RISK FACTORS
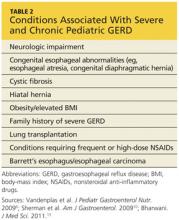
Certain pediatric groups are at increased risk for severe GERD, with or without complications. Neurologic impairment can cause dysphagia, and anatomic abnormalities such as hiatal hernia can impair lower esophageal sphincter function, allowing acid to rise into the esophagus.6,11 Table 26,10,13 lists illnesses and congenital conditions that are considered predisposing factors for severe, chronic GERD.
When seeing patients in these populations, clinicians should specifically focus on relevant GI symptoms during the history and physical exam. Clinicians should also consider long-term monitoring for complications or changes that might indicate new-onset GERD.
Overweight and Obesity
Although data are limited on the relationship between pediatric GERD and obesity,14 associated research findings seem to conflict with the established relationship in adult patients. While certain study groups found an association between obesity, elevated BMI, and increased waist circumference with an increase in symptoms of GERD (eg, regurgitation, heartburn),15,16 others found no significant correlation between overweight and reflux esophagitis.14,17 Notably, one analysis found a significant correlation between male gender and incidence of GERD.17
Although the evidence is not conclusive, clinicians are encouraged to counsel the older children among their patients on the benefits of weight and BMI reduction—encouraging them to achieve an overall healthier lifestyle and avoid diseases associated with excess weight.
DIFFERENTIAL DIAGNOSIS
In infants with unusual symptoms, certain GI conditions such as obstructive disorders (eg, pyloric stenosis), motility disorders, and peptic ulcer disease must be ruled out with further diagnostic testing.6,7 Red-flag symptoms that warrant further investigation include hematemesis, hematochezia, diarrhea, abdominal tenderness or distention, constipation, bilious vomiting, onset of vomiting after age 6 months, failure to thrive, macrocephaly or microcephaly, fever, lethargy, and hepatosplenomegaly.6,7 More common differentials are described below.
Eosinophilic Esophagitis
Eosinophilic esophagitis is an inflammatory condition of the esophagus, an apparent manifestation of food allergy (eg, milk protein), characterized by infiltrating mucosal eosinophils.6,18 First identified in children (though also occurring in adults), eosinophilic esophagitis is recognized as a more common cause of dysphagia than GERD.6
This recently discovered disease is often mistaken for GERD. While symptoms including heartburn and dysphagia occur in both conditions, eosinophilic esophagitis can only be diagnosed via multiple endoscopic mucosal biopsies. Corticosteroid therapy has been found to be a more effective treatment for this condition than acid suppression therapy.19
Current research is focused on a possible link between eosinophilic esophagitis and autoimmune disease, as many affected patients also have asthma, allergic rhinitis, and/or eczema.19 The increasing prevalence of childhood allergies should prompt clinicians to place eosinophilic esophagitis on the short list of differentials when evaluating a child for GERD-type symptoms. Referral for evaluation by an allergist may also be beneficial.
Asthma
GER may actually trigger asthma in some patients, even without symptoms of GERD.6 While there is support for a possible link between GERD and asthma in infants and children, a definitive relationship cannot be confirmed without more reliable studies.20 However, clinicians must not overlook the possibility of GERD in a child who presents with symptoms indicative of asthma, such as wheezing, shortness of breath, coughing, and chest tightness.
Other Extra-Esophageal Diseases
Concern exists over apparent associations between GERD and other extra-esophageal illnesses. In addition to asthma, the Montreal consensus group10,12 found a connection between GERD and other respiratory conditions, including chronic cough and chronic laryngitis. These conditions usually represent multifactorial disease processes, researchers state, and GER can be an exacerbating factor rather than an actual cause of these conditions.5,10
Further manifestations of extra-esophageal GERD include pneumonia, bronchiectasis, any apparent life-threatening event, laryngotracheitis, sinusitis, and dental erosion. Again, causality has not been clearly established, and the shortage of high-quality studies with adequate sample sizes makes it impossible to confirm clear relationships.21 It is therefore prudent for clinicians to evaluate any child with these non-GI conditions for reflux disease.
Continued on next page >>