An estimated 220,000 bariatric surgeries are performed annually in the United States and Canada, and 344,221 procedures worldwide.1 Not only are orthopedic surgeons seeing more patients who have had bariatric surgery, they are also referring morbidly obese patients to bariatric surgeons before elective procedures.2 Patients with body mass index (BMI) over 40 kg/m2 are candidates for surgical treatment of obesity. Comorbid conditions directly related to obesity, including diabetes, respiratory insufficiency, and pseudotumor cerebri, decrease the BMI of eligibility to 35 kg/m2. Other considerations are failure of nonsurgical weight-loss methods, such as dietary programs for weight reduction, behavioral modification programs, and pharmacotherapy. Patients’ psychological stability is extremely important given the rigorous dietary changes required after surgery.3 Although weight-loss surgery can eliminate many of the complications of obesity, bariatric patients even with weight loss have increased operative and postoperative risks, likely because of alterations in nutrient absorption. Knowledge of the pathophysiology associated with bariatric surgery can assist orthopedic surgeons in optimizing medical and surgical management of patients’ musculoskeletal issues.
Bariatric Surgery
Surgically induced weight loss works by reducing quantity of food consumed and absorption of calories. Jejunoileal bypass, one of the first procedures used, significantly decreased the absorptive area for nutrients, which led to complications such as diarrhea, cirrhosis, and nephrolithiasis.4 This surgery is no longer performed, and current procedures try to minimize the risks of malabsorption.5
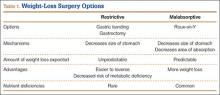
The 2 types of bariatric surgeries now available in the United States are gastroplasty and gastric bypass, both of which are performed laparoscopically.6 Gastroplasties are purely restrictive procedures, which reduce stomach volume. In gastric banding, the most common gastroplasty, a silicone band is placed around the proximal stomach to create a 15-mL pouch in the cardia. Sleeve gastrectomy also reduces stomach volume, to about 25%, by stapling along the greater curvature. In both procedures, consumed calories are restricted, but the gastrointestinal tract is left in continuity, and essential nutrients are properly absorbed.7 However, failure rates are higher, and weight loss more variable, than with gastric bypass procedures.8
Gastric bypass uses both restriction and malabsorption to increase weight loss.7 A gastric pouch (15-30 mL) is created by stapling across the cardia of the stomach. The jejunum is then divided, and the distal portion of the divided jejunum anastomosed to the small proximal stomach pouch. This creates the roux limb where food passes. The duodenum is excluded, and the proximal portion of the jejunum is attached to the roux limb to provide a conduit for biliary and pancreatic digestive secretions. Weight loss is caused by both reduction in stomach size and malabsorption of calories owing to the diversion of digestive enzymes and the decrease in absorptive surface area. Only 28% of ingested fat and 57% of ingested protein are absorbed9 (Table 1).
Metabolic Consequences
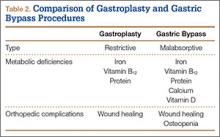
Nutrient deficiencies are seen more often in the malabsorptive procedures; however, patients with restrictive procedures may have poor eating habits and are therefore also at risk.10 In fact, many patients have nutritional deficiencies predating their bariatric surgery, as obesity creates a chronic inflammatory state that leads to anemia of chronic disease. Schweiger and colleagues11 assessed the nutritional status of bariatric surgery candidates and noted a high incidence of iron and folic acid deficiencies with corresponding anemia. They concluded these deficiencies stemmed from calorie-dense diets high in carbohydrates and fats. Although patients may improve their diet after surgery with concomitant nutritional counseling, deficiencies in iron, calcium, vitamin B12, folate, and vitamin D are common12 (Table 2).
Iron deficiency continues after bariatric surgery because dietary iron must be converted to its absorbable form by hydrochloric acid secreted from the stomach. As stomach volume is reduced, there is a corresponding decrease in acid secretion. The result is that iron deficiency occurs in both restrictive and malabsorptive procedures.13 Moreover, with the diversion from the duodenum and the proximal jejunum in bypass surgery, the main areas of absorption are excluded.10 Patients may require intravenous therapy for iron-deficiency anemia—or oral supplementation combined with ascorbic acid to increase stomach acidity.
As calcium is absorbed mainly in the duodenum and the jejunum, patients who undergo malabsorptive procedures can absorb only 20% of the amount ingested.14 Restrictive procedures do not have the same effect on calcium absorption; however, patients may have reduced dietary lactose intake and be at risk for deficiency.
A study by Ducloux and colleagues15 found that 96% of bariatric surgery patients had vitamin D deficiency before the procedure. After malabsorptive procedures, the decrease in bile salts leads to an inability to break down fat-soluble vitamins and to uncoordinated mixing of food and bile secretions.16 Restrictive procedures do not carry this risk, though many patients still require supplementation because of their underlying deficiency.