User login
Digestive Disease Week (DDW 2015)
Colon cancer, colonoscopy, and intestinal issues
Hereditary syndromes in gastroenterology have emerged from being esoteric to being common issues that all of us must deal with, according to Dr. Sapna Syngal of Dana-Farber/Brigham and Women’s Cancer Center, Boston. Screening, surveillance, and treatment of hereditary cancers are all different, compared with sporadic cancer. For colorectal cancers, an excellent resource is http://www.nccn.org/professionals/physician_gls/pdf/genetics_colon.pdf, and there are recent society summaries (Am. J. Gastroenterol. 2015;110:223-62). These recommend a family history of cancer be recorded for all patients, including type of cancer, age at diagnosis, and relationship to patient. Lynch syndrome testing should now be done on all newly diagnosed colorectal cancers by testing of mismatch repair proteins or microsatellite instability. Genetic testing should be done when these are detected and on all family members of affected individuals. Familial adenomatous polyposis testing, including the APC and MUTYH genes, should be done for individuals with more than 10 cumulative adenomas, or a family history of any familial adenomatous condition. Peutz-Jeghers syndrome should be tested for in individuals with perioral/buccal pigmentation or those with two or more hamartomatous polyps. Juvenile polyposis syndrome should be tested for in individuals with five or more juvenile polyps in the colorectum or any juvenile polyps in other parts of the GI tract. Simple clinical questions can help identify those who should be tested (Am. J. Gastroenterol. 2009;104:1508-18).
Modern evidence has refuted several long-held beliefs about diverticulosis and diverticulitis, said Dr. Neil Stollman of the University of California, San Francisco. Evidence now shows that diverticulosis is not associated with a low-fiber diet and that high-fiber diets are associated with higher rates of diverticular complications, although this may be due to confounding. Nonsteroidal anti-inflammatory drugs are associated with increased risk of diverticular bleeding. The risk of diverticulitis is much lower than previously thought. Prior estimates of 10%-25% have now been revised downward to 1%-4%. Nuts and seeds do not cause acute diverticulitis and do not need to be avoided. Diverticulitis is a spectrum of diseases from asymptomatic to symptomatic uncomplicated diverticular disease (SUDD) to acute diverticulitis. Mesalamine may be effective in SUDD and acute diverticulitis but evidence is mixed. Cyclic rifaximin and probiotics may also be helpful in SUDD. Antibiotics, previously thought to be mandatory in acute diverticulitis, have not been clearly beneficial in large randomized trials. Surgery, which was also previously recommended after a second attack of acute diverticulitis, is now considered optional and should be individualized.
Dr. Douglas K. Rex of Indiana University Health, Indianapolis, reviewed key measures of quality in colonoscopy and how to achieve these, even under difficult circumstances. Key measures include adenoma detection rate, which can be improved through careful attention to good technique (looking behind folds, adequate distention, and washing) and recognition of flat and sessile polyps. New technologies include high definition, special endoscope caps that flatten folds, and new wide-angle colonoscopes. Water immersion and CO2 insufflation have also improved quality through easier insertion and less gas distention and pain after the procedure. For removal of large, lateral spreading polyps, the technique of endoscopic mucosal resection has been highly effective. Use of a “bulking agent” for submucosal injection such as hydroxyethyl starch, injectable contrast agent, underwater endoscopic mucosal resection, and avulsion (with cold or hot forceps) of fibrotic/scarred polyps have all been demonstrated to be effective in expert hands.
Dr. Charlene M. Prather of Saint Louis University summarized the increasing prevalence of constipation and reviewed risk factors (decreased activity, low fiber consumption, and use of multiple constipating medications). Constipation can be divided into three types: normal transit, slow transit, and pelvic floor dysfunction (PFD). Physical exam, particularly a high-quality rectal exam, can be very effective with high negative predictive value for PFD. Treatment includes fiber supplementation (most effective for mild/moderate constipation, less helpful in slow transit or PFD), laxatives (best data are for osmotic laxatives and bisacodyl), and newer agents that stimulate chloride secretion. Testing is appropriate for refractory constipation and includes transit time studies, balloon expulsion, and anorectal manometry.
Dr. Brennan Spiegel of the Cedars-Sinai Center for Outcomes Research and Education, Los Angeles, provided a summary of current national efforts to measure, report, and improve quality in gastroenterology. He highlighted several reports of high variability in quality such as adenoma detection, testing in patients with uncomplicated inflammatory bowel disease, and approaches to diagnosis of irritable bowel syndrome. A general approach to achieving quality was outlined, including: 1. standardization, 2. measurement, 3. reporting, 4. incentivizing (getting paid for performance), and 5. improving. U.S. Medicare oversight groups (PQRS) have chosen four general areas of quality (polyp surveillance, gastroesophageal reflux disease, hepatitis C, and IBD) measures. Gastroenterology societies have provided effective tools to measure and report these, including GIQUIC and the AGA Digestive Health Recognition Program.
Dr. Wallace is professor of medicine and director, digestive diseases research program, Mayo Clinic, Jacksonville, Fla. He has received grants from BSCI and Cosmo and has consulted for Olympus and iLumen. This is a summary provided by the moderator of one of the spring postgraduate course sessions held at DDW 2015.
Hereditary syndromes in gastroenterology have emerged from being esoteric to being common issues that all of us must deal with, according to Dr. Sapna Syngal of Dana-Farber/Brigham and Women’s Cancer Center, Boston. Screening, surveillance, and treatment of hereditary cancers are all different, compared with sporadic cancer. For colorectal cancers, an excellent resource is http://www.nccn.org/professionals/physician_gls/pdf/genetics_colon.pdf, and there are recent society summaries (Am. J. Gastroenterol. 2015;110:223-62). These recommend a family history of cancer be recorded for all patients, including type of cancer, age at diagnosis, and relationship to patient. Lynch syndrome testing should now be done on all newly diagnosed colorectal cancers by testing of mismatch repair proteins or microsatellite instability. Genetic testing should be done when these are detected and on all family members of affected individuals. Familial adenomatous polyposis testing, including the APC and MUTYH genes, should be done for individuals with more than 10 cumulative adenomas, or a family history of any familial adenomatous condition. Peutz-Jeghers syndrome should be tested for in individuals with perioral/buccal pigmentation or those with two or more hamartomatous polyps. Juvenile polyposis syndrome should be tested for in individuals with five or more juvenile polyps in the colorectum or any juvenile polyps in other parts of the GI tract. Simple clinical questions can help identify those who should be tested (Am. J. Gastroenterol. 2009;104:1508-18).
Modern evidence has refuted several long-held beliefs about diverticulosis and diverticulitis, said Dr. Neil Stollman of the University of California, San Francisco. Evidence now shows that diverticulosis is not associated with a low-fiber diet and that high-fiber diets are associated with higher rates of diverticular complications, although this may be due to confounding. Nonsteroidal anti-inflammatory drugs are associated with increased risk of diverticular bleeding. The risk of diverticulitis is much lower than previously thought. Prior estimates of 10%-25% have now been revised downward to 1%-4%. Nuts and seeds do not cause acute diverticulitis and do not need to be avoided. Diverticulitis is a spectrum of diseases from asymptomatic to symptomatic uncomplicated diverticular disease (SUDD) to acute diverticulitis. Mesalamine may be effective in SUDD and acute diverticulitis but evidence is mixed. Cyclic rifaximin and probiotics may also be helpful in SUDD. Antibiotics, previously thought to be mandatory in acute diverticulitis, have not been clearly beneficial in large randomized trials. Surgery, which was also previously recommended after a second attack of acute diverticulitis, is now considered optional and should be individualized.
Dr. Douglas K. Rex of Indiana University Health, Indianapolis, reviewed key measures of quality in colonoscopy and how to achieve these, even under difficult circumstances. Key measures include adenoma detection rate, which can be improved through careful attention to good technique (looking behind folds, adequate distention, and washing) and recognition of flat and sessile polyps. New technologies include high definition, special endoscope caps that flatten folds, and new wide-angle colonoscopes. Water immersion and CO2 insufflation have also improved quality through easier insertion and less gas distention and pain after the procedure. For removal of large, lateral spreading polyps, the technique of endoscopic mucosal resection has been highly effective. Use of a “bulking agent” for submucosal injection such as hydroxyethyl starch, injectable contrast agent, underwater endoscopic mucosal resection, and avulsion (with cold or hot forceps) of fibrotic/scarred polyps have all been demonstrated to be effective in expert hands.
Dr. Charlene M. Prather of Saint Louis University summarized the increasing prevalence of constipation and reviewed risk factors (decreased activity, low fiber consumption, and use of multiple constipating medications). Constipation can be divided into three types: normal transit, slow transit, and pelvic floor dysfunction (PFD). Physical exam, particularly a high-quality rectal exam, can be very effective with high negative predictive value for PFD. Treatment includes fiber supplementation (most effective for mild/moderate constipation, less helpful in slow transit or PFD), laxatives (best data are for osmotic laxatives and bisacodyl), and newer agents that stimulate chloride secretion. Testing is appropriate for refractory constipation and includes transit time studies, balloon expulsion, and anorectal manometry.
Dr. Brennan Spiegel of the Cedars-Sinai Center for Outcomes Research and Education, Los Angeles, provided a summary of current national efforts to measure, report, and improve quality in gastroenterology. He highlighted several reports of high variability in quality such as adenoma detection, testing in patients with uncomplicated inflammatory bowel disease, and approaches to diagnosis of irritable bowel syndrome. A general approach to achieving quality was outlined, including: 1. standardization, 2. measurement, 3. reporting, 4. incentivizing (getting paid for performance), and 5. improving. U.S. Medicare oversight groups (PQRS) have chosen four general areas of quality (polyp surveillance, gastroesophageal reflux disease, hepatitis C, and IBD) measures. Gastroenterology societies have provided effective tools to measure and report these, including GIQUIC and the AGA Digestive Health Recognition Program.
Dr. Wallace is professor of medicine and director, digestive diseases research program, Mayo Clinic, Jacksonville, Fla. He has received grants from BSCI and Cosmo and has consulted for Olympus and iLumen. This is a summary provided by the moderator of one of the spring postgraduate course sessions held at DDW 2015.
Hereditary syndromes in gastroenterology have emerged from being esoteric to being common issues that all of us must deal with, according to Dr. Sapna Syngal of Dana-Farber/Brigham and Women’s Cancer Center, Boston. Screening, surveillance, and treatment of hereditary cancers are all different, compared with sporadic cancer. For colorectal cancers, an excellent resource is http://www.nccn.org/professionals/physician_gls/pdf/genetics_colon.pdf, and there are recent society summaries (Am. J. Gastroenterol. 2015;110:223-62). These recommend a family history of cancer be recorded for all patients, including type of cancer, age at diagnosis, and relationship to patient. Lynch syndrome testing should now be done on all newly diagnosed colorectal cancers by testing of mismatch repair proteins or microsatellite instability. Genetic testing should be done when these are detected and on all family members of affected individuals. Familial adenomatous polyposis testing, including the APC and MUTYH genes, should be done for individuals with more than 10 cumulative adenomas, or a family history of any familial adenomatous condition. Peutz-Jeghers syndrome should be tested for in individuals with perioral/buccal pigmentation or those with two or more hamartomatous polyps. Juvenile polyposis syndrome should be tested for in individuals with five or more juvenile polyps in the colorectum or any juvenile polyps in other parts of the GI tract. Simple clinical questions can help identify those who should be tested (Am. J. Gastroenterol. 2009;104:1508-18).
Modern evidence has refuted several long-held beliefs about diverticulosis and diverticulitis, said Dr. Neil Stollman of the University of California, San Francisco. Evidence now shows that diverticulosis is not associated with a low-fiber diet and that high-fiber diets are associated with higher rates of diverticular complications, although this may be due to confounding. Nonsteroidal anti-inflammatory drugs are associated with increased risk of diverticular bleeding. The risk of diverticulitis is much lower than previously thought. Prior estimates of 10%-25% have now been revised downward to 1%-4%. Nuts and seeds do not cause acute diverticulitis and do not need to be avoided. Diverticulitis is a spectrum of diseases from asymptomatic to symptomatic uncomplicated diverticular disease (SUDD) to acute diverticulitis. Mesalamine may be effective in SUDD and acute diverticulitis but evidence is mixed. Cyclic rifaximin and probiotics may also be helpful in SUDD. Antibiotics, previously thought to be mandatory in acute diverticulitis, have not been clearly beneficial in large randomized trials. Surgery, which was also previously recommended after a second attack of acute diverticulitis, is now considered optional and should be individualized.
Dr. Douglas K. Rex of Indiana University Health, Indianapolis, reviewed key measures of quality in colonoscopy and how to achieve these, even under difficult circumstances. Key measures include adenoma detection rate, which can be improved through careful attention to good technique (looking behind folds, adequate distention, and washing) and recognition of flat and sessile polyps. New technologies include high definition, special endoscope caps that flatten folds, and new wide-angle colonoscopes. Water immersion and CO2 insufflation have also improved quality through easier insertion and less gas distention and pain after the procedure. For removal of large, lateral spreading polyps, the technique of endoscopic mucosal resection has been highly effective. Use of a “bulking agent” for submucosal injection such as hydroxyethyl starch, injectable contrast agent, underwater endoscopic mucosal resection, and avulsion (with cold or hot forceps) of fibrotic/scarred polyps have all been demonstrated to be effective in expert hands.
Dr. Charlene M. Prather of Saint Louis University summarized the increasing prevalence of constipation and reviewed risk factors (decreased activity, low fiber consumption, and use of multiple constipating medications). Constipation can be divided into three types: normal transit, slow transit, and pelvic floor dysfunction (PFD). Physical exam, particularly a high-quality rectal exam, can be very effective with high negative predictive value for PFD. Treatment includes fiber supplementation (most effective for mild/moderate constipation, less helpful in slow transit or PFD), laxatives (best data are for osmotic laxatives and bisacodyl), and newer agents that stimulate chloride secretion. Testing is appropriate for refractory constipation and includes transit time studies, balloon expulsion, and anorectal manometry.
Dr. Brennan Spiegel of the Cedars-Sinai Center for Outcomes Research and Education, Los Angeles, provided a summary of current national efforts to measure, report, and improve quality in gastroenterology. He highlighted several reports of high variability in quality such as adenoma detection, testing in patients with uncomplicated inflammatory bowel disease, and approaches to diagnosis of irritable bowel syndrome. A general approach to achieving quality was outlined, including: 1. standardization, 2. measurement, 3. reporting, 4. incentivizing (getting paid for performance), and 5. improving. U.S. Medicare oversight groups (PQRS) have chosen four general areas of quality (polyp surveillance, gastroesophageal reflux disease, hepatitis C, and IBD) measures. Gastroenterology societies have provided effective tools to measure and report these, including GIQUIC and the AGA Digestive Health Recognition Program.
Dr. Wallace is professor of medicine and director, digestive diseases research program, Mayo Clinic, Jacksonville, Fla. He has received grants from BSCI and Cosmo and has consulted for Olympus and iLumen. This is a summary provided by the moderator of one of the spring postgraduate course sessions held at DDW 2015.
Upper GI tract
This year’s session on esophagus/upper GI at the AGA Spring Postgraduate Course was packed with pragmatic, useful information for the evaluation of patients with upper GI disorders. The session began with a talk on the manifestations of extraesophageal reflux disease. The take-home message of this talk was that putative extraesophageal manifestations of gastroesophageal reflux disease rarely respond to high-dose therapy with PPIs (proton-pump inhibitors), in the absence of concurrent esophageal symptoms such as heartburn or regurgitation. In such situations, investigation of other etiologies of patients’ symptoms, including occult postnasal drainage or cough-variant asthma, may be more rewarding than escalating anti-acid therapy.
Dr. John E. Pandolfino, AGAF, of Northwestern University, Chicago, discussed the utilization of high-resolution manometry in the evaluation of dysphagia. A central focus of this discussion was the use of the Chicago classification of motility abnormalities in assessing these patients. In the future, it is likely that the care of these patients will be dictated by the type of abnormality the patient has in this classification scheme. Especially in the setting of achalasia, data are emerging that some subtypes of achalasia are less likely to respond to some therapies. For instance, type 3 achalasia is unlikely to respond to pneumatic balloon dilatation.
Dr. Rhonda Souza of the University of Texas Southwestern Medical Center, Dallas, taught us that a diagnosis of eosinophilic esophagitis requires an 8-week trial of PPI therapy with no resolution of the eosinophilia. Esophageal dilation is generally safe in the setting of a dominant stricture, but it can be delayed prior to medical therapy if the patient is tolerating oral intake well. Although the most commonly used therapies for EoE now involve either swallowed steroids or dietary elimination therapy, several new agents are on the horizon that may give us new treatment options.
Finally, Dr. Amitabh Chak of Case Western Reserve University, Cleveland, reviewed the care of patients with Barrett’s esophagus and low-grade dysplasia. This is an especially difficult group of patients to care for, due in part to the low reproducibility in the diagnosis of low-grade dysplasia, as well as the highly variable reported cancer outcomes in this patient population. Level 1 evidence now exists demonstrating that treatment with radiofrequency ablation decreases the incidence of cancer in patients with low-grade dysplasia, but most patients with this finding will not progress. Therefore, the field would benefit from better risk stratification of these patients.
Dr. Shaheen is professor of medicine and epidemiology and chief of the division of gastroenterology & hepatology, University of North Carolina School of Medicine, Chapel Hill. This is a summary provided by the moderator of one of the spring postgraduate course sessions held at DDW 2015.
This year’s session on esophagus/upper GI at the AGA Spring Postgraduate Course was packed with pragmatic, useful information for the evaluation of patients with upper GI disorders. The session began with a talk on the manifestations of extraesophageal reflux disease. The take-home message of this talk was that putative extraesophageal manifestations of gastroesophageal reflux disease rarely respond to high-dose therapy with PPIs (proton-pump inhibitors), in the absence of concurrent esophageal symptoms such as heartburn or regurgitation. In such situations, investigation of other etiologies of patients’ symptoms, including occult postnasal drainage or cough-variant asthma, may be more rewarding than escalating anti-acid therapy.
Dr. John E. Pandolfino, AGAF, of Northwestern University, Chicago, discussed the utilization of high-resolution manometry in the evaluation of dysphagia. A central focus of this discussion was the use of the Chicago classification of motility abnormalities in assessing these patients. In the future, it is likely that the care of these patients will be dictated by the type of abnormality the patient has in this classification scheme. Especially in the setting of achalasia, data are emerging that some subtypes of achalasia are less likely to respond to some therapies. For instance, type 3 achalasia is unlikely to respond to pneumatic balloon dilatation.
Dr. Rhonda Souza of the University of Texas Southwestern Medical Center, Dallas, taught us that a diagnosis of eosinophilic esophagitis requires an 8-week trial of PPI therapy with no resolution of the eosinophilia. Esophageal dilation is generally safe in the setting of a dominant stricture, but it can be delayed prior to medical therapy if the patient is tolerating oral intake well. Although the most commonly used therapies for EoE now involve either swallowed steroids or dietary elimination therapy, several new agents are on the horizon that may give us new treatment options.
Finally, Dr. Amitabh Chak of Case Western Reserve University, Cleveland, reviewed the care of patients with Barrett’s esophagus and low-grade dysplasia. This is an especially difficult group of patients to care for, due in part to the low reproducibility in the diagnosis of low-grade dysplasia, as well as the highly variable reported cancer outcomes in this patient population. Level 1 evidence now exists demonstrating that treatment with radiofrequency ablation decreases the incidence of cancer in patients with low-grade dysplasia, but most patients with this finding will not progress. Therefore, the field would benefit from better risk stratification of these patients.
Dr. Shaheen is professor of medicine and epidemiology and chief of the division of gastroenterology & hepatology, University of North Carolina School of Medicine, Chapel Hill. This is a summary provided by the moderator of one of the spring postgraduate course sessions held at DDW 2015.
This year’s session on esophagus/upper GI at the AGA Spring Postgraduate Course was packed with pragmatic, useful information for the evaluation of patients with upper GI disorders. The session began with a talk on the manifestations of extraesophageal reflux disease. The take-home message of this talk was that putative extraesophageal manifestations of gastroesophageal reflux disease rarely respond to high-dose therapy with PPIs (proton-pump inhibitors), in the absence of concurrent esophageal symptoms such as heartburn or regurgitation. In such situations, investigation of other etiologies of patients’ symptoms, including occult postnasal drainage or cough-variant asthma, may be more rewarding than escalating anti-acid therapy.
Dr. John E. Pandolfino, AGAF, of Northwestern University, Chicago, discussed the utilization of high-resolution manometry in the evaluation of dysphagia. A central focus of this discussion was the use of the Chicago classification of motility abnormalities in assessing these patients. In the future, it is likely that the care of these patients will be dictated by the type of abnormality the patient has in this classification scheme. Especially in the setting of achalasia, data are emerging that some subtypes of achalasia are less likely to respond to some therapies. For instance, type 3 achalasia is unlikely to respond to pneumatic balloon dilatation.
Dr. Rhonda Souza of the University of Texas Southwestern Medical Center, Dallas, taught us that a diagnosis of eosinophilic esophagitis requires an 8-week trial of PPI therapy with no resolution of the eosinophilia. Esophageal dilation is generally safe in the setting of a dominant stricture, but it can be delayed prior to medical therapy if the patient is tolerating oral intake well. Although the most commonly used therapies for EoE now involve either swallowed steroids or dietary elimination therapy, several new agents are on the horizon that may give us new treatment options.
Finally, Dr. Amitabh Chak of Case Western Reserve University, Cleveland, reviewed the care of patients with Barrett’s esophagus and low-grade dysplasia. This is an especially difficult group of patients to care for, due in part to the low reproducibility in the diagnosis of low-grade dysplasia, as well as the highly variable reported cancer outcomes in this patient population. Level 1 evidence now exists demonstrating that treatment with radiofrequency ablation decreases the incidence of cancer in patients with low-grade dysplasia, but most patients with this finding will not progress. Therefore, the field would benefit from better risk stratification of these patients.
Dr. Shaheen is professor of medicine and epidemiology and chief of the division of gastroenterology & hepatology, University of North Carolina School of Medicine, Chapel Hill. This is a summary provided by the moderator of one of the spring postgraduate course sessions held at DDW 2015.
Liver and functional GI issues
Dr. Lin Chang at the University of California, Los Angeles, discussed how to work-up and manage functional abdominal pain. She reviewed a diagnostic algorithm that is evidence based and uses characteristics of the abdominal pain, coexisting warning signs, and a diagnostic work-up. A patient must be diagnosed with functional abdominal pain only after careful medical history, physical examination, and adequate consideration of competing etiologies.
Physical examination can be helpful in differentiating abdominal wall pain from that of visceral pain (Carnett’s sign) although some patients with functional abdominal pain may exhibit positive Carnett’s sign. Managing a patient with suspected functional abdominal pain includes careful attention to warning signs for organic disease (for example, unintended weight loss, hematochezia, abnormal labs, fever, or family history of serious GI disorders), avoiding unnecessary diagnostic testing, consideration of mental health consultation and pharmacotherapy as appropriate.
Dr. Chang reviewed the role of various pharmacologic agents for irritable bowel syndrome (IBS) with diarrhea (alosetron, rifaximin, and loperamide), IBS with constipation (linaclotide, lubiprostone, and polyethylene glycol) and agents such antispasmodics, tricyclic antidepressants, and SSRIs (reviewed extensively in the AGA Technical Review and Guidelines for Pharmacotherapy for IBS published in Gastroenterology. 2014 Nov;147[5]:1149-72.e2). It is important to establish a strong patient-provider relationship and to incorporate behavioral therapies into management of patients with recurrent or chronic functional abdominal pain.
Dr. Peter Gibson at Monash University in Melbourne discussed non–celiac gluten sensitivity and low-FODMAP diet in managing food sensitivity and functional bowel disorders. He pointed out that recent dietary strategies have changed from patient-initiated, whole-food strategies to avoiding specific dietary components such as FODMAPs and gluten and wheat products. FODMAPS (fermentable oligo-, di-, and monosaccharides and polyols) are foods that are generally high in fructose, lactose, oligosaccharides (e.g., beans, onions, garlic, complex carbohydrates) and polyols (e.g., mushrooms). FODMAPs are generally osmotic and lead to fermentation and diarrhea, bloating, and flatulence. General principles in offering a low-FODMAP diet are the selection of appropriate patients; correct education about FODMAP diets, preferably by a trained dietitian; and a step-down approach in which a strict diet is slowly liberalized. Dr. Gibson pointed out that there are a subset of IBS patients who are gluten sensitive but recent data suggest that wheat protein sensitivity may not be as common as it has been suggested and, in fact, FODMAPs may indeed be the major inducers of symptoms in individuals with supposed wheat intolerance. The potential risks of dietary manipulation such as creation of a dietary cripple or induction of an eating disorder should be kept in mind.
Dr. Anna Mae Diehl at Duke University Medical Center in Durham, N.C., spoke about the diagnosis, role of the microbiome, and the treatment of nonalcoholic fatty liver disease (NAFLD). It was pointed out that most patients with NAFLD have benign progression although individuals with nonalcoholic steatohepatitis (NASH), especially those with significant fibrosis, are at risk for developing cirrhosis, liver failure, and liver cancer. Therapeutic investigations undertaken to date have not sufficiently focused on improving fibrosis although several ongoing clinical trials are directed at this goal. Gut microbiome might be a new NAFLD diagnostic/therapeutic target because several recent animal studies have shown that gut microbiome may play a role in conferring susceptibility to liver injury, fibrosis, and cancer.
Dr. Lawrence J. Brandt at Albert Einstein College of Medicine, New York, gave an update on fecal microbiota therapy (FMT). He highlighted that FMT has historic roots going back to the 4th century when Ge Hong described use of human fecal suspension to treat food poisoning or severe diarrhea. He made it clear that FMT should be offered only to those with recurrent Clostridium difficile infections (CDI), meeting selected criteria such as severe illness and prior treatment failures. The protocol for FMT in recurrent CDI includes careful selection of donor (may range from any healthy person, universal donor, or stool-bank product) and testing stool and blood of potential donors for any transmittable agents. A recent systematic review showed that the success rate for FMT in individuals with CDI is generally quite high (greater than 80%) but it may depend on the site of FMT – for example, if FMT is administered to duodenum/jejunum, the success rate is 86%, whereas if it is delivered to right colon/cecum, then the success rate can be as high as 93%. He highlighted the efficacy of FMT in severe, complicated CDI, which generally carries high morbidity and mortality. Practitioners offering FMT should carefully review the FDA guidance that was issued in March 2014. He noted that long-term consequences of FMT are not well understood and thus, risks versus benefits of FMT on a patient-by-patient basis must be carefully weighed.
Dr. Naga P. Chalasani is the David W. Crabb Professor and director of the division of gastroenterology and hepatology, Indiana University, Indianapolis. He has consulting agreements and receives research support from several pharmaceutical companies but none represent a conflict of interest for this activity.
This is a summary provided by the moderator of one of the spring postgraduate course sessions held at DDW 2015.
Dr. Lin Chang at the University of California, Los Angeles, discussed how to work-up and manage functional abdominal pain. She reviewed a diagnostic algorithm that is evidence based and uses characteristics of the abdominal pain, coexisting warning signs, and a diagnostic work-up. A patient must be diagnosed with functional abdominal pain only after careful medical history, physical examination, and adequate consideration of competing etiologies.
Physical examination can be helpful in differentiating abdominal wall pain from that of visceral pain (Carnett’s sign) although some patients with functional abdominal pain may exhibit positive Carnett’s sign. Managing a patient with suspected functional abdominal pain includes careful attention to warning signs for organic disease (for example, unintended weight loss, hematochezia, abnormal labs, fever, or family history of serious GI disorders), avoiding unnecessary diagnostic testing, consideration of mental health consultation and pharmacotherapy as appropriate.
Dr. Chang reviewed the role of various pharmacologic agents for irritable bowel syndrome (IBS) with diarrhea (alosetron, rifaximin, and loperamide), IBS with constipation (linaclotide, lubiprostone, and polyethylene glycol) and agents such antispasmodics, tricyclic antidepressants, and SSRIs (reviewed extensively in the AGA Technical Review and Guidelines for Pharmacotherapy for IBS published in Gastroenterology. 2014 Nov;147[5]:1149-72.e2). It is important to establish a strong patient-provider relationship and to incorporate behavioral therapies into management of patients with recurrent or chronic functional abdominal pain.
Dr. Peter Gibson at Monash University in Melbourne discussed non–celiac gluten sensitivity and low-FODMAP diet in managing food sensitivity and functional bowel disorders. He pointed out that recent dietary strategies have changed from patient-initiated, whole-food strategies to avoiding specific dietary components such as FODMAPs and gluten and wheat products. FODMAPS (fermentable oligo-, di-, and monosaccharides and polyols) are foods that are generally high in fructose, lactose, oligosaccharides (e.g., beans, onions, garlic, complex carbohydrates) and polyols (e.g., mushrooms). FODMAPs are generally osmotic and lead to fermentation and diarrhea, bloating, and flatulence. General principles in offering a low-FODMAP diet are the selection of appropriate patients; correct education about FODMAP diets, preferably by a trained dietitian; and a step-down approach in which a strict diet is slowly liberalized. Dr. Gibson pointed out that there are a subset of IBS patients who are gluten sensitive but recent data suggest that wheat protein sensitivity may not be as common as it has been suggested and, in fact, FODMAPs may indeed be the major inducers of symptoms in individuals with supposed wheat intolerance. The potential risks of dietary manipulation such as creation of a dietary cripple or induction of an eating disorder should be kept in mind.
Dr. Anna Mae Diehl at Duke University Medical Center in Durham, N.C., spoke about the diagnosis, role of the microbiome, and the treatment of nonalcoholic fatty liver disease (NAFLD). It was pointed out that most patients with NAFLD have benign progression although individuals with nonalcoholic steatohepatitis (NASH), especially those with significant fibrosis, are at risk for developing cirrhosis, liver failure, and liver cancer. Therapeutic investigations undertaken to date have not sufficiently focused on improving fibrosis although several ongoing clinical trials are directed at this goal. Gut microbiome might be a new NAFLD diagnostic/therapeutic target because several recent animal studies have shown that gut microbiome may play a role in conferring susceptibility to liver injury, fibrosis, and cancer.
Dr. Lawrence J. Brandt at Albert Einstein College of Medicine, New York, gave an update on fecal microbiota therapy (FMT). He highlighted that FMT has historic roots going back to the 4th century when Ge Hong described use of human fecal suspension to treat food poisoning or severe diarrhea. He made it clear that FMT should be offered only to those with recurrent Clostridium difficile infections (CDI), meeting selected criteria such as severe illness and prior treatment failures. The protocol for FMT in recurrent CDI includes careful selection of donor (may range from any healthy person, universal donor, or stool-bank product) and testing stool and blood of potential donors for any transmittable agents. A recent systematic review showed that the success rate for FMT in individuals with CDI is generally quite high (greater than 80%) but it may depend on the site of FMT – for example, if FMT is administered to duodenum/jejunum, the success rate is 86%, whereas if it is delivered to right colon/cecum, then the success rate can be as high as 93%. He highlighted the efficacy of FMT in severe, complicated CDI, which generally carries high morbidity and mortality. Practitioners offering FMT should carefully review the FDA guidance that was issued in March 2014. He noted that long-term consequences of FMT are not well understood and thus, risks versus benefits of FMT on a patient-by-patient basis must be carefully weighed.
Dr. Naga P. Chalasani is the David W. Crabb Professor and director of the division of gastroenterology and hepatology, Indiana University, Indianapolis. He has consulting agreements and receives research support from several pharmaceutical companies but none represent a conflict of interest for this activity.
This is a summary provided by the moderator of one of the spring postgraduate course sessions held at DDW 2015.
Dr. Lin Chang at the University of California, Los Angeles, discussed how to work-up and manage functional abdominal pain. She reviewed a diagnostic algorithm that is evidence based and uses characteristics of the abdominal pain, coexisting warning signs, and a diagnostic work-up. A patient must be diagnosed with functional abdominal pain only after careful medical history, physical examination, and adequate consideration of competing etiologies.
Physical examination can be helpful in differentiating abdominal wall pain from that of visceral pain (Carnett’s sign) although some patients with functional abdominal pain may exhibit positive Carnett’s sign. Managing a patient with suspected functional abdominal pain includes careful attention to warning signs for organic disease (for example, unintended weight loss, hematochezia, abnormal labs, fever, or family history of serious GI disorders), avoiding unnecessary diagnostic testing, consideration of mental health consultation and pharmacotherapy as appropriate.
Dr. Chang reviewed the role of various pharmacologic agents for irritable bowel syndrome (IBS) with diarrhea (alosetron, rifaximin, and loperamide), IBS with constipation (linaclotide, lubiprostone, and polyethylene glycol) and agents such antispasmodics, tricyclic antidepressants, and SSRIs (reviewed extensively in the AGA Technical Review and Guidelines for Pharmacotherapy for IBS published in Gastroenterology. 2014 Nov;147[5]:1149-72.e2). It is important to establish a strong patient-provider relationship and to incorporate behavioral therapies into management of patients with recurrent or chronic functional abdominal pain.
Dr. Peter Gibson at Monash University in Melbourne discussed non–celiac gluten sensitivity and low-FODMAP diet in managing food sensitivity and functional bowel disorders. He pointed out that recent dietary strategies have changed from patient-initiated, whole-food strategies to avoiding specific dietary components such as FODMAPs and gluten and wheat products. FODMAPS (fermentable oligo-, di-, and monosaccharides and polyols) are foods that are generally high in fructose, lactose, oligosaccharides (e.g., beans, onions, garlic, complex carbohydrates) and polyols (e.g., mushrooms). FODMAPs are generally osmotic and lead to fermentation and diarrhea, bloating, and flatulence. General principles in offering a low-FODMAP diet are the selection of appropriate patients; correct education about FODMAP diets, preferably by a trained dietitian; and a step-down approach in which a strict diet is slowly liberalized. Dr. Gibson pointed out that there are a subset of IBS patients who are gluten sensitive but recent data suggest that wheat protein sensitivity may not be as common as it has been suggested and, in fact, FODMAPs may indeed be the major inducers of symptoms in individuals with supposed wheat intolerance. The potential risks of dietary manipulation such as creation of a dietary cripple or induction of an eating disorder should be kept in mind.
Dr. Anna Mae Diehl at Duke University Medical Center in Durham, N.C., spoke about the diagnosis, role of the microbiome, and the treatment of nonalcoholic fatty liver disease (NAFLD). It was pointed out that most patients with NAFLD have benign progression although individuals with nonalcoholic steatohepatitis (NASH), especially those with significant fibrosis, are at risk for developing cirrhosis, liver failure, and liver cancer. Therapeutic investigations undertaken to date have not sufficiently focused on improving fibrosis although several ongoing clinical trials are directed at this goal. Gut microbiome might be a new NAFLD diagnostic/therapeutic target because several recent animal studies have shown that gut microbiome may play a role in conferring susceptibility to liver injury, fibrosis, and cancer.
Dr. Lawrence J. Brandt at Albert Einstein College of Medicine, New York, gave an update on fecal microbiota therapy (FMT). He highlighted that FMT has historic roots going back to the 4th century when Ge Hong described use of human fecal suspension to treat food poisoning or severe diarrhea. He made it clear that FMT should be offered only to those with recurrent Clostridium difficile infections (CDI), meeting selected criteria such as severe illness and prior treatment failures. The protocol for FMT in recurrent CDI includes careful selection of donor (may range from any healthy person, universal donor, or stool-bank product) and testing stool and blood of potential donors for any transmittable agents. A recent systematic review showed that the success rate for FMT in individuals with CDI is generally quite high (greater than 80%) but it may depend on the site of FMT – for example, if FMT is administered to duodenum/jejunum, the success rate is 86%, whereas if it is delivered to right colon/cecum, then the success rate can be as high as 93%. He highlighted the efficacy of FMT in severe, complicated CDI, which generally carries high morbidity and mortality. Practitioners offering FMT should carefully review the FDA guidance that was issued in March 2014. He noted that long-term consequences of FMT are not well understood and thus, risks versus benefits of FMT on a patient-by-patient basis must be carefully weighed.
Dr. Naga P. Chalasani is the David W. Crabb Professor and director of the division of gastroenterology and hepatology, Indiana University, Indianapolis. He has consulting agreements and receives research support from several pharmaceutical companies but none represent a conflict of interest for this activity.
This is a summary provided by the moderator of one of the spring postgraduate course sessions held at DDW 2015.
Genetics and epigenetics in gastroenterology
Genetics in the context of disease causation refers to gene expression altered by DNA mutations. Epigenetics refers to gene expression altered without DNA mutations, but instead by other cellular mechanisms that will be described here. Together, genetic and epigenetic gene expression determine both physiologic and pathologic cellular processes and functions.
Many areas of gastroenterology are now known to involve these mechanisms as part of disease pathophysiology. The area most investigated in gastroenterology is perhaps colon cancer, which will be used as an example in describing clinically pertinent mechanisms and findings in both genetics and epigenetics.
Inherited DNA mutations of certain genes result in colon cancer susceptibility syndromes. Somatic mutations of many of the same genes are part of colon cancer pathogenesis in common or sporadic cases. Pertinent syndromes include familial adenomatous polyposis (APC gene), Lynch syndrome (mismatch repair genes [MMR]), MUTY-associated polyposis (MUTYH gene), Peutz-Jeghers syndrome (STK11 gene), juvenile polyposis (SMAD4 and BMPR1A genes), Cowden syndrome (PTEN gene), and variant polyposis (POLE, POLD1, and Gremm1 genes). For each of these syndromes, genetic testing is now an accepted part of clinical management for diagnosis and guidance as to who should receive more aggressive screening and surveillance for colon cancer prevention.
Acquired or somatic mutations of the same and other genes are involved in the process of benign to malignant transformation in the colon. Involved genes are often divided into three pathways, although there is much overlap between these pathways.
The first pathway is the chromosomal instability pathway that begins with acquired APC gene mutations of a colonocyte. These mutations are followed by the accumulation of additional mutations as normal cells progress to forming adenomatous polyps and then cancer. Such genes include KRAS, SMAD, TP53, PTEN, PI3KCA, and perhaps others. The second pathway involves acquired mutations of the mismatch repair genes early in the benign to malignant process, with mutations occurring especially in the MLH1 gene. It is called the microsatellite instability pathway. Different genes are then involved through mutation in this pathway to cancer. These include TGF beta, BAX, IGF2R, and others. The third pathway is called CIMP for “CpG island methylation phenotype.” It is actually an epigenetic pathway and involves the accumulation of mutations in yet other genes including MLH1, WRN, p16, RARB2, BRAF, and possibly many others, and gives rise to both adenomatous polyps and sessile serrated polyps.
Clinical relevance of somatic mutations of the genes in these three pathways is already informing clinical practice. Cancers with MMR gene mutations, for example, exhibit a better prognosis than other colon cancers but a decreased responsiveness to fluorouracil drugs. Tumors with KRAS or BRAF mutations have little or no response to EGFR-inhibitor drugs. Many of the genes in which acquired mutations occur are now interrogated as part of stool DNA screening tests.
Epigenetic processes change gene expression without DNA mutation and include three primary categories: DNA methylation, histone and chromatin changes, and microRNA changes.
Half of human genes have promotor regions rich in CpG islands. When methylation occurs in these CpG islands, gene expression is usually inhibited. This is the main mechanism of the CIMP pathway and in turn affects numerous cell functions important to cancer pathogenesis. Histones are proteins around which DNA coils. The proteins with coiled DNA are called chromatin units. Histones have protein tails that repress gene transcription when acetylation and specific methylations occur. Some histone proteins have already been observed to be overexpressed in colon cancer. MicroRNAs are short noncoding RNAs that induce gene repression in up to 30% of genes. Altered MicroRNA expression has been observed in many colon cancer–associated genes, and specific microRNA patterns have characterized certain colon cancers.
Epigenetic cancer markers are only beginning to be understood but are being examined for use in early detection and prognosis, tumor subclassifications, following the effectiveness of chemotherapy, and providing targets of intervention.
In summary, colon cancer genetics has provided genetic testing for inherited syndromes and guides to therapy with acquired mutations, while epigenetic mechanisms have the potential of being important to many areas of cancer diagnosis and treatment.
Dr. Burt is professor of medicine and holder of the Barnes Presidential Endowed Chair in Medicine at the Huntsman Cancer Institute and the University of Utah, Salt Lake City. He has consulted for Myriad Genetics. His comments were made during the ASGE and AGA joint Presidential Plenary at the annual Digestive Disease Week.
Genetics in the context of disease causation refers to gene expression altered by DNA mutations. Epigenetics refers to gene expression altered without DNA mutations, but instead by other cellular mechanisms that will be described here. Together, genetic and epigenetic gene expression determine both physiologic and pathologic cellular processes and functions.
Many areas of gastroenterology are now known to involve these mechanisms as part of disease pathophysiology. The area most investigated in gastroenterology is perhaps colon cancer, which will be used as an example in describing clinically pertinent mechanisms and findings in both genetics and epigenetics.
Inherited DNA mutations of certain genes result in colon cancer susceptibility syndromes. Somatic mutations of many of the same genes are part of colon cancer pathogenesis in common or sporadic cases. Pertinent syndromes include familial adenomatous polyposis (APC gene), Lynch syndrome (mismatch repair genes [MMR]), MUTY-associated polyposis (MUTYH gene), Peutz-Jeghers syndrome (STK11 gene), juvenile polyposis (SMAD4 and BMPR1A genes), Cowden syndrome (PTEN gene), and variant polyposis (POLE, POLD1, and Gremm1 genes). For each of these syndromes, genetic testing is now an accepted part of clinical management for diagnosis and guidance as to who should receive more aggressive screening and surveillance for colon cancer prevention.
Acquired or somatic mutations of the same and other genes are involved in the process of benign to malignant transformation in the colon. Involved genes are often divided into three pathways, although there is much overlap between these pathways.
The first pathway is the chromosomal instability pathway that begins with acquired APC gene mutations of a colonocyte. These mutations are followed by the accumulation of additional mutations as normal cells progress to forming adenomatous polyps and then cancer. Such genes include KRAS, SMAD, TP53, PTEN, PI3KCA, and perhaps others. The second pathway involves acquired mutations of the mismatch repair genes early in the benign to malignant process, with mutations occurring especially in the MLH1 gene. It is called the microsatellite instability pathway. Different genes are then involved through mutation in this pathway to cancer. These include TGF beta, BAX, IGF2R, and others. The third pathway is called CIMP for “CpG island methylation phenotype.” It is actually an epigenetic pathway and involves the accumulation of mutations in yet other genes including MLH1, WRN, p16, RARB2, BRAF, and possibly many others, and gives rise to both adenomatous polyps and sessile serrated polyps.
Clinical relevance of somatic mutations of the genes in these three pathways is already informing clinical practice. Cancers with MMR gene mutations, for example, exhibit a better prognosis than other colon cancers but a decreased responsiveness to fluorouracil drugs. Tumors with KRAS or BRAF mutations have little or no response to EGFR-inhibitor drugs. Many of the genes in which acquired mutations occur are now interrogated as part of stool DNA screening tests.
Epigenetic processes change gene expression without DNA mutation and include three primary categories: DNA methylation, histone and chromatin changes, and microRNA changes.
Half of human genes have promotor regions rich in CpG islands. When methylation occurs in these CpG islands, gene expression is usually inhibited. This is the main mechanism of the CIMP pathway and in turn affects numerous cell functions important to cancer pathogenesis. Histones are proteins around which DNA coils. The proteins with coiled DNA are called chromatin units. Histones have protein tails that repress gene transcription when acetylation and specific methylations occur. Some histone proteins have already been observed to be overexpressed in colon cancer. MicroRNAs are short noncoding RNAs that induce gene repression in up to 30% of genes. Altered MicroRNA expression has been observed in many colon cancer–associated genes, and specific microRNA patterns have characterized certain colon cancers.
Epigenetic cancer markers are only beginning to be understood but are being examined for use in early detection and prognosis, tumor subclassifications, following the effectiveness of chemotherapy, and providing targets of intervention.
In summary, colon cancer genetics has provided genetic testing for inherited syndromes and guides to therapy with acquired mutations, while epigenetic mechanisms have the potential of being important to many areas of cancer diagnosis and treatment.
Dr. Burt is professor of medicine and holder of the Barnes Presidential Endowed Chair in Medicine at the Huntsman Cancer Institute and the University of Utah, Salt Lake City. He has consulted for Myriad Genetics. His comments were made during the ASGE and AGA joint Presidential Plenary at the annual Digestive Disease Week.
Genetics in the context of disease causation refers to gene expression altered by DNA mutations. Epigenetics refers to gene expression altered without DNA mutations, but instead by other cellular mechanisms that will be described here. Together, genetic and epigenetic gene expression determine both physiologic and pathologic cellular processes and functions.
Many areas of gastroenterology are now known to involve these mechanisms as part of disease pathophysiology. The area most investigated in gastroenterology is perhaps colon cancer, which will be used as an example in describing clinically pertinent mechanisms and findings in both genetics and epigenetics.
Inherited DNA mutations of certain genes result in colon cancer susceptibility syndromes. Somatic mutations of many of the same genes are part of colon cancer pathogenesis in common or sporadic cases. Pertinent syndromes include familial adenomatous polyposis (APC gene), Lynch syndrome (mismatch repair genes [MMR]), MUTY-associated polyposis (MUTYH gene), Peutz-Jeghers syndrome (STK11 gene), juvenile polyposis (SMAD4 and BMPR1A genes), Cowden syndrome (PTEN gene), and variant polyposis (POLE, POLD1, and Gremm1 genes). For each of these syndromes, genetic testing is now an accepted part of clinical management for diagnosis and guidance as to who should receive more aggressive screening and surveillance for colon cancer prevention.
Acquired or somatic mutations of the same and other genes are involved in the process of benign to malignant transformation in the colon. Involved genes are often divided into three pathways, although there is much overlap between these pathways.
The first pathway is the chromosomal instability pathway that begins with acquired APC gene mutations of a colonocyte. These mutations are followed by the accumulation of additional mutations as normal cells progress to forming adenomatous polyps and then cancer. Such genes include KRAS, SMAD, TP53, PTEN, PI3KCA, and perhaps others. The second pathway involves acquired mutations of the mismatch repair genes early in the benign to malignant process, with mutations occurring especially in the MLH1 gene. It is called the microsatellite instability pathway. Different genes are then involved through mutation in this pathway to cancer. These include TGF beta, BAX, IGF2R, and others. The third pathway is called CIMP for “CpG island methylation phenotype.” It is actually an epigenetic pathway and involves the accumulation of mutations in yet other genes including MLH1, WRN, p16, RARB2, BRAF, and possibly many others, and gives rise to both adenomatous polyps and sessile serrated polyps.
Clinical relevance of somatic mutations of the genes in these three pathways is already informing clinical practice. Cancers with MMR gene mutations, for example, exhibit a better prognosis than other colon cancers but a decreased responsiveness to fluorouracil drugs. Tumors with KRAS or BRAF mutations have little or no response to EGFR-inhibitor drugs. Many of the genes in which acquired mutations occur are now interrogated as part of stool DNA screening tests.
Epigenetic processes change gene expression without DNA mutation and include three primary categories: DNA methylation, histone and chromatin changes, and microRNA changes.
Half of human genes have promotor regions rich in CpG islands. When methylation occurs in these CpG islands, gene expression is usually inhibited. This is the main mechanism of the CIMP pathway and in turn affects numerous cell functions important to cancer pathogenesis. Histones are proteins around which DNA coils. The proteins with coiled DNA are called chromatin units. Histones have protein tails that repress gene transcription when acetylation and specific methylations occur. Some histone proteins have already been observed to be overexpressed in colon cancer. MicroRNAs are short noncoding RNAs that induce gene repression in up to 30% of genes. Altered MicroRNA expression has been observed in many colon cancer–associated genes, and specific microRNA patterns have characterized certain colon cancers.
Epigenetic cancer markers are only beginning to be understood but are being examined for use in early detection and prognosis, tumor subclassifications, following the effectiveness of chemotherapy, and providing targets of intervention.
In summary, colon cancer genetics has provided genetic testing for inherited syndromes and guides to therapy with acquired mutations, while epigenetic mechanisms have the potential of being important to many areas of cancer diagnosis and treatment.
Dr. Burt is professor of medicine and holder of the Barnes Presidential Endowed Chair in Medicine at the Huntsman Cancer Institute and the University of Utah, Salt Lake City. He has consulted for Myriad Genetics. His comments were made during the ASGE and AGA joint Presidential Plenary at the annual Digestive Disease Week.
IBD surveillance: Quality not quantity
Optimizing colonoscopy quality in patients with ulcerative colitis or Crohn’s disease involving the colon is important. Their risk for the development of colorectal cancer (CRC) and of interval CRC is significantly higher compared with the non–inflammatory bowel disease (IBD) population.
Most CRC cases in IBD are believed to arise from dysplasia, and thus, surveillance colonoscopy is recommended to detect dysplasia. Key factors that influence the success of surveillance colonoscopy in IBD patients include: 1) endoscopic recognition of dysplasia, 2) adequacy of mucosal sampling, 3) awareness of interfering anatomy, such as strictures and pseudopolyps, 4) appropriate differentiation of dysplastic lesions as endoscopically resectable, 5) complete removal of endoscopically resectable dysplasia, and 6) patient compliance.
Over a decade ago, we learned that most dysplasia discovered in patients with IBD is actually visible. The use of high-definition video-endoscopy and newer methods, such as chromoendoscopy with mucosal dye spraying, enhance the detection of dysplasia. Today, with the widespread use of newer technologies and techniques, the literature indicates that targeted biopsies of visible lesions account for approximately 90% of cases, whereas random biopsy (resulting in detection of an endoscopically invisible lesion) accounts for only 10% of cases of identified dysplasia.
The endoscopic recognition of dysplastic colorectal lesions may have important implications for the surveillance and management of dysplasia, and shift it away from the traditional random biopsy technique, where less than 0.1% of the colonic mucosal surface area is sampled, and from colectomy for any diagnosis of dysplasia.
Enhanced endoscopy techniques such as chromoendoscopy can have a substantial impact upon IBD surveillance, increasing the dysplasia detection rates, as well as informing management decisions. Chromoendoscopy, using a dye solution of either methylene blue or indigo carmine applied onto the colonic mucosa to enhance contrast during surveillance colonoscopy, is performed either in a pancolonic fashion to detect lesions or in a targeted fashion to allow for detailed viewing of an identified lesion (Figure 1).
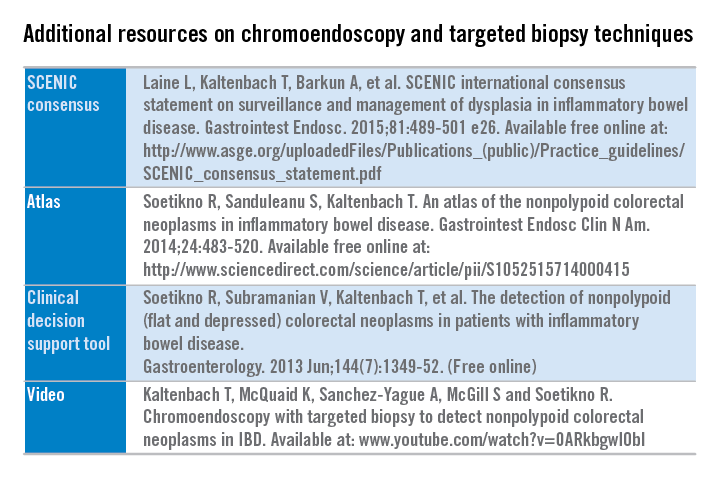
Additional resources are freely available detailing the technique and suggested steps to implement chromoendoscopy into practice. (See additional resources on chromoendoscopy and targeted biopsy techniques.)
An international multidisciplinary group, SCENIC (Surveillance for Colorectal Endoscopic Neoplasia Detection and Management in Inflammatory Bowel Disease Patients: International Consensus), which represents a wide spectrum of stakeholders and attitudes regarding IBD surveillance, sought to develop unifying consensus recommendations addressing two issues: 1) how should surveillance colonoscopy to detect dysplasia be performed, and 2) how should dysplasia identified at colonoscopy be managed. The SCENIC group adhered to suggested standards for guideline development from the Institute of Medicine and others and that incorporated the GRADE methodology. A systematic review was performed for each focused clinical question, followed by a review of a full synthesis of evidence by panelists.
SCENIC key summary recommendations
Detection
• High definition is recommended over standard definition for performance of surveillance colonoscopy.
• Routine performance of chromoendoscopy during IBD surveillance is suggested as an adjunct to high-definition colonoscopy.
• Narrowband imaging is not recommended as an alternative for high-definition, white-light colonoscopy or chromoendoscopy.
• No specific recommendation on performance of random biopsies was made in patients undergoing high-definition, white-light colonoscopy plus chromoendoscopy. The panel did not reach consensus on this topic because 60% of the panel members disagreed with performing random biopsies during chromoendoscopy, and a recommendation required 80% agreement or disagreement.
Management
• When dysplasia is detected, it should be characterized as “endoscopically resectable” or “nonendoscopically resectable” (The terms “dysplasia-associated lesion or mass (DALM),” “adenoma-like,” and “nonadenoma-like” should be abandoned).
• Visible dysplasia should be characterized according to the Paris classification polypoid or nonpolypoid, with modifications including the addition of terms for ulceration and border of the lesion.
• The term endoscopically resectable indicates that 1) distinct margins of the lesion could be identified, 2) the lesion appears to be completely removed on visual inspection after endoscopic resection, 3) histologic examination of the resected specimen is consistent with complete removal, and 4) biopsy specimens taken from mucosa immediately adjacent to the resection site are free of dysplasia on histologic examination.
• After complete removal of endoscopically resectable polypoid or nonpolypoid dysplasia, surveillance colonoscopy is recommended rather than colectomy.
• For patients with endoscopically invisible dysplasia (confirmed by a GI pathologist), referral is suggested to an endoscopist with expertise in IBD surveillance using chromoendoscopy with high-definition colonoscopy.
The SCENIC recommendations aim to optimize the detection and management of dysplasia in IBD patients. Future research in IBD surveillance should assess the potential for chromoendoscopy to improve risk stratification to elucidate optimal surveillance intervals, and the impact on CRC incidence and mortality. In addition, the role of resection of nonpolypoid dysplasia in the reduction in CRC incidence or need for colectomy requires further investigation.
Dr. Kaltenbach is a gastroenterologist at Veterans Affairs, and a clinical assistant professor of medicine at Stanford (Calif.) University. She has no conflicts of interest. Her comments were made during the ASGE and AGA joint Presidential Plenary at the annual Digestive Disease Week.
Optimizing colonoscopy quality in patients with ulcerative colitis or Crohn’s disease involving the colon is important. Their risk for the development of colorectal cancer (CRC) and of interval CRC is significantly higher compared with the non–inflammatory bowel disease (IBD) population.
Most CRC cases in IBD are believed to arise from dysplasia, and thus, surveillance colonoscopy is recommended to detect dysplasia. Key factors that influence the success of surveillance colonoscopy in IBD patients include: 1) endoscopic recognition of dysplasia, 2) adequacy of mucosal sampling, 3) awareness of interfering anatomy, such as strictures and pseudopolyps, 4) appropriate differentiation of dysplastic lesions as endoscopically resectable, 5) complete removal of endoscopically resectable dysplasia, and 6) patient compliance.
Over a decade ago, we learned that most dysplasia discovered in patients with IBD is actually visible. The use of high-definition video-endoscopy and newer methods, such as chromoendoscopy with mucosal dye spraying, enhance the detection of dysplasia. Today, with the widespread use of newer technologies and techniques, the literature indicates that targeted biopsies of visible lesions account for approximately 90% of cases, whereas random biopsy (resulting in detection of an endoscopically invisible lesion) accounts for only 10% of cases of identified dysplasia.
The endoscopic recognition of dysplastic colorectal lesions may have important implications for the surveillance and management of dysplasia, and shift it away from the traditional random biopsy technique, where less than 0.1% of the colonic mucosal surface area is sampled, and from colectomy for any diagnosis of dysplasia.
Enhanced endoscopy techniques such as chromoendoscopy can have a substantial impact upon IBD surveillance, increasing the dysplasia detection rates, as well as informing management decisions. Chromoendoscopy, using a dye solution of either methylene blue or indigo carmine applied onto the colonic mucosa to enhance contrast during surveillance colonoscopy, is performed either in a pancolonic fashion to detect lesions or in a targeted fashion to allow for detailed viewing of an identified lesion (Figure 1).
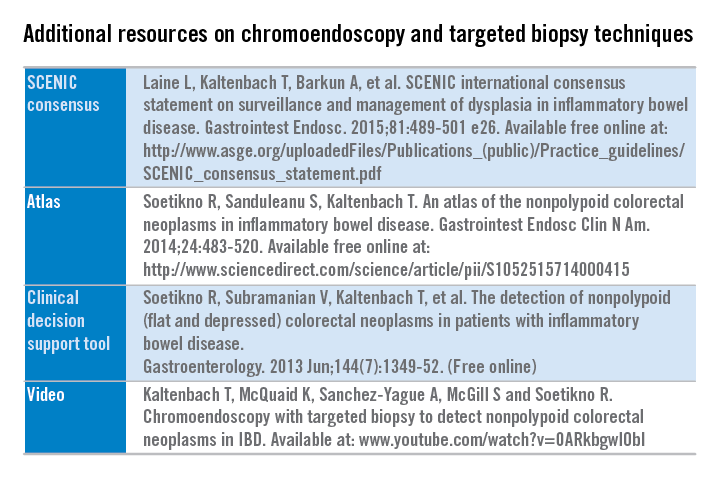
Additional resources are freely available detailing the technique and suggested steps to implement chromoendoscopy into practice. (See additional resources on chromoendoscopy and targeted biopsy techniques.)
An international multidisciplinary group, SCENIC (Surveillance for Colorectal Endoscopic Neoplasia Detection and Management in Inflammatory Bowel Disease Patients: International Consensus), which represents a wide spectrum of stakeholders and attitudes regarding IBD surveillance, sought to develop unifying consensus recommendations addressing two issues: 1) how should surveillance colonoscopy to detect dysplasia be performed, and 2) how should dysplasia identified at colonoscopy be managed. The SCENIC group adhered to suggested standards for guideline development from the Institute of Medicine and others and that incorporated the GRADE methodology. A systematic review was performed for each focused clinical question, followed by a review of a full synthesis of evidence by panelists.
SCENIC key summary recommendations
Detection
• High definition is recommended over standard definition for performance of surveillance colonoscopy.
• Routine performance of chromoendoscopy during IBD surveillance is suggested as an adjunct to high-definition colonoscopy.
• Narrowband imaging is not recommended as an alternative for high-definition, white-light colonoscopy or chromoendoscopy.
• No specific recommendation on performance of random biopsies was made in patients undergoing high-definition, white-light colonoscopy plus chromoendoscopy. The panel did not reach consensus on this topic because 60% of the panel members disagreed with performing random biopsies during chromoendoscopy, and a recommendation required 80% agreement or disagreement.
Management
• When dysplasia is detected, it should be characterized as “endoscopically resectable” or “nonendoscopically resectable” (The terms “dysplasia-associated lesion or mass (DALM),” “adenoma-like,” and “nonadenoma-like” should be abandoned).
• Visible dysplasia should be characterized according to the Paris classification polypoid or nonpolypoid, with modifications including the addition of terms for ulceration and border of the lesion.
• The term endoscopically resectable indicates that 1) distinct margins of the lesion could be identified, 2) the lesion appears to be completely removed on visual inspection after endoscopic resection, 3) histologic examination of the resected specimen is consistent with complete removal, and 4) biopsy specimens taken from mucosa immediately adjacent to the resection site are free of dysplasia on histologic examination.
• After complete removal of endoscopically resectable polypoid or nonpolypoid dysplasia, surveillance colonoscopy is recommended rather than colectomy.
• For patients with endoscopically invisible dysplasia (confirmed by a GI pathologist), referral is suggested to an endoscopist with expertise in IBD surveillance using chromoendoscopy with high-definition colonoscopy.
The SCENIC recommendations aim to optimize the detection and management of dysplasia in IBD patients. Future research in IBD surveillance should assess the potential for chromoendoscopy to improve risk stratification to elucidate optimal surveillance intervals, and the impact on CRC incidence and mortality. In addition, the role of resection of nonpolypoid dysplasia in the reduction in CRC incidence or need for colectomy requires further investigation.
Dr. Kaltenbach is a gastroenterologist at Veterans Affairs, and a clinical assistant professor of medicine at Stanford (Calif.) University. She has no conflicts of interest. Her comments were made during the ASGE and AGA joint Presidential Plenary at the annual Digestive Disease Week.
Optimizing colonoscopy quality in patients with ulcerative colitis or Crohn’s disease involving the colon is important. Their risk for the development of colorectal cancer (CRC) and of interval CRC is significantly higher compared with the non–inflammatory bowel disease (IBD) population.
Most CRC cases in IBD are believed to arise from dysplasia, and thus, surveillance colonoscopy is recommended to detect dysplasia. Key factors that influence the success of surveillance colonoscopy in IBD patients include: 1) endoscopic recognition of dysplasia, 2) adequacy of mucosal sampling, 3) awareness of interfering anatomy, such as strictures and pseudopolyps, 4) appropriate differentiation of dysplastic lesions as endoscopically resectable, 5) complete removal of endoscopically resectable dysplasia, and 6) patient compliance.
Over a decade ago, we learned that most dysplasia discovered in patients with IBD is actually visible. The use of high-definition video-endoscopy and newer methods, such as chromoendoscopy with mucosal dye spraying, enhance the detection of dysplasia. Today, with the widespread use of newer technologies and techniques, the literature indicates that targeted biopsies of visible lesions account for approximately 90% of cases, whereas random biopsy (resulting in detection of an endoscopically invisible lesion) accounts for only 10% of cases of identified dysplasia.
The endoscopic recognition of dysplastic colorectal lesions may have important implications for the surveillance and management of dysplasia, and shift it away from the traditional random biopsy technique, where less than 0.1% of the colonic mucosal surface area is sampled, and from colectomy for any diagnosis of dysplasia.
Enhanced endoscopy techniques such as chromoendoscopy can have a substantial impact upon IBD surveillance, increasing the dysplasia detection rates, as well as informing management decisions. Chromoendoscopy, using a dye solution of either methylene blue or indigo carmine applied onto the colonic mucosa to enhance contrast during surveillance colonoscopy, is performed either in a pancolonic fashion to detect lesions or in a targeted fashion to allow for detailed viewing of an identified lesion (Figure 1).
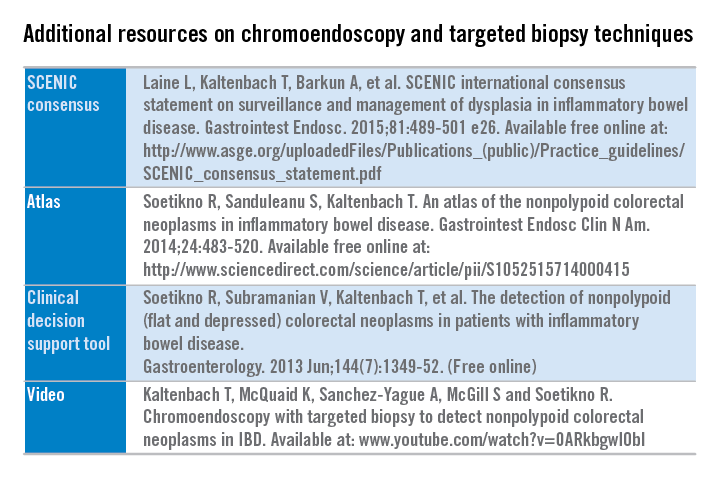
Additional resources are freely available detailing the technique and suggested steps to implement chromoendoscopy into practice. (See additional resources on chromoendoscopy and targeted biopsy techniques.)
An international multidisciplinary group, SCENIC (Surveillance for Colorectal Endoscopic Neoplasia Detection and Management in Inflammatory Bowel Disease Patients: International Consensus), which represents a wide spectrum of stakeholders and attitudes regarding IBD surveillance, sought to develop unifying consensus recommendations addressing two issues: 1) how should surveillance colonoscopy to detect dysplasia be performed, and 2) how should dysplasia identified at colonoscopy be managed. The SCENIC group adhered to suggested standards for guideline development from the Institute of Medicine and others and that incorporated the GRADE methodology. A systematic review was performed for each focused clinical question, followed by a review of a full synthesis of evidence by panelists.
SCENIC key summary recommendations
Detection
• High definition is recommended over standard definition for performance of surveillance colonoscopy.
• Routine performance of chromoendoscopy during IBD surveillance is suggested as an adjunct to high-definition colonoscopy.
• Narrowband imaging is not recommended as an alternative for high-definition, white-light colonoscopy or chromoendoscopy.
• No specific recommendation on performance of random biopsies was made in patients undergoing high-definition, white-light colonoscopy plus chromoendoscopy. The panel did not reach consensus on this topic because 60% of the panel members disagreed with performing random biopsies during chromoendoscopy, and a recommendation required 80% agreement or disagreement.
Management
• When dysplasia is detected, it should be characterized as “endoscopically resectable” or “nonendoscopically resectable” (The terms “dysplasia-associated lesion or mass (DALM),” “adenoma-like,” and “nonadenoma-like” should be abandoned).
• Visible dysplasia should be characterized according to the Paris classification polypoid or nonpolypoid, with modifications including the addition of terms for ulceration and border of the lesion.
• The term endoscopically resectable indicates that 1) distinct margins of the lesion could be identified, 2) the lesion appears to be completely removed on visual inspection after endoscopic resection, 3) histologic examination of the resected specimen is consistent with complete removal, and 4) biopsy specimens taken from mucosa immediately adjacent to the resection site are free of dysplasia on histologic examination.
• After complete removal of endoscopically resectable polypoid or nonpolypoid dysplasia, surveillance colonoscopy is recommended rather than colectomy.
• For patients with endoscopically invisible dysplasia (confirmed by a GI pathologist), referral is suggested to an endoscopist with expertise in IBD surveillance using chromoendoscopy with high-definition colonoscopy.
The SCENIC recommendations aim to optimize the detection and management of dysplasia in IBD patients. Future research in IBD surveillance should assess the potential for chromoendoscopy to improve risk stratification to elucidate optimal surveillance intervals, and the impact on CRC incidence and mortality. In addition, the role of resection of nonpolypoid dysplasia in the reduction in CRC incidence or need for colectomy requires further investigation.
Dr. Kaltenbach is a gastroenterologist at Veterans Affairs, and a clinical assistant professor of medicine at Stanford (Calif.) University. She has no conflicts of interest. Her comments were made during the ASGE and AGA joint Presidential Plenary at the annual Digestive Disease Week.
Bugs and drugs in inflammatory bowel disease
Important new themes are whether we can actually find a cure for inflammatory bowel disease and, in particular, whether there are common pathogenetic mechanisms leading to Crohn’s disease and ulcerative colitis. Are Crohn’s and ulcerative colitis infectious diseases? If the answer to that question is ‘yes,’ then eliminating that “pathogen” would turn off the immune response. Crohn’s disease and ulcerative colitis share common genetic origins with the majority of genes shared between both disorders. Indeed, 110 of the 163 confirmed loci in IBD are common between the two disorders (Nature 2012;491:119–24).
In addition to there being many genes contributing even a small amount to the development of IBD, there are also some genetic pathways that have a far more impactful role in IBD. By studying very-early-onset IBD, we have discovered that the IL-10 receptor pathway is very important in controlling intestinal inflammation, such that if you have a mutation in the receptor for IL-10 it can lead to very-early-onset IBD. Children who are born with these disorders can be treated with a hematopoietic bone marrow transplant. At this year’s Digestive Disease Week (DDW) in fact, there was the presentation of the ASTIC trial; it described patients having a prolonged remission after an autologous hematopoietic stem cell transplant.
One of the big advances that has been made in terms of the treatment of IBD is based on an understanding of the pathogenetic pathways; in particular, there has been an increase in the number of medications that are currently available to treat IBD from a variety of different avenues. There was a recent publication describing an anti-sense treatment against SMAD7 in restoring TGF-beta signaling that produced a very rapid and profound improvement in the clinical symptoms of Crohn’s disease. We await more data on that particular compound.
We now know that an antibody against P40, which is the common subunit between IL-12 and IL-23, is effective in the treatment of Crohn’s disease and is commercially available as ustekinumab. At this year’s DDW we heard about an antibody that is specific for anti-IL-23 since it only antagonizes the P19 subunit of the cytokine; it also shows great promise for treating IBD. At DDW 2014, vedolizumab had just obtained approval for the treatment of ulcerative colitis and Crohn’s disease and that has been a big advance in treating patients. On its heels are a variety of other compounds that work by a similar mechanism by inhibiting the trafficking of effector lymphocytes to the intestine; these include anti-beta7 strategies and anti-MAdCAM. Both of these have been shown to be more effective in ulcerative colitis than in Crohn’s disease, as has been a common theme.
The other important presentation that took place at DDW 2015 is the use of ozanimod to treat ulcerative colitis; again, this is an oral agent that has a very dramatic effect in treating ulcerative colitis in a very short period of time by inhibiting the exit of effector T cells from lymph nodes. This tells us about the host immune response. We can now sequence all the bacteria that are present in the gut and using that approach we have found broad patterns of decreased diversity in patients who have IBD, although we have not identified a particular pathogen or pathogens.
The laboratory of Dr. Richard Flavell used a strategy in which they identified bacteria that were IgA coated and reasoned that IgA-coated bacteria were more likely to be pathogens (Cell. 2014 Aug 28;158(5):1000-1010). Indeed, by giving mice these IgA-coated bacteria found in IBD patients, the mice were more likely to develop colitis than if you gave non–IgA-coated bacteria to the same mice.
Another very important observation was in a study that was published in Nature, which demonstrated that emulsifiers really changed the relationship between the host and the microbiome. In particular, the investigators found that interactions with the microbiota led to metabolic syndrome. They also found that with dietary emulsifiers there is encroachment of the epithelium because of a thinning of the mucous layer and the study animals were more susceptible to developing colitis. I think that this is a sign to our patients that it is better to avoid processed foods.
Dr. Abreu is professor of medicine, professor of microbiology and immunology, chief of the division of gastroenterology, the Martin Kalser Chair in gastroenterology, and the director, Crohn’s & Colitis Center at the University of Miami Miller School of Medicine. She consults for AbbVie, Focus Medical Communications, GSK, and many other biopharmaceutical companies. Her comments were made during the ASGE and AGA joint Presidential Plenary at the annual Digestive Disease Week.
Important new themes are whether we can actually find a cure for inflammatory bowel disease and, in particular, whether there are common pathogenetic mechanisms leading to Crohn’s disease and ulcerative colitis. Are Crohn’s and ulcerative colitis infectious diseases? If the answer to that question is ‘yes,’ then eliminating that “pathogen” would turn off the immune response. Crohn’s disease and ulcerative colitis share common genetic origins with the majority of genes shared between both disorders. Indeed, 110 of the 163 confirmed loci in IBD are common between the two disorders (Nature 2012;491:119–24).
In addition to there being many genes contributing even a small amount to the development of IBD, there are also some genetic pathways that have a far more impactful role in IBD. By studying very-early-onset IBD, we have discovered that the IL-10 receptor pathway is very important in controlling intestinal inflammation, such that if you have a mutation in the receptor for IL-10 it can lead to very-early-onset IBD. Children who are born with these disorders can be treated with a hematopoietic bone marrow transplant. At this year’s Digestive Disease Week (DDW) in fact, there was the presentation of the ASTIC trial; it described patients having a prolonged remission after an autologous hematopoietic stem cell transplant.
One of the big advances that has been made in terms of the treatment of IBD is based on an understanding of the pathogenetic pathways; in particular, there has been an increase in the number of medications that are currently available to treat IBD from a variety of different avenues. There was a recent publication describing an anti-sense treatment against SMAD7 in restoring TGF-beta signaling that produced a very rapid and profound improvement in the clinical symptoms of Crohn’s disease. We await more data on that particular compound.
We now know that an antibody against P40, which is the common subunit between IL-12 and IL-23, is effective in the treatment of Crohn’s disease and is commercially available as ustekinumab. At this year’s DDW we heard about an antibody that is specific for anti-IL-23 since it only antagonizes the P19 subunit of the cytokine; it also shows great promise for treating IBD. At DDW 2014, vedolizumab had just obtained approval for the treatment of ulcerative colitis and Crohn’s disease and that has been a big advance in treating patients. On its heels are a variety of other compounds that work by a similar mechanism by inhibiting the trafficking of effector lymphocytes to the intestine; these include anti-beta7 strategies and anti-MAdCAM. Both of these have been shown to be more effective in ulcerative colitis than in Crohn’s disease, as has been a common theme.
The other important presentation that took place at DDW 2015 is the use of ozanimod to treat ulcerative colitis; again, this is an oral agent that has a very dramatic effect in treating ulcerative colitis in a very short period of time by inhibiting the exit of effector T cells from lymph nodes. This tells us about the host immune response. We can now sequence all the bacteria that are present in the gut and using that approach we have found broad patterns of decreased diversity in patients who have IBD, although we have not identified a particular pathogen or pathogens.
The laboratory of Dr. Richard Flavell used a strategy in which they identified bacteria that were IgA coated and reasoned that IgA-coated bacteria were more likely to be pathogens (Cell. 2014 Aug 28;158(5):1000-1010). Indeed, by giving mice these IgA-coated bacteria found in IBD patients, the mice were more likely to develop colitis than if you gave non–IgA-coated bacteria to the same mice.
Another very important observation was in a study that was published in Nature, which demonstrated that emulsifiers really changed the relationship between the host and the microbiome. In particular, the investigators found that interactions with the microbiota led to metabolic syndrome. They also found that with dietary emulsifiers there is encroachment of the epithelium because of a thinning of the mucous layer and the study animals were more susceptible to developing colitis. I think that this is a sign to our patients that it is better to avoid processed foods.
Dr. Abreu is professor of medicine, professor of microbiology and immunology, chief of the division of gastroenterology, the Martin Kalser Chair in gastroenterology, and the director, Crohn’s & Colitis Center at the University of Miami Miller School of Medicine. She consults for AbbVie, Focus Medical Communications, GSK, and many other biopharmaceutical companies. Her comments were made during the ASGE and AGA joint Presidential Plenary at the annual Digestive Disease Week.
Important new themes are whether we can actually find a cure for inflammatory bowel disease and, in particular, whether there are common pathogenetic mechanisms leading to Crohn’s disease and ulcerative colitis. Are Crohn’s and ulcerative colitis infectious diseases? If the answer to that question is ‘yes,’ then eliminating that “pathogen” would turn off the immune response. Crohn’s disease and ulcerative colitis share common genetic origins with the majority of genes shared between both disorders. Indeed, 110 of the 163 confirmed loci in IBD are common between the two disorders (Nature 2012;491:119–24).
In addition to there being many genes contributing even a small amount to the development of IBD, there are also some genetic pathways that have a far more impactful role in IBD. By studying very-early-onset IBD, we have discovered that the IL-10 receptor pathway is very important in controlling intestinal inflammation, such that if you have a mutation in the receptor for IL-10 it can lead to very-early-onset IBD. Children who are born with these disorders can be treated with a hematopoietic bone marrow transplant. At this year’s Digestive Disease Week (DDW) in fact, there was the presentation of the ASTIC trial; it described patients having a prolonged remission after an autologous hematopoietic stem cell transplant.
One of the big advances that has been made in terms of the treatment of IBD is based on an understanding of the pathogenetic pathways; in particular, there has been an increase in the number of medications that are currently available to treat IBD from a variety of different avenues. There was a recent publication describing an anti-sense treatment against SMAD7 in restoring TGF-beta signaling that produced a very rapid and profound improvement in the clinical symptoms of Crohn’s disease. We await more data on that particular compound.
We now know that an antibody against P40, which is the common subunit between IL-12 and IL-23, is effective in the treatment of Crohn’s disease and is commercially available as ustekinumab. At this year’s DDW we heard about an antibody that is specific for anti-IL-23 since it only antagonizes the P19 subunit of the cytokine; it also shows great promise for treating IBD. At DDW 2014, vedolizumab had just obtained approval for the treatment of ulcerative colitis and Crohn’s disease and that has been a big advance in treating patients. On its heels are a variety of other compounds that work by a similar mechanism by inhibiting the trafficking of effector lymphocytes to the intestine; these include anti-beta7 strategies and anti-MAdCAM. Both of these have been shown to be more effective in ulcerative colitis than in Crohn’s disease, as has been a common theme.
The other important presentation that took place at DDW 2015 is the use of ozanimod to treat ulcerative colitis; again, this is an oral agent that has a very dramatic effect in treating ulcerative colitis in a very short period of time by inhibiting the exit of effector T cells from lymph nodes. This tells us about the host immune response. We can now sequence all the bacteria that are present in the gut and using that approach we have found broad patterns of decreased diversity in patients who have IBD, although we have not identified a particular pathogen or pathogens.
The laboratory of Dr. Richard Flavell used a strategy in which they identified bacteria that were IgA coated and reasoned that IgA-coated bacteria were more likely to be pathogens (Cell. 2014 Aug 28;158(5):1000-1010). Indeed, by giving mice these IgA-coated bacteria found in IBD patients, the mice were more likely to develop colitis than if you gave non–IgA-coated bacteria to the same mice.
Another very important observation was in a study that was published in Nature, which demonstrated that emulsifiers really changed the relationship between the host and the microbiome. In particular, the investigators found that interactions with the microbiota led to metabolic syndrome. They also found that with dietary emulsifiers there is encroachment of the epithelium because of a thinning of the mucous layer and the study animals were more susceptible to developing colitis. I think that this is a sign to our patients that it is better to avoid processed foods.
Dr. Abreu is professor of medicine, professor of microbiology and immunology, chief of the division of gastroenterology, the Martin Kalser Chair in gastroenterology, and the director, Crohn’s & Colitis Center at the University of Miami Miller School of Medicine. She consults for AbbVie, Focus Medical Communications, GSK, and many other biopharmaceutical companies. Her comments were made during the ASGE and AGA joint Presidential Plenary at the annual Digestive Disease Week.
The value proposition comes home: The Jack A. Vennes, M.D. and Stephen E. Silvis, M.D. Honorary Lecture
Value in health care is often defined as “health outcomes achieved per dollar spent,” or “outcomes/costs.” Value encompasses efficiency, but is primarily results oriented and not based on volume. For purposes of comparison and assessment, value assessments apply to patient- and condition-specific episodes of care.
As the dominant driver of value-based reimbursement (VBR), the Center for Medicare & Medicaid Services, has defined a payment taxonomy for coming years based upon the degree of linkage between quality and reimbursement (JAMA 2014;311:1967-8). Four categories of reimbursement extend from traditional fee for service (FFS; Category 1) to FFS with significant reliance on quality measures and outcome (Cat. 2), entirely population-based models with payments stimulated by delivery of care (Cat. 3), and payment based entirely on capitated coverage of individuals over time (Cat. 4).
Category 2 reimbursement for physicians is largely based upon the Physicians Quality Reporting System (PQRS) with Value-Based Payment Modifiers (VBPM). Incentives for participation in PQRS ended in 2014. For select groups of more than 100 physicians, 2015 payments will be based on 2013 PQRS submissions, with a 1% cut for groups that didn’t submit data in 2013. For all physicians, failure to participate in 2015 will result in a downward adjustment of 2% in 2017. Participation will generate bonuses or penalties of 1%-4% in 2017, based on group size, claims-based cost data, and submission of PQRS quality data, via one of three mechanisms. The most attractive option for many groups will be submission of data for 50% of applicable patients via a Qualified Clinical Data Registry, such as the ASGE & ACG’s GI Quality Improvement Consortium (GIQUIC) or the AGA’s Digestive Health Registry (DHR).
Category 3 in the CMS payment taxonomy triggers reimbursement by delivery of care, but links it to episodes of care or to population management, with varied mechanisms for providers to share in the potential benefits and risks of cost extremes. Programs include Accountable Care Organizations (ACOs), medical homes for specified conditions, and shared savings for comprehensive primary care and end-stage renal disease. Presently, most employ a modest potential upside in reimbursement for savings but only limited downside risk. In 2015, ACOs cover about 23 million lives, or 7% of the population of the United States. Estimates suggest coverage of 72 million (22%) by 2020 (Leavitt Partners, Salt Lake, 2015).
In Category 4 of the CMS taxonomy, the Next Generation ACO Model drops all links between reimbursement and actual delivery of care, in favor of reimbursement for the assumption of care of individuals over time frames greater than 1 year, with greater participation in savings and risk. Several inducements and tools are included to enhance participation and the management of care, including: 1) reward to beneficiaries for participation, 2) reimbursement for skilled nursing care without prior hospitalization, and 3) expanded coverage for tele-health and home services. CMS aims to increase Categories 3 (alternative FFS) and 4 (population-based payment models) to 50% of covered individuals by 2018.
VBR by nongovernmental payers lags behind that of federal and state programs. CMS is currently testing more than 20 models for care and reimbursement, with aims to pull private payers into VBR and the final common pathway of management of populations while conserving health care resources (JAMA 2014;311:1967-8).
For gastroenterology, VBR will require practice redesign, with the expectation that physicians will focus their care toward their maximal level of licensure and privileging, while enabling employed advanced practice R.N.’s (certified nurse practitioner, or CNP) and physician assistants to do the same (Clin. Gastroenterol. Hepatol. 2014;12:1584-6 ).
This trend is already well established in many environments. Redesign is also stimulating consolidation of practices to better enable contracts for population management by the group. A second development will be increasing use of risk-bearing contracts for episodes of care, particularly for colorectal cancer surveillance and liver transplantation. Specialty medical homes, as opposed to primary care medical homes, will grow for care of inflammatory bowel disease and perhaps for chronic liver disease patients. Success with these initiatives, with both preservation of adequate reimbursement and appropriate constraint in delivery of care, will require extensive reliance on big data for demonstration of quality and patient engagement for optimizing the frequency and intensity of care.
Dr. Petersen is professor of medicine, Mayo Graduate School of Medicine, Mayo Clinic College of Medicine, Rochester, Minn. He has no conflicts of interest. His comments were made during the ASGE and AGA joint Presidential Plenary at the annual Digestive Disease Week.
Value in health care is often defined as “health outcomes achieved per dollar spent,” or “outcomes/costs.” Value encompasses efficiency, but is primarily results oriented and not based on volume. For purposes of comparison and assessment, value assessments apply to patient- and condition-specific episodes of care.
As the dominant driver of value-based reimbursement (VBR), the Center for Medicare & Medicaid Services, has defined a payment taxonomy for coming years based upon the degree of linkage between quality and reimbursement (JAMA 2014;311:1967-8). Four categories of reimbursement extend from traditional fee for service (FFS; Category 1) to FFS with significant reliance on quality measures and outcome (Cat. 2), entirely population-based models with payments stimulated by delivery of care (Cat. 3), and payment based entirely on capitated coverage of individuals over time (Cat. 4).
Category 2 reimbursement for physicians is largely based upon the Physicians Quality Reporting System (PQRS) with Value-Based Payment Modifiers (VBPM). Incentives for participation in PQRS ended in 2014. For select groups of more than 100 physicians, 2015 payments will be based on 2013 PQRS submissions, with a 1% cut for groups that didn’t submit data in 2013. For all physicians, failure to participate in 2015 will result in a downward adjustment of 2% in 2017. Participation will generate bonuses or penalties of 1%-4% in 2017, based on group size, claims-based cost data, and submission of PQRS quality data, via one of three mechanisms. The most attractive option for many groups will be submission of data for 50% of applicable patients via a Qualified Clinical Data Registry, such as the ASGE & ACG’s GI Quality Improvement Consortium (GIQUIC) or the AGA’s Digestive Health Registry (DHR).
Category 3 in the CMS payment taxonomy triggers reimbursement by delivery of care, but links it to episodes of care or to population management, with varied mechanisms for providers to share in the potential benefits and risks of cost extremes. Programs include Accountable Care Organizations (ACOs), medical homes for specified conditions, and shared savings for comprehensive primary care and end-stage renal disease. Presently, most employ a modest potential upside in reimbursement for savings but only limited downside risk. In 2015, ACOs cover about 23 million lives, or 7% of the population of the United States. Estimates suggest coverage of 72 million (22%) by 2020 (Leavitt Partners, Salt Lake, 2015).
In Category 4 of the CMS taxonomy, the Next Generation ACO Model drops all links between reimbursement and actual delivery of care, in favor of reimbursement for the assumption of care of individuals over time frames greater than 1 year, with greater participation in savings and risk. Several inducements and tools are included to enhance participation and the management of care, including: 1) reward to beneficiaries for participation, 2) reimbursement for skilled nursing care without prior hospitalization, and 3) expanded coverage for tele-health and home services. CMS aims to increase Categories 3 (alternative FFS) and 4 (population-based payment models) to 50% of covered individuals by 2018.
VBR by nongovernmental payers lags behind that of federal and state programs. CMS is currently testing more than 20 models for care and reimbursement, with aims to pull private payers into VBR and the final common pathway of management of populations while conserving health care resources (JAMA 2014;311:1967-8).
For gastroenterology, VBR will require practice redesign, with the expectation that physicians will focus their care toward their maximal level of licensure and privileging, while enabling employed advanced practice R.N.’s (certified nurse practitioner, or CNP) and physician assistants to do the same (Clin. Gastroenterol. Hepatol. 2014;12:1584-6 ).
This trend is already well established in many environments. Redesign is also stimulating consolidation of practices to better enable contracts for population management by the group. A second development will be increasing use of risk-bearing contracts for episodes of care, particularly for colorectal cancer surveillance and liver transplantation. Specialty medical homes, as opposed to primary care medical homes, will grow for care of inflammatory bowel disease and perhaps for chronic liver disease patients. Success with these initiatives, with both preservation of adequate reimbursement and appropriate constraint in delivery of care, will require extensive reliance on big data for demonstration of quality and patient engagement for optimizing the frequency and intensity of care.
Dr. Petersen is professor of medicine, Mayo Graduate School of Medicine, Mayo Clinic College of Medicine, Rochester, Minn. He has no conflicts of interest. His comments were made during the ASGE and AGA joint Presidential Plenary at the annual Digestive Disease Week.
Value in health care is often defined as “health outcomes achieved per dollar spent,” or “outcomes/costs.” Value encompasses efficiency, but is primarily results oriented and not based on volume. For purposes of comparison and assessment, value assessments apply to patient- and condition-specific episodes of care.
As the dominant driver of value-based reimbursement (VBR), the Center for Medicare & Medicaid Services, has defined a payment taxonomy for coming years based upon the degree of linkage between quality and reimbursement (JAMA 2014;311:1967-8). Four categories of reimbursement extend from traditional fee for service (FFS; Category 1) to FFS with significant reliance on quality measures and outcome (Cat. 2), entirely population-based models with payments stimulated by delivery of care (Cat. 3), and payment based entirely on capitated coverage of individuals over time (Cat. 4).
Category 2 reimbursement for physicians is largely based upon the Physicians Quality Reporting System (PQRS) with Value-Based Payment Modifiers (VBPM). Incentives for participation in PQRS ended in 2014. For select groups of more than 100 physicians, 2015 payments will be based on 2013 PQRS submissions, with a 1% cut for groups that didn’t submit data in 2013. For all physicians, failure to participate in 2015 will result in a downward adjustment of 2% in 2017. Participation will generate bonuses or penalties of 1%-4% in 2017, based on group size, claims-based cost data, and submission of PQRS quality data, via one of three mechanisms. The most attractive option for many groups will be submission of data for 50% of applicable patients via a Qualified Clinical Data Registry, such as the ASGE & ACG’s GI Quality Improvement Consortium (GIQUIC) or the AGA’s Digestive Health Registry (DHR).
Category 3 in the CMS payment taxonomy triggers reimbursement by delivery of care, but links it to episodes of care or to population management, with varied mechanisms for providers to share in the potential benefits and risks of cost extremes. Programs include Accountable Care Organizations (ACOs), medical homes for specified conditions, and shared savings for comprehensive primary care and end-stage renal disease. Presently, most employ a modest potential upside in reimbursement for savings but only limited downside risk. In 2015, ACOs cover about 23 million lives, or 7% of the population of the United States. Estimates suggest coverage of 72 million (22%) by 2020 (Leavitt Partners, Salt Lake, 2015).
In Category 4 of the CMS taxonomy, the Next Generation ACO Model drops all links between reimbursement and actual delivery of care, in favor of reimbursement for the assumption of care of individuals over time frames greater than 1 year, with greater participation in savings and risk. Several inducements and tools are included to enhance participation and the management of care, including: 1) reward to beneficiaries for participation, 2) reimbursement for skilled nursing care without prior hospitalization, and 3) expanded coverage for tele-health and home services. CMS aims to increase Categories 3 (alternative FFS) and 4 (population-based payment models) to 50% of covered individuals by 2018.
VBR by nongovernmental payers lags behind that of federal and state programs. CMS is currently testing more than 20 models for care and reimbursement, with aims to pull private payers into VBR and the final common pathway of management of populations while conserving health care resources (JAMA 2014;311:1967-8).
For gastroenterology, VBR will require practice redesign, with the expectation that physicians will focus their care toward their maximal level of licensure and privileging, while enabling employed advanced practice R.N.’s (certified nurse practitioner, or CNP) and physician assistants to do the same (Clin. Gastroenterol. Hepatol. 2014;12:1584-6 ).
This trend is already well established in many environments. Redesign is also stimulating consolidation of practices to better enable contracts for population management by the group. A second development will be increasing use of risk-bearing contracts for episodes of care, particularly for colorectal cancer surveillance and liver transplantation. Specialty medical homes, as opposed to primary care medical homes, will grow for care of inflammatory bowel disease and perhaps for chronic liver disease patients. Success with these initiatives, with both preservation of adequate reimbursement and appropriate constraint in delivery of care, will require extensive reliance on big data for demonstration of quality and patient engagement for optimizing the frequency and intensity of care.
Dr. Petersen is professor of medicine, Mayo Graduate School of Medicine, Mayo Clinic College of Medicine, Rochester, Minn. He has no conflicts of interest. His comments were made during the ASGE and AGA joint Presidential Plenary at the annual Digestive Disease Week.
DDW: Study finds pancreatic cancer misdiagnosis rate at 31%
WASHINGTON – Initial misdiagnoses were common and were associated with a later disease stage at diagnosis, in a study of 313 patients diagnosed with pancreatic cancer, Dr. Douglas Swords said at the annual Digestive Disease Week.
“By far, the most common misdiagnosis was gallbladder disease,” and there was about a 3-month longer time period, on average, from the first visit to a physician to the actual cancer diagnosis, in patients who were initially misdiagnosed, said Dr. Swords, a surgery resident at the University of Utah, Salt Lake City.
In the series of 313 patients diagnosed with pancreatic cancer, 98 (31.3%) were initially misdiagnosed, with a total of 119 diagnoses other than pancreatic cancer, he said. The most common misdiagnosis was gallbladder disease, which led to a cholecystectomy in 38 cases, followed by gastroesophageal reflux disease in 15 cases, and peptic ulcer disease in 11 cases. Those initially misdiagnosed were an average of about 5 years younger.
Patients with an initial misdiagnosis had significantly greater rates of abdominal pain (about 85% vs. about 60%), weight loss (about 85% vs. about 75%), nausea/vomiting (50% vs. almost 40%), and pancreatitis (almost 30% vs. less than 5%), Dr. Swords said. In addition, patients with an initial misdiagnosis had significantly lower rates of jaundice (about 50% vs. almost 80%). The rates of diarrhea and anorexia were not significantly different between the two groups.
The study also looked at the time intervals from when the patient developed symptoms to the physician visit, from the physician visit to the cancer diagnosis, and from the physician visit to the performance of axial imaging. There was no difference in the time of symptom onset to the first visit with a physician in the two groups (0.5 month among those initially misdiagnosed and 0.7 month among those correctly diagnosed).
However, the time from the physician visit to the cancer diagnosis was 3.5 months among those initially misdiagnosed, vs. less than a month (0.6 month) among those who were correctly diagnosed, a statistically significant difference (P <.001), he said.
In addition, for those patients initially misdiagnosed, it took about 1 month longer from the physician visit to the time a CT scan or other type of axial imaging was ordered (an average of 1.1 months vs. 0.1 month, P <.001).
There was also a statistically significant association between a more advanced stage and initial misdiagnosis. Patients who were initially misdiagnosed had a 1.4-fold greater risk of having stage III or IV disease at the time of the pancreatic cancer diagnosis, Dr. Swords said.
Almost 40% (39) of those who were initially misdiagnosed were diagnosed with stage IV disease when they were correctly diagnosed, compared with 23.7% (51 patients) of those who were correctly diagnosed. The proportion diagnosed with stage III disease was similar, 21.4% among those initially misdiagnosed and 20% of those correctly diagnosed. Almost 51% of those correctly diagnosed were diagnosed with stage II disease, vs. 33.7% of those who were initially misdiagnosed. Of those initially misdiagnosed, 5.1% were diagnosed with stage I disease, compared with 5.6% of those correctly diagnosed.
However, the earlier stage at diagnosis for those with an initial correct diagnosis “did not translate into a survival difference,” Dr. Swords said, noting that there was a trend toward shorter survival among those who were initially misdiagnosed (median overall survival of 9.6 vs. 10.3 months).
Based on these results, Dr. Swords said, “surgeons should consider the diagnosis of pancreatic cancer when a patient referred for cholecystectomy has vague or atypical symptoms.”
He said he had no relevant financial disclosures.
WASHINGTON – Initial misdiagnoses were common and were associated with a later disease stage at diagnosis, in a study of 313 patients diagnosed with pancreatic cancer, Dr. Douglas Swords said at the annual Digestive Disease Week.
“By far, the most common misdiagnosis was gallbladder disease,” and there was about a 3-month longer time period, on average, from the first visit to a physician to the actual cancer diagnosis, in patients who were initially misdiagnosed, said Dr. Swords, a surgery resident at the University of Utah, Salt Lake City.
In the series of 313 patients diagnosed with pancreatic cancer, 98 (31.3%) were initially misdiagnosed, with a total of 119 diagnoses other than pancreatic cancer, he said. The most common misdiagnosis was gallbladder disease, which led to a cholecystectomy in 38 cases, followed by gastroesophageal reflux disease in 15 cases, and peptic ulcer disease in 11 cases. Those initially misdiagnosed were an average of about 5 years younger.
Patients with an initial misdiagnosis had significantly greater rates of abdominal pain (about 85% vs. about 60%), weight loss (about 85% vs. about 75%), nausea/vomiting (50% vs. almost 40%), and pancreatitis (almost 30% vs. less than 5%), Dr. Swords said. In addition, patients with an initial misdiagnosis had significantly lower rates of jaundice (about 50% vs. almost 80%). The rates of diarrhea and anorexia were not significantly different between the two groups.
The study also looked at the time intervals from when the patient developed symptoms to the physician visit, from the physician visit to the cancer diagnosis, and from the physician visit to the performance of axial imaging. There was no difference in the time of symptom onset to the first visit with a physician in the two groups (0.5 month among those initially misdiagnosed and 0.7 month among those correctly diagnosed).
However, the time from the physician visit to the cancer diagnosis was 3.5 months among those initially misdiagnosed, vs. less than a month (0.6 month) among those who were correctly diagnosed, a statistically significant difference (P <.001), he said.
In addition, for those patients initially misdiagnosed, it took about 1 month longer from the physician visit to the time a CT scan or other type of axial imaging was ordered (an average of 1.1 months vs. 0.1 month, P <.001).
There was also a statistically significant association between a more advanced stage and initial misdiagnosis. Patients who were initially misdiagnosed had a 1.4-fold greater risk of having stage III or IV disease at the time of the pancreatic cancer diagnosis, Dr. Swords said.
Almost 40% (39) of those who were initially misdiagnosed were diagnosed with stage IV disease when they were correctly diagnosed, compared with 23.7% (51 patients) of those who were correctly diagnosed. The proportion diagnosed with stage III disease was similar, 21.4% among those initially misdiagnosed and 20% of those correctly diagnosed. Almost 51% of those correctly diagnosed were diagnosed with stage II disease, vs. 33.7% of those who were initially misdiagnosed. Of those initially misdiagnosed, 5.1% were diagnosed with stage I disease, compared with 5.6% of those correctly diagnosed.
However, the earlier stage at diagnosis for those with an initial correct diagnosis “did not translate into a survival difference,” Dr. Swords said, noting that there was a trend toward shorter survival among those who were initially misdiagnosed (median overall survival of 9.6 vs. 10.3 months).
Based on these results, Dr. Swords said, “surgeons should consider the diagnosis of pancreatic cancer when a patient referred for cholecystectomy has vague or atypical symptoms.”
He said he had no relevant financial disclosures.
WASHINGTON – Initial misdiagnoses were common and were associated with a later disease stage at diagnosis, in a study of 313 patients diagnosed with pancreatic cancer, Dr. Douglas Swords said at the annual Digestive Disease Week.
“By far, the most common misdiagnosis was gallbladder disease,” and there was about a 3-month longer time period, on average, from the first visit to a physician to the actual cancer diagnosis, in patients who were initially misdiagnosed, said Dr. Swords, a surgery resident at the University of Utah, Salt Lake City.
In the series of 313 patients diagnosed with pancreatic cancer, 98 (31.3%) were initially misdiagnosed, with a total of 119 diagnoses other than pancreatic cancer, he said. The most common misdiagnosis was gallbladder disease, which led to a cholecystectomy in 38 cases, followed by gastroesophageal reflux disease in 15 cases, and peptic ulcer disease in 11 cases. Those initially misdiagnosed were an average of about 5 years younger.
Patients with an initial misdiagnosis had significantly greater rates of abdominal pain (about 85% vs. about 60%), weight loss (about 85% vs. about 75%), nausea/vomiting (50% vs. almost 40%), and pancreatitis (almost 30% vs. less than 5%), Dr. Swords said. In addition, patients with an initial misdiagnosis had significantly lower rates of jaundice (about 50% vs. almost 80%). The rates of diarrhea and anorexia were not significantly different between the two groups.
The study also looked at the time intervals from when the patient developed symptoms to the physician visit, from the physician visit to the cancer diagnosis, and from the physician visit to the performance of axial imaging. There was no difference in the time of symptom onset to the first visit with a physician in the two groups (0.5 month among those initially misdiagnosed and 0.7 month among those correctly diagnosed).
However, the time from the physician visit to the cancer diagnosis was 3.5 months among those initially misdiagnosed, vs. less than a month (0.6 month) among those who were correctly diagnosed, a statistically significant difference (P <.001), he said.
In addition, for those patients initially misdiagnosed, it took about 1 month longer from the physician visit to the time a CT scan or other type of axial imaging was ordered (an average of 1.1 months vs. 0.1 month, P <.001).
There was also a statistically significant association between a more advanced stage and initial misdiagnosis. Patients who were initially misdiagnosed had a 1.4-fold greater risk of having stage III or IV disease at the time of the pancreatic cancer diagnosis, Dr. Swords said.
Almost 40% (39) of those who were initially misdiagnosed were diagnosed with stage IV disease when they were correctly diagnosed, compared with 23.7% (51 patients) of those who were correctly diagnosed. The proportion diagnosed with stage III disease was similar, 21.4% among those initially misdiagnosed and 20% of those correctly diagnosed. Almost 51% of those correctly diagnosed were diagnosed with stage II disease, vs. 33.7% of those who were initially misdiagnosed. Of those initially misdiagnosed, 5.1% were diagnosed with stage I disease, compared with 5.6% of those correctly diagnosed.
However, the earlier stage at diagnosis for those with an initial correct diagnosis “did not translate into a survival difference,” Dr. Swords said, noting that there was a trend toward shorter survival among those who were initially misdiagnosed (median overall survival of 9.6 vs. 10.3 months).
Based on these results, Dr. Swords said, “surgeons should consider the diagnosis of pancreatic cancer when a patient referred for cholecystectomy has vague or atypical symptoms.”
He said he had no relevant financial disclosures.
AT DDW® 2015
Key clinical point: Pancreatic cancer is often misdiagnosed, and should be considered in patients with vague or atypical symptoms who are referred for a cholecystectomy.
Major finding: About 31% of patients with pancreatic cancer were initially misdiagnosed, most often with a gallbladder disease–related diagnosis.
Data source: A study of 313 patients diagnosed with pancreatic cancer comparing presenting symptoms, the time it took to reach the correct diagnosis, and other features in patients initially misdiagnosed and those who were not misdiagnosed.
Disclosures: Dr. Swords said he had no relevant financial disclosures.
DDW: LINX device beneficial, safe for GERD
WASHINGTON – Five-year follow-up data on the magnetic device approved for treating gastroesophageal reflux disease confirm its long-term safety and efficacy, Dr. Robert A. Ganz reported at the annual Digestive Disease Week.
Five years after device implantation, the proportion of patients experiencing moderate to severe regurgitation had dropped to about 1%, from almost 60% at baseline, and two-thirds of patients were not taking any proton pump inhibitors (PPIs), said Dr. Ganz, chief of gastroenterology at Abbott Northwestern Hospital, Minneapolis, and one of the study investigators. These were among the results of the study that evaluated the device, the LINX Reflux Management System. The device was approved by the Food and Drug Administration FDA) in 2012 and is for the treatment of people with GERD as defined by abnormal pH testing, who continue to have chronic GERD symptoms that persist despite maximum medical therapy for the treatment of reflux.
“Magnetic sphincter augmentation should be considered first-line surgical therapy for those with gastroesophageal reflux disease, based on the results of this study,” he said.
The 2-year results of the prospective, multicenter study were the basis of the FDA approval of the device, described by the manufacturer, Torax Medical, as a “small implant [composed] of interlinked titanium beads with magnetic cores,” implanted during standard laparoscopy. The magnetic attraction between the beads augments the existing esophageal sphincter’s barrier function to prevent reflux,” according to the company.
The study enrolled 100 patients with reflux disease with a median age of 53 years, who had experienced typical heartburn for at least 6 months with or without regurgitation and were taking PPIs daily for at least 3 months (median use 5 years). Patients had GERD for a median of 10 years (range: 1-40 years). People who had any type of previous gastric or esophageal surgery, Barrett’s esophagus, a hiatal hernia greater than 3 cm, a body mass index over 35 kg/m2, or grade C or D esophagitis were excluded.
The device was implanted in all patients, who served as their own controls; 85 patients were followed through 5 years (6 were lost to follow-up, the device was explanted in 6 patients, 2 patients did not consent to extended follow-up, and 1 patient died of an unrelated cancer). The median procedure time was 36 minutes with a range of 7-125 minutes); all procedures were successfully completed with no intraoperative complications and all patients were discharged within 24 hours on an unrestricted diet.
The median total Gastroesophageal Reflux Disease–Health-Related Quality of Life (GERD-HRQL) score at baseline was 27 points among those not on PPIs and 11 points on PPIs, dropping to 4 points at 5 years off PPIs. At baseline, 95% of patients expressed dissatisfaction related to reflux, which dropped to 7% at year 5. Moderate to severe heartburn was reported by 89% at baseline, dropping to about 12% at year 5. The proportion of patients experiencing moderate to severe regurgitation dropped from 57% at baseline to about 1% at 5 years, Dr. Ganz said.
At baseline, 100% were taking PPIs every day, compared with 15% at 5 years. (At 5 years, 75% had discontinued PPIs, and about 9% reported PRN use only). Grade A and B esophagitis decreased from 40% at baseline to 16% at 5 years, at which point most cases were grade A, and there were no patients with grade C or D esophagitis, he said. In addition, at 5 years, 100% of patients “reported the ability to belch, and those needing to vomit – about 16% – reported the ability to vomit,” demonstrating that normal physiology was preserved with the device.
At 5 years, there were no device erosions or migrations, or any significant adverse events other than dysphagia, which “was typically mild and not associated with weight loss and tended to resolve over time,” from about 70% in the first few weeks after surgery to 11% at 1 year and 7% at 5 years, Dr. Ganz said.
In seven cases, the device was removed laparoscopically, with no complications and gastric anatomy was preserved for future treatments. All removals were elective. The device was removed in four patients because of dysphagia, which completely resolved in those patients. One patient had the device removed because of vomiting of unknown cause that persisted after removal. Another two patients who “had the device removed for disease management” continued to experience reflux and had “uneventful” Nissen fundoplication,” he said.
“Five years after magnetic augmentation, we have demonstrated objective evidence of reduction in acid exposure and in the majority of patients, normalized pH [and] we demonstrated significant and durable improvement in all group parameters measured, with preservation of fundic anatomy and normal physiology, with the ability to belch and vomit,” Dr. Ganz concluded. The results also show that the “procedure is reproducible, safe and reversible if necessary,” he added, noting that one of the limitations of the study was that subjects served as their own controls. During the discussion period, he was asked about hiatal hernia repairs, an apparent trend to “decay” from years 1 to 5 in some parameters measured, and dysphagia after the procedure.
About 40% of the patients in the study had a hiatal hernia, and about one-third of these patients had a hernia repair. A subgroup analysis of the data is being performed to evaluate the impact of hernia repair, Dr. Ganz said.
PPI use increased from 8% in year 4, to 15% in year 5. The reason for this s difficult to determine but “even though there is a bit of a decay, patients are still quite satisfied at 5 years,” Dr. Ganz remarked, also referring to the marked impact on regurgitation. Many U.S. patients use PPIs for reasons other than reflux, and studies show that many patients are on PPIs after the Nissen procedure in the absence of pathologic pH scores, he pointed out.
Compared with the type of dysphagia patients experience after the Nissen procedure, which is immediate and improves with time, Dr. Ganz said that the dysphagia associated with the device “seemed to peak around 2 weeks and then it slowly improved with time, so this may be more of a scar tissue–associated dysphagia than an edema dysphagia, but … it does improve with time.
Three-year results of the study were published in 2013 (N. Engl. J. Med. 2013;368:719-72), Dr. Ganz was the lead author.
The study was funded by Torax Medical. Dr. Ganz had no disclosures related to the topic of this presentation.
*This story was updated 7/9/2015.
At DDW this year, Dr. Ganz reported on the 5-year follow-up of the original LINX data that was published in the New England Journal of Medicine in 2013 (368:2039-40). The original study enrolled and followed 100 reflux patients for 3 years after implantation of the magnetic sphincter augmentation device, and it appears that the successful outcomes are sustained over the 5-year period. Most notable are the lasting improvement in regurgitation and the dramatic reduction in requirement for maintenance PPI therapy. These findings led the investigators to suggest that this should be considered a first-line surgical therapy for GERD. Overall, this is not an unreasonable statement when one considers the current model wherein antireflux surgery fits in the treatment of GERD. Medical therapy with proton pump inhibitors is extremely safe and effective for a substantial number of patients with GERD and based on this risk/benefit profile should be the first line therapy (Am. J. Gastroenterol. 2013;108:308-28; quiz 329). However, this treatment is not perfect and there are many patients who continue to have persistent symptoms despite PPI therapy (Clin. Gastroenterol. Hepatol. 2012;10:612-9). Although the majority of PPI nonresponders have a functional etiology, there is a distinct population that continue to have refractory reflux-related symptoms, such as regurgitation, that escape the therapeutic target of PPIs. These patients will require an augmentation of the antireflux barrier and the LINX approach appears to be as effective as fundoplication in this regard (J. Am. Coll. Surg. 2015;221:123-8). The question is whether the side effect profile and durability of LINX is better than fundoplication. The answer here is not clear and I would carefully state that LINX and fundoplication can be considered first-line surgical therapies for GERD patients who have documented pathologic acid gastroesophageal reflux and are intolerant to PPIs or not responding to PPIs.
Dr. John E. Pandolfino is professor of medicine and chief of the division of gastroenterology and hepatology at Northwestern University, Chicago. He is a speaker for Astra Zeneca/Takeda and a consultant for EndoGastric Solutions.
At DDW this year, Dr. Ganz reported on the 5-year follow-up of the original LINX data that was published in the New England Journal of Medicine in 2013 (368:2039-40). The original study enrolled and followed 100 reflux patients for 3 years after implantation of the magnetic sphincter augmentation device, and it appears that the successful outcomes are sustained over the 5-year period. Most notable are the lasting improvement in regurgitation and the dramatic reduction in requirement for maintenance PPI therapy. These findings led the investigators to suggest that this should be considered a first-line surgical therapy for GERD. Overall, this is not an unreasonable statement when one considers the current model wherein antireflux surgery fits in the treatment of GERD. Medical therapy with proton pump inhibitors is extremely safe and effective for a substantial number of patients with GERD and based on this risk/benefit profile should be the first line therapy (Am. J. Gastroenterol. 2013;108:308-28; quiz 329). However, this treatment is not perfect and there are many patients who continue to have persistent symptoms despite PPI therapy (Clin. Gastroenterol. Hepatol. 2012;10:612-9). Although the majority of PPI nonresponders have a functional etiology, there is a distinct population that continue to have refractory reflux-related symptoms, such as regurgitation, that escape the therapeutic target of PPIs. These patients will require an augmentation of the antireflux barrier and the LINX approach appears to be as effective as fundoplication in this regard (J. Am. Coll. Surg. 2015;221:123-8). The question is whether the side effect profile and durability of LINX is better than fundoplication. The answer here is not clear and I would carefully state that LINX and fundoplication can be considered first-line surgical therapies for GERD patients who have documented pathologic acid gastroesophageal reflux and are intolerant to PPIs or not responding to PPIs.
Dr. John E. Pandolfino is professor of medicine and chief of the division of gastroenterology and hepatology at Northwestern University, Chicago. He is a speaker for Astra Zeneca/Takeda and a consultant for EndoGastric Solutions.
At DDW this year, Dr. Ganz reported on the 5-year follow-up of the original LINX data that was published in the New England Journal of Medicine in 2013 (368:2039-40). The original study enrolled and followed 100 reflux patients for 3 years after implantation of the magnetic sphincter augmentation device, and it appears that the successful outcomes are sustained over the 5-year period. Most notable are the lasting improvement in regurgitation and the dramatic reduction in requirement for maintenance PPI therapy. These findings led the investigators to suggest that this should be considered a first-line surgical therapy for GERD. Overall, this is not an unreasonable statement when one considers the current model wherein antireflux surgery fits in the treatment of GERD. Medical therapy with proton pump inhibitors is extremely safe and effective for a substantial number of patients with GERD and based on this risk/benefit profile should be the first line therapy (Am. J. Gastroenterol. 2013;108:308-28; quiz 329). However, this treatment is not perfect and there are many patients who continue to have persistent symptoms despite PPI therapy (Clin. Gastroenterol. Hepatol. 2012;10:612-9). Although the majority of PPI nonresponders have a functional etiology, there is a distinct population that continue to have refractory reflux-related symptoms, such as regurgitation, that escape the therapeutic target of PPIs. These patients will require an augmentation of the antireflux barrier and the LINX approach appears to be as effective as fundoplication in this regard (J. Am. Coll. Surg. 2015;221:123-8). The question is whether the side effect profile and durability of LINX is better than fundoplication. The answer here is not clear and I would carefully state that LINX and fundoplication can be considered first-line surgical therapies for GERD patients who have documented pathologic acid gastroesophageal reflux and are intolerant to PPIs or not responding to PPIs.
Dr. John E. Pandolfino is professor of medicine and chief of the division of gastroenterology and hepatology at Northwestern University, Chicago. He is a speaker for Astra Zeneca/Takeda and a consultant for EndoGastric Solutions.
WASHINGTON – Five-year follow-up data on the magnetic device approved for treating gastroesophageal reflux disease confirm its long-term safety and efficacy, Dr. Robert A. Ganz reported at the annual Digestive Disease Week.
Five years after device implantation, the proportion of patients experiencing moderate to severe regurgitation had dropped to about 1%, from almost 60% at baseline, and two-thirds of patients were not taking any proton pump inhibitors (PPIs), said Dr. Ganz, chief of gastroenterology at Abbott Northwestern Hospital, Minneapolis, and one of the study investigators. These were among the results of the study that evaluated the device, the LINX Reflux Management System. The device was approved by the Food and Drug Administration FDA) in 2012 and is for the treatment of people with GERD as defined by abnormal pH testing, who continue to have chronic GERD symptoms that persist despite maximum medical therapy for the treatment of reflux.
“Magnetic sphincter augmentation should be considered first-line surgical therapy for those with gastroesophageal reflux disease, based on the results of this study,” he said.
The 2-year results of the prospective, multicenter study were the basis of the FDA approval of the device, described by the manufacturer, Torax Medical, as a “small implant [composed] of interlinked titanium beads with magnetic cores,” implanted during standard laparoscopy. The magnetic attraction between the beads augments the existing esophageal sphincter’s barrier function to prevent reflux,” according to the company.
The study enrolled 100 patients with reflux disease with a median age of 53 years, who had experienced typical heartburn for at least 6 months with or without regurgitation and were taking PPIs daily for at least 3 months (median use 5 years). Patients had GERD for a median of 10 years (range: 1-40 years). People who had any type of previous gastric or esophageal surgery, Barrett’s esophagus, a hiatal hernia greater than 3 cm, a body mass index over 35 kg/m2, or grade C or D esophagitis were excluded.
The device was implanted in all patients, who served as their own controls; 85 patients were followed through 5 years (6 were lost to follow-up, the device was explanted in 6 patients, 2 patients did not consent to extended follow-up, and 1 patient died of an unrelated cancer). The median procedure time was 36 minutes with a range of 7-125 minutes); all procedures were successfully completed with no intraoperative complications and all patients were discharged within 24 hours on an unrestricted diet.
The median total Gastroesophageal Reflux Disease–Health-Related Quality of Life (GERD-HRQL) score at baseline was 27 points among those not on PPIs and 11 points on PPIs, dropping to 4 points at 5 years off PPIs. At baseline, 95% of patients expressed dissatisfaction related to reflux, which dropped to 7% at year 5. Moderate to severe heartburn was reported by 89% at baseline, dropping to about 12% at year 5. The proportion of patients experiencing moderate to severe regurgitation dropped from 57% at baseline to about 1% at 5 years, Dr. Ganz said.
At baseline, 100% were taking PPIs every day, compared with 15% at 5 years. (At 5 years, 75% had discontinued PPIs, and about 9% reported PRN use only). Grade A and B esophagitis decreased from 40% at baseline to 16% at 5 years, at which point most cases were grade A, and there were no patients with grade C or D esophagitis, he said. In addition, at 5 years, 100% of patients “reported the ability to belch, and those needing to vomit – about 16% – reported the ability to vomit,” demonstrating that normal physiology was preserved with the device.
At 5 years, there were no device erosions or migrations, or any significant adverse events other than dysphagia, which “was typically mild and not associated with weight loss and tended to resolve over time,” from about 70% in the first few weeks after surgery to 11% at 1 year and 7% at 5 years, Dr. Ganz said.
In seven cases, the device was removed laparoscopically, with no complications and gastric anatomy was preserved for future treatments. All removals were elective. The device was removed in four patients because of dysphagia, which completely resolved in those patients. One patient had the device removed because of vomiting of unknown cause that persisted after removal. Another two patients who “had the device removed for disease management” continued to experience reflux and had “uneventful” Nissen fundoplication,” he said.
“Five years after magnetic augmentation, we have demonstrated objective evidence of reduction in acid exposure and in the majority of patients, normalized pH [and] we demonstrated significant and durable improvement in all group parameters measured, with preservation of fundic anatomy and normal physiology, with the ability to belch and vomit,” Dr. Ganz concluded. The results also show that the “procedure is reproducible, safe and reversible if necessary,” he added, noting that one of the limitations of the study was that subjects served as their own controls. During the discussion period, he was asked about hiatal hernia repairs, an apparent trend to “decay” from years 1 to 5 in some parameters measured, and dysphagia after the procedure.
About 40% of the patients in the study had a hiatal hernia, and about one-third of these patients had a hernia repair. A subgroup analysis of the data is being performed to evaluate the impact of hernia repair, Dr. Ganz said.
PPI use increased from 8% in year 4, to 15% in year 5. The reason for this s difficult to determine but “even though there is a bit of a decay, patients are still quite satisfied at 5 years,” Dr. Ganz remarked, also referring to the marked impact on regurgitation. Many U.S. patients use PPIs for reasons other than reflux, and studies show that many patients are on PPIs after the Nissen procedure in the absence of pathologic pH scores, he pointed out.
Compared with the type of dysphagia patients experience after the Nissen procedure, which is immediate and improves with time, Dr. Ganz said that the dysphagia associated with the device “seemed to peak around 2 weeks and then it slowly improved with time, so this may be more of a scar tissue–associated dysphagia than an edema dysphagia, but … it does improve with time.
Three-year results of the study were published in 2013 (N. Engl. J. Med. 2013;368:719-72), Dr. Ganz was the lead author.
The study was funded by Torax Medical. Dr. Ganz had no disclosures related to the topic of this presentation.
*This story was updated 7/9/2015.
WASHINGTON – Five-year follow-up data on the magnetic device approved for treating gastroesophageal reflux disease confirm its long-term safety and efficacy, Dr. Robert A. Ganz reported at the annual Digestive Disease Week.
Five years after device implantation, the proportion of patients experiencing moderate to severe regurgitation had dropped to about 1%, from almost 60% at baseline, and two-thirds of patients were not taking any proton pump inhibitors (PPIs), said Dr. Ganz, chief of gastroenterology at Abbott Northwestern Hospital, Minneapolis, and one of the study investigators. These were among the results of the study that evaluated the device, the LINX Reflux Management System. The device was approved by the Food and Drug Administration FDA) in 2012 and is for the treatment of people with GERD as defined by abnormal pH testing, who continue to have chronic GERD symptoms that persist despite maximum medical therapy for the treatment of reflux.
“Magnetic sphincter augmentation should be considered first-line surgical therapy for those with gastroesophageal reflux disease, based on the results of this study,” he said.
The 2-year results of the prospective, multicenter study were the basis of the FDA approval of the device, described by the manufacturer, Torax Medical, as a “small implant [composed] of interlinked titanium beads with magnetic cores,” implanted during standard laparoscopy. The magnetic attraction between the beads augments the existing esophageal sphincter’s barrier function to prevent reflux,” according to the company.
The study enrolled 100 patients with reflux disease with a median age of 53 years, who had experienced typical heartburn for at least 6 months with or without regurgitation and were taking PPIs daily for at least 3 months (median use 5 years). Patients had GERD for a median of 10 years (range: 1-40 years). People who had any type of previous gastric or esophageal surgery, Barrett’s esophagus, a hiatal hernia greater than 3 cm, a body mass index over 35 kg/m2, or grade C or D esophagitis were excluded.
The device was implanted in all patients, who served as their own controls; 85 patients were followed through 5 years (6 were lost to follow-up, the device was explanted in 6 patients, 2 patients did not consent to extended follow-up, and 1 patient died of an unrelated cancer). The median procedure time was 36 minutes with a range of 7-125 minutes); all procedures were successfully completed with no intraoperative complications and all patients were discharged within 24 hours on an unrestricted diet.
The median total Gastroesophageal Reflux Disease–Health-Related Quality of Life (GERD-HRQL) score at baseline was 27 points among those not on PPIs and 11 points on PPIs, dropping to 4 points at 5 years off PPIs. At baseline, 95% of patients expressed dissatisfaction related to reflux, which dropped to 7% at year 5. Moderate to severe heartburn was reported by 89% at baseline, dropping to about 12% at year 5. The proportion of patients experiencing moderate to severe regurgitation dropped from 57% at baseline to about 1% at 5 years, Dr. Ganz said.
At baseline, 100% were taking PPIs every day, compared with 15% at 5 years. (At 5 years, 75% had discontinued PPIs, and about 9% reported PRN use only). Grade A and B esophagitis decreased from 40% at baseline to 16% at 5 years, at which point most cases were grade A, and there were no patients with grade C or D esophagitis, he said. In addition, at 5 years, 100% of patients “reported the ability to belch, and those needing to vomit – about 16% – reported the ability to vomit,” demonstrating that normal physiology was preserved with the device.
At 5 years, there were no device erosions or migrations, or any significant adverse events other than dysphagia, which “was typically mild and not associated with weight loss and tended to resolve over time,” from about 70% in the first few weeks after surgery to 11% at 1 year and 7% at 5 years, Dr. Ganz said.
In seven cases, the device was removed laparoscopically, with no complications and gastric anatomy was preserved for future treatments. All removals were elective. The device was removed in four patients because of dysphagia, which completely resolved in those patients. One patient had the device removed because of vomiting of unknown cause that persisted after removal. Another two patients who “had the device removed for disease management” continued to experience reflux and had “uneventful” Nissen fundoplication,” he said.
“Five years after magnetic augmentation, we have demonstrated objective evidence of reduction in acid exposure and in the majority of patients, normalized pH [and] we demonstrated significant and durable improvement in all group parameters measured, with preservation of fundic anatomy and normal physiology, with the ability to belch and vomit,” Dr. Ganz concluded. The results also show that the “procedure is reproducible, safe and reversible if necessary,” he added, noting that one of the limitations of the study was that subjects served as their own controls. During the discussion period, he was asked about hiatal hernia repairs, an apparent trend to “decay” from years 1 to 5 in some parameters measured, and dysphagia after the procedure.
About 40% of the patients in the study had a hiatal hernia, and about one-third of these patients had a hernia repair. A subgroup analysis of the data is being performed to evaluate the impact of hernia repair, Dr. Ganz said.
PPI use increased from 8% in year 4, to 15% in year 5. The reason for this s difficult to determine but “even though there is a bit of a decay, patients are still quite satisfied at 5 years,” Dr. Ganz remarked, also referring to the marked impact on regurgitation. Many U.S. patients use PPIs for reasons other than reflux, and studies show that many patients are on PPIs after the Nissen procedure in the absence of pathologic pH scores, he pointed out.
Compared with the type of dysphagia patients experience after the Nissen procedure, which is immediate and improves with time, Dr. Ganz said that the dysphagia associated with the device “seemed to peak around 2 weeks and then it slowly improved with time, so this may be more of a scar tissue–associated dysphagia than an edema dysphagia, but … it does improve with time.
Three-year results of the study were published in 2013 (N. Engl. J. Med. 2013;368:719-72), Dr. Ganz was the lead author.
The study was funded by Torax Medical. Dr. Ganz had no disclosures related to the topic of this presentation.
*This story was updated 7/9/2015.
AT DDW 2015
Key clinical point: A magnetic device designed to augment the lower esophageal sphincter is a surgical option that can be expected to provide long-term control of reflux symptoms in patients with GERD.
Major finding: Improvements 5 years after treatment with the Linx Reflux Management System include a drop from 60% experiencing regurgitation to 1%, and two-third of patients no longer taking PPIs.
Data source: The multicenter, prospective study evaluated the long-term safety and efficacy of the device over 5 years in 100 patients with GERD, who served as their own controls; 85 were included in the 5-year follow-up.
Disclosures: The study was funded by the device manufacturer, Torax Medical. Dr. Ganz had no disclosures related to the topic of this presentation.
DDW: Antibiotic rifaximin eases functional dyspepsia
WASHINGTON – Two weeks of antibiotic therapy with rifaximin provided relief from functional dyspepsia symptoms in a phase III double-blind, randomized trial.
“This is the first study that demonstrates that rifaximin is efficacious in the treatment of functional dyspepsia, particularly for global dyspeptic symptoms, bloating, and possibly belching. Our finding may suggest a role for the gut microbiota in the pathogenesis of functional dyspepsia,” Dr. Victoria Tan said at the annual Digestive Disease Week.
Rifaximin (Xifaxan) works by reducing or altering bacteria in the gut and has been shown to be efficacious in the treatment of diarrhea-predominant irritable bowel syndrome. It is approved to treat traveler’s diarrhea caused by Escherichia coli and to prevent hepatic encephalopathy.
The study randomly assigned 95 consecutive adults with functional dyspepsia as per ROME III criteria who had a normal gastroscopy within the last 2 years, had active symptoms in the month prior to enrollment, and were Helicobacter pylori negative, to rifaximin 400 mg or placebo three times a day for 2 weeks. In all, 33 rifaximin and 39 placebo patients were evaluable for the primary efficacy outcome of adequate relief of global dyspeptic symptoms (either no or mild dyspeptic symptoms) at any of the follow-up time points.
At baseline, 77% of patients had moderate to severe global dyspepsia symptoms, 74% of the placebo group and 55%% of the rifaximin group had moderate to severe belching, and roughly half of all patients were not on any GI medications. Mean age of the patients was 52 years.
Global dyspepsia symptoms improved with rifaximin beginning at week 2 and significantly favored rifaximin by week 8, with 23.5% of rifaximin patients reporting moderate to severe symptoms compared with 47.4% given placebo (P value = .04), said Dr. Tan of the University of Hong Kong.
Rates of moderate to severe belching were significantly improved with rifaximin at week 4 compared with placebo (14.3% vs. 35.7%; P = .03), but this difference was no longer significant at week 8 (26.5% vs. 29%).
The story was similar for moderate to severe bloating: Rates declined significantly with rifaximin at week 4 (20% vs. 43%; P = .03), but were no longer significant at week 8 (26.5% vs. 34.2%), she said.
A subgroup analysis of female patients showed significant improvements in moderate to severe global dyspeptic symptoms with rifaximin compared with placebo at week 4 (20.8% vs. 59.4%; P = .006) and week 8 (20% vs. 48.4%; P = .048).
Treatment response was not reflected in change in hydrogen breath response, Dr. Tan said. Results of a 3-hour hydrogen breath test performed after a 12-hour overnight fast showed no differences between the rifaximin and placebo groups for H2 peak above baseline (2.94 ppm vs. 0.11 ppm; P = .29), H2 area under the curve (+43.64 ppm vs. –49.71 ppm; P = .76), and oro-cecal transit time (24.23 minutes vs. 16.5 minutes; P = .68).
Adverse events were very similar between the two groups at both 4 and 8 weeks, Dr. Tan said. Only one major event occurred, a severe case of acute hepatitis in a woman in the placebo arm who also took traditional Chinese herbs.
On Twitter @pwendl
WASHINGTON – Two weeks of antibiotic therapy with rifaximin provided relief from functional dyspepsia symptoms in a phase III double-blind, randomized trial.
“This is the first study that demonstrates that rifaximin is efficacious in the treatment of functional dyspepsia, particularly for global dyspeptic symptoms, bloating, and possibly belching. Our finding may suggest a role for the gut microbiota in the pathogenesis of functional dyspepsia,” Dr. Victoria Tan said at the annual Digestive Disease Week.
Rifaximin (Xifaxan) works by reducing or altering bacteria in the gut and has been shown to be efficacious in the treatment of diarrhea-predominant irritable bowel syndrome. It is approved to treat traveler’s diarrhea caused by Escherichia coli and to prevent hepatic encephalopathy.
The study randomly assigned 95 consecutive adults with functional dyspepsia as per ROME III criteria who had a normal gastroscopy within the last 2 years, had active symptoms in the month prior to enrollment, and were Helicobacter pylori negative, to rifaximin 400 mg or placebo three times a day for 2 weeks. In all, 33 rifaximin and 39 placebo patients were evaluable for the primary efficacy outcome of adequate relief of global dyspeptic symptoms (either no or mild dyspeptic symptoms) at any of the follow-up time points.
At baseline, 77% of patients had moderate to severe global dyspepsia symptoms, 74% of the placebo group and 55%% of the rifaximin group had moderate to severe belching, and roughly half of all patients were not on any GI medications. Mean age of the patients was 52 years.
Global dyspepsia symptoms improved with rifaximin beginning at week 2 and significantly favored rifaximin by week 8, with 23.5% of rifaximin patients reporting moderate to severe symptoms compared with 47.4% given placebo (P value = .04), said Dr. Tan of the University of Hong Kong.
Rates of moderate to severe belching were significantly improved with rifaximin at week 4 compared with placebo (14.3% vs. 35.7%; P = .03), but this difference was no longer significant at week 8 (26.5% vs. 29%).
The story was similar for moderate to severe bloating: Rates declined significantly with rifaximin at week 4 (20% vs. 43%; P = .03), but were no longer significant at week 8 (26.5% vs. 34.2%), she said.
A subgroup analysis of female patients showed significant improvements in moderate to severe global dyspeptic symptoms with rifaximin compared with placebo at week 4 (20.8% vs. 59.4%; P = .006) and week 8 (20% vs. 48.4%; P = .048).
Treatment response was not reflected in change in hydrogen breath response, Dr. Tan said. Results of a 3-hour hydrogen breath test performed after a 12-hour overnight fast showed no differences between the rifaximin and placebo groups for H2 peak above baseline (2.94 ppm vs. 0.11 ppm; P = .29), H2 area under the curve (+43.64 ppm vs. –49.71 ppm; P = .76), and oro-cecal transit time (24.23 minutes vs. 16.5 minutes; P = .68).
Adverse events were very similar between the two groups at both 4 and 8 weeks, Dr. Tan said. Only one major event occurred, a severe case of acute hepatitis in a woman in the placebo arm who also took traditional Chinese herbs.
On Twitter @pwendl
WASHINGTON – Two weeks of antibiotic therapy with rifaximin provided relief from functional dyspepsia symptoms in a phase III double-blind, randomized trial.
“This is the first study that demonstrates that rifaximin is efficacious in the treatment of functional dyspepsia, particularly for global dyspeptic symptoms, bloating, and possibly belching. Our finding may suggest a role for the gut microbiota in the pathogenesis of functional dyspepsia,” Dr. Victoria Tan said at the annual Digestive Disease Week.
Rifaximin (Xifaxan) works by reducing or altering bacteria in the gut and has been shown to be efficacious in the treatment of diarrhea-predominant irritable bowel syndrome. It is approved to treat traveler’s diarrhea caused by Escherichia coli and to prevent hepatic encephalopathy.
The study randomly assigned 95 consecutive adults with functional dyspepsia as per ROME III criteria who had a normal gastroscopy within the last 2 years, had active symptoms in the month prior to enrollment, and were Helicobacter pylori negative, to rifaximin 400 mg or placebo three times a day for 2 weeks. In all, 33 rifaximin and 39 placebo patients were evaluable for the primary efficacy outcome of adequate relief of global dyspeptic symptoms (either no or mild dyspeptic symptoms) at any of the follow-up time points.
At baseline, 77% of patients had moderate to severe global dyspepsia symptoms, 74% of the placebo group and 55%% of the rifaximin group had moderate to severe belching, and roughly half of all patients were not on any GI medications. Mean age of the patients was 52 years.
Global dyspepsia symptoms improved with rifaximin beginning at week 2 and significantly favored rifaximin by week 8, with 23.5% of rifaximin patients reporting moderate to severe symptoms compared with 47.4% given placebo (P value = .04), said Dr. Tan of the University of Hong Kong.
Rates of moderate to severe belching were significantly improved with rifaximin at week 4 compared with placebo (14.3% vs. 35.7%; P = .03), but this difference was no longer significant at week 8 (26.5% vs. 29%).
The story was similar for moderate to severe bloating: Rates declined significantly with rifaximin at week 4 (20% vs. 43%; P = .03), but were no longer significant at week 8 (26.5% vs. 34.2%), she said.
A subgroup analysis of female patients showed significant improvements in moderate to severe global dyspeptic symptoms with rifaximin compared with placebo at week 4 (20.8% vs. 59.4%; P = .006) and week 8 (20% vs. 48.4%; P = .048).
Treatment response was not reflected in change in hydrogen breath response, Dr. Tan said. Results of a 3-hour hydrogen breath test performed after a 12-hour overnight fast showed no differences between the rifaximin and placebo groups for H2 peak above baseline (2.94 ppm vs. 0.11 ppm; P = .29), H2 area under the curve (+43.64 ppm vs. –49.71 ppm; P = .76), and oro-cecal transit time (24.23 minutes vs. 16.5 minutes; P = .68).
Adverse events were very similar between the two groups at both 4 and 8 weeks, Dr. Tan said. Only one major event occurred, a severe case of acute hepatitis in a woman in the placebo arm who also took traditional Chinese herbs.
On Twitter @pwendl
AT DDW® 2015