User login
HCV Hub
AbbVie
acid
addicted
addiction
adolescent
adult sites
Advocacy
advocacy
agitated states
AJO, postsurgical analgesic, knee, replacement, surgery
alcohol
amphetamine
androgen
antibody
apple cider vinegar
assistance
Assistance
association
at home
attorney
audit
ayurvedic
baby
ban
baricitinib
bed bugs
best
bible
bisexual
black
bleach
blog
bulimia nervosa
buy
cannabis
certificate
certification
certified
cervical cancer, concurrent chemoradiotherapy, intravoxel incoherent motion magnetic resonance imaging, MRI, IVIM, diffusion-weighted MRI, DWI
charlie sheen
cheap
cheapest
child
childhood
childlike
children
chronic fatigue syndrome
Cladribine Tablets
cocaine
cock
combination therapies, synergistic antitumor efficacy, pertuzumab, trastuzumab, ipilimumab, nivolumab, palbociclib, letrozole, lapatinib, docetaxel, trametinib, dabrafenib, carflzomib, lenalidomide
contagious
Cortical Lesions
cream
creams
crime
criminal
cure
dangerous
dangers
dasabuvir
Dasabuvir
dead
deadly
death
dementia
dependence
dependent
depression
dermatillomania
die
diet
direct-acting antivirals
Disability
Discount
discount
dog
drink
drug abuse
drug-induced
dying
eastern medicine
eat
ect
eczema
electroconvulsive therapy
electromagnetic therapy
electrotherapy
epa
epilepsy
erectile dysfunction
explosive disorder
fake
Fake-ovir
fatal
fatalities
fatality
fibromyalgia
financial
Financial
fish oil
food
foods
foundation
free
Gabriel Pardo
gaston
general hospital
genetic
geriatric
Giancarlo Comi
gilead
Gilead
glaucoma
Glenn S. Williams
Glenn Williams
Gloria Dalla Costa
gonorrhea
Greedy
greedy
guns
hallucinations
harvoni
Harvoni
herbal
herbs
heroin
herpes
Hidradenitis Suppurativa,
holistic
home
home remedies
home remedy
homeopathic
homeopathy
hydrocortisone
ice
image
images
job
kid
kids
kill
killer
laser
lawsuit
lawyer
ledipasvir
Ledipasvir
lesbian
lesions
lights
liver
lupus
marijuana
melancholic
memory loss
menopausal
mental retardation
military
milk
moisturizers
monoamine oxidase inhibitor drugs
MRI
MS
murder
national
natural
natural cure
natural cures
natural medications
natural medicine
natural medicines
natural remedies
natural remedy
natural treatment
natural treatments
naturally
Needy
needy
Neurology Reviews
neuropathic
nightclub massacre
nightclub shooting
nude
nudity
nutraceuticals
OASIS
oasis
off label
ombitasvir
Ombitasvir
ombitasvir/paritaprevir/ritonavir with dasabuvir
orlando shooting
overactive thyroid gland
overdose
overdosed
Paolo Preziosa
paritaprevir
Paritaprevir
pediatric
pedophile
photo
photos
picture
post partum
postnatal
pregnancy
pregnant
prenatal
prepartum
prison
program
Program
Protest
protest
psychedelics
pulse nightclub
puppy
purchase
purchasing
rape
recall
recreational drug
Rehabilitation
Retinal Measurements
retrograde ejaculation
risperdal
ritonavir
Ritonavir
ritonavir with dasabuvir
robin williams
sales
sasquatch
schizophrenia
seizure
seizures
sex
sexual
sexy
shock treatment
silver
sleep disorders
smoking
sociopath
sofosbuvir
Sofosbuvir
sovaldi
ssri
store
sue
suicidal
suicide
supplements
support
Support
Support Path
teen
teenage
teenagers
Telerehabilitation
testosterone
Th17
Th17:FoxP3+Treg cell ratio
Th22
toxic
toxin
tragedy
treatment resistant
V Pak
vagina
velpatasvir
Viekira Pa
Viekira Pak
viekira pak
violence
virgin
vitamin
VPak
weight loss
withdrawal
wrinkles
xxx
young adult
young adults
zoloft
financial
sofosbuvir
ritonavir with dasabuvir
discount
support path
program
ritonavir
greedy
ledipasvir
assistance
viekira pak
vpak
advocacy
needy
protest
abbvie
paritaprevir
ombitasvir
direct-acting antivirals
dasabuvir
gilead
fake-ovir
support
v pak
oasis
harvoni
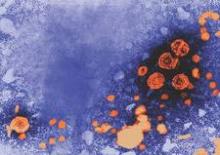
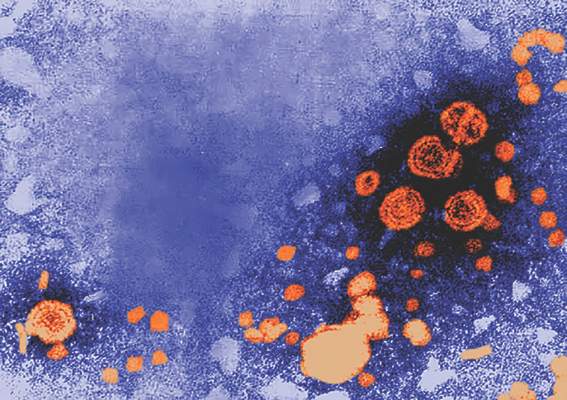
FDA report provides overview of HCV drug approvals
In a report published in Hepatology, scientists from the FDA’s Division of Antiviral Products in the Center for Drug Evaluation and Research (CDER) have provided a brief overview of the FDA’s scientific approaches and regulatory processes designed to accelerate the approval of drugs to treat hepatitis C virus (HCV).
The decision to publish the paper was made because of concerns regarding the efficacy of new, interferon- and ribavirin-free regimens that have gained traction in the drug marketplace. Publishing the paper should clear up some concerns that the drugs are not being properly evaluated, the authors write.
“This paper intends to provide increased transparency to various stakeholders about FDA’s scientific approaches and regulatory processes that supported drug development and marketing approval of [direct-acting antiviral agents] for the treatment of hepatitis C,” writes lead author Dr. Poonam Mishra, a deputy director in CDER.
Read the full article in Hepatology (doi:10.1002/hep.27880).
In a report published in Hepatology, scientists from the FDA’s Division of Antiviral Products in the Center for Drug Evaluation and Research (CDER) have provided a brief overview of the FDA’s scientific approaches and regulatory processes designed to accelerate the approval of drugs to treat hepatitis C virus (HCV).
The decision to publish the paper was made because of concerns regarding the efficacy of new, interferon- and ribavirin-free regimens that have gained traction in the drug marketplace. Publishing the paper should clear up some concerns that the drugs are not being properly evaluated, the authors write.
“This paper intends to provide increased transparency to various stakeholders about FDA’s scientific approaches and regulatory processes that supported drug development and marketing approval of [direct-acting antiviral agents] for the treatment of hepatitis C,” writes lead author Dr. Poonam Mishra, a deputy director in CDER.
Read the full article in Hepatology (doi:10.1002/hep.27880).
In a report published in Hepatology, scientists from the FDA’s Division of Antiviral Products in the Center for Drug Evaluation and Research (CDER) have provided a brief overview of the FDA’s scientific approaches and regulatory processes designed to accelerate the approval of drugs to treat hepatitis C virus (HCV).
The decision to publish the paper was made because of concerns regarding the efficacy of new, interferon- and ribavirin-free regimens that have gained traction in the drug marketplace. Publishing the paper should clear up some concerns that the drugs are not being properly evaluated, the authors write.
“This paper intends to provide increased transparency to various stakeholders about FDA’s scientific approaches and regulatory processes that supported drug development and marketing approval of [direct-acting antiviral agents] for the treatment of hepatitis C,” writes lead author Dr. Poonam Mishra, a deputy director in CDER.
Read the full article in Hepatology (doi:10.1002/hep.27880).
FROM HEPATOLOGY
VIDEO: Is it IBS? Blood test may offer conclusive answer
WASHINGTON – A new blood test could conclusively determine if a patient with chronic diarrhea has diarrhea-predominant irritable bowel syndrome (D-IBS).
The IBSchek blood test detects the presence of antibodies to cytolethal distending toxin B and vinculin. In a study presented at the annual Digestive Disease Week and published in PLoS ONE, the positive predictive value for D-IBS of just one of the antibodies was greater than 98%, explained study lead author Dr. Mark Pimentel of Cedars-Sinai Medical Center, Los Angeles. If the test is positive for both antibodies, “the post-test probability is 95% that you have IBS.”
In a video interview, Dr. Pimentel discussed the study’s findings and the potential impact for physicians and patients. The search for diagnostic answers leads to “a lot of doctor-shopping, certainly a lot of colonoscopies and unnecessary testing that are always negative with these patients,” he noted. “Maybe this will put an end to that.
“People used to think this is all psychological,” Dr. Pimentel added. “Now we can say, No, it’s organic. There’s something real going on; I’ve got a test that proves that.”
Dr. Pimentel has received consulting fees from Commonwealth Laboratories, which makes the IBSchek blood test.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WASHINGTON – A new blood test could conclusively determine if a patient with chronic diarrhea has diarrhea-predominant irritable bowel syndrome (D-IBS).
The IBSchek blood test detects the presence of antibodies to cytolethal distending toxin B and vinculin. In a study presented at the annual Digestive Disease Week and published in PLoS ONE, the positive predictive value for D-IBS of just one of the antibodies was greater than 98%, explained study lead author Dr. Mark Pimentel of Cedars-Sinai Medical Center, Los Angeles. If the test is positive for both antibodies, “the post-test probability is 95% that you have IBS.”
In a video interview, Dr. Pimentel discussed the study’s findings and the potential impact for physicians and patients. The search for diagnostic answers leads to “a lot of doctor-shopping, certainly a lot of colonoscopies and unnecessary testing that are always negative with these patients,” he noted. “Maybe this will put an end to that.
“People used to think this is all psychological,” Dr. Pimentel added. “Now we can say, No, it’s organic. There’s something real going on; I’ve got a test that proves that.”
Dr. Pimentel has received consulting fees from Commonwealth Laboratories, which makes the IBSchek blood test.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WASHINGTON – A new blood test could conclusively determine if a patient with chronic diarrhea has diarrhea-predominant irritable bowel syndrome (D-IBS).
The IBSchek blood test detects the presence of antibodies to cytolethal distending toxin B and vinculin. In a study presented at the annual Digestive Disease Week and published in PLoS ONE, the positive predictive value for D-IBS of just one of the antibodies was greater than 98%, explained study lead author Dr. Mark Pimentel of Cedars-Sinai Medical Center, Los Angeles. If the test is positive for both antibodies, “the post-test probability is 95% that you have IBS.”
In a video interview, Dr. Pimentel discussed the study’s findings and the potential impact for physicians and patients. The search for diagnostic answers leads to “a lot of doctor-shopping, certainly a lot of colonoscopies and unnecessary testing that are always negative with these patients,” he noted. “Maybe this will put an end to that.
“People used to think this is all psychological,” Dr. Pimentel added. “Now we can say, No, it’s organic. There’s something real going on; I’ve got a test that proves that.”
Dr. Pimentel has received consulting fees from Commonwealth Laboratories, which makes the IBSchek blood test.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT DDW 2015
DDW: Ozanimod active in moderate-severe UC, without cardiac signal in TOUCHSTONE trial
WASHINGTON– The oral S1P receptor modulator ozanimod is clinically active and well tolerated in patients with moderate to severe ulcerative colitis (UC), phase II study results show.
Importantly, no notable cardiac, opthalmologic, or infectious treatment-related adverse events were observed, Dr. William Sandborn said at the annual Digestive Disease Week.
The first sphingosine-1-phosphate (S1P) receptor modulator, Fingolimod (Gilenya), carries a warning for first-dose cardiac effects, liver function test elevations, and macular edema and targets S1P receptors 1, 3, 4, and 5. Ozanimod is a next-generation S1P receptor modulator that has increased selectivity for the S1P receptors 1 and 5, compared with receptor 3, which may be related to safety concerns with fingolimod, said Dr. Sandborn, chief of gastroenterology at the University of California-San Diego.
He reported on the double-blind, phase II TOUCHSTONE trial involving 197 adults with moderate to severe UC who were receiving oral aminosalicylates and/or prednisone, and were randomly assigned to receive ozanimod 0.5 mg (n = 65) or 1 mg (n = 67) or placebo (n = 65). Doses were titrated through week 1, followed by 8 weeks of full-dose therapy.
The study’s primary efficacy endpoint was the proportion of patients in clinical remission at week 8, defined as a Mayo score of 2 or less, with no subscore of more than 1.
At week 8, 16.4% of patients on ozanimod 1 mg were in remission vs. 6.2% on placebo (P = .0482) and 13.8% on ozanimod 0.5 mg (P = .1422), Dr. Sandborn reported.
Rates of clinical response at 8 weeks were 56.7% with the high-dose ozanimod, 53.8% with the low dose, and 37% with placebo. Once again, the between-group difference was significant only for high-dose ozanimod (P = .0207).
Mucosal improvement was significantly more common with either high-dose ozanimod (34.3% vs. 12.3% placebo; P = .0023) or low-dose ozanimod (27.7% vs. 12.3% placebo; P = .0348), he said.
The most common adverse events were anemia/decreased hemoglobin, occurring in four patients in the placebo and low-dose ozanimod groups, and worsening of UC, occurring in three patients on placebo, two on low-dose ozanimod, and one on high-dose ozanimod.
Serious treatment-related adverse events were reported in four patients on placebo, one on ozanimod 0.5 mg (hyperpyrexia), and one on ozanimod 1 mg (UC).
The overall incidence of cardiac events was low, with two palpitations reported in the placebo group, one sinus bradycardia and one first-degree AV block in the ozanimod 0.5-mg group, and none in the 1-mg group.
“Ozanimod was well tolerated with a favorable benefit-risk profile supporting the planned phase III trial in ulcerative colitis and the phase II study in Crohn’s disease,” said Dr. Sandborn, who also reported the results earlier this year in Europe.
On Twitter@pwendl
WASHINGTON– The oral S1P receptor modulator ozanimod is clinically active and well tolerated in patients with moderate to severe ulcerative colitis (UC), phase II study results show.
Importantly, no notable cardiac, opthalmologic, or infectious treatment-related adverse events were observed, Dr. William Sandborn said at the annual Digestive Disease Week.
The first sphingosine-1-phosphate (S1P) receptor modulator, Fingolimod (Gilenya), carries a warning for first-dose cardiac effects, liver function test elevations, and macular edema and targets S1P receptors 1, 3, 4, and 5. Ozanimod is a next-generation S1P receptor modulator that has increased selectivity for the S1P receptors 1 and 5, compared with receptor 3, which may be related to safety concerns with fingolimod, said Dr. Sandborn, chief of gastroenterology at the University of California-San Diego.
He reported on the double-blind, phase II TOUCHSTONE trial involving 197 adults with moderate to severe UC who were receiving oral aminosalicylates and/or prednisone, and were randomly assigned to receive ozanimod 0.5 mg (n = 65) or 1 mg (n = 67) or placebo (n = 65). Doses were titrated through week 1, followed by 8 weeks of full-dose therapy.
The study’s primary efficacy endpoint was the proportion of patients in clinical remission at week 8, defined as a Mayo score of 2 or less, with no subscore of more than 1.
At week 8, 16.4% of patients on ozanimod 1 mg were in remission vs. 6.2% on placebo (P = .0482) and 13.8% on ozanimod 0.5 mg (P = .1422), Dr. Sandborn reported.
Rates of clinical response at 8 weeks were 56.7% with the high-dose ozanimod, 53.8% with the low dose, and 37% with placebo. Once again, the between-group difference was significant only for high-dose ozanimod (P = .0207).
Mucosal improvement was significantly more common with either high-dose ozanimod (34.3% vs. 12.3% placebo; P = .0023) or low-dose ozanimod (27.7% vs. 12.3% placebo; P = .0348), he said.
The most common adverse events were anemia/decreased hemoglobin, occurring in four patients in the placebo and low-dose ozanimod groups, and worsening of UC, occurring in three patients on placebo, two on low-dose ozanimod, and one on high-dose ozanimod.
Serious treatment-related adverse events were reported in four patients on placebo, one on ozanimod 0.5 mg (hyperpyrexia), and one on ozanimod 1 mg (UC).
The overall incidence of cardiac events was low, with two palpitations reported in the placebo group, one sinus bradycardia and one first-degree AV block in the ozanimod 0.5-mg group, and none in the 1-mg group.
“Ozanimod was well tolerated with a favorable benefit-risk profile supporting the planned phase III trial in ulcerative colitis and the phase II study in Crohn’s disease,” said Dr. Sandborn, who also reported the results earlier this year in Europe.
On Twitter@pwendl
WASHINGTON– The oral S1P receptor modulator ozanimod is clinically active and well tolerated in patients with moderate to severe ulcerative colitis (UC), phase II study results show.
Importantly, no notable cardiac, opthalmologic, or infectious treatment-related adverse events were observed, Dr. William Sandborn said at the annual Digestive Disease Week.
The first sphingosine-1-phosphate (S1P) receptor modulator, Fingolimod (Gilenya), carries a warning for first-dose cardiac effects, liver function test elevations, and macular edema and targets S1P receptors 1, 3, 4, and 5. Ozanimod is a next-generation S1P receptor modulator that has increased selectivity for the S1P receptors 1 and 5, compared with receptor 3, which may be related to safety concerns with fingolimod, said Dr. Sandborn, chief of gastroenterology at the University of California-San Diego.
He reported on the double-blind, phase II TOUCHSTONE trial involving 197 adults with moderate to severe UC who were receiving oral aminosalicylates and/or prednisone, and were randomly assigned to receive ozanimod 0.5 mg (n = 65) or 1 mg (n = 67) or placebo (n = 65). Doses were titrated through week 1, followed by 8 weeks of full-dose therapy.
The study’s primary efficacy endpoint was the proportion of patients in clinical remission at week 8, defined as a Mayo score of 2 or less, with no subscore of more than 1.
At week 8, 16.4% of patients on ozanimod 1 mg were in remission vs. 6.2% on placebo (P = .0482) and 13.8% on ozanimod 0.5 mg (P = .1422), Dr. Sandborn reported.
Rates of clinical response at 8 weeks were 56.7% with the high-dose ozanimod, 53.8% with the low dose, and 37% with placebo. Once again, the between-group difference was significant only for high-dose ozanimod (P = .0207).
Mucosal improvement was significantly more common with either high-dose ozanimod (34.3% vs. 12.3% placebo; P = .0023) or low-dose ozanimod (27.7% vs. 12.3% placebo; P = .0348), he said.
The most common adverse events were anemia/decreased hemoglobin, occurring in four patients in the placebo and low-dose ozanimod groups, and worsening of UC, occurring in three patients on placebo, two on low-dose ozanimod, and one on high-dose ozanimod.
Serious treatment-related adverse events were reported in four patients on placebo, one on ozanimod 0.5 mg (hyperpyrexia), and one on ozanimod 1 mg (UC).
The overall incidence of cardiac events was low, with two palpitations reported in the placebo group, one sinus bradycardia and one first-degree AV block in the ozanimod 0.5-mg group, and none in the 1-mg group.
“Ozanimod was well tolerated with a favorable benefit-risk profile supporting the planned phase III trial in ulcerative colitis and the phase II study in Crohn’s disease,” said Dr. Sandborn, who also reported the results earlier this year in Europe.
On Twitter@pwendl
AT DDW 2015
Key clinical point: Ozanimod 1 mg induced clinical remission at week 8 in patients with moderate to severe ulcerative colitis.
Major finding: At week 8, 16.4% of patients on ozanimod 1 mg were in remission vs. 6.2% on placebo (P = .0482) and 13.8% on ozanimod 0.5 mg (P = .1422).
Data source: Randomized, double-blind trial of 197 patients with moderate to severe ulcerative colitis.
Disclosures: Dr. Sandborn reported financial relationships with numerous firms including Receptos, which funded the study.
DDW: Gestational diabetes linked to increased NAFLD risk in middle age
WASHINGTON – Gestational diabetes was identified as a significant, independent risk factor for developing non-alcoholic fatty liver disease later in life, according to a study of more than 1,000 women followed for 25 years.
This study “is the first to show a strong association between gestational diabetes in young adulthood and non-alcoholic fatty liver disease in middle-age,” Dr. Veeral Ajmera of the department of gastroenterology at the University of California, San Francisco, reported at the annual Digestive Disease Week.
The study evaluated 1,115 women from the Coronary Artery Risk Development in Young Adults (CARDIA) study, who had at least one delivery, did not have a diabetes diagnosis before pregnancy, and had a CT evaluation for hepatic steatosis at the 25-year visit, in 2010 and 2011. Women were excluded if they did not have a complete CT scan at that time, they had more than 14 drinks of alcohol per week, used medications associated with steatosis, or had chronic viral hepatitis or HIV infections.
At baseline the median age was 25-26 years, about 55%-56% were black, and the prevalence of hypertension (2%-3%) and dyslipidemia were similar. The CARDIA study enrolled about 5,100 men and women aged 18-30 years at four U.S. medical centers in the mid 1980s. Patients had 7 study visits over a 25-year follow-up period.
Of the 1,115 women evaluated, 124 (11%) went on to develop GDM and 75 (7%) met the CT definition for NAFLD (liver attenuation less than or equal to 40 Hounsfield units on CT scan) by the 25-year follow-up, when they were a median age of 50-51 years.
At 25 years, 14% of those with a history of GDM had NAFLD, compared with 5.8% of those who did not have GDM, for an unadjusted odds ratio of 2.56 (p <0.01), Dr. Ajmera said.
In the statistical analysis, the researchers determined that baseline homeostatic model assessment of insulin resistance (HOMA-IR) and baseline triglycerides were also ”strongly associated” with NAFLD at year 25.
“Importantly,” he noted, the measure of the association between GDM and NAFLD remained statistically significant, after adjusting for these covariates (OR, 2.29). At the start of the study, women who went on to develop GDM had significantly higher body mass index (BMI), HOMA-IR, waist circumference, and triglycerides than those who did not develop GDM, but the magnitude of those differences was small.
Additionally, after adjustment for a diagnosis of diabetes at year 25, the association between a history of GDM and NAFLD was stronger (OR, 1.99) than the association between a diagnosis of diabetes at year 25 and NAFLD (OR, 1.5), he said.
The researchers added BMI to their multivariate analysis to determine whether women with a gestational diabetes history gained more weight, and whether that weight explained the increased prevalence of NAFLD, “and found that the association between gestational diabetes and non-alcoholic fatty liver disease remained,” Dr. Ajmera added.
Evaluations of race, baseline BMI, and baseline HOMA-IR as effect modifiers of the relationship between GDM and NAFLD were not significant.
“Gestational diabetes represents insulin resistance unmasked by the stress of pregnancy, and offers the unique opportunity to identify those at risk of NAFLD at a young age,” Dr. Ajmera concluded.
Limitations of the study included not being able to determine if the women had NAFLD before they were diagnosed with GDM. However, based on the participants’ young age at enrollment, that is unlikely, he said. In addition, the researchers had no information on liver biochemistry tests, which, however, are not sensitive or specific for diagnosing NAFLD. The strengths of the study include the length of follow-up of a large biracial population, with measurement of well-characterized metabolic covariates measured, he added.
Dr. Ajmera reported having no relevant financial disclosures. The CARDIA study is supported by the National Heart, Lung, and Blood Institute, part of the National Institutes of Health.
Nonalcoholic fatty liver disease is the most common and fastest growing liver disease worldwide. Identifying individuals at high risk for NAFLD remains challenging. Dr. Ajmera and his colleagues highlight the association between gestational diabetes mellitus (GDM) and NAFLD. Their work confirms and extends earlier studies that reported increased hepatic fat content and a substantially increased risk for NAFLD, in women with a prior history of GDM. In the present study, a more racially diverse U.S.-based population was followed for a much longer duration than was previous cohorts. After adjusted multivariate analysis, GDM remained a strong, independent predictor of future NAFLD. Indeed, GDM was a a better NAFLD predictor than the diagnosis of diabetes alone was. It is unclear if prepregnancy NAFLD might have affected the risk for GDM, as subjects were not assessed for hepatic steatosis or liver test elevations at baseline. Also, the percentage of 50-year-old women with NAFLD was much lower in this cohort (7%) than in the general U.S. population (at least 25%), perhaps because the study population was enriched with individuals who are typically at low risk for NAFLD (i.e., African Americans, people with low body mass index, and/or low serum triglycerides).
Additional research is needed to clarify these issues and to investigate how maternal GDM affected the health of their children. Intrauterine exposure to metabolic stresses increases the risk for obesity and other metabolic disorders later in life, suggesting that offspring of mothers with GDM may require specialized surveillance or other precautions during childhood. Given that more young women are entering their reproductive years affected by diabetes and obesity, increased attention to these issues will be required to curb the growing public health burden of NAFLD.
Dr. Cynthia A. Moylan, M.H.S., is assistant professor of medicine, Duke University Medical Center and Veterans Affairs Medical Center, Durham, N.C. She is has no relevant financial conflicts of interests.
Nonalcoholic fatty liver disease is the most common and fastest growing liver disease worldwide. Identifying individuals at high risk for NAFLD remains challenging. Dr. Ajmera and his colleagues highlight the association between gestational diabetes mellitus (GDM) and NAFLD. Their work confirms and extends earlier studies that reported increased hepatic fat content and a substantially increased risk for NAFLD, in women with a prior history of GDM. In the present study, a more racially diverse U.S.-based population was followed for a much longer duration than was previous cohorts. After adjusted multivariate analysis, GDM remained a strong, independent predictor of future NAFLD. Indeed, GDM was a a better NAFLD predictor than the diagnosis of diabetes alone was. It is unclear if prepregnancy NAFLD might have affected the risk for GDM, as subjects were not assessed for hepatic steatosis or liver test elevations at baseline. Also, the percentage of 50-year-old women with NAFLD was much lower in this cohort (7%) than in the general U.S. population (at least 25%), perhaps because the study population was enriched with individuals who are typically at low risk for NAFLD (i.e., African Americans, people with low body mass index, and/or low serum triglycerides).
Additional research is needed to clarify these issues and to investigate how maternal GDM affected the health of their children. Intrauterine exposure to metabolic stresses increases the risk for obesity and other metabolic disorders later in life, suggesting that offspring of mothers with GDM may require specialized surveillance or other precautions during childhood. Given that more young women are entering their reproductive years affected by diabetes and obesity, increased attention to these issues will be required to curb the growing public health burden of NAFLD.
Dr. Cynthia A. Moylan, M.H.S., is assistant professor of medicine, Duke University Medical Center and Veterans Affairs Medical Center, Durham, N.C. She is has no relevant financial conflicts of interests.
Nonalcoholic fatty liver disease is the most common and fastest growing liver disease worldwide. Identifying individuals at high risk for NAFLD remains challenging. Dr. Ajmera and his colleagues highlight the association between gestational diabetes mellitus (GDM) and NAFLD. Their work confirms and extends earlier studies that reported increased hepatic fat content and a substantially increased risk for NAFLD, in women with a prior history of GDM. In the present study, a more racially diverse U.S.-based population was followed for a much longer duration than was previous cohorts. After adjusted multivariate analysis, GDM remained a strong, independent predictor of future NAFLD. Indeed, GDM was a a better NAFLD predictor than the diagnosis of diabetes alone was. It is unclear if prepregnancy NAFLD might have affected the risk for GDM, as subjects were not assessed for hepatic steatosis or liver test elevations at baseline. Also, the percentage of 50-year-old women with NAFLD was much lower in this cohort (7%) than in the general U.S. population (at least 25%), perhaps because the study population was enriched with individuals who are typically at low risk for NAFLD (i.e., African Americans, people with low body mass index, and/or low serum triglycerides).
Additional research is needed to clarify these issues and to investigate how maternal GDM affected the health of their children. Intrauterine exposure to metabolic stresses increases the risk for obesity and other metabolic disorders later in life, suggesting that offspring of mothers with GDM may require specialized surveillance or other precautions during childhood. Given that more young women are entering their reproductive years affected by diabetes and obesity, increased attention to these issues will be required to curb the growing public health burden of NAFLD.
Dr. Cynthia A. Moylan, M.H.S., is assistant professor of medicine, Duke University Medical Center and Veterans Affairs Medical Center, Durham, N.C. She is has no relevant financial conflicts of interests.
WASHINGTON – Gestational diabetes was identified as a significant, independent risk factor for developing non-alcoholic fatty liver disease later in life, according to a study of more than 1,000 women followed for 25 years.
This study “is the first to show a strong association between gestational diabetes in young adulthood and non-alcoholic fatty liver disease in middle-age,” Dr. Veeral Ajmera of the department of gastroenterology at the University of California, San Francisco, reported at the annual Digestive Disease Week.
The study evaluated 1,115 women from the Coronary Artery Risk Development in Young Adults (CARDIA) study, who had at least one delivery, did not have a diabetes diagnosis before pregnancy, and had a CT evaluation for hepatic steatosis at the 25-year visit, in 2010 and 2011. Women were excluded if they did not have a complete CT scan at that time, they had more than 14 drinks of alcohol per week, used medications associated with steatosis, or had chronic viral hepatitis or HIV infections.
At baseline the median age was 25-26 years, about 55%-56% were black, and the prevalence of hypertension (2%-3%) and dyslipidemia were similar. The CARDIA study enrolled about 5,100 men and women aged 18-30 years at four U.S. medical centers in the mid 1980s. Patients had 7 study visits over a 25-year follow-up period.
Of the 1,115 women evaluated, 124 (11%) went on to develop GDM and 75 (7%) met the CT definition for NAFLD (liver attenuation less than or equal to 40 Hounsfield units on CT scan) by the 25-year follow-up, when they were a median age of 50-51 years.
At 25 years, 14% of those with a history of GDM had NAFLD, compared with 5.8% of those who did not have GDM, for an unadjusted odds ratio of 2.56 (p <0.01), Dr. Ajmera said.
In the statistical analysis, the researchers determined that baseline homeostatic model assessment of insulin resistance (HOMA-IR) and baseline triglycerides were also ”strongly associated” with NAFLD at year 25.
“Importantly,” he noted, the measure of the association between GDM and NAFLD remained statistically significant, after adjusting for these covariates (OR, 2.29). At the start of the study, women who went on to develop GDM had significantly higher body mass index (BMI), HOMA-IR, waist circumference, and triglycerides than those who did not develop GDM, but the magnitude of those differences was small.
Additionally, after adjustment for a diagnosis of diabetes at year 25, the association between a history of GDM and NAFLD was stronger (OR, 1.99) than the association between a diagnosis of diabetes at year 25 and NAFLD (OR, 1.5), he said.
The researchers added BMI to their multivariate analysis to determine whether women with a gestational diabetes history gained more weight, and whether that weight explained the increased prevalence of NAFLD, “and found that the association between gestational diabetes and non-alcoholic fatty liver disease remained,” Dr. Ajmera added.
Evaluations of race, baseline BMI, and baseline HOMA-IR as effect modifiers of the relationship between GDM and NAFLD were not significant.
“Gestational diabetes represents insulin resistance unmasked by the stress of pregnancy, and offers the unique opportunity to identify those at risk of NAFLD at a young age,” Dr. Ajmera concluded.
Limitations of the study included not being able to determine if the women had NAFLD before they were diagnosed with GDM. However, based on the participants’ young age at enrollment, that is unlikely, he said. In addition, the researchers had no information on liver biochemistry tests, which, however, are not sensitive or specific for diagnosing NAFLD. The strengths of the study include the length of follow-up of a large biracial population, with measurement of well-characterized metabolic covariates measured, he added.
Dr. Ajmera reported having no relevant financial disclosures. The CARDIA study is supported by the National Heart, Lung, and Blood Institute, part of the National Institutes of Health.
WASHINGTON – Gestational diabetes was identified as a significant, independent risk factor for developing non-alcoholic fatty liver disease later in life, according to a study of more than 1,000 women followed for 25 years.
This study “is the first to show a strong association between gestational diabetes in young adulthood and non-alcoholic fatty liver disease in middle-age,” Dr. Veeral Ajmera of the department of gastroenterology at the University of California, San Francisco, reported at the annual Digestive Disease Week.
The study evaluated 1,115 women from the Coronary Artery Risk Development in Young Adults (CARDIA) study, who had at least one delivery, did not have a diabetes diagnosis before pregnancy, and had a CT evaluation for hepatic steatosis at the 25-year visit, in 2010 and 2011. Women were excluded if they did not have a complete CT scan at that time, they had more than 14 drinks of alcohol per week, used medications associated with steatosis, or had chronic viral hepatitis or HIV infections.
At baseline the median age was 25-26 years, about 55%-56% were black, and the prevalence of hypertension (2%-3%) and dyslipidemia were similar. The CARDIA study enrolled about 5,100 men and women aged 18-30 years at four U.S. medical centers in the mid 1980s. Patients had 7 study visits over a 25-year follow-up period.
Of the 1,115 women evaluated, 124 (11%) went on to develop GDM and 75 (7%) met the CT definition for NAFLD (liver attenuation less than or equal to 40 Hounsfield units on CT scan) by the 25-year follow-up, when they were a median age of 50-51 years.
At 25 years, 14% of those with a history of GDM had NAFLD, compared with 5.8% of those who did not have GDM, for an unadjusted odds ratio of 2.56 (p <0.01), Dr. Ajmera said.
In the statistical analysis, the researchers determined that baseline homeostatic model assessment of insulin resistance (HOMA-IR) and baseline triglycerides were also ”strongly associated” with NAFLD at year 25.
“Importantly,” he noted, the measure of the association between GDM and NAFLD remained statistically significant, after adjusting for these covariates (OR, 2.29). At the start of the study, women who went on to develop GDM had significantly higher body mass index (BMI), HOMA-IR, waist circumference, and triglycerides than those who did not develop GDM, but the magnitude of those differences was small.
Additionally, after adjustment for a diagnosis of diabetes at year 25, the association between a history of GDM and NAFLD was stronger (OR, 1.99) than the association between a diagnosis of diabetes at year 25 and NAFLD (OR, 1.5), he said.
The researchers added BMI to their multivariate analysis to determine whether women with a gestational diabetes history gained more weight, and whether that weight explained the increased prevalence of NAFLD, “and found that the association between gestational diabetes and non-alcoholic fatty liver disease remained,” Dr. Ajmera added.
Evaluations of race, baseline BMI, and baseline HOMA-IR as effect modifiers of the relationship between GDM and NAFLD were not significant.
“Gestational diabetes represents insulin resistance unmasked by the stress of pregnancy, and offers the unique opportunity to identify those at risk of NAFLD at a young age,” Dr. Ajmera concluded.
Limitations of the study included not being able to determine if the women had NAFLD before they were diagnosed with GDM. However, based on the participants’ young age at enrollment, that is unlikely, he said. In addition, the researchers had no information on liver biochemistry tests, which, however, are not sensitive or specific for diagnosing NAFLD. The strengths of the study include the length of follow-up of a large biracial population, with measurement of well-characterized metabolic covariates measured, he added.
Dr. Ajmera reported having no relevant financial disclosures. The CARDIA study is supported by the National Heart, Lung, and Blood Institute, part of the National Institutes of Health.
AT DDW® 2015
Key clinical point: Gestational diabetes could be used to identify young women at increased risk of having non-alcoholic fatty liver disease (NAFLD) in middle age.
Major finding: Having been diagnosed with gestational diabetes was associated with about a two-fold increased risk of having NAFLD in middle age.
Data source: The research involved 1,115 women enrolled in the 25-year Coronary Artery Risk Development in Young Adults (CARDIA) study.
Disclosures: Dr. Ajmera reported having no relevant financial disclosures. The CARDIA study is supported by the National Heart, Lung, and Blood Institute.
DDW: Recurrent C. difficile infections take heavy toll on IBD patients
WASHINGTON – Patients with inflammatory bowel disease had a one-third higher risk for having a recurrent Clostridium difficile infection than did the general population, and a 20-fold higher risk for needing a total colectomy because of the infection, a study showed.
Risk factors for recurrent C. difficile infection (rCDI) in patients with inflammatory bowel disease (IBD) include a recent hospitalization, immunosuppressive drugs, and antibiotics, but which drugs are most culpable is unclear, according to Dr. Roshan Razik of Mount Sinai Hospital, Toronto, and the University of Toronto.
“The drugs that we’re using do place patients at higher risk for recurrent C. difficile, but it’s yet to come out which drugs within drug categories – immunomodulators, antibiotics, biologics – pose a higher risk, although we are beginning to see evidence, for example, that azathioprine is higher risk than methotrexate, infliximab might be higher risk than adalimumab, so we have to continue to parse through the data,” he said in an interview.
He and his colleagues conducted two retrospective studies to assess the effects of rCDI on patients with IBD.
The first study used a case-control design, including patients with IBD who had two or more documented instances of rCDI from 2010 through 2013 as cases, and IBD patients with only one infection as controls.
The second study used a retrospective cohort to calculate the incidence of rCDI in patients with IBD, compared with patients without IBD, Dr. Razik reported at the annual Digestive Disease Week.
There were a total of 503 patients who tested positive for CDI included in the studies: 110 patients with IBD (49% with Crohn’s disease and 51% with ulcerative colitis) and 393 without. The mean age was 58.8 years, and 61.4% were female.
Compared with patients without IBD, patients with Crohn’s disease or ulcerative colitis developed CDI at a younger age (39 years vs. 64 years, P < .001), used more steroids (39.1% vs. 12%, P < .001), used more immunosuppressive agents (42.7% vs. 13.2%, P < .001), and were more likely to have a prior bowel resection (28.2% vs. 11.5%, P < .001).
In all, 32% of patients with IBD had a recurrent CDI, compared with 24% of non-IBD patients (P < .01). There were no significant differences between the groups in the number of hospitalizations due to CDI, but patients with IBD were significantly more likely to require colectomy because of the infections (6.4% vs. 0.3%, P < .001).
In a multivariate analysis, risk factors for rCDI in patients with IBD included nonileal Crohn’s disease (odds ratio, 2.59; P < .001), recent antibiotic therapy (OR, 2.60; P < .001), use of a 5-aminosalicylic acid drug (OR, 3.06; P < .001), steroid use (OR, 2.94; P < .001), biologic therapy (OR, 2.50; P = .001), a recent hospitalization (OR, 2.62; P < .001), and no previous bowel resections (OR, 1.72; P = .020).
Clinicians need to look beyond the usual suspects, antibiotics, as causative agents for rCDI. Immunomodulators and biologic agents also were strongly associated with rCDI in the study, Dr. Razik noted.
The study source was not disclosed. He reported having no relevant financial conflicts of interest.
WASHINGTON – Patients with inflammatory bowel disease had a one-third higher risk for having a recurrent Clostridium difficile infection than did the general population, and a 20-fold higher risk for needing a total colectomy because of the infection, a study showed.
Risk factors for recurrent C. difficile infection (rCDI) in patients with inflammatory bowel disease (IBD) include a recent hospitalization, immunosuppressive drugs, and antibiotics, but which drugs are most culpable is unclear, according to Dr. Roshan Razik of Mount Sinai Hospital, Toronto, and the University of Toronto.
“The drugs that we’re using do place patients at higher risk for recurrent C. difficile, but it’s yet to come out which drugs within drug categories – immunomodulators, antibiotics, biologics – pose a higher risk, although we are beginning to see evidence, for example, that azathioprine is higher risk than methotrexate, infliximab might be higher risk than adalimumab, so we have to continue to parse through the data,” he said in an interview.
He and his colleagues conducted two retrospective studies to assess the effects of rCDI on patients with IBD.
The first study used a case-control design, including patients with IBD who had two or more documented instances of rCDI from 2010 through 2013 as cases, and IBD patients with only one infection as controls.
The second study used a retrospective cohort to calculate the incidence of rCDI in patients with IBD, compared with patients without IBD, Dr. Razik reported at the annual Digestive Disease Week.
There were a total of 503 patients who tested positive for CDI included in the studies: 110 patients with IBD (49% with Crohn’s disease and 51% with ulcerative colitis) and 393 without. The mean age was 58.8 years, and 61.4% were female.
Compared with patients without IBD, patients with Crohn’s disease or ulcerative colitis developed CDI at a younger age (39 years vs. 64 years, P < .001), used more steroids (39.1% vs. 12%, P < .001), used more immunosuppressive agents (42.7% vs. 13.2%, P < .001), and were more likely to have a prior bowel resection (28.2% vs. 11.5%, P < .001).
In all, 32% of patients with IBD had a recurrent CDI, compared with 24% of non-IBD patients (P < .01). There were no significant differences between the groups in the number of hospitalizations due to CDI, but patients with IBD were significantly more likely to require colectomy because of the infections (6.4% vs. 0.3%, P < .001).
In a multivariate analysis, risk factors for rCDI in patients with IBD included nonileal Crohn’s disease (odds ratio, 2.59; P < .001), recent antibiotic therapy (OR, 2.60; P < .001), use of a 5-aminosalicylic acid drug (OR, 3.06; P < .001), steroid use (OR, 2.94; P < .001), biologic therapy (OR, 2.50; P = .001), a recent hospitalization (OR, 2.62; P < .001), and no previous bowel resections (OR, 1.72; P = .020).
Clinicians need to look beyond the usual suspects, antibiotics, as causative agents for rCDI. Immunomodulators and biologic agents also were strongly associated with rCDI in the study, Dr. Razik noted.
The study source was not disclosed. He reported having no relevant financial conflicts of interest.
WASHINGTON – Patients with inflammatory bowel disease had a one-third higher risk for having a recurrent Clostridium difficile infection than did the general population, and a 20-fold higher risk for needing a total colectomy because of the infection, a study showed.
Risk factors for recurrent C. difficile infection (rCDI) in patients with inflammatory bowel disease (IBD) include a recent hospitalization, immunosuppressive drugs, and antibiotics, but which drugs are most culpable is unclear, according to Dr. Roshan Razik of Mount Sinai Hospital, Toronto, and the University of Toronto.
“The drugs that we’re using do place patients at higher risk for recurrent C. difficile, but it’s yet to come out which drugs within drug categories – immunomodulators, antibiotics, biologics – pose a higher risk, although we are beginning to see evidence, for example, that azathioprine is higher risk than methotrexate, infliximab might be higher risk than adalimumab, so we have to continue to parse through the data,” he said in an interview.
He and his colleagues conducted two retrospective studies to assess the effects of rCDI on patients with IBD.
The first study used a case-control design, including patients with IBD who had two or more documented instances of rCDI from 2010 through 2013 as cases, and IBD patients with only one infection as controls.
The second study used a retrospective cohort to calculate the incidence of rCDI in patients with IBD, compared with patients without IBD, Dr. Razik reported at the annual Digestive Disease Week.
There were a total of 503 patients who tested positive for CDI included in the studies: 110 patients with IBD (49% with Crohn’s disease and 51% with ulcerative colitis) and 393 without. The mean age was 58.8 years, and 61.4% were female.
Compared with patients without IBD, patients with Crohn’s disease or ulcerative colitis developed CDI at a younger age (39 years vs. 64 years, P < .001), used more steroids (39.1% vs. 12%, P < .001), used more immunosuppressive agents (42.7% vs. 13.2%, P < .001), and were more likely to have a prior bowel resection (28.2% vs. 11.5%, P < .001).
In all, 32% of patients with IBD had a recurrent CDI, compared with 24% of non-IBD patients (P < .01). There were no significant differences between the groups in the number of hospitalizations due to CDI, but patients with IBD were significantly more likely to require colectomy because of the infections (6.4% vs. 0.3%, P < .001).
In a multivariate analysis, risk factors for rCDI in patients with IBD included nonileal Crohn’s disease (odds ratio, 2.59; P < .001), recent antibiotic therapy (OR, 2.60; P < .001), use of a 5-aminosalicylic acid drug (OR, 3.06; P < .001), steroid use (OR, 2.94; P < .001), biologic therapy (OR, 2.50; P = .001), a recent hospitalization (OR, 2.62; P < .001), and no previous bowel resections (OR, 1.72; P = .020).
Clinicians need to look beyond the usual suspects, antibiotics, as causative agents for rCDI. Immunomodulators and biologic agents also were strongly associated with rCDI in the study, Dr. Razik noted.
The study source was not disclosed. He reported having no relevant financial conflicts of interest.
AT DDW 2015
Key clinical point: Patients with inflammatory bowel disease are at higher risk for recurrent Clostridium difficile infections.
Major finding: 32% of patients with IBD had a recurrent CDI, compared with 24% of non-IBD patients
Data source: Retrospective case-control studies with 503 patients, comparing patients with IBD with and without recurrent C. difficile infections and comparing patients with IBD with non-IBD patients.
Disclosures: The study source was not disclosed. Dr. Razik reported having no relevant financial conflicts of interest.
DDW: Menopausal hormone therapy increases major GI bleed risk
Menopausal hormone therapy is associated with an increased risk of major gastrointestinal bleeding, particularly in the lower gastrointestinal tract, that is associated with duration of use, a study has found.
Analysis of data from 73,863 women enrolled in the Nurses’ Health Study II in 1989 showed that current users of menopausal hormone therapy had a 46% increase in the risk of a major gastrointestinal bleed and a more than twofold increase in the risk of a lower GI bleed or ischemic colitis, compared with never users, said Dr. Prashant Singh of Massachusetts General Hospital, Boston.
Past users showed a much smaller increase risk of bleeding, while increasing duration of hormone therapy was significantly associated with increasing risk of major and low gastrointestinal bleeding.
“Although our findings show that menopausal hormone therapy may increase the risk of major GI bleeding, especially in the lower GI tract, it is important for these patients to know that this therapy is still an effective treatment; however, both clinician and patient should be more cautious in using this therapy in some cases, such as with patients who have a history of ischemic colitis,” Dr. Singh said at the annual Digestive Disease Week.
Dr. Singh does not have any relevant financial or other relationship with any manufacturer or provider of commercial products or services that he discussed during the presentation.
Menopausal hormone therapy is associated with an increased risk of major gastrointestinal bleeding, particularly in the lower gastrointestinal tract, that is associated with duration of use, a study has found.
Analysis of data from 73,863 women enrolled in the Nurses’ Health Study II in 1989 showed that current users of menopausal hormone therapy had a 46% increase in the risk of a major gastrointestinal bleed and a more than twofold increase in the risk of a lower GI bleed or ischemic colitis, compared with never users, said Dr. Prashant Singh of Massachusetts General Hospital, Boston.
Past users showed a much smaller increase risk of bleeding, while increasing duration of hormone therapy was significantly associated with increasing risk of major and low gastrointestinal bleeding.
“Although our findings show that menopausal hormone therapy may increase the risk of major GI bleeding, especially in the lower GI tract, it is important for these patients to know that this therapy is still an effective treatment; however, both clinician and patient should be more cautious in using this therapy in some cases, such as with patients who have a history of ischemic colitis,” Dr. Singh said at the annual Digestive Disease Week.
Dr. Singh does not have any relevant financial or other relationship with any manufacturer or provider of commercial products or services that he discussed during the presentation.
Menopausal hormone therapy is associated with an increased risk of major gastrointestinal bleeding, particularly in the lower gastrointestinal tract, that is associated with duration of use, a study has found.
Analysis of data from 73,863 women enrolled in the Nurses’ Health Study II in 1989 showed that current users of menopausal hormone therapy had a 46% increase in the risk of a major gastrointestinal bleed and a more than twofold increase in the risk of a lower GI bleed or ischemic colitis, compared with never users, said Dr. Prashant Singh of Massachusetts General Hospital, Boston.
Past users showed a much smaller increase risk of bleeding, while increasing duration of hormone therapy was significantly associated with increasing risk of major and low gastrointestinal bleeding.
“Although our findings show that menopausal hormone therapy may increase the risk of major GI bleeding, especially in the lower GI tract, it is important for these patients to know that this therapy is still an effective treatment; however, both clinician and patient should be more cautious in using this therapy in some cases, such as with patients who have a history of ischemic colitis,” Dr. Singh said at the annual Digestive Disease Week.
Dr. Singh does not have any relevant financial or other relationship with any manufacturer or provider of commercial products or services that he discussed during the presentation.
FROM DDW 2015
Key clinical point: Menopausal hormone therapy is associated with an increased risk of major gastrointestinal bleeding, particularly in the lower gastrointestinal tract.
Major finding: Current users of menopausal hormone therapy had a 46% increase in the risk of a major gastrointestinal bleed and a more than twofold increase in the risk of a lower GI bleed or ischemic colitis.
Data source: Analysis of data from 73,863 women enrolled in the Nurses’ Health Study II.
Disclosures: No conflicts of interest were disclosed.
DDW: Urinary enzymes hint at gastric cancer
WASHINGTON – A simple urine test could detect gastric cancer even at an early stage, the test’s developers say.
The test, which looks for the presence of two metalloprotease enzymes labeled ADAM 12 and MMP-9/NGAL had 77.1% sensitivity and 82.9% specificity for gastric cancer when tested in 35 patients with the malignancy and an equal number of healthy controls, reported Dr. Takaya Shimura from the department of surgery at Boston Children’s Hospital and Harvard Medical School in Boston.
“This study represents the first demonstration of the presence of ADAM 12 and MMO-9/NGAL complex in the urine of gastric cancer patients,” he said at the annual Digestive Disease Week.
Dr. Stephen J. Meltzer of Johns Hopkins University, Baltimore, commented in an interview that the findings are convincing but preliminary.
A randomized clinical trial enrolling a larger number of patients and controls would be required before he would consider screening patients for the enzymes, said Dr. Meltzer, who was not involved in the study and comoderated the meeting session where the results were presented.
ADAM 12 (a disintegrin and metalloprotease 12) and MMP-9 (matrix metalloprotease 9) are both members of a family of enzymes involved in cellular adhesion, invasion, growth, and angiogenesis, Dr. Shimura explained. MMP-9, when complexed with NGAL (neutrophil gelatinase associated lipocalin) is protected from autodegradation.
The investigators, from the lab of Dr. Marsha A. Moses at Boston Children’s Hospital, and their collaborators in Japan had previously reported that MMPs in urine were independent predictors of both organ-confined and metastatic cancer.
Urinary assays are noninvasive, using easily accessed tissues that can be handled simply and inexpensively, making them ideal for cancer detection, Dr, Shimura said.
Current tests for gastric cancer, such as carcinoembryonic antigen (CEA) and cancer antigens (CA) 19-9 and 72-4, have poor sensitivity for detecting advanced disease, and are even worse at spotting early disease, he noted.
To see whether they could improve on the current lot of tests, the investigators enrolled 106 patients in a case-control study, settling eventually, after age and sex matching, on a cohort of 70 patients: 35 with primarily early-stage gastric cancer, and 35 healthy controls.
After screening the urine of participants for about 50 different antigenic proteins, they found that the patients with gastric cancer had significantly higher levels in their urine of both ADAM 12 (P < .001) and the MMP-9/NGAL complex (P = .020).
In a multivariate analysis, they showed that both enzymes were strong, independent predictors of gastric cancer, with an odds ratio for urinary MMO-9/NGAL of 6.71 (P = .002), and an OR of 15.4 for ADAM 12 (P = .002). In contrast, Helicobacter pylori infection was associated with a nonsignificant OR of 2.54.
In a receiver operating characteristic (ROC) analysis, they also found that MMP-9/NGAL was associated with an area-under-the curve (AUC) of 0.657 (P = .024), ADAM 12 was associated with an AUC of 0.757 (P < .001), and that the two combined had an AUC of 0.825 (P < .001).
As noted before, the sensitivity of the combined enzymes was 77%, and the specificity was 83%.
Finally, using immunohistochemical analysis, the investigators were able to show that gastric cancer tissues had high levels of coexpression of MMP-9 and NGAL (P <.001) and high expression levels of ADAM 12 (P < .001), compared with adjacent normal tissues.
WASHINGTON – A simple urine test could detect gastric cancer even at an early stage, the test’s developers say.
The test, which looks for the presence of two metalloprotease enzymes labeled ADAM 12 and MMP-9/NGAL had 77.1% sensitivity and 82.9% specificity for gastric cancer when tested in 35 patients with the malignancy and an equal number of healthy controls, reported Dr. Takaya Shimura from the department of surgery at Boston Children’s Hospital and Harvard Medical School in Boston.
“This study represents the first demonstration of the presence of ADAM 12 and MMO-9/NGAL complex in the urine of gastric cancer patients,” he said at the annual Digestive Disease Week.
Dr. Stephen J. Meltzer of Johns Hopkins University, Baltimore, commented in an interview that the findings are convincing but preliminary.
A randomized clinical trial enrolling a larger number of patients and controls would be required before he would consider screening patients for the enzymes, said Dr. Meltzer, who was not involved in the study and comoderated the meeting session where the results were presented.
ADAM 12 (a disintegrin and metalloprotease 12) and MMP-9 (matrix metalloprotease 9) are both members of a family of enzymes involved in cellular adhesion, invasion, growth, and angiogenesis, Dr. Shimura explained. MMP-9, when complexed with NGAL (neutrophil gelatinase associated lipocalin) is protected from autodegradation.
The investigators, from the lab of Dr. Marsha A. Moses at Boston Children’s Hospital, and their collaborators in Japan had previously reported that MMPs in urine were independent predictors of both organ-confined and metastatic cancer.
Urinary assays are noninvasive, using easily accessed tissues that can be handled simply and inexpensively, making them ideal for cancer detection, Dr, Shimura said.
Current tests for gastric cancer, such as carcinoembryonic antigen (CEA) and cancer antigens (CA) 19-9 and 72-4, have poor sensitivity for detecting advanced disease, and are even worse at spotting early disease, he noted.
To see whether they could improve on the current lot of tests, the investigators enrolled 106 patients in a case-control study, settling eventually, after age and sex matching, on a cohort of 70 patients: 35 with primarily early-stage gastric cancer, and 35 healthy controls.
After screening the urine of participants for about 50 different antigenic proteins, they found that the patients with gastric cancer had significantly higher levels in their urine of both ADAM 12 (P < .001) and the MMP-9/NGAL complex (P = .020).
In a multivariate analysis, they showed that both enzymes were strong, independent predictors of gastric cancer, with an odds ratio for urinary MMO-9/NGAL of 6.71 (P = .002), and an OR of 15.4 for ADAM 12 (P = .002). In contrast, Helicobacter pylori infection was associated with a nonsignificant OR of 2.54.
In a receiver operating characteristic (ROC) analysis, they also found that MMP-9/NGAL was associated with an area-under-the curve (AUC) of 0.657 (P = .024), ADAM 12 was associated with an AUC of 0.757 (P < .001), and that the two combined had an AUC of 0.825 (P < .001).
As noted before, the sensitivity of the combined enzymes was 77%, and the specificity was 83%.
Finally, using immunohistochemical analysis, the investigators were able to show that gastric cancer tissues had high levels of coexpression of MMP-9 and NGAL (P <.001) and high expression levels of ADAM 12 (P < .001), compared with adjacent normal tissues.
WASHINGTON – A simple urine test could detect gastric cancer even at an early stage, the test’s developers say.
The test, which looks for the presence of two metalloprotease enzymes labeled ADAM 12 and MMP-9/NGAL had 77.1% sensitivity and 82.9% specificity for gastric cancer when tested in 35 patients with the malignancy and an equal number of healthy controls, reported Dr. Takaya Shimura from the department of surgery at Boston Children’s Hospital and Harvard Medical School in Boston.
“This study represents the first demonstration of the presence of ADAM 12 and MMO-9/NGAL complex in the urine of gastric cancer patients,” he said at the annual Digestive Disease Week.
Dr. Stephen J. Meltzer of Johns Hopkins University, Baltimore, commented in an interview that the findings are convincing but preliminary.
A randomized clinical trial enrolling a larger number of patients and controls would be required before he would consider screening patients for the enzymes, said Dr. Meltzer, who was not involved in the study and comoderated the meeting session where the results were presented.
ADAM 12 (a disintegrin and metalloprotease 12) and MMP-9 (matrix metalloprotease 9) are both members of a family of enzymes involved in cellular adhesion, invasion, growth, and angiogenesis, Dr. Shimura explained. MMP-9, when complexed with NGAL (neutrophil gelatinase associated lipocalin) is protected from autodegradation.
The investigators, from the lab of Dr. Marsha A. Moses at Boston Children’s Hospital, and their collaborators in Japan had previously reported that MMPs in urine were independent predictors of both organ-confined and metastatic cancer.
Urinary assays are noninvasive, using easily accessed tissues that can be handled simply and inexpensively, making them ideal for cancer detection, Dr, Shimura said.
Current tests for gastric cancer, such as carcinoembryonic antigen (CEA) and cancer antigens (CA) 19-9 and 72-4, have poor sensitivity for detecting advanced disease, and are even worse at spotting early disease, he noted.
To see whether they could improve on the current lot of tests, the investigators enrolled 106 patients in a case-control study, settling eventually, after age and sex matching, on a cohort of 70 patients: 35 with primarily early-stage gastric cancer, and 35 healthy controls.
After screening the urine of participants for about 50 different antigenic proteins, they found that the patients with gastric cancer had significantly higher levels in their urine of both ADAM 12 (P < .001) and the MMP-9/NGAL complex (P = .020).
In a multivariate analysis, they showed that both enzymes were strong, independent predictors of gastric cancer, with an odds ratio for urinary MMO-9/NGAL of 6.71 (P = .002), and an OR of 15.4 for ADAM 12 (P = .002). In contrast, Helicobacter pylori infection was associated with a nonsignificant OR of 2.54.
In a receiver operating characteristic (ROC) analysis, they also found that MMP-9/NGAL was associated with an area-under-the curve (AUC) of 0.657 (P = .024), ADAM 12 was associated with an AUC of 0.757 (P < .001), and that the two combined had an AUC of 0.825 (P < .001).
As noted before, the sensitivity of the combined enzymes was 77%, and the specificity was 83%.
Finally, using immunohistochemical analysis, the investigators were able to show that gastric cancer tissues had high levels of coexpression of MMP-9 and NGAL (P <.001) and high expression levels of ADAM 12 (P < .001), compared with adjacent normal tissues.
AT DDW 2015
Key clinical point: Urinary levels of two metalloproteases were significantly elevated in the urine of patients with gastric cancer, compared with controls.
Major finding: High expression of ADAM 12 and MMP-9/NGAL complex had a 77% sensitivity and 83% specificity for gastric cancer.
Data source: Case-control study of 35 patients with gastric cancer and 35 controls.
Disclosures: The study was supported by the Advanced Medical Research Foundation in the United States and the Research Fellowship of the Uehara Memorial Foundation, Japan. Dr. Shimura reported having no conflicts of interest.
VIDEO: Stroop app predicts hepatic encephalopathy
WASHINGTON – One of the many comorbidities of cirrhosis is hepatic encephalopathy and its development is insidious. Often the patient is unaware and symptoms may not be so obvious to the physician that testing seems imperative, according to Dr. Jasmohan Bajaj of Virginia Commonwealth University in Richmond and McGuire VAMC.
He and his coworkers have developed an easy-to-use smartphone screening tool that tests the patient’s cognitive speed and flexibility, which physicians can administer themselves without having to refer the patient to psychiatric services. Currently, the need for a referral often means that these end-stage liver patients are not screened or treated for hepatic encephalopathy until their cognitive symptoms are overt.
Dr. Bajaj has received support or consulting fees from, or has been on advisory committees for, Merz, Otsuka, Salix, and Grifols.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WASHINGTON – One of the many comorbidities of cirrhosis is hepatic encephalopathy and its development is insidious. Often the patient is unaware and symptoms may not be so obvious to the physician that testing seems imperative, according to Dr. Jasmohan Bajaj of Virginia Commonwealth University in Richmond and McGuire VAMC.
He and his coworkers have developed an easy-to-use smartphone screening tool that tests the patient’s cognitive speed and flexibility, which physicians can administer themselves without having to refer the patient to psychiatric services. Currently, the need for a referral often means that these end-stage liver patients are not screened or treated for hepatic encephalopathy until their cognitive symptoms are overt.
Dr. Bajaj has received support or consulting fees from, or has been on advisory committees for, Merz, Otsuka, Salix, and Grifols.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WASHINGTON – One of the many comorbidities of cirrhosis is hepatic encephalopathy and its development is insidious. Often the patient is unaware and symptoms may not be so obvious to the physician that testing seems imperative, according to Dr. Jasmohan Bajaj of Virginia Commonwealth University in Richmond and McGuire VAMC.
He and his coworkers have developed an easy-to-use smartphone screening tool that tests the patient’s cognitive speed and flexibility, which physicians can administer themselves without having to refer the patient to psychiatric services. Currently, the need for a referral often means that these end-stage liver patients are not screened or treated for hepatic encephalopathy until their cognitive symptoms are overt.
Dr. Bajaj has received support or consulting fees from, or has been on advisory committees for, Merz, Otsuka, Salix, and Grifols.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT DDW 2015
DDW: HBV, tuberculosis reactivations rare in IBD patients on biologic therapy
WASHINGTON – Reactivation of tuberculosis and hepatitis B infections after starting treatment with anti–tumor necrosis factor therapy was “rare” in a large national cohort study of veterans with inflammatory bowel disease, Dr. Jason Hou reported at the annual Digestive Disease Week.
The estimated rate of tuberculosis reactivations was 2.8 per 10,000 patient-years of exposure to anti-TNF therapy “in a fairly well-screened cohort of IBD patients,” said Dr. Hou, codirector of the Inflammatory Bowel Disease Center at Baylor College of Medicine, Houston. The estimate for HBV reactivation or acute liver failure in this cohort was less than 1.4 per 10,000 patient-years of exposure, he noted.
Practice guidelines recommend that patients with IBD should be screened for latent tuberculosis and HBV before starting treatment with an anti-TNF drug, but how often reactivation actually occurs in this population is not known, he pointed out. Moreover, recent studies have questioned the cost-effectiveness of universal screening for HBV before starting treatment, and TB reactivation rates in patients with IBD treated with anti-TNF drugs “have not been assessed on a national population level.”
Dr. Hou and his associates used a national Veterans Affairs database to identify patients who had been diagnosed between 2003 and 2011 with Crohn’s disease or ulcerative colitis, based on ICD-9 codes, and had filled at least one prescription for infliximab, adalimumab, or certolizumab pegol; they also looked for codes related to possible tuberculosis reactivation or acute liver failure related to HBV reactivation at the time of or after anti-TNF therapy was started. Cases were then verified by reviewing electronic medical records of patients to confirm the diagnosis of tuberculosis or HBV, exposure to an anti-TNF drug, and completion of pretreatment screening.
They identified 3,357 patients with IBD who had received a prescription for an anti-TNF treatment, representing 7,210 patient-years of anti-TNF treatment; most were men and were white. The mean time on treatment was about 2 years, and they had started treatment at a mean age of 57 years. Screening rates for tuberculosis were relatively high and remained stable throughout the study period, at 72% overall, but HBV screening rates were low, at 24% overall. HBV screening was not included in practice guidelines until 2006, and the rate significantly increased from under 10% at the beginning of the period studied to 42% at the end, Dr. Hou noted.
They identified 23 patients with ICD-9 codes related to tuberculosis occurring after they started anti-TNF therapy, but “on chart review, only two patients were confirmed to have tuberculosis reactivation” related to anti-TNF therapy, which occurred at 8 and 18 months of treatment, he said. “Very interestingly, both of these patients had latent tuberculosis and documented completed courses of INH [isonicotinylhydrazine] and a negative chest x-ray prior to [anti-]TNF initiation.” Because the only cases of tuberculosis reactivation occurred in patients with a prior history of latent tuberculosis, “we should maintain extra diligence in those patients even if appropriate screening has been performed,” he advised.
They identified 12 patients with codes related to hepatitis B after the treatment started, two had clinically relevant outcomes, but the chart review indicated that neither case was HPV reactivation. There were two cases of patients with positive HBV tests. One of these patients, who developed acute jaundice with serologies consistent with acute HBV infection, reported a possible exposure to HBV and was newly diagnosed with HIV, associated with the same encounter. This patient was on infliximab and continued treatment, and HBV viremia spontaneously cleared without antiviral treatment, Dr. Hou said.
The second “clinically relevant” case was a patient with chronic HBV infection, identified in a presurgical screen, who was asymptomatic and had normal liver function tests. Infliximab was discontinued and the patient started antiviral therapy; viremia resolved and the patient resumed treatment with infliximab “without complications,” Dr. Hou said.
Another four patients were identified related to codes for acute liver failure, but on chart review, none had liver failure related to hepatitis B.
The study’s limitations include the possibility that patients may receive medical care outside the VA system, which would not be picked up in the analysis, he said, but added, “when we look at our estimate of tuberculosis reactivation, they mirror almost exactly those reported in the rheumatology literature in screened populations.” Another limitation is that the study depended on the accuracy of ICD-9 codes for the diagnoses, but all outcomes were verified in the chart review, he said.
Dr. Hou is also director of Inflammatory Bowel Diseases and an investigator in the clinical epidemiology and outcomes program in the Center for Innovations in Quality Effectiveness and Safety at the Michael E. DeBakey VA Medical Center, Houston.
His financial disclosures include receiving consulting, speaking, teaching, and/or advisory fees from Janssen, Aptalis, and AbbVie.
WASHINGTON – Reactivation of tuberculosis and hepatitis B infections after starting treatment with anti–tumor necrosis factor therapy was “rare” in a large national cohort study of veterans with inflammatory bowel disease, Dr. Jason Hou reported at the annual Digestive Disease Week.
The estimated rate of tuberculosis reactivations was 2.8 per 10,000 patient-years of exposure to anti-TNF therapy “in a fairly well-screened cohort of IBD patients,” said Dr. Hou, codirector of the Inflammatory Bowel Disease Center at Baylor College of Medicine, Houston. The estimate for HBV reactivation or acute liver failure in this cohort was less than 1.4 per 10,000 patient-years of exposure, he noted.
Practice guidelines recommend that patients with IBD should be screened for latent tuberculosis and HBV before starting treatment with an anti-TNF drug, but how often reactivation actually occurs in this population is not known, he pointed out. Moreover, recent studies have questioned the cost-effectiveness of universal screening for HBV before starting treatment, and TB reactivation rates in patients with IBD treated with anti-TNF drugs “have not been assessed on a national population level.”
Dr. Hou and his associates used a national Veterans Affairs database to identify patients who had been diagnosed between 2003 and 2011 with Crohn’s disease or ulcerative colitis, based on ICD-9 codes, and had filled at least one prescription for infliximab, adalimumab, or certolizumab pegol; they also looked for codes related to possible tuberculosis reactivation or acute liver failure related to HBV reactivation at the time of or after anti-TNF therapy was started. Cases were then verified by reviewing electronic medical records of patients to confirm the diagnosis of tuberculosis or HBV, exposure to an anti-TNF drug, and completion of pretreatment screening.
They identified 3,357 patients with IBD who had received a prescription for an anti-TNF treatment, representing 7,210 patient-years of anti-TNF treatment; most were men and were white. The mean time on treatment was about 2 years, and they had started treatment at a mean age of 57 years. Screening rates for tuberculosis were relatively high and remained stable throughout the study period, at 72% overall, but HBV screening rates were low, at 24% overall. HBV screening was not included in practice guidelines until 2006, and the rate significantly increased from under 10% at the beginning of the period studied to 42% at the end, Dr. Hou noted.
They identified 23 patients with ICD-9 codes related to tuberculosis occurring after they started anti-TNF therapy, but “on chart review, only two patients were confirmed to have tuberculosis reactivation” related to anti-TNF therapy, which occurred at 8 and 18 months of treatment, he said. “Very interestingly, both of these patients had latent tuberculosis and documented completed courses of INH [isonicotinylhydrazine] and a negative chest x-ray prior to [anti-]TNF initiation.” Because the only cases of tuberculosis reactivation occurred in patients with a prior history of latent tuberculosis, “we should maintain extra diligence in those patients even if appropriate screening has been performed,” he advised.
They identified 12 patients with codes related to hepatitis B after the treatment started, two had clinically relevant outcomes, but the chart review indicated that neither case was HPV reactivation. There were two cases of patients with positive HBV tests. One of these patients, who developed acute jaundice with serologies consistent with acute HBV infection, reported a possible exposure to HBV and was newly diagnosed with HIV, associated with the same encounter. This patient was on infliximab and continued treatment, and HBV viremia spontaneously cleared without antiviral treatment, Dr. Hou said.
The second “clinically relevant” case was a patient with chronic HBV infection, identified in a presurgical screen, who was asymptomatic and had normal liver function tests. Infliximab was discontinued and the patient started antiviral therapy; viremia resolved and the patient resumed treatment with infliximab “without complications,” Dr. Hou said.
Another four patients were identified related to codes for acute liver failure, but on chart review, none had liver failure related to hepatitis B.
The study’s limitations include the possibility that patients may receive medical care outside the VA system, which would not be picked up in the analysis, he said, but added, “when we look at our estimate of tuberculosis reactivation, they mirror almost exactly those reported in the rheumatology literature in screened populations.” Another limitation is that the study depended on the accuracy of ICD-9 codes for the diagnoses, but all outcomes were verified in the chart review, he said.
Dr. Hou is also director of Inflammatory Bowel Diseases and an investigator in the clinical epidemiology and outcomes program in the Center for Innovations in Quality Effectiveness and Safety at the Michael E. DeBakey VA Medical Center, Houston.
His financial disclosures include receiving consulting, speaking, teaching, and/or advisory fees from Janssen, Aptalis, and AbbVie.
WASHINGTON – Reactivation of tuberculosis and hepatitis B infections after starting treatment with anti–tumor necrosis factor therapy was “rare” in a large national cohort study of veterans with inflammatory bowel disease, Dr. Jason Hou reported at the annual Digestive Disease Week.
The estimated rate of tuberculosis reactivations was 2.8 per 10,000 patient-years of exposure to anti-TNF therapy “in a fairly well-screened cohort of IBD patients,” said Dr. Hou, codirector of the Inflammatory Bowel Disease Center at Baylor College of Medicine, Houston. The estimate for HBV reactivation or acute liver failure in this cohort was less than 1.4 per 10,000 patient-years of exposure, he noted.
Practice guidelines recommend that patients with IBD should be screened for latent tuberculosis and HBV before starting treatment with an anti-TNF drug, but how often reactivation actually occurs in this population is not known, he pointed out. Moreover, recent studies have questioned the cost-effectiveness of universal screening for HBV before starting treatment, and TB reactivation rates in patients with IBD treated with anti-TNF drugs “have not been assessed on a national population level.”
Dr. Hou and his associates used a national Veterans Affairs database to identify patients who had been diagnosed between 2003 and 2011 with Crohn’s disease or ulcerative colitis, based on ICD-9 codes, and had filled at least one prescription for infliximab, adalimumab, or certolizumab pegol; they also looked for codes related to possible tuberculosis reactivation or acute liver failure related to HBV reactivation at the time of or after anti-TNF therapy was started. Cases were then verified by reviewing electronic medical records of patients to confirm the diagnosis of tuberculosis or HBV, exposure to an anti-TNF drug, and completion of pretreatment screening.
They identified 3,357 patients with IBD who had received a prescription for an anti-TNF treatment, representing 7,210 patient-years of anti-TNF treatment; most were men and were white. The mean time on treatment was about 2 years, and they had started treatment at a mean age of 57 years. Screening rates for tuberculosis were relatively high and remained stable throughout the study period, at 72% overall, but HBV screening rates were low, at 24% overall. HBV screening was not included in practice guidelines until 2006, and the rate significantly increased from under 10% at the beginning of the period studied to 42% at the end, Dr. Hou noted.
They identified 23 patients with ICD-9 codes related to tuberculosis occurring after they started anti-TNF therapy, but “on chart review, only two patients were confirmed to have tuberculosis reactivation” related to anti-TNF therapy, which occurred at 8 and 18 months of treatment, he said. “Very interestingly, both of these patients had latent tuberculosis and documented completed courses of INH [isonicotinylhydrazine] and a negative chest x-ray prior to [anti-]TNF initiation.” Because the only cases of tuberculosis reactivation occurred in patients with a prior history of latent tuberculosis, “we should maintain extra diligence in those patients even if appropriate screening has been performed,” he advised.
They identified 12 patients with codes related to hepatitis B after the treatment started, two had clinically relevant outcomes, but the chart review indicated that neither case was HPV reactivation. There were two cases of patients with positive HBV tests. One of these patients, who developed acute jaundice with serologies consistent with acute HBV infection, reported a possible exposure to HBV and was newly diagnosed with HIV, associated with the same encounter. This patient was on infliximab and continued treatment, and HBV viremia spontaneously cleared without antiviral treatment, Dr. Hou said.
The second “clinically relevant” case was a patient with chronic HBV infection, identified in a presurgical screen, who was asymptomatic and had normal liver function tests. Infliximab was discontinued and the patient started antiviral therapy; viremia resolved and the patient resumed treatment with infliximab “without complications,” Dr. Hou said.
Another four patients were identified related to codes for acute liver failure, but on chart review, none had liver failure related to hepatitis B.
The study’s limitations include the possibility that patients may receive medical care outside the VA system, which would not be picked up in the analysis, he said, but added, “when we look at our estimate of tuberculosis reactivation, they mirror almost exactly those reported in the rheumatology literature in screened populations.” Another limitation is that the study depended on the accuracy of ICD-9 codes for the diagnoses, but all outcomes were verified in the chart review, he said.
Dr. Hou is also director of Inflammatory Bowel Diseases and an investigator in the clinical epidemiology and outcomes program in the Center for Innovations in Quality Effectiveness and Safety at the Michael E. DeBakey VA Medical Center, Houston.
His financial disclosures include receiving consulting, speaking, teaching, and/or advisory fees from Janssen, Aptalis, and AbbVie.
AT DDW 2015
Key clinical point: Significant clinical events related to tuberculosis and hepatitis B virus reactivation after initiating anti–tumor necrosis factor therapy in a screened population are rare.
Major finding: Rates of tuberculosis and HBV were estimated at 2.8 and less than 1.4 cases per 10,000 patient-years of exposure to treatment, respectively, in a large, fairly well screened national cohort of veterans with IBD treated with an anti-TNF drug.
Data source: A retrospective cohort study evaluated the rates of tuberculosis and HBV reactivation, identifying cases of IBD treated with anti-TNF therapy in a Veterans Health Administration database during 2003-2011, confirming cases, treatment, and HBV and TB screening status with electronic medical record review.
Disclosures: Dr. Hou’s financial disclosure includes receiving consulting, speaking, teaching, and/or advisory fees from Janssen, Aptalis, and Abbvie.
The GLUTOX Trial: Getting closer to identifying nonceliac gluten sensitivity
WASHINGTON – A simple dietary challenge may help identify nonceliac gluten sensitivity in patients with gastrointestinal functional disorders, results of the ongoing, randomized GLUTOX trial suggest.
Nonceliac gluten sensitivity (NCGS) is an emergent syndrome that causes mainly gastrointestinal symptoms and has been thought to be present in about 6% of the population. The problem is that there is no established or well-defined diagnostic flow chart to identify these patients, study author Dr. Luca Elli said at the annual Digestive Disease Week.
To determine whether gluten induces symptoms in patients responding positively to a gluten-free diet and identify those potentially affected by NCGS, GLUTOXenrolled 100 adults with functional GI symptoms and placed them on a gluten-free diet for 21 days. Severity of symptoms was measured before and after the diet using a 10-cm visual analogue scale (VAS) and the 36-item Short Form Health Survey (SF-36).
Patients with at least a 3-cm improvement in baseline VAS were then double-blind, randomly assigned to gluten (5.6 g per day) or placebo capsules for 7 days, followed by a 7-day washout period, and then crossed over to another 7-day cycle of gluten or placebo capsules.
At baseline, the mean age was 38 years, 90% of patients were female, 55 had irritable bowel syndrome (IBS), 36 functional dyspepsia, and 9 had other unspecified functional nonspecific gastrointestinal symptoms by ROME III criteria. Patients with celiac disease or a wheat allergy or who were on an ongoing GFD were excluded.
In all, 81 patients reported a symptomatic improvement from baseline after the 21-day gluten-free-diet (mean VAS 7.5 vs. 3.3; P value = .001),Dr. Elli, from Fondazione IRCCS Ca’ Granda, Ospedale Maggiore Policlinico, Milan, Italy, reported in a distinguished abstract plenary session.
“All of the symptoms we found were reduced by the gluten-free diet, but especially patient satisfaction about stool consistency, bloating, and the global satisfaction were improved in an important way,” he said.
Symptom improvements were also associated with significant improvements in the SF-36 physical component summary and mental component summary. Most responders were female (88%), 48 had IBS, 25 dyspepsia, and 8 other.
After the gluten capsule challenge, 25 of the 81 gluten-free diet responders had a severe symptomatic relapse especially in stool consistency satisfaction, bloating, and abdominal pain, Dr. Elli said.
The relapses were also associated with a significant decrease in SF-36 physical and mental component summaries.
No demographic or biochemical parameters were significantly associated with a response to the gluten challenge, Dr. Elli said. Most of those having a response were female (96%), 13 had IBS, 10 dyspepsia, and 2 other.
The sequence of the gluten and placebo capsules also had no effect on the results.
If the data are confirmed, it’s possible the double-blind challenge could be used to select gluten-free diet responders and inserted into the diagnostic flow chart for patients with gastrointestinal functional disorders, Dr. Elli said.
A very important open issue is also the 56% of enrolled subjects who responded to the gluten-free diet, but did not show symptoms with the gluten double-blind challenge, he added.
During a discussion of the results, attendees questioned whether the study design, particularly the failure to biopsy patients for celiac disease at enrollment and the short 7-day washout period, was sufficient to answer the question of identifying patients with NCGS.
Session co-moderatorDr. Bernd Schnabl, from University of California–San Diego, agreed that the study design was not ideal and that the study would have been strengthened by using biopsy to rule out patients with celiac disease. That said, the study represents a start.
“If we can stratify these patients and re-challenge them longer, it could be helpful in identifying a subpopulation of functional patients who might benefit from a gluten-free diet,” he said.
The study was funded by Fondazione IRCCS Ca’ Granda, Ospedale Maggiore Policlinico. Dr. Elli reported consulting fees from and serving on an advisory committee or review panel for the Dr. Schär Institute.
On Twitter @pwendl
WASHINGTON – A simple dietary challenge may help identify nonceliac gluten sensitivity in patients with gastrointestinal functional disorders, results of the ongoing, randomized GLUTOX trial suggest.
Nonceliac gluten sensitivity (NCGS) is an emergent syndrome that causes mainly gastrointestinal symptoms and has been thought to be present in about 6% of the population. The problem is that there is no established or well-defined diagnostic flow chart to identify these patients, study author Dr. Luca Elli said at the annual Digestive Disease Week.
To determine whether gluten induces symptoms in patients responding positively to a gluten-free diet and identify those potentially affected by NCGS, GLUTOXenrolled 100 adults with functional GI symptoms and placed them on a gluten-free diet for 21 days. Severity of symptoms was measured before and after the diet using a 10-cm visual analogue scale (VAS) and the 36-item Short Form Health Survey (SF-36).
Patients with at least a 3-cm improvement in baseline VAS were then double-blind, randomly assigned to gluten (5.6 g per day) or placebo capsules for 7 days, followed by a 7-day washout period, and then crossed over to another 7-day cycle of gluten or placebo capsules.
At baseline, the mean age was 38 years, 90% of patients were female, 55 had irritable bowel syndrome (IBS), 36 functional dyspepsia, and 9 had other unspecified functional nonspecific gastrointestinal symptoms by ROME III criteria. Patients with celiac disease or a wheat allergy or who were on an ongoing GFD were excluded.
In all, 81 patients reported a symptomatic improvement from baseline after the 21-day gluten-free-diet (mean VAS 7.5 vs. 3.3; P value = .001),Dr. Elli, from Fondazione IRCCS Ca’ Granda, Ospedale Maggiore Policlinico, Milan, Italy, reported in a distinguished abstract plenary session.
“All of the symptoms we found were reduced by the gluten-free diet, but especially patient satisfaction about stool consistency, bloating, and the global satisfaction were improved in an important way,” he said.
Symptom improvements were also associated with significant improvements in the SF-36 physical component summary and mental component summary. Most responders were female (88%), 48 had IBS, 25 dyspepsia, and 8 other.
After the gluten capsule challenge, 25 of the 81 gluten-free diet responders had a severe symptomatic relapse especially in stool consistency satisfaction, bloating, and abdominal pain, Dr. Elli said.
The relapses were also associated with a significant decrease in SF-36 physical and mental component summaries.
No demographic or biochemical parameters were significantly associated with a response to the gluten challenge, Dr. Elli said. Most of those having a response were female (96%), 13 had IBS, 10 dyspepsia, and 2 other.
The sequence of the gluten and placebo capsules also had no effect on the results.
If the data are confirmed, it’s possible the double-blind challenge could be used to select gluten-free diet responders and inserted into the diagnostic flow chart for patients with gastrointestinal functional disorders, Dr. Elli said.
A very important open issue is also the 56% of enrolled subjects who responded to the gluten-free diet, but did not show symptoms with the gluten double-blind challenge, he added.
During a discussion of the results, attendees questioned whether the study design, particularly the failure to biopsy patients for celiac disease at enrollment and the short 7-day washout period, was sufficient to answer the question of identifying patients with NCGS.
Session co-moderatorDr. Bernd Schnabl, from University of California–San Diego, agreed that the study design was not ideal and that the study would have been strengthened by using biopsy to rule out patients with celiac disease. That said, the study represents a start.
“If we can stratify these patients and re-challenge them longer, it could be helpful in identifying a subpopulation of functional patients who might benefit from a gluten-free diet,” he said.
The study was funded by Fondazione IRCCS Ca’ Granda, Ospedale Maggiore Policlinico. Dr. Elli reported consulting fees from and serving on an advisory committee or review panel for the Dr. Schär Institute.
On Twitter @pwendl
WASHINGTON – A simple dietary challenge may help identify nonceliac gluten sensitivity in patients with gastrointestinal functional disorders, results of the ongoing, randomized GLUTOX trial suggest.
Nonceliac gluten sensitivity (NCGS) is an emergent syndrome that causes mainly gastrointestinal symptoms and has been thought to be present in about 6% of the population. The problem is that there is no established or well-defined diagnostic flow chart to identify these patients, study author Dr. Luca Elli said at the annual Digestive Disease Week.
To determine whether gluten induces symptoms in patients responding positively to a gluten-free diet and identify those potentially affected by NCGS, GLUTOXenrolled 100 adults with functional GI symptoms and placed them on a gluten-free diet for 21 days. Severity of symptoms was measured before and after the diet using a 10-cm visual analogue scale (VAS) and the 36-item Short Form Health Survey (SF-36).
Patients with at least a 3-cm improvement in baseline VAS were then double-blind, randomly assigned to gluten (5.6 g per day) or placebo capsules for 7 days, followed by a 7-day washout period, and then crossed over to another 7-day cycle of gluten or placebo capsules.
At baseline, the mean age was 38 years, 90% of patients were female, 55 had irritable bowel syndrome (IBS), 36 functional dyspepsia, and 9 had other unspecified functional nonspecific gastrointestinal symptoms by ROME III criteria. Patients with celiac disease or a wheat allergy or who were on an ongoing GFD were excluded.
In all, 81 patients reported a symptomatic improvement from baseline after the 21-day gluten-free-diet (mean VAS 7.5 vs. 3.3; P value = .001),Dr. Elli, from Fondazione IRCCS Ca’ Granda, Ospedale Maggiore Policlinico, Milan, Italy, reported in a distinguished abstract plenary session.
“All of the symptoms we found were reduced by the gluten-free diet, but especially patient satisfaction about stool consistency, bloating, and the global satisfaction were improved in an important way,” he said.
Symptom improvements were also associated with significant improvements in the SF-36 physical component summary and mental component summary. Most responders were female (88%), 48 had IBS, 25 dyspepsia, and 8 other.
After the gluten capsule challenge, 25 of the 81 gluten-free diet responders had a severe symptomatic relapse especially in stool consistency satisfaction, bloating, and abdominal pain, Dr. Elli said.
The relapses were also associated with a significant decrease in SF-36 physical and mental component summaries.
No demographic or biochemical parameters were significantly associated with a response to the gluten challenge, Dr. Elli said. Most of those having a response were female (96%), 13 had IBS, 10 dyspepsia, and 2 other.
The sequence of the gluten and placebo capsules also had no effect on the results.
If the data are confirmed, it’s possible the double-blind challenge could be used to select gluten-free diet responders and inserted into the diagnostic flow chart for patients with gastrointestinal functional disorders, Dr. Elli said.
A very important open issue is also the 56% of enrolled subjects who responded to the gluten-free diet, but did not show symptoms with the gluten double-blind challenge, he added.
During a discussion of the results, attendees questioned whether the study design, particularly the failure to biopsy patients for celiac disease at enrollment and the short 7-day washout period, was sufficient to answer the question of identifying patients with NCGS.
Session co-moderatorDr. Bernd Schnabl, from University of California–San Diego, agreed that the study design was not ideal and that the study would have been strengthened by using biopsy to rule out patients with celiac disease. That said, the study represents a start.
“If we can stratify these patients and re-challenge them longer, it could be helpful in identifying a subpopulation of functional patients who might benefit from a gluten-free diet,” he said.
The study was funded by Fondazione IRCCS Ca’ Granda, Ospedale Maggiore Policlinico. Dr. Elli reported consulting fees from and serving on an advisory committee or review panel for the Dr. Schär Institute.
On Twitter @pwendl
AT DDW 2015
Key clinical point: A randomized, double-blind dietary challenge may be useful in identifying nonceliac gluten sensitivity.
Major finding: More than 30% of patients with functional gastrointestinal disorders were classified as possibly having nonceliac gluten sensitivity.
Data source: Randomized, double-blind study in 100 patients with suspected nonceliac gluten sensitivity.
Disclosures: The study was funded by Fondazione IRCCS Ca’ Granda, Ospedale Maggiore Policlinico. Dr. Elli reported consulting fees from and serving on an advisory committee or review panel for the Dr. Schär Institute.