User login
Case of the Month: Subungual Myxoma
LAS VEGAS – A 39-year-old male patient presented with a 5-year history of an isolated, nonpainful, nonfluctuant left thumbnail deformity. He had no other skin findings, and no other known medical problems. His thumbnail was distinctly curved, with what appeared to be a slight pinkish growth underneath the nail. The nail was avulsed, revealing a readily visible and protruding tumor from the nail bed, extending from underneath the nail matrix to the level of the distal phalanx, with only a small portion of the nail bed not affected.
Digital myxomas are rare neoplasms, and the subungual location is rarer still, according to Dr. Miriam S. Bettencourt.
There have been just four mentions of subungual myxoma in the medical literature since 1982, all of which were case reports. Surgical excision is usually curative, without the need for repeat surgery. One previous case report described a midlateral approach that spared the nail apparatus and demonstrated remodeling of the nail despite a void left under the nail matrix after excision of the tumor (J. Hand Surg. Am. 1998;23:178-80).
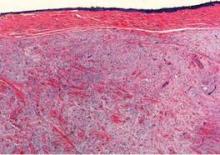
In this case, the patient’s histology revealed a large, circumscribed nonencapsulated nodular deposition of myxoid material, associated with a slight increase in spindle-shaped fibroblasts and thin intervening fibrocollagenous tissue underneath the nail bed epithelium. Scattered mast cells were visible within the lesion.
The tumor was sharply excised and the nail bed was roughly debrided using a small curette. A piece of tinfoil from a suture pack was fashioned into a pseudo nail shape and sutured beneath the patient’s cuticle in order to maintain the opening of the nail matrix during the excision, said Dr. Bettencourt, who presented the case at the Las Vegas Dermatology Seminar, sponsored by Skin Disease Education Foundation (SDEF).
Differential diagnosis included subungual glomus tumor, which causes a bluish-red discoloration of the nail plate and, unlike myxoma, is painful and temperature-sensitive. Onychomatricoma can cause a nail curvature similar to that of myxoma. However, this rare benign tumor of the nail matrix causes a yellowish discoloration and splinter hemorrhages, which are not seen with myxoma.
Fibromas in the digits, including periungual fibroma (a marker of tuberous sclerosis), acquired digital fibrokeratoma, dermatofibroma, and recurrent digital fibrous tumors of childhood may also be considered in the differential diagnosis. So can myxoid cysts, for which there are three presentations in the nail apparatus: one related to the interphalangeal joint, a second having no connection with joints, and a third submatrical type. Patients with myxoid cysts tend to be female and middle-age or older. Squamous cell carcinomas, the most common of subungual malignancies, should also be considered, said Dr. Bettencourt, of the University of Nevada, Las Vegas.
When a subungual myxoma is identified, it is important to investigate the patient for signs of myxoma syndrome, the name of a group of diseases characterized by atrial and cutaneous myxomas, as well as lentigines.
The patient has not presented with any nail deformity or recurrence in the year since surgical recovery, she noted.
"Dermatologists need to and care for patients with nail problems, in place of having the patient be seen solely by a podiatrist, since nail diseases are part of our specialty," Dr. Bettencourt concluded.
She reported having no disclosures. SDEF and this news organization are owned by Elsevier.
LAS VEGAS – A 39-year-old male patient presented with a 5-year history of an isolated, nonpainful, nonfluctuant left thumbnail deformity. He had no other skin findings, and no other known medical problems. His thumbnail was distinctly curved, with what appeared to be a slight pinkish growth underneath the nail. The nail was avulsed, revealing a readily visible and protruding tumor from the nail bed, extending from underneath the nail matrix to the level of the distal phalanx, with only a small portion of the nail bed not affected.
Digital myxomas are rare neoplasms, and the subungual location is rarer still, according to Dr. Miriam S. Bettencourt.
There have been just four mentions of subungual myxoma in the medical literature since 1982, all of which were case reports. Surgical excision is usually curative, without the need for repeat surgery. One previous case report described a midlateral approach that spared the nail apparatus and demonstrated remodeling of the nail despite a void left under the nail matrix after excision of the tumor (J. Hand Surg. Am. 1998;23:178-80).
In this case, the patient’s histology revealed a large, circumscribed nonencapsulated nodular deposition of myxoid material, associated with a slight increase in spindle-shaped fibroblasts and thin intervening fibrocollagenous tissue underneath the nail bed epithelium. Scattered mast cells were visible within the lesion.
The tumor was sharply excised and the nail bed was roughly debrided using a small curette. A piece of tinfoil from a suture pack was fashioned into a pseudo nail shape and sutured beneath the patient’s cuticle in order to maintain the opening of the nail matrix during the excision, said Dr. Bettencourt, who presented the case at the Las Vegas Dermatology Seminar, sponsored by Skin Disease Education Foundation (SDEF).
Differential diagnosis included subungual glomus tumor, which causes a bluish-red discoloration of the nail plate and, unlike myxoma, is painful and temperature-sensitive. Onychomatricoma can cause a nail curvature similar to that of myxoma. However, this rare benign tumor of the nail matrix causes a yellowish discoloration and splinter hemorrhages, which are not seen with myxoma.
Fibromas in the digits, including periungual fibroma (a marker of tuberous sclerosis), acquired digital fibrokeratoma, dermatofibroma, and recurrent digital fibrous tumors of childhood may also be considered in the differential diagnosis. So can myxoid cysts, for which there are three presentations in the nail apparatus: one related to the interphalangeal joint, a second having no connection with joints, and a third submatrical type. Patients with myxoid cysts tend to be female and middle-age or older. Squamous cell carcinomas, the most common of subungual malignancies, should also be considered, said Dr. Bettencourt, of the University of Nevada, Las Vegas.
When a subungual myxoma is identified, it is important to investigate the patient for signs of myxoma syndrome, the name of a group of diseases characterized by atrial and cutaneous myxomas, as well as lentigines.
The patient has not presented with any nail deformity or recurrence in the year since surgical recovery, she noted.
"Dermatologists need to and care for patients with nail problems, in place of having the patient be seen solely by a podiatrist, since nail diseases are part of our specialty," Dr. Bettencourt concluded.
She reported having no disclosures. SDEF and this news organization are owned by Elsevier.
LAS VEGAS – A 39-year-old male patient presented with a 5-year history of an isolated, nonpainful, nonfluctuant left thumbnail deformity. He had no other skin findings, and no other known medical problems. His thumbnail was distinctly curved, with what appeared to be a slight pinkish growth underneath the nail. The nail was avulsed, revealing a readily visible and protruding tumor from the nail bed, extending from underneath the nail matrix to the level of the distal phalanx, with only a small portion of the nail bed not affected.
Digital myxomas are rare neoplasms, and the subungual location is rarer still, according to Dr. Miriam S. Bettencourt.
There have been just four mentions of subungual myxoma in the medical literature since 1982, all of which were case reports. Surgical excision is usually curative, without the need for repeat surgery. One previous case report described a midlateral approach that spared the nail apparatus and demonstrated remodeling of the nail despite a void left under the nail matrix after excision of the tumor (J. Hand Surg. Am. 1998;23:178-80).
In this case, the patient’s histology revealed a large, circumscribed nonencapsulated nodular deposition of myxoid material, associated with a slight increase in spindle-shaped fibroblasts and thin intervening fibrocollagenous tissue underneath the nail bed epithelium. Scattered mast cells were visible within the lesion.
The tumor was sharply excised and the nail bed was roughly debrided using a small curette. A piece of tinfoil from a suture pack was fashioned into a pseudo nail shape and sutured beneath the patient’s cuticle in order to maintain the opening of the nail matrix during the excision, said Dr. Bettencourt, who presented the case at the Las Vegas Dermatology Seminar, sponsored by Skin Disease Education Foundation (SDEF).
Differential diagnosis included subungual glomus tumor, which causes a bluish-red discoloration of the nail plate and, unlike myxoma, is painful and temperature-sensitive. Onychomatricoma can cause a nail curvature similar to that of myxoma. However, this rare benign tumor of the nail matrix causes a yellowish discoloration and splinter hemorrhages, which are not seen with myxoma.
Fibromas in the digits, including periungual fibroma (a marker of tuberous sclerosis), acquired digital fibrokeratoma, dermatofibroma, and recurrent digital fibrous tumors of childhood may also be considered in the differential diagnosis. So can myxoid cysts, for which there are three presentations in the nail apparatus: one related to the interphalangeal joint, a second having no connection with joints, and a third submatrical type. Patients with myxoid cysts tend to be female and middle-age or older. Squamous cell carcinomas, the most common of subungual malignancies, should also be considered, said Dr. Bettencourt, of the University of Nevada, Las Vegas.
When a subungual myxoma is identified, it is important to investigate the patient for signs of myxoma syndrome, the name of a group of diseases characterized by atrial and cutaneous myxomas, as well as lentigines.
The patient has not presented with any nail deformity or recurrence in the year since surgical recovery, she noted.
"Dermatologists need to and care for patients with nail problems, in place of having the patient be seen solely by a podiatrist, since nail diseases are part of our specialty," Dr. Bettencourt concluded.
She reported having no disclosures. SDEF and this news organization are owned by Elsevier.
Evidence Builds for Switching Biologics After Psoriasis Treatment Failure
LAS VEGAS – Emerging data support the practice of switching biologic agents after an initial biologic therapy fails in psoriasis, and even the possibility of rotating back to a biologic that didn’t work previously, according to Dr. Francisco Kerdel, director of the dermatology inpatient service at the University of Miami Hospital.
In one recent series of 747 psoriasis patients on biologics, the 4-year drug response was in the range of 40% for etanercept or adalimumab and 70% for infliximab (Br. J. Dermatol. 2011;164:1091-6). "Thus, there is a logical need for ‘switching’ [biologic] therapy," he noted at the SDEF Las Vegas Dermatology Seminar.
The reasons for treatment failure are not known. Antibody production has been suspected of playing a role, but the presence of antibodies seldom correlates with clinical response, he said.
In a 16-week, open-label trial, a Physician Global Assessment (PGA) rating of "clear" or "minimal" was achieved in 52% of 152 patients who had chronic plaque psoriasis and were switched to adalimumab following suboptimal responses to etanercept, methotrexate, or phototherapy (J. Am. Acad. Dermatol. 2011;64:671-81).
In the PSUNRISE study (a prospective, multicenter, open-label study of infliximab treatment in 215 patients with plaque psoriasis who had had a prior inadequate response to etanercept), a PGA score of 0 (clear) or 1 was achieved by week 10 in 65% of the 179 completers, and 60% remained at PGA 0-1 in weeks 14-26. These data have been submitted for publication, according to Dr. Kerdel, who was one of the study authors.
Good to excellent responses were achieved with ustekinumab at doses of either 45 mg or 90 mg, depending on body weight, in 9 of 11 psoriasis patients who had experienced treatment failures on multiple biologics, including infliximab (11 patients), etanercept (10), efalizumab (9), adalimumab (7), and golimumab (3) (Int. J. Dermatol. 2011;50:478-82).
There is even some evidence that patients can return with success to a biologic therapy that they had previously failed.
Dr. Kerdel and his associates have conducted an open-label study of etanercept re-treatment in 20 patients with moderate to severe psoriasis (defined as a PGA score of 3 or greater) who had had prior therapy with etanercept for a minimum of 6 months but had discontinued it because of loss of efficacy. The 10 men and 10 women had an average age of 49 years, with an average of 3.5 years between stopping and restarting etanercept. Five patients withdrew and were classified as treatment failures, regardless of the reason for withdrawal.
The proportion of responders (defined as those achieving a PGA score of 0 or 1) was 5 of 20 (25%) at week 8, and 8 of 20 (40%) at week 12. Body weight appeared to play a role. Among the 14 patients who had a PGA score of 2 or less at week 12, the average weight was 198.4 pounds, compared with 217.6 pounds for the 6 who did not have that response.
These preliminary findings suggest that rotational therapy is possible, at least in cases of secondary failure with etanercept. Rotational therapy may be possible with other biologics as well, but further studies are necessary, Dr. Kerdel concluded.
It had been thought that this practice would be of limited value because of the development of circulating antibodies, which were found in one study to range in prevalence from 5% of rheumatoid arthritis patients on ustekinumab to 87% of those treated with adalimumab (Clin. Rev. Allergy Immunol. 2010;38:82-9). However, the therapeutic relevance of non-neutralizing vs. neutralizing antibodies is currently unknown, he said.
In a recent prospective cohort study of 272 RA patients treated with adalimumab, 28% had developed antiadalimumab antibodies, which appeared within the first 28 weeks of treatment in two-thirds of them. Over 3 years of follow-up, 38% of the patients with antibodies discontinued adalimumab therapy because of treatment failure, compared with 14% of those who did not develop antibodies. Minimal disease activity was achieved in 48% without antibodies, compared with 13% who had antibodies (JAMA 2011;305:1460-8).
And in a retrospective observational study of 97 psoriasis patients who had been treated with anti–tumor necrosis factor–alpha therapy (60 on a first agent, 22 having failed one agent, 9 having failed two agents, and 6 having failed all three agents), antinuclear antibodies developed in 17%, 54%, 78% and 83%, respectively (Br. J. Dermatol. 2010;162:780-5). "So, antibodies do seem to play a role" in treatment failure, Dr. Kerdel commented.
Dr. Kerdel disclosed that he has been involved in clinical studies, has participated in advisory boards, and is a speaker for Amgen, Abbott, Janssen, Genentech, Astellas, Stiefel, Pfizer, Merck, Novartis, Eisai, and Celgene. SDEF and this news organization are owned by Elsevier.
LAS VEGAS – Emerging data support the practice of switching biologic agents after an initial biologic therapy fails in psoriasis, and even the possibility of rotating back to a biologic that didn’t work previously, according to Dr. Francisco Kerdel, director of the dermatology inpatient service at the University of Miami Hospital.
In one recent series of 747 psoriasis patients on biologics, the 4-year drug response was in the range of 40% for etanercept or adalimumab and 70% for infliximab (Br. J. Dermatol. 2011;164:1091-6). "Thus, there is a logical need for ‘switching’ [biologic] therapy," he noted at the SDEF Las Vegas Dermatology Seminar.
The reasons for treatment failure are not known. Antibody production has been suspected of playing a role, but the presence of antibodies seldom correlates with clinical response, he said.
In a 16-week, open-label trial, a Physician Global Assessment (PGA) rating of "clear" or "minimal" was achieved in 52% of 152 patients who had chronic plaque psoriasis and were switched to adalimumab following suboptimal responses to etanercept, methotrexate, or phototherapy (J. Am. Acad. Dermatol. 2011;64:671-81).
In the PSUNRISE study (a prospective, multicenter, open-label study of infliximab treatment in 215 patients with plaque psoriasis who had had a prior inadequate response to etanercept), a PGA score of 0 (clear) or 1 was achieved by week 10 in 65% of the 179 completers, and 60% remained at PGA 0-1 in weeks 14-26. These data have been submitted for publication, according to Dr. Kerdel, who was one of the study authors.
Good to excellent responses were achieved with ustekinumab at doses of either 45 mg or 90 mg, depending on body weight, in 9 of 11 psoriasis patients who had experienced treatment failures on multiple biologics, including infliximab (11 patients), etanercept (10), efalizumab (9), adalimumab (7), and golimumab (3) (Int. J. Dermatol. 2011;50:478-82).
There is even some evidence that patients can return with success to a biologic therapy that they had previously failed.
Dr. Kerdel and his associates have conducted an open-label study of etanercept re-treatment in 20 patients with moderate to severe psoriasis (defined as a PGA score of 3 or greater) who had had prior therapy with etanercept for a minimum of 6 months but had discontinued it because of loss of efficacy. The 10 men and 10 women had an average age of 49 years, with an average of 3.5 years between stopping and restarting etanercept. Five patients withdrew and were classified as treatment failures, regardless of the reason for withdrawal.
The proportion of responders (defined as those achieving a PGA score of 0 or 1) was 5 of 20 (25%) at week 8, and 8 of 20 (40%) at week 12. Body weight appeared to play a role. Among the 14 patients who had a PGA score of 2 or less at week 12, the average weight was 198.4 pounds, compared with 217.6 pounds for the 6 who did not have that response.
These preliminary findings suggest that rotational therapy is possible, at least in cases of secondary failure with etanercept. Rotational therapy may be possible with other biologics as well, but further studies are necessary, Dr. Kerdel concluded.
It had been thought that this practice would be of limited value because of the development of circulating antibodies, which were found in one study to range in prevalence from 5% of rheumatoid arthritis patients on ustekinumab to 87% of those treated with adalimumab (Clin. Rev. Allergy Immunol. 2010;38:82-9). However, the therapeutic relevance of non-neutralizing vs. neutralizing antibodies is currently unknown, he said.
In a recent prospective cohort study of 272 RA patients treated with adalimumab, 28% had developed antiadalimumab antibodies, which appeared within the first 28 weeks of treatment in two-thirds of them. Over 3 years of follow-up, 38% of the patients with antibodies discontinued adalimumab therapy because of treatment failure, compared with 14% of those who did not develop antibodies. Minimal disease activity was achieved in 48% without antibodies, compared with 13% who had antibodies (JAMA 2011;305:1460-8).
And in a retrospective observational study of 97 psoriasis patients who had been treated with anti–tumor necrosis factor–alpha therapy (60 on a first agent, 22 having failed one agent, 9 having failed two agents, and 6 having failed all three agents), antinuclear antibodies developed in 17%, 54%, 78% and 83%, respectively (Br. J. Dermatol. 2010;162:780-5). "So, antibodies do seem to play a role" in treatment failure, Dr. Kerdel commented.
Dr. Kerdel disclosed that he has been involved in clinical studies, has participated in advisory boards, and is a speaker for Amgen, Abbott, Janssen, Genentech, Astellas, Stiefel, Pfizer, Merck, Novartis, Eisai, and Celgene. SDEF and this news organization are owned by Elsevier.
LAS VEGAS – Emerging data support the practice of switching biologic agents after an initial biologic therapy fails in psoriasis, and even the possibility of rotating back to a biologic that didn’t work previously, according to Dr. Francisco Kerdel, director of the dermatology inpatient service at the University of Miami Hospital.
In one recent series of 747 psoriasis patients on biologics, the 4-year drug response was in the range of 40% for etanercept or adalimumab and 70% for infliximab (Br. J. Dermatol. 2011;164:1091-6). "Thus, there is a logical need for ‘switching’ [biologic] therapy," he noted at the SDEF Las Vegas Dermatology Seminar.
The reasons for treatment failure are not known. Antibody production has been suspected of playing a role, but the presence of antibodies seldom correlates with clinical response, he said.
In a 16-week, open-label trial, a Physician Global Assessment (PGA) rating of "clear" or "minimal" was achieved in 52% of 152 patients who had chronic plaque psoriasis and were switched to adalimumab following suboptimal responses to etanercept, methotrexate, or phototherapy (J. Am. Acad. Dermatol. 2011;64:671-81).
In the PSUNRISE study (a prospective, multicenter, open-label study of infliximab treatment in 215 patients with plaque psoriasis who had had a prior inadequate response to etanercept), a PGA score of 0 (clear) or 1 was achieved by week 10 in 65% of the 179 completers, and 60% remained at PGA 0-1 in weeks 14-26. These data have been submitted for publication, according to Dr. Kerdel, who was one of the study authors.
Good to excellent responses were achieved with ustekinumab at doses of either 45 mg or 90 mg, depending on body weight, in 9 of 11 psoriasis patients who had experienced treatment failures on multiple biologics, including infliximab (11 patients), etanercept (10), efalizumab (9), adalimumab (7), and golimumab (3) (Int. J. Dermatol. 2011;50:478-82).
There is even some evidence that patients can return with success to a biologic therapy that they had previously failed.
Dr. Kerdel and his associates have conducted an open-label study of etanercept re-treatment in 20 patients with moderate to severe psoriasis (defined as a PGA score of 3 or greater) who had had prior therapy with etanercept for a minimum of 6 months but had discontinued it because of loss of efficacy. The 10 men and 10 women had an average age of 49 years, with an average of 3.5 years between stopping and restarting etanercept. Five patients withdrew and were classified as treatment failures, regardless of the reason for withdrawal.
The proportion of responders (defined as those achieving a PGA score of 0 or 1) was 5 of 20 (25%) at week 8, and 8 of 20 (40%) at week 12. Body weight appeared to play a role. Among the 14 patients who had a PGA score of 2 or less at week 12, the average weight was 198.4 pounds, compared with 217.6 pounds for the 6 who did not have that response.
These preliminary findings suggest that rotational therapy is possible, at least in cases of secondary failure with etanercept. Rotational therapy may be possible with other biologics as well, but further studies are necessary, Dr. Kerdel concluded.
It had been thought that this practice would be of limited value because of the development of circulating antibodies, which were found in one study to range in prevalence from 5% of rheumatoid arthritis patients on ustekinumab to 87% of those treated with adalimumab (Clin. Rev. Allergy Immunol. 2010;38:82-9). However, the therapeutic relevance of non-neutralizing vs. neutralizing antibodies is currently unknown, he said.
In a recent prospective cohort study of 272 RA patients treated with adalimumab, 28% had developed antiadalimumab antibodies, which appeared within the first 28 weeks of treatment in two-thirds of them. Over 3 years of follow-up, 38% of the patients with antibodies discontinued adalimumab therapy because of treatment failure, compared with 14% of those who did not develop antibodies. Minimal disease activity was achieved in 48% without antibodies, compared with 13% who had antibodies (JAMA 2011;305:1460-8).
And in a retrospective observational study of 97 psoriasis patients who had been treated with anti–tumor necrosis factor–alpha therapy (60 on a first agent, 22 having failed one agent, 9 having failed two agents, and 6 having failed all three agents), antinuclear antibodies developed in 17%, 54%, 78% and 83%, respectively (Br. J. Dermatol. 2010;162:780-5). "So, antibodies do seem to play a role" in treatment failure, Dr. Kerdel commented.
Dr. Kerdel disclosed that he has been involved in clinical studies, has participated in advisory boards, and is a speaker for Amgen, Abbott, Janssen, Genentech, Astellas, Stiefel, Pfizer, Merck, Novartis, Eisai, and Celgene. SDEF and this news organization are owned by Elsevier.
EXPERT ANALYSIS FROM THE SDEF LAS VEGAS DERMATOLOGY SEMINAR
Most Lymphomatoid Papulosis Has Benign Course
LAS VEGAS – Although certain characteristics of lymphomatoid papulosis appear be associated with progression to lymphoma, the majority of patients will have a benign course of disease.
The recurrent papulonodular skin eruption lymphomatoid papulosis (LyP) can be a confusing dermatologic entity because it appears malignant histologically, but it usually follows a clinically benign and indolent course (Arch. Dermatol. 1968;97:23-30). And even the 10%-20% of patients who do progress to lymphoma tend to have less aggressive disease, said Dr. Lawrence E. Gibson, professor of dermatology at the Mayo Clinic in Rochester, Minn. The reasons for this disconnect are not yet known.
"Patients with LyP look like lymphoma under the microscope but have clinically indolent cutaneous disease. ... It is an example of a very important clinical-pathological relationship that really needs to be made to help us understand how to treat patients better," he said.
"The bottom line is most of our patients who have LyP do not go on to have aggressive lymphomas."
To identify which LyP patients are more likely to progress to lymphoma, Dr. Gibson, Dr. Rokea A. el-Azhary, Dr. Aieska de Souza, and their associates conducted a retrospective analysis of 123 patients seen at the Mayo Clinic between 1991 and 2008. The patients were followed for a mean of 4 years (range, 2 months to 14 years). The 65 males and 58 females had a mean age of 47 years (range, 1-83 years), and a mean of 14 lesions (range, 1-100). Most (88%) of the lesions were papules, with a reported mean duration of 5.5 weeks. Pruritis was present in 38% and scar formation in 58%, the researchers reported (J. Am. Acad. Dermatol. 2011 [doi:10.1016/j.jaad.2011.07.012]).
Hematologic malignancies were present in 17 patients (14%). Of those, 10 were cutaneous lymphomas – 8 mycosis fungoides (MF) and 2 anaplastic large-cell lymphomas (ALCL). Hodgkin lymphoma was present in three patients (including the two with ALCL), multiple myeloma or monoclonal gammopathy in three, and myelodysplastic syndrome in one.
"The bottom line is most of our patients who have LyP do not go on to have aggressive lymphomas. They certainly don’t have cytotoxic lymphomas. And if they have lymphoma, they usually have MF. I think that’s somewhat reassuring to us. And for the most part, most of the patients don’t have anything. They have a normal life," Dr. Gibson said at the seminar sponsored by Skin Disease Education Foundation (SDEF).
Of 97 LyP patients for whom original biopsy slides were available, the majority (69) had World Health Organization/European Organization for Research and Treatment of Cancer histologic classification type A, including 35 with immunophenotypic subtype CD8 and 34 with subtype CD4. Another 13 patients had type B lesions (8 CD4, 5 CD8), and 6 had type C, all of which were CD4. The other 9 patients had more than one histologic type (A, B, or C), and/or more than one immunophenotypic subtype (CD4 or CD8). They were designated mixed type.
Clinically, there were no distinguishing features among the subtypes. This finding contrasts with some previous reports that the CD8 subtype might predispose to worse disease outcome (Am. J. Pathol. 1999;155:483-92).
"Our findings indicated that the LyP subtype CD8 does not signify more aggressive disease, a poor prognosis, or an association with malignancy," Dr. Gibson and his colleagues wrote.
Hematologic malignancies were present in 5 of the 9 mixed-type patients (55.5%), compared with 4 of the 34 with A/CD4 (12%), 4 of the 35 A/CD8 (11.5%), 1 of the 8 B/CD4 patients (12.5%), and 1 of the 5 B/CD8 patients (20%). (Two of the 17 malignancies were excluded from analysis because original slides were not available.) The odds ratio for malignancy for the patients with mixed-type LyP versus all other types was a statistically significant 4.33 (P = .03).
In a molecular genetics substudy of 84 LyP lesions from 76 patients, 42 (50%) were positive for clonal T-cell receptor gene rearrangement (TCRGR), 34 (40%) were negative, and 8 (10%) showed equivocal results or had insufficient DNA for analysis. Among the LyP patients who had a hematologic malignancy, 9 of 11 (82%) had positive TCRGR, compared with 30 of 68 (44%) LyP patients without malignancy. That association was also significant, with an odds ratio of 5.7 (P = .02), noted the investigators.
"A positive T-cell receptor gene rearrangement or having more than one type of LyP may have a higher risk of progression to lymphoma, but the evidence is not hard and fast. ... The take-home message is most of these patients do just fine," Dr. Gibson said.
Dr. Gibson stated that he had no relevant financial disclosures or conflicts of interest. SDEF and this news organization are owned by Elsevier.
LAS VEGAS – Although certain characteristics of lymphomatoid papulosis appear be associated with progression to lymphoma, the majority of patients will have a benign course of disease.
The recurrent papulonodular skin eruption lymphomatoid papulosis (LyP) can be a confusing dermatologic entity because it appears malignant histologically, but it usually follows a clinically benign and indolent course (Arch. Dermatol. 1968;97:23-30). And even the 10%-20% of patients who do progress to lymphoma tend to have less aggressive disease, said Dr. Lawrence E. Gibson, professor of dermatology at the Mayo Clinic in Rochester, Minn. The reasons for this disconnect are not yet known.
"Patients with LyP look like lymphoma under the microscope but have clinically indolent cutaneous disease. ... It is an example of a very important clinical-pathological relationship that really needs to be made to help us understand how to treat patients better," he said.
"The bottom line is most of our patients who have LyP do not go on to have aggressive lymphomas."
To identify which LyP patients are more likely to progress to lymphoma, Dr. Gibson, Dr. Rokea A. el-Azhary, Dr. Aieska de Souza, and their associates conducted a retrospective analysis of 123 patients seen at the Mayo Clinic between 1991 and 2008. The patients were followed for a mean of 4 years (range, 2 months to 14 years). The 65 males and 58 females had a mean age of 47 years (range, 1-83 years), and a mean of 14 lesions (range, 1-100). Most (88%) of the lesions were papules, with a reported mean duration of 5.5 weeks. Pruritis was present in 38% and scar formation in 58%, the researchers reported (J. Am. Acad. Dermatol. 2011 [doi:10.1016/j.jaad.2011.07.012]).
Hematologic malignancies were present in 17 patients (14%). Of those, 10 were cutaneous lymphomas – 8 mycosis fungoides (MF) and 2 anaplastic large-cell lymphomas (ALCL). Hodgkin lymphoma was present in three patients (including the two with ALCL), multiple myeloma or monoclonal gammopathy in three, and myelodysplastic syndrome in one.
"The bottom line is most of our patients who have LyP do not go on to have aggressive lymphomas. They certainly don’t have cytotoxic lymphomas. And if they have lymphoma, they usually have MF. I think that’s somewhat reassuring to us. And for the most part, most of the patients don’t have anything. They have a normal life," Dr. Gibson said at the seminar sponsored by Skin Disease Education Foundation (SDEF).
Of 97 LyP patients for whom original biopsy slides were available, the majority (69) had World Health Organization/European Organization for Research and Treatment of Cancer histologic classification type A, including 35 with immunophenotypic subtype CD8 and 34 with subtype CD4. Another 13 patients had type B lesions (8 CD4, 5 CD8), and 6 had type C, all of which were CD4. The other 9 patients had more than one histologic type (A, B, or C), and/or more than one immunophenotypic subtype (CD4 or CD8). They were designated mixed type.
Clinically, there were no distinguishing features among the subtypes. This finding contrasts with some previous reports that the CD8 subtype might predispose to worse disease outcome (Am. J. Pathol. 1999;155:483-92).
"Our findings indicated that the LyP subtype CD8 does not signify more aggressive disease, a poor prognosis, or an association with malignancy," Dr. Gibson and his colleagues wrote.
Hematologic malignancies were present in 5 of the 9 mixed-type patients (55.5%), compared with 4 of the 34 with A/CD4 (12%), 4 of the 35 A/CD8 (11.5%), 1 of the 8 B/CD4 patients (12.5%), and 1 of the 5 B/CD8 patients (20%). (Two of the 17 malignancies were excluded from analysis because original slides were not available.) The odds ratio for malignancy for the patients with mixed-type LyP versus all other types was a statistically significant 4.33 (P = .03).
In a molecular genetics substudy of 84 LyP lesions from 76 patients, 42 (50%) were positive for clonal T-cell receptor gene rearrangement (TCRGR), 34 (40%) were negative, and 8 (10%) showed equivocal results or had insufficient DNA for analysis. Among the LyP patients who had a hematologic malignancy, 9 of 11 (82%) had positive TCRGR, compared with 30 of 68 (44%) LyP patients without malignancy. That association was also significant, with an odds ratio of 5.7 (P = .02), noted the investigators.
"A positive T-cell receptor gene rearrangement or having more than one type of LyP may have a higher risk of progression to lymphoma, but the evidence is not hard and fast. ... The take-home message is most of these patients do just fine," Dr. Gibson said.
Dr. Gibson stated that he had no relevant financial disclosures or conflicts of interest. SDEF and this news organization are owned by Elsevier.
LAS VEGAS – Although certain characteristics of lymphomatoid papulosis appear be associated with progression to lymphoma, the majority of patients will have a benign course of disease.
The recurrent papulonodular skin eruption lymphomatoid papulosis (LyP) can be a confusing dermatologic entity because it appears malignant histologically, but it usually follows a clinically benign and indolent course (Arch. Dermatol. 1968;97:23-30). And even the 10%-20% of patients who do progress to lymphoma tend to have less aggressive disease, said Dr. Lawrence E. Gibson, professor of dermatology at the Mayo Clinic in Rochester, Minn. The reasons for this disconnect are not yet known.
"Patients with LyP look like lymphoma under the microscope but have clinically indolent cutaneous disease. ... It is an example of a very important clinical-pathological relationship that really needs to be made to help us understand how to treat patients better," he said.
"The bottom line is most of our patients who have LyP do not go on to have aggressive lymphomas."
To identify which LyP patients are more likely to progress to lymphoma, Dr. Gibson, Dr. Rokea A. el-Azhary, Dr. Aieska de Souza, and their associates conducted a retrospective analysis of 123 patients seen at the Mayo Clinic between 1991 and 2008. The patients were followed for a mean of 4 years (range, 2 months to 14 years). The 65 males and 58 females had a mean age of 47 years (range, 1-83 years), and a mean of 14 lesions (range, 1-100). Most (88%) of the lesions were papules, with a reported mean duration of 5.5 weeks. Pruritis was present in 38% and scar formation in 58%, the researchers reported (J. Am. Acad. Dermatol. 2011 [doi:10.1016/j.jaad.2011.07.012]).
Hematologic malignancies were present in 17 patients (14%). Of those, 10 were cutaneous lymphomas – 8 mycosis fungoides (MF) and 2 anaplastic large-cell lymphomas (ALCL). Hodgkin lymphoma was present in three patients (including the two with ALCL), multiple myeloma or monoclonal gammopathy in three, and myelodysplastic syndrome in one.
"The bottom line is most of our patients who have LyP do not go on to have aggressive lymphomas. They certainly don’t have cytotoxic lymphomas. And if they have lymphoma, they usually have MF. I think that’s somewhat reassuring to us. And for the most part, most of the patients don’t have anything. They have a normal life," Dr. Gibson said at the seminar sponsored by Skin Disease Education Foundation (SDEF).
Of 97 LyP patients for whom original biopsy slides were available, the majority (69) had World Health Organization/European Organization for Research and Treatment of Cancer histologic classification type A, including 35 with immunophenotypic subtype CD8 and 34 with subtype CD4. Another 13 patients had type B lesions (8 CD4, 5 CD8), and 6 had type C, all of which were CD4. The other 9 patients had more than one histologic type (A, B, or C), and/or more than one immunophenotypic subtype (CD4 or CD8). They were designated mixed type.
Clinically, there were no distinguishing features among the subtypes. This finding contrasts with some previous reports that the CD8 subtype might predispose to worse disease outcome (Am. J. Pathol. 1999;155:483-92).
"Our findings indicated that the LyP subtype CD8 does not signify more aggressive disease, a poor prognosis, or an association with malignancy," Dr. Gibson and his colleagues wrote.
Hematologic malignancies were present in 5 of the 9 mixed-type patients (55.5%), compared with 4 of the 34 with A/CD4 (12%), 4 of the 35 A/CD8 (11.5%), 1 of the 8 B/CD4 patients (12.5%), and 1 of the 5 B/CD8 patients (20%). (Two of the 17 malignancies were excluded from analysis because original slides were not available.) The odds ratio for malignancy for the patients with mixed-type LyP versus all other types was a statistically significant 4.33 (P = .03).
In a molecular genetics substudy of 84 LyP lesions from 76 patients, 42 (50%) were positive for clonal T-cell receptor gene rearrangement (TCRGR), 34 (40%) were negative, and 8 (10%) showed equivocal results or had insufficient DNA for analysis. Among the LyP patients who had a hematologic malignancy, 9 of 11 (82%) had positive TCRGR, compared with 30 of 68 (44%) LyP patients without malignancy. That association was also significant, with an odds ratio of 5.7 (P = .02), noted the investigators.
"A positive T-cell receptor gene rearrangement or having more than one type of LyP may have a higher risk of progression to lymphoma, but the evidence is not hard and fast. ... The take-home message is most of these patients do just fine," Dr. Gibson said.
Dr. Gibson stated that he had no relevant financial disclosures or conflicts of interest. SDEF and this news organization are owned by Elsevier.
FROM THE SDEF LAS VEGAS DERMATOLOGY SEMINAR
Major Finding: Hematologic malignancies were present in 17 patients (14%).
Data Source: Retrospective analysis of 123 LyP patients seen at the Mayo Clinic between 1991 and 2008.
Disclosures: Dr. Gibson has no relevant financial disclosures or conflicts of interest. SDEF and this news organization are owned by Elsevier.
Safety Assurance Awaits Further Data for New Psoriasis Drugs
LAS VEGAS – New agents for treating psoriasis have shown great promise in terms of efficacy, but assurances of safety await further data from larger studies.
Thus far, phase II data show impressive efficacy and no worrisome safety signals for the anti-interleukin-17 agents AMG 827 and secukinumab and the small molecules apremilast and tofacitinib. However, the studies have been too small and of insufficient duration to definitively rule out cardiovascular, infectious, and cancer risks, said Dr. Kenneth B. Gordon at the Las Vegas Dermatology Seminar, sponsored by Skin Disease Education Foundation (SDEF).
"It is my hope that these drugs are going to be fantastic. We just have to maintain a level of concern and vigilance for both biologics and small molecules ... We just desperately need large trials," said Dr. Gordon, head of the division of dermatology at NorthShore University HealthSystem, Chicago.
The discovery of IL-17 as a key player in psoriatic plaque formation has led to a new understanding of psoriasis pathophysiology and has become a new target for drug development. However, experience with one agent that blocks IL-12/23 – which induces activated IL-17 – gives pause.
Briakinumab, an extremely effective anti-psoriatic agent that blocks IL 12/23, was withdrawn from development after phase III studies showed a signal – albeit statistically insignificant – for serious infections including cellulitis and pneumonia, MACE events (cardiac arrest, myocardial infarction, and stroke), and malignancies (nonmelanoma skin cancer and squamous cell carcinoma of the lung and nasopharynx).
The absolute MACE event numbers were small, but were counter to what would be expected from a systemic anti-inflammatory agent, which should reduce cardiovascular disease, Dr. Craig L. Leonardi, a clinical professor of dermatology at St. Louis University, said in a separate presentation.
According to Dr. Gordon, "It’s really an exciting time for new psoriatic therapies based on a better understanding of psoriasis pathophysiology. However, we are less excited about phase II data because of what happened to briakinumab in phase III."
It will be essential to determine the etiology of the adverse effects, he said. "If the effects are not related to how well the agent controls psoriasis but to mechanisms like IL-12 blockade that may not have relevance to IL-17, they may not show up [with the new agents in development]. That’s what the phase II studies suggest, but it’s too early to really make a final statement," Dr. Gordon said in an interview.
Phase II data on the anti-IL17 and small molecules were presented earlier this year at the European Academy of Dermatology and Venereology meeting in Lisbon and at the World Congress of Dermatology in Seoul. Among the findings:
• AMG 827: This fully-human monoclonal antibody binds to and blocks the IL-17 receptor. In a phase II, double-blind, randomized, placebo-controlled trial of 198 patients who were randomized to subcutaneous AMG 827 at 280 mg monthly; to 70, 140, or 210 mg every 2 weeks; or to placebo. The primary end point, PASI 75 response rate at week 12, was highest (83%) in patients who received 210 mg every 2 weeks. Moreover, at that dose, the proportion achieving a PASI 100 score, indicating no psoriasis activity, was 63%.
"This is an extraordinarily high-responding drug, similar only to briakinumab," Dr. Gordon commented.
Changes in neutrophil counts were seen, as to be expected from IL-17 and IL-12 blockade. "Some of the changes were significant. We need to keep an eye on this," he said.
• Secukinumab: This novel, fully human antibody to IL-17A was investigated in three separate phase II trials of patients with moderate to severe plaque psoriasis. An intravenous induction dose-ranging study of 100 patients yielded PASI 75 response rates at 12 weeks of 40%-83%. A subcutaneous dose-ranging study of 125 patients produced PASI 75 response rates of 19%-81%, and a subcutaneous regimen-finding trial involving 404 patients determined that a regimen of 150 mg at weeks 0, 1, 2, and 4 produced the best PASI 75 response at week 12, of 55%.
While the safety analysis showed no significant differences from placebo, there were two cases of cardiac disorders – one angina pectoris and one coronary artery disease – in the intravenous dose-ranging study and two cases listed as "cardiac disorders" in the regimen-finding study. "We don’t know if these are significant. We have to look at phase III trials," Dr. Gordon said.
• Apremilast: This small molecule, taken orally, works by inhibiting type 4 phosphodiesterase. In a randomized, placebo-controlled phase II trial of 352 patients with moderate to severe plaque psoriasis, the PASI 75 response rate at 16 weeks was 41% with a 30-mg twice-daily dose.
Adverse effects were dose-dependent. Adverse events that occurred in 5% or more of patients included headache, nausea, diarrhea, and upper respiratory tract infections. These typically occurred early in the course of treatment.
Serious adverse events included one myocardial infarction and one case of prostate cancer in the 30-mg BID group. But there was also a prostate cancer and a sudden death among the placebo recipients. "We really don’t have enough patients to look at adverse effects," Dr. Gordon said.
• Tofacitinib: This oral Janus kinase inhibitor demonstrated dose-dependent efficacy, with 67% of patients randomized at 15 mg twice a day achieving PASI 75 and "clear" or "almost clear." The phase II, 12-week, double-blind, placebo-controlled trial enrolled 197 patients with moderate to severe plaque psoriasis.
Concomitant overall decreases in hemoglobin and neutrophil counts from baseline were also dose-dependent. The finding did not specify the proportion of patients who had the decreases or the individual degree of change. "If everyone had a small change, it’s not going to bother me too much. But, if 10% of patients had a big change, it’s a really important finding. Those are the questions we need to ask," Dr. Gordon said.
Dr. Gordon said that so far the phase II safety data for the agents are encouraging, but enthusiasm should still be tempered. "When multiple drugs with the same mechanism have [similar] results, you start to feel more confident. But still, we need to see larger studies."
"It’s really an exciting time for new psoriatic therapies based on a better understanding of psoriasis pathophysiology."
Dr. Leonardi’s presentation focused on anti-IL 12/23 inhibitor treatment; he noted that the recently-approved monoclonal antibody ustekinumab binds to the same shared p40 subunit of IL-12 and IL-23 as briakinumab, the agent that was withdrawn from development in phase III. "There are more similarities than differences" between the two agents, he commented.
He and his colleagues recently conducted a meta-analysis of 22 randomized controlled clinical trials of biologic therapies comprising 10,183 patients with chronic plaque psoriasis, in which 10 of 3,179 patients receiving either ustekinumab or briakinumab experienced a MACE, compared with 0 events in 1,474 patients receiving placebo, for a MACE rate of 1.33 per 100 patient-years.
In contrast, no difference was seen among patients in the anti-TNF-alpha trials, with only 1 of 3,858 patients receiving anti-TNF-alpha agents experiencing a MACE, compared with 1 of 1,812 patients receiving placebo (JAMA 2011;306:864-71).
Although the difference for the anti-IL 12/23 agents was not statistically significant, the data set was not large enough to detect rare events. "This is a class effect in my mind," Dr. Leonardi said, adding that he uses ustekinumab as a second-line agent, after the TNF antagonists.
"It’s important to remember that all new drugs are ‘new’ ... We will learn more and more about these drugs as time goes on," he said.
Dr. Gordon disclosed that he has received research support or honoraria as a consultant from Abbott, Amgen, Centocor, Eli Lilly, Merck, Novartis, and Pfizer. Dr. Leonardi disclosed that he has had financial relationships with 23 companies that are involved in psoriasis treatment development, including Abbott and Centocor.
SDEF and this news organization are owned by Elsevier.
LAS VEGAS – New agents for treating psoriasis have shown great promise in terms of efficacy, but assurances of safety await further data from larger studies.
Thus far, phase II data show impressive efficacy and no worrisome safety signals for the anti-interleukin-17 agents AMG 827 and secukinumab and the small molecules apremilast and tofacitinib. However, the studies have been too small and of insufficient duration to definitively rule out cardiovascular, infectious, and cancer risks, said Dr. Kenneth B. Gordon at the Las Vegas Dermatology Seminar, sponsored by Skin Disease Education Foundation (SDEF).
"It is my hope that these drugs are going to be fantastic. We just have to maintain a level of concern and vigilance for both biologics and small molecules ... We just desperately need large trials," said Dr. Gordon, head of the division of dermatology at NorthShore University HealthSystem, Chicago.
The discovery of IL-17 as a key player in psoriatic plaque formation has led to a new understanding of psoriasis pathophysiology and has become a new target for drug development. However, experience with one agent that blocks IL-12/23 – which induces activated IL-17 – gives pause.
Briakinumab, an extremely effective anti-psoriatic agent that blocks IL 12/23, was withdrawn from development after phase III studies showed a signal – albeit statistically insignificant – for serious infections including cellulitis and pneumonia, MACE events (cardiac arrest, myocardial infarction, and stroke), and malignancies (nonmelanoma skin cancer and squamous cell carcinoma of the lung and nasopharynx).
The absolute MACE event numbers were small, but were counter to what would be expected from a systemic anti-inflammatory agent, which should reduce cardiovascular disease, Dr. Craig L. Leonardi, a clinical professor of dermatology at St. Louis University, said in a separate presentation.
According to Dr. Gordon, "It’s really an exciting time for new psoriatic therapies based on a better understanding of psoriasis pathophysiology. However, we are less excited about phase II data because of what happened to briakinumab in phase III."
It will be essential to determine the etiology of the adverse effects, he said. "If the effects are not related to how well the agent controls psoriasis but to mechanisms like IL-12 blockade that may not have relevance to IL-17, they may not show up [with the new agents in development]. That’s what the phase II studies suggest, but it’s too early to really make a final statement," Dr. Gordon said in an interview.
Phase II data on the anti-IL17 and small molecules were presented earlier this year at the European Academy of Dermatology and Venereology meeting in Lisbon and at the World Congress of Dermatology in Seoul. Among the findings:
• AMG 827: This fully-human monoclonal antibody binds to and blocks the IL-17 receptor. In a phase II, double-blind, randomized, placebo-controlled trial of 198 patients who were randomized to subcutaneous AMG 827 at 280 mg monthly; to 70, 140, or 210 mg every 2 weeks; or to placebo. The primary end point, PASI 75 response rate at week 12, was highest (83%) in patients who received 210 mg every 2 weeks. Moreover, at that dose, the proportion achieving a PASI 100 score, indicating no psoriasis activity, was 63%.
"This is an extraordinarily high-responding drug, similar only to briakinumab," Dr. Gordon commented.
Changes in neutrophil counts were seen, as to be expected from IL-17 and IL-12 blockade. "Some of the changes were significant. We need to keep an eye on this," he said.
• Secukinumab: This novel, fully human antibody to IL-17A was investigated in three separate phase II trials of patients with moderate to severe plaque psoriasis. An intravenous induction dose-ranging study of 100 patients yielded PASI 75 response rates at 12 weeks of 40%-83%. A subcutaneous dose-ranging study of 125 patients produced PASI 75 response rates of 19%-81%, and a subcutaneous regimen-finding trial involving 404 patients determined that a regimen of 150 mg at weeks 0, 1, 2, and 4 produced the best PASI 75 response at week 12, of 55%.
While the safety analysis showed no significant differences from placebo, there were two cases of cardiac disorders – one angina pectoris and one coronary artery disease – in the intravenous dose-ranging study and two cases listed as "cardiac disorders" in the regimen-finding study. "We don’t know if these are significant. We have to look at phase III trials," Dr. Gordon said.
• Apremilast: This small molecule, taken orally, works by inhibiting type 4 phosphodiesterase. In a randomized, placebo-controlled phase II trial of 352 patients with moderate to severe plaque psoriasis, the PASI 75 response rate at 16 weeks was 41% with a 30-mg twice-daily dose.
Adverse effects were dose-dependent. Adverse events that occurred in 5% or more of patients included headache, nausea, diarrhea, and upper respiratory tract infections. These typically occurred early in the course of treatment.
Serious adverse events included one myocardial infarction and one case of prostate cancer in the 30-mg BID group. But there was also a prostate cancer and a sudden death among the placebo recipients. "We really don’t have enough patients to look at adverse effects," Dr. Gordon said.
• Tofacitinib: This oral Janus kinase inhibitor demonstrated dose-dependent efficacy, with 67% of patients randomized at 15 mg twice a day achieving PASI 75 and "clear" or "almost clear." The phase II, 12-week, double-blind, placebo-controlled trial enrolled 197 patients with moderate to severe plaque psoriasis.
Concomitant overall decreases in hemoglobin and neutrophil counts from baseline were also dose-dependent. The finding did not specify the proportion of patients who had the decreases or the individual degree of change. "If everyone had a small change, it’s not going to bother me too much. But, if 10% of patients had a big change, it’s a really important finding. Those are the questions we need to ask," Dr. Gordon said.
Dr. Gordon said that so far the phase II safety data for the agents are encouraging, but enthusiasm should still be tempered. "When multiple drugs with the same mechanism have [similar] results, you start to feel more confident. But still, we need to see larger studies."
"It’s really an exciting time for new psoriatic therapies based on a better understanding of psoriasis pathophysiology."
Dr. Leonardi’s presentation focused on anti-IL 12/23 inhibitor treatment; he noted that the recently-approved monoclonal antibody ustekinumab binds to the same shared p40 subunit of IL-12 and IL-23 as briakinumab, the agent that was withdrawn from development in phase III. "There are more similarities than differences" between the two agents, he commented.
He and his colleagues recently conducted a meta-analysis of 22 randomized controlled clinical trials of biologic therapies comprising 10,183 patients with chronic plaque psoriasis, in which 10 of 3,179 patients receiving either ustekinumab or briakinumab experienced a MACE, compared with 0 events in 1,474 patients receiving placebo, for a MACE rate of 1.33 per 100 patient-years.
In contrast, no difference was seen among patients in the anti-TNF-alpha trials, with only 1 of 3,858 patients receiving anti-TNF-alpha agents experiencing a MACE, compared with 1 of 1,812 patients receiving placebo (JAMA 2011;306:864-71).
Although the difference for the anti-IL 12/23 agents was not statistically significant, the data set was not large enough to detect rare events. "This is a class effect in my mind," Dr. Leonardi said, adding that he uses ustekinumab as a second-line agent, after the TNF antagonists.
"It’s important to remember that all new drugs are ‘new’ ... We will learn more and more about these drugs as time goes on," he said.
Dr. Gordon disclosed that he has received research support or honoraria as a consultant from Abbott, Amgen, Centocor, Eli Lilly, Merck, Novartis, and Pfizer. Dr. Leonardi disclosed that he has had financial relationships with 23 companies that are involved in psoriasis treatment development, including Abbott and Centocor.
SDEF and this news organization are owned by Elsevier.
LAS VEGAS – New agents for treating psoriasis have shown great promise in terms of efficacy, but assurances of safety await further data from larger studies.
Thus far, phase II data show impressive efficacy and no worrisome safety signals for the anti-interleukin-17 agents AMG 827 and secukinumab and the small molecules apremilast and tofacitinib. However, the studies have been too small and of insufficient duration to definitively rule out cardiovascular, infectious, and cancer risks, said Dr. Kenneth B. Gordon at the Las Vegas Dermatology Seminar, sponsored by Skin Disease Education Foundation (SDEF).
"It is my hope that these drugs are going to be fantastic. We just have to maintain a level of concern and vigilance for both biologics and small molecules ... We just desperately need large trials," said Dr. Gordon, head of the division of dermatology at NorthShore University HealthSystem, Chicago.
The discovery of IL-17 as a key player in psoriatic plaque formation has led to a new understanding of psoriasis pathophysiology and has become a new target for drug development. However, experience with one agent that blocks IL-12/23 – which induces activated IL-17 – gives pause.
Briakinumab, an extremely effective anti-psoriatic agent that blocks IL 12/23, was withdrawn from development after phase III studies showed a signal – albeit statistically insignificant – for serious infections including cellulitis and pneumonia, MACE events (cardiac arrest, myocardial infarction, and stroke), and malignancies (nonmelanoma skin cancer and squamous cell carcinoma of the lung and nasopharynx).
The absolute MACE event numbers were small, but were counter to what would be expected from a systemic anti-inflammatory agent, which should reduce cardiovascular disease, Dr. Craig L. Leonardi, a clinical professor of dermatology at St. Louis University, said in a separate presentation.
According to Dr. Gordon, "It’s really an exciting time for new psoriatic therapies based on a better understanding of psoriasis pathophysiology. However, we are less excited about phase II data because of what happened to briakinumab in phase III."
It will be essential to determine the etiology of the adverse effects, he said. "If the effects are not related to how well the agent controls psoriasis but to mechanisms like IL-12 blockade that may not have relevance to IL-17, they may not show up [with the new agents in development]. That’s what the phase II studies suggest, but it’s too early to really make a final statement," Dr. Gordon said in an interview.
Phase II data on the anti-IL17 and small molecules were presented earlier this year at the European Academy of Dermatology and Venereology meeting in Lisbon and at the World Congress of Dermatology in Seoul. Among the findings:
• AMG 827: This fully-human monoclonal antibody binds to and blocks the IL-17 receptor. In a phase II, double-blind, randomized, placebo-controlled trial of 198 patients who were randomized to subcutaneous AMG 827 at 280 mg monthly; to 70, 140, or 210 mg every 2 weeks; or to placebo. The primary end point, PASI 75 response rate at week 12, was highest (83%) in patients who received 210 mg every 2 weeks. Moreover, at that dose, the proportion achieving a PASI 100 score, indicating no psoriasis activity, was 63%.
"This is an extraordinarily high-responding drug, similar only to briakinumab," Dr. Gordon commented.
Changes in neutrophil counts were seen, as to be expected from IL-17 and IL-12 blockade. "Some of the changes were significant. We need to keep an eye on this," he said.
• Secukinumab: This novel, fully human antibody to IL-17A was investigated in three separate phase II trials of patients with moderate to severe plaque psoriasis. An intravenous induction dose-ranging study of 100 patients yielded PASI 75 response rates at 12 weeks of 40%-83%. A subcutaneous dose-ranging study of 125 patients produced PASI 75 response rates of 19%-81%, and a subcutaneous regimen-finding trial involving 404 patients determined that a regimen of 150 mg at weeks 0, 1, 2, and 4 produced the best PASI 75 response at week 12, of 55%.
While the safety analysis showed no significant differences from placebo, there were two cases of cardiac disorders – one angina pectoris and one coronary artery disease – in the intravenous dose-ranging study and two cases listed as "cardiac disorders" in the regimen-finding study. "We don’t know if these are significant. We have to look at phase III trials," Dr. Gordon said.
• Apremilast: This small molecule, taken orally, works by inhibiting type 4 phosphodiesterase. In a randomized, placebo-controlled phase II trial of 352 patients with moderate to severe plaque psoriasis, the PASI 75 response rate at 16 weeks was 41% with a 30-mg twice-daily dose.
Adverse effects were dose-dependent. Adverse events that occurred in 5% or more of patients included headache, nausea, diarrhea, and upper respiratory tract infections. These typically occurred early in the course of treatment.
Serious adverse events included one myocardial infarction and one case of prostate cancer in the 30-mg BID group. But there was also a prostate cancer and a sudden death among the placebo recipients. "We really don’t have enough patients to look at adverse effects," Dr. Gordon said.
• Tofacitinib: This oral Janus kinase inhibitor demonstrated dose-dependent efficacy, with 67% of patients randomized at 15 mg twice a day achieving PASI 75 and "clear" or "almost clear." The phase II, 12-week, double-blind, placebo-controlled trial enrolled 197 patients with moderate to severe plaque psoriasis.
Concomitant overall decreases in hemoglobin and neutrophil counts from baseline were also dose-dependent. The finding did not specify the proportion of patients who had the decreases or the individual degree of change. "If everyone had a small change, it’s not going to bother me too much. But, if 10% of patients had a big change, it’s a really important finding. Those are the questions we need to ask," Dr. Gordon said.
Dr. Gordon said that so far the phase II safety data for the agents are encouraging, but enthusiasm should still be tempered. "When multiple drugs with the same mechanism have [similar] results, you start to feel more confident. But still, we need to see larger studies."
"It’s really an exciting time for new psoriatic therapies based on a better understanding of psoriasis pathophysiology."
Dr. Leonardi’s presentation focused on anti-IL 12/23 inhibitor treatment; he noted that the recently-approved monoclonal antibody ustekinumab binds to the same shared p40 subunit of IL-12 and IL-23 as briakinumab, the agent that was withdrawn from development in phase III. "There are more similarities than differences" between the two agents, he commented.
He and his colleagues recently conducted a meta-analysis of 22 randomized controlled clinical trials of biologic therapies comprising 10,183 patients with chronic plaque psoriasis, in which 10 of 3,179 patients receiving either ustekinumab or briakinumab experienced a MACE, compared with 0 events in 1,474 patients receiving placebo, for a MACE rate of 1.33 per 100 patient-years.
In contrast, no difference was seen among patients in the anti-TNF-alpha trials, with only 1 of 3,858 patients receiving anti-TNF-alpha agents experiencing a MACE, compared with 1 of 1,812 patients receiving placebo (JAMA 2011;306:864-71).
Although the difference for the anti-IL 12/23 agents was not statistically significant, the data set was not large enough to detect rare events. "This is a class effect in my mind," Dr. Leonardi said, adding that he uses ustekinumab as a second-line agent, after the TNF antagonists.
"It’s important to remember that all new drugs are ‘new’ ... We will learn more and more about these drugs as time goes on," he said.
Dr. Gordon disclosed that he has received research support or honoraria as a consultant from Abbott, Amgen, Centocor, Eli Lilly, Merck, Novartis, and Pfizer. Dr. Leonardi disclosed that he has had financial relationships with 23 companies that are involved in psoriasis treatment development, including Abbott and Centocor.
SDEF and this news organization are owned by Elsevier.
EXPERT ANALYSIS FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR
Dermatologists Not Immune to Burnout
LAS VEGAS – A growing body of medical literature suggests that physicians are increasingly feeling burned out and dissatisfied with their profession.
In a 2009 survey of 7,905 surgeons, 40% described themselves as burned out, 30% screened positive for symptoms of depression, and 28% had a mental quality of life score that was greater than one-half of a standard deviation below the population norm (Annals Surg. 2009;250:463-71).
"In addition, 49% said they would not want their children to be physicians," Dr. Stephen H. Mandy reported at SDEF Las Vegas Dermatology Seminar.
In a more recent survey of 16,394 internal medicine residents, 52% reported burnout, 46% reported high levels of emotional exhaustion, and 29% reported high levels of depersonalization (JAMA 2011;306: 952-60). Level of debt was correlated with a sense of burnout.
Common causes of burnout range from personal and professional financial debt to health problems and increased regulatory demands, but other reasons "are mostly due to boredom, which usually starts around age 45," said Dr. Mandy, a dermatologist who practices in Miami Beach. "Most people affected by burnout are very good at their job but they’re not learning anything new, they’re not challenged, and they’re not deriving satisfaction form their work."
A long list of potentially dire consequences face burned out dermatologists, he said, including loss of staff, divorce, alcoholism, medical errors that may translate into lawsuits, and other personal problems, as well as loss of patient confidence, trust, and satisfaction.
In a 2006 article, Dr. Mandy suggested that dermatologists and great culinary chefs share a certain kinship, including a thirst for knowledge, an artistic eye and sensitivity, and attention to detail (Clin. Dermatol. 2006;24:543-4). Both professions embrace "rigorous consistency and methodology, respect for tradition of the trade, service, and long years of training," he said.
Despite the parallels of the professions, he cautioned that success in dermatology comes with a price, including increased public exposure that may result in less privacy. "And if you’re expanding your business empire, expect to spend more time with management issues and personnel problems and less time doing what you like to do," he said.
Dr. Mandy offered the following tips for dermatologists on the verge of burnout:
• Reflect on why you chose medicine as a profession. "It is not only about the money; it’s about the service of others," Dr. Mandy emphasized. "If you forget why you went to medical school, volunteer for a month in a third-world country or inner-city clinic to remember."
• Be mindful of your lifestyle choices. "Practice in a peaceful place," he advised. "Engage and enjoy your patients – it’s fun and good business; and run your office in a manner that is fun."
Setting aside time for "the things you love" – be it family, pets, sports, hobbies, or other interests outside of work – is also key, as is a willingness to seek professional help in getting your life on track. In one recent study, primary care physicians who participated in an intensive educational program in mindfulness, communication, and self-awareness experienced short-term and sustained improvements in well being and attitudes associated with patient-centered care (JAMA 2009;302:1284-93).
• Know your capabilities. "You cannot build satisfaction on your weaknesses," he said. Build your body of knowledge, perfect your skills, and demonstrate your mastery by publishing and mentoring.
• Tune in to how your practice delivers service. "This means treating your patients well and your employees better," he said. "Easier is better than faster and cheaper."
• Manage your patient load. "Don’t overschedule," Dr. Mandy cautioned. "Keep a small, integrated, mutually dependent staff, and strive for excellence and service. Your receptionist is your biggest asset."
• Lead by example. "Be prompt and dress well, in a manner that reflects your style," he said. "Be professional."
Dr. Mandy said that he had no relevant financial conflicts to disclose.
SDEF and this news organization are owned by Elsevier.
LAS VEGAS – A growing body of medical literature suggests that physicians are increasingly feeling burned out and dissatisfied with their profession.
In a 2009 survey of 7,905 surgeons, 40% described themselves as burned out, 30% screened positive for symptoms of depression, and 28% had a mental quality of life score that was greater than one-half of a standard deviation below the population norm (Annals Surg. 2009;250:463-71).
"In addition, 49% said they would not want their children to be physicians," Dr. Stephen H. Mandy reported at SDEF Las Vegas Dermatology Seminar.
In a more recent survey of 16,394 internal medicine residents, 52% reported burnout, 46% reported high levels of emotional exhaustion, and 29% reported high levels of depersonalization (JAMA 2011;306: 952-60). Level of debt was correlated with a sense of burnout.
Common causes of burnout range from personal and professional financial debt to health problems and increased regulatory demands, but other reasons "are mostly due to boredom, which usually starts around age 45," said Dr. Mandy, a dermatologist who practices in Miami Beach. "Most people affected by burnout are very good at their job but they’re not learning anything new, they’re not challenged, and they’re not deriving satisfaction form their work."
A long list of potentially dire consequences face burned out dermatologists, he said, including loss of staff, divorce, alcoholism, medical errors that may translate into lawsuits, and other personal problems, as well as loss of patient confidence, trust, and satisfaction.
In a 2006 article, Dr. Mandy suggested that dermatologists and great culinary chefs share a certain kinship, including a thirst for knowledge, an artistic eye and sensitivity, and attention to detail (Clin. Dermatol. 2006;24:543-4). Both professions embrace "rigorous consistency and methodology, respect for tradition of the trade, service, and long years of training," he said.
Despite the parallels of the professions, he cautioned that success in dermatology comes with a price, including increased public exposure that may result in less privacy. "And if you’re expanding your business empire, expect to spend more time with management issues and personnel problems and less time doing what you like to do," he said.
Dr. Mandy offered the following tips for dermatologists on the verge of burnout:
• Reflect on why you chose medicine as a profession. "It is not only about the money; it’s about the service of others," Dr. Mandy emphasized. "If you forget why you went to medical school, volunteer for a month in a third-world country or inner-city clinic to remember."
• Be mindful of your lifestyle choices. "Practice in a peaceful place," he advised. "Engage and enjoy your patients – it’s fun and good business; and run your office in a manner that is fun."
Setting aside time for "the things you love" – be it family, pets, sports, hobbies, or other interests outside of work – is also key, as is a willingness to seek professional help in getting your life on track. In one recent study, primary care physicians who participated in an intensive educational program in mindfulness, communication, and self-awareness experienced short-term and sustained improvements in well being and attitudes associated with patient-centered care (JAMA 2009;302:1284-93).
• Know your capabilities. "You cannot build satisfaction on your weaknesses," he said. Build your body of knowledge, perfect your skills, and demonstrate your mastery by publishing and mentoring.
• Tune in to how your practice delivers service. "This means treating your patients well and your employees better," he said. "Easier is better than faster and cheaper."
• Manage your patient load. "Don’t overschedule," Dr. Mandy cautioned. "Keep a small, integrated, mutually dependent staff, and strive for excellence and service. Your receptionist is your biggest asset."
• Lead by example. "Be prompt and dress well, in a manner that reflects your style," he said. "Be professional."
Dr. Mandy said that he had no relevant financial conflicts to disclose.
SDEF and this news organization are owned by Elsevier.
LAS VEGAS – A growing body of medical literature suggests that physicians are increasingly feeling burned out and dissatisfied with their profession.
In a 2009 survey of 7,905 surgeons, 40% described themselves as burned out, 30% screened positive for symptoms of depression, and 28% had a mental quality of life score that was greater than one-half of a standard deviation below the population norm (Annals Surg. 2009;250:463-71).
"In addition, 49% said they would not want their children to be physicians," Dr. Stephen H. Mandy reported at SDEF Las Vegas Dermatology Seminar.
In a more recent survey of 16,394 internal medicine residents, 52% reported burnout, 46% reported high levels of emotional exhaustion, and 29% reported high levels of depersonalization (JAMA 2011;306: 952-60). Level of debt was correlated with a sense of burnout.
Common causes of burnout range from personal and professional financial debt to health problems and increased regulatory demands, but other reasons "are mostly due to boredom, which usually starts around age 45," said Dr. Mandy, a dermatologist who practices in Miami Beach. "Most people affected by burnout are very good at their job but they’re not learning anything new, they’re not challenged, and they’re not deriving satisfaction form their work."
A long list of potentially dire consequences face burned out dermatologists, he said, including loss of staff, divorce, alcoholism, medical errors that may translate into lawsuits, and other personal problems, as well as loss of patient confidence, trust, and satisfaction.
In a 2006 article, Dr. Mandy suggested that dermatologists and great culinary chefs share a certain kinship, including a thirst for knowledge, an artistic eye and sensitivity, and attention to detail (Clin. Dermatol. 2006;24:543-4). Both professions embrace "rigorous consistency and methodology, respect for tradition of the trade, service, and long years of training," he said.
Despite the parallels of the professions, he cautioned that success in dermatology comes with a price, including increased public exposure that may result in less privacy. "And if you’re expanding your business empire, expect to spend more time with management issues and personnel problems and less time doing what you like to do," he said.
Dr. Mandy offered the following tips for dermatologists on the verge of burnout:
• Reflect on why you chose medicine as a profession. "It is not only about the money; it’s about the service of others," Dr. Mandy emphasized. "If you forget why you went to medical school, volunteer for a month in a third-world country or inner-city clinic to remember."
• Be mindful of your lifestyle choices. "Practice in a peaceful place," he advised. "Engage and enjoy your patients – it’s fun and good business; and run your office in a manner that is fun."
Setting aside time for "the things you love" – be it family, pets, sports, hobbies, or other interests outside of work – is also key, as is a willingness to seek professional help in getting your life on track. In one recent study, primary care physicians who participated in an intensive educational program in mindfulness, communication, and self-awareness experienced short-term and sustained improvements in well being and attitudes associated with patient-centered care (JAMA 2009;302:1284-93).
• Know your capabilities. "You cannot build satisfaction on your weaknesses," he said. Build your body of knowledge, perfect your skills, and demonstrate your mastery by publishing and mentoring.
• Tune in to how your practice delivers service. "This means treating your patients well and your employees better," he said. "Easier is better than faster and cheaper."
• Manage your patient load. "Don’t overschedule," Dr. Mandy cautioned. "Keep a small, integrated, mutually dependent staff, and strive for excellence and service. Your receptionist is your biggest asset."
• Lead by example. "Be prompt and dress well, in a manner that reflects your style," he said. "Be professional."
Dr. Mandy said that he had no relevant financial conflicts to disclose.
SDEF and this news organization are owned by Elsevier.
EXPERT ANALYSIS FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR
Psoriasis Patients Face Increased Risk of CVD
LAS VEGAS – The list of disease states and behaviors that potentially increase morbidity and mortality and lower quality of life for psoriasis patients is well known and includes psoriatic arthritis, Crohn’s disease, depression, alcoholism, and smoking.
Perhaps less well appreciated is the fact that psoriasis is also associated with multiple comorbidities that increase the risk of cardiovascular disease, including hypertension, diabetes, dyslipidemia, and obesity, Dr. Bruce E. Strober said at the SDEF Las Vegas Dermatology Seminar.
"The metabolic syndrome, a chronic inflammatory state that is associated with increased cardiovascular mortality, is also common in patients with psoriasis," noted Dr. Strober of the department of dermatology at the University of Connecticut, Farmington. The syndrome is associated with at least three of the following five factors: increased waist circumference or abdominal obesity, hypertension, hypertriglyceridemia, reduced high-density lipoprotein levels, and insulin resistance.
In 2006 German researchers published results from a trial that compared the prevalence of metabolic syndrome in 581 adults hospitalized with plaque-type psoriasis to the prevalence in 1,044 controls who were treated surgically for localized melanoma during the same time period (Arch. Dermatol. Res. 2006;298:321-8). Charts were screened for the presence of concomitant forms of chronic internal diseases.
The researchers discovered that compared with controls, psoriasis patients had a significantly higher prevalence of three components of metabolic syndrome, including diabetes mellitus (odds ratio, 2.48); hyperlipidemia (OR, 2.09); and arterial hypertension (OR, 3.27).
A separate, larger trial conducted in the United Kingdom set out to determine whether the prevalence of major cardiovascular risk factors was higher in mild or severe psoriasis patients, or in patients without psoriasis (J. Am. Acad. Dermatol. 2006;55:829-35). Patients were defined as having severe psoriasis if they received a code for psoriasis as well as systemic therapy used for the treatment of psoriasis, while patients were defined as having mild psoriasis if they ever received a psoriasis code but no systemic therapy.
The population-based study included 127,706 patients with mild psoriasis and 3,854 with severe disease. The researchers found that patients with mild psoriasis had a higher adjusted odds of diabetes (odds ratio, 1.13); hypertension (OR, 1.03); hyperlipidemia (OR, 1.16); obesity (OR, 1.27); and smoking (OR, 1.31), compared with controls, while patients with severe psoriasis had a higher adjusted odds of diabetes (OR, 1.62); obesity (OR, 1.79);and smoking (OR, 1.31) than controls, Dr. Strober reported at the seminar sponsored by Skin Disease Education Foundation (SDEF).
In addition, diabetes (OR, 1.39) and obesity (OR 1.47) were more prevalent in those with severe psoriasis than with mild psoriasis.
According to Dr. Strober, one of the largest studies to evaluate the association between obesity and the risk of psoriasis comes from 78,626 women who participated in the ongoing Nurses’ Health Study (Arch. Intern. Med. 2007;167:1670-5). After adjustment for age, alcohol consumption, and smoking status, the researchers found that the relative risk of developing psoriasis increased with advancing body mass index category: 1.40 for a BMI of 25-29.9 kg/m2, 1.48 for a BMI of 30-34.9 kg/m2, and 2.69 for a BMI of 35 kg/m2 or greater.
A higher waist circumference, hip circumference, and waist-hip ratio were also associated with a higher risk of incident psoriasis.
Myocardial infarction is also associated with psoriasis, according to a population-based study in the United Kingdom that evaluated outcomes in 556,995 controls, 127,139 patients with mild psoriasis, and 3,837 patients with severe psoriasis (JAMA 2006;296:1735-41). The researchers found that the adjusted relative risk of myocardial infarction was 3.58 among controls, 4.04 among those with mild psoriasis, and 5.13 among those with severe psoriasis.
"Possible causes for increased cardiovascular risks in psoriasis include the use of dyslipidemic therapies, such as corticosteroids, acitretin, and cyclosporine; the increased prevalence of obesity and other associated risk factors; and uncontrolled inflammation leading to endothelial dysfunction and dyslipidemia," Dr. Strober said.
He emphasized that many questions remain about the association between psoriasis and cardiovascular risk factors. "Do the associations have any clinical relevance?" he asked. "Do specific comorbidities influence the response to therapy for psoriasis? Does psoriasis influence the response to therapy for any specific comorbidity? Will specific psoriasis therapies reduce the negative health consequences of a comorbidity of psoriasis?"
For now, he said, dermatologists might consider screening patients for the prevalence of cardiovascular risk factors through laboratory evaluations such as a comprehensive metabolic panel and fasting lipids, assessing blood pressure and weight status, and asking patients about their history of smoking, alcohol use, depression, and arthritis.
Dr. Strober disclosed that he is a member of the scientific advisory board for Abbott, Amgen, Janssen, Novartis, and Pfizer. He also disclosed that he is a consultant for Abbott, Amgen, Celgene, Centocor, Galderma, Leo, Maruho, Novartis, and Pfizer, and that he has received honoraria from Abbott.
SDEF and this news organization are owned by Elsevier.
LAS VEGAS – The list of disease states and behaviors that potentially increase morbidity and mortality and lower quality of life for psoriasis patients is well known and includes psoriatic arthritis, Crohn’s disease, depression, alcoholism, and smoking.
Perhaps less well appreciated is the fact that psoriasis is also associated with multiple comorbidities that increase the risk of cardiovascular disease, including hypertension, diabetes, dyslipidemia, and obesity, Dr. Bruce E. Strober said at the SDEF Las Vegas Dermatology Seminar.
"The metabolic syndrome, a chronic inflammatory state that is associated with increased cardiovascular mortality, is also common in patients with psoriasis," noted Dr. Strober of the department of dermatology at the University of Connecticut, Farmington. The syndrome is associated with at least three of the following five factors: increased waist circumference or abdominal obesity, hypertension, hypertriglyceridemia, reduced high-density lipoprotein levels, and insulin resistance.
In 2006 German researchers published results from a trial that compared the prevalence of metabolic syndrome in 581 adults hospitalized with plaque-type psoriasis to the prevalence in 1,044 controls who were treated surgically for localized melanoma during the same time period (Arch. Dermatol. Res. 2006;298:321-8). Charts were screened for the presence of concomitant forms of chronic internal diseases.
The researchers discovered that compared with controls, psoriasis patients had a significantly higher prevalence of three components of metabolic syndrome, including diabetes mellitus (odds ratio, 2.48); hyperlipidemia (OR, 2.09); and arterial hypertension (OR, 3.27).
A separate, larger trial conducted in the United Kingdom set out to determine whether the prevalence of major cardiovascular risk factors was higher in mild or severe psoriasis patients, or in patients without psoriasis (J. Am. Acad. Dermatol. 2006;55:829-35). Patients were defined as having severe psoriasis if they received a code for psoriasis as well as systemic therapy used for the treatment of psoriasis, while patients were defined as having mild psoriasis if they ever received a psoriasis code but no systemic therapy.
The population-based study included 127,706 patients with mild psoriasis and 3,854 with severe disease. The researchers found that patients with mild psoriasis had a higher adjusted odds of diabetes (odds ratio, 1.13); hypertension (OR, 1.03); hyperlipidemia (OR, 1.16); obesity (OR, 1.27); and smoking (OR, 1.31), compared with controls, while patients with severe psoriasis had a higher adjusted odds of diabetes (OR, 1.62); obesity (OR, 1.79);and smoking (OR, 1.31) than controls, Dr. Strober reported at the seminar sponsored by Skin Disease Education Foundation (SDEF).
In addition, diabetes (OR, 1.39) and obesity (OR 1.47) were more prevalent in those with severe psoriasis than with mild psoriasis.
According to Dr. Strober, one of the largest studies to evaluate the association between obesity and the risk of psoriasis comes from 78,626 women who participated in the ongoing Nurses’ Health Study (Arch. Intern. Med. 2007;167:1670-5). After adjustment for age, alcohol consumption, and smoking status, the researchers found that the relative risk of developing psoriasis increased with advancing body mass index category: 1.40 for a BMI of 25-29.9 kg/m2, 1.48 for a BMI of 30-34.9 kg/m2, and 2.69 for a BMI of 35 kg/m2 or greater.
A higher waist circumference, hip circumference, and waist-hip ratio were also associated with a higher risk of incident psoriasis.
Myocardial infarction is also associated with psoriasis, according to a population-based study in the United Kingdom that evaluated outcomes in 556,995 controls, 127,139 patients with mild psoriasis, and 3,837 patients with severe psoriasis (JAMA 2006;296:1735-41). The researchers found that the adjusted relative risk of myocardial infarction was 3.58 among controls, 4.04 among those with mild psoriasis, and 5.13 among those with severe psoriasis.
"Possible causes for increased cardiovascular risks in psoriasis include the use of dyslipidemic therapies, such as corticosteroids, acitretin, and cyclosporine; the increased prevalence of obesity and other associated risk factors; and uncontrolled inflammation leading to endothelial dysfunction and dyslipidemia," Dr. Strober said.
He emphasized that many questions remain about the association between psoriasis and cardiovascular risk factors. "Do the associations have any clinical relevance?" he asked. "Do specific comorbidities influence the response to therapy for psoriasis? Does psoriasis influence the response to therapy for any specific comorbidity? Will specific psoriasis therapies reduce the negative health consequences of a comorbidity of psoriasis?"
For now, he said, dermatologists might consider screening patients for the prevalence of cardiovascular risk factors through laboratory evaluations such as a comprehensive metabolic panel and fasting lipids, assessing blood pressure and weight status, and asking patients about their history of smoking, alcohol use, depression, and arthritis.
Dr. Strober disclosed that he is a member of the scientific advisory board for Abbott, Amgen, Janssen, Novartis, and Pfizer. He also disclosed that he is a consultant for Abbott, Amgen, Celgene, Centocor, Galderma, Leo, Maruho, Novartis, and Pfizer, and that he has received honoraria from Abbott.
SDEF and this news organization are owned by Elsevier.
LAS VEGAS – The list of disease states and behaviors that potentially increase morbidity and mortality and lower quality of life for psoriasis patients is well known and includes psoriatic arthritis, Crohn’s disease, depression, alcoholism, and smoking.
Perhaps less well appreciated is the fact that psoriasis is also associated with multiple comorbidities that increase the risk of cardiovascular disease, including hypertension, diabetes, dyslipidemia, and obesity, Dr. Bruce E. Strober said at the SDEF Las Vegas Dermatology Seminar.
"The metabolic syndrome, a chronic inflammatory state that is associated with increased cardiovascular mortality, is also common in patients with psoriasis," noted Dr. Strober of the department of dermatology at the University of Connecticut, Farmington. The syndrome is associated with at least three of the following five factors: increased waist circumference or abdominal obesity, hypertension, hypertriglyceridemia, reduced high-density lipoprotein levels, and insulin resistance.
In 2006 German researchers published results from a trial that compared the prevalence of metabolic syndrome in 581 adults hospitalized with plaque-type psoriasis to the prevalence in 1,044 controls who were treated surgically for localized melanoma during the same time period (Arch. Dermatol. Res. 2006;298:321-8). Charts were screened for the presence of concomitant forms of chronic internal diseases.
The researchers discovered that compared with controls, psoriasis patients had a significantly higher prevalence of three components of metabolic syndrome, including diabetes mellitus (odds ratio, 2.48); hyperlipidemia (OR, 2.09); and arterial hypertension (OR, 3.27).
A separate, larger trial conducted in the United Kingdom set out to determine whether the prevalence of major cardiovascular risk factors was higher in mild or severe psoriasis patients, or in patients without psoriasis (J. Am. Acad. Dermatol. 2006;55:829-35). Patients were defined as having severe psoriasis if they received a code for psoriasis as well as systemic therapy used for the treatment of psoriasis, while patients were defined as having mild psoriasis if they ever received a psoriasis code but no systemic therapy.
The population-based study included 127,706 patients with mild psoriasis and 3,854 with severe disease. The researchers found that patients with mild psoriasis had a higher adjusted odds of diabetes (odds ratio, 1.13); hypertension (OR, 1.03); hyperlipidemia (OR, 1.16); obesity (OR, 1.27); and smoking (OR, 1.31), compared with controls, while patients with severe psoriasis had a higher adjusted odds of diabetes (OR, 1.62); obesity (OR, 1.79);and smoking (OR, 1.31) than controls, Dr. Strober reported at the seminar sponsored by Skin Disease Education Foundation (SDEF).
In addition, diabetes (OR, 1.39) and obesity (OR 1.47) were more prevalent in those with severe psoriasis than with mild psoriasis.
According to Dr. Strober, one of the largest studies to evaluate the association between obesity and the risk of psoriasis comes from 78,626 women who participated in the ongoing Nurses’ Health Study (Arch. Intern. Med. 2007;167:1670-5). After adjustment for age, alcohol consumption, and smoking status, the researchers found that the relative risk of developing psoriasis increased with advancing body mass index category: 1.40 for a BMI of 25-29.9 kg/m2, 1.48 for a BMI of 30-34.9 kg/m2, and 2.69 for a BMI of 35 kg/m2 or greater.
A higher waist circumference, hip circumference, and waist-hip ratio were also associated with a higher risk of incident psoriasis.
Myocardial infarction is also associated with psoriasis, according to a population-based study in the United Kingdom that evaluated outcomes in 556,995 controls, 127,139 patients with mild psoriasis, and 3,837 patients with severe psoriasis (JAMA 2006;296:1735-41). The researchers found that the adjusted relative risk of myocardial infarction was 3.58 among controls, 4.04 among those with mild psoriasis, and 5.13 among those with severe psoriasis.
"Possible causes for increased cardiovascular risks in psoriasis include the use of dyslipidemic therapies, such as corticosteroids, acitretin, and cyclosporine; the increased prevalence of obesity and other associated risk factors; and uncontrolled inflammation leading to endothelial dysfunction and dyslipidemia," Dr. Strober said.
He emphasized that many questions remain about the association between psoriasis and cardiovascular risk factors. "Do the associations have any clinical relevance?" he asked. "Do specific comorbidities influence the response to therapy for psoriasis? Does psoriasis influence the response to therapy for any specific comorbidity? Will specific psoriasis therapies reduce the negative health consequences of a comorbidity of psoriasis?"
For now, he said, dermatologists might consider screening patients for the prevalence of cardiovascular risk factors through laboratory evaluations such as a comprehensive metabolic panel and fasting lipids, assessing blood pressure and weight status, and asking patients about their history of smoking, alcohol use, depression, and arthritis.
Dr. Strober disclosed that he is a member of the scientific advisory board for Abbott, Amgen, Janssen, Novartis, and Pfizer. He also disclosed that he is a consultant for Abbott, Amgen, Celgene, Centocor, Galderma, Leo, Maruho, Novartis, and Pfizer, and that he has received honoraria from Abbott.
SDEF and this news organization are owned by Elsevier.
EXPERT ANALYSIS FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR