User login
European Society of Cardiology (ESC): Annual Congress
Doc says fatal bleeding with extended DAPT is rare

Photo by Sage Ross
LONDON—Fatal bleeding is rare with extended dual antiplatelet therapy (DAPT), according to research presented at the ESC Congress 2015.
The study included patients with a coronary stent who were receiving 30 months or 12 months of DAPT to prevent stent thrombosis and major cardiovascular and cerebrovascular events.
The results showed that bleeding-related mortality accounted for a minority of deaths in both patient groups.
Laura Mauri, MD, of Harvard Medical School in Boston, Massachusetts, presented these results as abstract 3916. The study, known as the DAPT trial, was funded by a consortium of 8 device and drug manufacturers and other entities.
The trial enrolled patients who were set to receive a drug-eluting or bare-metal stent. After stent placement, they received DAPT—aspirin plus thienopyridine (clopidogrel or prasugrel)—for at least 12 months.
After 12 months of therapy, patients who were treatment-compliant and event-free (no myocardial infarction, stroke, or moderate or severe bleeding) were randomized to continued thienopyridine or placebo, each in addition to aspirin, for an additional 18 months. At month 30, patients discontinued randomized treatment but remained on aspirin for 3 months.
Results from patients with drug-eluting stents were published in NEJM in 2014.
But Dr Mauri reported on causes of death in all 11,648 randomized patients. All deaths were reviewed and adjudicated by an independent committee of cardiologists and oncologists who were blinded to the randomized treatment groups.
Any death that was possibly, probably, or definitely related to any prior clinically evident bleeding event was adjudicated as “bleeding-related,” and any death that was possibly, probably, or definitely related to a malignancy or to complications from treatments specifically administered for the malignancy was adjudicated as “cancer-related.” Fatal bleeding was defined using the Bleeding Academic Research Consortium (BARC) definition.
All-cause mortality
At 30 months (end of the randomization period), the mortality rate was 1.9% in the 30-month treatment group and 1.5% in 12-month group (P=0.07).
There was no significant difference between the groups for cardiovascular mortality—both about 1% (P=0.97)—but there was a significant difference for non-cardiovascular mortality—0.9% and 0.5%, respectively (P=0.01).
At 33 months (combined randomization and aspirin monotherapy periods), the mortality rate was 2.2% in the 30-month treatment group and 1.8% in the 12-month treatment group (P=0.05).
The rates of cardiovascular mortality were 1.2% and 1.1%, respectively (P=0.51). And the rates of non-cardiovascular mortality were 1.0% and 0.7%, respectively (P=0.02).
Bleeding-related deaths
At 33 months, there was no significant difference in bleeding-related mortality. Fatal bleeding occurred in 0.3% of patients in the 30-month group and 0.2% of those in the 12-month group (P=0.36).
There was no significant difference between the groups for bleeding-related death without cancer or trauma (P>0.99), bleeding-related death with cancer (P=0.25), bleeding-related death with trauma (P=0.58), trauma-related death (P=0.30), or trauma-related death without bleeding (P=0.50).
“This analysis of the DAPT study provides valuable insight to suggest that fatal bleeding is rare with extended dual antiplatelet therapy and may be avoided with careful patient selection,” Dr Mauri said.
Cancer-related deaths
Dr Mauri noted that there was no significant difference in the incidence of cancer between the randomized groups (P=0.12). But there was a significant difference in the incidence of cancer-related mortality at 33 months. It was 0.6% in the 30-month group and 0.3% in the 12-month group (P=0.02).
However, when the investigators excluded the cancer-related deaths that occurred in patients whose cancer was diagnosed before they enrolled in the DAPT study, the difference in cancer-related death became non-significant (0.4% and 0.3%, respectively, P=0.16).
“Given the clear benefits of dual antiplatelet therapy in reducing myocardial infarction, these medications remain essential for patients with acute coronary syndromes or coronary stents,” Dr Mauri said. “The relationship with cancer requires further investigation.” ![]()

Photo by Sage Ross
LONDON—Fatal bleeding is rare with extended dual antiplatelet therapy (DAPT), according to research presented at the ESC Congress 2015.
The study included patients with a coronary stent who were receiving 30 months or 12 months of DAPT to prevent stent thrombosis and major cardiovascular and cerebrovascular events.
The results showed that bleeding-related mortality accounted for a minority of deaths in both patient groups.
Laura Mauri, MD, of Harvard Medical School in Boston, Massachusetts, presented these results as abstract 3916. The study, known as the DAPT trial, was funded by a consortium of 8 device and drug manufacturers and other entities.
The trial enrolled patients who were set to receive a drug-eluting or bare-metal stent. After stent placement, they received DAPT—aspirin plus thienopyridine (clopidogrel or prasugrel)—for at least 12 months.
After 12 months of therapy, patients who were treatment-compliant and event-free (no myocardial infarction, stroke, or moderate or severe bleeding) were randomized to continued thienopyridine or placebo, each in addition to aspirin, for an additional 18 months. At month 30, patients discontinued randomized treatment but remained on aspirin for 3 months.
Results from patients with drug-eluting stents were published in NEJM in 2014.
But Dr Mauri reported on causes of death in all 11,648 randomized patients. All deaths were reviewed and adjudicated by an independent committee of cardiologists and oncologists who were blinded to the randomized treatment groups.
Any death that was possibly, probably, or definitely related to any prior clinically evident bleeding event was adjudicated as “bleeding-related,” and any death that was possibly, probably, or definitely related to a malignancy or to complications from treatments specifically administered for the malignancy was adjudicated as “cancer-related.” Fatal bleeding was defined using the Bleeding Academic Research Consortium (BARC) definition.
All-cause mortality
At 30 months (end of the randomization period), the mortality rate was 1.9% in the 30-month treatment group and 1.5% in 12-month group (P=0.07).
There was no significant difference between the groups for cardiovascular mortality—both about 1% (P=0.97)—but there was a significant difference for non-cardiovascular mortality—0.9% and 0.5%, respectively (P=0.01).
At 33 months (combined randomization and aspirin monotherapy periods), the mortality rate was 2.2% in the 30-month treatment group and 1.8% in the 12-month treatment group (P=0.05).
The rates of cardiovascular mortality were 1.2% and 1.1%, respectively (P=0.51). And the rates of non-cardiovascular mortality were 1.0% and 0.7%, respectively (P=0.02).
Bleeding-related deaths
At 33 months, there was no significant difference in bleeding-related mortality. Fatal bleeding occurred in 0.3% of patients in the 30-month group and 0.2% of those in the 12-month group (P=0.36).
There was no significant difference between the groups for bleeding-related death without cancer or trauma (P>0.99), bleeding-related death with cancer (P=0.25), bleeding-related death with trauma (P=0.58), trauma-related death (P=0.30), or trauma-related death without bleeding (P=0.50).
“This analysis of the DAPT study provides valuable insight to suggest that fatal bleeding is rare with extended dual antiplatelet therapy and may be avoided with careful patient selection,” Dr Mauri said.
Cancer-related deaths
Dr Mauri noted that there was no significant difference in the incidence of cancer between the randomized groups (P=0.12). But there was a significant difference in the incidence of cancer-related mortality at 33 months. It was 0.6% in the 30-month group and 0.3% in the 12-month group (P=0.02).
However, when the investigators excluded the cancer-related deaths that occurred in patients whose cancer was diagnosed before they enrolled in the DAPT study, the difference in cancer-related death became non-significant (0.4% and 0.3%, respectively, P=0.16).
“Given the clear benefits of dual antiplatelet therapy in reducing myocardial infarction, these medications remain essential for patients with acute coronary syndromes or coronary stents,” Dr Mauri said. “The relationship with cancer requires further investigation.” ![]()

Photo by Sage Ross
LONDON—Fatal bleeding is rare with extended dual antiplatelet therapy (DAPT), according to research presented at the ESC Congress 2015.
The study included patients with a coronary stent who were receiving 30 months or 12 months of DAPT to prevent stent thrombosis and major cardiovascular and cerebrovascular events.
The results showed that bleeding-related mortality accounted for a minority of deaths in both patient groups.
Laura Mauri, MD, of Harvard Medical School in Boston, Massachusetts, presented these results as abstract 3916. The study, known as the DAPT trial, was funded by a consortium of 8 device and drug manufacturers and other entities.
The trial enrolled patients who were set to receive a drug-eluting or bare-metal stent. After stent placement, they received DAPT—aspirin plus thienopyridine (clopidogrel or prasugrel)—for at least 12 months.
After 12 months of therapy, patients who were treatment-compliant and event-free (no myocardial infarction, stroke, or moderate or severe bleeding) were randomized to continued thienopyridine or placebo, each in addition to aspirin, for an additional 18 months. At month 30, patients discontinued randomized treatment but remained on aspirin for 3 months.
Results from patients with drug-eluting stents were published in NEJM in 2014.
But Dr Mauri reported on causes of death in all 11,648 randomized patients. All deaths were reviewed and adjudicated by an independent committee of cardiologists and oncologists who were blinded to the randomized treatment groups.
Any death that was possibly, probably, or definitely related to any prior clinically evident bleeding event was adjudicated as “bleeding-related,” and any death that was possibly, probably, or definitely related to a malignancy or to complications from treatments specifically administered for the malignancy was adjudicated as “cancer-related.” Fatal bleeding was defined using the Bleeding Academic Research Consortium (BARC) definition.
All-cause mortality
At 30 months (end of the randomization period), the mortality rate was 1.9% in the 30-month treatment group and 1.5% in 12-month group (P=0.07).
There was no significant difference between the groups for cardiovascular mortality—both about 1% (P=0.97)—but there was a significant difference for non-cardiovascular mortality—0.9% and 0.5%, respectively (P=0.01).
At 33 months (combined randomization and aspirin monotherapy periods), the mortality rate was 2.2% in the 30-month treatment group and 1.8% in the 12-month treatment group (P=0.05).
The rates of cardiovascular mortality were 1.2% and 1.1%, respectively (P=0.51). And the rates of non-cardiovascular mortality were 1.0% and 0.7%, respectively (P=0.02).
Bleeding-related deaths
At 33 months, there was no significant difference in bleeding-related mortality. Fatal bleeding occurred in 0.3% of patients in the 30-month group and 0.2% of those in the 12-month group (P=0.36).
There was no significant difference between the groups for bleeding-related death without cancer or trauma (P>0.99), bleeding-related death with cancer (P=0.25), bleeding-related death with trauma (P=0.58), trauma-related death (P=0.30), or trauma-related death without bleeding (P=0.50).
“This analysis of the DAPT study provides valuable insight to suggest that fatal bleeding is rare with extended dual antiplatelet therapy and may be avoided with careful patient selection,” Dr Mauri said.
Cancer-related deaths
Dr Mauri noted that there was no significant difference in the incidence of cancer between the randomized groups (P=0.12). But there was a significant difference in the incidence of cancer-related mortality at 33 months. It was 0.6% in the 30-month group and 0.3% in the 12-month group (P=0.02).
However, when the investigators excluded the cancer-related deaths that occurred in patients whose cancer was diagnosed before they enrolled in the DAPT study, the difference in cancer-related death became non-significant (0.4% and 0.3%, respectively, P=0.16).
“Given the clear benefits of dual antiplatelet therapy in reducing myocardial infarction, these medications remain essential for patients with acute coronary syndromes or coronary stents,” Dr Mauri said. “The relationship with cancer requires further investigation.” ![]()
Score ‘modestly accurate’ for predicting thromboembolism

Image by Kevin MacKEnzie
LONDON—A score used to predict the risk of thromboembolic events, ischemic stroke, and death is only modestly accurate in patients with heart failure (HF), according to researchers.
They found the accuracy of the CHA2DS2-VASc score was dependent upon the endpoint being assessed and the duration of follow-up.
The score proved least effective for predicting thromboembolism, and its negative predictive values (NPVs) were inferior at 5 years of follow-up compared to 1 year.
Gregory Y. H Lip, MD, of Aalborg University in Denmark, and his colleagues reported these findings in JAMA and at the ESC Congress 2015 (abstract 1830*).
The team noted that the CHA2DS2-VASc score (congestive heart failure, hypertension, age 75 years or older [doubled], diabetes, stroke/transient ischemic attack/thromboembolism [doubled], vascular disease [prior heart attack, peripheral artery disease, or aortic plaque], age 65-75 years, sex category [female]) is already used clinically for stroke risk stratification in patients with atrial fibrillation (AF).
But its usefulness in a population of patients with HF has been unclear. So the researchers investigated whether CHA2DS2-VASc predicts ischemic stroke, thromboembolism, and death in patients with a new diagnosis of HF, with or without AF.
Using Danish registries, the researchers compiled data from 42,987 patients (22% with concomitant AF). The patients were not receiving anticoagulation and had been diagnosed with new-onset HF from 2000 to 2012.
The end of follow-up was December 31, 2012. Levels of the CHA2DS2-VASc score (based on 10 possible points, with higher scores indicating higher risk) were stratified by the presence of AF at study entry.
Among patients without AF, the incidence of thromboembolism was 3.5%, the rate of ischemic stroke was 1%, and the death rate was 7.2%. Among patients with AF, the rates were 4.2%, 2%, and 13.2%, respectively.
Predictive accuracy
For predicting thromboembolism in patients without AF, the C statistics were 0.63 at 1 year and 0.67 at 5 years. The NPVs were 88% and 73%, respectively.
For predicting thromboembolism in patients with AF, the C statistics were 0.62 at 1 year and 0.69 at 5 years. The NPVs were 88% and 61%, respectively.
For predicting ischemic stroke in patients without AF, the C statistics were 0.67 at 1 year and 0.69 at 5 years. The NPVs were 92% and 78%, respectively.
For predicting ischemic stroke in patients with AF, the C statistics were 0.64 at 1 year and 0.71 at 5 years. The NPVs were 91% and 69%, respectively.
For predicting death in patients without AF, the C statistics were 0.64 at 1 year and 0.68 at 5 years. The NPVs were 93% and 81%, respectively.
For predicting death in patients with AF, the C statistics were 0.63 at 1 year and 0.70 at 5 years. The NPVs were 94% and 76%, respectively.
Based on these results, the researchers said the clinical usefulness of the CHA2DS2-VASc score for patients with HF remains to be determined. And preventative strategies to reduce thromboembolism and ischemic stroke among these patients require further investigation. ![]()
*Information in the abstract differs from that presented.

Image by Kevin MacKEnzie
LONDON—A score used to predict the risk of thromboembolic events, ischemic stroke, and death is only modestly accurate in patients with heart failure (HF), according to researchers.
They found the accuracy of the CHA2DS2-VASc score was dependent upon the endpoint being assessed and the duration of follow-up.
The score proved least effective for predicting thromboembolism, and its negative predictive values (NPVs) were inferior at 5 years of follow-up compared to 1 year.
Gregory Y. H Lip, MD, of Aalborg University in Denmark, and his colleagues reported these findings in JAMA and at the ESC Congress 2015 (abstract 1830*).
The team noted that the CHA2DS2-VASc score (congestive heart failure, hypertension, age 75 years or older [doubled], diabetes, stroke/transient ischemic attack/thromboembolism [doubled], vascular disease [prior heart attack, peripheral artery disease, or aortic plaque], age 65-75 years, sex category [female]) is already used clinically for stroke risk stratification in patients with atrial fibrillation (AF).
But its usefulness in a population of patients with HF has been unclear. So the researchers investigated whether CHA2DS2-VASc predicts ischemic stroke, thromboembolism, and death in patients with a new diagnosis of HF, with or without AF.
Using Danish registries, the researchers compiled data from 42,987 patients (22% with concomitant AF). The patients were not receiving anticoagulation and had been diagnosed with new-onset HF from 2000 to 2012.
The end of follow-up was December 31, 2012. Levels of the CHA2DS2-VASc score (based on 10 possible points, with higher scores indicating higher risk) were stratified by the presence of AF at study entry.
Among patients without AF, the incidence of thromboembolism was 3.5%, the rate of ischemic stroke was 1%, and the death rate was 7.2%. Among patients with AF, the rates were 4.2%, 2%, and 13.2%, respectively.
Predictive accuracy
For predicting thromboembolism in patients without AF, the C statistics were 0.63 at 1 year and 0.67 at 5 years. The NPVs were 88% and 73%, respectively.
For predicting thromboembolism in patients with AF, the C statistics were 0.62 at 1 year and 0.69 at 5 years. The NPVs were 88% and 61%, respectively.
For predicting ischemic stroke in patients without AF, the C statistics were 0.67 at 1 year and 0.69 at 5 years. The NPVs were 92% and 78%, respectively.
For predicting ischemic stroke in patients with AF, the C statistics were 0.64 at 1 year and 0.71 at 5 years. The NPVs were 91% and 69%, respectively.
For predicting death in patients without AF, the C statistics were 0.64 at 1 year and 0.68 at 5 years. The NPVs were 93% and 81%, respectively.
For predicting death in patients with AF, the C statistics were 0.63 at 1 year and 0.70 at 5 years. The NPVs were 94% and 76%, respectively.
Based on these results, the researchers said the clinical usefulness of the CHA2DS2-VASc score for patients with HF remains to be determined. And preventative strategies to reduce thromboembolism and ischemic stroke among these patients require further investigation. ![]()
*Information in the abstract differs from that presented.

Image by Kevin MacKEnzie
LONDON—A score used to predict the risk of thromboembolic events, ischemic stroke, and death is only modestly accurate in patients with heart failure (HF), according to researchers.
They found the accuracy of the CHA2DS2-VASc score was dependent upon the endpoint being assessed and the duration of follow-up.
The score proved least effective for predicting thromboembolism, and its negative predictive values (NPVs) were inferior at 5 years of follow-up compared to 1 year.
Gregory Y. H Lip, MD, of Aalborg University in Denmark, and his colleagues reported these findings in JAMA and at the ESC Congress 2015 (abstract 1830*).
The team noted that the CHA2DS2-VASc score (congestive heart failure, hypertension, age 75 years or older [doubled], diabetes, stroke/transient ischemic attack/thromboembolism [doubled], vascular disease [prior heart attack, peripheral artery disease, or aortic plaque], age 65-75 years, sex category [female]) is already used clinically for stroke risk stratification in patients with atrial fibrillation (AF).
But its usefulness in a population of patients with HF has been unclear. So the researchers investigated whether CHA2DS2-VASc predicts ischemic stroke, thromboembolism, and death in patients with a new diagnosis of HF, with or without AF.
Using Danish registries, the researchers compiled data from 42,987 patients (22% with concomitant AF). The patients were not receiving anticoagulation and had been diagnosed with new-onset HF from 2000 to 2012.
The end of follow-up was December 31, 2012. Levels of the CHA2DS2-VASc score (based on 10 possible points, with higher scores indicating higher risk) were stratified by the presence of AF at study entry.
Among patients without AF, the incidence of thromboembolism was 3.5%, the rate of ischemic stroke was 1%, and the death rate was 7.2%. Among patients with AF, the rates were 4.2%, 2%, and 13.2%, respectively.
Predictive accuracy
For predicting thromboembolism in patients without AF, the C statistics were 0.63 at 1 year and 0.67 at 5 years. The NPVs were 88% and 73%, respectively.
For predicting thromboembolism in patients with AF, the C statistics were 0.62 at 1 year and 0.69 at 5 years. The NPVs were 88% and 61%, respectively.
For predicting ischemic stroke in patients without AF, the C statistics were 0.67 at 1 year and 0.69 at 5 years. The NPVs were 92% and 78%, respectively.
For predicting ischemic stroke in patients with AF, the C statistics were 0.64 at 1 year and 0.71 at 5 years. The NPVs were 91% and 69%, respectively.
For predicting death in patients without AF, the C statistics were 0.64 at 1 year and 0.68 at 5 years. The NPVs were 93% and 81%, respectively.
For predicting death in patients with AF, the C statistics were 0.63 at 1 year and 0.70 at 5 years. The NPVs were 94% and 76%, respectively.
Based on these results, the researchers said the clinical usefulness of the CHA2DS2-VASc score for patients with HF remains to be determined. And preventative strategies to reduce thromboembolism and ischemic stroke among these patients require further investigation. ![]()
*Information in the abstract differs from that presented.
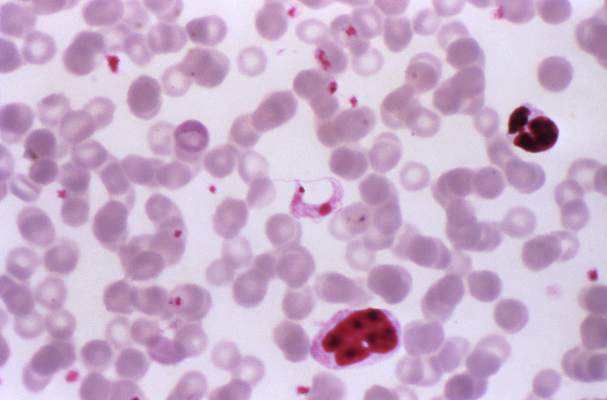
Research reveals potential target for stent thrombosis

Image by Volker Brinkmann
LONDON—Immune cells may represent an important therapeutic target for preventing stent thrombosis, according to investigators from the PRESTIGE study.
The team analyzed more than 250 thrombus specimens and observed leukocyte infiltration in the context of early and late stent thrombosis.
Neutrophils were the most common leukocyte detected, and eosinophils were present in thrombi from all stent types.
The investigators reported these findings in the European Heart Journal and at the ESC Congress 2015 (abstract 1996*).
“Our results suggest that immune-cell-mediated thrombotic processes may be a realistic target for novel therapies to prevent [stent thrombosis],” said study investigator Steffen Massberg, PhD, of Ludwig-Maximilians University in Munich, Germany.
“Inhibition of triggers, such as extracellular nucleic acids activating the contact phase, may not only result in efficient anticoagulation in the setting of [stent thrombosis] but might also yield less therapy-associated bleeding. Future studies should evaluate whether inhibition of immune-cell-driven thrombotic pathways are effective and safe in clinical practice.”
The PRESTIGE study included patients with stent thrombosis who underwent thrombus aspiration at 9 centers in Europe between 2010 and 2014. In all, the investigators analyzed 253 thrombus specimens from these patients.
Seventy-nine specimens (31.2%) were from patients presenting with early stent thrombosis, and 174 (68.8%) were from patients with late stent thrombosis. Seventy-nine (31.2%) were from bare metal stents, 166 (65.6%) were from drug-eluting stents, and 8 (3.2%) were from stents of unknown type.
The thrombus specimens had heterogeneous morphology, with platelet-rich thrombus and fibrin/fibrinogen fragments being most abundant.
The investigators said leukocyte infiltrations were hallmarks of both early and late stent thrombosis, with neutrophils representing the most prominent subset. Neutrophils were found in similar amounts in early and late stent thrombosis.
“It is important to note that leukocyte counts were significantly higher compared with a control group of patients with thrombus aspiration in spontaneous myocardial infarction,” Dr Massberg said.
He and his colleagues also observed neutrophil extracellular traps (NETs) in 23% of samples.
And they found that eosinophils were present in all stent types, but there were higher numbers in patients with late stent thrombosis in sirolimus-eluting and everolimus-eluting stents.
“The presence of NETs supports their pathophysiological relevance in [stent thrombosis], while eosinophil recruitment suggests an allergic component to the process of [stent thrombosis],” Dr Massberg said. ![]()
*Information in the abstract differs from that presented.

Image by Volker Brinkmann
LONDON—Immune cells may represent an important therapeutic target for preventing stent thrombosis, according to investigators from the PRESTIGE study.
The team analyzed more than 250 thrombus specimens and observed leukocyte infiltration in the context of early and late stent thrombosis.
Neutrophils were the most common leukocyte detected, and eosinophils were present in thrombi from all stent types.
The investigators reported these findings in the European Heart Journal and at the ESC Congress 2015 (abstract 1996*).
“Our results suggest that immune-cell-mediated thrombotic processes may be a realistic target for novel therapies to prevent [stent thrombosis],” said study investigator Steffen Massberg, PhD, of Ludwig-Maximilians University in Munich, Germany.
“Inhibition of triggers, such as extracellular nucleic acids activating the contact phase, may not only result in efficient anticoagulation in the setting of [stent thrombosis] but might also yield less therapy-associated bleeding. Future studies should evaluate whether inhibition of immune-cell-driven thrombotic pathways are effective and safe in clinical practice.”
The PRESTIGE study included patients with stent thrombosis who underwent thrombus aspiration at 9 centers in Europe between 2010 and 2014. In all, the investigators analyzed 253 thrombus specimens from these patients.
Seventy-nine specimens (31.2%) were from patients presenting with early stent thrombosis, and 174 (68.8%) were from patients with late stent thrombosis. Seventy-nine (31.2%) were from bare metal stents, 166 (65.6%) were from drug-eluting stents, and 8 (3.2%) were from stents of unknown type.
The thrombus specimens had heterogeneous morphology, with platelet-rich thrombus and fibrin/fibrinogen fragments being most abundant.
The investigators said leukocyte infiltrations were hallmarks of both early and late stent thrombosis, with neutrophils representing the most prominent subset. Neutrophils were found in similar amounts in early and late stent thrombosis.
“It is important to note that leukocyte counts were significantly higher compared with a control group of patients with thrombus aspiration in spontaneous myocardial infarction,” Dr Massberg said.
He and his colleagues also observed neutrophil extracellular traps (NETs) in 23% of samples.
And they found that eosinophils were present in all stent types, but there were higher numbers in patients with late stent thrombosis in sirolimus-eluting and everolimus-eluting stents.
“The presence of NETs supports their pathophysiological relevance in [stent thrombosis], while eosinophil recruitment suggests an allergic component to the process of [stent thrombosis],” Dr Massberg said. ![]()
*Information in the abstract differs from that presented.

Image by Volker Brinkmann
LONDON—Immune cells may represent an important therapeutic target for preventing stent thrombosis, according to investigators from the PRESTIGE study.
The team analyzed more than 250 thrombus specimens and observed leukocyte infiltration in the context of early and late stent thrombosis.
Neutrophils were the most common leukocyte detected, and eosinophils were present in thrombi from all stent types.
The investigators reported these findings in the European Heart Journal and at the ESC Congress 2015 (abstract 1996*).
“Our results suggest that immune-cell-mediated thrombotic processes may be a realistic target for novel therapies to prevent [stent thrombosis],” said study investigator Steffen Massberg, PhD, of Ludwig-Maximilians University in Munich, Germany.
“Inhibition of triggers, such as extracellular nucleic acids activating the contact phase, may not only result in efficient anticoagulation in the setting of [stent thrombosis] but might also yield less therapy-associated bleeding. Future studies should evaluate whether inhibition of immune-cell-driven thrombotic pathways are effective and safe in clinical practice.”
The PRESTIGE study included patients with stent thrombosis who underwent thrombus aspiration at 9 centers in Europe between 2010 and 2014. In all, the investigators analyzed 253 thrombus specimens from these patients.
Seventy-nine specimens (31.2%) were from patients presenting with early stent thrombosis, and 174 (68.8%) were from patients with late stent thrombosis. Seventy-nine (31.2%) were from bare metal stents, 166 (65.6%) were from drug-eluting stents, and 8 (3.2%) were from stents of unknown type.
The thrombus specimens had heterogeneous morphology, with platelet-rich thrombus and fibrin/fibrinogen fragments being most abundant.
The investigators said leukocyte infiltrations were hallmarks of both early and late stent thrombosis, with neutrophils representing the most prominent subset. Neutrophils were found in similar amounts in early and late stent thrombosis.
“It is important to note that leukocyte counts were significantly higher compared with a control group of patients with thrombus aspiration in spontaneous myocardial infarction,” Dr Massberg said.
He and his colleagues also observed neutrophil extracellular traps (NETs) in 23% of samples.
And they found that eosinophils were present in all stent types, but there were higher numbers in patients with late stent thrombosis in sirolimus-eluting and everolimus-eluting stents.
“The presence of NETs supports their pathophysiological relevance in [stent thrombosis], while eosinophil recruitment suggests an allergic component to the process of [stent thrombosis],” Dr Massberg said. ![]()
*Information in the abstract differs from that presented.
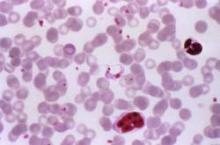
Benznidazole: No clinical impact on Chagas cardiomyopathy
Among patients with Chagas cardiomyopathy, trypanocidal therapy with benznidazole significantly reduced serum parasite detection but did not reduce cardiac clinical deterioration through 5 years of follow-up, a randomized trial showed.
Those are key findings from the Benznidazole Evaluation for Interrupting Trypanosomiasis (BENEFIT) trial, which were presented at the annual congress of the European Society of Cardiology and published simultaneously in the New England Journal of Medicine (doi: 10.1056/NEJMoa1507574).
According to lead study authors Dr. Carlos A. Morillo of the Population Health Research Institute at Hamilton Health Sciences and McMaster University, Hamilton, Ont., and Dr. Jose Antonio Marin-Neto of the division of cardiology at the Medical School of Riberao Preto, Brazil, Chagas cardiomyopathy develops in about one-quarter of patients infected with Trypanosoma cruzi. “The identification of T. cruzi antigens in inflamed myocardium with the use of sensitive techniques, such as immunohistochemical analysis and polymerase chain reaction (PCR) assay, suggests that parasite persistence may be an important factor that, in conjunction with individual host factors, triggers the inflammatory process,” they wrote. “In assessing whether trypanocidal therapy prevents or reduces cardiac disease, experimental models of chronic Chagas infection have shown that trypanocidal therapy attenuates the pathologic consequences by reducing the parasite burden. A few small observational and randomized studies involving patients with Chagas disease have shown that benznidazole reduced the circulating parasite load, enhances seroconversion, and may halt the progression of cardiomyopathy.”
In a study of 2,854 patients with chronic Chagas cardiomyopathy conducted at 49 centers in Argentina, Bolivia, Brazil, Columbia, and El Salvador, the researchers set out to evaluate the efficacy and safety of benznidazole, compared with placebo, in reducing the clinical outcomes in patients with chronic Chagas cardiomyopathy. Of the 2,854 patients, slightly more than half (1,431) received benznidazole, while the remaining 1,423 received placebo for up to 80 days and were followed for a mean of 5.4 years. The primary outcome was the first event of any of the components of the composite outcome of death, resuscitated cardiac arrest, sustained ventricular tachycardia, insertion of a pacemaker or implantable cardioverter-defibrillator, cardiac transplantation, new heart failure, stroke, or other thromboembolic event. Secondary outcomes included the response to treatment on the basis of results on PCR assay overall and according to geographic region.
The proportion of study participants who achieved the primary outcome was statistically similar between the two groups: 27.% in the benznidazole group, compared with 29.1% in the placebo group (adjusted hazard ratio of .092; P = .26). The researchers observed no significant between-group differences in any component of the primary outcome.
In terms of secondary outcomes, the rates of conversion to negative PCR results were 66.2% in the benznidazole group, compared with 33.5% in the placebo group at the end of treatment. Between-group differences were sustained at 2 years (55.4% and 35.3%, respectively) and at 5 years or more (46.7% vs. 33.1%; P less than .001 for all comparisons). At the same time, rates of PCR conversion varied according to geographic region. For example, the odds ratio for PCR conversion was highest in Brazil (odds ratio, 3.03 at 2 years and OR, 1.87 at 5 or more years) and lowest in Columbia and El Salvador (OR, 1.33 at 2 years and OR, 0.96 at 5 years). “Since we do not have genotype information, we had to infer that patients in certain geographic regions were likely to have distinct T. cruzi strains,” the authors wrote.
They acknowledged certain limitations of the study, including the fact that “variable responses to benznidazole have been reported previously and may have contributed to our neutral findings. Further analyses of stored blood samples by means of quantitative PCR and genotyping may provide a more precise characterization of T. cruzi that can be used to assess whether genotype influences the clinical response to benznidazole.”
They concluded that the current findings “do not challenge current guidelines that recommend treatment with trypanocidal therapy in the early stages of chronic Chagas infection. ... and should not detract from the pursuit of general goals for exploring more effective or earlier treatments with new drugs or drug combinations.”
The study was funded by several sources, including the Population Health Research Institute, the Canadian Institutes of Health Research, the United Nations Children’s Fund, and the World Bank. Dr. Morillo disclosed that he has received lecture fees from Bayer and Boehringer Ingelheim and grant support from Boston Scientific and Merck & Co. Another study author, Dr. Janis Lazdins, disclosed having received consulting fees from Merck. The remaining study authors reporting having no financial disclosures.
Among patients with Chagas cardiomyopathy, trypanocidal therapy with benznidazole significantly reduced serum parasite detection but did not reduce cardiac clinical deterioration through 5 years of follow-up, a randomized trial showed.
Those are key findings from the Benznidazole Evaluation for Interrupting Trypanosomiasis (BENEFIT) trial, which were presented at the annual congress of the European Society of Cardiology and published simultaneously in the New England Journal of Medicine (doi: 10.1056/NEJMoa1507574).
According to lead study authors Dr. Carlos A. Morillo of the Population Health Research Institute at Hamilton Health Sciences and McMaster University, Hamilton, Ont., and Dr. Jose Antonio Marin-Neto of the division of cardiology at the Medical School of Riberao Preto, Brazil, Chagas cardiomyopathy develops in about one-quarter of patients infected with Trypanosoma cruzi. “The identification of T. cruzi antigens in inflamed myocardium with the use of sensitive techniques, such as immunohistochemical analysis and polymerase chain reaction (PCR) assay, suggests that parasite persistence may be an important factor that, in conjunction with individual host factors, triggers the inflammatory process,” they wrote. “In assessing whether trypanocidal therapy prevents or reduces cardiac disease, experimental models of chronic Chagas infection have shown that trypanocidal therapy attenuates the pathologic consequences by reducing the parasite burden. A few small observational and randomized studies involving patients with Chagas disease have shown that benznidazole reduced the circulating parasite load, enhances seroconversion, and may halt the progression of cardiomyopathy.”
In a study of 2,854 patients with chronic Chagas cardiomyopathy conducted at 49 centers in Argentina, Bolivia, Brazil, Columbia, and El Salvador, the researchers set out to evaluate the efficacy and safety of benznidazole, compared with placebo, in reducing the clinical outcomes in patients with chronic Chagas cardiomyopathy. Of the 2,854 patients, slightly more than half (1,431) received benznidazole, while the remaining 1,423 received placebo for up to 80 days and were followed for a mean of 5.4 years. The primary outcome was the first event of any of the components of the composite outcome of death, resuscitated cardiac arrest, sustained ventricular tachycardia, insertion of a pacemaker or implantable cardioverter-defibrillator, cardiac transplantation, new heart failure, stroke, or other thromboembolic event. Secondary outcomes included the response to treatment on the basis of results on PCR assay overall and according to geographic region.
The proportion of study participants who achieved the primary outcome was statistically similar between the two groups: 27.% in the benznidazole group, compared with 29.1% in the placebo group (adjusted hazard ratio of .092; P = .26). The researchers observed no significant between-group differences in any component of the primary outcome.
In terms of secondary outcomes, the rates of conversion to negative PCR results were 66.2% in the benznidazole group, compared with 33.5% in the placebo group at the end of treatment. Between-group differences were sustained at 2 years (55.4% and 35.3%, respectively) and at 5 years or more (46.7% vs. 33.1%; P less than .001 for all comparisons). At the same time, rates of PCR conversion varied according to geographic region. For example, the odds ratio for PCR conversion was highest in Brazil (odds ratio, 3.03 at 2 years and OR, 1.87 at 5 or more years) and lowest in Columbia and El Salvador (OR, 1.33 at 2 years and OR, 0.96 at 5 years). “Since we do not have genotype information, we had to infer that patients in certain geographic regions were likely to have distinct T. cruzi strains,” the authors wrote.
They acknowledged certain limitations of the study, including the fact that “variable responses to benznidazole have been reported previously and may have contributed to our neutral findings. Further analyses of stored blood samples by means of quantitative PCR and genotyping may provide a more precise characterization of T. cruzi that can be used to assess whether genotype influences the clinical response to benznidazole.”
They concluded that the current findings “do not challenge current guidelines that recommend treatment with trypanocidal therapy in the early stages of chronic Chagas infection. ... and should not detract from the pursuit of general goals for exploring more effective or earlier treatments with new drugs or drug combinations.”
The study was funded by several sources, including the Population Health Research Institute, the Canadian Institutes of Health Research, the United Nations Children’s Fund, and the World Bank. Dr. Morillo disclosed that he has received lecture fees from Bayer and Boehringer Ingelheim and grant support from Boston Scientific and Merck & Co. Another study author, Dr. Janis Lazdins, disclosed having received consulting fees from Merck. The remaining study authors reporting having no financial disclosures.
Among patients with Chagas cardiomyopathy, trypanocidal therapy with benznidazole significantly reduced serum parasite detection but did not reduce cardiac clinical deterioration through 5 years of follow-up, a randomized trial showed.
Those are key findings from the Benznidazole Evaluation for Interrupting Trypanosomiasis (BENEFIT) trial, which were presented at the annual congress of the European Society of Cardiology and published simultaneously in the New England Journal of Medicine (doi: 10.1056/NEJMoa1507574).
According to lead study authors Dr. Carlos A. Morillo of the Population Health Research Institute at Hamilton Health Sciences and McMaster University, Hamilton, Ont., and Dr. Jose Antonio Marin-Neto of the division of cardiology at the Medical School of Riberao Preto, Brazil, Chagas cardiomyopathy develops in about one-quarter of patients infected with Trypanosoma cruzi. “The identification of T. cruzi antigens in inflamed myocardium with the use of sensitive techniques, such as immunohistochemical analysis and polymerase chain reaction (PCR) assay, suggests that parasite persistence may be an important factor that, in conjunction with individual host factors, triggers the inflammatory process,” they wrote. “In assessing whether trypanocidal therapy prevents or reduces cardiac disease, experimental models of chronic Chagas infection have shown that trypanocidal therapy attenuates the pathologic consequences by reducing the parasite burden. A few small observational and randomized studies involving patients with Chagas disease have shown that benznidazole reduced the circulating parasite load, enhances seroconversion, and may halt the progression of cardiomyopathy.”
In a study of 2,854 patients with chronic Chagas cardiomyopathy conducted at 49 centers in Argentina, Bolivia, Brazil, Columbia, and El Salvador, the researchers set out to evaluate the efficacy and safety of benznidazole, compared with placebo, in reducing the clinical outcomes in patients with chronic Chagas cardiomyopathy. Of the 2,854 patients, slightly more than half (1,431) received benznidazole, while the remaining 1,423 received placebo for up to 80 days and were followed for a mean of 5.4 years. The primary outcome was the first event of any of the components of the composite outcome of death, resuscitated cardiac arrest, sustained ventricular tachycardia, insertion of a pacemaker or implantable cardioverter-defibrillator, cardiac transplantation, new heart failure, stroke, or other thromboembolic event. Secondary outcomes included the response to treatment on the basis of results on PCR assay overall and according to geographic region.
The proportion of study participants who achieved the primary outcome was statistically similar between the two groups: 27.% in the benznidazole group, compared with 29.1% in the placebo group (adjusted hazard ratio of .092; P = .26). The researchers observed no significant between-group differences in any component of the primary outcome.
In terms of secondary outcomes, the rates of conversion to negative PCR results were 66.2% in the benznidazole group, compared with 33.5% in the placebo group at the end of treatment. Between-group differences were sustained at 2 years (55.4% and 35.3%, respectively) and at 5 years or more (46.7% vs. 33.1%; P less than .001 for all comparisons). At the same time, rates of PCR conversion varied according to geographic region. For example, the odds ratio for PCR conversion was highest in Brazil (odds ratio, 3.03 at 2 years and OR, 1.87 at 5 or more years) and lowest in Columbia and El Salvador (OR, 1.33 at 2 years and OR, 0.96 at 5 years). “Since we do not have genotype information, we had to infer that patients in certain geographic regions were likely to have distinct T. cruzi strains,” the authors wrote.
They acknowledged certain limitations of the study, including the fact that “variable responses to benznidazole have been reported previously and may have contributed to our neutral findings. Further analyses of stored blood samples by means of quantitative PCR and genotyping may provide a more precise characterization of T. cruzi that can be used to assess whether genotype influences the clinical response to benznidazole.”
They concluded that the current findings “do not challenge current guidelines that recommend treatment with trypanocidal therapy in the early stages of chronic Chagas infection. ... and should not detract from the pursuit of general goals for exploring more effective or earlier treatments with new drugs or drug combinations.”
The study was funded by several sources, including the Population Health Research Institute, the Canadian Institutes of Health Research, the United Nations Children’s Fund, and the World Bank. Dr. Morillo disclosed that he has received lecture fees from Bayer and Boehringer Ingelheim and grant support from Boston Scientific and Merck & Co. Another study author, Dr. Janis Lazdins, disclosed having received consulting fees from Merck. The remaining study authors reporting having no financial disclosures.
FROM THE ESC CONGRESS 2015
Key clinical point: Benznidazole for Chagas cardiomyopathy did not reduce long-term cardiac clinical deterioration.
Major finding: The proportion of study participants who achieved the primary outcome was statistically similar between the two groups: 27.% in the benznidazole group, compared with 29.1% in the placebo group (adjusted hazard ratio of .92; P = .26).
Data source: A prospective, randomized trial in which 2,854 patients with Chagas cardiomyopathy received benznidazole or placebo for up to 80 days and were followed for a mean of 5.4 years.
Disclosures: The study was funded by several sources, including the Population Health Research Institute, the Canadian Institutes of Health Research, the United Nations Children’s Fund, and the World Bank. Dr. Morillo disclosed that he has received lecture fees from Bayer and Boehringer Ingelheim and grant support from Boston Scientific and Merck & Co. Another study author, Dr. Janis Lazdins, disclosed having received consulting fees from Merck. The remaining study authors reported having no financial disclosures.
ESC: Novel apnea treatment not helpful, possibly harmful in heart failure
Adaptive servo-ventilation is not beneficial and may even be harmful for patients who have predominantly central sleep apnea accompanying heart failure with reduced ejection fraction, Dr. Martin R. Cowie reported at the annual congress of the European Society of Cardiology.
The noninvasive therapy did control central sleep apnea in a large international randomized controlled trial, but nevertheless did not affect the composite end point of death from any cause, lifesaving cardiovascular intervention, or unplanned hospitalization for worsening HF. Moreover, it unexpectedly raised the risk of cardiovascular death by 34%, and significantly increased all-cause mortality as well, said Dr. Cowie of Imperial College London.
Adaptive servo-ventilation delivers servo-controlled inspiratory pressure on top of expiratory positive airway pressure during sleep, to alleviate central sleep apnea. This form of sleep-disordered breathing, which may manifest as Cheyne-Stokes respiration in patients who have HF with reduced ejection fraction, is reported to affect up to 40% of this patient population. Its prevalence rises as the severity of HF increases, and it is an independent risk marker for poor prognosis and death in HF.
A recent trial showed that continuous positive airway pressure (CPAP) did not improve morbidity or mortality in patients who had HF with central sleep apnea, but suggested that a treatment that could reduce the apnea-hypopnea index (AHI) – the number of apnea or hypopnea events per hour of sleep – to below 15 might be effective. Adaptive servo-ventilation can accomplish this, and small studies and meta-analyses have shown that the treatment improves surrogate markers including plasma concentration of brain natriuretic peptide, left ventricular ejection fraction (LVEF), and functional outcomes in heart failure.
Dr. Cowie and his associates conducted the SERVE-HF trial, assessing the effect of adding adaptive servo-ventilation to guideline-based medical therapy on survival and cardiovascular outcomes. He presented the trial results at the meeting, and they were simultaneously published online (N Engl J Med. 2015 Sep 1. doi:10.1056/NEJMoa1506459).
The industry-sponsored study comprised 1,325 patients aged 22 and older treated and followed at 91 medical centers for a median of 31 months (range, 0-80 months). They were randomly assigned to receive medical therapy plus adaptive servo-ventilation delivered through a face mask for at least 5 hours every night (666 intervention subjects) or medical therapy alone (659 control subjects).
Central sleep apnea was well controlled only in the intervention group. At 1 year, their mean AHI was 6.6 events per hour, and the oxygen desaturation index – the number of times per hour that the blood oxygen level dropped by 3 or more percentage points from baseline level – was 8.6.
Yet the primary composite end point was not significantly different between the two study groups: The rate of death from any cause, lifesaving cardiovascular intervention, and unplanned hospitalization for worsening HF was 54.1% with adaptive servo-ventilation and 50.8% without it. The treatment also had no significant effect on a broad spectrum of secondary measures such as symptoms and quality of life. Six-minute walk distance gradually declined in both groups, but that decline was significantly more pronounced in the intervention group, the investigator said.
Even more worrisome was the significant increase in mortality associated with adaptive servo-ventilation. Cardiovascular mortality was 29.9% with the treatment, compared with 24.0% without it, for a hazard ratio of 1.34. All-cause mortality was 34.8% with the treatment and 29.3% without it, for an HR of 1.28.
The reason for this unexpected result is not yet known. One explanation is that central sleep apnea may be a compensatory mechanism with potentially beneficial effects in patients who have HF. Attenuating those effects with adaptive servo-ventilation may then have been detrimental. For example, central sleep apnea, and particularly Cheyne-Stokes breathing, may beneficially activate the respiratory muscles, increase sympathetic nervous system activity, induce hypercapnic acidosis, increase end-expiratory lung volume, and raise intrinsic positive airway pressure.
Another possibility is that applying positive airway pressure with adaptive servo-ventilation may impair cardiac function in at least a portion of patients who have HF by decreasing cardiac output and stroke volume during treatment.
ResMed, maker of the AutoSet adaptive servo-ventilator, sponsored SERVE-HF, which was also supported by the National Institute for Health Research and the National Institutes of Health. Dr. Cowie disclosed ties with Servier, Novartis, Pfizer, St. Jude Medical, Boston Scientific, Respicardia,Medtronic, and Bayer; his associates reported ties to numerous industry sources.
Adaptive servo-ventilation should not be used outside of clinical trials in heart failure patients who have predominantly central sleep apnea, at least until the reason for the unexpected 34% increase in cardiovascular mortality is understood.
The issue is important because at least one new technique to abolish Cheyne-Stokes respiration that doesn’t use positive pressure therapy – phrenic-nerve stimulation – has already been developed and is being assessed in a clinical trial. If Cheyne-Stokes respiration is actually beneficial in HF, this strategy may prove harmful.
Dr. Ulysses J. Magalang is in the division of pulmonary, allergy, critical care, and sleep medicine at Ohio State University Wexner Medical Center, Columbus. Dr. Allan I. Pack is at the Center for Sleep and Circadian Neurobiology at the University of Pennsylvania, Philadelphia. Dr. Magalang reported grants support from the Rudi Schulte Family Foundation, Hill-Rom, and the Tzagournis Medical Research Endowment; Dr. Pack reported having no relevant financial disclosures. They made these remarks in an editorial accompanying the SERVE-HF report (N Engl J Med. 2015 Sep 1. doi:10.1056/NEJMe1510397Th).
Adaptive servo-ventilation should not be used outside of clinical trials in heart failure patients who have predominantly central sleep apnea, at least until the reason for the unexpected 34% increase in cardiovascular mortality is understood.
The issue is important because at least one new technique to abolish Cheyne-Stokes respiration that doesn’t use positive pressure therapy – phrenic-nerve stimulation – has already been developed and is being assessed in a clinical trial. If Cheyne-Stokes respiration is actually beneficial in HF, this strategy may prove harmful.
Dr. Ulysses J. Magalang is in the division of pulmonary, allergy, critical care, and sleep medicine at Ohio State University Wexner Medical Center, Columbus. Dr. Allan I. Pack is at the Center for Sleep and Circadian Neurobiology at the University of Pennsylvania, Philadelphia. Dr. Magalang reported grants support from the Rudi Schulte Family Foundation, Hill-Rom, and the Tzagournis Medical Research Endowment; Dr. Pack reported having no relevant financial disclosures. They made these remarks in an editorial accompanying the SERVE-HF report (N Engl J Med. 2015 Sep 1. doi:10.1056/NEJMe1510397Th).
Adaptive servo-ventilation should not be used outside of clinical trials in heart failure patients who have predominantly central sleep apnea, at least until the reason for the unexpected 34% increase in cardiovascular mortality is understood.
The issue is important because at least one new technique to abolish Cheyne-Stokes respiration that doesn’t use positive pressure therapy – phrenic-nerve stimulation – has already been developed and is being assessed in a clinical trial. If Cheyne-Stokes respiration is actually beneficial in HF, this strategy may prove harmful.
Dr. Ulysses J. Magalang is in the division of pulmonary, allergy, critical care, and sleep medicine at Ohio State University Wexner Medical Center, Columbus. Dr. Allan I. Pack is at the Center for Sleep and Circadian Neurobiology at the University of Pennsylvania, Philadelphia. Dr. Magalang reported grants support from the Rudi Schulte Family Foundation, Hill-Rom, and the Tzagournis Medical Research Endowment; Dr. Pack reported having no relevant financial disclosures. They made these remarks in an editorial accompanying the SERVE-HF report (N Engl J Med. 2015 Sep 1. doi:10.1056/NEJMe1510397Th).
Adaptive servo-ventilation is not beneficial and may even be harmful for patients who have predominantly central sleep apnea accompanying heart failure with reduced ejection fraction, Dr. Martin R. Cowie reported at the annual congress of the European Society of Cardiology.
The noninvasive therapy did control central sleep apnea in a large international randomized controlled trial, but nevertheless did not affect the composite end point of death from any cause, lifesaving cardiovascular intervention, or unplanned hospitalization for worsening HF. Moreover, it unexpectedly raised the risk of cardiovascular death by 34%, and significantly increased all-cause mortality as well, said Dr. Cowie of Imperial College London.
Adaptive servo-ventilation delivers servo-controlled inspiratory pressure on top of expiratory positive airway pressure during sleep, to alleviate central sleep apnea. This form of sleep-disordered breathing, which may manifest as Cheyne-Stokes respiration in patients who have HF with reduced ejection fraction, is reported to affect up to 40% of this patient population. Its prevalence rises as the severity of HF increases, and it is an independent risk marker for poor prognosis and death in HF.
A recent trial showed that continuous positive airway pressure (CPAP) did not improve morbidity or mortality in patients who had HF with central sleep apnea, but suggested that a treatment that could reduce the apnea-hypopnea index (AHI) – the number of apnea or hypopnea events per hour of sleep – to below 15 might be effective. Adaptive servo-ventilation can accomplish this, and small studies and meta-analyses have shown that the treatment improves surrogate markers including plasma concentration of brain natriuretic peptide, left ventricular ejection fraction (LVEF), and functional outcomes in heart failure.
Dr. Cowie and his associates conducted the SERVE-HF trial, assessing the effect of adding adaptive servo-ventilation to guideline-based medical therapy on survival and cardiovascular outcomes. He presented the trial results at the meeting, and they were simultaneously published online (N Engl J Med. 2015 Sep 1. doi:10.1056/NEJMoa1506459).
The industry-sponsored study comprised 1,325 patients aged 22 and older treated and followed at 91 medical centers for a median of 31 months (range, 0-80 months). They were randomly assigned to receive medical therapy plus adaptive servo-ventilation delivered through a face mask for at least 5 hours every night (666 intervention subjects) or medical therapy alone (659 control subjects).
Central sleep apnea was well controlled only in the intervention group. At 1 year, their mean AHI was 6.6 events per hour, and the oxygen desaturation index – the number of times per hour that the blood oxygen level dropped by 3 or more percentage points from baseline level – was 8.6.
Yet the primary composite end point was not significantly different between the two study groups: The rate of death from any cause, lifesaving cardiovascular intervention, and unplanned hospitalization for worsening HF was 54.1% with adaptive servo-ventilation and 50.8% without it. The treatment also had no significant effect on a broad spectrum of secondary measures such as symptoms and quality of life. Six-minute walk distance gradually declined in both groups, but that decline was significantly more pronounced in the intervention group, the investigator said.
Even more worrisome was the significant increase in mortality associated with adaptive servo-ventilation. Cardiovascular mortality was 29.9% with the treatment, compared with 24.0% without it, for a hazard ratio of 1.34. All-cause mortality was 34.8% with the treatment and 29.3% without it, for an HR of 1.28.
The reason for this unexpected result is not yet known. One explanation is that central sleep apnea may be a compensatory mechanism with potentially beneficial effects in patients who have HF. Attenuating those effects with adaptive servo-ventilation may then have been detrimental. For example, central sleep apnea, and particularly Cheyne-Stokes breathing, may beneficially activate the respiratory muscles, increase sympathetic nervous system activity, induce hypercapnic acidosis, increase end-expiratory lung volume, and raise intrinsic positive airway pressure.
Another possibility is that applying positive airway pressure with adaptive servo-ventilation may impair cardiac function in at least a portion of patients who have HF by decreasing cardiac output and stroke volume during treatment.
ResMed, maker of the AutoSet adaptive servo-ventilator, sponsored SERVE-HF, which was also supported by the National Institute for Health Research and the National Institutes of Health. Dr. Cowie disclosed ties with Servier, Novartis, Pfizer, St. Jude Medical, Boston Scientific, Respicardia,Medtronic, and Bayer; his associates reported ties to numerous industry sources.
Adaptive servo-ventilation is not beneficial and may even be harmful for patients who have predominantly central sleep apnea accompanying heart failure with reduced ejection fraction, Dr. Martin R. Cowie reported at the annual congress of the European Society of Cardiology.
The noninvasive therapy did control central sleep apnea in a large international randomized controlled trial, but nevertheless did not affect the composite end point of death from any cause, lifesaving cardiovascular intervention, or unplanned hospitalization for worsening HF. Moreover, it unexpectedly raised the risk of cardiovascular death by 34%, and significantly increased all-cause mortality as well, said Dr. Cowie of Imperial College London.
Adaptive servo-ventilation delivers servo-controlled inspiratory pressure on top of expiratory positive airway pressure during sleep, to alleviate central sleep apnea. This form of sleep-disordered breathing, which may manifest as Cheyne-Stokes respiration in patients who have HF with reduced ejection fraction, is reported to affect up to 40% of this patient population. Its prevalence rises as the severity of HF increases, and it is an independent risk marker for poor prognosis and death in HF.
A recent trial showed that continuous positive airway pressure (CPAP) did not improve morbidity or mortality in patients who had HF with central sleep apnea, but suggested that a treatment that could reduce the apnea-hypopnea index (AHI) – the number of apnea or hypopnea events per hour of sleep – to below 15 might be effective. Adaptive servo-ventilation can accomplish this, and small studies and meta-analyses have shown that the treatment improves surrogate markers including plasma concentration of brain natriuretic peptide, left ventricular ejection fraction (LVEF), and functional outcomes in heart failure.
Dr. Cowie and his associates conducted the SERVE-HF trial, assessing the effect of adding adaptive servo-ventilation to guideline-based medical therapy on survival and cardiovascular outcomes. He presented the trial results at the meeting, and they were simultaneously published online (N Engl J Med. 2015 Sep 1. doi:10.1056/NEJMoa1506459).
The industry-sponsored study comprised 1,325 patients aged 22 and older treated and followed at 91 medical centers for a median of 31 months (range, 0-80 months). They were randomly assigned to receive medical therapy plus adaptive servo-ventilation delivered through a face mask for at least 5 hours every night (666 intervention subjects) or medical therapy alone (659 control subjects).
Central sleep apnea was well controlled only in the intervention group. At 1 year, their mean AHI was 6.6 events per hour, and the oxygen desaturation index – the number of times per hour that the blood oxygen level dropped by 3 or more percentage points from baseline level – was 8.6.
Yet the primary composite end point was not significantly different between the two study groups: The rate of death from any cause, lifesaving cardiovascular intervention, and unplanned hospitalization for worsening HF was 54.1% with adaptive servo-ventilation and 50.8% without it. The treatment also had no significant effect on a broad spectrum of secondary measures such as symptoms and quality of life. Six-minute walk distance gradually declined in both groups, but that decline was significantly more pronounced in the intervention group, the investigator said.
Even more worrisome was the significant increase in mortality associated with adaptive servo-ventilation. Cardiovascular mortality was 29.9% with the treatment, compared with 24.0% without it, for a hazard ratio of 1.34. All-cause mortality was 34.8% with the treatment and 29.3% without it, for an HR of 1.28.
The reason for this unexpected result is not yet known. One explanation is that central sleep apnea may be a compensatory mechanism with potentially beneficial effects in patients who have HF. Attenuating those effects with adaptive servo-ventilation may then have been detrimental. For example, central sleep apnea, and particularly Cheyne-Stokes breathing, may beneficially activate the respiratory muscles, increase sympathetic nervous system activity, induce hypercapnic acidosis, increase end-expiratory lung volume, and raise intrinsic positive airway pressure.
Another possibility is that applying positive airway pressure with adaptive servo-ventilation may impair cardiac function in at least a portion of patients who have HF by decreasing cardiac output and stroke volume during treatment.
ResMed, maker of the AutoSet adaptive servo-ventilator, sponsored SERVE-HF, which was also supported by the National Institute for Health Research and the National Institutes of Health. Dr. Cowie disclosed ties with Servier, Novartis, Pfizer, St. Jude Medical, Boston Scientific, Respicardia,Medtronic, and Bayer; his associates reported ties to numerous industry sources.
FROM THE ESC CONGRESS 2015
Key clinical point: Adaptive servo-ventilation is not beneficial and may even be harmful for central sleep apnea accompanying heart failure.
Major finding: The composite rate of death from any cause, lifesaving cardiovascular intervention, and unplanned hospitalization for worsening HF was 54.1% with adaptive servo-ventilation and 50.8% without it, a nonsignificant difference.
Data source: An international randomized clinical trial involving 1,325 adults followed for a median of 31 months.
Disclosures: ResMed, maker of the AutoSet adaptive servo-ventilator, sponsored SERVE-HF, which was also supported by the National Institute for Health Research and the National Institutes of Health. Dr. Cowie disclosed ties with Servier, Novartis, Pfizer, St. Jude Medical, Boston Scientific, Respicardia,Medtronic, and Bayer; his associates reported ties to numerous industry sources.
VIDEO: Newer Type 2 Diabetes Drugs Pose No Significant Heart Failure Risk
LONDON – Neither the GLP-1 receptor agonist lixisenatide nor the DPP-4 inhibitor sitagliptin significantly increased the risk of heart failure or associated hospitalizations in patients with type 2 diabetes, according to data from two large cardiovascular safety trials.
Further analysis from ELIXA (Evaluation of Lixisenatide [Lyxumia] in Acute Coronary Syndrome) showed that the hazard ratios for several secondary heart failure endpoints were 1.00 or below. Although the risk for heart failure hospitalization was found to be nine times higher in patients who had a prior history of heart failure than in those who did not, there was there was no difference between treatment with the GLP-1 (glucagon-like peptide 1) agonist or placebo.
The findings add to those already presented in June at the annual scientific sessions of the American Diabetes Association from the 6,068-patient trial, which enrolled patients with type 2 diabetes who had experienced an acute coronary syndrome within the past 6 months.
Other reassuring data on the safety of newer diabetes medicines came from an updated analysis of TECOS (Trial Evaluating Cardiovascular Outcomes With Sitagliptin [Januvia]). The time to first hospitalization for heart failure did not differ between the placebo and sitagliptin arms, and there were no differences between the treatments in terms of hospitalization for heart failure or cardiovascular death or hospitalization for heart failure or all-cause death with the DPP-4 (dipeptyl peptidase 4) inhibitor. TECOS enrolled nearly 15,000 patients with type 2 diabetes and concurrent cardiovascular disease who were aged 50 years or older and the primary findings have been published (N Engl J Med. 2015 July 15;373:232-42).
These trials provide accumulating evidence that there is no heart failure risk with these particular diabetes medications, Dr. Lars Rydén, professor of cardiology at the Karolinska Institute in Stockholm, commented in an interview at the annual congress of the European Society of Cardiology. Dr. Rydén added that the trial results everyone is waiting to hear about concern the cardiovascular safety of the selective sodium–glucose cotransporter-2 (SGLT-2) inhibitor empagliflozin (Jardiance).
Advance information issued by manufacturer Boehringer-Ingelheim suggests that this drug actually may lower cardiovascular risk in patients at high risk for cardiovascular events, Dr. Rydén observed. “Now, if that is true, it is the only modern glucose-lowering drug to have shown such a capacity.” Results of the EMPA-REG OUTCOME study will be presented in September at the annual meeting of the European Association for the Study of Diabetes in Stockholm.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LONDON – Neither the GLP-1 receptor agonist lixisenatide nor the DPP-4 inhibitor sitagliptin significantly increased the risk of heart failure or associated hospitalizations in patients with type 2 diabetes, according to data from two large cardiovascular safety trials.
Further analysis from ELIXA (Evaluation of Lixisenatide [Lyxumia] in Acute Coronary Syndrome) showed that the hazard ratios for several secondary heart failure endpoints were 1.00 or below. Although the risk for heart failure hospitalization was found to be nine times higher in patients who had a prior history of heart failure than in those who did not, there was there was no difference between treatment with the GLP-1 (glucagon-like peptide 1) agonist or placebo.
The findings add to those already presented in June at the annual scientific sessions of the American Diabetes Association from the 6,068-patient trial, which enrolled patients with type 2 diabetes who had experienced an acute coronary syndrome within the past 6 months.
Other reassuring data on the safety of newer diabetes medicines came from an updated analysis of TECOS (Trial Evaluating Cardiovascular Outcomes With Sitagliptin [Januvia]). The time to first hospitalization for heart failure did not differ between the placebo and sitagliptin arms, and there were no differences between the treatments in terms of hospitalization for heart failure or cardiovascular death or hospitalization for heart failure or all-cause death with the DPP-4 (dipeptyl peptidase 4) inhibitor. TECOS enrolled nearly 15,000 patients with type 2 diabetes and concurrent cardiovascular disease who were aged 50 years or older and the primary findings have been published (N Engl J Med. 2015 July 15;373:232-42).
These trials provide accumulating evidence that there is no heart failure risk with these particular diabetes medications, Dr. Lars Rydén, professor of cardiology at the Karolinska Institute in Stockholm, commented in an interview at the annual congress of the European Society of Cardiology. Dr. Rydén added that the trial results everyone is waiting to hear about concern the cardiovascular safety of the selective sodium–glucose cotransporter-2 (SGLT-2) inhibitor empagliflozin (Jardiance).
Advance information issued by manufacturer Boehringer-Ingelheim suggests that this drug actually may lower cardiovascular risk in patients at high risk for cardiovascular events, Dr. Rydén observed. “Now, if that is true, it is the only modern glucose-lowering drug to have shown such a capacity.” Results of the EMPA-REG OUTCOME study will be presented in September at the annual meeting of the European Association for the Study of Diabetes in Stockholm.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LONDON – Neither the GLP-1 receptor agonist lixisenatide nor the DPP-4 inhibitor sitagliptin significantly increased the risk of heart failure or associated hospitalizations in patients with type 2 diabetes, according to data from two large cardiovascular safety trials.
Further analysis from ELIXA (Evaluation of Lixisenatide [Lyxumia] in Acute Coronary Syndrome) showed that the hazard ratios for several secondary heart failure endpoints were 1.00 or below. Although the risk for heart failure hospitalization was found to be nine times higher in patients who had a prior history of heart failure than in those who did not, there was there was no difference between treatment with the GLP-1 (glucagon-like peptide 1) agonist or placebo.
The findings add to those already presented in June at the annual scientific sessions of the American Diabetes Association from the 6,068-patient trial, which enrolled patients with type 2 diabetes who had experienced an acute coronary syndrome within the past 6 months.
Other reassuring data on the safety of newer diabetes medicines came from an updated analysis of TECOS (Trial Evaluating Cardiovascular Outcomes With Sitagliptin [Januvia]). The time to first hospitalization for heart failure did not differ between the placebo and sitagliptin arms, and there were no differences between the treatments in terms of hospitalization for heart failure or cardiovascular death or hospitalization for heart failure or all-cause death with the DPP-4 (dipeptyl peptidase 4) inhibitor. TECOS enrolled nearly 15,000 patients with type 2 diabetes and concurrent cardiovascular disease who were aged 50 years or older and the primary findings have been published (N Engl J Med. 2015 July 15;373:232-42).
These trials provide accumulating evidence that there is no heart failure risk with these particular diabetes medications, Dr. Lars Rydén, professor of cardiology at the Karolinska Institute in Stockholm, commented in an interview at the annual congress of the European Society of Cardiology. Dr. Rydén added that the trial results everyone is waiting to hear about concern the cardiovascular safety of the selective sodium–glucose cotransporter-2 (SGLT-2) inhibitor empagliflozin (Jardiance).
Advance information issued by manufacturer Boehringer-Ingelheim suggests that this drug actually may lower cardiovascular risk in patients at high risk for cardiovascular events, Dr. Rydén observed. “Now, if that is true, it is the only modern glucose-lowering drug to have shown such a capacity.” Results of the EMPA-REG OUTCOME study will be presented in September at the annual meeting of the European Association for the Study of Diabetes in Stockholm.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
VIDEO: Newer type 2 diabetes drugs pose no significant heart failure risk
LONDON – Neither the GLP-1 receptor agonist lixisenatide nor the DPP-4 inhibitor sitagliptin significantly increased the risk of heart failure or associated hospitalizations in patients with type 2 diabetes, according to data from two large cardiovascular safety trials.
Further analysis from ELIXA (Evaluation of Lixisenatide [Lyxumia] in Acute Coronary Syndrome) showed that the hazard ratios for several secondary heart failure endpoints were 1.00 or below. Although the risk for heart failure hospitalization was found to be nine times higher in patients who had a prior history of heart failure than in those who did not, there was there was no difference between treatment with the GLP-1 (glucagon-like peptide 1) agonist or placebo.
The findings add to those already presented in June at the annual scientific sessions of the American Diabetes Association from the 6,068-patient trial, which enrolled patients with type 2 diabetes who had experienced an acute coronary syndrome within the past 6 months.
Other reassuring data on the safety of newer diabetes medicines came from an updated analysis of TECOS (Trial Evaluating Cardiovascular Outcomes With Sitagliptin [Januvia]). The time to first hospitalization for heart failure did not differ between the placebo and sitagliptin arms, and there were no differences between the treatments in terms of hospitalization for heart failure or cardiovascular death or hospitalization for heart failure or all-cause death with the DPP-4 (dipeptyl peptidase 4) inhibitor. TECOS enrolled nearly 15,000 patients with type 2 diabetes and concurrent cardiovascular disease who were aged 50 years or older and the primary findings have been published (N Engl J Med. 2015 July 15;373:232-42).
These trials provide accumulating evidence that there is no heart failure risk with these particular diabetes medications, Dr. Lars Rydén, professor of cardiology at the Karolinska Institute in Stockholm, commented in an interview at the annual congress of the European Society of Cardiology. Dr. Rydén added that the trial results everyone is waiting to hear about concern the cardiovascular safety of the selective sodium–glucose cotransporter-2 (SGLT-2) inhibitor empagliflozin (Jardiance).
Advance information issued by manufacturer Boehringer-Ingelheim suggests that this drug actually may lower cardiovascular risk in patients at high risk for cardiovascular events, Dr. Rydén observed. “Now, if that is true, it is the only modern glucose-lowering drug to have shown such a capacity.” Results of the EMPA-REG OUTCOME study will be presented in September at the annual meeting of the European Association for the Study of Diabetes in Stockholm.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LONDON – Neither the GLP-1 receptor agonist lixisenatide nor the DPP-4 inhibitor sitagliptin significantly increased the risk of heart failure or associated hospitalizations in patients with type 2 diabetes, according to data from two large cardiovascular safety trials.
Further analysis from ELIXA (Evaluation of Lixisenatide [Lyxumia] in Acute Coronary Syndrome) showed that the hazard ratios for several secondary heart failure endpoints were 1.00 or below. Although the risk for heart failure hospitalization was found to be nine times higher in patients who had a prior history of heart failure than in those who did not, there was there was no difference between treatment with the GLP-1 (glucagon-like peptide 1) agonist or placebo.
The findings add to those already presented in June at the annual scientific sessions of the American Diabetes Association from the 6,068-patient trial, which enrolled patients with type 2 diabetes who had experienced an acute coronary syndrome within the past 6 months.
Other reassuring data on the safety of newer diabetes medicines came from an updated analysis of TECOS (Trial Evaluating Cardiovascular Outcomes With Sitagliptin [Januvia]). The time to first hospitalization for heart failure did not differ between the placebo and sitagliptin arms, and there were no differences between the treatments in terms of hospitalization for heart failure or cardiovascular death or hospitalization for heart failure or all-cause death with the DPP-4 (dipeptyl peptidase 4) inhibitor. TECOS enrolled nearly 15,000 patients with type 2 diabetes and concurrent cardiovascular disease who were aged 50 years or older and the primary findings have been published (N Engl J Med. 2015 July 15;373:232-42).
These trials provide accumulating evidence that there is no heart failure risk with these particular diabetes medications, Dr. Lars Rydén, professor of cardiology at the Karolinska Institute in Stockholm, commented in an interview at the annual congress of the European Society of Cardiology. Dr. Rydén added that the trial results everyone is waiting to hear about concern the cardiovascular safety of the selective sodium–glucose cotransporter-2 (SGLT-2) inhibitor empagliflozin (Jardiance).
Advance information issued by manufacturer Boehringer-Ingelheim suggests that this drug actually may lower cardiovascular risk in patients at high risk for cardiovascular events, Dr. Rydén observed. “Now, if that is true, it is the only modern glucose-lowering drug to have shown such a capacity.” Results of the EMPA-REG OUTCOME study will be presented in September at the annual meeting of the European Association for the Study of Diabetes in Stockholm.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LONDON – Neither the GLP-1 receptor agonist lixisenatide nor the DPP-4 inhibitor sitagliptin significantly increased the risk of heart failure or associated hospitalizations in patients with type 2 diabetes, according to data from two large cardiovascular safety trials.
Further analysis from ELIXA (Evaluation of Lixisenatide [Lyxumia] in Acute Coronary Syndrome) showed that the hazard ratios for several secondary heart failure endpoints were 1.00 or below. Although the risk for heart failure hospitalization was found to be nine times higher in patients who had a prior history of heart failure than in those who did not, there was there was no difference between treatment with the GLP-1 (glucagon-like peptide 1) agonist or placebo.
The findings add to those already presented in June at the annual scientific sessions of the American Diabetes Association from the 6,068-patient trial, which enrolled patients with type 2 diabetes who had experienced an acute coronary syndrome within the past 6 months.
Other reassuring data on the safety of newer diabetes medicines came from an updated analysis of TECOS (Trial Evaluating Cardiovascular Outcomes With Sitagliptin [Januvia]). The time to first hospitalization for heart failure did not differ between the placebo and sitagliptin arms, and there were no differences between the treatments in terms of hospitalization for heart failure or cardiovascular death or hospitalization for heart failure or all-cause death with the DPP-4 (dipeptyl peptidase 4) inhibitor. TECOS enrolled nearly 15,000 patients with type 2 diabetes and concurrent cardiovascular disease who were aged 50 years or older and the primary findings have been published (N Engl J Med. 2015 July 15;373:232-42).
These trials provide accumulating evidence that there is no heart failure risk with these particular diabetes medications, Dr. Lars Rydén, professor of cardiology at the Karolinska Institute in Stockholm, commented in an interview at the annual congress of the European Society of Cardiology. Dr. Rydén added that the trial results everyone is waiting to hear about concern the cardiovascular safety of the selective sodium–glucose cotransporter-2 (SGLT-2) inhibitor empagliflozin (Jardiance).
Advance information issued by manufacturer Boehringer-Ingelheim suggests that this drug actually may lower cardiovascular risk in patients at high risk for cardiovascular events, Dr. Rydén observed. “Now, if that is true, it is the only modern glucose-lowering drug to have shown such a capacity.” Results of the EMPA-REG OUTCOME study will be presented in September at the annual meeting of the European Association for the Study of Diabetes in Stockholm.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ESC: Aldosterone blockade fails to fly for early MI in ALBATROSS
LONDON – Aldosterone blockade with oral spironolactone showed a disappointing lack of clinical benefit when initiated in the first hours after an acute MI without heart failure in the large, randomized ALBATROSS trial.
ALBATROSS did, however, flash a silver lining under one wing: A whopping 80% reduction in 6-month mortality in a prespecified subgroup analysis restricted to the 1,229 participants with ST-elevation MI, Dr. Gilles Montalescot reported at the annual congress of the European Society of Cardiology.
Although this finding is intriguing, hypothesis-generating, and definitely warrants a confirmatory study, he continued, mortality was nevertheless merely a secondary endpoint in ALBATROSS (Aldosterone Lethal Effects Blockade in Acute Myocardial Infarction Treated With or Without Reperfusion to Improve Outcome and Survival at Six Months Follow-up).
In contrast, the primary composite outcome was negative, so the takeaway message is clear: “The results of the ALBATROSS study do not warrant the extension of aldosterone blockade to MI patients without heart failure,” said Dr. Montalescot, professor of cardiology at the University of Paris.
ALBATROSS was a multicenter French trial that randomly assigned 1,603 acute MI patients to standard therapy alone or with added mineralocorticoid antagonist therapy started within the first 2 days of their coronary event. Often the aldosterone antagonist was begun in the ambulance en route to the hospital.
The primary endpoint was a composite of death, resuscitated cardiac arrest, ventricular fibrillation or tachycardia, heart failure, or an indication for an implantable cardioverter defibrillator. There were 194 such events, and they occurred at a similar rate in the patients who got 25 mg/day of spironolactone and those who did not.
The rationale for ALBATROSS was sound, according to the cardiologist. Aldosterone is a stress hormone released in acute MI. It has deleterious cardiac effects, including arrhythmias, heart failure, and a dose-dependent increase in mortality, so it makes good sense to block it as soon as possible in MI patients. In the EPHESUS trial, the aldosterone antagonist eplerenone, when started 3-14 days post MI in patients with early heart failure, significantly reduced mortality (N Engl J Med. 2003 Apr 3;348[14]:1309-2), with the bulk of the benefit occurring in patients in whom the drug was started 3-7 days post MI.
Last year, Dr. Montalescot and his coinvestigators published the REMINDER study, in which 1,012 ST-elevation MI (STEMI) patients without heart failure were randomized to eplerenone or placebo within the first 24 hours. The study showed a significant reduction in levels of brain natriuretic peptide or N-terminal pro-BNP in the eplerenone arm (Eur Heart J. 2014 Sep 7;35[34]:2295-302), but that’s not a clinical endpoint. ALBATROSS was the first study to look at the clinical impact of commencing mineralocorticoid antagonist therapy prior to day 3 post MI.
Discussant Dr. John McMurray, professor of cardiology at the University of Glasgow, said that ALBATROSS was simply underpowered and thus leaves unanswered the clinically important question of whether early initiation of aldosterone blockade post MI in patients without heart failure confers clinical benefit. The investigators projected a total of 269 events in the composite endpoint but got only 194 because the study participants were so well treated and contemporary medical and interventional therapies are quite effective.
He dismissed the sharp reduction seen in 6-month mortality with spironolactone in the STEMI patients as “just implausible – we don’t know of any treatments in medicine that reduce mortality by 80%.”
Noting that there were only 28 deaths in the study, Dr. McMurray asserted that “a subgroup analysis on such a small number of events is never going to give you a reliable result.” Moreover, he added, “subgroup analysis is even more treacherous when the overall trial is underpowered.”
Dr. Montalescot replied that, while he considers the signal of a mortality benefit for aldosterone blockade in STEMI patients worthy of pursuit in a large randomized trial, the prospects for mounting such a study are poor. The medications are now available as generics, so there is no commercial incentive. The French Ministry of Health, which funded ALBATROSS, isn’t prepared to back a follow-up study. The best hope is that eventually one of the pharmaceutical companies developing third-generation aldosterone antagonists, now in phase II studies, will become interested, he said.
Dr. Montalescot said that, while he receives research grants and consulting fees from numerous pharmaceutical companies, these commercial relationships aren’t relevant to the government-funded ALBATROSS trial.
LONDON – Aldosterone blockade with oral spironolactone showed a disappointing lack of clinical benefit when initiated in the first hours after an acute MI without heart failure in the large, randomized ALBATROSS trial.
ALBATROSS did, however, flash a silver lining under one wing: A whopping 80% reduction in 6-month mortality in a prespecified subgroup analysis restricted to the 1,229 participants with ST-elevation MI, Dr. Gilles Montalescot reported at the annual congress of the European Society of Cardiology.
Although this finding is intriguing, hypothesis-generating, and definitely warrants a confirmatory study, he continued, mortality was nevertheless merely a secondary endpoint in ALBATROSS (Aldosterone Lethal Effects Blockade in Acute Myocardial Infarction Treated With or Without Reperfusion to Improve Outcome and Survival at Six Months Follow-up).
In contrast, the primary composite outcome was negative, so the takeaway message is clear: “The results of the ALBATROSS study do not warrant the extension of aldosterone blockade to MI patients without heart failure,” said Dr. Montalescot, professor of cardiology at the University of Paris.
ALBATROSS was a multicenter French trial that randomly assigned 1,603 acute MI patients to standard therapy alone or with added mineralocorticoid antagonist therapy started within the first 2 days of their coronary event. Often the aldosterone antagonist was begun in the ambulance en route to the hospital.
The primary endpoint was a composite of death, resuscitated cardiac arrest, ventricular fibrillation or tachycardia, heart failure, or an indication for an implantable cardioverter defibrillator. There were 194 such events, and they occurred at a similar rate in the patients who got 25 mg/day of spironolactone and those who did not.
The rationale for ALBATROSS was sound, according to the cardiologist. Aldosterone is a stress hormone released in acute MI. It has deleterious cardiac effects, including arrhythmias, heart failure, and a dose-dependent increase in mortality, so it makes good sense to block it as soon as possible in MI patients. In the EPHESUS trial, the aldosterone antagonist eplerenone, when started 3-14 days post MI in patients with early heart failure, significantly reduced mortality (N Engl J Med. 2003 Apr 3;348[14]:1309-2), with the bulk of the benefit occurring in patients in whom the drug was started 3-7 days post MI.
Last year, Dr. Montalescot and his coinvestigators published the REMINDER study, in which 1,012 ST-elevation MI (STEMI) patients without heart failure were randomized to eplerenone or placebo within the first 24 hours. The study showed a significant reduction in levels of brain natriuretic peptide or N-terminal pro-BNP in the eplerenone arm (Eur Heart J. 2014 Sep 7;35[34]:2295-302), but that’s not a clinical endpoint. ALBATROSS was the first study to look at the clinical impact of commencing mineralocorticoid antagonist therapy prior to day 3 post MI.
Discussant Dr. John McMurray, professor of cardiology at the University of Glasgow, said that ALBATROSS was simply underpowered and thus leaves unanswered the clinically important question of whether early initiation of aldosterone blockade post MI in patients without heart failure confers clinical benefit. The investigators projected a total of 269 events in the composite endpoint but got only 194 because the study participants were so well treated and contemporary medical and interventional therapies are quite effective.
He dismissed the sharp reduction seen in 6-month mortality with spironolactone in the STEMI patients as “just implausible – we don’t know of any treatments in medicine that reduce mortality by 80%.”
Noting that there were only 28 deaths in the study, Dr. McMurray asserted that “a subgroup analysis on such a small number of events is never going to give you a reliable result.” Moreover, he added, “subgroup analysis is even more treacherous when the overall trial is underpowered.”
Dr. Montalescot replied that, while he considers the signal of a mortality benefit for aldosterone blockade in STEMI patients worthy of pursuit in a large randomized trial, the prospects for mounting such a study are poor. The medications are now available as generics, so there is no commercial incentive. The French Ministry of Health, which funded ALBATROSS, isn’t prepared to back a follow-up study. The best hope is that eventually one of the pharmaceutical companies developing third-generation aldosterone antagonists, now in phase II studies, will become interested, he said.
Dr. Montalescot said that, while he receives research grants and consulting fees from numerous pharmaceutical companies, these commercial relationships aren’t relevant to the government-funded ALBATROSS trial.
LONDON – Aldosterone blockade with oral spironolactone showed a disappointing lack of clinical benefit when initiated in the first hours after an acute MI without heart failure in the large, randomized ALBATROSS trial.
ALBATROSS did, however, flash a silver lining under one wing: A whopping 80% reduction in 6-month mortality in a prespecified subgroup analysis restricted to the 1,229 participants with ST-elevation MI, Dr. Gilles Montalescot reported at the annual congress of the European Society of Cardiology.
Although this finding is intriguing, hypothesis-generating, and definitely warrants a confirmatory study, he continued, mortality was nevertheless merely a secondary endpoint in ALBATROSS (Aldosterone Lethal Effects Blockade in Acute Myocardial Infarction Treated With or Without Reperfusion to Improve Outcome and Survival at Six Months Follow-up).
In contrast, the primary composite outcome was negative, so the takeaway message is clear: “The results of the ALBATROSS study do not warrant the extension of aldosterone blockade to MI patients without heart failure,” said Dr. Montalescot, professor of cardiology at the University of Paris.
ALBATROSS was a multicenter French trial that randomly assigned 1,603 acute MI patients to standard therapy alone or with added mineralocorticoid antagonist therapy started within the first 2 days of their coronary event. Often the aldosterone antagonist was begun in the ambulance en route to the hospital.
The primary endpoint was a composite of death, resuscitated cardiac arrest, ventricular fibrillation or tachycardia, heart failure, or an indication for an implantable cardioverter defibrillator. There were 194 such events, and they occurred at a similar rate in the patients who got 25 mg/day of spironolactone and those who did not.
The rationale for ALBATROSS was sound, according to the cardiologist. Aldosterone is a stress hormone released in acute MI. It has deleterious cardiac effects, including arrhythmias, heart failure, and a dose-dependent increase in mortality, so it makes good sense to block it as soon as possible in MI patients. In the EPHESUS trial, the aldosterone antagonist eplerenone, when started 3-14 days post MI in patients with early heart failure, significantly reduced mortality (N Engl J Med. 2003 Apr 3;348[14]:1309-2), with the bulk of the benefit occurring in patients in whom the drug was started 3-7 days post MI.
Last year, Dr. Montalescot and his coinvestigators published the REMINDER study, in which 1,012 ST-elevation MI (STEMI) patients without heart failure were randomized to eplerenone or placebo within the first 24 hours. The study showed a significant reduction in levels of brain natriuretic peptide or N-terminal pro-BNP in the eplerenone arm (Eur Heart J. 2014 Sep 7;35[34]:2295-302), but that’s not a clinical endpoint. ALBATROSS was the first study to look at the clinical impact of commencing mineralocorticoid antagonist therapy prior to day 3 post MI.
Discussant Dr. John McMurray, professor of cardiology at the University of Glasgow, said that ALBATROSS was simply underpowered and thus leaves unanswered the clinically important question of whether early initiation of aldosterone blockade post MI in patients without heart failure confers clinical benefit. The investigators projected a total of 269 events in the composite endpoint but got only 194 because the study participants were so well treated and contemporary medical and interventional therapies are quite effective.
He dismissed the sharp reduction seen in 6-month mortality with spironolactone in the STEMI patients as “just implausible – we don’t know of any treatments in medicine that reduce mortality by 80%.”
Noting that there were only 28 deaths in the study, Dr. McMurray asserted that “a subgroup analysis on such a small number of events is never going to give you a reliable result.” Moreover, he added, “subgroup analysis is even more treacherous when the overall trial is underpowered.”
Dr. Montalescot replied that, while he considers the signal of a mortality benefit for aldosterone blockade in STEMI patients worthy of pursuit in a large randomized trial, the prospects for mounting such a study are poor. The medications are now available as generics, so there is no commercial incentive. The French Ministry of Health, which funded ALBATROSS, isn’t prepared to back a follow-up study. The best hope is that eventually one of the pharmaceutical companies developing third-generation aldosterone antagonists, now in phase II studies, will become interested, he said.
Dr. Montalescot said that, while he receives research grants and consulting fees from numerous pharmaceutical companies, these commercial relationships aren’t relevant to the government-funded ALBATROSS trial.
AT THE ESC CONGRESS 2015
Key clinical point: Giving aldosterone antagonists to acute MI patients without heart failure doesn’t improve clinical outcomes.
Major finding: The 6-month rate of a multipronged composite clinical endpoint was closely similar, regardless of whether patients with acute MI without heart failure were placed on spironolactone within the first couple of days post-MI.
Data source: ALBATROSS was an open-label, multicenter French study in which 1,603 patients were randomized to 6 months of aldosterone blockade or not within the first hours after an acute MI without heart failure.
Disclosures: The investigator-initiated ALBATROSS trial was funded by the French Ministry of Health.
Prolonged TV watching linked to fatal PE
LONDON—Results of a large study suggest that watching television for prolonged periods may increase a person’s risk of fatal pulmonary embolism (PE).
The study, which included more than 86,000 subjects, showed that watching an average of 5 or more hours of TV per day was associated with more than twice the risk of fatal PE as watching less than 2.5 hours daily.
And the risk was higher among younger subjects than older ones.
Toru Shirakawa, of Osaka University in Japan, presented this research at the ESC Congress 2015 (abstract P2686*).
“We showed that prolonged television viewing may be a risky behavior for death from pulmonary embolism,” Shirakawa said. “Leg immobility during television viewing may, in part, explain the finding. Public awareness of the risk of pulmonary embolism from lengthy leg immobility is essential.”
For this research, Shirakawa and his colleagues evaluated 86,024 individuals—36,007 men and 50,017 women ages 40 to 79—who were participating in the Japanese Collaborative Cohort Study.
The subjects completed a self-administered questionnaire that included information about average time spent watching TV each day. They were followed for a median of 18.4 years until 2009. Mortality from PE was determined from death certificates.
Subjects were divided into 3 groups according to the amount of TV they watched per day: less than 2.5 hours, 2.5 to 4.9 hours, and 5 or more hours.
The researchers calculated the risk of death from PE according to the amount of TV watched after adjusting for subjects’ age at baseline, gender, history of hypertension, history of diabetes, smoking status, drinking status, body mass index, walking and sports habits, and menopausal status.
During the follow-up period, there were 59 deaths from PE. And the multiavariate analysis revealed a link between extended TV viewing and fatal PE.
Compared to subjects who tended to watch less than 2.5 hours of TV per day, those who watched an average of 2.5 to 4.9 hours had an increased risk of fatal PE (hazard ratio [HR]=1.59). And the risk was greater among subjects whose average TV viewing time was more than 5 hours per day (HR=2.36).
Among subjects ages 40 to 59, the association between prolonged TV watching and fatal PE was more prominent.
Watching 2.5 to 4.9 hours of TV a day more than tripled the risk of fatal PE when compared to watching less than 2.5 hours (HR=3.24). And watching TV for more than 5 hours a day was associated with a more than 6-fold greater risk of fatal PE than watching less than 2.5 hours (HR=6.49).
Because prolonged leg immobility may explain these findings, Shirakawa and his colleagues recommend taking simple steps to prevent PE while watching TV for extended periods.
“[T]ake a break, stand up, and walk around during the television viewing,” he said. “Drinking water for preventing dehydration is also important.”
Shirakawa also noted that other media-based activities involving prolonged sitting may pose a risk of fatal PE.
“In this era of information technology, use of other visual-based media devices, such as personal computers or smartphones, is popular,” he said.
“Prolonged computer gaming has been associated with death from pulmonary embolism, but, to our knowledge, a relationship with prolonged smartphone use has not yet been reported. More research is needed to assess the risks of prolonged use of new technologies on pulmonary embolism morbidity and mortality.” ![]()
*Information in the abstract differs from that presented at the meeting.
LONDON—Results of a large study suggest that watching television for prolonged periods may increase a person’s risk of fatal pulmonary embolism (PE).
The study, which included more than 86,000 subjects, showed that watching an average of 5 or more hours of TV per day was associated with more than twice the risk of fatal PE as watching less than 2.5 hours daily.
And the risk was higher among younger subjects than older ones.
Toru Shirakawa, of Osaka University in Japan, presented this research at the ESC Congress 2015 (abstract P2686*).
“We showed that prolonged television viewing may be a risky behavior for death from pulmonary embolism,” Shirakawa said. “Leg immobility during television viewing may, in part, explain the finding. Public awareness of the risk of pulmonary embolism from lengthy leg immobility is essential.”
For this research, Shirakawa and his colleagues evaluated 86,024 individuals—36,007 men and 50,017 women ages 40 to 79—who were participating in the Japanese Collaborative Cohort Study.
The subjects completed a self-administered questionnaire that included information about average time spent watching TV each day. They were followed for a median of 18.4 years until 2009. Mortality from PE was determined from death certificates.
Subjects were divided into 3 groups according to the amount of TV they watched per day: less than 2.5 hours, 2.5 to 4.9 hours, and 5 or more hours.
The researchers calculated the risk of death from PE according to the amount of TV watched after adjusting for subjects’ age at baseline, gender, history of hypertension, history of diabetes, smoking status, drinking status, body mass index, walking and sports habits, and menopausal status.
During the follow-up period, there were 59 deaths from PE. And the multiavariate analysis revealed a link between extended TV viewing and fatal PE.
Compared to subjects who tended to watch less than 2.5 hours of TV per day, those who watched an average of 2.5 to 4.9 hours had an increased risk of fatal PE (hazard ratio [HR]=1.59). And the risk was greater among subjects whose average TV viewing time was more than 5 hours per day (HR=2.36).
Among subjects ages 40 to 59, the association between prolonged TV watching and fatal PE was more prominent.
Watching 2.5 to 4.9 hours of TV a day more than tripled the risk of fatal PE when compared to watching less than 2.5 hours (HR=3.24). And watching TV for more than 5 hours a day was associated with a more than 6-fold greater risk of fatal PE than watching less than 2.5 hours (HR=6.49).
Because prolonged leg immobility may explain these findings, Shirakawa and his colleagues recommend taking simple steps to prevent PE while watching TV for extended periods.
“[T]ake a break, stand up, and walk around during the television viewing,” he said. “Drinking water for preventing dehydration is also important.”
Shirakawa also noted that other media-based activities involving prolonged sitting may pose a risk of fatal PE.
“In this era of information technology, use of other visual-based media devices, such as personal computers or smartphones, is popular,” he said.
“Prolonged computer gaming has been associated with death from pulmonary embolism, but, to our knowledge, a relationship with prolonged smartphone use has not yet been reported. More research is needed to assess the risks of prolonged use of new technologies on pulmonary embolism morbidity and mortality.” ![]()
*Information in the abstract differs from that presented at the meeting.
LONDON—Results of a large study suggest that watching television for prolonged periods may increase a person’s risk of fatal pulmonary embolism (PE).
The study, which included more than 86,000 subjects, showed that watching an average of 5 or more hours of TV per day was associated with more than twice the risk of fatal PE as watching less than 2.5 hours daily.
And the risk was higher among younger subjects than older ones.
Toru Shirakawa, of Osaka University in Japan, presented this research at the ESC Congress 2015 (abstract P2686*).
“We showed that prolonged television viewing may be a risky behavior for death from pulmonary embolism,” Shirakawa said. “Leg immobility during television viewing may, in part, explain the finding. Public awareness of the risk of pulmonary embolism from lengthy leg immobility is essential.”
For this research, Shirakawa and his colleagues evaluated 86,024 individuals—36,007 men and 50,017 women ages 40 to 79—who were participating in the Japanese Collaborative Cohort Study.
The subjects completed a self-administered questionnaire that included information about average time spent watching TV each day. They were followed for a median of 18.4 years until 2009. Mortality from PE was determined from death certificates.
Subjects were divided into 3 groups according to the amount of TV they watched per day: less than 2.5 hours, 2.5 to 4.9 hours, and 5 or more hours.
The researchers calculated the risk of death from PE according to the amount of TV watched after adjusting for subjects’ age at baseline, gender, history of hypertension, history of diabetes, smoking status, drinking status, body mass index, walking and sports habits, and menopausal status.
During the follow-up period, there were 59 deaths from PE. And the multiavariate analysis revealed a link between extended TV viewing and fatal PE.
Compared to subjects who tended to watch less than 2.5 hours of TV per day, those who watched an average of 2.5 to 4.9 hours had an increased risk of fatal PE (hazard ratio [HR]=1.59). And the risk was greater among subjects whose average TV viewing time was more than 5 hours per day (HR=2.36).
Among subjects ages 40 to 59, the association between prolonged TV watching and fatal PE was more prominent.
Watching 2.5 to 4.9 hours of TV a day more than tripled the risk of fatal PE when compared to watching less than 2.5 hours (HR=3.24). And watching TV for more than 5 hours a day was associated with a more than 6-fold greater risk of fatal PE than watching less than 2.5 hours (HR=6.49).
Because prolonged leg immobility may explain these findings, Shirakawa and his colleagues recommend taking simple steps to prevent PE while watching TV for extended periods.
“[T]ake a break, stand up, and walk around during the television viewing,” he said. “Drinking water for preventing dehydration is also important.”
Shirakawa also noted that other media-based activities involving prolonged sitting may pose a risk of fatal PE.
“In this era of information technology, use of other visual-based media devices, such as personal computers or smartphones, is popular,” he said.
“Prolonged computer gaming has been associated with death from pulmonary embolism, but, to our knowledge, a relationship with prolonged smartphone use has not yet been reported. More research is needed to assess the risks of prolonged use of new technologies on pulmonary embolism morbidity and mortality.” ![]()
*Information in the abstract differs from that presented at the meeting.
Extra education about apixaban may be unnecessary

Photo courtesy of Pfizer
and Bristol-Myers Squibb
LONDON—An educational program designed to improve adherence to the anticoagulant apixaban proved ineffective in a phase 4 trial of patients with atrial fibrillation (AF).
But that’s because adherence was high whether patients completed the program or not.
This suggests current measures used to inform patients about apixaban may be sufficient to ensure treatment adherence, researchers said.
They presented these findings at the ESC Congress 2015 (abstract 2191).
The research, known as the AEGEAN trial, was sponsored by Bristol-Myers Squibb, the company co-developing apixaban (Eliquis) with Pfizer.
“We used the best possible tools for the educational program, including the usual staff and procedures of the anticoagulation clinics, and all of this was useless,” said study investigator Gilles Montalescot, MD, PhD, of Hospitalier Universitaire Pitié-Salpêtrière in Paris, France.
“However, the trial showed very good adherence to apixaban, leaving little room for improvement with an educational program, suggesting one more advantage of prescribing non-vitamin K antagonists (VKAs) over VKAs in that there is apparently no need for additional education and information.”
Dr Montalescot and his colleagues conducted this study in 1162 AF patients receiving apixaban as stroke prophylaxis.
Roughly half of the patients (n=579) completed an educational program promoting treatment adherence, and the other half (n=583) received the usual information about their disease and the treatment.
The educational program included a patient information booklet explaining AF and anticoagulant treatment for stroke prevention, reminder tools (eg, a key ring and mobile phone alerts), and access to a virtual clinic utilizing staff from existing VKA monitoring clinics.
The researchers assessed differences between the 2 patient groups with regard to treatment adherence (defined as continuous, twice-daily dosing, with an occasional missed dose allowed) and treatment persistence (defined as absence of discontinuation for 30 consecutive days) over a 6-month observational period.
Adherence/persistence was measured using an electronic device that holds a blister pack of medication and records each time the pack is removed.
The researchers found no additional value of the educational program for either outcome.
At 24 weeks, the adherence rate was 88.5% in the control group and 88.3% in the education group (P=0.89). Treatment persistence rates were 90.5% and 91.1%, respectively (P=0.76).
For the second part of this study, the researchers are investigating long-term treatment adherence and the value of an educational program beyond 6 months.
“Future studies may want to test more aggressive and more costly educational programs,” Dr Montalescot noted. “But, in the meantime, the adherence and persistence rates we measured are quite reassuring with the common practice and usual mode of prescription of this medication.” ![]()

Photo courtesy of Pfizer
and Bristol-Myers Squibb
LONDON—An educational program designed to improve adherence to the anticoagulant apixaban proved ineffective in a phase 4 trial of patients with atrial fibrillation (AF).
But that’s because adherence was high whether patients completed the program or not.
This suggests current measures used to inform patients about apixaban may be sufficient to ensure treatment adherence, researchers said.
They presented these findings at the ESC Congress 2015 (abstract 2191).
The research, known as the AEGEAN trial, was sponsored by Bristol-Myers Squibb, the company co-developing apixaban (Eliquis) with Pfizer.
“We used the best possible tools for the educational program, including the usual staff and procedures of the anticoagulation clinics, and all of this was useless,” said study investigator Gilles Montalescot, MD, PhD, of Hospitalier Universitaire Pitié-Salpêtrière in Paris, France.
“However, the trial showed very good adherence to apixaban, leaving little room for improvement with an educational program, suggesting one more advantage of prescribing non-vitamin K antagonists (VKAs) over VKAs in that there is apparently no need for additional education and information.”
Dr Montalescot and his colleagues conducted this study in 1162 AF patients receiving apixaban as stroke prophylaxis.
Roughly half of the patients (n=579) completed an educational program promoting treatment adherence, and the other half (n=583) received the usual information about their disease and the treatment.
The educational program included a patient information booklet explaining AF and anticoagulant treatment for stroke prevention, reminder tools (eg, a key ring and mobile phone alerts), and access to a virtual clinic utilizing staff from existing VKA monitoring clinics.
The researchers assessed differences between the 2 patient groups with regard to treatment adherence (defined as continuous, twice-daily dosing, with an occasional missed dose allowed) and treatment persistence (defined as absence of discontinuation for 30 consecutive days) over a 6-month observational period.
Adherence/persistence was measured using an electronic device that holds a blister pack of medication and records each time the pack is removed.
The researchers found no additional value of the educational program for either outcome.
At 24 weeks, the adherence rate was 88.5% in the control group and 88.3% in the education group (P=0.89). Treatment persistence rates were 90.5% and 91.1%, respectively (P=0.76).
For the second part of this study, the researchers are investigating long-term treatment adherence and the value of an educational program beyond 6 months.
“Future studies may want to test more aggressive and more costly educational programs,” Dr Montalescot noted. “But, in the meantime, the adherence and persistence rates we measured are quite reassuring with the common practice and usual mode of prescription of this medication.” ![]()

Photo courtesy of Pfizer
and Bristol-Myers Squibb
LONDON—An educational program designed to improve adherence to the anticoagulant apixaban proved ineffective in a phase 4 trial of patients with atrial fibrillation (AF).
But that’s because adherence was high whether patients completed the program or not.
This suggests current measures used to inform patients about apixaban may be sufficient to ensure treatment adherence, researchers said.
They presented these findings at the ESC Congress 2015 (abstract 2191).
The research, known as the AEGEAN trial, was sponsored by Bristol-Myers Squibb, the company co-developing apixaban (Eliquis) with Pfizer.
“We used the best possible tools for the educational program, including the usual staff and procedures of the anticoagulation clinics, and all of this was useless,” said study investigator Gilles Montalescot, MD, PhD, of Hospitalier Universitaire Pitié-Salpêtrière in Paris, France.
“However, the trial showed very good adherence to apixaban, leaving little room for improvement with an educational program, suggesting one more advantage of prescribing non-vitamin K antagonists (VKAs) over VKAs in that there is apparently no need for additional education and information.”
Dr Montalescot and his colleagues conducted this study in 1162 AF patients receiving apixaban as stroke prophylaxis.
Roughly half of the patients (n=579) completed an educational program promoting treatment adherence, and the other half (n=583) received the usual information about their disease and the treatment.
The educational program included a patient information booklet explaining AF and anticoagulant treatment for stroke prevention, reminder tools (eg, a key ring and mobile phone alerts), and access to a virtual clinic utilizing staff from existing VKA monitoring clinics.
The researchers assessed differences between the 2 patient groups with regard to treatment adherence (defined as continuous, twice-daily dosing, with an occasional missed dose allowed) and treatment persistence (defined as absence of discontinuation for 30 consecutive days) over a 6-month observational period.
Adherence/persistence was measured using an electronic device that holds a blister pack of medication and records each time the pack is removed.
The researchers found no additional value of the educational program for either outcome.
At 24 weeks, the adherence rate was 88.5% in the control group and 88.3% in the education group (P=0.89). Treatment persistence rates were 90.5% and 91.1%, respectively (P=0.76).
For the second part of this study, the researchers are investigating long-term treatment adherence and the value of an educational program beyond 6 months.
“Future studies may want to test more aggressive and more costly educational programs,” Dr Montalescot noted. “But, in the meantime, the adherence and persistence rates we measured are quite reassuring with the common practice and usual mode of prescription of this medication.” ![]()