User login
Antithrombotics no deterrent for emergent lap appendectomy
HOUSTON – Few studies have looked at the risk of irreversible antithrombotic therapy in patients who need emergent or urgent laparoscopic appendectomy, but a new study showed that the operation poses no significantly greater risk for such patients, compared with people who are not on antithrombotics.
The study’s findings do not apply to all patients on anticoagulation, specifically those on new novel oral anticoagulants (NOACs), said Christopher Pearcy, MD, of Methodist Dallas Medical Center.
NOAC agents include dabigatran, rivaroxaban, and apixaban.
Appendicitis is the third most common indication for abdominal surgery in the elderly, Dr. Pearcy noted, and their mortality rates are eight times greater than those of younger patients. However, these patients often proceed to operation with minimal workup, “given that laparoscopic appendectomy is a relatively benign procedure,” he said at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
The retrospective study evaluated two groups of 195 patients who had urgent or emergent laparoscopic appendectomy at three centers from 2010 to 2014. One group was on irreversible antithrombotic therapy, and the other served as controls.
The primary outcomes were blood loss, transfusion requirement, and mortality. Secondary outcomes were duration of operation, length of hospital stay, rates of infections, complications, and 30-day readmissions.
“Compared with controls, we didn’t find any significant difference in any outcome whatsoever after laparoscopic appendectomy in patients on prehospital antithrombotic therapy,” Dr. Pearcy said.
Specifically, average estimated blood loss was 18 cc in controls vs. 22 cc in patients on antithrombotics, and mortality was 0% in the former vs. 1% in the latter. Patients on antithrombotics had a lower rate of complications: 3% vs. 11%.
Dr. Pearcy discussed a case of a 70-year-old man with acute appendicitis. He had a history of coronary artery disease, hypertension, hyperlipidemia, type 2 diabetes, and stroke, and was taking clopidogrel and aspirin daily.
“Is it safe to proceed with surgery given this patient’s irreversible antithrombotic therapy? We would say yes,” he said.
Dr. Pearcy reported having no financial disclosures.
HOUSTON – Few studies have looked at the risk of irreversible antithrombotic therapy in patients who need emergent or urgent laparoscopic appendectomy, but a new study showed that the operation poses no significantly greater risk for such patients, compared with people who are not on antithrombotics.
The study’s findings do not apply to all patients on anticoagulation, specifically those on new novel oral anticoagulants (NOACs), said Christopher Pearcy, MD, of Methodist Dallas Medical Center.
NOAC agents include dabigatran, rivaroxaban, and apixaban.
Appendicitis is the third most common indication for abdominal surgery in the elderly, Dr. Pearcy noted, and their mortality rates are eight times greater than those of younger patients. However, these patients often proceed to operation with minimal workup, “given that laparoscopic appendectomy is a relatively benign procedure,” he said at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
The retrospective study evaluated two groups of 195 patients who had urgent or emergent laparoscopic appendectomy at three centers from 2010 to 2014. One group was on irreversible antithrombotic therapy, and the other served as controls.
The primary outcomes were blood loss, transfusion requirement, and mortality. Secondary outcomes were duration of operation, length of hospital stay, rates of infections, complications, and 30-day readmissions.
“Compared with controls, we didn’t find any significant difference in any outcome whatsoever after laparoscopic appendectomy in patients on prehospital antithrombotic therapy,” Dr. Pearcy said.
Specifically, average estimated blood loss was 18 cc in controls vs. 22 cc in patients on antithrombotics, and mortality was 0% in the former vs. 1% in the latter. Patients on antithrombotics had a lower rate of complications: 3% vs. 11%.
Dr. Pearcy discussed a case of a 70-year-old man with acute appendicitis. He had a history of coronary artery disease, hypertension, hyperlipidemia, type 2 diabetes, and stroke, and was taking clopidogrel and aspirin daily.
“Is it safe to proceed with surgery given this patient’s irreversible antithrombotic therapy? We would say yes,” he said.
Dr. Pearcy reported having no financial disclosures.
HOUSTON – Few studies have looked at the risk of irreversible antithrombotic therapy in patients who need emergent or urgent laparoscopic appendectomy, but a new study showed that the operation poses no significantly greater risk for such patients, compared with people who are not on antithrombotics.
The study’s findings do not apply to all patients on anticoagulation, specifically those on new novel oral anticoagulants (NOACs), said Christopher Pearcy, MD, of Methodist Dallas Medical Center.
NOAC agents include dabigatran, rivaroxaban, and apixaban.
Appendicitis is the third most common indication for abdominal surgery in the elderly, Dr. Pearcy noted, and their mortality rates are eight times greater than those of younger patients. However, these patients often proceed to operation with minimal workup, “given that laparoscopic appendectomy is a relatively benign procedure,” he said at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
The retrospective study evaluated two groups of 195 patients who had urgent or emergent laparoscopic appendectomy at three centers from 2010 to 2014. One group was on irreversible antithrombotic therapy, and the other served as controls.
The primary outcomes were blood loss, transfusion requirement, and mortality. Secondary outcomes were duration of operation, length of hospital stay, rates of infections, complications, and 30-day readmissions.
“Compared with controls, we didn’t find any significant difference in any outcome whatsoever after laparoscopic appendectomy in patients on prehospital antithrombotic therapy,” Dr. Pearcy said.
Specifically, average estimated blood loss was 18 cc in controls vs. 22 cc in patients on antithrombotics, and mortality was 0% in the former vs. 1% in the latter. Patients on antithrombotics had a lower rate of complications: 3% vs. 11%.
Dr. Pearcy discussed a case of a 70-year-old man with acute appendicitis. He had a history of coronary artery disease, hypertension, hyperlipidemia, type 2 diabetes, and stroke, and was taking clopidogrel and aspirin daily.
“Is it safe to proceed with surgery given this patient’s irreversible antithrombotic therapy? We would say yes,” he said.
Dr. Pearcy reported having no financial disclosures.
AT SAGES 2017
Key clinical point: Emergent laparoscopic appendectomy poses no significant risk for patients on irreversible antithrombotic therapy.
Major finding: Average estimated blood loss was 18 cc in controls vs. 22 cc in patients on antithrombotics, and mortality was 0% vs. 1%, respectively.
Data source: A retrospective study of 390 patients who had urgent or emergent laparoscopic appendectomy at three centers from 2010 to 2014.
Disclosures: Dr. Pearcy reported having no financial disclosures.
Series supports viability of ambulatory laparoscopic sleeve gastrectomy
HOUSTON – An ambulatory approach to laparoscopic sleeve gastrectomy is a safe and viable option to improve patient satisfaction and soften the economic blow of these procedures on patients, based on a large series at one surgery center in Cincinnati.
“With proper patient selection, utilization of enhanced recovery pathways with an overall low readmission rate and the complication profile point to the feasibility of laparoscopic sleeve gastrectomy [LSG] as a safe outpatient procedure,” said Sepehr Lalezari, MD, now a surgical fellow at Johns Hopkins University, Baltimore.
About 105,000 LSG operations were performed in the United States in 2015, representing 54% of all bariatric operations, according to the American Society for Metabolic and Bariatric Surgery.
Patient selection and strict adherence to protocols are keys to success for ambulatory LSG, Dr. Lalezari said. Suitable patients were found to be ambulatory, between ages 18 and 65 years; had a body mass index (BMI) less than 55 kg/m2 for males and less than 60 kg/m2 for females; weighed less than 500 lb; had an American Society of Anesthesiologists’ classification score less than 4; and had no significant cardiopulmonary impairment, had no history of renal failure or organ transplant, and were not on a transplant wait list.
In this series, 71% of patients (579) were female, and the average BMI was 43. The total complication rate was 2.3% (19); 17 of these patients required hospital admission.
Postoperative complications included gastric leaks (seven, 0.9%); intra-abdominal abscess requiring percutaneous drainage (four, 0.5%); dehydration, nausea, and/or vomiting (four, 0.5%); and one of each of the following: acute cholecystitis, postoperative bleeding, surgical site infection (SSI), and portal vein thrombosis/pulmonary embolism.
The two complications managed on an outpatient basis were the SSI and one intra-abdominal abscess, Dr. Lalezari said.
“The only readmissions in our series that could have been possibly prevented with an overnight stay in the hospital were the four cases of nausea, vomiting, and/or dehydration,” he said. “These only accounted for 0.5% of the total cases performed.”
The readmission rates for ambulatory LSG in this series compared favorably with large trials that did not distinguish between ambulatory and inpatient LSG procedures, Dr. Lalezari noted. A 2016 analysis of 35,655 patients in the American College of Surgeons National Surgical Quality Improvement Program database reported a readmission rate of 3.7% for LSG (Surg Endosc. 2016 Jun;30[6]:2342-50).
A larger study of 130,000 patients who had bariatric surgery reported an LSG readmission rate of 2.8% (Ann Surg. 2016 Nov 15. doi: 10.1097/SLA.0000000000002079). The most common cause for readmissions these trials reported were nausea, vomiting, and/or dehydration.
Bariatric surgeons have embraced enhanced recovery pathways and fast-track surgery, with good results, Dr. Lalezari said, citing work by Zhamak Khorgami, MD, and colleagues at the Cleveland Clinic (Surg Obes Relat Dis. 2017 Feb;13[2]:273-80).
“Looking at fast-track surgery, they found that patients discharged on postoperative day 1 vs. day 2 or 3 did not change outcomes”; those discharged later than postoperative day 1 trended toward a higher readmission rate of 2.8% vs. 3.6%, Dr. Lalezari said.
The enhanced recovery/fast track protocol Dr. Lalezari and his coauthors used involves placing intravenous lines and infusing 1 L crystalloid before starting the procedure, and administration of famotidine and metoclopramide prior to anesthesia. The protocol utilizes sequential compression devices and avoids Foley catheters and intra-abdominal drains. Patients receive dexamethasone and ondansetron during the operation. The protocol emphasizes early ambulation and resumption of oral intake.
The operation uses a 36-French bougie starting about 5 cm from the pylorus, and all staple lines are reinforced with buttress material. At the end of the surgery, all incisions are infiltrated with 30 cc of 0.5% bupivacaine with epinephrine.
Patients are ambulating about 90 minutes after surgery and are monitored for 3-4 hours. They receive a total volume of 3-4 L crystalloids. When they’re tolerating clear liquids, voiding spontaneously, and walking independently, and their pain is well controlled (pain score less than 5/10) and vital signs are within normal limits, they’re discharged.
Postoperative follow-up involves a call at 48 hours and in-clinic follow-up at weeks 1 and 4. Additional follow-up is scheduled at 3-month intervals for 1 year, then at 6 months for up to 2 years, and then yearly afterward.
“With proper patient selection and utilization of enhanced recovery pathways, the low overall readmission rate (2.1%) and complication profile (2.3%) in our series point to the feasibility of laparoscopic sleeve gastrectomy as a safe outpatient procedure,” Dr. Lalezari said.
He reported having no relevant financial disclosures.
HOUSTON – An ambulatory approach to laparoscopic sleeve gastrectomy is a safe and viable option to improve patient satisfaction and soften the economic blow of these procedures on patients, based on a large series at one surgery center in Cincinnati.
“With proper patient selection, utilization of enhanced recovery pathways with an overall low readmission rate and the complication profile point to the feasibility of laparoscopic sleeve gastrectomy [LSG] as a safe outpatient procedure,” said Sepehr Lalezari, MD, now a surgical fellow at Johns Hopkins University, Baltimore.
About 105,000 LSG operations were performed in the United States in 2015, representing 54% of all bariatric operations, according to the American Society for Metabolic and Bariatric Surgery.
Patient selection and strict adherence to protocols are keys to success for ambulatory LSG, Dr. Lalezari said. Suitable patients were found to be ambulatory, between ages 18 and 65 years; had a body mass index (BMI) less than 55 kg/m2 for males and less than 60 kg/m2 for females; weighed less than 500 lb; had an American Society of Anesthesiologists’ classification score less than 4; and had no significant cardiopulmonary impairment, had no history of renal failure or organ transplant, and were not on a transplant wait list.
In this series, 71% of patients (579) were female, and the average BMI was 43. The total complication rate was 2.3% (19); 17 of these patients required hospital admission.
Postoperative complications included gastric leaks (seven, 0.9%); intra-abdominal abscess requiring percutaneous drainage (four, 0.5%); dehydration, nausea, and/or vomiting (four, 0.5%); and one of each of the following: acute cholecystitis, postoperative bleeding, surgical site infection (SSI), and portal vein thrombosis/pulmonary embolism.
The two complications managed on an outpatient basis were the SSI and one intra-abdominal abscess, Dr. Lalezari said.
“The only readmissions in our series that could have been possibly prevented with an overnight stay in the hospital were the four cases of nausea, vomiting, and/or dehydration,” he said. “These only accounted for 0.5% of the total cases performed.”
The readmission rates for ambulatory LSG in this series compared favorably with large trials that did not distinguish between ambulatory and inpatient LSG procedures, Dr. Lalezari noted. A 2016 analysis of 35,655 patients in the American College of Surgeons National Surgical Quality Improvement Program database reported a readmission rate of 3.7% for LSG (Surg Endosc. 2016 Jun;30[6]:2342-50).
A larger study of 130,000 patients who had bariatric surgery reported an LSG readmission rate of 2.8% (Ann Surg. 2016 Nov 15. doi: 10.1097/SLA.0000000000002079). The most common cause for readmissions these trials reported were nausea, vomiting, and/or dehydration.
Bariatric surgeons have embraced enhanced recovery pathways and fast-track surgery, with good results, Dr. Lalezari said, citing work by Zhamak Khorgami, MD, and colleagues at the Cleveland Clinic (Surg Obes Relat Dis. 2017 Feb;13[2]:273-80).
“Looking at fast-track surgery, they found that patients discharged on postoperative day 1 vs. day 2 or 3 did not change outcomes”; those discharged later than postoperative day 1 trended toward a higher readmission rate of 2.8% vs. 3.6%, Dr. Lalezari said.
The enhanced recovery/fast track protocol Dr. Lalezari and his coauthors used involves placing intravenous lines and infusing 1 L crystalloid before starting the procedure, and administration of famotidine and metoclopramide prior to anesthesia. The protocol utilizes sequential compression devices and avoids Foley catheters and intra-abdominal drains. Patients receive dexamethasone and ondansetron during the operation. The protocol emphasizes early ambulation and resumption of oral intake.
The operation uses a 36-French bougie starting about 5 cm from the pylorus, and all staple lines are reinforced with buttress material. At the end of the surgery, all incisions are infiltrated with 30 cc of 0.5% bupivacaine with epinephrine.
Patients are ambulating about 90 minutes after surgery and are monitored for 3-4 hours. They receive a total volume of 3-4 L crystalloids. When they’re tolerating clear liquids, voiding spontaneously, and walking independently, and their pain is well controlled (pain score less than 5/10) and vital signs are within normal limits, they’re discharged.
Postoperative follow-up involves a call at 48 hours and in-clinic follow-up at weeks 1 and 4. Additional follow-up is scheduled at 3-month intervals for 1 year, then at 6 months for up to 2 years, and then yearly afterward.
“With proper patient selection and utilization of enhanced recovery pathways, the low overall readmission rate (2.1%) and complication profile (2.3%) in our series point to the feasibility of laparoscopic sleeve gastrectomy as a safe outpatient procedure,” Dr. Lalezari said.
He reported having no relevant financial disclosures.
HOUSTON – An ambulatory approach to laparoscopic sleeve gastrectomy is a safe and viable option to improve patient satisfaction and soften the economic blow of these procedures on patients, based on a large series at one surgery center in Cincinnati.
“With proper patient selection, utilization of enhanced recovery pathways with an overall low readmission rate and the complication profile point to the feasibility of laparoscopic sleeve gastrectomy [LSG] as a safe outpatient procedure,” said Sepehr Lalezari, MD, now a surgical fellow at Johns Hopkins University, Baltimore.
About 105,000 LSG operations were performed in the United States in 2015, representing 54% of all bariatric operations, according to the American Society for Metabolic and Bariatric Surgery.
Patient selection and strict adherence to protocols are keys to success for ambulatory LSG, Dr. Lalezari said. Suitable patients were found to be ambulatory, between ages 18 and 65 years; had a body mass index (BMI) less than 55 kg/m2 for males and less than 60 kg/m2 for females; weighed less than 500 lb; had an American Society of Anesthesiologists’ classification score less than 4; and had no significant cardiopulmonary impairment, had no history of renal failure or organ transplant, and were not on a transplant wait list.
In this series, 71% of patients (579) were female, and the average BMI was 43. The total complication rate was 2.3% (19); 17 of these patients required hospital admission.
Postoperative complications included gastric leaks (seven, 0.9%); intra-abdominal abscess requiring percutaneous drainage (four, 0.5%); dehydration, nausea, and/or vomiting (four, 0.5%); and one of each of the following: acute cholecystitis, postoperative bleeding, surgical site infection (SSI), and portal vein thrombosis/pulmonary embolism.
The two complications managed on an outpatient basis were the SSI and one intra-abdominal abscess, Dr. Lalezari said.
“The only readmissions in our series that could have been possibly prevented with an overnight stay in the hospital were the four cases of nausea, vomiting, and/or dehydration,” he said. “These only accounted for 0.5% of the total cases performed.”
The readmission rates for ambulatory LSG in this series compared favorably with large trials that did not distinguish between ambulatory and inpatient LSG procedures, Dr. Lalezari noted. A 2016 analysis of 35,655 patients in the American College of Surgeons National Surgical Quality Improvement Program database reported a readmission rate of 3.7% for LSG (Surg Endosc. 2016 Jun;30[6]:2342-50).
A larger study of 130,000 patients who had bariatric surgery reported an LSG readmission rate of 2.8% (Ann Surg. 2016 Nov 15. doi: 10.1097/SLA.0000000000002079). The most common cause for readmissions these trials reported were nausea, vomiting, and/or dehydration.
Bariatric surgeons have embraced enhanced recovery pathways and fast-track surgery, with good results, Dr. Lalezari said, citing work by Zhamak Khorgami, MD, and colleagues at the Cleveland Clinic (Surg Obes Relat Dis. 2017 Feb;13[2]:273-80).
“Looking at fast-track surgery, they found that patients discharged on postoperative day 1 vs. day 2 or 3 did not change outcomes”; those discharged later than postoperative day 1 trended toward a higher readmission rate of 2.8% vs. 3.6%, Dr. Lalezari said.
The enhanced recovery/fast track protocol Dr. Lalezari and his coauthors used involves placing intravenous lines and infusing 1 L crystalloid before starting the procedure, and administration of famotidine and metoclopramide prior to anesthesia. The protocol utilizes sequential compression devices and avoids Foley catheters and intra-abdominal drains. Patients receive dexamethasone and ondansetron during the operation. The protocol emphasizes early ambulation and resumption of oral intake.
The operation uses a 36-French bougie starting about 5 cm from the pylorus, and all staple lines are reinforced with buttress material. At the end of the surgery, all incisions are infiltrated with 30 cc of 0.5% bupivacaine with epinephrine.
Patients are ambulating about 90 minutes after surgery and are monitored for 3-4 hours. They receive a total volume of 3-4 L crystalloids. When they’re tolerating clear liquids, voiding spontaneously, and walking independently, and their pain is well controlled (pain score less than 5/10) and vital signs are within normal limits, they’re discharged.
Postoperative follow-up involves a call at 48 hours and in-clinic follow-up at weeks 1 and 4. Additional follow-up is scheduled at 3-month intervals for 1 year, then at 6 months for up to 2 years, and then yearly afterward.
“With proper patient selection and utilization of enhanced recovery pathways, the low overall readmission rate (2.1%) and complication profile (2.3%) in our series point to the feasibility of laparoscopic sleeve gastrectomy as a safe outpatient procedure,” Dr. Lalezari said.
He reported having no relevant financial disclosures.
AT SAGES 2017
Key clinical point: Laparoscopic sleeve gastrectomy is a safe outpatient procedure – with strict adherence to enhanced recovery pathways and fast-track protocols.
Major finding: This series reported an overall readmission rate of 2.1% and a complication rate of 2.3% in patients who had outpatient LSG.
Data source: A retrospective review of 821 patients who had ambulatory LSG by a single surgeon from 2011 to 2015.
Disclosures: Dr. Lalezari reported having no relevant financial disclosures.
Same-day discharge for lap hiatal procedures found feasible, safe
HOUSTON – Selected patients who need operations, such as paraesophageal hernia repair and Heller myotomy, for benign hiatal diseases can have laparoscopic outpatient procedures with outcomes comparable with those of inpatients, a Canadian retrospective cohort study found.
“When comparing planned day-case patients with those who had planned admissions, we found that postoperative complication was the only statistically significant different outcome. Our data show same-day discharge resulted in no postoperative mortality, and no difference in postoperative morbidity, emergency room visits, and readmissions compared to traditional inpatient care,” said Juan Carlos Molina, MD, of McGill University Health Centre in Montreal, reporting the study results at the annual meeting of the American Society of Gastrointestinal and Endoscopic Surgeons.
The McGill researchers analyzed outcomes for 261 patients who had laparoscopic hiatal procedures from April 2011 to August 2016 – 163 as inpatients, 98 as outpatients, whom the study called planned day-case patients. The outpatient cohort consisted of younger patients (aged 60 vs. 66 years), but otherwise demographics between the two cohorts were similar. Discharge requirements after same-day hiatal procedures were the same as those for other outpatient procedures, Dr. Molina said.
The procedures included primary or revisional paraesophageal hernia repair (PEHR) in 123 (47.1%) patients; Heller myotomy in 94 (36%), 9 of which also underwent resection of an epiphrenic diverticulum; and Nissen fundoplication for gastroesophageal reflux disease in 44 (16.9%), of which 20 (45.5%) had a concomitant type I hiatal hernia. Among PEHR patients, 90% were at least type III.
“We include complex cases, such as revisional surgery, massive paraesophageal hernias, patients who had previous treatments for achalasia before surgery, or concurrent epiphrenic diverticulum resection,” Dr. Molina said. “To our knowledge, this report is the first to describe successful outpatient surgery in these complex patients, with comparable outcomes to admitted patients and to those described for more well-established outpatient procedures.”
The overall success rate of planned day surgery was 81.6%. Of the 18 unplanned admissions, patient preference to stay in the hospital and pain were the most common factors. Dr. Molina-Franjola said, “We identified factors that might be predictors of unplanned admission, and we found that female [sex], intraoperative complication, postoperative complications, and procedure performed in the afternoon were significant risk factors.”
Women accounted for 94.4% of the unplanned admissions after outpatient surgery, and PEHR/fundoplication represented 72.2% of unplanned admissions. No day-case patients with unplanned admission group required a reoperation within 30 days, although one who did not have an unplanned admission did.
With time, the share of outpatient procedures increased, Dr. Molina said. “In 2011, around 10% of procedures were day-case and that increased progressively to 67% in 2016,” he said.
Dr. Molina said that patients were sent home with antinauseates and instructions to call immediately if nausea or vomiting ensued. About 5% of outpatients returned for reflux, nausea, or vomiting, he said.
Dr. Molina reported having no financial disclosures.
HOUSTON – Selected patients who need operations, such as paraesophageal hernia repair and Heller myotomy, for benign hiatal diseases can have laparoscopic outpatient procedures with outcomes comparable with those of inpatients, a Canadian retrospective cohort study found.
“When comparing planned day-case patients with those who had planned admissions, we found that postoperative complication was the only statistically significant different outcome. Our data show same-day discharge resulted in no postoperative mortality, and no difference in postoperative morbidity, emergency room visits, and readmissions compared to traditional inpatient care,” said Juan Carlos Molina, MD, of McGill University Health Centre in Montreal, reporting the study results at the annual meeting of the American Society of Gastrointestinal and Endoscopic Surgeons.
The McGill researchers analyzed outcomes for 261 patients who had laparoscopic hiatal procedures from April 2011 to August 2016 – 163 as inpatients, 98 as outpatients, whom the study called planned day-case patients. The outpatient cohort consisted of younger patients (aged 60 vs. 66 years), but otherwise demographics between the two cohorts were similar. Discharge requirements after same-day hiatal procedures were the same as those for other outpatient procedures, Dr. Molina said.
The procedures included primary or revisional paraesophageal hernia repair (PEHR) in 123 (47.1%) patients; Heller myotomy in 94 (36%), 9 of which also underwent resection of an epiphrenic diverticulum; and Nissen fundoplication for gastroesophageal reflux disease in 44 (16.9%), of which 20 (45.5%) had a concomitant type I hiatal hernia. Among PEHR patients, 90% were at least type III.
“We include complex cases, such as revisional surgery, massive paraesophageal hernias, patients who had previous treatments for achalasia before surgery, or concurrent epiphrenic diverticulum resection,” Dr. Molina said. “To our knowledge, this report is the first to describe successful outpatient surgery in these complex patients, with comparable outcomes to admitted patients and to those described for more well-established outpatient procedures.”
The overall success rate of planned day surgery was 81.6%. Of the 18 unplanned admissions, patient preference to stay in the hospital and pain were the most common factors. Dr. Molina-Franjola said, “We identified factors that might be predictors of unplanned admission, and we found that female [sex], intraoperative complication, postoperative complications, and procedure performed in the afternoon were significant risk factors.”
Women accounted for 94.4% of the unplanned admissions after outpatient surgery, and PEHR/fundoplication represented 72.2% of unplanned admissions. No day-case patients with unplanned admission group required a reoperation within 30 days, although one who did not have an unplanned admission did.
With time, the share of outpatient procedures increased, Dr. Molina said. “In 2011, around 10% of procedures were day-case and that increased progressively to 67% in 2016,” he said.
Dr. Molina said that patients were sent home with antinauseates and instructions to call immediately if nausea or vomiting ensued. About 5% of outpatients returned for reflux, nausea, or vomiting, he said.
Dr. Molina reported having no financial disclosures.
HOUSTON – Selected patients who need operations, such as paraesophageal hernia repair and Heller myotomy, for benign hiatal diseases can have laparoscopic outpatient procedures with outcomes comparable with those of inpatients, a Canadian retrospective cohort study found.
“When comparing planned day-case patients with those who had planned admissions, we found that postoperative complication was the only statistically significant different outcome. Our data show same-day discharge resulted in no postoperative mortality, and no difference in postoperative morbidity, emergency room visits, and readmissions compared to traditional inpatient care,” said Juan Carlos Molina, MD, of McGill University Health Centre in Montreal, reporting the study results at the annual meeting of the American Society of Gastrointestinal and Endoscopic Surgeons.
The McGill researchers analyzed outcomes for 261 patients who had laparoscopic hiatal procedures from April 2011 to August 2016 – 163 as inpatients, 98 as outpatients, whom the study called planned day-case patients. The outpatient cohort consisted of younger patients (aged 60 vs. 66 years), but otherwise demographics between the two cohorts were similar. Discharge requirements after same-day hiatal procedures were the same as those for other outpatient procedures, Dr. Molina said.
The procedures included primary or revisional paraesophageal hernia repair (PEHR) in 123 (47.1%) patients; Heller myotomy in 94 (36%), 9 of which also underwent resection of an epiphrenic diverticulum; and Nissen fundoplication for gastroesophageal reflux disease in 44 (16.9%), of which 20 (45.5%) had a concomitant type I hiatal hernia. Among PEHR patients, 90% were at least type III.
“We include complex cases, such as revisional surgery, massive paraesophageal hernias, patients who had previous treatments for achalasia before surgery, or concurrent epiphrenic diverticulum resection,” Dr. Molina said. “To our knowledge, this report is the first to describe successful outpatient surgery in these complex patients, with comparable outcomes to admitted patients and to those described for more well-established outpatient procedures.”
The overall success rate of planned day surgery was 81.6%. Of the 18 unplanned admissions, patient preference to stay in the hospital and pain were the most common factors. Dr. Molina-Franjola said, “We identified factors that might be predictors of unplanned admission, and we found that female [sex], intraoperative complication, postoperative complications, and procedure performed in the afternoon were significant risk factors.”
Women accounted for 94.4% of the unplanned admissions after outpatient surgery, and PEHR/fundoplication represented 72.2% of unplanned admissions. No day-case patients with unplanned admission group required a reoperation within 30 days, although one who did not have an unplanned admission did.
With time, the share of outpatient procedures increased, Dr. Molina said. “In 2011, around 10% of procedures were day-case and that increased progressively to 67% in 2016,” he said.
Dr. Molina said that patients were sent home with antinauseates and instructions to call immediately if nausea or vomiting ensued. About 5% of outpatients returned for reflux, nausea, or vomiting, he said.
Dr. Molina reported having no financial disclosures.
AT SAGES 2017
Key clinical point: Same-day surgery for benign laparoscopic hiatal procedures have outcomes comparable with those of inpatient procedures.
Major finding: Postoperative complications were 9.2% for outpatient operations vs. 19% for inpatient, and 81.7% of patients who had same-day surgery did not have an unplanned admission.
Data source: Retrospective single-center study of 261 patients who had inpatient and outpatient laparoscopic hiatal procedures from April 2011 to August 2016.
Disclosures: Dr. Molina-Franjola reported having no financial disclosures.
Transanal TME comparable to open, lap approaches to rectal cancer
HOUSTON – Transanal total mesorectal excision can consistently achieve good pathological results for obtaining specimens in rectal cancer, and overcome the shortcomings of the open and laparoscopic approaches to rectal cancer surgery, particularly in the distal part of the rectum where obtaining quality specimens can be technically challenging, researchers at the Hospital Clinic of Barcelona have found.
Reporting at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons, Jacqueline van Laarhoven, MD, PhD, said, “Pathologically, transanal total mesorectal excision [TME] provides good results on integrity of the mesorectum, negative circumferential and distal resection margins, and lymph nodes per specimen.” This study represents the first results of a relatively large, single-institution cohort, Dr. van Laarhoven said.
The study involved 187 patients with mid- or low-rectal cancer who had transanal TME from November 2011 to June 2016. Dr. van Laarhoven explained that obtaining high-quality specimens is an important prognostic factor for determining locoregional recurrence in rectal cancer. The study analyzed results of excised specimens in the mesorectum, circumferential and distal resected margins, and lymph nodes, and compared outcomes with those in two randomized clinical trials of both open and laparoscopic TME – the COLOR II (Lancet Oncol. 2013;14:210-8) and COREAN trials (Lancet Oncol. 2014;15:767-74) – where applicable.
In the Barcelona study population, 63.1% had tumors in the midrectum and 36.9% in the low rectum. Transanal TME yielded complete mesorectal quality in 95.7% of cases, almost-complete quality in 1.6% and incomplete in 1.1%, but comparison with COLOR II and COREAN trials was difficult because of differing inclusion criteria, Dr. van Laarhoven said.
Mean distal margin was 2.1 cm in midrectal cancer with a positive distal resection margin in 3.2%. In low-rectal cancer, the mean distal margin was 1.1 cm with a positive distal resection margin in 7.8%. Dr. van Laarhoven noted the overall circumferential resection margin (CRM) was 8.6% in this study, compared with 8.3% overall for the COREAN trial. As for COLOR II, the overall rate for positive CRM in mid- and low-rectal tumors was around 9%, Dr. van Laarhoven said, but in the open group the positive CRM was 3% in the midrectal excisions and 22% in low-rectal disease.
With regard to lymph nodes, the Barcelona study reported a median of 14 per specimen, with a range of 11 to 18, Dr. van Laarhoven said. However, in nonirradiated patients, the median was 15 per specimen. “This is consistent with the fact that neoadjuvant radiotherapy leads to a decrease in the lymph-node harvest,” she said. “These results are comparable to the COREAN and the COLOR II trials.”
Sixty-two percent of patients received neoadjuvant chemoradiotherapy, 3.2% received radiotherapy only, and 2.1% chemotherapy only.
On preoperative staging, 3.2% had T1 tumors, 20.3% T2, 67.9% T3, and 7.5% T4. The overall positive CRM (less than 1 mm) was 8.6% (including T4 tumors).
Postoperative pathological staging showed complete remission in 16% of patients, pT1 in 6.4%, pT2 in 28.9%, pT3 in 42.8%, pT4 in 2.7%, and pTis in 1.6%.
Dr. van Laarhoven commented, “As the quality of the surgical treatment is a surrogate marker for survival, transanal TME can be regarded as an oncologically safe method to treat patients with rectal cancer.”
Dr. van Laarhoven reported having no financial disclosures.
HOUSTON – Transanal total mesorectal excision can consistently achieve good pathological results for obtaining specimens in rectal cancer, and overcome the shortcomings of the open and laparoscopic approaches to rectal cancer surgery, particularly in the distal part of the rectum where obtaining quality specimens can be technically challenging, researchers at the Hospital Clinic of Barcelona have found.
Reporting at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons, Jacqueline van Laarhoven, MD, PhD, said, “Pathologically, transanal total mesorectal excision [TME] provides good results on integrity of the mesorectum, negative circumferential and distal resection margins, and lymph nodes per specimen.” This study represents the first results of a relatively large, single-institution cohort, Dr. van Laarhoven said.
The study involved 187 patients with mid- or low-rectal cancer who had transanal TME from November 2011 to June 2016. Dr. van Laarhoven explained that obtaining high-quality specimens is an important prognostic factor for determining locoregional recurrence in rectal cancer. The study analyzed results of excised specimens in the mesorectum, circumferential and distal resected margins, and lymph nodes, and compared outcomes with those in two randomized clinical trials of both open and laparoscopic TME – the COLOR II (Lancet Oncol. 2013;14:210-8) and COREAN trials (Lancet Oncol. 2014;15:767-74) – where applicable.
In the Barcelona study population, 63.1% had tumors in the midrectum and 36.9% in the low rectum. Transanal TME yielded complete mesorectal quality in 95.7% of cases, almost-complete quality in 1.6% and incomplete in 1.1%, but comparison with COLOR II and COREAN trials was difficult because of differing inclusion criteria, Dr. van Laarhoven said.
Mean distal margin was 2.1 cm in midrectal cancer with a positive distal resection margin in 3.2%. In low-rectal cancer, the mean distal margin was 1.1 cm with a positive distal resection margin in 7.8%. Dr. van Laarhoven noted the overall circumferential resection margin (CRM) was 8.6% in this study, compared with 8.3% overall for the COREAN trial. As for COLOR II, the overall rate for positive CRM in mid- and low-rectal tumors was around 9%, Dr. van Laarhoven said, but in the open group the positive CRM was 3% in the midrectal excisions and 22% in low-rectal disease.
With regard to lymph nodes, the Barcelona study reported a median of 14 per specimen, with a range of 11 to 18, Dr. van Laarhoven said. However, in nonirradiated patients, the median was 15 per specimen. “This is consistent with the fact that neoadjuvant radiotherapy leads to a decrease in the lymph-node harvest,” she said. “These results are comparable to the COREAN and the COLOR II trials.”
Sixty-two percent of patients received neoadjuvant chemoradiotherapy, 3.2% received radiotherapy only, and 2.1% chemotherapy only.
On preoperative staging, 3.2% had T1 tumors, 20.3% T2, 67.9% T3, and 7.5% T4. The overall positive CRM (less than 1 mm) was 8.6% (including T4 tumors).
Postoperative pathological staging showed complete remission in 16% of patients, pT1 in 6.4%, pT2 in 28.9%, pT3 in 42.8%, pT4 in 2.7%, and pTis in 1.6%.
Dr. van Laarhoven commented, “As the quality of the surgical treatment is a surrogate marker for survival, transanal TME can be regarded as an oncologically safe method to treat patients with rectal cancer.”
Dr. van Laarhoven reported having no financial disclosures.
HOUSTON – Transanal total mesorectal excision can consistently achieve good pathological results for obtaining specimens in rectal cancer, and overcome the shortcomings of the open and laparoscopic approaches to rectal cancer surgery, particularly in the distal part of the rectum where obtaining quality specimens can be technically challenging, researchers at the Hospital Clinic of Barcelona have found.
Reporting at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons, Jacqueline van Laarhoven, MD, PhD, said, “Pathologically, transanal total mesorectal excision [TME] provides good results on integrity of the mesorectum, negative circumferential and distal resection margins, and lymph nodes per specimen.” This study represents the first results of a relatively large, single-institution cohort, Dr. van Laarhoven said.
The study involved 187 patients with mid- or low-rectal cancer who had transanal TME from November 2011 to June 2016. Dr. van Laarhoven explained that obtaining high-quality specimens is an important prognostic factor for determining locoregional recurrence in rectal cancer. The study analyzed results of excised specimens in the mesorectum, circumferential and distal resected margins, and lymph nodes, and compared outcomes with those in two randomized clinical trials of both open and laparoscopic TME – the COLOR II (Lancet Oncol. 2013;14:210-8) and COREAN trials (Lancet Oncol. 2014;15:767-74) – where applicable.
In the Barcelona study population, 63.1% had tumors in the midrectum and 36.9% in the low rectum. Transanal TME yielded complete mesorectal quality in 95.7% of cases, almost-complete quality in 1.6% and incomplete in 1.1%, but comparison with COLOR II and COREAN trials was difficult because of differing inclusion criteria, Dr. van Laarhoven said.
Mean distal margin was 2.1 cm in midrectal cancer with a positive distal resection margin in 3.2%. In low-rectal cancer, the mean distal margin was 1.1 cm with a positive distal resection margin in 7.8%. Dr. van Laarhoven noted the overall circumferential resection margin (CRM) was 8.6% in this study, compared with 8.3% overall for the COREAN trial. As for COLOR II, the overall rate for positive CRM in mid- and low-rectal tumors was around 9%, Dr. van Laarhoven said, but in the open group the positive CRM was 3% in the midrectal excisions and 22% in low-rectal disease.
With regard to lymph nodes, the Barcelona study reported a median of 14 per specimen, with a range of 11 to 18, Dr. van Laarhoven said. However, in nonirradiated patients, the median was 15 per specimen. “This is consistent with the fact that neoadjuvant radiotherapy leads to a decrease in the lymph-node harvest,” she said. “These results are comparable to the COREAN and the COLOR II trials.”
Sixty-two percent of patients received neoadjuvant chemoradiotherapy, 3.2% received radiotherapy only, and 2.1% chemotherapy only.
On preoperative staging, 3.2% had T1 tumors, 20.3% T2, 67.9% T3, and 7.5% T4. The overall positive CRM (less than 1 mm) was 8.6% (including T4 tumors).
Postoperative pathological staging showed complete remission in 16% of patients, pT1 in 6.4%, pT2 in 28.9%, pT3 in 42.8%, pT4 in 2.7%, and pTis in 1.6%.
Dr. van Laarhoven commented, “As the quality of the surgical treatment is a surrogate marker for survival, transanal TME can be regarded as an oncologically safe method to treat patients with rectal cancer.”
Dr. van Laarhoven reported having no financial disclosures.
AT SAGES 2017
Key clinical point: Transanal total mesorectal excision (TME) is a viable alternative to open or laparoscopic TME in cancers of the low and midrectum.
Major finding: Postoperative pathological staging showed complete remission in 16%, with pT1 in 6.4%, pT2 in 28.9%, pT3 in 42.8%, pT4 in 2.7%, and pTis in 1.6%.
Data source: Analysis of 187 patients prospectively enrolled in a standardized database who had transanal TME from November 2011 to June 2016 at a single center.
Disclosures: Dr. van Laarhoven reported having no financial disclosures.
Robot-assisted surgery: Twice the price
HOUSTON – Robot-assisted operations for inguinal hernia repair (IHR) and cholecystectomy have grown steadily in recent years, but these procedures can be done equally well by traditional operations at a fraction of the cost, according to a study from Geisinger Medical Center in Pennsylvania.
Ellen Vogels, DO, of Geisinger, reported results of a study of 1,248 cholecystectomies and 723 initial IHRs from 2007 to 2016. The cholecystectomies were done via robot-assisted surgery or laparoscopy in the hospital or via laparoscopy in an ambulatory surgery center (ASC). The IHRs were done robotically, open, or laparoscopically in the hospital, or open or laparoscopically in an ASC.
Dr. Vogels quoted statistics from the ECRI Institute that showed robotic surgery procedures have increased 178% between 2009 and 2014, and the two procedures the group studied are the most frequently performed robotic procedures.
Within the Geisinger system, the study found a 3:1 cost disparity for IHR: $6,292 total cost for hospital-based robotic surgery vs. $3,421 for ASC-based laparoscopy IHR and $1,853 for ASC-based open repair. For cholecystectomy, the disparity isn’t as wide – it’s 2:1 – but is still significant: Total costs for hospital-based robotic surgery are $6,057 vs. $3,443 for ASC-based cholecystectomy and $3,270 for hospital-based laparoscopic cholecystectomy (the study did not include any open cholecystectomies).
Total costs not only include costs for the procedure but also all related pre- and postoperative care. The cost analysis did not account for the cost of the robot, including maintenance contracts, or costs for laparoscopic instruments. Variable costs also ranged from about $3,000 for robotic IHR to $942 for ASC open repair – which means the lowest per-procedure cost for the latter was around $900.
“Translating this into the fact that cholecystectomies and inguinal hernia repairs are the most often performed general surgery procedures, ambulatory surgery centers can save over $60 billion over the next 10 years in just overhead costs as well as increased efficiency,” Dr. Vogels said.
The study also found access issues depending on where patients had their operations. “As far as service and access in our institution alone, we found that patients going to the main hospital spent as much as two times longer getting these procedures done as compared to the ambulatory surgery centers,” Dr. Vogels said.
Robotic procedures also required longer operative times, the study found – an average of 109 minutes for IHR vs. about an hour for ASC procedures and hospital-based open surgery (but averaging 78 minutes for in-hospital laparoscopy); and 73 minutes for robotic cholecystectomy, 60 minutes for hospital laparoscopy, and 45 minutes for ASC laparoscopy.
Robotic session moderator Dmitry Oleynikov, MD, FACS, of the University of Nebraska Medical Center, Omaha, asked Dr. Vogels if putting a robotic platform in an ambulatory surgery setting would make it more cost effective.
That’s not practical from a cost or efficiency perspective, she said.
“When you look at the cost of the ASCs, specifically in the hernia group, the lowest-cost hernia repair is about $800; with the robot it’s going to be significantly higher than that, up to three times higher than that,” Dr. Vogels replied. “Then you’re also changing all those simple ambulatory surgery procedures to more involved robotic procedures, so it’s hard to justify doing that in the ASC.”
Dr. Vogels and her coauthors had no relevant financial disclosures.
HOUSTON – Robot-assisted operations for inguinal hernia repair (IHR) and cholecystectomy have grown steadily in recent years, but these procedures can be done equally well by traditional operations at a fraction of the cost, according to a study from Geisinger Medical Center in Pennsylvania.
Ellen Vogels, DO, of Geisinger, reported results of a study of 1,248 cholecystectomies and 723 initial IHRs from 2007 to 2016. The cholecystectomies were done via robot-assisted surgery or laparoscopy in the hospital or via laparoscopy in an ambulatory surgery center (ASC). The IHRs were done robotically, open, or laparoscopically in the hospital, or open or laparoscopically in an ASC.
Dr. Vogels quoted statistics from the ECRI Institute that showed robotic surgery procedures have increased 178% between 2009 and 2014, and the two procedures the group studied are the most frequently performed robotic procedures.
Within the Geisinger system, the study found a 3:1 cost disparity for IHR: $6,292 total cost for hospital-based robotic surgery vs. $3,421 for ASC-based laparoscopy IHR and $1,853 for ASC-based open repair. For cholecystectomy, the disparity isn’t as wide – it’s 2:1 – but is still significant: Total costs for hospital-based robotic surgery are $6,057 vs. $3,443 for ASC-based cholecystectomy and $3,270 for hospital-based laparoscopic cholecystectomy (the study did not include any open cholecystectomies).
Total costs not only include costs for the procedure but also all related pre- and postoperative care. The cost analysis did not account for the cost of the robot, including maintenance contracts, or costs for laparoscopic instruments. Variable costs also ranged from about $3,000 for robotic IHR to $942 for ASC open repair – which means the lowest per-procedure cost for the latter was around $900.
“Translating this into the fact that cholecystectomies and inguinal hernia repairs are the most often performed general surgery procedures, ambulatory surgery centers can save over $60 billion over the next 10 years in just overhead costs as well as increased efficiency,” Dr. Vogels said.
The study also found access issues depending on where patients had their operations. “As far as service and access in our institution alone, we found that patients going to the main hospital spent as much as two times longer getting these procedures done as compared to the ambulatory surgery centers,” Dr. Vogels said.
Robotic procedures also required longer operative times, the study found – an average of 109 minutes for IHR vs. about an hour for ASC procedures and hospital-based open surgery (but averaging 78 minutes for in-hospital laparoscopy); and 73 minutes for robotic cholecystectomy, 60 minutes for hospital laparoscopy, and 45 minutes for ASC laparoscopy.
Robotic session moderator Dmitry Oleynikov, MD, FACS, of the University of Nebraska Medical Center, Omaha, asked Dr. Vogels if putting a robotic platform in an ambulatory surgery setting would make it more cost effective.
That’s not practical from a cost or efficiency perspective, she said.
“When you look at the cost of the ASCs, specifically in the hernia group, the lowest-cost hernia repair is about $800; with the robot it’s going to be significantly higher than that, up to three times higher than that,” Dr. Vogels replied. “Then you’re also changing all those simple ambulatory surgery procedures to more involved robotic procedures, so it’s hard to justify doing that in the ASC.”
Dr. Vogels and her coauthors had no relevant financial disclosures.
HOUSTON – Robot-assisted operations for inguinal hernia repair (IHR) and cholecystectomy have grown steadily in recent years, but these procedures can be done equally well by traditional operations at a fraction of the cost, according to a study from Geisinger Medical Center in Pennsylvania.
Ellen Vogels, DO, of Geisinger, reported results of a study of 1,248 cholecystectomies and 723 initial IHRs from 2007 to 2016. The cholecystectomies were done via robot-assisted surgery or laparoscopy in the hospital or via laparoscopy in an ambulatory surgery center (ASC). The IHRs were done robotically, open, or laparoscopically in the hospital, or open or laparoscopically in an ASC.
Dr. Vogels quoted statistics from the ECRI Institute that showed robotic surgery procedures have increased 178% between 2009 and 2014, and the two procedures the group studied are the most frequently performed robotic procedures.
Within the Geisinger system, the study found a 3:1 cost disparity for IHR: $6,292 total cost for hospital-based robotic surgery vs. $3,421 for ASC-based laparoscopy IHR and $1,853 for ASC-based open repair. For cholecystectomy, the disparity isn’t as wide – it’s 2:1 – but is still significant: Total costs for hospital-based robotic surgery are $6,057 vs. $3,443 for ASC-based cholecystectomy and $3,270 for hospital-based laparoscopic cholecystectomy (the study did not include any open cholecystectomies).
Total costs not only include costs for the procedure but also all related pre- and postoperative care. The cost analysis did not account for the cost of the robot, including maintenance contracts, or costs for laparoscopic instruments. Variable costs also ranged from about $3,000 for robotic IHR to $942 for ASC open repair – which means the lowest per-procedure cost for the latter was around $900.
“Translating this into the fact that cholecystectomies and inguinal hernia repairs are the most often performed general surgery procedures, ambulatory surgery centers can save over $60 billion over the next 10 years in just overhead costs as well as increased efficiency,” Dr. Vogels said.
The study also found access issues depending on where patients had their operations. “As far as service and access in our institution alone, we found that patients going to the main hospital spent as much as two times longer getting these procedures done as compared to the ambulatory surgery centers,” Dr. Vogels said.
Robotic procedures also required longer operative times, the study found – an average of 109 minutes for IHR vs. about an hour for ASC procedures and hospital-based open surgery (but averaging 78 minutes for in-hospital laparoscopy); and 73 minutes for robotic cholecystectomy, 60 minutes for hospital laparoscopy, and 45 minutes for ASC laparoscopy.
Robotic session moderator Dmitry Oleynikov, MD, FACS, of the University of Nebraska Medical Center, Omaha, asked Dr. Vogels if putting a robotic platform in an ambulatory surgery setting would make it more cost effective.
That’s not practical from a cost or efficiency perspective, she said.
“When you look at the cost of the ASCs, specifically in the hernia group, the lowest-cost hernia repair is about $800; with the robot it’s going to be significantly higher than that, up to three times higher than that,” Dr. Vogels replied. “Then you’re also changing all those simple ambulatory surgery procedures to more involved robotic procedures, so it’s hard to justify doing that in the ASC.”
Dr. Vogels and her coauthors had no relevant financial disclosures.
AT SAGES 2017
Key clinical point: Outcomes for robot-assisted inguinal hernia repair and cholecystectomy are similar to those for outpatient open and laparoscopic procedures.
Major finding: Robotic IHR costs up to three times more than open outpatient surgery, and robotic cholecystectomy costs twice as much as outpatient surgery.
Data source: Study of 1,971 in-hospital robotic, laparoscopic, and open procedures, and outpatient laparoscopic and open operations done from 2007 to 2016 at Geisinger Medical Center.
Disclosures: Dr. Vogels and coauthors reported having no financial disclosures.
Robotics: General surgery goes its own way
HOUSTON – Subspecialties such as urology and gynecology have seen a steady increase in robot-assisted surgery and an offsetting decline in open procedures, but in general surgery, robot-assisted procedures seem to be making gains at the expense of laparoscopy, according to researchers from the University of Nebraska.
In two specific operations, ventral and inguinal hernia repairs (VHR and IHR), the percentage of open procedures has increased or held steady over the 7-year study period while the share of laparoscopic operations declined and robot-assisted surgeries (RAS) increased, Priscila Rodrigues Armijo, MD, reported at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
This shift to RAS rather than laparoscopy could have significant implications because RAS is significantly more costly than laparoscopy, Dr. Armijo said. “In our study, the open procedures were the most expensive, followed by the robot-assisted surgeries and then laparoscopy,” she said. Median direct costs were $14,364 for open procedures, $11,376 for RAS and $7,945 for laparoscopy.
The Nebraska study retrospectively analyzed five different general surgery procedures: colectomy, cholecystectomy, and bariatric procedures in addition to VHR and IHR. The researchers analyzed 857,468 operations entered into the University HealthSystem Consortium Clinical Database Resource Manager from October 2008 to September 2015.
Dr. Armijo explained that the goal was to study trends in general surgery because while several studies have examined trends in urologic and gynecologic surgery, few studies have done so in general surgery.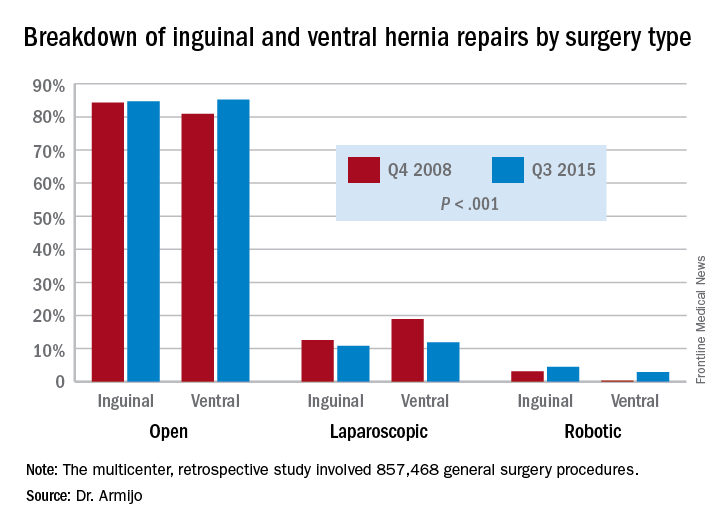
“There was a significant increase in minimally invasive utilizations over time, and robotic surgery increased disproportionately compared to the laparoscope counterpart,” Dr. Armijo said. “And although we cannot prove where those patients are coming from, we believe that, especially for inguinal and ventral hernia repairs, they are coming from laparoscopic surgeons who now are adopting robotic techniques and not from open surgeons switching to the robotic approach.”
In 7 years, the study showed a significant decrease in the share of open procedures in colectomy (from 71.8% to 61.9%), cholecystectomy (35.7% to 27.1%), and bariatric surgery (20.1% to 10.1%), but an increase in both laparoscopic and RAS approaches in these surgeries.
However, in IHR, open procedures held steady at around 84% through the study period, while laparoscopic procedures declined from 12.6% to 10.8% and RAS jumped 3.1% to 4.5%. For VHR, the share of open procedures actually jumped from 80.9% to 85.2%, while the proportion of laparoscopic procedures fell from 18.9% to 11.9% and RAS operations jumped more than tenfold, from 0.2% to 2.9%.
“For ventral hernia repair there was a significant decrease in the laparoscopic approach with a significant increase in both open and robotic procedures, which may be due to new open techniques, including component separation, that have been shown to be more durable as a repair,” Dr. Armijo said. “In addition, those repair techniques are more easily performed with the robotic approach. Laparoscopic surgeons are finding that robotic technology is enabling them to execute surgical tasks, such as suturing mesh.”
Coauthor Dmitry Oleynikov, MD, FACS, disclosed he is a stockholder in Virtual Incision Corp. Dr. Armijo and other coauthors had no financial relationships to disclose.
HOUSTON – Subspecialties such as urology and gynecology have seen a steady increase in robot-assisted surgery and an offsetting decline in open procedures, but in general surgery, robot-assisted procedures seem to be making gains at the expense of laparoscopy, according to researchers from the University of Nebraska.
In two specific operations, ventral and inguinal hernia repairs (VHR and IHR), the percentage of open procedures has increased or held steady over the 7-year study period while the share of laparoscopic operations declined and robot-assisted surgeries (RAS) increased, Priscila Rodrigues Armijo, MD, reported at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
This shift to RAS rather than laparoscopy could have significant implications because RAS is significantly more costly than laparoscopy, Dr. Armijo said. “In our study, the open procedures were the most expensive, followed by the robot-assisted surgeries and then laparoscopy,” she said. Median direct costs were $14,364 for open procedures, $11,376 for RAS and $7,945 for laparoscopy.
The Nebraska study retrospectively analyzed five different general surgery procedures: colectomy, cholecystectomy, and bariatric procedures in addition to VHR and IHR. The researchers analyzed 857,468 operations entered into the University HealthSystem Consortium Clinical Database Resource Manager from October 2008 to September 2015.
Dr. Armijo explained that the goal was to study trends in general surgery because while several studies have examined trends in urologic and gynecologic surgery, few studies have done so in general surgery.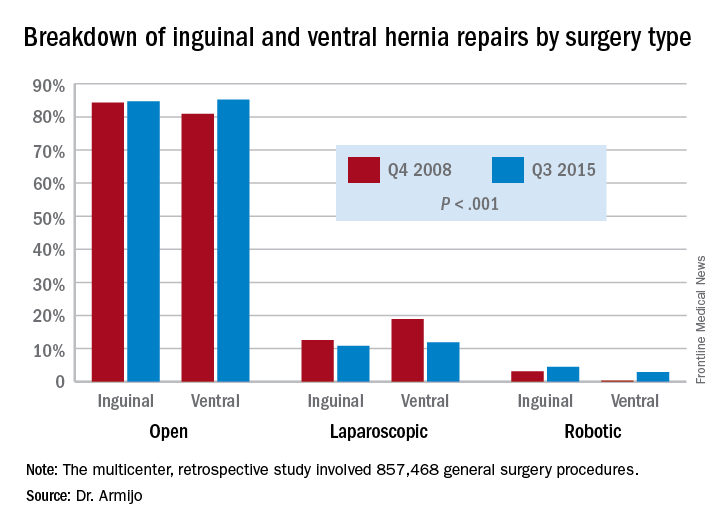
“There was a significant increase in minimally invasive utilizations over time, and robotic surgery increased disproportionately compared to the laparoscope counterpart,” Dr. Armijo said. “And although we cannot prove where those patients are coming from, we believe that, especially for inguinal and ventral hernia repairs, they are coming from laparoscopic surgeons who now are adopting robotic techniques and not from open surgeons switching to the robotic approach.”
In 7 years, the study showed a significant decrease in the share of open procedures in colectomy (from 71.8% to 61.9%), cholecystectomy (35.7% to 27.1%), and bariatric surgery (20.1% to 10.1%), but an increase in both laparoscopic and RAS approaches in these surgeries.
However, in IHR, open procedures held steady at around 84% through the study period, while laparoscopic procedures declined from 12.6% to 10.8% and RAS jumped 3.1% to 4.5%. For VHR, the share of open procedures actually jumped from 80.9% to 85.2%, while the proportion of laparoscopic procedures fell from 18.9% to 11.9% and RAS operations jumped more than tenfold, from 0.2% to 2.9%.
“For ventral hernia repair there was a significant decrease in the laparoscopic approach with a significant increase in both open and robotic procedures, which may be due to new open techniques, including component separation, that have been shown to be more durable as a repair,” Dr. Armijo said. “In addition, those repair techniques are more easily performed with the robotic approach. Laparoscopic surgeons are finding that robotic technology is enabling them to execute surgical tasks, such as suturing mesh.”
Coauthor Dmitry Oleynikov, MD, FACS, disclosed he is a stockholder in Virtual Incision Corp. Dr. Armijo and other coauthors had no financial relationships to disclose.
HOUSTON – Subspecialties such as urology and gynecology have seen a steady increase in robot-assisted surgery and an offsetting decline in open procedures, but in general surgery, robot-assisted procedures seem to be making gains at the expense of laparoscopy, according to researchers from the University of Nebraska.
In two specific operations, ventral and inguinal hernia repairs (VHR and IHR), the percentage of open procedures has increased or held steady over the 7-year study period while the share of laparoscopic operations declined and robot-assisted surgeries (RAS) increased, Priscila Rodrigues Armijo, MD, reported at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
This shift to RAS rather than laparoscopy could have significant implications because RAS is significantly more costly than laparoscopy, Dr. Armijo said. “In our study, the open procedures were the most expensive, followed by the robot-assisted surgeries and then laparoscopy,” she said. Median direct costs were $14,364 for open procedures, $11,376 for RAS and $7,945 for laparoscopy.
The Nebraska study retrospectively analyzed five different general surgery procedures: colectomy, cholecystectomy, and bariatric procedures in addition to VHR and IHR. The researchers analyzed 857,468 operations entered into the University HealthSystem Consortium Clinical Database Resource Manager from October 2008 to September 2015.
Dr. Armijo explained that the goal was to study trends in general surgery because while several studies have examined trends in urologic and gynecologic surgery, few studies have done so in general surgery.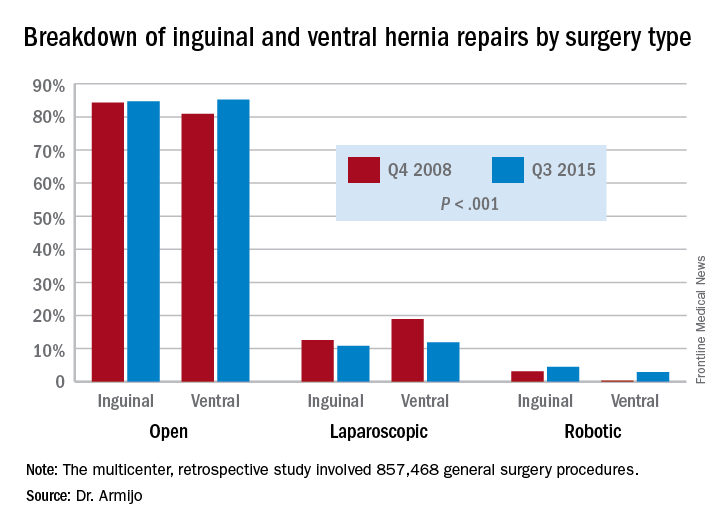
“There was a significant increase in minimally invasive utilizations over time, and robotic surgery increased disproportionately compared to the laparoscope counterpart,” Dr. Armijo said. “And although we cannot prove where those patients are coming from, we believe that, especially for inguinal and ventral hernia repairs, they are coming from laparoscopic surgeons who now are adopting robotic techniques and not from open surgeons switching to the robotic approach.”
In 7 years, the study showed a significant decrease in the share of open procedures in colectomy (from 71.8% to 61.9%), cholecystectomy (35.7% to 27.1%), and bariatric surgery (20.1% to 10.1%), but an increase in both laparoscopic and RAS approaches in these surgeries.
However, in IHR, open procedures held steady at around 84% through the study period, while laparoscopic procedures declined from 12.6% to 10.8% and RAS jumped 3.1% to 4.5%. For VHR, the share of open procedures actually jumped from 80.9% to 85.2%, while the proportion of laparoscopic procedures fell from 18.9% to 11.9% and RAS operations jumped more than tenfold, from 0.2% to 2.9%.
“For ventral hernia repair there was a significant decrease in the laparoscopic approach with a significant increase in both open and robotic procedures, which may be due to new open techniques, including component separation, that have been shown to be more durable as a repair,” Dr. Armijo said. “In addition, those repair techniques are more easily performed with the robotic approach. Laparoscopic surgeons are finding that robotic technology is enabling them to execute surgical tasks, such as suturing mesh.”
Coauthor Dmitry Oleynikov, MD, FACS, disclosed he is a stockholder in Virtual Incision Corp. Dr. Armijo and other coauthors had no financial relationships to disclose.
AT SAGES 2017
Key clinical point: In inguinal and ventral hernia repair, laparoscopic surgeons are more likely than are open surgery counterparts to move to surgical robot.
Major finding: Over the 7-year study period, the share of open ventral hernia repair procedures increased from 80.9% to 85.2%, while the proportion of laparoscopic procedures fell from 18.9% to 11.9% and RAS operations increased from 0.2% to 2.9%.
Data source: Multicenter, retrospective study of 857,468 general surgery procedures from 2008 to 2015 in the University HealthSystem Consortium Clinical Database Resource Manager.
Disclosures: Dr. Armijo reported having no financial disclosures. Coauthor Dmitry Oleynikov, MD, disclosed stock holding in Virtual Incision Corp.











