failure patients: an ADHERE registry analysis. Acad EM. 2008;15(4):355–362. doi:10.1111/j.1553-2712.2008.00059.x.
45. Pang D, Keenan SP, Cook DJ, Sibbald WJ. The effect of positive pressure airway support on mortality and the need for intubation in cardiogenic pulmonary edema: a systematic review. Chest. 1998;114(4):1185-1192.
46. Peter JV, Moran JL, Phillips-Hughes J, Graham P, Bersten AD. Effect of non-invasive positive pressure ventilation (NIPPV) on mortality in patients with acute cardiogenic pulmonary oedema: a meta-analysis. Lancet. 2006;367(9517):1155-1163.
47. Weng CL, Zhao YT, Liu QH, et al. Meta-analysis: Noninvasive ventilation in acute cardiogenic pulmonary edema. Ann Intern Med. 2010;152(9):590-600
48. Vital FM, Saconato H, Ladeira MT, et al. Noninvasive positive pressure ventilation (CPAP or bilevel NPPV) for cardiogenic pulmonary edema. Cochrane Database Syst Rev. 2008;(3):CD005351. doi:10.1002/14651858.CD005351.pub2.
49. Vital FM, Ladeira MT, Atallah AN. Non-invasive positive pressure ventilation (CPAP or bilevel NPPV) for cardiogenic pulmonary oedema. Cochrane Database Syst Rev. 2013;(5):CD005351. doi:10.1002/14651858.CD005351.pub3.
50. Gray A, Goodacre S, Seah M, Tilley S. Diuretic, opiate and nitrate use in severe acidotic acute cardiogenic pulmonary oedema: analysis from the 3CPO trial. QJM. 2010;103(8):573-581. doi:10.1093/qjmed/hcq077.
51. Collins SP, Storrow AB, Levy PD, et al. Early management of patients with acute heart failure: state of the art and future directions—a consensus document from the SAEM/HFSA acute heart failure working group. Acad Emerg Med. 2015;22(1):94-112. doi:10.1111/acem.12538.]
52. O’Connor CM, Gattis WA, Uretsky BF, et al. Continuous intravenous dobutamine is associated with an increased risk of death in patients with advanced heart failure: insights from the Flolan International Randomized Survival Trial (FIRST). Am Heart J. 1999;138(1 Pt 1):78-86.
53. Hershberger RE, Nauman D, Walker TL, Dutton D, Burgess D. Care processes and clinical outcomes of continuous outpatient support with inotropes (COSI) in patients with refractory endstage heart failure. J Card Fail. 2003;(9):180-187.
54. Gorodeski EZ, Chu EC, Reese JR, Shishehbor MH, Hsich E, Starling RC. Prognosis on chronic dobutamine or milrinone infusions for stage D heart failure. Circ Heart Fail. 2009;2(4):320-324. doi:10.1161/CIRCHEARTFAILURE.108.839076.
55. Collins SP, Levy PD, Martindale JL, et al. Clinical and research considerations for patients with hypertensive acute heart failure: A consensus statement from the Society for Academic Emergency Medicine and the Heart Failure Society of America Acute Heart Failure Working Group. Acad Emerg Med. 2016;23(8):922-931. doi:10.1111/acem.13025.
56. Felker GM, Lee KL, Bull DA, et al. Diuretic strategies in patients with acute decompensated heart failure. N Engl J Med. 2011; 364(9):797-805. doi:10.1056/NEJMoa1005419.

57. Publication Committee for the VMAC Investigators (Vasodilatation in the Management of Acute CHF). Intravenous nesiritide vs nitroglycerin for treatment of decompensated congestive heart failure: a randomized controlled trial. JAMA. 2002;287(12):1531-1540.
58. Gradman AH, Vekeman F, Eldar-Lissai A, Trahey A, Ong SH, Duh MS. Is addition of vasodilators to loop diuretics of value in the care of hospitalized acute heart failure patients? Real-world evidence from a retrospective analysis of a large United States hospital database. J Card Fail. 2014;20(11):853-863. doi:10.1016/j.cardfail.2014.08.006.
59. Wilson SS, Kwiatkowski GM, Millis SR, Purakal JD, Mahajan AP, Levy PD. Use of nitroglycerin by bolus prevents intensive care unit admission in patients with acute hypertensive heart failure. Am J Emerg Med. 2017;35(1):126-131. doi:10.1016/j.ajem.2016.10.038.
60. Eryonucu B, Guler N, Guntekin U, Tuncer M. Comparison of the effects of nitroglycerin and nitroprusside on transmitral Doppler flow parameters in patients with hypertensive urgency. Ann Pharmacother. 2005;39(6):997–1001.
61. O’Connor CM, Starling RC, Hernandez AF, et al. Effect of nesiritide in patients with acute decompensated heart failure. N Engl J Med. 2011;365(1):32-43. doi:10.1056/NEJMoa1100171.
62. Peacock WF 4th, Holland R, Gyarmathy R, et al. Observation unit treatment of heart failure with nesiritide: results from the proaction trial. J Emerg Med. 2005;29(3):243-252.
63. Ayaz SI, Sharkey CM, Kwiatkowski GM, et al. Intravenous enalaprilat for treatment of acute hypertensive heart failure in the emergency department. Int J Emerg Med. 2016;9(1):28. doi:10.1186/s12245-016-0125-4.
64. Peacock WF 4th, Chandra A, Char D, et al. Clevidipine in acute heart failure: results of the A study of BP control in acute heart failure-a pilot study (PRONTO). Am Heart J. 2014;167(4):529-536. doi:10.1016/j.ahj.2013.12.023.
65. Peacock WF 4th, Hollander JE, Diercks DB, et al. Morphine and outcomes in acute decompensated heart failure: an ADHERE analysis. Emerg Med J. 2008;25(4):205-209. doi:10.1136/emj.2007.050419.
66. Miró Ò, Gil V, Martín-Sánchez FJ, Herrero-Puente P, Jet al; ICA-SEMES Research Group. Morphine use in the ED and outcomes of patients with acute heart failure: a propensity score-matching analysis based on the EAHFE registry. [published ahead of print April 12, 2017] Chest. pii:S0012-3692(17)30707-9. doi:10.1016/j.chest.2017.03.037.
67. Wuerz RC, Meador SA. Effects of prehospital medications on mortality and length of stay in congestive heart failure. Ann Emerg Med. 1992;21(6):669-674.
68. Peacock WF 4th, Fonarow GC, Emerman CL, Mills RM, Wynne J; ADHERE Scientific Advisory Committee and Investigators; Adhere Study Group. Impact of early initiation of intravenous therapy for acute decompensated heart failure on outcomes in ADHERE. Cardiology. 2007; 107(1):44-51. doi:10.1159/000093612.
69. Peacock WF, Emerman C, Costanzo MR, Diercks DB, Lopatin M, Fonarow GC. Early vasoactive drugs improve heart failure outcomes. Congest Heart Fail. 2009;15(6): 256-264. doi:10.1111/j.1751-7133.2009.00112.x.
70. Maisel AS, Peacock WF, McMullin N, et al. Timing of immunoreactive B-type natriuretic peptide levels and treatment delay in acute decompensated heart failure: an ADHERE (Acute Decompensated Heart Failure National Registry) analysis. J Am Coll Cardiol. 2008;52(7):534-540. doi:10.1016/j.jacc.2008.05.010.
71. Matsue Y, Damman K, Voors AA, et al. Time-to-Furosemide Treatment and Mortality in Patients Hospitalized With Acute Heart Failure. J Am Coll Cardiol. 2017 Jun 27;69(25):3042-3051. doi:10.1016/j.jacc.2017.04.042.
72. Claret PG, Stiell IG, Yan JW, et al. Hemodynamic, management, and outcomes of patients admitted to emergency department with heart failure. Scand J Trauma Resusc Emerg Med. 2016;24(1):132.
73. Stiell IG, Perry JJ, Clement CM, et al. Prospective and explicit clinical validation of the Ottawa Heart Failure Risk Scale, with and without use of quantitative NT-proBNP. Acad Emerg Med. 2017;24(3):316-327. doi:10.1111/acem.13141.
74. Pang PS, Jesse R, Collins SP, Maisel A. Patients with acute heart failure in the emergency department: do they all need to be admitted? J Card Fail. 2012;18:900-903. doi:10.1016/j.cardfail.2012.10.014.
75. Peacock WF 4th, Young J, Collins S, Emerman C, Diercks D. Heart failure observation units: optimizing care. Ann Emerg Med. 2006;47(1):22-33.
76. Storrow AB, Collins SP, Lyons MS, Wagoner LE, Gibler WB, Lindsell CJ. Emergency department observation of heart failure: preliminary analysis of safety and cost. Congest Heart Fail. 2005;11(2):68-72.
77. Peacock WF 4th, Remer EE, Aponte J, Moffa DA, Emerman CE, Albert NM. Effective observation unit treatment of decompensated heart failure. Congest Heart Fail. 2002;8(2):68 -73.
78. Peacock WF 4th, Albert NM. Observation unit management of heart failure. Emerg Med Clin North Am. 2001;19(1):209-232.
79. Miró O, Carbajosa V, Peacock WF 4th, et al; ICA-SEMES group. The effect of a short-stay unit on hospital admission and length of stay in acute heart failure: REDUCE-AHF study. Eur J Intern Med. 2017;40:30-36. doi:10.1016/j.ejim.2017.01.015.
80. Ekman I, Andersson B, Ehnfors M, Matejka G, Persson B, Fagerberg B. Feasibility of a nurse-monitored, outpatient-care programme for elderly patients with moderate-to-severe, chronic heart failure. Eur Heart J. 1998;19(8):1254-1260.
81. Riegel B, Carlson B, Kopp Z, LePetri B, Glaser D, Unger A. Effect of a standardized nurse case-management telephone intervention on resource use in patients with chronic heart failure. Arch Intern Med. 2002;162(6):705-712.
82. Laramee AS, Levinsky SK, Sargent J, Ross R, Callas P. Case management in a heterogeneous congestive heart failure population: a randomized controlled trial. Arch Intern Med. 2003;163(7):809-817.
83. Stewart S, Pearson S, Horowitz JD. Effects of a home-based intervention among patients with congestive heart failure discharged from acute hospital care. Arch Intern Med. 1998;158(10):1067-1072.
84. Stewart S, Marley JE, Horowitz JD. Effects of a multidisciplinary, home-based intervention on unplanned readmissions and survival among patients with chronic congestive heart failure: a randomised controlled study. Lancet. 1999;354(9184):1077-1083.
85. Weinberger M, Oddone EZ, Henderson WG; Veterans Affairs Cooperative Study Group. Does increased access to primary care reduce hospital readmissions? Veterans Affairs Cooperative Study Group on primary care and hospital readmission. N Engl J Med. 1996;334(22):1441-1447.
86. Asthana V, Sundararajan M, Karun V, et al. Educational strategy for management of heart failure markedly reduces 90-day emergency department and hospital readmissions in un- and underinsured patients. J Am Coll Cardiol. 2017;69(11Suppl): 780. doi:10.1016/S0735-1097(17)34169-4.
87. Bell SP, Schnipper JL, Goggins K, et al; Pharmacist Intervention for Low Literacy in Cardiovascular Disease (PILL-CVD) Study Group. Effect of pharmacist counseling intervention on health care utilization following hospital discharge: a randomized control trial. J Gen Intern Med. 2016;31(5):470-477. doi:10.1007/s11606-016-3596-3.
Platelet response in practice: Applying new insights and tools for testing and treatment
CASE STUDY: THROMBOSIS AFTER STENTING DESPITE ANTIPLATELET THERAPY
Dr. Deepak Bhatt: We have taken in a wealth of terrific information from the three preceding talks in this symposium. Let’s now share some questions from the audience and explore some of the points raised in the preceding talks in a bit more practical detail for clinicians. Our three prior speakers are joined in this panel discussion by Cleveland Clinic’s Dr. Frank Peacock, who brings an emergency medicine perspective.
Let’s begin with a case-based question supplied from the audience. The patient is a 42-year-old morbidly obese man without diabetes who had a non-ST-elevation myocardial infarction (MI) less than 1 year ago. A drug-eluting stent was placed at the time of his MI, and now restenosis has occurred. He is on aspirin and clopidogrel 75 mg/day. Do you recommend running a vasodilator-stimulated phosphoprotein (VASP) test and possibly increasing the clopidogrel dose to 150 mg/ day, or should the patient just be switched to prasugrel (assuming it is commercially available) without running the VASP test?
I’ll take a quick initial stab at this question. Studies of antiplatelet therapies to prevent instent restenosis have been a mixed bag. Some of the trials with glycoprotein IIb/IIIa inhibitors have shown an effect on restenosis, but most have not. Similarly, some of the analyses of the thienopyridines ticlopodine and clopidogrel have shown an effect on restenosis, but most have not.
For the most part, restenosis does not appear to be heavily mediated by platelets, at least not in a way that we can influence by therapy. On the other hand, stent thrombosis is highly platelet mediated, so I would alter the case to one in which stent thrombosis is the clinical problem. Assuming that the patient has been adherent to his antiplatelet regimen, which tests would you perform, and how would you act on the information from those tests?
Dr. Kandice Kottke-Marchant: The 2007 guidelines on acute coronary syndrome (ACS) management from the American College of Cardiology and American Heart Association (ACC/AHA)1 do not address platelet function testing, and almost none of the clinical trials of antiplatelet agents had an arm that included testing and dose adjustment based on platelet function studies. Platelet testing is available at some centers; at Cleveland Clinic, we use platelet aggregation testing. One can do platelet aggregation testing on a patient-by-patient basis; if inhibition appears to be suboptimal, a treatment decision should be made, but there is little guidance from the literature to steer that decision. I have seen clinicians increase the dose of clopidogrel or aspirin in response to platelet function tests, which occasionally triggers a confirmatory call from the pharmacy department.
Dr. Bhatt: When I was still at Cleveland Clinic, our chief medical resident did an analysis of platelet function testing, and it was remarkable how much testing was performed and how often it changed management, largely in the absence of any outcomes data, as Dr. Kottke-Marchant pointed out. Dr. Alexander, what are your recommendations with respect to platelet function testing today?
Dr. John Alexander: The case you describe is one in which applying evidence is not easy. There are no trials to supply any evidence to change therapy in this patient, a morbidly obese man receiving 75 mg/day of clopidogrel. There is certainly a rationale, however, to believe that a standard “one size fits all” 75-mg daily dose of clopidogrel may not be enough for him. The trade-off with a higher dosage is a higher risk of bleeding, however, so I would first be sure that he has been adherent to his current regimen of clopidogrel and aspirin.
Dr. Bhatt: Is there a role for point-of-care testing to determine whether he is adherent to the medicines?
Dr. Kottke-Marchant: Several of the point-of-care tests, such as the VerifyNow rapid platelet function analyzer, have specific cartridges for aspirin and for clopidogrel. If platelets were not being inhibited, it would suggest that the doses were too low, given the patient’s weight, but you probably would not be able to determine whether he was resistant to clopidogrel.
Dr. W. Frank Peacock: One way to verify that patients are taking their aspirin is to take a small urine sample and squirt in 2 mL of ferric chloride. If the sample turns purple, it means they are taking their aspirin. Once that is established, you can try to determine whether the drug is working on their platelets.
Dr. Alexander: Another potential explanation for stent thrombosis is faulty stent placement. In this case I would consider asking an interventional colleague to perform intravascular ultrasonography to make sure the stent was implanted properly before I changed the patient’s antithrombotic therapy.
Dr. Bhatt: That’s a great technical point. We always want to make sure that a case of stent thrombosis is not due to a mechanical problem. We should be asking: Is the stent properly sized and well opposed? Is there a distal dissection or any other issue that could predispose to stent thrombosis?
Dr. Alexander: This case illustrates a host of other challenges that underscore how much more work we need to do to define optimal antiplatelet therapy. Suppose we perform platelet function testing and find a low level of platelet inhibition in this patient with stent thrombosis, and we change his antiplatelet regimen. When should we test him again? If we retest in 3 months and find that he has a higher than expected level of platelet inhibition on the new antiplatelet regimen, do we dial down the intensity? Once again, there is no evidence to guide these decisions, and levels of platelet inhibition are driven not just by the medications but also by what is going on in the patient’s platelets—it is quite multifactorial.
POINT-OF-CARE PLATELET FUNCTION TESTING: CURRENT LIMITS, FUTURE ROLES
Dr. Bhatt: While we’re discussing platelet function testing, I found it interesting, Dr. Kottke-Marchant, that you said the use of bleeding time as a platelet test is finally going away. Testing of bleeding time has been around forever, but I agree that it doesn’t have much value in clinical practice. Do you think bleeding time will continue to have any role in drug development? Most phase 2 trials, and certainly phase 1 trials, still capture bleeding time to assess whether or not a drug is working. Should that, too, be jettisoned, or does bleeding time still have some merit in this context?
Dr. Kottke-Marchant: I would jettison it in drug development as well because of the considerable variability in bleeding time. It is not a test that can be standardized, and no quality control can be done. The results depend on skin turgor, age, and many other variables.
We need a global assay that will pick up multiple aspects of platelet function, such as flow-based adhesion, aggregation, and granule release. The bleeding time is a shear-dependent test, whereas the platelet aggregation test that is used in most drug trials is an artificial assay that measures only aggregation, but not under shear. The VerifyNow rapid platelet function analyzer does not measure platelets under shear and is not a global assay.
Dr. Marc Sabatine: I would underscore the need for a reliable point-of-care test of platelet function. When we prescribe a statin or an antihypertensive drug, we don’t just send the patient out the door and hope that everything will be okay. We measure the response, knowing that genotype, environmental factors, or medication factors can affect the response. When we prescribe an antiplatelet drug, we need a reliable point-of-care device to make certain that the patient is getting appropriate platelet inhibition.
I am reminded of a recent study of point-of-care measurement of platelet inhibition in patients receiving clopidogrel prior to nonemergent percutaneous coronary intervention (PCI).2 Rather than just treating patients with PCI and sending them out the door, the investigators kept giving patients clopidogrel and measuring their platelet inhibition until they achieved an appropriate degree of inhibition, after which PCI was performed. Event rates were significantly reduced in the patient group treated this way, which suggests a need to individualize therapy and move away from the “one size fits all” mindset.
Dr. Bhatt: Dr. Peacock, you’ve led a study of point-of-care assays in the emergency department. What might ultimately be the role of point-of-care testing in emergency medicine, and might it influence drug selection?
Dr. Peacock: My short answer is that I think there will be a role for point-of-care testing, with all the caveats that have been discussed. There may even be a day when we do genetic testing and look for DNA. Honestly, though, I’m somewhat of a skeptic because I’m not looking at the genetics. I see many patients who do crack cocaine who come to the emergency room with chest pain and have risk factors, but I send these patients home because they are not having an event. The real question is, “Is it an event?” If a patient is having an event and he or she has platelet resistance or hyperreactivity—whatever we term it—then you have to decide the next step.
As you mentioned, we just completed a study that evaluated a couple hundred patients for platelet inhibition resistance to aspirin, and one finding was that the incidence of platelet resistance to aspirin was much lower than we had anticipated. Studies from the literature suggest that the prevalence of resistance is around 30%, but in our study it was 6.5%.3
Dr. Kottke-Marchant: It depends on how and in whom you measure resistance. Different tests will give you different numbers. Even among studies using the same measurement techniques, the results depend on the patient population. If it’s a fairly stable cardiac population, you may see aspirin resistance rates of 4% or 5%. If it’s a population of patients who have had multiple MIs, the rate may be higher.
Dr. Peacock: That’s exactly my point. In the emergency department we see a mixed bag. We see many people who have had no prior events and have no acute event occurring. So in that setting you are going to get results that suggest that no intervention is required, whereas in that small percentage of patients in whom something is happening, your drug choice may be different.
Dr. Alexander: We are still talking about resistance to antiplatelet drugs as though it were a patient-level variable, but it’s my impression that it changes over time and within a patient.
Dr. Kottke-Marchant: It can change over time. There aren’t many good longitudinal studies. Most of the studies of “aspirin resistance” are really snapshot studies with measurements taken at one point in time. A term I prefer is “platelet reactivity.” To really assess treatment efficacy, we are going to have to look at the basal level of platelet reactivity.
WHAT ROLE FOR GENOTYPING IN GUIDING ANTIPLATELET THERAPY?
Dr. Bhatt: Dr. Peacock alluded to a potential role for genetic testing. Dr. Sabatine, you have done a lot of interesting work with genotyping in the TRITON-TIMI 38 study of prasugrel and clopidogrel. What is the future role of genotyping in determining which antiplatelet therapy is best for which patient?
Dr. Sabatine: As I mentioned, cytochrome P450 enzymes play a critical role in the metabolism of clopidogrel. These enzymes are fairly polymorphic—mutations in their encoding genes are responsible for subtle changes in effect, unlike the traditional mutations that we think about for sickle cell disease, for example. A wealth of data has been published showing that genetic variants are associated with decreased functional activity of cytochrome P450 enzymes, demonstrating the pharmacologic importance of these variants.
Individuals who carry variant alleles appear to respond differently to clopidogrel. A variety of small studies show that those who carry specific variants—particularly in the CYP2C19 enzyme, but in other enzymes as well—appear to have a diminished response to clopidogrel. There are also data showing that individuals with a diminished response to clopidogrel have worse outcomes.4 Our group is studying the impact of genetic variants that decrease the functional activity of cytochrome P450 enzymes on clinical outcomes. (Editor’s note: This study has since been published by Mega et al.5)
The practical implication may lie in point-of-care genotyping, which appears possible and will be clinically useful if a strong link can be demonstrated between genotype and outcomes. If point-of-care genotyping becomes practical, it will raise the question of whether both genotyping and platelet aggregation testing are needed. I think they might indeed be complementary in risk prediction, as is the case with genetic variants that affect low-density lipoprotein cholesterol (LDL-C) levels. In the lipid arena, we have seen that genetic effects and lipid levels provide independent incremental information about risk. That’s because of the high degree of variation in LDL-C levels: an LDL-C measurement is a snapshot in time, yet a variety of factors can influence LDL-C levels. In contrast, genotype is an invariant factor. Similarly, in the platelet arena, platelet aggregation studies and genotyping may be synergistic in predicting an individual’s predisposition to events and response to medications.
Dr. Bhatt: While we’re discussing pathways of metabolism, the literature, though scant, suggests a potential interaction between proton pump inhibitors and clopidogrel. I was co-chair of a recent American College of Cardiology/ American Heart Association/American College of Gastro-enterology consensus document that endorsed liberal use of proton pump inhibitors in patients who are at gastrointestinal risk, including those on antiplatelet therapy.6 The gastroenterologists believed strongly that proton pump inhibitors were safe and in fact underused in these patients. What do you think about the clopidogrel–proton pump inhibitor interaction? Should we be concerned?
Dr. Sabatine: Proton pump inhibitors are not only substrates for, but also inhibitors of, CYP2C19, a key enzyme that helps transform clopidogrel into an active metabolite. For this reason, there has been interest in whether concomitant use of proton pump inhibitors would blunt the efficacy of clopidogrel. The same concern was raised about giving clopidogrel with certain statin drugs that are also metabolized by the cytochrome P450 system, and several studies have shown an effect of these statins on clopidogrel’s platelet inhibition. However, there is no evidence that coadministration of these statins has affected clinical outcomes with clopidogrel in clinical trials. So it may be that while competition for the cytochrome P450 system is one factor, it’s not enough of a factor to tip the scale and result in a clinical event. The same may be true of coadministration of proton pump inhibitors; meanwhile, we await definitive data that concomitant use with clopidogrel leads to higher rates of ischemic events.
DIAGNOSTIC UNCERTAINTY IN THE EMERGENCY SETTING
Dr. Bhatt: We heard about quite a few new antiplatelet drugs in Dr. Sabatine’s presentation, some of which will likely be taken up in clinical practice. Dr. Peacock, from an emergency department perspective, how will you integrate all these new agents with the numerous therapies already available? What should emergency departments do to come to grips with and ultimately take advantage of these different forms of therapy as well as emerging platelet function tests?
Dr. Peacock: The piece that’s unique or especially pertinent to the emergency department is diagnostic uncertainty. Diagnosis and management are easy when a patient has an ST-elevation MI because we all know what that looks like and we know what to do in response. To some extent non-ST-elevation MI is fairly simple too. ACS is a lot more difficult because we don’t have a good definition for unstable angina, and that’s where diagnosis and management become problematic. And with high-sensitivity troponins coming out now, the question of non-ST-elevation MI is going to get more and more confusing because we will have a lot more patients who meet criteria without having an acute coronary artery event.
So it is going to be important that studies be designed correctly. A lot of the studies reviewed today were efficacy studies, showing that a particular drug works well in a carefully defined population, but they were not efficiency studies: they did not take into account the real-world diagnostic uncertainty—and inevitable misdiagnoses—that emergency departments encounter before starting therapy.
Take the CURE trial, for example. It was a great study, showing that clopidogrel reduced the hazard ratio for major coronary events by 20% in patients with unstable angina,7 and the message was that everybody should be using clopidogrel. A close look at the study, however, reveals that about half the patients did not receive clopidogrel in the emergency department. When patients did receive it early, it was driven by the cardiologist, who was absolutely certain of the diagnosis. But if the study was not designed to test early use, then it is a big leap to extrapolate its findings to this circumstance.
Many of the patients in the CURE trial were enrolled the day after presentation, when their diagnosis was certain—ie, they had a rise in troponin after their symptoms. But when a patient first arrives in the emergency department, we are not certain of the diagnosis. And if we use a drug such as clopidogrel, with a duration of action as long as 5 days, we have committed the entire medical system to a certain course of management for that period of time. If we get the diagnosis wrong, this commitment could restrict management options for up to 5 days.
The question for emergency physicians becomes, “How long is long enough to know whether I can pull the trigger on a therapy and be correct?” With all the new drugs coming along, the way to answer this is to do efficiency studies in a real-world environment in addition to efficacy studies.
Dr. Alexander: Yes, one of the biggest limitations of antiplatelet drug studies to date is that they usually haven’t really addressed the timing of drug initiation. We often assume that if a drug is shown to be beneficial, then it should be started as soon as possible. As we just heard, that may have been an unfounded extrapolation from the CURE trial. The same sort of thing happened with the ISIS trial of aspirin in patients with ST-elevation MI.8 In response to the ISIS results, clinicians rushed to give patients aspirin right away even though many of the patients in the trial may have received their aspirin the day after presentation. For these reasons, the EARLY-ACS study,9 which is addressing a very simple question—whether early upstream use of glycoprotein IIb/IIIa inhibitors is beneficial—has been a challenging trial to complete.
WHAT ROLE FOR THIENOPYRIDINE PRETREATMENT?
Dr. Bhatt: Dr. Sabatine, you presented data from the large TRITON-TIMI 38 trial comparing prasugrel with clopidogrel. I’m interested in how you would use prasugrel in practice, assuming it receives marketing approval, especially in light of its bleeding risk, particularly in patients in whom coronary artery bypass graft surgery (CABG) is planned. Many hospitals pretreat patients with clopidogrel in the emergency department. How would you manage a patient who shows up in the emergency room with ACS? Would you give clopidogrel, would you wait and give prasugrel, or would you do something else? If you gave clopidogrel, what loading dose would you use—300 mg, 600 mg, or, as some have suggested, 900 or 1,200 mg?
Dr. Sabatine: I am a strong proponent of pretreatment. Data from multiple studies show a benefit to this strategy, and even the original CURE trial showed a roughly 30% reduction in ischemic events within the first 24 hours of clopidogrel initiation.7
I think the dosing strategy depends on how the patient is going to be managed. If management is going to be conservative, then I would start the patient on 300 mg of clopidogrel when he or she came in. If the patient is going to the cardiac catheterization laboratory in a few hours, I would pretreat with 600 mg of clopidogrel. For prasugrel, the need for pretreatment is less clear, given the drug’s faster onset of action and greater degree of platelet inhibition. In the TRITON-TIMI 38 study,10 prasugrel was given, by and large, after diagnostic angiography, and thus one could use that approach in practice.
In terms of clopidogrel versus prasugrel, I would embrace prasugrel for the large majority of my patients, being mindful of the risk of bleeding. I would not hesitate to give the medication to diabetics or to younger, more robust patients. The 50% reduction in stent thrombosis with prasugrel versus clopidogrel in TRITON-TIMI 38 is huge,11 given that the risk of death with stent thrombosis is probably 25% or greater. So I would want to have prasugrel on board to reduce the risk of stent thrombosis, especially if a drug-eluting stent were being implanted.
Dr. Bhatt: Dr. Alexander, let’s get your take on a similar scenario. Assuming that prasugrel gains marketing approval, how would you manage patients with non-ST-elevation MI who present to the emergency department? Would you pretreat with clopidogrel? Would you wait until angiography and then, depending on the anatomy, treat with prasugrel? Or would you potentially pretreat with prasugrel, which has not been studied and would not be a labeled indication? How would you reconcile the data?
Dr. Alexander: At Duke, I expect that prasugrel will not be used prior to the catheterization laboratory in patients with non-ST-elevation ACS due to concerns about whether the patients will undergo PCI or be managed medically or with CABG.
Dr. Bhatt: That makes sense, since there was a fair amount of bleeding with prasugrel in those patients in TRITON-TIMI 38.
Dr. Alexander: Correct. Moreover, at Duke we don’t use as much upstream clopidogrel as we would, based on the evidence, if I were managing all the patients. There is still a lot of pushback about upstream clopidogrel from our surgeons because patients are going to surgery quickly these days, sometimes just a day after catheterization, and that’s when a loading dose of clopidogrel can be problematic. We are also still fairly heavy users of glycoprotein IIb/IIIa inhibitors.
Where I can see prasugrel being used prior to the cath lab at Duke is in ST-elevation MI, where the rate of PCI is very high. In primary angioplasty for ST-elevation MI, it would likely be given upstream. The bigger issue for us will be that we serve as a referral base for a lot of regional hospitals, and thus have some influence on their practices.
Dr. Bhatt: In that case, what would you advise those regional hospitals to do for non-ST-elevation MI?
Dr. Alexander: For the time being, we would advise continuing with our current practice, which is to load clopidogrel in patients in whom there is a reasonable certainty that CABG will not be performed, and to use glycoprotein IIb/IIIa inhibitors in high-risk patients. As we get more experience with prasugrel or with additional trial results, however, that practice could easily change.
Dr. Bhatt: So you would still use glycoprotein IIb/IIIa inhibitors?
Dr. Alexander: Yes, I advocate upstream clopidogrel use, but not all my colleagues do. Based on the guidelines, I’d use one or the other—either clopidogrel or a glycoprotein IIb/IIIa inhibitor. As I mentioned in my talk, if a patient is at high risk for bleeding, I am more inclined to use clopidogrel, although patients at higher risk of bleeding are often at higher risk for ischemic events as well.
WHAT’S DRIVEN THE DROPOFF IN GLYCOPROTEIN IIb/IIIa INHIBITOR USE?
Dr. Bhatt: While we’re on the topic of glycoprotein IIb/IIIa inhibitors, a question card from the audience asks why there has been a decrease in glycoprotein IIb/ IIIa inhibitor use and whether this decline is appropriate or inappropriate. Have clopidogrel pretreatment, higher loading doses of clopidogrel, and use of the direct thrombin inhibitor bivalirudin contributed to the decrease in glycoprotein IIb/IIIa inhibitor use?
Dr. Alexander: I do think that the decline has been driven by the changing environment, with greater use of other antithrombotic strategies that include clopidogrel and bivalirudin, as you suggest, as well as an increased attention to bleeding. From an evidence-based standpoint, we don’t know whether the decrease in glycoprotein IIb/IIIa use is appropriate or not because the studies of these agents were conducted before the widespread upstream use of clopidogrel and bivalirudin. Clopidogrel is attractive because it’s a pill given as one dose in the emergency department, the wards, or the catheterization laboratory, rather than a much more complicated infusion with weight-based dosing and dosage adjustments based on creatinine clearance. It is possible that we should perhaps be dosing clopidogrel the same way, but we don’t know that yet.
PRASUGREL IN PRACTICE: HOW LOW CAN THE DOSE GO, AND IS THERE A GENDER EFFECT?
Dr. Bhatt: Let’s stick with this focus on dosing but turn back to discussion of prasugrel. In your presentation of the TRITON-TIMI 38 data, Dr. Sabatine, you proposed a potential prasugrel dosage modification, down to a 5-mg loading dose, in subgroups that were identified as being at high bleeding risk—namely, elderly patients and patients with low body weight. However, no outcomes data with 5 mg of prasugrel came out of TRITON-TIMI 38.10 Is this proposed modification based on pharmacokinetic extrapolation? Could clinicians be comfortable using 5 mg of prasugrel, assuming the drug receives regulatory approval and a 5-mg tablet would be available?
Dr. Sabatine: Of course, evidence at the grade A level would consist of a trial showing that patients who received a lower dose enjoyed the same benefit as those who got standard dosing in TRITON-TIMI 38—a 60-mg loading dose followed by 10 mg/day—with an acceptable risk profile. However, such a trial would be difficult and costly to conduct, and would take roughly half a decade to pull off. It is only through large trials like TRITON-TIMI 38 that you identify subgroups that respond differently, and then to go back and do a separate trial for those subgroups takes a great deal of time. It may not be practical.
I think the Food and Drug Administration is moving toward embracing careful pharmacokinetic/pharmacodynamic substudies within trials, with these substudies having adequate numbers of subjects to provide a sense for the ideal target dose and what an acceptable dose range would be, without limiting approval to a single dose. The analogy would be warfarin dosing, with the aim being to figure out an acceptable dose range, discover which patients fall outside that range, and then model the effect of a lower dose in those patients. Thus, approving a 5-mg dose of prasugrel based on TRITON-TIMI 38 would be a reasonable approach if this dose passed muster under pharmacokinetic/pharmacodynamic modeling. If this approach were taken, there would clearly be a need for postmarketing surveillance to confirm whether the modeling on the effects of the lower dose was borne out by actual outcomes.
Dr. Bhatt: The audience has posed another interesting question raised by TRITON-TIMI 38: Can you comment on the lesser effect of prasugrel in women?
Dr. Sabatine: It is true that there was not a statistically significant effect of prasugrel among women in TRITON-TIMI 38, but statistical tests among subgroups found no significant heterogeneity for the effect between men and women, and that is the relevant measure to determine any gender effect. Keep in mind that not all subgroups represent a univariate slice of the population. For example, women generally have lower body weight than men, and since prasugrel’s net clinical benefit was reduced in patients with lower body weight, that may explain some of the differing extent of effect between men and women.
Dr. Bhatt: That’s a good point about the lack of heterogeneity between men and women. In fact, a meta-analysis of clopidogrel data conducted by one of the fellows I work with revealed that men and women appear to benefit similarly from clopidogrel.12 There was a slight signal of excess bleeding in women, but there were more elderly women in the pooled population, which may have been a confounding factor. As best as anyone can tell, antiplate-let therapy works well in both men and women.
NAVIGATING MANAGEMENT ACROSS THE SPECTRUM OF CARE
Dr. Bhatt: I would like to explore a bit further how all of these issues translate across the spectrum of care, beginning in the emergency department, which we know is a key component of the entire ACS management strategy for a health care system. What should emergency medicine doctors do, given all of the potential options—clopidogrel, different loading doses of clopidogrel, prasugrel, glycoprotein IIb/IIIa inhibitors, even bivalirudin?
Dr. Peacock: It depends on the practice setting. Some emergency physicians work at community hospitals with no backup. They must have relationships with the larger centers to which they’ll be transferring patients, because ACS patients should not be staying at community hospitals. These emergency physicians must have close relationships with the physicians who will be receiving their patients, and they know the potential head-butting with surgeons surrounding early clopidogrel use better than anybody does. If they treat with clopidogrel in the emergency room, and it turns out that the patient needs to go to the catheterization laboratory, can the receiving hospital use platelet testing to shorten the standard 5-day interval from treatment to catheterization?
Dr. Bhatt: Yes, that’s a rather useful, although not completely validated, way of using point-of-care platelet testing—to potentially reduce the time to surgery.
Dr. Peacock: Right. So if the policies for handling these types of transfer-related issues are worked out in advance, all players have a pathway to follow, which can allow quick action when necessary. If you don’t have these issues worked out in advance, you either lose many opportunities to act quickly in the emergency room or you risk taking actions that will cause problems later in the course of management.
Dr. Alexander: I totally agree. The key is to sit down with all the players involved—the surgeons, the interventional cardiologists, the intensivists, the emergency room personnel—and come up with strategies for different populations of patients. Write down the collective strategy and hang it on the wall so that everybody can be comfortable with it. The strategy can be reevaluated when prasugrel or other new antithrombotic drugs come on the market.
Dr. Peacock: The other environment is the academic center, which is even more challenging, but for different reasons. At a large academic center like the Cleveland Clinic, any of 25 different cardiologists may be taking call and receiving patients from the emergency department on a particular night. A lot of phone interaction is required to elicit the planned management strategy, including if and when the patient will be going to the cath lab. Individualizing care to a particular cardiologist then becomes a time-consuming challenge, especially in clinical situations where outcomes are time-dependent.
Dr. Alexander: Agreed. Management needs to be integrated across the entire spectrum of care. The anticoagulants that we plan to use in the cath lab will affect the antithrombotic regimen used upstream.
Dr. Kottke-Marchant: One circumstance where platelet function testing has been helpful is in determining the washout of the clopidogrel effect before surgery. At Cleveland Clinic, we have implemented platelet function testing in this circumstance instead of waiting a blanket 5 days after clopidogrel administration to go to surgery. A return to normal platelet function on platelet aggregation testing, depending on the cutoff value used, is an indicator that the patient can proceed to surgery.
Dr. Bhatt: That’s a logical approach. How should we be using antiplatelet therapy in the medically managed patient, Dr. Alexander?
Dr. Alexander: When I think of medical management, I include patients who don’t go to the cath lab, but also those who do, with regards to their management prior to and following their time in the cath lab.
In patients who don’t go to the cath lab for angiography, the ACC/AHA guidelines recommend aspirin and either clopidogrel, a glycoprotein IIb/IIIa inhibitor, or both.1 In making this choice, I consider the patient’s risk of bleeding and the dosing complexity of the regimen, especially with the use of glycoprotein IIb/IIIa inhibitors in a patient with renal insufficiency. In a patient at relatively low risk for bleeding, I often use both clopidogrel and a glycoprotein IIb/IIIa inhibitor, although this strategy does not have a lot of data to support it.
The more challenging population consists of patients who go to the cath lab but do not undergo PCI; this population is managed medically too. We often drop the ball with clopidogrel in this population. Many patients in whom PCI is not performed do not receive clopidogrel upstream, for all of the reasons we’ve discussed, and there is pretty good evidence that if clopidogrel is not instituted before hospital discharge, the patient is not likely to be receiving it at 30 days either. We have an obligation to treat these patients.
Treatment following bypass surgery is much murkier, and I don’t really know what we should be doing. The ACC/AHA guidelines suggest that clopidogrel be started in a patient with non-ST-elevation ACS after bypass surgery,1 but I believe the evidence to support that recommendation is pretty weak.
Dr. Bhatt: Well, the CURE trial did contain a sizeable group that underwent bypass surgery,7 and although this group was underpowered in some respects, it was still a very large group, so I personally favor treatment in those patients. We should mention that an ongoing trial called TRILOGY ACS is comparing clopidogrel and prasugrel specifically in patients who are being managed medically,13 so more data on this strategy will be emerging.
ARE GUIDELINES DESTINED TO BECOME EVER MORE COMPLEX?
Dr. Bhatt: Here’s a comment and question from the audience that pulls together a lot of what we’ve discussed while also looking forward: The antiplatelet therapy guidelines are already complicated. If the ongoing studies of emerging antiplatelet drugs all have results that are qualitatively similar to those of the TRITON-TIMI 38 study of prasugrel—ie, better efficacy with more potent therapy but more bleeding—how do you foresee these antiplatelet drugs being used in clinical practice?
Dr. Sabatine: The contrast between the US guidelines and the European guidelines for ACS management is stark. The US guidelines—from the ACC and AHA1—are essentially an encyclopedia that includes nearly every trial of anti-platelet therapy in ACS along with complicated algorithms; they do a wonderful job of being complete. The European guidelines14 are probably one tenth the size of their US counterpart document, and they suggest treatments for various patient types; they are very simple.
In a sense, the US guidelines lay out the data and force practitioners to evaluate the trials and consider how our patients fit into the study populations. In this way they are analogous to current guidelines for anticoagulant therapy. Several anticoagulants have been compared with heparin in clinical trials. These newer anticoagulants appear to reduce the risk of ischemic events compared with heparin; some have lower rates of bleeding, while others have higher rates of bleeding. There have been few head-to-head studies of these agents, however, so we wind up with guidelines that are not definitive but rather suggest agents to “consider” in various settings.
It’s unlikely that a head-to-head trial will be conducted comparing prasugrel with the reversible P2Y12 antagonist AZD6140, assuming that both are approved for marketing. If the drugs appear equally efficacious in placebo-controlled trials, it will take consensus to determine the appropriate choice at your hospital, factoring in your patient profile, the cost of the drugs, and other variables. It’s more complicated when one agent is slightly more efficacious but causes more bleeding or, conversely, a little less efficacious but less apt to cause bleeding. In such cases, you may need to tailor therapy to the patient, trying to gauge bleeding risk. All of the emerging data appear to point to the importance of bleeding on outcomes: patients who bleed fare poorly, in part due to the bleeding itself and in part perhaps because they have a proclivity for bleeding.
THE FUTURE: MONITORING-BASED DOSING AND NICHE ANTIPLATELETS?
Dr. Bhatt: That’s a good observation. Let’s wrap up by having the other panelists share any final thoughts you may have.
Dr. Alexander: I’d like to return to the issue of measuring antiplatelet response and using it to guide therapy. Earlier we cited the examples of antihypertensive therapy and lipid-lowering therapy to support this model of monitoring-based treatment. Guidelines for dyslipidemia treatment recommend using LDL-C levels to guide therapy, but this practice is difficult to study in a randomized trial. In fact, none of the randomized trials of statins used LDL-C levels to guide therapy. They all studied fixed doses of statins versus placebo or fixed doses of another statin. Higher doses of statins were always beneficial compared with lower doses, and this finding was extrapolated into the guidelines as a justification to treat to target LDL-C levels.
Dr. Bhatt: It’s not even necessarily clear that LDL-C level is the best target, if you consider the JUPITER trial, in which patients received statin therapy based on their baseline level of high-sensitivity C-reactive protein, not their LDL-C level.15 It goes to show how incomplete our knowledge of a class of drugs may be, even decades after the drugs are introduced.
Dr. Kottke-Marchant: To speak to Dr. Alexander’s point, dose adjustment guided by platelet monitoring is a bit more problematic for antiplatelet drugs that are irreversible inhibitors, such as clopidogrel and aspirin, than for those that are reversible inhibitors, which are being developed and may eventually make more sense to use. From a drug development standpoint, a drug that requires monitoring and dose adjustment will not gain wide acceptance because it will increase medical costs and morbidity.
Dr. Bhatt: Yes, we know from experience with warfarin that doctors and patients don’t like the ongoing need for monitoring and testing.
Dr. Peacock: The drugs that are going to be adopted by the emergency department are those with the shortest half-lives, for several reasons: (1) using a drug with a short half-life won’t commit us to a particular course of action; (2) the potential for drug interactions is lower; and (3) in the event of an erroneous diagnosis, the consequence of misapplication may be mitigated by early recognition and termination of the drug. If we later decide that we’ve gone down the wrong therapeutic road or reached a wrong diagnosis, or if a complication occurs, we can turn off the therapy quickly. That level of flexibility is needed.
Dr. Kottke-Marchant: I think we are moving into an era of niche antiplatelet drugs. One might be used in a patient going to surgery, for example, and another for long-term therapy.
Dr. Peacock: One thing that I don’t have a feel for is how to transition from one drug to another. When you change drugs for a patient, it so often seems like it goes badly. If we’re eventually going to use drugs with ultra-short half-lives in the in the emergency department for the first day or two, and then switch patients to a pill for a week, a lot more platelet function testing may be needed.
- Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/ non-ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2007; 50:e1–e157.
- Bonello L, Camoin-Jau L, Arques S, et al. Adjusted clopidogrel loading doses according to vasodilator-stimulated phosphoprotein phosphorylation index decrease rate of major adverse cardiovascular events in patients with clopidogrel resistance: a multicenter randomized prospective study. J Am Coll Cardiol 2008; 51:1404–1411.
- Glauser J, Emerman CL, Bhatt DL, Peacock WF. Platelet aspirin resistance in emergency department patients with suspected acute coronary syndrome. Am J Emerg Med. In press
- Patti G, Nusca A, Mangiacapra F, Gatto L, D’Ambrosio A, Di Sciascio G. Point-of-care measurement of clopidogrel responsiveness predicts clinical outcome in patients undergoing percutaneous coronary intervention. J Am Coll Cardiol 2008; 52:1128–1133.
- Mega JL, Close SL, Wiviott SD, et al. Cytochrome P-450 polymorphisms and response to clopidogrel. N Engl J Med 2009; 360:354–362.
- Bhatt DL, Scheiman J, Abraham NS, et al. ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use. J Am Coll Cardiol 2008; 52:1502–1517.
- Fox KA, Mehta SR, Peters R, et al. Benefits and risks of the combination of clopidogrel and aspirin in patients undergoing surgical revascularization for non-ST-elevation acute coronary syndrome: the Clopidogrel in Unstable angina to prevent Recurrent ischemic Events (CURE) Trial. Circulation 2004; 110:1202–1208.
- ISIS-2 Collaborative Group. Randomised trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. Lancet 1988; 2:349–360.
- EARLY-ACS: Glycoprotein IIb/IIIa inhibition in patients with non-ST-segment elevation acute coronary syndrome. Clinical Trials.gov Web site. http://clinicaltrials.gov/ct2/show/NCT00089895. Updated December 17, 2008. Accessed December 18, 2008.
- Wiviott SD, Braunwald E, McCabe CH, et al; TRITON-TIMI 38 Investigators. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 2007; 357:2001–2015.
- Wiviott SD, Braunwald E, McCabe CH, et al. Intensive oral anti-platelet therapy for reduction of ischaemic events including stent thrombosis in patients with acute coronary dyndromes treated with percutaneous coronary intervention and stenting in the TRITON-TIMI 38 trial: a subanalysis of a randomised trial. Lancet 2008; 371:1353–1363.
- Berger JS, Bhatt DL, Chen Z, et al. The relationship between sex, mortality and cardiovascular events among patients with established cardiovascular disease: a meta-analysis [ACC abstract 1012-149]. J Am Coll Cardiol 2008; 51 10 suppl A:A247.
- TRILOGY ACS: A comparison of prasugrel and clopidogrel in acute coronary syndrome subjects. ClinicalTrials.gov Web site. http://clinicaltrials.gov/ct2/show/NCT00699998. Updated December 15, 2008. Accessed January 2, 2009.
- Guidelines for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes. Eur Heart J 2007; 28:1598–1660.
- Ridker PM, Danielson E, Fonseca FA, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med 2008; 359:2195–2207.
CASE STUDY: THROMBOSIS AFTER STENTING DESPITE ANTIPLATELET THERAPY
Dr. Deepak Bhatt: We have taken in a wealth of terrific information from the three preceding talks in this symposium. Let’s now share some questions from the audience and explore some of the points raised in the preceding talks in a bit more practical detail for clinicians. Our three prior speakers are joined in this panel discussion by Cleveland Clinic’s Dr. Frank Peacock, who brings an emergency medicine perspective.
Let’s begin with a case-based question supplied from the audience. The patient is a 42-year-old morbidly obese man without diabetes who had a non-ST-elevation myocardial infarction (MI) less than 1 year ago. A drug-eluting stent was placed at the time of his MI, and now restenosis has occurred. He is on aspirin and clopidogrel 75 mg/day. Do you recommend running a vasodilator-stimulated phosphoprotein (VASP) test and possibly increasing the clopidogrel dose to 150 mg/ day, or should the patient just be switched to prasugrel (assuming it is commercially available) without running the VASP test?
I’ll take a quick initial stab at this question. Studies of antiplatelet therapies to prevent instent restenosis have been a mixed bag. Some of the trials with glycoprotein IIb/IIIa inhibitors have shown an effect on restenosis, but most have not. Similarly, some of the analyses of the thienopyridines ticlopodine and clopidogrel have shown an effect on restenosis, but most have not.
For the most part, restenosis does not appear to be heavily mediated by platelets, at least not in a way that we can influence by therapy. On the other hand, stent thrombosis is highly platelet mediated, so I would alter the case to one in which stent thrombosis is the clinical problem. Assuming that the patient has been adherent to his antiplatelet regimen, which tests would you perform, and how would you act on the information from those tests?
Dr. Kandice Kottke-Marchant: The 2007 guidelines on acute coronary syndrome (ACS) management from the American College of Cardiology and American Heart Association (ACC/AHA)1 do not address platelet function testing, and almost none of the clinical trials of antiplatelet agents had an arm that included testing and dose adjustment based on platelet function studies. Platelet testing is available at some centers; at Cleveland Clinic, we use platelet aggregation testing. One can do platelet aggregation testing on a patient-by-patient basis; if inhibition appears to be suboptimal, a treatment decision should be made, but there is little guidance from the literature to steer that decision. I have seen clinicians increase the dose of clopidogrel or aspirin in response to platelet function tests, which occasionally triggers a confirmatory call from the pharmacy department.
Dr. Bhatt: When I was still at Cleveland Clinic, our chief medical resident did an analysis of platelet function testing, and it was remarkable how much testing was performed and how often it changed management, largely in the absence of any outcomes data, as Dr. Kottke-Marchant pointed out. Dr. Alexander, what are your recommendations with respect to platelet function testing today?
Dr. John Alexander: The case you describe is one in which applying evidence is not easy. There are no trials to supply any evidence to change therapy in this patient, a morbidly obese man receiving 75 mg/day of clopidogrel. There is certainly a rationale, however, to believe that a standard “one size fits all” 75-mg daily dose of clopidogrel may not be enough for him. The trade-off with a higher dosage is a higher risk of bleeding, however, so I would first be sure that he has been adherent to his current regimen of clopidogrel and aspirin.
Dr. Bhatt: Is there a role for point-of-care testing to determine whether he is adherent to the medicines?
Dr. Kottke-Marchant: Several of the point-of-care tests, such as the VerifyNow rapid platelet function analyzer, have specific cartridges for aspirin and for clopidogrel. If platelets were not being inhibited, it would suggest that the doses were too low, given the patient’s weight, but you probably would not be able to determine whether he was resistant to clopidogrel.
Dr. W. Frank Peacock: One way to verify that patients are taking their aspirin is to take a small urine sample and squirt in 2 mL of ferric chloride. If the sample turns purple, it means they are taking their aspirin. Once that is established, you can try to determine whether the drug is working on their platelets.
Dr. Alexander: Another potential explanation for stent thrombosis is faulty stent placement. In this case I would consider asking an interventional colleague to perform intravascular ultrasonography to make sure the stent was implanted properly before I changed the patient’s antithrombotic therapy.
Dr. Bhatt: That’s a great technical point. We always want to make sure that a case of stent thrombosis is not due to a mechanical problem. We should be asking: Is the stent properly sized and well opposed? Is there a distal dissection or any other issue that could predispose to stent thrombosis?
Dr. Alexander: This case illustrates a host of other challenges that underscore how much more work we need to do to define optimal antiplatelet therapy. Suppose we perform platelet function testing and find a low level of platelet inhibition in this patient with stent thrombosis, and we change his antiplatelet regimen. When should we test him again? If we retest in 3 months and find that he has a higher than expected level of platelet inhibition on the new antiplatelet regimen, do we dial down the intensity? Once again, there is no evidence to guide these decisions, and levels of platelet inhibition are driven not just by the medications but also by what is going on in the patient’s platelets—it is quite multifactorial.
POINT-OF-CARE PLATELET FUNCTION TESTING: CURRENT LIMITS, FUTURE ROLES
Dr. Bhatt: While we’re discussing platelet function testing, I found it interesting, Dr. Kottke-Marchant, that you said the use of bleeding time as a platelet test is finally going away. Testing of bleeding time has been around forever, but I agree that it doesn’t have much value in clinical practice. Do you think bleeding time will continue to have any role in drug development? Most phase 2 trials, and certainly phase 1 trials, still capture bleeding time to assess whether or not a drug is working. Should that, too, be jettisoned, or does bleeding time still have some merit in this context?
Dr. Kottke-Marchant: I would jettison it in drug development as well because of the considerable variability in bleeding time. It is not a test that can be standardized, and no quality control can be done. The results depend on skin turgor, age, and many other variables.
We need a global assay that will pick up multiple aspects of platelet function, such as flow-based adhesion, aggregation, and granule release. The bleeding time is a shear-dependent test, whereas the platelet aggregation test that is used in most drug trials is an artificial assay that measures only aggregation, but not under shear. The VerifyNow rapid platelet function analyzer does not measure platelets under shear and is not a global assay.
Dr. Marc Sabatine: I would underscore the need for a reliable point-of-care test of platelet function. When we prescribe a statin or an antihypertensive drug, we don’t just send the patient out the door and hope that everything will be okay. We measure the response, knowing that genotype, environmental factors, or medication factors can affect the response. When we prescribe an antiplatelet drug, we need a reliable point-of-care device to make certain that the patient is getting appropriate platelet inhibition.
I am reminded of a recent study of point-of-care measurement of platelet inhibition in patients receiving clopidogrel prior to nonemergent percutaneous coronary intervention (PCI).2 Rather than just treating patients with PCI and sending them out the door, the investigators kept giving patients clopidogrel and measuring their platelet inhibition until they achieved an appropriate degree of inhibition, after which PCI was performed. Event rates were significantly reduced in the patient group treated this way, which suggests a need to individualize therapy and move away from the “one size fits all” mindset.
Dr. Bhatt: Dr. Peacock, you’ve led a study of point-of-care assays in the emergency department. What might ultimately be the role of point-of-care testing in emergency medicine, and might it influence drug selection?
Dr. Peacock: My short answer is that I think there will be a role for point-of-care testing, with all the caveats that have been discussed. There may even be a day when we do genetic testing and look for DNA. Honestly, though, I’m somewhat of a skeptic because I’m not looking at the genetics. I see many patients who do crack cocaine who come to the emergency room with chest pain and have risk factors, but I send these patients home because they are not having an event. The real question is, “Is it an event?” If a patient is having an event and he or she has platelet resistance or hyperreactivity—whatever we term it—then you have to decide the next step.
As you mentioned, we just completed a study that evaluated a couple hundred patients for platelet inhibition resistance to aspirin, and one finding was that the incidence of platelet resistance to aspirin was much lower than we had anticipated. Studies from the literature suggest that the prevalence of resistance is around 30%, but in our study it was 6.5%.3
Dr. Kottke-Marchant: It depends on how and in whom you measure resistance. Different tests will give you different numbers. Even among studies using the same measurement techniques, the results depend on the patient population. If it’s a fairly stable cardiac population, you may see aspirin resistance rates of 4% or 5%. If it’s a population of patients who have had multiple MIs, the rate may be higher.
Dr. Peacock: That’s exactly my point. In the emergency department we see a mixed bag. We see many people who have had no prior events and have no acute event occurring. So in that setting you are going to get results that suggest that no intervention is required, whereas in that small percentage of patients in whom something is happening, your drug choice may be different.
Dr. Alexander: We are still talking about resistance to antiplatelet drugs as though it were a patient-level variable, but it’s my impression that it changes over time and within a patient.
Dr. Kottke-Marchant: It can change over time. There aren’t many good longitudinal studies. Most of the studies of “aspirin resistance” are really snapshot studies with measurements taken at one point in time. A term I prefer is “platelet reactivity.” To really assess treatment efficacy, we are going to have to look at the basal level of platelet reactivity.
WHAT ROLE FOR GENOTYPING IN GUIDING ANTIPLATELET THERAPY?
Dr. Bhatt: Dr. Peacock alluded to a potential role for genetic testing. Dr. Sabatine, you have done a lot of interesting work with genotyping in the TRITON-TIMI 38 study of prasugrel and clopidogrel. What is the future role of genotyping in determining which antiplatelet therapy is best for which patient?
Dr. Sabatine: As I mentioned, cytochrome P450 enzymes play a critical role in the metabolism of clopidogrel. These enzymes are fairly polymorphic—mutations in their encoding genes are responsible for subtle changes in effect, unlike the traditional mutations that we think about for sickle cell disease, for example. A wealth of data has been published showing that genetic variants are associated with decreased functional activity of cytochrome P450 enzymes, demonstrating the pharmacologic importance of these variants.
Individuals who carry variant alleles appear to respond differently to clopidogrel. A variety of small studies show that those who carry specific variants—particularly in the CYP2C19 enzyme, but in other enzymes as well—appear to have a diminished response to clopidogrel. There are also data showing that individuals with a diminished response to clopidogrel have worse outcomes.4 Our group is studying the impact of genetic variants that decrease the functional activity of cytochrome P450 enzymes on clinical outcomes. (Editor’s note: This study has since been published by Mega et al.5)
The practical implication may lie in point-of-care genotyping, which appears possible and will be clinically useful if a strong link can be demonstrated between genotype and outcomes. If point-of-care genotyping becomes practical, it will raise the question of whether both genotyping and platelet aggregation testing are needed. I think they might indeed be complementary in risk prediction, as is the case with genetic variants that affect low-density lipoprotein cholesterol (LDL-C) levels. In the lipid arena, we have seen that genetic effects and lipid levels provide independent incremental information about risk. That’s because of the high degree of variation in LDL-C levels: an LDL-C measurement is a snapshot in time, yet a variety of factors can influence LDL-C levels. In contrast, genotype is an invariant factor. Similarly, in the platelet arena, platelet aggregation studies and genotyping may be synergistic in predicting an individual’s predisposition to events and response to medications.
Dr. Bhatt: While we’re discussing pathways of metabolism, the literature, though scant, suggests a potential interaction between proton pump inhibitors and clopidogrel. I was co-chair of a recent American College of Cardiology/ American Heart Association/American College of Gastro-enterology consensus document that endorsed liberal use of proton pump inhibitors in patients who are at gastrointestinal risk, including those on antiplatelet therapy.6 The gastroenterologists believed strongly that proton pump inhibitors were safe and in fact underused in these patients. What do you think about the clopidogrel–proton pump inhibitor interaction? Should we be concerned?
Dr. Sabatine: Proton pump inhibitors are not only substrates for, but also inhibitors of, CYP2C19, a key enzyme that helps transform clopidogrel into an active metabolite. For this reason, there has been interest in whether concomitant use of proton pump inhibitors would blunt the efficacy of clopidogrel. The same concern was raised about giving clopidogrel with certain statin drugs that are also metabolized by the cytochrome P450 system, and several studies have shown an effect of these statins on clopidogrel’s platelet inhibition. However, there is no evidence that coadministration of these statins has affected clinical outcomes with clopidogrel in clinical trials. So it may be that while competition for the cytochrome P450 system is one factor, it’s not enough of a factor to tip the scale and result in a clinical event. The same may be true of coadministration of proton pump inhibitors; meanwhile, we await definitive data that concomitant use with clopidogrel leads to higher rates of ischemic events.
DIAGNOSTIC UNCERTAINTY IN THE EMERGENCY SETTING
Dr. Bhatt: We heard about quite a few new antiplatelet drugs in Dr. Sabatine’s presentation, some of which will likely be taken up in clinical practice. Dr. Peacock, from an emergency department perspective, how will you integrate all these new agents with the numerous therapies already available? What should emergency departments do to come to grips with and ultimately take advantage of these different forms of therapy as well as emerging platelet function tests?
Dr. Peacock: The piece that’s unique or especially pertinent to the emergency department is diagnostic uncertainty. Diagnosis and management are easy when a patient has an ST-elevation MI because we all know what that looks like and we know what to do in response. To some extent non-ST-elevation MI is fairly simple too. ACS is a lot more difficult because we don’t have a good definition for unstable angina, and that’s where diagnosis and management become problematic. And with high-sensitivity troponins coming out now, the question of non-ST-elevation MI is going to get more and more confusing because we will have a lot more patients who meet criteria without having an acute coronary artery event.
So it is going to be important that studies be designed correctly. A lot of the studies reviewed today were efficacy studies, showing that a particular drug works well in a carefully defined population, but they were not efficiency studies: they did not take into account the real-world diagnostic uncertainty—and inevitable misdiagnoses—that emergency departments encounter before starting therapy.
Take the CURE trial, for example. It was a great study, showing that clopidogrel reduced the hazard ratio for major coronary events by 20% in patients with unstable angina,7 and the message was that everybody should be using clopidogrel. A close look at the study, however, reveals that about half the patients did not receive clopidogrel in the emergency department. When patients did receive it early, it was driven by the cardiologist, who was absolutely certain of the diagnosis. But if the study was not designed to test early use, then it is a big leap to extrapolate its findings to this circumstance.
Many of the patients in the CURE trial were enrolled the day after presentation, when their diagnosis was certain—ie, they had a rise in troponin after their symptoms. But when a patient first arrives in the emergency department, we are not certain of the diagnosis. And if we use a drug such as clopidogrel, with a duration of action as long as 5 days, we have committed the entire medical system to a certain course of management for that period of time. If we get the diagnosis wrong, this commitment could restrict management options for up to 5 days.
The question for emergency physicians becomes, “How long is long enough to know whether I can pull the trigger on a therapy and be correct?” With all the new drugs coming along, the way to answer this is to do efficiency studies in a real-world environment in addition to efficacy studies.
Dr. Alexander: Yes, one of the biggest limitations of antiplatelet drug studies to date is that they usually haven’t really addressed the timing of drug initiation. We often assume that if a drug is shown to be beneficial, then it should be started as soon as possible. As we just heard, that may have been an unfounded extrapolation from the CURE trial. The same sort of thing happened with the ISIS trial of aspirin in patients with ST-elevation MI.8 In response to the ISIS results, clinicians rushed to give patients aspirin right away even though many of the patients in the trial may have received their aspirin the day after presentation. For these reasons, the EARLY-ACS study,9 which is addressing a very simple question—whether early upstream use of glycoprotein IIb/IIIa inhibitors is beneficial—has been a challenging trial to complete.
WHAT ROLE FOR THIENOPYRIDINE PRETREATMENT?
Dr. Bhatt: Dr. Sabatine, you presented data from the large TRITON-TIMI 38 trial comparing prasugrel with clopidogrel. I’m interested in how you would use prasugrel in practice, assuming it receives marketing approval, especially in light of its bleeding risk, particularly in patients in whom coronary artery bypass graft surgery (CABG) is planned. Many hospitals pretreat patients with clopidogrel in the emergency department. How would you manage a patient who shows up in the emergency room with ACS? Would you give clopidogrel, would you wait and give prasugrel, or would you do something else? If you gave clopidogrel, what loading dose would you use—300 mg, 600 mg, or, as some have suggested, 900 or 1,200 mg?
Dr. Sabatine: I am a strong proponent of pretreatment. Data from multiple studies show a benefit to this strategy, and even the original CURE trial showed a roughly 30% reduction in ischemic events within the first 24 hours of clopidogrel initiation.7
I think the dosing strategy depends on how the patient is going to be managed. If management is going to be conservative, then I would start the patient on 300 mg of clopidogrel when he or she came in. If the patient is going to the cardiac catheterization laboratory in a few hours, I would pretreat with 600 mg of clopidogrel. For prasugrel, the need for pretreatment is less clear, given the drug’s faster onset of action and greater degree of platelet inhibition. In the TRITON-TIMI 38 study,10 prasugrel was given, by and large, after diagnostic angiography, and thus one could use that approach in practice.
In terms of clopidogrel versus prasugrel, I would embrace prasugrel for the large majority of my patients, being mindful of the risk of bleeding. I would not hesitate to give the medication to diabetics or to younger, more robust patients. The 50% reduction in stent thrombosis with prasugrel versus clopidogrel in TRITON-TIMI 38 is huge,11 given that the risk of death with stent thrombosis is probably 25% or greater. So I would want to have prasugrel on board to reduce the risk of stent thrombosis, especially if a drug-eluting stent were being implanted.
Dr. Bhatt: Dr. Alexander, let’s get your take on a similar scenario. Assuming that prasugrel gains marketing approval, how would you manage patients with non-ST-elevation MI who present to the emergency department? Would you pretreat with clopidogrel? Would you wait until angiography and then, depending on the anatomy, treat with prasugrel? Or would you potentially pretreat with prasugrel, which has not been studied and would not be a labeled indication? How would you reconcile the data?
Dr. Alexander: At Duke, I expect that prasugrel will not be used prior to the catheterization laboratory in patients with non-ST-elevation ACS due to concerns about whether the patients will undergo PCI or be managed medically or with CABG.
Dr. Bhatt: That makes sense, since there was a fair amount of bleeding with prasugrel in those patients in TRITON-TIMI 38.
Dr. Alexander: Correct. Moreover, at Duke we don’t use as much upstream clopidogrel as we would, based on the evidence, if I were managing all the patients. There is still a lot of pushback about upstream clopidogrel from our surgeons because patients are going to surgery quickly these days, sometimes just a day after catheterization, and that’s when a loading dose of clopidogrel can be problematic. We are also still fairly heavy users of glycoprotein IIb/IIIa inhibitors.
Where I can see prasugrel being used prior to the cath lab at Duke is in ST-elevation MI, where the rate of PCI is very high. In primary angioplasty for ST-elevation MI, it would likely be given upstream. The bigger issue for us will be that we serve as a referral base for a lot of regional hospitals, and thus have some influence on their practices.
Dr. Bhatt: In that case, what would you advise those regional hospitals to do for non-ST-elevation MI?
Dr. Alexander: For the time being, we would advise continuing with our current practice, which is to load clopidogrel in patients in whom there is a reasonable certainty that CABG will not be performed, and to use glycoprotein IIb/IIIa inhibitors in high-risk patients. As we get more experience with prasugrel or with additional trial results, however, that practice could easily change.
Dr. Bhatt: So you would still use glycoprotein IIb/IIIa inhibitors?
Dr. Alexander: Yes, I advocate upstream clopidogrel use, but not all my colleagues do. Based on the guidelines, I’d use one or the other—either clopidogrel or a glycoprotein IIb/IIIa inhibitor. As I mentioned in my talk, if a patient is at high risk for bleeding, I am more inclined to use clopidogrel, although patients at higher risk of bleeding are often at higher risk for ischemic events as well.
WHAT’S DRIVEN THE DROPOFF IN GLYCOPROTEIN IIb/IIIa INHIBITOR USE?
Dr. Bhatt: While we’re on the topic of glycoprotein IIb/IIIa inhibitors, a question card from the audience asks why there has been a decrease in glycoprotein IIb/ IIIa inhibitor use and whether this decline is appropriate or inappropriate. Have clopidogrel pretreatment, higher loading doses of clopidogrel, and use of the direct thrombin inhibitor bivalirudin contributed to the decrease in glycoprotein IIb/IIIa inhibitor use?
Dr. Alexander: I do think that the decline has been driven by the changing environment, with greater use of other antithrombotic strategies that include clopidogrel and bivalirudin, as you suggest, as well as an increased attention to bleeding. From an evidence-based standpoint, we don’t know whether the decrease in glycoprotein IIb/IIIa use is appropriate or not because the studies of these agents were conducted before the widespread upstream use of clopidogrel and bivalirudin. Clopidogrel is attractive because it’s a pill given as one dose in the emergency department, the wards, or the catheterization laboratory, rather than a much more complicated infusion with weight-based dosing and dosage adjustments based on creatinine clearance. It is possible that we should perhaps be dosing clopidogrel the same way, but we don’t know that yet.
PRASUGREL IN PRACTICE: HOW LOW CAN THE DOSE GO, AND IS THERE A GENDER EFFECT?
Dr. Bhatt: Let’s stick with this focus on dosing but turn back to discussion of prasugrel. In your presentation of the TRITON-TIMI 38 data, Dr. Sabatine, you proposed a potential prasugrel dosage modification, down to a 5-mg loading dose, in subgroups that were identified as being at high bleeding risk—namely, elderly patients and patients with low body weight. However, no outcomes data with 5 mg of prasugrel came out of TRITON-TIMI 38.10 Is this proposed modification based on pharmacokinetic extrapolation? Could clinicians be comfortable using 5 mg of prasugrel, assuming the drug receives regulatory approval and a 5-mg tablet would be available?
Dr. Sabatine: Of course, evidence at the grade A level would consist of a trial showing that patients who received a lower dose enjoyed the same benefit as those who got standard dosing in TRITON-TIMI 38—a 60-mg loading dose followed by 10 mg/day—with an acceptable risk profile. However, such a trial would be difficult and costly to conduct, and would take roughly half a decade to pull off. It is only through large trials like TRITON-TIMI 38 that you identify subgroups that respond differently, and then to go back and do a separate trial for those subgroups takes a great deal of time. It may not be practical.
I think the Food and Drug Administration is moving toward embracing careful pharmacokinetic/pharmacodynamic substudies within trials, with these substudies having adequate numbers of subjects to provide a sense for the ideal target dose and what an acceptable dose range would be, without limiting approval to a single dose. The analogy would be warfarin dosing, with the aim being to figure out an acceptable dose range, discover which patients fall outside that range, and then model the effect of a lower dose in those patients. Thus, approving a 5-mg dose of prasugrel based on TRITON-TIMI 38 would be a reasonable approach if this dose passed muster under pharmacokinetic/pharmacodynamic modeling. If this approach were taken, there would clearly be a need for postmarketing surveillance to confirm whether the modeling on the effects of the lower dose was borne out by actual outcomes.
Dr. Bhatt: The audience has posed another interesting question raised by TRITON-TIMI 38: Can you comment on the lesser effect of prasugrel in women?
Dr. Sabatine: It is true that there was not a statistically significant effect of prasugrel among women in TRITON-TIMI 38, but statistical tests among subgroups found no significant heterogeneity for the effect between men and women, and that is the relevant measure to determine any gender effect. Keep in mind that not all subgroups represent a univariate slice of the population. For example, women generally have lower body weight than men, and since prasugrel’s net clinical benefit was reduced in patients with lower body weight, that may explain some of the differing extent of effect between men and women.
Dr. Bhatt: That’s a good point about the lack of heterogeneity between men and women. In fact, a meta-analysis of clopidogrel data conducted by one of the fellows I work with revealed that men and women appear to benefit similarly from clopidogrel.12 There was a slight signal of excess bleeding in women, but there were more elderly women in the pooled population, which may have been a confounding factor. As best as anyone can tell, antiplate-let therapy works well in both men and women.
NAVIGATING MANAGEMENT ACROSS THE SPECTRUM OF CARE
Dr. Bhatt: I would like to explore a bit further how all of these issues translate across the spectrum of care, beginning in the emergency department, which we know is a key component of the entire ACS management strategy for a health care system. What should emergency medicine doctors do, given all of the potential options—clopidogrel, different loading doses of clopidogrel, prasugrel, glycoprotein IIb/IIIa inhibitors, even bivalirudin?
Dr. Peacock: It depends on the practice setting. Some emergency physicians work at community hospitals with no backup. They must have relationships with the larger centers to which they’ll be transferring patients, because ACS patients should not be staying at community hospitals. These emergency physicians must have close relationships with the physicians who will be receiving their patients, and they know the potential head-butting with surgeons surrounding early clopidogrel use better than anybody does. If they treat with clopidogrel in the emergency room, and it turns out that the patient needs to go to the catheterization laboratory, can the receiving hospital use platelet testing to shorten the standard 5-day interval from treatment to catheterization?
Dr. Bhatt: Yes, that’s a rather useful, although not completely validated, way of using point-of-care platelet testing—to potentially reduce the time to surgery.
Dr. Peacock: Right. So if the policies for handling these types of transfer-related issues are worked out in advance, all players have a pathway to follow, which can allow quick action when necessary. If you don’t have these issues worked out in advance, you either lose many opportunities to act quickly in the emergency room or you risk taking actions that will cause problems later in the course of management.
Dr. Alexander: I totally agree. The key is to sit down with all the players involved—the surgeons, the interventional cardiologists, the intensivists, the emergency room personnel—and come up with strategies for different populations of patients. Write down the collective strategy and hang it on the wall so that everybody can be comfortable with it. The strategy can be reevaluated when prasugrel or other new antithrombotic drugs come on the market.
Dr. Peacock: The other environment is the academic center, which is even more challenging, but for different reasons. At a large academic center like the Cleveland Clinic, any of 25 different cardiologists may be taking call and receiving patients from the emergency department on a particular night. A lot of phone interaction is required to elicit the planned management strategy, including if and when the patient will be going to the cath lab. Individualizing care to a particular cardiologist then becomes a time-consuming challenge, especially in clinical situations where outcomes are time-dependent.
Dr. Alexander: Agreed. Management needs to be integrated across the entire spectrum of care. The anticoagulants that we plan to use in the cath lab will affect the antithrombotic regimen used upstream.
Dr. Kottke-Marchant: One circumstance where platelet function testing has been helpful is in determining the washout of the clopidogrel effect before surgery. At Cleveland Clinic, we have implemented platelet function testing in this circumstance instead of waiting a blanket 5 days after clopidogrel administration to go to surgery. A return to normal platelet function on platelet aggregation testing, depending on the cutoff value used, is an indicator that the patient can proceed to surgery.
Dr. Bhatt: That’s a logical approach. How should we be using antiplatelet therapy in the medically managed patient, Dr. Alexander?
Dr. Alexander: When I think of medical management, I include patients who don’t go to the cath lab, but also those who do, with regards to their management prior to and following their time in the cath lab.
In patients who don’t go to the cath lab for angiography, the ACC/AHA guidelines recommend aspirin and either clopidogrel, a glycoprotein IIb/IIIa inhibitor, or both.1 In making this choice, I consider the patient’s risk of bleeding and the dosing complexity of the regimen, especially with the use of glycoprotein IIb/IIIa inhibitors in a patient with renal insufficiency. In a patient at relatively low risk for bleeding, I often use both clopidogrel and a glycoprotein IIb/IIIa inhibitor, although this strategy does not have a lot of data to support it.
The more challenging population consists of patients who go to the cath lab but do not undergo PCI; this population is managed medically too. We often drop the ball with clopidogrel in this population. Many patients in whom PCI is not performed do not receive clopidogrel upstream, for all of the reasons we’ve discussed, and there is pretty good evidence that if clopidogrel is not instituted before hospital discharge, the patient is not likely to be receiving it at 30 days either. We have an obligation to treat these patients.
Treatment following bypass surgery is much murkier, and I don’t really know what we should be doing. The ACC/AHA guidelines suggest that clopidogrel be started in a patient with non-ST-elevation ACS after bypass surgery,1 but I believe the evidence to support that recommendation is pretty weak.
Dr. Bhatt: Well, the CURE trial did contain a sizeable group that underwent bypass surgery,7 and although this group was underpowered in some respects, it was still a very large group, so I personally favor treatment in those patients. We should mention that an ongoing trial called TRILOGY ACS is comparing clopidogrel and prasugrel specifically in patients who are being managed medically,13 so more data on this strategy will be emerging.
ARE GUIDELINES DESTINED TO BECOME EVER MORE COMPLEX?
Dr. Bhatt: Here’s a comment and question from the audience that pulls together a lot of what we’ve discussed while also looking forward: The antiplatelet therapy guidelines are already complicated. If the ongoing studies of emerging antiplatelet drugs all have results that are qualitatively similar to those of the TRITON-TIMI 38 study of prasugrel—ie, better efficacy with more potent therapy but more bleeding—how do you foresee these antiplatelet drugs being used in clinical practice?
Dr. Sabatine: The contrast between the US guidelines and the European guidelines for ACS management is stark. The US guidelines—from the ACC and AHA1—are essentially an encyclopedia that includes nearly every trial of anti-platelet therapy in ACS along with complicated algorithms; they do a wonderful job of being complete. The European guidelines14 are probably one tenth the size of their US counterpart document, and they suggest treatments for various patient types; they are very simple.
In a sense, the US guidelines lay out the data and force practitioners to evaluate the trials and consider how our patients fit into the study populations. In this way they are analogous to current guidelines for anticoagulant therapy. Several anticoagulants have been compared with heparin in clinical trials. These newer anticoagulants appear to reduce the risk of ischemic events compared with heparin; some have lower rates of bleeding, while others have higher rates of bleeding. There have been few head-to-head studies of these agents, however, so we wind up with guidelines that are not definitive but rather suggest agents to “consider” in various settings.
It’s unlikely that a head-to-head trial will be conducted comparing prasugrel with the reversible P2Y12 antagonist AZD6140, assuming that both are approved for marketing. If the drugs appear equally efficacious in placebo-controlled trials, it will take consensus to determine the appropriate choice at your hospital, factoring in your patient profile, the cost of the drugs, and other variables. It’s more complicated when one agent is slightly more efficacious but causes more bleeding or, conversely, a little less efficacious but less apt to cause bleeding. In such cases, you may need to tailor therapy to the patient, trying to gauge bleeding risk. All of the emerging data appear to point to the importance of bleeding on outcomes: patients who bleed fare poorly, in part due to the bleeding itself and in part perhaps because they have a proclivity for bleeding.
THE FUTURE: MONITORING-BASED DOSING AND NICHE ANTIPLATELETS?
Dr. Bhatt: That’s a good observation. Let’s wrap up by having the other panelists share any final thoughts you may have.
Dr. Alexander: I’d like to return to the issue of measuring antiplatelet response and using it to guide therapy. Earlier we cited the examples of antihypertensive therapy and lipid-lowering therapy to support this model of monitoring-based treatment. Guidelines for dyslipidemia treatment recommend using LDL-C levels to guide therapy, but this practice is difficult to study in a randomized trial. In fact, none of the randomized trials of statins used LDL-C levels to guide therapy. They all studied fixed doses of statins versus placebo or fixed doses of another statin. Higher doses of statins were always beneficial compared with lower doses, and this finding was extrapolated into the guidelines as a justification to treat to target LDL-C levels.
Dr. Bhatt: It’s not even necessarily clear that LDL-C level is the best target, if you consider the JUPITER trial, in which patients received statin therapy based on their baseline level of high-sensitivity C-reactive protein, not their LDL-C level.15 It goes to show how incomplete our knowledge of a class of drugs may be, even decades after the drugs are introduced.
Dr. Kottke-Marchant: To speak to Dr. Alexander’s point, dose adjustment guided by platelet monitoring is a bit more problematic for antiplatelet drugs that are irreversible inhibitors, such as clopidogrel and aspirin, than for those that are reversible inhibitors, which are being developed and may eventually make more sense to use. From a drug development standpoint, a drug that requires monitoring and dose adjustment will not gain wide acceptance because it will increase medical costs and morbidity.
Dr. Bhatt: Yes, we know from experience with warfarin that doctors and patients don’t like the ongoing need for monitoring and testing.
Dr. Peacock: The drugs that are going to be adopted by the emergency department are those with the shortest half-lives, for several reasons: (1) using a drug with a short half-life won’t commit us to a particular course of action; (2) the potential for drug interactions is lower; and (3) in the event of an erroneous diagnosis, the consequence of misapplication may be mitigated by early recognition and termination of the drug. If we later decide that we’ve gone down the wrong therapeutic road or reached a wrong diagnosis, or if a complication occurs, we can turn off the therapy quickly. That level of flexibility is needed.
Dr. Kottke-Marchant: I think we are moving into an era of niche antiplatelet drugs. One might be used in a patient going to surgery, for example, and another for long-term therapy.
Dr. Peacock: One thing that I don’t have a feel for is how to transition from one drug to another. When you change drugs for a patient, it so often seems like it goes badly. If we’re eventually going to use drugs with ultra-short half-lives in the in the emergency department for the first day or two, and then switch patients to a pill for a week, a lot more platelet function testing may be needed.
CASE STUDY: THROMBOSIS AFTER STENTING DESPITE ANTIPLATELET THERAPY
Dr. Deepak Bhatt: We have taken in a wealth of terrific information from the three preceding talks in this symposium. Let’s now share some questions from the audience and explore some of the points raised in the preceding talks in a bit more practical detail for clinicians. Our three prior speakers are joined in this panel discussion by Cleveland Clinic’s Dr. Frank Peacock, who brings an emergency medicine perspective.
Let’s begin with a case-based question supplied from the audience. The patient is a 42-year-old morbidly obese man without diabetes who had a non-ST-elevation myocardial infarction (MI) less than 1 year ago. A drug-eluting stent was placed at the time of his MI, and now restenosis has occurred. He is on aspirin and clopidogrel 75 mg/day. Do you recommend running a vasodilator-stimulated phosphoprotein (VASP) test and possibly increasing the clopidogrel dose to 150 mg/ day, or should the patient just be switched to prasugrel (assuming it is commercially available) without running the VASP test?
I’ll take a quick initial stab at this question. Studies of antiplatelet therapies to prevent instent restenosis have been a mixed bag. Some of the trials with glycoprotein IIb/IIIa inhibitors have shown an effect on restenosis, but most have not. Similarly, some of the analyses of the thienopyridines ticlopodine and clopidogrel have shown an effect on restenosis, but most have not.
For the most part, restenosis does not appear to be heavily mediated by platelets, at least not in a way that we can influence by therapy. On the other hand, stent thrombosis is highly platelet mediated, so I would alter the case to one in which stent thrombosis is the clinical problem. Assuming that the patient has been adherent to his antiplatelet regimen, which tests would you perform, and how would you act on the information from those tests?
Dr. Kandice Kottke-Marchant: The 2007 guidelines on acute coronary syndrome (ACS) management from the American College of Cardiology and American Heart Association (ACC/AHA)1 do not address platelet function testing, and almost none of the clinical trials of antiplatelet agents had an arm that included testing and dose adjustment based on platelet function studies. Platelet testing is available at some centers; at Cleveland Clinic, we use platelet aggregation testing. One can do platelet aggregation testing on a patient-by-patient basis; if inhibition appears to be suboptimal, a treatment decision should be made, but there is little guidance from the literature to steer that decision. I have seen clinicians increase the dose of clopidogrel or aspirin in response to platelet function tests, which occasionally triggers a confirmatory call from the pharmacy department.
Dr. Bhatt: When I was still at Cleveland Clinic, our chief medical resident did an analysis of platelet function testing, and it was remarkable how much testing was performed and how often it changed management, largely in the absence of any outcomes data, as Dr. Kottke-Marchant pointed out. Dr. Alexander, what are your recommendations with respect to platelet function testing today?
Dr. John Alexander: The case you describe is one in which applying evidence is not easy. There are no trials to supply any evidence to change therapy in this patient, a morbidly obese man receiving 75 mg/day of clopidogrel. There is certainly a rationale, however, to believe that a standard “one size fits all” 75-mg daily dose of clopidogrel may not be enough for him. The trade-off with a higher dosage is a higher risk of bleeding, however, so I would first be sure that he has been adherent to his current regimen of clopidogrel and aspirin.
Dr. Bhatt: Is there a role for point-of-care testing to determine whether he is adherent to the medicines?
Dr. Kottke-Marchant: Several of the point-of-care tests, such as the VerifyNow rapid platelet function analyzer, have specific cartridges for aspirin and for clopidogrel. If platelets were not being inhibited, it would suggest that the doses were too low, given the patient’s weight, but you probably would not be able to determine whether he was resistant to clopidogrel.
Dr. W. Frank Peacock: One way to verify that patients are taking their aspirin is to take a small urine sample and squirt in 2 mL of ferric chloride. If the sample turns purple, it means they are taking their aspirin. Once that is established, you can try to determine whether the drug is working on their platelets.
Dr. Alexander: Another potential explanation for stent thrombosis is faulty stent placement. In this case I would consider asking an interventional colleague to perform intravascular ultrasonography to make sure the stent was implanted properly before I changed the patient’s antithrombotic therapy.
Dr. Bhatt: That’s a great technical point. We always want to make sure that a case of stent thrombosis is not due to a mechanical problem. We should be asking: Is the stent properly sized and well opposed? Is there a distal dissection or any other issue that could predispose to stent thrombosis?
Dr. Alexander: This case illustrates a host of other challenges that underscore how much more work we need to do to define optimal antiplatelet therapy. Suppose we perform platelet function testing and find a low level of platelet inhibition in this patient with stent thrombosis, and we change his antiplatelet regimen. When should we test him again? If we retest in 3 months and find that he has a higher than expected level of platelet inhibition on the new antiplatelet regimen, do we dial down the intensity? Once again, there is no evidence to guide these decisions, and levels of platelet inhibition are driven not just by the medications but also by what is going on in the patient’s platelets—it is quite multifactorial.
POINT-OF-CARE PLATELET FUNCTION TESTING: CURRENT LIMITS, FUTURE ROLES
Dr. Bhatt: While we’re discussing platelet function testing, I found it interesting, Dr. Kottke-Marchant, that you said the use of bleeding time as a platelet test is finally going away. Testing of bleeding time has been around forever, but I agree that it doesn’t have much value in clinical practice. Do you think bleeding time will continue to have any role in drug development? Most phase 2 trials, and certainly phase 1 trials, still capture bleeding time to assess whether or not a drug is working. Should that, too, be jettisoned, or does bleeding time still have some merit in this context?
Dr. Kottke-Marchant: I would jettison it in drug development as well because of the considerable variability in bleeding time. It is not a test that can be standardized, and no quality control can be done. The results depend on skin turgor, age, and many other variables.
We need a global assay that will pick up multiple aspects of platelet function, such as flow-based adhesion, aggregation, and granule release. The bleeding time is a shear-dependent test, whereas the platelet aggregation test that is used in most drug trials is an artificial assay that measures only aggregation, but not under shear. The VerifyNow rapid platelet function analyzer does not measure platelets under shear and is not a global assay.
Dr. Marc Sabatine: I would underscore the need for a reliable point-of-care test of platelet function. When we prescribe a statin or an antihypertensive drug, we don’t just send the patient out the door and hope that everything will be okay. We measure the response, knowing that genotype, environmental factors, or medication factors can affect the response. When we prescribe an antiplatelet drug, we need a reliable point-of-care device to make certain that the patient is getting appropriate platelet inhibition.
I am reminded of a recent study of point-of-care measurement of platelet inhibition in patients receiving clopidogrel prior to nonemergent percutaneous coronary intervention (PCI).2 Rather than just treating patients with PCI and sending them out the door, the investigators kept giving patients clopidogrel and measuring their platelet inhibition until they achieved an appropriate degree of inhibition, after which PCI was performed. Event rates were significantly reduced in the patient group treated this way, which suggests a need to individualize therapy and move away from the “one size fits all” mindset.
Dr. Bhatt: Dr. Peacock, you’ve led a study of point-of-care assays in the emergency department. What might ultimately be the role of point-of-care testing in emergency medicine, and might it influence drug selection?
Dr. Peacock: My short answer is that I think there will be a role for point-of-care testing, with all the caveats that have been discussed. There may even be a day when we do genetic testing and look for DNA. Honestly, though, I’m somewhat of a skeptic because I’m not looking at the genetics. I see many patients who do crack cocaine who come to the emergency room with chest pain and have risk factors, but I send these patients home because they are not having an event. The real question is, “Is it an event?” If a patient is having an event and he or she has platelet resistance or hyperreactivity—whatever we term it—then you have to decide the next step.
As you mentioned, we just completed a study that evaluated a couple hundred patients for platelet inhibition resistance to aspirin, and one finding was that the incidence of platelet resistance to aspirin was much lower than we had anticipated. Studies from the literature suggest that the prevalence of resistance is around 30%, but in our study it was 6.5%.3
Dr. Kottke-Marchant: It depends on how and in whom you measure resistance. Different tests will give you different numbers. Even among studies using the same measurement techniques, the results depend on the patient population. If it’s a fairly stable cardiac population, you may see aspirin resistance rates of 4% or 5%. If it’s a population of patients who have had multiple MIs, the rate may be higher.
Dr. Peacock: That’s exactly my point. In the emergency department we see a mixed bag. We see many people who have had no prior events and have no acute event occurring. So in that setting you are going to get results that suggest that no intervention is required, whereas in that small percentage of patients in whom something is happening, your drug choice may be different.
Dr. Alexander: We are still talking about resistance to antiplatelet drugs as though it were a patient-level variable, but it’s my impression that it changes over time and within a patient.
Dr. Kottke-Marchant: It can change over time. There aren’t many good longitudinal studies. Most of the studies of “aspirin resistance” are really snapshot studies with measurements taken at one point in time. A term I prefer is “platelet reactivity.” To really assess treatment efficacy, we are going to have to look at the basal level of platelet reactivity.
WHAT ROLE FOR GENOTYPING IN GUIDING ANTIPLATELET THERAPY?
Dr. Bhatt: Dr. Peacock alluded to a potential role for genetic testing. Dr. Sabatine, you have done a lot of interesting work with genotyping in the TRITON-TIMI 38 study of prasugrel and clopidogrel. What is the future role of genotyping in determining which antiplatelet therapy is best for which patient?
Dr. Sabatine: As I mentioned, cytochrome P450 enzymes play a critical role in the metabolism of clopidogrel. These enzymes are fairly polymorphic—mutations in their encoding genes are responsible for subtle changes in effect, unlike the traditional mutations that we think about for sickle cell disease, for example. A wealth of data has been published showing that genetic variants are associated with decreased functional activity of cytochrome P450 enzymes, demonstrating the pharmacologic importance of these variants.
Individuals who carry variant alleles appear to respond differently to clopidogrel. A variety of small studies show that those who carry specific variants—particularly in the CYP2C19 enzyme, but in other enzymes as well—appear to have a diminished response to clopidogrel. There are also data showing that individuals with a diminished response to clopidogrel have worse outcomes.4 Our group is studying the impact of genetic variants that decrease the functional activity of cytochrome P450 enzymes on clinical outcomes. (Editor’s note: This study has since been published by Mega et al.5)
The practical implication may lie in point-of-care genotyping, which appears possible and will be clinically useful if a strong link can be demonstrated between genotype and outcomes. If point-of-care genotyping becomes practical, it will raise the question of whether both genotyping and platelet aggregation testing are needed. I think they might indeed be complementary in risk prediction, as is the case with genetic variants that affect low-density lipoprotein cholesterol (LDL-C) levels. In the lipid arena, we have seen that genetic effects and lipid levels provide independent incremental information about risk. That’s because of the high degree of variation in LDL-C levels: an LDL-C measurement is a snapshot in time, yet a variety of factors can influence LDL-C levels. In contrast, genotype is an invariant factor. Similarly, in the platelet arena, platelet aggregation studies and genotyping may be synergistic in predicting an individual’s predisposition to events and response to medications.
Dr. Bhatt: While we’re discussing pathways of metabolism, the literature, though scant, suggests a potential interaction between proton pump inhibitors and clopidogrel. I was co-chair of a recent American College of Cardiology/ American Heart Association/American College of Gastro-enterology consensus document that endorsed liberal use of proton pump inhibitors in patients who are at gastrointestinal risk, including those on antiplatelet therapy.6 The gastroenterologists believed strongly that proton pump inhibitors were safe and in fact underused in these patients. What do you think about the clopidogrel–proton pump inhibitor interaction? Should we be concerned?
Dr. Sabatine: Proton pump inhibitors are not only substrates for, but also inhibitors of, CYP2C19, a key enzyme that helps transform clopidogrel into an active metabolite. For this reason, there has been interest in whether concomitant use of proton pump inhibitors would blunt the efficacy of clopidogrel. The same concern was raised about giving clopidogrel with certain statin drugs that are also metabolized by the cytochrome P450 system, and several studies have shown an effect of these statins on clopidogrel’s platelet inhibition. However, there is no evidence that coadministration of these statins has affected clinical outcomes with clopidogrel in clinical trials. So it may be that while competition for the cytochrome P450 system is one factor, it’s not enough of a factor to tip the scale and result in a clinical event. The same may be true of coadministration of proton pump inhibitors; meanwhile, we await definitive data that concomitant use with clopidogrel leads to higher rates of ischemic events.
DIAGNOSTIC UNCERTAINTY IN THE EMERGENCY SETTING
Dr. Bhatt: We heard about quite a few new antiplatelet drugs in Dr. Sabatine’s presentation, some of which will likely be taken up in clinical practice. Dr. Peacock, from an emergency department perspective, how will you integrate all these new agents with the numerous therapies already available? What should emergency departments do to come to grips with and ultimately take advantage of these different forms of therapy as well as emerging platelet function tests?
Dr. Peacock: The piece that’s unique or especially pertinent to the emergency department is diagnostic uncertainty. Diagnosis and management are easy when a patient has an ST-elevation MI because we all know what that looks like and we know what to do in response. To some extent non-ST-elevation MI is fairly simple too. ACS is a lot more difficult because we don’t have a good definition for unstable angina, and that’s where diagnosis and management become problematic. And with high-sensitivity troponins coming out now, the question of non-ST-elevation MI is going to get more and more confusing because we will have a lot more patients who meet criteria without having an acute coronary artery event.
So it is going to be important that studies be designed correctly. A lot of the studies reviewed today were efficacy studies, showing that a particular drug works well in a carefully defined population, but they were not efficiency studies: they did not take into account the real-world diagnostic uncertainty—and inevitable misdiagnoses—that emergency departments encounter before starting therapy.
Take the CURE trial, for example. It was a great study, showing that clopidogrel reduced the hazard ratio for major coronary events by 20% in patients with unstable angina,7 and the message was that everybody should be using clopidogrel. A close look at the study, however, reveals that about half the patients did not receive clopidogrel in the emergency department. When patients did receive it early, it was driven by the cardiologist, who was absolutely certain of the diagnosis. But if the study was not designed to test early use, then it is a big leap to extrapolate its findings to this circumstance.
Many of the patients in the CURE trial were enrolled the day after presentation, when their diagnosis was certain—ie, they had a rise in troponin after their symptoms. But when a patient first arrives in the emergency department, we are not certain of the diagnosis. And if we use a drug such as clopidogrel, with a duration of action as long as 5 days, we have committed the entire medical system to a certain course of management for that period of time. If we get the diagnosis wrong, this commitment could restrict management options for up to 5 days.
The question for emergency physicians becomes, “How long is long enough to know whether I can pull the trigger on a therapy and be correct?” With all the new drugs coming along, the way to answer this is to do efficiency studies in a real-world environment in addition to efficacy studies.
Dr. Alexander: Yes, one of the biggest limitations of antiplatelet drug studies to date is that they usually haven’t really addressed the timing of drug initiation. We often assume that if a drug is shown to be beneficial, then it should be started as soon as possible. As we just heard, that may have been an unfounded extrapolation from the CURE trial. The same sort of thing happened with the ISIS trial of aspirin in patients with ST-elevation MI.8 In response to the ISIS results, clinicians rushed to give patients aspirin right away even though many of the patients in the trial may have received their aspirin the day after presentation. For these reasons, the EARLY-ACS study,9 which is addressing a very simple question—whether early upstream use of glycoprotein IIb/IIIa inhibitors is beneficial—has been a challenging trial to complete.
WHAT ROLE FOR THIENOPYRIDINE PRETREATMENT?
Dr. Bhatt: Dr. Sabatine, you presented data from the large TRITON-TIMI 38 trial comparing prasugrel with clopidogrel. I’m interested in how you would use prasugrel in practice, assuming it receives marketing approval, especially in light of its bleeding risk, particularly in patients in whom coronary artery bypass graft surgery (CABG) is planned. Many hospitals pretreat patients with clopidogrel in the emergency department. How would you manage a patient who shows up in the emergency room with ACS? Would you give clopidogrel, would you wait and give prasugrel, or would you do something else? If you gave clopidogrel, what loading dose would you use—300 mg, 600 mg, or, as some have suggested, 900 or 1,200 mg?
Dr. Sabatine: I am a strong proponent of pretreatment. Data from multiple studies show a benefit to this strategy, and even the original CURE trial showed a roughly 30% reduction in ischemic events within the first 24 hours of clopidogrel initiation.7
I think the dosing strategy depends on how the patient is going to be managed. If management is going to be conservative, then I would start the patient on 300 mg of clopidogrel when he or she came in. If the patient is going to the cardiac catheterization laboratory in a few hours, I would pretreat with 600 mg of clopidogrel. For prasugrel, the need for pretreatment is less clear, given the drug’s faster onset of action and greater degree of platelet inhibition. In the TRITON-TIMI 38 study,10 prasugrel was given, by and large, after diagnostic angiography, and thus one could use that approach in practice.
In terms of clopidogrel versus prasugrel, I would embrace prasugrel for the large majority of my patients, being mindful of the risk of bleeding. I would not hesitate to give the medication to diabetics or to younger, more robust patients. The 50% reduction in stent thrombosis with prasugrel versus clopidogrel in TRITON-TIMI 38 is huge,11 given that the risk of death with stent thrombosis is probably 25% or greater. So I would want to have prasugrel on board to reduce the risk of stent thrombosis, especially if a drug-eluting stent were being implanted.
Dr. Bhatt: Dr. Alexander, let’s get your take on a similar scenario. Assuming that prasugrel gains marketing approval, how would you manage patients with non-ST-elevation MI who present to the emergency department? Would you pretreat with clopidogrel? Would you wait until angiography and then, depending on the anatomy, treat with prasugrel? Or would you potentially pretreat with prasugrel, which has not been studied and would not be a labeled indication? How would you reconcile the data?
Dr. Alexander: At Duke, I expect that prasugrel will not be used prior to the catheterization laboratory in patients with non-ST-elevation ACS due to concerns about whether the patients will undergo PCI or be managed medically or with CABG.
Dr. Bhatt: That makes sense, since there was a fair amount of bleeding with prasugrel in those patients in TRITON-TIMI 38.
Dr. Alexander: Correct. Moreover, at Duke we don’t use as much upstream clopidogrel as we would, based on the evidence, if I were managing all the patients. There is still a lot of pushback about upstream clopidogrel from our surgeons because patients are going to surgery quickly these days, sometimes just a day after catheterization, and that’s when a loading dose of clopidogrel can be problematic. We are also still fairly heavy users of glycoprotein IIb/IIIa inhibitors.
Where I can see prasugrel being used prior to the cath lab at Duke is in ST-elevation MI, where the rate of PCI is very high. In primary angioplasty for ST-elevation MI, it would likely be given upstream. The bigger issue for us will be that we serve as a referral base for a lot of regional hospitals, and thus have some influence on their practices.
Dr. Bhatt: In that case, what would you advise those regional hospitals to do for non-ST-elevation MI?
Dr. Alexander: For the time being, we would advise continuing with our current practice, which is to load clopidogrel in patients in whom there is a reasonable certainty that CABG will not be performed, and to use glycoprotein IIb/IIIa inhibitors in high-risk patients. As we get more experience with prasugrel or with additional trial results, however, that practice could easily change.
Dr. Bhatt: So you would still use glycoprotein IIb/IIIa inhibitors?
Dr. Alexander: Yes, I advocate upstream clopidogrel use, but not all my colleagues do. Based on the guidelines, I’d use one or the other—either clopidogrel or a glycoprotein IIb/IIIa inhibitor. As I mentioned in my talk, if a patient is at high risk for bleeding, I am more inclined to use clopidogrel, although patients at higher risk of bleeding are often at higher risk for ischemic events as well.
WHAT’S DRIVEN THE DROPOFF IN GLYCOPROTEIN IIb/IIIa INHIBITOR USE?
Dr. Bhatt: While we’re on the topic of glycoprotein IIb/IIIa inhibitors, a question card from the audience asks why there has been a decrease in glycoprotein IIb/ IIIa inhibitor use and whether this decline is appropriate or inappropriate. Have clopidogrel pretreatment, higher loading doses of clopidogrel, and use of the direct thrombin inhibitor bivalirudin contributed to the decrease in glycoprotein IIb/IIIa inhibitor use?
Dr. Alexander: I do think that the decline has been driven by the changing environment, with greater use of other antithrombotic strategies that include clopidogrel and bivalirudin, as you suggest, as well as an increased attention to bleeding. From an evidence-based standpoint, we don’t know whether the decrease in glycoprotein IIb/IIIa use is appropriate or not because the studies of these agents were conducted before the widespread upstream use of clopidogrel and bivalirudin. Clopidogrel is attractive because it’s a pill given as one dose in the emergency department, the wards, or the catheterization laboratory, rather than a much more complicated infusion with weight-based dosing and dosage adjustments based on creatinine clearance. It is possible that we should perhaps be dosing clopidogrel the same way, but we don’t know that yet.
PRASUGREL IN PRACTICE: HOW LOW CAN THE DOSE GO, AND IS THERE A GENDER EFFECT?
Dr. Bhatt: Let’s stick with this focus on dosing but turn back to discussion of prasugrel. In your presentation of the TRITON-TIMI 38 data, Dr. Sabatine, you proposed a potential prasugrel dosage modification, down to a 5-mg loading dose, in subgroups that were identified as being at high bleeding risk—namely, elderly patients and patients with low body weight. However, no outcomes data with 5 mg of prasugrel came out of TRITON-TIMI 38.10 Is this proposed modification based on pharmacokinetic extrapolation? Could clinicians be comfortable using 5 mg of prasugrel, assuming the drug receives regulatory approval and a 5-mg tablet would be available?
Dr. Sabatine: Of course, evidence at the grade A level would consist of a trial showing that patients who received a lower dose enjoyed the same benefit as those who got standard dosing in TRITON-TIMI 38—a 60-mg loading dose followed by 10 mg/day—with an acceptable risk profile. However, such a trial would be difficult and costly to conduct, and would take roughly half a decade to pull off. It is only through large trials like TRITON-TIMI 38 that you identify subgroups that respond differently, and then to go back and do a separate trial for those subgroups takes a great deal of time. It may not be practical.
I think the Food and Drug Administration is moving toward embracing careful pharmacokinetic/pharmacodynamic substudies within trials, with these substudies having adequate numbers of subjects to provide a sense for the ideal target dose and what an acceptable dose range would be, without limiting approval to a single dose. The analogy would be warfarin dosing, with the aim being to figure out an acceptable dose range, discover which patients fall outside that range, and then model the effect of a lower dose in those patients. Thus, approving a 5-mg dose of prasugrel based on TRITON-TIMI 38 would be a reasonable approach if this dose passed muster under pharmacokinetic/pharmacodynamic modeling. If this approach were taken, there would clearly be a need for postmarketing surveillance to confirm whether the modeling on the effects of the lower dose was borne out by actual outcomes.
Dr. Bhatt: The audience has posed another interesting question raised by TRITON-TIMI 38: Can you comment on the lesser effect of prasugrel in women?
Dr. Sabatine: It is true that there was not a statistically significant effect of prasugrel among women in TRITON-TIMI 38, but statistical tests among subgroups found no significant heterogeneity for the effect between men and women, and that is the relevant measure to determine any gender effect. Keep in mind that not all subgroups represent a univariate slice of the population. For example, women generally have lower body weight than men, and since prasugrel’s net clinical benefit was reduced in patients with lower body weight, that may explain some of the differing extent of effect between men and women.
Dr. Bhatt: That’s a good point about the lack of heterogeneity between men and women. In fact, a meta-analysis of clopidogrel data conducted by one of the fellows I work with revealed that men and women appear to benefit similarly from clopidogrel.12 There was a slight signal of excess bleeding in women, but there were more elderly women in the pooled population, which may have been a confounding factor. As best as anyone can tell, antiplate-let therapy works well in both men and women.
NAVIGATING MANAGEMENT ACROSS THE SPECTRUM OF CARE
Dr. Bhatt: I would like to explore a bit further how all of these issues translate across the spectrum of care, beginning in the emergency department, which we know is a key component of the entire ACS management strategy for a health care system. What should emergency medicine doctors do, given all of the potential options—clopidogrel, different loading doses of clopidogrel, prasugrel, glycoprotein IIb/IIIa inhibitors, even bivalirudin?
Dr. Peacock: It depends on the practice setting. Some emergency physicians work at community hospitals with no backup. They must have relationships with the larger centers to which they’ll be transferring patients, because ACS patients should not be staying at community hospitals. These emergency physicians must have close relationships with the physicians who will be receiving their patients, and they know the potential head-butting with surgeons surrounding early clopidogrel use better than anybody does. If they treat with clopidogrel in the emergency room, and it turns out that the patient needs to go to the catheterization laboratory, can the receiving hospital use platelet testing to shorten the standard 5-day interval from treatment to catheterization?
Dr. Bhatt: Yes, that’s a rather useful, although not completely validated, way of using point-of-care platelet testing—to potentially reduce the time to surgery.
Dr. Peacock: Right. So if the policies for handling these types of transfer-related issues are worked out in advance, all players have a pathway to follow, which can allow quick action when necessary. If you don’t have these issues worked out in advance, you either lose many opportunities to act quickly in the emergency room or you risk taking actions that will cause problems later in the course of management.
Dr. Alexander: I totally agree. The key is to sit down with all the players involved—the surgeons, the interventional cardiologists, the intensivists, the emergency room personnel—and come up with strategies for different populations of patients. Write down the collective strategy and hang it on the wall so that everybody can be comfortable with it. The strategy can be reevaluated when prasugrel or other new antithrombotic drugs come on the market.
Dr. Peacock: The other environment is the academic center, which is even more challenging, but for different reasons. At a large academic center like the Cleveland Clinic, any of 25 different cardiologists may be taking call and receiving patients from the emergency department on a particular night. A lot of phone interaction is required to elicit the planned management strategy, including if and when the patient will be going to the cath lab. Individualizing care to a particular cardiologist then becomes a time-consuming challenge, especially in clinical situations where outcomes are time-dependent.
Dr. Alexander: Agreed. Management needs to be integrated across the entire spectrum of care. The anticoagulants that we plan to use in the cath lab will affect the antithrombotic regimen used upstream.
Dr. Kottke-Marchant: One circumstance where platelet function testing has been helpful is in determining the washout of the clopidogrel effect before surgery. At Cleveland Clinic, we have implemented platelet function testing in this circumstance instead of waiting a blanket 5 days after clopidogrel administration to go to surgery. A return to normal platelet function on platelet aggregation testing, depending on the cutoff value used, is an indicator that the patient can proceed to surgery.
Dr. Bhatt: That’s a logical approach. How should we be using antiplatelet therapy in the medically managed patient, Dr. Alexander?
Dr. Alexander: When I think of medical management, I include patients who don’t go to the cath lab, but also those who do, with regards to their management prior to and following their time in the cath lab.
In patients who don’t go to the cath lab for angiography, the ACC/AHA guidelines recommend aspirin and either clopidogrel, a glycoprotein IIb/IIIa inhibitor, or both.1 In making this choice, I consider the patient’s risk of bleeding and the dosing complexity of the regimen, especially with the use of glycoprotein IIb/IIIa inhibitors in a patient with renal insufficiency. In a patient at relatively low risk for bleeding, I often use both clopidogrel and a glycoprotein IIb/IIIa inhibitor, although this strategy does not have a lot of data to support it.
The more challenging population consists of patients who go to the cath lab but do not undergo PCI; this population is managed medically too. We often drop the ball with clopidogrel in this population. Many patients in whom PCI is not performed do not receive clopidogrel upstream, for all of the reasons we’ve discussed, and there is pretty good evidence that if clopidogrel is not instituted before hospital discharge, the patient is not likely to be receiving it at 30 days either. We have an obligation to treat these patients.
Treatment following bypass surgery is much murkier, and I don’t really know what we should be doing. The ACC/AHA guidelines suggest that clopidogrel be started in a patient with non-ST-elevation ACS after bypass surgery,1 but I believe the evidence to support that recommendation is pretty weak.
Dr. Bhatt: Well, the CURE trial did contain a sizeable group that underwent bypass surgery,7 and although this group was underpowered in some respects, it was still a very large group, so I personally favor treatment in those patients. We should mention that an ongoing trial called TRILOGY ACS is comparing clopidogrel and prasugrel specifically in patients who are being managed medically,13 so more data on this strategy will be emerging.
ARE GUIDELINES DESTINED TO BECOME EVER MORE COMPLEX?
Dr. Bhatt: Here’s a comment and question from the audience that pulls together a lot of what we’ve discussed while also looking forward: The antiplatelet therapy guidelines are already complicated. If the ongoing studies of emerging antiplatelet drugs all have results that are qualitatively similar to those of the TRITON-TIMI 38 study of prasugrel—ie, better efficacy with more potent therapy but more bleeding—how do you foresee these antiplatelet drugs being used in clinical practice?
Dr. Sabatine: The contrast between the US guidelines and the European guidelines for ACS management is stark. The US guidelines—from the ACC and AHA1—are essentially an encyclopedia that includes nearly every trial of anti-platelet therapy in ACS along with complicated algorithms; they do a wonderful job of being complete. The European guidelines14 are probably one tenth the size of their US counterpart document, and they suggest treatments for various patient types; they are very simple.
In a sense, the US guidelines lay out the data and force practitioners to evaluate the trials and consider how our patients fit into the study populations. In this way they are analogous to current guidelines for anticoagulant therapy. Several anticoagulants have been compared with heparin in clinical trials. These newer anticoagulants appear to reduce the risk of ischemic events compared with heparin; some have lower rates of bleeding, while others have higher rates of bleeding. There have been few head-to-head studies of these agents, however, so we wind up with guidelines that are not definitive but rather suggest agents to “consider” in various settings.
It’s unlikely that a head-to-head trial will be conducted comparing prasugrel with the reversible P2Y12 antagonist AZD6140, assuming that both are approved for marketing. If the drugs appear equally efficacious in placebo-controlled trials, it will take consensus to determine the appropriate choice at your hospital, factoring in your patient profile, the cost of the drugs, and other variables. It’s more complicated when one agent is slightly more efficacious but causes more bleeding or, conversely, a little less efficacious but less apt to cause bleeding. In such cases, you may need to tailor therapy to the patient, trying to gauge bleeding risk. All of the emerging data appear to point to the importance of bleeding on outcomes: patients who bleed fare poorly, in part due to the bleeding itself and in part perhaps because they have a proclivity for bleeding.
THE FUTURE: MONITORING-BASED DOSING AND NICHE ANTIPLATELETS?
Dr. Bhatt: That’s a good observation. Let’s wrap up by having the other panelists share any final thoughts you may have.
Dr. Alexander: I’d like to return to the issue of measuring antiplatelet response and using it to guide therapy. Earlier we cited the examples of antihypertensive therapy and lipid-lowering therapy to support this model of monitoring-based treatment. Guidelines for dyslipidemia treatment recommend using LDL-C levels to guide therapy, but this practice is difficult to study in a randomized trial. In fact, none of the randomized trials of statins used LDL-C levels to guide therapy. They all studied fixed doses of statins versus placebo or fixed doses of another statin. Higher doses of statins were always beneficial compared with lower doses, and this finding was extrapolated into the guidelines as a justification to treat to target LDL-C levels.
Dr. Bhatt: It’s not even necessarily clear that LDL-C level is the best target, if you consider the JUPITER trial, in which patients received statin therapy based on their baseline level of high-sensitivity C-reactive protein, not their LDL-C level.15 It goes to show how incomplete our knowledge of a class of drugs may be, even decades after the drugs are introduced.
Dr. Kottke-Marchant: To speak to Dr. Alexander’s point, dose adjustment guided by platelet monitoring is a bit more problematic for antiplatelet drugs that are irreversible inhibitors, such as clopidogrel and aspirin, than for those that are reversible inhibitors, which are being developed and may eventually make more sense to use. From a drug development standpoint, a drug that requires monitoring and dose adjustment will not gain wide acceptance because it will increase medical costs and morbidity.
Dr. Bhatt: Yes, we know from experience with warfarin that doctors and patients don’t like the ongoing need for monitoring and testing.
Dr. Peacock: The drugs that are going to be adopted by the emergency department are those with the shortest half-lives, for several reasons: (1) using a drug with a short half-life won’t commit us to a particular course of action; (2) the potential for drug interactions is lower; and (3) in the event of an erroneous diagnosis, the consequence of misapplication may be mitigated by early recognition and termination of the drug. If we later decide that we’ve gone down the wrong therapeutic road or reached a wrong diagnosis, or if a complication occurs, we can turn off the therapy quickly. That level of flexibility is needed.
Dr. Kottke-Marchant: I think we are moving into an era of niche antiplatelet drugs. One might be used in a patient going to surgery, for example, and another for long-term therapy.
Dr. Peacock: One thing that I don’t have a feel for is how to transition from one drug to another. When you change drugs for a patient, it so often seems like it goes badly. If we’re eventually going to use drugs with ultra-short half-lives in the in the emergency department for the first day or two, and then switch patients to a pill for a week, a lot more platelet function testing may be needed.
- Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/ non-ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2007; 50:e1–e157.
- Bonello L, Camoin-Jau L, Arques S, et al. Adjusted clopidogrel loading doses according to vasodilator-stimulated phosphoprotein phosphorylation index decrease rate of major adverse cardiovascular events in patients with clopidogrel resistance: a multicenter randomized prospective study. J Am Coll Cardiol 2008; 51:1404–1411.
- Glauser J, Emerman CL, Bhatt DL, Peacock WF. Platelet aspirin resistance in emergency department patients with suspected acute coronary syndrome. Am J Emerg Med. In press
- Patti G, Nusca A, Mangiacapra F, Gatto L, D’Ambrosio A, Di Sciascio G. Point-of-care measurement of clopidogrel responsiveness predicts clinical outcome in patients undergoing percutaneous coronary intervention. J Am Coll Cardiol 2008; 52:1128–1133.
- Mega JL, Close SL, Wiviott SD, et al. Cytochrome P-450 polymorphisms and response to clopidogrel. N Engl J Med 2009; 360:354–362.
- Bhatt DL, Scheiman J, Abraham NS, et al. ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use. J Am Coll Cardiol 2008; 52:1502–1517.
- Fox KA, Mehta SR, Peters R, et al. Benefits and risks of the combination of clopidogrel and aspirin in patients undergoing surgical revascularization for non-ST-elevation acute coronary syndrome: the Clopidogrel in Unstable angina to prevent Recurrent ischemic Events (CURE) Trial. Circulation 2004; 110:1202–1208.
- ISIS-2 Collaborative Group. Randomised trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. Lancet 1988; 2:349–360.
- EARLY-ACS: Glycoprotein IIb/IIIa inhibition in patients with non-ST-segment elevation acute coronary syndrome. Clinical Trials.gov Web site. http://clinicaltrials.gov/ct2/show/NCT00089895. Updated December 17, 2008. Accessed December 18, 2008.
- Wiviott SD, Braunwald E, McCabe CH, et al; TRITON-TIMI 38 Investigators. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 2007; 357:2001–2015.
- Wiviott SD, Braunwald E, McCabe CH, et al. Intensive oral anti-platelet therapy for reduction of ischaemic events including stent thrombosis in patients with acute coronary dyndromes treated with percutaneous coronary intervention and stenting in the TRITON-TIMI 38 trial: a subanalysis of a randomised trial. Lancet 2008; 371:1353–1363.
- Berger JS, Bhatt DL, Chen Z, et al. The relationship between sex, mortality and cardiovascular events among patients with established cardiovascular disease: a meta-analysis [ACC abstract 1012-149]. J Am Coll Cardiol 2008; 51 10 suppl A:A247.
- TRILOGY ACS: A comparison of prasugrel and clopidogrel in acute coronary syndrome subjects. ClinicalTrials.gov Web site. http://clinicaltrials.gov/ct2/show/NCT00699998. Updated December 15, 2008. Accessed January 2, 2009.
- Guidelines for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes. Eur Heart J 2007; 28:1598–1660.
- Ridker PM, Danielson E, Fonseca FA, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med 2008; 359:2195–2207.
- Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/ non-ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2007; 50:e1–e157.
- Bonello L, Camoin-Jau L, Arques S, et al. Adjusted clopidogrel loading doses according to vasodilator-stimulated phosphoprotein phosphorylation index decrease rate of major adverse cardiovascular events in patients with clopidogrel resistance: a multicenter randomized prospective study. J Am Coll Cardiol 2008; 51:1404–1411.
- Glauser J, Emerman CL, Bhatt DL, Peacock WF. Platelet aspirin resistance in emergency department patients with suspected acute coronary syndrome. Am J Emerg Med. In press
- Patti G, Nusca A, Mangiacapra F, Gatto L, D’Ambrosio A, Di Sciascio G. Point-of-care measurement of clopidogrel responsiveness predicts clinical outcome in patients undergoing percutaneous coronary intervention. J Am Coll Cardiol 2008; 52:1128–1133.
- Mega JL, Close SL, Wiviott SD, et al. Cytochrome P-450 polymorphisms and response to clopidogrel. N Engl J Med 2009; 360:354–362.
- Bhatt DL, Scheiman J, Abraham NS, et al. ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use. J Am Coll Cardiol 2008; 52:1502–1517.
- Fox KA, Mehta SR, Peters R, et al. Benefits and risks of the combination of clopidogrel and aspirin in patients undergoing surgical revascularization for non-ST-elevation acute coronary syndrome: the Clopidogrel in Unstable angina to prevent Recurrent ischemic Events (CURE) Trial. Circulation 2004; 110:1202–1208.
- ISIS-2 Collaborative Group. Randomised trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. Lancet 1988; 2:349–360.
- EARLY-ACS: Glycoprotein IIb/IIIa inhibition in patients with non-ST-segment elevation acute coronary syndrome. Clinical Trials.gov Web site. http://clinicaltrials.gov/ct2/show/NCT00089895. Updated December 17, 2008. Accessed December 18, 2008.
- Wiviott SD, Braunwald E, McCabe CH, et al; TRITON-TIMI 38 Investigators. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 2007; 357:2001–2015.
- Wiviott SD, Braunwald E, McCabe CH, et al. Intensive oral anti-platelet therapy for reduction of ischaemic events including stent thrombosis in patients with acute coronary dyndromes treated with percutaneous coronary intervention and stenting in the TRITON-TIMI 38 trial: a subanalysis of a randomised trial. Lancet 2008; 371:1353–1363.
- Berger JS, Bhatt DL, Chen Z, et al. The relationship between sex, mortality and cardiovascular events among patients with established cardiovascular disease: a meta-analysis [ACC abstract 1012-149]. J Am Coll Cardiol 2008; 51 10 suppl A:A247.
- TRILOGY ACS: A comparison of prasugrel and clopidogrel in acute coronary syndrome subjects. ClinicalTrials.gov Web site. http://clinicaltrials.gov/ct2/show/NCT00699998. Updated December 15, 2008. Accessed January 2, 2009.
- Guidelines for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes. Eur Heart J 2007; 28:1598–1660.
- Ridker PM, Danielson E, Fonseca FA, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med 2008; 359:2195–2207.