Current cigarette smokers were 22/64 (34.4%) of the population, higher than in national databases but similar to many behavioral health populations [23]. The BMI was 25 or less in 21/64 (32.8%), similar to the national distribution demonstrating that approximately 2/3 of patients are overweight or obese; 12/64 (18.8%) had a BMI of 25–30 (overweight), lower than national data, and 33/64 (48.5%) had a BMI >30 (obesity), higher than national data [24]. Similar increased rates of obesity are found in other behavioral health populations [25].
Mode of Symptom Presentation
Psychological symptoms were the sole mode of presentation in 21/64 (32.8%), while physical symptoms were the sole presenting complaint in 16/64 (25.0%). Combined psychological and physical symptoms were the predominant pattern at 27/64 (42.2%). Thus, 43/64 (67.2%) had physical symptoms and 48/64 (75.0%) had psychological symptoms at presentation. The mean duration of presenting symptoms was > 5 years in 52/64 (81.3%); only 5/64 (7.8%) had symptoms < 12 months in duration.
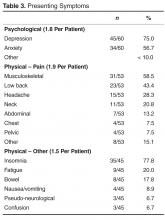
Presenting Symptoms
Psychological symptoms were present in 60/64 (93.8%) and averaged 1.8 per patient. Depression and anxiety/fear were the predominant psychological symptoms ( Table 3 ).Pain symptoms were present in 53/64 (82.8%) and averaged 1.9 per patient. The details presented in Table 3 demonstrate a high frequency of musculoskeletal problems.
Non-pain physical symptoms were present in 45/64 (70.3%) and averaged 1.5 per patient. There was a very high frequency of insomnia (Table 3).
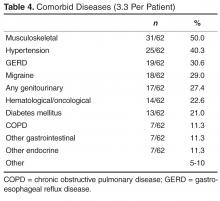
Comorbid Physical Diseases
Comorbid diseases were present in 62/64 (96.9%) and averaged 3.3 per patient. There was a large number of muscular/skeletal/rheumatologic, hypertension, gastroesophageal reflux disease, and migraine diagnoses ( Table 4 ).Medications
Narcotic use was found in 35/64 (54.7%) patients; of these, 23/35 (65.7%) were using 80 or fewer morphine equivalents and 12/35 (34.3%) were using > 80 morphine equivalents, only 7/35 (20.0%) at > 120 morphine equivalents. Thus, only the latter took unsafe doses. There was no narcotic use in 29/64 (45.3%).
Antidepressant use was found in 46/64 (71.9%); only 6/46 (13.0%) were on subtherapeutic doses while 40/46 (87.0%) were on “usual therapeutic” doses. There was no antidepressant use in 18/64 (28.1%).
Benzodiazepine use was found in 31/64 (48.4%), antipsychotic use in 8/64 (12.5%), and mood stabilizer use in 10/64 (15.6%).
Impairment/Disability
Major physical impairment was present in 27/64 (42.2%), major economic impairment was present in 45/64 (70.3%), and major social impairment occurred in 49/64 (76.6%).
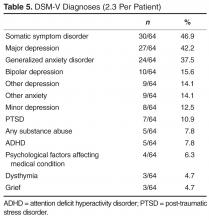
Diagnoses
The PHQ-9 was available in 41/64 (64.1%) of cases. Of these, it was < 5 (normal) in 3/41 (7.3%), from 5–10 (mild depression) in 11/41 (26.8%), from 10–15 (moderate depression) in 13/41 (31.7%), from 15–20 (severe depression) in 3/41 (7.3%), and > 20 (very severe depression) in 11/41 (26.8%).
All 64 patients had DSM-V diagnoses and averaged 2.3 per patient, the details in Table 5 demonstrating the high frequency of somatic symptom disorder, major depressive disorder, and generalized anxiety disorder.Prior Care History
Behavioral health care for problems prior to the presentation problem had been received by 27/64 (42.2%): 11/27 (40.7%) from non-psychiatrists, 10/27 (37.0%) from psychiatrists, and 6/27 (22.2%) from both. Behavioral care for the presentation problem had been received by only 18/64 (28.1%): 11/18 (61.1%) from non-psychiatrists, 3/18 (16.7%) from psychiatrists, and 4/18 (22.2%) from both. Thus, of all 64 CPC patients, only 7 (10.9%) had received psychiatric care. Patients had received care in the same medical clinic for an average of 71.9 months.