User login
Women’s Cancers: Clinicians Research, Advise on Sexual Dysfunction
Decreased sexual function is a side effect of many types of cancer, notably uterine, cervical, ovarian, and breast cancer, that often goes unaddressed, according to the authors of several studies presented at the Society of Gynecologic Oncology (SGO)’s Annual Meeting on Women’s Cancer.
Patients want to talk about sex, but not necessarily at the start of their diagnosis or treatment, suggest the findings of a study presented at the meeting. Jesse T. Brewer of Weill Cornell Medicine in New York City and colleagues enrolled 63 patients who underwent surgery with documented hereditary breast cancer, ovarian cancer, or Lynch syndrome in a cross-sectional survey.
Overall, 86% said that sexuality and intimacy were very or somewhat important, and 78% said that the healthcare team addressing the issue was very or somewhat important, the researchers found. However, only 40% of the respondents said that they wanted to discuss sexuality at the time of diagnosis because the idea was too overwhelming.
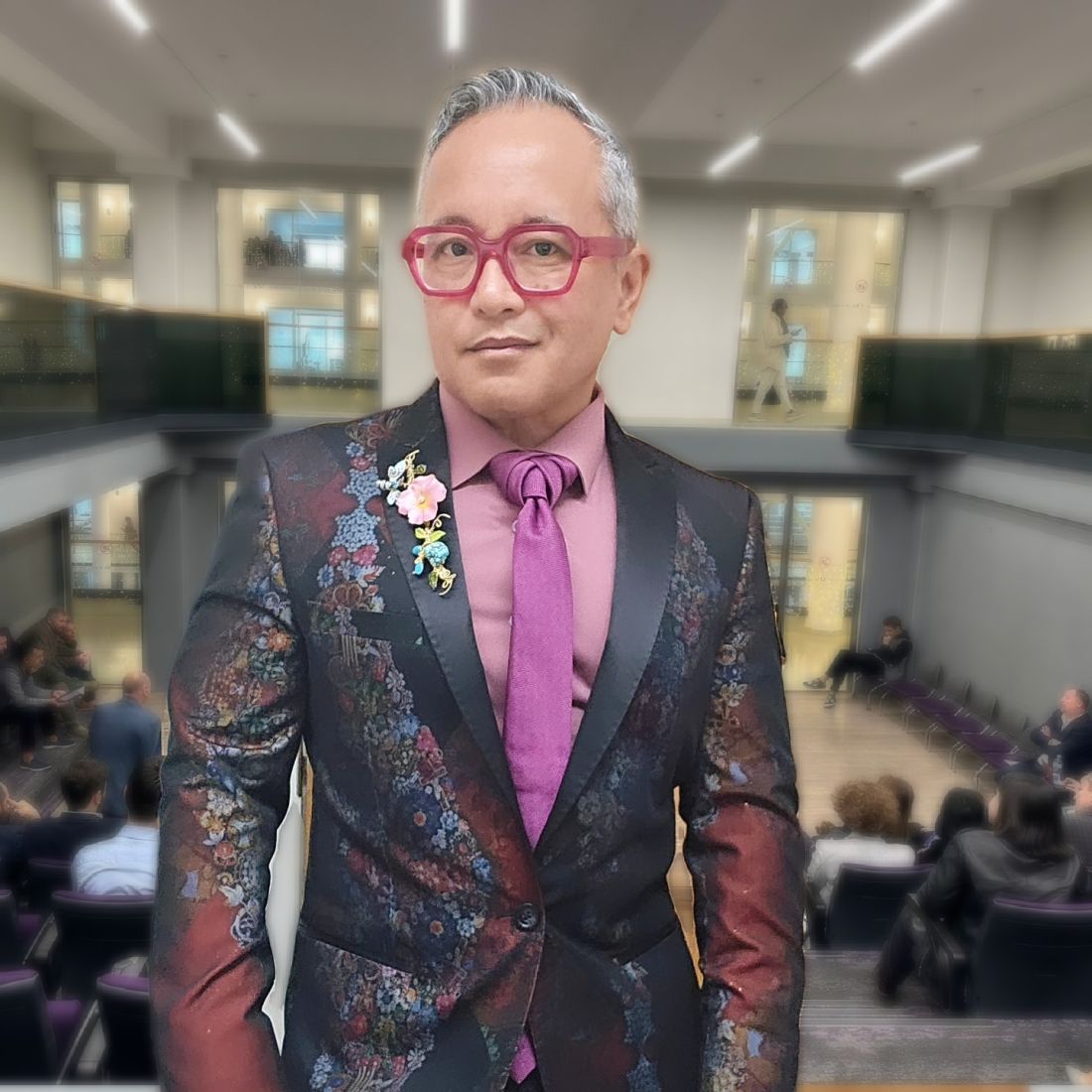
Oncologists are more aware of sexual side effects and the potential for sexual issues that persist long after treatment, but many patients may not have opportunities to talk about sexual concerns, said Don S. Dizon, MD, an oncologist specializing in women’s cancers at Brown University, Providence, Rhode Island, in an interview.
“It is important that we [oncologists] be the ones to open the door to these conversations; people with cancer will not bring it up spontaneously, for fear of making their provider uncomfortable, especially if they’ve never been asked about it before,” Dr. Dizon said in an interview.
He advised clinicians to find a network within their health systems so they can refer patients to specialized services, such as sex therapy, couples counseling, pelvic rehabilitation, or menopausal experts as needed.
In another study presented at the meeting, Naaman Mehta, MD, of NYU Langone Health, and colleagues reviewed data from 166 healthcare providers who completed a 23-item survey about evaluating and managing sexual health concerns of their patients. Most of the respondents were gynecologic oncologists (93.4%), but one radiation oncologist and 10 other healthcare providers also completed the survey.
Overall, approximately 60% of the respondents routinely asked about the sexual health concerns of their patients, and 98% of these said they believed that sexual health discussions should be held with a gynecologic oncologist. Just over half (54%) also said that the patient should be the one to initiate a discussion of sexual health concerns.
Female providers were significantly more likely to discuss sexual health with patients, compared with male providers, after controlling for the hospital setting and training level, the researchers noted (odds ratio, 1.4;P < .01).
The results suggest a need for more ways to integrate sexual health screening into gynecologic oncologic clinics, the researchers concluded.
The provider survey findings are similar to the results of a survey conducted by Dr. Dizon and colleagues in 2007. In that study, less than half of respondents took a sexual history, but 80% felt there was insufficient time to explore sexual issues.
“It is critical to understand that people with cancer do not expect their oncologists to be sexual health experts, but as with all other side effects caused by treatment and the diagnosis, we can be the ones who recognize it,” Dr. Dizon noted, in an interview.
Common Complaints and Causes
In Dr. Dizon’s experience, local symptoms including vaginal dryness, pain with penetration, and vaginal thinning, are common sexual complaints in women with cancer, as are systemic issues such as lack of interest and menopause-type symptoms.
“For those undergoing radiation, the vaginal tunnel can actually develop adhesions, and if not treated proactively this can lead to vaginal stenosis,” said Dr. Dizon, who was not involved in the studies presented at the meeting.
Comorbidities such as diabetes, cardiovascular disease, and musculoskeletal conditions can contribute to sexual issues in women with cancer, according to Nora Lersch, DNP, FNP-BC, AOCNP, and Nicole Dreibelbis, CRNP, the authors of other research presented at the meeting.
Culture, religion, fitness level, history of sexual violence, and gender spectrum health also play a role, as do anxiety and depression, dementia, and substance abuse disorders, the authors wrote in their presentation, “Prioritizing Sexual Health in Gynecological Oncology Care.”
Low libido is a frequent complaint across all cancer types, Ms. Dreibelbis, a nurse practitioner specializing in gynecologic oncology at the UPMC Hillman Cancer Center, Pittsburgh, Pennsylvania, said in an interview.
“Breast cancer patients, especially those on [aromatase inhibitor] therapy, often experience vaginal dryness and therefore dyspareunia,” she added.
The pelvic floor muscles, with their important role in sexual response, can be weakened by cancer treatment or surgery, and the pudendal nerves, which are the primary nerves responsible for sexual response in women, can be affected as well, Dr. Lersch and Ms. Dreibelbis wrote.
Taking Sex Seriously
Researchers are exploring the impact of different cancer prevention treatments for women to mitigate sexual side effects, as illustrated by another study presented at the meeting.
Dr. Barbara Norquist, MD, a gynecologic oncologist at the University of Washington, Seattle, and colleagues compared the sexual function and menopausal symptoms of patients at high risk of ovarian carcinoma who underwent either interval salpingectomy/delayed oophorectomy (ISDO) or risk-reducing salpingo-oophorectomy (RRSO).
“For patients at high risk for ovarian cancer, surgical removal of the tubes and ovaries is the mainstay of prevention, as screening is not effective at reducing death from ovarian cancer. As a result of surgery, many patients become suddenly postmenopausal from losing their ovaries,” Dr. Norquist said in an interview.
Some patients delay surgery out of concern for health and quality of life, including sexual function, she said.
In the study (known as the WISP trial) the researchers compared data from 166 patients who underwent immediate removal of the fallopian tubes and ovaries and 171 who underwent fallopian tube removal and delayed oophorectomy. All patients completed questionnaires about sexual function. The primary outcome was change in sexual function based on the sexual function index (FSFI) from baseline to 6 months after surgery.
Overall, changes in sexual function were significantly greater in the immediate oophorectomy group, compared with the delayed oophorectomy group at 6 months (33% vs 17%) and also at 12 months (43% vs 20%).
A further review of patients using hormone therapy showed that those in the immediate oophorectomy group still had greater decreases in sexual function, compared with the delayed group, though the difference between groups of patients using hormone therapy was less dramatic.
“I was surprised that, even with hormone replacement therapy, patients undergoing removal of the ovaries still had significant detrimental changes to sexual function when compared to those having the tubes removed, although this was even worse in those who could not take HRT,” Dr. Norquist said, in an interview. “I was reassured that menopausal symptoms in general were well managed with HRT, as these patients did not score differently on menopause symptoms, compared with those having their tubes removed,” she said.
Patients deserve accurate information about predicted changes in menopausal symptoms and sexual function as a result of ovary removal, and HRT should be provided when there is no contraindication, Dr. Norquist told this news organization.
Dr. Norquist and colleagues are awaiting the results of clinical trials investigating the safety of salpingectomy with delayed oophorectomy in terms of ovarian cancer prevention, but more research is needed to identify optimal management of the menopausal and sexual side effects associated with surgical menopause, she noted.
“Findings from the WISP study show the importance of hormones in women undergoing prophylactic surgery,” Dr. Dizon said. The findings indicate that salpingectomy has less of a negative influence on sexual function compared to removal of the ovaries, and the impact of hormone therapy and the relatively young age of the patients who took hormones reinforces current knowledge about hormones and sex, he added.
Barriers and Solutions
Barriers to asking women with cancer about sexual issues reported by providers include limited time, lack of training in sexual health, a desire to avoid offending the patient or making them uncomfortable, and uncertainty about how to answer the questions, Dr. Lersch and Ms. Dreibelbis wrote in their presentation.
Barriers to asking healthcare providers about their sexual issues reported by patients include the beliefs that the clinician should initiate the discussion, that sexual function will not be taken seriously, and that they might make the provider uncomfortable.
“Fortunately, more information and research has been done on sexual health and gynecological cancer in recent years, so oncologists are becoming more aware of the issues women may have,” said Dr. Lersch who is an oncology nurse practitioner at Providence Franz Cancer Institute in Portland, Oregon, in an interview.
Telling patients early in their cancer treatment about potential sexual side effects and opportunities for help is essential, she added.
Although oncologists have become more aware of the importance of sexual health and well-being for their patients, “I think there has historically been a disconnect in including sexual health education in medical training,” Ms. Dreibelbis said in an interview.
Dr. Lersch and Ms. Dreibelbis advised a multidimensional approach to managing sexual problems in cancer patients that includes consideration of biological and psychological symptoms, but also social, cultural, and interpersonal factors, in their presentation.
Their suggestions include discussing dyspareunia with their patients, asking for details such as whether the pain is internal or external, whether it occurs with activities outside of sex including masturbation, and whether bleeding is present.
Oncology therapies and surgeries can decrease or eliminate an individual’s ability to produce their own lubricant; for example, removal of the cervix eliminates cervical mucous, which helps with internal lubrication, they wrote in their presentation.
For patients with dyspareunia, Dr. Lersch and Ms. Dreibelbis recommend a vaginal moisturizer especially formulated for vaginal tissue that can be absorbed by the mucosal tissue of the vagina. Use of this type of product can increase the effectiveness of lubricants and help restore integrity of the vaginal tissue. Such moisturizers are available as gels, creams, or suppositories over the counter, and do not contain hormones.
Vaginal estrogen can be helpful for burning, itching, irritation, tissue fragility, and pain with sex, according to Dr. Lersch and Ms. Dreibelbis. Adequate estrogen therapy can promote normalization of vaginal pH and microflora, as well increase vaginal secretion and reduce pain and dryness with intercourse, the presenters stated in their presentation. In addition, dilator therapy can be used to help prevent vaginal stenosis, and penetration bumpers can help relieve discomfort during intercourse, they wrote.
Looking ahead, more research is needed to serve a wider patient population, Ms. Dreibelbis said, in an interview.
“LGBTQIA [individuals] have not been included in sexual health research and there are more people than ever who identify within this group of people. I know there has also been some very early work on shielding the clitoris from the impacts of radiation, and I believe this is extremely important up-and-coming research,” she said.
Dr. Lersch, Ms. Dreibelbi, Dr. Dizon, Dr. Norquist, Ms. Brewer, and Dr. Mehta had no financial conflicts to disclose.
Decreased sexual function is a side effect of many types of cancer, notably uterine, cervical, ovarian, and breast cancer, that often goes unaddressed, according to the authors of several studies presented at the Society of Gynecologic Oncology (SGO)’s Annual Meeting on Women’s Cancer.
Patients want to talk about sex, but not necessarily at the start of their diagnosis or treatment, suggest the findings of a study presented at the meeting. Jesse T. Brewer of Weill Cornell Medicine in New York City and colleagues enrolled 63 patients who underwent surgery with documented hereditary breast cancer, ovarian cancer, or Lynch syndrome in a cross-sectional survey.
Overall, 86% said that sexuality and intimacy were very or somewhat important, and 78% said that the healthcare team addressing the issue was very or somewhat important, the researchers found. However, only 40% of the respondents said that they wanted to discuss sexuality at the time of diagnosis because the idea was too overwhelming.
Oncologists are more aware of sexual side effects and the potential for sexual issues that persist long after treatment, but many patients may not have opportunities to talk about sexual concerns, said Don S. Dizon, MD, an oncologist specializing in women’s cancers at Brown University, Providence, Rhode Island, in an interview.
“It is important that we [oncologists] be the ones to open the door to these conversations; people with cancer will not bring it up spontaneously, for fear of making their provider uncomfortable, especially if they’ve never been asked about it before,” Dr. Dizon said in an interview.
He advised clinicians to find a network within their health systems so they can refer patients to specialized services, such as sex therapy, couples counseling, pelvic rehabilitation, or menopausal experts as needed.
In another study presented at the meeting, Naaman Mehta, MD, of NYU Langone Health, and colleagues reviewed data from 166 healthcare providers who completed a 23-item survey about evaluating and managing sexual health concerns of their patients. Most of the respondents were gynecologic oncologists (93.4%), but one radiation oncologist and 10 other healthcare providers also completed the survey.
Overall, approximately 60% of the respondents routinely asked about the sexual health concerns of their patients, and 98% of these said they believed that sexual health discussions should be held with a gynecologic oncologist. Just over half (54%) also said that the patient should be the one to initiate a discussion of sexual health concerns.
Female providers were significantly more likely to discuss sexual health with patients, compared with male providers, after controlling for the hospital setting and training level, the researchers noted (odds ratio, 1.4;P < .01).
The results suggest a need for more ways to integrate sexual health screening into gynecologic oncologic clinics, the researchers concluded.
The provider survey findings are similar to the results of a survey conducted by Dr. Dizon and colleagues in 2007. In that study, less than half of respondents took a sexual history, but 80% felt there was insufficient time to explore sexual issues.
“It is critical to understand that people with cancer do not expect their oncologists to be sexual health experts, but as with all other side effects caused by treatment and the diagnosis, we can be the ones who recognize it,” Dr. Dizon noted, in an interview.
Common Complaints and Causes
In Dr. Dizon’s experience, local symptoms including vaginal dryness, pain with penetration, and vaginal thinning, are common sexual complaints in women with cancer, as are systemic issues such as lack of interest and menopause-type symptoms.
“For those undergoing radiation, the vaginal tunnel can actually develop adhesions, and if not treated proactively this can lead to vaginal stenosis,” said Dr. Dizon, who was not involved in the studies presented at the meeting.
Comorbidities such as diabetes, cardiovascular disease, and musculoskeletal conditions can contribute to sexual issues in women with cancer, according to Nora Lersch, DNP, FNP-BC, AOCNP, and Nicole Dreibelbis, CRNP, the authors of other research presented at the meeting.
Culture, religion, fitness level, history of sexual violence, and gender spectrum health also play a role, as do anxiety and depression, dementia, and substance abuse disorders, the authors wrote in their presentation, “Prioritizing Sexual Health in Gynecological Oncology Care.”
Low libido is a frequent complaint across all cancer types, Ms. Dreibelbis, a nurse practitioner specializing in gynecologic oncology at the UPMC Hillman Cancer Center, Pittsburgh, Pennsylvania, said in an interview.
“Breast cancer patients, especially those on [aromatase inhibitor] therapy, often experience vaginal dryness and therefore dyspareunia,” she added.
The pelvic floor muscles, with their important role in sexual response, can be weakened by cancer treatment or surgery, and the pudendal nerves, which are the primary nerves responsible for sexual response in women, can be affected as well, Dr. Lersch and Ms. Dreibelbis wrote.
Taking Sex Seriously
Researchers are exploring the impact of different cancer prevention treatments for women to mitigate sexual side effects, as illustrated by another study presented at the meeting.
Dr. Barbara Norquist, MD, a gynecologic oncologist at the University of Washington, Seattle, and colleagues compared the sexual function and menopausal symptoms of patients at high risk of ovarian carcinoma who underwent either interval salpingectomy/delayed oophorectomy (ISDO) or risk-reducing salpingo-oophorectomy (RRSO).
“For patients at high risk for ovarian cancer, surgical removal of the tubes and ovaries is the mainstay of prevention, as screening is not effective at reducing death from ovarian cancer. As a result of surgery, many patients become suddenly postmenopausal from losing their ovaries,” Dr. Norquist said in an interview.
Some patients delay surgery out of concern for health and quality of life, including sexual function, she said.
In the study (known as the WISP trial) the researchers compared data from 166 patients who underwent immediate removal of the fallopian tubes and ovaries and 171 who underwent fallopian tube removal and delayed oophorectomy. All patients completed questionnaires about sexual function. The primary outcome was change in sexual function based on the sexual function index (FSFI) from baseline to 6 months after surgery.
Overall, changes in sexual function were significantly greater in the immediate oophorectomy group, compared with the delayed oophorectomy group at 6 months (33% vs 17%) and also at 12 months (43% vs 20%).
A further review of patients using hormone therapy showed that those in the immediate oophorectomy group still had greater decreases in sexual function, compared with the delayed group, though the difference between groups of patients using hormone therapy was less dramatic.
“I was surprised that, even with hormone replacement therapy, patients undergoing removal of the ovaries still had significant detrimental changes to sexual function when compared to those having the tubes removed, although this was even worse in those who could not take HRT,” Dr. Norquist said, in an interview. “I was reassured that menopausal symptoms in general were well managed with HRT, as these patients did not score differently on menopause symptoms, compared with those having their tubes removed,” she said.
Patients deserve accurate information about predicted changes in menopausal symptoms and sexual function as a result of ovary removal, and HRT should be provided when there is no contraindication, Dr. Norquist told this news organization.
Dr. Norquist and colleagues are awaiting the results of clinical trials investigating the safety of salpingectomy with delayed oophorectomy in terms of ovarian cancer prevention, but more research is needed to identify optimal management of the menopausal and sexual side effects associated with surgical menopause, she noted.
“Findings from the WISP study show the importance of hormones in women undergoing prophylactic surgery,” Dr. Dizon said. The findings indicate that salpingectomy has less of a negative influence on sexual function compared to removal of the ovaries, and the impact of hormone therapy and the relatively young age of the patients who took hormones reinforces current knowledge about hormones and sex, he added.
Barriers and Solutions
Barriers to asking women with cancer about sexual issues reported by providers include limited time, lack of training in sexual health, a desire to avoid offending the patient or making them uncomfortable, and uncertainty about how to answer the questions, Dr. Lersch and Ms. Dreibelbis wrote in their presentation.
Barriers to asking healthcare providers about their sexual issues reported by patients include the beliefs that the clinician should initiate the discussion, that sexual function will not be taken seriously, and that they might make the provider uncomfortable.
“Fortunately, more information and research has been done on sexual health and gynecological cancer in recent years, so oncologists are becoming more aware of the issues women may have,” said Dr. Lersch who is an oncology nurse practitioner at Providence Franz Cancer Institute in Portland, Oregon, in an interview.
Telling patients early in their cancer treatment about potential sexual side effects and opportunities for help is essential, she added.
Although oncologists have become more aware of the importance of sexual health and well-being for their patients, “I think there has historically been a disconnect in including sexual health education in medical training,” Ms. Dreibelbis said in an interview.
Dr. Lersch and Ms. Dreibelbis advised a multidimensional approach to managing sexual problems in cancer patients that includes consideration of biological and psychological symptoms, but also social, cultural, and interpersonal factors, in their presentation.
Their suggestions include discussing dyspareunia with their patients, asking for details such as whether the pain is internal or external, whether it occurs with activities outside of sex including masturbation, and whether bleeding is present.
Oncology therapies and surgeries can decrease or eliminate an individual’s ability to produce their own lubricant; for example, removal of the cervix eliminates cervical mucous, which helps with internal lubrication, they wrote in their presentation.
For patients with dyspareunia, Dr. Lersch and Ms. Dreibelbis recommend a vaginal moisturizer especially formulated for vaginal tissue that can be absorbed by the mucosal tissue of the vagina. Use of this type of product can increase the effectiveness of lubricants and help restore integrity of the vaginal tissue. Such moisturizers are available as gels, creams, or suppositories over the counter, and do not contain hormones.
Vaginal estrogen can be helpful for burning, itching, irritation, tissue fragility, and pain with sex, according to Dr. Lersch and Ms. Dreibelbis. Adequate estrogen therapy can promote normalization of vaginal pH and microflora, as well increase vaginal secretion and reduce pain and dryness with intercourse, the presenters stated in their presentation. In addition, dilator therapy can be used to help prevent vaginal stenosis, and penetration bumpers can help relieve discomfort during intercourse, they wrote.
Looking ahead, more research is needed to serve a wider patient population, Ms. Dreibelbis said, in an interview.
“LGBTQIA [individuals] have not been included in sexual health research and there are more people than ever who identify within this group of people. I know there has also been some very early work on shielding the clitoris from the impacts of radiation, and I believe this is extremely important up-and-coming research,” she said.
Dr. Lersch, Ms. Dreibelbi, Dr. Dizon, Dr. Norquist, Ms. Brewer, and Dr. Mehta had no financial conflicts to disclose.
Decreased sexual function is a side effect of many types of cancer, notably uterine, cervical, ovarian, and breast cancer, that often goes unaddressed, according to the authors of several studies presented at the Society of Gynecologic Oncology (SGO)’s Annual Meeting on Women’s Cancer.
Patients want to talk about sex, but not necessarily at the start of their diagnosis or treatment, suggest the findings of a study presented at the meeting. Jesse T. Brewer of Weill Cornell Medicine in New York City and colleagues enrolled 63 patients who underwent surgery with documented hereditary breast cancer, ovarian cancer, or Lynch syndrome in a cross-sectional survey.
Overall, 86% said that sexuality and intimacy were very or somewhat important, and 78% said that the healthcare team addressing the issue was very or somewhat important, the researchers found. However, only 40% of the respondents said that they wanted to discuss sexuality at the time of diagnosis because the idea was too overwhelming.
Oncologists are more aware of sexual side effects and the potential for sexual issues that persist long after treatment, but many patients may not have opportunities to talk about sexual concerns, said Don S. Dizon, MD, an oncologist specializing in women’s cancers at Brown University, Providence, Rhode Island, in an interview.
“It is important that we [oncologists] be the ones to open the door to these conversations; people with cancer will not bring it up spontaneously, for fear of making their provider uncomfortable, especially if they’ve never been asked about it before,” Dr. Dizon said in an interview.
He advised clinicians to find a network within their health systems so they can refer patients to specialized services, such as sex therapy, couples counseling, pelvic rehabilitation, or menopausal experts as needed.
In another study presented at the meeting, Naaman Mehta, MD, of NYU Langone Health, and colleagues reviewed data from 166 healthcare providers who completed a 23-item survey about evaluating and managing sexual health concerns of their patients. Most of the respondents were gynecologic oncologists (93.4%), but one radiation oncologist and 10 other healthcare providers also completed the survey.
Overall, approximately 60% of the respondents routinely asked about the sexual health concerns of their patients, and 98% of these said they believed that sexual health discussions should be held with a gynecologic oncologist. Just over half (54%) also said that the patient should be the one to initiate a discussion of sexual health concerns.
Female providers were significantly more likely to discuss sexual health with patients, compared with male providers, after controlling for the hospital setting and training level, the researchers noted (odds ratio, 1.4;P < .01).
The results suggest a need for more ways to integrate sexual health screening into gynecologic oncologic clinics, the researchers concluded.
The provider survey findings are similar to the results of a survey conducted by Dr. Dizon and colleagues in 2007. In that study, less than half of respondents took a sexual history, but 80% felt there was insufficient time to explore sexual issues.
“It is critical to understand that people with cancer do not expect their oncologists to be sexual health experts, but as with all other side effects caused by treatment and the diagnosis, we can be the ones who recognize it,” Dr. Dizon noted, in an interview.
Common Complaints and Causes
In Dr. Dizon’s experience, local symptoms including vaginal dryness, pain with penetration, and vaginal thinning, are common sexual complaints in women with cancer, as are systemic issues such as lack of interest and menopause-type symptoms.
“For those undergoing radiation, the vaginal tunnel can actually develop adhesions, and if not treated proactively this can lead to vaginal stenosis,” said Dr. Dizon, who was not involved in the studies presented at the meeting.
Comorbidities such as diabetes, cardiovascular disease, and musculoskeletal conditions can contribute to sexual issues in women with cancer, according to Nora Lersch, DNP, FNP-BC, AOCNP, and Nicole Dreibelbis, CRNP, the authors of other research presented at the meeting.
Culture, religion, fitness level, history of sexual violence, and gender spectrum health also play a role, as do anxiety and depression, dementia, and substance abuse disorders, the authors wrote in their presentation, “Prioritizing Sexual Health in Gynecological Oncology Care.”
Low libido is a frequent complaint across all cancer types, Ms. Dreibelbis, a nurse practitioner specializing in gynecologic oncology at the UPMC Hillman Cancer Center, Pittsburgh, Pennsylvania, said in an interview.
“Breast cancer patients, especially those on [aromatase inhibitor] therapy, often experience vaginal dryness and therefore dyspareunia,” she added.
The pelvic floor muscles, with their important role in sexual response, can be weakened by cancer treatment or surgery, and the pudendal nerves, which are the primary nerves responsible for sexual response in women, can be affected as well, Dr. Lersch and Ms. Dreibelbis wrote.
Taking Sex Seriously
Researchers are exploring the impact of different cancer prevention treatments for women to mitigate sexual side effects, as illustrated by another study presented at the meeting.
Dr. Barbara Norquist, MD, a gynecologic oncologist at the University of Washington, Seattle, and colleagues compared the sexual function and menopausal symptoms of patients at high risk of ovarian carcinoma who underwent either interval salpingectomy/delayed oophorectomy (ISDO) or risk-reducing salpingo-oophorectomy (RRSO).
“For patients at high risk for ovarian cancer, surgical removal of the tubes and ovaries is the mainstay of prevention, as screening is not effective at reducing death from ovarian cancer. As a result of surgery, many patients become suddenly postmenopausal from losing their ovaries,” Dr. Norquist said in an interview.
Some patients delay surgery out of concern for health and quality of life, including sexual function, she said.
In the study (known as the WISP trial) the researchers compared data from 166 patients who underwent immediate removal of the fallopian tubes and ovaries and 171 who underwent fallopian tube removal and delayed oophorectomy. All patients completed questionnaires about sexual function. The primary outcome was change in sexual function based on the sexual function index (FSFI) from baseline to 6 months after surgery.
Overall, changes in sexual function were significantly greater in the immediate oophorectomy group, compared with the delayed oophorectomy group at 6 months (33% vs 17%) and also at 12 months (43% vs 20%).
A further review of patients using hormone therapy showed that those in the immediate oophorectomy group still had greater decreases in sexual function, compared with the delayed group, though the difference between groups of patients using hormone therapy was less dramatic.
“I was surprised that, even with hormone replacement therapy, patients undergoing removal of the ovaries still had significant detrimental changes to sexual function when compared to those having the tubes removed, although this was even worse in those who could not take HRT,” Dr. Norquist said, in an interview. “I was reassured that menopausal symptoms in general were well managed with HRT, as these patients did not score differently on menopause symptoms, compared with those having their tubes removed,” she said.
Patients deserve accurate information about predicted changes in menopausal symptoms and sexual function as a result of ovary removal, and HRT should be provided when there is no contraindication, Dr. Norquist told this news organization.
Dr. Norquist and colleagues are awaiting the results of clinical trials investigating the safety of salpingectomy with delayed oophorectomy in terms of ovarian cancer prevention, but more research is needed to identify optimal management of the menopausal and sexual side effects associated with surgical menopause, she noted.
“Findings from the WISP study show the importance of hormones in women undergoing prophylactic surgery,” Dr. Dizon said. The findings indicate that salpingectomy has less of a negative influence on sexual function compared to removal of the ovaries, and the impact of hormone therapy and the relatively young age of the patients who took hormones reinforces current knowledge about hormones and sex, he added.
Barriers and Solutions
Barriers to asking women with cancer about sexual issues reported by providers include limited time, lack of training in sexual health, a desire to avoid offending the patient or making them uncomfortable, and uncertainty about how to answer the questions, Dr. Lersch and Ms. Dreibelbis wrote in their presentation.
Barriers to asking healthcare providers about their sexual issues reported by patients include the beliefs that the clinician should initiate the discussion, that sexual function will not be taken seriously, and that they might make the provider uncomfortable.
“Fortunately, more information and research has been done on sexual health and gynecological cancer in recent years, so oncologists are becoming more aware of the issues women may have,” said Dr. Lersch who is an oncology nurse practitioner at Providence Franz Cancer Institute in Portland, Oregon, in an interview.
Telling patients early in their cancer treatment about potential sexual side effects and opportunities for help is essential, she added.
Although oncologists have become more aware of the importance of sexual health and well-being for their patients, “I think there has historically been a disconnect in including sexual health education in medical training,” Ms. Dreibelbis said in an interview.
Dr. Lersch and Ms. Dreibelbis advised a multidimensional approach to managing sexual problems in cancer patients that includes consideration of biological and psychological symptoms, but also social, cultural, and interpersonal factors, in their presentation.
Their suggestions include discussing dyspareunia with their patients, asking for details such as whether the pain is internal or external, whether it occurs with activities outside of sex including masturbation, and whether bleeding is present.
Oncology therapies and surgeries can decrease or eliminate an individual’s ability to produce their own lubricant; for example, removal of the cervix eliminates cervical mucous, which helps with internal lubrication, they wrote in their presentation.
For patients with dyspareunia, Dr. Lersch and Ms. Dreibelbis recommend a vaginal moisturizer especially formulated for vaginal tissue that can be absorbed by the mucosal tissue of the vagina. Use of this type of product can increase the effectiveness of lubricants and help restore integrity of the vaginal tissue. Such moisturizers are available as gels, creams, or suppositories over the counter, and do not contain hormones.
Vaginal estrogen can be helpful for burning, itching, irritation, tissue fragility, and pain with sex, according to Dr. Lersch and Ms. Dreibelbis. Adequate estrogen therapy can promote normalization of vaginal pH and microflora, as well increase vaginal secretion and reduce pain and dryness with intercourse, the presenters stated in their presentation. In addition, dilator therapy can be used to help prevent vaginal stenosis, and penetration bumpers can help relieve discomfort during intercourse, they wrote.
Looking ahead, more research is needed to serve a wider patient population, Ms. Dreibelbis said, in an interview.
“LGBTQIA [individuals] have not been included in sexual health research and there are more people than ever who identify within this group of people. I know there has also been some very early work on shielding the clitoris from the impacts of radiation, and I believe this is extremely important up-and-coming research,” she said.
Dr. Lersch, Ms. Dreibelbi, Dr. Dizon, Dr. Norquist, Ms. Brewer, and Dr. Mehta had no financial conflicts to disclose.
FROM SGO 2024
New Data: Black Women More Likely to Die From Common Endometrial Cancer Subtype
A recent analysis identified significant disparities in survival outcomes as well as clinical and genetic features between Black and White women with a common subtype of endometrial cancer.
In addition to observing differences in clinical and molecular characteristics, the analysis of real-world registries and clinical trials revealed that Black patients with endometrioid endometrial carcinoma had about a twofold higher risk for cancer-related deaths than White patients.
“Even with propensity-score matching, Black patients had a significantly increased risk of death,” Zachary Kopelman, DO, with Walter Reed National Military Medical Center, Bethesda, Maryland, noted in a presentation at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer.
Importantly, Dr. Kopelman added, the analysis also confirmed “dramatic” underrepresentation of Black patients with endometrioid endometrial carcinoma in clinical trials.
Endometrial cancer is one of the most common cancers among women in the United States, with data showing rising incidence and mortality rates. “Worryingly, endometrial cancer is estimated to overtake ovarian cancer as the deadliest gynecologic malignancy this year,” Dr. Kopelman told attendees.
Previous studies have shown that Black patients with endometrial cancer consistently are more likely to have aggressive histologic subtypes, high-grade tumors, and advanced-stage disease and are twice as likely to die from the disease as White patients, he noted.
Within endometrial cancer, the most common histologic subtype is endometrioid, comprising 65%-75% of cases. In other studies examining racial disparities, the endometrioid histology is often combined with other subtypes, such as aggressive uterine serous carcinoma, which may influence study outcomes, Dr. Kopelman explained.
Dr. Kopelman and colleagues focused their analyses on Black and White women with endometrioid endometrial carcinoma, with the goal of identifying disparities in cancer-related and non-cancer deaths, as well as clinical and molecular features in this patient population.
All women included in the analysis had undergone hysterectomy with or without adjuvant treatment. The researchers used a four-pronged approach incorporating data from the SEER program (2004-2016), the National Cancer Database (2004-2017), eight National Cancer Institute-sponsored randomized phase 3 clinical trials, and the Genomics Evidence Neoplasia Information Exchange project.
Dr. Kopelman and colleagues then performed propensity score matching in the National Cancer Database and exact matching in the randomized controlled trials.
When comparing 47,959 White patients with 4397 Black patients in the SEER dataset, Dr. Kopelman and colleagues found that Black patients had more than two times the risk of dying from their cancer (hazard ratio [HR], 2.04) and a 22% greater risk for a non-cancer death compared with White patients (HR, 1.22).
In the overall National Cancer Database cohort comparing 155,706 White and 13,468 Black patients, Black patients had a 52% greater risk of dying from any cause (HR, 1.52). In the propensity score-matched cohort of 13,468 White and 13,468 Black patients, survival among Black patients remained significantly worse, with a 29% greater risk of dying from any cause (HR, 1.29).
When looking at clinical trial data, Black patients were more likely than White patients to have worse performance status and a higher grade or recurrent disease, Dr. Kopelman noted.
Black patients in the clinical trials also had significantly worse progression-free survival in both the original cohort (HR, 2.05) and the matched cohort (adjusted HR [aHR], 1.22), which matched patients for grade, stage, and treatment arm within each trial and balanced age and performance status. Black patients also had worse overall survival in the original cohort (HR, 2.19) and matched cohort (aHR, 1.32).
Looking at molecular features, Black patients had significantly fewer mutations in a handful of cancer-related gene pathways, including PTEN, PIK3R1, FBXW7, NF1, mTOR, CCND1, and PI3K pathways.
One caveat, said Dr. Kopelman, is that mutations in PTEN are still present in a high percentage of both Black (62%) and White (72%), which «offers a potential attractive therapeutic opportunity.»
The analysis also revealed a major gap in the number of Black vs White patients enrolled in randomized clinical trials, which is a major “problem,” said Dr. Kopelman.
The study confirms “ongoing disparities in enrollment and underrepresentation of minorities in gynecologic cancer clinical trials, as well as poor outcomes, and should really promote us to enhance research in these areas,” said study discussant Mariam AlHilli, MD, with Cleveland Clinic Lerner College of Medicine and Case Western Reserve University, Cleveland, Ohio.
David M. O’Malley, MD, who gave a separate talk during the same session on practical considerations for implication of clinical trials, encouraged clinicians to “just ask.”
“Just ask the patient in front of you — no matter what their ethnicity, their race, or where they’re coming from — are they interested in participating in a clinical trial?” Or better yet, “I have a clinical trial now which I’m excited about for you,” said Dr. O’Malley, with The Ohio State University, James Comprehensive Cancer Center, Columbus, Ohio.The study had no commercial funding. Dr. Kopelman, Dr. O’Malley, and Dr. AlHilli had no relevant disclosures.
A version of this article appeared on Medscape.com .
A recent analysis identified significant disparities in survival outcomes as well as clinical and genetic features between Black and White women with a common subtype of endometrial cancer.
In addition to observing differences in clinical and molecular characteristics, the analysis of real-world registries and clinical trials revealed that Black patients with endometrioid endometrial carcinoma had about a twofold higher risk for cancer-related deaths than White patients.
“Even with propensity-score matching, Black patients had a significantly increased risk of death,” Zachary Kopelman, DO, with Walter Reed National Military Medical Center, Bethesda, Maryland, noted in a presentation at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer.
Importantly, Dr. Kopelman added, the analysis also confirmed “dramatic” underrepresentation of Black patients with endometrioid endometrial carcinoma in clinical trials.
Endometrial cancer is one of the most common cancers among women in the United States, with data showing rising incidence and mortality rates. “Worryingly, endometrial cancer is estimated to overtake ovarian cancer as the deadliest gynecologic malignancy this year,” Dr. Kopelman told attendees.
Previous studies have shown that Black patients with endometrial cancer consistently are more likely to have aggressive histologic subtypes, high-grade tumors, and advanced-stage disease and are twice as likely to die from the disease as White patients, he noted.
Within endometrial cancer, the most common histologic subtype is endometrioid, comprising 65%-75% of cases. In other studies examining racial disparities, the endometrioid histology is often combined with other subtypes, such as aggressive uterine serous carcinoma, which may influence study outcomes, Dr. Kopelman explained.
Dr. Kopelman and colleagues focused their analyses on Black and White women with endometrioid endometrial carcinoma, with the goal of identifying disparities in cancer-related and non-cancer deaths, as well as clinical and molecular features in this patient population.
All women included in the analysis had undergone hysterectomy with or without adjuvant treatment. The researchers used a four-pronged approach incorporating data from the SEER program (2004-2016), the National Cancer Database (2004-2017), eight National Cancer Institute-sponsored randomized phase 3 clinical trials, and the Genomics Evidence Neoplasia Information Exchange project.
Dr. Kopelman and colleagues then performed propensity score matching in the National Cancer Database and exact matching in the randomized controlled trials.
When comparing 47,959 White patients with 4397 Black patients in the SEER dataset, Dr. Kopelman and colleagues found that Black patients had more than two times the risk of dying from their cancer (hazard ratio [HR], 2.04) and a 22% greater risk for a non-cancer death compared with White patients (HR, 1.22).
In the overall National Cancer Database cohort comparing 155,706 White and 13,468 Black patients, Black patients had a 52% greater risk of dying from any cause (HR, 1.52). In the propensity score-matched cohort of 13,468 White and 13,468 Black patients, survival among Black patients remained significantly worse, with a 29% greater risk of dying from any cause (HR, 1.29).
When looking at clinical trial data, Black patients were more likely than White patients to have worse performance status and a higher grade or recurrent disease, Dr. Kopelman noted.
Black patients in the clinical trials also had significantly worse progression-free survival in both the original cohort (HR, 2.05) and the matched cohort (adjusted HR [aHR], 1.22), which matched patients for grade, stage, and treatment arm within each trial and balanced age and performance status. Black patients also had worse overall survival in the original cohort (HR, 2.19) and matched cohort (aHR, 1.32).
Looking at molecular features, Black patients had significantly fewer mutations in a handful of cancer-related gene pathways, including PTEN, PIK3R1, FBXW7, NF1, mTOR, CCND1, and PI3K pathways.
One caveat, said Dr. Kopelman, is that mutations in PTEN are still present in a high percentage of both Black (62%) and White (72%), which «offers a potential attractive therapeutic opportunity.»
The analysis also revealed a major gap in the number of Black vs White patients enrolled in randomized clinical trials, which is a major “problem,” said Dr. Kopelman.
The study confirms “ongoing disparities in enrollment and underrepresentation of minorities in gynecologic cancer clinical trials, as well as poor outcomes, and should really promote us to enhance research in these areas,” said study discussant Mariam AlHilli, MD, with Cleveland Clinic Lerner College of Medicine and Case Western Reserve University, Cleveland, Ohio.
David M. O’Malley, MD, who gave a separate talk during the same session on practical considerations for implication of clinical trials, encouraged clinicians to “just ask.”
“Just ask the patient in front of you — no matter what their ethnicity, their race, or where they’re coming from — are they interested in participating in a clinical trial?” Or better yet, “I have a clinical trial now which I’m excited about for you,” said Dr. O’Malley, with The Ohio State University, James Comprehensive Cancer Center, Columbus, Ohio.The study had no commercial funding. Dr. Kopelman, Dr. O’Malley, and Dr. AlHilli had no relevant disclosures.
A version of this article appeared on Medscape.com .
A recent analysis identified significant disparities in survival outcomes as well as clinical and genetic features between Black and White women with a common subtype of endometrial cancer.
In addition to observing differences in clinical and molecular characteristics, the analysis of real-world registries and clinical trials revealed that Black patients with endometrioid endometrial carcinoma had about a twofold higher risk for cancer-related deaths than White patients.
“Even with propensity-score matching, Black patients had a significantly increased risk of death,” Zachary Kopelman, DO, with Walter Reed National Military Medical Center, Bethesda, Maryland, noted in a presentation at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer.
Importantly, Dr. Kopelman added, the analysis also confirmed “dramatic” underrepresentation of Black patients with endometrioid endometrial carcinoma in clinical trials.
Endometrial cancer is one of the most common cancers among women in the United States, with data showing rising incidence and mortality rates. “Worryingly, endometrial cancer is estimated to overtake ovarian cancer as the deadliest gynecologic malignancy this year,” Dr. Kopelman told attendees.
Previous studies have shown that Black patients with endometrial cancer consistently are more likely to have aggressive histologic subtypes, high-grade tumors, and advanced-stage disease and are twice as likely to die from the disease as White patients, he noted.
Within endometrial cancer, the most common histologic subtype is endometrioid, comprising 65%-75% of cases. In other studies examining racial disparities, the endometrioid histology is often combined with other subtypes, such as aggressive uterine serous carcinoma, which may influence study outcomes, Dr. Kopelman explained.
Dr. Kopelman and colleagues focused their analyses on Black and White women with endometrioid endometrial carcinoma, with the goal of identifying disparities in cancer-related and non-cancer deaths, as well as clinical and molecular features in this patient population.
All women included in the analysis had undergone hysterectomy with or without adjuvant treatment. The researchers used a four-pronged approach incorporating data from the SEER program (2004-2016), the National Cancer Database (2004-2017), eight National Cancer Institute-sponsored randomized phase 3 clinical trials, and the Genomics Evidence Neoplasia Information Exchange project.
Dr. Kopelman and colleagues then performed propensity score matching in the National Cancer Database and exact matching in the randomized controlled trials.
When comparing 47,959 White patients with 4397 Black patients in the SEER dataset, Dr. Kopelman and colleagues found that Black patients had more than two times the risk of dying from their cancer (hazard ratio [HR], 2.04) and a 22% greater risk for a non-cancer death compared with White patients (HR, 1.22).
In the overall National Cancer Database cohort comparing 155,706 White and 13,468 Black patients, Black patients had a 52% greater risk of dying from any cause (HR, 1.52). In the propensity score-matched cohort of 13,468 White and 13,468 Black patients, survival among Black patients remained significantly worse, with a 29% greater risk of dying from any cause (HR, 1.29).
When looking at clinical trial data, Black patients were more likely than White patients to have worse performance status and a higher grade or recurrent disease, Dr. Kopelman noted.
Black patients in the clinical trials also had significantly worse progression-free survival in both the original cohort (HR, 2.05) and the matched cohort (adjusted HR [aHR], 1.22), which matched patients for grade, stage, and treatment arm within each trial and balanced age and performance status. Black patients also had worse overall survival in the original cohort (HR, 2.19) and matched cohort (aHR, 1.32).
Looking at molecular features, Black patients had significantly fewer mutations in a handful of cancer-related gene pathways, including PTEN, PIK3R1, FBXW7, NF1, mTOR, CCND1, and PI3K pathways.
One caveat, said Dr. Kopelman, is that mutations in PTEN are still present in a high percentage of both Black (62%) and White (72%), which «offers a potential attractive therapeutic opportunity.»
The analysis also revealed a major gap in the number of Black vs White patients enrolled in randomized clinical trials, which is a major “problem,” said Dr. Kopelman.
The study confirms “ongoing disparities in enrollment and underrepresentation of minorities in gynecologic cancer clinical trials, as well as poor outcomes, and should really promote us to enhance research in these areas,” said study discussant Mariam AlHilli, MD, with Cleveland Clinic Lerner College of Medicine and Case Western Reserve University, Cleveland, Ohio.
David M. O’Malley, MD, who gave a separate talk during the same session on practical considerations for implication of clinical trials, encouraged clinicians to “just ask.”
“Just ask the patient in front of you — no matter what their ethnicity, their race, or where they’re coming from — are they interested in participating in a clinical trial?” Or better yet, “I have a clinical trial now which I’m excited about for you,” said Dr. O’Malley, with The Ohio State University, James Comprehensive Cancer Center, Columbus, Ohio.The study had no commercial funding. Dr. Kopelman, Dr. O’Malley, and Dr. AlHilli had no relevant disclosures.
A version of this article appeared on Medscape.com .
FROM SGO 2024
Minimally Invasive Cytoreductive Approach Comparable to Open Surgery for Ovarian Cancer
This was a finding of a retrospective study presented by Judy Hayek, MD, during an oral abstract session at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer, in San Diego.
Among 2,412 women in the National Cancer Database with tumor-free surgical margins (R0 resections) after interval debulking surgery (IDS), the median overall survival (OS) was 46 months for those who had undergone an open procedure or minimally invasive surgery (MIS) that was converted to an open procedure. In contrast, the median OS was 51 months for patients who underwent laparoscopic or robot-assisted minimally invasive surgery, reported Dr. Hayek, a gynecologic oncology fellow at SUNY Downstate Health Sciences University in Brooklyn, New York.
“R0 resection at the time of interval debulking surgery has similar survival outcomes by minimally invasive surgery versus laparotomy, while R0 resection via laparotomy is associated with higher perioperative mortality. There is no interaction between the extent of surgery and the impact of MIS on survival,” she said during her presentation.
The session included a debate on the pros and cons of minimally invasive vs. open surgery in this population.
Growing Use of MIS
Over the last decade, minimally invasive surgery for interval debulking was shown to be safe and feasible. More recently, two studies using National Cancer Database cohorts showed that survival was similar and perioperative outcomes were better with a minimally invasive approach at the time of IDS for patients with early disease, Dr. Hayek said (Obstet Gynecol 2017 Jul;130(1):71-79; and Gynecol Oncol 2023 May:172:130-137).
Potential limitations of MIS include the absence of haptic feedback compared with open surgery, and the possibility that limited visualization of the surgical field could lead to missed residual disease and subsequent poor outcomes for patients who were presumed to have complete gross resections, she said.
Outcomes Compared
Dr. Hayek and colleagues conducted their study to evaluate survival outcomes after R0 resections by MIS or laparotomy in IDS for patients with advanced epithelial ovarian cancer.
As noted before, they looked at outcomes for 2,412 women with stage IIIC or IV cancers of all histology types who were diagnosed from 2010 through 2019. A total of 624 patients (25.9%) had minimally invasive procedures, and 1,788 (74.1%) had open surgery or MIS that had been converted to open procedures.
Of the minimally invasive procedures, 48.7% were robot-assisted, and the remainder were laparoscopic.
Over the decade of the study, the frequency of minimally invasive surgery steadily increased, from 11.9% of all procedures in 2010 to 36.5% in 2019.
Also as noted, there was no difference in median overall survival, at 46 months for open/converted procedures vs. 51 months for minimally invasive procedures.
As might be expected, the mean length of stay was shorter with the less invasive surgery: 3.3 days compared with 5.3 days with open surgery (P less than .001). In addition, 30-day and 90-day mortality rates were also lower with MIS, at 0.8% and 1.9%, respectively, compared with 1.6% and 3.5% with laparotomy (P = .006 for 30-day mortality, and .003 for 90-day).
There were also no differences in overall survival between the procedure types when the cases were stratified according to extent of surgery. Within the minimally invasive surgery groups there were no differences in median OS for patients whose surgery was performed laparoscopically or with robotic assistance.
The study was limited by a lack of data on either patient-specific tumor burden, neoadjuvant chemotherapy use, progression-free survival, cause of death, or surgical morbidity, Dr. Hayek acknowledged.
MIS Use Debatable: CON
Despite the good outcomes with minimally invasive techniques in this favorable-risk population, critics contend that MIS interval cytoreduction is too risky in the majority of cases.
In the debate portion of the session, Kara Long Roche, MD, an associate attending in the section of ovarian cancer surgery at Memorial Sloan Kettering Cancer Center in New York, argued that the potential for MIS missing residual disease is too great.
“We know from almost every retrospective and prospective study done that the volume of residual disease after debulking, whether primary or interval, is the most important prognostic factor for our patients that we can modify,” she said.
Rather than debating morbidity, mortality, or criteria for resection, “I would argue that the question we need to debate is can MIS interval debulking achieve a completeness of resection, i.e., volume of residual disease?” she said.
Dr. Roche contended that retrospective studies such as that reported by Dr. Hayek cannot adequately answer this question because of selection bias. Patients selected for MIS have better responses to neoadjuvant chemotherapy and more favorable tumor biology; and, therefore, overall survival may not be the optimal endpoint for retrospective studies.
In addition, neoadjuvant chemotherapy does not automatically preclude the need for extensive upper abdominal surgery since almost half of patients who receive neoadjuvant chemotherapy are found to have bulky upper abdominal disease at the time of debulking.
Dr. Roche especially cautioned against what she called the WNL or “We Never Looked” phenomenon, in which patients are found on open surgery and organ mobilization to have disease that was not evident on presurgical imaging.
She acknowledged that for some patients the risks of laparotomy are likely to outweigh the benefit of a radical resection, and stressed that for such patients forgoing surgery or optimizing perioperative care may be more important than the size of the incision.
MIS IDS should be the exception, not the rule. We need prospective data with appropriate endpoints. We need surgical quality control in both arms, and we need to continue to focus on surgical education and training so that our trainees can graduate doing these procedures via any approach,” she concluded.
Debate: PRO
Arguing in favor of MIS for ovarian cancer, J. Alejandro Rauh-Hain, MD, MPH, associate professor of gynecologic oncology at the University of Texas MD Anderson Cancer Center in Houston, told attendees “the only bias I have is that I actually love doing open surgery, but I’m going to try to convince you that there is a potential role for minimally invasive surgery in the future for selected patients with ovarian cancer after neoadjuvant chemotherapy.”
He noted that several studies have convincingly shown that neoadjuvant chemotherapy does not adversely affect oncologic outcomes for patients with advanced-stage ovarian cancer, and decreases perioperative morbidity in patients who receive it, including reductions in serious adverse events, risk of stoma, and 30-day postoperative mortality.
In addition, low use of neoadjuvant chemotherapy is associated with increased risks for 90-day postoperative deaths in both low- and high surgical volume centers in the US, according to unpublished National Cancer Database data.
Dr. Rauh-Hain noted that neoadjuvant chemotherapy use has steadily increased from 2010 through 2020, and added that in 2022, 32% of interval cytoreductive surgeries in the United States were performed with a minimally invasive approach.
To get a better handle on the MIS vs. open-surgery question, Dr. Rauh-Hain and colleagues at MD Anderson and 13 other centers in the United States, Canada, and Europe are currently recruiting patients for the Laparoscopic Cytoreduction After Neoadjuvant Chemotherapy (LANCE) trial. In this phase 3 noninferiority study, patients with stage IIIC-IV ovarian, primary peritoneal, or fallopian tube cancer who have complete or partial responses and CA125 normalization after three or four cycles of neoadjuvant chemotherapy will be randomized to laparotomy or MIS, followed by adjuvant platinum- and taxane-based chemotherapy.
The study by Hayek et al. was internally supported. Dr. Hayek and Dr. Roche reported having no conflicts of interest. Dr. Rauh-Hain disclosed financial relationships with Guidepoint Consulting, and the Schlesinger Group.
This was a finding of a retrospective study presented by Judy Hayek, MD, during an oral abstract session at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer, in San Diego.
Among 2,412 women in the National Cancer Database with tumor-free surgical margins (R0 resections) after interval debulking surgery (IDS), the median overall survival (OS) was 46 months for those who had undergone an open procedure or minimally invasive surgery (MIS) that was converted to an open procedure. In contrast, the median OS was 51 months for patients who underwent laparoscopic or robot-assisted minimally invasive surgery, reported Dr. Hayek, a gynecologic oncology fellow at SUNY Downstate Health Sciences University in Brooklyn, New York.
“R0 resection at the time of interval debulking surgery has similar survival outcomes by minimally invasive surgery versus laparotomy, while R0 resection via laparotomy is associated with higher perioperative mortality. There is no interaction between the extent of surgery and the impact of MIS on survival,” she said during her presentation.
The session included a debate on the pros and cons of minimally invasive vs. open surgery in this population.
Growing Use of MIS
Over the last decade, minimally invasive surgery for interval debulking was shown to be safe and feasible. More recently, two studies using National Cancer Database cohorts showed that survival was similar and perioperative outcomes were better with a minimally invasive approach at the time of IDS for patients with early disease, Dr. Hayek said (Obstet Gynecol 2017 Jul;130(1):71-79; and Gynecol Oncol 2023 May:172:130-137).
Potential limitations of MIS include the absence of haptic feedback compared with open surgery, and the possibility that limited visualization of the surgical field could lead to missed residual disease and subsequent poor outcomes for patients who were presumed to have complete gross resections, she said.
Outcomes Compared
Dr. Hayek and colleagues conducted their study to evaluate survival outcomes after R0 resections by MIS or laparotomy in IDS for patients with advanced epithelial ovarian cancer.
As noted before, they looked at outcomes for 2,412 women with stage IIIC or IV cancers of all histology types who were diagnosed from 2010 through 2019. A total of 624 patients (25.9%) had minimally invasive procedures, and 1,788 (74.1%) had open surgery or MIS that had been converted to open procedures.
Of the minimally invasive procedures, 48.7% were robot-assisted, and the remainder were laparoscopic.
Over the decade of the study, the frequency of minimally invasive surgery steadily increased, from 11.9% of all procedures in 2010 to 36.5% in 2019.
Also as noted, there was no difference in median overall survival, at 46 months for open/converted procedures vs. 51 months for minimally invasive procedures.
As might be expected, the mean length of stay was shorter with the less invasive surgery: 3.3 days compared with 5.3 days with open surgery (P less than .001). In addition, 30-day and 90-day mortality rates were also lower with MIS, at 0.8% and 1.9%, respectively, compared with 1.6% and 3.5% with laparotomy (P = .006 for 30-day mortality, and .003 for 90-day).
There were also no differences in overall survival between the procedure types when the cases were stratified according to extent of surgery. Within the minimally invasive surgery groups there were no differences in median OS for patients whose surgery was performed laparoscopically or with robotic assistance.
The study was limited by a lack of data on either patient-specific tumor burden, neoadjuvant chemotherapy use, progression-free survival, cause of death, or surgical morbidity, Dr. Hayek acknowledged.
MIS Use Debatable: CON
Despite the good outcomes with minimally invasive techniques in this favorable-risk population, critics contend that MIS interval cytoreduction is too risky in the majority of cases.
In the debate portion of the session, Kara Long Roche, MD, an associate attending in the section of ovarian cancer surgery at Memorial Sloan Kettering Cancer Center in New York, argued that the potential for MIS missing residual disease is too great.
“We know from almost every retrospective and prospective study done that the volume of residual disease after debulking, whether primary or interval, is the most important prognostic factor for our patients that we can modify,” she said.
Rather than debating morbidity, mortality, or criteria for resection, “I would argue that the question we need to debate is can MIS interval debulking achieve a completeness of resection, i.e., volume of residual disease?” she said.
Dr. Roche contended that retrospective studies such as that reported by Dr. Hayek cannot adequately answer this question because of selection bias. Patients selected for MIS have better responses to neoadjuvant chemotherapy and more favorable tumor biology; and, therefore, overall survival may not be the optimal endpoint for retrospective studies.
In addition, neoadjuvant chemotherapy does not automatically preclude the need for extensive upper abdominal surgery since almost half of patients who receive neoadjuvant chemotherapy are found to have bulky upper abdominal disease at the time of debulking.
Dr. Roche especially cautioned against what she called the WNL or “We Never Looked” phenomenon, in which patients are found on open surgery and organ mobilization to have disease that was not evident on presurgical imaging.
She acknowledged that for some patients the risks of laparotomy are likely to outweigh the benefit of a radical resection, and stressed that for such patients forgoing surgery or optimizing perioperative care may be more important than the size of the incision.
MIS IDS should be the exception, not the rule. We need prospective data with appropriate endpoints. We need surgical quality control in both arms, and we need to continue to focus on surgical education and training so that our trainees can graduate doing these procedures via any approach,” she concluded.
Debate: PRO
Arguing in favor of MIS for ovarian cancer, J. Alejandro Rauh-Hain, MD, MPH, associate professor of gynecologic oncology at the University of Texas MD Anderson Cancer Center in Houston, told attendees “the only bias I have is that I actually love doing open surgery, but I’m going to try to convince you that there is a potential role for minimally invasive surgery in the future for selected patients with ovarian cancer after neoadjuvant chemotherapy.”
He noted that several studies have convincingly shown that neoadjuvant chemotherapy does not adversely affect oncologic outcomes for patients with advanced-stage ovarian cancer, and decreases perioperative morbidity in patients who receive it, including reductions in serious adverse events, risk of stoma, and 30-day postoperative mortality.
In addition, low use of neoadjuvant chemotherapy is associated with increased risks for 90-day postoperative deaths in both low- and high surgical volume centers in the US, according to unpublished National Cancer Database data.
Dr. Rauh-Hain noted that neoadjuvant chemotherapy use has steadily increased from 2010 through 2020, and added that in 2022, 32% of interval cytoreductive surgeries in the United States were performed with a minimally invasive approach.
To get a better handle on the MIS vs. open-surgery question, Dr. Rauh-Hain and colleagues at MD Anderson and 13 other centers in the United States, Canada, and Europe are currently recruiting patients for the Laparoscopic Cytoreduction After Neoadjuvant Chemotherapy (LANCE) trial. In this phase 3 noninferiority study, patients with stage IIIC-IV ovarian, primary peritoneal, or fallopian tube cancer who have complete or partial responses and CA125 normalization after three or four cycles of neoadjuvant chemotherapy will be randomized to laparotomy or MIS, followed by adjuvant platinum- and taxane-based chemotherapy.
The study by Hayek et al. was internally supported. Dr. Hayek and Dr. Roche reported having no conflicts of interest. Dr. Rauh-Hain disclosed financial relationships with Guidepoint Consulting, and the Schlesinger Group.
This was a finding of a retrospective study presented by Judy Hayek, MD, during an oral abstract session at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer, in San Diego.
Among 2,412 women in the National Cancer Database with tumor-free surgical margins (R0 resections) after interval debulking surgery (IDS), the median overall survival (OS) was 46 months for those who had undergone an open procedure or minimally invasive surgery (MIS) that was converted to an open procedure. In contrast, the median OS was 51 months for patients who underwent laparoscopic or robot-assisted minimally invasive surgery, reported Dr. Hayek, a gynecologic oncology fellow at SUNY Downstate Health Sciences University in Brooklyn, New York.
“R0 resection at the time of interval debulking surgery has similar survival outcomes by minimally invasive surgery versus laparotomy, while R0 resection via laparotomy is associated with higher perioperative mortality. There is no interaction between the extent of surgery and the impact of MIS on survival,” she said during her presentation.
The session included a debate on the pros and cons of minimally invasive vs. open surgery in this population.
Growing Use of MIS
Over the last decade, minimally invasive surgery for interval debulking was shown to be safe and feasible. More recently, two studies using National Cancer Database cohorts showed that survival was similar and perioperative outcomes were better with a minimally invasive approach at the time of IDS for patients with early disease, Dr. Hayek said (Obstet Gynecol 2017 Jul;130(1):71-79; and Gynecol Oncol 2023 May:172:130-137).
Potential limitations of MIS include the absence of haptic feedback compared with open surgery, and the possibility that limited visualization of the surgical field could lead to missed residual disease and subsequent poor outcomes for patients who were presumed to have complete gross resections, she said.
Outcomes Compared
Dr. Hayek and colleagues conducted their study to evaluate survival outcomes after R0 resections by MIS or laparotomy in IDS for patients with advanced epithelial ovarian cancer.
As noted before, they looked at outcomes for 2,412 women with stage IIIC or IV cancers of all histology types who were diagnosed from 2010 through 2019. A total of 624 patients (25.9%) had minimally invasive procedures, and 1,788 (74.1%) had open surgery or MIS that had been converted to open procedures.
Of the minimally invasive procedures, 48.7% were robot-assisted, and the remainder were laparoscopic.
Over the decade of the study, the frequency of minimally invasive surgery steadily increased, from 11.9% of all procedures in 2010 to 36.5% in 2019.
Also as noted, there was no difference in median overall survival, at 46 months for open/converted procedures vs. 51 months for minimally invasive procedures.
As might be expected, the mean length of stay was shorter with the less invasive surgery: 3.3 days compared with 5.3 days with open surgery (P less than .001). In addition, 30-day and 90-day mortality rates were also lower with MIS, at 0.8% and 1.9%, respectively, compared with 1.6% and 3.5% with laparotomy (P = .006 for 30-day mortality, and .003 for 90-day).
There were also no differences in overall survival between the procedure types when the cases were stratified according to extent of surgery. Within the minimally invasive surgery groups there were no differences in median OS for patients whose surgery was performed laparoscopically or with robotic assistance.
The study was limited by a lack of data on either patient-specific tumor burden, neoadjuvant chemotherapy use, progression-free survival, cause of death, or surgical morbidity, Dr. Hayek acknowledged.
MIS Use Debatable: CON
Despite the good outcomes with minimally invasive techniques in this favorable-risk population, critics contend that MIS interval cytoreduction is too risky in the majority of cases.
In the debate portion of the session, Kara Long Roche, MD, an associate attending in the section of ovarian cancer surgery at Memorial Sloan Kettering Cancer Center in New York, argued that the potential for MIS missing residual disease is too great.
“We know from almost every retrospective and prospective study done that the volume of residual disease after debulking, whether primary or interval, is the most important prognostic factor for our patients that we can modify,” she said.
Rather than debating morbidity, mortality, or criteria for resection, “I would argue that the question we need to debate is can MIS interval debulking achieve a completeness of resection, i.e., volume of residual disease?” she said.
Dr. Roche contended that retrospective studies such as that reported by Dr. Hayek cannot adequately answer this question because of selection bias. Patients selected for MIS have better responses to neoadjuvant chemotherapy and more favorable tumor biology; and, therefore, overall survival may not be the optimal endpoint for retrospective studies.
In addition, neoadjuvant chemotherapy does not automatically preclude the need for extensive upper abdominal surgery since almost half of patients who receive neoadjuvant chemotherapy are found to have bulky upper abdominal disease at the time of debulking.
Dr. Roche especially cautioned against what she called the WNL or “We Never Looked” phenomenon, in which patients are found on open surgery and organ mobilization to have disease that was not evident on presurgical imaging.
She acknowledged that for some patients the risks of laparotomy are likely to outweigh the benefit of a radical resection, and stressed that for such patients forgoing surgery or optimizing perioperative care may be more important than the size of the incision.
MIS IDS should be the exception, not the rule. We need prospective data with appropriate endpoints. We need surgical quality control in both arms, and we need to continue to focus on surgical education and training so that our trainees can graduate doing these procedures via any approach,” she concluded.
Debate: PRO
Arguing in favor of MIS for ovarian cancer, J. Alejandro Rauh-Hain, MD, MPH, associate professor of gynecologic oncology at the University of Texas MD Anderson Cancer Center in Houston, told attendees “the only bias I have is that I actually love doing open surgery, but I’m going to try to convince you that there is a potential role for minimally invasive surgery in the future for selected patients with ovarian cancer after neoadjuvant chemotherapy.”
He noted that several studies have convincingly shown that neoadjuvant chemotherapy does not adversely affect oncologic outcomes for patients with advanced-stage ovarian cancer, and decreases perioperative morbidity in patients who receive it, including reductions in serious adverse events, risk of stoma, and 30-day postoperative mortality.
In addition, low use of neoadjuvant chemotherapy is associated with increased risks for 90-day postoperative deaths in both low- and high surgical volume centers in the US, according to unpublished National Cancer Database data.
Dr. Rauh-Hain noted that neoadjuvant chemotherapy use has steadily increased from 2010 through 2020, and added that in 2022, 32% of interval cytoreductive surgeries in the United States were performed with a minimally invasive approach.
To get a better handle on the MIS vs. open-surgery question, Dr. Rauh-Hain and colleagues at MD Anderson and 13 other centers in the United States, Canada, and Europe are currently recruiting patients for the Laparoscopic Cytoreduction After Neoadjuvant Chemotherapy (LANCE) trial. In this phase 3 noninferiority study, patients with stage IIIC-IV ovarian, primary peritoneal, or fallopian tube cancer who have complete or partial responses and CA125 normalization after three or four cycles of neoadjuvant chemotherapy will be randomized to laparotomy or MIS, followed by adjuvant platinum- and taxane-based chemotherapy.
The study by Hayek et al. was internally supported. Dr. Hayek and Dr. Roche reported having no conflicts of interest. Dr. Rauh-Hain disclosed financial relationships with Guidepoint Consulting, and the Schlesinger Group.
FROM SGO 2024
Therapeutic HPV16 vaccine clears virus in most patients with CIN
The vaccine, pNGVL4a-CRTE6E7L2, also showed signs of efficacy in patients living with HIV, reported Kimberly Lynn Levinson, MD, MPH, associate professor of obstetrics and gynecology at Johns Hopkins Medicine in Baltimore.
“We demonstrated a 78% rate of clearance for both histologic regression and HPV16, with some clearance of other HPV types,” she said in an oral abstract presentation at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer, held in San Diego.
Further evaluation of the vaccine in vulvar, vaginal, and other tissue types is required, and evaluation of immune response at the local and systemic is ongoing, Dr. Levinson said.
In contrast to HPV16 prophylactic vaccines, which form an antibody-specific response to HPV, therapeutic vaccines elicit a cell-mediated immunity, primarily focusing on the virus’ E6 and E7 proteins.
There are currently only three Food and Drug Administration–approved therapeutic vaccines for cancer, but none are as yet approved for treatment of gynecologic malignancies.
According to the US National Institutes of Health, there are multiple therapeutic HPV vaccines in development using either vector-based, peptide and protein-based, or nucleic-acid based approaches, or whole cell (dendritic cell) approaches.
Current Study
Dr. Levinson noted that “DNA vaccines are both well tolerated and simple to produce, and the addition of calreticulin enhances immune response.”
The investigational vaccine is delivered via an electoporation device (TriGrid delivery system) that stimulates muscle at the injection site to produce an enhanced immune response.
In preclinical studies the device was associated with an enhanced immune response compared with standard intramuscular injection. The enhance immune effect persisted despite CD4 T cell depletion.
The investigators conducted a phase 1 dose-escalation study, administering the vaccine to two separate cohorts: women without HIV who had HPV16-positive cervical dysplasia (CIN 2/3) and women living with HIV with HPV16-positive cervical or vulvovaginal dysplasia (CIN 2/3, VIN 2/3 or VAIN 2/3).
The vaccine was delivered at weeks 0, 4, and 8, at doses of 0.3 mg, 1.0 mg, or 3.0 mg. At week 12, all patients underwent site-specific biopsy to verify non-progression.
At 6 months, the patients then underwent definitive treatment with either loop electro excision or vulvar/vaginal excision. At 12 months, all patients had standard evaluations with biopsies.
Dr. Levinson reported results for the first 14 women enrolled, 10 of whom were HIV-negative and 4 of whom were HIV-positive.
Of nine women in the HIV-negative arm who had completed 6-month visits and were evaluable, two had HPV16 clearance by 2-month follow-up, and seven had clearance at 6 months. Other HPV subtypes cleared in two of five patients at 3 months and in three of five at 6 months.
In addition, seven of nine patients in this arm had histologic regression at 6 months.
In the HIV-positive arm, the two patients with CIN had no HPV16 clearance at 3 months, but both had clearance at 16 months. The vaccine did not clear other HPV subtypes in these patients, however.
Of the two women in this arm who had VIN, one had HPV16 clearance and histologic regression at 6 months. The other patient had neither viral clearance nor histologic regression.
All participants tolerated each vaccine well. Adverse events were all grade 1 in severity and resolved within 4 weeks. The most common event was tenderness at the injection site. There were also three cases of mild headache, two cases of drowsiness, and one of nausea.
What’s Next?
In the question-and-answer session following the presentation, Ronald D. Alvarez, MD, MBA, chairman and clinical service chief of obstetrics and gynecology at Vanderbilt University Medical Center in Nashville, Tennessee, asked Dr. Levinson how the vaccine development will proceed.
“Obviously, you have more data to collect and analyze, but how are you going to move forward with what looks like equal efficacy between the 1 milligram and the 3 milligram doses? Are you just going to go with the maximum tolerated dose, or consider a lower dose if it shows equal efficacy in terms of histologic regression as well as HPV clearance?” he asked.
“This is something we’re very interested in, and we do plan for the dose-expansion phase to go with the higher dose,” Dr. Levinson replied. “We need to evaluate it further and we may need to do further randomization between the medium dose and the highest dose to determine if there are differences both with systemic and local responses.”
Robert DeBernardo, MD, section head of obstetrics and gynecology and the Women’s Health Institute at the Cleveland Clinic, asked whether Dr. Levinson and colleagues were considering evaluating the vaccine in transplant recipients, “because we have a lot of persistent HPV in that subgroup.”
Dr. Levinson said that one of the dose-expansion cohorts for further study is a population of patients scheduled for transplantation.
“What we’re interested in is looking at whether we can ‘cure’ HPV prior to transplantation, and we think that’s going to be the best way to show that this vaccine potentially eliminates the virus, because if we can eliminate the virus and then take a population that’s going to be immunodeficient, then that would show that there’s no reactivation of the virus,” she said.
The study is supported by the National Institutes of Health. Dr. Levinson, Dr. Alvarez, and Dr. DeBernardo had no conflicts of interest to report.
The vaccine, pNGVL4a-CRTE6E7L2, also showed signs of efficacy in patients living with HIV, reported Kimberly Lynn Levinson, MD, MPH, associate professor of obstetrics and gynecology at Johns Hopkins Medicine in Baltimore.
“We demonstrated a 78% rate of clearance for both histologic regression and HPV16, with some clearance of other HPV types,” she said in an oral abstract presentation at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer, held in San Diego.
Further evaluation of the vaccine in vulvar, vaginal, and other tissue types is required, and evaluation of immune response at the local and systemic is ongoing, Dr. Levinson said.
In contrast to HPV16 prophylactic vaccines, which form an antibody-specific response to HPV, therapeutic vaccines elicit a cell-mediated immunity, primarily focusing on the virus’ E6 and E7 proteins.
There are currently only three Food and Drug Administration–approved therapeutic vaccines for cancer, but none are as yet approved for treatment of gynecologic malignancies.
According to the US National Institutes of Health, there are multiple therapeutic HPV vaccines in development using either vector-based, peptide and protein-based, or nucleic-acid based approaches, or whole cell (dendritic cell) approaches.
Current Study
Dr. Levinson noted that “DNA vaccines are both well tolerated and simple to produce, and the addition of calreticulin enhances immune response.”
The investigational vaccine is delivered via an electoporation device (TriGrid delivery system) that stimulates muscle at the injection site to produce an enhanced immune response.
In preclinical studies the device was associated with an enhanced immune response compared with standard intramuscular injection. The enhance immune effect persisted despite CD4 T cell depletion.
The investigators conducted a phase 1 dose-escalation study, administering the vaccine to two separate cohorts: women without HIV who had HPV16-positive cervical dysplasia (CIN 2/3) and women living with HIV with HPV16-positive cervical or vulvovaginal dysplasia (CIN 2/3, VIN 2/3 or VAIN 2/3).
The vaccine was delivered at weeks 0, 4, and 8, at doses of 0.3 mg, 1.0 mg, or 3.0 mg. At week 12, all patients underwent site-specific biopsy to verify non-progression.
At 6 months, the patients then underwent definitive treatment with either loop electro excision or vulvar/vaginal excision. At 12 months, all patients had standard evaluations with biopsies.
Dr. Levinson reported results for the first 14 women enrolled, 10 of whom were HIV-negative and 4 of whom were HIV-positive.
Of nine women in the HIV-negative arm who had completed 6-month visits and were evaluable, two had HPV16 clearance by 2-month follow-up, and seven had clearance at 6 months. Other HPV subtypes cleared in two of five patients at 3 months and in three of five at 6 months.
In addition, seven of nine patients in this arm had histologic regression at 6 months.
In the HIV-positive arm, the two patients with CIN had no HPV16 clearance at 3 months, but both had clearance at 16 months. The vaccine did not clear other HPV subtypes in these patients, however.
Of the two women in this arm who had VIN, one had HPV16 clearance and histologic regression at 6 months. The other patient had neither viral clearance nor histologic regression.
All participants tolerated each vaccine well. Adverse events were all grade 1 in severity and resolved within 4 weeks. The most common event was tenderness at the injection site. There were also three cases of mild headache, two cases of drowsiness, and one of nausea.
What’s Next?
In the question-and-answer session following the presentation, Ronald D. Alvarez, MD, MBA, chairman and clinical service chief of obstetrics and gynecology at Vanderbilt University Medical Center in Nashville, Tennessee, asked Dr. Levinson how the vaccine development will proceed.
“Obviously, you have more data to collect and analyze, but how are you going to move forward with what looks like equal efficacy between the 1 milligram and the 3 milligram doses? Are you just going to go with the maximum tolerated dose, or consider a lower dose if it shows equal efficacy in terms of histologic regression as well as HPV clearance?” he asked.
“This is something we’re very interested in, and we do plan for the dose-expansion phase to go with the higher dose,” Dr. Levinson replied. “We need to evaluate it further and we may need to do further randomization between the medium dose and the highest dose to determine if there are differences both with systemic and local responses.”
Robert DeBernardo, MD, section head of obstetrics and gynecology and the Women’s Health Institute at the Cleveland Clinic, asked whether Dr. Levinson and colleagues were considering evaluating the vaccine in transplant recipients, “because we have a lot of persistent HPV in that subgroup.”
Dr. Levinson said that one of the dose-expansion cohorts for further study is a population of patients scheduled for transplantation.
“What we’re interested in is looking at whether we can ‘cure’ HPV prior to transplantation, and we think that’s going to be the best way to show that this vaccine potentially eliminates the virus, because if we can eliminate the virus and then take a population that’s going to be immunodeficient, then that would show that there’s no reactivation of the virus,” she said.
The study is supported by the National Institutes of Health. Dr. Levinson, Dr. Alvarez, and Dr. DeBernardo had no conflicts of interest to report.
The vaccine, pNGVL4a-CRTE6E7L2, also showed signs of efficacy in patients living with HIV, reported Kimberly Lynn Levinson, MD, MPH, associate professor of obstetrics and gynecology at Johns Hopkins Medicine in Baltimore.
“We demonstrated a 78% rate of clearance for both histologic regression and HPV16, with some clearance of other HPV types,” she said in an oral abstract presentation at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer, held in San Diego.
Further evaluation of the vaccine in vulvar, vaginal, and other tissue types is required, and evaluation of immune response at the local and systemic is ongoing, Dr. Levinson said.
In contrast to HPV16 prophylactic vaccines, which form an antibody-specific response to HPV, therapeutic vaccines elicit a cell-mediated immunity, primarily focusing on the virus’ E6 and E7 proteins.
There are currently only three Food and Drug Administration–approved therapeutic vaccines for cancer, but none are as yet approved for treatment of gynecologic malignancies.
According to the US National Institutes of Health, there are multiple therapeutic HPV vaccines in development using either vector-based, peptide and protein-based, or nucleic-acid based approaches, or whole cell (dendritic cell) approaches.
Current Study
Dr. Levinson noted that “DNA vaccines are both well tolerated and simple to produce, and the addition of calreticulin enhances immune response.”
The investigational vaccine is delivered via an electoporation device (TriGrid delivery system) that stimulates muscle at the injection site to produce an enhanced immune response.
In preclinical studies the device was associated with an enhanced immune response compared with standard intramuscular injection. The enhance immune effect persisted despite CD4 T cell depletion.
The investigators conducted a phase 1 dose-escalation study, administering the vaccine to two separate cohorts: women without HIV who had HPV16-positive cervical dysplasia (CIN 2/3) and women living with HIV with HPV16-positive cervical or vulvovaginal dysplasia (CIN 2/3, VIN 2/3 or VAIN 2/3).
The vaccine was delivered at weeks 0, 4, and 8, at doses of 0.3 mg, 1.0 mg, or 3.0 mg. At week 12, all patients underwent site-specific biopsy to verify non-progression.
At 6 months, the patients then underwent definitive treatment with either loop electro excision or vulvar/vaginal excision. At 12 months, all patients had standard evaluations with biopsies.
Dr. Levinson reported results for the first 14 women enrolled, 10 of whom were HIV-negative and 4 of whom were HIV-positive.
Of nine women in the HIV-negative arm who had completed 6-month visits and were evaluable, two had HPV16 clearance by 2-month follow-up, and seven had clearance at 6 months. Other HPV subtypes cleared in two of five patients at 3 months and in three of five at 6 months.
In addition, seven of nine patients in this arm had histologic regression at 6 months.
In the HIV-positive arm, the two patients with CIN had no HPV16 clearance at 3 months, but both had clearance at 16 months. The vaccine did not clear other HPV subtypes in these patients, however.
Of the two women in this arm who had VIN, one had HPV16 clearance and histologic regression at 6 months. The other patient had neither viral clearance nor histologic regression.
All participants tolerated each vaccine well. Adverse events were all grade 1 in severity and resolved within 4 weeks. The most common event was tenderness at the injection site. There were also three cases of mild headache, two cases of drowsiness, and one of nausea.
What’s Next?
In the question-and-answer session following the presentation, Ronald D. Alvarez, MD, MBA, chairman and clinical service chief of obstetrics and gynecology at Vanderbilt University Medical Center in Nashville, Tennessee, asked Dr. Levinson how the vaccine development will proceed.
“Obviously, you have more data to collect and analyze, but how are you going to move forward with what looks like equal efficacy between the 1 milligram and the 3 milligram doses? Are you just going to go with the maximum tolerated dose, or consider a lower dose if it shows equal efficacy in terms of histologic regression as well as HPV clearance?” he asked.
“This is something we’re very interested in, and we do plan for the dose-expansion phase to go with the higher dose,” Dr. Levinson replied. “We need to evaluate it further and we may need to do further randomization between the medium dose and the highest dose to determine if there are differences both with systemic and local responses.”
Robert DeBernardo, MD, section head of obstetrics and gynecology and the Women’s Health Institute at the Cleveland Clinic, asked whether Dr. Levinson and colleagues were considering evaluating the vaccine in transplant recipients, “because we have a lot of persistent HPV in that subgroup.”
Dr. Levinson said that one of the dose-expansion cohorts for further study is a population of patients scheduled for transplantation.
“What we’re interested in is looking at whether we can ‘cure’ HPV prior to transplantation, and we think that’s going to be the best way to show that this vaccine potentially eliminates the virus, because if we can eliminate the virus and then take a population that’s going to be immunodeficient, then that would show that there’s no reactivation of the virus,” she said.
The study is supported by the National Institutes of Health. Dr. Levinson, Dr. Alvarez, and Dr. DeBernardo had no conflicts of interest to report.
FROM SGO 2024
ctDNA May Predict Early Response to Radiation of Gynecologic Cancers
Among 15 patients with vulvar, cervical, or endometrial malignancies who had serum ctDNA draws prior to, during, and after radiation therapy (RT) or chemoradiotherapy (CRT), both persistence or clearance of residual ctDNA were prognostic of patient outcomes from 3 to 6 months after the end of radiation therapy, reported A. Gabriella Wernicke, MD, MSc, a radiation oncologist at Lenox Hill Hospital in New York City.
“Our early findings in this limited cohort suggest that a mid-treatment ctDNA draw identified responders to radiation, and that may potentially serve as an early predictive biomarker of response. And clearly, these findings need to be validated in a prospective manner, a trial which will be starting in our center soon,” she said in an oral abstract session at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer, held in San Diego, California.
Gynecologic malignancies are challenging to manage with radiotherapy because of the treatment’s toxicities and because outcomes may not be known until several months after the end of therapy. Early identification of responses to radiation therapy with simple blood draws has the potential to help clinicians identify those patients whose tumors are responding to radiation early in the course of therapy, she said.
Correlating treatment with responses
Dr. Wernicke and colleagues tested their hypothesis that the ctDNA is predictive of treatment response in patients receiving RT or CRT by retrospectively assessing the correlation of clinical responses to ctDNA detection and dynamics.
Their sample included 15 women with vulvar, cervical, or recurrent endometrial cancer who were treated with RT or CRT in 2022 and 2023.
The samples were collected prior to radiation therapy, mid-treatment, prior to boost dose with brachytherapy or stereotactic body radiation therapy, at the end of treatment, and at follow-up at 1, 3, and 6 months after the end of therapy and every 6 months thereafter.
The ctDNA analysis was performed with a personalized assay consisting of multiplex polymerase chain reaction and next-generation sequencing. The assays assessed clonal mutations found in the tumors of each patient.
Of the 15 patients, 5 had vulvar/vaginal tumors, all of squamous cell carcinoma histology. Six patients had squamous cell carcinoma of the cervix, and one had neuroendocrine cervical tumors. The two remaining patients had recurrent endometrial adenocarcinomas.
Eight of the patients had stage III disease, four had stage I or II, one had stage IV, and two had recurrent disease.
Results
At baseline 13 of the patients had detectable ctDNA, measured as greater than 0.00 mean tumor molecules per milliliter of plasma (MTM/mL).
There was a strong correlation between elevated ctDNA and measurable disease evaluated by standardized uptake values (SUV) on imaging pre treatment (correlation coefficient = 0.87, P less than .0001).
All patients had reductions in ctDNA from baseline to post-RT/CRT, with 2 having a reduction (partial metabolic response) and 13 having undetectable ctDNA (complete metabolic response) at the end of RT/CRT.
From the mid-treatment blood draw to the posttreatment draw 33% of patients had a partial metabolic response, and 67% had a complete response.
Reduction or clearance of ctDNA also correlated with a decrease in disease burden on MRI during the pre-boost phase of RT.
“Patients with undetectable ctDNA, meaning a complete metabolic response, at mid-radiation and at the end of radiation continued to be clinically without evidence of disease and with undetectable ctDNA at follow-up,” Dr. Wernicke said.
In contrast, the two patients who had partial metabolic responses had disease progression at the end of treatment. Dr. Wernicke noted that one of these patients, who was treated for a neuroendocrine carcinoma of the cervix and had undergone both systemic therapy and CRT, was found to have disease metastatic to the liver and lungs at the 3-month follow-up.
How to Use It?
Invited discussant Casey M. Cosgrove, MD, a gynecologic oncologist at Ohio State University Comprehensive Cancer Centers facility in Hilliard, Ohio, said that the reduction of ctDNA levels in all patients was “great,” but the question remains about how the information from ctDNA might be used to guide care in patients undergoing radiation therapy.
“The main questions I have are: If I don’t clear the ctDNA do I need to do more therapy? If I do clear does that mean I need to do less therapy? And if I have negative ctDNA to start what do I do?” he said.
The answers will be found only with further prospective studies, he emphasized.
“These technologies are only going to get better, and better, and better, and this is going to be a conversation that our patients are going to be bringing up, and this is going to be technology that we’re going to be using in our clinics in the very near future,” he added.
Session comoderator Michael Bookman, MD, a gynecology oncologist at Kaiser Permanente in San Francisco, said “it’s worth remembering that FDA approval of a diagnostic test can be obtained prior to showing any clinical benefit. So these are tests that measure what they say they’re measuring, but they haven’t been validated as improving clinical outcomes, which is the task that clearly lies ahead of us.”
The study was internally funded. Dr. Wernicke reported no relevant disclosures. Dr. Cosgrove reported a consulting or advisory role for Intuitive Ltd., GlaxoSmithKline, AstraZeneca, ImmunoGen, and Merck, and research fees from GSK. Dr. Bookman reported clinical trial advising/monitoring for Immunogen and Clovis Oncology, with fees paid to his institution.
Among 15 patients with vulvar, cervical, or endometrial malignancies who had serum ctDNA draws prior to, during, and after radiation therapy (RT) or chemoradiotherapy (CRT), both persistence or clearance of residual ctDNA were prognostic of patient outcomes from 3 to 6 months after the end of radiation therapy, reported A. Gabriella Wernicke, MD, MSc, a radiation oncologist at Lenox Hill Hospital in New York City.
“Our early findings in this limited cohort suggest that a mid-treatment ctDNA draw identified responders to radiation, and that may potentially serve as an early predictive biomarker of response. And clearly, these findings need to be validated in a prospective manner, a trial which will be starting in our center soon,” she said in an oral abstract session at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer, held in San Diego, California.
Gynecologic malignancies are challenging to manage with radiotherapy because of the treatment’s toxicities and because outcomes may not be known until several months after the end of therapy. Early identification of responses to radiation therapy with simple blood draws has the potential to help clinicians identify those patients whose tumors are responding to radiation early in the course of therapy, she said.
Correlating treatment with responses
Dr. Wernicke and colleagues tested their hypothesis that the ctDNA is predictive of treatment response in patients receiving RT or CRT by retrospectively assessing the correlation of clinical responses to ctDNA detection and dynamics.
Their sample included 15 women with vulvar, cervical, or recurrent endometrial cancer who were treated with RT or CRT in 2022 and 2023.
The samples were collected prior to radiation therapy, mid-treatment, prior to boost dose with brachytherapy or stereotactic body radiation therapy, at the end of treatment, and at follow-up at 1, 3, and 6 months after the end of therapy and every 6 months thereafter.
The ctDNA analysis was performed with a personalized assay consisting of multiplex polymerase chain reaction and next-generation sequencing. The assays assessed clonal mutations found in the tumors of each patient.
Of the 15 patients, 5 had vulvar/vaginal tumors, all of squamous cell carcinoma histology. Six patients had squamous cell carcinoma of the cervix, and one had neuroendocrine cervical tumors. The two remaining patients had recurrent endometrial adenocarcinomas.
Eight of the patients had stage III disease, four had stage I or II, one had stage IV, and two had recurrent disease.
Results
At baseline 13 of the patients had detectable ctDNA, measured as greater than 0.00 mean tumor molecules per milliliter of plasma (MTM/mL).
There was a strong correlation between elevated ctDNA and measurable disease evaluated by standardized uptake values (SUV) on imaging pre treatment (correlation coefficient = 0.87, P less than .0001).
All patients had reductions in ctDNA from baseline to post-RT/CRT, with 2 having a reduction (partial metabolic response) and 13 having undetectable ctDNA (complete metabolic response) at the end of RT/CRT.
From the mid-treatment blood draw to the posttreatment draw 33% of patients had a partial metabolic response, and 67% had a complete response.
Reduction or clearance of ctDNA also correlated with a decrease in disease burden on MRI during the pre-boost phase of RT.
“Patients with undetectable ctDNA, meaning a complete metabolic response, at mid-radiation and at the end of radiation continued to be clinically without evidence of disease and with undetectable ctDNA at follow-up,” Dr. Wernicke said.
In contrast, the two patients who had partial metabolic responses had disease progression at the end of treatment. Dr. Wernicke noted that one of these patients, who was treated for a neuroendocrine carcinoma of the cervix and had undergone both systemic therapy and CRT, was found to have disease metastatic to the liver and lungs at the 3-month follow-up.
How to Use It?
Invited discussant Casey M. Cosgrove, MD, a gynecologic oncologist at Ohio State University Comprehensive Cancer Centers facility in Hilliard, Ohio, said that the reduction of ctDNA levels in all patients was “great,” but the question remains about how the information from ctDNA might be used to guide care in patients undergoing radiation therapy.
“The main questions I have are: If I don’t clear the ctDNA do I need to do more therapy? If I do clear does that mean I need to do less therapy? And if I have negative ctDNA to start what do I do?” he said.
The answers will be found only with further prospective studies, he emphasized.
“These technologies are only going to get better, and better, and better, and this is going to be a conversation that our patients are going to be bringing up, and this is going to be technology that we’re going to be using in our clinics in the very near future,” he added.
Session comoderator Michael Bookman, MD, a gynecology oncologist at Kaiser Permanente in San Francisco, said “it’s worth remembering that FDA approval of a diagnostic test can be obtained prior to showing any clinical benefit. So these are tests that measure what they say they’re measuring, but they haven’t been validated as improving clinical outcomes, which is the task that clearly lies ahead of us.”
The study was internally funded. Dr. Wernicke reported no relevant disclosures. Dr. Cosgrove reported a consulting or advisory role for Intuitive Ltd., GlaxoSmithKline, AstraZeneca, ImmunoGen, and Merck, and research fees from GSK. Dr. Bookman reported clinical trial advising/monitoring for Immunogen and Clovis Oncology, with fees paid to his institution.
Among 15 patients with vulvar, cervical, or endometrial malignancies who had serum ctDNA draws prior to, during, and after radiation therapy (RT) or chemoradiotherapy (CRT), both persistence or clearance of residual ctDNA were prognostic of patient outcomes from 3 to 6 months after the end of radiation therapy, reported A. Gabriella Wernicke, MD, MSc, a radiation oncologist at Lenox Hill Hospital in New York City.
“Our early findings in this limited cohort suggest that a mid-treatment ctDNA draw identified responders to radiation, and that may potentially serve as an early predictive biomarker of response. And clearly, these findings need to be validated in a prospective manner, a trial which will be starting in our center soon,” she said in an oral abstract session at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer, held in San Diego, California.
Gynecologic malignancies are challenging to manage with radiotherapy because of the treatment’s toxicities and because outcomes may not be known until several months after the end of therapy. Early identification of responses to radiation therapy with simple blood draws has the potential to help clinicians identify those patients whose tumors are responding to radiation early in the course of therapy, she said.
Correlating treatment with responses
Dr. Wernicke and colleagues tested their hypothesis that the ctDNA is predictive of treatment response in patients receiving RT or CRT by retrospectively assessing the correlation of clinical responses to ctDNA detection and dynamics.
Their sample included 15 women with vulvar, cervical, or recurrent endometrial cancer who were treated with RT or CRT in 2022 and 2023.
The samples were collected prior to radiation therapy, mid-treatment, prior to boost dose with brachytherapy or stereotactic body radiation therapy, at the end of treatment, and at follow-up at 1, 3, and 6 months after the end of therapy and every 6 months thereafter.
The ctDNA analysis was performed with a personalized assay consisting of multiplex polymerase chain reaction and next-generation sequencing. The assays assessed clonal mutations found in the tumors of each patient.
Of the 15 patients, 5 had vulvar/vaginal tumors, all of squamous cell carcinoma histology. Six patients had squamous cell carcinoma of the cervix, and one had neuroendocrine cervical tumors. The two remaining patients had recurrent endometrial adenocarcinomas.
Eight of the patients had stage III disease, four had stage I or II, one had stage IV, and two had recurrent disease.
Results
At baseline 13 of the patients had detectable ctDNA, measured as greater than 0.00 mean tumor molecules per milliliter of plasma (MTM/mL).
There was a strong correlation between elevated ctDNA and measurable disease evaluated by standardized uptake values (SUV) on imaging pre treatment (correlation coefficient = 0.87, P less than .0001).
All patients had reductions in ctDNA from baseline to post-RT/CRT, with 2 having a reduction (partial metabolic response) and 13 having undetectable ctDNA (complete metabolic response) at the end of RT/CRT.
From the mid-treatment blood draw to the posttreatment draw 33% of patients had a partial metabolic response, and 67% had a complete response.
Reduction or clearance of ctDNA also correlated with a decrease in disease burden on MRI during the pre-boost phase of RT.
“Patients with undetectable ctDNA, meaning a complete metabolic response, at mid-radiation and at the end of radiation continued to be clinically without evidence of disease and with undetectable ctDNA at follow-up,” Dr. Wernicke said.
In contrast, the two patients who had partial metabolic responses had disease progression at the end of treatment. Dr. Wernicke noted that one of these patients, who was treated for a neuroendocrine carcinoma of the cervix and had undergone both systemic therapy and CRT, was found to have disease metastatic to the liver and lungs at the 3-month follow-up.
How to Use It?
Invited discussant Casey M. Cosgrove, MD, a gynecologic oncologist at Ohio State University Comprehensive Cancer Centers facility in Hilliard, Ohio, said that the reduction of ctDNA levels in all patients was “great,” but the question remains about how the information from ctDNA might be used to guide care in patients undergoing radiation therapy.
“The main questions I have are: If I don’t clear the ctDNA do I need to do more therapy? If I do clear does that mean I need to do less therapy? And if I have negative ctDNA to start what do I do?” he said.
The answers will be found only with further prospective studies, he emphasized.
“These technologies are only going to get better, and better, and better, and this is going to be a conversation that our patients are going to be bringing up, and this is going to be technology that we’re going to be using in our clinics in the very near future,” he added.
Session comoderator Michael Bookman, MD, a gynecology oncologist at Kaiser Permanente in San Francisco, said “it’s worth remembering that FDA approval of a diagnostic test can be obtained prior to showing any clinical benefit. So these are tests that measure what they say they’re measuring, but they haven’t been validated as improving clinical outcomes, which is the task that clearly lies ahead of us.”
The study was internally funded. Dr. Wernicke reported no relevant disclosures. Dr. Cosgrove reported a consulting or advisory role for Intuitive Ltd., GlaxoSmithKline, AstraZeneca, ImmunoGen, and Merck, and research fees from GSK. Dr. Bookman reported clinical trial advising/monitoring for Immunogen and Clovis Oncology, with fees paid to his institution.
FROM SGO 2024
Non-Radical Surgery a Win-Win for Early Cervical Cancer
according to results of the GOG-278 trial.
In fact, patients’ quality of life was improved after surgery in both groups, and their concerns about cancer recurrence decreased, especially for those undergoing simple hysterectomy, said Allan Covens, MD, in his late-breaking abstract presentation at the Society of Gynecologic Oncology (SGO)’s Annual Meeting on Women’s Cancer.
“Cone biopsy patients reported less concerns about reproductive fertility after surgery and over time compared to preop assessments,” he added.
Due to screening in developed countries, a large proportion of cervical cancers are discovered at an early stage. Treatment of these cancers with radical surgery is associated with high cure rates but significant adverse effects on quality of life, said Dr. Covens, who is with the University of Toronto, Toronto, Ontario, Canada.
He and his colleagues wanted to see if non-radical surgery could be safely used instead. “Multiple case series have indicated that non-radical surgery is associated with less morbidity and improved quality of life,” he explained. “If this can be proven in a prospective evaluation, it will change future practice.”
GOG-278 was a prospective cohort study of women with stage IA1 (lymph-vascular space invasion+) and IA2-IB1 (≤ 2 cm) carcinoma of the cervix who underwent non-radical surgery (simple hysterectomy or fertility-preserving cone biopsy) and pelvic lymphadenectomy. Criteria included ≤ 10 mm stromal invasion and negative margins on the final cone biopsy.
The primary objectives were to assess changes in functional outcomes of quality of life (bladder/bowel function, sexual function, cancer worry, and reproductive concerns), using validated instruments. Findings were based on 55 patients who underwent cone biopsy and 113 who underwent simple hysterectomy.
Both simple hysterectomy and cone biopsy were associated with “small” declines in sexual function and bladder/bowel function at 4-6 weeks after surgery, but function “quickly” recovered to baseline by 6 months, Dr. Covens reported.
Twelve patients reported a diagnosis of lymphedema, with a Gynecologic Cancer Lymphedema Questionnaire score change of 4 or higher on at least two consecutive evaluations from baseline. This occurred in six cone biopsy and six simple hysterectomy patients.
In a separate presentation, Dr. Covens reported secondary oncologic outcomes from GOG-278, which suggest that non-radical surgery for early-stage cervical cancer is safe, with low perioperative morbidity, although longer follow-up is needed.
He also reported 16 pregnancies in 15 patients who had undergone cone biopsies; 12 of these were successful, and there were four early pregnancy losses.
‘Impressive’ Data
Study discussant Kristin Bixel, MD, with The Ohio State University, Columbus, Ohio, said the data are “impressive” and clearly show that non-radical surgery has “minimal impact on bladder/bowel function, with no long-term differences from baseline.”
She added that the incidence of lymphedema was “honestly significantly lower than what I typically counsel patients about” and wondered if the percentage of patients with lymphedema would increase over time.
Dr. Bixel particularly noted the decrease in cancer worry scores after surgery, as sometimes patients who have less radical procedures fear that this comes with an increased risk for recurrence.
The “growing body of data suggests that less radical surgery is safe and effective for early-stage low-risk cervical cancer and highlights the potential reproductive success,” she concluded.
Funding for the study was provided by grants from NRG Oncology. Dr. Covens had no disclosures. Dr. Bixel has received research funding from the Intuitive Foundation.
A version of this article appeared on Medscape.com.
according to results of the GOG-278 trial.
In fact, patients’ quality of life was improved after surgery in both groups, and their concerns about cancer recurrence decreased, especially for those undergoing simple hysterectomy, said Allan Covens, MD, in his late-breaking abstract presentation at the Society of Gynecologic Oncology (SGO)’s Annual Meeting on Women’s Cancer.
“Cone biopsy patients reported less concerns about reproductive fertility after surgery and over time compared to preop assessments,” he added.
Due to screening in developed countries, a large proportion of cervical cancers are discovered at an early stage. Treatment of these cancers with radical surgery is associated with high cure rates but significant adverse effects on quality of life, said Dr. Covens, who is with the University of Toronto, Toronto, Ontario, Canada.
He and his colleagues wanted to see if non-radical surgery could be safely used instead. “Multiple case series have indicated that non-radical surgery is associated with less morbidity and improved quality of life,” he explained. “If this can be proven in a prospective evaluation, it will change future practice.”
GOG-278 was a prospective cohort study of women with stage IA1 (lymph-vascular space invasion+) and IA2-IB1 (≤ 2 cm) carcinoma of the cervix who underwent non-radical surgery (simple hysterectomy or fertility-preserving cone biopsy) and pelvic lymphadenectomy. Criteria included ≤ 10 mm stromal invasion and negative margins on the final cone biopsy.
The primary objectives were to assess changes in functional outcomes of quality of life (bladder/bowel function, sexual function, cancer worry, and reproductive concerns), using validated instruments. Findings were based on 55 patients who underwent cone biopsy and 113 who underwent simple hysterectomy.
Both simple hysterectomy and cone biopsy were associated with “small” declines in sexual function and bladder/bowel function at 4-6 weeks after surgery, but function “quickly” recovered to baseline by 6 months, Dr. Covens reported.
Twelve patients reported a diagnosis of lymphedema, with a Gynecologic Cancer Lymphedema Questionnaire score change of 4 or higher on at least two consecutive evaluations from baseline. This occurred in six cone biopsy and six simple hysterectomy patients.
In a separate presentation, Dr. Covens reported secondary oncologic outcomes from GOG-278, which suggest that non-radical surgery for early-stage cervical cancer is safe, with low perioperative morbidity, although longer follow-up is needed.
He also reported 16 pregnancies in 15 patients who had undergone cone biopsies; 12 of these were successful, and there were four early pregnancy losses.
‘Impressive’ Data
Study discussant Kristin Bixel, MD, with The Ohio State University, Columbus, Ohio, said the data are “impressive” and clearly show that non-radical surgery has “minimal impact on bladder/bowel function, with no long-term differences from baseline.”
She added that the incidence of lymphedema was “honestly significantly lower than what I typically counsel patients about” and wondered if the percentage of patients with lymphedema would increase over time.
Dr. Bixel particularly noted the decrease in cancer worry scores after surgery, as sometimes patients who have less radical procedures fear that this comes with an increased risk for recurrence.
The “growing body of data suggests that less radical surgery is safe and effective for early-stage low-risk cervical cancer and highlights the potential reproductive success,” she concluded.
Funding for the study was provided by grants from NRG Oncology. Dr. Covens had no disclosures. Dr. Bixel has received research funding from the Intuitive Foundation.
A version of this article appeared on Medscape.com.
according to results of the GOG-278 trial.
In fact, patients’ quality of life was improved after surgery in both groups, and their concerns about cancer recurrence decreased, especially for those undergoing simple hysterectomy, said Allan Covens, MD, in his late-breaking abstract presentation at the Society of Gynecologic Oncology (SGO)’s Annual Meeting on Women’s Cancer.
“Cone biopsy patients reported less concerns about reproductive fertility after surgery and over time compared to preop assessments,” he added.
Due to screening in developed countries, a large proportion of cervical cancers are discovered at an early stage. Treatment of these cancers with radical surgery is associated with high cure rates but significant adverse effects on quality of life, said Dr. Covens, who is with the University of Toronto, Toronto, Ontario, Canada.
He and his colleagues wanted to see if non-radical surgery could be safely used instead. “Multiple case series have indicated that non-radical surgery is associated with less morbidity and improved quality of life,” he explained. “If this can be proven in a prospective evaluation, it will change future practice.”
GOG-278 was a prospective cohort study of women with stage IA1 (lymph-vascular space invasion+) and IA2-IB1 (≤ 2 cm) carcinoma of the cervix who underwent non-radical surgery (simple hysterectomy or fertility-preserving cone biopsy) and pelvic lymphadenectomy. Criteria included ≤ 10 mm stromal invasion and negative margins on the final cone biopsy.
The primary objectives were to assess changes in functional outcomes of quality of life (bladder/bowel function, sexual function, cancer worry, and reproductive concerns), using validated instruments. Findings were based on 55 patients who underwent cone biopsy and 113 who underwent simple hysterectomy.
Both simple hysterectomy and cone biopsy were associated with “small” declines in sexual function and bladder/bowel function at 4-6 weeks after surgery, but function “quickly” recovered to baseline by 6 months, Dr. Covens reported.
Twelve patients reported a diagnosis of lymphedema, with a Gynecologic Cancer Lymphedema Questionnaire score change of 4 or higher on at least two consecutive evaluations from baseline. This occurred in six cone biopsy and six simple hysterectomy patients.
In a separate presentation, Dr. Covens reported secondary oncologic outcomes from GOG-278, which suggest that non-radical surgery for early-stage cervical cancer is safe, with low perioperative morbidity, although longer follow-up is needed.
He also reported 16 pregnancies in 15 patients who had undergone cone biopsies; 12 of these were successful, and there were four early pregnancy losses.
‘Impressive’ Data
Study discussant Kristin Bixel, MD, with The Ohio State University, Columbus, Ohio, said the data are “impressive” and clearly show that non-radical surgery has “minimal impact on bladder/bowel function, with no long-term differences from baseline.”
She added that the incidence of lymphedema was “honestly significantly lower than what I typically counsel patients about” and wondered if the percentage of patients with lymphedema would increase over time.
Dr. Bixel particularly noted the decrease in cancer worry scores after surgery, as sometimes patients who have less radical procedures fear that this comes with an increased risk for recurrence.
The “growing body of data suggests that less radical surgery is safe and effective for early-stage low-risk cervical cancer and highlights the potential reproductive success,” she concluded.
Funding for the study was provided by grants from NRG Oncology. Dr. Covens had no disclosures. Dr. Bixel has received research funding from the Intuitive Foundation.
A version of this article appeared on Medscape.com.
FROM SGO 2024
RUBY: ‘A Huge Win’ for Patients With Advanced or Recurrent Endometrial Cancer
The benefit of the combination of the programmed death protein 1 (PD-1) inhibitor dostarlimab (Jemperli) and chemotherapy was even more pronounced among patients with DNA mismatch repair deficient/microsatellite instability high (dMMR/MSI-H) tumors.
These results, from the second interim analysis of the phase 3 ENGOT-EN6-NSGO/GOG-3031/RUBY trial, were cheered by audience members when they were reported at the Society of Gynecologic Oncology (SGO)’s Annual Meeting on Women’s Cancer, held in San Diego, California.
“Overall survival benefit to the addition of PD-1 inhibitor to chemotherapy upfront for patients with advanced and recurrent MSI-high endometrial cancer: SOLD!” said invited discussant Gini Fleming, medical director of gynecologic oncology at the University of Chicago.
“I think this is a huge win for our patients. It’s something that none of us have seen before over many years of working with endometrial cancer and should be incorporated into everybody’s practice as of yesterday,” she said.
Continued Improvement
Results from the first interim analysis of the trial showed that dostarlimab and chemotherapy significantly improved progression-free survival (PFS) in the dMMR/MSI-H population, and there was an early trend toward improved overall survival, compared with chemotherapy plus placebo.
As Matthew A. Powell, MD from Washington University School of Medicine in Saint Louis, Missouri reported at SGO 2024, that early trend has become an undeniable survival advantage.
At a median follow-up of 37.2 months, the median overall survival was 44.6 months for patients randomized to the combination, compared with 28.2 months for those assigned to chemotherapy plus placebo.
The respective 3-year overall survival (OS) rates were 54.9% and 42.9%, translating into a hazard ratio (HR) for death with dostarlimab/chemotherapy of 0.69 (P = .002).
Among the subset of patients with dMMR/MSI-H tumors the survival benefit conferred by the combination was even greater, with median OS not reached in the dostarlimab group vs 31.4 months in the chemotherapy-alone arm, with respective 3-year OS rates of 78% and 46%. This difference translated into a HR for death with the combination of 0.32 (P = .0002) for patients with deficient mismatch-repair cancers.
“Dostarlimab plus carboplatin-paclitaxel chemotherapy demonstrated statistically significant and clinically meaningful overall survival improvements in the overall population, a substantial unprecedented overall survival benefit in patients with defective mismatch-repair tumors, and a clinically meaningful; 7-month improvement in the OS difference in patients with proficient mismatch-repair tumors,” Dr. Powell said.
RUBY Details
The trial was conducted in 494 patients with primary advanced stage III or IV or first recurrent endometrial cancer who received first-line treatment with standard chemotherapy with carboplatin (area under the concentration–time curve, 5 mg/mL per minute) and paclitaxel (175 mg/m2 of body surface area), every 3 weeks (six cycles). They were also randomized to receive either dostarlimab (1000 mg) or dostarlimab placebo every 6 weeks for up to 3 years.
Within the cohort, 118 patients (23.9%) had dMMR/MSI-H tumors.
At the time of the first interim analysis the estimated progression-free survival at 24 months in the dMMR–MSI-H subgroup was 61.4% in the dostarlimab group vs 15.7 in the placebo group (HR for progression or death, 0.28; P < .001). For the entire cohort, progression-free survival at 24 months was 36.1% vs 18.1% (HR, 0.64; P < .001).
A prespecified exploratory analysis of progression-free survival in proficient MMR, microsatellite stable (MSS) patients was also done, and a clinically relevant benefit was observed.
Overall survival at that time also favored dostarlimab, although it was only mature for 33% of the population. But at 24 months, OS rates were 71.3% vs 56.0% among placebo recipients; this difference approached but did not reach statistical significance.
The overall response rate in the dMMR–MSI-H population vs the placebo group was 77.6% vs 69%, respectively, and 68.1% and 63.4% in the pMMR/MSS population.
The most common adverse events observed were nausea, alopecia, and fatigue. Grade 3 and higher adverse events at the most recent follow-up were more frequent in the dostarlimab group than in the placebo group (72.2% vs 60.2%).
“Importantly, safety was maintained” at the second interim analysis, Dr. Powell said.
“No new safety signals were noted, no new deaths related to therapy were noted with the subsequent 1-year additional analysis time,” he said.
What’s Next?
Dr. Fleming reviewed potential strategies for further improving care of patients with advanced or recurrent endometrial cancer during her discussion.
“What are the next directions for patients with MSI-high disease? Well, obviously could we use immune checkpoint inhibitors without chemotherapy and not compromise results? There are two ongoing trials or trials that we’re awaiting results of that have compared single-agent immune checkpoint inhibitor to just chemotherapy in mismatch repair-deficient advanced disease, and hopefully we can extrapolate from these trials to determine if this might be a more patient-friendly and equally effective strategy, but we don’t yet know,” she said.
Dr. Fleming also noted that ongoing or planned clinical trials will address questions about potential options for patients with MSI-H tumors whose disease progresses on frontline chemotherapy and immunotherapy. Other trials are assessing whether combining radiotherapy with checkpoint inhibitors will be effective in treating patients with earlier-stage tumors, or whether the addition of a PARP inhibitor might offer additional benefit for these patients.
“Immune checkpoint inhibitor should be given first line to patients with advanced/recurrent microsatellite [instability] endometrial cancer, and they should be considered as front line in patients with microsatellite stable disease. At this point, unfortunately, we have no reasonable predictive factors to know which of those patients with microsatellite stable disease will truly benefit. Multiple other agents are being tested in this setting, and will hopefully prove useful in subgroups,” she said.
The study is funded by GlaxoSmithKline. Dr. Powell reports grants/research support from GSK and honoraria/consultation fees from AstraZeneca, Clovis Oncology, Eisai, GSK, Immunogen, and Merck. Dr. Fleming reports serving as an institutional principal investigator for trials sponsored by multiple companies, not including GSK.
The benefit of the combination of the programmed death protein 1 (PD-1) inhibitor dostarlimab (Jemperli) and chemotherapy was even more pronounced among patients with DNA mismatch repair deficient/microsatellite instability high (dMMR/MSI-H) tumors.
These results, from the second interim analysis of the phase 3 ENGOT-EN6-NSGO/GOG-3031/RUBY trial, were cheered by audience members when they were reported at the Society of Gynecologic Oncology (SGO)’s Annual Meeting on Women’s Cancer, held in San Diego, California.
“Overall survival benefit to the addition of PD-1 inhibitor to chemotherapy upfront for patients with advanced and recurrent MSI-high endometrial cancer: SOLD!” said invited discussant Gini Fleming, medical director of gynecologic oncology at the University of Chicago.
“I think this is a huge win for our patients. It’s something that none of us have seen before over many years of working with endometrial cancer and should be incorporated into everybody’s practice as of yesterday,” she said.
Continued Improvement
Results from the first interim analysis of the trial showed that dostarlimab and chemotherapy significantly improved progression-free survival (PFS) in the dMMR/MSI-H population, and there was an early trend toward improved overall survival, compared with chemotherapy plus placebo.
As Matthew A. Powell, MD from Washington University School of Medicine in Saint Louis, Missouri reported at SGO 2024, that early trend has become an undeniable survival advantage.
At a median follow-up of 37.2 months, the median overall survival was 44.6 months for patients randomized to the combination, compared with 28.2 months for those assigned to chemotherapy plus placebo.
The respective 3-year overall survival (OS) rates were 54.9% and 42.9%, translating into a hazard ratio (HR) for death with dostarlimab/chemotherapy of 0.69 (P = .002).
Among the subset of patients with dMMR/MSI-H tumors the survival benefit conferred by the combination was even greater, with median OS not reached in the dostarlimab group vs 31.4 months in the chemotherapy-alone arm, with respective 3-year OS rates of 78% and 46%. This difference translated into a HR for death with the combination of 0.32 (P = .0002) for patients with deficient mismatch-repair cancers.
“Dostarlimab plus carboplatin-paclitaxel chemotherapy demonstrated statistically significant and clinically meaningful overall survival improvements in the overall population, a substantial unprecedented overall survival benefit in patients with defective mismatch-repair tumors, and a clinically meaningful; 7-month improvement in the OS difference in patients with proficient mismatch-repair tumors,” Dr. Powell said.
RUBY Details
The trial was conducted in 494 patients with primary advanced stage III or IV or first recurrent endometrial cancer who received first-line treatment with standard chemotherapy with carboplatin (area under the concentration–time curve, 5 mg/mL per minute) and paclitaxel (175 mg/m2 of body surface area), every 3 weeks (six cycles). They were also randomized to receive either dostarlimab (1000 mg) or dostarlimab placebo every 6 weeks for up to 3 years.
Within the cohort, 118 patients (23.9%) had dMMR/MSI-H tumors.
At the time of the first interim analysis the estimated progression-free survival at 24 months in the dMMR–MSI-H subgroup was 61.4% in the dostarlimab group vs 15.7 in the placebo group (HR for progression or death, 0.28; P < .001). For the entire cohort, progression-free survival at 24 months was 36.1% vs 18.1% (HR, 0.64; P < .001).
A prespecified exploratory analysis of progression-free survival in proficient MMR, microsatellite stable (MSS) patients was also done, and a clinically relevant benefit was observed.
Overall survival at that time also favored dostarlimab, although it was only mature for 33% of the population. But at 24 months, OS rates were 71.3% vs 56.0% among placebo recipients; this difference approached but did not reach statistical significance.
The overall response rate in the dMMR–MSI-H population vs the placebo group was 77.6% vs 69%, respectively, and 68.1% and 63.4% in the pMMR/MSS population.
The most common adverse events observed were nausea, alopecia, and fatigue. Grade 3 and higher adverse events at the most recent follow-up were more frequent in the dostarlimab group than in the placebo group (72.2% vs 60.2%).
“Importantly, safety was maintained” at the second interim analysis, Dr. Powell said.
“No new safety signals were noted, no new deaths related to therapy were noted with the subsequent 1-year additional analysis time,” he said.
What’s Next?
Dr. Fleming reviewed potential strategies for further improving care of patients with advanced or recurrent endometrial cancer during her discussion.
“What are the next directions for patients with MSI-high disease? Well, obviously could we use immune checkpoint inhibitors without chemotherapy and not compromise results? There are two ongoing trials or trials that we’re awaiting results of that have compared single-agent immune checkpoint inhibitor to just chemotherapy in mismatch repair-deficient advanced disease, and hopefully we can extrapolate from these trials to determine if this might be a more patient-friendly and equally effective strategy, but we don’t yet know,” she said.
Dr. Fleming also noted that ongoing or planned clinical trials will address questions about potential options for patients with MSI-H tumors whose disease progresses on frontline chemotherapy and immunotherapy. Other trials are assessing whether combining radiotherapy with checkpoint inhibitors will be effective in treating patients with earlier-stage tumors, or whether the addition of a PARP inhibitor might offer additional benefit for these patients.
“Immune checkpoint inhibitor should be given first line to patients with advanced/recurrent microsatellite [instability] endometrial cancer, and they should be considered as front line in patients with microsatellite stable disease. At this point, unfortunately, we have no reasonable predictive factors to know which of those patients with microsatellite stable disease will truly benefit. Multiple other agents are being tested in this setting, and will hopefully prove useful in subgroups,” she said.
The study is funded by GlaxoSmithKline. Dr. Powell reports grants/research support from GSK and honoraria/consultation fees from AstraZeneca, Clovis Oncology, Eisai, GSK, Immunogen, and Merck. Dr. Fleming reports serving as an institutional principal investigator for trials sponsored by multiple companies, not including GSK.
The benefit of the combination of the programmed death protein 1 (PD-1) inhibitor dostarlimab (Jemperli) and chemotherapy was even more pronounced among patients with DNA mismatch repair deficient/microsatellite instability high (dMMR/MSI-H) tumors.
These results, from the second interim analysis of the phase 3 ENGOT-EN6-NSGO/GOG-3031/RUBY trial, were cheered by audience members when they were reported at the Society of Gynecologic Oncology (SGO)’s Annual Meeting on Women’s Cancer, held in San Diego, California.
“Overall survival benefit to the addition of PD-1 inhibitor to chemotherapy upfront for patients with advanced and recurrent MSI-high endometrial cancer: SOLD!” said invited discussant Gini Fleming, medical director of gynecologic oncology at the University of Chicago.
“I think this is a huge win for our patients. It’s something that none of us have seen before over many years of working with endometrial cancer and should be incorporated into everybody’s practice as of yesterday,” she said.
Continued Improvement
Results from the first interim analysis of the trial showed that dostarlimab and chemotherapy significantly improved progression-free survival (PFS) in the dMMR/MSI-H population, and there was an early trend toward improved overall survival, compared with chemotherapy plus placebo.
As Matthew A. Powell, MD from Washington University School of Medicine in Saint Louis, Missouri reported at SGO 2024, that early trend has become an undeniable survival advantage.
At a median follow-up of 37.2 months, the median overall survival was 44.6 months for patients randomized to the combination, compared with 28.2 months for those assigned to chemotherapy plus placebo.
The respective 3-year overall survival (OS) rates were 54.9% and 42.9%, translating into a hazard ratio (HR) for death with dostarlimab/chemotherapy of 0.69 (P = .002).
Among the subset of patients with dMMR/MSI-H tumors the survival benefit conferred by the combination was even greater, with median OS not reached in the dostarlimab group vs 31.4 months in the chemotherapy-alone arm, with respective 3-year OS rates of 78% and 46%. This difference translated into a HR for death with the combination of 0.32 (P = .0002) for patients with deficient mismatch-repair cancers.
“Dostarlimab plus carboplatin-paclitaxel chemotherapy demonstrated statistically significant and clinically meaningful overall survival improvements in the overall population, a substantial unprecedented overall survival benefit in patients with defective mismatch-repair tumors, and a clinically meaningful; 7-month improvement in the OS difference in patients with proficient mismatch-repair tumors,” Dr. Powell said.
RUBY Details
The trial was conducted in 494 patients with primary advanced stage III or IV or first recurrent endometrial cancer who received first-line treatment with standard chemotherapy with carboplatin (area under the concentration–time curve, 5 mg/mL per minute) and paclitaxel (175 mg/m2 of body surface area), every 3 weeks (six cycles). They were also randomized to receive either dostarlimab (1000 mg) or dostarlimab placebo every 6 weeks for up to 3 years.
Within the cohort, 118 patients (23.9%) had dMMR/MSI-H tumors.
At the time of the first interim analysis the estimated progression-free survival at 24 months in the dMMR–MSI-H subgroup was 61.4% in the dostarlimab group vs 15.7 in the placebo group (HR for progression or death, 0.28; P < .001). For the entire cohort, progression-free survival at 24 months was 36.1% vs 18.1% (HR, 0.64; P < .001).
A prespecified exploratory analysis of progression-free survival in proficient MMR, microsatellite stable (MSS) patients was also done, and a clinically relevant benefit was observed.
Overall survival at that time also favored dostarlimab, although it was only mature for 33% of the population. But at 24 months, OS rates were 71.3% vs 56.0% among placebo recipients; this difference approached but did not reach statistical significance.
The overall response rate in the dMMR–MSI-H population vs the placebo group was 77.6% vs 69%, respectively, and 68.1% and 63.4% in the pMMR/MSS population.
The most common adverse events observed were nausea, alopecia, and fatigue. Grade 3 and higher adverse events at the most recent follow-up were more frequent in the dostarlimab group than in the placebo group (72.2% vs 60.2%).
“Importantly, safety was maintained” at the second interim analysis, Dr. Powell said.
“No new safety signals were noted, no new deaths related to therapy were noted with the subsequent 1-year additional analysis time,” he said.
What’s Next?
Dr. Fleming reviewed potential strategies for further improving care of patients with advanced or recurrent endometrial cancer during her discussion.
“What are the next directions for patients with MSI-high disease? Well, obviously could we use immune checkpoint inhibitors without chemotherapy and not compromise results? There are two ongoing trials or trials that we’re awaiting results of that have compared single-agent immune checkpoint inhibitor to just chemotherapy in mismatch repair-deficient advanced disease, and hopefully we can extrapolate from these trials to determine if this might be a more patient-friendly and equally effective strategy, but we don’t yet know,” she said.
Dr. Fleming also noted that ongoing or planned clinical trials will address questions about potential options for patients with MSI-H tumors whose disease progresses on frontline chemotherapy and immunotherapy. Other trials are assessing whether combining radiotherapy with checkpoint inhibitors will be effective in treating patients with earlier-stage tumors, or whether the addition of a PARP inhibitor might offer additional benefit for these patients.
“Immune checkpoint inhibitor should be given first line to patients with advanced/recurrent microsatellite [instability] endometrial cancer, and they should be considered as front line in patients with microsatellite stable disease. At this point, unfortunately, we have no reasonable predictive factors to know which of those patients with microsatellite stable disease will truly benefit. Multiple other agents are being tested in this setting, and will hopefully prove useful in subgroups,” she said.
The study is funded by GlaxoSmithKline. Dr. Powell reports grants/research support from GSK and honoraria/consultation fees from AstraZeneca, Clovis Oncology, Eisai, GSK, Immunogen, and Merck. Dr. Fleming reports serving as an institutional principal investigator for trials sponsored by multiple companies, not including GSK.
FROM SGO 2024