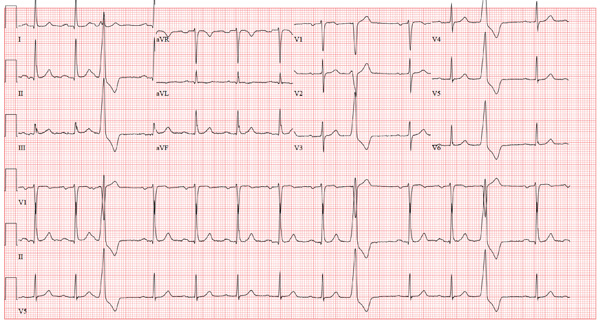
An 80-year-old man presents to your office after having two separate episodes of chest pain. The first occurred two weeks ago, while the patient was arguing with his home health nurse. He describes the pain as a “burning” sensation deep in his chest—similar to that from his long-standing history of esophageal reflux, with the exception that the onset and resolution were much quicker. A second, similar episode occurred two days ago, again during an argument with his nurse. He did not disclose either episode to the nurse. However, he was sufficiently concerned about the possibility of a cardiac cause that he decided to see you. When questioning him about his chest pain, you learn that there was no associated diaphoresis, shortness of breath, or pain radiation to the neck or arm. He denies symptoms of bradycardia, tachycardia, or palpitations. When you question him about the argument with his nurse, you learn that he has been eating chips and salsa, which you have previously advised against, given his history of esophageal reflux, Barrett’s esophagus, and endoscopic confirmation of esophageal dysplasia. The medical history is also significant for bilateral below-knee amputations from trauma sustained during army service in the Korean War. He has had multiple bilateral stump revisions, such that he can no longer wear prostheses and is wheelchair bound. Adenomatous colonic polyps, iron-deficiency anemia, hypothyroidism, asthma, benign prostatic hypertrophy, glaucoma, and Parkinson’s disease complete the medical history. The family history is remarkable for a father who died of a hemorrhagic stroke and a mother who died of renal failure. The patient, a widower, resides at home with a live-in nurse and a housekeeper. His medication list includes aspirin, lisinopril, levothyroxine, carbidopa/levodopa, and travoprost and timolol eye drops. He is allergic to sulfa. The review of symptoms is remarkable for urinary retention and recent resolution of diarrhea. Pertinent physical findings in this pleasant elderly man include audible wheezing and a raspy voice. The lungs are diffusely wheezy on expiration, and there is no conversational dyspnea or accessory muscle use. The neck veins are flat, and while heart sounds are distant, there are no murmurs, rubs, or extra heart sounds. The abdomen is soft and nontender. A low-amplitude tremor is present in both hands, and there is no cogwheeling. Serum B-type natriuretic peptide is 190 pg/mL and serum troponin levels are negative. An ECG reveals the following: a ventricular rate of 79 beats/min; PR interval, 212 ms; QRS duration, 92 ms; QT/QTc interval, 358/410 ms; P axis, 35°; R axis, 47°; and T axis, 69°. What is your interpretation of this ECG?