ANSWER
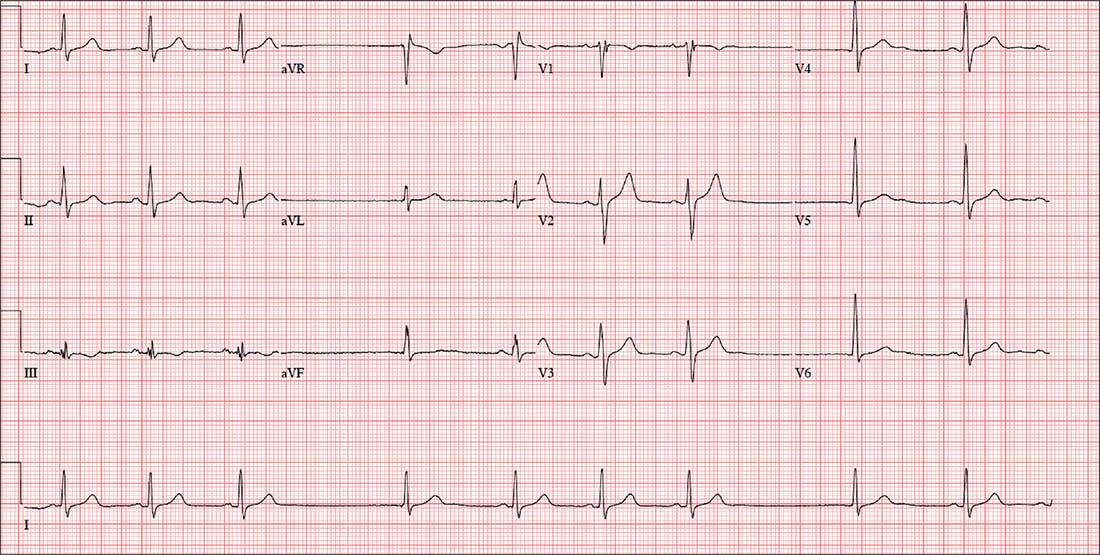
The correct interpretation includes sinus bradycardia, marked sinus arrhythmia, junctional escape beats with sinus arrest or a transient atrioventricular (AV) block, and an intraventricular conduction defect.
Sinus bradycardia is diagnosed based on narrow QRS intervals < 60 beats/min. Marked sinus arrhythmia is indicated by the narrow QRS intervals of similar size but with an irregular rhythm.
When the rate is slow and irregular, rather than use the 300/150/100 method, it is more accurate to count the number of QRS complexes in the rhythm strip and multiply by six (an ECG at standard paper speed takes 10 s; 6 × 10 s = 60 s). If the patient does not have a pacemaker, a range within two to three beats of the computer measurement is acceptable. In this case, 9 × 6 = 54 beats/min—very close to the interval measured by the computer.
The first three beats on the rhythm strip are sinus with a normal PQRST complex. After that, there is a pause (either sinus arrest or a transient AV block—we can’t tell which) that is interrupted by a junctional escape beat (no P wave, but the QRS is similar to the prior, normal complexes). The fifth, sixth, and seventh beats are normal sinus, followed by another pause with an ensuing junctional escape. The last QRS complex is another sinus beat.
Finally, although the QRS duration (122 ms) is greater than normal, the complexes in leads V1 and V6 do not constitute a right or left bundle branch block.